Abstract
Consumption of sugar and alternative low- or no-energy sweeteners has increased in recent decades. However, it is still uncertain how consumption of sugar and alternative sweeteners during pregnancy affects pregnancy outcomes and long-term offspring health. This review aims to collate the available evidence surrounding the consequences of sugar and alternative sweetener consumption during pregnancy, a so-called secondhand sugar effect. We found evidence that sugar consumption during pregnancy may contribute to increased gestational weight gain and the development of pregnancy complications, including gestational diabetes, preeclampsia and preterm birth. Further, we found a growing body of the animal and human evidence that maternal sugar intake during pregnancy may impact neonatal and childhood metabolism, taste perception and obesity risk. Emerging evidence also suggests that both maternal and paternal preconception sugar intakes are linked to offspring metabolic outcomes, perhaps via epigenetic alterations to the germline. While there have been fewer studies of the impacts of alternative sweetener consumption before and during pregnancy, there is some evidence to suggest effects on infant outcomes including preterm birth risk, increased infant body composition and offspring preference for sweet foods, although mechanisms are unclear. We conclude that preconception and gestational sugar and alternative sweetener consumption may negatively impact pregnancy outcomes and offspring health and that there is a need for further observational, mechanistic and intervention research in this area.
Keywords: Sugar, Pregnancy, Infant health, Artificial sweeteners, Alternative sweeteners, Preconception, Obesity
Our food supply has become largely processed and higher in sugars than it was in previous generations. A significant amount of research has examined the association between excessive sugar consumption and the risk of obesity and an array of other health issues. This has included consideration of both regular dietary sugars (sucrose, fructose, etc.) and alternative sweeteners, encompassing artificial sweeteners (aspartame, sucralose, etc.) and natural low or zero energy sweeteners (stevia, sugar alcohols, etc.), that are abundant in the food supply. However, the concept of sugars and alternative sweeteners as environmental exposures that can have secondhand effects on the developing infant has not been widely explored.
Secondhand sugars include regular dietary sugars and alternative sweeteners in the food supply that individuals do not actively choose to consume but are inadvertently exposed to. This concept is similar to that of secondhand tobacco smoke, where non-smokers can be exposed to and harmed by the smoke produced by those around them. Exposure to secondhand sugars can occur during various life stages. Even before birth, fetuses can be exposed to sugars and sweeteners that their mothers consume via the placenta. There is also evidence that maternal and paternal diet prior to conception can epigenetically affect the germline, and influence offspring growth and development. After birth, babies are exposed to sugars through breast milk and/or in infant formula and other products. As growing children and adolescents are usually not responsible for their own food choices, instead of relying on adults to prepare their meals, they are often also exposed to secondhand sugars.
Arguably the most vulnerable population to consider when it comes to secondhand sugar exposure is fetuses. Fetuses are completely reliant on nutrients supplied by their mothers for healthy growth and development. Exposure to harmful substances during these important phases can derail healthy development and potentially lead to irreversible future health problems. The purpose of this review is to summarise the existing literature related to how prenatal exposure to secondhand sugars and alternative sweeteners impact child development and health. We will also discuss how high sugar consumption in pregnancy impacts maternal health, as these effects, such as excessive weight gain, can also cause pregnancy complications that impact the fetus. Finally, we will highlight specific gaps in the research in this arena that we believe should be priorities for future work.
Sugar consumption during pregnancy and maternal weight gain
While an adequate amount of maternal weight gain in pregnancy is important for ensuring the healthy growth and development of the fetus, it is estimated that nearly 50 % of women gain more weight than is recommended during pregnancy(1). As we will discuss later, excessive gestational weight gain can contribute to various health issues for both mother and fetus. There is no clear consensus in the literature about which dietary factors contribute the most to excessive weight gain during pregnancy. Review papers that cover this topic(2–4) conclude that excess energy intake is a risk factor, but that the evidence for other macronutrients and food groups has been mixed.
Although few studies have specifically evaluated the effects of excessive sugar consumption on gestational weight gain, there is emerging evidence suggesting a positive association. To our knowledge, the largest study to evaluate this relationship was a prospective cohort study of 46 262 women in Denmark(5). The authors found that consumption of added sugars during pregnancy was strongly and positively associated with excessive gestational weight gain. In contrast, a higher protein to carbohydrate ratio was inversely associated with weight gain(5). Furthermore, through statistical modelling, they found that replacing carbohydrates with protein reduced weight gain, and this was driven specifically by a reduction in added sugars. Translating their results, the authors estimated that women in the highest ν. lowest quintiles of added sugar intake (89 (SD 26) ν. 19 (SD 5) g/d) gain an extra 1·4 kg weight during pregnancy on average. In secondary analyses, they found that the intake of sweets (primarily chocolate and mixed candy) was directly associated with gestational weight gain, but data for other foods or beverages was not presented.
There have also been observational studies conducted in other countries including Germany, South Africa, the Netherlands, the USA and Iceland. These studies found similar associations between sugar consumption in pregnancy and excess maternal weight gain, either through examination of single nutrients(6), food groups(7), or dietary patterns that include a high intake of added sugars(8–10). Observational studies evaluating the effects of alternative sweeteners on weight gain in pregnancy have been more limited. One study showed that consuming diet beverages in pregnancy increases the risk for excess pregnancy weight gain(11), which is consistent with findings from the general population(12).
There have also been a few intervention studies that reported on changes in sugar intake and their relationship with gestational weight gain(11,13,14), although not all were designed specifically to reduce sugar intake. For example, in a study of 342 obese women in Denmark, participants were randomised to either a control group, a physical activity intervention group, or a physical activity plus dietary intervention group(11). The physical activity plus dietary intervention group received instruction from trained dietitians on how to adhere to a hypoenergetic diet that was low in saturated fat and Mediterranean in style and were advised to aim for 11 000 steps daily (measured by a pedometer). No details were published regarding if women were given specific guidance on dietary sugars. Compared with the controls, the diet plus physical activity group had significant increases in the intake of protein and PUFA, as well as decreases in intake of added sugars and saturated fat. The diet plus physical activity intervention group also showed a lower relative risk of excessive weight gain as compared with the controls (0·73 (95 % CI 0·57, 0·94)), while the physical activity intervention group alone showed no difference in gestational weight gain compared with controls. The authors also conducted a pooled analysis evaluating potential associations between baseline dietary variables and change in gestational weight gain, regardless of randomisation group. They found that the intake of added sugars in foods was the only dietary variable associated with gestational weight gain. In an analysis of specific food groups, baseline intake of sweets, snacks and cakes was associated with an increased risk of excessive weight gain (>9 kg). Women consuming two or more servings of sweets daily (such as chocolates, caramels, licorice, gummy and jelly sweets) gained an additional 5·5 kg weight compared with women who consumed them less than once weekly. The results for soft drinks were more mixed: intake of sugar-sweetened sodas was inversely associated with weight gain at baseline but was not associated with weight gain at the endpoint measurement (36–37 weeks gestation), whereas intake of diet sodas was positively associated with weight gain only for consumption levels at the endpoint measurement. The authors concluded that reducing intakes of these (sugary) foods may be more relevant for limiting gestational weight gain than encouraging strict compliance to more specific diets.
Maternal sugar consumption and common pregnancy complications
There is also evidence to suggest that, independent of gestational weight gain and/or obesity, excessive sugar consumption during pregnancy is associated with pregnancy complications. Of the various types of sugar, fructose is thought to be particularly damaging(15). One study that investigated the effects of maternal carbohydrate and sugar consumption and their relation to gallbladder disease in 3070 pregnant women reported that fructose was associated with adverse outcomes, whereas other types of sugars were not(16). These results held strong even after controlling for overall carbohydrate intake and weight-related variables. Animal studies have also shown that increased fructose intake during pregnancy increases the risk of maternal fatty liver disease(17–19), insulin resistance/glucose intolerance(17,18,20), as well as hypertension(18) and/or preeclampsia(20). While the majority of studies conducted in human subjects have not evaluated the specific effects of fructose, the literature suggests that an overall increased consumption of sugars is associated with increased risk for common pregnancy complications, including gestational diabetes, preeclampsia and premature delivery, all of which we will discuss later.
Gestational diabetes
A high intake of added sugars during pregnancy is one of the dietary variables that has been shown to be related to the development of gestational diabetes mellitus (GDM). A study that used National Health and Nutrition Examination Survey data to look at dietary patterns of pregnant women and risk for gestational diabetes found that a diet characterised by high added sugar and organ meats; low fruits, vegetables and seafood was the pattern with the highest risk for GDM(21). The authors concluded that this risk was largely explained by the high consumption of added sugars and low consumption of fruit and vegetables. Another article using data from the Nurses’ Health Study II reported that intake of sugar-sweetened beverages before pregnancy was associated with the development of GDM(22). More specifically, consuming >5 sugar-sweetened cola drinks per week increased the risk of gestational diabetes by 22 %. Note that this study did not include an examination of juices in the analysis, and the findings were very specific to sugar-sweetened cola drinks in particular. Another study also examined the relationship between pre-pregnancy sugar-sweetened soft drink consumption and future risk for GDM and found a positive association which persisted even after controlling for potential confounders including family history of diabetes, BMI, total energy intake and fibre intake(23).
Preeclampsia
While research is limited, there is some evidence to suggest that drinking sugar-sweetened beverages in pregnancy can increase a woman’s risk of preeclampsia. A large study conducted in Norway that examined the diets of over 32 000 pregnant women showed that increased consumption of sugar-sweetened carbonated and noncarbonated drinks was associated with a higher risk for preeclampsia, after adjustment for total energy intake and other confounding variables (OR for the combined beverages 1·27 (95 % CI 1·05, 1·54) for high intake (>125 ml/d) compared with no intake)(24). In contrast, eating fresh or dried fruit was associated with a lower risk, perhaps due to their fibre content. Interestingly, the authors found that while the positive association between sugar-sweetened beverage consumption and preeclampsia was significant in both normal and overweight women, the risk was higher in women with a BMI <25 as compared with 25 or above (crude OR 1·32 ν. 1·28). A smaller Norwegian study (n 3133) also showed a positive relationship between high sucrose consumption (>25 % of total energy) and preeclampsia(25). While potential relationships with other types of sugars were not presented, the authors did evaluate specific food items and found that consumption of sugar-sweetened soft drinks was related to increased risk.
Premature delivery
While many factors can contribute to risk for premature delivery, and often times the cause for its occurrence is unknown, maintaining a healthy diet in pregnancy can serve as an additional safeguard(26). There is specific evidence to suggest that increased intake of sweetened beverages is related to risk for premature delivery. For example, Englund-Ogge et al. examined the relationship between sweetened beverage consumption in pregnancy and preterm delivery in 60 000 women in Norway(27). They found that one daily serving of sugar-sweetened beverages increased the risk of preterm delivery by 25 %. In addition, daily one serving of diet beverages increased the risk by 11 %. In a study of the same size from Denmark, researchers found that just one daily serving of diet beverage consumption increased the risk of a preterm delivery by 38 %, and four daily servings increased the risk by 78 %(28). Interestingly, in this study, which used slightly different methods, there was no effect of regular sugar-sweetened beverages on preterm delivery. In contrast, a smaller study from the UK showed that consumption of sugar-sweetened cola beverages did increase the risk of preterm delivery, but did not show a relationship with artificial sweeteners(29).
Possible mechanisms that could explain the observed effects of sugar-sweetened beverages on the pregnancy complications presented here include pathways related to insulin sensitivity and inflammation. Normal pregnancy is characterised by reduced maternal insulin sensitivity in peripheral tissues, but this is more pronounced in overweight individuals or those with gestational diabetes(30). These effects can be exacerbated by a high sugar diet. Decreased insulin sensitivity can lead to glucose intolerance, which is a known risk factor for preeclampsia and preterm delivery and the defining feature of GDM(31–33). Additionally, increased sugar consumption is associated with increased circulating pro-inflammatory cytokine concentrations, particularly in individuals with impaired glucose tolerance(34). Increased circulating pro-inflammatory cytokine concentrations, in turn, are associated with GDM, preeclampsia and preterm delivery(35). Interestingly, in the study discussed in the previous paragraph, Englund-Ogge et al.(27) found that the consumption of sugar-sweetened beverages was more highly correlated with early preterm delivery, while consumption of artificially sweetened beverages was correlated with late preterm delivery. The authors hypothesised that this could be due to the fact that younger fetuses are more sensitive to inflammatory interleukins.
In terms of alternative sweeteners, the exact mechanism of how they may contribute to preterm delivery is not known. One possible explanation is the way these compounds are broken down by the body. Aspartame, for example, is metabolised into aspartic acid, phenylalanine and methanol. The methanol is then converted into formaldehyde and formic acid, which is toxic in high doses. In animal studies, exposure to even a low dose of methanol can result in pregnancy complications including preterm delivery(36). Another possible explanation relates to how these alternative sweeteners affect the gut microbiome. Animal studies have demonstrated that artificial sweeteners disrupt the normal/healthy composition of bacteria that reside in the gut(37). Alteration of gut bacteria can increase numbers of unhealthy bacteria that promote inflammation and increased gut permeability and reduce numbers of healthy bacteria that assist in fermentation and satiety hormone production(38,39). However, it must be noted that this evidence is reliant on animal studies and its applicability to human biology remains unknown.
Effects of sugar consumption before pregnancy on fetal development and offspring health
While the majority of this review focuses on the impact of maternal diet during pregnancy on maternal and offspring outcomes, there is mounting evidence for a role of diet prior to conception(40). Animal studies have demonstrated that overfeeding prior to pregnancy (and not during pregnancy) can have long-lasting programming effects on offspring(41). For example, sheep embryos from dams overfed in the periconceptional period and transferred to the wombs of non-obese dams show increased fat mass at 4 months(42). While it is more difficult to separate the effects of preconception and prenatal nutrition in human subjects, some researchers have developed methods of doing so. Dominguez-Salas et al. used seasonal differences in nutrition in Gambian women to pinpoint the influence of the preconception period. They reported that maternal nutrition around the time of conception influenced DNA methylation in lymphocytes and hair follicles from infants postnatally(43) Another study found that maternal lipid profile at conception successfully predicted preterm birth, regardless of whether the women were provided essential fatty acid supplementation during pregnancy(44). Indeed, it may be the case that by the time sugar-related pregnancy complications are realised, the optimal window for intervention has passed. Therefore, pre-pregnancy sugar intake may be just as or more influential than intake during pregnancy.
Importantly, the relevance of preconception nutrition does not appear to be limited to mothers. There are now a series of animal studies to show that poor diet quality in fathers can be transmitted to offspring through the germ-line. Carone et al., demonstrated that a high sucrose, low protein diet consumed by male mice affects the expression of key metabolic genes in offspring, including upregulation of cholesterol biosynthesis genes. The mechanisms underlying this appear to be epigenetic, as paternal diet was highly correlated with cytosine methylation of the enhancer of lipid transcription factor Ppara(45). However, direct examination of sperm methylation patterns did not show an effect of diet, suggesting alternative epigenetic information carriers such as RNA. Indeed, a subsequent study reported that direct injection of naive one-cell embryos with sperm or testis RNA from high sugar/high fat-fed donors induced obesity and metabolic dysfunction in the resulting progeny(46). To the best of our knowledge, there do not yet exist studies examining the impact of preconception maternal and paternal alternative sweetener intake on offspring health. However, these existing studies suggest that both maternal and paternal preconception diet are important contributors to the health of offspring, and if possible, nutritional interventions should not be limited to pregnancy alone.
Effects of sugar consumption in pregnancy on fetal development and offspring health
Transfer of regular sugars across the placenta and effects on fetal development
While studies conducted in human subjects are limited due to ethical issues, it is well established that both glucose and fructose cross the human placenta(47), and therefore reach and can affect the developing baby. Human studies also suggest that fructose concentrations are higher in the fetal bloodstream relative to that of the mother, suggesting active transport of fructose across the placenta(48) and animal studies have confirmed this(15). For example, one study in rats showed that gestational exposure to fructose led to pups who were hyperglycemic at birth(49).
The developing fetus lacks the ability to undergo gluconeogenesis, and thus relies on the transport of glucose from the maternal bloodstream(50). One key player in the placental transport of both glucose and fructose is facilitative GLUT-9, which consists of the isoforms GLUT-9a and 9b(51). GLUT-9 is unique in that it can also transport fructose and uric acid. The protein expression of GLUT-9 is directly associated with blood glucose concentrations; hyperglycemia increases expression and hypoglycemia decreases expression(51). Thus, insulin-resistant and diabetic individuals will tend to have increased expression of GLUT-9. This increased expression has also been observed in the placental tissue of pregnant diabetic women(50). This has been suggested as playing a key role in fetal pathologies frequently seen in diabetic pregnancies, likely due to increased placental and fetal exposure to glucose and fructose(50).
The exact effects of exposure to increased fructose levels on placental and embryonic tissue are not fully understood. Rodriquez et al. demonstrated that fetuses from fructose-fed pregnant rats had hypertriglyceridemia and higher hepatic TAG content(52). These fetuses also had higher expression of genes related to lipogenesis and a low expression of genes related to fatty acid catabolism. Additionally, it was noted that these fetuses had an impairment in the leptin signalling pathway. Vickers et al. similarly demonstrated markers of impaired metabolic function including hyperglycemia and hyperleptinemia in fetuses and neonates of fructose-fed mothers, particularly in female offspring(53). Together, these effects could predispose pups to obesity early in life. Further studies are necessary to determine if similar outcomes hold true in human subjects. Additionally, it has been demonstrated that elevated fructose levels are associated with increased levels of reactive oxygen species, In fact, it has been suggested that reactive oxygen species-related oxidative damage could be a ‘unifying mechanism’ to explain diabetic complications(54).
Maternal transfer of alternative sugars and their by-products to the fetus
It is known that saccharin crosses the placenta(55), as do the breakdown products of aspartame(56), and it is hypothesised that sucralose and acesulfame-K cross the placenta as well(57,58). While animal studies have not found these products to have toxic effects on the fetus(59), research has been limited and results from animal studies must be interpreted with caution due to differences in physiology as compared with human subjects. Therefore, the complete effects of these products in human subjects are not known. It has been previously concluded that moderate consumption of artificial sweeteners is safe during pregnancy(59). However, given the observational research we describe in this review that suggests negative effects of maternal consumption on outcomes such as premature birth(27,28) and future offspring adiposity(60,61), it is possible that there are mechanistic links and risks that are not yet fully understood. Studies on the effects of other alternative sweeteners such as stevia and sugar alcohols are also lacking.
Effects of maternal sugar and alternative sweetener intake on future childhood obesity
Regular sugars.
A variety of studies conducted in human subjects have shown that excess maternal sugar consumption during pregnancy can increase the chances that a child will become overweight or obese(62–65). For example, a study conducted in Singapore with 910 mother/child pairs found that higher sugar and carbohydrate intakes during late pregnancy were associated with the higher BMI in the children at ages 2–4 years, whereas fat and protein intake were not related to these markers(63). Another study, conducted in the Netherlands, evaluated 3312 mother–child pairs and found that daily one additional serving of a sugar-sweetened beverage during pregnancy resulted in a 0.05 standard deviation score higher fat mass index in the child at age 6 years. Furthermore, when types of drinks were evaluated separately, intakes of 100 % fruit juice, but not of soda or sweetened juice concentrate drinks, were associated with a higher child fat mass. These findings were independent of gestational weight gain, birth weight, and children’s insulin concentrations. Similarly, an American study conducted with 1078 mother–child pairs found that maternal sugar-sweetened beverage consumption was related to future childhood obesity. Specifically, each serving of sugar-sweetened beverage consumed daily during the second trimester was related to measures of child overweight at age 7 years, including BMI, fat mass index and waist circumference(65). Finally, a smaller study in the USA of 285 mothers/children found that in overweight or obese mothers, consumption of sweets was a predictor of birthweight, such that each 1 % increase in percentage of energy consumed from sweets early in pregnancy increased the odds of macrosomia by 10 % and weight for age >90th percentile by 20 %(62). Also, in the overweight or obese group, at 6 months, the strongest predictors of higher weight for age z-scores were a greater percentage of energy from sweets early in pregnancy. In normal-weight women, higher intake of sugary drinks was the strongest predictor of birth weight but was not related to infant weight at 6 months.
In addition to dietary sugar content, the overall glycemic load of the maternal diet during pregnancy has been linked to increased risk of offspring obesity. A study conducted in the UK with 906 mother–child pairs found that both maternal dietary glycemic index and glycemic load in early pregnancy (11 weeks) were positively associated with child fat mass at age 4 and 6 years, whereas maternal glycemic index during late pregnancy (34 weeks) was not(66). Another study that evaluated the effects of the maternal glycemic index on neonatal adiposity in 542 mother–child pairs in the UK found that maternal glycemic load in the second trimester was associated with neonatal central adiposity as measured by waist to length ratio(67). Additional studies are required to help clarify the role of the maternal glycemic index on parameters of offspring obesity and in particular which trimester of pregnancy is the most influential.
Alternative sweeteners.
The effects of maternal consumption of alternative sweeteners during pregnancy on infant and child outcomes have not been extensively studied. One detailed study in 3033 mother–infant dyads in Canada showed that 30 % of women consumed artificial sweeteners during pregnancy(61). Women who consumed artificial sweeteners daily had a 2-fold higher risk of an infant being overweight by age 1 year. Another study conducted in Denmark with 918 mother–child dyads found that approximately half of the mothers consumed artificially sweetened beverages and 9 % consumed them on a daily basis. Compared with those participants who never consumed artificial sweeteners, the daily consumers were more likely to have children who were large for gestational age at birth (relative risk 1·57; 95 % CI 1·05, 2·35) and who were overweight or obese by age 7 years (relative risk 1·93; 95 % CI 1·24, 3·01). Furthermore, they found that substituting artificially sweetened beverages with water reduced risk for overweight at age 7 years, but substituting regular sweetened beverages with artificially sweetened alternatives did not confer a reduced risk.
Effects of maternal sugar consumption on future child feeding behaviours and metabolism.
One of the ways that exposure to excess sugars during gestation can promote future obesity is through fetal programming(68). While the brain, vital organs and adipose tissue are developing in utero, they are particularly vulnerable to nutritional insults. As we will explain later, a maternal diet that is high in sugar may lead to structural and functional alterations that can predispose a child to poor feeding behaviours and a metabolism that favours fat storage.
During early gestation, the structures and pathways of the brain that are responsible for feeding behaviour are already developing. The hypothalamus, which begins to develop as early as 9 weeks gestation, plays a key role in energy and glucose homeostasis and disruption of its healthy development is thought to create a predisposition for metabolic diseases(69). Although research in human subjects has been limited, studies in animals suggest that a maternal diet that is high in sugar is associated with altered gene expression, hyperphagia and disrupted glucose homeostasis in the offspring(69). The central reward system is also important in determining feeding behaviour. Studies in human subjects, while limited, suggest that dopamine and opioids are expressed in the fetal striatum by 12 weeks gestation and their associated receptors can be detected by about 20 weeks gestation(70). A maternal diet that is high in sugars stimulates the synthesis and release of these compounds that are related to pleasure and reward and can predispose a child to prefer sweet tastes and even to become addicted to them(70).
While much of the evidence for the association between a high sugar diet and alterations in feeding behaviours and metabolism come from animal studies, there have been observational studies conducted in human subjects that support the same conclusions. For example, Brion et al. evaluated maternal dietary data both during pregnancy and at 47 weeks postpartum, paternal dietary data at 47 weeks and child dietary data at age 10 years(71). They found that maternal gestational intakes of protein, fat and carbohydrates were positively associated with the child’s intakes at age 10 years, whereas paternal diet was not strongly associated. Furthermore, for protein and fat intake, maternal prenatal diet was more strongly associated with the child’s future intakes than were the mother’s postnatal intakes. These results suggest a programming effect and that the in utero food environmental may have a larger influence on the child’s diet than the eventual family food environment. There has also been research to suggest that a child’s taste preferences are shaped in utero by the maternal diet(72). In a classic study, it was shown that when infants were tested before weaning, those infants who were exposed to carrot flavour via maternal consumption in pregnancy exhibited more liking for carrot flavour compared with those infants who were not exposed in utero(73). While to our knowledge, a similar study has not been conducted with a maternal exposure to sugar, we do know that a preference for sweet tastes is present at birth and probably before(74). For example, a study in preterm infants found they sucked stronger and more frequently on a nipple that had been soaked in sucrose compared with one that had not(75). One potential reason for this is that an innate desire for sweetness is advantageous in evolutionary terms.
Of the various types of sugars, fructose, in particular, should be considered as a prenatal exposure that has the potential for negative programming effects on offspring metabolism(76). There is only limited data available on the long-term effects of high fructose exposure during gestation. However, there are some studies, mostly in animals that suggest that high fructose consumption in pregnancy can lead to persistent neuroendocrine and metabolic alterations in the baby related to the development of feeding behaviour and propensity to develop obesity later in life(15,76). Several potential mechanisms could explain the adverse effects of high fructose exposure during these periods. For example, we know that even very low levels of fructose can directly promote the process of building new fat cells during critical periods of development(77). High fructose intake during development might also promote obesity by disrupting the normal signalling that occurs between the brain and adipose tissue(15,52,76,78). Results from a well-controlled human study evaluated changes in appetite-related hormone concentrations over 24 h in response to meals containing either glucose or fructose. Levels of insulin and leptin were significantly lower after the fructose meal than after the glucose meal, and fructose failed to suppress post-meal ghrelin levels as effectively as glucose, which suggests that consumption of fructose could disrupt energy balance signalling to the brain and result in excess energy consumption and obesity(78).
Alternative sugars are also important to consider in terms of their effects on fetal programming of feeding behaviours and future metabolic health(79). In animals, prenatal exposure to artificial sweeteners leads to higher selection and taste preference for sweet foods in adulthood(58,80). Beyond influencing behaviour, these exposures also can have metabolic consequences. Chronic exposure to aspartame in mice in utero and early life has also been shown to be associated with elevated fasting blood glucose as well as reduced insulin sensitivity in later life(81).
A summary diagram of the secondhand effects of sugars and alternative sweeteners is depicted in Fig. 1.
Fig. 1.
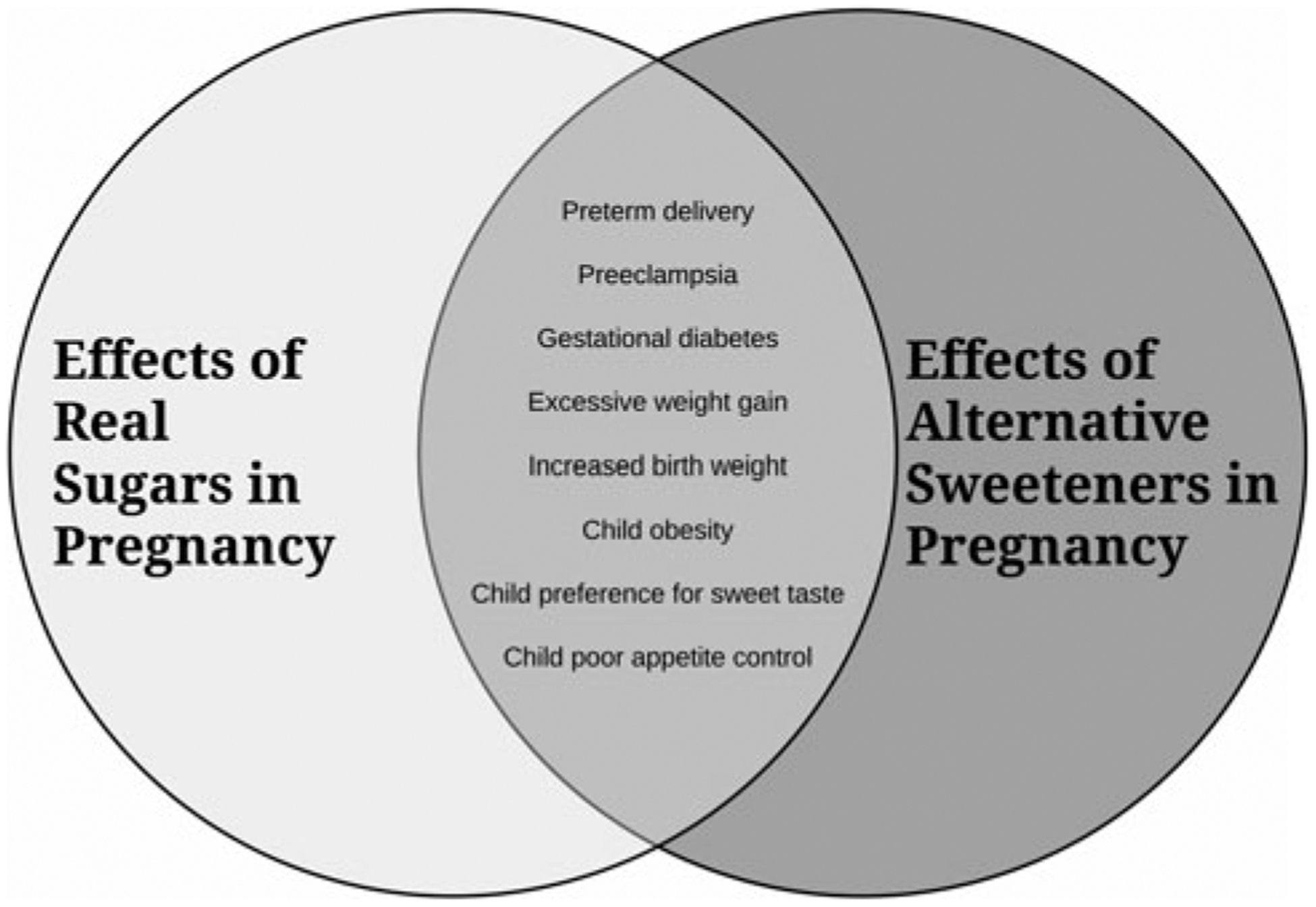
An overview of how consumption of excess sugars and alternative sweeteners in pregnancy impacts maternal and infant/child health.
Future research priorities/needs
From our review of the literature, we suggest that future research is required in three categories to further our understanding of how exposure to sugars in pregnancy can affect maternal and child health: (1) further observational studies with more rigorous dietary assessment during pregnancy combined with detailed assessment of infant/child changes in body composition during growth;(2) additional mechanistic studies to understand exactly how gestational sugars impact fetal growth and development including effects on infant brain development, food intake regulation, taste preference and microbiome; and,(3) novel intervention studies that focus specifically on examining the effects of reduction of dietary sugars during pregnancy on future offspring behaviour, metabolism and health. In each of these categories, there is a need in particular for an additional focus on fructose and artificial sweeteners, both of which are hypothesised to have detrimental effects, as well as other alternative sweeteners, such as sugar alcohols or stevia, which have not yet been rigorously studied.
The first category relates to the increased need for observational studies that would help to further our understanding of the associations between consumption of various sugars in pregnancy and specific maternal and child health outcomes. For example, of the three studies that we are aware of that examined the relationship between sugar intake during pregnancy and risk for preterm delivery, results were mixed. One showed an effect of both regular and artificially sweetened beverages, while one found an association with just sugar-sweetened beverages and the other with just artificially sweetened beverages. Additional studies are required to confirm these findings and also to explore the effects of other specific types of sugars, sweeteners and categories of foods and beverages that contain them. Many of the studies conducted to date have not evaluated the effects of specific types of sugars, such as fructose, and/or specific alternative sweeteners. In addition, only a few studies have evaluated the effects of maternal glycemic index/load. Additional studies that evaluate these specific exposures using more precise dietary methods, as well as specific child outcomes measures such as detailed body composition and fat distribution outcomes, fatty liver disease and insulin resistance, would help to deepen our understanding. Finally, studies that include longer follow-up periods would help us to further understand the distal effects of secondhand sugar exposure on offspring health.
The second category of future research priorities pertains to studies that increase our understanding of the mechanisms that drive the observed associations between maternal sugar consumption in pregnancy and adverse child outcomes. Some of the mechanistic gaps in the literature are difficult to address because of the ethical and logistical challenges of conducting maternal–infant research. However, additional, targeted animal studies would be useful. As an example, we still only have a limited understanding of how exactly exposure to various types of sugars and sweeteners may influence the development of the hypothalamus and the wiring of the central reward system. We also do not know much about the specific effects of in utero exposure to some of the popular artificial sweeteners, such as sucralose, or popular non-energetic natural alternatives, such as stevia, on future offspring health.
The third category for future research is a need for additional intervention studies conducted with women who are either trying to conceive and/or already pregnant that focus specifically on reducing sugar intake. Programmes have been designed and tested to improve maternal diet in pregnancy and test their effects on maternal and child outcomes, but few have focused specifically or exclusively on sugar consumption. For example, a study conducted in the UK involved an intervention designed to reduce glycemic load, sugar-sweetened beverage consumption and saturated fat intake in obese pregnant women (n 1555) in order to reduce the incidence of gestational diabetes and large-for-gestational-age infants(13). While there were no significant effects on the primary study outcomes, the authors did report significant reductions in maternal glycemic index values and gestational weight gain. Future studies could be more targeted and focus solely on the reduction of sugar consumption in pregnancy. Once we have a better understanding of what types of programmes are effective, they can be translated for use in larger settings and serve as preventive measures for secondhand sugar exposures.
Limitations
Limitations of the available evidence discussed in this review include the potential for reverse causality, the fact that the food vehicles mostly (but not exclusively) studied were beverages, and the challenges of isolating effects of specific types of sugars and alternative sweeteners (e.g. fructose independently of glucose etc.). Further, the evidence presented is mostly (and understandably, for ethical reasons) observational, making it difficult to determine causality. Where available, prospective cohort studies usually relied on FFQ over the more rigorous 24-h dietary recall or provided meals, and sugars were not always considered separately from other dietary factors such as a high-fat diet. We must also acknowledge that it is difficult to assess sugar intake, especially considering the different forms available, (e.g. added, free, total sugars), which can also vary based on geographical location (for example, the USA often utilises high fructose maize syrup in beverages, while the equivalent beverage in other countries may comprise sucrose). There are also several forms of alternative sweeteners on the market, including artificial and natural sweeteners, which are used at different dosages and intensities, and may have differential effects in a secondhand sugar context. Quantifying alternative sweetener intake is also very difficult because the exact amounts used in products are not usually reported. Finally, we would like to acknowledge that it will be a challenge for nutrition science to disentangle sugar as a food ingredient, considering its use for functional properties such as mouthfeel, bulk, taste and food preservation in addition to its use as a nutrient. However, given the available evidence for detrimental effects of excessive sugar intake, including that of a secondhand sugar effect presented in the present paper, we believe the ongoing pervasiveness of sugar and alternative sweeteners in the food supply requires careful consideration.
Conclusion
In summary, although research has been limited, especially in human subjects, the available evidence suggests that there can be detrimental secondhand effects of in utero exposure to sugars from the maternal diet on offspring health. These exposures may have adverse consequences for both the mother and fetus, shape feeding behaviours and taste preferences in the offspring, and increase future risk for obesity and related metabolic diseases. As depicted in Fig. 1, the available research suggests that alternative sugars may be equally or more harmful than regular sugars. While further research including well-controlled prospective cohort trials is required, we suggest that sugars be viewed as an environmental health hazard for developing babies and that public health initiatives should be developed to help raise awareness and assist pregnant women to monitor and reduce their consumption of both regular and alternative sugars.
Financial Support
Dr Goran’s research is supported by The Dr Robert C and Veronica Atkins Foundation, The Gerber Foundation and the National Institutes of Health (RO1 DK 110793; RO1 DK 109161; and RO1 MD 10358).
Abbreviation:
- GDM
gestational diabetes mellitus
Footnotes
Conflict of Interest
None.
References
- 1.Goldstein RF, Abell SK, Ranasinha S et al. (2017) Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis. JAMA 317, 2207–2225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tielemans MJ, Garcia AH, Santos P et al. (2016) Macronutrient composition and gestational weight gain: a systematic review. Am J Clin Nutr 103, 83–99. [DOI] [PubMed] [Google Scholar]
- 3.Samura T, Steer J, Michelis LD et al. (2016) Factors associated with excessive gestational weight gain: review of current literature. Glob Adv Health Med 5, 87–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Streuling I, Beyerlein A, Rosenfeld E et al. (2011) Weight gain and dietary intake during pregnancy in industrialized countries–a systematic review of observational studies. J Perinat Med 39, 123–129. [DOI] [PubMed] [Google Scholar]
- 5.Maslova E, Halldorsson TI, Astrup A et al. (2015) Dietary protein-to-carbohydrate ratio and added sugar as determinants of excessive gestational weight gain: a prospective cohort study. BMJ Open 5, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diemert A, Lezius S, Pagenkemper M et al. (2016) Maternal nutrition, inadequate gestational weight gain and birth weight: results from a prospective birth cohort. BMC Pregnancy Childbirth 16, 224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olafsdottir AS, Skuladottir GV, Thorsdottir I et al. (2006) Maternal diet in early and late pregnancy in relation to weight gain. Int J Obes (Lond) 30, 492–499. [DOI] [PubMed] [Google Scholar]
- 8.Wrottesley SV, Pisa PT & Norris SA (2017) The influence of maternal dietary patterns on body mass index and gestational weight gain in urban black South African Women. Nutrients 9, [Epublication ahead of print version]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tielemans MJ, Erler NS, Leermakers ET et al. (2015) A priori and a posteriori dietary patterns during pregnancy and gestational weight gain: the generation R study. Nutrients 7, 9383–9399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Starling AP, Sauder KA, Kaar JL et al. (2017) Maternal dietary patterns during pregnancy are associated with newborn body composition. J Nutr 147, 1334–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Renault KM, Carlsen EM, Norgaard K et al. (2015) Intake of sweets, snacks and soft drinks predicts weight gain in obese pregnant women: detailed analysis of the results of a randomised controlled trial. PLoS ONE 10, 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Swithers SE (2013) Artificial sweeteners produce the counterintuitive effect of inducing metabolic derangements. Trends Endocrinol Metab 24, 431–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poston L, Bell R, Croker H et al. (2015) Effect of a behavioural intervention in obese pregnant women (the Upbeat Study): a multicentre, randomised controlled trial. Lancet Diabetes Endocrinol 3, 767–777. [DOI] [PubMed] [Google Scholar]
- 14.Petrella E, Malavolti M, Bertarini V et al. (2014) Gestational weight gain in overweight and obese women enrolled in a healthy lifestyle and eating habits program. J Matern Fetal Neonatal Med 27, 1348–1352. [DOI] [PubMed] [Google Scholar]
- 15.Regnault TRH, Gentili S, Sarr O et al. (2013) Fructose, pregnancy and later life impacts. Clin Exp Pharmacol Physiol 40, 824–837. [DOI] [PubMed] [Google Scholar]
- 16.Wong AC & Ko CW (2013) Carbohydrate intake as a risk factor for biliary sludge and stones during pregnancy. J Clin Gastroenterol 47, 700–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zou M, Arentson EJ, Teegarden D et al. (2012) Fructose consumption during pregnancy and lactation induces fatty liver and glucose intolerance in rats. Nutr Res 32, 588–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shortliffe LM, Hammam O, Han X et al. (2015) Dietary fructose in pregnancy induces hyperglycemia, hypertension, and pathologic kidney and liver changes in a rodent model. Pregnancy Hypertens 5, 308–314. [DOI] [PubMed] [Google Scholar]
- 19.Clayton ZE, Vickers MH, Bernal A et al. (2015) Early life exposure to fructose alters maternal, fetal and neonatal hepatic gene expression and leads to sex-dependent changes in lipid metabolism in rat offspring. PLoS ONE 10, e0141962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alzamendi A, Del Zotto H, Castrogiovanni D et al. (2012) Oral metformin treatment prevents enhanced insulin demand and placental dysfunction in the pregnant rat fed a fructose-rich diet. ISRN Endocrinol 2012, 757913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shin D, Lee KW & Song WO (2015) Dietary patterns during pregnancy are associated with risk of gestational diabetes mellitus. Nutrients 7, 9369–9382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen L, Hu FB, Yeung E et al. (2009) Prospective study of pre-gravid sugar-sweetened beverage consumption and the risk of gestational diabetes mellitus. Diabetes Care 32, 2236–2241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Donazar-Ezcurra M, Lopez-Del Burgo C, Martinez-Gonzalez MA et al. (2017) Soft drink consumption and gestational diabetes risk in the sun project. Clin Nutr 37, 638–645. [DOI] [PubMed] [Google Scholar]
- 24.Borgen I, Aamodt G, Harsem N et al. (2012) Maternal sugar consumption and risk of preeclampsia in nulliparous Norwegian women. Eur J Clin Nutr 66, 920–925. [DOI] [PubMed] [Google Scholar]
- 25.Clausen T, Slott M, Solvoll K et al. (2001) High intake of energy, sucrose, and polyunsaturated fatty acids is associated with increased risk of preeclampsia. Am J Obstet Gynecol 185, 451–458. [DOI] [PubMed] [Google Scholar]
- 26.Abu-Saad K & Fraser D (2010) Maternal nutrition and birth outcomes. Epidemiol Rev 32, 5–25. [DOI] [PubMed] [Google Scholar]
- 27.Englund-Ögge L, Brantsæter AL, Haugen M et al. (2012) Association between intake of artificially sweetened and sugar-sweetened beverages and preterm delivery: a large prospective cohort study. Am J Clin Nutr 96, 552–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Halldorsson TI, Strøm M, Petersen SB et al. (2010) Intake of artificially sweetened soft drinks and risk of preterm delivery: a prospective cohort study in 59 334 Danish pregnant women. Am J Clin Nutr 92, 626–633. [DOI] [PubMed] [Google Scholar]
- 29.Petherick ES, Goran MI & Wright J (2014) Relationship between artificially sweetened and sugar-sweetened cola beverage consumption during pregnancy and preterm delivery in a multi-ethnic cohort: analysis of the born in Bradford cohort study. Eur J Clin Nutr 68, 404–407. [DOI] [PubMed] [Google Scholar]
- 30.Catalano PM, Huston L, Amini SB et al. (1999) Longitudinal changes in glucose metabolism during pregnancy in obese women with normal glucose tolerance and gestational diabetes mellitus. Am J Obstet Gynecol 180, 903–916. [DOI] [PubMed] [Google Scholar]
- 31.Lao TT & Ho LF (2003) Does maternal glucose intolerance affect the length of gestation in singleton pregnancies? J Soc Gynecol Investig 10, 366–371. [DOI] [PubMed] [Google Scholar]
- 32.Carr DB, Newton KM, Utzschneider KM et al. (2011) Gestational diabetes or lesser degrees of glucose intolerance and risk of preeclampsia. Hypertens Pregnancy 30, 153–163. [DOI] [PubMed] [Google Scholar]
- 33.(2014) Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy: a world health organization guideline. Diabetes Res Clin Pract 103, 341–363. [DOI] [PubMed] [Google Scholar]
- 34.Esposito K, Nappo F, Marfella R et al. (2002) Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: role of oxidative stress. Circulation 106, 2067–2072. [DOI] [PubMed] [Google Scholar]
- 35.Wenstrom KD, Andrews WW, Hauth JC et al. (1998) Elevated second-trimester amniotic fluid interleukin-6 levels predict preterm delivery. Am J Obstet Gynecol 178, 546–550. [DOI] [PubMed] [Google Scholar]
- 36.Burbacher TM, Grant KS, Shen DD et al. (2004) Chronic maternal methanol inhalation in nonhuman primates (Macaca Fascicularis): reproductive performance and birth outcome. Neurotoxicol Teratol 26, 639–650. [DOI] [PubMed] [Google Scholar]
- 37.Suez J, Korem T, Zilberman-Schapira G et al. (2015) Non-caloric artificial sweeteners and the microbiome: findings and challenges. Gut Microbes 6, 149–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Taylor BL, Woodfall GE, Sheedy KE et al. (2017) Effect of probiotics on metabolic outcomes in pregnant women with gestational diabetes: a systematic review and meta-analysis of randomized controlled trials. Nutrients 9, [Epublication ahead of the print version]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tilg H & Moschen AR (2015) Food, immunity, and the microbiome. Gastroenterology 148, 1107–1119. [DOI] [PubMed] [Google Scholar]
- 40.Nicholas LM, Rattanatray L, MacLaughlin SM et al. (2013) Differential effects of maternal obesity and weight loss in the periconceptional period on the epigenetic regulation of hepatic insulin-signaling pathways in the offspring. FASEB J 27, 3786–3796. [DOI] [PubMed] [Google Scholar]
- 41.Shankar K, Harrell A, Liu X et al. (2008) Maternal obesity at conception programs obesity in the offspring. Am J Physiol Regul Integr Comp Physiol 294, R528–R538. [DOI] [PubMed] [Google Scholar]
- 42.Rattanatray L, MacLaughlin SM, Kleemann DO et al. (2010) Impact of maternal periconceptional overnutrition on fat mass and expression of adipogenic and lipogenic genes in visceral and subcutaneous fat depots in the postnatal lamb. Endocrinology 151, 5195–5205. [DOI] [PubMed] [Google Scholar]
- 43.Dominguez-Salas P, Moore SE, Baker MS et al. (2014) Maternal nutrition at conception modulates DNA methylation of human metastable epialleles. Nat Commun 5, 3746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ogundipe E, Johnson MR, Wang Y et al. (2016) Peri-conception maternal lipid profiles predict pregnancy outcomes. Prostaglandins Leukot Essent Fatty Acids 114, 35–43. [DOI] [PubMed] [Google Scholar]
- 45.Carone BR, Fauquier L, Habib N et al. (2010) Paternally induced transgenerational environmental reprogramming of metabolic gene expression in mammals. Cell 143, 1084–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Grandjean V, Fourré S, De Abreu DA et al. (2015) RNA-mediated paternal heredity of diet-induced obesity and metabolic disorders. Sci Rep 5, 18193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Holmberg NG, Kaplan B, Karvonen MJ et al. (1956) Permeability of human placenta to glucose, fructose, and xylose. Acta Physiologica Scandinavica 36, 291–299. [DOI] [PubMed] [Google Scholar]
- 48.Hagerman DD & Villee CA (1952) The transport of fructose by human placenta. J Clin Invest 31, 911–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jen KL, Rochon C, Zhong SB et al. (1991) Fructose and sucrose feeding during pregnancy and lactation in rats changes maternal and pup fuel metabolism. J Nutr 121, 1999–2005. [DOI] [PubMed] [Google Scholar]
- 50.Bibee KP, Illsley NP & Moley KH (2011) Asymmetric syncytial expression of GLUT9 splice variants in human term placenta and alterations in diabetic pregnancies. Reprod Sci 18, 20–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Doblado M & Moley KH (2009) Facilitative glucose transporter 9, a unique hexose and urate transporter. Am J Physiol Endocrinol Metab 297, E831–E835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rodríguez L, Panadero MI, Roglans N et al. (2013) Fructose during pregnancy affects maternal and fetal leptin signaling. J Nutr Biochem 24, 1709–1716. [DOI] [PubMed] [Google Scholar]
- 53.Vickers MH, Clayton ZE, Yap C et al. (2011) Maternal fructose intake during pregnancy and lactation alters placental growth and leads to sex-specific changes in fetal and neonatal endocrine function. Endocrinology 152, 1378–1387. [DOI] [PubMed] [Google Scholar]
- 54.Brownlee M (2005) The pathobiology of diabetic complications: a unifying mechanism. Diabetes 54, 1615–1625. [DOI] [PubMed] [Google Scholar]
- 55.Cohen-Addad N, Chatterjee M, Bekersky I et al. (1986) In utero-exposure to saccharin: athreat? Cancer Lett 32, 151–154. [DOI] [PubMed] [Google Scholar]
- 56.Sturtevant FM (1985) Use of aspartame in pregnancy. Int J Fertil 30, 85–87. [PubMed] [Google Scholar]
- 57.Rodero AB, Batig á lia F, Azoubel R et al. (2010) Effects of sucralose ingestion on fetal and placental weights and umbilical-cord length: experimental study. Int J Morphol 28, 823–827. [Google Scholar]
- 58.Zhang GH, Chen ML, Liu SS et al. (2011) Effects of mother’s dietary exposure to Acesulfame-K in pregnancy or lactation on the adult offspring’s sweet preference. Chem Senses 36, 763–770. [DOI] [PubMed] [Google Scholar]
- 59.Pope E, Koren G & Bozzo P (2014) Sugar substitutes during pregnancy. Canadian Family Physician 60, 1003–1005. [PMC free article] [PubMed] [Google Scholar]
- 60.Zhu Y, Olsen SF, Mendola P et al. (2017) Maternal consumption of artificially sweetened beverages during pregnancy, and offspring growth through 7 years of age: a prospective cohort study. Int J Epidemiol 46, 1499–1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Azad MB, Sharma AK, de Souza RJ et al. (2016) Association between artificially sweetened beverage consumption during pregnancy and infant body mass index. JAMA Pediatr 170, 662–670. [DOI] [PubMed] [Google Scholar]
- 62.Phelan S, Hart C, Phipps M et al. (2011) Maternal behaviors during pregnancy impact offspring obesity risk. Exp Diabetes Res 2011, 985139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chen LW, Aris IM, Bernard JY et al. (2017) Associations of maternal macronutrient intake during pregnancy with Infant BMI peak characteristics and childhood BMI. Am J Clin Nutr 105, 705–713. [DOI] [PubMed] [Google Scholar]
- 64.Jen V, Erler NS, Tielemans MJ et al. (2017) Mothers’ intake of sugar-containing beverages during pregnancy and body composition of their children during childhood: the generation R study. Am J Clin Nutr 105, 834–841. [DOI] [PubMed] [Google Scholar]
- 65.Gillman MW, Rifas-Shiman SL, Fernandez-Barres S et al. (2017) Beverage intake during pregnancy and childhood adiposity. Pediatrics 140, [Epublication ahead of print version]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Okubo H, Crozier SR, Harvey NC et al. (2014) Maternal dietary glycemic index and glycemic load in early pregnancy are associated with offspring adiposity in childhood: the Southampton women’s survey. Am J Clin Nutr 100, 676–683. [DOI] [PubMed] [Google Scholar]
- 67.Horan MK, McGowan CA, Gibney ER et al. (2014) Maternal low glycaemic index diet, fat intake and postprandial glucose influences neonatal adiposity–secondary analysis from the Rolo study. Nutr J 13, 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ojha S, Fainberg HP, Sebert S et al. (2015) Maternal health and eating habits: metabolic consequences and impact on child health. Trends Mol Med 21, 126–133. [DOI] [PubMed] [Google Scholar]
- 69.Dearden L & Ozanne SE (2015) Early life origins of metabolic disease: developmental programming of hypothalamic pathways controlling energy homeostasis. Front Neuroendocrinol 39, 3–16. [DOI] [PubMed] [Google Scholar]
- 70.Gugusheff JR, Ong ZY & Muhlhausler BS (2015) The early origins of food preferences: targeting the critical windows of development. FASEB J 29, 365–373. [DOI] [PubMed] [Google Scholar]
- 71.Brion MJ, Ness AR, Rogers I et al. (2010) Maternal macronutrient and energy intakes in pregnancy and offspring intake at 10 Y: exploring parental comparisons and prenatal effects. Am J Clin Nutr 91, 748–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ventura AK & Worobey J (2013) Early influences on the development of food preferences. Curr Biol 23, R401–R408. [DOI] [PubMed] [Google Scholar]
- 73.Mennella JA, Jagnow CP & Beauchamp GK (2001) Prenatal and postnatal flavor learning by human infants. Pediatrics 107, E88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ventura AK & Mennella JA (2011) Innate and learned preferences for sweet taste during childhood. Curr Opin Clin Nutr Metab Care 14, 379–384. [DOI] [PubMed] [Google Scholar]
- 75.Maone TR, Mattes RD, Bernbaum JC et al. (1990) A new method for delivering a taste without fluids to preterm and term infants. Dev Psychobiol 23, 179–191. [DOI] [PubMed] [Google Scholar]
- 76.Goran MI, Dumke K, Bouret SG et al. (2013) The obesogenic effect of high fructose exposure during early development. Nat Rev Endocrinol 9, 494–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Du L & Heaney AP (2012) Regulation of adipose differentiation by fructose and GLUT5. Mol Endocrinol 26, 1773–1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Teff KL, Elliott SS, Tschöp M et al. (2004) Dietary fructose reduces circulating insulin and leptin, attenuates postprandial suppression of ghrelin, and increases triglycerides in women. J Clin Endocrinol Metab 89, 2963–2972. [DOI] [PubMed] [Google Scholar]
- 79.Araújo JR, Martel F & Keating E (2014) Exposure to nonnutritive sweeteners during pregnancy and lactation: impact in programming of metabolic diseases in the progeny later in life. Reprod Toxicol 49, 196–201. [DOI] [PubMed] [Google Scholar]
- 80.Toigo EV, Huffell AP, Mota CS et al. (2015) Metabolic and feeding behavior alterations provoked by prenatal exposure to aspartame. Appetite 87, 168–174. [DOI] [PubMed] [Google Scholar]
- 81.Collison KS, Makhoul NJ, Zaidi MZ et al. (2012) Interactive effects of neonatal exposure to monosodium glutamate and aspartame on glucose homeostasis. Nutr Metab (Lond) 9, 58. [DOI] [PMC free article] [PubMed] [Google Scholar]


