Abstract
Objectives:
The Supporting Family Caregivers with Technology trial tested the FamTechCare video support intervention against telephone support. Dementia caregivers’ video-recorded challenging care encounters and an interdisciplinary team provided tailored feedback. This paper reports on the effects of the intervention on caregiver confidence in managing priority challenges, a secondary outcome of this non-blinded parallel randomized controlled trial.
Methods:
Caregiver/person living with dementia dyads were randomized to the experimental FamTechCare video support (n=43) or attention control telephone support (n=41) groups. Caregivers providing in-home care to a person living with mild or more severe dementia were eligible. Caregivers identified three priority challenges using the Caregiver Target Problems Questionnaire and rated the frequency and severity of each challenge and their confidence managing the challenge at baseline and 3-months. Challenges were classified using the FamTechCare Technology-supported Dementia Care Typology. Effects on confidence were compared between groups using the Wilcoxon rank-sum test and within groups using the Wilcoxon signed-rank test.
Results:
Caregiver priority challenges included managing dementia behaviors, understanding disease expectations, and performing activity of daily living care. Improvements were observed across the three categories in both groups; however, not all changes were statistically significant. No significant differences were identified between groups.
Conclusion:
Caregivers in the FamTechCare group reported benefit across all priority challenges including managing dementia behaviors, understanding disease expectations, and performing activity of daily living care.
Clinical Implications:
Innovative technology provides new opportunities to support family caregivers in dementia home care. Video-recording can be used to enhance support for family caregivers facing care challenges.
Keywords: Alzheimer Disease, Behavioral Symptoms, Caregivers, Dementia, Telemedicine
Introduction
Supporting caregivers in providing cost-effective dementia care is a public health priority with a predicted increase to 75 million persons living with dementia (PLWD) globally by 2030 (Prince et al., 2015; World Health Organization, 2017). Supporting caregivers is a critical component to this growing public health need (World Health Organization, 2017). In the United States alone, it is estimated that informal caregivers currently provide 18.5 billion hours of unpaid care annually (Alzheimer’s Association, 2019).
Dementia caregiving responsibilities are vast, leading caregivers to experience a variety of unmet needs and care challenges ranging from managing behavioral and psychological symptoms of dementia (BPSD), to creating a safe environment, to performing activities of daily living (ADL) (Johnston et al., 2011; Kim, Shaw, Williams, & Hein, 2019; Zwingmann et al., 2019). Community-dwelling caregivers of PLWD continue to report high rates of unmet needs, with caregivers typically having greater than two unmet needs (Johnston et al., 2011; Zwingmann et al., 2019). These dementia care challenges, particularly managing BPSD, lead to declines in caregiver well-being (Feast, Moniz-Cook, Stoner, Charlesworth, & Orrell, 2016; Monin & Schulz, 2009) and contribute to nursing home placement for PLWD (Porter et al., 2016). With caregiver well-being and satisfaction directly associated with low caregiving competence and high caregiving stress (Quinn et al., 2019), it is essential to create interventions to support caregivers in managing dementia care challenges.
Robust interventions for dementia care are needed that are individually tailored to the caregiver-person living with dementia dyad’s unmet needs. Interventions that focus on the caregiver or person living with dementia individually and provide general rather than tailored support have not been successful in reducing BPSD and improving caregiver mental health outcomes (Caspar, Davis, Douziech, & Scott, 2018; Gilhooly et al., 2016). Technology provides a means to not only reach caregivers but also to achieve individualized support. Numerous technological interventions for dementia caregiver support have been evaluated that connect caregivers to professionals, peers, and education and have generally demonstrated modest benefits in improving caregiver mental health outcomes (Deeken, Rezo, Hinz, Discher, & Rapp, 2019; Hopwood et al., 2018). Although many of these interventions use technology as a means for connection, the ability for professionals to provide tailored support may be limited by caregiver retrospective recall of their care challenges.
The Kales, Gitlin, Lyketosos (2015) conceptual model for managing BPSD posits that the neurodegeneration associated with dementia combined with person living with dementia factors, caregiver factors, and environmental factors impact the vulnerability of PLWD to stressors that ultimately lead to BPSD (Kales, Gitlin, & Lyketsos, 2015). Relying on caregivers to effectively identify, remember, and report all of these factors to clinicians can limit the effectiveness of potential interventions. Caregiver challenges may be limited by caregiver retrospective recall when the caregiver cannot remember and report the specific details that contributed to the challenging care encounter. Even when caregivers are reliable historians, their ability to identify behaviors as unmet needs of the person living with dementia may limit the description to the professional for guidance. As caregivers are also directly involved in care, they may not be aware of all contributing factors. These limitations can be addressed with evolving technology by creating interventions that link caregivers to providers.
The FamTechCare telehealth intervention was developed to address limitations of caregiver report of challenging care situations and tested in the Supporting Family Caregivers with Technology for Dementia Home Care clinical trial (Williams et al., 2018; Williams et al., 2019). The purpose of this paper is to evaluate the efficacy of the FamTechCare intervention on caregiver challenges and unmet needs, a secondary outcome of the Supporting Family Caregivers with Technology for Dementia Home Care trial. It was hypothesized that FamTechCare caregivers would have greater decreases in the frequency and severity of identified challenges and greater gains in confidence in managing these care challenges compared to attention control caregivers.
Methods
Design
A multi-site parallel randomized controlled trial was conducted to test the effects of the FamTechCare intervention versus telephone-support on caregiver-identified outcomes in Kansas and Iowa. Study procedures were IRB-approved by both sites. The current paper reports the within-group and between-group changes of caregiver reported frequency, severity, and confidence in managing the caregiver’s priority care challenges in the FamTechCare trial (ClinicalTrials.gov identifier: NCT02483520).
Sample
A convenience sample of caregiver-PLWD dyads were recruited between October 2014 and June 2018. Inclusion criteria for PLWD were living at home and having a dementia diagnosis rated as mild or more severe on the Functional Assessment Staging (FAST) (Reisberg, 2007; Sclan & Reisberg, 1992). There was no exclusion based on the type of dementia. Exclusion criteria for PLWD were having a diagnosis of Huntington’s disease, schizophrenia, manic-depressive disorder, deafness, and/or intellectual disability. At both sites, dyads were recruited from the community through presentations at local caregiving meetings and through advertisements in local magazines and newspapers. In addition, one site used mass email notifications through the university community while the other used electronic medical record screening at an NIA-designated Alzheimer’s Disease Center. Informed consent was obtained from all participants and/or their surrogate decision makers, and assent was obtained from PLWD who were unable to consent independently.
Caregiver-PLWD dyads were randomly assigned to the FamTechCare group or the attention control group using a quarter-based blocking strategy with 1:1 allocation developed by the study statistician. More than one family caregiver for each person living with dementia was able to enroll and dyads with the same person living with dementia were cluster randomized to the same group. The dyads and study enrollment personnel were blinded to the group allocation until consent was completed. See the published FamTechCare protocol (Williams et al., 2018) and published main outcome analysis (Williams et al., 2019) for specific details on participant recruitment and eligibility, the protection of human subjects, intervention development, study procedures and fidelity, and changes in the primary outcomes.
Supporting Family Caregivers with Technology for Dementia Home Care clinical trial
The Supporting Family Caregivers with Technology for Dementia Home Care randomized controlled trial evaluated the FamTechCare video-recording intervention by testing changes in caregiver psychosocial outcomes. The experimental (FamTechCare) group was compared to an attention control (telephone support) group over the 3-month study. The FamTechCare video-recording intervention is a multicomponent telehealth intervention in which caregivers video-record challenging care episodes and receive tailored feedback on the video from an interdisciplinary expert team (Figure 1).
Figure 1.
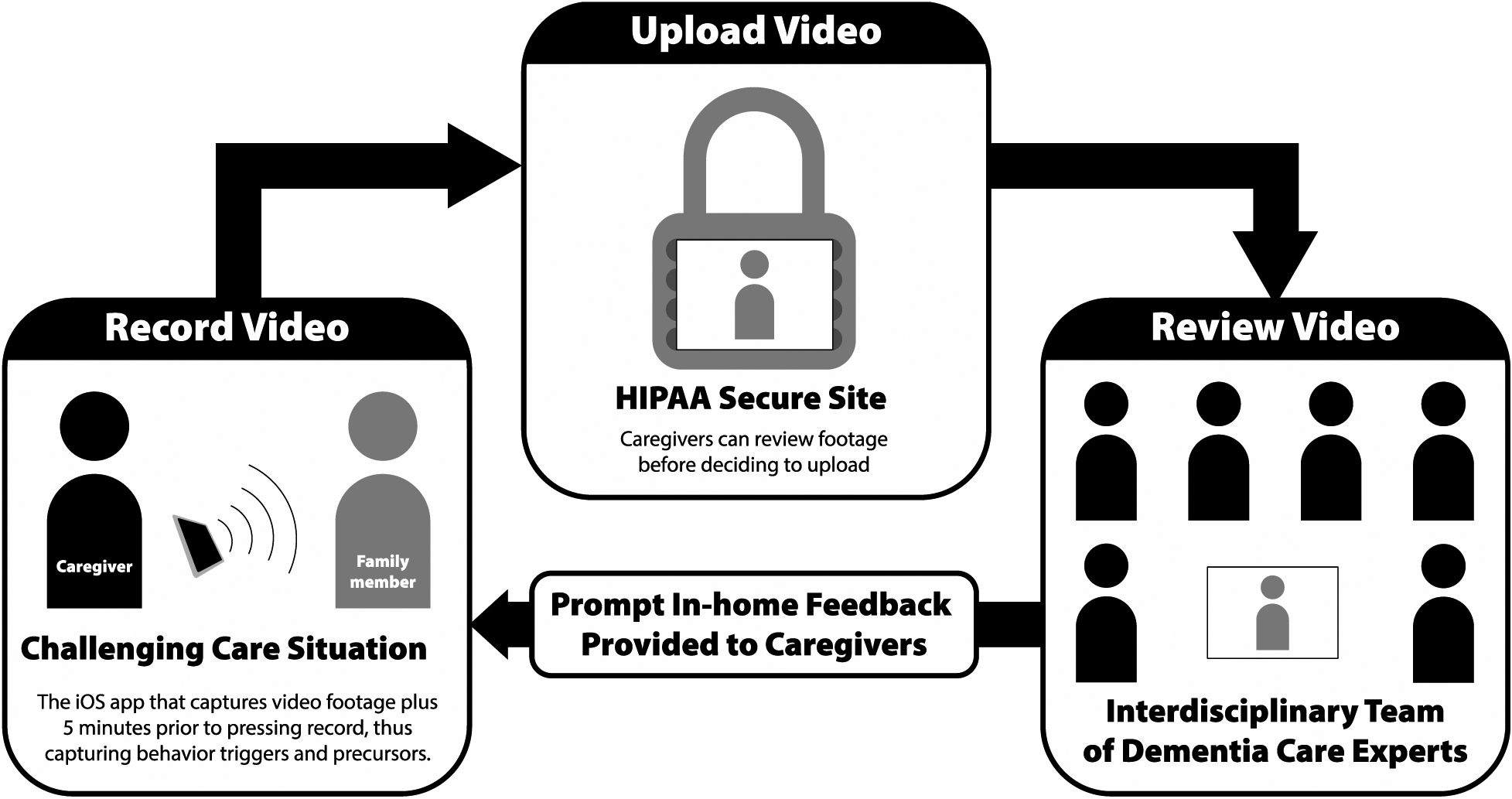
FamTechCare Study Procedure
Dementia caregivers video recorded challenging care situations using an iPad Mini with a novel application that captures antecedent behavior through a buffering technology integrated within the application. To ensure privacy, caregivers reviewed the recordings and decided whether to delete or upload the videos to a HIPAA-secure website for expert review. The interdisciplinary expert team reviewed the videos weekly and developed tailored interventions through group discussion. Tailored interventions covered a broad spectrum of caregiver needs focusing on managing BPSD, performing ADL care, providing education about dementia, increasing knowledge related to medication administration, improving medical care utilization, increasing home and personal safety, providing caregiver social support, enhancing caregiver self-care, acquiring and utilizing respite services, as well as providing positive reinforcement to the caregiver (Kim et al., 2019). The team developing the tailored interventions included research and clinical professionals from the fields of nursing, geriatric psychiatry, social work, and psychology. The feedback from the expert team was then relayed to each caregiver during a scheduled weekly phone call with the interventionist.
The FamTechCare caregivers were compared to the attention control caregivers who received weekly telephone support with a nurse with graduate education or a social worker interventionist who provided similar tailored interventions based only on caregiver retrospective recall. The attention control caregivers were provided with the video monitoring equipment and were trained to record and submit weekly videos. However, their videos were reviewed and feedback was provided by the expert team only at the completion of the 3-month trial, after data collection related to the outcomes was completed. The main outcome analysis, focused on 3-month changes in caregiver psychosocial outcomes (i.e., caregiver burden, depression, sleep disturbance, competence, desire to institutionalize the PLWD, and reaction to behavioral symptoms of the PLWD), is reported elsewhere (Williams et al., 2019). Analysis of intervention fidelity revealed that the topics of and amounts of tailored interventions provided to the caregivers did not differ by group (Williams et al., 2019). Using linear mixed modeling, it was demonstrated that the FamTechCare group had reductions in caregiver depression and gains in caregiver perceived competence after 3-months when compared to the attention control group.
Data collection
Demographic information was collected for both the caregivers and PLWD at baseline. Caregivers reported their three priority care challenges at baseline using the Caregiver Target Problems Questionnaire (Teri, McCurry, Logsdon, & Gibbons, 2005). The Caregiver Target Problems Questionnaire was adapted and used to identify caregiver priority care challenges for frequency, severity, and confidence at baseline and 3-months (Teri et al., 2005). Prior to group allocation, caregivers identified three priority care challenges and rated them on 5-point Likert scales: frequency of the challenge (0 = None to 4 = Daily or more often), severity of the challenge (0 = Trivial to 4 = Severe), and confidence in managing the challenge (0 = Unable to manage to 4 = Very confident). At the end of the 3-month trial, caregivers repeated their ratings of the baseline care challenges. Improvement was indicated by a decrease in frequency and severity and increase in confidence from baseline to 3-months.
Data analysis
The care challenges were categorized using the FamTechCare Technology-Supported Dementia Care Typology (Kim et al., 2019). The typology has 10 categories of dementia caregiver interventions and was applied to categorize the challenges experienced by families caring for PLWD. Categories related to PLWD are BPSD, disease expectations, activities and instrumental activities of daily living (ADLs), safety, medical care utilization, and medication education and use. Categories related to caregivers are social and financial support, self-care, respite, and positive reinforcement. For care challenge categories that had sufficient sample size, changes were compared between FamTechCare and attention control groups using the Wilcoxon rank-sum test. Within-group mean changes in ratings of severity, frequency, and confidence were tested using the Wilcoxon signed-rank test. SAS software (version 9.4) was used for all statistical analyses. Findings at alpha <.05 were considered statistically significant. Effect sizes for within group changes and differences between group changes were calculated using the rank-biserial correlation approach (Kerby, 2014).
Results
Sample
The final sample for FamTechCare trial included 84 dyads made up of 83 caregivers and 71 PLWD; one caregiver (adult child) provided care for two PLWD (parents). Forty-three dyads received the FamTechCare intervention, and 41 dyads received the attention control intervention. Twenty-three dyads (n=8 FamTechCare; n=15 attention control) were excluded from the final analysis: 9 dyads for discontinuing before 1 month, 8 dyads with formal (i.e., paid) caregivers, 5 dyads for the PLWD having no disruptive behaviors at baseline, 1 month, or 3 months, and 1 dyad with significant outliers. See Williams et al. (2019) for the CONSORT diagram and detailed description of the analysis sample. No reportable adverse events were experienced by dyads in either group.
The majority of caregivers cared for a spouse (66.3%), were female (71.2%), non-Hispanic (94.0%) white (92.8%), with a bachelor’s degree or higher (59.0%), and a mean age of 64.2±12.8 years (range = 32.0–90.0). The majority of PLWD were male (59.2%), non-Hispanic (94.4%) white (95.8%), with less than a bachelor’s degree (54.9%), and a mean age of 75.7±9.5 years (range = 54.0–93.0). Over half of the PLWD had a primary dementia diagnosis of Alzheimer’s disease (52.1%) with dementia rated as moderately severe (50.7%) on the FAST. Demographic characteristics are reported in Table 1. There were no significant differences in demographic characteristics between groups.
Table 1.
Demographic Characteristics of Caregivers and Persons Living with Dementia
| FamTechCare | Attention Control | |||
|---|---|---|---|---|
| Caregiver | ||||
| n | Mean (SD) | n | Mean (SD) | |
| Age | 42 | 64.6 (12.2) | 41 | 63.9 (13.7) |
| Number of years as caregiver | 41 | 4.4 (3.0) | 41 | 3.8 (3.5) |
| n | %3 | n | %3 | |
| Gender | ||||
| Female | 30 | 71.4 | 29 | 70.7 |
| Male | 12 | 28.6 | 12 | 29.3 |
| Race | ||||
| White | 37 | 88.1 | 40 | 97.6 |
| African American | 4 | 9.5 | 1 | 2.4 |
| More than one race | 1 | 2.4 | 0 | 0.0 |
| Ethnicity | ||||
| Not Hispanic/Latino | 41 | 97.6 | 37 | 90.2 |
| Unknown/Not reported | 1 | 2.4 | 4 | 9.8 |
| Relationship to PLWD1 | ||||
| Spouse | 29 | 69.1 | 26 | 63.4 |
| Child/Spouse of child | 12 | 28.6 | 15 | 36.6 |
| Other2 | 1 | 2.4 | 0 | 0.0 |
| Education level | ||||
| Less than Bachelor’s degree | 19 | 45.2 | 15 | 36.6 |
| Bachelor’s degree | 13 | 31.0 | 20 | 48.8 |
| Master’s degree or higher | 10 | 23.8 | 6 | 14.6 |
| Persons Living with Dementia | ||||
| n | Mean (SD) | n | Mean (SD) | |
| Age | 39 | 75.5 (9.7) | 32 | 75.9 (9.3) |
| n | %3 | n | %3 | |
| Gender | ||||
| Male | 24 | 61.5 | 18 | 56.3 |
| Female | 15 | 38.5 | 14 | 43.8 |
| Race | ||||
| White | 37 | 94.9 | 31 | 96.9 |
| African American | 2 | 5.1 | 1 | 3.1 |
| Ethnicity | ||||
| Not Hispanic/Latino | 38 | 97.4 | 29 | 90.6 |
| Unknown/Not reported | 1 | 2.6 | 3 | 9.4 |
| Education level | ||||
| Less than Bachelor’s degree | 22 | 56.4 | 17 | 53.1 |
| Bachelor’s degree | 5 | 12.8 | 9 | 28.1 |
| Master’s degree or higher | 12 | 30.8 | 6 | 18.8 |
| Type of dementia | ||||
| Alzheimer’s disease | 21 | 53.9 | 16 | 50.0 |
| Other diagnosed dementia | 15 | 38.5 | 9 | 28.1 |
| Unknown | 3 | 7.7 | 7 | 21.9 |
| Dementia Stage (FAST) | ||||
| Incipient | 0 | 0.0 | 1 | 3.1 |
| Mild | 10 | 25.6 | 10 | 31.3 |
| Moderate | 7 | 18.0 | 6 | 18.8 |
| Moderately severe | 21 | 53.9 | 15 | 46.9 |
| Severe | 1 | 2.6 | 0 | 0.0 |
Note.
PLWD = person living with dementia;
Other relationship with the person with dementia was girlfriend;
Percentages may total more than 100% due to rounding.
Priority Care Challenges
Priority care challenges (N = 252) identified by caregivers at baseline are described in Table 2. Challenges were categorized into seven of the ten typology categories: BPSD (n=103, 40.9%), disease expectations (n=73, 29.0%), ADL (n=52, 20.6%), safety (n=16, 6.3%), caregiver social and financial support (n=5, 2.0%), caregiver self-care (n=2, 0.8%), and respite (n=1, 0.4%). No care challenges were identified in medical care utilization, medication purpose and use, and caregiver positive reinforcement categories.
Table 2.
Caregiver Priority Challenges (N=252) by FamTechCare Technology-Supported Dementia Care Typology
| Typology Category | N | Caregiver Priority Challenge (n) |
|---|---|---|
| Behavioral and psychological symptoms of dementia | 103 | Disinterest (22), Depression (16), Sleep disturbance (14), Frustration (10), Verbal aggression (9), Anxiety (7), Agitation (6), Rummaging/hoarding (4), Self-harm (3), Embarrassing socially (3), Physical aggression (2), Withdrawn (2), Paranoia (2), Sun downing (1), Vocalizations (1), Hallucinations (1) |
| Disease expectations | 73 | Communication (19), Losing/misplacing objects (11), Memory loss (10), Forgetfulness (9), Following directions (7), Repetitiveness (4), Difficult to redirect (4), Decreased focus (4), Unclear dementia trajectory (3), Caregiver reliance (1), Lack of dementia education (1), |
| Activities and instrumental activities of daily living | 52 | Eating (15), Bathing/hygiene (14), Toileting/incontinence (6), Mobility (5), Dressing (5), Medication administration (4), Oral care (2), Dexterity (1) |
| Safety | 16 | Getting lost (8), Driving (5), Personal safety (3) |
| Caregiver social and financial support | 5 | Caregiver helplessness (2), Family dynamics (2), Financial constraints (1) |
| Caregiver self-care | 2 | Caregiver emotional management (1), Caregiver health (1) |
| Caregiver respite | 1 | Respite (1) |
| Medical care utilization | 0 | |
| Medication purpose and use | 0 | |
| Positive reinforcement | 0 |
The frequencies of priority challenges for which caregivers’ ratings of frequency, severity, and confidence were provided at both baseline and 3 months were sufficient for assessing changes in the BPSD (n=78), disease expectations (n=62), and ADL (n=42) categories. Within the typology, BPSD is defined as agitation, aggression, apathy, anxiety, delusions, depression, disinhibition, hallucinations, irritability, motor disturbances, and/or nighttime wakefulness exhibited by the PLWD. Disease expectations are defined as challenges specifically related to dementia’s progressive trajectory related to memory loss (e.g., increasing forgetfulness, difficulty following directions, and increasing functional decline). The ADL category includes any challenge related to activities or instrumental activities of daily living (e.g., bathing, oral hygiene, medication administration).
Table 3 summarizes ratings of frequency, severity, and confidence in managing care challenges for BPSD, disease expectations, and ADL categories at baseline and 3 months and reports p-values for the statistical tests. At baseline, FamTechCare and attention control caregivers differed significantly on confidence in managing BPSD challenges (1.7±1.1 vs. 2.3±1.0, p=.023) and frequencies of disease expectations (2.8±1.2 vs. 3.5±0.9, p=.017). Other differences between the groups were not statistically significant. Improvements from baseline to 3 months were observed for all three categories for both FamTechCare and attention control groups, even though not all changes were statistically significant. Differences between FamTechCare and attention control groups with respect to changes from baseline to 3 months were not statistically significant.
Table 3.
Changes in Priority Caregiver Challenges
| FamTechCare | Attention Control | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Baseline | 3-Month | r4 | p5 | N | Baseline | 3-Month | r4 | p5 | r4 | p6 | ||
| BPSD | |||||||||||||
| Frequency1 | 43 | 3.3 (1.2) | 2.5 (1.2) | 0.63 | .001 | 35 | 3.1 (1.0) | 2.7 (1.3) | 0.36 | .130 | 0.22 | .094 | |
| Severity2 | 43 | 2.5 (1.0) | 2.0 (1.0) | 0.44 | .024 | 33 | 2.4 (0.9) | 1.8 (1.1) | 0.67 | .001 | −0.02 | .892 | |
| Confidence3 | 43 | 1.7 (1.1) | 2.6 (1.1) | 0.70 | <.001 | 33 | 2.3 (1.0) | 2.8 (1.0) | 0.40 | .085 | 0.17 | .211 | |
| Disease Expectations | |||||||||||||
| Frequency1 | 31 | 2.8 (1.2) | 2.5 (1.5) | 0.33 | .228 | 31 | 3.5 (0.9) | 3.2 (1.1) | 0.75 | .043 | −0.01 | .969 | |
| Severity2 | 29 | 2.7 (1.0) | 1.8 (1.3) | 0.75 | .002 | 31 | 2.5 (0.9) | 2.0 (1.0) | 0.54 | .021 | 0.15 | .306 | |
| Confidence3 | 29 | 2.3 (0.9) | 2.9 (1.2) | 0.62 | .005 | 31 | 2.2 (0.9) | 2.8 (0.7) | 0.53 | .023 | 0.11 | .476 | |
| ADL | |||||||||||||
| Frequency1 | 17 | 2.9 (1.2) | 2.8 (1.2) | 0.10 | .750 | 24 | 3.3 (1.0) | 3.0 (1.3) | 0.30 | .345 | −0.09 | .615 | |
| Severity2 | 18 | 2.8 (1.1) | 2.1 (1.1) | 0.65 | .034 | 24 | 2.3 (1.0) | 2.2 (1.2) | 0.09 | .724 | 0.24 | .192 | |
| Confidence3 | 18 | 2.3 (1.0) | 2.8 (0.9) | 0.82 | .020 | 24 | 2.2 (1.1) | 2.6 (0.9) | 0.50 | .117 | 0.07 | .677 | |
Note.
Decrease in frequency and severity ratings indicates improvement;
increase in confidence ratings indicates improvement;
Rank-biserial correlation indicates effect sizes for within-group changes and between groups differences in changes;
p-values were calculated for within-group changes using Wilcoxon signed-rank test;
p-values were calculated for differences between mean group changes using Wilcoxon rank-sum test.
The improvements in ratings of frequency, severity and confidence in managing of BPSD challenges were statistically significant for FamTechCare caregivers (r=.63, p=.001; r=.44, p=.024; r=.70, p<.001; respectively); while only a decrease in severity ratings was statistically significant for attention controls (r=.67, p=.001). The improvements in ratings of severity and confidence in managing of disease expectations challenges were statistically significant for FamTechCare caregivers (r=.75, p=.002; r=.62, p=.005; respectively); while improvements in all three ratings were statistically significant for attention controls (r=.75, p=.043; r=.54, p=.021; r=.53, p=.023). Finally, the improvements in ratings of severity and confidence in managing of ADL challenges were statistically significant for FamTechCare caregivers (r=.65, p=.034; r=.82, p=.020; respectively); while no improvements were statistically significant for attention controls.
Discussion
Providing care for a loved one with dementia includes taking on new roles and developing new skills such as providing intimate personal care and managing BPSD with recognized stress and burden to caregivers. Caregiving for a person living with dementia has well established negative effects on caregiver health and well-being (Feast et al., 2016; Monin & Schulz, 2009). This paper evaluated efficacy of the FamTechCare intervention on caregiver challenges and unmet needs. The FamTechCare intervention provided expert feedback to in-home dementia caregivers based on video-recordings and was compared to telephone support based on caregiver retrospective recall. It was hypothesized that FamTechCare caregivers would have greater decreases in the frequency and severity of identified challenges and greater gains in confidence in managing these care challenges compared to attention control caregivers. Although FamTechCare caregivers consistently saw improvements across managing BPSD, performing ADL care, and understanding disease expectations over the 3-month study period, between group differences were not significant.
This analysis identified unmet needs from the perspective of dementia caregivers. Knowledge about the types and relative importance of the care challenges experienced by caregivers is valuable for healthcare providers offering supportive interventions. Care challenges that are most commonly identified should be addressed across caregiver support interventions. Interventions that address managing challenges and caregiver lack of confidence may yield the greatest benefit in reducing the stress and burden of caregiving. Challenges related to BPSD, disease expectations, and ADL categories were most frequently identified by caregivers; the top challenges were PLWD- disinterest, communication, depression, eating, and sleep disturbance.
In contrast, some categories were infrequently identified as priorities; many had small counts making statistical testing impossible. For example, caregivers infrequently noted a need for interventions focused on the caregivers themselves, such as respite. These care challenges may have been noted less frequently because caregivers were focused on care of the PLWD and topics caregivers thought the FamTechCare intervention would address. In addition, caregivers may not identify their own social and financial constraints as a priority for professional intervention. Other research using tools and/or provider assessment to identify caregiver unmet needs rather than caregiver self-reported identification has also determined that caregivers lack resources for managing PLWD mental/behavioral health, performing ADL care, ensuring environmental safety, and prioritizing caregiver support (Johnston et al., 2011; Zwingmann et al., 2019).
This study illustrated how video-recording technology can be used in the home to enhance support for family caregivers. Although caregivers reported improvements in both groups, the improvements were demonstrated across all categories in the FamTechCare group. This occurred even though the attention control caregivers also received an intervention using telephone support that is beyond usual dementia care. Attention control caregivers received an equivalent amount of interventionist contact compared to FamTechCare caregivers (136.0 ± 110.4 minutes compared to 132.8 ± 94.4 minutes).
The attention control intervention, a simple educational intervention based on caregiver retrospective recall, also yielded some benefits to caregivers who reported specific care challenges. Specifically, attention control caregivers noted positive effects related to challenges of disease expectations. Traditional education and support based on retrospective recall may be a successful strategy when it comes to understanding disease expectations that focus on dementia education. Disease expectations were a common concern making up 26.0% of the caregivers’ reported priority challenges (i.e. memory loss and forgetfulness). Finding ways to provide effective dementia education to caregivers continues to be a research priority with a recent meta-analysis finding that dementia education demonstrates reduction in caregiver depression but inconsistently improves caregiver burden (Moore, Lee, Sampson, & Candy, 2019).
In contrast, FamTechCare caregivers demonstrated consistent improvements in behavioral and psychological symptoms and ADL care challenges. This may be due to the fact that the video data allows viewing of actual behaviors and their antecedents by dementia care experts which may not have been observed by caregivers or reported in adequate detail in order to identify effective interventions. Caregivers in the FamTechCare intervention group not only reported increased confidence in managing BPSD, they also reported decreased severity and frequency of BPSD which is a critical component in supporting in-home dementia caregivers and reducing nursing home placement (Porter et al., 2016). Both groups reported improvements in managing ADL challenges, but only the FamTechCare group demonstrated statistically significantly improvements regarding ADL challenges. Similar to BPSD, ADL interventions may be best tailored through actual viewing by allowing experts to see care delivery rather than retrospective recall. Finding effective ways for caregivers to efficiently complete ADL care is also a critical component of supporting dementia caregivers because the hours spent providing this type of care directly impacts caregiver burden (Lin, Shih, & Ku, 2019).
The FamTechCare intervention allowed experts to provide tailored feedback rather than just general support and education to caregivers. This intervention meets the current recommendations that dementia care interventions need to be tailored to specific dyad needs rather than general coping and care strategies (Caspar et al., 2018; Gilhooly et al., 2016). Future research should address how to pragmatically implement video support into care models or existing dementia support interventions.
This study was limited as it enrolled a convenience sample of volunteers with limited diversity and included caregivers who were self-selected as willing to record and submit videos of care in their homes. Race and ethnicity may impact caregiver’s confidence in dealing with BPSD (Hansen, Hodgson, Budhathoki, & Gitlin, 2018), thus this research should be replicated in more diverse samples. Evaluation of the caregiver benefits is also limited by reliance on self-report.
Both video-based and telephone interventions allowed caregivers flexibility in selecting what care challenges were addressed from week to week, acknowledging that dementia caregiver challenges and needs change over time. Although caregivers in both the FamTechCare and attention control group selected three priority care challenges at baseline, there was no requirement that caregivers in the FamTechCare group had to send videos related only to their baseline priority challenges or that caregivers in the attention control group had to retrospectively report only on baseline challenges. Therefore, the interventions provided from week to week may have focused on topics differing from the baseline priorities and caregivers may not have seen benefits in managing baseline care challenges.
This study identified in-home dementia caregiver perceptions of the benefit of video-based feedback for managing challenging care situations based on caregiver self-identified unmet needs. Caregivers in the video-supported intervention group reported benefit from the FamTechCare intervention across all priority care challenges including managing BPSD, understanding disease expectations, and performing ADL care. Caregivers receiving the FamTechCare intervention specifically demonstrated improvements in the frequency, severity, and confidence in managing BPSD. Video data provides an effective approach to extend caregiver support in fulfilling the important role of caring for loved ones with dementia.
Clinical Implications.
In-home dementia caregivers report that their priority care challenges are managing behavioral and psychological symptoms of dementia, understanding disease expectations, and performing activities of daily living care.
Using available technology, family caregivers of persons living with dementia can be supported with individualized intervention tailoring through expert feedback based on caregiver-initiated video-recordings.
Caregivers participating in the video intervention reported improved confidence and reduced frequency and severity for all types of priority care challenges.
Acknowledgements
The University of Kansas Alzheimer’s Disease Center (P30AG035982) provided essential infrastructure and recruitment support. The authors thank other research team members who were involved in the conduct of the FamTechCare study including Eric Vidoni, Diane Blyler, Denise Seabold, Michelle Cochran, JoEllen Wurth, Ann Arthur, Michelle Niedens, Phyllis Switzer, Ann Bossen, and Sohyun Kim.
Funding details
This work was supported by the National Institute of Nursing Research of the National Institutes of Health under grant number R01NR014737. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Clinical Trials registration NCT02483520.
Footnotes
Declaration of interest statement
We have no conflict of interest to declare.
References
- Alzheimer’s Association. (2019). 2019 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, 15(3), 321–387. doi: 10.1016/j.jalz.2019.01.010 [DOI] [Google Scholar]
- Caspar S, Davis ED, Douziech A, & Scott DR (2018). Nonpharmacological management of behavioral and psychological symptoms of dementia: What works, in what circumstances, and why? Innovations in Aging, 2(1). doi: 10.1093/geroni/igy001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeken F, Rezo A, Hinz M, Discher R, & Rapp MA (2019). Evaluation of technology-based interventions for informal caregivers of patients with dementia: A meta-analysis of randomized controlled trials. The American Journal of Geriatric Psychiatry, 27(4), 426–445. doi: 10.1016/j.jagp.2018.12.003 [DOI] [PubMed] [Google Scholar]
- Feast A, Moniz-Cook E, Stoner C, Charlesworth G, & Orrell M (2016). A systematic review of the relationship between behavioral and psychological symptoms (BPSD) and caregiver well-being. International Psychogeriatrics, 28(11), 1761–1774. doi: 10.1017/s1041610216000922 [DOI] [PubMed] [Google Scholar]
- Gilhooly KJ, Gilhooly ML, Sullivan MP, McIntyre A, Wilson L, Harding E, … Crutch S (2016). A meta-review of stress, coping and interventions in dementia and dementia caregiving. BMC Geriatrics, 16, 106. doi: 10.1186/s12877-016-0280-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen BR, Hodgson NA, Budhathoki C, & Gitlin LN (2018). Caregiver reactions to aggressive behaviors in persons with dementia in a diverse, community-dwelling sample. Journal of Applied Gerontology, 0733464818756999. doi: 10.1177/0733464818756999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood J, Walker N, McDonagh L, Rait G, Walters K, Iliffe S, … Davies N (2018). Internet-based interventions aimed at supporting family caregivers of people with dementia: Systematic review. Journal of Medical Internet Research, 20(6), e216. doi: 10.2196/jmir.9548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston D, Samus QM, Morrison A, Leoutsakos JS, Hicks K, Handel S, … Black BS (2011). Identification of community-residing individuals with dementia and their unmet needs for care. International Journal of Geriatric Psychiatry, 26(3), 292–298. doi: 10.1002/gps.2527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kales HC, Gitlin LN, & Lyketsos CG (2015). Assessment and management of behavioral and psychological symptoms of dementia. BMJ, 350. doi: 10.1136/bmj.h369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerby DS (2014). The simple difference formula: An approach to teaching nonparametric correlation. Comprehensive Psychology, 3(1), 1–9. doi: 10.2466/11.it.3.1 [DOI] [Google Scholar]
- Kim S, Shaw C, Williams K, & Hein M (2019). Typology of technology-supported dementia care guidance from an in-home telehealth trial. Western Journal of Nursing Research, Epub ahead of print. doi: 10.1177/0193945919825861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C-Y, Shih P-Y, & Ku L-JE (2019). Activities of daily living function and neuropsychiatric symptoms of people with dementia and caregiver burden: The mediating role of caregiving hours. Archives of Gerontology and Geriatrics, 81, 25–30. doi: 10.1016/j.archger.2018.11.009 [DOI] [PubMed] [Google Scholar]
- Monin JK, & Schulz R (2009). Interpersonal effects of suffering in older adult caregiving relationships. Psychology and Aging, 24(3), 681–695. doi: 10.1037/a0016355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore KJ, Lee CY, Sampson EL, & Candy B (2019). Do interventions that include education on dementia progression improve knowledge, mental health and burden of family carers? A systematic review. Dementia, 1471301219831530. doi: 10.1177/1471301219831530 [DOI] [PubMed] [Google Scholar]
- Porter CN, Miller MC, Lane M, Cornman C, Sarsour K, & Kahle-Wrobleski K (2016). The influence of caregivers and behavioral and psychological symptoms on nursing home placement of persons with Alzheimer’s disease: A matched case–control study. SAGE Open Med, 4, 2050312116661877. doi: 10.1177/2050312116661877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince M, Wimo A, Guerchet M, Ali G, Wu Y, Prina M, & Alzheimer’s Disease International. (2015). World Alzheimer Report 2015: The Global Impact of Dementia. Retrieved July 17, 2019 from https://www.alz.co.uk/research/WorldAlzheimerReport2015.pdf
- Quinn C, Nelis SM, Martyr A, Victor C, Morris RG, & Clare L (2019). Influence of positive and negative dimensions of dementia caregiving on caregiver well-being and satisfaction with life: Findings from the IDEAL study. The American Journal of Geriatric Psychiatry. doi: 10.1016/j.jagp.2019.02.005 [DOI] [PubMed] [Google Scholar]
- Reisberg B (2007). Global measures: Utility in defining and measuring treatment response in dementia. International Psychogeriatrics, 19(3), 421–456. doi: 10.1017/s1041610207005261 [DOI] [PubMed] [Google Scholar]
- Sclan SG, & Reisberg B (1992). Functional assessment staging (FAST) in Alzheimer’s disease: Reliability, validity, and ordinality. International Psychogeriatrics, 4(1), 55–69. doi: 10.1017/S1041610292001157 [DOI] [PubMed] [Google Scholar]
- Teri L, McCurry SM, Logsdon R, & Gibbons LE (2005). Training community consultants to help family members improve dementia care: A randomized controlled trial. Gerontologist, 45(6), 802–811. doi: 10.1093/geront/45.6.802 [DOI] [PubMed] [Google Scholar]
- Williams K, Blyler D, Vidoni Eric D, Shaw C, Wurth J, Seabold D, … Van Sciver A (2018). A randomized trial using telehealth technology to link caregivers with dementia care experts for in‐home caregiving support: FamTechCare protocol. Research in Nursing and Health, 41(3), 219–227. doi: 10.1002/nur.21869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams KN, Perkhounkova Y, Shaw CA, Hein M, Vidoni ED, & Coleman CK (2019). Supporting family caregivers with technology for dementia home care: A randomized controlled trial. Innovations in Aging, 3(3), 1–19. doi: 10.1093/geroni/igz037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2017). Global Action Plan on the Public Health Response to Dementia 2017–2025. Retrieved July 17, 2019 from https://www.who.int/mental_health/neurology/dementia/action_plan_2017_2025/en/
- Zwingmann I, Michalowsky B, Esser A, Kaczynski A, Monsees J, Keller A, … Hoffmann W (2019). Identifying unmet needs of family dementia caregivers: Results of the baseline assessment of a cluster-randomized controlled intervention trial. Journal of Alzheimer’s Disease, 67(2), 527–539. doi: 10.3233/jad-180244 [DOI] [PMC free article] [PubMed] [Google Scholar]


