Abstract
Social distancing is the most visible public health response to the COVID-19 pandemic, but its implications for mental health are unknown. In a nationwide online sample of 435 U.S. adults, conducted in March 2020 as the pandemic accelerated and states implemented stay-at-home orders, we examined whether stay-at-home orders and individuals’ personal distancing behavior were associated with symptoms of depression, generalized anxiety disorder (GAD), intrusive thoughts, insomnia, and acute stress. Stay-at-home order status and personal distancing were independently associated with higher symptoms, beyond protective effects of available social resources (social support and social network size). A subsample of 118 participants who had completed symptom measures earlier in the outbreak (February 2020) showed increases in depression and GAD between February and March, and personal distancing behavior was associated with these increases. Findings suggest that there are negative mental health correlates of social distancing, which should be addressed in research, policy, and clinical approaches to the COVID-19 pandemic.
Keywords: Coronavirus, COVID-19, Social distancing, Mental health, Depression, Anxiety, Stress
1. Introduction
COVID-19, the disease caused by the coronavirus SARS-CoV-2, emerged in December 2019 in China and quickly became a global pandemic. Since then, as of late August 2020, over 22.5 million people have contracted COVID-19, with over 800,000 deaths; these include over 5.6 million cases and 170,000 deaths in the United States, with more expected as the pandemic continues (CDC, 2020; World Health Organization, 2020). Beyond this enormous global threat to physical health and life, researchers and clinicians have voiced concern over its impact on mental health (Cao et al., 2020; Gruber et al., 2020; Pfefferbaum and North, 2020; Van Bavel et al., 2020). As a highly contagious viral disease, COVID-19 is an inherently social phenomenon, and the success of containment depends on effectively limiting social contact. Public health responses emphasizing social distancing, including stay-at-home orders and individual behavior change, appear to have slowed the trajectory of COVID-19 when implemented. Although essential for containing the virus, these social interventions may deleteriously affect mental health, as observed following earlier epidemics, like the 2003 SARS outbreak (Cava et al., 2005; Hawryluck et al., 2004; Mak et al., 2009) and 2009 H1N1 outbreak (Pfefferbaum et al., 2012).
The interventions most essential for pandemics necessarily disrupt the very social processes that facilitate mental health, including social support availability, day-to-day interaction, and social influences on coping (Marroquín et al., 2017). Research on true quarantine (i.e., complete isolation to contain an illness) shows substantial effects on emotional distress and mental health including depression, generalized anxiety, insomnia, and post-traumatic stress (Brooks et al., 2020). There is therefore an urgent need to examine the mental health consequences of current social distancing measures. Recent studies in China showed that COVID-19-related disruption (e.g., stopping work) was associated with more anxiety and psychological distress (Cao et al., 2020; Zhang et al., 2020). In the U.S., stay-at-home orders have been associated with concurrent health anxiety, financial worry, and loneliness (Tull et al., 2020). Still, it remains to be confirmed whether mental health symptoms are increasing over time as COVID-19 unfolds, as presumed (Gruber et al., 2020; Van Bavel et al., 2020). It also remains to be seen whether prospective symptom increases, not only cross-sectional symptom severities, are associated with social distancing. Answering these questions would have implications for clinical and public health measures that aim to ameliorate the mental health burden of COVID-19 andrelated policies.
We propose two additional considerations in order to understand the effects of social distancing more comprehensively. First, the umbrella term “social distancing” comprises interventions spanning both public and private levels that may have different implications. At the public level, government-imposed “stay-at-home” (colloquially “quarantine” or “lockdown”) policies, while varying by region, tend to prohibit travel outside the home for activities other than those deemed necessary (e.g., procuring food, obtaining medical care, completing “essential” or “front-line” work). But even before such public measures were enacted for COVID-19, people were encouraged by authorities, media, and peers to voluntarily adopt “personal distancing” behaviors to reduce virus transmission (e.g., avoiding physical contact or close proximity with non-household members; reducing use of shared public spaces). Both forms of social distancing have caused wide-ranging social disruption, but their potentially independent effects on mental health are unknown, given that existing studies have so far focused on government-imposed stay-at-home status only (Cao et al., 2020; Tull et al., 2020; Zhang et al., 2020). Second, effects of social distancing on mental health do not occur in a vacuum. People's adaptation to stressors depends in part on social resources. Social support – receiving advice, assistance, or caring, or perceiving that such support is available – is positively associated with mental health (Cohen and Wills, 1985; Thoits, 2011), as are larger and more diverse social networks (Cohen, 2004; Uchino, 2009). Individuals “bring with them” such protective resources to psychological challenges like COVID-19, but whether these resources mitigate the potential negative effects of social distancing is an open question.
1.1. Current investigation
This study examines relationships among social distancing (stay-at-home status and personal distancing behavior), social resources (perceived social support and social network size), and mental health during the early course of the COVID-19 pandemic (mid-February to late March 2020). We focused on depression, generealized anxiety disorder, intrusive thoughts, insomnia, and acute stress, all of which are sensitive to social influences and are known outcomes of exposure to negative events, including disasters and epidemics (Mak et al., 2009; Pfefferbaum et al., 2012). Depression and generalized anxiety disorder (GAD) are consistently associated with exposure to stressful life events (Kendler and Gardner, 2016; Kendler et al., 2003). Intrusive thoughts, anxious thoughts that are unwanted, recurrent, and often come out of the blue, are stressful in and of themselves, and are also associated with several stress-related disorders (e.g., obsessive-compulsive disorder, Pascual-Vera et al., 2019; posttraumatic stress disorder, Falsetti et al., 2002). Insomnia, which contributes to a wide array of mental health and quality of life impairments, is often prompted by negative life events (Sinha, 2016). Lastly, acute stress is not only a broadly applicable non-clinical index of mental health in the context of negative events, but also a major transdiagnostic precipitant of psychological disorders (Harkness and Hayden, 2020).
We made three specific predictions. First, social distancing would be associated cross-sectionally with more mental health symptoms in late March 2020, above and beyond expected protective effects of individuals’ social resources. This finding would elaborate previous cross-sectional findings on psychological distress during COVID-19 (Cao et al., 2020; Tull et al., 2020; Zhang et al., 2020) and extend them to a broader set of mental health symptoms. Second, we predicted that March levels of prospectively measured symptoms would represent an increase over mid-February levels. Third, we expected the magnitudes of these prospective symptom increases to be positively associated with the extent of social distancing, independently of social resources.
2. Method
2.1. Procedure
This article reports on 2 time points from an ongoing multi-wave study in a national online sample of adults. A COVID-focused battery of measures was collected online during a 3-day period (the “March 2020” wave), March 26 to March 28, 2020, which yielded a sample of 435 participants, as described below. Of these participants, 118 also had prospective mental health symptom data available from a previous study on emotion regulation and psychopathology (the “February 2020” wave), collected from February 18 to March 1, 2020, before COVID-19 had disrupted daily life on a widespread scale in the U.S.
Participants were recruited initially via Amazon's Mechanical Turk (MTurk) platform and directed to the survey in Qualtrics. After providing informed consent, participants completed a section of questionnaires, including those described below. The study was approved by an Institutional Review Board and followed APA ethical standards; participants were debriefed and provided with local mental health resources.
2.2. COVID-19 context
2.2.1. February 2020
By the end of February data collection (i.e., by March 1, 2020), there were only 75 reported cases of COVID-19 in the United States, with the first death announced on February 29 (Worldometer, 2020). At that time, no stay-at-home orders had been issued by any local, state, or federal government.
2.2.2. March 2020
Between the two waves of data collection, the World Health Organization declared COVID-19 a pandemic (on March 11) and the U.S. President declared a national emergency (March 13). The first local stay-at-home order in the U.S. went into effect (March 17, in the San Francisco Bay Area), followed quickly by the first statewide order (March 19, in California). By the beginning of March data collection (initiated March 26), 21 states had issued stay-at-home or similar orders, weekly unemployment filings reached a then-record 3 million, and the Dow Jones Industrial Average was 23.7% down from its February peak. By this time there were 86,379 cases of COVID-19 in the U.S. and 1,614 deaths (Worldometer, 2020). During the 3 days of data collection, cases rose to 124,788, deaths to 2,754, and 6 additional states enacted stay-at-home orders, for a total of 27 states.
2.3. Participants
2.3.1. Inclusion criteria and quality control
Recruitment was limited to adults in the U.S. Following recommendations for maximizing valid data in MTurk samples (e.g., Paolacci and Chandler, 2014; Peer et al., 2014), participants were required to have an approval rate for past MTurk tasks of 99% or above, and to have completed at least 500 previously approved tasks. Initial data collected from 499 individuals were inspected for quality, and 29 were removed for failing 3 or more of 6 attention check items distributed throughout the study (e.g., “Please leave this question blank;” “Enter the value equal to 6 minus 1”). Of the remaining 470, cases were further excluded for any one of the following reasons: taking less than half the median completion time of 34.1 min (i.e., less than 17.05 min; n = 14); invalid response style on more than 1 questionnaire (e.g., choosing the same response for all items; n = 11); invalid response to an open-ended text item about personal experiences, not part of the present report (i.e., using no personal pronouns, or nonsensical text; n = 10).
2.3.2. March 2020 sample
These criteria yielded a final sample of 435 participants residing in 46 states (all except Alaska, Montana, North Dakota, and Vermont) and the District of Columbia. The most frequent states were California (11.3%), Florida (10.4%), New York (7.1%), Pennsylvania (7.1%), and Texas (6.5%), also the five most populous states in the U.S. The sample consisted of 230 men (52.9%), 202 women (46.4%), and 3 another gender (0.7%), aged 39.2 years on average (SD = 11.5; range 20–73). Racial/ethnic self-identification was 75.9% white, 9.4% Black/African-American, 8.0% Asian/Asian-American, 3.0% Hispanic/Latino, 0.2% Native American, and 3.4% multiracial. Median annual household income was $40,000–59,999, distributed as follows: below $20,000 (12.0%), $20,000–39,999 (23.4%), $40,000–59,999 (20.7%), $60,000–79,000 (21.8%), $80,000–99,999 (10.1%), $100,000–119,999 (4.8%) and $120,000 or more (7.1%). Approximately half the sample had less than a bachelor's degree, with education attainment distributed as follows: no diploma (0.7%), high school diploma (26.4%), GED (2.5%), associate's degree (17.0%), bachelor's degree (43.9%), master's degree (8.3%), and doctoral degree (1.1%).
2.3.3. Prospective February 2020 subsample
118 of the individuals in the final March sample had previously participated in an unrelated study in late February and provided valid data, including the same measures of depression and GAD symptoms. Prospective subsample participants did not differ significantly in gender, racial/ethnic identification, income, or education from new participants in March (all ps > .09), but were approximately 3 years older on average (M = 41.54, SD = 11.19 versus M = 38.34, SD = 11.54), t(433) = 2.60, p = .010.
2.4. Mental health measures
Depressive symptoms (February and March). The Center for Epidemiological Studies Depression Scale (CES-D; Radloff, 1977) is a widely-used 20-item general-population measure of depressive symptoms with good psychometric properties. Participants rated how frequently they had experienced symptoms within the previous week (e.g., “I had crying spells,” “I was bothered by things that usually don't bother me”) on a scale from 0 (rarely or none of the time/less than 1 day) to 3 (all of the time/5–7 days). Reliability was excellent in both February (ɑ = .96) and March (ɑ = .94).
Generalized anxiety disorder symptoms (February and March). The GAD-7 (Spitzer et al., 2006) is a 7-item measure of GAD symptoms over the last 2 weeks. Participants rated how much they had been bothered by, e.g., “Not being able to stop or control worrying,” and “Feeling nervous, anxious, or on edge,” on a scale from 0 (not at all) to 3 (nearly every day). Validity and reliability were good in past studies (e.g., Spitzer et al., 2006), and in this study reliability was excellent in both February (ɑ = .95) and March (ɑ = .93).
Intrusive thoughts (March). The Experience of Intrusions scale (EIS; Salters-Pedneault et al., 2009) is a 5-item measure of the presence of intrusive symptoms, including both frequency and quality (intensity, suddenness, distress, and disruptiveness) of unwanted intrusive thoughts about an index event or topic that can be specified by the researcher. In this study, participants rated intrusive thoughts over the previous 24 h, specifically regarding COVID-19, on scales from 0 to 4. The scale has shown convergent validity with a standard measure of PTSD symptom severity (r = .63) in an MTurk sample (Takarangi et al., 2016), and reliability in this sample was good (ɑ = .86).
Insomnia (March). The Insomnia Severity Index (ISI; Bastien et al., 2001) is a widely-used 7-item measure of sleep difficulties over the previous 2 weeks, including sleep problems (e.g., difficulty falling or staying asleep, or waking up early), dissatisfaction, distress, and interference. Items are scored from 0 to 4 and summed. The ISI has strong psychometric properties (Bastien et al., 2001; Morin et al., 2011), and reliability in this sample was excellent (ɑ = .92).
Acute stress (March). The Stress Overload Scale-Short Form (SOS-S; Amirkhan, 2018) is a 10-item version of the longer Stress Overload Scale (Amirkhan, 2012), and measures stress within the last week. Total scores are the sum of five items assessing event load (e.g., “felt swamped by your responsibilities”) and five items assessing personal vulnerability (e.g., “felt like nothing was going right”), all scored from 1 (not at all) to 5 (a lot). The SOS-S has shown good internal reliability and concurrent and predictive validity in diverse community samples (Amirkhan, 2018). Reliability in this sample was excellent (ɑ = .95).
2.5. Social distancing measures
Stay-at-home order status. Participants self-reported whether they had been told to “stay inside your home and avoid social contact by government officials (for example, with a ‘stay at home’ or ‘shelter in place’ order).” Responses were coded 1 for “yes” and 0 for “no.”
Personal distancing behavior. Participants estimated how many times they engaged in each of 12 activities during two time periods: “in the last 3 days,” and “in a typical 3-day period before the coronavirus outbreak.” Items were developed to represent a range of behavioral domains being discussed publicly in late March for limiting virus transmission: leaving one's home; riding public transportation; working from home/staying away from work; shaking hands; sitting/standing within 3 feet of someone not from one's household; hugging/kissing someone not from one's household; using a public restroom; going to a cafe, restaurant, or bar; going to a store; taking a taxi or rideshare service; visiting someone in their home; and having someone visit one's own home. Each item was scored as 1 if the reported last-3-day frequency differed from the pre-virus frequency in the distancing direction (e.g., if the participant reported shaking hands fewer times, or staying away from work more times, in the last 3 days as compared to before). Each behavior was scored as −1 if the reported last-3-day frequency differed in the opposite direction (increased social contact), and it was scored as 0 if the two frequencies were equal. Exploratory factor analyses suggested a single factor solution for all 12 items, and removing any item weakened internal consistency. Thus, all 12 scores were averaged to reflect the extent of each individual's distancing behavior, with possible averages falling between −1 (reduced distancing) and 1 (increased distancing). Reliability was good (ɑ = .80).
2.6. Social resource measures
Social support. Perceived social support was measured with the 24-item Social Provisions Scale (SPS; Cutrona and Russell, 1987). On a scale of 1 (strongly disagree) to 4 (strongly agree), participants rated statements tapping 6 domains of social support in their current relationships (e.g., “There are people I can depend on to help me if I really need it;” “I feel a strong emotional bond with at least one other person”). Responses were summed to provide a global social support score, which had excellent reliability (ɑ = .96).
Social network size. The network size score of the Social Network Index (SNI; Cohen et al., 1997) measures the number of all individuals with whom the individual has contact at least once every 2 weeks, within 12 possible social roles (including partners, parents, children, coworkers, neighbors, community group members, and others). The measure is a hybrid of categorical and count-based items, such that the relevance of each social role is established first (e.g., “Do you attend any classes on a regular basis?”), before assessing, if relevant, the degree of social contact within that role over a 2 week time frame (e.g., “How many fellow students or teachers do you talk to at least once every two weeks?”) Given this hybrid structure, internal consistency is not reported for the SNI (Cohen et al., 1997).
2.7. Analytic plan
Preliminary analyses were conducted to describe the sample, including prevalence of clinically significant symptoms, and to examine relevant bivariate relationships (i.e., differences in main study variables based on demographics, bivariate correlations among study variables, and differences in all variables based on stay-at-home status). Main analyses proceeded in three phases. First, to examine cross-sectional hypotheses regarding social distancing correlates of mental health symptoms even in the context of other, more established social factors, both social distancing variables (stay-at-home status and personal distancing behavior) were entered into a series of multiple regression analyses, one for each mental health outcome, together with social resource variables and demographic covariates. Demographic covariates were identified by including all demographics in initial regression models and retaining any demographic variable that was a statistically significant predictor of any outcome variable (p < .05), and were held constant across models. Second, the hypothesis that depression and GAD symptoms in the population increased from late February to late March was tested with repeated-measures tests of symptoms in the prospective subsample. Third, the hypothesis that social distancing would predict March symptoms, above and beyond social resources and February symptoms, was tested in multiple regression analyses identical to those conducted cross-sectionally in the full sample, but holding constant February symptoms.
3. Results
3.1. Preliminary analyses
3.1.1. Descriptive analyses
Descriptive statistics for all study variables in the March wave are presented in Table 1 . To assess the prevalence of clinically-relevant symptoms, we examined recommended clinical cutoffs where available. The common cutoff of 16 on the CES-D (Radloff, 1977) indicated that 38.4% of the sample was experiencing at least mild depression; a more stringent cutoff of 20 (Vilagut et al., 2016) identified 27.4% of participants in the clinical range. Recommended cutoffs for the GAD-7 (Spitzer et al., 2006) indicated that 22.8% were experiencing mild symptoms, 15.6% moderate symptoms (suggestive of a potential GAD diagnosis), and 9.0% severe symptoms. The ISI cutoff of 10, for the general population, showed 38.6% were experiencing insomnia symptoms within the clinical range (Morin et al., 2011).
Table 1.
Descriptive statistics and zero-order differences by stay-at-home order status in late March 2020 (N = 435).
| March 2020 Sample Descriptives |
Differences by Stay-at-Home Order Status |
||||||
|---|---|---|---|---|---|---|---|
| Mean (SD) |
Observed Range |
Stay-at-Home Statusa |
t(433) |
p |
d |
||
| Yes | No | ||||||
| n (%) | 283 (65.1%) | 152 (34.9%) | |||||
| Distancing Behavior | 0.48 (0.28) | −0.25–1.00 | 0.50 (0.27) | 0.46 (0.29) | 1.45 | .148 | .14 |
| Social Resources | |||||||
| Social support | 77.81 (14.97) | 30–96 | 78.51 (14.08) | 76.49 (16.48) | 1.34 | .180 | .13 |
| Social network size | 13.67 (8.71) | 0–56 | 13.71 (8.99) | 13.57 (8.18) | 0.17 | .869 | .02 |
| Mental Health Symptoms | |||||||
| Depression | 14.90 (11.99) | 0–53 | 15.84 (12.43) | 13.13 (10.96) | 2.26 | .025* | .23 |
| GAD | 5.66 (5.50) | 0–21 | 6.18 (5.73) | 4.70 (4.92) | 2.71 | .007** | .28 |
| Intrusive thoughts | 8.26 (4.36) | 0–20 | 8.55 (4.45) | 7.71 (4.14) | 1.92 | .055† | .20 |
| Insomnia | 7.44 (6.11) | 0–27 | 7.77 (6.18) | 6.84 (5.96) | 1.52 | .128 | .15 |
| Acute stress | 22.12 (11.02) | 10–50 | 23.28 (11.77) | 19.97 (9.12) | 3.01 | .003** | .31 |
Note. a Unless otherwise indicated, values are in the format M (SD).
* p < .05, ** p < .01, † p = .055.
3.1.2. Demographic differences in study variables
Older age was associated with lower mental health symptoms of several types (depression, r = −.15; GAD symptoms, r = −.16; acute stress, r = −.16, all ps < .001). Older age was also associated with less personal distancing behavior (r = −.12, p = .016). Women reported more intrusive thoughts (M = 9.05, SD = 4.48) than men (M = 7.50, SD = 4.12), t(430) = 3.73, p < .001, marginally more GAD symptoms (M = 6.18, SD = 5.66 versus M = 5.16, SD = 5.29), t(430) = 1.94, p = .053, and higher social support (M = 80.42, SD = 13.76 versus M = 75.62, SD = 15.52), t(430) = 3.38, p = .001. There were no significant racial/ethnic differences in any study variables, whether comparing individual racial/ethnic categories (all ps > .44) or minority status as a binary variable (all ps > .15). Several differences emerged based on income (ANOVA ps ≤ .01). Participants with the lowest annual household income (less than $20,000) were significantly higher in depression than all other income categories (all post-hoc comparison ps < .05), and those with an income of $20,000–39,999 were significantly higher in depression than those in the highest bracket ($120,000 or more), p < .05. Personal distancing behavior, social support, and social network size all increased with income, with differences largest at the extremes. Higher education was associated with a larger social network (ANOVA p < .001), except among doctoral degree holders (n = 5), whose social networks were significantly smaller than those with master's degrees.
3.1.3. Zero-order associations among study variables
Group comparisons on all study variables by stay-at-home status are presented in Table 1. More than half of the sample (65.1%; 283 participants) reported being under a stay-at-home order. Participants under a stay-at-home order reported significantly higher depression, GAD symptoms, and acute stress and marginally higher intrusive thoughts, but did not differ in insomnia. Personal distancing behavior, social support, and social network size did not differ based on stay-at-home status. Correlations among all continuous study variables are in Table 2 . Personal distancing behavior was significantly and positively associated with intrusive thoughts, but not with other mental health symptoms in these zero-order analyses. Social support was negatively associated with all symptom types. Social network size was correlated with fewer depressive symptoms but more intrusive thoughts.
Table 2.
Zero-order correlations among study variables in late March 2020 (N = 435).
| Social support | Social network size | Depression | GAD | Intrusive thoughts | Insomnia | Acute stress | |
|---|---|---|---|---|---|---|---|
| Social Distancing | |||||||
| Personal distancing behavior | .23** | .38** | .02 | .08 | .23** | −.03 | .06 |
| Social Resources | |||||||
| Social support | – | .40** | −.55** | −.33** | −.10* | −.35** | −.38** |
| Social network size | – | −.17** | −.05 | .12* | −.08 | −.06 | |
| Mental Health Symptoms | |||||||
| Depression | – | .82** | .53** | .65** | .77** | ||
| GAD | – | .65** | .62** | .71** | |||
| Intrusive thoughts | – | .38** | .49** | ||||
| Insomnia | – | .53** | |||||
| Acute stress | – | ||||||
Note. * p < .05, ** p < .01.
3.2. Main analyses
3.2.1. Social distancing and mental health symptoms (March 2020)
We hypothesized that social distancing behavior would be associated with higher symptoms cross-sectionally, above and beyond adaptive effects of social support and social network size. Results of the multiple regression analyses examining this question are depicted in the upper half of Table 3 ; all analyses adjusted for identified demographic effects of age, gender, and income. As expected, social support had relatively strong and independent negative associations with all symptom types. Social network size was independently associated with intrusive thoughts and acute stress; surprisingly, this association was in the positive direction.
Table 3.
Social distancing and social resources as predictors of mental health symptoms in late March 2020 (top) and as predictors of symptom change from February to March 2020 (bottom).
| Depression | GAD | Intrusive thoughts | Insomnia | Acute stress | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | β | b | SE | β | b | SE | β | b | SE | β | b | SE | β | |
| Full Sample (N = 435) | |||||||||||||||
| Age | −0.15 | .04 | −.15** | −0.08 | .02 | −.18** | −0.03 | .02 | −.08 | −0.04 | .03 | −.08 | −0.15 | .04 | −.16** |
| Gender | 3.59 | .96 | .15** | 2.14 | .50 | .20** | 2.06 | .41 | .24** | 1.07 | .58 | .09 | 2.32 | .99 | .11* |
| Income | −0.64 | .30 | −.09* | −0.16 | .16 | −.05 | −0.21 | .13 | −.08 | −0.23 | .18 | −.06 | −0.47 | .31 | −.07 |
| Social support | −0.49 | .03 | −.61** | −0.15 | .02 | −.42** | −0.07 | .02 | −.23** | −0.16 | .02 | −.39** | −0.33 | .04 | −.45** |
| Social network size | 0.08 | .06 | .06 | 0.06 | .03 | .09 | 0.07 | .03 | .14** | 0.06 | .04 | .09 | 0.15 | .07 | .12* |
| Stay-at-home status | 3.21 | .97 | .13** | 1.48 | .50 | .13** | 0.66 | .41 | .07 | 1.17 | .58 | .09* | 3.62 | .99 | .16** |
| Distancing behavior | 6.12 | 1.83 | .14** | 2.72 | .95 | .14** | 3.89 | .78 | .25** | 0.73 | 1.09 | .03 | 4.37 | 1.88 | .11* |
| F (7, 427) | 37.99** | 16.37** | 10.59** | 10.82** | 17.83** | ||||||||||
| Adjusted R2 | 0.37 | 0.20 | 0.13 | 0.14 | 0.21 | ||||||||||
| Prospective Subsample Controlling for Prior (February) Symptoms (n = 118) | |||||||||||||||
| Time 0 Symptoms | 0.69 | .06 | .75** | 0.68 | .06 | .72** | |||||||||
| Age | −0.05 | .06 | −.04 | −0.03 | .03 | −.07 | |||||||||
| Gender | 4.16 | 1.32 | .17** | 1.72 | .65 | .16** | |||||||||
| Income | −0.14 | .41 | −.02 | 0.03 | .20 | .01 | |||||||||
| Social support | −0.13 | .06 | −.15* | −0.06 | .03 | −.16* | |||||||||
| Social network size | −0.02 | .08 | −.01 | 0.01 | .04 | .03 | |||||||||
| Stay-at-home status | 1.10 | 1.25 | .04 | 0.49 | .62 | .04 | |||||||||
| Distancing behavior | 9.91 | 2.50 | .23** | 4.34 | 1.23 | .23** | |||||||||
| F (8, 109) | 37.46** | 27.30** | |||||||||||||
| Adjusted R2 | 0.71 | 0.64 | |||||||||||||
Note. Gender is coded such that 1 = female. Stay-at-home status is coded such that 1 = yes. Time 0 Symptoms refers to the corresponding symptom type at the February 2020 timepoint. *p < .05, **p < .01.
Stay-at-home status and personal distancing behavior were each significantly and independently associated with mental health symptoms. Being under a stay-at-home order was associated with higher depression, GAD symptoms, insomnia, and acute stress, but not associated with intrusive thoughts. Personal distancing behavior was associated with higher depression, GAD symptoms, intrusive thoughts, and acute stress, but not with insomnia. In sum, both measures of social distancing (stay-at-home status and distancing behavior) were associated independently with concurrent symptoms, and these effects were evident above and beyond the expected, protective effects of social resources.1
3.2.2. February-to-March mental health symptom change
Our second hypothesis was that mental health symptoms would increase from February to March. Repeated-measures tests using the two prospectively measured symptom types (depression and GAD) in the prospective subsample showed that indeed, depressive symptoms increased between late February and late March, from 12.60 (SD = 13.14) to 14.78 (SD = 12.02), t(117) = 3.12, p = .002, d = 0.29. Similarly, GAD symptoms increased during this time period, from M = 4.42 (SD = 5.55) to M = 5.42 (SD = 5.28), t(117) = 2.99, p = .003, d = 0.28. Symptom levels in March did not differ between prospective vs. March-only participants [depression M = 14.94, SD = 12.00, t(433) = 0.12, p = .902; GAD M = 5.76, SD = 5.58, t(433) = 0.58, p = .565], suggesting the observed increase was not unique to the prospective sample, but rather might have been detected similarly had the full sample been measured prospectively.
3.2.3. Social distancing and February-to-March symptom change
Our final hypothesis was that magnitudes of prospective symptom increases would be associated with the extent of social distancing, independently of social resources. For both prospectively measured symptom types (depression and GAD), we conducted multiple regression analyses identical to those in the full sample, but adding to each model the corresponding February symptom level as an additional covariate.2 Results are displayed in the lower half of Table 3.
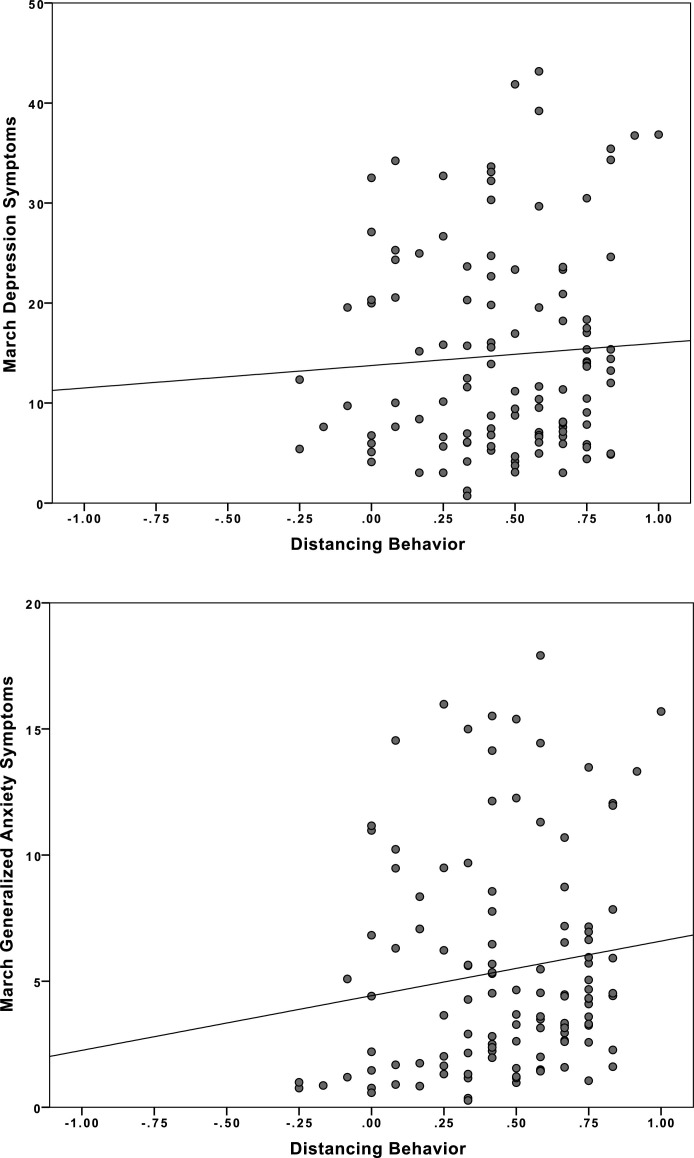
Not surprisingly, February symptoms were strong predictors of March symptoms. When accounting for early symptoms, stay-at-home status was no longer significantly associated with March symptoms, and social support was less strongly associated with lower symptoms. However, personal distancing behavior remained significantly positively associated with both depression and GAD symptoms in March. The independent associations between distancing behavior and March depression and GAD symptoms, adjusting for all predictors in the models including respective February symptoms, are depicted in Fig. 1 . Unstandardized coefficients can be consulted to interpret the magnitude of this effect: engaging in all 12 measured distancing behaviors (which would yield a “perfect” distancing score of 1) would account for nearly 10 points in depression severity (on the 60-point CES-D scale), and over 4 points in GAD severity (on the 21-point GAD-7 scale), controlling for all predictors including February symptom levels.
Fig. 1.
Association between Personal Social Distancing Behaviors and Increases in Depression and Anxiety Symptoms from February to March 2020. Note. March symptom levels are adjusted for all covariates reported in the respective, prospective multiple regression models, including February symptom levels. Distancing behavior: −1 = increased social contact, 0 = no reported change in behaviors from before COVID-19, 1 = distancing behavior reported in all 12 behavioral domains.
4. Discussion
This study examined the mental health effects associated with social distancing, the most broadly visible public health intervention to fight the global spread of COVID-19. In a nationwide sample of U.S. adults at two time points early in the American experience of the pandemic, we found evidence that both governmental stay-at-home orders and individuals’ personal social distancing behavior were associated with symptoms of a range of mental health conditions. In late March 2020, as the pandemic escalated dramatically and states began implementing stay-at-home orders, being subject to those orders was associated with more symptoms of depression, GAD, acute stress, and insomnia. Independently, engaging in personal social distancing behavior was associated with more depression, GAD, acute stress, and intrusive thoughts. These associations with social distancing existed despite individuals’ levels of perceived social support, suggesting that even social resources known to protect mental health do not eliminate the impact of social distancing. Indeed, our approach disentangled the role of social distancing from other important components of the social context of the pandemic, and also identified distinct roles of stay-at-home orders and personal distancing behavior.
These findings replicate early cross-sectional evidence that the COVID-19 pandemic may be impairing mental health in the general population (Cao et al., 2020; Tull et al., 2020) and extend them to a broader range of mental health outcomes. Our approach also makes a contribution by examining simultaneous effects of public and private levels of social distancing, showing that both are independently linked with symptom severity. As such, this study extends findings from past, less widespread viral epidemics outside of the U.S. (Cava et al., 2005; Mak et al., 2009; Pfefferbaum et al., 2012) and from studies of the more severe distancing of quarantine (Brooks et al., 2020; Hawryluck et al., 2004).
Importantly, using data available prospectively in mid-to-late February, the present study shows both temporal increases in depression and anxiety symptoms as the presence of COVID-19 grew in the U.S.and a relationship of social distancing to these increases. Cross-sectional approaches (e.g., Cao et al., 2020; Tull et al., 2020) are agnostic on causal direction: instead of social distancing harming mental health, perhaps people with elevated symptoms are simply more likely to distance. This study does not establish direction of effects or causality, given that distancing behavior was not manipulated or measured in February, but our findings do suggest that distancing was at least associated with worsening mental health course during this period. These models also suggested that perhaps the private, behavioral forms of social distancing may be particularly relevant to worsening mental health, compared to public interventions. A caveat to this possibility, however, is that distancing behaviors may have had more robust effects due to being in place for relatively longer than stay-at-home orders at the time of data collection. Ongoing follow-up studies can help untangle these possibilities. It is also important to note that although prospective analyses showed associations of distancing behavior with symptom change that correspond to clinically-meaningful magnitudes, absolute changes in depression and GAD symptoms, although statistically significant, were relatively modest (2.18 points on the CES-D and 1 point on the GAD-7) and should not be interpreted as evidence of marked clinically-relevant increases across the sample or the general population.
Although this study provides consistent evidence of social distancing associations with five major mental health outcomes, its limitations can guide future research as the pandemic unfolds. Most importantly, even with its longitudinal elements, our design remains correlational, which raises several issues. First is causal direction: the present findings do not rule out the possibility that symptoms (including change in symptoms) affect personal distancing behavior, although this is less likely for stay-at-home order effects, which are externally determined. Second is a number of plausible confounding variables. Stay-at-home orders and personal distancing behaviors have proven to be meaningful, highly salient, and uniquely impactful aspects of the pandemic experience, but they may correlate with other constructs not measured here, such as prevalence of cases in one's geographical area, social norms around distancing, and non-governmental actions (e.g., employer work-from-home policies). A range of pandemic-related experiences that were not measured here are likely implicated in mental health, including personal, family, and community exposure to COVID-19; impact on daily life stressors, including child care and elder care responsibilities; and economic and employment impact, including job loss or working from home. Many of these coincided with social distancing interventions (e.g., stay-at-home orders were enacted earlier in states with more COVID-19 risk, and both forms of distancing involved changes in daily routines, demands, and resources). Thus, social distancing and social resource effects may also reflect associated effects of pandemic-related stressors.3 Research currently underway, including ongoing longitudinal follow-up in the present study, can determine whether links between mental health and social distancing are better explained by other contemporaneous factors.
As the dynamics of COVID-19 unfold, longitudinal studies will be needed to determine the mechanistic psychological processes that social distancing may either introduce (e.g., isolation), exacerbate (e.g., emotion dysregulation), or disrupt (e.g., relationship quality), as well as specificity to particular symptom outcomes (e.g., depression versus insomnia). This research should also examine moderators of distancing effects, including pre-existing mental health conditions, physical vulnerability to COVID-19, the degree to which distancing impacts ability to work or care for family, and whether distancing essentially means true isolation for some (e.g., those who live alone). Longitudinal work can also address another important question: Do symptoms early in the pandemic represent true phenomena of clinical concern, or normative, non-pathological responses to the initial emergence of a unique and overwhelming event? Of course, experienced symptoms are meaningful regardless of whether they reflect psychiatric abnormality, but for this reason we have emphasized “mental health” as opposed to clinical psychopathology.
The COVID-19 threat increases reliance on online research methods (Gruber et al., 2020). Mechanical Turk, while more demographically diverse than many online and traditional samples (Buhrmester et al., 2011), can have limitations related to participant inattentiveness and lack of researcher control over the study session (Paolacci and Chandler, 2014). We preempted these data quality concerns by following rigorous recruitment and data quality practices (Buhrmester et al., 2011; Paolacci and Chandler, 2014; Peer et al., 2014). Despite the relative representativeness of our sample on most demographic indicators, the sample should not be considered nationally representative; other characteristics of MTurk participants may limit generalizability (e.g., they may be more liberal, more introverted, and more frequent Internet users than the general population; Paolacci and Chandler, 2014; Chandler and Shapiro, 2016). Although the sample was relatively demographically diverse overall, it was less so in terms of race/ethnicity. There were no racial/ethnic differences in study variables, which may be a function of statistical power in the present, majority-white sample. However, evidence is building that individuals of marginalized racial and ethnic backgrounds are disproportionately impacted by COVID-19 in terms of contracting the virus, facing severe health outcomes, and death (Webb Hooper et al., 2020), and this may extend to psychological processes. Future research could examine how stressors specific to marginalized groups, including chronic risk factors (e.g., experiences of racism) and acute risk factors (e.g., disproportionate COVID-19 risk and impact to daily life), may impact the relationship between social distancing and mental health symptoms.
Finally, constructs were measured by self-report. While well-suited to measurement of mental health symptoms and perceived social resources, self-report may not correspond with objective governmental distancing initiatives or personal distancing, a construct perhaps especially subject to reporting biases (e.g., social desirability). Moreover, symptom measures vary somewhat in their time frame, e.g., depression within the last week and GAD symptoms within the last 2 weeks. Retaining standard time frames is essential for maintaining psychometric properties and allowing comparison with other studies, but aspects of the pandemic change quickly, and measures with shorter time frames may naturally be more temporally precise with respect to external events.
The present study has several strengths. First, it used a national sample of adults that was fairly representative of the U.S. in terms of age, gender, education, and income. Second, we examined 2 time points that captured the extraordinary period of initial adjustment to COVID-19, beginning well before the pandemic was prominent in awareness and disrupting life in the U.S. on a widespread scale. Third, our inclusion of social support and social network size addressed social distancing in the context of other social factors implicated in mental health. Fourth, we used well-validated measures of specific mental health outcomes, and our sample represented a wide range of most symptom types. Lastly, our novel approach to assessing the extent of social distancing behavior dimensionally appears psychometrically sound based on this initial research, and could be promising for future COVID-19 studies.
The COVID-19 pandemic is expected to have profound mental health effects, which research, policy, and clinical science have been called on to address (Gruber et al., 2020; Pfefferbaum and North, 2020). The present findings provide empirical evidence of negative mental health impact to underscore these calls. In the absence of a vaccine, the upcoming year(s) are expected to bring periodic outbreaks and cyclical reinstatements of social distancing recommendations. Social distancing interventions should not be avoided, as they appear critical to controlling the virus; it is for biomedical sciences, public health, and related fields to determine interventions at the public level (e.g., phased state “re-opening” standards) and private level (e.g., encouraging individuals to wear masks) that promise to protect lives. Rather, the present study highlights the possible mental health correlates of virus-containment initiatives, and the need for simultaneous investment into mental health interventions to mitigate these effects. Already-effective interventions for mental health and psychological distress may benefit from more explicit targeting of the role of social disruption in psychological responses during the pandemic, and from increased access to telehealth modalities that allow clinicians to reach those most vulnerable to the mental health impact of the pandemic.
Author statement
Study conceptualization: B. Marroquín and V. Vine. Study design and data collection: B. Marroquín, V. Vine, and R. Morgan. Data analysis and interpretation: B. Marroquín and V. Vine. Drafting and revision of manuscript: B. Marroquín and V. Vine. All authors approved the final manuscript.
Funding
This work was supported in part by the Monica Lester Endowment for Psychology at Loyola Marymount University.
Declaration of Competing Interest
The authors have no interests to declare.
Footnotes
Results of stepwise versions of these regression models are presented in Supplementary Tables 1 and 2. Social distancing variables explained statistically significant additional variance, compared to models including only demographic covariates and social resources, in March depression, GAD, intrusive thoughts, and acute stress, and in February-to-March changes in depression and GAD.
All zero-order correlations in the prospective subsample among social distancing, social resources, depressive symptoms, and GAD symptoms in late March showed the same patterns as in the main sample, including statistical significance. Mirroring findings with March depressive symptoms, February depressive symptoms were correlated with March social support (r = −.66, p < .001) and social network size (r = −.27, p = .003), and not personal distancing behavior (r = −.12, p = .192). February GAD symptoms were correlated with March social support (r = −.49, p < .001) and not personal distancing behavior (r = −.07, p = .425), but unlike March GAD symptoms, February GAD symptoms were significantly correlated with social network size (r = −.19, p = .036).
We conducted a series of exploratory analyses to examine potential external factors that might have been associated with stay-at-home orders and personal distancing behavior and might provide alternative explanations for our findings, including personal exposure to COVID-19 and geographical proximity to cases. At the beginning of data collection on March 26, the 86,379 COVID-19 cases in the country represented approximately 0.026% of the U.S. population. Accordingly, when asked, all participants in our sample denied being positive for COVID-19. 395 individuals (90.8%) in our sample reported not knowing any other person who was ill or diagnosed with COVID-19, and 40 (9.2%) reported knowing between 1 and 9 such people. T-tests comparing these groups showed that the latter group experienced higher depressive symptoms and acute stress in March, but including this term in all original regression models resulted in no change to the pattern or significance of findings. To examine geographical proximity, we used cumulative COVID-19 case data for each state on March 26, assigning each participant the number of cases in their state, from 46 (South Dakota) to 6,876 (New Jersey), with an extreme outlier of 39,058 (New York). Correlational analyses (excluding New York participants, whose extreme case values rendered their inclusion statistically inappropriate) indicated that the number of cases in one's state was not significantly associated with any of the study variables, and adding participants' state case count to our original regression analyses did not affect the patterns or statistical significance. Although replicating our regression analyses was impossible among New Yorkers only (n = 31), correlational analyses showed that among New Yorkers more personal distancing behavior was significantly associated with higher depression, GAD symptoms, intrusive thoughts, and acute stress, and was not correlated with social resource variables. Although these analyses represent rough tests of potential alternative explanations related to personal and geographical COVID-19 exposure, together they suggest that neither personal COVID-19 status, the awareness of social contacts with COVID-19, nor the levels of COVID-19 cases in one's state account for our primary findings.
Supplementary material associated with this article can be found, in the online version, at doi: 10.1016/j.psychres.2020.113419.
Appendix. Supplementary materials
References
- Amirkhan J.H. Stress overload: a new approach to the assessment of stress. Am. J. Community Psychol. 2012;49:55–71. doi: 10.1007/s10464-011-9438-x. [DOI] [PubMed] [Google Scholar]
- Amirkhan J.H. A brief stress diagnostic tool: the Short Stress Overload Scale. Assessment. 2018;25:1001–1013. doi: 10.1177/1073191116673173. [DOI] [PubMed] [Google Scholar]
- Bastien C.H., Vallières A., Morin C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/S1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhrmester M., Kwang T., Gosling S.D. Amazon’s Mechanical Turk: a new source of inexpensive, yet high-quality, data? Perspect. Psychol. Sci. 2011;6:3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cava M.A., Fay K.E., Beanlands H.J., McCay E.A., Wignall R. The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nurs. 2005;22:398–406. doi: 10.1111/j.0737-1209.2005.220504.x. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2020. Coronavirus (COVID-19). https://www.cdc.gov/coronavirus/2019-ncov/ (accessed 21 August 2020).
- Chandler J., Shapiro D. Conducting clinical research using crowdsourced convenience samples. Ann. Rev. Clin. Psych. 2016;12:53–81. doi: 10.1146/annurev-clinpsy-021815-093623. [DOI] [PubMed] [Google Scholar]
- Cohen S. Social relationships and health. Am. Psychol. 2004;59:676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Cohen S., Doyle W.J., Skoner D.P., Rabin B.S., Gwaltney J.S., Jr. Social ties and susceptibility to the common cold. JAMA. 1997;277:1940–1944. doi: 10.1001/jama.1997.03540480040036. [DOI] [PubMed] [Google Scholar]
- Cohen S., Wills T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985;98:310–357. doi: 10.1037/0033-2909.98.2.310. [DOI] [PubMed] [Google Scholar]
- Cutrona C.E., Russell D.W. In: Jones W.H., Perlman D., editors. Vol. 1. JAI Press; Greenwich, CT: 1987. The provisions of social relationships and adaptation to stress; pp. 37–67. (Advances in Personal Relationships). [Google Scholar]
- Falsetti S.A., Monnier J., Davis J.L., Resnick H.S. Intrusive thoughts in posttraumatic stress disorder. J. Cogn. Psychother. 2002;16:127–143. doi: 10.1891/jcop.16.2.127.63993. [DOI] [Google Scholar]
- Gruber, J., Prinstein, M.J., Clark, L.A., Rottenberg, J., Abramowitz, J.S., Albano, A.M., Aldao, A., Borelli, J.L., Davila, J., Forbes, E.E., Gee, D.G., Hall, G.C.N., Hallion, L.S., Hinshaw, S.P., Hofmann, S.G., Hollon, S.D., Joormann, J., Kazdin, A.E., Klein, D.N., Levenson, R.W., MacDonald A.W., III, McKay, D., McLaughlin, K.A., Mendle, J., Miller, A.B., Neblett, E., Nock, M., Olatunji, B.O., Persons, J.B., Rozek, D.C., Schleider, J.L., Slavich, G.M., Teachman, B.A., Vine, V.J., Weinstock, L., 2020. Mental health and clinical psychological science in the time of COVID-19: challenges, opportunities, and a call to action. American Psychologist. Advance online publication. 10.1037/amp0000707. [DOI] [PMC free article] [PubMed]
- Harkness, K.L., Hayden, E.P., 2020. The Oxford handbook of stress and mental health. Oxford University Press. 10.1093/oxfordhb/9780190681777.001.0001.
- Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004;10:1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb Hooper M., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. JAMA. 2020;323:2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler K.S., Gardner C.O. Depressive vulnerability, stressful life events and episode onset of major depression: a longitudinal model. Psychol. Med. 2016;46:1865–1874. doi: 10.1017/S0033291716000349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler K.S., Hettema J.M., Butera F., Gardner C.O., Prescott C.A. Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Arch. Gen. Psychiatry. 2003;60:789–796. doi: 10.1001/archpsyc.60.8.789. [DOI] [PubMed] [Google Scholar]
- Mak I.W.C., Chu C.M., Pan P.C., Yiu M.G.C., Chan V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry. 2009;31:318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marroquín, B., Tennen, H., Stanton, A., 2017. Coping, emotion regulation, and well-being: intrapersonal and interpersonal processes, in: The Happy Mind: Cognitive Contributions to Well-Being. pp. 253–274. 10.1007/978-3-319-58763-9_14.
- Morin C.M., Belleville G., Bélanger L., Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paolacci G., Chandler J. Inside the Turk. Curr. Dir. Psychol. Sci. 2014;23:184–188. doi: 10.1177/0963721414531598. [DOI] [Google Scholar]
- Pascual-Vera B., Akin B., Belloch A., Bottesi G., Clark D.A., Doron G., Fernández-Alvarez H., Ghisi M., Gómez B., Inozu M., Jiménez-Ros A., Moulding R., Ruiz M.A., Shams G., Sica C. The cross-cultural and transdiagnostic nature of unwanted mental intrusions. Int. J. Clin. Heal. Psychol. 2019;19:85–96. doi: 10.1016/j.ijchp.2019.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peer E., Vosgerau J., Acquisti A. Reputation as a sufficient condition for data quality on Amazon Mechanical Turk. Behav. Res. Methods. 2014;46:1023–1031. doi: 10.3758/s13428-013-0434-y. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum, B., North, C.S., 2020. Mental health and the Covid-19 pandemic. N. Engl. J. Med.10.1056/NEJMp2008017. [DOI] [PubMed]
- Pfefferbaum B., Schonfeld D., Flynn B.W., Norwood A.E., Dodgen D., Kaul R.E., Donato D., Stone B., Brown L.M., Reissman D.B., Jacobs G.A., Hobfoll S.E., Jones R.T., Herrmann J., Ursano R.J., Ruzek J.I. The H1N1 crisis: a case study of the integration of mental and behavioral health in public health crises. Disaster Med. Public Health Prep. 2012;6:67–71. doi: 10.1001/dmp.2012.2. [DOI] [PubMed] [Google Scholar]
- Radloff L.S. The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Salters-Pedneault K., Vine V., Mills M.A., Park C., Litz B.T. The Experience of Intrusions scale: a preliminary examination. Anxiety Stress Coping. 2009;22:27–37. doi: 10.1080/10615800802403823. [DOI] [PubMed] [Google Scholar]
- Sinha S.S. Trauma-induced insomnia: a novel model for trauma and sleep research. Sleep Med. Rev. 2016;25:74–83. doi: 10.1016/j.smrv.2015.01.008. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Takarangi M.K.T., Oulton J.M., Green D.M., Strange D. Boundary restriction for negative emotional images is an example of memory amplification. Clin. Psychol. Sci. 2016;4:82–95. doi: 10.1177/2167702615569912. [DOI] [Google Scholar]
- Thoits P.A. Mechanisms linking social ties and support to physical and mental health. J. Health Soc. Behav. 2011;52:145–161. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- Tull M.T., Edmonds K.A., Scamaldo K.M., Richmond J.R., Rose J.P., Gratz K.L. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino B.N. Understanding the links between social support and physical health: a life-span perspective with emphasis on the separability of perceived and received support. Perspect. Psychol. Sci. 2009;4:236–255. doi: 10.1111/j.1745-6924.2009.01122.x. [DOI] [PubMed] [Google Scholar]
- Van Bavel J.J., Baicker K., Boggio P.S., Capraro V., Cichocka A., Cikara M., Crockett M.J., Crum A.J., Douglas K.M., Druckman J.N., Drury J., Dube O., Ellemers N., Finkel E.J., Fowler J.H., Gelfand M., Han S., Haslam S.A., Jetten J., Kitayama S., Mobbs D., Napper L.E., Packer D.J., Pennycook G., Peters E., Petty R.E., Rand D.G., Reicher S.D., Schnall S., Shariff A., Skitka L.J., Smith S.S., Sunstein C.R., Tabri N., Tucker J.A., van der Linden S., van Lange P., Weeden K.A., Wohl M.J.A., Zaki J., Zion S.R., Willer R. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020;4:460–471. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- Vilagut G., Forero C.G., Barbaglia G., Alonso J. Screening for depression in the general population with the Center for Epidemiologic Studies Depression (CES-D): a systematic review with meta-analysis. PLoS ONE. 2016;11 doi: 10.1371/journal.pone.0155431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2020. Coronavirus disease (COVID-19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed 21 August 2020).
- Worldometer, 2020. COVID-19 coronavirus pandemic. https://www.worldometers.info/coronavirus(accessed 18 May 2020).
- Zhang S.X., Wang Y., Rauch A., Wei F. Unprecedented disruption of lives and work: health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112958. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.