Abstract
Phosphorus-containing drugs belong to an important class of therapeutic agents and are widely applied in daily clinical practices. Structurally, the phosphorus-containing drugs can be classified into phosphotriesters, phosphonates, phosphinates, phosphine oxides, phosphoric amides, bisphosphonates, phosphoric anhydrides, and others; functionally, they are often designed as prodrugs with improved selectivity and bioavailability, reduced side effects and toxicity, or biomolecule analogues with endogenous materials and antagonistic endoenzyme supplements. This review summarized the phosphorus-containing drugs currently on the market as well as a few promising molecules at clinical studies, with particular emphasis on their structural features, biological mechanism, and indications.
Keywords: Phosphorus-containing drugs; Prodrugs; Drug modification; Phosphite, phosphate
1. Introduction
Phosphorus belongs to one of the most essential elements of life and is extensively distributed in nature. For example, phosphate-containing units are important building-blocks for nucleotides, which are the basic structures of deoxyribonucleic acid (DNA) and ribonucleic acid (RNA). Phosphorus-containing compounds are involved in vital processes or functions ranging from biochemistry, biogeochemistry, ecology, agriculture, to industry. For example, one of the most famous agricultural and industrial application was dichlorvos (DDVP), which used to be a broad spectrum insecticide and acaricide but was banned since 1998 due to its high toxicity in inhibiting acetyl cholinesterase [1]. Phosphorus-containing drugs constitute to be an important class of therapeutic agents targeting a wide range of diseases. Their development has long attracted significant attention from drug companies and pharmaceutical industry. For instance, menadiol sodium diphosphate developed by Roche was approved in 1941 as a vitamin K4 derivative in reducing risk of hemorrhage [2]. Classified by the structural character of phosphorus-containing functional groups, they can be categorized as phosphoesters, phosphoric amides, phosphonates, phosphinates, phosphine oxides, bisphosphonates, phosphoric anhydrides, and et al. Mechanistically, these phosphorus-containing drugs are designed either from the modification of present drugs to improve their properties, or derived from biological analogues [[3], [4]]. A number of phosphorus-containing drugs are designed as prodrugs in the form of phosphotriesters, phosphonates, phosphinates and phosphine oxides to achieve higher selectivity and bioavailability. Such prodrugs modified with phosphorus functionalities are believed to have a higher polarity and provide stronger hydrogen bonding in vivo compared to its unmodified one in clinical administration [5]. For example, monoester clindamycin phosphate is developed against bacterial infections and used in various drug combinations known as Benzaclin®2000, Ziana/Veltin®2006 and so forth [[6], [7]]. Synthetic steroids such as betamethasone, dexamethasome, prednisolone, hydrocortisone, and estramustine are developed to their corresponding sodium phosphates for the treatment of inflammations [[8], [9], [10]]. Another important type of phosphorus-containing drugs is biological analogues. For example, sofosbuvir is a nucleotide analogue inhibitor of NS5B polymerase developed for hepatitis C therapy [[11], [12], [13]], while remdesivir* is an antiviral nucleotide analog recently authorized for emergency use as a drug against COVID-19 [[14], [15], [16]].
The purpose of this review is to provide a brief overview of the phosphorus-containing drugs on market. Although there have been a few reviews related to the design of phosphorus-containing drugs, a comprehensive review with particular emphasis on their chemical structures and indications remains in high demand [[3], [4],17]. We hope this review can provide a clear structural landscape and therapeutic information of the current phosphorus-containing drugs on market, as well as an overview of the fast-developing area, trends, and opportunities in the discovery of new phosphorus-containing therapeutics.
2. Nomenclature of P-Containing Molecules
One unique aspect of phosphorus atom is its valence, which can be either 0, I, II, III, or V. Most phosphorus-containing organic compounds are P(III)- and P(V)-containing molecules. Both are useful and common in nature, with myriad biological and chemical functions. Hence, it is important to classify different phosphorus-containing organic compounds with unambiguous nomenclature for identification.
2.1. P(III)-containing molecules
Most P(III)-containing compounds are essential chemical feedstocks such as phosphine (PH3), phosphorus trichloride (PCl3), triphenylphosphine (PPh3), and so on. On the basis of the element directly bound to the phosphorus center, P(III)-containing molecules can be divided into phosphite esters, phosphonites, phosphinites, phosphine, phosphorothioite, phosphorodithioite, phosphoamidite, and so on (Table 1 ) [4,18]. Due to the presence of a lone pair on the P(III) atom with strong coordinating ability, P(III)-containing molecules are rarely developed as therapeutic agents.
Table 1.
Nomenclature of P(III)-containing molecules
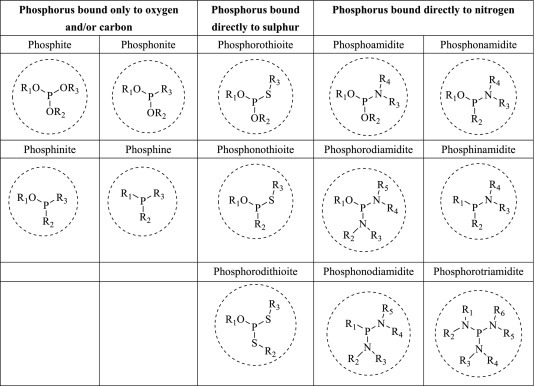
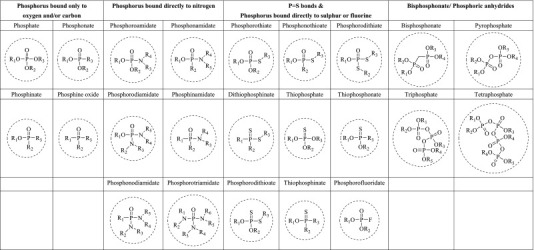
2.2. P(V)-Containing Molecules
Most phosphorus-containing drugs are P(V)-containing molecules. Organophosphorus compounds with pentavalent phosphorus atom are called phosphoranes; phosphoranes of the type R3P=CR2 with a phosphorus carbon double bond are known as phosphonium ylides. However, most phosphorus-containing drugs possess phosphoryl (P=O) groups, which are typically bound directly to oxygen (phosphate), nitrogen (phosphoroamidate), carbon (phosphonate, phosphinate, and phosphine oxide), sulphur (phosphorothionate), and fluorine (phosphorofluoridate) [18]. Other major types of P(V)-containing drugs include thiophosphate containing P=S bonds, phosphoric anhydrides with one or multiple P-O-P units, and bisphosphonate bearing P-C-P units, as shown in Table 2 .
Table 2.
Nomenclature of P (V)-containing molecules
3. Classification of P (V)-Containing Drugs
(Mark* means the drug is not on the market)
3.1. Phosphomonoester and Phosphodiester Drugs
The development of phosphoester and phosphodiester drugs have attracted significant attention ever since menadiol sodium diphosphate (Synkayvite®) was first developed and approved by FDA in 1941 (Figure 1 ) [19]. Today more than 37 phosphoesters and phosphodiesters are in the market and their combinational drugs are not even included.
Fig. 1.
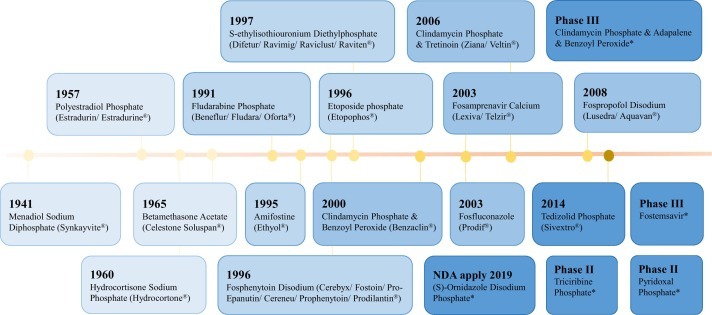
Time line of main phosphomonoester and phosphodiester drugs.
Most phosphoester drugs are developed based on the modification of currently existing drugs to improve efficacy, by tethering a phosphoric monoester to the drug molecule through a hydroxyl functionality, while most phosphodiester drugs were derived from essential biomolecules or bio-markers, such as glycerol, nucleotides, and enzymes.
3.1.1. Phosphomonoester Drugs
Phosphomonoester features the direct connection of the phosphate group to the hydroxyl group of an existing drug molecule, which is designed to circumvent the insufficient solubility issue of the parent drug. The presence of phosphomonoester moiety improves the efficacy and the aqueous solubility of the corresponding drug molecule during the absorption and distribution process (Figure 2 ) [5]. The phosphate prodrug undergoes conversion to its parent drug in vivo and inorganic phosphate through the interaction with alkaline phosphatase, an abundant enzyme in human body [20].
Fig. 2.
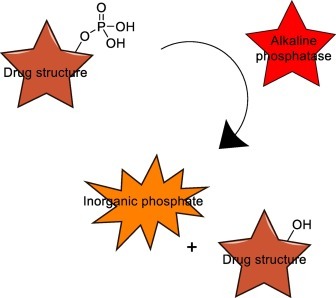
Interconversion of phosphomonoesters prodrugs into their hydroxyl parent drugs and inorganic phosphate during the absorption and distribution process.
Clindamycin (1) is a 50S ribosomal subunit inhibitor for treating gram-positive bacterial infections (Figure 3 ). However, irritation at the injection site was observed with this parent drug. The topical application of clindamycin phosphate (Cleocin/Dalacin-S/Evoclin®, 2) can replace the parent drug clindamycin (1) due to its higher aqueous solubility and efficient release of drugs in vivo [7]. Clindamycin is also in combination with benzoyl peroxide (Benzaclin®2000), tretinoin (Ziana/Veltin®2006), adapalene and benzoyl peroxide* (phase III) in treating acne [6,21]. Fosfluconazole (Prodif®2003, 3) has been considered as a triazole antifungal and lanosterol 14 α-demethylase (CYP51A1) inhibitors. It is prescribed for the treatment of fungal infections caused by Cryptococcus neoformans and Candida [22]. The application of fosfluconazole increases the efficacy of the parent drug fluconazole in vivo due to the rapid transport of phosphate derivative across cell membranes [23]. Polyestradiol phosphate (PEP) (Estradurin/Estradurine®1957, 4) is a polymeric synthetic estrange steroid for the treatment of metastatic prostate cancer [24]. As slow hydrolysis rate is presented for phosphoesters of secondary and tertiary alcohols due to decreased catalytic efficiency of the enzyme by steric hindrance at the cleavage site, polyestradiol phosphate (4) represents a long-lasting prodrug with slow release of estradiol in the body [25].
Fig. 3.
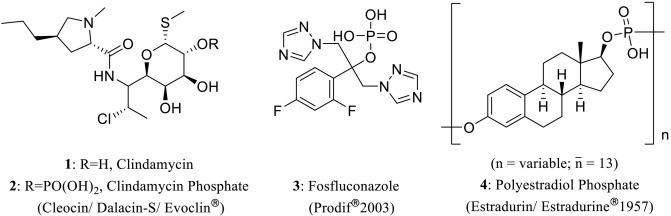
Structures of secondary and tertiary alcohol-derived phosphomonoester drugs 2–4.
Effective clinical applications are also achieved by phosphatization of related biomolecules, such as endogenous structures. This is exemplified by vidarabine monophosphate (5), a phosphorylated vidarabine, actively treating the systematic herpes virus infection (Figure 4 ) [26]. Its fluorine derivative, fludarabine phosphate (Beneflur/Fludara/Oforta®1991, 6), is a DNA synthesis inhibitor and applied in therapy of chronic lymphocytic leukemia (CLL) [[27], [28]]. Many molecules of this type are still in clinical trials. For instance, triciribine phosphate* (TCN-P, 7) is currently at phase II clinical studies and is designed for the treatment of breast cancer, acute myeloid leukemia and ovarian cancer by inhibiting protein kinase B (PKB) at the target AKT1 [[29], [30]]. Pyridoxal phosphate* (PLP, 8) as a purinergic P2 receptor antagonist, is currently tested in tardive dyskinesia (phrase II) [31]. Fostemsavir* (9) is under phase III stage as envelope glycoprotein inhibitors, gp120 attachment inhibitors, and HIV gp120 protein inhibitors [32].
Fig. 4.
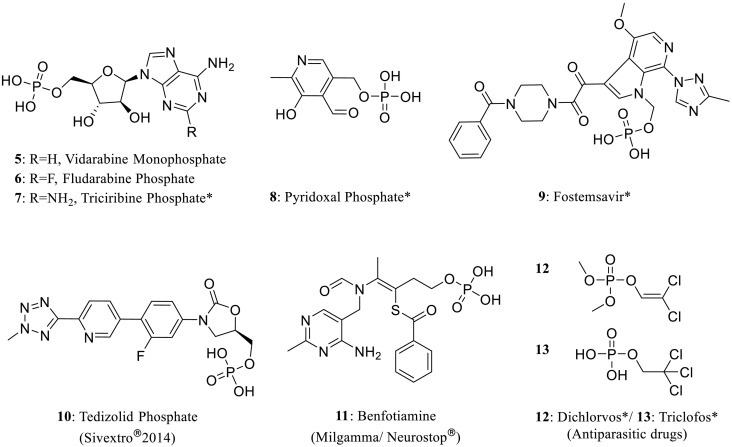
Structures of primary alcohol-derived phosphomonoester drugs 5–13.
Tedizolid phosphate (Sivextro®2014, 10) is one of the most important protein synthesis inhibitors, 50S ribosomal subunit inhibitors, and oxazolidinone antibiotics. This pharmaceutical product is used for the treatment of methicillin resistant to staphylococcus aureus and bacterial skin infections [33]. Other phosphomonoester drugs derived from primary alcohols include benfotiamine (Milgamma/Neurostop®) (11) for vitamin B1 deficiency, chlorinated drugs dichlorvos (DDVP)* (12) and triclofos* (13) [[34], [35]].
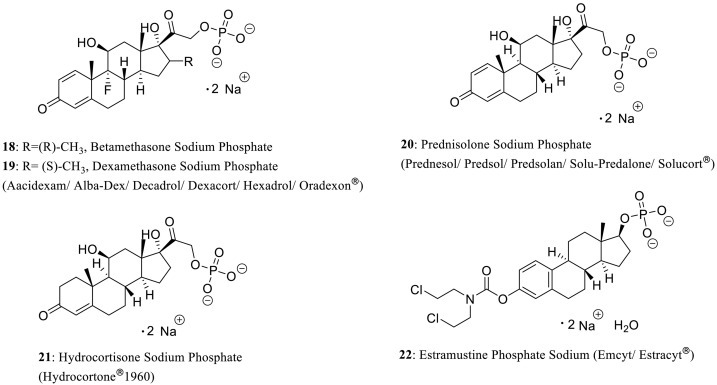
Besides parent drugs containing aliphatic alcohols, those with phenolic moieties are also applicable to design as phosphomonoester prodrugs (Figure 5 ) [36]. For example, fosfestrol sodium* (15) is an estrogen receptor (ER) agonist in prostatic cancer therapy and this drug is derived from the phosphorylation of hormone drug fosdestrol* (Distilbene/Stilbestrol/Stilbetin®) (14). Fosfosal (Aydolid/Disdolen®) (16) is a salicylic acid phosphate serving as a nonsteroidal anti-inflammatory and analgesic drug (NSAID) [37]. As a topoisomerase (DNA) II alpha (TOP2A) inhibitor, etoposide phosphate (Etopophos®1996, 17) exhibits sufficient aqueous solubility to minimize the probability of drug precipitation by injection, which is widely used for treating testicular cancer, small cell lung cancer, multiple myeloma, acute lymphoblastic leukemia, and non-Hodgkin’s lymphoma [5,[38], [39], [40]].
Fig. 5.
Structures of phenol-derived phosphomonoester drugs 15-17.
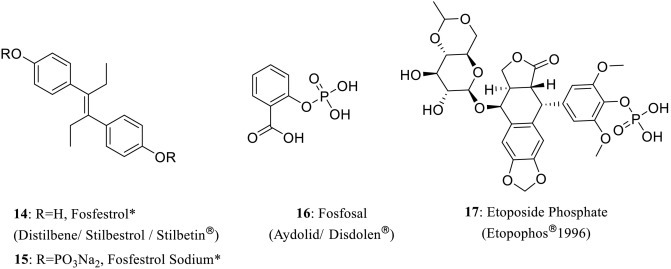
The modification by forming sodium and calcium phosphates also shows a tremendous improvement in aqueous affinity of the parent drugs, facilitating drug absorption and distribution, as well as relieving skin irritation. One of the most classical examples is betamethasone, a steroid medication which acts as a glucocorticoid receptor (GR) agonist for various infections, allergic diseases, and immune inflammations (Figure 6 ) [[41], [42]]. Betamethasone sodium phosphate (18) is involved in intramuscular use when the oral therapy is not feasible. This prodrug is also used in clinical application to interact with drugs such as betamethasone acetate (Celestone Soluspan®1965) and fradiomycin sulfate (Rinderon-A®), to stimulate additional inhibitory activity against cell wall biosynthesis [[43], [44]].
Fig. 6.
Structures of steroid hormone-derived sodium phosphate drugs 18–22.
The anabolic steroids analogues, dexamethasone sodium phosphate (Aacidexam/Alba-Dex/Decadrol/Dexacort/Hexadrol/Oradexon®) (19) is developed to replace its parent drug testosterone in clinical application. For example, aciont (Visulex®) is currently in phase II clinical trial for treating uveitis [8,[45], [46]]. Other synthetic glucocorticoid corticosteroid analogues include hydrocortisone sodium phosphate (Hydrocortone®1960, 21) and prednisolone sodium phosphate (Prednesol/Predsol/Predsolan/Solu-Predalone/Solucort®) (20), which are also used in combination with sulfacetamide sodium (Vasocidin®1988) and phenoxazoline* [9,[47], [48]]. In addition, estramustine phosphate sodium (Emcyt/Estracyt®) (22) has been approved as an alkylating agent to treat prostatic cancer [10].
Most phosphomonoester drugs are pharmacologically designed from either existing clinical drugs or naturally occurring compounds by esterification to form sodium and calcium phosphate (Figure 7 ). Fosphenytoin disodium (Cerebyx/Fostoin/Pro-Epanutin/Cereneu/Prophenytoin/Prodilantin®1996, 23) is applied to deliver phenytoin more efficiently due to its excellent water-solubility [13,[49], [50]]. Fospropofol disodium (Lusedra/Aquavan®2008, 24) is also a water-soluble form of fospropofol which is a hypnotic alkylphenol derivative to be related to the effects on GABA-mediated chloride channels in the central nervous system (CNS) [[51], [52], [53]]. This drug molecule can be hydrolyzed by alkaline phosphatase in vivo to propofol, possessing greater potential than propofol for hyperlipidemia at long-time administration. It is noted that riboflavin sodium phosphate (Hyryl/Ribo®) (25) is developed from natural riboflavin (vitamin B2) and menadiol sodium diphosphate (Synkayvite®1941, 26) is modified from Vitamin K4 [19]. Other promising and important phosphomonoester drugs currently under clinical studies include gadofosveset trisodium* (Ablavar/AngioMARK/Vasovist®2015, 28), (S)-ornidazole disodium phosphate* (NDA apply) (27), and mifamurtide sodium* [[54], [55], [56]]. There are only a few calcium phosphate drugs on the market. Calcium glycerylphosphate (or calcium glycerophosphate, 29) is a mineral supplement and fosamprenavir calcium (Lexiva/Telzir®2003, 30) is a derivative of HIV-1 protease inhibitor and antiretroviral drug amprenavir [[57], [58]].
Fig. 7.
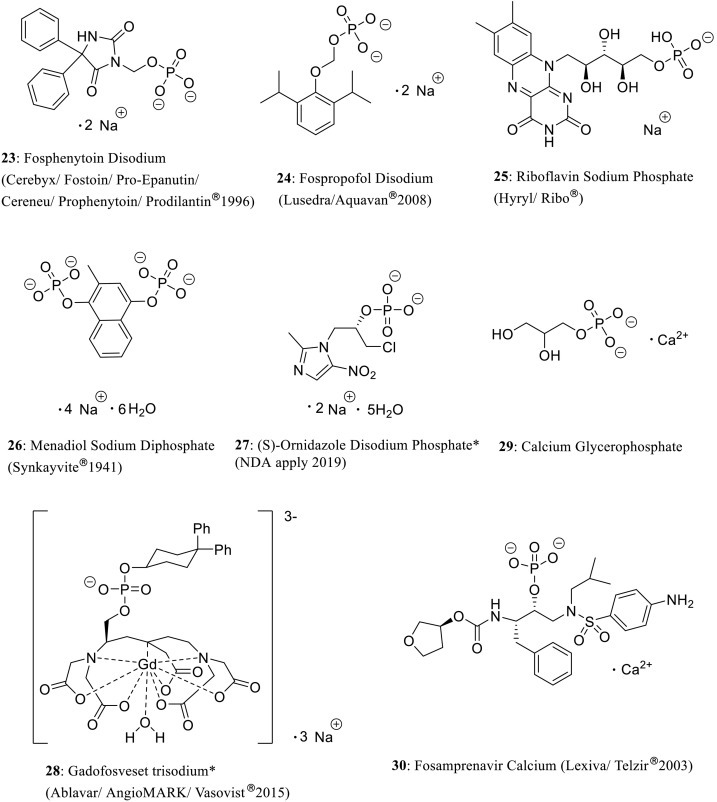
Structures of sodium and calcium phosphate drugs 23-30.
3.1.2. Phosphodiester Drugs
Besides phosphomonoester drugs designed from direct connection between the phosphate group and a hydroxyl group of the parent drug, phosphodiester drugs derived from natural and biologically active chemicals constitute another important class of phosphate drugs (Figure 8 ). For example, (S)-ethylisothiouronium diethylphosphate (Difetur/Ravimig/Raviclust/Raviten®1997, 31) is a specific inhibitor of inducible nitric oxide (NO) synthase on hepatic NO production level [[59], [60]]. Other distinct phosphodiester structures are cyclic esters such as bucladesine, cifostodine (neurodrug) (37), and adenosine cyclophosphate (36) [17,61]. Bucladesine sodium (Actosin®) (35) is modified from bucladesine, which is a nucleotide derivative of phosphodiesterase (PDE) inhibitor to mimic the action of endogenous cAMP [[62], [63]]. Derived from a natural choline compound in brain, choline alfoscerate (α-GPC) (Brezal/Delecit/Gliatilin®) (33) was designed as a parasympathomimetic acetylcholine precursor to deliver choline across the blood-brain barrier (BBB) for treating Alzheimer's disease and other dementias [[64], [65]]. BBB is a highly selective semipermeable border of endothelial cells. Solutes are not permitted to cross into extracellular fluid of neurons reside-containing CNS from the circulating blood, such as pathogens. As a result, one major challenge in drug discovery of the CNS therapy is to allow the therapeutics to pass through BBB [[66], [67], [68]]. It is believed that the high polarity of choline alfoscerate makes it readily pass through BBB to provide good therapeutic effect [69]. Other renowned phosphodiester drugs are exemplified by colfosceril palmitate (Surfexo®Neonatal™) (34) applied as a pulmonary surfactant, and vitamin B12-derived methylcobalamine* (MeCbl/MeB12) (32) as a cardiovascular drug [[70], [71], [72]].
Fig. 8.
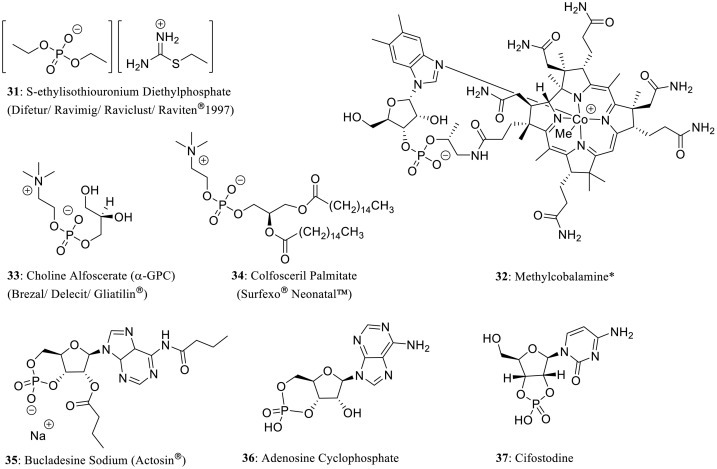
Structures of phosphodiester drugs 31-34 and cyclic phosphodiester drugs 35-37.
3.2. Phosphoric Amide Drugs
Phosphoric amide drugs, such as phosphoromonoamidates, phosphorodiamidates and phosphorotriamides, are designed as prodrugs from the corresponding active parent drugs by direct connection between nitrogen and phosphorus atom. Figure 9 delineated the time line for the development of main phosphoric amide drugs. Among them, fosaprepitant dimeglumine (EMEND/Ivemend/Proemend®2007, 38) is a prodrug of apreitant, which is used to prevent chemotherapy-induced nausea and vomiting (CINV), and postoperative nausea and vomiting (PONV) [73]. Creatine and phosphocreatine are naturally occurring chemicals within the body primarily stored in skeletal muscle. Because phosphocreatine is capable of anaerobically donating a phosphate group to ADP to regenerate ATP, and excess ATP can be dephosphorylated during periods of low muscle activity to convert creatine to phosphocreatine, phosphocreatine is a crucial energy buffer in body muscle cells. The pharmacological role of creatine phosphate sodium (39) is to facilitate recycling of ATP for reducing the risk of muscular and cardiovascular disease [[74], [75]]. (See Fig. 10 .)
Fig. 9.
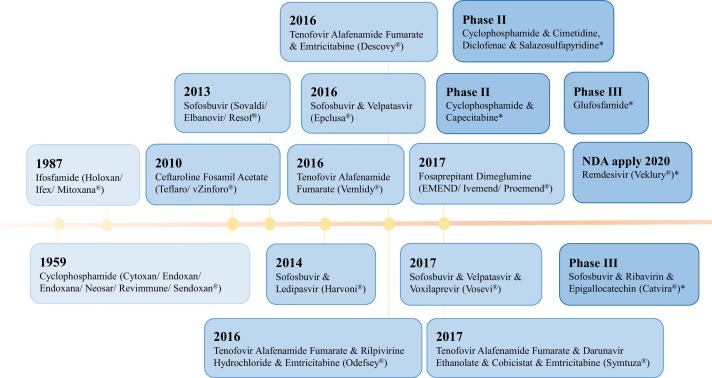
Time line of main phosphoric amide drugs.
Fig. 10.
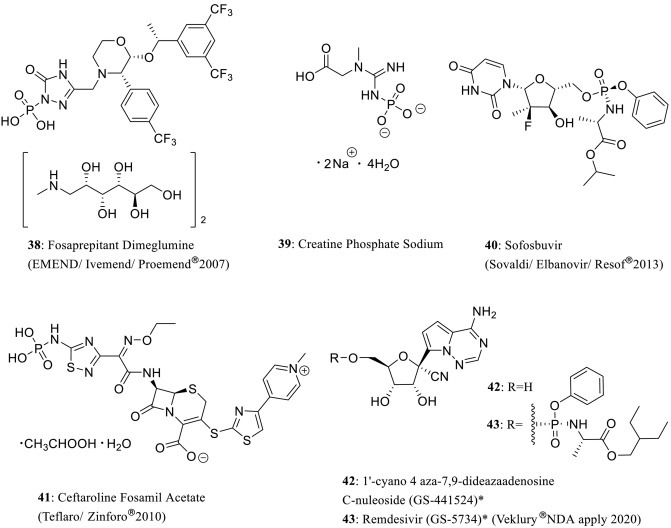
Structures of phosphoromonoamidate drugs 38–43.
Sofosbuvir (Sovaldi/Elbanovir/Resof®2013, 40) is developed as a prodrug in antihepatitis C treatment. This phosphoric amide compound is metabolized in vivo to triphosphate form as the active antiviral agent, which functions as a defective substrate for NS5B protein (viral RNA polymerase) to inhibit viral RNA synthesis [[11], [12],[76], [77]]. Sofosbuvir is also combined with ledipasvir (Harvoni®2014), velpatasvir (Epclusa®2016), velpatasvir, voxilaprevir (Vosevi®2017), ribavirin, and epigallocatechin* (Catvira® phase III) in clinical applications [13,[78], [79], [80]]. Ceftaroline fosamil acetate (Teflaro/Zinforo®2010, 41) is developed as a prodrug of ceftaroline, which is a novel cephalosporin for inhibiting MRSA. It converts to active metabolise caftaroline and inactive caftaroline-M1 in vivo [81]. Antiviral remdesivir* (GS-5734) (Veklury®NDA apply) (43) is a RNA polymerase inhibitor recently authorized for emergency use as a drug against COVID-19. Remdesivir is reported to inhibit murine hepatitis virus (MHV) replication, potently inhibit SARS-CoV, and MERS-CoV in primary human airway epithelial cells. By comparing with its parent adenosine nucleoside without possessing the phosphoramide moiety, 1′-cyano 4-aza 7,9-dideazaadenosine C-nucleoside (GS-441524, 42), remdesivir has provided markedly enhanced antiviral activities. It is more potent (EC50 = 0.03 μmol/L) in inhibition of MHV than GS-441524 (EC50 = 1.1 μmol/L). In addition, remdesivir has shown 3 to 30 times more active than GS-441524 in all tested coronaviruses (CoVs) due to its more efficient metabolization of remdesivir [[14], [15], [16]].
Cyclophosphoamide is a vital structure of phosphorodiamidate drugs and is commonly featured by the presence of two P-N bonds. Drugs of this type have been used as nitrogen mustard alkylating agents for cancer treatment (Figure 11 ). It has been reported that the phosphoryl group is involved as the carrier structure of alkylation reaction at β-chloroethylamino functionality, which can be selectively activated by phosphoramidase in tumor cells for alkylation of DNA through a cationic aziridinium intermediate [3,82]. Cyclophosphamide (Cytoxan/Endoxan/Endoxana/Neosar/Revimmune/Sendoxan®1959, 44) is a chemotherapy medicine suppressing the immune system [[83], [84]]. Normally, it is in drug interactions with cimetidine, diclofenac and salazosulfapyridine (SASP)* (phase II) for clinical treatment of solid tumor, metastatic pancreatic cancer, as a Histamine H2 receptor antagonist, alkylating agent, COX inhibitor, PGSI and LT synthesis inhibitor [[85], [86], [87]]. In addition, the combination of cyclophosphamide and capecitabine* (phase II) is applicable for treatment of mammary cancer by further inhibiting nucleoside metabolism and thymidylate synthase (TYMS) [[88], [89]]. As the alkylating agents, ifosfamide (Holoxan/Ifex/Mitoxana®1987, 45) is used for treating testicular cancer, breast cancer, solid tumor, lung cancer, sarcoma, lymphoma, and ovarian cancer, while trofosfamide (Ixoten®) (46) is used for targeting malignant tumor [90]. Several phosphordiamidate drugs are currently under investigation as alkylating agents and DNA synthesis inhibitors such as glufosfamide* (47) currently in phase III clinical trial for treating advanced breast cancer and pancreatic cancer [[91], [92]].
Fig. 11.
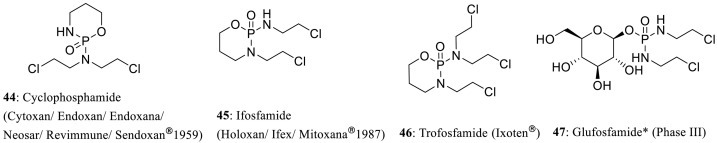
Structures of phosphorodiamidate 44–47.
Phosphorotriamidate alkylating agents bearing aziridine rings are also important nitrogen mustards as antineoplastic agents such as azetepa* (48), uredepa* (49), dipin* (50), fopurine* (51), and meturedepa* (52) (Figure 12 ) [17]. Glyciphosphoramide* (53) bearing β-chloroethylamino moieties is an effective DNA crosslinking agent with antitumor activities [[93], [94]]. However, some phosphorostriamideates are enzyme inhibitors such as urease inhibitors tolfamide* (54) and flurofamide* (55) [[95], [96], [97]].
Fig. 12.
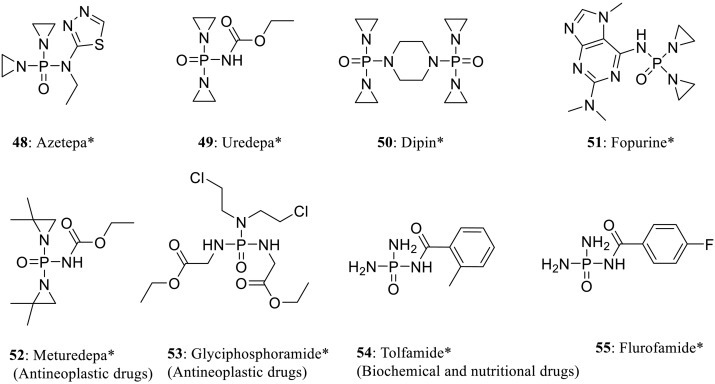
Structures of phosphorotriamidate 48–55.
Tenofovir alafenamide fumarate (Vemlidy®2016, 56) is a phosphate-containing drug having distinct chemical structures with respect to the phosphoric amides moieties [98]. It possesses a phosphorus center connecting directly with one P-C, P-N, and P-N bond (Figure 13 ). As a HBV nucleotide reverse transcriptase inhibitor (NRTI), this drug is approved for treatment of hepatitis B. It is also involved in a series of cooperative drugs for treatment of AIDS. For example, it is used in combination with emtricitabine (Descovy®2016), rilpivirine hydrochloride, and emtricitabine (Odefsey®2016) to inhibit additional nucleoside analog and non-nucleoside, HIV nucleoside analog reverse transcriptase [[99], [100]]. Alternatively, it is combined with darunavir ethanolate, cobicistat and emtricitabine (Symtuza®2017) to inhibit additional HIV-1 protease and cytochrome P450 3A (CYP3A) enzyme [101].
Fig. 13.
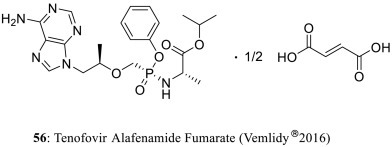
Structures of tenofovir slafenamide fumarate 56.
3.3. Phosphonate, Phosphinate, and Phosphine Oxide Drugs
Compounds containing a phosphorus atom binding directly to one or more carbon atoms feature different structure characters from phosphates, usually rendering a more hydrophilic surface and having better chemical stability. In a wide range of technologically important applications in chemical synthesis, a good catalytic activity is achieved by using phosphonate, phosphinate, and phosphine oxide as the catalyst due to the stronger adsorption capacity of the P-C bond for metal ions and organic molecules [102]. Fig. 14 delineates the progress in the development of phosphonate, phosphinate, phosphine oxide, and related drugs.
Fig. 14.
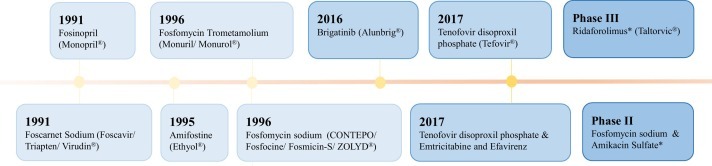
Time line of main phosphonate, phosphinate, phosphine oxide and other drugs.
The synthetic phosphonate analogues are mainly used as acyclic enzyme inhibitors, normally as phosphonate analogue prodrugs in clinical application (Figure 15 ). For example, the phosphonic acid derivative, foscarnet sodium (Foscavir/Triapten/Virudin®1991, 57) was developed from foscarnet (phosphonomethanoic acid) in treatment of herpes viruses, including drug-resistant cytomegalovirus (CMV) and herpes simplex viruses (HSV-1 and HSV-2) [[103], [104]]. It selectively acts against the pyrophosphate binding site due to the structural mimic of anion pyrophosphate [[105], [106]]. Antiparasitic drug metrifonate (Bilarcil/Memobay/ProMem®) (58) is an acetylcholinesterase inhibitor [107]. However, this drug was banned due to its high toxicity of metabolism dichlorvos in plants [108]. The phosphonodipeptides are also developed possessing antibacterial and antifungal properties, such as alafosfalin* (59) and LeuAlaP* (60) which are used as antibacterial drugs [[109], [110]].
Fig. 15.
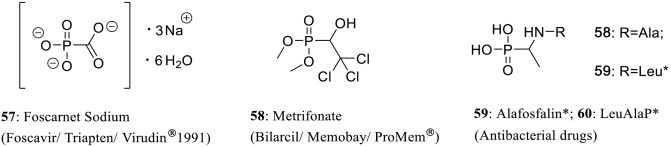
Structures of phosphonate drugs 57–60.
Phosphonate derivatives of heterocyclic bases have shown to inhibit nucleoside phosphorylase (Figure 16 ) [17]. Adefovir dipivoxil (ADV) (Preceon/Hepsera®, 62), a prodrug of pivoxil, is formulated to improve the fat solubility in vivo from adefovir, which is more polar and has a low oral bioavailability because of its free phosphonic acid functionality [3,111]; Tenofovir disoproxil phosphate (Tefovir®2017) (63) also inhibits nucleotide analogues reverse-transcriptase (NtRTI) for hepatitis B therapy. The interaction of tenofovir disoproxil phosphate with emtricitabine and efavirenz (2017) has been applied for AIDS treatment [[112], [113]]. In addition, (S)-HPMPA (61) possess potent and selective inhibitory activities against a broad spectrum of DNA viruses [114].
Fig. 16.
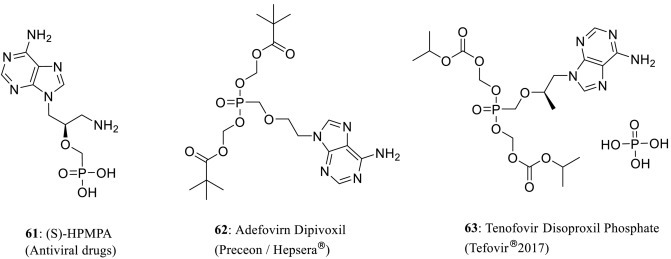
Structures of antiviral phosphonate drugs 61–63.
The high value of biological compounds with structures containing C-P bonds was gradually recognized with the identification of more and more naturally produced phosphonates. Their unique structural features and chemical biosyntheses are widely exploited in drug discovery and agricultural application (Figure 17 ) [115]. For example, fosfomycin is a phosphoenolpyruvate (PEP) analogue that inhibits the enzyme UDP-N-acetylglucosamine-3-enolpyruvyltransferase (MurA). It has been reported that this drug inhibits the biosynthesis of bacterial cell wall by alkylating an active site cysteine residue [[116], [117], [118]]. Fosfomycin sodium (CONTEPO/Fosfocine/Fosmicin-S/ZOLYD®1996, 64), as an antibiotic, was primarily used to treat bladder infections [119]. This drug is also involved in drug combination with amikacin sulfate* (phase II) for further inhibiting protein 30S ribosomal subunit [[120], [121]]. Another clinical application of aliphatic phosphate is fosfomycin trometamolium (Monuril/Monurol®1996, 65), which is mainly used for lowering urinary tract infection caused by sensitive bacteria [3,[121], [122]]. Drugs in this category remain in clinical trials including antiviral drugs fosarilate* (68), cardiovascular drugs fostedil* (66) and mifobate* (67) [17,123].
Fig. 17.
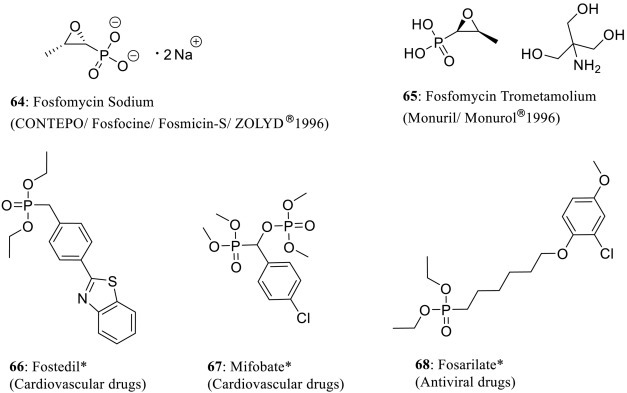
Structures of phosphonate drugs and bioactive molecules 64–68.
The replacement of the P-O bonds of phosphates with two or three P-C bonds has been applied in phosphorus-containing drug design (Figure 18 ). Unlike most angiotensin converting enzyme (ACE) inhibitors of cardiovascular drugs, fosinopril (Monopril®1991, 69) with a phosphinate structure is a more positive choice for treating hypertension and chronic heart failure through the body elimination by both renal and hepatic pathways [[124], [125]]; fosinoprilat is developed from the de-esterfication of fosinopril, which competitively binds to ACE in vivo [126]. Ridaforolimus* (Taltorvic®phase III, 70) is a small-molecule inhibitor of rapamycin (mTOR), interfering growth, division, metabolism, and angiogenesis of tumor cells [127]. As for phosphine oxide drugs containing three P-C bonds, fosazepam (71) is a water soluble derivative of diazepam (Valium1963), which is substituted with a dimethylphosphoryl group to improve its solubility in water [128]. This drug is a benzodiazepine derivative and acts as a positive allosteric modulator of the GABA type A receptors (GABAA) [129]. Small-molecule drug brigatinib (Alunbrig®2016, 72) acts as both an anaplastic lymphoma kinase (ALK) and a epidermal growth factor receptor (EGFR) inhibitor. It is also used in targeted cancer therapy [[130], [131]]. Fosenazide (73) is a neurodrug with strong inhibiting activities of adrenaline and 5-hydroxyrtryptamine (serotonin) [17].
Fig. 18.
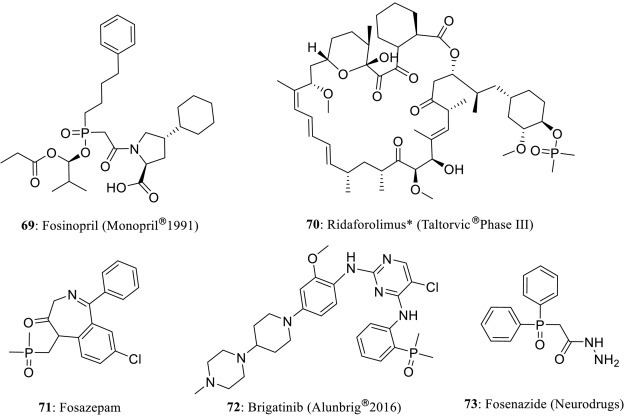
Structures of phosphinate and phosphine oxide drugs 69–73.
3.4. Other Phosphate Drugs
Besides the above introduced drugs, there are a series of phosphate drugs with close biological similarities, such as irreversible acetylcholinesterase inhibitors, dyflos and ecothiopate iodide (Figure 19 ) [132]. Dyflos (Floropryl®) (74) is a parasympathomimetic drug acting as irreversible anticholinesterase and being able to induce delayed peripheral neuropathy. This drug is used in ophthalmology as a miotic agent in veterinary medicine and treatment of chronic glaucoma [133]. Both dyflos and ecothiopate iodide (Ecothiopate Iodide®) (75) are used as ocular antihypertensives for chronic glaucoma therapy by covalently binding to serine group at the active site of the cholinesterase [134]. Amifostine (Ethyol®1995, 76) is a cytoprotective adjuvant and is used as an organic phosphorothiate prodrug for cancer chemotherapy and radiotherapy. After administration, it is hydrolyzed in vivo by alkaline phosphatase to the active cytoprotective thiol metabolite as a DNA-binding chemotherapeutic agent [135].
Fig. 19.
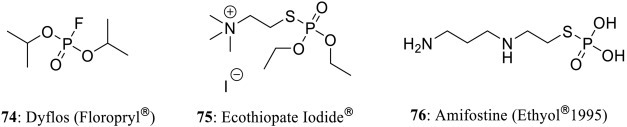
Structures of phosphorofluoridate drug 74 and phosphorothiate drugs 75–76.
3.5. Bisphosphonate and Phosphoric Anhydride Drugs
Main bisphosphonate and phosphoric anhydride drugs have been developed since 1970s (Figure 20 ), and more than 14 medical molecules of bisphosphonates and 8 phosphoric anhydrides are developed (both not include drug combination). Both of them constituted with at least two phosphorus functionalities, whose definition was based on P-containing linkages of ‘P-C-P’ or ‘P-O-P’.
Fig. 20.
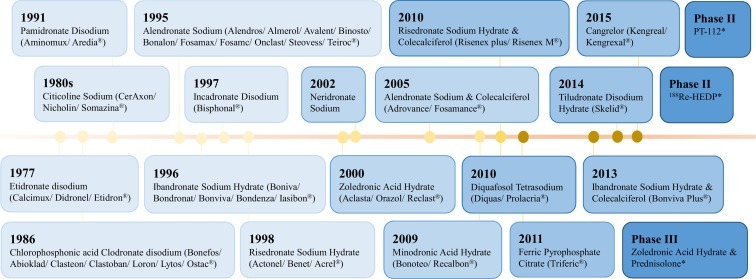
Time line of bisphosphonate and phosphoric anhydrides drugs
3.5.1. Bisphosphonate Drugs
Bisphosphonate drugs are characterized by the presence of two phosphonate moieties connected with a substituted carbon atom. Substitution with a hydroxyl group on the carbon atom has been shown to reduce osteoclastic activity and inhibit bone resorption, construction, and reconstruction. Drugs of this type are used for the treatment of hypercalcemia caused by osteoporosis, deformable osteoarthritis, and bone tumor [[136], [137]].
As bone resorption inhibitors, non-nitrogenous bisphosphonate drugs belong to the first generation of anti-osteoporotic drug (Figure 21 ). They are absorbed and metabolized by osteoclasts into ATP analogues and have been approved for preventing and treating osteoporosis in postmenopause [[138], [139]]. For example, etidronate disodium and clodronate disodium contain both hydroxyl and chlorine substitutions on the carbon atom connecting the two phosphate groups, respectively [[3], [4]]. Etidronate disodium (Calcimux/Didronel/Etidron®1977, 77) has been approved for the treatment of osteoporosis and Paget's disease of bone, while chlorophosphonic acid clodronate disodium (Bonefos/Abioklad/Clasteon/Clastoban/Loron/Lytos/Ostac®1986, 78) is used for reducing vertebral fractures, hyperparathyroidism, hypercalcemia in malignancy, multiple myeloma, and pain related in fracture (reduction in inflammatory markers like IL-1β, IL-6, and TNF-α) [[140], [141], [142]]. Chlorophosphonic acid clodronate disodium is also involved in drug interaction with clodronic acid and hyaluronic acid* (phase I) in osteoarthritis therapy due to its potent anti-inflammatory and analgesic effects [143].
Fig. 21.
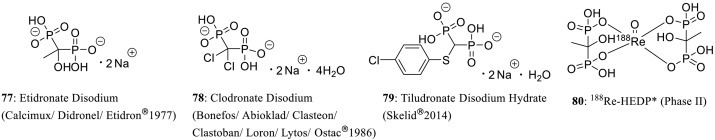
Structures of non-nitrogenous bisphosphonate drugs 77–80.
Tiludronate disodium hydrate (Skelid ®2014, 79) is a bisphosphonate derivative with a p-thiochlorobenzene ring-containing side chain for treatment of navicular disease. This drug is metabolized by osteoclasts to inhibit ATP in the cell competitively [144]. Another non-nitrogenous bisphosphonate drug is 188Re-HEDP* (phase II) (80) which contains rare metal rhenium [145].
Unlike the above-introduced first generation of bisphosphonates, the second and third generation of bisphosphonate drugs have been developed with nitrogen-containing substitution or nitrogen-containing heterocycles in side chains, respectively. This specific design allow these drugs to interfere farnesylation and protein geranylation of ATP by combining with farnesyl pyrophosphate (FPP) synthetase and isopentene pyrophosphate (IPP) of mevalonate channel to form a stable ternary complex [3,[146], [147]].
Drugs belong to the second generation of bisphosphonate derivatives include pamidronate disodium (Aminomux/Aredia®1991, 81) for preventing bone loss and strengthening bone, ibandronate sodium hydrate (Boniva/Bondronat/Bonviva/Bondenza/Iasibon®1996, 82) for use in drugs interactions with colecalciferol (Bonviva Plus®2013) to treat osteoporosis and osteoporosis in post-menopausal women (phase III), alendronate sodium (Alendros/Almerol/Avalent/Binosto/Bonalon/Fosamax/Fosamc/Onclast/Steovess/Teiroc®1995, 83) which has been approved in drug combination with colecalciferol (Adrovance/Fosamance®2005), and alendronate, in combination with calcitriol (Maxmarvil®) (Figure 22 ) [[3], [4]]. In addition, LLP2A alendronate* (phase I) (84), neridronic acid (Attila/Nerixia®) (85), and neridronate sodium (2002) (86) are used for treating osteoporosis and Paget’s disease [[148], [149], [150]]. It should be indicated that incadronate disodium (Bisphonal®1997, 87) is a nitrogen-containing bisphosphonate drug that contributes a cycloheptyl substituted amino group [151].
Fig. 22.
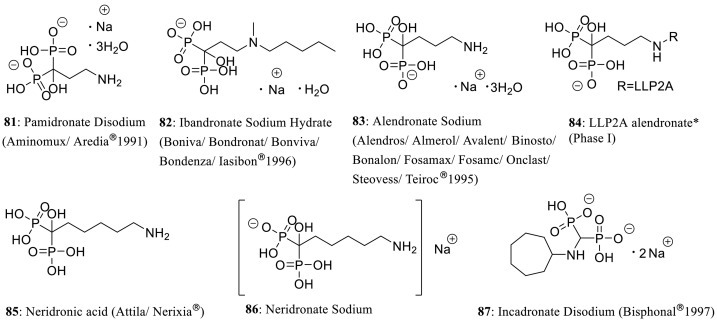
Structures of nitrogenous bisphosphonate drugs 81–87.
The third generation of bisphosphonate derivatives have been reported to possess more effective activity than drugs from the first two generations (Figure 23 ). For example, risedronate sodium hydrate (Actonel/Benet/Acrel®1998, 88) is involved in the interaction between risedronate sodium with colecalciferol (Risenex plus/Risenex M®2010) [[152], [153]]. Zoledronic acid hydrate (Aclasta/Orazol/Reclast®2000, 89) has been shown to interact with prednisolone* (phase III) and minodronic acid hydrate (Bonoteo/Recalbon®2009, 90) [[154], [155]].
Fig. 23.
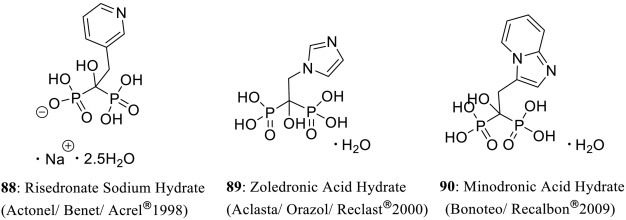
Structures of nitrogenous bisphosphonate drugs 88–90.
3.5.2. Phosphoric Anhydrides Drugs
Phosphoric anhydrides drugs are another major class of phosphates derivatives, including pyrophosphates, nucleoside diphosphates, nucleoside triphosphates, and tetraphosphates.
Pyrophosphates are phosphorus oxyanions containing two phosphorus atoms in a P-O-P linkage. Drugs of this type normally exist as pyrophosphate salt. The pyrophosphates drugs are developed from mimicking biochemical molecules with respect to the phosphate-phosphate bonds which are related to some endogenous important compounds, such as adenosine diphosphate (ADP) and adenosine triphosphate (ATP). For example, ferric pyrophosphate citrate (Triferic®2011, 91) is an iron(III) pyrophosphate for iron supplementation (Figure 24 ). It is used as a key element in the formation of new red blood cells for anemic dialysis patients [[156], [157]]. Cocarboxylase (TPP/ThPP/ThDP) (92) is a hiamine (vitamin B1) derivative for VB1 supplementation which is produced by the enzyme thiamine diphosphokinase [158]. As apoptosis stimulant and platinum-pyrophosphate agent, PT-112 (phase II) (93) is a platinum complex for treatment of solid tumor, multiple myeloma, and hepatoma [159].
Fig. 24.
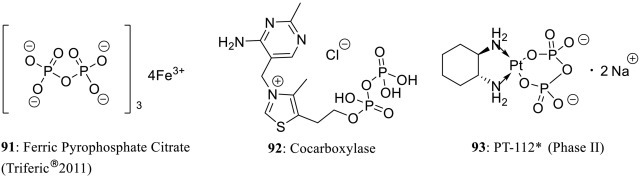
Structures of pyrophosphate drugs 91–93.
Other nucleoside derivatives are developed from the endogenous compounds with high-energy phosphate, such as adenosine diphosphate (ADP) and adenosine triphosphate (ATP) (Figure 25 ). As the nucleoside diphosphates analogues, citicoline sodium (CerAxon/Nicholin/Somazina®) (94) can improve cardiovascular and cerebrovascular circulation, and is used in treatment of brain damage, apoplexy, cerebrovascular, and Parkinson’s disease. This drug is hydrolyzed to choline and cytosine nucleosides in circulatory system and after crossing the blood-brain barrier, it is recombined again in the brain tissue to promote the biosynthesis of phospholipids in the cell membrane in brain tissue [[160], [161]]. Flavin adenine dinucleotide sodium (FAD) (Adeflavin/Flavitan/Flaziren/Wakadenin®) (95) is approved for treating acne, keratitis, vitamin B2 deficiency, conjunctivitis, acne rosacea, eczema, seborrheic dermatitis, and stomatitis. It is a redox-active coenzyme derivative with flavin mononucleotide, which is involved with several important enzymatic reactions of riboflavin in metabolism [162].
Fig. 25.
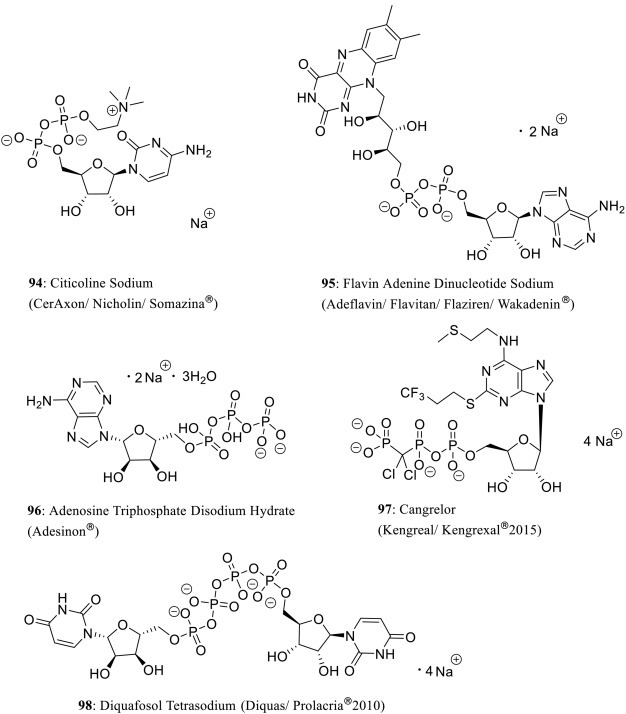
Structures of nucleoside pyrophosphate drugs 94-98.
It is widely known that adenosine triphosphate (ATP) is the most direct energy source involved in metabolism of organism. As its nucleoside analogues, adenosine triphosphate disodium hydrate (Adesinon®, 96) is approved for treating supraventricular arrhythmia and peripheral vascular disease in clinical practice. It is anticipated that a special antiplatelet drug, cangrelor (Kengreal/Kengrexal®2015, 97) has phosphorus oxyanions containing two phosphorus atoms in a P-O-P linkage [163]; one carbon atom and one phosphorus atom in P-C-P linkage, it is used to interfere P2Y12 receptors reversibly, which involves in ADP-induced platelet aggregate [164].
As a P2Y2 purinoceptor receptor (P2Y2) agonist, diquafosol tetrasodium (Diquas/Prolacria®2010, 98) is a tetraphosphate and has been approved for treating xerophthalmia [165].
3.6. Miscellaneous
Phosphorus-containing pharmaceutical molecules also include phosphorodithioate drugs and more (Figure 26 ). Thiotepa (Tepadina/Thioplex®1959, 99) is an alkylating agent and has been approved in treatment of gastrointestinal tumor, mammary, bladder, and ovarian cancer [[166], [167]]. Malathion (Ovide®1982, 100) has been reported to inhibit acetylcholinesterase (AChE) and is used for treating head louse [168]. As an anti-rheumatic agent and phosphorus triethyl-phosphine coordinated gold salt, auranofin (Ridaura®) (101) is a nonsteroidal anti-inflammatory and analgesic drug. Besides treating rheumatoid arthritis, it also shows moderate effects in clinical treatments of HIV infection, amebiasis, tuberculosis and ovarian cancer, which may be against on coronavirus (COVID-19) [[169], [170]].
Fig. 26.
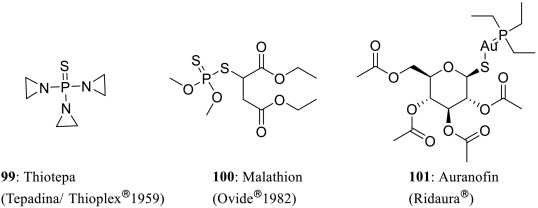
Structures of other phosphate drugs 99–101.
4. Conclusion and Outlook
This review summarizes the phosphorus-containing drugs on the market and related promising agents that are currently under clinical studies. Most P-containing drugs are designed as prodrugs for reducing side effects and toxicity, increasing the selectivity and bioavailability. Drugs of this type are characterized by either direct connection between phosphate group and the hydroxyl group of the parent drugs or possessing an indirect linker bearing function groups such as amino and halogens. The solubility and aqueous affinity of parent drugs are improved significantly. While slow conversion rate is confronted for prodrugs derived from the phosphomonester of secondary and tertiary alcohols in some cases, such as sodium phosphates and calcium phosphates, they are all developed by simple substitutions from chemical synthesis.
In a wide range of important clinical applications, phosphoric anhydrides and polyphosphates derivatives of P-containing drugs are developed by mimicking biochemical molecules in vivo, including some endogenous structures (ATP and ADP) and enzymes. For example, bisphosphonates with hydroxyl substitution on the carbon atom are active for bone resorption, construction, and reconstruction by reducing osteoclastic activities. Future generations of phosphorus-containing osteoporosis drugs and others with more complicated chemical structures share the same advantage.
It has been showcased that various forms of P-containing drug molecules have been developed from a rapidly progressing clinical research with various biological activities including anticancer, antibacterial, anti-inflammatory, anti-osteoporosis, and cerebrovascular circulation. Most common applications are consistently developed due to their potential advantages, including prodrugs modifying and resemblance to biochemical entities. It is certain that phosphorus-containing drugs will continue to be an important class of valuable therapeutic agents in clinical applications.
CRediT author statement
Hanxiao Yu: Information collecting, original draft writing.
He Yang: Writing-draft, review, editing.
Enxue Shi: Conceptualization.
Wenjun Tang: Conceptualization, writing-draft, review, editing, Supervision.
Conflict of interest
The authors declare that they do not have any conflicts of interest.
Acknowledgments
Acknowledgments
We are grateful to the Strategic Priority Research Program of the Chinese Academy of Sciences XDB20000000, CAS (QYZDY-SSW-SLH029), NSFC (21725205, 21432007, 21572246), STCSM-18520712200, and K. C. Wong Education Foundation.
References
- 1.Okoroiwu H.U., Iwara I.A. Dichlorvos toxicity: a public health perspective. Interdiscip Toxicol. 2018;11:129–137. doi: 10.2478/intox-2018-0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andrew W. Pharmaceutical Manufacturing Encyclopedia. 3rd ed.. William Andrew Publishing, Norwish NY: Elsevier; 2007; p. 56m-57m. ISBN-13: 9870815515265.
- 3.Yao Q., Reng L., Ran M., He J., Xiang D. Review on the structures of phosphorus-containing drugs used in clinical practice. Hua xue Shi ji. 2019;41:139–146. doi: 10.13822/j.cnki.hxsj.2019006737. [DOI] [Google Scholar]
- 4.Rodriguez J.B., Gallo-Rodriguez C. The role of the phosphorus atom in drug design. Chem Med Chem Rev. 2019;14:1–28. doi: 10.1002/cmdc.201800693. [DOI] [PubMed] [Google Scholar]
- 5.Karaman R. 1th ed. Nova Science Publisher, Inc; Nova Biomedical, New York: 2014. Prodrugs Design: A New Era (Pharmacology- Research, Safety Testing and Reaction) pp. 112–115. ISBN: 9781631177019. [Google Scholar]
- 6.Thielitz A., Gollnick H. Recent therapeutic developments for acne. Expert Rev Dermatol. 2013;8:37–50. doi: 10.1586/edm.12.70. [DOI] [Google Scholar]
- 7.Cambazard F. Clinical efficacy of VeIac®, a new tretinoin and clindamycin phosphate gel in acne vulgaris. J Eur Acad Dermatol Venerol. 1998;11:20–27. doi: 10.1111/j.1468-3083.1998.tb00903.x. [DOI] [PubMed] [Google Scholar]
- 8.Kulkarni P.S., Bhattacherjee K.E., Srinivasan B.D. Anti-inflammatory effects of betamethasone phosphate, dexamethasone phosphate and indomethacin on rabbit ocular inflammation induced by bovine serum albumin. Curr Eye Res. 2010;35:43–47. doi: 10.3109/02713688109019971. [DOI] [PubMed] [Google Scholar]
- 9.Esselinckx W., Bacon P.A., Ring E.F.J., Crooke D., Collins A.J., Demottaz D. A Thermographic assessment of three intra-articular prednisolone analogues given in rheumatoid synovitis. Br J Clin Parmac. 1978;5:447–451. doi: 10.1111/j.1365-2125.1978.tb01653.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benson R. Hartley-Asp. Mechanisms of action and clinical uses of estramustine. Cancer Invest. 2009;8:375–380. doi: 10.3109/07357909009012056. [DOI] [PubMed] [Google Scholar]
- 11.Pol S., Corouge M., Vallet-Pichard A. Daclatasvir–sofosbuvir combination therapy with or without ribavirin for hepatitis C virus infection: from the clinical trials to real life. Hepa Med Evid Res. 2016;8:21–26. doi: 10.2147/HMER.S62014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fung A., Jin Z., Dyatkina N., Wang G., Beigelman L., Deval J. Efficiency of incorporation and chain termination determines the inhibition potency of 2′-modified nucleotide analogs against hepatitis c virus polymerase. Antimicrob Agents Chemther. 2014;58:3636–3645. doi: 10.1128/AAC.02666-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shiha G., Soliman R., Elbasiony M., Darwish N.H.E., Mousa S.A. Addition of epigallocatechin gallate 400mg to sofosbuvir 400mg+daclatisvir 60mg with or without ribavirin in treatment of patients with chronic hepatitis c improves the safety profile: a pilot study. Sci Rep. 2019;9:13593. doi: 10.1038/s41598-019-49973-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Warren T.K., Jordan R., Lo M.K., Ray A.S., Mackman R.L., Soloveva V., et al. Therapeutic efficacy of the small molecule GS-5734 against Ebola virus in rhesus monkeys. Nature. 2016;531:381–385. doi: 10.1038/nature17180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agostini M.L., Andres E.L., Sims A.C., Graham R.L., Sheahan T.P., Lu X., et al. Coronavirus susceptibility to the antiviral remdesivir (GS- 5734) is mediated by the viral polymerase and the proofreading exoribonuclease. Mbio Asm Org. 2018;9 doi: 10.1128/mBio.00221-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gilead Sciences, Inc.; Jun, 2020. Fact sheet for health care providers emergency use authorization (EUA) of remdesivir (GS-5734™) https://www.fda.gov/media/137566/download
- 17.Yu X. Vol. 19. Pharma Industry; 1988. Development of Phosphorous-containing Drugs; pp. 513–520. [DOI] [Google Scholar]
- 18.Quin L.D.A. A John Wiley & Sons. Inc; Hoboken: 2000. Guide to Organophosphorus Chemistry. 1st ed.. Wiley Interscience. ISBN: 0471318248. [Google Scholar]
- 19.Song P.S., Moore T.A. Mechanism of the photodephosphorylation of menadiol diphosphate. a model for bioquantum conversion. J Am Chem Soc. 1968;90:6507–6514. doi: 10.1021/ja01025a049. [DOI] [PubMed] [Google Scholar]
- 20.Gani D., Wilkie J. Stereochemical, mechanistic, and structural features of enzyme-catalysed phosphate monoester hydrolyses. Chem Soc Rev. 1995:55–63. doi: 10.1039/CS9952400055. [DOI] [Google Scholar]
- 21.Kawashima M., Hashimoto H., Sáenz A., Ono M., Yamada M. Clindamycin phosphate 1.2%-benzoyl peroxide 3.0% fixed-dose combination gel has an effective and acceptable safety and tolerability profile for the treatment of acne vulgaris in Japanese patients: a phase iii, multicentre, randomised, single-blinded, active-controlled, parallel-group study. Br J Dermato. 2015;172:494–503. doi: 10.1111/bjd.13265. [DOI] [PubMed] [Google Scholar]
- 22.Richardson K., Cooper K., Marriott M.S., Tarbit M.H., Troke P.F., Whittle P.J. Discovery of fluconazole, a novel antifungal agent. Rew Infect Dis. 1990;12:S267–S271. doi: 10.1093/clinids/12.supplement_3.s267. [DOI] [PubMed] [Google Scholar]
- 23.Johnson D.S., Li J.J. A John Wiley & Sons. Inc; Wiley Interscience, Hoboken: 2007. The Art of Drug Synthesis; pp. 80–81. 9780471752158. [Google Scholar]
- 24.Jönsson G., Diczfalusy E., Plantin L.O., Röhl L., Birke G. Estradurin® (Polyestradiol Phosphate) in the treatment of prostatic carcinoma. AClinical and Stedoid Metabolic Study. Eur J Endocrino. 1963;44:S3–S41. doi: 10.1530/acta.0.044S003. [DOI] [PubMed] [Google Scholar]
- 25.Safadi M., Oliyai R., Stella V.J. Phosphoryloxymethyl carbamates and carbonates—novel water-soluble prodrugs for amines and hindered alcohols. Pharma Res. 1993;10:1350–1355. doi: 10.1023/a:1018934200343. [DOI] [PubMed] [Google Scholar]
- 26.Whitley R.J., Tucker B.C., Kinkel A.W., Barton N.H., Pass R.F., Whelchel J.D., et al. Pharmacology, tolerance, and antiviral activity of vidarabine monophosphate in humans. Antmicrob Agent Chemother. 1980;18:709–715. doi: 10.1128/AAC.18.5.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Keating M.J. Fludarabine phosphate in the treatment of chronic lymphocytic leukemia. Semin Oncol. 1990;17:49–62. [PubMed] [Google Scholar]
- 28.Chun H.G., Leyland-Jones B., Cheson B.D. Fludarabine phosphate: a synthetic purine antimetabolite with significant activity against lymphoid malignancies. J Clin Oncol. 1991;9:175–188. doi: 10.1200/JCO.1991.9.1.175. [DOI] [PubMed] [Google Scholar]
- 29.Hoffman K., Holmes F.A., Fraschini G., Esparza L., Frye D., Raber M.N., et al. Phase I-II study: triciribine (tricyclic nucleoside phosphate) for metastatic breast cancer. Cancer Chemother Pharmacol. 1996;37:254–258. doi: 10.1007/BF00688325. [DOI] [PubMed] [Google Scholar]
- 30.Phase I. Pharmacokinetic and pharmacodynamic study of triciribine phosphate monohydrate, a small-molecule inhibitor of AKT phosphorylation, in adult subjects with solid tumors containing activated AKT. Invest New Drugs. 2011;29:1381–1389. doi: 10.1007/s10637-010-9479-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ricciardi L., Pringsheim T., Barnes T.R.E., Martino D., Gemington G., Addington D., et al. Treatment recommendations for tardive dyskinesia. Canadia J Psychia. 2019;64:388–399. doi: 10.1177/0706743719828968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lataillade M., Zhou N., Joshi S.R., Lee S., Stock D.A., Hanna G.J., et al. Viral drug resistance through 48 weeks, in a phase 2b, randomized, controlled trial of the HIV-1 attachment inhibitor prodrug, fostemsavir. J Acquir Immune Defic Syndr. 2018;77:299–307. doi: 10.1097//QAI.0000000000001602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rybak J.M., Roberts K. Tedizolid phosphate: a next-generation oxazolidinone. Infect Dis Ther. 2015;4:1–14. doi: 10.1007/s40121-015-0060-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stracke H., Lindemann A., Federlin K.A. Benfotiamine-vitamin B combination in treatment of diabetic polyneuropathy. Exp Clin Endocrinol Diabetes. 1996;104:311–316. doi: 10.1055/s-0029-1211460. [DOI] [PubMed] [Google Scholar]
- 35.Murakami T., Iwamuro Y., Chinaka S., Takayama N., Komatsu T. Highly sensitive detection of organophosphorus pesticides using 5,10,15,20-tetrakis(4-hydroxyphenyl)porphyrin. Anal Sci. 2015;31:1325–1328. doi: 10.2116/analsci.31.1325. [DOI] [PubMed] [Google Scholar]
- 36.Odlo K., Klaceness J., Rongved P., Hansen T.V. Synthesis of combretastatins A-1 and B-1. Tetra Lett. 2006;47:1101–1103. doi: 10.1016/j.tetlet.2005.12.037. [DOI] [Google Scholar]
- 37.Jeromin L. Clinical follow-up of prostatic cancer patients under intermittent treatment with fosfestrol and bromocriptine. Urol Int. 1988;43:41–43. doi: 10.1159/000281431. [DOI] [PubMed] [Google Scholar]
- 38.Shah J.C., Chen J.R., Chow D. Preformulation study of etoposide: identification of physicochemical characteristics responsible for the low and erratic oral bioavailbility of etoposide. Pharma Res. 1989;6:408–412. doi: 10.1023/a:1015935532725. [DOI] [PubMed] [Google Scholar]
- 39.Budman D.R., Lgwemezie L.N., Kaul S., Behr J., Lichtman S., Schulman P., et al. Phase I evaluation of a water-soluble etoposide prodrug, etoposide phosphate, given as a 5-minute infusion on days 1, 3, and 5 in patients with solid tumors. J Clin Oncol. 1994;12:1902–1909. doi: 10.1200/JCO.1994.12.9.1902. [DOI] [PubMed] [Google Scholar]
- 40.Hande K.R. Etoposide: four decades of development of a topoisomerase II inhibitor. Eur J Cancer. 1998;34:1514–1521. doi: 10.1016/S0959-8049(98)00228-7. [DOI] [PubMed] [Google Scholar]
- 41.Papangkorn K., Prendergast E., Higuchi J.W., Brar B., Higuchi W.I. Noninvasive ocular drug delivery system of dexamethasone sodium phosphate in the treatment of experimental Uveitis rabbit. J Ocular Phar Therapeu. 2017;33:1–10. doi: 10.1089/jop.2017.0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Golladay E.S. Treatment of keloids by single intraoperative perilesional injection of repository steroid. Sou Med J. 1988;81:736–738. doi: 10.1097/00007611-198806000-00013. [DOI] [PubMed] [Google Scholar]
- 43.Roberts H.J. Local injection of a preparation containing two betamethasone esters in the treatment of noninfectious musculoskeletal disorders. J Am Geria Soc. 1965;13:275–291. doi: 10.1111/j.1532-5415.1965.tb02677.x. [DOI] [PubMed] [Google Scholar]
- 44.Okada N, Hashimoto K, Sato K, Yamamura T, Yoshikawa K. Clinical Evaluation of Betamethasone 17,21-Dipropionate (Rinderon DP® Ointment and Cream) for Eczematous Dermatitis. Skin Res. 1992; 34: 402-408. doi:10.11340/skinresearch1959.34.402.
- 45.Jungsuwadee P., Dekan G., Stingl G., Epstein M.M. Inhaled dexamethasone differentially attenuates disease relapse andestablished allergic asthma in mice. Clin Immunol. 2004;110:13–21. doi: 10.1016/j.clim.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 46.Papangkorn K., Truett K.R., Vitale A.T., Jhaveri C., Scales D.K., Foster C.S., et al. Novel dexamethasone sodium phosphate treatment (DSP-Visulex) for noninfectious anterior Uveitis: a randomized phase I/II clinical trial. Curr Eye Res. 2018;44:185–193. doi: 10.1080/02713683.2018.1540707. [DOI] [PubMed] [Google Scholar]
- 47.Sunaga Y., Kurosawa M., Nemoto T., Fueki R., Kobayashi S. A case of hydrocortisone sodium succinate-induced asthma. KITAKANTO Med J. 1985;35:565–570. doi: 10.2974/kmj1951.35.565. [DOI] [Google Scholar]
- 48.Searles G.E., DesGroseilliers J.P. Excipients in topical corticosteroid preparations in Canada. Can Med Assoc J. 1989;141:399–405. [PMC free article] [PubMed] [Google Scholar]
- 49.Ramsay R.E., Wilder B.J., Uthman B.M., Garnett W.R., Pellock J.M., Barkley G.L., et al. Intramuscular fosphenytoin (Cerebyx®) in patients requiring a loading dose of phenytoin. Epilepsy Res. 1997;28:181–187. doi: 10.1016/S0920-1211(97)00054-5. [DOI] [PubMed] [Google Scholar]
- 50.Johnson J., Wrenn K. Inappropriate fosphenytoin use in the ED. Am J Emer Med. 2001;19:293–294. doi: 10.1053/ajem.2001.24471. [DOI] [PubMed] [Google Scholar]
- 51.Cooke A., Anderson A., Buchanan K., Byford A., Gemmell D., Hamilton N., et al. Water-soluble propofol analogues with intravenous anaesthetic activity. Bioorg Med Chem Lett. 2001;11:927–930. doi: 10.1016/s0960-894x(01)00088-9. [DOI] [PubMed] [Google Scholar]
- 52.Bennett D.J., Anderson A., Buchanan K., Byford A., Cooke A., Gemmell D.K., et al. Novel water soluble 2,6-dimethoxyphenyl ester derivatives with intravenous anaesthetic activity. Bioorg Med Chem Lett. 2003;13:1971–1975. doi: 10.1016/S0960-894X(03)00346-9. [DOI] [PubMed] [Google Scholar]
- 53.Chidambaran V., Costandi A., D’Mello A. Propofol: a review of its role in pediatric anesthesia and sedation. CNS Druggs. 2015;29:543–563. doi: 10.1007/s40263-015-0259-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Turkbey B., Hoyt R.F., Agarwal H.K., Bernardo M., Sankineni S., Johnson L., et al. Magnetic resonance sentinel lymph node imaging of the prostate with gadofosveset trisodium–albumin: Preliminary Results in a Canine Model. Acad Radiol. 2015;22:646–652. doi: 10.1016/j.acra.2014.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Duan Y., Zhang S., Liu X. Study on pharmacokinetics methodology of S-(-)-ornidazol disodium phosphate. J Sou Uni (Med Sci Ed) 2011;02 [Google Scholar]
- 56.Brosa M., García D.M.X., Mora J., Villacampa A., Pozo T., Adán C., et al. Economic considerations on the use of mifamurtide in the treatment of osteosarcoma in Spain. Val Healt. 2014;17:A526–A527. doi: 10.1016/j.jval.2014.08.1662. [DOI] [PubMed] [Google Scholar]
- 57.Lynch R.J.M. Calcium glycerophosphate and caries: a review of the literature. Intern Dent J. 2010;54:310–314. doi: 10.1111/j.1875-595X.2004.tb00004.x. [DOI] [PubMed] [Google Scholar]
- 58.Chapman T.M., Plosker G.L., Perry C.M. Fosamprenavir: a review of its use in the management of antiretroviral therapy-naive patients with HIV infection. Drugs. 2004;64:2101–2124. doi: 10.2165/00003495-200464180-00014. [DOI] [PubMed] [Google Scholar]
- 59.Garvey E.P., Oplinger J.A., Tanoury G.J., Sherman P.A., Fowler M., Marshall S., et al. Potent and selective inhibition of human nitric oxide Synthases. Inhibition by non-amino acid isothioureas. J Bio Chem. 1994;269:26669–26676. [PubMed] [Google Scholar]
- 60.Vromen A., Southan S.G.J., Salzman A.L. Effects of S-isopropyl isothiourea, a potent inhibitor of nitric oxide synthase, in severe hemorrhagic shock. Am Physiol Soc. 1996;81:707–715. doi: 10.1152/jappl.1996.81.2.707. [DOI] [PubMed] [Google Scholar]
- 61.Petersen T.S., Kristensen S.G., Jeppesen J.V., Grøndahl M.L., Wissing M.L., Macklon K.T., et al. Distribution and function of 3′,5′-Cyclic-AMP phosphodiesterases in the human ovary. Mol Cel Endocrinol. 2015;403:10–20. doi: 10.1016/j.mce.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 62.Bucladesine Sodium Ye H. World Clin. Drugs. 1986;5 [Google Scholar]
- 63.Hosseini-Zare M.S., Salehi F., Seyedi S.Y., Azami K., Ghadiri T., Mobasseri M., et al. Effects of pentoxifylline and H-89 on epileptogenic activity of bucladesine in pentylenetetrazol-treated mice. Eur J Pharm. 2011;670:464–470. doi: 10.1016/j.ejphar.2011.09.026. [DOI] [PubMed] [Google Scholar]
- 64.Moreno M.D.J. Cognitive improvement in mild to moderate Alzheimer’s dementia after treatment with the acetylcholine precursor choline alfoscerate: a multicenter, double-blind, randomized, placebo-controlled trial. Excerpta Medica. 2002:178–193. doi: 10.1016/s0149-2918(03)90023-3. [DOI] [PubMed] [Google Scholar]
- 65.Nikonov V.V., Savitskaya I.B., Beletsky A.V. Choline alfoscerate in the treatment of acute ischemic stroke. Emerg Med. 2013;48:68–71. doi: 10.22141/2224-0586.1.48.2013.90391. [DOI] [Google Scholar]
- 66.Pardridge W.M. Blood-brain barrirer drug targeting: the future of brain drug development. Molec Inter. 2003;3:90–105. doi: 10.1124/mi.3.2.90. [DOI] [PubMed] [Google Scholar]
- 67.Pardridge W.M. Blood–brain barrier delivery. Drug Discov Today. 2007;12:54–61. doi: 10.1016/j.drudis.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 68.Di L., Kerns E.H., Carter G.T. Strategies to assess blood–brain barrier penetration. Expert Opin Drug Discov. 2008;3:677–687. doi: 10.1517/17460441.3.6.677. [DOI] [PubMed] [Google Scholar]
- 69.Anfuso C.D., Sipione S., Lupo G., Ragusa N., Alberghina M. Characterization of glycerophosphocholine phosphodiesterase activity and phosphatidylcholine biosynthesis in cultured retinal microcapillary pericytes. Effect of adenosine and endothelin-1. Lipids. 2003;38:45–52. doi: 10.1007/s11745-003-1030-z. [DOI] [PubMed] [Google Scholar]
- 70.Dechant K.L., Faulds D. Colfosceril palmitate—a review of the therapeutic efficacy and clinical tolerability of a synthetic surfactant preparation (Exosurf® NeonatalTM) in neonatal respiratory distress syndrome. Drugs. 1991;42:877–894. doi: 10.2165/00003495-199142050-00009. [DOI] [PubMed] [Google Scholar]
- 71.Kuwabara S., Nakazawa R., Azuma N., Suzuki M., Miyajima K., Fukutake T., et al. Intravenous methylcobalamin treatment for uremic and diabetic neuropathy in chronic hemodialysis patients. Intern Med. 1999;38:472–475. doi: 10.2169/internalmedicine.38.472. [DOI] [PubMed] [Google Scholar]
- 72.James S.J., Melnyk S., Fuchs G., Reid T., Jernigan S., Pavliv O., et al. Efficacy of methylcobalamin and folinic acid treatment on glutathione redox status in children with autism. Am J Clin Nutr. 2009;89:425–430. doi: 10.3945/ajcn.2008.26615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Garnock-Jones K.P. Fosaprepitant dimeglumine: a review in the prevention of nausea and vomiting associated with chemotherapy. Drugs. 2016;76:1365–1372. doi: 10.1007/s40265-016-0627-7. [DOI] [PubMed] [Google Scholar]
- 74.Barcelos R.P., Stefanello S.T., Mauriz J.L., González-Gallego J., Soares F.A.A. Creatine and the liver-metabolism and possible interactions. Mini-Rev Med Chem. 2016;16:12–18. doi: 10.2174/1389557515666150722102613. [DOI] [PubMed] [Google Scholar]
- 75.Green A.L., Hultman E., Macdonald I.A., Sewell D.A., Greenhaff P.L. Carbohydrate ingestion augments skeletal muscle creatine accumulation During creatine supplementation in humans. J Phoysiol. 1996:821–826. doi: 10.1152/ajpendo.1996.271.5.E821. [DOI] [PubMed] [Google Scholar]
- 76.Ma H, Jiang WR, Robledo N, Leveque V, Ali S, Lara-Jaime T, et al. Characterization of the metabolic activation of hepatitis c virus nucleoside inhibitor β-D-2′-Deoxy-2′-fluoro-2′-C-methylcytidine (PSI-6130) and identification of a novel active 5′-triphosphate species. J Bio Chem. 2007; 282: 29812-29820. doi: 10.1074/jbc.M705274200. [DOI] [PubMed]
- 77.Murakami E., Tolstykh T., Bao H., Niu C., Steuer H.M.M., Bao D., et al. Mechanism of activation of PSI-7851 and its diastereoisomer PSI-7977. J Bio Chem. 2010;285:34337–34347. doi: 10.1074/jbc.M110.161802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Do A., Mittal Y., Liapakis A., Cohen E., Chau H., Bertuccio C., et al. Drug authorization for sofosbuvir/ledipasvir (Harvoni) for chronic HCV infection in a real world cohort: a new barrier in the HCV care cascade. PLoS One. 2015;10 doi: 10.1371/journal.pone.0135645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Greig S.L. Sofosbuvir/velpatasvir: a review in chronic hepatitis C. Drugs. 2016;76:1567–1578. doi: 10.1007/s40265-016-0648-2. [DOI] [PubMed] [Google Scholar]
- 80.Heo Y.A., Deeks E.D. Sofosbuvir/velpatasvir/voxilaprevir: a review in chronic hepatitis C. Drugs. 2018;78:577–587. doi: 10.1007/s40265-018-0895-5. [DOI] [PubMed] [Google Scholar]
- 81.Ikeda Y., Ban J., Ishikawa T., Hashiguchi S., Urayama S., Horibe H. Stability and stabilization studies of TAK-599 (ceftaroline fosamil), a novel N-phosphono type prodrug of anti-methicillin resistant Staphylococcus aureus cephalosporin T-91825. Chem Pharm Bull. 2008;56:1406–1411. doi: 10.1248/cpb.56.1406. [DOI] [PubMed] [Google Scholar]
- 82.Griskevicius L., Yasar Ü., Sandberg M., Hidestrand M., Eliasson E., Tybring G., et al. Bioactivation of cyclophosphamide: the role of polymorphic CYP2C enzymes. Eur J Clin Pharmacol. 2003;59:103–109. doi: 10.1007/s00228-003-0590-6. [DOI] [PubMed] [Google Scholar]
- 83.Foye L.V., Chapman C.G., Willett F.M., Adams W.S. Cyclophosphamide: A preliminary study of a new alkylating agent. Arch Intern Med. 1960;106:365–367. doi: 10.1001/archinte.1960.03820030053009. [DOI] [PubMed] [Google Scholar]
- 84.Hall A.G., Tilby M.J. Mechanisms of action of, and modes of resistance to, alkylating agents used in the treatment of haematological malignancies. Blood Rev. 1992;6:163–173. doi: 10.1016/0268-960x(92)90028-o. [DOI] [PubMed] [Google Scholar]
- 85.Kohn F.R., Sladek N.E. Aldehyde dehydrogenase activity as the basis for the relative insensitivity of murine pluripotent hematopoietic stem cells to oxazaphosphorines. Biochem Pharm. 1985;34:3465–3471. doi: 10.1016/0006-2952(85)90719-1. [DOI] [PubMed] [Google Scholar]
- 86.Immonen K., Finne P., Grönhangen-riska C., Pettersson T., Klaukka T., Kautiainen H., et al. A marked decline in the incidence of renal replacement therapy for amyloidosis associated with inflammatory rheumatic diseases - data from nationwide registries in Finland. Amyloid. 2011;18:25–28. doi: 10.3109/13506129.2010.549252. [DOI] [PubMed] [Google Scholar]
- 87.Sistigu A., Viaud S., Chaput N., Bracci L., Proietti E., Zitvogel L. Immunomodulatory effects of cyclophosphamide and implementations for vaccine design. Semin Immunopathol. 2011;33:369–383. doi: 10.1007/s00281-011-0245-0. [DOI] [PubMed] [Google Scholar]
- 88.Dellapasqua S., Bertolini F., Bagnardi V., Campagnoli E., Scarano E., Torrisi R., et al. Metronomic cyclophosphamide and capecitabine combined with bevacizumab in advanced breast cancer. J Clin Oncol. 2008;26:4899–4905. doi: 10.1200/JCO.2008.17.4789. [DOI] [PubMed] [Google Scholar]
- 89.Pagnoux C. Updates in ANCA-associated vasculitis. Eur J Rheumatol. 2016;3:122–133. doi: 10.5152/eurjrheum.2015.0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jahnke K., Thiel E., Bechrakis N.E., Willerding G., Kraemer D.F., Fischer L., et al. Ifosfamide or trofosfamide in patients with intraocular lymphoma. J Neurooncol. 2009;93:213–217. doi: 10.1007/s11060-008-9761-8. [DOI] [PubMed] [Google Scholar]
- 91.Ciuleanu T.E., Pavlovsky A.V., Bodoky G., Garin A.M., Langmuir V.K., Kroll S., et al. A randomised phase III trial of glufosfamide compared with best supportive care in metastatic pancreatic adenocarcinoma previously treated with gemcitabine. Eur J Cancer. 2009;45:1589–1596. doi: 10.1016/j.ejca.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 92.Lacombe D. Glufosfamide: can we Improve the process of anticancer agent development. Exp Op Invest Drugs. 2012;21:749–754. doi: 10.1517/13543784.2012.670218. [DOI] [PubMed] [Google Scholar]
- 93.Sun Y. Clinical phase II trial of a new antineoplastic drug - glyciphosphoramide. Clinical Trial. 1984;6 273–26. [PubMed] [Google Scholar]
- 94.Juan L., Hong Z., Xun Z., Chen L., Qiang Y., Shu L., et al. Influence of zhuqin formula extract on the cellular and humoral immune response in cyclophosphamide-immunocompromised mice. J Anim Plant Sci. 2015;25:1335–1343. [Google Scholar]
- 95.McCarty G.W., Bremner J.M., Lee J.S. Inhibition of plant and microbial ureases by phosphoroamides. Plant and Soil. 1990;127:269–283. doi: 10.1007/BF00014435. [DOI] [Google Scholar]
- 96.Martens D.A., Bremner J.M. Effectiveness of phosphoroamides for retardation of urea hydrolysis in soils. Soil Sci Soc Am J. 1984;48:302–305. doi: 10.2136/sssaj1984.0361599500480002001. [DOI] [Google Scholar]
- 97.Ohta T., Shibata H., Kawamori T., Iimuro M., Sugimura T., Wakabayashi K. Marked reduction of helicobacter pylori-induced gastritis by urease inhibitors, acetohydroxamic acid and flurofamide, in mongolian gerbils. Biochem Biophys Res Commun. 2001;285:728–733. doi: 10.1006/bbrc.2001.5229. [DOI] [PubMed] [Google Scholar]
- 98.William E., James C. Tenofovir alafenamide tablets (Vemlidy) Intern Med Alert. 2017;39:3. [Google Scholar]
- 99.Clercq E.D. Tenofovir alafenamide (TAF) as the successor of tenofovir disoproxil fumarate (TDF) Biochem Pharma. 2016;119:1–7. doi: 10.1016/j.bcp.2016.04.015. [DOI] [PubMed] [Google Scholar]
- 100.Clercq E.D. Tenofovir at the crossroad of the therapy and prophylaxis of HIV and HBV infections. J Cell Immunol. 2020;2:23–30. https://doi.org/ [Google Scholar]
- 101.Deeks E.D. Darunavir/cobicistat/emtricitabine/tenofovir alafenamide: a review in HIV-1 infection. Drugs. 2018;78:1013–1024. doi: 10.1007/s40265-018-0934-2. [DOI] [PubMed] [Google Scholar]
- 102.Puziy A.M., Poddubnaya O.I., Gawdzik B., Tascón J.M.D. Phosphorus-containing carbons: preparation, properties and utilization. Carbon. 2020;157:796–846. doi: 10.1016/j.carbon.2019.10.018. [DOI] [Google Scholar]
- 103.Minor J.R., Baltz J.K. Foscarnet sodium. DICP. 1991;25:41–47. doi: 10.1177/106002809102500109. [DOI] [PubMed] [Google Scholar]
- 104.Clercq E.D. Antiviral drugs: current state of the art. J Clin Virol. 2001;22:73–89. doi: 10.1016/S1386-6532(01)00167-6. [DOI] [PubMed] [Google Scholar]
- 105.Canestri A., Ghosn J., Wirden M., Marguet F., Ktorza N., Boubezari I., et al. Foscarnet salvage therapy for patients with late-stage HIV disease and multiple drug resistance. Antivir Ther. 2006;11:561–566. [PubMed] [Google Scholar]
- 106.Meyer P.R., Rutvisuttinunt W., Matsuura S.E., So A.G., Scott W.A. Stable complexes formed by HIV-1 reverse transcriptase at distinct positions on the primer-template controlled by binding deoxynucleoside triphosphates or foscarnet. J Mol Biol. 2007;369:41–54. doi: 10.1016/j.jmb.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Nordgren I., Bengtsson E., Holmstedt B., Pettersson B.M. Levels of metrifonate and dichlorvos in plasma and erythrocytes during treatment of schistosomiasis with Bilarcil®. Acta Pharmacol Toxicol. 2009;49:79–86. doi: 10.1111/j.1600-0773.1981.tb03256.x. [DOI] [PubMed] [Google Scholar]
- 108.Bakes D., Karalliedde L., Murray V., Maynard R.L., Parkinson N.H.T. 2nd ed. Oxford Unviersity Press; Health Protection Agency, Oxford: 2012. Essentials of Toxicology of Health Protection: A Handbook for Field Professionals; pp. 192–194. 9780199652549. [Google Scholar]
- 109.Khomutov R.M., Osipova T.I., Khurs E.N., Dzhavakhiya V.G. Synthesis of alafosfalin and its phosphinic analogue and their fungicidal activity. Mendeleev Commun. 2008;18:295–296. doi: 10.1016/j.mencom.2008.11.001. [DOI] [Google Scholar]
- 110.Atherton F.R., Hassall C.H., Lambert R.W. Synthesis and Structure-activity relationships of antibacterial phosphonopeptides incorporating (1-aminoethyl) phosphonic acid and (aminomethyl) phosphonic acid. J Med Chem. 1986;29:29–40. doi: 10.1021/jm00151a005. [DOI] [PubMed] [Google Scholar]
- 111.Reddy K.R., Matelich M.C., Ugarkar B.G., Gómez-Galeno J.E., DaRe J., Ollis K., et al. Pradefovir: a prodrug that targets adefovir to the liver for the treatment of hepatitis B. J Med Chem. 2008;51:666–676. doi: 10.1021/jm7012216. [DOI] [PubMed] [Google Scholar]
- 112.Lu L., Yip B., Trinh H., Pan C.Q., Han S.H.B., Wong C.C., et al. Tenofovir-based alternate therapies for chronic hepatitis B patients with partial virological response to entecavir. J Viral Hepat. 2015;22:675–681. doi: 10.1111/jvh.12368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Martin P., Lau D.T., Nguyen M.H., Janssen H.L.A., Dieterich D.T., Peters M.G., et al. A treatment algorithm for the management of chronic Hepatitis B virus infection in the United States: 2015 update. Clin Gastroenterol Hepatol. 2015;13:2071–2087. doi: 10.1016/j.cgh.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 114.Clercq E.D., Holý A., Rosenberg I., Sakuma T., Balzarni J., Maudgal P.C. A novel selective broad-spectrum anti-DNA virus agent. Nature. 1986;323:464–467. doi: 10.1038/323464a0. [DOI] [PubMed] [Google Scholar]
- 115.Metcalf W.W., Donk W.A. Biosynthesis of phosphonic and phosphinic acid natural products. Annu Rev Biochem. 2009;78:65–94. doi: 10.1146/annurev.biochem.78.091707.100215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Brown E.D., Vivas E.I., Wslsh C.T., Kolter R. MurA (MurZ), the enzyme that catalyzes the first committed step in peptidoglycan biosynthesis, is essential in Escherichia coli. J Bacteriol. 1995;177:4194–4197. doi: 10.1128/jb.177.14.4194-4197.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zhu JY, Yang Y, Han H, Betzi S, Olesen SH, Marsilio F, et al. Enzymology: functional consequence of covalent reaction of phosphoenolpyruvate with UDP-N-acetylglucosamine 1-carboxyvinyltransferase (MurA). J Bio Chem. 2012; 287: 12657-12667. doi:10.1074/jbc.M112.342725. [DOI] [PMC free article] [PubMed]
- 118.Falagas M.E., Vouloumanou E.K., Samonis G., Vardakas K.Z. Fosfomycin. Clin Microbiol Rev. 2016;29:321–347. doi: 10.1128/CMR.00068-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Tsuruoka T. Clinical pharmacology of fosfomycin sodium. Antibiot Chemother. 1996;12:85–93. [Google Scholar]
- 120.Santoro A., Cappello A.R., Madeo M., Martello E., Iacopetta D., Dolce V. Interaction of fosfomycin with the glycerol 3-phosphate transporter of Escherichia coli. Biochimica et Biophysica Acta (BBA) 2011;1810:1323–1329. doi: 10.1016/j.bbagen.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 121.Patel S.S., Balfour J.A., Bryson H.M. Fosfomycin tromethamine. a review of its antibacterial activity, pharmacokinetic properties and therapeutic efficacy as a single-dose oral treatment for acute uncomplicated lower urinary tract infections. Drugs. 1997;53:637–656. doi: 10.2165/00003495-199753040-00007. [DOI] [PubMed] [Google Scholar]
- 122.García-Rodríguez J.A., Martín I.T., Baquero F., Cisterna R., Gobernado M., Liñares F., et al. In vitro activity of fosfomycin trometamol against pathogens from urinary tract infections: a Spanish multicenter study. J Chemo. 1997;9:394–402. doi: 10.1179/joc.1997.9.6.394. [DOI] [PubMed] [Google Scholar]
- 123.Yoshino K., Kohno T., Uno T., Morita T., Tsukamoto G. Organic phosphorus compounds 1.4-(Benzothiazol-2-yl) benzylphosphonate as potent calcium antagonistic vasodilator. J Med Chem. 1986;29:820–825. doi: 10.1021/jm00155a037. [DOI] [PubMed] [Google Scholar]
- 124.Pilote L., Abrahamowicz M., Eisenberg M., Humphries K., Behlouli H., Tu J.V. Effect of different angiotensin-converting-enzyme inhibitors on mortality among elderly patients with congestive heart failure. Can Med Assoc J. 2008;178:1303–1311. doi: 10.1503/cmaj.060068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Greenbaum R., Zucchelli P., Caspi A., Nouriel H., Paz R., Sclarovsky S., et al. Comparison of the pharmacokinetics of fosinoprilat with enalaprilat and lisinopril in patients with congestive heart failure and chronic renal insufficiency. Br J Clin Pharmacol. 2000;49:23–31. doi: 10.1046/j.1365-2125.2000.00103.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Duchin K.L., Waclawki A.P., Tu J.I., Manning J., Frantz M., Willard D.A. Pharmacokinetics, safety, and pharmacologic effects of fosinopril sodium, an angiotensin-converting enzyme inhibitor in healthy subjects. J Clin Pharmacol. 1991;31:58–64. doi: 10.1002/j.1552-4604.1991.tb01887.x. [DOI] [PubMed] [Google Scholar]
- 127.Boers-Doets C.B., Raber-Durlacher J.E., Treister N.S., Epstein J.B., Arends A.B., Wiersma D.R., et al. Mammalian target of rapamycin inhibitor-associated stomatitis. Future Oncol. 2013;9:1883–1892. doi: 10.2217/fon.13.141. [DOI] [PubMed] [Google Scholar]
- 128.Saintonge D.M.C., Vere D.W., Sharman V.L. Activity of fosazepam, a soluble analogue of diazepam. Br J Clin Pharmacol. 1976:494–496. doi: 10.1111/j.1365-2125.1977.tb00773.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Tan K.R., Rudolph U., Lüscher C. Hooked on benzodiazepines: GABAA receptor subtypes and addiction. Trends Neurosci. 2011;34:188–197. doi: 10.1016/j.tins.2011.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Huang W., Liu S., Zou D., Thomas M., Wang Y., Zhou T., et al. Discovery of brigatinib (AP26113), a phosphine oxide-containing, potent, orally active inhibitor of anaplastic lymphoma kinase. J Med Chem. 2016;59:4948–4964. doi: 10.1021/acs.jmedchem.6b00306. [DOI] [PubMed] [Google Scholar]
- 131.Sequist L.V., Waltman B.A., Dias-Santagata D., Digumarthy S., Turke A.B., Fidias P., et al. Genotypic and histological evolution of lung cancers Acquiring resistance to EGFR inhibitors. Sci Transl Med. 2011;3:75ra26. doi: 10.1126/scitranslmed.3002003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Lembeck F, Sewing K. Pharmacological Facts and Figures. 1st ed.. Springer-Verlag Berlin. Heidelberg. 1969; ISBN-13: 9780387900100. doi:10.1007/978-1-4684-6243-2.
- 133.Kanski J.J. Miotics. Br J Ophthalmol. 1968;52:936–937. doi: 10.1136/bjo.52.12.936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Gabelt B’.A.T., Hennes E.A., Seeman J.L., Tian B., Kaufman P.L. H-7 Effect on outflow facility after trabecular obstruction following long-term echothiophate treatment in monkeys. Invest Ophthalmol Vis Sci. 2004;45:2732–2736. doi: 10.1167/iovs.04-0083. [DOI] [PubMed] [Google Scholar]
- 135.Kouvaris J.R., Kouloulias V.E., Vlahos L.J. Amifostine: the first selective-target and broad-spectrum radioprotector. Oncologist. 2007;12:738–747. doi: 10.1634/theoncologist.12-6-738. [DOI] [PubMed] [Google Scholar]
- 136.Drake M.T., Clarke B.L., Khosla S. Bisphosphonates: mechanism of action and role in clinical practice. Mayo Clin Proc. 2008;83:1032–1045. doi: 10.4065/83.9.1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Chhipa N.M.R., Sen D.J. Aminobiphosphonates in osteoporosis: a review. Int J Drug Dev & Res. 2013;5:120–132. [Google Scholar]
- 138.Frith J.C., Mönkkönen J., Blackburn G.M., Russell R.G.G., Rogers M.J. Clodronate and liposome-encapsulated clodronate are metabolized to a toxic ATP analog, adenosine 5′- (β, γ-dichloromethylene) triphosphate, by mammalian cells in vitro. J Bone Miner Res. 1997;12:1358–1367. doi: 10.1359/jbmr.1997.12.9.1358. [DOI] [PubMed] [Google Scholar]
- 139.Brown J.P., Morin S., Leslie W., Papaioannou A., Cheung A.M., Davison K.S., et al. Bisphosphonates for treatment of osteoporosis: expected benefits, potential harms, and Drug Holidays. Can Fam Physician. 2014;60:324–333. [PMC free article] [PubMed] [Google Scholar]
- 140.Kanis J.A., Evanson J.M., Russell R.G.G. Paget’s bloom of bone : diagnosis and management. Metab Bone Dis & Rel Res. 1981;3:219–230. doi: 10.1016/0221-8747(81)90036-9. [DOI] [PubMed] [Google Scholar]
- 141.Ala-Houhala I., Saha H., Liukko-Sipi S., Ylitalo P., Pasternack A. Pharmacokinetics of clodronate in haemodialysis patients. Nephrol Dial Transplant. 1999;14:699–705. doi: 10.1093/ndt/14.3.699. [DOI] [PubMed] [Google Scholar]
- 142.Pennanen N., Lapinjoki S., Urtti A., Mönkkönen J. MonEffect of liposomal and free bisphosphonates on the IL-1β, IL-6 and TNFα secretion from RAW 264 cells in vitro. Pharm Res. 1995;12:916–922. doi: 10.1023/a:1016281608773. [DOI] [PubMed] [Google Scholar]
- 143.Arlov Ø., Öztürk E., Steinwachs M., Skjåki-Bræk G., Zenobi-Wong M. Biomimetic sulphated alginate hydrogels suppress IL-1B-induced inflammatory responses in human chondrocytes. Eur Cells Mater. 2017;33:76–89. doi: 10.22203/eCM.v033a06. [DOI] [PubMed] [Google Scholar]
- 144.Denoix J.M., Thibaud D., Riccio B. Tiludronate as a new therapeutic agent in the treatment of navicular disease: a double-blind placebo-controlled clinical trial. Equine Vet J. 2003;35:407–413. doi: 10.2746/042516403776014226. [DOI] [PubMed] [Google Scholar]
- 145.Biersack H.J., Palmedo H., Andris A., Rogenhofer S., Knapp F.F., Guhlke S., et al. Palliation and survival after repeated 188Re-HEDP therapy of hormone-refractory bone metastases of prostate cancer: a retrospective analysis. J Nuc Med. 2011;52:1721–1726. doi: 10.2967/jnumed.111.093674. [DOI] [PubMed] [Google Scholar]
- 146.Beek E.V., löwik C., Pluijm G.D., Papapoulos S. The role of geranylgeranylation in bone resorption and its suppression by bisphosphonates in fetal bone explants in vitro: a clue to the mechanism of action of nitrogen-containing bisphosphonates. J Bone Min Res. 1999;14:722–729. doi: 10.1359/jbmr.1999.14.5.722. [DOI] [PubMed] [Google Scholar]
- 147.Kavanagh K.L., Guo K., Dunford J.E., Wu X., Knapp S., Ebetino F.H., et al. The molecular mechanism of nitrogen-containing bisphosphonates as antiosteoporosis drugs. Pro Natl Acad Sci U S A. 2006;103:7829–7834. doi: 10.1073/pnas.0601643103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Baas T. Rebuilding a better bone. Sci-Bus eXchange. 2012;5:194. doi: 10.1038/scibx.2012.194. [DOI] [Google Scholar]
- 149.Gatti D., Viapiana O., Idolazzi L., Fracassi E., Adami S. Neridronic acid for the treatment of bone metabolic diseases. Expert Opin Drug Metab Toxicol. 2009;5:1305–1311. doi: 10.1517/17425250903029190. [DOI] [PubMed] [Google Scholar]
- 150.Otto S. Springer-Verlag; Berlin Heidelberg: 2015. Medication-related Osteonecrosis of the Jaws. Bisphosphonates, Denosumab, and New Agents; pp. 207–215. ISBN. _20. [DOI] [Google Scholar]
- 151.Sugisaki M. Clinical coping with bisphosphonate-induced osteonecrosis of the jaws. Tokyo Jikeikai Med J. 2011;126:59–70. [Google Scholar]
- 152.PMDA Releases updates for levetiracetam. Bisphosphonates Scholar J. 2016;4 [Google Scholar]
- 153.Min B., Song K., Bae K., Cho C., Son E., Lee K. Nonsurgical treatment strategies after osteoporotic hip fractures. Hip Pelvis. 2015;27:9–16. doi: 10.5371/hp.2015.27.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Chaplin S., Dennison E. Zoledronic acid: a once-yearly injection for osteoporosis. Prescriber. 2008;19:40–44. doi: 10.1002/psb.254. [DOI] [Google Scholar]
- 155.Kimoto A., Tanaka M., Nozaki K., Mori M., Fukushima S., Mori H., et al. Intermittent minodronic acid treatment with sufficient bone resorption inhibition prevents reduction in bone mass and strength in ovariectomized rats with established osteopenia comparable with daily treatment. Bone. 2013;55:189–197. doi: 10.1016/j.bone.2013.02.013. [DOI] [PubMed] [Google Scholar]
- 156.Pratt R.D., Swinkels D.W., Ikizler T.A., Gupta A. Pharmacokinetics of ferric pyrophosphate citrate, a novel iron salt, administered intravenously to healthy volunteers. J Clin Pharmacol. 2016;57:312–320. doi: 10.1002/jcph.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Fishbane S.N., Singh A.K., Cournoyer S.H., Jindal K.K., Fanti P., Guess C.D., et al. Ferric pyrophosphate citrate (TrifericTM) administration via the dialysate maintains hemoglobin and iron balance in chronic hemodialysis patients. Nephrol Dial Transplant. 2015;30:2019–2026. doi: 10.1093/ndt/gfv277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Jordan F. Semiempirical calculations on the electronic structure and preferred conformation of thiamine (vitamin b1) and thiamine pyrophosphate (cocarboxylase) J Am Chem Soc. 1974;96:3623–3630. doi: 10.1021/ja00818a041. [DOI] [PubMed] [Google Scholar]
- 159.Ames T.D., Sharik M.E. Rather GM, Hochart G, Bonnel D, Linehan S, et al. Translational research of PT-112, a clinical agent in advanced phase i development: evident bone tropism, synergy in vitro with Bortezomib and lenalidomide, and potent efficacy in the Vk*MYC mouse model of multiple myeloma. Blood. 2017;130:1797. doi: 10.1182/blood.V130.Suppl_1.1797.1797. [DOI] [Google Scholar]
- 160.Secades JJ. Citicoline: Pharmacological and Clinical Review, 2010 Update. Rev Neurol. 2011; 52: S1-S62. doi:10.33588/rn.52S02.2010787. [PubMed]
- 161.Roberti G., Tanga L., Michelessi M., Quaranta L., Parisi V., Manni G., et al. Cytidine 51-diphosphocholine (citicoline) in glaucoma: rationale of its use, current evidence and future perspectives. Int J Mol Sci. 2015;16:28401–28417. doi: 10.3390/ijms161226099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Baile M., Giancaspero T., Brizio C., Panebianco C., Indiveri C., Galliccio M., et al. Biosynthesis of flavin cofactors in man: implications in health and disease. Curr Pharm Des. 2013;19:2649–2675. doi: 10.2174/1381612811319140014. [DOI] [PubMed] [Google Scholar]
- 163.Keating G.M. Cangrelor: a review in percutaneous coronary intervention. Drugs. 2015;75:1425–1434. doi: 10.1007/s40265-015-0445-3. [DOI] [PubMed] [Google Scholar]
- 164.Angiolillo D.J., Capranzano P. Pharmacology of emerging novel platelet inhibitors. Am Heart J. 2008;156:10–15. doi: 10.1016/j.ahj.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 165.Pendergast W., Yerxa B.R., Douglass J.G., Shaver S.R., Dougherty R.W., Redick C.C., et al. Synthesis and P2Y receptor activity of a series of uridine dinucleoside 5’-polyphosphates. Bioorg Med Chem Lett. 2000;11:157–160. doi: 10.1016/s0960-894x(00)00612-0. [DOI] [PubMed] [Google Scholar]
- 166.Fingert H.J., Pu A.T., Chen Z., Googe P.B., Alley M.C., Pardee A.B. In vivo and in vitro enhanced antitumor effects by pentoxifylline in human cancer cells treated with thiotepa. Cancer Res. 1988;48:4375–4381. [PubMed] [Google Scholar]
- 167.Kaldor J.M., Day N.E., Kittelmann B., Pettersson F., Langmark F., Pedersen D., et al. Bladder tumours following chemotherapy and radiotherapy for ovarian cancer: a case–control study. Int J Cancer. 1995;63:1–6. doi: 10.1002/ijc.2910630102. [DOI] [PubMed] [Google Scholar]
- 168.Gao J., Yoon K., Frisbie R.K., Coles G.C., Clark J.M. Esterase-mediated malathion resistance in the human head louse, Pediculus capitis (Anoplura: Pediculidae) Pestic Biochem Physiol. 2006;85:28–37. doi: 10.1016/j.pestbp.2005.09.003. [DOI] [Google Scholar]
- 169.Kean W.F., Hart L., Buchanan W.W. Disease-modifying drugs series Editor: T. Pullar-Auranofin. Brit J Rheumatol. 1997;36:560–572. doi: 10.1093/rheumatology/36.5.560. [DOI] [PubMed] [Google Scholar]
- 170.Marzo T., Messori L. A Role for metal-based drugs in fighting COVID-19 infection? The case of auranofin. ACS Med Chem Lett. 2020;11:1067–1068. doi: 10.1021/acsmedchemlett.0c00190. [DOI] [PMC free article] [PubMed] [Google Scholar]


