Abstract
Objective
This study aimed to describe changes in families’ home food environment and parent feeding practices, from before to during the coronavirus disease 2019 (COVID‐19) pandemic, and examine whether changes differed by food security status.
Methods
Parents (N = 584) in the US completed a single online survey, reporting on food security, home food availability, and feeding practices both retrospectively (considering before COVID‐19) and currently (during COVID‐19). χ2 and univariate regressions examined associations by food security status.
Results
The percent of families reporting very low food security increased by 20% from before to during COVID‐19 (P < 0.01). About one‐third of families increased the amount of high‐calorie snack foods, desserts/sweets, and fresh foods in their home; 47% increased nonperishable processed foods. Concern about child overweight increased during COVID‐19, with a greater increase for food‐insecure versus food‐secure parents (P < 0.01). Use of restriction, pressure to eat, and monitoring increased, with a greater increase in pressure to eat for parents with food insecurity compared with food‐secure parents (P < 0.05).
Conclusions
During COVID‐19, increases in very low food security and changes in the home food environment and parent feeding practices were observed. Results highlight the need to address negative impacts of COVID‐19 on children’s obesity risk, particularly among those facing health disparities.
Study Importance.
What is already known?
-
►
The coronavirus disease 2019 (COVID‐19) pandemic is expected to increase the number of families experiencing food insecurity and the prevalence of childhood obesity in the US.
-
►
The social and economic impacts of COVID‐19 will likely result in changes in the home food environment and parent feeding practices that may contribute to possible rising obesity rates.
What does this study add?
-
►
Changes in families’ home food environments, increased concern about child overweight, and increased controlling feeding practices were observed during COVID‐19 compared with before COVID‐19.
-
►
Greater changes in parents’ concern about child overweight and pressure to eat were observed for families experiencing food insecurity, compared with food‐secure families.
How might these results change the direction of research or the focus of clinical practice?
-
►
These results can inform public health policies and initiatives to provide nutrition support for children most at need during the COVID‐19 pandemic.
-
►
These results support the need for clinical interventions to provide evidence‐based obesity prevention and treatment programs for children, during and after COVID‐19.
Introduction
Coronavirus disease 2019 (COVID‐19) has caused sudden and unexpected changes in families’ everyday lives. To slow the spread of this novel virus, US government mandates required individuals to adopt a new way of living, causing changes in employment, income, childcare, education, and community resources. There has been a drastic rise in job losses, with more than 40 million Americans having filed for unemployment between March and May 2020 (1). As a result, millions more Americans will experience food insecurity over the next year (2). Food insecurity is defined as limited or uncertain availability of nutritionally adequate and safe foods or ability to acquire acceptable foods in socially acceptable ways (3). Before COVID‐19, one in six children experienced food insecurity (4), and in 2020, that number is expected to rise drastically (2). This increase will impact the health and nutrition of children nationwide, with particular concern for vulnerable populations who are already at greatest risk for diseases such as obesity (4, 5, 6, 7, 8). To offset these forthcoming health impacts, information is needed on how factors that influence children’s dietary intake and eating behaviors are currently being affected during this period in history.
Social distancing mandates imposed because of COVID‐19 may be influencing the types and amounts of food brought into the home, thus influencing children’s dietary intake through changes in their home food environment. Families, regardless of food security status, may be purchasing more lower‐cost, shelf‐stable foods that are often less healthy and lower in key nutrients (9). Moreover, to reduce the number of shopping trips and social exposure, families might purchase more food, including greater amounts of nonperishable, highly processed foods and fewer fresh foods such as fruits and vegetables. These purchasing behaviors change the home food availability and can influence children’s dietary intake. The home food environment is even more salient during COVID‐19, as children are consuming more meals at home given the widespread stay‐at‐home mandates and school closures. For food‐insecure families in particular, this change means reduced access to school‐provided meals (5) that low‐income children previously relied on for a substantial portion of their daily energy intake (10). As such, changes in families’ home food environments are likely to be more pronounced for children in food‐insecure families.
COVID‐19 might also impact children’s eating behaviors through changes in parent feeding practices. Controlling feeding practices include restricting certain foods, pressuring children to eat, and using food as a reward (11). During the COVID‐19 pandemic, parents might use controlling feeding practices more often, because of higher levels of stress, fewer resources, and less access to food (real or perceived). For example, restrictive feeding practices are used more often when parents report higher stress and depression and live in food‐insecure households (12, 13), and data have shown increased stress, depression, and food insecurity during COVID‐19 (2, 14, 15). Parents may also experience or perceive a lack of food access and affordability, and therefore restrict the amount of food their children eat, in order to make the food in their homes last longer. Furthermore, parents might use food as a reward to shape children’s behavior as they navigate working from home while simultaneously caring for their children. Controlling feeding practices have been associated with poorer regulation of energy intake, weight, and adiposity in children (16, 17, 18, 19, 20, 21); thus, a sustained increase of these feeding practices during COVID‐19 and beyond may increase children’s risk for obesity and/or unhealthy eating behaviors.
The purpose of this study was to describe associations among changes in food insecurity, the home food environment, and parent feeding practices, from before to during the COVID‐19 pandemic, in order to inform public health interventions that can work to offset any detrimental impacts of COVID‐19 on children’s health. A nationwide survey was administered at a single timepoint during the COVID‐19 pandemic to describe how parent‐reported food insecurity, the home food environment, and parent feeding practices have changed from before the COVID‐19 pandemic (retrospective report) to during the COVID‐19 pandemic in a nationwide convenience sample of parents living in the US. We then examine whether these changes in the home food environment and parent feeding practices differ by food security status. We hypothesize that an increase in food insecurity, obesogenic home food environments, and controlling feeding practices will be observed, from before the pandemic to during the pandemic, with greater changes for families currently experiencing food insecurity.
Methods
Participants and procedures
This cross‐sectional, observational study used an online survey to measure parent‐reported food security status, the home food environment, and parent feeding practices before the COVID‐19 pandemic (retrospective report) and during the COVID‐19 pandemic (at the time of survey completion). The survey was disseminated on April 30, 2020, and data collection ended on May 23, 2020. For perspective, the first confirmed case of COVID‐19 in the US was reported about 3 months prior to the start of data collection (on January 20, 2020) (22), and beginning in early March 2020, almost all US states had ordered school closures (23). Parents were primarily recruited through social media advertisements on Facebook (Menlo Park, California). These advertisements targeted parents whose Facebook activity suggested they were from racial or ethnic minority backgrounds (e.g., Hispanic, African American), who reported lower educational attainment (e.g., high school degree, some college), and who lived in lower‐income ZIP codes in the US, in order to ensure a sample that included individuals most vulnerable to COVID‐19 impacts on food insecurity. Additional participants were recruited using a snowball technique by circulating the survey link via email to colleagues across several sectors (e.g., academic, health care workers, community partners, YMCAs, nonprofits, schools) and on list‐servs. The survey link was also posted on social media platforms, including Facebook parenting groups and on the Virginia Commonwealth University Facebook pages. Recruitment text encouraged individuals to share the link nationwide.
Parents who clicked on the link were directed to a secure website to complete the survey using Qualtrics (Provo, Utah). Completely Automated Public Turing test to tell Computers and Humans Apart (CAPTCHA) features were used to protect against bots. The survey began with screening questions that were first asked to ensure eligibility. Parents living in the US who were 18 years of age or older and had at least one child between 5 and 18 years of age were eligible. Being a parent of a school‐aged child was chosen as an eligibility criterion, given that these families were almost all impacted by school closures and the transition to online instruction (vs. parents of younger children who could have been at home or in a variety of different childcare settings). If parents had more than one child in this age range, they were asked to answer the survey according to the child whose weight most concerned them. Fifty‐eight individuals completed these screening questions and did not qualify. A total of 1,342 parents started the survey (e.g., completed at least one item), with 603 complete survey responses. Of these, 19 were deemed invalid (e.g., bots) and excluded, resulting in a final sample size of 584. Each parent in the final sample size was contacted to verify they were human. The full survey took approximately 20 minutes to complete. Parents were compensated with a $10 gift card upon survey completion. Given the minimal risks of participating, passive permission was used with an informational letter at the start of the survey. The study was approved by the Institutional Review Board of [redacted] University.
Measures
Food insecurity
Parent‐reported food security was assessed using the six‐item US Department of Agriculture Household Food Security Module (24). This short form reduces participant burden while still providing a reliable measure of food security with minimal bias (25). Parents responded to questions when thinking about their situation before the COVID‐19 pandemic and again when thinking about their situation during the pandemic. For the question pertaining to cutting or skipping meals, participants reported on the number of days this occurred in the past 30 days, with a response of ≥ 3 days considered as an affirmative response. Results for this item specifically are reported below, in order to provide a perspective on the change in frequency for which this had occurred. All affirmative responses were totaled, and participants were categorized as having either “high food security,” “low food security,” or “very low food security” based on retrospective reports pertaining to before COVID‐19, as well as current reports during COVID‐19. A change in food security status was quantified by identifying families whose food security status before the pandemic differed from that during the pandemic (e.g., having food security prior to the pandemic and having low or very low food security during the pandemic).
Household food environment
Seven items developed by the research team were used to assess family’s home food environment. Five of these questions asked about the amount of total food, high‐calorie snack foods (e.g., chips, crackers), desserts and sweets (e.g., cookies, cake), fresh foods (e.g., meat, fruits, vegetables), and nonperishable processed food (e.g., boxed or canned) in participants’ homes. Two questions asked about the amount of takeout/fast‐food/already prepared meals and home‐cooked meals. Respondents indicated whether each item was available in their home “much less,” “slightly less,” “about the same,” “slightly more,” or “much more” during the COVID‐19 pandemic, compared with before the pandemic, using a five‐point Likert scale. Response options were collapsed into three categories representing an increase (i.e., slightly more/much more), a decrease (i.e., slightly less/much less), or no change, from before to during the pandemic.
Parent feeding practices
Parent feeding practices were assessed using four subscales from the Child Feeding Questionnaire (CFQ) (11). Parents completed the CFQ twice, first when thinking about their situation prior to COVID‐19 and again when thinking about their current situation during COVID‐19. This validated measure has been widely used to assess parental beliefs, attitudes, and practices regarding child feeding and obesity proneness (26, 27). The subscales used included (1) parents’ concern about child overweight, (2) monitoring (i.e., extent to which parents supervise their child’s eating), (3) restriction (i.e., extent to which parents restrict child’s access to certain foods), and (4) pressure to eat (i.e., tendency to pressure child to eat more food). Each item was scored on a five‐point Likert‐type scale. Items within each subscale were averaged, and possible subscale scores ranged from 1 to 5.
Demographics and COVID‐19‐related questions
Demographic questions included parent and child age; parent and child sex; parent and child race/ethnicity; parent education, current family income, and marital status; insurance status; number of children and adults in the home; and parent‐perceived child weight status. COVID‐19‐related questions included personal and family diagnoses and related health outcomes; job layoffs, furloughs, income changes, or newly filed unemployment; changes to working from home; current stay‐at‐home state policies and social distancing practices; and use of government assistance benefits (including the Supplemental Nutrition Assistance Program; the Special Supplemental Nutrition Program for Women, Infants, and Children; and pick‐up school‐provided meals).
Statistical analysis
Descriptive statistics were calculated for all variables. This included mean and standard deviation for continuous variables and percentages for categorical variables. These descriptive statistics are representative of the full sample, unless otherwise noted. To describe changes in food security status, the percentage of parents that reported food security, low food security, and very low food security were calculated before and during COVID‐19. A χ2 test of independence was used to explore differences in aspects of the home food environment by food security status. Paired‐sample t tests examined whether there were significant changes in CFQ subscales from before to during COVID‐19. Changes were calculated as responses during COVID‐19 minus responses before COVID‐19, so that positive values indicated an increase. Values are reported as mean difference (95% confidence interval) and Cohen’s d where appropriate. Lastly, univariate regression models were used to test whether food security status during COVID‐19 was associated with changes in each of the CFQ subscales. Data were analyzed with SAS statistical software version 9.4 (SAS Institute Inc., Cary, North Carolina). Significance was determined a priori as P < 0.05.
Results
Demographics
Parent and child demographics are listed in Table 1. Most parents were white (83%), not Hispanic/Latino (85%), and married or in a domestic partnership (78%). Parent education and current household income varied, with approximately half of the sample earning ≤ $50,000/year. Just over half of families had private insurance (59%), while the remaining had Medicaid (35%) or no insurance (6%). Children were on average 9.6 ± 3.8 years of age, with 26.4% reported as having overweight or obesity. In total, there were an average of 2.2 ± 1.2 children and 2.1 ± 0.8 adults living in families’ homes.
Table 1.
Participant demographics in nationwide sample of US parents with child 5 to 18 years of age (N = 584)
| Variable | Parent | Child |
|---|---|---|
| Age, y (mean ± SD) | 40.4 ± 7.2 | 9.6 ± 3.8 |
| Female sex (%) | 94.5 | 52.1 |
| Race (%) | ||
| Caucasian/white | 82.7 | 82.4 |
| African American | 6.0 | 10.1 |
| Asian | 4.3 | 5.0 |
| American/Indian | 2.9 | 3.3 |
| Other | 6.5 | 9.1 |
| Hispanic/Latino (%) | 14.7 | 19.0 |
| Marital status (%) | ||
| Married or in domestic partnership | 78.1 | |
| Single | 14.2 | |
| Divorced or widowed | 7.7 | |
| Education (%) | ||
| High school degree or less | 19.0 | |
| Some college | 18.3 | |
| Associate’s degree | 14.4 | |
| Bachelor’s degree | 21.9 | |
| Some graduate school or more | 26.4 | |
| Current family income (%) | ||
| $25,000/y or less | 22.6 | |
| $25,000‐$50,000/y | 24.1 | |
| $50,000‐$75,000/y | 17.3 | |
| $75,000/y or more | 36.0 | |
| Insurance status (%) | ||
| Medicaid | 35.3 | |
| Private insurance | 58.9 | |
| No insurance | 5.8 |
COVID‐19 exposure and impact
At the time of survey completion, 1.7% of parents had been diagnosed with COVID‐19, and 9.3% had a family member diagnosed. In the full sample, few parents or their family members had become physically ill (7.7%), were hospitalized (3.6%), or were deceased (1.7%) because of COVID‐19. Almost all parents (98.3%) were practicing social distancing, while 71.4% were in voluntary self‐isolation (i.e., encouraged, not legally enforced), and 25.9% were in mandatory self‐isolation (i.e., legally enforced). About one‐fourth (27.6%) of parents reported working from home who did not previously work from home before the pandemic.
More than half (60.1%) of families experienced a decrease in income. Of those that did, most had low food security (23.4%) or very low food security (42.5%). About 40.9% experienced a job loss or were furloughed, and 34.6% filed for unemployment benefits. Pick‐up school‐provided meals were received by 40.0% of families, while 27.8% received Supplemental Nutrition Assistance Program benefits, 11.7% received WIC benefits, and 16.5% received meals from local food banks or food assistance programs.
Changes in household food security status
The distribution for the prevalence of food security before COVID‐19 differed from that during COVID‐19, as shown in Figure 1 (P < 0.01). Notably, the overall percentage of food‐secure families decreased by 17%, while the overall percentage of families experiencing very low food security increased by 20%. Of the households that were food secure before the pandemic, 15.6% experienced low food security, and 15.3% experienced very low food security during the pandemic. Of the households with low food security before the pandemic, 46.5% experienced very low food security during COVID‐19. Overall, few households reported a positive change in being food insecure before the pandemic to being food secure during the pandemic (2.3%) or going from very low food security to low food security from before to during the pandemic (1.7%). As part of the food security questionnaire (22), parents were asked whether and how often they cut meal sizes or skipped meals because there was not enough money for food; those with affirmative responses reported cutting or skipping meals an average of 2.9 ± 2.2 (range: 1‐8) days/month before the pandemic and 11.0 ± 7.5 (range: 2‐30) days/month during the pandemic.
Figure 1.
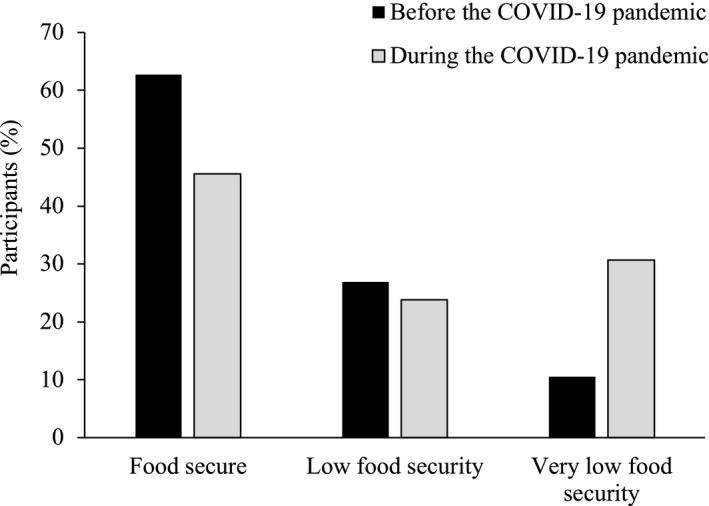
Distribution in the percentage of food‐secure and food‐insecure families differed from before the COVID‐19 pandemic (retrospective report) to during the COVID‐19 pandemic, in a nationwide sample of US parents with a child 5‐18 years of age (N = 584). A 3 × 3 χ2 analysis was used to test distribution differences (P < 0.01). COVID‐19, coronavirus disease 2019.
Home food environment
During COVID‐19, the majority of parents reported a decrease in their family’s consumption of takeout/fast‐food/already prepared meals (62.0%) and an increase in home‐cooked meals (73.3%). See Table 2 for the changes in the amount and types of foods in families’ homes. Overall, the total amount of food in the home increased for 42% of families and decreased for 23% of families. About one‐third of families reported an increase in the amount of high‐calorie snack foods and desserts/sweets in their home, while almost half reported an increase in nonperishable processed foods during the pandemic.
Table 2.
Home food environment changes during COVID‐19 pandemic, compared with before pandemic, in nationwide sample of US parents with a child age 5 to 18 years (N = 584)
| Amount of food in home during COVID‐19 pandemic by food category | Overall | Food security status during COVID‐19 | ||
|---|---|---|---|---|
| Food security | Low food security | Very low food security | ||
| Total food, P < 0.01 | ||||
| Increased (%) | 42.0 | 56.4 | 41.0 | 21.2 |
| Decreased (%) | 23.5 | 2.3 | 25.9 | 53.1 |
| Stayed the same (%) | 34.6 | 41.4 | 33.1 | 25.7 |
| High‐calorie snack foods, P < 0.01 | ||||
| Increased (%) | 33.2 | 32.7 | 33.1 | 34.1 |
| Decreased (%) | 20.0 | 10.2 | 25.9 | 30.2 |
| Stayed the same (%) | 46.8 | 57.1 | 41.0 | 35.8 |
| Desserts and sweets, P < 0.01 | ||||
| Increased (%) | 35.6 | 41.4 | 33.8 | 28.5 |
| Decreased (%) | 22.8 | 12.8 | 24.5 | 36.3 |
| Stayed the same (%) | 41.6 | 45.9 | 41.7 | 35.2 |
| Fresh foods, P < 0.01 | ||||
| Increased (%) | 37.0 | 35.7 | 38.1 | 38.0 |
| Decreased (%) | 21.8 | 10.9 | 23.7 | 36.3 |
| Stayed the same (%) | 41.3 | 53.4 | 38.1 | 25.7 |
| Nonperishable processed food, P < 0.01 | ||||
| Increased (%) | 46.6 | 40.6 | 46.0 | 55.9 |
| Decreased (%) | 13.0 | 8.3 | 21.6 | 13.4 |
| Stayed the same (%) | 40.4 | 51.3 | 32.4 | 30.7 |
Results are presented for the overall sample and by food security status during COVID‐19. Increased = greater during the COVID‐19 pandemic compared with before the pandemic. Decreased = lower during the COVID‐19 pandemic compared with before the pandemic. Stayed the same = no reported change during the COVID‐19 pandemic compared with before the pandemic. χ2 (3 × 3) analyses were conducted for each variable on home food environment changes by food security status.
COVID‐19, coronavirus disease 2019.
Distributions for changes in the amount of total food, high‐calorie snack foods, desserts/sweets, fresh foods, and nonperishable foods in the home differed by food security status (all P < 0.01). Total amount of food in the home increased for 56% of food‐secure families yet decreased for 53% of families experiencing very low food security. The amount of high‐calorie snack foods and desserts/sweets increased or remained the same for ~90% of food‐secure families yet decreased for ~30%‐36% of families experiencing low or very low food security. The amount of fresh foods in the home increased for about one‐third of families, across each food security status. In contrast, a decrease of fresh foods in the home was reported by 11% of food‐secure families, 24% of families with low food security, and 36% of families with very low food security. Furthermore, a greater percentage of families experiencing very low food security (56%) reported an increase in nonperishable processed foods during the pandemic, compared with 41% of food‐secure families.
Child feeding practices
Scores for parents’ concern about child overweight and use of controlling feeding practices, before and during COVID‐19, are shown in Table 3. Overall, parents’ concern about child overweight increased from before to during COVID‐19 (mean difference: 0.40 [95% CI: 0.88‐0.99]; P < 0.01). Parent‐reported use of restrictive feeding practices, pressure to eat, and monitoring also increased (restriction: 0.23 [95% CI: 0.62‐0.69]; P < 0.01; pressure: 0.15 [95% CI: 0.57‐0.64]; P < 0.01; monitoring: 0.18 [95% CI: 0.69‐0.78]; P < 0.01).
Table 3.
Subscale scores (mean ± SD) for parent feeding practices reported on Child Feeding Questionnaire, pertaining to before and during COVID‐19 pandemic in nationwide sample of US parents of children age 5 to 18 years (N = 584)
| Overall | P a | Cohen’s d | Food security status during COVID‐19 | P b | |||
|---|---|---|---|---|---|---|---|
| Food security | Low food security | Very low food security | |||||
| Concern about child overweight c | < 0.01 | 0.42 | < 0.01 | ||||
| Before COVID‐19 | 2.4 ± 1.3 | 2.2 ± 1.3 | 2.6 ± 1.4 | 2.5 ± 1.3 | |||
| During COVID‐19 | 2.8 ± 1.5 | 2.5 ± 1.4 | 3.1 ± 1.5 | 3.1 ± 1.5 | |||
| Restriction | < 0.01 | 0.35 | 0.08 | ||||
| Before COVID‐19 | 3.1 ± 1.0 | 3.0 ± 0.9 | 3.2 ± 1.0 | 3.2 ± 1.0 | |||
| During COVID‐19 | 3.4 ± 1.1 | 3.2 ± 1.0 | 3.5 ± 1.0 | 3.5 ± 1.1 | |||
| Pressure c | < 0.01 | 0.24 | < 0.01 | ||||
| Before COVID‐19 | 2.6 ± 1.1 | 2.4 ± 1.1 | 2.7 ± 1.2 | 2.8 ± 1.1 | |||
| During COVID‐19 | 2.8 ± 1.2 | 2.4 ± 1.1 | 2.9 ± 1.2 | 3.2 ± 1.2 | |||
| Monitoring | < 0.01 | 0.24 | 0.08 | ||||
| Before COVID‐19 | 3.4 ± 1.1 | 3.4 ± 1.1 | 3.3 ± 1.2 | 3.5 ± 1.2 | |||
| During COVID‐19 | 3.6 ± 1.1 | 3.5 ± 1.1 | 3.5 ± 1.0 | 3.7 ± 1.2 | |||
Possible subscale scores ranged from 1 to 5.
Tested for differences in mean values of each subscale in the overall sample from before to during COVID‐19.
Tested for differences in mean values of each subscale from before to during COVID‐19 by food security status.P values listed are for the overall test. Specific comparisons, in which mean differences for low and/or very low food security differed from food security, are bolded if significant.
All P < 0.01 for mean differences (during COVID‐19 minus before COVID‐19) for low food security versus food security and/or very low food security versus food security.
COVID‐19, coronavirus disease 2019.
Changes in parents’ concern about child overweight and use of controlling feeding practices differed by food security status. Families with low food security and very low food security reported greater increases in concern about child overweight, compared with food‐secure families (Table 3; P < 0.01). Parents’ increased use of pressure feeding practices was greater for families with low and very low food security, compared with food‐secure families (all P < 0.05). There were no differences in the increased use of restriction or monitoring by food security status (all P > 0.05).
Discussion
This study highlights concerning changes to families’ food security, home food environment, and parent feeding practices, from before to during the COVID‐19 pandemic, among parents living in the US. During the pandemic, parents reported an increase in concern about child overweight and use of controlling feeding practices. Many families also reported an increase in the total amount of food in their homes, with about one‐third having increased the amount of unhealthy foods (e.g., desserts/sweets) and also fresh foods (e.g., fruits, vegetables). There was a substantial increase in the percentage of families experiencing very low food security during the pandemic, and for these families in particular, greater increases in concern about child overweight and use of controlling feeding practices were observed, compared with food‐secure families. These changes highlight the need to mitigate possible adverse effects on children’s health and nutrition because of COVID‐19.
Experts have raised concern regarding children’s weight gain and obesity during COVID‐19 (6, 28), which arose primarily because of school closures, causing children to experience more than double their typical out‐of‐school time (6). Multiple studies have shown accelerated weight gain for children during the summer months (29, 30, 31), during which eating behaviors, physical activity, sleep, and routines/structure often change in ways that support weight gain (31). Our data suggest that parents also have a heightened concerned about child overweight during the COVID‐19 pandemic, with a greater increase in child weight concern for food‐insecure families. Families experiencing food insecurity during COVID‐19 are likely more impacted by the school closures, given that school meals typically provide low‐income children with necessary nutrients each day (10). In the midst of this pandemic, it has become increasingly important to support programs and policies that provide access to healthy meals for food‐insecure families (5). For example, the US Department of Agriculture instituted waivers and flexibilities to help maintain school‐provided meals for families most at need while navigating the social distancing mandates (32). Moving into the summer months and beyond, these initiatives and other safety net programs need our nation’s full support. Suggested approaches for addressing food insecurity and feeding low‐income children during COVID‐19 are well‐described elsewhere (5, 33, 34) and include amending policies to increase participation and benefits for nutrition safety net programs, innovative ways to provide meals through pickup or delivery, and elevating voices in communities that have been marginalized in order to learn how to best serve these populations. Furthermore, research funding and clinical interventions are essential to supporting evidence‐based obesity prevention and treatment programs that can help improve the health and well‐being of children who may have experienced substantial weight gain during this time. Primary care physicians should be actively informed about the enhanced public health crisis around childhood obesity, and clinics should ensure that pediatricians are well‐equipped to help address these concerns, including the use of COVID‐19 resources provided by the American Academy of Pediatrics (35). Addressing weight gain during this pandemic and beyond will require compassion, empathy, non‐stigmatization, and particular attention to the many unique and challenging factors that families are currently facing.
About one‐third of parents in the current study reported an increase in the amount of high‐calorie snack foods and desserts/sweets in their home, while almost half reported an increase in the amount of nonperishable, processed foods. With children spending more time at home, the types/amounts of food in families’ home food environments have become more salient for shaping children’s dietary intake. During this pandemic, grocery store purchasing patterns indicate that families are stocking up on more shelf‐stable, calorie‐dense “comfort foods”; (36) our data also support this trend for many families. Future research is needed to now quantify how greater access to these foods in the home have impacted children’s dietary intake. A small study in Italy found that children and adolescents consumed more potato chips, red meat, sugary drinks, and fruit after 3 weeks of mandatory stay‐at‐home confinement during COVID‐19 (37). Negative effects on children’s nutrition may result if greater access to and consumption of these calorie‐dense foods, which are often high in saturated fat and added sugar, persist for many months. On a positive note, it is also important to mention that the amount of fresh foods in families’ homes also increased for 37% of families in this study, suggesting that many children also have greater access to healthy foods at home during this pandemic. Most families reported consuming more home‐cooked meals and less takeout, fast‐food, and already prepared meals during COVID‐19, which may have positive impacts for some children given that home‐cooked meals tend to be healthier (38, 39) and provide opportunities for more family time and communication (40, 41). Regarding food insecurity, it is concerning that half of families with very low food security reported a decrease in the total amount of food in their homes during the pandemic. This finding reinforces the importance for safety net programs to adjust and meet the needs of disadvantaged families during this time, in order to prevent a further increase in health disparities.
Overly controlling parent feeding practices limit children’s ability to regulate energy intake and are associated with child weight and unhealthy eating behaviors (16, 17, 18, 19, 20, 21, 42). Parents reported a greater use of controlling feeding practices, including increased pressure and restriction of children’s eating during COVID‐19. The increased use of controlling feeding practices may be due to a variety of reasons, including maternal psychosocial factors and/or child characteristics (43). For example, parents with increased anxiety during the pandemic could have also increased their use of restrictive feeding practices (43), which have been associated with greater consumption of restricted foods when given access (44, 45). A greater use of pressure to eat could be due to a perceived lack of food access and wanting children to consume enough, particularly for families experiencing food insecurity. With parents reporting that they cut or skipped meals an average of 11 d/mo during the pandemic (8 more days than they did prior to COVID‐19), the uncertainty and shortage of food availability could have contributed to parents trying to ensure their child had enough to eat. Greater parental monitoring could have been due to less structure/routines at home, compared with at school, and greater access to food throughout the day, so parents felt they needed to more closely monitor what their children were eating. The magnitude of change in parent feeding practices found in this study showed small to medium effect sizes yet is comparable to a recent study that also found greater pressure to eat and concern about child overweight among parents of younger children from food‐insecure households (46). The lack of a clinically meaningful threshold or magnitude of change for CFQ subscales on outcomes such as child BMI makes the interpretation of these values in the context of clinical outcomes challenging. Most studies report correlations between CFQ subscales and child BMI, showing, for example, that greater restriction is associated with higher BMI and pressure to eat is associated with lower BMI (47). It is notable that changes to parent feeding practices observed in this study were reported to occur over a very short period of time (i.e., reflecting only a few months) and have the potential to continue to be negatively impacted given the persistence of the COVID‐19 pandemic in the US. While more research is needed to fully understand the specific reasons as to why parent feeding practices may have changed for families during the COVID‐19 pandemic, these data are an important first step in recognizing how this pandemic may be affecting parent feeding, so that future obesity prevention and treatment initiatives can account for these changes moving forward. Furthermore, this serves as evidence for the potential changes in parent feeding that may arise in future pandemics or national crises of a similar scale.
The limitations of this study include the use of a convenience sample that is not nationally representative of all US parents. There was limited racial/ethnic diversity across survey respondents, thus limiting generalizability; however, there was a range of family income and educational diversity represented. Parenting behaviors likely varied based on local laws and infection rates that differed across states at the time of survey completion; therefore, these findings represent average changes across respondents’ locations. Preliminary data reported here show that 54% of families were food insecure (low and very low food insecurity) during COVID‐19; yet larger, nationally representative data sets should be used to further examine changes in food insecurity on a national level. For example, the US Census Household Pulse Survey showed that 50% of households with children reported food insufficiency and 30% reported food insecurity during COVID‐19, according to data collected during a similar time period as this study (48). Furthermore, all survey measures that examined constructs prior to COVID‐19 were retrospective self‐report. Given the sudden and unexpected nature of this pandemic, it was not feasible to obtain baseline measures before the start of the pandemic in this sample; yet this survey was administered only a few months after the start of the pandemic, thus minimizing the duration of parents’ retrospective recall. Questions related to the home food environment were developed by experts on the study team and are not validated measures. Lastly, this study measured factors associated with children’s dietary intake and eating behaviors yet did not measure these constructs directly. Future research should examine whether there have been changes to children’s dietary intake and eating behaviors during COVID‐19. Despite these limitations, this study provides important and timely data on how families’ home food environment and parent feeding practices have changed during this global pandemic.
Conclusion
This study shows that, in the midst of COVID‐19, more families are experiencing very low food security and that changes in the home food environment and parent feeding practices have occurred. Given the uncertainty of how long the effects of COVID‐19 will last, continual assessment of children’s health and nutrition are needed to examine whether these effects are sustained or change over time. These data can be used by public health professionals, policy makers, and researchers to inform the development and implementation of public health interventions to reduce the negative impacts of COVID‐19 on children’s obesity risk. Such initiatives can help families to resume more positive feeding practices and reduce subsequent obesity risk following the pandemic.
Funding agencies
This study was funded by the Virginia Commonwealth University COVID‐19 Rapid Research Funding program. This work was also supported by the National Institutes of Health (2T32CA093423) for ELA’s postdoctoral work.
Disclosure
The authors declared no conflict of interest.
Author contributions
ELA and MKB conceptualized the research questions and obtained grant funding. ELA completed data collection and data analyses and drafted the initial version of the manuscript. All authors designed the study, interpreted the data, critically reviewed the manuscript, and approved the final version as submitted.
References
- 1. U.S. Department of Labor . Unemployment insurance weekly claims [news release]. Updated October 2020. Accessed June 8, 2020. https://www.dol.gov/ui/data.pdf
- 2. Feeding America . The impact of the coronavirus on food insecurity. Updated April 22, 2020. Accessed June 8, 2020. https://hungerandhealth.feedingamerica.org/wp‐content/uploads/2020/03/Brief_Impact‐of‐Covid‐on‐Food‐Insecurity‐4.22.pdf
- 3. Measurement information page . Food security in the U.S. United States Department of Agriculture Economic Research Service. Updated September 9, 2020. Accessed June 8, 2020. https://www.ers.usda.gov/topics/food‐nutrition‐assistance/food‐security‐in‐the‐us/measurement.aspx
- 4. Coleman‐Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States in 2018. Economic Research Report Number 270. U.S. Department of Agriculture, Economic Research Service; 2019. [Google Scholar]
- 5. Dunn CG, Kenney E, Fleischhacker SE, Bleich SN. Feeding low‐income children during the COVID‐19 pandemic. New Eng J Med 2020;382:e40. doi: 10.1056/NEJMp2005638 [DOI] [PubMed] [Google Scholar]
- 6. Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID‐19‐related school closing and risk of weight gain among children. Obesity (Silver Spring) 2020;28:1008‐1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lancker WV, Parolin Z. COVID‐19 school closures, and child poverty: a social crisis in the making. Lancet Public Health 2020;5:E243‐E244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pérez‐Escamilla R, Cunningham K, Moran VH. COVID‐19, food and nutrition insecurity and the wellbeing of children, pregnant and lactating women: a complex syndemic. Matern Child Nutr 2020;16:e13036. doi: 10.1111/mcn.13036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rao M, Afshin A, Singh G, Mozaffarian D. Do healthier foods and diet patterns cost more than less healthy options? A systematic review and meta‐analysis. BMJ Open 2013;3:e003277. doi: 10.1136/bmjopen-2013-004277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Weber Cullen K, Chen TA. The contribution of the USDA school breakfast and lunch program meals to student daily dietary intake. Prev Med Rep 2017;5:82‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Birch LL, Fisher JO, Grimm‐Thomas K, Markey CN, Sawyer R, Johnson Sl. Confirmatory factor analysis of the Child Feeding Questionnaire: a measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite 2001;36:201‐210. [DOI] [PubMed] [Google Scholar]
- 12. Berge JM, Tate A, Trofholz A, et al. Momentary parental stress and food‐related parenting practices. Pediatrics 2017;140:e20172295. doi: 10.1542/peds.2017-2295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kral TVE, Chittams J, Moore RH. Relationship between food insecurity, child weight status, and parent‐reported child eating and snacking behaviors. J Spec Pediatr Nurs 2017;22: e12177. doi: 10.1111/jspn.12177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Panchal N, Kamal R, Orgera K, et al.The implications of COVID‐19 for mental health and substance use. Kaiser Family Foundation. Updated August 21, 2020. Accessed June 8, 2020. https://www.kff.org/coronavirus‐covid‐19/issue‐brief/the‐implications‐of‐covid‐19‐for‐mental‐health‐and‐substance‐use/
- 15. Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. Int J Environ Res Public Health 2020;17:1729. doi: 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Savage JS, Fisher JO, Birch LL. Parental influence on eating behavior: conception to adolescence. J Law Med Ethics 2007;35:22‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ventura AK, Birch LL. Does parenting affect children’s eating and weight status? Int J Behav Nutr Phys Act 2008;5:15. doi: 10.1186/1479-5868-5-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Faith M, Scanlon K, Birch LL, Francis LA, Sherry B. Parent‐child feeding strategies and their relationship to child eating and weight status. Obes Res 2004;12:1711‐1722. [DOI] [PubMed] [Google Scholar]
- 19. Birch LL, Fisher JO. Development of eating behaviours among children and adolescents. Pediatrics 1998;101:539‐549. [PubMed] [Google Scholar]
- 20. Fisher JO, Birch LL. Restricting access to foods and children's eating. Appetite 1999;32:405‐419. [DOI] [PubMed] [Google Scholar]
- 21. Spruijt‐Metz D, Lindquist CH, Birch LL, Fisher JO, Goran MI. Relation between mothers' child‐feeding practices and children's adiposity. Am J Clin Nutr 2002;75:581‐586. [DOI] [PubMed] [Google Scholar]
- 22. Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020;382:929‐936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Education Week . Map: coronavirus and school closures in 2019‐2020. Published March 6, 2020. Accessed June 8, 2020. https://www.edweek.org/ew/section/multimedia/map‐coronavirus‐and‐school‐closures.html
- 24. United States Department of Agriculture Economic Research Service . U.S. household food security survey module: six‐item short form. Published September 2012. Accessed June 8, 2020. https://www.ers.usda.gov/media/8282/short2012.pdf
- 25. Blumberg SJ, Bialostosky K, Hamilton WL, Briefel RR. The effectiveness of a short form of the household food security scale. Am J Public Health 1999;89:1231‐1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vaughn AE, Tabak RG, Bryant MJ, Ward DS. Measuring parent food practices: a systematic review of existing measures and examination of instruments. Int J Behav Nutr Phys Act 2013;10:61. doi: 10.1186/1479-5868-10-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. De Lauzon‐Guillain B, Oliveira A, Charles MA, et al. A review of methods to assess parental feeding practices and preschool children's eating behavior: the need for further development of tools. J Acad Nutr Diet 2012;112:1578‐1602. [DOI] [PubMed] [Google Scholar]
- 28. An R. Projecting the impact of COVID‐19 pandemic on childhood obesity in the U.S.: a microsimulation model. J Sport Health Sci 2020;9:302‐312. doi: 10.1016/j.jsh.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Franckle R, Adler R, Davison K. Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: a systematic review. Prev Chronic Dis 2014;11:E101. doi: 10.5888/pcd11.130355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Von Hippel PT, Workman J. From kindergarten through second grade, U.S. children's obesity prevalence grows only during summer vacations. Obesity (Silver Spring) 2016;24:2296‐2300. [DOI] [PubMed] [Google Scholar]
- 31. Wang YC, Vine S, Hsiao A, Rundle A, Goldsmith J. Weight‐related behaviors when children are in school versus on summer breaks: does income matter? J Sch Health 2015;85:458‐466. [DOI] [PubMed] [Google Scholar]
- 32. No Kid Hungry. Center for Best Practices. Summary of COVID‐19 child nutrition program response nationwide waivers & memos. Updated June 1, 2020. Accessed September 14, 2020. http://bestpractices.nokidhungry.org/sites/default/files/2020-09/COVID%20CNP%20Waiver%20%20Memo%20Summary_9-14-20_0.pdf
- 33. Dooley DG, Bandealy A, Tschudy MM. Low‐income children and coronavirus disease 2019 (COVID‐19) in the US [published online May 13, 2020]. JAMA Pediatr 2020. doi: 10.1001/jamapediatrics.2020.2065 [DOI] [PubMed] [Google Scholar]
- 34. Fleischhacker S, Campbell E. Ensuring equitable access to school meals. J Acad Nutr Diet 2020;120:893‐897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. COVID‐19 information page . American Academy of Pediatrics website. Accessed July 9, 2020. https://www.healthychildren.org/English/health‐issues/conditions/COVID‐19/Pages/default.aspx
- 36. Creswell J. ‘I just need the comfort’: processed foods make a pandemic comeback. The New York Times. April 7, 2020. Accessed June 8, 2020. https://www.nytimes.com/2020/04/07/business/coronavirus-processed-foods.html [Google Scholar]
- 37. Pietrobelli A, Pecoraro L, Ferruzzi A, et al. Effects of COVID‐19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity (Silver Spring) 2020;28:1382‐1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hammons AJ, Fiese BH. Is frequency of shared family meals related to the nutritional health of children and adolescents? Pediatrics 2011;127:e1565‐e1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Fertig AR, Loth KA, Trofholz AC, et al. Compared to pre‐prepared meals, fully and partially home‐cooked meals in diverse families with young children are more likely to include nutritious ingredients. J Acad Nutr Diet 2019;119:818‐830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ochs E, Shohet M. The cultural structuring of mealtime socialization. New Dir Child Adolesc Dev 2006;111:35‐49. [DOI] [PubMed] [Google Scholar]
- 41. Fulkerson JA, Pasch KE, Stigler MH, Farbakhsh K, Perry CL, Komro KA. Longitudinal associations between family dinner and adolescent perceptions of parent‐child communication among racially‐diverse urban youth. J Fam Psychol 2010;24:261‐270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Johnson SL, Birch LL. Parents’ and children’s adiposity and eating style. Pediatrics 1994;94:653‐661. [PubMed] [Google Scholar]
- 43. Mitchell S, Brennan L, Hayes L, Miles CL. Maternal psychosocial predictors of controlling parental feeding styles and practices. Appetite 2009;53:384‐389. [DOI] [PubMed] [Google Scholar]
- 44. Birch LL, Fisher JO, Davison KK. Learning to overeat: maternal use of restrictive feeding practices promotes girls’ eating in the absence of hunger. Am J Clin Nutr 2003;78:215‐220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Fisher JO, Birch LL. Eating in the absence of hunger and overweight in girls from 5 to 7 y of age. Am J Clin Nutr 2002;76:226‐231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Orr CJ, Ravanbakht S, Flower KB, et al. Associations between food insecurity and parental feeding behaviors of toddlers [published online June 1, 2020]. Acad Pediatr 2020. doi: 10.1016/j.acap.2020.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hurley KM, Cross MB, Hughes SO. A systematic review of responsive feeding and child obesity in high‐income countries. J Nutr 2011;141:495‐501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Schanzenbach D, Pitts A. How much has food insecurity risen? Evidence from the Census Household Pulse Survey. Institute for Policy Research (IPR) Rapid Research Report. Northwestern Institute for Policy Research. Published June 10, 2020. Accessed July 12, 2020. Updated September 9, 2020. https://www.ipr.northwestern.edu/documents/reports/ipr‐rapid‐research‐reports‐pulse‐hh‐data‐10‐june‐2020.pdf [Google Scholar]


