Abstract
Background:
We examined the probabilities of longitudinal care outcomes of working-aged patients with alcohol-use disorder (AUD) and their alcohol-related treatment utilisation patterns across the healthcare services, by using linked electronic health records.
Methods:
A random sample (n = 396) of patients with alcohol-related visits to healthcare services in 2011–2012 was collected retrospectively from the electronic health record data in the North Karelia region of Finland and followed prospectively in time until the end of 2016. Data on care outcomes and alcohol-related healthcare use were gathered from the electronic health records. Three outcome groups were identified: (1) dead, (2) present AUD, and (3) remission. Group differences in alcohol-related health service use were compared.
Results:
At the end of the follow-up period, an increased mortality rate of 22.9% was observed, and 18.4% had achieved stable remission, while for the majority (56%), the AUD remained. Most of those in remission had contact with either specialised AUD services or mental health services. Conversely, the majority of those who had died had no contact with specialised AUD services during the follow-up period.
Conclusions:
The electronic-health-record-based register analysis captured mainly individuals with advanced forms of AUD. An excess mortality rate and other negative health consequences were observed. Training providers to identify and treat earlier the less severe forms of AUD could have major benefit to patients and also reduce health system costs.
Keywords: alcohol-use disorder, care outcomes, electronic health records, register study, treatment utilisation
Alcohol-use disorders (AUDs) cause excess mortality, disease burden and remarkable costs to society in the form of increased healthcare costs (Graham et al., 2017; Kendler, Ohlsson, Sundquist, & Sundquist, 2016; Moos, Brennan, Schutte, & Moos, 2004; Rehm et al., 2009; Room, Babor, & Rehm, 2005; WHO, 2014a). The estimated prevalence of AUDs is 7.5% in the European region adult population and 11.8% in the primary care setting (Manthey et al., 2016; WHO, 2014a). In Finland, the prevalence of AUDs is 7% in the adult population (WHO, 2014b) and 12-month prevalence of alcohol dependence is 3.9% (Pirkola, Poikolainen, & Lönnqvist, 2006).
Although AUDs are commonly represented in social and healthcare settings (Tai, Wu, & Clark, 2012), previous studies have revealed the treatment gap for AUDs is larger than in any other mental disorder (Roerecke & Rehm, 2014) and that only a minority of individuals with AUD use alcohol-treatment services (Cohen, Feinn, Arias, & Kranzler, 2007; Grant et al., 2004; Heinälä et al., 2001; Rehm et al., 2015; Watkins, Burnam, Kung, & Paddock, 2001; Wu, Ringwalt, & Williams, 2003). In Europe, treatment rate estimates of AUD vary between 10.0 and 17.7% (Manthey et al., 2016; Rehm et al., 2016). Several reasons for the low treatment rates have been identified, including different barriers to AUD care, such as social stigma and problem awareness (Grant, 1997; Keyes et al., 2010; Probst, Manthey, Martinez, & Rehm, 2015), challenges in the identification of AUDs in healthcare settings (Manthey et al., 2016; Rehm et al., 2016) and unavailability of services (Saunders, Zygowicz, & D’Angelo, 2006), which are all causing delays in treatment initiation (Kessler et al., 2001; Kessler, Olfson, & Berglund, 1998). Long-term recovery rates in treated populations vary between 20 and 50% (Anglin, Hser, & Grella, 1997; Dennis, Scott, Funk, & Foss, 2005; Vaillant, 2003), while the mortality risk associated with AUD is 3.38 for men and 4.57 for women, in clinical samples (Roerecke & Rehm, 2013). Furthermore, people with AUD have approximately 24–28 years shorter life expectancy compared with the general population (Westman et al., 2015).
As AUDs are chronic relapsing disorders (Dennis & Scott, 2007; Hser, Anglin, Grella, Longshore, & Prendergast, 1997; McLellan, McKay, Forman, Cacciola, & Kemp, 2005), often with co-occurring mental health (MH) problems and varying treatment careers with several treatment episodes (Chi & Weisner, 2008; Kessler et al., 1996; Timko, Moos, Finney, Moos, & Kaplowitz, 1999), an extensive follow-up period is required to identify alcohol-related treatment utilisation profiles and care outcomes (Anglin et al., 1997). A plethora of literature exists on factors associated with long-term care outcomes (Cohen et al., 2007; Krenek, Prince, & Maisto, 2017; Laudet, Savage, & Mahmood, 2002; Trim, Schuckit, & Smith, 2013; Vaillant, 2003). However, knowledge of the care outcomes regarding previous longitudinal alcohol-related treatment utilisation profiles across health services of patients with AUD is limited.
Prior studies on alcohol-related treatment utilisation profiles of those accessing treatment have identified that the majority of alcohol-dependent individuals have previously been in short-term inpatient treatment, one-third in long-term residential care and approximately 20% in detoxification (Anglin et al., 1997). Cohen et al. (2007) noted that around half of individuals with an alcohol abuse or dependence diagnosis received alcohol or drug rehabilitation and 38.4% received alcohol or drug detoxification. A previous study in Finland identified that only 35.5% of alcohol dependent individuals had previous treatment contact (Heinälä et al., 2001). In addition, Edlund, Booth, and Han (2012) assessed patterns and predictors of AUD and MH treatment use among individuals with AUDs and identified MH treatment as the more common treatment option. Additionally, substance-use disorder treatment has been associated with marked reductions in substance use and costs to society (Salomé, French, Scott, Foss, & Dennis, 2003).
In this article, we examine the possibilities of using electronic health records (EHRs) to estimate the probabilities of longitudinal care outcomes of AUD patients and their alcohol-related treatment utilisation patterns across the healthcare services. Electronic health records contain a remarkable amount of information on health and health-service use that can increase our understanding of AUD and MH treatment utilisation patterns and care outcomes of patients with AUDs (Bell et al., 2017; Lid, Eide, Dalen, & Meland, 2016; Tai et al., 2012; Wu et al., 2015). In Finland, primary healthcare EHR registers have not been used comprehensively in the previous register studies.
Thus, this register-based prospective cohort study (n = 396) aimed to estimate the probability of different care outcomes, including (1) death, (2) present AUD, and (3) AUD in remission. The alcohol-related treatment utilisation profiles of these outcome groups are described during a 6-year follow-up, by using manually evaluated linked primary and secondary care EHRs.
Materials and methods
Data source and treatment system
The EHR data were collected in the North Karelia region of Eastern Finland, for the years 2011–2016. The study was approved by the Research Ethics Committee of the Northern Savo Hospital District; consent was not obtained, as the study was based on registry information. North Karelia comprises 13 municipalities and has approximately 165,000 inhabitants. The same structured EHR system is used across the region in both primary and specialised care, as well as in specialised addiction services. In Finland, the social and health service system is decentralised and, currently, municipalities are responsible for organising social and healthcare services, including alcohol and drug treatment. The Welfare for Substance Abusers Act (41/1986) regulates addiction as well as MH services, and provision of these services can be organised as part of the primary healthcare services or as specialised addiction services, providing treatment for substance use disorders, including AUDs.
Study sample
The study sample was formed retrospectively, based on the medical diagnoses (ICD-10 codes) in the EHR register; all the individuals with at least one alcohol-related visit (i.e., having an alcohol-related diagnosis as the main diagnosis or side diagnosis) in primary or specialised care between the years 2011–2012 were identified (n = 6246). Alcohol-related visits included the following ICD-10 codes: G312, G405, G4050, G4051, G4052, G621, I426, K292, F100, F101, F102, F103, F104, F105, F106, F108, F109, K860, K700, K701, K702, K703, K704, K709, T510, T511, T512, T513, T518, T519, X45, and X69. A broad set of alcohol-related diagnoses was used in the sampling, as previous studies have identified under diagnosing and under-recording of AUD diagnoses (Abidi, Oenema, van den Akker, & van de Mheen, 2018; Mitchell, Meader, Bird, & Rizzo, 2012). After excluding the residents of municipalities outside North Karelia, 5778 individuals remained. The number of the working aged (18–65 years) subjects was 3935 (approximately 4.1% of the working-age population of North Karelia), from which a random cohort of 396 individuals was formed for detailed examination of EHRs. The cohort was followed prospectively in time for 6 years, from January 2011 until December 2016.
Measures
Alcohol-use disorders were defined to include alcohol abuse/harmful use and alcohol dependence, based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) and International Statistical Classification of Disease (ICD-10). All study subjects filled this definition at the baseline.
The data were divided into three mutually exclusive categories, according to the outcome status at the end of the follow-up period: (1) dead, (2) present AUD, and (3) AUD in remission. Data on outcome variables were manually collected from the EHR notes, except the date of death, which was automatically linked to the EHR from the population register centre. Based on the AUD definition, present AUD was defined as having alcohol-related visits (ICD-10 code F10 as main diagnosis) and health professionals’ mentions of harmful use of alcohol or alcohol dependence in the EHR notes in each year of the follow-up period. Remission was defined as sustained abstinence or managed use, and short abstinence periods (max. few months) were excluded. Assessment of the time estimate in AUD remission was based on health professionals’ notes and diagnosis information, i.e., the notes systematically identified the patient as abstinent or managing their alcohol use and time estimate of the remission/managed use was given or the patient had ICD-10 diagnosis code F1020–F1023 indicating sustained remission. Furthermore, in case of mixed reviews between the health professionals’ notes, the patient was assessed as having present AUD. Patients with no comments on alcohol status due to lack of yearly visits were excluded (n = 11), as it would not have been possible to reliably estimate their outcome status.
Data on baseline measures (age, gender, permanent alcohol diagnosis or another permanent mental health diagnosis) and contact with specialised AUD services and MH services were collected from the routinely compiled EHR statistics. In the EHR, permanent diagnosis is used for chronic or long-term diseases that are considered to affect the care of the patient for a long time-period. These diagnoses remain in the EHR even after the disease is cured. Permanent alcohol diagnosis was defined as ICD-10 codes F100, F101, F102, F103, F104, F105, F106, F108, or F109 (mental and behavioural disorders due to use of alcohol) and permanent MH diagnosis as ICD-10 codes F00–F99 (mental and behavioural disorders), excluding F10 codes.
Study participants were profiled according to the patterns of alcohol-related service use, based on the information in the structured EHR notes. First, all notes mentioning alcohol use for the years 2011–2016 were manually collected and classified. Patients were assigned into three groups according to their health-service use patterns: (1) only mental health contact, (2) specialised AUD service contact, and (3) no specialised AUD contact. Alcohol-related health service contacts were then further classified into mutually exclusive groups according to contact type (primary or specialised care, etc.), to identify the alcohol-related service-use profile.
Statistical analysis
IBM SPSS Modeler version 18.0 was used to derive the health-service use variables from the EHR data, and IBM SPSS Statistics 24 was used in the statistical analyses. Descriptive statistics were used to compare the background variables, specialised AUD service use and MH service use of the outcome groups. Specialised AUD service use and MH service use were measured as a yearly mean number of visits, by considering the eligibility time of the study subjects; eligibility time was calculated within 6 months’ accuracy for each person, and the yearly mean number of visits was divided by the eligibility time, in order to compare the outcome groups. For those with present AUD the follow-up time was 6 years, whereas for those who died or achieved remission, the follow-up time varied from 6 months to 6 years. The χ2, Fischer’s exact and Kruskal–Wallis tests were used for the group comparisons.
Results
Characteristics of the cohort
The baseline characteristics of the cohort, according to the outcome status, are described in Table 1. The mean age was 47.5 years, and the proportion of women was 25%. The majority (68.2%) had received income support during the follow-up period. Permanent AUD diagnosis was recorded for 32.3%, and prevalence of other permanent MH diagnoses was 22%. In addition, only 9.8% of the study participants had co-morbid AUD and MH diagnosis recorded as a permanent diagnosis.
Table 1.
Baseline patient characteristics.
| Outcome 2016 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Present AUD (n = 228) | Dead (n = 93) |
Remission (n = 75) | Total (n = 396) | Kruskall- Wallis (CI 95%) | ||||||
| n | % | n | % | n | % | n | % | p | ||
| Age at baseline | 0.570a | < 0.001 p,d* | ||||||||
| 18–24 years | 12 | 5.3 | 1 | 1.1 | 3 | 4.0 | 16 | 4.0 | ||
| 25–34 years | 28 | 12.3 | 7 | 7.5 | 9 | 12.0 | 44 | 11.1 | ||
| 35–44 years | 45 | 19.7 | 12 | 12.9 | 12 | 16.0 | 69 | 17.4 | ||
| 45–54 years | 89 | 39.0 | 33 | 35.5 | 26 | 34.7 | 148 | 37.4 | ||
| 55–64 years | 54 | 23.7 | 40 | 43.0 | 25 | 33.3 | 119 | 30.1 | ||
| Gender | ||||||||||
| Male | 165 | 72.4 | 75 | 80.6 | 55 | 73.3 | 295 | 74.5 | 0.294a | |
| Female | 63 | 27.6 | 18 | 19.4 | 20 | 26.7 | 101 | 25.5 | ||
| Permanent Dg F10 | < 0.001a | < 0.001 r,p* | ||||||||
| Yes | 89 | 39.0 | 26 | 27.9 | 13 | 17.3 | 128 | 32.3 | ||
| No | 139 | 61.0 | 67 | 72.0 | 62 | 82.7 | 268 | 67.7 | ||
| Permanent Dg F (excl. F10) | < 0.050a | < 0.050 p,d* | ||||||||
| Yes | 55 | 24.1 | 11 | 11.8 | 21 | 28.0 | 87 | 22.0 | < 0.050 d,r* | |
| No | 173 | 75.9 | 82 | 88.2 | 54 | 72.0 | 309 | 78.0 | ||
| Income support | 0.068a | |||||||||
| Yes | 163 | 71.5 | 59 | 63.4 | 48 | 64.0 | 270 | 68.2 | ||
| No | 53 | 23.3 | 33 | 35.5 | 26 | 34.7 | 112 | 28.3 | ||
| Missing | 12 | 5.2 | 1 | 1.1 | 1 | 1.3 | 14 | 3.5 | ||
| Contacts with AUD services | < 0.001a | < 0.001 p,d* | ||||||||
| 0 | 70 | 30.7 | 54 | 58.1 | 40 | 53.3 | 164 | 41.4 | ||
| < 1 | 45 | 19.7 | 12 | 12.9 | 4 | 5.3 | 61 | 15.4 | ||
| 1.0–2.9 | 47 | 20.6 | 12 | 12.9 | 12 | 16.0 | 71 | 17.9 | ||
| 3.0–9.9 | 49 | 21.5 | 8 | 8.6 | 10 | 13.3 | 67 | 16.9 | ||
| 10.0+ | 17 | 7.5 | 7 | 7.5 | 9 | 12.0 | 33 | 8.3 | ||
| Contacts with MH services | < 0.001a | < 0.001 d,r* | ||||||||
| 0 | 128 | 56.1 | 65 | 69.9 | 32 | 42.7 | 225 | 56.8 | < 0.010 p,r* | |
| < 1 | 52 | 22.8 | 8 | 8.6 | 13 | 17.3 | 73 | 18.4 | ||
| 1.0–2.9 | 29 | 12.7 | 9 | 9.7 | 12 | 16.0 | 50 | 12.6 | ||
| 3.0–9.9 | 12 | 5.3 | 7 | 7.5 | 6 | 8.0 | 25 | 6.3 | ||
| 10.0+ | 7 | 3.1 | 4 | 4.3 | 12 | 16.0 | 23 | 5.8 | ||
AUD = alcohol-use disorder; Dg F = ICD-10 codes F00-F99 (mental and behavioural disorders), excl. F10; MH = mental health.
a Pearson chi-square.
*Kruskall–Wallis pairwise comparisons: p = present AUD problem; d = dead; r = remission.
Outcome status
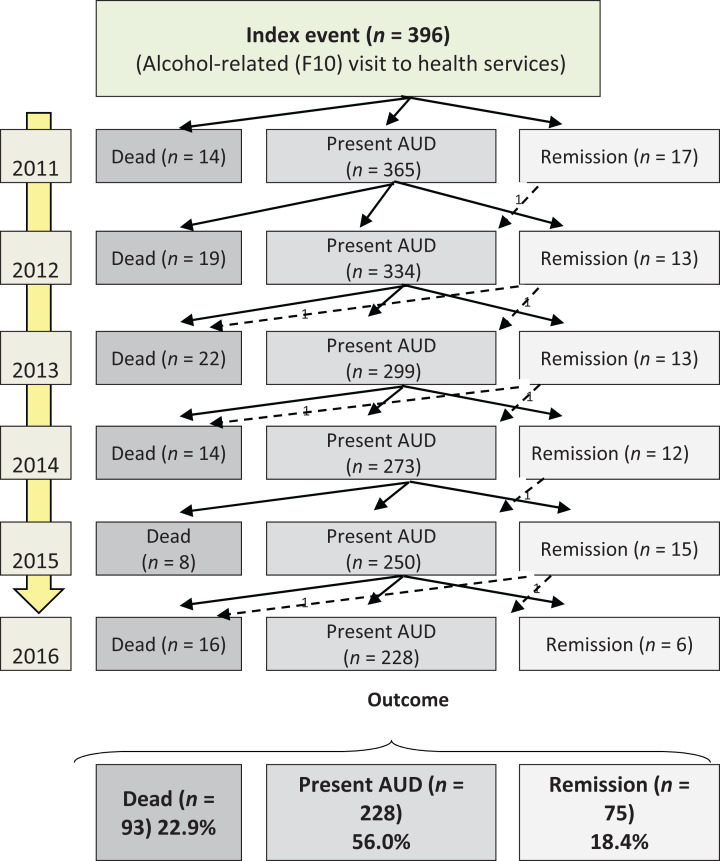
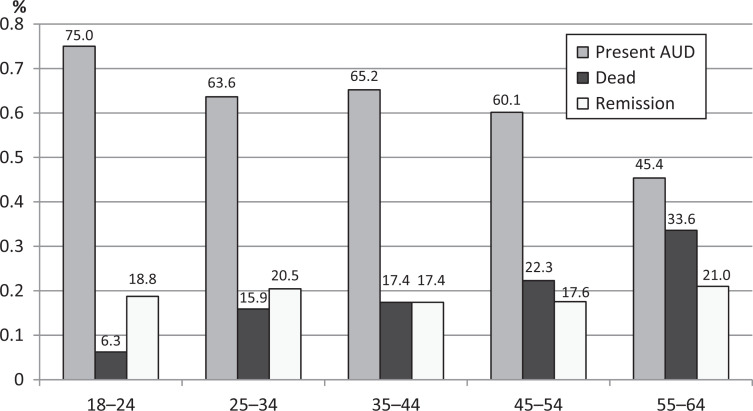
A flow-chart of the outcome events is presented in Figure 1. A mortality rate of 22.9% was observed at the end of the follow-up, and the remission rate was 18.4%. The most prevalent outcome was present AUD (56%). Seven individuals experienced a short relapse after at least 1 year of abstinence. The cumulative outcome, according to the age groups, is presented in Figure 2.
Figure 1.
Flow-chart of outcome events during the follow-up.
AUD = alcohol-use disorder.
Figure 2.
Proportion of outcome status by age group.
AUD = alcohol-use disorder.
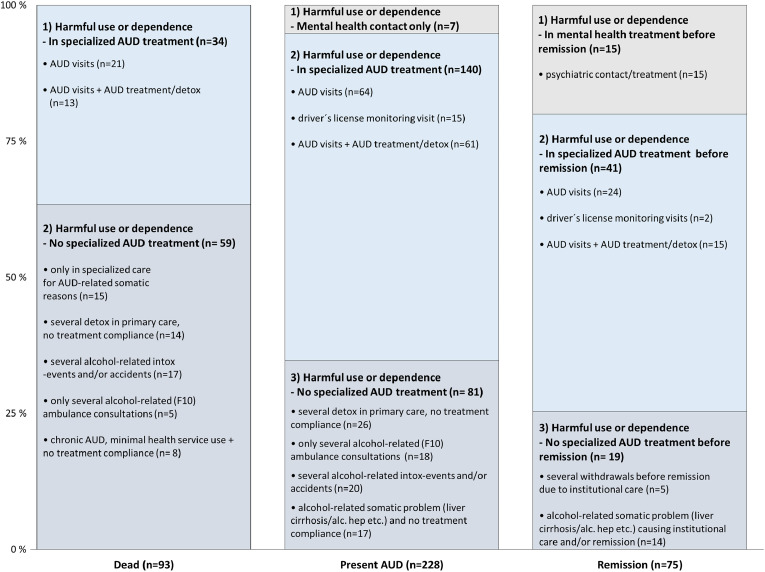
Patterns of alcohol-related service utilisation
Figure 3 shows the description of the alcohol-related health-service use patterns of the outcome groups. Alcohol-related health-service contacts were classified into mutually exclusive groups according to most prevalent contact type, to identify the alcohol-related service-use profile. All study participants filled the definition of AUD, and were described in the health professionals’ notes as either alcohol abusers/harmful users, with mentions of somatic or mental harm caused by alcohol, or being alcohol dependent with varying treatment careers. Particular patterns of service use were observed; for instance, only 39.8% of those who had died had used specialised AUD services, i.e., having either visits to physician and/or nurse (n = 21) or having additionally received detoxification and/or rehabilitation (n = 13). Notably, the majority (58.1%) of the dead had not used specialised AUD services during the follow-up period. Instead, their alcohol-related visits occurred mainly in (1) specialized care due to alcohol-related somatic complication (n = 15), while some had (2) several detoxification treatments in primary care but no compliance with treatment (n = 14), whereas others were characterised as (3) having recurrent intoxications and accidents (n = 17), and few had (4) several ambulance consultations due to alcohol-related issues but no actual treatment contact (n = 5), and some were (5) diagnosed with chronic alcoholism but had no compliance with treatment and minimal health-service utilisation (n = 8).
Figure 3.
Description of the patterns of alcohol-related service use according to outcome group.
AUD = alcohol-use disorder.
Examination of the characteristics of those with present AUD at the end of the follow-up period (n = 228) revealed that 61.4% of the present AUD problem group had received treatment in specialised AUD services. This treatment was in the form of (1) visits to AUD physician/nurse/social worker (n = 64), (2) additionally receiving detoxification and/or AUD rehabilitation (n = 61), or (3) were ordered into driver’s license monitoring due to drunk driving (n = 15). Approximately one-third of the patients in the present AUD problem group had not received treatment in specialised AUD services, although they had repeated mentions of alcohol abuse/harmful use in the EHRs. Instead, they had (1) several withdrawals in primary care setting and had no commitment to any AUD treatment (n = 26), (2) several ambulance consultations for alcohol-related reasons (n = 18), which did not result in referral to treatment, (3) experienced recurrent alcohol-related intoxications and/or accidents (n = 20), or had been (4) diagnosed with liver cirrhosis or other chronic alcohol-related somatic disorder but had no compliance with any treatment (n = 17).
In contrast, most of those achieving remission were using either specialised AUD services or received care for MH reasons, and their AUD was treated simultaneously. Notably, approximately one-third of those in remission had not used specialised AUD services before achieving remission but were institutionalised (i.e., located in long-term in-patient treatment, sheltered housing etc.) (n = 5) or had severe somatic health problems that forced abstinence (n = 14).
Specialised AUD service and MH service contact according to the outcome groups
Table 2 presents the proportions of individuals having contact with either specialised AUD services, MH services or both. Slight differences in numbers compared with Figure 3 are explained by the differences in interpretation; those study subjects having merely cancelled and missed specialised AUD service visits (i.e., visits where the appointment time was not used, as the study participant did not show up) were interpreted as not having contact with the service in question in Figure 3, whereas, in Table 2, the numbers are from the EHR registers. The number of visits may, therefore, appear exaggeratedly optimistic in the EHR, as the cancelled and missed visits are occasionally erroneously registered as actual visits. In addition, in the remission group, six individuals had specialised AUD nurse contact in primary care, but these visits in the EHRs were classified as regular primary healthcare visits.
Table 2.
Electronic health record (EHR) register information on specialised alcohol-use disorder (AUD) contact and mental health (MH) service contact according to outcome groups.
| Present AUD (n = 228) | Dead (n = 93) | Remission (n = 75) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mental-health contact | Mental-health contact | Mental-health contact | |||||||
| AUD service contact | No | Yes | Total | No | Yes | Total | No | Yes | Total |
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |
| No | 52 (22.8) | 18 (7.9) | 70 (30.7) | 40 (43.0) | 14 (15.1) | 54 (58.1) | 21 (28.0) | 19 (25.3) | 40 (53.3) |
| Yes | 76 (33.3) | 82 (35.9) | 158 (69.3) | 25 (26.9) | 14 (15.1) | 39 (41.9) | 11 (14.7) | 24 (32.0) | 35 (46.7) |
| Total | 128 (56.1) | 100 (43.9) | 228 (100.0) | 65 (69.9) | 28 (30.1) | 93 (100.0) | 32 (42.7) | 43 (57.3) | 75 (100.0) |
Discussion
This study had two aims. First, to examine the probabilities of death and remission of individuals with AUD and, second, to profile their alcohol-related health-service utilisation across the health-service system, by using data from the EHRs. We observed high mortality rate, relatively low AUD remission rate and highly fragmented AUD treatment utilisation patterns. Only one-quarter of the study participants had regular contact with specialised AUD services, i.e., three or more visits per year. Underutilisation of AUD services was prevalent, especially among those who later died. Moreover, under-diagnosis of AUD was identified, possibly indicating under-treatment of individuals with AUDs accessing health services.
A total of 3935 working-aged individuals with alcohol-related visits to health services in 2011–2012 were detected from the EHR, corresponding to approximately 4.1% of the working-age population of North Karelia. This proportion is less than the national prevalence of AUDs, which is about 7% of the adult population in Finland. Thus, these numbers reflect the current challenges to use alcohol-related diagnoses for less advanced AUDs, as has been noted in previous studies by Mitchell et al. (2012) and Abidi et al. (2018). We used a broad set of alcohol-related diagnoses in the sampling, as focusing only on F10 codes (ICD-10) would potentially have biased the sampling to those already in AUD treatment. A random sample from the EHR mostly captured individuals receiving income support and having an advanced form of AUD described in their EHR records, possibly indicating a somewhat deprived background. It is known that individuals accessing treatment tend to have more severe AUD (Rehm et al., 2015), and that people with lower socioeconomic status experience greater alcohol-related consequences (Collins, 2016). Therefore, it is considered important to examine how the current social and healthcare system can address the care needs of those with a deprived background, regarding the AUD treatment.
After the 6-year follow-up, the following distribution of care outcomes was observed: over one-fifth of the study participants had died, and 18.4% were in remission, whereas the majority were still classified in the present AUD group. The increased probability of death concurs with the findings of previous studies (Kendler et al., 2016; Laramée et al., 2015; Roerecke & Rehm, 2013; Westman et al., 2015). However, the observed death rate was notably higher compared with a previous Finnish population study, in which 8.8% of individuals with AUD died after an 8-year follow-up period (Markkula et al., 2012). This difference may at least partly be explained by the different characteristics of the cohorts, as individuals with heavy alcohol use are unlikely to respond to population surveys. The proportion of individuals in remission corroborated the results described by Dawson et al. (2005). In that study, 18.2% of patients with previous alcohol dependence became abstainers, while the remission rate in our study remained low compared with general estimates of long-term recovery rates of 20–50% in treated populations (Anglin et al., 1997; Dennis et al., 2005; Vaillant, 2003). Notably, one-quarter of the remissions resulted from institutionalisation. In our study, remission rate also remained stable across age groups. This finding contradicts those of previous studies identifying that remission rate increases with age and varies across age groups (Bland, Newman, & Orn, 1997; Pirkola et al., 2006). All this may reflect the severity of the AUD in our study cohort. The large proportion of individuals with present AUD demonstrates the persistent nature of AUD, as previously noted in work conducted by Grella, Stein, Weisner, Chi, and Moos (2010).
Although the study participants were described in the EHR notes as heavy drinkers with a history of severe AUD, permanent AUD diagnosis was recorded for only 32.3% of the study participants and the prevalence of other permanent MH diagnoses was 22%. Also, just 9.8% of the study participants had co-morbid AUD and MH diagnosis recorded as a permanent diagnosis. These rates were lower than expected, raising a question of possible under-diagnosing and inadequate practices to record permanent diagnoses, as earlier studies have identified that most individuals with AUD who access treatment have higher levels of co-occurring MH and other co-morbidities (Flensborg-Madsen, Mortensen, Knop, Becker, & Gronbaek, 2009; Rehm et al., 2015). For instance, Kuussaari and Hirschovits-Gerz (2016) determined a 50% prevalence of co-occurring MH and substance-use-related problems, and a Swedish study estimated a 50–75% co-morbidity prevalence in an addiction-treatment population (Lundgren et al., 2014).
The EHR-based register analysis of alcohol-related health-service use patterns during the 6-year period revealed significant differences among the outcome groups. The majority of those who had died had not used specialised AUD services. Instead, they had made alcohol-related visits to specialised care, due to severe alcohol-related somatic complications or they had several intoxications, accidents and detoxifications in primary care, but active treatment attempts seemed to be lacking. Then there were those with alcohol-related ambulance consultations and minimal health-service use, and mention of low compliance with treatment was often recorded in their EHR notes, indicating a total drop-out from the service system. Respectively, in the present AUD group, the majority received help for their AUD, although approximately only one-third had somewhat regular contact with AUD services, having a yearly mean number of three or more visits to specialised AUD services. Individuals achieving stable remission differed from the other outcome groups regarding the use of MH services. Mental health service use was most common among those in remission, even though no differences in the permanent MH diagnosis prevalence between those in remission and the present AUD group were observed. This finding agrees with the literature, identifying an association between the use of MH services and better addiction treatment outcomes (McLellan et al., 1996; Moos, Finney, Federman, & Suchinsky, 2000; Ray, Weisner, & Mertens, 2005).
Limitations
The 6-year follow-up can only capture a certain period of the AUD treatment career, which should be noted when interpreting the results. Besides, despite the random selection of study subjects from the EHR registers, this research represents mostly individuals with an advanced-stage AUD and, naturally, the results are representative only in the North Karelia district. Although it is known that those with more severe AUD typically enter treatment, we were, nonetheless, expecting to find also those with less advanced AUD and emerging alcohol-related harms. This finding may indicate that the threshold for physicians to set an alcohol-related diagnosis is rather high.
In future research, other sampling methods should be considered to complement the ICD-10 diagnosis based sampling to identify patient cohorts with less advanced AUD from the EHRs. Text mining methods could provide useful tools to detect the presence of AUD.
The following issues arose during the analysis that should be addressed: (1) The data were available only for the years 2011–2016 as the EHR was established in 2010 and has been fully in use since 2011. Thereby, we were not able to estimate prior service contacts. Also, those who died had less time to use specialised AUD services as those in other outcome groups. Although, we estimated that it would have been likely that treatment contacts would have been mentioned in the EHR even if the person died earlier, as the cohort included individuals with advanced forms of AUD. (2) Some errors in the number of registered AUD visits were detected; the appointed time was not always used, although these missed visits were registered as visits in the EHR registers, which led to exaggerated numbers for specialised AUD service utilisation if the service use was assessed only based on the register data. (3) The thorough examination of EHR notes revealed that alcohol-related diagnosis was not always recorded, although the patient was described as being intoxicated, raising a question as to whether only individuals with severe forms of AUD in the first place have alcohol-related diagnosis marked as a secondary diagnosis for the visits.
In this study, it was not possible to examine the duration of the AUD or whether the AUD was caused by MH problems or vice versa. Additionally, assessment of the AUD status was based on the clinicians’ estimates. Furthermore, only one study subject had a score for the alcohol-use disorder identification test (AUDIT) recorded in the structured EHR, although references to AUDIT scores appeared in some of the notes indicating that AUDIT has been conducted but not recorded in a structured manner. Therefore, structured comparisons were not possible. Lastly, this study was not able to assess private health-service use or occupational health-service use provided by private service providers, as they use different EHR systems, though the proportion of these services was assessed as low, as only two private providers existed in one of the 13 municipalities and municipal health services provided the occupational health services in majority of the municipalities. In the future, a more detailed examination of alcohol-related social and health-service use across the treatment system could potentially identify factors associated with different care outcomes. Furthermore, examination of geographical and socioeconomic equality in access to and use of care could provide important insights into AUD treatment research.
Conclusions
Identification of AUD patients from the EHRs, based on the ICD-10 diagnosis information, mainly captures individuals with advanced forms of AUD, indicating that diagnosis of AUD is given only when the disease has reached an advanced state. The outcomes of the follow-up period reflected the serious and negative health consequences of an advanced AUD; a high mortality rate was observed, but also institutional care, detoxifications and alcohol-related somatic problems were common. Only a minority of those who had died had used specialised AUD services during the 6-year follow-up. Moreover, continuity of the specialised AUD service use varied: those achieving remission had higher AUD service utilisation rates and more visits to MH services, and vice versa. The observed advanced state of AUDs in this cohort, the low number of permanent AUD diagnoses and the relatively low frequency of AUD service contacts, especially among those who had died, raise questions of care quality and functionality of the current AUD treatment system. Training service providers to identify and treat earlier the less severe forms of AUD, combined with active treatment guidance and integrated care would most likely benefit this patient group and also reduce health-system costs. One effective way to enhance identification of AUD is the use of three first questions of the AUDIT test, as suggested in the Finnish Current Care Guidelines (2015). These findings may serve as a description of the present state of AUD treatment in one region of Finland, and inform the decision makers regarding the development of addiction service delivery systems in the forthcoming social and healthcare reform.
Acknowledgements
We wish to thank research assistant Laura Kekäläinen for valuable help with the data collection, and senior data analyst Antti Rautiainen for SPSS Modeler training.
Footnotes
Author’s contributors: All the authors participated in planning and designing this study. E. Rautiainen performed all data management and analysis and drafted the article. T. Laatikainen and O.-P. Ryynänen critically reviewed the document. All authors contributed to and have approved the final manuscript.
Declaration of conflicting interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Elina Rautiainen was supported by the Finnish Foundation for Alcohol Studies and by the University of Eastern Finland graduate school. This study also received funding from the Strategic Research Council at the Academy of Finland (consortium 312703).
Contributor Information
Elina Rautiainen, University of Eastern Finland, Finland.
Olli-Pekka Ryynänen, University of Eastern Finland, Finland; Kuopio University Hospital, Finland.
Tiina Laatikainen, University of Eastern Finland, Finland; National Institute for Health and Welfare, Finland; Joint Municipal Authority for North Karelia Social and Health Services, Finland.
References
- Abidi L., Oenema A., van der Akker M., van de Mheen D. (2018). Do general practitioners record alcohol abuse in the electronic medical records? A comparison of survey and medical record data. Current Medical Research and Opinion, 34, 567–572. [DOI] [PubMed] [Google Scholar]
- Anglin M. D., Hser Y.-I., Grella C. E. (1997). Drug addiction and treatment careers among clients in the Drug Abuse Treatment Outcome Study (DATOS). Psychology of Addictive Behaviors, 11, 308–323. [Google Scholar]
- Bell S. Daskalopoulou M. Rapsomaniki E. George J. Britton A. Bobak M.…Hemingway H. (2017). Association between clinically recorded alcohol consumption and initial presentation of 12 cardiovascular diseases: Population based cohort study using linked health records. BMJ, 356, j909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland R., Newman S., Orn H. (1997). Age and remission of psychiatric disorders. Canadian Journal of Psychiatry, 42, 722–729. [DOI] [PubMed] [Google Scholar]
- Chi F. W., Weisner C. M. (2008). Nine-year psychiatric trajectories and substance use outcomes: An application of the group-based modeling approach. Evaluation Review, 32, 39–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen E., Feinn R., Arias A., Kranzler H. R. (2007). Alcohol treatment utilization: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence, 86, 214–221. [DOI] [PubMed] [Google Scholar]
- Collins S. E. (2016). Associations between socioeconomic factors and alcohol outcomes. Alcohol Research, 38, 83–94. [PMC free article] [PubMed] [Google Scholar]
- Dawson D. A., Grant B. F., Stinson F. S., Chou P. S., Huang B., Ruan W. J. (2005). Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction, 100, 281–292. [DOI] [PubMed] [Google Scholar]
- Dennis M., Scott C. (2007). Managing addiction as a chronic condition. Addiction Science & Clinical Practice, 46, 45–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M. L., Scott C. K., Funk R., Foss M. A. (2005). The duration and correlates of addiction and treatment careers. Journal of Substance Abuse Treatment, 28, S51–S62. [DOI] [PubMed] [Google Scholar]
- Edlund M. J., Booth B. M., Han X. (2012). Who seeks care where? Utilization of mental health and substance disorder treatment in two national samples of individuals with alcohol use disorders. Journal of Studies on Alcohol and Drugs, 73, 635–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finnish Current Care Guidelines. (2015). Alkoholiongelmaisen hoito. Lisätietoa. Alkoholinkäytön ongelmakäytön määritelmät ja diagnoosit [Treatment of alcohol abuse. Additional information. Definitions and diagnoses of problematic alcohol use] Current Care Guidelines. Working group appointed by the Finnish Medical society Duodecim and the Finnish Society of Addiction Medicine. Helsinki, Finland: The Finnish Medical Society Duodecim; Retrieved from http://www.kaypahoito.fi/web/kh/suositukset/suositus?id=nix00353 [Google Scholar]
- Flensborg-Madsen T., Mortensen E., Knop J., Becker U., Gronbaek M. (2009). Comorbidity and temporal ordering of alcohol use disorders and other psychiatric disorders: Results from a Danish register-based study. Comprehensive Psychiatry, 50, 307–314. [DOI] [PubMed] [Google Scholar]
- Graham K., Cheng J., Bernards S., Wells S., Rehm J., Kurdyak P. (2017). How much do mental health and substance use/addiction affect use of general medical services? Extent of use, reasons for use, and associated costs? Canadian Journal of Psychiatry, 62, 48–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant B. F. (1997). Barriers to alcoholism treatment: Reasons for not seeking treatment in a general population sample. Journal of Studies on Alcohol, 58, 365–371. [DOI] [PubMed] [Google Scholar]
- Grant B. F., Dawson D. A., Stinson F. S., Chou S. P., Dufour M. C., Pickering R. P. (2004). The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug and Alcohol Dependence, 74, 223–234. [DOI] [PubMed] [Google Scholar]
- Grella C. E., Stein J. A., Weisner C., Chi F., Moos R. (2010). Predictors of longitudinal substance use and mental health outcomes for patients in two integrated service delivery systems. Drug and Alcohol Dependence, 110, 92–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinälä P., Alho H., Kiianmaa K., Lönnqvist J., Kuoppasalmi K., Sinclair J. (2001). Targeted use of naltrexone without prior detoxification in the treatment of alcohol dependence: A factorial double-blind, placebo-controlled trial. Journal of Clinical Psychopharmacology, 21, 287–292. [DOI] [PubMed] [Google Scholar]
- Hser Y.-I., Anglin M. D., Grella C., Longshore D., Prendergast M. L. (1997). Drug treatment careers: A Conceptual framework and existing research findings. Journal of Substance Abuse Treatment, 14, 543–558. [DOI] [PubMed] [Google Scholar]
- Kendler K. S., Ohlsson H., Sundquist J., Sundquist K. (2016). Alcohol use disorder and mortality across the lifespan: A longitudinal cohort and co-relative analysis. JAMA Psychiatry, 73, 575–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R. C. Aguilar-Gaxiola S. Berglund P. A. Caraveo-Anduaga J. J. DeWit D. J. Greenfield S. F.…Vega W. A. (2001). Patterns and predictors of treatment seeking after onset of a substance use disorder. Archives of General Psychiatry, 58, 1065–1071. [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Nelson C. B., McGonagle K. A., Edlund M. J., Frank R. G., Leaf P. J. (1996). The epidemiology of co-occurring addictive and mental disorders: Implications for prevention and service utilization. American Journal of Orthopsychiatry, 66, 17–31. [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Olfson M., Berglund P. A. (1998). Patterns and predictors of treatment contact after first onset of psychiatric disorders. American Journal of Psychiatry, 155, 62–69. [DOI] [PubMed] [Google Scholar]
- Keyes K. M., Hatzenbuehler M. L., McLaughlin K. A., Link B., Olfson M., Grant B. F., Hasin D. (2010). Stigma and treatment for alcohol disorders in the United States. American Journal of Epidemiology, 172, 1364–1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krenek M., Prince M. A., Maisto S. A. (2017). Life events and alcohol use disorder clinical course: Modeling the dynamic association. Drug and Alcohol Dependence, 180, 137–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuussaari K., Hirschovits-Gerz T. (2016). Co-occurrence of substance use related and mental health problems in the Finnish social and health care system. Scandinavian Journal of Public Health, 44, 202–208. [DOI] [PubMed] [Google Scholar]
- Laramée P., Leonard S., Buchanan-Hughes A., Warnakula S., Daeppen J.-B., Rehm J. (2015). Risk of all-cause mortality in alcohol-dependent individuals: A systematic literature review and meta-analysis. EBioMedicine, 2, 1394–1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet A. B., Savage R., Mahmood D. (2002). Pathways to long-term recovery: A preliminary investigation. Journal of Psychoactive Drugs, 34, 305–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lid T. G., Eide G. E., Dalen I., Meland E. (2016). Can routine information from electronic patient records predict a future diagnosis of alcohol use disorder? Scandinavian Journal of Primary Health Care, 34, 215–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundgren L., Wilkey C., Chassler D., Sandlund M., Armelius B.-Å., Armelius K., Brännström J. (2014). Integrating addiction and mental health treatment within a national addiction treatment system: Using multiple statistical methods to analyze client and interviewer assessment of co-occurring mental health problems. Nordic Studies on Alcohol and Drugs, 31, 59–79. [Google Scholar]
- Manthey J. Gual A. Jakubczyk A. Pieper L. Probst C. Struzzo P.…Rehm J. (2016). Alcohol use disorders in Europe: A comparison of general population and primary health care prevalence rates. Journal of Substance Use, 21, 478–484. [Google Scholar]
- Markkula N. Härkänen T. Perälä J. Partti K. Peña S. Koskinen S.…Saarni S.I. (2012). Mortality in people with depressive, anxiety and alcohol use disorders in Finland. British Journal of Psychiatry, 200, 143–149. [DOI] [PubMed] [Google Scholar]
- McLellan A. T., McKay J. R., Forman R., Cacciola C., Kemp J. (2005). Reconsidering the evaluation of addiction treatment: From retrospective follow-up to concurrent recovery monitoring. Addiction, 100, 447–458. [DOI] [PubMed] [Google Scholar]
- McLellan A. T., Woody G. E., Metzger D., McKay J., Durrell J., Alterman A. I., O’Brien C. P. (1996). Evaluating the effectiveness of addiction treatments: Reasonable expectations, appropriate comparisons. The Milbank Quarterly, 74, 51–85. [PubMed] [Google Scholar]
- Mitchell A. J., Meader N., Bird V., Rizzo M. (2012). Clinical recognition and recording of alcohol disorders by clinicians in primary and secondary care: Meta-analysis. The British Journal of Psychiatry, 201, 93–100. [DOI] [PubMed] [Google Scholar]
- Moos R. H., Brennan P. L., Schutte K. K., Moos B. S. (2004). High-risk alcohol consumption and late-life alcohol use problems. American Journal of Public Health, 94, 1985–1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos R. H., Finney J. W., Federman E. B., Suchinsky R. (2000). Specialty mental health care improves patient’s outcomes: Findings from a nationwide program to monitor the quality of care for patients with substance use disorders. Journal of Studies on Alcohol, 61, 704–713. [DOI] [PubMed] [Google Scholar]
- Pirkola S., Poikolainen K., Lönnqvist J. (2006). Currently active and remitted alcohol dependence in a nationwide adult general population: Results from the Finnish health 2000 study. Alcohol and Alcoholism, 41, 315–320. [DOI] [PubMed] [Google Scholar]
- Probst C., Manthey J., Martinez A., Rehm J. (2015). Alcohol use disorder severity and reported reasons not to seek treatment: A cross-sectional study in European primary care practices. Substance Abuse Treatment, Prevention, and Policy, 10, 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray G. T., Weisner C. M., Mertens J. R. (2005). Relationship between use of psychiatric services and five-year alcohol and drug treatment outcomes. Psychiatric Services, 56, 164–171. [DOI] [PubMed] [Google Scholar]
- Rehm J. Allamani A. Elekes Z. Jakubczyk A. Manthey J. Probst C.…Wojnar M. (2015). Alcohol dependence and treatment utilization in Europe: A representative cross-sectional study in primary care. BMC Family Practice, 16, 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J., Anderson P., Manthey J., Shield K. D., Struzzo P., Wojnar M., Gual A. (2016). Alcohol use disorders in primary health care: What do we know and where do we go? Alcohol and Alcoholism, 51, 422–427. [DOI] [PubMed] [Google Scholar]
- Rehm J., Mathers C., Popova S., Thavorncharoensap M., Teerawattananon Y., Patra J. (2009). Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet, 373, 2223–2233. [DOI] [PubMed] [Google Scholar]
- Roerecke M., Rehm J. (2013). Alcohol use disorders and mortality: A systematic review and meta-analysis. Addiction, 108, 1562–1578. [DOI] [PubMed] [Google Scholar]
- Roerecke M., Rehm J. (2014). Cause-specific mortality risk in alcohol use disorder treatment patients: A systematic review and meta-analysis. International Journal of Epidemiology, 43, 906–919. [DOI] [PubMed] [Google Scholar]
- Room R., Babor T., Rehm J. (2005). Alcohol and public health. Lancet, 365, 519–530. [DOI] [PubMed] [Google Scholar]
- Salomé H. J., French M. T., Scott C., Foss M., Dennis M. (2003). Investigating variation in the costs and benefits of addiction treatment: Econometric analysis of the Chicago Target Cities Project. Evaluation and Program Planning, 26, 325–338. [Google Scholar]
- Saunders S. M., Zygowicz K. M., D’Angelo B. R. (2006). Person-related and treatment-related barriers to alcohol treatment. Journal of Substance Abuse Treatment, 30, 261–270. [DOI] [PubMed] [Google Scholar]
- Tai B., Wu L.-T., Clark H. W. (2012). Electronic health records: Essential tools in integrating substance abuse treatment with primary care. Substance Abuse and Rehabilitation, 3, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timko C., Moos R. H., Finney J. W., Moos B. S., Kaplowitz M. S. (1999). Long-term treatment careers and outcomes of previously untreated alcoholics. Journal of Studies on Alcohol, 60, 437–447. [DOI] [PubMed] [Google Scholar]
- Trim R. S., Schuckit M. A., Smith T. L. (2013). Predictors of initial and sustained remission from alcohol use disorders: Findings from the 30-year follow-up of the San Diego prospective study. Alcoholism, Clinical and Experimental Research, 37, 1424–1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaillant G. E. (2003). A 60-year follow-up of alcoholic men. Addiction, 98, 1043–1051. [DOI] [PubMed] [Google Scholar]
- Watkins K. E., Burnam A., Kung F.-Y., Paddock S. (2001). A national survey of care for persons with co-occurring mental and substance use disorders. Psychiatric Services, 52, 1062–1068. [DOI] [PubMed] [Google Scholar]
- Westman J. Wahlbeck K. Laursen T. M. Gissler M. Nordentoft M. Hällgren J.…Ösby U. (2015). Mortality and life expectancy of people with alcohol use disorder in Denmark, Finland and Sweden. Acta Psychiatrica Scandinavica, 131, 297–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. (2014. a). Global status report on alcohol and health 2014. Retrieved from http://www.who.int/substance_abuse/publications/global_alcohol_report/msb_gsr_2014_1.pdf?ua=1
- WHO. (2014. b). Global alcohol report. Country profile: Finland. Retrieved from http://www.who.int/substance_abuse/publications/global_alcohol_report/profiles/fin.pdf
- Wu L.-T. Ghitza U. E. Batch B. C. Pencina M. J. Rojas L. F. Goldstein B. A.…Brady K. T. (2015). Substance use and mental diagnoses among adults with and without type 2 diabetes: Results from electronic health records data. Drug and Alcohol Dependence, 156, 162–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L.-T., Ringwalt C. L., Williams C. E. (2003). Use of substance abuse treatment services by persons with mental and substance use problems. Psychiatric Services, 54, 363–369. [DOI] [PubMed] [Google Scholar]