Abstract
Background and Aims.
Recreational cannabis has been legalized in 11 states and DC in the US. Among them, 10 states further permitted retail sale to provide a legal supply to adults. This study examined the associations of cannabis exposures with recreational cannabis legalization and commercialization.
Design.
Secondary data analysis of state-quarter level cannabis exposures during 2010–2017 in the US. Linear regressions with difference-in-difference design were used to compare pre- and post-legalization trends in states that legalized recreational cannabis to contemporaneous trends in states that did not legalize recreational cannabis.
Setting.
United States, including all 50 states and DC.
Cases.
Cannabis exposures reported to the US National Poison Data System.
Measurements.
The primary outcome was state age-adjusted cannabis exposures reported to the US National Poison Data System per 1,000,000 population per quarter. The two policy variables of interest included 1) the enactment of recreational cannabis legalization (i.e., removing penalties for adults’ possession of cannabis in a small amount for recreational use), and 2) the initiation of recreational cannabis commercialization (i.e., providing a legal supply of cannabis to adults through licensed dispensaries).
Findings.
The association between a state’s enactment of recreational cannabis legalization and its changes in cannabis exposures was overall statistically nonsignificant. After controlling for recreational cannabis legalization, however, the initiation of recreational cannabis commercialization was associated with 5.06–5.80 more exposures per 1,000,000 population per quarter (67–77% increase relative to the pre-legalization average) depending on the composition of comparison states. The increase associated with commercialization was higher among minors than adults (7.97–9.53 vs. 3.83–4.21 more exposures), higher among males than females (6.16–7.56 vs. 3.76–3.91 more exposures), and higher among exposures with medical consequences than those without medical consequences (4.09–4.79 vs. 0.97–1.01 more exposures).
Conclusion.
An increase in cannabis exposures reported to the US National Poison Data System was observed following recreational cannabis commercialization in the US.
Keywords: Cannabis, recreational cannabis legalization, retail sale, recreational cannabis dispensaries
Introduction
Cannabis liberalization has been a momentum in many American and European countries, particularly in the US. Notwithstanding the federal prohibition against cannabis, since 2012, recreational cannabis has been legalized in eleven states and DC. Over a quarter of US adults aged 21 years or older are now permitted to use cannabis for recreational purposes. Among these jurisdictions, seven states further started to provide a legal supply of cannabis in licensed dispensaries as of 2019, and three additional states anticipated to do so in the near future.
Despite the considerable debates in the US on recreational cannabis legalization (RCL, i.e., removing all penalties for adults’ possession of cannabis in small amount for recreational use) and recreational cannabis commercialization (RCC, i.e., providing a legal supply of cannabis to adults through licensed dispensaries), (1) scientific evidence regarding their public health consequences is scanty. Most existing studies focused on changes in self-reported cannabis use prevalence following RCL among US adolescents and college students. With between-state comparisons of time trends, they suggested mixed impacts of RCL on cannabis use. (2–5) Very little attention has been devoted to RCC. (6)
RCC is a more radical approach of cannabis liberalization, (7) with potential to generate broader and greater impacts than passing RCL alone. RCL impacts cannabis use primarily through more favorable social norms and reductions in pecuniary and non-pecuniary costs of cannabis possession. While RCC is also expected to modify perceptions and attitudes, (8) it directly increases availability and accessibility, (9) reduces price, (10) promotes awareness and purchase through marketing, (11, 12) improves product appeal such as quality control and higher potency, (9) and diversifies consumption modes such as vaping, dabbing, and edibles (9, 13, 14). A jurisdiction with RCL in the US does not necessarily have RCC in place. Retail sale in DC and Vermont remains illegal. Even in states that allowed retail sale, the operation of licensed dispensaries could be delayed for a few months or even a few years after RCL took effect.
In this study, we report estimates on the associations of cannabis exposures with RCL and RCC, respectively. We examined exposures reported to the US National Poison Data System (NPDS), one of the key outcome indicators noted in Fischer et al. 2018 for the monitoring and evaluation of cannabis legalization. (15) The study period spanned from 2010 through 2017, during which eight states and DC legalized recreational cannabis and five of them further commercialized recreational cannabis. By taking advantage of the variations in the presence and timing of RCC, we were able to test whether RCC had additional association with cannabis exposures after controlling for the presence of RCL.
Methods
The is a population-based ecological study conducted at state-quarter aggregate level. A quasi-experimental difference-in-difference design was used to compare pre- and post-legalization trends in cannabis exposures in states that legalized recreational cannabis to contemporaneous trends in states that did not legalize recreational cannabis. The Human Research Protections Program at the University of California San Diego required no review of this study, as it used publicly available data. The analysis was not pre-registered and the results should be considered exploratory.
Data
The primary data source was the US National Poison Data System (NPDS) administered by the American Association of Poison Control Centers. A total of 55 regional poison centers nationwide provide immediate expert treatment advice and referral to healthcare facilities to residents who call the poison help hotline. Poison centers also use follow-up calls to monitor progress and determine medical consequences. They have nationally standardized and consistent protocol to obtain and record information on each poison exposure, including caller and patient characteristics such as basic demographics and geographic location, exposure information such as reason, route, acuity, and substance involved, and information on case management and medical consequences. The information is submitted to NPDS automatically in near real-time. (16) Annually, these poison centers record nearly 3.5 million encounters, (17) estimated to account for half of the total poison exposures in the US. (18) NPDS data cover not only exposures treated in healthcare facilities but also those managed outside of healthcare facilities. They are complementary to and consistent with emergency department visits collected from the Drug Abuse Warning Network and mortality data recorded in the National Vital Statistics Systems. (19–21) In this study, we used NPDS data reported from all the 50 states and DC in the US from January 1st, 2010 through December 31st, 2017.
Outcome Measure
The outcome was the state age-adjusted rates of human exposures involving cannabis per 1,000,000 population per quarter. Exposure to cannabis was limited to the form of dry plants, which was consistently recorded during the study period. Exposure to other forms, such as concentrates and edibles, was not recorded in NPDS until 2016. Because the exposure cases were reported to NPDS for expert treatment advice, they can be perceived as indicators of problem use of cannabis. Among cannabis exposure cases, 69.4% reported medical consequences from minor effects to death and 86% were treated or being referred to healthcare facilities (Table S1). The quarterly number of cannabis exposure cases in a state was standardized to age-adjusted rate in 1,000,000 population to facilitate comparisons across states and over time.
Policy Exposure Measures
Two policy exposures varying at state-quarter level were examined: 1) the enactment of RCL, coded on the date of RCL legislation passed, and 2) the initiation of RCC, coded on the opening date of the first legal recreational cannabis dispensary. The policy dates were obtained from several sources and verified in legislative databases (Table S2). During the study period, nine jurisdictions (Alaska, California, Colorado, Maine, Massachusetts, Nevada, Oregon, Washington, and DC) enacted RCL, and five of them (Alaska, Colorado, Nevada, Oregon, Washington) further initiated RCC.
Covariates
State medical cannabis policy variables included the presence of medical cannabis legalization (MCL) and the presence of active medical cannabis dispensaries (Table S2). State health policy variables included the presence of Prescription Drug Monitoring Programs with data accessible to users, the presence of mandates on Prescription Drug Monitoring Program data use, and the presence of Medicaid expansion as part of the Affordable Care Act. Socioeconomic factors included number of active physicians per 1,000 population, median household income in 2017 thousand dollars, poverty rate, and unemployment rate. Total human exposures reported to NPDS per 1,000,1000 population per quarter were also included to control for residents’ overall awareness and willingness to call poison centers in a state. The details about variable definitions and data sources are described in Technical Note S1.
Statistical Analyses
Difference-in-difference design was used to compare the changes in cannabis exposures before and after RCL between states with and without RCL. The treatment states were the nine jurisdictions that implemented RCL in the study period. Three groups of comparison states were constructed to account for the heterogeneity of cannabis legality in the 42 remaining states without RCL. Comparison A compared treatment states to six states (Hawaii, Michigan, Montana, New Mexico, Rhode Island, and Vermont) that had implemented MCL as of January 1st, 2010 but had not passed RCL as of December 31st, 2017. Because all the treatment states already implemented MCL prior to RCL, this comparison estimated the independent association of RCL with cannabis exposures on top of MCL. Comparison B compared treatment states to 22 states (Alabama, Arkansas, Georgia, Idaho, Indiana, Iowa, Kansas, Kentucky, Louisiana, Mississippi, Missouri, Nebraska, North Carolina, Oklahoma, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, Wisconsin, and Wyoming) that had not passed RCL or MCL as of December 31st, 2017. This comparison estimated the association of RCL with cannabis exposures relative to the absence of any form of cannabis legalization. Comparison C compared treatment states to all the remaining 42 states that did not adopt RCL during the study period. This comparison estimated the association of RCL with cannabis exposures regardless of cannabis legalization status in the comparison states.
Statistically, we estimated two sets of linear regressions for each of the three comparisons. Model 1 estimated the association between RCL and cannabis exposures. It included the enactment of RCL as the primary policy exposure of interest. Model 2 estimated the association between RCC and cannabis exposures. It included the initiation of RCC as the primary policy exposure of interest, while controlling for the enactment of RCL. Both Models 1 and 2 controlled for covariates described above. They also included state fixed effects to account for state time-invariant unobserved heterogeneities, year and quarter fixed effects to account for time-specific unobserved heterogeneities common to all the states at the same time, and state-specific linear time trends to account for state linear trends in outcomes. Standard errors were clustered at state level. Model specifications are described in detail in Technical Note S1.
The coefficient estimates of RCL (or RCC) from linear regressions with difference-in-difference design can be interpreted as the absolute changes in age-adjusted rates of cannabis exposures associated with the enactment of RCL (or the initiation of RCC). To ease the interpretation, we also divided the estimated coefficients by the average age-adjusted rates prior to RCL to provide estimates on relative percentage changes. Projections of the annualized total number of exposures were made, assuming that RCC was initiated in 2017 in 1) all the jurisdictions with RCL, 2) all the states with MCL, 3) all the states without RCL or MCL, and 4) all the 50 states and DC, respectively.
To detect heterogeneities in the associations, we further stratified the sample by age (below vs. above 21 years), sex (male vs. female), intention of exposures (unintentional vs. intentional), severity of medical consequences (any consequences from minor effects to death vs. no consequences), and source of reporting (health care facilities vs. elsewhere). Separate regressions were conducted in each subsample. To test whether the between-subsample differences were statistically significant, we performed Chi-squared tests with consideration of covariance matrices in the separate regressions using seemingly unrelated estimations.
For subsample analysis, when case-level observations were aggregated to state level, we dropped cases missing key subsample identifiers. Specifically, 3.88%, 0.51%, and 3.32% cases were dropped during age, sex, and intention subsample aggregation, respectively. No cases were dropped during the aggregation of subsamples by medical consequences or source of reporting.
Sensitivity Analyses
Four sensitivity analyses were conducted to test the validity of the results. First, event studies were performed to validate the parallel time trend assumption, which required a parallel trend in the outcome between treatment and comparison states prior to the policy exposure. (22) Any significant association detected prior to RCL would indicate a violation of the assumption. Second, we replaced the indicator of RCL enactment with the indicator of RCL implementation, which was coded on the dates that RCL took effect (Table S2). Third, we removed state-specific time trends from the regressions, which may attenuate the estimates of policy impact if the policy affects the trend itself. (23, 24) Lastly, we performed placebo tests in 500 repetitions. In a placebo test where the assignment of the policy exposure (RCL or RCC in our study) was random, we expect the coefficient of the policy to be statistically nonsignificant. (25) Empirically, for Model 1, we randomly assigned the RCL enactment dates to the nine jurisdictions in the treatment state group. For Model 2, we first randomly assigned the RCL enactment dates to the nine jurisdictions in the treatment state group, then randomly assigned RCC initiation dates to the five states that initiated RCC.
Results
Table S3 presents characteristics of the states by cannabis legalization status. The treatment states had higher rates of cannabis exposures during the study period than the remaining states.
Main Analysis Results
Table 1 (Tables S4–S9 in detail) reports the estimates on the association between the enactment of RCL and cannabis exposures (Model 1). In the full sample analysis, the association between RCL and changes in cannabis exposures was nonsignificant in any of the three comparisons. In subsample analysis, RCL was associated with an increase in cannabis exposures only among unintentional exposures (by 1.30–1.44 per 1,000,000 population per quarter) and among exposures without medical consequences (by 0.65–0.74 per 1,000,000 population per quarter).
Table 1.
The Association of Recreational Cannabis Legalization with Cannabis Exposures Reported to the National Poison Data System, 2010–2017.
| Study Sample | Comparison A | Comparison B | Comparison C | |||
|---|---|---|---|---|---|---|
| Association of Recreational Cannabis Legalization with Cannabis Exposures per 1,000,000 Population per Quarter | ||||||
| Coefficient of Linear Regression (95% CI) |
Estimated Percentage Change | Coefficient of Linear Regression (95% CI) |
Estimated Percentage Change | Coefficient of Linear Regression (95% CI) |
Estimated Percentage Change | |
| All population | ||||||
| Exposures among All Population | 1.21 (−1.86, 4.28) |
15.99% | 0.75 (−2.02, 3.53) |
9.91% | 0.68 (−2.16, 3.51) |
8.99% |
| Subgroup Analysis | ||||||
| By Age | ||||||
| Exposures among Age 21 Below | 2.91 (−2.25, 8.06) |
21.33% | 2.52 (−2.19, 7.24) |
18.47% | 2.24 (−2.78, 7.26) |
16.42% |
| Exposures among Age 21 or Older | 0.48 (−2.10, 3.05) |
9.70% | −0.036 (−2.41, 2.34) |
−0.73% | 0.0060 (−2.29, 2.31) |
0.12% |
| By Sex | ||||||
| Exposures among Males | 1.74 (−0.94, 4.41) |
20.37% | 1.19 (−1.50, 3.87) |
13.93% | 1.11 (−1.64, 3.87) |
12.99% |
| Exposures among Females | 0.64 (−3.24, 4.52) |
9.78% | 0.30 (−3.46, 4.05) |
4.59% | 0.22 (−3.43, 3.87) |
3.36% |
| By Intention | ||||||
| Unintentional Exposures |
1.44** (0.47, 2.42) |
61.35% |
1.38** (0.57, 2.20) |
58.79% |
1.30** (0.46, 2.13) |
55.38% |
| Intentional Exposures | −0.23 (−2.71, 2.24) |
−4.41% | −0.63 (−3.04, 1.78) |
−12.07% | −0.62 (−3.03, 1.79) |
−11.88% |
| By Severity of Outcome | ||||||
| Exposures with Medical Consequences | 0.47 (−2.14, 3.08) |
22.13% | 0.0051 (−2.45, 2.46) |
0.24% | 0.026 (−2.46, 2.51) |
1.22% |
| Exposures without Medical Consequences |
0.74* (0.11, 1.37) |
13.60% |
0.75** (0.26, 1.23) |
13.78% |
0.65* (0.16, 1.14) |
11.94% |
| By Source of Reporting | ||||||
| Exposures Reported from Health Care Facilities | 0.18 (−2.03, 2.39) |
7.14% | −0.22 (−2.33, 1.89) |
−8.73% | −0.23 (−2.33, 1.87) |
−9.13% |
| Exposures Reported Elsewhere | 1.03 (−0.12, 2.18) |
20.41% | 0.97 (−0.015, 1.96) |
19.22% | 0.91 (−0.067, 1.88) |
18.03% |
p<0.05,
p<0.01
- Data were analyzed at state-quarter level.
- All regressions also controlled for medical cannabis legalization, active medical cannabis dispensaries, data access of Prescription Drug Monitoring Programs, mandatory use of Prescription Drug Monitoring Programs, Medicaid expansion, number of active physicians, median household income, poverty rate, unemployment rate, total number of human exposures reported to the National Poison Data System, state indicators, year indicators, quarter indicators, and state-specific time trends.
- Standard errors were clustered at state level.
- Comparison A compared 9 jurisdictions with recreational cannabis legalized during the study period (Alaska, California, Colorado, DC, Maine, Massachusetts, Nevada, Oregon, and Washington) to 6 states without recreational cannabis legalized but with medical cannabis legalized before 2010 (Hawaii, Michigan, Montana, New Mexico, Rhode Island, Vermont). Comparison B compared 9 jurisdictions with recreational cannabis legalization to 22 states that had not legalized medical cannabis by the end of 2017 (Alabama, Arkansas, Georgia, Idaho, Indiana, Iowa, Kansas, Kentucky, Louisiana, Mississippi, Missouri, Nebraska, North Carolina, Oklahoma, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, Wisconsin, Wyoming). Comparison C compared 9 jurisdictions with recreational cannabis legalization to all the remaining 42 states without recreational cannabis legalization.
- Estimated percentage changes were computed as the coefficient estimates from linear regressions divided by the pre-legalization average cannabis exposure rates.
Table 2 (Tables S4–S9 in detail) reports the estimates on the association between the initiation of RCC and cannabis exposures while controlling for the enactment of RCL (Model 2). In the full sample analysis, RCC was associated with a significant increase in cannabis exposures in all the three comparisons. The increase was 5.80 (95% CI: 1.64–9.96, p=0.010) in Comparison A, 5.17 (95% CI: 1.87–8.48, p=0.003) in Comparison B, and 5.06 (95% CI: 2.01–8.12, p=0.002) in Comparison C per 1,000,000 population per quarter. The increase relative to pre-RCL rate ranged from 67% to 77%, depending on the composition of comparison states. In subsample analysis, the increase in cannabis exposures following RCC was significant in almost all the subsamples and comparisons with only one exception in females in Comparison A. The tests on coefficient differences between subsamples (Table 3) indicate that, a higher increase was consistently seen in all the three comparisons among minors relative to adults (ps<.001), among males relative to females (ps<.015), and among exposures with medical consequences relative to those without medical consequences (ps<0.022).
Table 2.
The Association of Recreational Cannabis Commercialization with Cannabis Exposures Reported to the National Poison Data System, 2010–2017.
| Study Sample | Comparison A | Comparison B | Comparison C | |||
|---|---|---|---|---|---|---|
| Association of Recreational Cannabis Commercialization with Cannabis Exposures per 1,000,000 Population per Quarter | ||||||
| Coefficient of Linear Regression (95% CI) |
Estimated Percentage Change | Coefficient of Linear Regression (95% CI) |
Estimated Percentage Change | Coefficient of Linear Regression (95% CI) |
Estimated Percentage Change | |
| All population | ||||||
| Exposures among All Population |
5.80* (1.64, 9.96) |
76.65% |
5.17** (1.87, 8.48) |
68.33% |
5.06** (2.01, 8.12) |
66.87% |
| Subgroup Analysis | ||||||
| By Age | ||||||
| Exposures among Age 21 Below |
9.53** (4.00, 15.06) |
69.84% |
8.39** (3.87, 12.90) |
61.48% |
7.97*** (3.94, 12.01) |
58.41% |
| Exposures among Age 21 or Older |
4.21* (0.50, 7.91) |
85.08% |
3.83* (0.93, 6.72) |
77.40% |
3.85** (1.11, 6.59) |
77.80% |
| By Sex | ||||||
| Exposures among Males |
7.56** (2.86, 12.25) |
88.50% |
6.52** (2.79, 10.25) |
76.32% |
6.16** (2.62, 9.70) |
72.11% |
| Exposures among Females | 3.91 (−0.11, 7.93) |
59.77% |
3.76* (0.65, 6.88) |
57.48% |
3.91** (1.21, 6.61) |
59.77% |
| By Intention | ||||||
| Unintentional Exposures |
2.00* (0.23, 3.78) |
85.21% |
1.94* (0.43, 3.45) |
82.65% |
1.78* (0.28, 3.27) |
75.83% |
| Intentional Exposures |
3.79* (1.07, 6.52) |
72.61% |
3.24** (0.89, 5.59) |
62.07% |
3.29** (1.04, 5.53) |
63.03% |
| By Severity of Outcome | ||||||
| Exposures with Medical Consequences |
4.79* (0.96, 8.62) |
225.55% |
4.19* (1.05, 7.32) |
197.30% |
4.09** (1.26, 6.93) |
192.59% |
| Exposures without Medical Consequences |
1.01*** (0.55, 1.47) |
18.56% |
0.99*** (0.71, 1.27) |
18.19% |
0.97*** (0.71, 1.23) |
17.82% |
| By Source of Reporting | ||||||
| Exposures Reported from Health Care Facilities |
3.97* (0.86, 7.09) |
157.57% |
3.29* (0.79, 5.78) |
130.58% |
3.25** (0.85, 5.64) |
128.99% |
| Exposures Reported Elsewhere |
1.82* (0.50, 3.15) |
36.06% |
1.89** (0.83, 2.95) |
37.45% |
1.82*** (0.89, 2.75) |
36.06% |
p<0.05,
p<0.01,
p<0.001
- Data were analyzed at state-quarter level.
- In addition to regressors included in Table 1, all regressions also controlled for recreational cannabis legalization.
- Standard errors were clustered at state level.
- Comparison A compared 9 jurisdictions with recreational cannabis legalized during the study period (Alaska, California, Colorado, DC, Maine, Massachusetts, Nevada, Oregon, and Washington) to 6 states without recreational cannabis legalized but with medical cannabis legalized before 2010 (Hawaii, Michigan, Montana, New Mexico, Rhode Island, Vermont). Comparison B compared 9 jurisdictions with recreational cannabis legalization to 22 states that had not legalized medical cannabis by the end of 2017 (Alabama, Arkansas, Georgia, Idaho, Indiana, Iowa, Kansas, Kentucky, Louisiana, Mississippi, Missouri, Nebraska, North Carolina, Oklahoma, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, Wisconsin, Wyoming). Comparison C compared 9 jurisdictions with recreational cannabis legalization to all the remaining 42 states without recreational cannabis legalization.
- Estimated percentage changes were computed as the coefficient estimates from linear regressions divided by the pre-legalization average cannabis exposure rates.
Table 3.
Test Results for Subsample Differences in the Association between Recreational Cannabis Commercialization and Cannabis Exposures.
| Subsamples Being Compared | Comparison A | Comparison B | Comparison C |
|---|---|---|---|
| P-value for the Test on Subsample Coefficient Differences | |||
| Age 21 Below vs. Age 21 or older | <0.001 | <0.001 | <0.001 |
| Male vs. Female | 0.006 | 0.006 | 0.015 |
| Unintentional Exposures vs. Intentional Exposures | 0.040 | 0.198 | 0.169 |
| With Medical Consequences vs. Without Any Medical Consequences | 0.015 | 0.022 | 0.013 |
| Reported from Health Care Facilities vs. Reported Elsewhere | 0.040 | 0.123 | 0.129 |
Notes: Chi-squared tests were conducted on coefficient differences with consideration of covariance matrices in the separate regressions using seemingly unrelated estimations.
Figure 1 presents the projected, annualized total number of cannabis exposures in different hypothetical scenarios based on Model 2 results. If all the nine jurisdictions with RCL had RCC in 2017, the annual number of exposures would have increased from 1,618 in status quo to 2,707. Similarly, the increase would have been from 728 to 1,132 in six states with MCL and from 2,058 to 4,837 in 22 states without RCL or MCL. If all the 50 states and DC had RCC in 2017, the national annual number of exposures would have increased from 7,976 in status quo to 13,053.
Figure 1. Projected Annual Number of Cannabis Exposures Reported to the National Poison Data System, Assuming that States in Each Category All Commercialized Recreational Cannabis in 2017.
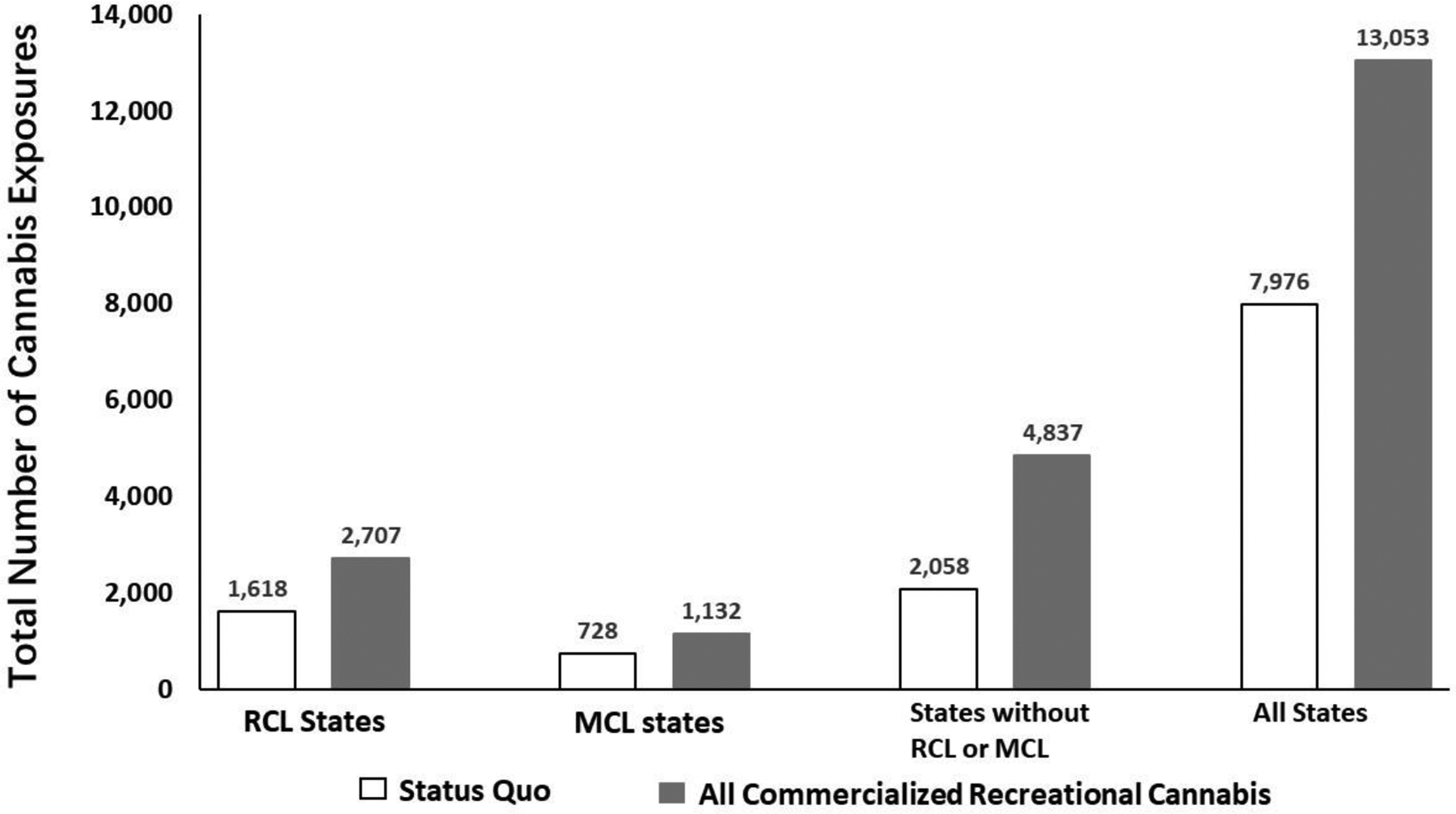
Notes.
“RCL States” represent 9 jurisdictions with recreational cannabis legalization during the study period (Alaska, California, Colorado, DC, Maine, Massachusetts, Nevada, Oregon, and Washington). “MCL States” represent 6 states without recreational cannabis legalization but with medical cannabis legalized before 2010 (Hawaii, Michigan, Montana, New Mexico, Rhode Island, and Vermont). “States without RCL or MCL” represent 22 states that had not legalized medical cannabis by the end of 2017 (Alabama, Arkansas, Georgia, Idaho, Indiana, Iowa, Kansas, Kentucky, Louisiana, Mississippi, Missouri, Nebraska, North Carolina, Oklahoma, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, Wisconsin, and Wyoming). “All States” represent all 50 states and DC.
The bars of “Status Quo” represent the actual annual number of cannabis exposures reported to the National Poison Data System in 2017. The bars of “All Commercialized Recreational Cannabis” represent the annual number of cannabis exposures projected from Model 2, assuming that all the states in the category commercialized recreational cannabis in 2017.
Sensitivity Analysis Results
Figure S1 plots the results from event studies. No significant difference was observed between states with and without RCL prior to the enactment of RCL. This indicates that the parallel time trend assumption was not rejected. When RCL enactment dates were replaced by effective dates, the point estimates and significant levels were similar to the main analysis (Table S10). When state-specific linear trends were removed, the estimates on RCC were slightly attenuated but remained at the same significant levels (Table S11). In placebo tests, the association between RCC and cannabis exposures was no longer significant when policy dates were randomly assigned (Table S12).
Discussion
We examined the associations of cannabis exposures reported to NPDS with RCL and RCC during 2010–2017 in the US. We found little evidence that the enactment of RCL was associated with the changes in cannabis exposures. Nonetheless, the initiation of RCC was significantly and consistently associated with a considerable increase in cannabis exposures after controlling for RCL status. Had all the 50 states and DC commercialized recreational cannabis in 2017, the total number of cannabis exposures nationwide would have risen by over 60% compared to status quo.
To our knowledge, this is the first national-level empirical evidence for negative health consequences associated with RCC. The only other study with quasi-experimental design found no association between RCC and traffic fatalities in the US. (6) The two other studies had limited causal inference on the association because their data were restricted to a single state in the US without a comparison group. (26, 27) The considerable increase after RCC could have several explanations. First, RCC modified attitudes and perceptions of cannabis use. However, this mechanism is not plausible as we did not observe the same change after RCL when social norms should have been already influenced. Second, RCC increased the availability and accessibility of cannabis, even among minors possibly through third-party purchase. Third, RCC decreased cannabis price due to removal of production barriers and increase in competitions. Fourth, RCC enabled marketing activities at the point-of-sale and some traditional media outlets. Fifth, RCC increased the appeal of cannabis products. Lastly, RCC increased the availability of non-plant products and, in turn, increased the use of alternative consumption methods. This last mechanism is unlikely the explanation for this study as exposures to non-plant forms were not included in analysis.
Minors’ possession of cannabis remained a criminal offense in most US states after they adopted RCL, and the associated arrest rates were not reduced. (28) It is thus not necessarily surprising that cannabis exposures among minors had no change after RCL. However, we observed an increase following RCC among minors, even greater than that among adults. This finding supports the 2015 cannabis policy statement (29) by American Academy of Pediatrics, which “strongly recommends strict enforcement of rules and regulations that limit access and marketing and advertising to youth”. Prevention and treatment endeavors should also target minors whose use of cannabis is associated with a wide range of short- and long-term adverse consequences. (29)
NPDS is a passive surveillance system, relying on voluntary reporting from healthcare facilities and patients/caregivers. It is likely that we observed an increase in cannabis exposures because people were more willing to call poison centers after the legal consequences of possessing cannabis were removed. We argue that, however, such reporting bias could not be the sole driver of the increasing trend. Assuming that the reporting was indeed completely determined by the willingness to call instead of true exposures, we should have observed the following. First, an increase should have been observed right after RCL, which directly changed the legality of cannabis. Second, exposures without any medical consequences should have seen a larger increase than exposures with medical consequences, because exposures with real needs for immediate medical treatment should be less likely influenced by cannabis legality. Third, exposures reported from individuals should have seen a larger increase than those reported from healthcare facilities. Healthcare facilities do not bear legal consequences of possessing cannabis and their reporting could be more objective than individual self-reporting if urine or blood drug tests were performed for the diagnosis. However, none of these three projections above were supported by our data. It indicates that the increasing trend following RCC was not entirely attributable to reporting bias. Future research is warranted to explicitly test whether and to what extent reporting bias affected the estimations.
This study suggested that the US commercialization model may be associated with negative health consequences. It should be noted that it would be premature to make any policy recommendations before the findings are validated and causality is established, yet we encourage US and other countries with cannabis commercialization to learn experience from each other. Alternative legal supply model has been implemented in Uruguay and Canada. (30) Unlike the for-profit standard commercialization model adopted by most legalizing states in the US, Uruguay chose a tightly controlled middle-ground model. (31) Pharmacies provide cannabis like dispensaries in the US, but very few have been approved. Government strictly controls the supply of cannabis; pharmacies can only obtain cannabis from the two companies contracted by the government. (31) In Canada, the legal supply model varies by province in terms of ownership (government-run or for-profit private) and mode of access (storefronts or online).
Limitations
This study has limitations. First, as in any ecological studies, the findings cannot be interpreted as causal effects. Unobserved time-variant confounding factors may remain even after we controlled for a rich set of covariates and state and time fixed effects and conducted sensitivity analyses. We were not able to directly assess the causal pathways at individual level, either. Second, poison exposures recorded in NPDS account for half of the poison exposures recorded in all sources in the US, (18) but how well they capture cannabis exposures specifically is unknown. The results may not be generalized to exposure data from other sources such as hospital records or survey data. Third, as discussed above, the increasing trend after RCC may be partially driven by the reporting bias associated with the changes in cannabis legality. Fourth, the outcome was restricted to exposure to cannabis dry plants due to data limitations. Dry plants accounted for 85% of the exposures involving any form of cannabis in NPDS in 2017. Considering that concentrates and edibles are increasingly popular in states with RCC, (13, 14) the associations may be underestimated in this study. Fifth, we did not consider dose of cannabis use due to data unavailability. Further, our study period had more policy variations in RCL and RCC than most existing studies, but post-RCC data points may be still limited to detect the impact of RCC in its full capacity or estimate delayed policy effects that built over time. In addition, we were not able to examine whether the degree of RCC (number and geographic distribution of dispensaries and speed of dispensary opening) had any impact in addition to the binary indicator of RCC initiation. Future research could address this limitation by utilizing longitudinal data on dispensary locations and sales. Lastly, the study findings may not be generalizable to Uruguay or Canada where different models of cannabis supply were adopted.
Conclusions
For the first time, our study suggested a substantial increase in cannabis exposures following RCC in the US using between-state comparisons. While further data are needed to examine the causal mechanisms and to validate findings with clinical data and self-reported behavioral data, a cautious interpretation of the findings suggests continuous surveillance and prevention endeavors in US states that have initiated RCC or had such plans. Particular attention should be given to minors.
Supplementary Material
Grant Support
This research was supported by grant R01DA042290 (PI: Shi) from the National Institute on Drug Abuse. This article is the sole responsibility of the authors and does not reflect the views of the National Institute on Drug Abuse.
Footnotes
Disclosures
Declarations of Competing Interest: The authors report no financial relationships with commercial interests.
Data Source
National Poison Data System data in 2010–2017 were obtained through a data use agreement with the American Association of Poison Control Centers (PI: Shi).
References
- 1.McGinty EE, Samples H, Bandara SN, Saloner B, Bachhuber MA, Barry CL The emerging public discourse on state legalization of marijuana for recreational use in the US: Analysis of news media coverage, 2010–2014, Prev Med 2016: 90: 114–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson DM, Hansen B, Rees DI, Sabia JJ Association of marijuana laws with teen marijuana use: New estimates from the youth risk behavior surveys, JAMA Pediatr 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cerda M, Wall M, Feng T, Keyes KM, Sarvet A, Schulenberg J et al. Association of state recreational marijuana laws with adolescent marijuana use, JAMA Pediatr 2017: 171: 142–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kerr DCR, Bae H, Koval AL Oregon recreational marijuana legalization: Changes in undergraduates’ marijuana use rates from 2008 to 2016, Psychol Addict Behav 2018: 32: 670–678. [DOI] [PubMed] [Google Scholar]
- 5.Kerr DCR, Bae H, Phibbs S, Kern AC Changes in undergraduates’ marijuana, heavy alcohol and cigarette use following legalization of recreational marijuana use in Oregon, Addiction 2017: 112: 1992–2001. [DOI] [PubMed] [Google Scholar]
- 6.Lane TJ, Hall W Traffic fatalities within US states that have legalized recreational cannabis sales and their neighbours, Addiction 2019. [DOI] [PubMed] [Google Scholar]
- 7.Caulkins JP, Kilmer B Considering marijuana legalization carefully: insights for other jurisdictions from analysis for Vermont, Addiction 2016: 111: 2082–2089. [DOI] [PubMed] [Google Scholar]
- 8.Lipperman-Kreda S, Grube JW Impacts of marijuana commercialization on adolescents’ marijuana beliefs, use, and co-use with other substances, J Adolesc Health 2018: 63: 5–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Orens A, Light M, Lewandowski B, Rowberry J, Saloga C Market size and demand for marijuana in Colorado 2017 market update. Available at https://www.colorado.gov/pacific/sites/default/files/MED%20Demand%20and%20Market%20%20Study%20%20082018.pdf. Accessed on 12/02/2018 : Marijuana Policy Group; 2018. [Google Scholar]
- 10.Hall W, Lynskey M Evaluating the public health impacts of legalizing recreational cannabis use in the United States, Addiction 2016: 111: 1764–1773. [DOI] [PubMed] [Google Scholar]
- 11.Fiala SC, Dilley JA, Firth CL, Maher JE Exposure to marijuana marketing after legalization of retail sales: Oregonians’ experiences, 2015–2016, American journal of public health 2018: 108: 120–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cao Y, Carrillo AS, Zhu S. h., Shi Y Point-of-sale marketing of recreational marijuana dispensaries around California schools. , J Adolesc Health 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tormohlen KN, Schneider KE, Johnson RM, Ma M, Levinson AH, Brooks-Russell A Changes in prevalence of marijuana consumption modes among Colorado high school students from 2015 to 2017, JAMA Pediatrics 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smart R, Caulkins JP, Kilmer B, Davenport S, Midgette G Variation in cannabis potency and prices in a newly legal market: evidence from 30 million cannabis sales in Washington state, Addiction 2017: 112: 2167–2177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fischer B, Russell C, Rehm J, Leece P Assessing the public health impact of cannabis legalization in Canada: core outcome indicators towards an ‘index’ for monitoring and evaluation, J Public Health (Oxf) 2019: 41: 412–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wolkin AF, Martin CA, Law RK, Schier JG, Bronstein AC Using poison center data for national public health surveillance for chemical and poison exposure and associated illness, Ann Emerg Med 2012: 59: 56–61. [DOI] [PubMed] [Google Scholar]
- 17.Gummin DD, Mowry JB, Spyker DA, Brooks DE, Osterthaler KM, Banner W 2017 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 35th annual report, Clin Toxicol (Phila) 2018: 56: 1213–1415. [DOI] [PubMed] [Google Scholar]
- 18.InstituteOfMedicine. Forging a poison prevention and control system Washington, DC: Institute of Medicine, The National Academies Press; 2004. [PubMed] [Google Scholar]
- 19.Davis JM, Severtson SG, Bucher-Bartelson B, Dart RC Using poison center exposure calls to predict prescription opioid abuse and misuse-related emergency department visits, Pharmacoepidem Dr S 2014: 23: 18–25. [DOI] [PubMed] [Google Scholar]
- 20.Dasgupta N, Davis J, Funk MJ, Dart R Using poison center exposure calls to predict methadone poisoning deaths, Plos One 2012: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iwanicki JL, Severtson SG, Margolin Z, Dasgupta N, Green JL, Dart RC Consistency between opioid-related mortality trends derived from poison center and national vital statistics system, United States, 2006–2016, American journal of public health 2018: 108: 1639–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Angrist JD, Pischke J-S Mostly harmless econometrics: An empiricist’s companion: Princeton university press; 2008. [Google Scholar]
- 23.Meer J, West J Effects of the minimum wage on employment dynamics, J Hum Resour 2016: 51: 500–522. [Google Scholar]
- 24.Wolfers J Did unilateral divorce laws raise divorce rates? A reconciliation and new results, Am Econ Rev 2006: 96: 1802–1820. [Google Scholar]
- 25.Gertler PJ, Martinez S, Premand P, Rawlings LB, Vermeersch CM Impact evaluation in practice Washington DC: International Bank for Reconstruction and Development / The World Bank; 2016. [Google Scholar]
- 26.Graves JM, Whitehill JM, Miller ME, Brooks-Russell A, Richardson SM, Dilley JA Employment and marijuana use among washington state adolescents before and after legalization of retail marijuana, J Adolesc Health 2019: 65: 39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brooks-Russell A, Ma M, Levinson AH, Kattari L, Kirchner T, Anderson Goodell EM et al. Adolescent marijuana use, marijuana-related perceptions, and use of other substances before and after initiation of retail marijuana sales in Colorado (2013–2015), Prev Sci 2019: 20: 185–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Plunk AD, Peglow SL, Harrell PT, Grucza RA Youth and adult arrests for cannabis possession after decriminalization and legalization of cannabis, JAMA Pediatr 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Committee on Substance Abuse and Committee on Adolescence. The impact of marijuana policies on youth: clinical, research, and legal update, Pediatrics 2015: 135: 584–587. [DOI] [PubMed] [Google Scholar]
- 30.Caulkins JP, Kilmer B, Kleiman MA, MacCoun RJ, Midgette G, Oglesby P et al. Considering marijuana legalization: Insights for Vermont and other jurisdictions: Rand Corporation; 2015. [Google Scholar]
- 31.Cerda M, Kilmer B Uruguay’s middle-ground approach to cannabis legalization, Int J Drug Policy 2017: 42: 118–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


