Abstract
BACKGROUND
Evolving requirements for patient and physician safety and rapid regulatory changes have stimulated interest in neurosurgical telemedicine in the COVID-19 era.
OBJECTIVE
To conduct a systematic literature review investigating treatment of neurosurgical patients via telemedicine, and to evaluate barriers and challenges. Additionally, we review recent regulatory changes that affect telemedicine in neurosurgery, and our institution's initial experience.
METHODS
A systematic review was performed including all studies investigating success regarding treatment of neurosurgical patients via telemedicine. We reviewed our department's outpatient clinic billing records after telemedicine was implemented from 3/23/2020 to 4/6/2020 and reviewed modifier 95 inclusion to determine the number of face-to-face and telemedicine visits, as well as breakdown of weekly telemedicine clinic visits by subspecialty.
RESULTS
A total of 52 studies (25 prospective and 27 retrospective) with 45 801 patients were analyzed. A total of 13 studies were conducted in the United States and 39 in foreign countries. Patient management was successful via telemedicine in 99.6% of cases. Telemedicine visits failed in 162 cases, 81.5% of which were due to technology failure, and 18.5% of which were due to patients requiring further face-to-face evaluation or treatment. A total of 16 studies compared telemedicine encounters to alternative patient encounter mediums; telemedicine was equivalent or superior in 15 studies. From 3/23/2020 to 4/6/2020, our department had 122 telemedicine visits (65.9%) and 63 face-to-face visits (34.1%). About 94.3% of telemedicine visits were billed using face-to-face procedural codes.
CONCLUSION
Neurosurgical telemedicine encounters appear promising in resource-scarce times, such as during global pandemics.
Keywords: Telemedicine, Telehealth, Neurosurgery, Stroke, Health policy, COVID-19, Coronavirus
ABBREVIATIONS
- CI
confidence interval
- CMS
Centers for Medicare & Medicaid Services
- CPT
Current Procedural Terminology
- ER
emergency room
- ICH
intracerebral hematoma
- mRS
modified Rankin Score
- NIHSS
National Institutes of Health Stroke Scale
- OR
odds ratio
Telemedicine is defined as the use of electronic means for exchange of health information for delivering health care remotely. Although utilized since at least 1995 in neurosurgery,1 telemedicine has not had widespread implementation in neurosurgery. Lack of reimbursement, inferiority of remote neurological exam, patient confidentiality concerns, the importance of in-person presence to establish the physician–patient bond, lack of technology, and acuity of disease processes treated are all reasons why the field of neurosurgery has been slow to adopt telemedicine.2 Telemedicine has had modest utilization in resource-poor countries3,4 and rural areas without access to neurosurgical services.5 However, with the advent of the COVID-19 pandemic, the urgent need to protect healthcare workers and patients from viral infection,6,7 as well as relaxation of regulatory barriers and facilitation of reimbursement in the United States, has stimulated new interest in telemedicine in neurosurgery.
Because of the dearth of data regarding success of telemedicine in neurosurgery, no guidelines have been published regarding its implementation during the COVID-19 era. Here, we aim to accomplish 3 objectives regarding telemedicine in neurosurgery. First, our primary aim is to perform a systematic literature review from 1995 to 2020 of all articles describing neurosurgical experience with telemedicine. Second, we aim to report a short interval initial assessment of how our department is performing billing and coding, as well as telemedicine implementation rates as categorized by subspecialty. Finally, we aim to consolidate and streamline the current telemedicine-related United States policy changes with regard for legal and financial viability for the practicing neurosurgeon.
METHODS
Study Selection
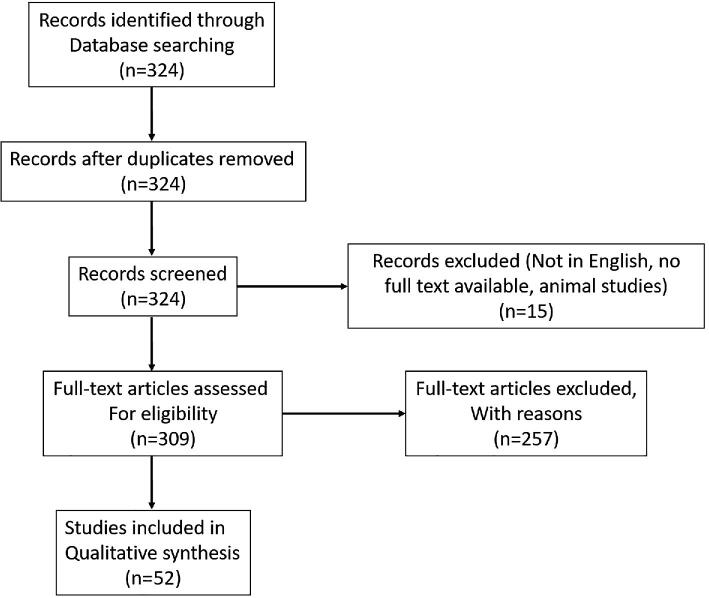
Using PubMed, Scopus, Medline, Ovid, Web of Science, EMBASE, and all major neurosurgical journals, a systematic literature search was performed using the medical subject heading terms “neurosurgery” and “telemedicine” in accordance with PRISMA guidelines.8 Articles were limited to English. Inclusion was limited to studies that specifically documented success of telemedicine visits for treatment of neurosurgical patients (including head and spine trauma, pediatric neurosurgery, stroke and vascular, brain tumors, hydrocephalus, spine surgery, and functional neurosurgery) in the prehospital, inpatient, outpatient, or hospital transfer triage settings. Retrospective studies and prospective analyses were included, while editorials and commentaries were excluded. Articles that described new technologies, but did not include neurosurgical consultation, and those that involved remote guidance of surgical procedures, were excluded. Country of origin of the study was recorded. The last literature search was performed April 5, 2020. A flow sheet describing the number of articles screened can be found in Figure 1.
FIGURE 1.
PRISMA flow diagram for systematic reviews.
Of the collected studies, studies in which a telemedicine encounter was compared to an alternative form of patient encounter were identified.
Data Extraction
The included studies were carefully analyzed for reported success of management by telemedicine encounter. Telemedicine encounter success was defined by achievement of the patient management goal specified by the individual study, which included the ability to evaluate a patient for transfer to a hospital with neurosurgical capabilities, ability to remotely program a neuromodulation device, ability to successfully perform a postoperative clinic visit, guide the administration of thrombolytics for stroke patients in the prehospital or hospital stage, or manage inpatients in the neurointensive care unit. The number of patients that were successfully managed by telemedicine was divided by the total number of patients, yielding a percentage of patients that were successfully treated.
The patients that were unsuccessfully managed by telemedicine were identified, and the reason for telemedicine inadequacy was tabulated and reported as percentages.
After identifying the studies in which a telemedicine encounter was compared to an alternative form of patient encounter, the superior medium of encounter as determined by the individual study was tabulated.
Institutional Experience
Our department's billing records for all outpatient clinic visits were retrospectively reviewed from 3/23/2020 to 4/6/2020 (1 wk after the telehealth portal was first implemented). Visits in which modifier 95 was included were classified as telemedicine visits, and visits without modifier 95 inclusion were classified as face-to-face visits. We then reviewed the Current Procedural Terminology (CPT) code submitted for the visit. Visits coded using the face-to-face evaluation and management services CPT codes 99 201 to 99 215 or 99 024 were classified as face-to-face. Visits coded using the telemedicine codes g2010 (remote image review) or g2012 (brief check-in) were classified as telemedicine visits.
Distribution of Telemedicine Clinic Visits by Subspecialty
The identified telemedicine clinic visits were then further categorized based on attending subspecialty as either spine or cranial. Weekly telemedicine clinic visits were totaled for each subspecialty. These values were then calculated as a percentage of the number of weekly total subspecialty clinic visits during the corresponding calendar week of 2019, which served as a pretelemedicine era baseline.
RESULTS
Study Characteristics
A total of 324 studies were initially identified with no duplicates (Figure 1). A total of 15 studies were excluded due to nonEnglish language. Of the remaining 309 studies, 257 did not meet the prespecified inclusion and exclusion criteria. Ultimately, our search yielded 52 articles with 45 801 patients and were included in our analysis, which are summarized in Table 1.1,3-5,9-56 A total of 25 studies were prospective and 27 were retrospective. A total of 13 studies were conducted in the United States and 39 were conducted in foreign countries. Of these studies, 16 studies in which a telemedicine encounter was compared to an alternative form of patient encounter were identified.
TABLE 1.
Publications Included in Systematic Review of Neurosurgical Telemedicine Articles
| Subspecialty | Publication | Number of patients | Prospective or retrospective | Telemedicine encounter setting | Country of Origin | % of patients telemedicine successful | |
|---|---|---|---|---|---|---|---|
| Trauma | 1 | Olldashi9 | 590 | Retrospective | Transfer triage | Albania | 100% |
| 2 | Ashkenazi (2015)10 | 561 | Retrospective | Transfer triage | Israel | 100% | |
| 3 | Moya11 | 39 | Retrospective | Transfer triage | USA | 100% | |
| 4 | Dulou12 | 16 | Retrospective | Transfer triage | France | 100% | |
| 5 | Klein13 | 98 | Retrospective | Transfer triage | Israel | 100% | |
| 6 | Zulu14 | 230 | Prospective | Transfer triage | South Africa | 100% | |
| 7 | Servadei15 | 1665 | Retrospective | Transfer triage | Italy | 100% | |
| 8 | Latifi16 | 146 | Retrospective | Transfer triage | Albania | 100% | |
| 9 | Ashkenazi (2007)17 | 209 | Retrospective | Transfer triage | Israel | 100% | |
| Functional | 10 | Mendez18 | 10 | Prospective | Outpatient care | Canada | 100% |
| Stroke | 11 | Angileri19 | 2819 (733 with intracerebral hematoma, ICH) | Retrospective | Inpatient care | Italy | 100% |
| 12 | Demaerschalk (2010)20 | 27 | Prospective | Inpatient care | USA | 100% | |
| 13 | Demaerschalk (2012)21 | 138 | Prospective | Inpatient care | USA | 100% | |
| 14 | Meyer22 | 111 | Prospective | Inpatient care | USA | 99.1% | |
| 15 | Valenzuela Espinoza23 | 2282 | Retrospective | Prehospital care | Belgium | 100% | |
| 16 | Shoirah24 | 182 | Retrospective | Prehospital care | USA | 100% | |
| 17 | Ionita1 | 27 | Retrospective | Prehospital care | USA | 100% | |
| 18 | Barrett25 | 11 | Prospective | Prehospital care | USA | 91% | |
| 19 | Chalouhi26 | 1643 | Prospective | Inpatient care | USA | 100% | |
| 20 | Audebert27 | 106 | Prospective | Inpatient care | Germany | 100% | |
| 21 | Hess28 | 194 | Retrospective | Inpatient care | USA | 100% | |
| 22 | Switzer29 | 50 | Retrospective | Inpatient care | USA | 100% | |
| 23 | Schwab30 | 170 | Prospective | Inpatient care | Germany | 100% | |
| 24 | Handschu31 | 77 | Prospective | Inpatient care | Germany | 100% | |
| Pediatrics | 25 | Pirris32 | 3 | Prospective | Outpatient care | USA | 100% |
| 26 | Owler33 | 9 | Prospective | Transfer triage | Australia | 100% | |
| 27 | James5 | 43 | Prospective | Outpatient care | USA | 100% | |
| 28 | Hayward34 | 55 | Retrospective | Outpatient care | USA | 100% | |
| 29 | Jackson35 | 8 | Retrospective | Prehospital care | USA | 100% | |
| Spine | 30 | Debono36 | 60 | Prospective | Outpatient care | France | 100% |
| NeuroICU care | 31 | Williams37 | 2 | Retrospective | Inpatient care | USA | 100% |
| All | 32 | Narenthiranathan38 | 944 | Retrospective | Transfer triage | Malaysia | 100% |
| 33 | Wong39 | 235 | Prospective | Transfer triage | China | 69.9% | |
| 34 | Stormo40 | 99 | Prospective | Transfer triage | Norway | 100% | |
| 35 | Dadlani41 | 1587 | Retrospective | Outpatient care | India | 100% | |
| 36 | Thapa42 | 120 | Prospective | Transfer triage | Nepal | 100% | |
| 37 | Jithoo4 | 100 | Prospective | Transfer triage | South Africa | 100% | |
| 38 | Rudinsky43 | 244 | Retrospective | Transfer triage | Slovakia | 100% | |
| 39 | Vuletic3 | 2071 | Retrospective | Transfer triage | Croatia | 100% | |
| 40 | Poon44 | 109 | Prospective | Transfer triage | China | 46.6% | |
| 41 | Goh45 | 31 | Prospective | Transfer triage | China | 100% | |
| 42 | Bailes46 | 100 | Prospective | Transfer triage | USA | 100% | |
| 43 | Urban47 | 432 | Retrospective | Transfer triage | Germany | 100% | |
| 44 | Goh48 | 66 | Prospective | Transfer triage | China | 100% | |
| 45 | Thakar49 | 1034 | Retrospective | Outpatient care | India | 97.1% | |
| 46 | Reider-Demer50 | 57 | Prospective | Outpatient care | USA | 100% | |
| 47 | Hassan51 | 349 | Prospective | Transfer triage | Malaysia | 100% | |
| 48 | Bertani52 | 138 | Retrospective | Transfer triage | Djbouti | 100% | |
| 49 | Mrak53 | 25 366 | Retrospective | Transfer triage | Croatia | 100% | |
| 50 | Waran54 | 14 | Retrospective | Transfer triage | Malaysia | 100% | |
| 51 | Kreutzer55 | 1024 | Retrospective | Transfer triage | Germany | 100% | |
| 52 | Yamada56 | 100 | Prospective | Transfer triage | Japan | 100% |
Studies by Subspecialty
A variety of neurosurgical subspecialties were represented in this review. A total of 21 studies comprised data from all neurosurgical subspecialties (40.4%). The majority of studies investigating 1 neurosurgical subspecialty were focused on either trauma (9, 17.3%), stroke (14, 26.9%), or pediatric care (5, 9.6%). Functional neurosurgery study, NeuroICU care, and spine study were also included 1 each (1, 1.9%).
Studies Stratified by Goals of Management
Patient Transfer
A total of 28 studies (53.8%) composing of 35 105 patients evaluated the use of telemedicine for rapid transfer triage of patients. Telemedicine was also used to evaluate the imaging and neurological exam of patients from regional hospitals to a hospital with neurosurgical services. Following evaluation of imaging sent from regional hospitals, telemedicine consultations were often performed either live (synchronous) or store-and-forward (asynchronous) or a combination of both.
Inpatient Care
A total of 11 studies (21.2%) composing 5337 patients assessed the use of telemedicine for inpatient care. For inpatient visits, interviews were conducted with directed neurological examinations with consultation conducted remotely via videoconference software. Often structured questionnaires were employed to standardize interviews to assess patient status and progress.
Outpatient Care
A total of 8t studies (15.4%) with a total 2849 patients investigated the efficacy of telemedicine in the outpatient clinic setting. One functional neurosurgery study involved telemedicine for remote programming of a neuromodulation device using a remote robot controlled by nonexpert nurses.28 A total of 5 studies comprised of 2510 patients assessed the use of telemedicine in prehospital outpatient urgent care, primarily for thrombolytic administration for ischemic stroke evaluation (9.6%). Prehospital consultation often involved in-ambulance automated transmission of patient vitals, identification, and functional assessments, such as the National Institutes of Health Stroke Scale (NIHSS) stroke scale57 to streamline patient admission and workflow.
Telemedicine Success in Neurosurgery
Across all included studies, in 99.6% of patients, study authors found that treatment of neurosurgical patients was successful with telemedicine. Telemedicine visits were unsuccessful in 162 cases, 81.5% of which were due to technology failure, and 18.5% of which were due to the provider determining that the patient required additional face-to-face treatment or evaluation at the inpatient clinic or hospital.
Comparative Studies
A total of 16 studies were found comparing telemedicine encounters to an alternative form of patient encounter (Table 2); telemedicine was equivalent or superior to nontelemedicine encounters in 15 studies. One study found that teleradiology alone to be superior to a telemedicine encounter; however, this study was severely biased by more than 30% of visits being incomplete due to technological issues.
TABLE 2.
List of Studies Comparing Neurosurgical Telemedicine Consults to Other Means of Consultation
| Study | Population | Study type | Patients included | Results | Interpretation | ||
|---|---|---|---|---|---|---|---|
| 1 | Klein13 | Head trauma transfer triage | Retrospective cohort comparative study | Group 1: 98 patients evaluated for transfer via telemedicine | Group 1: 58% patients not transferred; 0% neurological sequela | Neurosurgical telemedicine reduces unnecessary head trauma transfers without neurological sequela | 100% telemedicine encounters successful |
| Group 2: 73 patients evaluated for transfer by non-neurosurgeons via guidelines | Group 2: 26% patients not transferred. 0% Neurological sequela | ||||||
| 2 | Meyer22 | Thrombolytic administration for stroke | Randomized blinded prospective study | Group 1: 111 patients via telemedicine | Correct treatment decision made in 98% of group 1 vs 82% in group 2 (P = .0009) | Telemedicine is superior to telephone consultation for decision to administer thrombolytic | One telemedicine consult aborted for technical issues |
| Group 2: 111 patients via telephone consultation | |||||||
| 3 | Wong39 | Transfer triage (all subspecialties) | Randomized prospective study | Group 1: 235 patients via telephone consultation | Trend toward more favorable outcome (61%; P = .12) and reduced mortality (25%; P = .025) in group 2 compared with group 3 (54 and 33%, respectively) | Telemedicine had worse outcomes than teleradiology. However, interpretation complicated by high telemedicine technology failure rate | 30.1% telemedicine consultation failure rate (technical issues) |
| Group 2: 239 patients via Teleradiology consultation | |||||||
| Group 3: 236 patients via video consultation | |||||||
| 4 | Poon44 | Transfer triage (all subspecialties) | Randomized prospective study | Group 1: telephone consultation | Trend towards more favorable outcome in the group 3 (44%), vs group 2 (31%) and group 1 (38%) | Telemedicine had better outcomes than teleradiology and telephone consultations | 53.4% video consultation failure rate (technical issues) |
| Group 2: Teleradiology consultation | No P-values provided | ||||||
| Group 3: Video consultation | |||||||
| 327 patients total, subgroup numbers not provided | |||||||
| 5 | Thakar49 | Postoperative outpatient follow-up | Retrospective comparison study (patients chose face-to-face vs telemedicine visits | Group 1: 166 face-to-face visits | Group 1: mean cost of visit 6848 rupees | 3% telemedicine patients referred for face-to-face visit (0.9% for neurosurgical problem, 2.0% for non-neurosurgical medical problem). | Reasons for referral to face-to-face visits not described |
| Group 2: 1034 telemedicine visits | Group 2: mean cost of visit 2635 rupees | ||||||
| 6 | Reider-Deimer50 | Postoperative outpatient follow-up | Retrospective cohort comparison | Group 1: 42 face-to-face visits | In first 90 d postop, group 1: 2.4% ER visit rate and 2.4% readmission rate vs group 2: 0% ER visit rate and 4.2% readmission rate | No significant difference between telemedicine and face-to-face visits for postoperative care | 100% telemedicine encounters successful |
| Group 2: 57 telemedicine visits | |||||||
| 7 | Mendez18 | Remote programming of neuromodulation devices | Randomized prospective study | Group 1: 10 patients for face-to-face programming | No difference between groups for accuracy | No difference between groups for accuracy | 100% telemedicine encounters successful |
| Group 2: 10 patients for remote guidance of nurses for programming | |||||||
| 8 | Ionita1 | Thrombolytic administration for stroke | Retrospective study | Group 1: 128 patients treated face-to-face at hub site | No significant difference between groups 1 and 2 for mortality (10.9% vs 11.1%; P = .34), ICH (20.3% vs 33.3% P < .35), good outcome of mRS 4 to 6 (52.3% vs 51.9% P = .16), or length of stay (8.8 vs 10.7 d, P < .23) | No difference between groups for outcomes | 100% telemedicine encounters successful |
| Group 2: 27 patients treated via telemedicine at spoke sites | |||||||
| 9 | Shoira24 | Stroke trial enrollment | Retrospective review | Group 1: 117 patients enrolled face-to-face at hub site | Annual increase in trial enrollment higher in group 2 than group 1 (11.55 ± 11.30 vs 0.68 ± 1.03, P < .0005) and had increased correlation with total enrollment increase (0.98 vs 0.94, P < .0001) | Significantly more stroke patients successfully recruited to stroke trials in telemedicine group | 100% telemedicine encounters successful |
| Group 2: 182 patients enrolled via telemedicine at spoke sites | |||||||
| 10 | Jackson35 | Pediatric transfer triage | Retrospective review | All patients ≤ 18 y/o | Group 1 had trend towards decreased rates of repeat preoperative neuroimaging (P = .62), short time between trauma bay arrival and surgery (P = .22), diagnosis to surgery (P = .45), and higher home discharge rates (P = .28). | Telemedicine consult during interhospital transport of pediatric patients with operative intracranial hemorrhage appears to expedite emergent care and decrease decreased postoperative length of hospitalization | 100% telemedicine encounters successful |
| Group 1: 8 via telemedicine | Also trend towards shorter ICU stay (P = .338) and hospitalization (P = .409) | ||||||
| Group 2: 7 nontelemedicine | |||||||
| 11 | Angileri19 | Acute transfer triage | Retrospective review | Group 1: 2819 patients evaluated via telemedicine | Trend toward faster neurosurgical consult for group 1 (38 min vs 160 min) (P-value not specified) | Telemedicine consult faster for determining need to transfer than nontelemedicine consult | 100% telemedicine encounters successful infeasible |
| Group 2: patients evaluated before telemedicine implemented, number not specified | |||||||
| 12 | Demaerschalk (2010)20 | Thrombolytic administration for stroke | Prospective blinded study | Group 1: 138 patients evaluated via telemedicine | Correct treatment decision: 85% group 1 and 89% group 2 (P > .999), | Telemedicine is equivalent to telephone consultation for decision to administer thrombolytic | 100% telemedicine encounters successful |
| Group 2: 138 patients evaluated via telephone consultation | No difference between groups for good 90-d functional outcome, mRS, or mortality | ||||||
| 13 | Demaerschalk (2012)21 | Thrombolytic administration for stroke | Prospective blinded study | Group 1: 27 patients evaluated via telemedicine | Correct decision regarding thrombolytic administration 96% for group 1 and 83% for group 2 odds ratio (OR) 4.2; 95% CI | Telemedicine is superior to telephone consultation for decision to administer thrombolytic | 100% telemedicine encounters successful |
| Group 2: 27 patients evaluated via telephone consultation | CI 1.69-10.46; P = .002). | ||||||
| 14 | Schwab30 | Thrombolytic administration for stroke | Prospective study | Group 1: 170 patients evaluated via telemedicine | For group 1 and group 2, mortality rates were 11.2% vs 11.5% at 3 mo (P = .55), good functional outcome was 39.5% vs 30.9% (P = .10) | Telemedicine is equivalent to telephone consultation for decision to administer thrombolytic | 100% telemedicine encounters successful |
| Group 2: 132 patients evaluated face-to-face | |||||||
| 15 | Handschu31 | Stroke care | Prospective study | Group 1: 77 patients evaluated via telemedicine | Group 2 compared to group 1 had higher stroke center transfers (9.1% vs 14.9%, P < .05), higher 10 d mortality (6.8% vs 1.3%, P < .05), diagnosis had to be corrected more frequently (17.6% vs 7.1%, P < .05) | Telemedicine had fewer transfers, lower 10 d mortality, and more frequent correct diagnosis compared to telephone consultation | 100% telemedicine encounters successful |
| Group 2: 74 patients evaluated via telephone | |||||||
| 16 | Goh48 | Acute transfer triage | Prospective study | Group 1: 66 patients had telemedicine consult | Group 1 compared to group 2 had 21% fewer unnecessary transfers, fewer complications during transfers (8% vs 32%, P = .002), and transfer time shortened (72 min vs 80 min, P = .38) | Telemedicine resulted in fewer unnecessary transfers, fewer complications during transfers, and shorter time to transfer | 100% telemedicine encounters successful |
| Group 2: 50 patients before telemedicine available |
ER: emergency room; mRS: modified Rankin Score.
Institutional Results
Our department had 122 telehealth visits (65.9%) and 63 face-to-face visits (34.1%) over 30 d after the COVID-19 lock down occurred. Of the 122 telehealth visits, 115 (94.3%) visits were billed using face-to-face evaluation and management services CPT codes. A total of 4 visits were billed using the telehealth brief check-in code (g2012) and 3 visits were billed using the remote image review code (g2010).
Distribution of Telemedicine Clinic Visits by Subspecialty
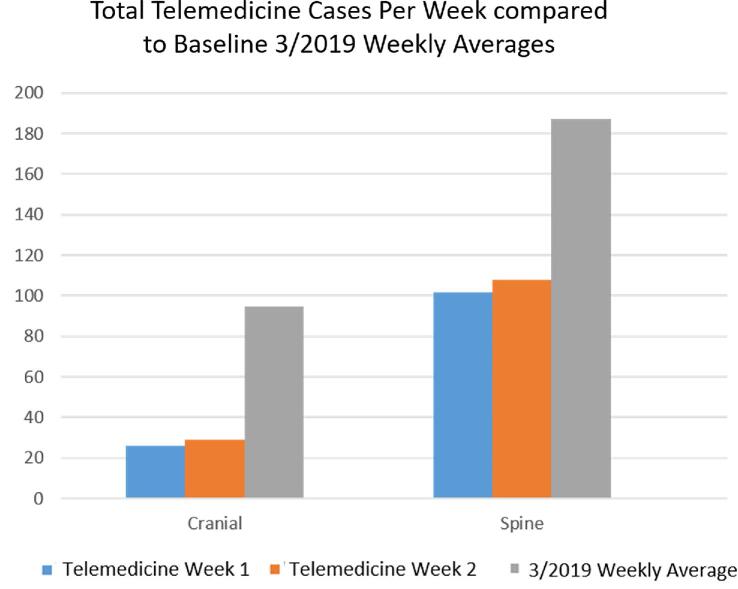
Weekly subspecialty telemedicine clinic visits from 3/23/2020 to 4/6/2020 were calculated as a percentage of baseline 2019 weekly subspecialty face-to-face clinic visits and are summarized in Figure 2.
FIGURE 2.
Breakdown of outpatient clinic telemedicine visits per week by sub-specialty as compared to the March 2019 weekly averages displayed as absolute number of cases.
DISCUSSION
The advent of the COVID-19 pandemic, as well as relaxation of regulatory barriers and facilitation of reimbursement, has stimulated new interest in neurosurgical telemedicine. The results of our systematic review suggest that remote telemedicine treatment of neurosurgical patients is feasible in the prehospital, inpatient, outpatient, and transfer triage settings, at least in resource-scarce situations.
In areas without access to neurosurgeons, remote neurosurgical visits may be preferable to no neurosurgical consultation at all, particularly in emergency cases. Resource-poor countries3,4 and medically underserved areas5 have a track record of telemedicine utilization for neurosurgical diseases, often regarding the decision to transfer a patient to a setting with neurosurgical services. Telemedicine-based neurosurgical visits may reduce patient travel time and costs,34 and may save health care systems significant expenditures.46
From our systematic review, the most common reason for telemedicine failure was technological failure (81.5%). We would expect this number to decrease over time as technology and user interface improves, and as the site becomes more familiar with its utilization. Interestingly, inability to obtain an accurate neurological exam was not mentioned as a reason for telemedicine encounter failure in any case. Although 18.5% of the telemedicine encounter failures were due to inability to deliver care remotely, resulting in the patient to be instructed to come to a face-to-face encounter, the ability to identify those who require a higher level of in-person care is in our opinion a success of telemedicine. We do not suggest that telemedicine be used to replace face-to-face visits, but rather to triage those who should be called in.
Of the 16 studies that compared telemedicine encounters to other methods of patient encounters, 15 found that telemedicine encounters were equivalent or superior to the alternative patient encounter medium. Wong et al39 found teleradiology encounters (in which the neurosurgeon was able to remotely view a patient's imaging, but not video of the patient's neurological exam) to have superior favorable outcome rates and reduced mortality rates compared to a telemedicine encounter in which a patient's imaging and video were available. However, these results are difficult to interpret, as a very high failure rate (30.1% failure rate) of the telemedicine technology was experienced. For the decision to administer thrombolytic therapy to patients with ischemic stroke, the American Heart Association/American Stroke Association recommends that if stroke site expertise is not physically available, a stroke expert should provide a recommendation via telemedicine.58 It is likely that telemedicine at best provides acceptable, near-equivalent clinical information as a face-to-face encounter, and at worst is able to identify patients who should be brought in for in-person evaluation.
It is possible to perform a near-full neurological exam remotely via telemedicine.59,60 A remote exam may be augmented with the remote guidance of an in-person health care provider, which may be particularly important in situations where the patient cannot comply with directions such as in comatose states or in the pediatric population. In fact, the American Heart Association/American Stroke Association suggests a telemedicine NIHSS assessment is comparable to a bedside NIHSS assessment.58 However, the telemedicine exam should be considered a screening tool, not the definitive neurological exam. If physical exam findings sound worrisome, the neurosurgeon should call in the patient to the clinic and/or emergency room for an in-person evaluation.
In the United States, new legislation has removed several regulatory hurdles, greatly facilitating telemedicine to be a legally and financially viable solution in neurosurgery. Much of what is driving whether telemedicine is adopted is billing. Prior to March 6, 2020, the Centers for Medicare & Medicaid Services (CMS) did not reimburse telephone calls, and telemedicine reimbursements were restricted to those performed for rural outreach. However, on March 6, 2020, access to telemedicine services has been greatly augmented on an emergency and temporary basis under the 1135 waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act.61 Under these new provisions, visits conducted through a telemedicine portal will be reimbursed by CMS with the same rate as with a face-to-face visit. In fact, the same evaluation and management codes as a face-to-face visit may be specified and the place of service code should be the same as it would have been for a face-to-face visit (ie, 01 for Medicare). Billing specialists should utilize a 95 modifier on evaluation and management codes to indicate that the service was rendered via telehealth. Because CMS may continue to change how telemedicine services are billed, practitioners should continue to monitor for such changes and modify their billing practices accordingly.
Additionally, CMS has waived the requirement that out-of-state providers be licensed in the state where they are providing services, further increasing the availability of telemedicine for treating neurosurgery patients out of state.62
Because telemedicine portals are a new technology that has not been rigorously proven to provide equivalent care to a face-to-face visit, providers should perform a verbal consent to treatment by telemedicine treatment, to which the patient must verbally agree. This consenting process should be documented. Clinicians must consider that as telemedicine is a new and rapidly evolving field, malpractice litigation in telemedicine could occur. Misdiagnoses or failure to identify pressing issues at home may create legal implications.
HIPAA-compliant technological availability was previously a major barrier to neurosurgical telemedicine adoption. However, most electronic medical record systems, such as Epic (Epic Systems Corporation, Madison, Wisconsin) have built-in HIPAA-compliant telemedicine scripting that is able to establish a secure audio-visual conference call between computers, laptops, tablets, or smartphones. Many health care systems have initiated rapid rollout of such functionality.6 Although such HIPAA-compliant platforms are secure, privacy considerations are important, and part of the verbal consent process for treatment with telemedicine should include a discussion of the possibility that protected health information may be compromised. Some neurosurgery patients, may require assistance with activating the telemedicine conference call. If technological challenges prove insurmountable with a patient, providers should have a low threshold to convert to a regular telephone call. If the failed attempt to initiate a telemedicine visit is documented (ie, the telehealth portal was attempted, failed, and the visit was converted to a phone call), the telephone call may be billed and reimbursed as if it were a full telemedicine visit.61
Patient Satisfaction
While no studies have described patient satisfaction rates with telemedicine visits in the COVID-19 era, prior telemedicine studies reported initially optimistic results. Reider-Deimer et al (2018) evaluated the use of telemedicine for postoperative follow-up after elective neurosurgery. In a sample of 99 patients, 100% reported satisfaction with the telemedicine appointment on postvisit questionnaires. Indeed, initial reports of patient satisfaction with telemedicine appointments appear promising and may warrant further innovation and investigation.
Telemedicine in the Post-COVID-19 Era
The expansion of telemedicine services under the 1135 waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act were intended to be temporary measures during this emergency pandemic period. However, if the data collected during this era demonstrates favorable clinical outcomes and patient preferences, it may be possible that the regulatory expansion could be made permanent.
Institutional Experience
Interestingly, we report variation among the neurosurgical subspecialties at our institution regarding telemedicine implementation in outpatient clinic visits.63 While spine subspecialists attained almost 60% of the clinical volume as seen during the corresponding weeks in 2019, cranial subspecialists only recaptured approximately 30% of the 2019 weekly baseline clinical volume (Figure 2). The most likely explanation for this unforeseen disparity is that there is typically a greater outpatient clinic backlog of spine patients compared to cranial patients, as spine patients often make their clinic appointments several weeks in advance. Therefore, a greater proportion of spine patients already have completed imaging studies and workups prior to being seen.
Limitations
Like all systematic reviews, this one is limited by the quantity and quality of studies included. While we believe the sample of studies presented here is comparatively quite substantial, the quality between each investigation may be highly variable. Although multiple reports included were randomized, prospective studies, most studies were of retrospective nature, which are characterized by their own inherent limitations. Additionally, the majority of studies were conducted at healthcare sites outside of the United States, within third-world countries as well as first-world countries with healthcare systems drastically different from the American healthcare institution. Thus, whether these studies may be generalizable to the American population remains questionable. However, we hope that the lessons learned in other countries with more telemedicine experience may be utilized in the United States as implementation becomes more widespread following policy changes. Because of the substantial differences in study design, patient population, and variables reported among studies, it is difficult to directly and objectively compare the quality and degree of bias of each study; however, we believe the large number of studies and patients included in the systematic review analysis will compensate for any intrastudy heterogeneity in quality and/or bias.
Another limitation is the complexity in comparing results of telemedicine studies within neurosurgical subspecialties. Although we tabulated telemedicine encounter success as achievement of the individual study's goals, encounter success has many facets including patient satisfaction, adequacy of care, physician evaluations, or percentage of transferred patients that ultimately required surgery, all of which are difficult to capture. Furthermore, methodology on how telemedicine visits were conducted varied greatly between each group.
Because telemedicine has been implemented for a relatively short period of time, interpretation of the data regarding our initial experience is limited. We are currently compiling our long term institutional data regarding our telemedicine experience, and anticipate it will inform future clinical and hospital decisions.
CONCLUSION
Our systematic review suggests that remote telemedicine visits for neurosurgical patients appears promising in the prehospital, inpatient, outpatient, and transfer triage settings, at least in resource-constrained situations. Further large-scale prospective randomized studies are required to determine equivalence of telemedicine visits compared to face-to-face visits. At the least, telemedicine is likely an acceptable screening tool to triage patients with concerning neurological exam and/or imaging findings to report for face-to-face visits with a neurosurgeon.
Disclosures
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
Contributor Information
Daniel G Eichberg, University of Miami, Department of Neurosurgery, Miami, Florida.
Gregory W Basil, University of Miami, Department of Neurosurgery, Miami, Florida.
Long Di, University of Miami, Department of Neurosurgery, Miami, Florida.
Ashish H Shah, University of Miami, Department of Neurosurgery, Miami, Florida.
Evan M Luther, University of Miami, Department of Neurosurgery, Miami, Florida.
Victor M Lu, University of Miami, Department of Neurosurgery, Miami, Florida.
Maggy Perez-Dickens, University of Miami, Department of Neurosurgery, Miami, Florida.
Ricardo J Komotar, University of Miami, Department of Neurosurgery, Miami, Florida; Sylvester Comprehensive Cancer Center, Miami, Florida.
Allan D Levi, University of Miami, Department of Neurosurgery, Miami, Florida.
Michael E Ivan, University of Miami, Department of Neurosurgery, Miami, Florida; Sylvester Comprehensive Cancer Center, Miami, Florida.
COMMENT
The authors present a timely systematic review on use of telemedicine in neurosurgical care, including both a systematic review of the literature, as well as detailing their own single-institution experience after COVID precautions were enacted. A total of 45,801 patients were analyzed and telemedicine was found to be successful in 99.6% of patients. In the remaining cases, technology failure was found to be the most common cause of a failed visit while the need for in-person clinical examination was found to be a factor in some cases. Their results demonstrate that neurosurgical telemedicine encounters appear to be a promising avenue to deliver care in resource-scarce times such as the COVID pandemic. While the authors analyze the results by subspecialty for their own practice, future studies evaluating the success of telemedicine should also aim to provide failure rates in each neurosurgical subspecialty. In addition, future studies might also investigate the surgical outcomes and patient satisfaction for cases that eventually go on to get operated. Finally, the reimbursement for telemedicine is an important consideration, particularly if we expect it telemedicine to grow in adoption in the post-COVID era.
Mohamad Bydon
Rochester, Minnesota
REFERENCES
- 1. Ionita CC, Sharma J, Janicke DM et al.. Acute ischemic stroke and thrombolysis location: comparing telemedicine and stroke center treatment outcomes. Hosp Pract. 2009;37(1):33-39. [DOI] [PubMed] [Google Scholar]
- 2. Kahn EN, La Marca F, Mazzola CA. Neurosurgery and telemedicine in the united states: assessment of the risks and opportunities. World Neurosurg. 2016;89:133-138. [DOI] [PubMed] [Google Scholar]
- 3. Vuletic S. Teleradiology in Croatia. J Telemed Telecare. 2001;7(Suppl 1):73-75. [DOI] [PubMed] [Google Scholar]
- 4. Jithoo R, Govender PV, Corr P, Nathoo N. Telemedicine and neurosurgery: experience of a regional unit based in South Africa. J Telemed Telecare. 2003;9(2):63-66. [DOI] [PubMed] [Google Scholar]
- 5. James HE. Pediatric neurosurgery telemedicine clinics: a model to provide care to geographically underserved areas of the united states and its territories. J Neurosurg Pediatr. 2016;25(6):753-757. [DOI] [PubMed] [Google Scholar]
- 6. Eichberg DG, Shah AH, Luther EM et al.. Letter: academic neurosurgery department response to COVID-19 pandemic: the University of Miami/Jackson Memorial Hospital model. Neurosurgery. 2020;87(1):E63-E65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zacharia BE, Eichberg DG, Ivan ME et al.. Letter: surgical management of brain tumor patients in the COVID-19 era. Neurosurgery. published online: April 29, 2020 (doi:10.1093/neuros/nyaa162). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Olldashi F, Latifi R, Parsikia A et al.. Telemedicine for neurotrauma prevents unnecessary transfers: an update from a nationwide program in Albania and analysis of 590 patients. World Neurosurg. 2019;128:e340-e346. [DOI] [PubMed] [Google Scholar]
- 10. Ashkenazi I, Zeina AR, Kessel B et al.. Effect of teleradiology upon pattern of transfer of head injured patients from a rural general hospital to a neurosurgical referral centre: follow-up study. Emerg Med J. 2015;32(12):946-950. [DOI] [PubMed] [Google Scholar]
- 11. Moya M, Valdez J, Yonas H, Alverson DC. The impact of a telehealth web-based solution on neurosurgery triage and consultation. Telemed J E Health. 2010;16(9):945-949. [DOI] [PubMed] [Google Scholar]
- 12. Dulou R, Dagain A, Delmas JM et al.. The French mobile neurosurgical unit. Neurosurg Focus. 2010;28(5):E13. [DOI] [PubMed] [Google Scholar]
- 13. Klein Y, Donchik V, Jaffe D et al.. Management of patients with traumatic intracranial injury in hospitals without neurosurgical service. J Trauma. 2010;69(3):544-548. [DOI] [PubMed] [Google Scholar]
- 14. Zulu BM, Mulaudzi TV, Madiba TE, Muckart DJ. Outcome of head injuries in general surgical units with an off-site neurosurgical service. Injury. 2007;38(5):576-583. [DOI] [PubMed] [Google Scholar]
- 15. Servadei F, Antonelli V, Mastrilli A, Cultrera F, Giuffrida M, Staffa G. Integration of image transmission into a protocol for head injury management: a preliminary report. Br J Neurosurg. 2002;16(1):36-42. [DOI] [PubMed] [Google Scholar]
- 16. Latifi R, Olldashi F, Dogjani A, Dasho E, Boci A, El-Menyar A. Telemedicine for neurotrauma in Albania: initial results from case series of 146 patients. World Neurosurg. 2018;112:e747-e753. [DOI] [PubMed] [Google Scholar]
- 17. Ashkenazi I, Haspel J, Alfici R, Kessel B, Khashan T, Oren M. Effect of teleradiology upon pattern of transfer of head injured patients from a rural general hospital to a neurosurgical referral centre. Emerg Med J. 2007;24(8):550-552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mendez I, Song M, Chiasson P, Bustamante L. Point-of-care programming for neuromodulation: a feasibility study using remote presence. Neurosurgery. 2013;72(1):99-108; discussion 108. [DOI] [PubMed] [Google Scholar]
- 19. Angileri FF, Cardali S, Conti A, Raffa G, Tomasello F. Telemedicine-assisted treatment of patients with intracerebral hemorrhage. Neurosurg Focus. 2012;32(4):E6. [DOI] [PubMed] [Google Scholar]
- 20. Demaerschalk BM, Bobrow BJ, Raman R et al.. Stroke team remote evaluation using a digital observation camera in Arizona: the initial mayo clinic experience trial. Stroke. 2010;41(6):1251-1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Demaerschalk BM, Raman R, Ernstrom K, Meyer BC. Efficacy of telemedicine for stroke: pooled analysis of the stroke team remote evaluation using a digital observation camera (STRokE DOC) and STRokE DOC Arizona telestroke trials. Telemed J E Health. 2012;18(3):230-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Meyer BC, Raman R, Hemmen T et al.. Efficacy of site-independent telemedicine in the STRokE DOC trial: a randomised, blinded, prospective study. Lancet Neurol. 2008;7(9):787-795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Valenzuela Espinoza A, Devos S, van Hooff RJ et al.. Time gain needed for in-ambulance telemedicine: cost-utility model. JMIR Mhealth Uhealth. 2017;5(11):e175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Shoirah H, Wechsler LR, Jovin TG, Jadhav AP. Acute stroke trial enrollment through a telemedicine network: a 12-year experience. J Stroke Cerebrovasc Dis. 2019;28(7):1926-1929. [DOI] [PubMed] [Google Scholar]
- 25. Barrett KM, Pizzi MA, Kesari V et al.. Ambulance-based assessment of NIH stroke scale with telemedicine: a feasibility pilot study. J Telemed Telecare. 2017;23(4):476-483. [DOI] [PubMed] [Google Scholar]
- 26. Chalouhi N, Dressler JA, Kunkel ES et al.. Intravenous tissue plasminogen activator administration in community hospitals facilitated by telestroke service. Neurosurgery. 2013;73(4):667-671; discussion 671-662. [DOI] [PubMed] [Google Scholar]
- 27. Audebert HJ, Kukla C, Clarmann von Claranau S et al.. Telemedicine for safe and extended use of thrombolysis in stroke: the telemedic pilot project for integrative stroke care (TEMPiS) in Bavaria. Stroke. 2005;36(2):287-291. [DOI] [PubMed] [Google Scholar]
- 28. Hess DC, Wang S, Hamilton W et al.. REACH: clinical feasibility of a rural telestroke network. Stroke. 2005;36(9):2018-2020. [DOI] [PubMed] [Google Scholar]
- 29. Switzer JA, Hall C, Gross H et al.. A web-based telestroke system facilitates rapid treatment of acute ischemic stroke patients in rural emergency departments. J Emerg Med. 2009;36(1):12-18. [DOI] [PubMed] [Google Scholar]
- 30. Schwab S, Vatankhah B, Kukla C et al.. Long-term outcome after thrombolysis in telemedical stroke care. Neurology. 2007;69(9):898-903. [DOI] [PubMed] [Google Scholar]
- 31. Handschu R, Scibor M, Willaczek B et al.. Telemedicine in acute stroke: remote video-examination compared to simple telephone consultation. J Neurol. 2008;255(11):1792-1797. [DOI] [PubMed] [Google Scholar]
- 32. Pirris SM, Monaco EA, Tyler-Kabara EC. Telemedicine through the use of digital cell phone technology in pediatric neurosurgery: a case series. Neurosurgery. 2010;66(5):999-1004. [DOI] [PubMed] [Google Scholar]
- 33. Owler BK, Carmo KA, Bladwell W et al.. Mobile pediatric neurosurgery: rapid response neurosurgery for remote or urgent pediatric patients. J Neurosurg Pediatr. 2015;16(3):340-345. [DOI] [PubMed] [Google Scholar]
- 34. Hayward K, Han SH, Simko A, James HE, Aldana PR. Socioeconomic patient benefits of a pediatric neurosurgery telemedicine clinic. J Neurosurg Pediatr. published online: October 25, 2019 (doi:10.3171/2019.8.PEDS1925). [DOI] [PubMed] [Google Scholar]
- 35. Jackson EM, Costabile PM, Tekes A et al.. Use of telemedicine during interhospital transport of children with operative intracranial hemorrhage. Pediatr Crit Care Med. 2018;19(11):1033-1038. [DOI] [PubMed] [Google Scholar]
- 36. Debono B, Bousquet P, Sabatier P, Plas JY, Lescure JP, Hamel O. Postoperative monitoring with a mobile application after ambulatory lumbar discectomy: an effective tool for spine surgeons. Eur Spine J. 2016;25(11):3536-3542. [DOI] [PubMed] [Google Scholar]
- 37. Williams GW, Buendia FI, Idowu OO. Utilization of a mobile videoconferencing tool (FaceTime) for real-time evaluation of critically ill neurosurgical patients. J Neurosurg Anesthesiol. 2015;27(1):72. [DOI] [PubMed] [Google Scholar]
- 38. Narenthiranathan NR, Adnan JS, Haspani MS. Tailoring teleconsultation to meet the current needs of neurosurgical services: a multimodality oriented neurosurgical consultation. Stud Health Technol Inform. 2010;161:112-121. [PubMed] [Google Scholar]
- 39. Wong HT, Poon WS, Jacobs P et al.. The comparative impact of video consultation on emergency neurosurgical referrals. Neurosurgery. 2006;59(3):607-613; discussion 607-613. [DOI] [PubMed] [Google Scholar]
- 40. Stormo A, Sollid S, Stormer J, Ingebrigtsen T. Neurosurgical teleconsultations in northern Norway. J Telemed Telecare. 2004;10(3):135-139. [DOI] [PubMed] [Google Scholar]
- 41. Dadlani R, Mani S, A UJ et al.. The impact of telemedicine in the postoperative care of the neurosurgery patient in an outpatient clinic: a unique perspective of this valuable resource in the developing world – an experience of more than 3000 teleconsultations. World Neurosurg. 2014;82(3-4):270-283. [DOI] [PubMed] [Google Scholar]
- 42. Thapa A, Shrestha D, Shrestha D, Giri S. Use of viber app: a fast, easy and cost effective method of communication in neurosurgery. Neurol India. 2013;61(6):610-613. [DOI] [PubMed] [Google Scholar]
- 43. Rudinsky B, Gubric J, Gubricova M, Rudinska L. Telemedicine in urgent neurosurgery. Bratisl Lek Listy. 2001;102(6):294-297. [PubMed] [Google Scholar]
- 44. Poon WS, Leung CH, Lam MK, Wai S, Ng CP, Kwok S. The comparative impact of video-consultation on neurosurgical health services. Int J Med Inform. 2001;62(2-3):175-180. [DOI] [PubMed] [Google Scholar]
- 45. Goh KY, Tsang KY, Poon WS. Does teleradiology improve inter-hospital management of head-injury? Can J Neurol Sci. 1997;24(3):235-239. [DOI] [PubMed] [Google Scholar]
- 46. Bailes JE, Poole CC, Hutchison W, Maroon JC, Fukushima T. Utilization and cost savings of a wide-area computer network for neurosurgical consultation. Telemed J. 1997;3(2):135-139. [DOI] [PubMed] [Google Scholar]
- 47. Urban V, Busert C, Huwel N, Perneczky A. Teleconsultation: a new neurosurgical image transfer system for daily routine and emergency cases – a four-year study. Eur J Emerg Med. 1996;3(1):5-8. [DOI] [PubMed] [Google Scholar]
- 48. Goh KY, Lam CK, Poon WS. The impact of teleradiology on the inter-hospital transfer of neurosurgical patients. Br J Neurosurg. 1997;11(1):52-56. [DOI] [PubMed] [Google Scholar]
- 49. Thakar S, Rajagopal N, Mani S et al.. Comparison of telemedicine with in-person care for follow-up after elective neurosurgery: results of a cost-effectiveness analysis of 1200 patients using patient-perceived utility scores. Neurosurg Focus. 2018;44(5):E17. [DOI] [PubMed] [Google Scholar]
- 50. Reider-Demer M, Raja P, Martin N, Schwinger M, Babayan D. Prospective and retrospective study of videoconference telemedicine follow-up after elective neurosurgery: results of a pilot program. Neurosurg Rev. 2018;41(2):497-501. [DOI] [PubMed] [Google Scholar]
- 51. Hassan R, Siregar JA, NA ARM. The implementation of teleneurosurgery in the management of referrals to a neurosurgical department in hospital Sultanah Amninah Johor Bahru. Malays J Med Sci. 2014;21(2):54-62. [PMC free article] [PubMed] [Google Scholar]
- 52. Bertani A, Menguy P, Delmas JM et al.. Assessment of surgical teleconsultations in a developing country: two years of experience in Djibouti. Med Sante Trop. 2012;22(4):405-408. [DOI] [PubMed] [Google Scholar]
- 53. Mrak G, Paladino J, Dzubur A, Desnica A. Telemedicine in neurosurgery: teleradiology connections in the Republic of Croatia. J Telemed Telecare. 2009;15(3):142-144. [DOI] [PubMed] [Google Scholar]
- 54. Waran V, Selladurai BM, Bahuri NF, George GJ, Lim GP, Khine M. Teleconferencing using multimedia messaging service (MMS) for long-range consultation of patients with neurosurgical problems in an acute situation. J Trauma. 2008;64(2):362-365; discussion 365. [DOI] [PubMed] [Google Scholar]
- 55. Kreutzer J, Akutsu H, Fahlbusch R, Buchfelder M, Nimsky C. Teleradiology in neurosurgery: experience in 1024 cases. J Telemed Telecare. 2008;14(2):67-70. [DOI] [PubMed] [Google Scholar]
- 56. Yamada M, Watarai H, Andou T, Sakai N. Emergency image transfer system through a mobile telephone in Japan: technical note. Neurosurgery. 2003;52(4):986-988; discussion 988-990. [DOI] [PubMed] [Google Scholar]
- 57. Lyden P, Brott T, Tilley B et al.. Improved reliability of the NIH stroke scale using video training. NINDS TPA stroke study group. Stroke. 1994;25(11):2220-2226. [DOI] [PubMed] [Google Scholar]
- 58. Schwamm LH, Holloway RG, Amarenco P et al.. A review of the evidence for the use of telemedicine within stroke systems of care: a scientific statement from the American Heart Association/American Stroke Association. Stroke. 2009;40(7):2616-2634. [DOI] [PubMed] [Google Scholar]
- 59. Craig JJ, McConville JP, Patterson VH, Wootton R. Neurological examination is possible using telemedicine. J Telemed Telecare. 1999;5(3):177-181. [DOI] [PubMed] [Google Scholar]
- 60. Meyer BC, Raman R, Chacon MR, Jensen M, Werner JD. Reliability of site-independent telemedicine when assessed by telemedicine-naive stroke practitioners. J Stroke Cerebrovasc Dis. 2008;17(4):181-186. [DOI] [PubMed] [Google Scholar]
- 61. Centers for Medicare & Medicaid Services Medicare Telemedicine Health Care Provider Fact Sheet. Baltimore, MD: Centers for Medicare & Medicaid Services; 2020. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Accessed 6 April, 2020. [Google Scholar]
- 62. Centers for Medicare & Medicaid Services COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers. Baltimore, MD: Centers for Medicare & Medicaid Services; 2020. https://www.cms.gov/about-cms/emergency-preparedness-response-operations/current-emergencies/coronavirus-waivers. Accessed 6 April, 2020. [Google Scholar]
- 63. Basil GW, Eichberg DG, Perez-Dickens M et al.. Letter: implementation of a neurosurgery telehealth program amid the COVID-19 crisis-challenges, lessons learned, and a way forward. Neurosurgery. published online: May 9, 2020 (doi:10.1093/neuros/nyaa215). [DOI] [PMC free article] [PubMed] [Google Scholar]