Abstract
Background
Substance Use Disorder (SUD) places a heavy burden on societal and health systems given its association with high mortality and morbidity rates worldwide, including Mauritius. Illicit substances act as a positive reinforcement and stimulate addiction through its pleasure-seeking attributes.
Aim
This study focused on identifying the risk factors leading to SUD among Mauritian male addicts as well as examining the potency of those factors in SUD development. The study also aimed at determining the prevalence of relapse and its causation.
Research setting
A cross-sectional study was conducted over a period of six months using a sample of 180 male addicts registered in a public hospital. A questionnaire investigating dimensions such as risk factors, self-esteem and peer pressure was administered.
Findings
A high percentage of relapse was noted amongst users within the first year of abstinence. Majority of respondents originated from nuclear or single parents’ family and were deprived of adequate social supports given their marital status. 57.5% of participants had a positive family history of SUD. Cannabis was the most commonly abused substance and 76.2% of the addicts were introduced to drugs through curiosity. Transposing the results against the Gateway Drug Theory showed a constant progression from soft to hard drugs for male addicts, a trend which was consistent with literature. Lastly, a theoretical model was developed based on the strong statistical association found between impulsivity and reduced thought processes prior to relapse; data revealing increased impulsivity which is a common trait in antisocial personality disorder and borderline personality disorder as being largely responsible for relapse.
Conclusion
The study was successful in bringing out the most common risk factors of SUDs which are linked to low socioeconomic status. The inability of addicts to progress with their rehabilitation given the alarming 92% of relapse was related to social pressure as prime deterrent to successful remission. Programmes involving relapse prevention must implemented in the first year of abstinence to facilitate rehabilitation.
Keywords: Psychology, Clinical psychology, Relapse, Substance use disorder (SUD), Risk factors, Gateway drug theory
Psychology; Clinical psychology; Relapse; Substance use disorder (SUD); Risk factors; Gateway drug theory.
1. Introduction
Substance use disorder (SUD), defined as “a cluster of cognitive, behavioural, and physiological symptoms indicating that the individual continues using the substance despite significant substance related problems” (DSM-V, 2013), is increasingly plaguing societies. African countries have reported 38.5% of its population to be suffering from alcohol use disorder (AUD) (WHO, 2018). Of the 15.3 million people diagnosed with SUD, cannabis abuse is reported to be the most common illicit substance used in African countries (WHO, 2017). For Mauritius, there is a dearth of data on the prevalence of SUD. In 2010, it was estimated that the drug addicts’ population was 1.9% of the population which corresponds to approximately 20000 in Mauritius (UNODC, 2010); while in 2018 statistics rose to approximately 20,000 intravenous drug abusers and an overall 80,000 consumers of illicit substances on the island (Leen, 2018). SUD is always characterized by tolerance and dependence (Houchins, 2018). The pathology of drug addiction is portrayed by the reward pathway which is over-ridden by faulty commands compelling drug abuse despite the onset of withdrawal symptoms; condition termed as “reward deficiency syndrome” (Fox et al., 2013). Clinical presentation and consequential effects of substance dependence can be divided into physical and behavioral attributes specific to the substance abused as shown in Table 1.
Table 1.
Signs and symptoms in substance withdrawal and consequences of substance abuse.
| SYMPTOMS | ALCOHOL | AMPHETAMINE | CANNABIS | INHALANT | OPIOID |
|---|---|---|---|---|---|
| PSYCHOMOTOR ACTIVITY | ↑ | Agitation/Retardation | Irritable | ||
| INSOMNIA | + | + | + | + | + |
| HALLUCINATIONS | + | + | + | ||
| FITS | + | ||||
| MOOD | Irritable | Low | Low | Low | Dysphoric |
| AUTONOMIC INSTABILITY | |||||
| SWEATING | + | + | + | ||
| HEART RATE | ↑ | ↑ | |||
| TREMORS | + | + | |||
| NAUSEA/VOMITING | + | ||||
| DIARRHOEA | + | ||||
| LACRIMATION | + | ||||
| RHINORRHEA | + | ||||
| YAWNING | + | ||||
| APPETITE | ↑ | ||||
| FATIGUE | + | ||||
| PUPILS | Dilate | ||||
| CONSEQUENCES | |||||
| DEPRESSION | + Suicidal thoughts |
Amotivational Syndrome | + | + | |
| ANXIETY | + | + | Panic Attacks | + | |
| PSYCHOSIS | Paranoid Delusions | Hallucinations, Delusions (Paranoid) |
+ | ||
KEY ↑: Increased ↓: Decreased +: Present.
Information retrieved from Sadock and Virginia, 2004
1.1. Risk factors promoting SUD
A number of studies have demonstrated the specificity of SUD when it comes to causality; it stretches across the developmental stages, genetics and environmental cues. SUD usually begins in adolescence and early adulthood, stemming from novel sensation-seeking behaviour and poor decision making (Poudel and Gautam, 2017). The earlier the onset of cannabis abuse, the higher is the risk of abusing other illicit drugs in later life; phenomenon commonly termed as the ‘Gateway Drug Theory’ (GDT) (Nkansah-Amankra and Minelli, 2016; Poudel and Gautam, 2017).
Social and personal factors are root causes of SUD. Socially, family type modulates substance abuse among adolescents as shown by the high SUD rates associated to upbringing in step- and single-families (Barrett and Turner, 2004; Hemovich and Crano, 2009). Parental-mediated substance abuse modelled by children, and ineffective parenting styles are determinants of substance addiction in later life (Schindler et al., 2005). Furthermore, a family history of psychiatric illnesses predispose children to many psychiatric disorders such as bipolar disorder, depression, suicide, behavioural disorders and SUD (Dellabella, 2018). A large volume of data has demonstrated the comorbid prevalence of Axis 1 mental disorders such as major depression and affective disorders, linked to AUD and SUD; conditioned referred to as dual diagnosis (Bradizza et al., 2006). Furthermore, individuals with autism spectrum disorder are more prone to develop SUD as opposed to a normal population (Kunreuther, 2020). In-depth understanding of the psychiatric co-morbidities and SUD, its directionality, and rank-order effect can prove to be elemental in isolating potent risk factors to relapse. Interestingly other factors such as neighbourhood poverty is tied to psychological distress and erosion of social relationships, hence furthering substance abuse as a ‘relief mechanism’ from painful situations (Mennis et al., 2016).
Low academic achievement, self-esteem and peer pressure are critical factors in the development of maladaptive behaviours such as drug addiction (Alavi, 2011; Ojo et al., 2013). Such factors are found to lower resilience to abrupt life changes, pushing the individuals towards pleasure seeking activities as a counter-measure against negative feelings (Alavi, 2011). Peer influence can be bidirectional; positively helping a deviant teen to learn more appropriate behaviours or adversely leading to delinquency, risky sexual behaviours and SUD progressing through adulthood (Allen et al., 2012).
1.2. Relapse and its aetiologies
Although much progress has been made in the rehabilitative approaches for SUD, relapse rate among abusers remains high. Studies have shown that 66% of adult addicts and 75% of adolescent addicts relapse within six months of stopping addiction treatment (Njoroge, 2018). Relapse can be attributed to a number of internal and external causes including mental illnesses (anxiety/neuroticism), withdrawal, cognitive deficits (intellectual and learning disabilities), boredom, unemployment, defective coping strategies, interpersonal conflict, social pressure, lack of support, stigmatisation, lack of leisure activities and treatment facilities (Njoroge, 2018; Ramo and Brown, 2008).
Most studies show that adolescents relapsing after a long period of abstinence fall prey to social pressure even after initiation of detoxification treatment (Ramo et al., 2005; Swanepoel et al., 2016). Negative intrapersonal state also explains relapse and accounts for 33% of relapse cases (Ramo and Brown, 2008). A proportion of addicts have defective coping strategies, precipitating the use of illicit substances as a means to escape from personal problems such as sense of frustration, anger, depression, anxiety, boredom and feeling of disappointment (Hyman and Sinha, 2009). Unemployment exhibits a two-fold effect as a risk factor in SUD. Economic recession and unemployment increase the likelihood to indulge in substance abuse or relapse due to increased psychological distress and social exclusion (Nagelhout et al., 2017).
The impact of drug abuse and most importantly relapse is multidimensional. Drug addiction not only affects the individual but also the interpersonal relationships which lead to disruption at the family, community and societal level (Fox et al., 2013). The major signs of impaired social functioning and behavioral changes are involvement in crimes, burdening the country financially and economically. Seen from a different perspective, the distribution of drug treatment facilities is unequal and acts as a barrier for addicts to access services (Pullen and Oser, 2014); the latter which may be a deterrent to successful recovery. Rural areas are exposed to highest challenges such as a lack of and/or underused services in conditions of increased addicts density due to easy availability of drugs (Pullen and Oser, 2014).
Emergence of SUD can be modulated by either reducing the risk factors or enhancing the protective factors. Hence, the aim of this study is to probe into the risk factors and prevalence of relapse linked to SUD in Mauritian male addicts; and to understand whether demographic factors are replicated across global-boundaries. Most importantly, this study aims at isolating key factors which will be useful for tailoring primary prevention programmes aimed at the young and vulnerable Mauritius population.
2. Materials and methods
2.1. Study design and location
The study was conducted at Dr A.G. Jeetoo Hospital which is located in the capital of Mauritius where all psychiatric cases from the northern region converges. Although not representative of the general addict population across Mauritius, this sample covers an essential demographic segment of the island known to be a ‘hotspot’ for substance dealings. The northern part of the island also catered for 39.8% of total in-patient treatment with respect to substance abuse. A cross sectional study was carried out over a period of six months. Mauritian male addicts were sampled as a result of their increased prevalence towards SUD as cited in the Mauritius Health Statistics Report (2018) with a 250:1 (M:F) gender ratio recorded at the main psychiatric hospital. They were either known cases of SUD diagnosed by the resident psychiatrists or in other Area/Community Health Care Centres, Accident and Emergency Department and out-patient psychiatric and addictology clinics which are referred to the hospital. The diagnosis of SUD was based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). The following inclusion and exclusion criteria were applied to increase accuracy and relevance of information sought from the chosen sample.
Male patients were recruited based on the following criteria; aged between 18-65 years, existing or newly diagnosed with SUD inclusive of patients who have previously not reported to treatment and most importantly patients in a sober state for consensual participation or validated by a family member. Patients with acute psychiatric conditions related or unrelated to SUD; exhibiting suicidal tendencies and acute psychosis were excluded from the study. Recruited patients would have been attributed one or a combination of either antidepressants, anti-histaminic, synthetic opioids in drug replacement therapy and assigned to psychological support programs depending on the severity of their addiction and withdrawal symptoms. The current healthcare framework at the chosen hospital has an inpatient system for acute withdrawal treatment within the addictology department and the same patients are evaluated as outpatients and supported with biopsychosocial treatment. Hence, given the redundancy in patients from both the inpatient and outpatient centres, no further stratification was undertaken.
2.2. Sample size
Hospital records have shown that 250 addicts were admitted with substance related disorders in 2017 and 210 addicts were seen at the addictology department in the same year. The sample size to be taken was 210 based on margin error of 5%, confidence interval of 95% and response distribution of 50%. Factoring the repetitive admission of some patients, the response distribution was adjusted to 75% resulting in a sample size of 180.
2.3. Research instrument and design
Data collection was carried out using a screened questionnaire restricted to patients meeting the inclusion criteria and consenting to the study. Patients were surveyed personally to maximize attentional focus of respondents. Patients who were under the influence of substances were omitted from the survey. Proforma socio-demographic data of each of the individuals were included in the first section of the questionnaire with the addition of items relating to the past psychiatric history, duration of disorder, family psychiatric history and drug consumption. A tabulated description of the questionnaire is provided in Table 2. The prominent dependent variable, relapse, was tested against the potential causative determinants, hence, self-esteem, peer pressure and socio-economic, the latter extracted from the demographic data as independent variables.
Table 2.
Questionnaire template and variables measured.
| SECTION | VARIABLES |
|---|---|
| A - Demographics | Residence, Education Level, Age Group, Occupation, Job Satisfaction, Job Performance, Income, Marital Status, Family Type, Family Involvement in SUDs, Family Psychiatric History, Perinatal Complications, Past Psychiatric History, |
| B - Drug use status | Cigarette Smoking Status, Alcohol Consumption, Illicit drugs Consumption, Modes of Administration, Stressor |
| C - Relapse and Causation | Abstinence, Causes of relapse, Nature of Relapse |
| D - Self-esteem scale | Rosenberg Self-esteem Scale |
| E - Peer pressure | Resistance to Peer Influence |
2.3.1. The Rosenberg self-esteem scale
The Rosenberg self-esteem scale was used verbatim to examine features of anxiety, negative affect and happiness (Richardson et al., 2009). Score was computed for each participant by summing up all items and a cut-off value of 15 was used to differentiate between low self-esteem and normal to high self-esteem (Heidari and Ghodusi, 2016). A Cronbach alpha value of 0.623 was obtained for the current sample reflecting an acceptable reliability (Wongpakaran and Wongpakaran, 2012). Most of the data collected was not self-administered, hence, respondents were not presented with the opportunity of retracting or substituting their preferred response to the items of the scale unless the questions were asked to be repeated at any point of time during the survey.
2.3.2. Resistance to Peer Influence Scale (RPIQ)
The Resistance to Peer Influence Scale (RPIQ) was used to assess peer pressure as a potential risk factor to relapse. It has a scoring of 1–4; with higher scores indicating a high resistance to peer influence (RPI) (Dekkers et al., 2017). The scale was adapted to the needs of the study. Modifications consisted of using only one descriptor given that the initial pre-tested instrument which carried both descriptors was confusing to the respondents. However, the contrasting statement was verbally described to the respondent to record the agreement level. Items were scored as per the instrument and descriptors 2, 6 and 10 were reverse scored. These adaptations were tested for consistency as reported by the Cronbach alpha value of 0.699, denoting a good internal consistency (DiGuiseppi et al., 2018).
2.4. Data analysis
SPSS V22.0 for Windows was used for data entry and processing. Descriptive measures were used to characterize the sample taken according to the dimension being investigated. Nominal data was expressed as percentage. Statistical levels were capped at p < 0.05. Normality of data was tested using the Shapiro-Wilk test with a cut-off value of p > 0.05, designating normality of data. Chi-Square test was used to determine the relationship between the risk factors of relapse versus its frequency while co-dependent variables were further assessed on their effect on relapse using multiple linear regression. In conditions where a specific variable was found to exert an effect on the dependent variable, i.e. relapse, the directionality of such causation was also measured using the Person's correlation co-efficient.
2.5. Ethical consideration
Approval was sought from the Ministry of Health and Quality of Life prior to the onset of data collection (MHC/CT/NETH/RAMSH).
3. Results
3.1. Demographic profile of respondents
A majority of the participants were from North (69.6%). All of the addicts sampled had been exposed to formal education of varying levels with secondary level reported as the highest (52%). A normalized age distribution of the male addicts was noted with a lower percentage, i.e. 18.8% and 7.2% were between 49-58 years old and above 59 years old respectively. 53% of the population earned a monthly income of less than Rs10,000 while only 5 of the participants earned more than Rs40,000. 33.1% of the participants were single and 37% of the sample grew up in a nuclear family, 28.7% had single parents, and 6.6% were single children (Table 3).
Table 3.
Socio-Demographic details of Male Addicts.
| Education | Primary | 47.50% | Locality | North | 69.60% |
| Secondary | 52.00% | South | 1.10% | ||
| Tertiary | 0.00% | East | 6.10% | ||
| Professional Qualification | 0.50% | West | 23.20% | ||
| Age | 18–28 | 22.70% | Marital Status | Single | 33.10% |
| 29–38 | 24.30% | Divorced | 26.00% | ||
| 39–48 | 27.10% | Cohabitation | 11.60% | ||
| 49–58 | 18.80% | Widowed | 5.50% | ||
| >59 | 7.20% | Married | 23.80% | ||
| Family Type | Both Biological Parents/No Siblings | 6.60% | Income | <Rs10,000 | 53.00% |
| Single Parents | 28.70% | Rs10,000-Rs40,000 | 44.20% | ||
| Extended Family | 14.40% | >Rs40,000 | 2.80% | ||
| Nuclear Family | 37.00% | ||||
| Grand Parents | 13.3% |
Data presented as percentage of total number of respondents.
3.2. Psychiatric illness and SUDs
Analysis of the entourage of the participants featured the following: 27% reported the non-involvement of their family members with drug use while out of the 73% identified positively for SUDs, relatives appeared to be the most prominent users with 58% (Table 4). 72.8% of the respondents had a family member suffering from a psychiatric disorder associated to the high rate of respondents (65%) who themselves exhibited abnormal mental health. The most prevalent psychiatric disorder recorded for the family member was psychotic disorder (17.1%) (Table 4).
Table 4.
Addicts’ family drug-related history and psychiatric disorders.
| Frequency (n) | Percentage (%) | |
|---|---|---|
| aFamily member with SUDs | ||
| Parents | 60 | 33.1 |
| Siblings | 46 | 25.4 |
| Partner | 13 | 7.2 |
| Relatives | 104 | 57.5 |
| None | 49 | 27.1 |
| bMental Illnesses exhibited by Family members | ||
| Epilepsy | 19 | 10.5 |
| Mood Disorder | 13 | 7.2 |
| Psychotic Disorder | 21 | 17.1 |
| Unsure | 1 | 0.6 |
| None | 117 | 64.6 |
Data presented as participants responding positively to the statements.
Percentage computed over 181 respondents for each sub-level given the multi-selection nature.
Poly-disorders were not assessed in this case, overall data computed based on the total number of respondents.
Among those respondents who had a positive past psychiatric history (17%), 2% suffered from attention deficit hyperactive disorder (ADHD), 9% and 6% from behavioral disorder and epilepsy respectively. Cross-tabulating the age of illicit substance abuse and presence of psychiatric illness among the male addicts revealed that 50% of the ADHD patients started taking illicit drugs from 10-20 years old; 43.8% suffering from behavioral disorder started between 15-20 years and interestingly, 45.5% of the epileptic patients did not consume illicit drugs. 38.7% of the participants who did not have any past psychiatric illness started taking illicit drugs as from 15-20 years. No significant relationship was drawn between past psychiatric illness and age of first illicit drug use in the current sample (X2 (12) = 13.38, p = .34).
3.3. Drug use status, relapse and causation
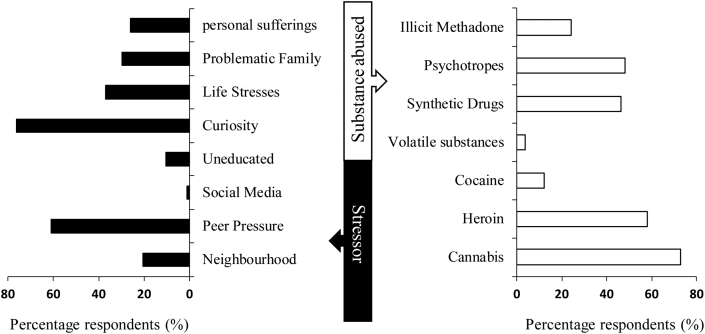
Thrill-seeking (55.80%), curiosity (76.2%) and peer pressure (60.8%) were the main factors related to drug initiation. Among the various classes of illicit substances, cannabis (72.9%) was the most consumed and to a lesser extent cocaine (12.2%), data which also reflects the international trends of substance abuse (Figure 1). Categorization of the participants according to number of substances abused showed 21.5% suffering from AUD, 7.7% and 16.6% abusing a single and two substances respectively; and the majority (54.1%) engaged into polysubstance consumption. 92% of the participants confirmed relapsing after a period of drug abuse cessation. 29% relapsed after less than 3 months while only 17% were able to extend the cessation for a period of 1–3 years. Cumulatively, 59% were not able to maintain a ‘sober’ state for more than one year. The most cited justifications provided for relapsing among the male addicts related to their social group still abusing drugs (44.2%) and dealing with life stresses (45.9%) (Table 5). It is noteworthy to mention the overlap in justifications provided for the initiation and resulting sustenance of SUD.
Figure 1.
Stressors leading to abuse and most preferred substance abused among male addicts.
Table 5.
Characterizing relapse causation in Mauritian male addicts.
| Frequency (n) | Percentage (%) | |
|---|---|---|
| Factors precipitating relapse | ||
| Difficulty finding employment | 26 | 14.4 |
| Dealing with life stresses | 83 | 45.9 |
| Lack of social support | 52 | 28.7 |
| Stigmatization | 11 | 6.1 |
| Boredom | 38 | 21 |
| Lack of recreational alternatives | 45 | 24.9 |
| Limited access to detoxification services | 28 | 15.5 |
| Social group still abusing drugs | 80 | 44.2 |
| Withdrawal symptoms | 38 | 21 |
These findings also support the fact that prior to relapse, 39.8% of the male addicts continuously thought about drugs, aligning with the short gap period before relapsing. 91.1% of the participants, who initially started abusing illicit drugs with a motive of new thrill-seeking sensation, relapsed after some time of abstinence. However, no significant relationship was found between the onset of illicit drug abuse due to thrill seeking sensation versus relapse (X2 (2) = 0.91, p = 0.63), which potentially endorses the addictive effect and augmented withdrawal symptoms over thrill-seeking behaviors in individuals relapsing.
A marginal percentage of male addicts thought about the effort they put during cessation prior to relapsing (19.4%), corroborating the findings of 16% of the participants who stopped taking drugs and never relapsed. Only 13.3% confirmed their assessment of the negative effects of drugs on their overall self, prior to relapse, validating the impulsive nature of drug use assigned to the majority of Mauritian male addicts. Assessing constructs namely, effort, impulsivity and thought process on the tendency to relapse gave an outlook on personality traits of the Mauritian male addicts, although this was secondary to the main objectives of these findings. A regression model was generated using the 3 constructs as predictors namely: impulsivity, thought, and effort. Each dimension independently associated to relapse (p < 0.001) (Table 6). 95.1% of variation recorded for relapse could be explained by the constructs. Furthermore, the model significantly predicted relapse (X2 (6) = 105.29, p < 0.001) and confirmed by the correlation coefficient (R2 = 0.951). The shared relationship across those 3 constructs was such that impulsivity negatively correlated to effort (-0.322) and thought process (-0.470); aligning with the strong relationship between the impulsive nature of the relapse versus the effort participants to stop consuming drugs (X2 (4) = 245, p < 0.001; Cramer V = 0.824), and thought process (X2 (4) = 104.98, p < 0.001; Cramer V = 0.539). A regression model using SES (independent variables: education, income and occupation) as a contributor to relapse revealed a non-significant effect (X2 (6) = 4.655, p = 0.589; R2 = 0.055).
Table 6.
Assessing personality constructs of Mauritian male addicts and relapse tendency.
| Frequency (n) |
Percentage (%) |
Association with Relapse |
|||
|---|---|---|---|---|---|
| Effort prior to relapse | X2 | Sig (p =) | Cramer V | ||
| Yes | 35 | 19.3 | 98.34 |
<0.001 |
0.737 |
| No | 117 | 64.6 | |||
| Not determined | 29 | 16 | |||
| Thought process mediating relapse | |||||
| Yes | 72 | 39.8 | 146.72 |
<0.001 |
0.900 |
| No | 93 | 51.4 | |||
| Not determined | 16 | 8.8 | |||
| Impulsivity to relapse | |||||
| Yes | 130 | 71.8 | 79.52 | <0.001 | 0.663 |
| No | 24 | 13.3 | |||
| Not determined | 27 | 14.9 | |||
3.4. Effect of drug initiation age and poly-consumption on relapse
Coupling the descriptive data on drug poly-consumption, the age of drug onset was cross-tabulated against the number of substances abused (Table 7). A transitional pattern was denoted in the number of substances consumed within the age gap of 16–25 years such that 79 respondents were already engaged in poly-substance use within that age period. There was a significant relationship between age of drug onset and development of poly-substance use disorder (X2 (12) = 164.27, p < 0.001; Cramer V = 0.550). These variables negatively correlated (Pearson's R = -0.652), strongly indicating the early onset of drug initiation leading to drug poly-consumption across a temporal scale. Drug poly-consumption was not significantly associated to relapse (X2 (3) = 4.166, p = 0.244; Cramer V = 0.152); suggesting that relapse was independent of the number of substances consumed.
Table 7.
Onset of drug initiation and poly-consumption.
| Age Onset | AUD | One substance | Two substances | Poly-substance | Total |
|---|---|---|---|---|---|
| 10–15yrs | 2 | 1 | 1 | 6 | 10 |
| 16–20yrs | 2 | 4 | 15 | 49 | 70 |
| 21–25yrs | 0 | 4 | 13 | 30 | 47 |
| 26–30yrs | 0 | 4 | 1 | 13 | 18 |
| >30yrs | 35 | 1 | 0 | 0 | 36 |
| Total | 39 | 14 | 30 | 98 | 181 |
Data presented as the frequency of participants (n).
AUD: Alcohol Use Disorder.
3.5. Self esteem profile and peer pressure among addicts
A mean score of 14.93 ± 3.79 was recorded for the whole sample with only 19 respondents scoring 20 and above. 45.3% of the Mauritian male addicts had low self-esteem level, i.e. a computed score lower than 15; notably with responses of not being good at all (47.5%) as per the Rosenberg Self-Esteem Scale. 54.7% had normal self-esteem level, with a greater proportion disagreeing that they failed in their life (43.6%). Majority of the male addicts tend to say that they can do most things as others (77.3%) as they have many good qualities (78.5%) and this encourages them to take a positive attitude towards themselves (83.4%). Overall, the Mauritian male addicts were satisfied with themselves (55.6%) (Refer to appendix Table.A1).
The mean scores recorded from the Resistance to Peer Influence Scale ranged from 20 to 25 among the different age groups with an average mean score of 22.5 ± 4.56. Individuals from 18- 28 years old scored a mean of 23.20 ± 5.36 with a declining trend a represented by the mean score of 21.15 ± 4.36 in those aged 59 and above; potentially demonstrated a stronger resistance to peer pressure in young adults. Most of the addicts exhibited a lower resistance to peer influence as they were easily influenced by their friends (46.4%) and took more risks in the company of their peers (62.4%) (Refer to supplementary Table.A1).
3.6. Transposing the Gateway Drug hypothesis in the Mauritian male addicts
The findings suggest that the sample population satisfies the GDT as 38.8% of the participants started smoking in the age group of 10–15 years old while 48.3% of the participants started abusing illicit drugs from the age of 15–20 years old. 57.6% of the participants who were smokers went on to consume illicit drugs to seek new thrills and 17.6% of the smokers started consuming alcohol after some time. Findings also showed an association between smoking and illicit drug consumption due to new thrill-seeking sensation; X2 (2) = 19.36, p < 0.001; further implying the role of nicotine as a ‘Gateway Drug’ leading to the escalation towards illicit drugs.
4. Discussion
SUD is a major societal concern which disrupts the most important institution, i.e. the family and contributes to an array of psychological and social problems, criminal activities, destitution and violence. Interest in this field has evolved to safeguard the society and create a better social environment through dissection of its underpinnings and tailored root-driven solutions, hence, the need to identify the risk factors inhibiting successful remission of SUD-affected individuals through this study.
4.1. Demographic risk factors and its influence on SUD
The present data is indicative of a young-aged population, i.e. within the range of adolescents and young adults as being the prime targets of SUD. This correlates with studies demonstrating an incidence rate of 38% adolescent admissions at acute drug rehabilitation care centers (Chisolm and Kelleher, 2006), and 74% addicts initiated to substance abuse at an early age further leading to earlier appearance of psychosocial problems and admissions at hospitals or day care centers (Poudel and Gautam, 2017; Strashny, 2013). Given that the present study did not look into the retrospective data pertaining to substance abuse among the elderly, the data cannot be paired with findings as depicted by Khan (2018) who reported a 32% rise in the number of drug related admissions in people aged above 55 years. However, given the ageing demographics of Mauritius, these findings would potentially be replicated.
Almost half of the respondents were living under the poverty line, earning an income of less than Rs10,000. Individuals from this social stratum are usually exposed to inadequate food, poor housing conditions, high level of violence, and poor mental health; which may pre-dispose the individuals towards the consumption of illicit drugs and risky behaviors (Cerdá et al., 2011; Long et al., 2014). Inadequate support with respect to family structure has also been earmarked as a risk factor for SUD. Single parents and nuclear families were most commonly associated with SUD in the population investigated. This is justified by the higher incidence of disruptive behavior among children from single parent families scarred by marital conflicts and violence; impeding the proper development of a child by increasing the susceptibility to mental health disorders inclusive of SUD (Hemovich and Crano, 2009).
A strong inter-generational relationship of SUD running across the family was noted in the sample investigated, highlighting drug exposure as part of the psychodynamics within the family. It has previously been reported that children from parents with SUD have trust issues and bear the burden of their parents’ addiction (SAMHSA, 2004). This feeling of guilt creates a quagmire of negative thoughts and behavioral attributes as reflected by the ineffective attachment due to child abuse, poor interpersonal relationships, poor learning capacity and psychological disorders, hence cascading to SUD (Daley, 2013; Lander et al., 2013). Further endorsing the concept of inter-generational mediated SUD is the high percentage of family members with existing SUD conditions coupled with the young-age of drug initiation, potentially revealing drug initiation as a coping mechanism and to a lesser extent a modelling behavior. The young initiation age also puts forth the theory of temporal relationship between behavioral disorders and SUD (Chiu et al., 2018; DeMilio, 1989), given that the former often goes undiagnosed and untreated in early adolescence increasing vulnerability to SUD in later life (Erskine et al., 2015; Harstad and Levy, 2014). The present data pairing addicts initiated to illicit substances from a young age with a past psychiatric diagnosis of ADHD, corroborates with findings that showed 25% of adolescent drug addicts fulfilled the criteria for ADHD and 15.2% were diagnosed with adult ADHD during treatment (Kessler et al., 2005). The choice of willingly turning towards illicit substances as a control measure against symptoms of distractibility, emotional unsteadiness, reduced concentration and raised impulsivity explains the association between SUD and ADHD (Chamberlain et al., 2017; Mariani and Levin, 2007). The presence of behavioral disorders, plausibly as a consequential effect of genetic pre-disposition also supports the claim of such disorders being a precursor to SUD (Capella and Adan, 2017). Therefore, upstream targets, which is this case would be the treatment of behavioral disorders may potentially deter those individuals from drug-seeking behaviors to alleviate the behavioral symptoms.
Interestingly, almost half of the participants who were suffering from epilepsy did not consume illicit drugs. Similar findings were reported whereby epileptic patients refrained from abusing illicit substances due to their potentiating effect on medical and metabolic alterations, responsible for reducing the threshold for fits (Yeni et al., 2015). Although epileptic individuals are known to be in a ‘red zone’ with respect to substance abuse including AUD, this association has been poorly tested (Alavi, 2011; I. J. Bakken et al., 2014).
New thrill seeking, curiosity and peer pressure, prominently drive the Mauritian male addicts toward illicit drugs consumption which concurs with studies highlighting a weak innate control over new thrill seeking behavior of addicts (Dubey and Arora, 2008). An escalation in the consumption of drugs, i.e. from nicotine and alcohol in the early stages to heroin in later life was noted. The current data reflects a rise from ‘acceptable’ drugs in early adolescence to harder ones in early adulthood which satisfies the GDT, with cannabis being a potent precursor to such escalation as demonstrated by our findings and others (Fouad Moselhy and Awara, 2016; Nkansah-Amankra and Minelli, 2016). The transition to harder drugs can be explained by social learning theory which promotes the practice of maladaptive skills further accentuating the effects of the GDT on these individuals (Lindsay and Rainey, 1997; NIDA, 2018). Most importantly features of truncated neuro-mechanisms with respect to the reward systems are explanatory to the GDT such as nicotine-mediated augmentation of harder drug reward. Nicotine enhances the reward ‘feeling’ after a first exposure to a harder drug such as cocaine due to increased likeliness of such illicit substances, inducing an immediate dependence (McQuown et al., 2007).
4.2. Frequency and predictors of relapse among Mauritian male drug addicts
Relapse is a major challenge of being successfully free of SUD. Our findings denoting a high proportion of relapse during the first 12 months of remission along with a decrease in the relapse rate following the subsequent time frame is comparable to Kassani et al. (2015) whereby 37% of addicts relapsed within six months of remission and a 70% during the first year. This implies that the first year of remission is a critical period which should be targeted for relapse prevention strategies. Facilitation to de-addiction services should hence be a focal point in supporting successful remission; while other strategies such as psychoeducation and introduction to image and behavioral improvement programs during the treatment phases should be prioritized during the first year of remission (Melemis, 2015). Aspects of subjectivity and severity of withdrawal symptoms cannot be excluded during this critical period and therefore, relapse prevention methods should be tailored based on a risk-situation analysis and the contextual factors surrounding the individual (Hendershot et al., 2011). Overall, irrespective of timeframe for relapse, 92% of male addicts versus 8% relapsed, while the latter was buffered potentially as a result of their ongoing methadone substitution therapy which is known to reduce natural drug seeking behavior among heroin and cocaine addicts.
The main triggers of relapse in Mauritian male addicts were life stresses and social circle still abusing drugs, suggesting that addicts have a maladaptive coping strategy towards stress and resort to illicit drugs to deal with problems in life (Moos and Moos, 2006). Low self-efficacy among the relapsing individuals cannot be neglected, hence characterizing the social coercion to abuse drugs after remission (Brown et al., 1989). Majority of the male addicts mentioned that relapse was impulsive and the thought process on the effort channeled during the period of remission was inexistent. Addiction is a brain disorder entailing abnormal levels of impulsivity and rendering an individual more liable to relapse (Bell et al., 2014). High levels of impulsivity are a pre-cursor to substance abuse, progression to addiction, and raised relapse rates in vulnerable individuals (Pattij and De Vries, 2013). Most interestingly, low self-efficacy has been associated to high levels of impulsivity; therefore increasing the need to consume illicit substances (Hayaki et al., 2011). Therapeutical approaches have focused on increasing self-efficacy during the remission stages to increase self-regulation and concomitantly reduce impulsivity to enhance relapse prevention strategies (Kadden and Litt, 2011). This supports the need to identify the mediators and moderators of self-efficacy to potentiate the effectiveness of treatment programs, especially among the young-aged (Burleson and Kaminer, 2005).
4.3. Effect of drug initiation age and poly-substance consumption on relapse
The age at which the first exposure to an illicit substance is known to dictate the rate of progression towards SUD while also predicting the strength of substance dependence; observations most prominent for adolescents versus adult males aged 24 years and above (Clark et al., 1998). Our findings are in agreement with past reports of age onset as being critical for the escalation to SUD (Winters and Lee, 2008), although further investigation of the age of first use and age of SUD diagnosis over a temporal scale would have strengthened the association between those two variables as demonstrated by Sung et al. (2004). Drug onset age also modulates the transition from a single substance to poly-substance use such that the majority of individuals with an early onset of substance use find themselves consuming multiple substances (K. Bakken, Landheim and Vaglum, 2004). Our data is indicative of such behavior, negatively correlating age and number of substances abused. The high percentage of relapse noted among the Mauritian male addicts may also be attributed to substance poly-consumption, the latter thought to increase the SUD persistence rates (Evans et al., 2017). Substance poly-consumption did not influence relapse in the present study. This is in line with Ramo et al. (2005) showing the absence of relationship between the number of substance used and timing of relapse, although the study sample involved youth exhibiting co-morbid psychiatric disorders. An intricate links exists between age of onset and latency to SUD progression with declining clinical and mental states (Capella and Adan, 2017). This can be explained by the presence of maladaptive coping styles in young addicts which is manifested as issue avoidance, social withdrawal and help refusal (Capella and Adan, 2017). At the neuropsychological level, premorbid brain defects lead to lower intelligence and executive functioning such as impaired planning and judgement, paving the way for these individuals to fall prey to SUD (Capella Mdel, Benaiges and Adan, 2015). Given that addicts with severe cases of SUD feature increasing psychopathologies (Clark et al., 2006), dual diagnosis should not be overlooked as a result of its modulatory effect on coping strategies and subsequent impact on SUD treatment (Julia E. Marquez-Arrico et al., 2015).
4.4. Investigating the effect of self-esteem and peer influence on SUDs
Self-esteem, stemming from the fulfilment of basic needs and development of a sense of security, reflects personal appreciation which is necessary in protecting an individual against SUD (Alavi, 2011). Down-regulators of self-esteem are mostly chronic exposure to poverty, homelessness, physical, sexual and verbal abuse (Stein et al., 2002). Associations between self-esteem and SUD have been extensively reported such that child neglect is seen to be linked with the development of low resilience contributing to low self-esteem which finally ensues with adolescent substance abuse (Oshri et al., 2017). The present results are partly in contradiction to common patterns of addicts reported in other studies with the contributory role of self-esteem to self-efficacy and self-control, hence protective against SUD (Yang et al., 2019). Only half of the male addicts' sample in our studies exhibited low self-esteem in conditions where we would expect a higher percentage from the SUD population. This may partly be explained by the drug abuse profile of the respondents; as an equal proportion indulged in hard drugs such as heroin, latter exerting a direct negative impact on self-esteem (Khajehdaluee et al., 2013). McGee and Williams (2000) cautiously reported an insignificant association between self-esteem and substance use among adolescents; attributed to the uncontrolled confounding variables which may originate from the social background. As such, social competence may be a cushioning factor against low self-esteem given the evolution of addicts within a milieu where access to drugs is facilitated as reported in this study through the relapsing tendencies mediated by the social circle. Similar reports of social competence surrounding initiation and sustenance of substance use has been reported by Veselska et al. (2009) indicating the behavioral change being regarded as the new ‘normal and acceptable’ behavior among peers. Relevantly, addicts often display immature defense mechanisms such as denial, projection, acting out and rationalization when they were asked about self-esteem, feelings of failure and guilt (Iwanicka et al., 2017; Ward and Rothaus, 1991), pairing with the general tendency of male addicts to evaluate themselves positively against their ideal selves (Gossop, 1976). Defense mechanisms are insensible, habitual, rigid and instinctive coping strategies which arise when subjected to internal clashes where adaptations to reality are required (P. Cramer, 2015; Iwanicka et al., 2017). The use of immature defense mechanisms is commonly seen in people with low self-esteem and who exhibit identity crisis (Cramer, 1997; Treger et al., 2015). This may plausibly account for the normal self-esteem levels recorded.
Most addicts had low resistance to peer influence independent of the age group with a mean score of 22.5. Similar findings were reported by Andrews et al. (2002) with addicts surveyed having low resistance to peer influence across age irrespective of gender. This could plausibly be justified by the fact that respondents in our study originated mainly from a low SES background, latter which most certainly pre-disposes an individual to low resistance to peer influence. Indeed, the social sphere of adolescents appear to greatly influence their resistance to drug-use behaviors in conditions where incompatibility with the social norm is developed and acceptance is mainly seen from like-minded peers, resulting in a sense of belonging in unstructured social settings (Caldwell and Darling, 1999; Parsai et al., 2008). Peer influence should not be considered as a strong independent predictor as the micro-environment of the individual potentiates its effect on substance use (Spooner, 1999). Addicts aged between 18-28 years demonstrated a stronger resistance to peer pressure potentially inferring that young adults as opposed to adolescents are initiated to drugs out of free will and curiosity. The increase in resistance against peer influence has also been demonstrated in Monahan et al. (2009), suggestive of intervention programs targeting the young aged and empowering them with social and cognitive skills, especially in low SES regions through counselling programs to reduce the risk to peer-mediated substance initiation. Bio-mechanistically, regular consumption of drugs hijacks the neuro-reward mechanisms leading to a loss of free will as observed in addicts (Lavazza, 2016; Vohs and Baumeister, 2009); coupled with the presence of co-morbid psychiatric disorders (Deas and Thomas, 2001), the application of a combination of pharmacotherapy, psychoeducation, behavioral and psychosocial therapies may be the logical approach.
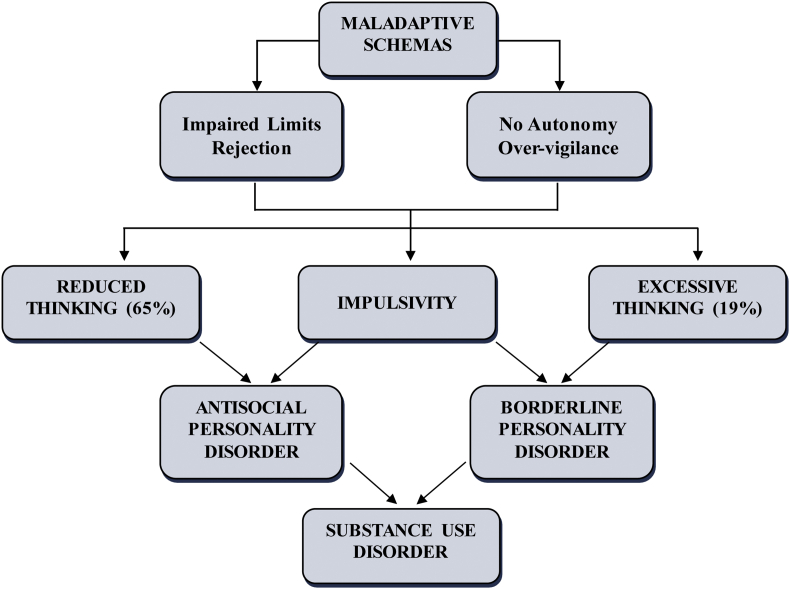
4.5. Conceptualizing impulsivity to personality disorders
Auxiliary to the main objectives of this study, a model was theoretically drawn based on personality traits and the relapsing status of the participants (Figure 2). A strong association was observed between impulsivity and reduced thought processes prior to relapse implying that relapse is impulsive and most of the addicts never thought about the effort made during remission. Illicit drugs are believed to raise impulsivity (Adinoff et al., 2007; Perry and Carroll, 2008); latter being a trait observed in individuals with personality disorders such as antisocial personality disorder (ASPD) or borderline personality disorder (BPD) (Jahng et al., 2011; Korsgaard et al., 2016; Martin et al., 2019). Research has shown that up to 23% and 53% of patients suffering from ASPD and BPD respectively are strongly linked to SUD. Poor prognosis and higher relapse rates has been demonstrated in patients with co-morbid personality disorders with only 17% addicts maintaining abstinence with a 1 year period (Sher and Trull, 2002).
Figure 2.
Theoretical framework associating SUDs and Personality Disorders.
Our data strongly indicates that impulsivity is an underlying personality trait among the Mauritian male addicts. Since impulsivity is included in both ASPD and BPD, emphasis must be laid on delineating these two conditions to support a more effective characterization of the addicts. ASPD patients lack empathy, are careless and act without any remorse (Goldstein et al., 2006), whereas BPD patients are inclined towards abandonment, have an unstable self-schema and indulge in self harm (Esmaeilian et al., 2019). BPD also induces vigilance, care, excessive thought process and dependence over assistance (Esmaeilian et al., 2019; Shorey et al., 2014).
4.6. Limitations of study
The present study potentially classifies Mauritian male addicts as being predisposed to ASPD given the lack of thought process during relapse although more ground work is needed to objectively characterize impulsivity and personality disorders with relapse and its underlying dimensions. This conceptual theory identifies the possibility of a dual diagnosis in these male addicts which can be the underlying reason for their progression to poly-substance use, relapse and treatment cessation (van den Bosch and Verheul, 2007). Early detection of a dual diagnosis could facilitate addict treatment plans with primary objective to improve remission rates and mitigate adverse somatic and psychological consequences related to both SUD and psychiatric co-morbidities (Grant et al., 2004; van den Bosch and Verheul, 2007); while an interesting avenue would also be to understand directionality of the coupled disorders in order of influence. A caveat in the current study was the inattention to mood disorders such as major depression which has been intimately linked to SUD and identified as a potent predictor of relapse as demonstrated by Julia Elena Marquez-Arrico, Río-Martínez, Navarro, Prat, and Adan (2019). This could have further facilitated the investigation of co-existing personality and mood disorders in the population of SUD as previously reported by Grilo et al. (1997).
One of the limitations tied to the use of the standardized Rosenberg self-esteem scale was the moderate internal consistency deviating from the normal ranges (Tavakol and Dennick, 2011). Given the demographic profile of the examined sample and past reports of similar reliability values within a population of addict (Xia and Yang, 2019), the moderate strength recorded could be normative of such characteristics. Alternately, data collected through face-to-face interviews may have driven the respondents to portray a better picture of themselves to ‘maintain’ the patient-physician relationship.This could have been curtailed through the local adaptation of the scale favoring self-administration. Lastly, numerous studies have probed into the drug of choice which may influence the latency of SUD generation and dependence; effect which was not accounted for in this study. The treatment profile of the addicts prior to relapse could also be more thoroughly investigated to provide empirical evidence about the success or failures of the current healthcare framework, enabling successful remission through tailored patient recovery-oriented approaches rather than using classical problem-centric measures. It may also prove to be beneficial to understand the sequential transition for one drug to another, ultimately leading to poly-substance consumption given that relapsing from the primary substance used strongly influences the abuse of a secondary substance.
5. Concluding remarks
SUD is a multi-factorial disorder, influenced by the cumulative effect of various intrinsic and extrinsic risk factors. The intrinsic factors are mainly a past history of behavioral disorder and an inner sense of thrill seeking and curiosity, while externally, development of SUD is shadowed by a low socioeconomic status with attributes ranging from low academic performance, low income and unskilled jobs, to family history of SUD, excessive peer pressure from the neighborhood and inadequate social support. Findings also highlighted the harboring of plausible antisocial personality traits perpetuating the addiction among the male addicts. This study has provided an outlook on the major predictors of relapse among Mauritian male addicts, referring mainly to maladaptive coping skills and social pressure as a potent barrier to successful remission. Therefore to increase effectiveness of treatment, programs targeting relapse prevention should be implemented during the first year of abstinence.
Declarations
Author contribution statement
S. Ramsewak: Conceived and designed the experiments, Performed the experiments, Analyzed and interpreted the data, Wrote the paper.
M. Putteeraj: Conceived and designed the experiments, Analyzed and interpreted the data, Wrote the paper.
J. Somanah: Conceived and designed the experiments, Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
We would like to thank Dr Nusrat Jahan Suffee (Dr A.G Jeetoo Hospital), Ms Rachel Shalini Anthony (Brain Research Institute, Monash University Malaysia) and Ms Numrata Moty for their feedback on the research framework.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- Adinoff B., Rilling L.M., Williams M.J., Schreffler E., Schepis T.S., Rosvall T., Rao U. Impulsivity, neural deficits, and the addictions: the "oops" factor in relapse. J. Addict. Dis. 2007;26(Suppl 1):25–39. doi: 10.1300/J069v26S01_04. (0 1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alavi H.R. The role of self-esteem in tendency towards drugs, theft and prostitution. Addiction Health. 2011;3(3-4):119–124. [PMC free article] [PubMed] [Google Scholar]
- Allen J.P., Chango J., Szwedo D., Schad M., Marston E. Predictors of susceptibility to peer influence regarding substance use in adolescence. Child Dev. 2012;83(1):337–350. doi: 10.1111/j.1467-8624.2011.01682.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews J.A., Tildesley E., Hops H., Li F. [Press release]; 2002. The Influence of Peers on Young Adult Substance Use. [DOI] [PubMed] [Google Scholar]
- Bakken I.J., Revdal E., Nesvåg R., Brenner E., Knudsen G.P., Surén P.…Brodtkorb E. Substance use disorders and psychotic disorders in epilepsy: a population-based registry study. Epilepsy Res. 2014;108(8):1435–1443. doi: 10.1016/j.eplepsyres.2014.06.021. [DOI] [PubMed] [Google Scholar]
- Bakken K., Landheim A.S., Vaglum P. Early and late onset groups of substance misusers: differences in primary and secondary psychiatric disorders. J. Subst. Use. 2004;9(5):224–235. [Google Scholar]
- Barrett A., Turner R.J. Family structure and substance use problems in adolescence and early adulthood: examining explanations for the relationship. Soc. Study Addiction. 2004;101:109–120. doi: 10.1111/j.1360-0443.2005.01296.x. [DOI] [PubMed] [Google Scholar]
- Bell R., Garavan H., Foxe J.J. Neural correlates of craving and impulsivity in abstinent former cocaine users: towards biomarkers of relapse risk. Neuropharmacology. 2014;85:461–470. doi: 10.1016/j.neuropharm.2014.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradizza C.M., Stasiewicz P.R., Paas N.D. Relapse to alcohol and drug use among individuals diagnosed with co-occurring mental health and substance use disorders: a review. Clin. Psychol. Rev. 2006;26(2):162–178. doi: 10.1016/j.cpr.2005.11.005. [DOI] [PubMed] [Google Scholar]
- Brown S.A., Vik P.W., Creamer V.A. Characteristics of relapse following adolescent substance abuse treatment. Addict. Behav. 1989;14(3):291–300. doi: 10.1016/0306-4603(89)90060-9. [DOI] [PubMed] [Google Scholar]
- Burleson J.A., Kaminer Y. Self-efficacy as a predictor of treatment outcome in adolescent substance use disorders. Addict. Behav. 2005;30(9):1751–1764. doi: 10.1016/j.addbeh.2005.07.006. [DOI] [PubMed] [Google Scholar]
- Caldwell L.L., Darling N. Leisure context, parental control, and resistance to peer pressure as predictors of adolescent partying and substance use: an ecological perspective. J. Leisure Res. 1999;31(1):57–77. [Google Scholar]
- Capella Mdel M., Benaiges I., Adan A. Neuropsychological performance in polyconsumer men under treatment. Influence of age of onset of substance use. Sci. Rep. 2015;5:12038. doi: 10.1038/srep12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capella M.D.M., Adan A. The age of onset of substance use is related to the coping strategies to deal with treatment in men with substance use disorder. Peer J. 2017;5 doi: 10.7717/peerj.3660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerdá M., Johnson-Lawrence V.D., Galea S. Lifetime income patterns and alcohol consumption: investigating the association between long- and short-term income trajectories and drinking. Soc. Sci. Med. 2011;73(8):1178–1185. doi: 10.1016/j.socscimed.2011.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain S.R., Ioannidis K., Leppink E.W., Niaz F., Redden S.A., Grant J.E. ADHD symptoms in non-treatment seeking young adults: relationship with other forms of impulsivity. CNS Spectr. 2017;22(1):22–30. doi: 10.1017/S1092852915000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chisolm D.J., Kelleher K.J. Admission to acute care hospitals for adolescent substance abuse: a national descriptive analysis. Subst. Abuse Treat. Prev. Pol. 2006;1 doi: 10.1186/1747-597X-1-17. 17-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu M.-L., Cheng C.-F., Liang W.-M., Lin P.-T., Wu T.-N., Chen C.-Y. The temporal relationship between selected mental disorders and substance-related disorders: a nationwide population-based cohort study. Psychiatry J. 2018;2018 doi: 10.1155/2018/5697103. 5697103-5697103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark D.B., Jones B.L., Wood D.S., Cornelius J.R. Substance use disorder trajectory classes: diachronic integration of onset age, severity, and course. Addict. Behav. 2006;31(6):995–1009. doi: 10.1016/j.addbeh.2006.03.016. [DOI] [PubMed] [Google Scholar]
- Clark D.B., Kirisci L., Tarter R.E. Adolescent versus adult onset and the development of substance use disorders in males. Drug Alcohol Depend. 1998;49(2):115–121. doi: 10.1016/s0376-8716(97)00154-3. [DOI] [PubMed] [Google Scholar]
- Cramer P. Identity, personality, and defense mechanisms: an observer-based study. J. Res. Pers. 1997;31(1):58–77. [Google Scholar]
- Cramer P. Understanding defense mechanisms. Psychodyn. Psychiatry. 2015;43(4):523–552. doi: 10.1521/pdps.2015.43.4.523. [DOI] [PubMed] [Google Scholar]
- Daley D.C. Family and social aspects of substance use disorders and treatment. J. Food Drug Anal. 2013;21(4):S73–S76. doi: 10.1016/j.jfda.2013.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deas D., Thomas S.E. An overview of controlled studies of adolescent substance abuse treatment. Am. J. Addict. 2001;10(2):178–189. doi: 10.1080/105504901750227822. [DOI] [PubMed] [Google Scholar]
- Dekkers L.M.S., Bexkens A., Hofman A.D., Boeck P.D., Collot d’Escury A.L., Huizenga H.M. Formal modeling of the resistance to peer influence questionnaire:A comparison of adolescent boys and girls with and without mild-to-borderline intellectual disability. Assessment. 2017 doi: 10.1177/1073191117698754. 1073191117698754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dellabella H. Family history of psychiatric illness increases risk in offspring. Psychiatric advisor. 2018. https://www.psychiatryadvisor.com/bipolar-disorder-advisor/multiple-generation-transmission-liability-psychiatric-illness-offspring-bipolar/article/782537/ Retrieved from.
- DeMilio L. Psychiatric syndromes in adolescent substance abusers. Am. J. Psychiatr. 1989;146(9):1212–1214. doi: 10.1176/ajp.146.9.1212. [DOI] [PubMed] [Google Scholar]
- DiGuiseppi G.T., Meisel M.K., Balestrieri S.G., Ott M.Q., Cox M.J., Clark M.A., Barnett N.P. Resistance to peer influence moderates the relationship between perceived (but not actual) peer norms and binge drinking in a college student social network. Addict. Behav. 2018;80:47–52. doi: 10.1016/j.addbeh.2017.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DSM-V . America: Library of Congress Cataloguing-in- Publication Data; 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Dubey C., Arora M. Sensation seeking level and drug of choice. J. Indian Acad. Appl. Psychol. 2008;34(1):73–82. [Google Scholar]
- Erskine H.E., Moffitt T.E., Copeland W.E., Costello E.J., Ferrari A.J., Patton G.…Scott J.G. A heavy burden on young minds: the global burden of mental and substance use disorders in children and youth. Psychol. Med. 2015;45(7):1551–1563. doi: 10.1017/S0033291714002888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esmaeilian N., Dehghani M., Koster E.H.W., Hoorelbeke K. Early maladaptive schemas and borderline personality disorder features in a nonclinical sample: a network analysis. Clin. Psychol. Psychother. 2019;26(3):388–398. doi: 10.1002/cpp.2360. [DOI] [PubMed] [Google Scholar]
- Evans E.A., Grella C.E., Washington D.L., Upchurch D.M. Gender and race/ethnic differences in the persistence of alcohol, drug, and poly-substance use disorders. Drug Alcohol Depend. 2017;174:128–136. doi: 10.1016/j.drugalcdep.2017.01.021. [DOI] [PubMed] [Google Scholar]
- Fouad Moselhy H., Awara M.A. Chapter 3 - Gateway hypothesis of addiction and substance misuse: the role of neurophysiology and psychological mechanisms. In: Preedy V.R., editor. Neuropathology of Drug Addictions and Substance Misuse. Academic Press; San Diego: 2016. pp. 25–35. [Google Scholar]
- Fox T.P., Oliver G., Ellis S.M. The destructive capacity of drug abuse: an overview exploring the harmful potential of drug abuse both to the individual and to society. ISRN Addiction. 2013;2013:6. doi: 10.1155/2013/450348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein R.B., Grant B.F., Huang B., Smith S.M., Stinson F.S., Dawson D.A., Chou S.P. Lack of remorse in antisocial personality disorder: sociodemographic correlates, symptomatic presentation, and comorbidity with Axis I and Axis II disorders in the National Epidemiologic Survey on Alcohol and Related Conditions. Compr. Psychiatr. 2006;47(4):289–297. doi: 10.1016/j.comppsych.2005.11.002. [DOI] [PubMed] [Google Scholar]
- Gossop M. Drug dependence and self-esteem. Int. J. Addict. 1976;11(5):741–753. doi: 10.3109/10826087609058810. [DOI] [PubMed] [Google Scholar]
- Grant B.F., Stinson F.S., Dawson D.A., Chou S.P., Ruan W.J., Pickering R.P. Co-occurrence of 12-month alcohol and drug use disorders and PersonalityDisorders in the United States: results from the national epidemiologic survey on alcohol and RelatedConditions. Arch. Gen. Psychiatr. 2004;61(4):361–368. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- Grilo C.M., Walker M.L., Becker D.F., Edell W.S., McGlashan T.H. Personality disorders in adolescents with major depression, substance use disorders, and coexisting major depression and substance use disorders. J. Consult. Clin. Psychol. 1997;65(2):328–332. doi: 10.1037//0022-006x.65.2.328. [DOI] [PubMed] [Google Scholar]
- Harstad E., Levy S. Attention-deficit/hyperactivity disorder and substance abuse. Pediatrics. 2014;134(1):e293. doi: 10.1542/peds.2014-0992. [DOI] [PubMed] [Google Scholar]
- Hayaki J., Herman D.S., Hagerty C.E., de Dios M.A., Anderson B.J., Stein M.D. Expectancies and self-efficacy mediate the effects of impulsivity on marijuana use outcomes: an application of the acquired preparedness model. Addict. Behav. 2011;36(4):389–396. doi: 10.1016/j.addbeh.2010.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heidari M., Ghodusi M. Relationship of assess self-esteem and locus of control with quality of life during treatment stages in patients referring to drug addiction rehabilitation centers. Mater. Sociomed. 2016;28(4):263–267. doi: 10.5455/msm.2016.28.263-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemovich V., Crano W.D. Family structure and adolescent drug use: an exploration of single-parent families. Subst. Use Misuse. 2009;44(14):2099–2113. doi: 10.3109/10826080902858375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendershot C.S., Witkiewitz K., George W.H., Marlatt G.A. Relapse prevention for addictive behaviors. Subst. Abuse Treat. Prev. Pol. 2011;6(1):17. doi: 10.1186/1747-597X-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houchins J. Drugabuse.com; 2018. Symptoms and Signs of Drug Abuse.https://drugabuse.com/library/symptoms-and-signs-of-drug-abuse/ 04/05/2018. Retrieved from. [Google Scholar]
- Hyman S.M., Sinha R. Stress-related factors in cannabis use and misuse: implications for prevention and treatment. J. Subst. Abuse Treat. 2009;36(4):400–413. doi: 10.1016/j.jsat.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwanicka K., Gerhant A., Olajossy M. Psychopathological symptoms, defense mechanisms and time perspectives among subjects with alcohol dependence (AD) presenting different patterns of coping with stress. Peer J. 2017;5 doi: 10.7717/peerj.3576. e3576-e3576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahng S., Trull T.J., Wood P.K., Tragesser S.L., Tomko R., Grant J.D.…Sher K.J. Distinguishing general and specific personality disorder features and implications for substance dependence comorbidity. J. Abnorm. Psychol. 2011;120(3):656–669. doi: 10.1037/a0023539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadden R.M., Litt M.D. The role of self-efficacy in the treatment of substance use disorders. Addict. Behav. 2011;36(12):1120–1126. doi: 10.1016/j.addbeh.2011.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassani A., Niazi M., Hassanzadeh J., Menati R. Survival analysis of drug abuse relapse in addiction treatment centers. Int. J. High Risk Behav. Addiction. 2015;4(3) doi: 10.5812/ijhrba.23402. e23402-e23402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Chiu W.T., Demler O., Merikangas K.R., Walters E.E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatr. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khajehdaluee M., Zavar A., Alidoust M., Pourandi R. The relation of self-esteem and illegal drug usage in high school students. Iran. Red Crescent Med. J. 2013;15(11) doi: 10.5812/ircmj.7682. e7682-e7682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan A. 2018. NHS Hospitals Treat Soaring Number of Older People for Drug Misuse the Guardian. 02/12/18. [Google Scholar]
- Korsgaard H.O., Torgersen S., Wentzel-Larsen T., Ulberg R. Substance abuse and personality disorder comorbidity in adolescent outpatients: are girls more severely ill than boys? Child Adolesc. Psychiatr. Ment. Health. 2016;10 doi: 10.1186/s13034-016-0096-5. 8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunreuther E. Autism spectrum disorder and substance use disorder: a dual diagnosis hiding in plain sight. Child Adolescent Psychiatric Clinics of North America. 2020;29(3):467–481. doi: 10.1016/j.chc.2020.03.002. [DOI] [PubMed] [Google Scholar]
- Lander L., Howsare J., Byrne M. The impact of substance use disorders on families and children: from theory to practice. Soc. Work. Publ. Health. 2013;28(3-4):194–205. doi: 10.1080/19371918.2013.759005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavazza A. Free will and neuroscience: from explaining freedom away to new ways of operationalizing and measuring it. Front. Hum. Neurosci. 2016;10 doi: 10.3389/fnhum.2016.00262. 262-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leen L.S. Comission of inquiry on drug trafficking. 2018. https://www.scribd.com/document/384828862/Drogue-voici-le-rapport-de-la-Commission-d-enquete-dans-son-integralite#fullscreen&from_embed Retrieved from.
- Lindsay G.B., Rainey J. Psychosocial and pharmacologic explanations of nicotine's “Gateway drug” function. J. Sch. Health. 1997;67(4):123–126. doi: 10.1111/j.1746-1561.1997.tb03430.x. [DOI] [PubMed] [Google Scholar]
- Long C., DeBeck K., Feng C., Montaner J., Wood E., Kerr T. Income level and drug related harm among people who use injection drugs in a Canadian setting. Int. J. Drug Pol. 2014;25(3):458–464. doi: 10.1016/j.drugpo.2013.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariani J.J., Levin F.R. Treatment strategies for co-occurring ADHD and substance use disorders. Am. J. Addict. 2007;16(Suppl 1):45–54. doi: 10.1080/10550490601082783. quiz 55-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquez-Arrico J.E., Benaiges I., Adan A. Strategies to cope with treatment in substance use disorder male patients with and without schizophrenia. Psychiatr. Res. 2015;228(3):752–759. doi: 10.1016/j.psychres.2015.05.028. [DOI] [PubMed] [Google Scholar]
- Marquez-Arrico J.E., Río-Martínez L., Navarro J.F., Prat G., Adan A. Personality profile and clinical correlates of patients with substance use disorder with and without comorbid depression under treatment. Front. Psychiatr. 2019;9(764) doi: 10.3389/fpsyt.2018.00764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin S., Zabala C., Del-Monte J., Graziani P., Aizpurua E., Barry T.J., Ricarte J. Examining the relationships between impulsivity, aggression, and recidivism for prisoners with antisocial personality disorder. Aggress. Violent Behav. 2019;49:101314. [Google Scholar]
- McGee R.O.B., Williams S. Does low self-esteem predict health compromising behaviours among adolescents? J. Adolesc. 2000;23(5):569–582. doi: 10.1006/jado.2000.0344. [DOI] [PubMed] [Google Scholar]
- McQuown S.C., Belluzzi J.D., Leslie F.M. Low dose nicotine treatment during early adolescence increases subsequent cocaine reward. Neurotoxicol. Teratol. 2007;29(1):66–73. doi: 10.1016/j.ntt.2006.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melemis S.M. Relapse prevention and the five rules of recovery. Yale J. Biol. Med. 2015;88(3):325–332. [PMC free article] [PubMed] [Google Scholar]
- Mennis J., Stahler G.J., Mason M.J. Risky substance use environments and addiction: a new frontier for environmental justice research. Int. J. Environ. Res. Publ. Health. 2016;13(6):607. doi: 10.3390/ijerph13060607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monahan K.C., Steinberg L., Cauffman E. Affiliation with antisocial peers, susceptibility to peer influence, and antisocial behavior during the transition to adulthood. Dev. Psychol. 2009;45(6):1520–1530. doi: 10.1037/a0017417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos R.H., Moos B.S. Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction. 2006;101(2):212–222. doi: 10.1111/j.1360-0443.2006.01310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagelhout G.E., Hummel K., de Goeij M.C.M., de Vries H., Kaner E., Lemmens P. How economic recessions and unemployment affect illegal drug use: a systematic realist literature review. Int. J. Drug Pol. 2017;44:69–83. doi: 10.1016/j.drugpo.2017.03.013. [DOI] [PubMed] [Google Scholar]
- NIDA . National Institute of Drug Abuse; 2018. Is Marijuana a Gateway Drug? June 25. [Google Scholar]
- Njoroge Review on treatment of substance use disorders. J. Addiction Res. Ther. 2018;9(1):353. [Google Scholar]
- Nkansah-Amankra S., Minelli M. Gateway hypothesis" and early drug use: additional findings from tracking a population-based sample of adolescents to adulthood. Preventive Med. Rep. 2016;4:134–141. doi: 10.1016/j.pmedr.2016.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ojo M.A., Akintoyese O., Adenibuyan P., Adegbohun A.A., Abiri K. National Institute on Drug Abuse; 2013. Relationship between Poor Self-Esteem and Adolescent Substance Use.https://www.drugabuse.gov/international/abstracts/relationship-between-poor-self-esteem-adolescent-substance-use Retrieved from. [Google Scholar]
- Oshri A., Carlson M.W., Kwon J.A., Zeichner A., Wickrama K.K.A.S. Developmental growth trajectories of self-esteem in adolescence: associations with child neglect and drug use and abuse in young adulthood. J. Youth Adolesc. 2017;46(1):151–164. doi: 10.1007/s10964-016-0483-5. [DOI] [PubMed] [Google Scholar]
- Parsai M., Voisine S., Marsiglia F.F., Kulis S., Nieri T. The protective and risk effects of parents and peers on substance use, attitudes, and behaviors of Mexican and Mexican American female and male adolescents. Youth Soc. 2008;40(3):353–376. doi: 10.1177/0044118X08318117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pattij T., De Vries T.J. The role of impulsivity in relapse vulnerability. Curr. Opin. Neurobiol. 2013;23(4):700–705. doi: 10.1016/j.conb.2013.01.023. [DOI] [PubMed] [Google Scholar]
- Perry J.L., Carroll M.E. The role of impulsive behavior in drug abuse. Psychopharmacology. 2008;200(1):1–26. doi: 10.1007/s00213-008-1173-0. [DOI] [PubMed] [Google Scholar]
- Poudel A., Gautam S. Age of onset of substance use and psychosocial problems among individuals with substance use disorders. BMC Psychiatr. 2017;17(1) doi: 10.1186/s12888-016-1191-0. 10-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pullen E., Oser C. Barriers to substance abuse treatment in rural and urban communities: a counselor perspective. Subst. Use Misuse. 2014;49(7):891–901. doi: 10.3109/10826084.2014.891615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo D.E., Anderson K.G., Tate S.R., Brown S.A. Characteristics of relapse to substance use in comorbid adolescents. Addict. Behav. 2005;30(9):1811–1823. doi: 10.1016/j.addbeh.2005.07.021. [DOI] [PubMed] [Google Scholar]
- Ramo D.E., Brown S.A. Classes of substance abuse relapse situations: a comparison of adolescents and adults. Psychol. Addict. Behav. 2008;22(3):372–379. doi: 10.1037/0893-164X.22.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson C.G., Ratner P.A., Zumbo B.D. Further support for multidimensionality within the Rosenberg self-esteem scale. Curr. Psychol. 2009;28(2):98–114. [Google Scholar]
- Sadock Benjamin, J, Sadock Virginia., A . Substance-Related Disorders. In: Sadock Virginia., A, editor. Kaplan & Sadock’s Concise Textbook of Clinical Psychiatry. Lippincott Williams & Wilkins; 2004. [Google Scholar]
- SAMHSA . Vol. 39. Center for Substance Abuse Treatment; Rockville: 2004. (Treatment Improvement Protocol). [Google Scholar]
- Schindler A., Thomasius R., Sack P.-M., Gemeinhardt B., KÜStner U., Eckert J. Attachment and substance use disorders: a review of the literature and a study in drug dependent adolescents. Am. J. Bioeth. 2005;7(3):207–228. doi: 10.1080/14616730500173918. [DOI] [PubMed] [Google Scholar]
- Sher K.J., Trull T.J. Substance use disorder and personality disorder. Curr. Psychiatr. Rep. 2002;4(1):25–29. doi: 10.1007/s11920-002-0008-7. [DOI] [PubMed] [Google Scholar]
- Shorey R.C., Anderson S., Stuart G.L. The relation between antisocial and borderline personality symptoms and early maladaptive schemas in a treatment seeking sample of male substance users. Clin. Psychol. Psychother. 2014;21(4):341–351. doi: 10.1002/cpp.1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spooner C. Causes and correlates of adolescent drug abuse and implications for treatment. Drug Alcohol Rev. 1999;18(4):453–475. [Google Scholar]
- Stein J.A., Leslie M.B., Nyamathi A. Relative contributions of parent substance use and childhood maltreatment to chronic homelessness, depression, and substance abuse problems among homeless women: mediating roles of self-esteem and abuse in adulthood. Child Abuse Negl. 2002;26(10):1011–1027. doi: 10.1016/s0145-2134(02)00382-4. [DOI] [PubMed] [Google Scholar]
- Strashny A. 2013. Age of Substance Use Initiation Among Treatment Admissions Aged 18 to 30 the CBHSQ Report; pp. 1–9. Rockville (MD) [PubMed] [Google Scholar]
- Sung M., Erkanli A., Angold A., Costello E.J. Effects of age at first substance use and psychiatric comorbidity on the development of substance use disorders. Drug Alcohol Depend. 2004;75(3):287–299. doi: 10.1016/j.drugalcdep.2004.03.013. [DOI] [PubMed] [Google Scholar]
- Swanepoel I., Geyer S., Crafford G. Risk factors for relapse among young African adults following in-patient treatment for drug abuse in the Gauteng Province. Soc. Work. 2016;52:414–438. [Google Scholar]
- Tavakol M., Dennick R. Making sense of Cronbach's alpha. Int. J. Med. Educ. 2011;2:53–55. doi: 10.5116/ijme.4dfb.8dfd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treger B., Matusiak F., Pilecki M., Rogoz M. The association between self-image and defence mechanisms in a group of adolescent patients receiving psychiatric treatment. Psychiatr. Pol. 2015;49(4):747–756. doi: 10.12740/PP/30017. [DOI] [PubMed] [Google Scholar]
- UNODC . 2010. World Drug Report. Retrieved from. [Google Scholar]
- van den Bosch L.M., Verheul R. Patients with addiction and personality disorder: treatment outcomes and clinical implications. Curr. Opin. Psychiatr. 2007;20(1):67–71. doi: 10.1097/YCO.0b013e328011740c. [DOI] [PubMed] [Google Scholar]
- Veselska Z., Geckova A.M., Orosova O., Gajdosova B., van Dijk J.P., Reijneveld S.A. Self-esteem and resilience: the connection with risky behavior among adolescents. Addict. Behav. 2009;34(3):287–291. doi: 10.1016/j.addbeh.2008.11.005. [DOI] [PubMed] [Google Scholar]
- Vohs K.D., Baumeister R.F. Addiction and free will. Addiction Res. Theor. 2009;17(3):231–235. doi: 10.1080/16066350802567103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward L.C., Rothaus P. The measurement of denial and rationalization in male alcoholics. J. Clin. Psychol. 1991;47(3):465–468. doi: 10.1002/1097-4679(199105)47:3<465::aid-jclp2270470322>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- WHO . Bare Facts; 2017. Substance Abuse.https://afro.who.int/health-topics/substance-abuse Retrieved from. [Google Scholar]
- WHO . Retrieved from; Geneva: 2018. Global Status Report on Alcohol and Health 2018. [Google Scholar]
- Winters K.C., Lee C.-Y.S. Likelihood of developing an alcohol and cannabis use disorder during youth: association with recent use and age. Drug Alcohol Depend. 2008;92(1):239–247. doi: 10.1016/j.drugalcdep.2007.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wongpakaran T., Wongpakaran N. A comparison of reliability and construct validity between the original and revised versions of the Rosenberg Self-Esteem Scale. Psychiatry. Investig. 2012;9(1):54–58. doi: 10.4306/pi.2012.9.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia M., Yang C. The relationship among social support, self-esteem, affect balance and loneliness in individuals with substance use disorders in China. J. Community Psychol. 2019;47(5):1269–1281. doi: 10.1002/jcop.22190. [DOI] [PubMed] [Google Scholar]
- Yang C., Zhou Y., Cao Q., Xia M., An J. The relationship between self-control and self-efficacy among patients with substance use disorders: resilience and self-esteem as mediators. Front. Psychiatr. 2019;10 doi: 10.3389/fpsyt.2019.00388. 388-388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeni N., Tumay F., Tonguç Ö., Azaroğlu E., Bozok N. Survey on smoking, consuming alcohol, and using illicit drugs in patients with epilepsy. Noro psikiyatri arsivi. 2015;52(4):354–358. doi: 10.5152/npa.2015.8772. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.