Abstract
Iliotibial band syndrome or friction syndrome is an overuse disorder of the lateral knee. It is commonly reported in athletes, such as runners and cyclists, and refers to pain related to physical activity. The diagnosis is based on clinical history and physical assessment. Imaging, including ultrasound, is mainly performed in recurrent or refractory cases. The purpose of this paper is to review the etiology, diagnosis, and therapy of iliotibial band syndrome with a focus on ultrasound imaging and ultrasound-guided treatment. Ultrasound findings include soft-tissue edematous swelling or discrete fluid collection, suggestive of bursitis, between the iliotibial band and the lateral femoral epicondyle. The thickening of the iliotibial band has been inconsistently reported. Treatment varies according to the disease phase and, in the acute phase, consists of rest, physical therapy, and anti-inflammatory medications. Ultrasound-guided local steroid injections are effective in relieving symptoms.
Keywords: Fascia lata, Gerdy tubercle, Iliotibial friction syndrome, Iliotibial tract, Knee, Sonography
Introduction
The iliotibial band is a portion of the fascia lata. It receives contributions from the tensor fascia lata and gluteus maximus muscles in the lateral thigh and terminates distally about the knee, having the main ribbon-shaped insertion into the Gerdy tubercle on the anterior aspect of the lateral tibial condyle [1]. The iliotibial band transmits forces from the hip to the knee, acts as a lateral stabilizer of the knee, and also serves an important postural function [2, 3].
Iliotibial band syndrome, also known as iliotibial band friction syndrome, is an overuse disorder of the lateral knee that refers to pain related to lower limb activity [4]. This syndrome is one of the most common knee injuries in runners and is also frequently encountered in other athletes, such as cyclists and basketball, soccer, or hockey players [5–7]. Particularly, it has been reported as a cause of knee pain in 62% and 38% of female and male runners, respectively [6], and in 24% of cyclists [7]. The diagnosis of iliotibial band syndrome is based on clinical assessment, and imaging is mostly performed in recurrent or refractory cases [4]. Both magnetic resonance imaging and ultrasound may be used to confirm the diagnosis. The role of magnetic resonance imaging has been well addressed in recent literature [8, 9] and is beyond the scope of this paper. As a cost-effective imaging modality that enables visualization of the superficial soft-tissue structures with high resolution, dynamic evaluation, and comparison with the contralateral healthy side [10–19], ultrasound is valuable for the assessment of iliotibial band syndrome. The purpose of this paper is to review the etiology, diagnosis, and therapy of iliotibial band syndrome, with a focus on ultrasound imaging and ultrasound-guided treatment.
Etiology and risk factors
Iliotibial band syndrome has several proposed causes, including friction of the iliotibial band against the lateral epicondyle of the femur [20] compression of the fat and connective tissue deep to the iliotibial band [21], and chronic inflammation of an adventitial bursa underneath the iliotibial band [22]. The first is linked to iliotibial band rubbing back and forth across the lateral femoral epicondyle during activities involving repetitive knee flexion and extension, thus resulting in friction of the iliotibial band and inflammation of the adjacent soft tissues [20]. This etiology has been debated over the years, particularly with regard to the direction and extent of the iliotibial band motion. However, an ultrasound study has demonstrated that the iliotibial band moves in an antero-posterior direction relative to the lateral femoral epicondyle during knee extension and flexion, thus supporting the central role of friction as an etiological factor [23]. Other proposed etiologies, such as fat compression [21] and soft-tissue irritation [24] deep to the iliotibial band, may coexist and explain why pathological changes primarily occur in the soft tissues rather than within the iliotibial band [25]. Particularly, chronic irritation can result in an adventitial or secondary bursitis underneath the iliotibial band, where no primary bursa has been consistently identified in cadaveric studies [22].
The predisposing factors associated with iliotibial band syndrome are both extrinsic and physical or intrinsic factors. The extrinsic factors include training errors, such as a rapid increase in mileage and downhill running [26, 27]. Particularly, in the latter case, knee flexion is reduced, and iliotibial band friction may be facilitated as this occurs around or slightly below 30° of flexion [27]. The main physical or intrinsic factors include genu varum, hip abduction weakness, and lower limb length discrepancy [27, 28]. Particularly, genu varum may favor the development of iliotibial band syndrome by increasing the strain of the iliotibial band during weight-bearing, as seen on sonoelastography in female athletes with genu varum in comparison with normal knee alignment [29].
Clinical presentation
Pain occurs at the level of the distal iliotibial band, between the lateral femoral epicondyle and its tibial insertion, and is associated with regular physical activity. Initially, lateral knee pain is often experienced late in or after completing a sporting activity. As the syndrome progresses, it begins earlier in the course of the activity [4]. On physical assessment, tenderness can be observed at the level of the lateral femoral epicondyle [4].
Ultrasound imaging
Ultrasound provides an excellent visualization of the superficial soft-tissue structures of the knee, including the iliotibial band, using linear high-frequency transducers [30, 31]. On ultrasound, the iliotibial band is assessed in the coronal plane on the lateral aspect of the knee. Under healthy conditions, it appears as a linear fibrillar structure that crosses over the lateral epicondyle of the femur and inserts distally into the Gerdy tubercle of the tibia [32]. The iliotibial band can also be easily depicted if the transducer is placed in the midline to visualize the patellar tendon along its longitudinal axis and then moved laterally. The iliotibial band is the first identifiable longitudinal structure that extends proximally from the lateral tibial condyle [33]. Additionally, the iliotibial band can be evaluated in the axial plane over the lateral femoral epicondyle. A dynamic assessment in the axial plane can reveal various degrees of snapping along the lateral femoral epicondyle [34].
In healthy individuals, iliotibial band mean thickness on ultrasound has been reported to be 1.1–1.9 mm at the level of the lateral femoral epicondyle [35, 36] and 3.4 mm at the level of the lateral tibial condyle [35]. A negative correlation has been found between iliotibial band thickness and age, i.e., mean thickness decreases with increasing age [35]. On the other hand, no association has been observed between iliotibial band thickness and height, weight, dominant limb, or the volume of training or sporting activity [35, 36].
The diagnosis of iliotibial band syndrome relies on clinical history and physical assessment [4]. Imaging, including ultrasound, is reserved for recurrent or refractory cases and requires correlation with clinical information [4]. Ultrasound findings of iliotibial band syndrome include soft-tissue edematous swelling (Fig. 1) and discrete fluid collection (Figs. 2, 3, 4), suggestive of adventitial bursitis, between the iliotibial band and the lateral femoral epicondyle [37–39]. The thickening of the iliotibial band has been reported inconsistently [40, 41], and researchers have questioned whether this finding occurs only in chronic cases [41]. Cortical irregularity of the adjacent femoral epicondyle can also be observed [33]. A common pitfall is the normal lateral recess of the knee joint as fluid is associated with the iliotibial band in a large number of asymptomatic runners, deep or anterior to it [42]. The lateral recess extends adjacent to the lateral femoral condyle, deep to the iliotibial band [24], and should not be mistaken for an adventitial bursitis. Continuity of the recess with the joint can be demonstrated with ultrasound (Figs. 5, 6) [43].
Fig. 1.
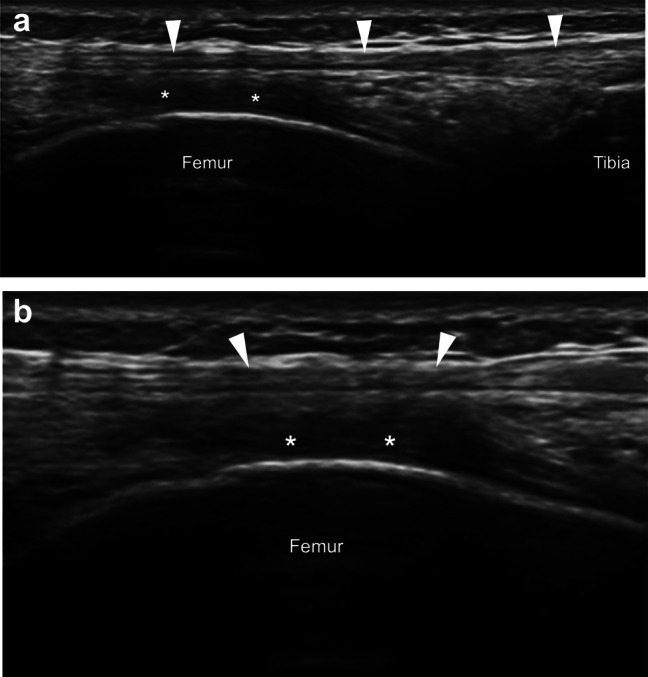
On longitudinal (a) and axial (b) sonograms, soft-tissue hypoechoic edematous swelling (asterisks) is noted between the iliotibial band (arrowheads) and the lateral femoral epicondyle
Fig. 2.

On longitudinal (a) and axial (b) sonograms, a discrete fluid collection suggestive of bursitis (asterisk) is noted between the iliotibial band (arrowheads) and the lateral femoral epicondyle
Fig. 3.
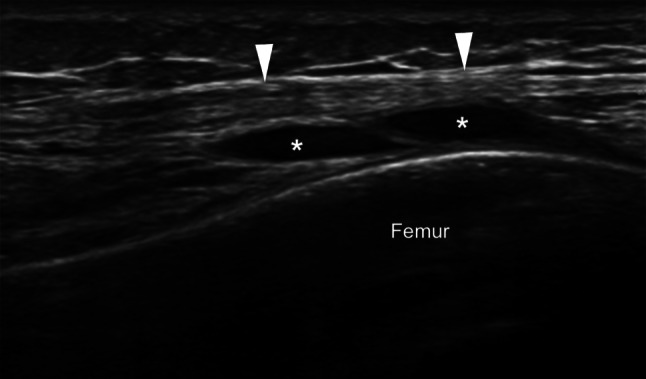
On a longitudinal sonogram, a septated bursa (asterisks) is noted between the iliotibial band (arrowheads) and the lateral femoral epicondyle
Fig. 4.

On longitudinal sonograms in different patients (a, b), bursae (arrows) are noted between the iliotibial band (IT band) and the lateral femoral epicondyle
Fig. 5.

On a longitudinal sonogram, knee joint effusion (V) and synovial hypertrophy are noted in the lateral recess of the joint, adjacent to the lateral femoral condyle and deep to the iliotibial band (arrowheads). Continuity of the effusion with the knee joint is demonstrated
Fig. 6.
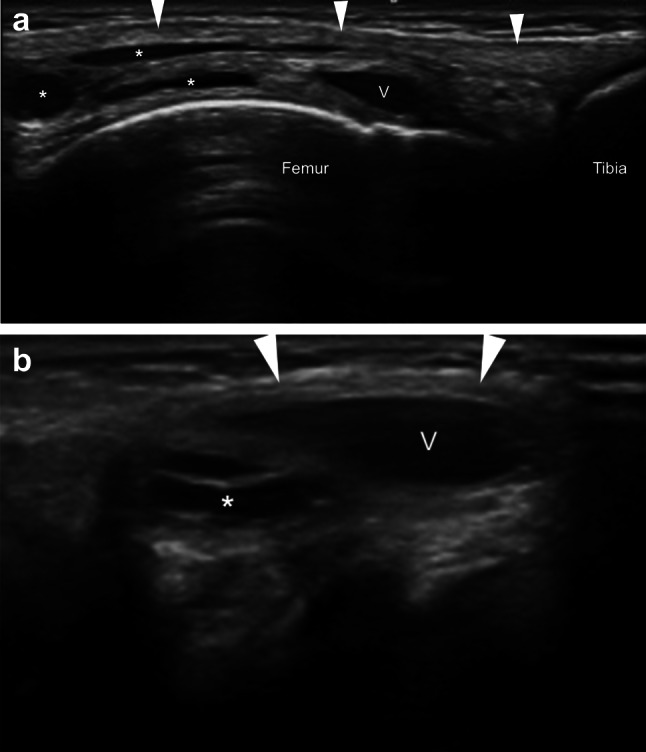
On longitudinal (a) and axial (b) sonograms, knee joint effusion (V) and multiple bursae (asterisks) are noted deep to the iliotibial band (arrowheads) and superficial to the lateral femoral epicondyle
Therapy
Iliotibial band syndrome is mainly managed non-operatively, and Fredericson et al. have proposed different treatment strategies according to three disease phases, such as the acute, subacute, and recovery strengthening phases [44]. The path to recovery involves the correction of facilitating factors, such as the weakness of the gluteus medius, the excessive adduction of the hip and internal rotation of the knee, the varus alignment of the knee, and lower limb length discrepancy [45].
In the acute phase, treatment is aimed at reducing local inflammation. Rest from physical activities such as running and cycling is a mainstay of treatment. In severe cases, patients should also avoid any activity involving repetitive flexion or extension of the knee and swim using only their arms and a pool buoy [45]. Concurrent therapies such as ice, phonophoresis, and iontophoresis play additional roles [46]. Both oral nonsteroidal anti-inflammatory medications and local corticosteroid injections can be used [46]. Local corticosteroid injections are considered in severe cases where physical therapies and oral medications fail to relieve symptoms [47–52]. They have been shown to effectively decrease pain in patients with recent onset of iliotibial band syndrome [53]. The response to corticosteroid injections helps diagnose iliotibial band syndrome as well [54]. Ultrasound is valuable in providing needle guidance throughout the procedure [55–62]. The procedure is performed with a sterile and local anesthetic technique. The transducer is positioned in the longitudinal or axial plane. Either an out-of-plane or an in-plane approach (Figs. 7, 8), such as distal to proximal [63] and medial to lateral [64], can be used. The tip of the needle is placed at the deep surface of the iliotibial band. Fluid aspiration can be performed if a focal fluid collection or bursitis is present. A combination of corticosteroid and anesthetic is injected [63, 64]. Up to 2 pain-free weeks are advised before returning to usual activity in a graded progression [45].
Fig. 7.

In a patient with iliotibial band syndrome (a), ultrasound-guided injection is performed using a distal-to-proximal in-plane approach. On a longitudinal sonogram (b), the tip of the needle is placed deep to the iliotibial band (ITB), superficial to the lateral femoral epicondyle, and the injectant flow (arrow) is noted
Fig. 8.
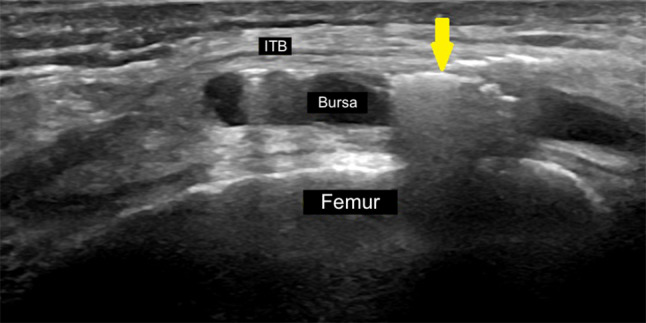
On a longitudinal sonogram, a bursitis is seen deep to the iliotibial band (ITB) and superficial to the lateral femoral epicondyle. An ultrasound-guided injection is performed using an out-of-plane approach, and the injectant flow (arrow) is noted
Once acute inflammation is under control, stretching exercises can be started. Thus, in the subacute phase, treatment focuses on achieving flexibility in the iliotibial band as a foundation to strength training. Iliotibial band stretching and soft-tissue mobilization aimed at reducing myofascial adhesions are performed [65].
Eliminating myofascial adhesions precedes strengthening and muscle reeducation. Hence, the recovery strengthening phase focuses on a series of exercises to improve gluteus medius strength. Exercises should be pain-free and include side-lying hip abduction, single-leg activities, pelvic drops, and multiplanar lunges [65].
Recalcitrant cases of iliotibial band syndrome require surgery. Surgical options include the release of the iliotibial band, iliotibial band bursectomy, and the resection of the lateral synovial recess [66–68].
Conclusions
Iliotibial band syndrome is a common source of pain in active individuals. Ultrasound is an effective imaging modality for the assessment of iliotibial band syndrome and proves a valuable aid in recalcitrant or refractory cases. A clear understanding of the anatomy, etiology, and clinical presentation is needed to achieve the correct diagnosis on ultrasound. Treatment varies according to the phase of the disease and, in the acute phase, may include ultrasound-guided local steroid injections.
Funding
None.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no competing interest.
Ethical approval
All performed procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cruells Vieira EL, Vieira EÁ, Teixeira da Silva R, et al. An anatomic study of the iliotibial tract. Arthroscopy. 2007;23:269–274. doi: 10.1016/j.arthro.2006.11.019. [DOI] [PubMed] [Google Scholar]
- 2.Hirschmann MT, Müller W. Complex function of the knee joint: the current understanding of the knee. Knee Surg Sports Traumatol Arthrosc. 2015;23:2780–2788. doi: 10.1007/s00167-015-3619-3. [DOI] [PubMed] [Google Scholar]
- 3.Evans P. The postural function of the iliotibial tract. Ann R Coll Surg Engl. 1979;61:271–280. [PMC free article] [PubMed] [Google Scholar]
- 4.Strauss EJ, Kim S, Calcei JG, Park D. Iliotibial band syndrome: evaluation and management. J Am Acad Orthop Surg. 2011;19:728–736. doi: 10.5435/00124635-201112000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Devan MR, Pescatello LS, Faghri P, Anderson J. A prospective study of overuse knee injuries among female athletes with muscle imbalances and structural abnormalities. J Athl Train. 2004;39:263–267. [PMC free article] [PubMed] [Google Scholar]
- 6.Taunton JE, Ryan MB, Clement DB, et al. A retrospective case–control analysis of 2002 running injuries. Br J Sports Med. 2002;36:95–101. doi: 10.1136/bjsm.36.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holmes JC, Pruitt AL, Whalen NJ. Iliotibial band syndrome in cyclists. Am J Sports Med. 1993;21:419–424. doi: 10.1177/036354659302100316. [DOI] [PubMed] [Google Scholar]
- 8.Flato R, Passanante GJ, Skalski MR, et al. The iliotibial tract: imaging, anatomy, injuries, and other pathology. Skelet Radiol. 2017;46:605–622. doi: 10.1007/s00256-017-2604-y. [DOI] [PubMed] [Google Scholar]
- 9.O’Keeffe SA, Hogan BA, Eustace SJ, Kavanagh EC. Overuse injuries of the knee. Magn Reson Imaging Clin N Am. 2009;17:725–739. doi: 10.1016/j.mric.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 10.Gitto S, Draghi F. Normal sonographic anatomy of the wrist with emphasis on assessment of tendons, nerves, and ligaments. J Ultrasound Med. 2016;35:1081–1094. doi: 10.7863/ultra.15.06105. [DOI] [PubMed] [Google Scholar]
- 11.Gitto S, Draghi AG, Bortolotto C, Draghi F. Sonography of the achilles tendon after complete rupture repair. J Ultrasound Med. 2016;35:2529–2536. doi: 10.7863/ultra.16.01092. [DOI] [PubMed] [Google Scholar]
- 12.Gitto S, Messina C, Mauri G, et al. Dynamic high-resolution ultrasound of intrinsic and extrinsic ligaments of the wrist: how to make it simple. Eur J Radiol. 2017;87:20–35. doi: 10.1016/j.ejrad.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 13.Draghi F, Bortolotto C, Draghi AG, Gitto S. Intrasheath instability of the peroneal tendons: dynamic ultrasound imaging. J Ultrasound Med. 2018;37:2753–2758. doi: 10.1002/jum.14633. [DOI] [PubMed] [Google Scholar]
- 14.Zappia M, Aliprandi A, Pozza S, et al. How is shoulder ultrasound done in Italy? A survey of clinical practice. Skelet Radiol. 2016;45:1629–1634. doi: 10.1007/s00256-016-2477-5. [DOI] [PubMed] [Google Scholar]
- 15.Sconfienza LM, Albano D, Allen G, et al. Clinical indications for musculoskeletal ultrasound updated in 2017 by European Society of Musculoskeletal Radiology (ESSR) consensus. Eur Radiol. 2018;28:5338–5351. doi: 10.1007/s00330-018-5474-3. [DOI] [PubMed] [Google Scholar]
- 16.Klauser AS, Tagliafico A, Allen GM, et al. Clinical indications for musculoskeletal ultrasound: a Delphi-based consensus paper of the European society of musculoskeletal radiology. Eur Radiol. 2012;22:1140–1148. doi: 10.1007/s00330-011-2356-3. [DOI] [PubMed] [Google Scholar]
- 17.Pozza S, De Marchi A, Albertin C, et al. Technical and clinical feasibility of contrastenhanced ultrasound evaluation of long bone non-infected nonunion healing. Radiol Med. 2018;123:703–709. doi: 10.1007/s11547-018-0902-7. [DOI] [PubMed] [Google Scholar]
- 18.Tagliafico A, Bignotti B, Rossi F, et al. Ultrasound of the hip joint, soft tissues, and nerves. Semin Musculoskelet Radiol. 2017;21:582–588. doi: 10.1055/s-0037-1606132. [DOI] [PubMed] [Google Scholar]
- 19.Möller I, Janta I, Backhaus M, et al. The 2017 EULAR standardised procedures for ultrasound imaging in rheumatology. Ann Rheum Dis. 2017;76:1974–1979. doi: 10.1136/annrheumdis-2017-211585. [DOI] [PubMed] [Google Scholar]
- 20.Renne JW. The iliotibial band friction syndrome. J Bone Jt Surg Am. 1975;57:1110–1111. doi: 10.2106/00004623-197557080-00014. [DOI] [PubMed] [Google Scholar]
- 21.Fairclough J, Hayashi K, Toumi H, et al. The functional anatomy of the iliotibial band during flexion and extension of the knee: implications for understanding iliotibial band syndrome. J Anat. 2006;208:309–316. doi: 10.1111/j.1469-7580.2006.00531.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Muhle C, Ahn JM, Yeh L, et al. Iliotibial band friction syndrome: MR imaging findings in 16 patients and MR arthrographic study of six cadaveric knees. Radiology. 1999;212:103–110. doi: 10.1148/radiology.212.1.r99jl29103. [DOI] [PubMed] [Google Scholar]
- 23.Jelsing EJ, Finnoff JT, Cheville AL, et al. Sonographic evaluation of the iliotibial band at the lateral femoral epicondyle: does the iliotibial band move? J Ultrasound Med. 2013;32:1199–1206. doi: 10.7863/ultra.32.7.1199. [DOI] [PubMed] [Google Scholar]
- 24.Nemeth WC, Sanders BL. The lateral synovial recess of the knee: anatomy and role in chronic iliotibial band friction syndrome. Arthroscopy. 1996;12:574–580. doi: 10.1016/S0749-8063(96)90197-8. [DOI] [PubMed] [Google Scholar]
- 25.Lavine R. Iliotibial band friction syndrome. Curr Rev Musculoskelet Med. 2010;3:18–22. doi: 10.1007/s12178-010-9061-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Messier SP, Edwards DG, Martin DF, et al. Etiology of iliotibial band friction syndrome in distance runners. Med Sci Sport Exerc. 1995;27:951–960. doi: 10.1249/00005768-199507000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Franco V, Cerullo G, Gianni E, Puddu G. Iliotibial band friction syndrome. Oper Tech Sports Med. 1997;5:153–156. doi: 10.1016/S1060-1872(97)80037-8. [DOI] [Google Scholar]
- 28.Noehren B, Davis I, Hamill J. ASB clinical biomechanics award winner 2006 Prospective study of the biomechanical factors associated with iliotibial band syndrome. Clin Biomech (Bristol, Avon) 2007;22:951–956. doi: 10.1016/j.clinbiomech.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 29.Kim DY, Miyakawa S, Fukuda T, Takemura M. Sex differences in iliotibial band strain under different knee alignments. PM R. 2019 doi: 10.1002/pmrj.12255. [DOI] [PubMed] [Google Scholar]
- 30.Razek AAKA, Fouda NS, Elmetwaley N, Elbogdady E. Sonography of the knee joint. J Ultrasound. 2009;12:53–60. doi: 10.1016/j.jus.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Robotti G, Draghi F, Bortolotto C, Canepa MG. Ultrasound of sports injuries of the musculoskeletal system: gender differences. J Ultrasound. 2020 doi: 10.1007/s40477-020-00438-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.De Maeseneer M, Marcelis S, Boulet C, et al. Ultrasound of the knee with emphasis on the detailed anatomy of anterior, medial, and lateral structures. Skelet Radiol. 2014;43:1025–1039. doi: 10.1007/s00256-014-1841-6. [DOI] [PubMed] [Google Scholar]
- 33.Alves TI, Girish G, Kalume Brigido M, Jacobson JA. US of the knee: scanning techniques, pitfalls, and pathologic conditions. Radiographics. 2016;36:1759–1775. doi: 10.1148/rg.2016160019. [DOI] [PubMed] [Google Scholar]
- 34.Marchand AJ, Proisy M, Ropars M, et al. Snapping knee: imaging findings with an emphasis on dynamic sonography. AJR Am J Roentgenol. 2012;199:142–150. doi: 10.2214/AJR.11.7817. [DOI] [PubMed] [Google Scholar]
- 35.Goh LA, Chhem RK, Wang SC, Chee T. Iliotibial band thickness: sonographic measurements in asymptomatic volunteers. J Clin Ultrasound. 2003;31:239–244. doi: 10.1002/jcu.10168. [DOI] [PubMed] [Google Scholar]
- 36.Gyaran IA, Spiezia F, Hudson Z, Maffulli N. Sonographic measurement of iliotibial band thickness: an observational study in healthy adult volunteers. Knee Surg Sports Traumatol Arthrosc. 2011;19:458–461. doi: 10.1007/s00167-010-1269-z. [DOI] [PubMed] [Google Scholar]
- 37.Díaz J (2017) ECOgrafía Musculoesqueletica. Marbán
- 38.Draghi F, Danesino GM, Coscia D, et al. Overload syndromes of the knee in adolescents: sonographic findings. J Ultrasound. 2008;11:151–157. doi: 10.1016/j.jus.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Draghi F, Corti R, Urciuoli L, et al. Knee bursitis: a sonographic evaluation. J Ultrasound. 2015;18:251–257. doi: 10.1007/s40477-015-0168-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ekman EF, Pope T, Martin DF, Curl WW. Magnetic resonance imaging of iliotibial band syndrome. Am J Sports Med. 1994;22:851–854. doi: 10.1177/036354659402200619. [DOI] [PubMed] [Google Scholar]
- 41.Nishimura G, Yamato M, Tamai K, et al. MR findings in iliotibial band syndrome. Skelet Radiol. 1997;26:533–537. doi: 10.1007/s002560050281. [DOI] [PubMed] [Google Scholar]
- 42.Jelsing EJ, Finnoff J, Levy B, Smith J. The prevalence of fluid associated with the iliotibial band in asymptomatic recreational runners: an ultrasonographic study. PM R. 2013;5:563–567. doi: 10.1016/j.pmrj.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 43.Draghi F, Urciuoli L, Alessandrino F, et al. Joint effusion of the knee: potentialities and limitations of ultrasonography. J Ultrasound. 2015;18:361–371. doi: 10.1007/s40477-015-0180-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fredericson M, Weir A. Practical management of iliotibial band friction syndrome in runners. Clin J Sport Med. 2006;16:261–268. doi: 10.1097/00042752-200605000-00013. [DOI] [PubMed] [Google Scholar]
- 45.Baker RL, Souza RB, Fredericson M. Iliotibial band syndrome: soft tissue and biomechanical factors in evaluation and treatment. PMR. 2011;3:550–561. doi: 10.1016/j.pmrj.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 46.Ellis R, Hing W, Reid D. Iliotibial band friction syndrome—a systematic review. Man Ther. 2007;12:200–208. doi: 10.1016/j.math.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 47.Albano D, Messina C, Usuelli FG, et al. Magnetic resonance and ultrasound in achilles tendinopathy: predictive role and response assessment to platelet-rich plasma and adiposederived stromal vascular fraction injection. Eur J Radiol. 2017;95:130–135. doi: 10.1016/j.ejrad.2017.08.006. [DOI] [PubMed] [Google Scholar]
- 48.Sartoris R, Orlandi D, Corazza A, et al. In vivo feasibility of real-time MR–US fusion imaging lumbar facet joint injections. J Ultrasound. 2017;20:23–31. doi: 10.1007/s40477-016-0233-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ferrero G, Fabbro E, Orlandi D, et al. Ultrasound-guided injection of platelet-rich plasma in chronic achilles and patellar tendinopathy. J Ultrasound. 2012;15:260–266. doi: 10.1016/j.jus.2012.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sconfienza LM, Chianca V, Messina C, et al. Upper limb interventions. Radiol Clin N Am. 2019;57:1073–1082. doi: 10.1016/j.rcl.2019.05.002. [DOI] [PubMed] [Google Scholar]
- 51.Orlandi D, Corazza A, Arcidiacono A, et al. Ultrasound-guided procedures to treat sport-related muscle injuries. Br J Radiol. 2016;89:20150484. doi: 10.1259/bjr.20150484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lueders DR, Smith J, Sellon JL. Ultrasound-guided knee procedures. Phys Med Rehabil Clin N Am. 2016;27:631–648. doi: 10.1016/j.pmr.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 53.Gunter P. Local corticosteroid injection in iliotibial band friction syndrome in runners: a randomised controlled trial. Br J Sports Med. 2004;38:269–272. doi: 10.1136/bjsm.2003.000283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hong JH, Kim JS. Diagnosis of iliotibial band friction syndrome and ultrasound guided steroid injection. Korean J Pain. 2013;26:387. doi: 10.3344/kjp.2013.26.4.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Messina C, Orlandi D, Sconfienza LM. Do we still need fluoroscopy to perform injections in the musculoskeletal system? Skelet Radiol. 2016;45:1717–1718. doi: 10.1007/s00256-016-2488-2. [DOI] [PubMed] [Google Scholar]
- 56.Silvestri E, Barile A, Albano D, et al. Interventional therapeutic procedures in the musculoskeletal system: an Italian Survey by the Italian College of Musculoskeletal Radiology. Radiol Med. 2018;123:314–321. doi: 10.1007/s11547-017-0842-7. [DOI] [PubMed] [Google Scholar]
- 57.Chianca V, Orlandi D, Messina C, et al. Interventional therapeutic procedures to treat degenerative and inflammatory musculoskeletal conditions: state of the art. Radiol Med. 2019;124:1112–1120. doi: 10.1007/s11547-019-01018-8. [DOI] [PubMed] [Google Scholar]
- 58.Allen G, Obradov M, Chianca V, et al. Ultrasound-guided musculoskeletal interventions for the most common hip and pelvis conditions: a step-by-step approach. Semin Musculoskelet Radiol. 2019;23:e58–e67. doi: 10.1055/s-0039-1683965. [DOI] [PubMed] [Google Scholar]
- 59.Albano D, Chianca V, Tormenta S, et al. Old and new evidence concerning the crucial role of ultrasound in guiding intra-articular injections. Skelet Radiol. 2017;46:963–964. doi: 10.1007/s00256-017-2644-3. [DOI] [PubMed] [Google Scholar]
- 60.Sconfienza LM, Adriaensen M, Albano D, et al. Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)—part I, shoulder. Eur Radiol. 2020;30:903–913. doi: 10.1007/s00330-019-06419-x. [DOI] [PubMed] [Google Scholar]
- 61.Sconfienza LM, Adriaensen M, Albano D, et al. Clinical indications for image guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)—part III, nerves of the upper limb. Eur Radiol. 2020;30:1498–1506. doi: 10.1007/s00330-019-06479-z. [DOI] [PubMed] [Google Scholar]
- 62.Sconfienza LM, Adriaensen M, Albano D, et al. Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)—part II, elbow and wrist. Eur Radiol. 2020;30:2220–2230. doi: 10.1007/s00330-019-06545-6. [DOI] [PubMed] [Google Scholar]
- 63.Díaz J (2020) Infiltraciones ecoguiadas. Marbán
- 64.Lalam RK, Winn N, Cassar-Pullicino VN. Interventional articular and para-articular knee procedures. Br J Radiol. 2016;89:1–15. doi: 10.1259/bjr.20150413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fredericson M, Wolf C. Iliotibial band syndrome in runners: innovations in treatment. Sports Med. 2005;35:451–459. doi: 10.2165/00007256-200535050-00006. [DOI] [PubMed] [Google Scholar]
- 66.Drogset JO, Rossvoll I, Grøntvedt T. Surgical treatment of iliotibial band friction syndrome A retrospective study of 45 patients. Scand J Med Sci Sports. 2007;9:296–298. doi: 10.1111/j.1600-0838.1999.tb00249.x. [DOI] [PubMed] [Google Scholar]
- 67.Hariri S, Savidge ET, Reinold MM, et al. Treatment of recalcitrant iliotibial band friction syndrome with open iliotibial band bursectomy. Am J Sports Med. 2009;37:1417–1424. doi: 10.1177/0363546509332039. [DOI] [PubMed] [Google Scholar]
- 68.Michels F, Jambou S, Allard M, et al. An arthroscopic technique to treat the iliotibial band syndrome. Knee Surg Sports Traumatol Arthrosc. 2009;17:233–236. doi: 10.1007/s00167-008-0660-5. [DOI] [PubMed] [Google Scholar]


