Over the last decade, social media has come to influence human lives in a manner that is unprecedented in its scale and magnitude. Of course, medicine has not been left untouched from its impact. In this extraordinary once-in-a-generation situation of a global lockdown that has redefined and obfuscated international borders, at the same time, the curtailment of physical mobility has led a heretofore upwardly mobile, ambitious generation of home-bound individuals to rediscover social media platforms (SMPs) with an even greater vengeance. Donning innovative roles, social media has captured new horizons and has come to play a central role in continued medical education, dissemination of scientific information, peer review, online discussions, and many more during the current pandemic (Figure).1
FIGURE.
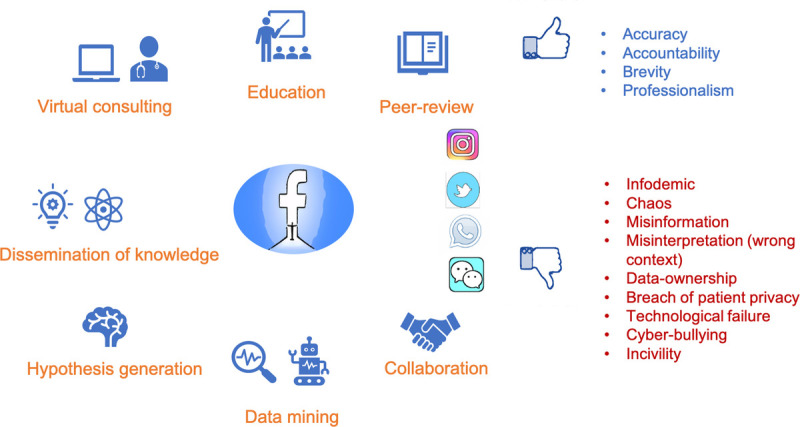
Social media—utility and pitfalls. Color online-figure is available at http://www.jclinrheum.com.
A literature search on MEDLINE and Scopus databases, using terms “social media” and “COVID-19,” yields nearly 100 publications that have appeared in the space of the last 4 months. For the purpose of this review, relevant articles were chosen, and the data pooled to gain insight into the prevalent practices. Written permissions were obtained from the editors of the Journal of Clinical Rheumatology to analyze and publish their social media data.
While most articles discussed the role of SMPs in the dissemination of information, a significant proportion (17/57 [30%]) expressed concern regarding the potential for misinformation.2,3 Another 36.8% were original articles, of which 6 were e-surveys and 15 data mining-based studies, most of which dealt with the prediction of the pandemic, with extrapolations drawn by geolocation linked social media messages with a time-sensitive model.4,5 A few referred to social media networks such the Diabetes UK for providing useful patient-related information and infographics for visually simulative learning among physicians.6
ROLE OF SOCIAL MEDIA PLATFORMS IN THE DISSEMINATION OF INFORMATION
Amid social distancing protocols, health care workers (HCWs) and medical students are using SMPs to access scientific literature.7,8 In the current pandemic, it has been noticed that although recommendations do not come with a use-by date, many guidelines appear to have an extremely short half-life. As their contribution, numerous journals have provided open access to COVID-19 articles. In contrast, others have announced special supplements dedicated to the situation, and authors clamor to upload preprints not only for early visibility but also wider dissemination.9,10 The COVID-19 Open Research Dataset is an open data set floated by a coalition between federal and research organizations to meet the challenge of rapid accelerations in COVID-19 literature.11 While Twitter has emerged as a global SMP of choice, use is also dependent on regional preference. Hence, in India, WhatsApp is accepted, but in China, WeChat may be more popular.12–15 The Twitter account of Journal of Clinical Rheumatology (@Jrheumatology) has recorded a 72.0% rise in tweet impressions and 95.4% increase in profile visits over the past month. Various strategies have been used for exponential dissemination of literature to the target audience, and infographics circulated on SMPs have found instant acceptance.15,16
DISTANCE LEARNING
In the words of Moran, “the process of teaching and learning mediated by technologies, where teachers and students are separated spatially and/or temporally” is the best conceptualization of distance education.17 Distance education has been used effectively for focused training of HCWs, volunteers, and also the community. Many federal agencies have used these platforms to train health care providers to improve surge capacity.18 Training undergraduate medical students and educated volunteers are being explored.19 Community preparedness to deal with a fomite and droplet borne disease can have far-reaching advantages. Mass education may be effective through portals such as Twitter and YouTube, but it may also be challenging to change people's preconceptions or political biases.1
REMOTE MONITORING AND HEALTH CARE
Over the last decade, health care monitoring and delivery have become increasingly distant, often the provider and the recipient have been separated not only in space but also in time. Mobile technology, coupled with the internet of things, has revolutionized monitoring and therapy. Today, with rapid cellular networks and widespread smartphone usage, the exchange of medical images and reports, has become routine.20 Telemedicine had come a long way from the time when an electrocardiogram was first transmitted over telephone lines.21 It could reduce in-person visits by 25% to 75% across specialties, including rheumatology.22–24 Virtual consulting has reduced mortality and length of hospital stay even in critical care settings.25 In developed countries with an established infrastructure, linking the app-based services with the hospital information services could provide a reliable record base of future reference as soon as logistics to resolve legal and insurance issues are developed.26 Ironically, with the advent of COVID-19, some of the most ardent critics of telemedicine have adopted e-consultations and begun accepting patient-reported outcome measures. Consequently, government agencies in developing countries are recognizing and legitimizing remote health care delivery and virtual consultation.27 Community paramedicine or mobile-integrated health care programs using smartphone app-based trackers may transform health care delivery.28
However, recent events of technological failure with Zoom calls throw light on the vulnerabilities of a poor electronic construct. This domain merits improvisation in the times to come, especially as they handle sensitive information such as patient data during e-consults. Although video conferencing may be more expensive in terms of equipment procurement, the patient-related cost in terms of time, transport, and the risk of COVID-19 can be mitigating factors.29 Notwithstanding the advances in health care technology, providers and recipients need to be equally mindful of blurring patient-physician relationships, opportunities for traps related to claims, malpractice, quackery, and false litigations.30
RESEARCH ON SOCIAL MEDIA PLATFORMS
The integration of online SMPs not only has made research more exciting but also has increased the reach of investigators manifold. Social media platforms may evolve into useful tools to gather survey information from wider, although still often biased, audiences.31,32 Opinion-based surveys can be the first step toward an evidence base to guide more structured studies.7 The Global Rheumatology Alliance has rapidly generated comprehensive data amid widespread concerns over the use of immunosuppressants.33,34
Artificial intelligence–mediated data-mining tools are being used to synthesize information out of social media discussions relevant to the pandemic.5,35 The use of geocoded and time-stamped tweets to develop prediction models in real time holds potential as a guiding resource for federal agencies, pending further validation. Social media can aid in containment of the COVID-19 pandemic, as well-planned analyses of online exchanges may provide for rapid assessment of the spread of the disease.5
LIMITATIONS OF SOCIAL MEDIA: POTENTIAL FOR MISINFORMATION
The greatest strength of SMPs is also their principal limitation. Because information is widely accessible and immediately available, it may also not be immediately reliable. Information constructs based on flawed hypotheses can easily find their way to a naive audience through an unregulated maze, resulting in the establishment of many myths before facts can be presented. Health care providers making clinical decisions need to be trained in quickly surfing through a haystack to find the needle.3,36,37
Not only have the authors been caught in a rush to publish, but the journals have also been trapped. Consequently, established peer-review processes may be impaired, and low-quality studies may find their way into high-impact journals, gaining a wider, and undeserved, audience. Incivility and cyberbullying have been another bane of free social media access.38,39 Human psychology experiments have suggested that the knowledge of being monitored may restore cognitive self-awareness of asocial behavior.40 Thus, policing of social media posts may help pull the brakes on exaggerated intuitive and emotional responses. Although unethical promotion of scientific misinformation for economic gains amounts to serious professional misconduct, there is often no penalty.41,42 Lamentably, this pandemic has exposed our world to a series of threats, and moral failure may be one of the most damaging ones.43,44
MEDICAL JOURNALS AND SOCIAL MEDIA
Medical journals have evolved rapidly over the last few decades and have transformed into gatekeepers and possibly trendsetters for current research. As the newest frontier, social media holds exciting opportunities and unforeseen challenges for both authors and editors alike. However, with the advantage comes the responsibility of a much larger reach to the public.
Rheumatologists and Immunologists have found themselves uniquely endowed with viral pathogenic and therapeutic insights as well as the skill-set to manage a critical illness.45 The artistry of this jack-of-all-trades among physicians can find utility in identifying valid evidence. This would be the first step toward going through reams of scientific information with the intent to verify and subsequently curate and deliver it to the right audience. Academicians, in general, and social media editors (SMEs), in particular, can assume this more substantial role of infodemic warriors in these times of scientific and moral failure amid plenty.
To date, 17 rheumatology journals have SMEs and Twitter accounts.1 Collaborative networks between official journal accounts can have a rapid and powerful social media presence with wide dissemination of credible information.13,46 Scientific societies at the local, national, and international levels can be approached to inform and direct subscribers to follow these networks. It might be prudent to embark on the challenging task of creating separate platforms for HCWs and patients to avoid mass panic from adverse scientific observations. This may be particularly important as social media may potentially be the invincible force soon.
The challenge and responsibility for an important role can incentivize SMEs toward handling the delicate synthesis of scientific literature on COVID-19 and correspondences on them. Creating alliances can reduce the burden on individual SMEs, whereas COVID-19 clinical duties keep them busy. Bots and automatic algorithms may come in handy for performing scheduled and unscheduled checks as well as sending reminders on the rules, including, but not limited to, forbidden personal opinions and biased statements on official platforms. For infographics and images, mandatory checks on copyright violations before circulation on social media could be the domain of SMEs. Lastly, didactic communication, such as journal clubs on Twitter, can facilitate crowd engagement on open-source platforms. These could be prioritized, hopefully replacing popular beliefs with definite answers. In such times, the academician community needs to come together for a powerful and credible social media presence.
In conclusion, social networks have become central to the rapid dissemination of scientific information and for administrative pandemic monitoring and control. Medical journals have promptly espoused online discussions, peer review, and scholarly collaboration to allow SMPs to attain a formidable medical research position despite initial limitations. In collaborative social media networks lies the potential to lead the way forward by delivering valid scientific observations in an organized manner to the appropriate audience.
Footnotes
L.G. is the social media editor of the Journal of Clinical Rheumatology and the Indian Journal of Rheumatology. The authors declare no conflict of interest.
Author Contributions: Both authors were involved in ideation, data collection, and manuscript preparation. Both agree with the submitted version of the article, take responsibility for the content of the entire manuscript, and affirm that any queries related to any aspect of the same would be appropriately managed.
REFERENCES
- 1.Zimba O, Radchenko O, Strilchuk L. Social media for research, education and practice in rheumatology. Rheumatol Int. 2020;40:183–190. [DOI] [PubMed] [Google Scholar]
- 2.Hua J, Shaw R. Corona virus (COVID-19) “infodemic” and emerging issues through a data lens: the case of China. Int J Environ Res Public Health. 2020;17:2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bastani P, Bahrami MA. COVID-19 related misinformation on social media: a qualitative study from Iran (preprint). J Med Internet Res. 2020. [DOI] [PubMed] [Google Scholar]
- 4.George DR, Rovniak LS, Kraschnewski JL. Dangers and opportunities for social media in medicine. Clin Obstet Gynecol. 2013;56:453–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li C Chen LJ Chen X, et al. Retrospective analysis of the possibility of predicting the COVID-19 outbreak from internet searches and social media data, China, 2020. Euro Surveill. 2020;25:2000199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iacobucci G. COVID-19: diabetes clinicians set up social media account to help alleviate patients' fears. BMJ. 2020;368:m1262. [DOI] [PubMed] [Google Scholar]
- 7.Gupta L Misra DP Agarwal V, et al. Management of rheumatic diseases in the time of covid-19 pandemic: perspectives of rheumatology practitioners from India. Annals of the Rheumatic Diseases. 2020. doi:10.1136/annrheumdis-2020-217509. [DOI] [PubMed] [Google Scholar]
- 8.Agarwal V Gupta L Davalbhakta S, et al. A Survey-Based Study on the Knowledge, Attitude, and the Practices Pertaining to the 2019 Novel Corona Virus Infection Amongst Undergraduate Medical Students in India.. Medarxiv. 2020. 10.1101/2020.04.11.20061333. [DOI]
- 9.deBronkart Dave. Open access as a revolution: knowledge alters power. J Med Internet Res. 2019;21:e16368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Open access to COVID-19 and related research. Available at: https://www.openaccess.nl/en/open-access-to-COVID-19-and-related-research. Accessed May 10, 2020.
- 11. COVID-19 Open Research Dataset Challenge (CORD-19). Available at: https://www.kaggle.com/allen-institute-for-ai/CORD-19-research-challenge.
- 12.Ahmed S, Gupta L. Perception about social media use by rheumatology journals: survey among the attendees of IRACON 2019. Indian J Rheumatol. doi: 10.4103/injr.injr_15_20 [published ahead of print]. [Google Scholar]
- 13.Allen CG Andersen B Chambers DA, et al. Twitter use at the 2016 Conference on the science of dissemination and implementation in health: analyzing #DIScience16. Implement Sci. 2018;13:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cardona-Grau D. Join the discussion on Twitter! J Pediatr Urol. 2016;12:334. [DOI] [PubMed] [Google Scholar]
- 15.McHeyzer-Williams LJ, McHeyzer-Williams MG. Our year on Twitter: science in #SocialMedia. Trends Immunol. 2016;37:260–265. [DOI] [PubMed] [Google Scholar]
- 16.Chan AKM Nickson CP Rudolph JW, et al. Social media for rapid knowledge dissemination: early experience from the COVID-19 pandemic. Anaesthesia. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nikolov R, Nikolova I. Distance Education in Schools: Perspectives and Realities. In: Voogt J, Knezek G, editors. International Handbook of Information Technology in Primary and Secondary Education vol. 20 Boston, MA: Springer US; 2008. p. 659–674. [Google Scholar]
- 18.Liew MF Siow WT MacLaren G, et al. Preparing for COVID-19: early experience from an intensive care unit in Singapore. Crit Care. 2020;24:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Joint statement: early provisional registration for final year medical students. Available at: https://www.gmc-uk.org/news/news-archive/early-provisional-registration-for-finalyear-medical-students. Accessed May 10, 2020.
- 20. History of telemedicine. Available at: http://mdportal.com/education/history-oftelemedicine/. Accessed May 10, 2020.
- 21.Chellaiyan V, Nirupama A, Taneja N. Telemedicine in India: where do we stand? J Family Med Prim Care. 2019;8:1872–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ahmed S Kelly YP Behera TR, et al. Utility, appropriateness, and content of electronic consultations across medical subspecialties. Ann Intern Med. 2020;172:641–647. [DOI] [PubMed] [Google Scholar]
- 23.Vimalananda VG, Fincke BG. Electronic consultations: complexities and promise. Ann Intern Med. 2020;172:693–694. [DOI] [PubMed] [Google Scholar]
- 24.Katz IJ Pirabhahar S Williamson P, et al. iConnect CKD—virtual medical consulting: a web-based chronic kidney disease, hypertension and diabetes integrated care program. Nephrol Ther. 2018;23:646–652. [DOI] [PubMed] [Google Scholar]
- 25.Lilly CM. Hospital mortality, length of stay, and preventable complications among critically ill patients before and after tele-ICU reengineering of critical care processes. JAMA. 2011;305:2175–2183. [DOI] [PubMed] [Google Scholar]
- 26.Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P T. 2014;39:356–364. [PMC free article] [PubMed] [Google Scholar]
- 27.Available at: https://www.mohfw.gov.in/pdf/Telemedicine.pdf Telemedicine practice guidelines enabling registered medical practitioners to provide healthcare using telemedicine. Accessed May 10, 2020.
- 28.Choi BY, Blumberg C, Williams K. Mobile integrated health care and community paramedicine: an emerging emergency medical services concept. Ann Emerg Med. 2016;67:361–366. [DOI] [PubMed] [Google Scholar]
- 29.Zandbelt LC, de Kanter FEC, Ubbink DT. E-consulting in a medical specialist setting: medicine of the future? Patient Educ Couns. 2016;99:689–705. [DOI] [PubMed] [Google Scholar]
- 30.Ateriya N Saraf A Meshram V, et al. Telemedicine and virtual consultation: the Indian perspective. Natl Med J India. 2018;31:215–218. [DOI] [PubMed] [Google Scholar]
- 31.Dost B Koksal E Terzi Ö, et al. Attitudes of anesthesiology specialists and residents toward patients infected with the novel coronavirus (COVID-19): a national survey study. Surg Infect. 2020;21:350–356. [DOI] [PubMed] [Google Scholar]
- 32.Nelson LM Simard JF Oluyomi A, et al. US public concerns about the COVID-19 pandemic from results of a survey given via social media. JAMA Intern Med. 2020;e201369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gianfrancesco MA Hyrich KL Gossec L, et al. Rheumatic disease and COVID-19: initial data from the COVID-19 Global Rheumatology Alliance provider registries. Lancet Rheumatol. 2020;2:e250–e253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Robinson PC, Yazdany J. The COVID-19 Global Rheumatology Alliance: collecting data in a pandemic. Nat Rev Rheumatol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McKendry RA Rees G Cox IJ, et al. Share mobile and social-media data to curb COVID-19. Nature. 2020;580:29–29. [DOI] [PubMed] [Google Scholar]
- 36. Misinformation, distrust may contribute to black Americans' COVID-19 deaths. Available at: https://www.npr.org/2020/04/10/831480462/misinformation-distrust-maycontribute-to-black-americans-COVID-19-deaths. Accessed May 10, 2020.
- 37. Here is no absolute truth’: an infectious disease expert on COVID-19, misinformation and ‘bullshit’. Available at: https://www.theguardian.com/world/2020/apr/28/there-is-noabsolute-truth-an-infectious-disease-expert-on-COVID-19-misinformation-and-bullshit. Accessed May 10, 2020.
- 38.Kim B. Effects of social grooming on incivility in COVID-19. Cyberpsychol Behav Soc Netw. 2020. [DOI] [PubMed] [Google Scholar]
- 39. Cyberbullying may increase during COVID-19 pandemic, expert says. Available at: https://www.healio.com/pediatrics/school-health/news/online/%7B2274659e-f0f1-4ae7-88e3-bd4ea062a8a0%7D/cyberbullying-may-increase-during-COVID-19-pandemicexpert-says. Accessed May 10, 2020.
- 40.Yu J Tseng P Muggleton NG, et al. Being watched by others eliminates the effect of emotional arousal on inhibitory control. Front Psychol. 2015;6:–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Denecke K Bamidis P Bond C, et al. Ethical issues of social media usage in healthcare. Yearb Med Inform. 2015;24:137–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.et al. International Bioethics Committee, World Commission on the Ethics of Scientific Knowledge and Technology International Bioethics Committee, World Commission on the Ethics of Scientific Knowledge. Available at: https://unesdoc.unesco.org/ark:/48223/pf0000373115.
- 43.Coulthard P. Dentistry and coronavirus (COVID-19)—moral decision-making. Br Dent J. 2020;228:503–505. [DOI] [PubMed] [Google Scholar]
- 44. COVID-19 poses a major quandary for the field of moral psychology. Available at: https://www.forbes.com/sites/traversmark/2020/04/15/COVID-19-poses-a-majorquandary-for-the-field-of-moral-psychology/#3527d84d6612. Accessed May 10, 2020.
- 45.Misra DP Agarwal V Gasparyan AY, et al. Rheumatologists' perspective on coronavirus disease 19 (COVID-19) and potential therapeutic targets. Clin Rheumatol. 2020;1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hutto CJ, Yardi S, Gilbert E. A longitudinal study of follow predictors on Twitter. In: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. 2013;821–830.


