Abstract
Objectives
The choice of drug treatment in advanced soft tissue sarcoma (STS) continues to be a challenge regarding efficacy, quality of life (QoL) and toxicity. Unlike other cancer types, where integrating patient-reported outcomes (PRO) has proven to be beneficial for QoL, there is no such evidence in patients with STS as of now. The YonLife trial aimed to explore the effect of a tailored multistep intervention on QoL, symptoms and survival in patients with advanced STS undergoing treatment with trabectedin as well as identifying predictors of QoL.
Design
YonLife is a cluster-randomised, open-label, proof-of-concept study. The intervention incorporates electronic PRO assessment, a case vignette and expert-consented treatment recommendations.
Participants
Six hospitals were randomised to the control arm (CA) or interventional arm (IA). Seventy-nine patients were included of whom 40 were analysed as per-protocol analysis set.
Primary and secondary outcome measures
The primary end point was the change of Functional Assessment for Cancer Therapy (FACT-G) total score after 9 weeks. Secondary outcomes included QoL (FACT-G subscales), anorexia and cachexia (Functional Assessment of Anorexia/Cachexia Therapy (FAACT)), symptoms (MD Anderson Symptom Inventory (MDASI)), anxiety and depression (HADS), pain intensity and interference (Brief Pain Inventory (BPI)) and survival assessment.
Results
After 9 weeks of treatment, QoL declined less in the IA (ΔFACT-G total score: −2.4, 95% CI: −9.2 to 4.5) as compared with CA (ΔFACT-G total score: −3.9; 95% CI:−11.3 to 3.5; p=0.765). In almost all FACT-G subscales, average declines were lower in IA, but without reaching statistical significance. Smaller adverse trends between arms were observed for MDASI, FAACT, HADS and BPI scales. These trends failed to reach statistical significance. Overall mean survival was longer in IA (648 days) than in CA (389 days, p=0.110). QoL was predicted by symptom severity, symptom interference, depression and anxiety.
Conclusion
Our data suggest a potentially favourable effect of an electronic patient-reported outcomes based intervention on QoL that needs to be reappraised in confirmatory studies.
Trial registration number
ClinicalTrials.gov Identifier (NCT02204111).
Keywords: sarcoma, quality in healthcare, cancer pain
Strengths and limitations of this study.
YonLife explores the value and efficacy of a patient-directed intervention on quality of life in sarcoma patients.
YonLife captures patient-reported outcomes electronically and provides a tailored expert-derived intervention in a multicentre setting.
Effect sizes are now available for conducting confirmatory trials to examine the YonLife results.
Introduction
The armamentarium of systemic treatment in advanced soft tissue sarcoma (STS) has evolved over the past decade. Yet, the burden of disease remains high and drug-related adverse events are frequent,1–3 even in patients who experience long-lasting clinical benefit. Overall, quality of life (QoL) in sarcoma patients is more impaired than in the general population,2 4 but comparable with patients with more frequent cancer diseases.5 Mental health problems such as distress, depression and anxiety are as frequent as in other cancer patients.6 7
Treatment algorithms for STS beyond first-line treatment do not show superiority between one regimen and another.8 On the other hand, there are distinct and drug-specific side effects. Therefore, the choice of which regimen should be applied becomes a matter of debate within the patient–doctor consultation with considerations comprising preferences and personal beliefs.9 Consequently, it is important to assess the treatment effectiveness in two ways. First, in terms of tumour burden as an outcome (eg, progression-free survival (PFS) or overall survival (OS)), and, second, in terms of symptoms and toxicities as assessed by patient-reported outcomes (PRO). As an individual might experience improvement in symptoms while a treatment is not superior on a group level, appropriate strategies to evaluate the individual patient benefit need to be applied. Especially, if there is no superiority in survival, further outcomes should be considered, such as evaluation of minimal clinical important difference (MCID) or the time to deterioration of QoL.10
Trabectedin (Yondelis) is a semisynthetic drug originally isolated from the sea squirt Ecteinascidia turbinata with a complex multimodal mechanism of action.11 12 Trabectedin was the first marine-derived antineoplastic drug approved in 2007 in the European Union and in over 70 countries across the globe for the treatment of patients with advanced STS after failure of anthracyclines and ifosfamide, or who are unsuited to receive these agents.13 In 2015, trabectedin was also approved in the USA based on a pivotal phase III trial, which demonstrated that trabectedin had a significantly longer PFS compared with dacarbazine in patients with advanced liposarcoma or leiomyosarcoma after failure of prior chemotherapy.14 Noteworthy, an ad hoc analysis of the phase III trial, which compared inpatient with outpatient infusion of trabectedin, showed that safety, efficacy and PRO outcomes were comparable between both treatment settings.15 In addition, an analysis of the MD Anderson Symptom Inventory (MDASI) PRO scores reported no clinically meaningful differences among patients reporting severe symptoms (MDASI score ≥7) who were treated with trabectedin in either an inpatient or outpatient treatment settings.15
Assessment and interventions based on PRO have been proven to yield beneficial outcomes in various settings and entities.16–21 For instance, Basch et al found benefits of their Symptom Tracking and Reporting (STAR) intervention in prolonging time on chemotherapy, less unexpected admissions and longer quality-adjusted survival.17 In brief, they randomised 766 patients from a single institution under chemotherapy for solid tumours to either usual care or STAR. The intervention consisted of 12 different symptoms collected remotely, providing treating physicians with graphical representations of results and alerting nurses when a preset cut-off of worsening condition was met. Another randomised multicentre trial evaluated the effect of a web-based, self-reported assessment and educational intervention on symptom distress during cancer therapy in 752 ambulatory patients from different entities and with various diagnoses.18 In this multicentre sample of participants they reported that web-based patients-rated symptoms and communication coaching reduced symptom distress after active cancer treatment, particularly in those aged >50 years. Nevertheless, PRO assessment in patients treated for STS struggle with serious barriers such as a relatively small patient population and the fact that no STS-specific QoL or symptom questionnaires are available.4 22 Considering that merely assessing PRO might not be beneficial,23 we believe that it should be accompanied by additional interventions such as nurse-led patient education, self-care support or a multiprofessional expert panel that discusses PRO results and derives treatment recommendations.24 Despite the increasing knowledge on benefits and assessment of PRO in general and the high symptom-burden of patients suffering from advanced STS, the proof of concept for such interventions remains open. Therefore, the cluster-randomised YonLife study was designed to evaluate the value and efficacy of a tailored, patient-directed palliative intervention based on various domains of QoL and to explore effect sizes using different PRO instruments in patients with advanced STS undergoing treatment with trabectedin.
Methods
Patients
Adult patients (≥18 years) suffering from advanced or metastatic STS who had received at least one dose of trabectedin 1.5 mg/m², given as a 24-hour intravenous infusion every 3 weeks, were included in this study. Physician-assessed life expectancy of patients had to be at least 6 months and Eastern Cooperative Oncology Group (ECOG) performance status score had to be ≤2.
Patient and public involvement
We are grateful to all patients who participated in the YonLife trial. A member of the national sarcoma patient advocacy group ‘Das Lebenhaus’ took part in the expert panel discussion.
Trial design and objectives
Full details of YonLife trial (ClinicalTrials.gov Identifier: NCT02204111) have been reported.25 Briefly, the YonLife trial was designed as a cluster-randomised, explorative, open-label, non-blinded, proof-of-concept study with the aim to compare the overall QoL between patients with STS receiving a multidimensional intervention, on the basis of patients’ individual PROs, and those patients receiving usual supportive treatment. Outcomes were assessed at baseline (ie, visit (V) 1) and after 3 (V2), 6 (V3) and 9 (V4) weeks. Follow-up was conducted 21 (V5), 35 (V6) and 61 (V7) weeks after baseline. Primary objective was the explorative comparison of QoL change after 9 weeks (V4) between interventional arm and control arm. Secondary objectives included explorative comparison between other PROs such as anxiety, depression, pain as well as survival. Furthermore, factors that predict QoL after 9 weeks were explored.
Intervention
Patients in the control arm (CA) received only electronic PRO assessment without feedback to the treatment team. Patients treated in the interventional arm (IA) received a comprehensive four-step evaluation comprising: (1) PROs were assessed electronically via handheld tablet PCs at each visit; (2) a case vignette was created based on the obtained PRO and clinical data at baseline; (3) supportive care recommendations were consented during discussion on patients’ vignettes in a multiprofessional expert panel and (4) these treatment suggestions as well as graphical representation of obtained PRO were provided to the treating physicians prior to V2 in the interventional centre. Clinicians in the IA had the opportunity to discuss the graphical presentation with their patients and initiate the treatment suggestions. The expert panel consisted of experts in the field of oncology, palliative care, social work, nursing, psycho-oncology as well as a patient advocate.
Randomisation
Six German centres were cluster-randomised in a 1:1 ratio in an IA (three centres) and a CA (three centres). This trial was designed as a cluster-randomised trials to avoid contamination that might result in a type 2 error. If randomised on patient level, contamination might have been occurred as patients talked to each other about the recommendations or the treating physician-transferred recommendations from one patient to another. Randomisation was conducted by a colleague not actively involved in this trial using random numbers generated in excel.
The seventh centre where the supportive care recommendations were created served as a reference centre (RC). Patients treated at the RC received the same intervention as in the IA but they were analysed separately. The RC was invented to avoid bias from a dual role of participating clinicians as being part of treatment staff in the centre and taking part in the expert panel at the same time. Furthermore, we initiated the RC at first centre to get to know and solve any technical or logistical barriers in a monocentre setting before spreading it to a multicentre setting.
Outcome measures
The primary outcome explored the changes of patients QoL in IA and CA after 9 weeks of treatment as measured with the Functional Assessment for Cancer Therapy (FACT-G) total score. Nine weeks was set as time for primary outcome assessment since this period provides enough time to take action concerning interventional proposals. The FACT-G is a PRO measure used to assess health-related QoL in patients undergoing cancer therapy as a total sum score (ranging from 0 to 108) comprising four subscales of QoL (physical, social, emotional and functional well-being).26 Furthermore, we evaluated the number of patients with a clinical improvement between V1 and V4. This equals a change in the FACT-G total score of at least 3.3 points to represent a MCID. Additionally, the time until QoL deterioration (TUD) was also assessed as a change of at least 3.3 points between V1 and V4 as defined by King et al.27 Analyses of long-term effects included the data collected from V1 until the end of the study at week 67 (V7). Visit schedule and outcomes of all secondary end points measured throughout the study are depicted in table 1.
Table 1.
Visit schedule and outcomes
| Study period | Baseline | Intervention phase | Follow-up phase | ||||
| Visit | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Week (±3 days) | 0 | 3 | 6 | 9 | |||
| Week (±1 week) | 21 | 35 | 61 | ||||
| Concomitant medication | x | x | x | x | x | x | x |
| FACT-G | x | x | x | x | x | x | x |
| MDASI | x | x | x | x | x | x | x |
| FAACT | x | x | x | x | x | ||
| BPI | x | x | x | x | x | ||
| IN-PATSAT32* | x | x | x | x | x | ||
| HADS | x | x | x | x | x | ||
| Tumour-specific and socio-demographic parameters | x | x | x | x | x | ||
| Feasibility scoring based on patients’ and doctors’ opinion* | x | ||||||
*Data are currently being analysed and are available on request.
BPI, Brief Pain Inventory; FAACT, Functional Assessment of Anorexia/Cachexia Therapy; FACT-G, Functional Assessment for Cancer Therapy; HADS, Hospital Anxiety and Depression Scale; IN-PATSAT32, Satisfaction with In-Patient Cancer Care; MDASI, MD Anderson Symptom Inventory.
Secondary outcomes included the subscales of the FACT-G questionnaire: physical (range: 0–28), emotional (range: 0–24), functional (range: 0–28) and social well-being (range: 0–28) explored at V4 and during follow-up (ie, V7).24 Moreover, the effect size of the intervention was measured as Cohen’s d.28 The MDASI was used to measure the severity of 13 cancer-related symptoms and their impact on six dimensions of daily life.29 Psychological distress was evaluated by the Hospital Anxiety and Depression Scale (HADS).30 It provided a total sum score (range: 0–42) and two self-rating subscales for anxiety and depression (range: 0–21). HADS also identified clinically relevant cases of anxiety and depression using predetermined cut-off scores.31 The Functional Assessment of Anorexia/Cachexia Therapy (FAACT) questionnaire measured the impact of cachexia and anorexia on patients’ QoL.32 Finally, the Brief Pain Inventory (BPI) in a scale range from 0 to 10 measured the intensity of pain and pain-related interference.33 We assessed the predictive value of the following variables at V1 for QoL: gender, age, performance status (ECOG), tumour stage (UICC classification), symptom severity (MDASI), symptom interference (MDASI), depression (HADS), anxiety (HADS), patients’ satisfaction (IN-PATSAT32)34 and anorexia/cachexia (FAACT).
Statistical considerations
The patients sample size was calculated for an explorative purpose. We assumed the superiority of our intervention concerning FACT-G total score. Type I error was set to α=0.05 (one-sided), with a statistical power of 1−β=0.80 and a medium effect27 between the groups in FACT-G=15, with an estimated SD of σ=17 and a conservatively estimated intracluster correlation coefficient of p=0.10.35 This calculation resulted in a cluster size of 11 patients. Additionally, 11 patients were recruited in the RC, for a total of 77 patients.
The full analysis set (FAS) comprised all patients included in the study and allocated to a treatment group irrespective of their compliance with the planned course of treatment (intention-to-treat principle). Analyses of efficacy end points were performed on the per-protocol analysis set (PPS) defined as the subset of patients of the FAS who have provided complete data at the first (V1) and last (V4) visits and who had no major protocol deviations.
Survival was assessed as means of PFS and OS. The PFS and OS analyses were defined as the time interval from the first administration of trabectedin to the earliest date of disease progression or death, regardless of cause (whichever occurred first) for PFS, whereas OS was defined as the time between the start of trabectedin and patient death from any cause. Patients were censored after the discontinuation of their study participation. Means of PFS and OS are reported to provide the ability to describe and compare the arms, as median value of OS is not defined for CI within the observation period of this study. Mann-Whitney U test, Fisher exact test and χ2 test were used for the detection of possible differences concerning demographics. The t-test was applied to detect possible differences between metric outcomes, whereas linear univariate and multivariate regression were calculated to identify determinants of QoL at V4.
Results
Patients and treatment arms
Between September 2014 and March 2018, 80 patients from 7 sites were screened for study participation (figure 1). The FAS encompasses 79 patients, as 1 patient had to be excluded from analysis due to protocol violation. In the FAS, mean age was 58 years (range: 22–86). Leiomyosarcoma (n=32) and liposarcoma (n=23) were the most prevalent histological type of sarcomas. At baseline, the IA included 38 patients (19 of whom included in PPS), while CA consisted of 29 patients (14 of whom included in PPS). No difference concerning age, gender and the number of previous cycles of trabectedin was observed between the arms. In the CA, more patients had a higher tumour stage (p=0.083) and less patients suffer from leiomyosarcoma (table 2).
Figure 1.
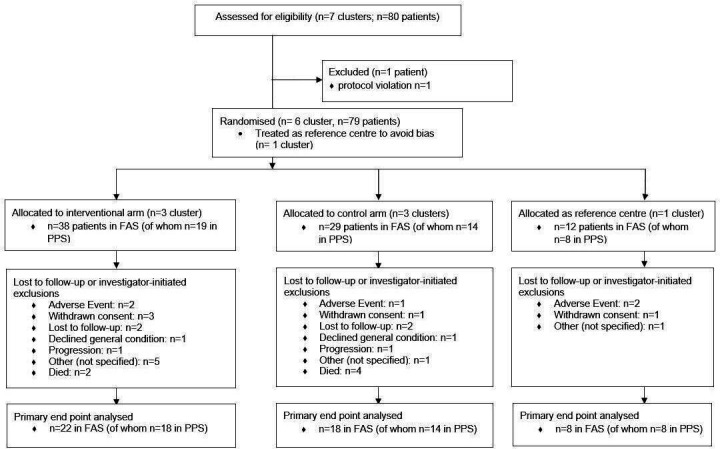
CONSORT flow chart. FAS, full analysis set; PPS, per-protocol analysis set.
Table 2.
Patient characteristic at baseline
| IA (3 centres), N=38 | CA (3 centres), N=29 | RC (1 centre), N=12 | FAS, N=79 | |
| FAS | ||||
| Gender | ||||
| Male | 20 | 15 | 6 | 41 |
| Female | 18 | 14 | 6 | 38 |
| Age | ||||
| Mean (SD) | 58 (12) | 56 (15) | 63 (16) | 58 (14) |
| Range (years) | 38–87 | 22–80 | 34–82 | 22–87 |
| Tumour histology | ||||
| Leiomyosarcoma | 19 | 5 | 5 | 29 |
| Liposarcoma | 6 | 11 | 3 | 20 |
| Others* | 13 | 12 | 4 | 29 |
| Missing | 0 | 1 | 0 | 1 |
| Metastatic disease | ||||
| M0 | 16 | 11 | 5 | 32 |
| M1 | 12 | 16 | 7 | 35 |
| Missing | 10 | 2 | 0 | 12 |
| ECOG PS | ||||
| 0 | 20 | 14 | 5 | 39 |
| 1 | 15 | 13 | 7 | 35 |
| 2 | 3 | 0 | 0 | 3 |
| Missing | 0 | 2 | 0 | 2 |
| Number of previous cycles of trabectedin | ||||
| Median | 0 | 1 | 1 | 1 |
| Range | 0–15 | 0–17 | 0–11 | 0–17 |
| Number of previous cycles of another chemotherapy | ||||
| Median | 1.5 | 1 | 2 | 2 |
| Range | 0–6 | 0–5 | 1–4 | 0–6 |
| Number of previous lines of another chemotherapy | ||||
| Median | 2.5 | 2.5 | 3 | 2 |
| Range | 0–6 | 0–6 | 2–5 | 0–6 |
| IA (3 centres), N=19 | CA (3 centres), N=14 | RC (1 centre), N=8 | PPS, N=41 | |
| PPS | ||||
| Gender | ||||
| Male | 8 | 6 | 3 | 17 |
| Female | 11 | 8 | 5 | 24 |
| Age | ||||
| Mean (SD) | 61 (12) | 55 (15) | 59 (17) | 58 (14) |
| Range (years) | 44–87 | 30–80 | 34–82 | 30–87 |
| Tumour histology | ||||
| Leiomyosarcoma | 5 | 6 | 4 | 15 |
| Liposarcoma | 11 | 1 | 3 | 15 |
| Others* | 3 | 7 | 1 | 11 |
| Missing | 0 | 0 | 0 | 0 |
| Metastatic disease | ||||
| M0 | 8 | 5 | 2 | 15 |
| M1 | 5 | 9 | 6 | 20 |
| Missing | 6 | 0 | 0 | 6 |
| ECOG PS | ||||
| 0 | 12 | 8 | 4 | 24 |
| 1 | 6 | 6 | 4 | 16 |
| 2 | 1 | 0 | 0 | 1 |
| Missing | 0 | 0 | 0 | 0 |
| Number of previous cycles of trabectedin | ||||
| Median | 0 | 1 | 1 | 1 |
| Range | 0–15 | 0–7 | 1–11 | 0–15 |
| Number of previous cycles of another chemotherapy | ||||
| Median | 1 | 1 | 2 | 2 |
| Range | 0–4 | 0–3 | 2–4 | 0–4 |
*All subtypes occurring less than four times were merged into this category.
CA, control arm; ECOG PS, Eastern Cooperative Oncology Group performance status; FAS, full analysis set; IA, interventional arm; M0, no distant metastasis; M1, distant metastasis; PPS, per-protocol analysis set; RC, reference centre.
Primary outcome
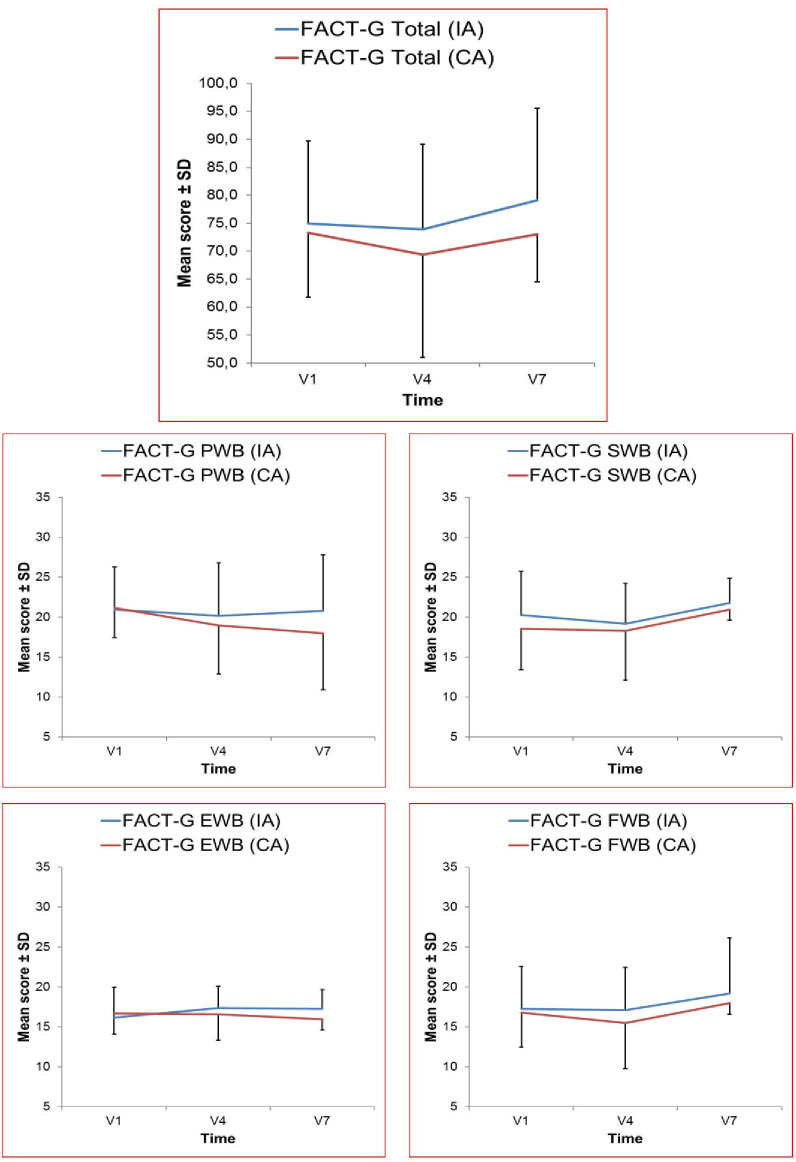
After 9 weeks at V4, FACT-G declined less in IA (Δ FACT-G total score: −2.4, 95% CI: −9.2 to 4.5) as compared with the CA (Δ FACT-G total score: −3.9, 95% CI: −11.3 to 3.5; p=0.765) (table 3). The effect size of the intervention on the FACT-G score was d=0.269 (small effect). Intracluster correlation was 0. Figure 2 and online supplementary table 1 depicts absolute FACT scores trajectories over time. The number of patients experiencing a MCID was equal in both groups (IA: 44% and CA: 43%). The median TUD differed slightly between IA (25 days, 95% CI: 6.2 to 43.8) and CA (22 days, 95% CI: 16.5 to 27.5; p=0.927).
Table 3.
Change scores after 9 weeks of treatment
| Mean change from baseline (V1) to 9 weeks (V4) | ||||||||
| Interventional arm | Control arm | P value | Interventional trend | |||||
| Mean | 95% CI | N | Mean | 95% CI | N | |||
| FACT-G total | −2.4 | −9.2 to 4.5 | 18 | −3.9 | −11.3 to 3.5 | 14 | 0.765 | Beneficial |
| FACT-G physical well-being | −1.2 | −4.4 to 2.1 | 18 | −2.2 | −5.4 to 1.0 | 14 | 0.722 | Beneficial |
| FACT-G social well-being | −1.6 | −3.1 to −0.1 | 18 | −0.2 | −2.2 to 1.7 | 14 | 0.193 | Adverse |
| FACT-G emotional well-being | 0.9 | −0.6 to 2.4 | 18 | −0.1 | −2.3 to 2.1 | 14 | 0.561 | Beneficial |
| FACT-G functional well-being | −0.5 | −2.7 to 1.7 | 18 | −1.3 | −4.0 to 1.4 | 14 | 0.536 | Beneficial |
| HADS depression | 0.3 | −0.6 to 1.2 | 18 | 0.2 | −2.1 to 2.5 | 14 | 0.419 | Equivalent |
| HADS anxiety | 0.3 | −1.7 to 2.2 | 18 | −0.8 | −3.0 to 1.4 | 14 | 0.710 | Adverse |
| BPI average pain | 0.6 | −0.3 to 1.5 | 19 | 0.2 | −0.5 to 1.0 | 14 | 0.788 | Adverse |
| BPI pain interference | 0.4 | −0.3 to 1.1 | 18 | 0.1 | −0.5 to 0.7 | 13 | 0.679 | Adverse |
| MDASI symptom severity | 0.7 | −0.1 to 1.4 | 18 | 0.2 | −0.4 to 0.8 | 14 | 0.442 | Adverse |
| MDASI symptom interference | 1.2 | 0.9 to 1.6 | 18 | 0.8 | −0.4 to 1.9 | 13 | 0.667 | Adverse |
BPI, Brief Pain Inventory; FACT-G, Functional Assessment for Cancer Therapy; HADS, Hospital Anxiety and Depression Scale; MDASI, MD Anderson Symptom Inventory; N, number of evaluable patients in respective cluster; V, visit.
Figure 2.
Absolute FACT scores at baseline (V1), after 9 weeks of treatment (V4; primary end point) and during follow-up visit (V7). Number of evaluated patients for all FACT-G dimensions per visit and cohort: V1: IA, N=19, CA, N=14; V4: IA, N=18, CA, N=14; V7: IA, N=9, CA, N=2. CA, control arm; EWB, emotional well-being; FACT-G, Functional Assessment for Cancer Therapy; FWB, functional well-being; IA, interventional arm; PWB, physical well-being; SWB, social well-being; V, visit.
bmjopen-2019-035546supp001.pdf (68.9KB, pdf)
Secondary outcomes
Regarding the change of QoL between V1 and V4 (as well as during follow-up V7), there was a beneficial impact of the patient-tailored intervention in IA in all FACT-G subscales except for social well-being (figure 2). There was less decline in physical well-being subscale in IA (ΔFACT-G PWB: −1.2, 95% CI: −4.4 to 2.1) than in CA (ΔFACT-G PWB: −2.2, 95% CI: −5.4 to 1.0; p=0.926). Emotional well-being subscale improved slightly in IA (ΔFACT-G EWB: 0.9, 95% CI: −0.6 to 2.4) and remained almost stable in CA (ΔFACT-G EWB: −0.1, 95% CI: −2.3 to 2.1; p=0.561). Functional well-being subscale declined less in IA (ΔFACT-G FWB: −0.5, 95% CI: −2.7 to 1.7) than in CA (ΔFACT-G FWB: −1.3, 95% CI: −4.0 to 1.4; p=0.536). Lastly, social well-being subscale remained almost stable (ΔFACT-G SWB: −0.2, 95% CI: −2.2 to 1.7) in CA while decreasing in IA (ΔFACT-G SWB: −1.6, 95% CI: −3.1 to −0.1; p=0.952). Overall, there were non-significant, adverse trends in other domains of PRO (MDASI, FAACT, HADS and BPI scales) (table 3 and online supplementary table 2).
bmjopen-2019-035546supp002.pdf (67.3KB, pdf)
Overall mean OS was longer in IA than in CA (648 vs 389 days) without reaching statistical significance (p=0.110), while means of PFS were almost identical in IA and CA (249 vs 232 days; p=0.899).
QoL prediction
Univariate regressions revealed that each of the following variables determined the FACT-G total score: symptom severity, symptom interference, depression and anxiety. No influence on the FACT-G total score was found for age, gender, ECOG performance status, patient satisfaction, tumour stage, anorexia and cachexia (table 4). In a multivariable regression, depression determines the FACT-G total score (table 4).
Table 4.
Univariate and multiple regression of FACT-G total score after 9 weeks (V4) on parameters measured at baseline (V1) over all groups
| P value | Estimate | 95% CI | |
| Univariate regression | |||
| Gender | 0.154 | 7.5 | −2.8 to 17.8 |
| Age | 0.228 | −0.2 | −0.5 to 0.1 |
| ECOG PS | 0.509 | −3.2 | −12.7 to 6.3 |
| Tumour stage | 0.284 | −1.8 | −5.1 to 1.5 |
| Symptom severity | 0.0 | −6.6 | −10.5 to −2.7 |
| Symptom interference | 0.011 | −3.4 | −6.0 to −0.8 |
| Depression | 0.0 | −2.7 | −4.3 to −1.1 |
| Anxiety | 0.034 | −1.4 | −2.7 to −0.1 |
| Patient satisfaction | 0.451 | 3.0 | −4.8 to 10.8 |
| Anorexia/cachexia | 0.143 | 0.8 | −0.3 to 1.9 |
| Multiple regression | |||
| Gender | 0.844 | 1.0 | −7.2 to 9.4 |
| Age | 0.103 | −0.3 | −0.6 to 0.1 |
| ECOG PS | 0.746 | 1.5 | −6.1 to 9.1 |
| Tumour stage | 0.586 | −0.8 | −3.4 to 1.7 |
| Symptom severity | 0.079 | −4.4 | −8.3 to −0.2 |
| Symptom interference | 0.744 | 0.5 | −1.8 to 2.8 |
| Depression | 0.025 | −2.2 | −3.9 to −0.7 |
| Anxiety | 0.869 | −0.1 | −1.5 to 1.3 |
| Patient satisfaction | 0.437 | −0.1 | −0.4 to 0.1 |
| Anorexia/cachexia | 0.161 | −0.9 | −2.0 to 0.2 |
ECOG PS, Eastern Cooperative Oncology Group performance status; FACT-G, Functional Assessment for Cancer Therapy.
Discussion
Principal findings
To the best of our knowledge, this is the first randomised trial using a patient-directed supportive care intervention to improve QoL and other PRO in sarcoma patients. We observed a trend in favour of the intervention, considering the primary end point (total FACT-G score) and other secondary outcomes (ie, physical, functional and emotional well-being QoL subscales). On the other side, MCID and TUD assessments slightly differed between the arms. Not surprisingly and due to the character of palliative disease, absolute numbers in FACT-G score decline over time. This change is well in line with findings from a multicentre randomised trial, which reported a comparable decline in FACT-G score of ~2 in 281 patients suffering from advanced solid cancers who received early palliative care or standard oncological care.36 In addition, the total FACT-G score they observed after 12 weeks (70.1 and 69.6) was comparable with the score found in IA (73.9) and CA (69.4) after 9 weeks of treatment. The total FACT-G score (76.4) was also comparable with the YonLife baseline score (74.2) in a sample of 42 patients suffering from different sarcoma histotypes in a single-centre, cross-sectional study.37
As the intervention appears to be favourable on QoL (without reaching statistical significance), it seemed adverse on symptom domains such as average pain, as well as anxiety and depression. For the former, the applied intervention might not have been timely enough, as adequate pain management needs immediate action instead of recommendation that takes several days. Complex syndromes such as anxiety and depression need ongoing treatment, either psycho-oncological or pharmaceutical, which usually takes more time to be effective.
YonLife intervention—unanswered questions and future research
There are still many unanswered questions regarding comprehensive QoL interventions. During the past years, several reports with different interventions tried to shed some more light on this issue. The YonLife intervention incorporates aspects of other programmes such as providing treating physician with precollected PROs17 24 and creating a QoL profile and using expert’s recommendations.19 In contrast, unlike recently evolving programmes,38 YonLife did not provide the possibility to answer questions using web-based questionnaires accessible from home or mobile device. Furthermore, the PRO results were automatically calculated, but they were not automatically compared with predefined cut-off or norm data nor were they available in the clinic information system like in other projects.39 40 Thus, the described YonLife intervention needed human support to create the case vignette that limits the application to busy clinical routine. Advancing technical opportunities could help overcoming these barriers. YonLife also provided recommendations thoroughly based on electronic capturing of PRO. Yet, it demonstrated to be beneficial on QoL in contrast to a palliative intervention based on the personal encounter.36 This could be even more relevant in a rare disease such as sarcoma care, where patients regularly travel long distances to specialised sarcoma centres.
Weaknesses and strengths
Our study has several limitations. As no preceding studies that incorporate a PRO-based individualised intervention existed, our study design and the sample size were set only for an explorative purpose. Therefore, results were determined to fail statistical significance and should be interpreted with caution. Furthermore, sarcoma-specific QoL or symptom measures are still missing, while the FACT-G and MDASI are generic instruments, which might not cover syndromes and aspects specific for sarcoma patients. On the other hand, to overcome the obstacles of limited statistical power, we applied measures of clinical rather than statistical importance such as the MCID or TUD, which might be even more important to clinicians in daily practice. Effect sizes are currently available for calculating sample sizes in a larger confirmatory trial.
In conclusion, the YonLife trial adds essential knowledge to the scarce data on PRO in patients with advanced STS. Unlike previous work, it is the first trial that applies an electronic PRO assessment and a remote tailored intervention of patients with STS. Our data suggest that incorporation of validated QoL measures in STS clinical treatment may further improve the care and understanding of patient well-being beyond traditional clinical measures. Additionally, beyond proving the statistical significance of clinically important effects, this study is an important prerequisite for future research and holistic care of patients with advanced STS.
Supplementary Material
Acknowledgments
The trial was coordinated by GWT-TUD, Dresden, Germany. We acknowledge the German Interdisciplinary Sarcoma Group (GISG) for providing support for this trial. The YonLife trial was associated with the German Interdisciplinary Sarcoma Group as GISG-12 project and as AIO-STS-0215 within the ‘Arbeitsgemeinschaft Internistische Onkologie’ of the ‘Deutsche Krebsgesellschaft’ (DKG). We would also like to thank Michael Kramer, Kristian Zinke and Rocco Haase for their support on statistical aspects of the study and Felicitas Lenz and Adnan Tanović for proof-reading.
Footnotes
Contributors: LH and MKS proposed the conception and design of the study, performed data analysis, interpretation and quality control of data and algorithms. MB, LH and MKS are responsible for the manuscript editing. MKS, SR, H-GK, BK, AK, VG, TK, UP and JMC performed the data acquisition. All aforementioned authors as well as US, JF, AS, BH and KA participated in the manuscript drafting and review with equal contribution.
Funding: This work was supported by an unrestricted grant from PharmaMar, Spain.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: All study procedures were conducted in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments. The YonLife trial was approved by the Ethics Committee of the University Hospital Carl Gustav Carus in Dresden on June 2014 (EK241062014), and all participating centres obtained the approval of the local ethics committee before patient enrolment. All patients provided written informed consent before inclusion in the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request from corresponding author.
References
- 1.Gough NJ, Smith C, Ross JR, et al. Symptom burden, survival and palliative care in advanced soft tissue sarcoma. Sarcoma 2011;2011:1–8. 10.1155/2011/325189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reichardt P, Leahy M, Garcia Del Muro X, et al. Quality of life and utility in patients with metastatic soft tissue and bone sarcoma: the sarcoma treatment and burden of illness in North America and Europe (sabine) study. Sarcoma 2012;2012:1–11. 10.1155/2012/740279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Storey L, Fern LA, Martins A, et al. A critical review of the impact of sarcoma on psychosocial wellbeing. Sarcoma 2019;2019:1–18. 10.1155/2019/9730867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McDonough J, Eliott J, Neuhaus S, et al. Health-related quality of life, psychosocial functioning, and unmet health needs in patients with sarcoma: a systematic review. Psychooncology 2019;28:653–64. 10.1002/pon.5007 [DOI] [PubMed] [Google Scholar]
- 5.Ostacoli L, Saini A, Zuffranieri M, et al. Quality of life, anxiety and depression in soft tissue sarcomas as compared to more common tumours: an observational study. Appl Res Qual Life 2014;9:123–31. 10.1007/s11482-013-9213-2 [DOI] [Google Scholar]
- 6.Tang MH, Pan DJW, Castle DJ, et al. A systematic review of the recent quality of life studies in adult extremity sarcoma survivors. Sarcoma 2012;2012:1–15. 10.1155/2012/171342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paredes T, Pereira M, Moreira H, et al. Quality of life of sarcoma patients from diagnosis to treatments: predictors and longitudinal trajectories. Eur J Oncol Nurs 2011;15:492–9. 10.1016/j.ejon.2011.01.001 [DOI] [PubMed] [Google Scholar]
- 8.Casali PG, Abecassis N, Aro HT, et al. Soft tissue and visceral sarcomas: ESMO-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 2018;29:iv268–9. 10.1093/annonc/mdy321 [DOI] [PubMed] [Google Scholar]
- 9.Blay J-Y, Sleijfer S, Schöffski P, et al. International expert opinion on patient-tailored management of soft tissue sarcomas. Eur J Cancer 2014;50:679–89. 10.1016/j.ejca.2013.11.011 [DOI] [PubMed] [Google Scholar]
- 10.Bonnetain F, Dahan L, Maillard E, et al. Time until definitive quality of life score deterioration as a means of longitudinal analysis for treatment trials in patients with metastatic pancreatic adenocarcinoma. Eur J Cancer 2010;46:2753–62. 10.1016/j.ejca.2010.07.023 [DOI] [PubMed] [Google Scholar]
- 11.D'Incalci M, Erba E, Damia G, et al. Unique features of the mode of action of ET-743. Oncologist 2002;7:210–6. 10.1634/theoncologist.7-3-210 [DOI] [PubMed] [Google Scholar]
- 12.Larsen AK, Galmarini CM, D'Incalci M. Unique features of trabectedin mechanism of action. Cancer Chemother Pharmacol 2016;77:663–71. 10.1007/s00280-015-2918-1 [DOI] [PubMed] [Google Scholar]
- 13.Demetri GD, Chawla SP, von Mehren M, et al. Efficacy and safety of trabectedin in patients with advanced or metastatic liposarcoma or leiomyosarcoma after failure of prior anthracyclines and ifosfamide: results of a randomized phase II study of two different schedules. J Clin Oncol 2009;27:4188–96. 10.1200/JCO.2008.21.0088 [DOI] [PubMed] [Google Scholar]
- 14.Demetri GD, von Mehren M, Jones RL, et al. Efficacy and safety of trabectedin or dacarbazine for metastatic liposarcoma or leiomyosarcoma after failure of conventional chemotherapy: results of a phase III randomized multicenter clinical trial. J Clin Oncol 2016;34:786–93. 10.1200/JCO.2015.62.4734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones RL, Maki RG, Patel SR, et al. Safety and efficacy of trabectedin when administered in the inpatient versus outpatient setting: clinical considerations for outpatient administration of trabectedin. Cancer 2019;125:4435–41. 10.1002/cncr.32462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Basch E, Deal AM, Dueck AC, et al. Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. JAMA 2017;318:197–8. 10.1001/jama.2017.7156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Basch E, Deal AM, Kris MG, et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol 2016;34:557–65. 10.1200/JCO.2015.63.0830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berry DL, Hong F, Halpenny B, et al. Electronic self-report assessment for cancer and self-care support: results of a multicenter randomized trial. J Clin Oncol 2014;32:199–205. 10.1200/JCO.2013.48.6662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Klinkhammer-Schalke M, Koller M, Steinger B, et al. Direct improvement of quality of life using a tailored quality of life diagnosis and therapy pathway: randomised trial in 200 women with breast cancer. Br J Cancer 2012;106:826–38. 10.1038/bjc.2012.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ruland CM, White T, Stevens M, et al. Effects of a computerized system to support shared decision making in symptom management of cancer patients: preliminary results. J Am Med Inform Assoc 2003;10:573–9. 10.1197/jamia.M1365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yount SE, Rothrock N, Bass M, et al. A randomized trial of weekly symptom telemonitoring in advanced lung cancer. J Pain Symptom Manage 2014;47:973–89. 10.1016/j.jpainsymman.2013.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Winnette R, Hess LM, Nicol SJ, et al. The patient experience with soft tissue sarcoma: a systematic review of the literature. Patient 2017;10:153–62. 10.1007/s40271-016-0200-1 [DOI] [PubMed] [Google Scholar]
- 23.Velikova G, Booth L, Smith AB, et al. Measuring quality of life in routine oncology practice improves communication and patient well-being: a randomized controlled trial. J Clin Oncol 2004;22:714–24. 10.1200/JCO.2004.06.078 [DOI] [PubMed] [Google Scholar]
- 24.Strasser F, Blum D, von Moos R, et al. The effect of real-time electronic monitoring of patient-reported symptoms and clinical syndromes in outpatient workflow of medical oncologists: E-MOSAIC, a multicenter cluster-randomized phase III study (SAKK 95/06). Ann Oncol 2016;27:324–32. 10.1093/annonc/mdv576 [DOI] [PubMed] [Google Scholar]
- 25.Schuler M, Richter S, Ehninger G, et al. A cluster-randomised, controlled proof-of-concept study to explore the feasibility and effect of a patient-directed intervention on quality of life in patients with advanced soft tissue sarcoma. BMJ Open 2017;7:e014614. 10.1136/bmjopen-2016-014614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cella DF, Tulsky DS, Gray G, et al. The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol 1993;11:570–9. 10.1200/JCO.1993.11.3.570 [DOI] [PubMed] [Google Scholar]
- 27.King MT, Cella D, Osoba D, et al. Meta-analysis provides evidence-based interpretation guidelines for the clinical significance of mean differences for the FACT-G, a cancer-specific quality of life questionnaire. Patient Relat Outcome Meas 2010;1:119–26. 10.2147/PROM.S10621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen J. Statistical power for the behavioral sciences. 2 edn Lawrence Erlbaum Associates, 1988. [Google Scholar]
- 29.Cleeland CS, Mendoza TR, Wang XS, et al. Assessing symptom distress in cancer patients. Cancer 2000;89:1634–46. [DOI] [PubMed] [Google Scholar]
- 30.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 31.Singer S, Kuhnt S, Götze H, et al. Hospital anxiety and depression scale cutoff scores for cancer patients in acute care. Br J Cancer 2009;100:908–12. 10.1038/sj.bjc.6604952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ribaudo JM, Cella D, Hahn EA, et al. Re-validation and shortening of the functional assessment of anorexia/cachexia therapy (FAACT) questionnaire. Qual Life Res 2000;9:1137–46. 10.1023/A:1016670403148 [DOI] [PubMed] [Google Scholar]
- 33.Radbruch L, Loick G, Kiencke P, et al. Validation of the German version of the brief pain inventory. J Pain Symptom Manage 1999;18:180–7. 10.1016/S0885-3924(99)00064-0 [DOI] [PubMed] [Google Scholar]
- 34.Brédart A, Bottomley A, Blazeby JM, et al. An international prospective study of the EORTC cancer in-patient satisfaction with care measure (EORTC IN-PATSAT32). Eur J Cancer 2005;41:2120–31. 10.1016/j.ejca.2005.04.041 [DOI] [PubMed] [Google Scholar]
- 35.Brucker PS, Yost K, Cashy J, et al. General population and cancer patient norms for the functional assessment of cancer Therapy-General (FACT-G). Eval Health Prof 2005;28:192–211. 10.1177/0163278705275341 [DOI] [PubMed] [Google Scholar]
- 36.Franciosi V, Maglietta G, Degli Esposti C, et al. Early palliative care and quality of life of advanced cancer patients-a multicenter randomized clinical trial. Ann Palliat Med 2019;8:381–9. 10.21037/apm.2019.02.07 [DOI] [PubMed] [Google Scholar]
- 37.Chan A, Lim E, Ng T, et al. Symptom burden and medication use in adult sarcoma patients. Support Care Cancer 2015;23:1709–17. 10.1007/s00520-014-2533-4 [DOI] [PubMed] [Google Scholar]
- 38.Warrington L, Absolom K, Holch P, et al. Online tool for monitoring adverse events in patients with cancer during treatment (eRAPID): field testing in a clinical setting. BMJ Open 2019;9:e025185. 10.1136/bmjopen-2018-025185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schuler MK, Trautmann F, Radloff M, et al. Implementation of a mobile inpatient quality of life (QOL) assessment for oncology nursing. Support Care Cancer 2016;24:3391–9. 10.1007/s00520-016-3163-9 [DOI] [PubMed] [Google Scholar]
- 40.Schuler M, Trautmann F, Radloff M, et al. Implementation and first results of a tablet-based assessment referring to patient-reported outcomes in an inpatient cancer care unit. Z Evid Fortbild Qual Gesundhwes 2017;121:64–72. 10.1016/j.zefq.2017.03.007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-035546supp001.pdf (68.9KB, pdf)
bmjopen-2019-035546supp002.pdf (67.3KB, pdf)