Highlights
-
•
This study was conducted in a nationally representative community sample.
-
•
Mental disorders were diagnosed using standardized diagnostic interview instruments.
-
•
Suicide risk persistently elevated for bipolar disorders.
-
•
Suicide risk declined over time for other mental disorders studied.
Keywords: Mental disorders; Major depressive disorders; Bipolar disorders; Anxiety disorders; Substance dependent, Suicide
Abstract
Objective
: This study examined the patterns of association between mental disorders and subsequent suicide in a community sample representative of the Canadian household population.
Methods
: This retrospective cohort study used data from the Canadian Community Health Survey 2002 linked to the Death Database 2000-2011 and the Hospitalization Database 1999/2000-2012/2013) (n=27,000). Mental disorders (past year major depressive episodes (MDE), bipolar disorders (BPD), anxiety disorders (AD), and substance dependence (SD)) and subsequent suicide events (deaths or hospitalizations for suicide attempts) were identified. Competing risk regression models were used to analyze the time-to-event data, adjusting for age, sex, marital status, and educational attainment.
Results
: Past year mental disorders were diagnosed in 11.38% of the cohort and 0.41% had suicide events. An increased hazard of suicide events associated with MDE, SD and AD weakened over-time, but this was not observed for BPD. For example, the HR of suicide events for MDE was 6.02 (95% confidence interval (CI)=2.65, 13.68) in the first 4 years, whereas, it was 2.03 (95% CI=0.91, 4.53) after 4 years. Whereas, the HRs of suicide events for BPD were 16.95 (95% CI=6.88, 41.75) and 15.81 (95% CI=5.89, 42.45) before and after 4 years.
Limitations
: Diagnostic data are likely to underestimate the prevalence of suicide events.
Conclusions
: The risk of suicide events declined over time for MDE, SA and AD, but remained high for BPD. This may reflect improvement over time in MDE, SA and AD, but indicates that people living with BPD have a persistent elevated hazard of suicide events.
1. Background
Suicide, a preventable cause of death, is the 10th leading cause of death worldwide (World Health Organization, 2014). Every 40 seconds a person dies by suicide in the world, which represents a worldwide suicide rate of 11.4 per 100,000 population (World Health Organization, 2014). In Canada, it is the 9th leading cause of death for the overall population and 2nd leading cause of death for young adults (Government of Canada, 2020). Currently, an average of 10 people die due to suicide each day in Canada (Government of Canada, 2020), representing 10.3 suicide deaths per 100,000 population (Statisitics Canada, 2020a). These estimates are likely to be even higher as suicide cases are likely to be under-reported. As suicide often affects young people, it makes a large contribution to years of potential life lost. Additionally, the repetition of suicidal behaviors is common (Government of Canada, 2020; Carroll et al., 2014; Kapur et al., 2006). Most suicidal deaths are associated with past suicidal behaviors involving suicidal ideation, suicide attempts, self-harm, and suicide-related hospitalizations (Government of Canada, 2020). Overall, suicide leads not only to the loss of individual life, but is also a burdensome issue for affected families, and for society as a whole. Therefore, suicide is a serious public health problem and it warrants public health attention for its prevention. An important step for development and refinement of preventative public health interventions for suicide is to establish its risk factors, specifically modifiable risk factors such as mental disorders.
Evidence exists for an association between mental disorders (such as major depressive disorders (MDE), bipolar disorder (BPD), substance dependence (SD), and anxiety disorders (SD)) and subsequent suicidality (including suicidal thoughts and attempts) and deaths by suicide (Gili et al., 2019; Harris and Barraclough, 1997; Nock et al., 2009; Nock et al., 2010; Too et al., 2019; Weissman et al., 1989). To illustrate, numerous studies including systematic reviews have reported that suicidal behaviors and deaths are common among those with mental disorders (Gili et al., 2019; Harris and Barraclough, 1997; Nock et al., 2009; Nock et al., 2010; Too et al., 2019; Weissman et al., 1989). More than 90% of people that attempted suicide or died by suicide were found to have one or more mental disorders in studies based on clinical samples (Arsenault-Lapierre et al., 2004; Cavanagh et al., 2003; Wunderlich et al., 1998). A recent systematic review conducted by Too, et al found the pooled risk ratio of suicide was 7.5 (95% CI= 6.6, 8.6) and the population attributable risk of suicide up to 21% for mental disorder (Too et al., 2019). However, these findings vary by the study sample (general vs clinical population), the mental disorders (single mental disorders and comorbid mental disorders) and the suicide outcomes (ideation, attempt, and death) (Bostwick and Pankratz, 2000; Harris and Barraclough, 1997; Nock et al., 2009; Nock et al., 2010; Too et al., 2019; Weissman et al., 1989; Wunderlich et al., 1998).
Existing evidence on the relationship between mental disorders and suicide is predominantly based on the psychological autopsy, cross-sectional study design, and clinical samples admitted to psychiatric hospitals utilizing mental health services (Bertolote et al., 2003; Borges et al., 2010; Bostwick and Pankratz, 2000; Cavanagh et al., 2003; Harris and Barraclough, 1997; Nock et al., 2010; Weissman et al., 1989). Studies that were conducted in clinical patients or that used cross-sectional study designs or psychological autopsy methods are vulnerable to biases and may have limited generalizability. For example, psychological autopsy studies potentially introduce recall bias as they retrospectively obtain information on mental disorders and suicidal behaviours of those who died by suicide through structured interviews with individuals who were close to them. Studies based on clinical samples are vulnerable to selection bias since they over-represent people with more severe illness, and suicidal ideation or risk is a common reason for admission to clinical services. Studies that assess mental disorders (as exposures) in a community-based sample and prospectively measure suicide (as outcome) with several years of follow up are needed to obtain valid estimates of the strength of association between mental disorders and suicide. Furthermore, to our knowledge, there are no such studies that have examined the characteristics of the relationship between mental disorders and suicide, particularly, suicide risk patterns over time. This current study examined the patterns of association between mental disorders and suicide events in a nationally representative sample of the Canadian household population.
2. Methods
2.1. Data sources
This is a retrospective cohort study that used data from the Canadian Community Health Survey (CCHS) cycle 1.2 (conducted in 2002) linked to the death data from the Canadian Vital Statistics Death Database (CVSD) 2000 to 2011, and hospitalization data from the Discharge Abstract Database (DAD), fiscal years 1999/2000 to 2012/2013. In Canada, health care is a provincial responsibility, and almost all hospitalizations occur in public hospitals. These hospitals submit data to the provincial government for reasons of remuneration, and all provinces except Quebec submit their data to a national registry maintained by the Canadian Institute for Health Information.
Briefly, the CCHS cycle 1.2 was a content focus survey on mental health and was conducted between June 2002 and December 2002 in a sample of approximately 37,000 individuals who were representative of the Canadian household population living in the 10 Canadian provinces. People who are institutionalized, full time members of the armed forces or residents of reserves and other Indigenous settlements are outside of the target population. These exclusions represent approximately 3% of the national population. Detailed information on this survey, including response rates, questionnaires, survey methodology, and data accuracy are available on the Statistics Canada website (Statisitics Canada, 2020b). As part of its record linkage initiatives, Statistics Canada linked the CCHS survey data to the CVSD 2000 to 2011 on December 31, 2011, and the DAD (fiscal year 1999/2000 to 2012/2013), housed at the Canadian Institute for Health Information. The record linkage collected mortality data from CVSD, including a death date and reported International Classification of Diseases Tenth Revision, Canadian Modification (ICD-10-CA) codes for the underlying causes of death, and hospitalization data from DAD, including hospitalization dates and reported ICD-9-CA and ICD-10-CA codes for 25 diagnoses. A detailed description of data linkage procedures and its quality assessment has been reported elsewhere (Sanmartin et al., 2016). The data were accessed through and analyzed at the Prairie Regional Data Centre, located at the University of Calgary. Ethics approval was not applicable as the University of Calgary does not require ethics review for secondary data analysis using Statistics Canada data.
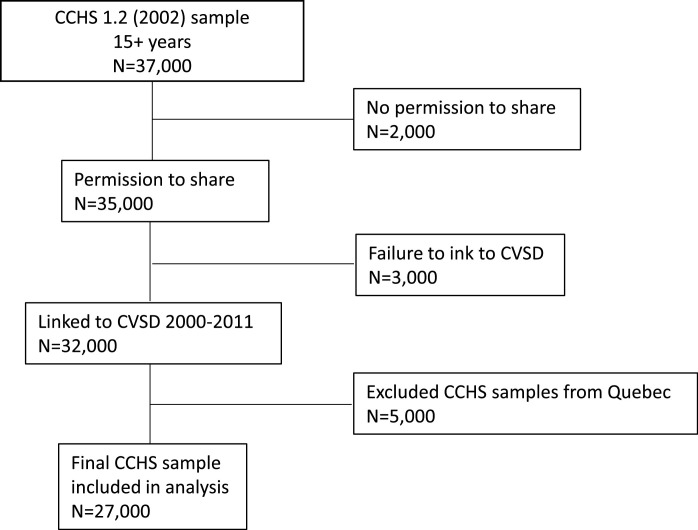
As shown in Figure 1 , out of 37,000 CCHS 2002 respondents, 35,000 respondents (approximately 90%) consented to have their survey data linked with other administrative data sources, including the CVSD and the DAD, at the time of their participation in the survey. Among those who providing consent for linkage, 32,000 survey respondents were successfully linked (using a probabilistic linkage conducted by Statistics Canada) to CVSD on December 31, 2011. As the DAD does not include hospitalization data from Quebec, this study excluded survey respondents from Quebec, leading to n= 27,000 being analyzed. These numbers were rounded as required by Statistics Canada's data release guidelines.
Fig. 1.
Flow diagram for data linkage CCHS 1.2 Sample (estimates are rounded in keeping with Statistics Canada data release guidelines)
CCHS: Canadian Community Health Survey; CVSD: Canadian Vital Statistics Database; DAD: Discharge Abstract Database
CCHS samples from Quebec province were excluded as DAD does not include hospitalization data from Quebec
2.2. Measures
Suicide events were defined as the first occurrence of hospitalization for suicide attempt or death due to suicide, a composite variable. Hospitalizations for suicide attempts were identified using ICD-9-CA (E950-E959) and ICD-10-CA (X60–X84, Y87.0) codes for intentional self-harm from the DAD (Statistics Canada, 2005). Both ICD-9-CA and ICD-10-CA codes were used as not all provinces fully transitioned to ICD-10 until 2004/05. Deaths due to suicide were identified using ICD-10-CA codes for intentional self-harm (X60–X84, Y87.0) from the CVSD (Statistics Canada, 2005). Past 12 months mental disorders – major depressive episodes (MDE), bipolar disorders (BPD), anxiety disorders (AD: includes panic anxiety disorder, social phobia, and agoraphobia), and substance dependent (SD) – of the survey respondents were identified in the survey data. The description on how these mental disorders were diagnosed is documented elsewhere (Statistics Canada, 2020b; Tjepkema, 2004). MDE and AD were diagnosed using a Canadian adaptation of the World Mental Health version of the Composite International Diagnostic Interview instrument (WMH-CIDI) . The WMH-CIDI measures episodes of symptoms and duration, frequency and severity of the symptoms to identify the presence of these mental disorders. SD was defined based on illicit drug dependence or alcohol dependence. At the time of the survey, cannabis was considered an illicit drug. Respondents were considered to have an illicit drug dependence if they experienced at least three symptoms of dependence related to their drug use at least monthly in the past 12 months. Respondents were considered alcohol dependence if they exhibited binge drinking (5 or more drinks during one occasion at least once a month during the past 12 months) and showed three or more symptoms affecting everyday activities (Statistics Canada, 2020b; Tjepkema, 2004). We identified respondents who had past 12-month MDE and life-time mania according to the WMH-CIDI in the survey data and considered the diagnosis of a manic episode to indicate BPD, in keeping with the DSM approach. Age, sex, marital status, and highest educational level achieved were chosen as covariates. Age was treated as a continuous variable. Marital status was dichotomized as married (included common-law) and single (included never married, previously married, widowed, and divorced). Additional covariates were not included since the goal of the analysis was to quantify the strength of association, not to isolate independent causal factors.
2.3. Data analysis
A recorded date of interview for each respondent in the survey was treated as the baseline time point. Survey respondents were followed up from the date of the interview to the data linkage date for CVSD (December 31, 2011) to see the suicide events (hospitalizations due to suicide attempts or deaths due to suicide). Survey participants who remained alive and were not hospitalized for suicide attempts before the data linkage date (December 31, 2011) were censored at that date. Time to event was calculated by subtracting the dates of baseline interview from the hospitalization dates for suicide attempts or the dates of deaths due to suicide (which ever occurred first). The total persons time at risk was 240,000 years (rounded).
The proportion of survey respondents who had mental disorders in the past 12 months and later had suicide events was assessed. Competing risk regression models that adjust for competing risk (i.e., other cause-related deaths) were used to estimate hazard ratios (HR) and 95% confidence intervals (CI). First, a model for each mental disorder was constructed to assess the hazard of suicide associated with each mental disorder compared to the absence of the disorder. The models were adjusted for age, sex, marital status, and educational attainment as these variables were associated with both mental disorders and suicide. Then, interaction terms between mental disorders were used to assess whether the hazard of suicide varied in relation to comorbidities. As none of the interaction terms were significant, the interaction terms were dropped from the models and are not discussed further in this report.
The Cox proportion hazard assumption (whether the effect of mental disorders is constant over time) was evaluated using log-log plots, a statistical test based on the Schoenfeld residuals, and by assessing the statistical significance of interaction terms involving time by exposure. The models for MDE and SD did not meet the assumption: significant violations of the proportional hazards assumption were observed, indicating that the relative hazard of suicide events for MDE and SD changed significantly over time. Therefore, the models were stratified using the time to event cut-off 4-year. These stratified models met the Cox proportional hazard assumption.
The CCHS survey used stratified, multistage sample selection techniques which included clustering and unequal selection probabilities. Sampling weights, provided by Statistics Canada, were used to ensure the representativeness of target population, with the provision that Quebec was excluded as this province does not participate in the DAD-CCHS linkage. All analyses were performed using STATA statistical software version 16.0. An alpha-level of 5% was used to assess statistical significance.
As we combined hospitalizations for suicide attempts and deaths due to suicide into a single variable (which was required to have an adequately powered analysis), we performed sensitivity analyses to compare the hazard ratios for suicide attempt and suicidal death. Furthermore, the risk patterns of suicide attempt and death were assessed across male and female groups to examine whether the patterns aligned with known characteristics from literature (i.e., males having lower suicide attempts, but higher death due to suicide, compared to females) (Government of Canada, 2020). For these analyses, two separate models were constructed, a Cox model for suicide attempts and a competing risk model for suicidal death. Each model included mental disorders, age, sex, marital status, and education attainment variables and the estimates were adjusted for every other variable included (simultaneous adjustment).
3. Results
Of the approximately 27,000 respondents eligible for this analysis, 0.41% had a suicide event (hospitalized for suicide attempts or died due to suicide). The respondents with suicide events were younger (mean age= 39.21 years) than those who did not (mean age=43.78 years). As shown in Table 1 , a high proportion of respondents with suicide events were single or previously married (including widow/separated/divorced) and had post-secondary education. Of those with suicide events, 15.58% had MDE, 14.47% had BPD, 27.40% had AD, and 15.58% had SD.
Table 1.
Characteristics of survey respondents (n= 27,000)
| Characteristics variables | Overall % (95% CI) | Hospitalizations for suicide attempts or death due to suicide: yes % (95% CI) | Hospitalizations for suicide attempts or death due to suicide: no % (95% CI) |
|---|---|---|---|
| Sex: | |||
| Female | 50.80 (50.80, 50.86) | 50.65 (50.30, 51.00) | 50.84 (50.82, 50.86) |
| Male | 49.16 (49.14, 49.18) | 50.65 (50.30, 51.00) | 49.16 (49.14, 49.18) |
| Marital status: | |||
| Married common-law | 62.31 (62.28, 62.33) | 36.36 (36.02, 36.700 | 62.41 (62.39, 62.43) |
| Widow/separated/divorced/single | 37.69 (37.67, 37.72) | 63.64 (63.30, 63.98) | 37.59 (37.57, 37.61) |
| Educational attainment: | |||
| Less than secondary school graduation | 24.50 (24.48, 24.52) | 38.16 (37.81, 38.50) | 24.44 (24.42, 24.46) |
| Secondary school graduation | 19.77 (19.75, 19.79) | 28.95 (28.63, 29.27) | 19.73 (19.71, 19.75) |
| Some post-secondary education | 9.11 (9.10, 9.13) | 3.95 (3.81, 4.09) | 9.13 (9.12, 9.15) |
| Post-secondary credit/diploma or university | 46.62 (46.60, 46.65) | 30.26 (29.94, 30.59) | 46.70 (46.67, 46.72) |
| Past 12 months mental disorders: | |||
| Major depressive disorder | 3.90 (3.89, 3.91) | 15.58 (15.33, 15.84) | 3.86 (3.85, 3.86) |
| Bipolar disorder | 0.87 (0.86, 0.87) | 14.47 (14.22, 14.73) | 0.80 (0.80, 0.80) |
| Any anxiety disorders | 5.13 (5.12, 5.14) | 27.40 (27.07, 27.72) | 5.04 (5.03, 5.05) |
| Substance dependence | 3.36 (3.35, 3.37) | 15.58 (15.33, 15.84) | 3.31 (3.30, 3.32) |
| Any mental disorder | 11.38 (11.36, 11.39) | 47.30 (47.94, 47.66) | 11.23 (11.22, 11.25) |
| Subsequent suicide events (hospitalizations for suicide attempts or death due to suicide) | 0.41 (0.40, 0.41) | - | - |
Note: any anxiety disorders include panic anxiety disorder or social phobia or agoraphobia; substance dependence includes illicit drug or alcohol dependence or both
Table 2 shows the association between past 12-month mental disorders and subsequent suicide event (hospitalization for suicide attempts or death due to suicide). All mental disorders were significantly associated with an increased hazard of suicide. The increased hazard of suicide events was different across mental disorders. Adjusting for age, sex, marital status, and educational attainment, the HR was 4.04 (95% CI=2.13, 7.66) for MDE, and the HR for BPD was 16.49 (95% CI=8.45, 32.17). Similarly, the HR was 6.23 (95% CI=3.69, 10.50) for AD and was 3.79 (95% CI=2.01, 7.15) for SD. In all of these HRs, the group with no disorder was included as the reference category. However, the strength of associations differed significantly over time for MDE (p-value for the time by exposure interaction was p=0.012) and for SD (p-value for the time by exposure interaction was p=0.047), but not for BPD (p-value for interaction term was p=0.770) and AD (p-value for interaction term was p=0.107) (Table 2).
Table 2.
Patterns of association between past 12 months mental disorders and subsequent suicide events
| Mental disordersa | Unadjusted HR (95% CI) | Adjusted b HR (95% CI) | P value for adjusted HR | P value for interaction with time to event |
|---|---|---|---|---|
| Major depressive disorder | 4.49 (2.32, 8.64) | 4.04 (2.13, 7.66) | <0.0001 | 0.012 |
| Bipolar disorder | 21.00 (11.44, 38.56) | 16.49 (8.45, 32.17) | <0.0001 | 0.770 |
| Any anxiety disorders | 6.99 (4.24, 11.51) | 6.23 (3.69, 10.50) | <0.0001 | 0.107 |
| Substance dependence | 5.11 (2.91, 8.98) | 3.79 (2.01, 7.15) | <0.0001 | 0.047 |
Individual model was constructed for each mental disorder, where reference group was absence of the mental disorder
Adjusted for age, sex, marital status and educational attainment; any anxiety disorders include panic anxiety disorder or social phobia or agoraphobia or their combination; substance dependence includes illicit drug or alcohol dependence or both
Based on the stratified models using the time to event cut-off 4 years, the adjusted HR of suicide among those with MDE was 6.02 (95% CI=2.65, 13.68) in the first 4 years, whereas, it was 2.03 (95% CI=0.91, 4.53) after 4 years. Similarly, the adjusted HRs of suicide for SD were 6.29 (95% CI=2.79, 14.17) and 1.82 (95% CI=0.65, 5.07) before and after 4 years. However, the risk of suicide associated with BPD remained high over time, similar HRs were observed in the first 4 years and after 4 years. The adjusted HRs of suicide for BPD were 16.95 (95% CI=6.88, 41.75) and 15.81 (95% CI=5.89, 42.45) before and after 4 years, respectively. Although the interaction term of AD with time was not significant, the adjusted HRs of suicide for AD were 8.74 (95% CI=4.32, 17.69) and 3.73 (95% CI=1.55, 8.96) before and after 4 years, respectively (Table 3 ).
Table 3.
Patterns of association between past 12 months mental disorder and subsequent suicide events stratified by time to the event
| Models stratified by time to the event (4 years) | ||||
|---|---|---|---|---|
| Time to the event ≤4 years | Time to the event >4 years | |||
| Mental disordersa | Unadjusted HR (95% CI) | Adjustedb HR (95% CI) | Unadjusted HR (95% CI) | Adjustedb HR (95% CI) |
| Major depressive disorder | 6.94 (2.97, 16.19) | 6.02 (2.65, 13.68) | 2.11 (0.95, 4.66) | 2.03 (0.91, 4.53) |
| Bipolar disorder | 22.29 (9.92, 50.05) | 16.95 (6.88, 41.75) | 19.19 (7.70, 47.84) | 15.81 (5.89, 42.45) |
| Any anxiety disorders | 10.38 (5.37, 20.07) | 8.74 (4.32, 17.69) | 3.88 (1.67, 9.04) | 3.73 (1.55, 8.96) |
| Any substance dependent | 7.34 (3.57, 15.09) | 6.29 (2.79, 14.17) | 2.82 (1.10, 7.20) | 1.82 (0.65, 5.07) |
Individual model was constructed for each mental disorder, where reference group was absence of the mental disorder
Adjusted for age, sex, marital status, and educational attainment; any anxiety disorders include panic anxiety disorder or social phobia or agoraphobia or their combination; substance dependence includes illicit drug or alcohol dependence or both
Sensitivity analysis, as shown in Table 4 , shows that the relative hazard of suicide attempts (HR=6.50, 95% CI=3.67, 11.50) and the relative hazard of death due to suicide (HR=7.74, 95% CI=2.93, 20.41) associated with any mental disorders are similar. Compared to females, males had lower hazard of suicide attempt (HR=0.82, 95% CI=0.48, 1.41) but higher the hazard of death due to suicide (HR=1.85, 95% CI=0.71, 4.87) although these differences were not statistically significant.
Table 4.
Association of past 12 months any mental disorder, separately with subsequent suicide attempt and death due to suicide (sensitivity analysis)
| Variables | Suicide attempt (cox model) Adjusted HR (95% CI)a | Death due to suicide (competing risk model) Adjusted HR (95% CI)a |
|---|---|---|
| Any mental disorder b | 6.50 (3.67, 11.50) | 7.74 (2.93, 20.41) |
| Age | 0.99 (0.98, 1.01) | 1.02 (1.00, 1.03) |
| Sex: | ||
| Female (reference) | - | - |
| Male | 0.82 (0.48, 1.41) | 1.85 (0.71, 4.87) |
| Marital status: | ||
| Married/common-law (reference) | - | - |
| Widow/separated/divorced/single | 2.19 (1.23, 3.87) | 2.35 (0.86, 6.44) |
| Educational attainment: | ||
| ˂ Secondary school graduation (reference) | - | - |
| Secondary school graduated | 0.78 (0.40, 1.53) | 1.35 (0.40, 4.54) |
| Some post-secondary education | 0.12 (0.04, 0.36) | 0.60 (0.10, 3.79) |
| Post-secondary credit/diploma or university degree | 0.47 (0.25, 0.85) | 0.51 (0.18, 1.43) |
Adjusted for every other variables in the model (simultaneous adjustment).
any mental disorder include mood disorders (major depressive disorder and mania), anxiety disorders (panic anxiety disorder, social phobia, and agoraphobia), and substance dependence (illicit drug and alcohol dependence), where reference group is absence of any mental disorder
4. Discussion
4.1. Main Findings
This study examined the patterns of association between mental disorders and subsequent suicide events in nationally representative community sample in Canada using national survey data 2002 linked with the national mortality database 1999/2000-2012/2013 and hospitalization database 2002-2011. It found an increased hazard of suicide associated with each mental disorder, namely MDE, BPD, AD, and SD. The hazard was distinct across these mental disorders. Importantly, the increased hazard of suicide events associated with MDE, SD, and AD was smaller after stratification by year, but the strongly elevated hazard ratio associated with BPD remained unchanged over time.
4.2. Interpretations
Previous studies have shown the association between mental disorders and suicidality, including the unique associations for individual mental disorders and comorbid mental disorders (Bertolote et al., 2003; Borges et al., 2010; Bostwick and Pankratz, 2000; Cavanagh et al., 2003; Harris and Barraclough, 1997; Nock et al., 2010; Weissman et al., 1989). These findings reinforce the widely accepted idea that better management of mental disorders, including improved access to and quality of mental health services, may be important for suicide prevention, although we did not attempt to adjust for the effects of treatment in this analysis. Our findings − that the association changes (declines) over time for MDE, SD, and AD but that it remains unchanged for BPD − enhance the prior understanding of the association between mental disorders and suicidality. The findings that the majority of suicide occurs in people with MDE, SD, and AD in the early years following documentation of a diagnosis, suggesting that this is a time of particularly high risk. Whereas, the findings that the risk of suicide persists over time in people with BPD suggest that continuous long-term follow up may be required in this group.
The association between mental disorders and suicide was stronger in previous studies than in our study. For example, the reported relative risk was 13.41 for depression, 18.82 for BPD, 27.60 for affective disorder, 9.40 for AD, and 11.98 for substance use (Hoye et al., 2016; Meier et al., 2016; Too et al., 2019; Webb et al., 2014; Webb et al., 2013). While the measurement variation, of exposures and/or outcomes, across studies affects the differences in strength of association, it is important to note that the previous studies were mostly conducted in clinical samples in hospital settings that mostly include more severely ill patients or vulnerable populations for suicide. Our study was conducted in a nationally representative community sample and confirms that these mental disorders are associated with suicide in community populations. Our study should encourage future studies to focus on examining interventions for suicide prevention in community-based samples.
Differences in the pattern of risk over time may be related to characteristics of these disorders. MDE may more often (compared to the other disorders we examined) be precipitated by environmental (stressful life events, such as stress, loss, threats, and social isolation) characteristics (Nabeshima and Kim, 2013). As time passes, the effects of life events and other environmental determinants may diminish. A similar pattern may not occur in BPD due to its greater heritability. BPD is considered 60% to 80% heritable (Nabeshima and Kim, 2013; Smoller and Finn, 2003), and thereby they may change less over time. Another possible explanation for the declining relative hazard of suicide over time in people with MDE could be the result of the lower severity of MDE over time due to treatment and management (Stone et al., 2009), but if this were the case a similar dynamic would be expected for BPD. Similarly, positive psychological changes in people managing their SD may underpin the apparently declining HR with time. However, we were unable to analyze the risks by severity of disorder since the CCHS did not measure severity of disorders.
4.3. Strengths/limitations
This study has several strengths. First, this study used CCHS data, which was collected in a nationally representative community sample, in contrast to previous studies which were mostly conducted in clinical samples in hospital settings. Second, the current study had access to approximately 10 years of follow up data. This provided an opportunity to analyze the association between past mental disorders and subsequent suicide using the time-to-event data, where the mental disorders (exposures) preceded the suicide outcomes or the directionality of association was clear. Furthermore, the use of record linkage data circumvented the issue of recall bias to which psychological autopsies are prone. We combined suicidal death cases and hospitalizations for suicide attempts as a single suicide variable to address the small sample size issue for such a rare outcome. As our sensitivity analyses showed similar risk patterns of suicide attempt and suicidal death by mental disorders, and the risk patterns of suicide attempt and suicidal death across males and females as existed in the literature, such combination was justifiable. While we used ICD-9 and ICD-10 case definitions for suicide diagnostic data contained in the administrative databases (DAD and mortality database), as recommended by Statistics Canada, the diagnostic data are likely to underestimate the prevalence of suicide, specifically attempts (Rahme et al., 2016), since not all attempts require hospitalization. This could have diluted the observed association biased towards the null. Although it can be expected that actual association is stronger than the observed association, it is unlikely that this influenced the observed suicide risk patterns over time.
Our regression models included mental disorders, age (continuous variable), sex, marital status, and education attainment variables to estimate the adjusted HRs of suicide events for mental disorders. We also estimated the adjusted HRs of suicide events (separately for suicide attempt and death due to suicide) across male and female groups, to assess whether the suicide patterns aligned with known characteristics from literature (males having lower suicide attempts, but higher death due to suicide, compared to females). However, we are unable to further analyze the hazards of suicide according to gender and age quartiles due to the COVID-19 related lockdown and entry permission restriction in the Prairie Regional Data Centre at the University of Calgary. This analysis is valuable as it allows to determine the hazards of suicide in each age quartile (HRs are more interpretable in categorical variables) and the hazards in males and females by each age quartile (i.e., effect modification by age in male and female).
5. Conclusions
The risk of suicidal behavior declined over time after a past year diagnosis of MDE, SA, and AD. This may reflect improvement over time in MDE, SA, and AD (where peak prevalence is observed in the young people) and their consequence on suicidal behavior. The findings underscore the well-known importance of management strategies employed soon after the diagnosis of MDE, SD, and ADs. The risk of suicide associated with BPD seems to strongly persist over time.
Authors contributions
Kamala Adhikari, Scott B Patten, and Amy Metcalfe involved in the conception and design of the study. Kamala was also responsible for conducting the analysis, interpreting the data, and drafting the manuscript. Scott B Patten contributed to interpretation of data and provided intellectual content and revisions to manuscript. Amy Metcalfe, Andrew GM Bulloch, and Jeanne VA Williams involved in the design of the study and provided interpretation to subsequent drafts of the manuscript. All authors read and approved the final draft.
Funding
This was an investigator-initiated project. No sources of funding are related to the research reported.
Ethics
The data were accessed through and analyzed at the Prairie Regional Data Centre, located at the University of Calgary. Ethics approval was not applicable as the University of Calgary does not require ethics review for secondary data analysis using Statistics Canada data.
Declaration of Competing Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgements
Kamala Adhikari was awarded the Vanier Canada Graduate Scholarship (Award code: 201611CGV-382013-267341) by the Canadian Institutes of Health Research and the Alberta Innovates Graduate Studentship Award (Award code: 201611CGV-382013-267341) by the Alberta Innovates for her PhD training. Funding agencies do not play any role on this study and the manuscript.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2020.08.053.
Appendix. Supplementary materials
References
- Arsenault-Lapierre G., Kim C., Turecki G. Psychiatric diagnoses in 3275 suicides: a meta-analysis. BMC Psychiatry. 2004;4:37. doi: 10.1186/1471-244X-4-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertolote J.M., Fleischmann A., De Leo D., Wasserman D. Suicide and mental disorders: do we know enough? Br. J. Psychiatry, England. 2003:382–383. doi: 10.1192/bjp.183.5.382. [DOI] [PubMed] [Google Scholar]
- Borges G., Nock M.K., Haro Abad J.M., Hwang I., Sampson N.A., Alonso J., Andrade L.H., Angermeyer M.C., Beautrais A., Bromet E., Bruffaerts R., de Girolamo G., Florescu S., Gureje O., Hu C., Karam E.G., Kovess-Masfety V., Lee S., Levinson D., Medina-Mora M.E., Ormel J., Posada-Villa J., Sagar R., Tomov T., Uda H., Williams D.R., Kessler R.C. Twelve-month prevalence of and risk factors for suicide attempts in the World Health Organization World Mental Health Surveys. J. Clin. Psychiatry. 2010;71:1617–1628. doi: 10.4088/JCP.08m04967blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostwick J.M., Pankratz V.S. Affective disorders and suicide risk: a reexamination. Am. J. Psychiatry. 2000;157:1925–1932. doi: 10.1176/appi.ajp.157.12.1925. [DOI] [PubMed] [Google Scholar]
- Carroll R., Metcalfe C., Gunnell D. Hospital presenting self-harm and risk of fatal and non-fatal repetition: systematic review and meta-analysis. PLoS One. 2014;9:e89944. doi: 10.1371/journal.pone.0089944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanagh J.T., Carson A.J., Sharpe M., Lawrie S.M. Psychological autopsy studies of suicide: a systematic review. Psychol. Med. 2003;33:395–405. doi: 10.1017/s0033291702006943. [DOI] [PubMed] [Google Scholar]
- Gili M., Castellví P., Vives M., de la Torre-Luque A., Almenara J., Blasco M.J., Cebrià A.I., Gabilondo A., Pérez-Ara M.A., A M.M., Lagares C., Parés-Badell O., Piqueras J.A., Rodríguez-Jiménez T., Rodríguez-Marín J., Soto-Sanz V., Alonso J., Roca M. Mental disorders as risk factors for suicidal behavior in young people: A meta-analysis and systematic review of longitudinal studies. J. Affect. Disord. 2019;245:152–162. doi: 10.1016/j.jad.2018.10.115. [DOI] [PubMed] [Google Scholar]
- Government of Canada. 2020. Suicide in Canada: Key statistics (infographic). 2020; [cited 2020 March 02]. Accessed from:https://www.canada.ca/en/public-health/services/publications/healthy-living/suicide-canada-key-statistics-infographic.html.
- Harris E.C., Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis . Br. J. Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- Hoye A., Nesvag R., Reichborn-Kjennerud T., Jacobsen B.K. Sex differences in mortality among patients admitted with affective disorders in North Norway: a 33-year prospective register study. Bipolar Disord. 2016;18:272–281. doi: 10.1111/bdi.12389. [DOI] [PubMed] [Google Scholar]
- Kapur N., Cooper J., King-Hele S., Webb R., Lawlor M., Rodway C., Appleby L. The repetition of suicidal behavior: a multicenter cohort study. J. Clin. Psychiatry. 2006;67:1599–1609. doi: 10.4088/jcp.v67n1016. [DOI] [PubMed] [Google Scholar]
- Meier S.M., Mattheisen M., Mors O., Mortensen P.B., Laursen T.M., Penninx B.W. Increased mortality among people with anxiety disorders: total population study. Br. J. Psychiatry. 2016;209:216–221. doi: 10.1192/bjp.bp.115.171975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabeshima T., Kim H.C. Involvement of genetic and environmental factors in the onset of depression. Exp. Neurobiol. 2013;22:235–243. doi: 10.5607/en.2013.22.4.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock M.K., Hwang I., Sampson N., Kessler R.C., Angermeyer M., Beautrais A., Borges G., Bromet E., Bruffaerts R., de Girolamo G., de Graaf R., Florescu S., Gureje O., Haro J.M., Hu C., Huang Y., Karam E.G., Kawakami N., Kovess V., Levinson D., Posada-Villa J., Sagar R., Tomov T., Viana M.C., Williams D.R. Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Med. 2009;6 doi: 10.1371/journal.pmed.1000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock M.K., Hwang I., Sampson N.A., Kessler R.C. Mental disorders, comorbidity and suicidal behavior: results from the National Comorbidity Survey Replication. Mol. Psychiatry. 2010;15:868–876. doi: 10.1038/mp.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahme E., Low N.C.P., Lamarre S., Daneau D., Habel Y., Turecki G., Bonin J.P., Morin S., Szkrumelak N., Singh S., Lesage A. Correlates of Attempted Suicide from the Emergency Room of 2 General Hospitals in Montreal, Canada. Can. J. Psychiatry. 2016:382–393. © The Author(s) 2016. [Google Scholar]
- Sanmartin C., Decady Y., Trudeau R., Dasylva A., Tjepkema M., Fines P., Burnett R., Ross N., Manuel D.G. Linking the Canadian Community Health Survey and the Canadian mortality database: an enhanced data source for the study of mortality. Health Rep. 2016;27:10–18. [PubMed] [Google Scholar]
- Smoller J.W., Finn C.T. Family, twin, and adoption studies of bipolar disorder. Am. J. Med. Genet. C Semin. Med. Genet. 2003;123c:48–58. doi: 10.1002/ajmg.c.20013. [DOI] [PubMed] [Google Scholar]
- Statistics Canada. 2020. Deaths and age-specific mortality rates, by selected grouped causes. 2020a; [cited 2020 March 02]. Access from:https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310039201.
- Statistics Canada. 2020. Canadian Community Health Survey - Mental Health and Well-being (CCHS). 2020b; [cited 2020 March 02]. Accessed from:https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=5285#a2.
- Statistics Canada . Statistics Canada; 2005. Comparability of ICD-10 and ICD-9 for mortality statistics in Canada. [Google Scholar]
- Stone M., Laughren T., Jones M.L., Levenson M., Holland P.C., Hughes A., Hammad T.A., Temple R., Rochester G. Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration. BMJ. 2009;339:b2880. doi: 10.1136/bmj.b2880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tjepkema M. Alcohol and illicit drug dependence. Statistics Canada, Catalogue: Suppl. Health Report. 2004 [PubMed] [Google Scholar]
- Too L.S., Spittal M.J., Bugeja L., Reifels L., Butterworth P., Pirkis J. The association between mental disorders and suicide: A systematic review and meta-analysis of record linkage studies. J. Affect. Disord. 2019;259:302–313. doi: 10.1016/j.jad.2019.08.054. [DOI] [PubMed] [Google Scholar]
- Webb R.T., Lichtenstein P., Larsson H., Geddes J.R., Fazel S. Suicide, hospital-presenting suicide attempts, and criminality in bipolar disorder: examination of risk for multiple adverse outcomes. J. Clin. Psychiatry. 2014;75:e809–e816. doi: 10.4088/JCP.13m08899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb R.T., Qin P., Stevens H., Appleby L., Shaw J., Mortensen P.B. Combined influence of serious mental illness and criminal offending on suicide risk in younger adults. Soc. Psychiatry Psychiatr. Epidemiol. 2013;48:49–57. doi: 10.1007/s00127-012-0517-6. [DOI] [PubMed] [Google Scholar]
- Weissman M.M., Klerman G.L., Markowitz J.S., Ouellette R. Suicidal ideation and suicide attempts in panic disorder and attacks. N. Engl. J. Med. 1989;321:1209–1214. doi: 10.1056/NEJM198911023211801. [DOI] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; 2014. Preventing suicide, a global imperative. [Google Scholar]
- Wunderlich U., Bronisch T., Wittchen H.U. Comorbidity patterns in adolescents and young adults with suicide attempts. Eur. Arch. Psychiatry Clin. Neurosci. 1998;248:87–95. doi: 10.1007/s004060050023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.