Abstract
Rhabdomyosarcoma (RMS) is the most common soft tissue sarcoma in children and represents a high-grade neoplasm of skeletal myoblast-like cells. Decades of clinical and basic research have gradually improved our understanding of the pathophysiology of RMS and helped to optimise clinical care. The two major subtypes of RMS, originally characterized based on light microscopic features, are driven by fundamentally different molecular mechanisms and pose distinct clinical challenges. Curative therapy depends on control of the primary tumor, which can arise at many distinct anatomic sites, as well as controlling disseminated disease that is known or assumed to be present in every case. Sophisticated risk-stratification for children with RMS incorporates a variety of clinical, pathological, and molecular features, and that information is used to guide the application of multi-faceted therapy. Such therapy has historically included cytotoxic chemotherapy as well as surgery, ionizing radiation, or both. This Primer describes our current understanding of RMS epidemiology, disease susceptibility factors, disease mechanisms, and elements of clinical care including diagnostics, risk-based care of newly diagnosed and relapsed disease, and the prevention and management of late effects in survivors. We also outline potential opportunities to further translate new biological insights into improved clinical outcomes.
Keywords: Rhabdomyosarcoma, soft tissue sarcoma, translocation-driven neoplasms, childhood cancer, PAX3-FOXO1 fusion protein
Introduction
Soft tissue sarcoma accounts for ~7% of cancers in children and 1% of cancers in adults1. Approximately half of the population of pediatric patients with soft tissue sarcoma have rhabdomyosarcoma (RMS), which is a high-grade, malignant neoplasm in which cancer cells have a propensity for myogenic differentiation. Two major RMS subtypes exist, ‘alveolar’ RMS (ARMS) and ‘embryonal’ RMS (ERMS), which are driven by fundamentally different mechanisms. Both subtypes pose substantial clinical challenges because achieving a cure requires controlling the primary tumor, which may arise in a wide variety of anatomical sites, by surgical resection and/or ionizing radiation and eradicating systemic metastatic disease using intensive chemotherapy. The past 30 years have witnessed dramatic improvements in survival for many children with RMS, as evidenced by the development and implementation of sequential clinical trials conducted nationally or internationally as cooperative groups spanning North America and Europe 2-7. Moreover, advancements in molecular biology and genetics have also enabled more sophisticated understanding of RMS pathogenesis. Those approaches continue to provide a platform to improve diagnosis, disease classification, patient risk-stratification and management strategies.
ARMS and ERMS have emerged as the two major RMS subtypes based on light microscopic features of cells distributed around an open central space 8 or cells resembling immature skeletal myoblasts 9. That distinction was supported by the recognition that ARMS was often associated with balanced chromosomal translocations involving chromosomes 2 or 1 and chromosome 13 (referred to here as t(2;13) and t(1;13)), originally detected by cytogenetics 10-12. As described in detail below, a small but substantial fraction of patients with ARMS do not harbor one of these translocations, and those tumors are biologically and clinically similar to ERMS.
The World Health Organization (WHO) also recognizes two rarer RMS subtypes. Pleomorphic RMS is a morphological variant of RMS that typically occurs in adults 13. Like ERMS, unifying molecular genetic aberrations in pleomorphic RMS are not yet clear. In children, a spindle cell/sclerosing RMS variant is seen; those tumors arising in the head/neck region seem to be more likely to carry specific somatic mutations and have a poorer prognosis13.
Disease classification of RMS subtypes has been further refined by the identification of ‘fusion positive’ (FP) and ‘fusion negative’ (FN) RMS. Molecular biology approaches and next-generation DNA and RNA sequencing have shown ARMS-associated translocations to generate novel fusion proteins involving paired box protein PAX3 or PAX7 and forkhead box protein O1 (FOXO1) 14,15,16. Excluding pleomorphic RMS that occurs in adults, most experts consider childhood RMS to be best described based on fusion status. We adhere to that convention in this Primer, but we use ARMS and ERMS as descriptors when describing pathology reports and earlier research based on those classifiers.
Despite many advances, the chance of cure for children with widely-metastatic and recurrent disease remains very low. Moreover, patients experience months of intensive, multifaceted therapies that can bring life-threatening acute toxicities and, in some cases, life-changing late effects.
In this Primer, focusing on pediatric RMS, we reveal new light being shed on RMS biology through the use of next-generation nucleic acid sequencing and the employment of whole organism-based models of disease. We also discuss how the application of functional approaches for therapeutic target identification and validation should propel further clinical advances.
Epidemiology
Global disease burden
Although a rare disease, RMS is a fairly common form of childhood cancer and is the most common soft tissue sarcoma in children. The overall incidence rate of RMS is approximately 4.5 patients per million individuals aged <20 years17. In the United States, this equates to ~350 new cases per year. On the basis of data from the Surveillance, Epidemiology and End Results (SEER) Program, we know that the incidence of RMS differs both by age and histology18 (Figure 1). Moreover, the incidence of RMS in Europe appears to be similar to that in the United States. For example, a 2016 report from Sweden indicates an overall annual incidence of 4.9 patients with RMS per million individuals aged <15 years19. Interestingly, the incidence of RMS appears to be lower in parts of Asia with just over 2 patients per million individuals reported in Japanese, Indian, and Chinese populations 20.
Figure 1: RMS incidence varies with age and subtype.
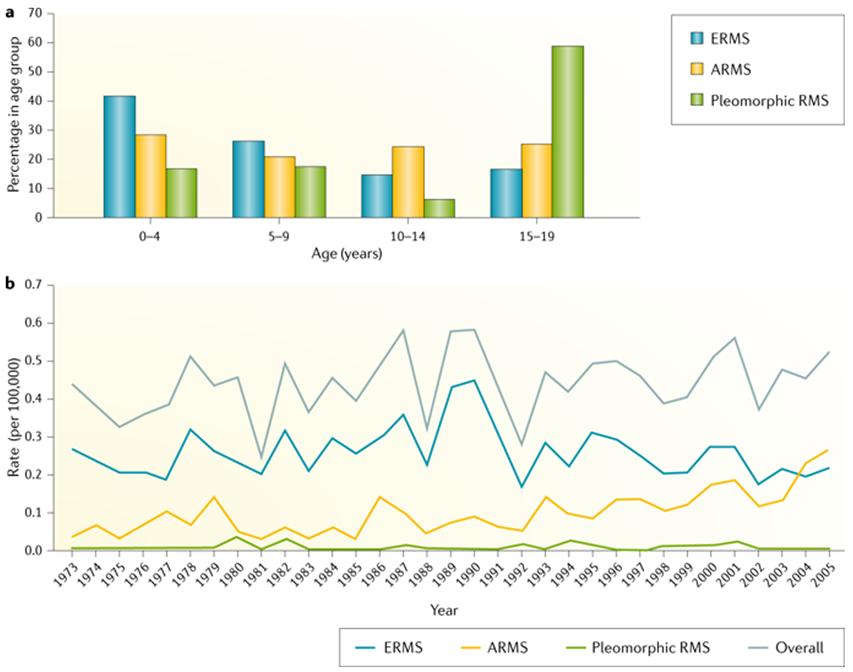
(A) Graph showing the relative proportion of each RMS subtypes presenting in various age groups. Spindle cell/sclerosing and botryoid forms not shown owing to their relative rarity. Note that relative frequency of PAX7-FOXO1 and PAX3-FOXO1 ARMS across the age spectrum has not been well studied and is captured by SEER. (B) Graph showing how the incidence of each major RMS subtype has changed or remained stable over the past ~30 years. The apparent increased incidence of ARMS since the 1990s, but that may, in part, relate to evolving diagnostic definitions, as described in the main text. Data are from the Surveillance, Epidemiology, and End Results (SEER) April 2008 release. Figure has been reproduced with permission from18. ARMS, alveolar rhabdomyosarcoma; ERMS, embryonal rhabdomyosarcoma.
Influence of age and sex
RMS incidence rates are influenced by several factors intrinsic to the tumor and to individual patients. For example, a recent analysis of SEER data showed the diagnosis of ERMS to be ~2.5-fold more frequent than ARMS18. However, the exact frequency of these two forms is affected by evolving diagnostic criteria (discussed below), especially in North America 13,18. Age also influences RMS incidence. ERMS is the most common form in early childhood (Figure 1A), but some data suggests a second peak in early adolescence for ERMS (Supplemental Figure 1) 21. Bimodal peaks are not evident in children with ARMS; incidence of ARMS remains constant throughout childhood and adolescence 17. We also note that one report showed the median age of children with PAX7–FOXO1-positive disease to be younger than those with PAX3–FOXO1 RMS (age 6 versus 13 years)22, but that conclusion from a small, retrospective analysis of a limited number of US institutions has uncertain significance. In contrast to ERMS and ARMS, WHO-classified pleomorphic RMS primarily occurs in adult males in their 6th decade of life 23. “Pleomorphic” RMS in children is typically classified as ERMS with diffuse anaplasia13.
RMS incidence also varies by sex, as male children have a higher incidence of ERMS compared to female children (male:female ratio of 1.51, 95% confidence interval (CI): 1.27–1.80) 21. On the basis of an analysis of pooled cancer registry data from five US states, which focused on the risk of RMS by parental ethnicity, overall notable differences in incidence by ethnicity have not been observed24. The only exception was that the risk of RMS in children was significantly lower when both parents were of Hispanic ethnicity (odds ratio of 0.65, 95% CI: 0.48–0.88).
Using data from SEER, several groups have reported the incidence of ERMS for the period 1975–2005 to have remained relatively stable 18,25. In contrast, a significant increase in the incidence of ARMS (annual percentage change of 4.20%, 95% CI: 2.60–5.82) was evident over the same period (Figure 1B). This apparent increase may be related to fluctuations in diagnostic criteria, such as the proportion of the tumor required to display alveolar features in order to diagnose ARMS. Although the use of a more objective RMS classification scheme based on presence or absence of the t(2;13) or t(1;13) translocations or expression of PAX3–FOXO1 or PAX7–FOXO1 fusion transcript may clarify this matter, that information has not been captured by SEER or many other large cancer registries.
Risk factors
As opposed to osteosarcoma 26 and Ewing sarcoma 27 (two other fairly common childhood soft tissue sarcomas), there has not been a published genome-wide associations study for RMS. Moreover, whole-exome and whole-genome sequencing has identified somatic mutations in RMS 28-30, but few studies have characterized the role of germline DNA on disease susceptibility. It remains challenging to define risk factors in a rare cancer type with an incidence of 4–5 patients per million individuals. However, a great deal of literature exists to support the hypothesis that genetic susceptibility and environmental factors play a part in RMS development.
Genetic risk factors.
Numerous reports highlight that children with certain genetic disorders develop RMS more frequently than unaffected peers. Syndromes that are most commonly seen in children with ERMS include Li-Fraumeni syndrome (germline mutation of TP53, a tumour suppressor)31; Neurofibromatosis type I (deletions in the NF1 gene) 32,33; Costello syndrome (HRAS mutation) 34,35; Noonan syndrome (germline genetic variants activating RAS–MAPK pathways) 34; Beckwith-Wiedemann syndrome 36, and DICER1 syndrome (germline DICER1 mutations) 37 (Table 1). However, on the basis of smaller clinic-based studies, only ~5% of patients with RMS are thought to have co-morbid germline susceptibility syndromes 38. Interestingly, cancer predisposition syndromes appear to be more frequent in patients with ERMS as compared to those with ARMS 33-35,39. This finding seems to contrast experimental studies showing that germline loss of specific tumor suppressors facilitates PAX3–FOXO1-driven neoplasia in genetically-engineered mouse models 40. Importantly, large population-based studies are required to systematically characterize mutations (Table 1) in children with RMS and to evaluate differences by fusion-protein status.
Table 1:
Heritable syndromes associated with an increased risk of RMS
| Syndrome | Phenotype | Associated gene(s) | References |
|---|---|---|---|
| Li-Fraumeni | Cancer susceptibility syndrome | TP53 | 31 |
| Neurofibromatosis type 1 | Systemic effects | NF1 | 32,33 |
| DICER1 | Cancer susceptibility syndrome | DICER1 | 37 |
| Costello | Systemic effects | HRAS | 34,35 |
| Noonan | Systemic effects | BRAF; KRAS; NRAS; PTPN11; RAF1; SOS1 | 34 |
| Beckwith-Wiedemann syndrome | Overgrowth disorder | IGF2; CDKN1C; H19; KCNQ1OT1 | 36 |
Environmental risk factors.
Several environmental exposures and other factors have been implicated in RMS risk in children. Many published reports are based on a large epidemiological case-control study of RMS that was enabled through the former Intergroup Rhabdomyosarcoma Study Group (IRSG) and current Children’s Oncology Group (COG), who drive therapeutic studies for 80–85% of all children with RMS in North America 41. In that study, 322 patients with RMS aged ≤20 at the time of diagnosis and 322 control individuals matched by sex, age and ethnicity were enrolled between April 1982 to July 1988. Key findings include prenatal X-ray exposures25, parental recreational drug use 42, and several other factors43-45, correlating with increased risk for RMS (Table 2).
Table 2:
Environmental and other risk factors associated with RMS development
| Risk factor | OR (95% CI) | Referencea |
|---|---|---|
| Birth defects | 2.4 (0.9–6.5) | 33 |
| Prenatal X-ray exposure | 1.9 (1.1–3.4) | 25 |
| Maternal drug use | 3.1 (1.4–6.7) | 42 |
| Paternal drug use | 2.0 (1.3–3.3) | 42 |
| Childhood allergies | 0.6 (0.4–0.9) | 44 |
| Use of fertility medications | 0.7 (0.2–2.3) | 43 |
| Vaginal bleeding during pregnancy | 1.8 (1.1–2.7) | 43 |
| Premature birth | 2.5 (0.7–8.5) | 43 |
| First–degree relative with ERMS | 2.4 (1.5–3.9)b | 45 |
| First-degree relative with ARMS | 1.0 (0.3–3.5) | 45 |
| Paternal exposure to Agent Orange | 1.7 (0.6–5.4) | 234 |
This table summarizes findings from a series of case-control studies of Intergroup Rhabdomyosarcoma Study III in which environmental exposure and other clinical factors are correlated with risk for RMS development.
Combined with data from the Utah Population Database
ARMS, alveolar RMS; ERMS, embryonic RMS; OR, odds ratio; CI, confidence interval; RMS, rhabdomyosarcoma. Ranges that are significant are highlighted by bold.
Knowledge gaps
In contrast to research into osteosarcoma and Ewing sarcoma 46,47, the epidemiology of RMS has been understudied. Although clusters of cases have been reported in the literature 48,49, it remains unclear if these patterns are indicative of specific aetiologies or due to chance alone. A molecular basis for the apparent influence of male sex or Hispanic ethnicity on RMS diagnosis also remains unknown. Additional studies are needed to describe the global distribution of RMS across the age spectrum and to identify risk factors for this childhood cancer, as prevention strategies are not well developed or routinely implemented. Future studies should be conducted in a large scale setting because some associations identified in smaller analyses have not been confirmed in independent assessments.
Mechanisms/pathophysiology
The two major subtypes of RMS, ARMS and ERMS, were originally recognized based on light microscopic features. However, the pathogenesis of those two subtypes is distinct, as ARMS tumour cells usually contain a balanced chromosomal translocation generating an oncogenic “fusion protein” that is absent in ERMS. As the fusion protein has considerable biological and clinical implications and not all ARMS cases harbor a fusion protein, most experts feel RMS is better classified as FP and FN disease. Many insights into RMS pathogenesis stemmed initially from analyses of tumor-derived DNA and RNA. Genomics approaches are being complemented by functional approaches to study disease mechanisms in a variety of models (Box 1).
Box 1: Functional genomic insights into RMS.
Functional genomics approaches are increasingly used to explore the importance of genes implicated by next-generation sequencing and to identify new candidate disease drivers that were not apparent based on mutations. These approaches include organism-level model systems and higher throughput, cell culture-based genomics studies.
Cultured cells and genetically-engineered mouse models are used to study fusion positive (FP) and fusion negative (FN) rhabdomyosarcoma (RMS). For example, expression of the alveolar RMS (ARMS) associated PAX3–FOXO1 fusion protein in a variety of cell types, including human fetal skeletal muscle cells 217 and mouse mesenchymal stem cells 224, promotes a malignant in vitro phenotype, which can be increased with other genetic manipulations of tumour suppressors, such as expression of a dominant negative form of p53 or knock-down of INK4A 50,224. Similarly, stable ectopic expression of oncoproteins RASV12G, SV40 T/t Ag, and hTERT in human skeletal muscle progenitor cells fosters the formation of embryonic RMS (ERMS)-like xenografts in immunocompromised mice 217.
Mouse models have been generated that conditionally express the mouse Pax3–Foxo1 allele only in skeletal muscle cells40. These animals develop ARMS-like tumors at a very low tumor incidence, which increases when bred into p53 or Ink4a/Arf deficient backgrounds40.
Several models of FN RMS have been established in mice and zebrafish. A heterozygous knockout of Ptch1 (encoding a receptor for sonic hedgehog) in mice causes a high frequency of RMS225. This finding suggested that sonic hedgehog deregulation might be sufficient for RMS, which is further evidenced as this pathway is activated in non-myogenic progenitors of RMS 51,226. This finding also suggests that RMS does not necessarily arise from cells destined to form skeletal muscle. Another FN mouse model was established by broad transgenic expression of Scatter Factor/Hepatocyte Growth Factor (SF/HGF) using the mouse metallothionein I promoter, which leads to high frequency RMS when bred into Cdkn2a (encoding a negative regulator of cell proliferation) knock-out animals 218.
A RAS-driven zebrafish model of ERMS has also been established 213. Microarray analysis identified a RAS-induced gene signature in common between the model and human ERMS – an interesting finding as activating mutations in RAS genes are among the most highly recurrent mutations in RMS 28,29,30. These models should enable discovery of cooperating genetic and gene expression changes in RMS 130 and be amenable to high throughput screening approaches.
It should be noted that, although all subtypes of RMS resemble skeletal myoblasts, the cell of origin is not well characterized. Indeed, elegant genetic models indicate that RMS-like tumors can form when certain oncogenic proteins are expressed in cells from the skeletal myoblast lineage 40,50, but also in non-myogenic cells 51. It is conceivable that RMS driven by different oncogenic changes or at different anatomic sites may originate in different types of cells that are programmed during tumor formation to express a complement of skeletal myocyte genes.
Fusion-positive RMS
Fusion proteins generated by translocations.
Cytogenetic studies identified recurrent chromosomal translocations, including a frequent t(2;13)(q35;q14) or a variant t(1;13)(p36;q14), in the majority of patients with ARMS52,53 (Figure 2). These translocations juxtapose PAX3 on chromosome 2 or PAX7 on chromosome 1 with FOXO1 on chromosome 13 14,15,54. PAX3 and PAX7 encode highly related members of the paired box transcription factor family, which are expressed in skeletal muscle progenitors, whereas FOXO1 encodes a widely-expressed member of the fork head transcription factor family. The t(2;13) and t(1;13) translocations respectively generate PAX3–FOXO1 and PAX7–FOXO1 fusion genes that are expressed as fusion transcripts and translated into neomorphic fusion proteins. These fusion genes encode chimeric transcription factors containing an N-terminal PAX3 or PAX7 region with an intact DNA binding domain and a carboxyl-terminal FOXO1 region containing an intact transcriptional activation domain. In contrast to wild-type PAX3 and PAX7 proteins, the PAX3–FOXO1 and PAX7–FOXO1 fusion proteins have enhanced transcriptional activity, which is attributed to decreased sensitivity of the FOXO1 transactivation domain to the inhibitory effects of N-terminal PAX3 or PAX7 domains 55,56. In addition to the functional effects, there is higher expression of PAX3–FOXO1 and PAX7–FOXO1 mRNA and protein relative to the wild-type products 57. The high level of PAX3–FOXO1 expression results from a copy number-independent increase in transcription of the fusion gene whereas the high level of PAX7–FOXO1 expression results from increased copy number due to in vivo amplification of the fusion gene57.
Figure 2: PAX–FOXO1 fusion gene drives RMS formation.
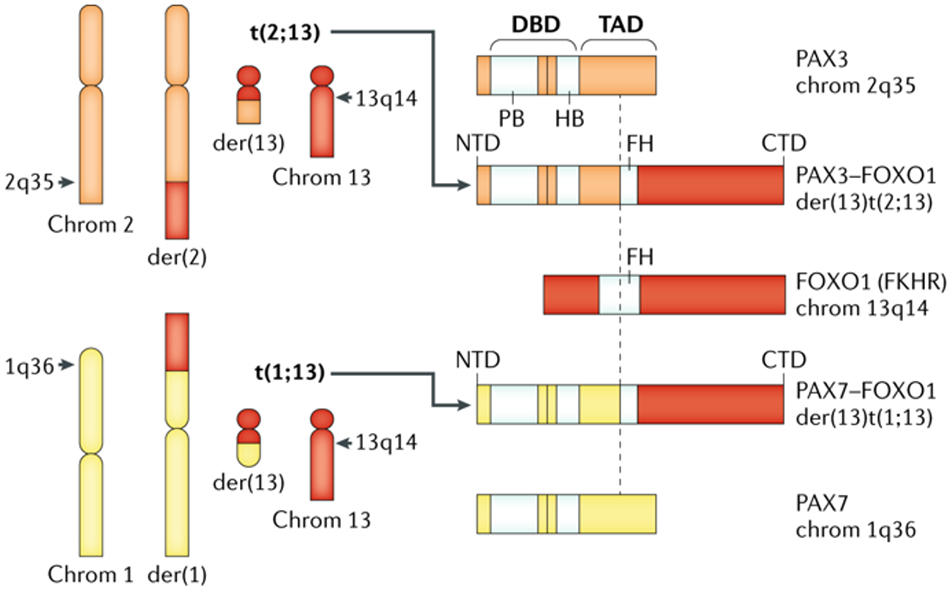
FP RMS is defined by balanced translocations between PAX3, residing in the Giemsa band 35 on the long (q) arm of chromosome 2 (2q35) or PAX7 on chromosome 1 (1q36) with the FOXO1 gene on chromosome 13 (13q14) generating fusion proteins. These balanced translocations generate two derivative (der) chromosomes (left side panel), only one of which encodes for the PAX3 (or PAX7)-FOXO1 fusion mRNA and protein (right side of panel). These fusion proteins contain the amino terminal portion of either PAX3 or, less commonly, PAX7 and the carboxyl portion of FOXO1. The amino terminus of the fusion protein includes motifs needed for DNA binding from the respective PAX gene, and the carboxyl terminus of the fusion protein is felt to alter the transcriptional activation domain of the oncogenic transcription factor. Note that the alternate derivative chromosomes are not known to contribute to RMS pathogenesis. Chrom, chromosome; FP, fusion positive; RMS rhabdomyosarcoma; der; derivative chromosome; DBD, DNA binding domain; TAD, transcriptional activation domain; PB, paired-box domain; HB, homeobox domain; FH, Forkhead-related domain; FKHR, forkhead homolog in RMS (original designation of FOXO1 gene).
Post-translational modifications.
The expression and/or function of the PAX3–FOXO1 fusion protein, the most well-studied of RMS-associated fusion proteins, is also influenced at the post-translational level. Within the C-terminal FOXO1 region, there are multiple phosphorylation and acetylation sites. Some of these sites, such as AKT kinase-dependent phosphorylation sites at S437 and S500, regulate the subcellular localization and degradation of wild-type FOXO1 but not PAX3–FOXO1 58. However, the stability of the fusion protein is influenced by post-translational modifications at other sites. Expression of the PAX3–FOXO1 fusion protein is stabilized by S503 phosphorylation mediated by the serine/threonine protein kinase PLK1 and by K426 and K429 acetylation mediated by the histone acetyltransferase KAT2B. Interestingly, pharmacological inhibition of PLK1 or KAT2B in ARMS-derived tumor cells results in ubiquitin-mediated degradation of PAX3–FOXO1, an observation which could lead to ultimately lead to a way to therapeutically target this oncogenic fusion protein59,60. In addition, studies with the pharmacological kinase inhibitor PKC412 revealed a regulatory role for phosphorylation of the N-terminal PAX3 region on DNA binding and transcriptional function of the fusion protein 61. As multiple phosphorylation sites appear to be involved, the specific proteins mediating these events have not been identified.
Transcriptional and epigenetic effects.
As a transcription factor, the PAX3–FOXO1 fusion protein usually functions in ARMS tumour cells as an activator that increases the expression of downstream target genes by binding to PAX3 binding sites near these genes. ChIP-Seq studies demonstrated that most regions bound by PAX3–FOXO1 are situated >2.5 kb distal to the nearest transcriptional start site and were associated with active enhancer chromatin marks, such as acetylation of histone 3 K27 62,63. Furthermore, these regions often contain E-box DNA binding motifs in addition to PAX3 binding sites. PAX3–FOXO1 binds to these regions along with the E-box-specific transcription factor N-Myc (encoded by MYCN), and myogenic basic helix-loop-helix transcription factors, MyoD1 and Myogenin (encoded by MYOD1 and MYOG), and generates super enhancers near a subset of target genes, including ALK (encoding Anaplastic Lymphoma Kinase), FGFR4 (encoding fibroblast Growth Factor Receptor 4), and MYCN, MYOD1 and MYOG. In addition, PAX3–FOXO1 also interacts directly or indirectly with chromatin-related proteins, including chromatin remodeling proteins Bromodomain Containing 4 (BRD4) and the Chromodomain Helix DNA binding protein CHD4 63,64. By interacting with these transcription factors and chromatin-related proteins, PAX3–FOXO1 likely reprograms the chromatin landscape and establishes super-enhancers that associate with target gene promoters by three-dimensional looping. The co-dependence of ARMS cells on the fusion protein as well as these other collaborating proteins is demonstrated by the high sensitivity of ARMS cells to siRNAs and small molecules targeting each of these proteins 63,64.
Oncogenic effects.
The PAX3–FOXO1 and PAX7–FOXO1 fusion proteins function as oncoproteins by dysregulating multiple cellular pathways (Table 3). Following gene transfer into several mammalian cell types, exogenous PAX3–FOXO1 expression is associated with transforming activity, including loss of contact inhibition of proliferation and gain of anchorage independence65,66. Repression of PAX3–FOXO1 expression in patient-derived human ARMS cell lines with siRNA or shRNA constructs results in decreased proliferation and survival, increased differentiation, and decreased motility and invasion 67,68. Moreover, a mouse knock-in model that conditionally expresses a Pax3–Foxo1 fusion in cells of the myogenic lineage develops ARMS-like tumors, and tumor susceptibility is greatly increased in animals lacking tumor suppressors encoded by either the p53 or Cdkn2a genes 40. The oncogenic effect of these fusion proteins on growth, survival, differentiation and other pathways is mediated through activation of numerous downstream target genes such as the aforementioned ALK, FGFR4, MYCN, and MYOD1 as well as genes encoding the C-X-C motif chemokine receptor 4 (CXCR4) and the MET proto-oncogene receptor tyrosine kinase (MET) 62.
Table 3:
Aberrant gene expression in RMS
| Cause
of aberrant gene expression |
Gene | Effect | Invasion/ Migration |
Proliferation | Transformation | Survival |
|---|---|---|---|---|---|---|
| PAX3/7–FOXO1 fusion protein | CDH3/P-Cadherin | Upregulation | ++ | ++ | − | − |
| CNR1 | Upregulation | ++ | − | − | − | |
| CXCR4 | Upregulation | ++ | ++ | − | − | |
| FGFR4 | Upregulation | − | ++ | − | − | |
| Mutation | − | ++ | ++ | − | ||
| IGF2 | Upregulation and/or loss of imprinting | − | ++ | ++ | ++ | |
| MET | Upregulation | ++ | ++ | − | ++ | |
| MYCN | Upregulation and/or amplification | − | ++ | ++ | − | |
| TFAP2B | Upregulation | ++ | − | − | ++ | |
| Somatic mutation | TP53 | Loss of Function | − | − | − | ++ |
| 12q13-15 | MDM2 | Amplification | − | − | − | ++ |
| CDK4 | Amplification | − | ++ | − | − | |
| 13q31-32 | miR-17-92 | Amplification | − | ++ | − | ++ |
| GPC5 | Amplification | − | ++ | − | − |
++, process is upregulated; −, no effect.
Data from table 3 was originally presented in Ref. 52.
Molecular differences between subtypes
RMS-specific fusion genes can be detected in clinical biopsy material by RT-PCR and fluorescent in situ hybridization (FISH) assays. These assays have revealed that 60% of patients with ARMS express PAX3–FOXO1, 20% express PAX7–FOXO1, and 20% are FN 69. A small subset of patients with ARMS lack detectable PAX3-FOXO1 or PAX7–FOXO1 fusion proteins, but have novel variants, such as PAX3–FOXO4 or PAX3–NCOA1 (NCOA1 encodes nuclear receptor coactivator 1) 70,71. The clinical or biological consequences of these variants are not clear. Nucleic acid sequencing has shown that patients with FN ARMS do not express fusion proteins but instead show genetic changes in tumour cells that are similar to ERMS tumors, such as whole chromosome gains, recurrent point mutations, and 11p15.5 allelic loss 28,30,72-74. In addition, studies of genome-wide mRNA expression revealed that ERMS and FN ARMS tumors have very similar expression profiles, which are distinct from the expression profiles in PAX3–FOXO1-positive and PAX7–FOXO1-positive ARMS tumors 71,72,75. These studies thus provide genetic evidence for the combination of ERMS and FN ARMS tumors into a single FN RMS subset and the combination of PAX3–FOXO1- and PAX7–FOXO1-positive ARMS tumors into a distinct FP RMS subset.
Aberrant signalling pathways
In FN RMS, various mutations have been identified that largely converge on a limited number of pathways. Interestingly, these pathways are also perturbed in FP RMS through upregulation of downstream targets of the fusion proteins and/or genomic amplification, indicating some commonality in the molecular driving forces in RMS (Figure 3).
Figure 3: Key functional pathways are perturbed in RMS.
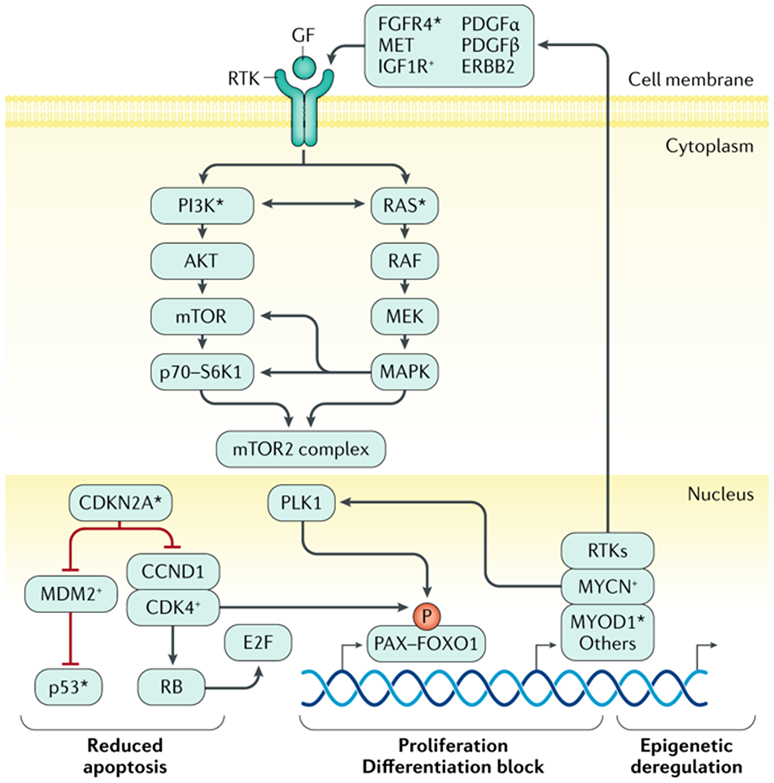
Key processes of apoptosis, cell proliferation, cellular differentiation, and epigenetic homeostasis are deregulated by mutation or gene copy-number and/or gene expression alterations in fusion negative (FN) or fusion positive (FP) rhabdomyosarcoma (RMS). In FP RMS, chromosomal translocations result in PAX3–FOXO1 or PAX7–FOXO1 fusion genes. The aberrant PAX3–FOXO1 fusion protein can synergize with loss of p16 or p53 functionality that is associated with CDKN2A gene loss and/or promoter methylation and TP53 mutation. The stability and subcellular localization of the PAX3–FOXO1 protein is dependent on phosphorylation of specific sites and it works in a complex that can include BRD4. The PAX3-FOXO1 containing complex acts as pioneer factor and drives expression of other transcription factors such as MYCN and MYOD1 via super-enhancers that lead to reprogramming of the transcriptional and epigenetic landscape of tumors. The genes encoding MYCN and MYOD1 transcription factors may themselves be genetically amplified or mutated, likely contributing to RMS formation or progression in a subset of cases, respectively. The fusion protein also drives expression of specific receptor tyrosine kinases (RTKs). Overexpression and activating mutations of genes encoding the same RTKs, and mutation of genes encoding downstream signaling components, are seen in FN RMS. Together this leads to frequent activation of PI3K and RAS pathway signaling in FP and FN RMS, which likely contribute to disease pathogenesis by altering cell proliferation, apoptosis, and other metabolic pathways in ways that are not yet precisely defined. Next-generation DNA sequencing and other molecular genetics tools have demonstrated deleterious mutations in genes encoding certain proteins involved in RMS pathogenesis (*). Exactly how these pathways driven RMS pathogenesis is not clear.
Mutations in RAS–PI3K pathway components.
Aberrations in various genes associated with RAS pathway signaling are predominant in FN RMS. Approximately one third of patients with FN RMS are reported to have activating mutations in key components of the RAS pathway, including mutations in NRAS, KRAS, and HRAS. NRAS mutations are predominant in adolescents and KRAS and HRAS mutations are more frequent in infants aged <1 year 28,74,76. Mutations in genes encoding proteins associated with RAS pathway intracellular signaling, such as protein tyrosine phosphatase, non-receptor type 11 (PTPN11), NF1, the B-Raf proto-oncogene, BRAF (encoding a serine/threonine kinase) and phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA, protein is also known as PI3Kα), are also described. Overall, >50% of patients with FN RMS harbor a mutation expected to impact RAS–RAF–MAPK (mitogen-activated protein kinase 1) and/or PI3K–AKT (serine–threonine kinase 1)–mTOR (mammalian target of rapamycin) pathways 28,30,74,77,76. Activation of these pathways in a large fraction of FN RMS is also supported by gene expression analyses 78-80. These findings are further supported by immunohistochemistry analyses of phosphorylated AKT, MAPK and ribosomal protein S6 kinase B1 (known as S6 Kinase) that show >80% of RMS biopsy samples show activation of the PI3K pathway, with co-activation of the MAPK pathway in over a third of ARMS biopsy samples and nearly half of ERMS biopsy samples81. Various cell surface receptor tyrosine kinases (RTKs) can signal through these pathways, including RTKs that are induced by the fusion protein 62, and these RTKs are implicated in RMS development and progression.
Receptor tyrosine kinase signaling.
Activating mutations in FGFR4 (encoding a fibroblast growth factor receptor), occur in ~7% of patients with FN RMS. The K535 and E550 FGFR mutants activate RAS and STAT (signal transducer and activator of transcription) signaling pathways and induce tumor growth and metastatic behavior in mouse tumor cells expressing the human protein 82. In FP RMS, expression of wild-type FGFR4 and FGFR2 is also elevated as these genes are downstream transcriptional targets of PAX3–FOXO1 62,63, and they contribute to tumor behavior 83-85 (Shipley, unpublished). Similarly, insulin growth factor receptor 1 (IGF1R) is highly expressed in FP RMS, occasionally via genomic amplification 86. Very frequent high expression of the ligand IGF2 also occurs in RMS, resulting from loss of heterozygosity or loss of imprinting of the 11p15.5 locus that encodes the IGF2 and H19 genes. This molecular lesion is more common in patients with FN RMS 28. IGF signaling is pro-survival and anti-apoptotic in RMS tumour cells and increases tyrosine phosphorylation of the insulin receptor substrate-1 (IRS-1) 87. In poor prognosis patients with RMS (that is, those with advanced or metastatic disease), IRS-1 activation appears refractory to normal negative feedback mediated by increased phosphorylated mTOR and S6 Kinase 88, and inhibiting IGF1R activity can promote compensatory regulatory activity of the SRC family kinase, YES 89. The epidermal growth factor receptor tyrosine kinase ERBB2 is frequently expressed 90,91 and upregulated with associated MAPK signalling in response to IGF1R inhibition 92. Furthermore, knockdown of PIK3CA leads to increased expression of PIK3CA isoforms and elevated RAS pathway signaling in cell line models 81. Changes in feedback loops and dynamic signaling after targeting specific pathway components suggests that RMS may need to be treated with combination therapeutic strategies
Other RTKs implicated in RMS development include Ephrin receptors 93. High PAX7 expression sustains migration and invasiveness in ERMS cells by upregulating the Ephrin receptors A3 (EPHA3) and A1 (EFNA1) 94. Moreover, ERMS cell lines deficient in ephrin receptors EPHA2 and EPHB2 have reduced migratory capacity and are induced to differentiate into a myogenic-like phenotype95. Similarly, increased signalling via MET in FN RMS contributes to invasive tumour growth96,97 and PAX3–FOXO1-driven MET expression in FP RMS promotes motility, mainly through extracellular signal-regulated kinase ERK2 98, and blocks myogenic differentiation 99,100. Platelet-derived growth factor receptor alpha (PDGFRA) gene expression is driven by the fusion protein in FP RMS, and PDGFRA is occasionally mutated in FN RMS, whereas the PDGFRB is primarily expressed in the vascular stroma of RMS 28,62,101. Together, PDGFR activity regulates cancer cell stemness, differentiation, senescence, and apoptosis, with the stromal compartment providing a supportive role 102.
Loss of PTEN, TP53 and CDKN2A.
Mutation or promoter methylation of the tumour suppressor PTEN can occur in FN RMS and negatively regulates PI3K signaling 30. In a recent targeted re-sequencing study of tumour cells from 631 patients with FN RMS, TP53 mutations were identified at a higher incidence of 12% than had been previously reported 28,103. High expression of MDM2 occurs in 10% of patients with RMS 28,30, and negatively regulates p53 (encoded by TP53). In addition, promoter methylation, allelic loss and mutation of tumour suppressor cyclin dependent kinase inhibitor 2A (CDKN2A) is frequent. The finding of p53 pathway disruption or loss of CDKN2A in RMS is concordant with model systems in which these changes are synergistic and critical for increasing penetrance in PAX3–FOXO1 transgenic mouse models (Box 1) 30,40,104,105.
Involvement of developmental pathways.
The Catenin Beta 1 gene, CTNNB1, is commonly mutated in FN RMS28,30,74, and β-Catenin and other proteins associated with canonical WNT signaling (a key pathway involved in development) are expressed in a high proportion of FN and FP RMS tumors 106. Notably, inhibition of Wnt Family Member 3a (Wnt3a) protein or Glycogen Synthase Kinase 3 Beta (GSK3B) in cultured RMS cells results in the nuclear translocation and transcriptional activation of β-Catenin in RMS cells, followed by decreased proliferation and the induction of differentiation, which suggests a potential therapeutic approach106,107. Analyses of primary tumors, cell lines, and mouse models supports other developmental pathways contributing to RMS development and progression including Hedgehog (Box 1) 51,108-110, Notch 111 and Hippo signaling pathways 79,112,113. Cross-talk between these developmental pathways and RAS signalling 114 creates an integrated signalling network that supports the development of RMS 111,115.
Myogenic regulation and epigenetics
Mutations in MYOD1 occurring together with mutations in genes of the PI3K–AKT pathway genes define a particularly aggressive form of FN RMS in children and adults 116. Interestingly, DNA binding sites of L122R mutant MYOD1 are similar to those of the MYC proto-oncogene protein117, potentially explaining a switch from differentiation to proliferation. In addition, mutations may lead to decreased MYOD1 binding adjacent to critical myogenic genes, which is thought to contribute to reduced expression of the myogenic program in RMS 118. In FP RMS, the histone methyltransferase KMT1A is highly expressed and associates with MYOD1, thereby adding repressive marks to histone H3K9 residues at MYOD1-regulated target genes, thus blocking differentiation 119. These findings add to our understanding of how MYOD1, which usually promotes the differentiation of skeletal myocytes, contributes to the undifferentiated phenotype of RMS. Similarly, PAX3–FOXO1-driven expression of JARID2 (a regulator of histone methyltransferase complexes) recruits PRC2 (a repressive histone methyltransferase) via EZH2 (the catalytic subunit of PRC2) to the MYOG and MYLH genes, also contributing to failed myogenic differentiation 120,121. Patients with RMS may have mutations in BCOR that inactivate the BCL6 Corepressor, which interacts with histone deacetylases 28,122. Mutations also occur in the gene encoding ARID1A, a protein involved in the SWI/SNF chromatin remodelling complex 28. Together with global and specific changes in DNA methylation and histone marks, and expression of microRNAs and other noncoding RNAs 30,63,123, there is increasing evidence for epigenetic regulation shaping RMS development and progression.
Cellular and physiological processes
From a physiological and cellular level, metastasis is particularly important and often the lethal component of RMS 124. Early studies of FP RMS suggested that presence of the PAX3–FOXO1 fusion transcript correlated with greater metastasis risk than PAX7–FOXO169, but that initial finding has not been consistently validated in clinical trials. Certain experimental models implicate the cannabinoid receptor 1 (Cnr1) or the cytoskeleton-associated protein Ezrin as potential mediators of metastasis induced by the PAX3–FOXO1 fusion protein125 or the Sine Oculis gene SIX1126, respectively. While PAX3-FOXO1 is clearly important in the human disease, whether SIX1 represents a potentially actionable vulnerability or biomarker for metastasis in RMS is not clear. In many epithelial cancers, the epithelial-to-mesenchymal transition (EMT: a complex series of molecular and cellular changes enabling epithelial cells to mobilize during normal organism development or in healing of certain epithelial wounds) plays a critical role to enhance cancer cell mobility and drive metastasis127,128. As a mesenchymal cancer, it remains unclear whether RMS undergoes an EMT-like process. Interestingly, genes well-known to induce EMT, SNAIL 129,130 and SNAIL2131,132, have been implicated as oncogenic drivers for RMS. Expression of SNAIL and SNAIL2 derails the myogenic differentiation program 129,133, which is associated with cell proliferation arrest. However, the underlying cellular mechanisms for metastasis control in RMS remain to be elucidated.
Evading immune surveillance is also widely-recognized as a key process in human cancer134-136. The immune landscape of RMS is understudied. Indeed, little is known about interactions between RMS cells and the tumor stroma and non-stromal elements of the tumor microenvironment, including immune cells. Large next generation-sequencing studies of RMS have focused on characterizing tumor cell-intrinsic features, like single nucleotide variants and gene copy-number alterations, not the tumor microenvironment or stroma 28,29. Similarly, transcriptome profiling identified gene expression signatures correlating with RMS subtype and prognosis 75,78,137, but did not reveal substantial insight into stromal elements, immune surveillance escape mechanisms, or metastasis. Interestingly, gene expression analysis of RMS occurring on the extremities 138 indicated that higher expression of immune genes (for example, β2-microglobulin, complement genes, major histocompatibility complex genes) in the primary tumor correlated with regional lymph node metastasis risk. Defining the tumor stroma and immune cell landscape in RMS may reveal new insights into disease biology. The potential for immune-based therapeutics could still be limited by the relatively low mutational burden in RMS 28,29. Obviously, the fusion proteins driving FP RMS represent neoantigens that, in principle, could be amenable to immune targeting. That possibility is supported by results from a small pilot study suggesting improved survival for children with FP RMS (and also Ewing sarcoma) who received post-cytoreductive consolidation using dendritic cells pulsed with peptides derived from the relevant fusion protein 139.
Diagnosis, screening and prevention
RMS is a global problem and many factors exist that influence delivery of care to childhood cancer patients, including those with RMS (Box 2). The following section focuses on how the disease presents and is managed in what could be construed as an idealized setting.
Box 2: Global Variation in RMS Management.
Little effort has been made to investigate RMS as a global disease. Hints exist that RMS incidence varies across certain ethnic groups, suggesting that population-based genetic variants can influence disease susceptibility and, perhaps disease biology227. Also, global variations in treatment approaches are likely to exist and influence outcomes, as witnessed between European and North American groups 1,177. When considering RMS diagnosis and treatment in low-income and middle-income countries, many factors may limit the delivery of effective childhood cancer therapy, including availability and training of physicians, nurses, and other medical staff; laboratory and pathology services; diagnostic imaging capabilities; availability and security of chemotherapy and blood products; and surgical and radiation oncology facilities and expertise 228. A study of children with RMS and other forms of soft tissue sarcoma in Guatemala highlighted that delayed diagnosis leads to increased numbers of children developing advanced stage disease, and treatment abandonment likely also contributes to poor outcomes229. Conceivably, rapidly improving capabilities of web-based telecommunications/telemedicine capabilities and “twinning” programs could help to realize improved global outcomes.
Clinical presentation
The diagnosis of RMS has been traditionally based on recognizing the features of skeletal myoblast-like tumor cells using light and, in some cases, electron microscopy, and the use of immunohistochemical (IHC) staining for skeletal muscle proteins13,140. RMS can arise in virtually any anatomic site, however, the most common sites depend on the histological subtype: ERMS most commonly arises in the head and neck, including the eye socket, or in genitourinary sites; ARMS typically arises at extremity sites, with a smaller fraction arising in the head and/or neck or torso17. Radiographic or clinical evidence for distant metastatic disease is present in ~20% of children at diagnosis1. Metastases arise by both lymphatic and hematogenous routes, and spread to lung, bone, and bone marrow are relatively common 141.
Few comprehensive studies exist of presenting signs or symptoms in children with RMS. Signs and symptoms are typically associated with soft tissue mass and are often described as painless masses found in the extremities, or head and/or neck region 142,143; they can also be associated with signs and symptoms due to mass effect on adjacent organs or neurovascular tissues, or associated with a visible mass protruding from an orifice. For example, a ‘grape-like’ mass in botryoid RMS of the vagina142,144,145. Orbital primary sites typically present as a unilateral, space occupying lesion with proptosis 146.
Pathological assessment
The diagnosis of RMS requires the direct analysis of tumor tissue from either an incisional or excisional biopsy or core needle biopsy and subjected to a series of histology and molecular pathology studies. The World Health Organization had recognized three histological variants of RMS – ARMS, ERMS, and pleomorphic RMS – with ARMS and ERMS being the most frequent childhood forms. A recent update from the WHO now includes spindle cell/sclerosing RMS as a distinct entity 13,147. Morphologically, RMS cells are of heterogeneous shapes ranging from undifferentiated and round cells, ovoid cells, ‘tadpole-like’ cells, spindle-shaped cells and fully differentiated rhabdomyoblasts. 148,149
As previously mentioned, RMS cells usually display some evidence for skeletal muscle lineage specification and/or differentiation evident by light or electron microscopy and/or IHC or molecular evidence for expression of skeletal muscle gene products like muscle-specific actin and myosin, desmin, myoglobin, Z-band protein, and MyoD1 or myogenin. Notably, a diagnosis of RMS can be made even if only a minority of tumor cells display detectable expression of skeletal muscle proteins. Such a finding reflects the failed terminal differentiation that is central to RMS. However, cellular morphology and architecture must also be considered for accurate diagnosis because myogenic proteins can be expressed in other childhood neoplasms, such as Wilms tumor and malignant triton tumor 149.
ARMS and ERMS.
ARMS and ERMS can be subdivided further based on histological or molecular features. For example, recognized histological variants include botryoid RMS and spindle cell/sclerosing RMS, which are generally associated with a superior prognosis 13. In addition, ARMS can be sub-divided based on the presence or absence of the PAX3–FOXO1 or PAX7–FOXO1 fusion transcript 72. ARMS is typically composed of densely packed, small, round cells lining septations that are reminiscent of pulmonary alveoli, whereas ERMS comprises immature “rhabdomyoblasts” in a less dense, stroma-rich background without an alveolar pattern (Figure 4)150. It should be noted that some RMS specimens can display intra-tumor heterogeneity with a “mixed” phenotype of both alveolar and embryonal features; fusion gene detection in tumor classification is particularly valuable in this context 151,152.
Figure 4: ERMS and ARMS can be distinguished based on histopathology features.
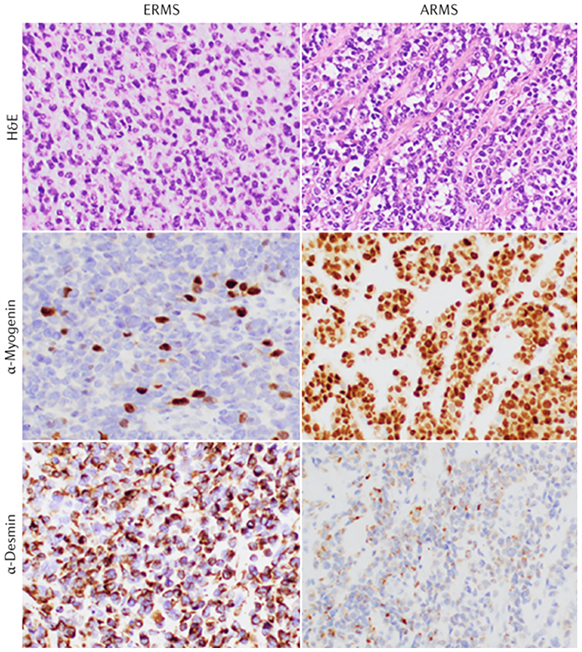
Representative photomicrographs of embryonal RMS (ERMS; left panels) and alveolar RMS (ARMS; right panels) following staining with hematoxylin and eosin (H&E; top panels) or with primary antibodies to detect Myogenin (middle panels) or Desmin (bottom panels) to mark the skeletal muscle lineage. ARMS often, but not always, displays loosely associated tumor cells in clusters resembling pulmonary alveoli and robust immunohistochemical staining for Myogenin; however, confirmation by analysis of PAX3–FOXO1 or PAX7–FOXO1 fusion is required to confirm FP state. Original magnification: 400x (Image provided by D. Rakheja, University of Texas Southwestern Medical Center)(contact information: dinesh.rakheja@utsouthwestern.edu)
Pleomorphic RMS.
Pleomorphic RMS is a rare adult variant of RMS that has distinct histological features (Box 3), which is similarly composed of cells displaying evidence of skeletal muscle lineage commitment or differentiation. Pathological review of biopsy samples from 38 primary tumors revealed three histological sub-types: classic, round cell, and spindle cell, based on general morphology. The pleomorphic rhabdomyoblasts that define this subtype express a range of skeletal muscle proteins detected by immunohistochemistry, which helps discriminate it from adult pleomorphic sarcoma23,153. Pleomorphic RMS generally arises in older adults, more commonly in males, and often involving the lower extremities154. Owing to its rarity, little is known about the pathogenesis of pleomorphic RMS. For example, one report describes very complex cytogenetic and/or chromosomal abnormalities, similar to that seen in children with FN RMS155. Defining molecular abnormalities are not clear for this disease.
Box 3: Adults with RMS.
Although RMS is typically a childhood cancer, it can rarely occur in adults. Scant information is available on the clinical and biological findings of adult RMS. All studies, however, highlight a poorer outcome than in children, with overall survival in the range of 20–50% 230,231. Using data from the Surveillance, Epidemiology and End Results (SEER) program, comparing the clinical features and outcome of 1,071 adults (age > 19 years) and 1,529 children (age ≤ 19 years), one group found that adults were more likely to have adverse prognostic variables (alveolar histology, unfavorable anatomic site like the extremity) and confirmed that adults do have a worse prognosis (5-year overall survival: 26.6% versus 60.5% in children), apparently independent of known prognostic variables 230. Different outcomes may be driven partly by different therapeutic approaches, which is supported by a study analyzing 171 patients aged >18 years with ERMS and ARMS; this team showed a poor 5-year overall survival of 40%, and they noted that only 39% of patients were treated in line with pediatric protocols231. In the patients treated in a manner that parallels childhood RMS therapy, the 5-year overall survival was 61%. In contrast, outcomes for adults with pleomorphic RMS are generally much poorer, with median overall survival of only 12.8 months for those with localized disease 154.
Although fundamental differences in disease mechanisms may exist between children and adults, these reports suggest that pediatric-style chemotherapy is active in adults with RMS, and adults with RMS may have better outcomes if treated with more intensive therapy. However, barriers to developing adult therapy exist. For example, older adults may simply not tolerate intensive treatments originally developed for children 203. A lack of physician familiarity with this disease or awareness of clinical trial opportunities in adults with RMS may also contribute. North American RMS studies often had upper age limits of age 50, but adults were rarely enrolled – a general problem for the adolescent and young adult cancer population 232. Continued efforts to foster communication between adult and pediatric cooperative groups in study trial design and implementation may begin to break down the barriers to management in adults.
Molecular diagnostics
The advent of tools for molecular diagnostics has greatly aided the identification of RMS. In particular, ARMS is more precisely diagnosed as FP RMS based on detecting the presence of PAX–FOXO1 fusion in tumour cells, observed using FISH, or by detecting the fusion transcript by RT-PCR assays156,157 (Figure 5). Systematic application of molecular diagnostic tests to biopsy samples from patients with pathologically diagnosed ARMS reveals that approximately 20% of these patients are negative for the fusion transcript 150. This finding is particularly important because FN ARMS has molecular features reminiscent of ERMS and the clinical outcome of children with FN ARMS parallels that of children with ERMS 158,159.
Figure 5: PAX–FOXO1 translocation can be detected by FISH.
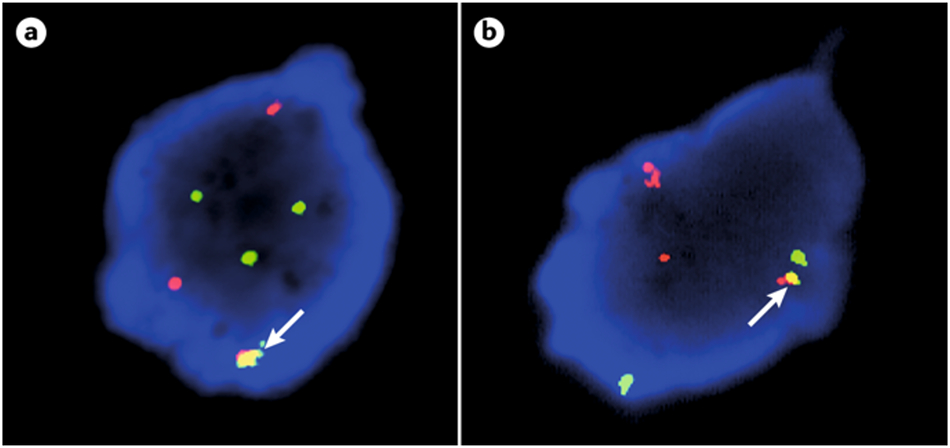
The clinical importance of determining PAX–FOXO1 fusion status in RMS has led to the development of clinical-grade molecular assays, such as fluorescence in situ hybridization (FISH). Here, FOXO1 (13q14) and PAX3 (2q36.1) break-apart probe sets (left and right, respectively) illustrate the splitting of the normally juxtaposed orange and green signals within the neoplastic interphase nuclei of alveolar rhabdomyosarcoma cells, indicating rearrangements of these loci. (Images provided by J. Bridge, University of Nebraska Medical Center)(contact information: jbridge@unmc.edu)
A molecular diagnosis based on fusion status clarifies some confusing issues regarding routine pathology of RMS. For example, the fusion transcript can be detected in many patients with ARMS tumours that have a solid morphology, with relatively few alveolar spaces and in some cases with ‘mixed’ alveolar and embryonal features, clarifying the diagnosis150. With the exception of pleomorphic RMS in adults, all patients with FN RMS are felt to have an equivalent disease to ERMS. However, spindle/sclerosing RMS and botryoid subtypes of ERMS disease can have distinct clinical features, and may also carry distinct molecular defects, such as MYOD1 mutation. Finally, trisomy of chromosome 8 and loss of heterozygosity (LOH) at 11p15 are also relatively common in FN RMS 28,29. Because these chromosomal aberrations are found in other childhood cancers (including some patients with FP RMS), they are not routinely employed to make a diagnosis of FN RMS.
The clinical relevance of fusion status over histology underlines the importance of evaluating fusion gene status to complement traditional pathology assessment, which will enable the diagnosis of FP RMS to be made using a molecular assay. A recent study evaluated the potential for FP and FN RMS to be distinguished by a panel of IHC stains, rather than FISH, a more accessible approach for smaller clinical programs. Strong IHC staining for myogenin, AP2β, and NOS-1 can identify FP status while HMGA2 expression is consistent with FN RMS, and the diagnosis may be made using an algorithmic approach160. On-going COG trials are incorporating fusion gene status into patient risk stratification (https://clinicaltrials.gov/ct2/show/NCT02567435), however, diagnosis only using fusion gene detection has not yet risen to routine practice, nor has the use of IHC staining as a surrogate for evaluating fusion status.
Surveillance and prevention
Surveillance strategies for RMS, like most childhood cancers, are still in early stages of development, and preventive strategies are not clear. In principle, the recognition of genetic syndromes that predispose to RMS (and other cancers) should provide a foundation to focus RMS surveillance strategies. Indeed, at least one report shows the potential value of biochemical and imaging-based surveillance for children with Li-Fraumeni syndrome 161. This research led to a consensus statement advocating for cancer surveillance in children with germline p53 variants 162, as well as recognition of the need for further study 163. Conceivably, advances in next-generation sequencing enabling sensitive detection of circulating, cell-free tumor DNA may lead to affordable and minimally-invasive surveillance for RMS in at-risk populations 164.
Management
General overview
Over >30 years of study in large, cooperative group clinical trials, the 5-year overall survival of pediatric RMS has improved substantially, such that it now exceeds 70% 2,5-7,165-167(Figure 6a). Notably, management and outcome for adults with RMS considerably differs (Box 3). Several factors contribute to this improved survival including: the use of multifaceted therapies that typically include surgical resection of the primary tumor, ionizing radiation to the primary tumor, and multi-agent, intensive chemotherapy; the development of clinical and pathological staging systems enabling risk-adapted therapy; and the systematic evaluation of new therapeutic approaches in multi-institutional clinical trials conducted on a national or international scale.
Figure 6: Survival in children with RMS.
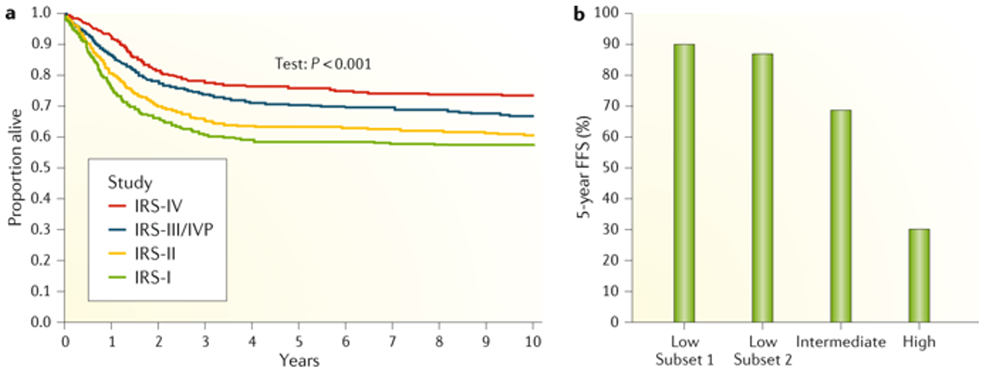
A. A graph showing Kaplan-Meier plots for proportion of children surviving when treated according to successive Intergroup Rhabdomyosarcoma Study Group (IRS) studies from 1972-1997. Overall survival improves in successive RMS clinical trials. Multiple factors contributed to the improved survival, as detailed in the text. B. Clinical outcomes in data from IRS-III and IRS-IV clinical trials, showing failure free survival (FFS) in children with RMS. Note that survival for Intermediate Risk group represents average of survival for children with Stage 2 or 3, Group III ERMS (73%) and those with Stage 1-3, Group I-III ARMS (65%).
Figure 6 part a reproduced from Ref 233. Data in figure 6 part b are from ref 168.
The three main cooperative groups dedicated to RMS are the COG Soft Tissue Sarcoma Committee in North America 168,1, the European pediatric Soft Tissue Sarcoma Study Group (EpSSG), which involves many European countries as well as Argentina, Brazil, and Israel 169, and Cooperative Weichteilsarkom Studiengruppe der GPOH (CWS) group, which includes predominantly German-speaking countries in Europe 170. Cooperative group trials of different childhood soft tissue sarcomas often include the majority of children with that specific disease. For example, a recent EpSSG study compared the number of children enrolled in EpSSG clinical trials with the expected RMS incidence between 2008–2015 showed that 77% of patients with RMS aged <14 years were enrolled 169. Notably, the rate of enrollment for older adolescents and young adults was somewhat lower, which highlights an opportunity to focus future trials on this population.
Curing RMS first requires eradication of the gross primary tumor (that is, local disease), which is often accomplished using a combination of surgery and/or external beam ionizing radiation. Curative therapy has also included systemic chemotherapy to eradicate disseminated disease that is assumed or proven to exist in most children with RMS. That most, if not all, patients have disseminated disease is based, in part, on observations from the 1960s and 1970s, including a Children’s Cancer Study Group A (CCSGA) trial in the US showing common regional and distant recurrence in eight of 15 children treated without chemotherapy 171. Further, sensitive molecular biology tools like reverse transcriptase-polymerase chain reaction has been reported to detect RMS cells in peripheral blood or bone marrow in 12 of 16 children with RMS, even those with grossly localized disease 172. The COG Soft Tissue Sarcoma Committee (and its predecessors, the CCSGA and IRSG) developed and systematically tested a wide variety of approaches to achieve both goals (reviewed in Ref. 1,168) over more than 40 years, and some differences in approaches have evolved over that time. The current standards of care – where they exist – and on-going research goals in the field are outlined in more detail below.
Risk stratification
A major advancement in RMS management is the capacity define risk groups, based on clinical, pathological and, increasingly, molecular features 1,173. Improvements in risk stratification have enabled tailored therapy. The IRSG first introduced the concept that RMS disease status can be described in terms of both “stage” and clinical “group” 168 (Table 4). RMS Stage, from 1 to 4, depends on the anatomic site of the primary tumor (with involvement of the bladder and/or prostate, or the extremities indicating a more advanced stage), tumor size, presence or absence of regional lymph node involvement, and presence or absence of distant metastasis 174. Clinical Group, from I to IV, applies surgical and/or pathological features, including the degree of resection of localized or regionally-spread tumor and presence or absence of distant metastasis 175. Recent recognition that molecularly-defined RMS (that is, FP or FN RMS) 152,158,159 and more detailed consideration of clinical features, including the number of metastatic sites 141, improves our ability to predict outcome, may enable further refined stratification. Further, a number of “metagene” expression signatures may have prognostic value, especially in FN RMS 137,158. The most robust of these is a 5-gene metagene (MG5) signature, which was first defined as a prognostic variable in FN RMS in a European cohort, and has been validated using additional cohorts, including one from the COG 176. Although promising, the MG5 signature has not yet been widely-incorporated in clinical practice.
Table 4:
Staging and clinical group classification systems for RMS
| Stage | Sites | Invasiveness | Size | Nodes | Metastasis |
|---|---|---|---|---|---|
| 1 | Orbit, H/N (non-PM), GU (non-BP), Biliary | T1 or T2 | a or b | N0, N1 or Nx | M0 |
| 2 | BP, Ext, PM, other | T1 or T2 | a | N0 or Nx | M0 |
| 3 | BP, Ext, PM, other | T1 or T2 | a | N1 | M0 |
| b | N0, N1 or Nx | ||||
| 4 | Any | T1 or T2 | a or b | N0, N1 or Nx | M1 |
| Clinical group |
Definition | ||||
| I | Localized disease, completely resected | ||||
| II | Total gross resection with evidence for regional spread | ||||
| II A | Grossly resected tumour with microscopic residual | ||||
| II B | Involved regional LNs, completely resected with no microscopic residual | ||||
| II C | Involved regional LNs, grossly resected with microscopic residual | ||||
| III | Biopsy only or partial resection with gross residual | ||||
| IV | Distant metastatic disease | ||||
Abbreviations: H/N, Head and Neck; PM, parameningeal; BP, bladder/prostate; Ext, extremity; T1, primary tumor confined to anatomic site of origin; T2, primary tumor with extension and/or fixation to surrounding tissue; Size a: primary tumor ≤ 5 cm; Size b: primary tumor > 5 cm; N0, regional nodes not involved; N1, regional nodes involved; Nx, status of regional nodes not known; M0, no distant metastasis; M1, metastasis present (includes positive CSF, pleural or peritoneal cytology).
Risk stratification is used to determine treatment allocation in clinical trials, however, the details of risk stratification differ in North American and European groups. For example, a recent EpSSG protocol (RMS 2005) defined low, standard, high, and very high risk groups for children with RMS, based on tumor histology, anatomic site and degree of surgical resection of the primary tumor, and presence or absence of detectable metastatic disease 177. By contrast, the most recent series of COG trials (ARST0331, ARST0431, and ARST0531) incorporated only three risk groups 1 (Table 5; Figure 6). The overlap between the EpSSG high risk and COG intermediate risk groups is particularly noteworthy because children with histologically-defined ARMS and regional lymph node involvement are classified as very high risk by EpSSG but intermediate risk by COG 1. Thus, developing informatics infrastructure to enable comparisons across these two cooperative groups represents a challenge and an opportunity to establish a global resource for collection, storage, and sharing of RMS clinical trial.
Table 5:
Risk stratification for patients with RMS
| COG risk group |
Stage | Group | Histology | COG study | Therapy |
|---|---|---|---|---|---|
| Low, subset 1 | 1 | I or II | ERMS | ARST0331 | VACx4, VAx4; 24 weeks |
| 1 | III (site of primary tumour: orbit) | ||||
| 2 | I or II | ||||
| Low, subset 2 | 1 | III (site of primary tumour: non-orbit) | ERMS | ARST0331 | VACx4, VAx12; 48 weeks |
| 3 | I or II | ||||
| Intermediate | 2 or 3 | III | ERMS | ARST0531 | VAC vs VAC/VI; 42 weeks |
| 1, 2, or 3 | I, II, or III | ARMS | |||
| High | 4 | IV | ERMS or ARMS | ARST08P1 | VI/VDC/IE/VAC with Cixutumumab or Temozolomide |
Abbreviations: VAC, vincristine, actinomycin, cyclophosphamide; ab, antibody; VA, vincristine, actinomycin; VI, vincristine, irinotecan; VDC, vincristine, doxorubicin, cyclophosphamide; IE, ifosfamide, etoposide.
Intermediate and high risk disease
Systemic therapy for RMS continues to be based on a foundation of intensive, alkylating-based, multi-agent chemotherapy administered at intervals over 6–9 months. In North America, combination of vincristine, actinomycin D, and cyclophosphamide (known as VAC) is the standard backbone therapy for RMS, whereas in Europe the standard is ifosfamide, vincristine, actinomycin D (known as IVA). It should be noted that a randomized comparison of either VAC or IVA as the initial therapy (followed by VAC for all patients) showed similar outcomes2.
The EpSSG RMS 2005 trial evaluated two randomized questions. First, the efficacy and safety of doxorubicin in patients with grossly-localized, but otherwise high risk RMS was studied after an initial pilot study demonstrated activity and safety of IVA plus doxorubicin (IVADo)178. However, the EpSSG RMS 2005 study failed to show that the addition of doxorubicin to the IVA backbone improved event-free survival 177. Second, this group studied the efficacy of 24 weeks of maintenance therapy with low-dose, continuous chemotherapy of oral cyclophosphamide and vinorelbine in children with localized RMS who achieved a complete radiographic response after 27 weeks of intensive therapy. Previous evaluation of the maintenance therapy in a pilot study had demonstrated activity in patients with recurrent RMS 179. In the EpSSG RMS 2005 trial, the addition of maintenance therapy improved overall survival (87.3% in maintenance arm vs 77.4% in standard treatment arm at three-years post randomization, p=0.011), with a marginal improvement in disease-free survival (78.4% vs 72.3%, p=0.061) 180.
In North America, the COG conducted trials to test the addition of a camptothecin drug to the VAC backbone in randomized studies of children with intermediate risk disease. The D9803 trial, conducted between 1999–2005, failed to show improved event free survival with the addition of topotecan 5. The subsequent ARST0531 trial compared standard VAC versus VAC alternating with vincristine-irinotecan, based on the particularly high activity of vincristine-irinotecan in a Phase II “window” study 181; and the 4-year event free survival and overall survival were similar in the two arms 182. Presently, the VAC backbone for RMS therapy remains a commonly accepted, North American standard for those with intermediate risk disease, whereas IVA is the European standard for those with localized disease, which includes patients similar to the COG intermediate risk stratum 177,183 (Table 5).
It should be emphasized that the outcome for children with metastatic disease is very poor, with overall survival rates at 3 years of ~25–30%, despite intensive systemic therapy, even therapy including high dose chemotherapy and autologous stem cell rescue 1,141,184. In a departure from the traditional approach, the COG recently conducted a Phase II study (ARST0431) testing whether an “interval compression” strategy, in which the interval between chemotherapy doses was decreased, utilizing doxorubicin, ifosfamide, etoposide, and irinotecan to the VAC backbone. ARST0431 showed an improved event free survival for a subset of children with metastatic RMS as compared to historical control individuals185.
Low risk disease
In contrast to children with metastatic disease, outcomes are excellent for children with low risk disease, generally considered to be those with localized, histologically confirmed ERMS (in favorable anatomic sites; localized and grossly resected ERMS; and ERMS localized to the orbit only (Table 4) 173. The most recent low risk study in the COG, ARST0331, investigated two strategies to reduce the burden of therapy without compromising survival. In one subset of patients with Stage 1 or 2–Group I or II ERMS, or Stage 1–Group III orbital ERMS, therapy was shortened to 24 weeks and total cyclophosphamide dose was decreased 186. This less intensive therapy resulted in excellent three year failure free survival (survival without relapse of disease) and overall survival (89% and 98%, respectively). The second subset of patients included those with Stage 1–Group III, non-orbital or Stage 3–Group I or II ERMS; in these patients total cyclophosphamide dose was decreased but VA chemotherapy was kept at a standard duration of 48 weeks. Notably, radiation therapy was also omitted for female patients with vaginal tumors achieving a complete response with or without surgical resection 187. Although the three-year overall survival was still very good (92%), the failure free survival was 70% overall and 57% for girls with genital tract tumors. COG investigators concluded that these failure free survival rates are sub-optimal, if the primary goal is to prevent disease recurrence and avoid the even more intensive therapy likely needed to achieve ultimate cure.
It is worth noting that the ‘philosophy’ in the European cooperative groups has been primarily on reducing morbidities associated with local control while retaining excellent overall survival. As such, a higher incidence of local disease recurrence has often been tolerated, with the understanding that a more intensive therapy may need to be employed at recurrence, but that the majority of individuals would not be exposed to that therapy 6. Studying the relative benefits and costs of the North American and European approaches would be valuable, especially for those in which chance of survival is high, therefore, concern for acute and late toxicities and cost effectiveness become more important.
Special management considerations
Local disease control.
Local control of RMS depends on surgical resection and/or use of ionizing radiation. RMS represents a cancer that is initially sensitive to cytotoxic chemotherapy and radiation, therefore surgical approaches are generally limited to those that are not form- or function-compromising 188,189. Nevertheless, the improved survival seen in patients with Group I and II versus Group III disease (Figure 6b) supports the importance of primary tumor resection when possible 3,175,190. Historically, ionizing radiation was classified a crucial adjunct to surgical resection to optimize local disease control. However, in current practice, the dose is adjusted based on degree of previous surgical resection to reduce radiation-related sequelae, such as skeletal muscle and/or soft tissue changes, joint stiffness, axial and appendicular skeletal growth problems, and secondary malignancy191-193. In European trials, radiation therapy is omitted in certain circumstances in an attempt to spare the majority of patients from adverse treatment effects as long as effective salvage therapy is available.
RMS in very young children.
Children aged <3 years, especially infants up to 12 months old, pose a management challenge because their outcome is often worse than in older children194,195. Reports suggest that the worse outcome might arise in part from hesitancy to offer the same local disease control or chemotherapy dose intensity that is typically applied to older children owing to toxicity concerns. Also conceivable is the fact that the pathophysiology of RMS may differ according to age. Indeed, a recent report showed variant gene fusions involving VGLL2 fusion to either CITED2 or NCOA2 in infants with sclerosing/spindle cell RMS 196. As next generation sequencing analyses move forward, correlation of molecular genotype with clinical prognostic features, like anatomic site, tumor stage and clinical group, and age, may provide additional evidence to support this possibility.
Management of recurrent RMS
Recurrent RMS has a very poor prognosis, and a standard of care has not been widely accepted. Overall survival following RMS relapse depends on several factors including the stage of disease at original diagnosis, the site of relapse, and tumor histology. In general, patients undergoing more intensive therapy at original diagnosis had worse outcomes following relapse than patients receiving less intensive therapy at the time of original diagnosis. For example, individuals with relapse after treatment for Stage 1–Group I ERMS disease displayed a 5-year event-free survival after relapse of 52% compared to ~20% for those with Stage 3–Group III disease and ~12% for those with Stage 4 disease at original diagnosis197. Also, children originally diagnosed with Stage 1–Group I disease who had a local recurrence also had a better prognosis than those with regional or distant recurrence197. Unfortunately, post-relapse treatment data were not included in this analysis.
Given the bleak outlook, cooperative groups in North America have been studying novel therapeutic approaches in children with relapsed RMS (and other sarcomas). Phase II trials of promising agents, such as the anti-IGF1 receptor antibody R1507 198 and the multi-RTK inhibitor sorafenib 199, were recently conducted within the COG, but unfortunately neither study showed evidence for significant, single-agent activity. The addition of the mTOR inhibitor temsirolimus to the anti-IGF1 receptor antibody cixutumumab also failed to significantly improve outcomes despite promising preclinical data 200. The most recent COG trial for relapsed RMS (ARST0921) employed a backbone of vinorelbine and cyclophosphamide, taking a cue from a previous European study showing these agents had some activity as low-dose, maintenance therapies179. To that backbone, ARST0921 randomized the addition of either the vascular endothelial growth factor inhibitor bevacizumab or temsirolimus in a Phase II pilot study to select one of the two agents for further study 168. This pilot study showed relatively more benefit from temsirolimus201 and informed the COG Soft Tissue Sarcoma Committee’s decision to study it in a randomized, Phase III study of children with intermediate risk RMS (ARST1431). Because overall survival was still poor for those children with relapsed RMS, despite the use of temsirolimus, investigators continue to study new therapeutic approaches in children with relapsed RMS.
Quality of life
For almost 40 years, the focus of North American and European clinical trials groups has been on improving survival. Some consideration has been given to Quality of Life (QOL) issues, such as the general philosophy to avoid form-compromising or function-compromising surgical interventions, however, few QOL data have been collected on those trials. As the majority of children with RMS will be long-term, disease-free survivors, greater consideration should be given to QOL data during and after RMS therapy.
Children with cancer are known to experience high levels of suffering and ongoing symptom burden related to their cancer and its treatment 202. Toxicity reporting in pediatric cooperative group studies relies on symptom descriptions documented by health-care providers, and then extracted from medical records by researchers. As such, these data may not reflect the experiences of patients. Prospective collection of patient-reported outcomes (PROs) could be used to explore symptom experience by children, from diagnosis and throughout initial therapy. Owing to the wide range of patient ages, and the widely-ranging sites of disease collection of PROs is a challenge with current clinical trial models.
Despite the historical challenges, some studies suggest progress in defining symptom and toxicity data and in examining age-based comparisons. For example, on the COG ARST0431 study of children with high-risk RMS, adolescents were less likely to complete therapy (63% of individuals aged greater than 13 years vs. 76% of children aged 13 or less) and more likely to have unplanned dose modifications outside of protocol guidelines (23% vs. 2.7%) compared to younger children203. Furthermore, nausea and vomiting (17% vs. 4%) and pain (20% vs. 6%) were more likely to be reported in adolescents compared to younger patients203. These findings should be interpreted with caution, as symptom reporting may be more effective in adolescents than younger children. It remains unclear whether PRO collection will overcome that obstacle. In settings where clinical balance exists, differences in PROs may help guide treatment decisions for an individual patient.
QOL assessments in survivors of RMS therapy are important, yet knowledge gaps still exist. Genitourinary and sexual and/or reproductive health are two areas where issues may arise in this population, yet those QOL data are mostly from small series studies. For example, one study of the effects of proton therapy in bladder and/or prostate disease was described in only five children cured of their disease with problems ranging from none to enuresis 204. In another small study of four patients >14 years of age and previously treated with multimodality therapy for prostate or bladder RMS, sexual function was assessed using a modified International Erectile Function Index and found that two of the four patients had moderate or good quality scores each, respectively, after pelvic radiation therapy and cystectomy 205. In a study of 13 patients (median age 20 years) who had survived pelvic RMS, erectile dysfunction (assessed by Self-Estimation Index of Erectile Function-No Sexual Intercourse (SIEF-NS) and the Erection Hardness Scale) was present in ten men, three of whom had radiation therapy, whereas three men without radiation therapy had no evidence of erectile dysfunction 206. In a separate study, 13 of 18 survivors who previously underwent partial cystectomy and/or partial prostatectomy, followed by low dose-rate interstitial brachytherapy, were found to have normal QOL, assessed by a questionnaire derived from the International Workshop on bladder and/or prostate RMS 207. In this study, although all pubertal patients reported having normal erections, the validated SIEF-NS tool was not used. In the largest review to date, medical records of 164 individuals who had survived bladder and/or prostate RMS were retrospectively reviewed to identify 44 who had undergone partial urinary bladder cystectomy and had medical record data regarding urinary continence. Of these 44 patients, 12 were described to have had urinary incontinence, frequency, or urgency208. How best to target ionizing radiation to large fields, such as the pelvis for those with bladder–prostate RMS, continues to be highly debated 209. If survival is similar with and without radiation therapy 138,210, prospective collection of data on bladder and sexual function becomes particularly important in order to guide treatment decisions in those likely to be cured of their disease.
Outlook
Basic research
Over the last thirty years, our understanding of the pathophysiology of RMS has become increasingly sophisticated, and these insights have enabled more robust clinical diagnostics and prognostic assessments, which have contributed to the development of more precise therapeutic approaches. These intensive or experimental approaches are aimed at improving the outcome of patients with a poor prognosis and also attempt to reduce harsh acute and lasting treatment-associated effects in individuals likely to be cured by standard approaches.
The next step toward precision medicine entails the development of robust, objective and accessible biomarkers that are highly predictive of response to targeted therapy. One major challenge for RMS is highlighted above: the paucity of highly-recurrent and targetable protein coding genes, especially in fusion-driven RMS 28-30. Current efforts for targeted re-sequencing of primary RMS biopsy samples will more precisely define the frequency of previously-identified somatic variants; correlation of these variants with clinical features, such as age, anatomic site, and outcome, should lead to better understanding of tumor biology and enable better risk stratification. However, it seems likely that integrative computational analyses, especially those considering gene expression changes driven by epigenetic reprogramming, will be required to find targetable oncogenic drivers that were not unmasked by nucleic acid sequencing.
In parallel, as the field progresses more clearly into a post-genomics era (Box 1), functional approaches and high-throughput screening also represent important laboratory-based paths toward better therapy. CRISPR–Cas9-based gene editing provides an opportunity for targeted (for example, kinome-wide) or completely unbiased searches for vulnerabilities in RMS 211, especially if utilized in well-characterized patient-derived xenograft models that are increasingly available 212. Organism-based models in zebrafish 213,214 and drosophila 215 are particularly intriguing ways to conduct high throughput chemical or genetic screens for targetable cancer drivers, especially for fusion oncogene-driven disease. Those non-mammalian systems have potential pitfalls, but findings there could be confirmed in the elegant mammalian models already employed (Box 1)40,216-218.
Another incompletely evaluated approach toward “personalized” RMS therapy includes immunotherapy. Immunotherapy in which the patient’s dendritic cells are purified, exposed in vitro to neoantigens from the patient’s tumor, and returned to the patient has shown some promise for high risk sarcoma 139,219. However, because immune checkpoint inhibitors such as ipilimumab 220 have demonstrated little single-agent activity in RMS, research should focus on identifying predictive biomarkers. In addition, researchers should investigate combination therapies, including coupling checkpoint blockade with ionizing radiation to increase neoantigen presentation and have a potential abscopal effect on systemic disease 221.
Clinical and translational research
Clinical and translational research efforts should continue to enable the development of personalized medical approaches. One short term goal should be to prospectively validate improved prognostic signatures, such as prospectively validating the 5-gene metagene signature, MG5, which has already been applied to several independent, retrospective cohorts 158,176. Moreover, efforts should be made to develop an MG5 score that could be used in treatment assignment for individual patients with RMS to further aid in risk stratification. In addition, translational studies should focus on whether prognostic biomarker signatures can be enhanced by additional molecular characteristics, such as presence or absence of RAS gene mutations. These mutations are relatively common and potentially a marker for more aggressive disease course in those with FN RMS 29.
Another direction for future research should be into molecularly targeted therapies, which may further improve outcomes, especially in children with metastatic or recurrent disease. The outcomes for these children remain bleak, and numerous attempts to intensify therapy by the addition of new cytotoxic agents or by interval compression have failed. One on-going COG trial (ARST1431) for children with intermediate risk disease is a randomized, Phase III study, adding the mTOR inhibitor temsirolimus to the VAC/VI therapy backbone used in North America. This trial is based on a previous study that found that the addition of temsirolimus to vinorelbine and cyclophosphamide improved survival in children with relapsed RMS compared to the addition of bevacizumab to vinorelbine and cyclophosphamide201. As new, molecularly-targeted therapies are identified, they could be studied in the context of a ‘basket’, such as the Pediatric MATCH trial, supported in North America by the COG and the National Cancer Institute 222. This ‘basket’ trial provides a mechanism to test a number of agents – such as larotrectinib, selumetinib, and pablociblib, targeting TRK, MEK, and CDK4/6, respectively – in parallel and in a number of different types of tumors, including RMS. This type of trial may identify an agent active against RMS, which could then be pursued in a more focused study.
Finally, effort should be devoted to building improved informatics systems, to better capture, assimilate, and curate the ever-increasing quantity of clinical data arising from cooperative group studies. Moreover, these clinical data can be paired with banked biopsy samples, pathology descriptions and/or actual digital photomicrographic images of pathology specimens, radiographic images, and molecular genetic, epigenetic and proteomic data could greatly facilitate efforts to improve outcomes for children with RMS. Building such a data commons for childhood cancer – or even just for RMS – could enable clinical and translational research discovery in many ways, especially by taking advantage of ever increasing artificial intelligence capabilities 223. Extending this type of effort across North America and Europe will greatly enable trans-Atlantic (or even global) analyses of what will likely become progressively smaller, clinically and molecularly-defined RMS subgroups. In addition, expanding the scope of such work to include QOL and PRO analyses may be progressively more important as the likelihood of patient survival continues to improve.
Supplementary Material
Reference List
- 1.Hawkins DS, Spunt SL & Skapek SX Children's Oncology Group's 2013 blueprint for research: Soft tissue sarcomas. Pediatric blood & cancer 60, 1001–1008 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crist WM, et al. Intergroup rhabdomyosarcoma study-IV: results for patients with nonmetastatic disease. Journal of Clinical Oncology 19, 3091–3102 (2001). [DOI] [PubMed] [Google Scholar]
- 3.Crist W, et al. The Third Intergroup Rhabdomyosarcoma Study. J Clin Oncol 13, 610–630 (1995). [DOI] [PubMed] [Google Scholar]
- 4.Raney RB, et al. The Intergroup Rhabdomyosarcoma Study Group (IRSG): Major Lessons From the IRS-I Through IRS-IV Studies as Background for the Current IRS-V Treatment Protocols. Sarcoma. 5, 9–15 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arndt CA, et al. Vincristine, actinomycin, and cyclophosphamide compared with vincristine, actinomycin, and cyclophosphamide alternating with vincristine, topotecan, and cyclophosphamide for intermediate-risk rhabdomyosarcoma: children's oncology group study D9803. J Clin Oncol 27, 5182–5188 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stevens MC, et al. Treatment of nonmetastatic rhabdomyosarcoma in childhood and adolescence: third study of the International Society of Paediatric Oncology--SIOP Malignant Mesenchymal Tumor 89. J Clin Oncol 23, 2618–2628 (2005). [DOI] [PubMed] [Google Scholar]
- 7.Oberlin O, et al. Randomized comparison of intensified six-drug versus standard three-drug chemotherapy for high-risk nonmetastatic rhabdomyosarcoma and other chemotherapy-sensitive childhood soft tissue sarcomas: long-term results from the International Society of Pediatric Oncology MMT95 study. J Clin Oncol 30, 2457–2465 (2012). [DOI] [PubMed] [Google Scholar]
- 8.Enterline HT & Horn RC Jr. Alveolar rhabdomyosarcoma; a distinctive tumor type. Am J Clin Pathol 29, 356–366 (1958). [DOI] [PubMed] [Google Scholar]
- 9.Patton RB & Horn RC Jr. Rhabdomyosarcoma: clinical and pathological features and comparison with human fetal and embryonal skeletal muscle. Surgery 52, 572–584 (1962). [PubMed] [Google Scholar]
- 10.Turc-Carel C, et al. Consistent chromosomal translocation in alveolar rhabdomyosarcoma. Cancer Genet Cytogenet 19, 361–362 (1986). [DOI] [PubMed] [Google Scholar]
- 11.Douglass EC, et al. Variant translocations of chromosome 13 in alveolar rhabdomyosarcoma. Genes Chromosomes Cancer 3, 480–482 (1991). [DOI] [PubMed] [Google Scholar]
- 12.Douglass EC, et al. A specific chromosomal abnormality in rhabdomyosarcoma. Cytogenetics and Cell Genetics 45, 148–155 (1987). [DOI] [PubMed] [Google Scholar]
- 13.Rudzinski ER, et al. The World Health Organization Classification of Skeletal Muscle Tumors in Pediatric Rhabdomyosarcoma: A Report From the Children's Oncology Group. Arch Pathol Lab Med 139, 1281–1287 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barr FG, et al. Rearrangement of the PAX3 paired box gene in the paediatric solid tumour alveolar rhabdomyosarcoma. Nat.Genet 3, 113–117 (1993). [DOI] [PubMed] [Google Scholar]
- 15.Davis RJ, D'Cruz CM, Lovell MA, Biegel JA & Barr FG Fusion of PAX7 to FKHR by the variant t(1;13)(p36;q14) translocation in alveolar rhabdomyosarcoma. Cancer Res. 54, 2869–2872 (1994). [PubMed] [Google Scholar]
- 16.Parham DM & Barr FG Classification of rhabdomyosarcoma and its molecular basis. Adv Anat Pathol 20, 387–397 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ries LAG, Smith MA, Gurney LG, Linet M, Tamran T, Young JL, Bunin GR Cancer incidence and survival among children and adolescents: United States SEER Program 1975-1999. National Cancer Institute, SEER Program NIH Pub. No. 99-4649(1999). [Google Scholar]
- 18.Perez EA, et al. Rhabdomyosarcoma in children: a SEER population based study. J Surg Res 170, e243–251 (2011). [DOI] [PubMed] [Google Scholar]
- 19.Lychou SE, Gustafsson GG & Ljungman GE Higher rates of metastatic disease may explain the declining trend in Swedish paediatric rhabdomyosarcoma survival rates. Acta Paediatr 105, 74–81 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stiller CA & Parkin DM International variations in the incidence of childhood soft-tissue sarcomas. Paediatr Perinat Epidemiol 8, 107–119 (1994). [DOI] [PubMed] [Google Scholar]
- 21.Ognjanovic S, Linabery AM, Charbonneau B & Ross JA Trends in childhood rhabdomyosarcoma incidence and survival in the United States, 1975-2005. Cancer 115, 4218–4226 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kelly KM, Womer RB, Sorensen PH, Xiong QB & Barr FG Common and variant gene fusions predict distinct clinical phenotypes in rhabdomyosarcoma. J Clin Oncol 15, 1831–1836 (1997). [DOI] [PubMed] [Google Scholar]
- 23.Furlong MA, Mentzel T & Fanburg-Smith JC Pleomorphic rhabdomyosarcoma in adults: a clinicopathologic study of 38 cases with emphasis on morphologic variants and recent skeletal muscle-specific markers. Mod Pathol 14, 595–603 (2001). [DOI] [PubMed] [Google Scholar]
- 24.Chow EJ, et al. Childhood cancer in relation to parental race and ethnicity: a 5-state pooled analysis. Cancer 116, 3045–3053 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grufferman S, Ruymann F, Ognjanovic S, Erhardt EB & Maurer HM Prenatal X-ray exposure and rhabdomyosarcoma in children: a report from the children's oncology group. Cancer Epidemiol Biomarkers Prev 18, 1271–1276 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Savage SA, et al. Genome-wide association study identifies two susceptibility loci for osteosarcoma. Nat Genet 45, 799–803 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Postel-Vinay S, et al. Common variants near TARDBP and EGR2 are associated with susceptibility to Ewing sarcoma. Nat Genet 44, 323–327 (2012). [DOI] [PubMed] [Google Scholar]
- 28.Shern JF, et al. Comprehensive Genomic Analysis of Rhabdomyosarcoma Reveals a Landscape of Alterations Affecting a Common Genetic Axis in Fusion-Positive and Fusion-Negative Tumors. Cancer Discovery (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen X, et al. Targeting oxidative stress in embryonal rhabdomyosarcoma. Cancer Cell 24, 710–724 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Seki M, et al. Integrated genetic and epigenetic analysis defines novel molecular subgroups in rhabdomyosarcoma. Nature communications 6, 7557 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Diller L, Sexsmith E, Gottlieb A, Li FP & Malkin D Germline p53 mutations are frequently detected in young children with rhabdomyosarcoma. J.Clin.Invest 95, 1606–1611 (1995). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hartley AL, Birch JM, Marsden HB, Harris M & Blair V Neurofibromatosis in children with soft tissue sarcoma. Pediatr Hematol Oncol 5, 7–16 (1988). [DOI] [PubMed] [Google Scholar]
- 33.Yang P, et al. Association of childhood rhabdomyosarcoma with neurofibromatosis type I and birth defects. Genet Epidemiol 12, 467–474 (1995). [DOI] [PubMed] [Google Scholar]
- 34.Kratz CP, Rapisuwon S, Reed H, Hasle H & Rosenberg PS Cancer in Noonan, Costello, cardiofaciocutaneous and LEOPARD syndromes. American journal of medical genetics. Part C, Seminars in medical genetics 157C, 83–89 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Estep AL, Tidyman WE, Teitell MA, Cotter PD & Rauen KA HRAS mutations in Costello syndrome: detection of constitutional activating mutations in codon 12 and 13 and loss of wild-type allele in malignancy. Am J Med Genet A 140, 8–16 (2006). [DOI] [PubMed] [Google Scholar]
- 36.Shuman C, Beckwith JB & Weksberg R Beckwith-Wiedemann Syndrome in GeneReviews((R)) (eds. Adam MP, et al.) (Seattle (WA: ), 1993). [Google Scholar]
- 37.Doros L, et al. DICER1 mutations in embryonal rhabdomyosarcomas from children with and without familial PPB-tumor predisposition syndrome. Pediatr Blood Cancer 59, 558–560 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Plon SE & Malkin D Childhood Cancer and Heredity in Principles and Practice of Pediatric Oncology (eds. Pizzo PA & Poplack DG) 1600 (Lippincott Williams & Wilkins, Philadelphia, PA, 2010). [Google Scholar]
- 39.Ognjanovic S, Olivier M, Bergemann TL & Hainaut P Sarcomas in TP53 germline mutation carriers: a review of the IARC TP53 database. Cancer 118, 1387–1396 (2012). [DOI] [PubMed] [Google Scholar]
- 40.Keller C, et al. Alveolar rhabdomyosarcomas in conditional Pax3:Fkhr mice: cooperativity of Ink4a/ARF and Trp53 loss of function. Genes and Development 18, 2614–2626 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grufferman S, Delzell E & Delong ER An approach to conducting epidemiologic research within cooperative clinical trials groups. J Clin Oncol 2, 670–675 (1984). [DOI] [PubMed] [Google Scholar]
- 42.Grufferman S, Schwartz AG, Ruymann FB & Maurer HM Parents' use of cocaine and marijuana and increased risk of rhabdomyosarcoma in their children. Cancer Causes Control 4, 217–224 (1993). [DOI] [PubMed] [Google Scholar]
- 43.Lupo PJ, et al. Maternal and birth characteristics and childhood rhabdomyosarcoma: a report from the Children's Oncology Group. Cancer Causes Control 25, 905–913 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lupo PJ, et al. Allergies, atopy, immune-related factors and childhood rhabdomyosarcoma: a report from the Children's Oncology Group. Int J Cancer 134, 431–436 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lupo PJ, et al. Family history of cancer and childhood rhabdomyosarcoma: a report from the Children's Oncology Group and the Utah Population Database. Cancer Med 4, 781–790 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ottaviani G & Jaffe N The epidemiology of osteosarcoma. Cancer Treat Res 152, 3–13 (2009). [DOI] [PubMed] [Google Scholar]
- 47.Eyre R, Feltbower RG, Mubwandarikwa E, Eden TO & McNally RJ Epidemiology of bone tumours in children and young adults. Pediatr Blood Cancer 53, 941–952 (2009). [DOI] [PubMed] [Google Scholar]
- 48.Grufferman S, et al. Environmental factors in the etiology of rhabdomyosarcoma in childhood. J Natl Cancer Inst 68, 107–113 (1982). [PubMed] [Google Scholar]
- 49.Grimson RC, Aldrich TE & Drane JW Clustering in sparse data and an analysis of rhabdomyosarcoma incidence. Stat Med 11, 761–768 (1992). [DOI] [PubMed] [Google Scholar]
- 50.Linardic CM, et al. The PAX3-FKHR fusion gene of rhabdomyosarcoma cooperates with loss of p16INK4A to promote bypass of cellular senescence. Cancer Res. 67, 6691–6699 (2007). [DOI] [PubMed] [Google Scholar]
- 51.Drummond CJ, et al. Hedgehog Pathway Drives Fusion-Negative Rhabdomyosarcoma Initiated From Non-myogenic Endothelial Progenitors. Cancer Cell 33, 108–124 e105 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Marshall AD & Grosveld GC Alveolar rhabdomyosarcoma - The molecular drivers of PAX3/7-FOXO1-induced tumorigenesis. Skelet Muscle 2, 25 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Barr FG Gene fusions involving PAX and FOX family members in alveolar rhabdomyosarcoma. Oncogene 20, 5736–5746. (2001). [DOI] [PubMed] [Google Scholar]
- 54.Galili N, et al. Fusion of a fork head domain gene to PAX3 in the solid tumour alveolar rhabdomyosarcoma. Nat.Genet. 5, 230–235 (1993). [DOI] [PubMed] [Google Scholar]
- 55.Bennicelli JL, Advani S, Schafer BW & Barr FG PAX3 and PAX7 exhibit conserved cis -acting transcription repression domains and utilize a common gain of function mechanism in alveolar rhabdomyosarcoma. Oncogene 18, 4348–4356 (1999). [DOI] [PubMed] [Google Scholar]
- 56.Bennicelli JL, Edwards RH & Barr FG Mechanism for transcriptional gain of function resulting from chromosomal translocation in alveolar rhabdomyosarcoma. Proc.Natl.Acad.Sci.U.S.A 93, 5455–5459 (1996). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Davis RJ & Barr FG Fusion genes resulting from alternative chromosomal translocations are overexpressed by gene-specific mechanisms in alveolar rhabdomyosarcoma. Proc Natl Acad Sci U S A 94, 8047–8051. (1997). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.del Peso L, Gonzalez VM, Hernandez R, Barr FG & Nunez G Regulation of the forkhead transcription factor FKHR, but not the PAX3- FKHR fusion protein, by the serine/threonine kinase Akt. Oncogene 18, 7328–7333 (1999). [DOI] [PubMed] [Google Scholar]
- 59.Thalhammer V, et al. PLK1 phosphorylates PAX3-FOXO1, the inhibition of which triggers regression of alveolar Rhabdomyosarcoma. Cancer Res 75, 98–110 (2015). [DOI] [PubMed] [Google Scholar]
- 60.Bharathy N, et al. P/CAF mediates PAX3-FOXO1-dependent oncogenesis in alveolar rhabdomyosarcoma. J Pathol 240, 269–281 (2016). [DOI] [PubMed] [Google Scholar]
- 61.Amstutz R, et al. Phosphorylation regulates transcriptional activity of PAX3/FKHR and reveals novel therapeutic possibilities. Cancer Res 68, 3767–3776 (2008). [DOI] [PubMed] [Google Scholar]
- 62.Cao L, et al. Genome-wide identification of PAX3-FKHR binding sites in rhabdomyosarcoma reveals candidate target genes important for development and cancer. Cancer Research 70, 6497–6508 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gryder BE, et al. PAX3-FOXO1 Establishes Myogenic Super Enhancers and Confers BET Bromodomain Vulnerability. Cancer Discov 7, 884–899 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bohm M, et al. Helicase CHD4 is an epigenetic coregulator of PAX3-FOXO1 in alveolar rhabdomyosarcoma. J Clin Invest 126, 4237–4249 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lam PYP, Sublett JE, Hollenbach AD & Roussel MF The oncogenic potential of the pax3-FKHR fusion protein requires the pax3 homeodomain recognition helix but not the pax3 paired-box DNA binding domain. Molecular & Cellular Biology 19, 594–601 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Xia SJ, Holder DD, Pawel BR, Zhang C & Barr FG High expression of the PAX3-FKHR oncoprotein is required to promote tumorigenesis of human myoblasts. Am J Pathol 175, 2600–2608 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kikuchi K, et al. Effects of PAX3-FKHR on malignant phenotypes in alveolar rhabdomyosarcoma. Biochemical and Biophysical Research Communications 365, 568–574 (2008). [DOI] [PubMed] [Google Scholar]
- 68.Ebauer M, Wachtel M, Niggli FK & Schafer BW Comparative expression profiling identifies an in vivo target gene signature with TFAP2B as a mediator of the survival function of PAX3/FKHR. Oncogene 26, 7267–7281 (2007). [DOI] [PubMed] [Google Scholar]
- 69.Sorensen PH, et al. PAX3-FKHR and PAX7-FKHR gene fusions are prognostic indicators in alveolar rhabdomyosarcoma: a report from the children's oncology group. J Clin Oncol 20, 2672–2679 (2002). [DOI] [PubMed] [Google Scholar]
- 70.Barr FG, et al. Genetic Heterogeneity in the Alveolar Rhabdomyosarcoma Subset without Typical Gene Fusions. Cancer Res 62, 4704–4710. (2002). [PubMed] [Google Scholar]
- 71.Wachtel M, et al. Gene expression signatures identify rhabdomyosarcoma subtypes and detect a novel t(2;2)(q35;p23) translocation fusing PAX3 to NCOA1. Cancer Research 64, 5539–5545 (2004). [DOI] [PubMed] [Google Scholar]
- 72.Williamson D, et al. Fusion gene-negative alveolar rhabdomyosarcoma is clinically and molecularly indistinguishable from embryonal rhabdomyosarcoma. J Clin Oncol 28, 2151–2158 (2010). [DOI] [PubMed] [Google Scholar]
- 73.Weber-Hall S, et al. Gains, losses, and amplification of genomic material in rhabdomyosarcoma analyzed by comparative genomic hybridization. Cancer Res. 56, 3220–3224 (1996). [PubMed] [Google Scholar]
- 74.Shukla N, et al. Oncogene mutation profiling of pediatric solid tumors reveals significant subsets of embryonal rhabdomyosarcoma and neuroblastoma with mutated genes in growth signaling pathways. Clin Cancer Res 18, 748–757 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Davicioni E, et al. Molecular classification of rhabdomyosarcoma - genotypic and phenotypic determinants of diagnosis. American Journal of Pathology 174, 550–564 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Stewart E, et al. Identification of Therapeutic Targets in Rhabdomyosarcoma through Integrated Genomic, Epigenomic, and Proteomic Analyses. Cancer Cell 34, 411–426 e419 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Martinelli S, et al. RAS signaling dysregulation in human embryonal Rhabdomyosarcoma. Genes Chromosomes.Cancer 48, 975–982 (2009). [DOI] [PubMed] [Google Scholar]
- 78.Davicioni E, et al. Identification of a PAX-FKHR gene expression signature that defines molecular classes and determines the prognosis of alveolar rhabdomyosarcomas. Cancer Research 66, 6936–6946 (2006). [DOI] [PubMed] [Google Scholar]
- 79.Tremblay AM, et al. The Hippo Transducer YAP1 Transforms Activated Satellite Cells and Is a Potent Effector of Embryonal Rhabdomyosarcoma Formation. Cancer Cell 26, 273–287 (2014). [DOI] [PubMed] [Google Scholar]
- 80.Romualdi C, et al. Defining the gene expression signature of rhabdomyosarcoma by meta-analysis. BMC Genomics 7, 287 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Renshaw J, et al. Dual blockade of the PI3K/AKT/mTOR (AZD8055) and RAS/MEK/ERK (AZD6244) pathways synergistically inhibits rhabdomyosarcoma cell growth in vitro and in vivo. Clin Cancer Res (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Taylor JG, et al. Identification of FGFR4-activating mutations in human rhabdomyosarcomas that promote metastasis in xenotransplanted models. J.Clin.Invest 119, 3395–3407 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Li SQ, et al. Targeting wild-type and mutationally activated FGFR4 in rhabdomyosarcoma with the inhibitor ponatinib (AP24534). PLoS One 8, e76551 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Crose LE, et al. FGFR4 blockade exerts distinct antitumorigenic effects in human embryonal versus alveolar rhabdomyosarcoma. Clin Cancer Res 18, 3780–3790 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wachtel M, et al. FGFR4 signaling couples to Bim and not Bmf to discriminate subsets of alveolar rhabdomyosarcoma cells. Int J Cancer 135, 1543–1552 (2014). [DOI] [PubMed] [Google Scholar]
- 86.Bridge JA, et al. Genomic gains and losses are similar in genetic and histologic subsets of rhabdomyosarcoma, whereas amplification predominates in embryonal with anaplasia and alveolar subtypes. Genes Chromosomes Cancer 33, 310–321. (2002). [DOI] [PubMed] [Google Scholar]
- 87.Martins AS, Olmos D, Missiaglia E & Shipley J Targeting the insulin-like growth factor pathway in rhabdomyosarcomas: rationale and future perspectives. Sarcoma 2011, 209736 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Petricoin EF 3rd, et al. Phosphoprotein pathway mapping: Akt/mammalian target of rapamycin activation is negatively associated with childhood rhabdomyosarcoma survival. Cancer Res 67, 3431–3440 (2007). [DOI] [PubMed] [Google Scholar]
- 89.Wan X, Yeung C, Heske C, Mendoza A & Helman LJ IGF-1R Inhibition Activates a YES/SFK Bypass Resistance Pathway: Rational Basis for Co-Targeting IGF-1R and Yes/SFK Kinase in Rhabdomyosarcoma. Neoplasia 17, 358–366 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ganti R, et al. Expression and genomic status of EGFR and ErbB-2 in alveolar and embryonal rhabdomyosarcoma. Modern Pathology 19, 1213–1220 (2006). [DOI] [PubMed] [Google Scholar]
- 91.Mark HF, Brown S, Sun CL, Samy M & Afify A Fluorescent in situ hybridization detection of HER-2/neu gene amplification in rhabdomyosarcoma. Pathobiology 66, 59–63 (1998). [DOI] [PubMed] [Google Scholar]
- 92.Abraham J, et al. Evasion mechanisms to Igf1r inhibition in rhabdomyosarcoma. Mol Cancer Ther 10, 697–707 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Blake J & Ziman MR Aberrant PAX3 and PAX7 expression. A link to the metastatic potential of embryonal rhabdomyosarcoma and cutaneous malignant melanoma? Histol Histopathol 18, 529–539 (2003). [DOI] [PubMed] [Google Scholar]
- 94.Chiappalupi S, Riuzzi F, Fulle S, Donato R & Sorci G Defective RAGE activity in embryonal rhabdomyosarcoma cells results in high PAX7 levels that sustain migration and invasiveness. Carcinogenesis 35, 2382–2392 (2014). [DOI] [PubMed] [Google Scholar]
- 95.Megiorni F, et al. Pharmacological targeting of the ephrin receptor kinase signalling by GLPG1790 in vitro and in vivo reverts oncophenotype, induces myogenic differentiation and radiosensitizes embryonal rhabdomyosarcoma cells. J Hematol Oncol 10, 161 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Rees H, et al. The MET receptor tyrosine kinase contributes to invasive tumour growth in rhabdomyosarcomas. Growth Factors 24, 197–208 (2006). [DOI] [PubMed] [Google Scholar]
- 97.Taulli R, et al. Validation of met as a therapeutic target in alveolar and embryonal rhabdomyosarcoma. Cancer Res 66, 4742–4749 (2006). [DOI] [PubMed] [Google Scholar]
- 98.Otabe O, et al. MET/ERK2 pathway regulates the motility of human alveolar rhabdomyosarcoma cells. Oncol Rep 37, 98–104 (2017). [DOI] [PubMed] [Google Scholar]
- 99.Skrzypek K, et al. Constitutive activation of MET signaling impairs myogenic differentiation of rhabdomyosarcoma and promotes its development and progression. Oncotarget 6, 31378–31398 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Miekus K, et al. The decreased metastatic potential of rhabdomyosarcoma cells obtained through MET receptor downregulation and the induction of differentiation. Cell Death Dis 4, e459 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Taniguchi E, et al. PDGFR-A is a therapeutic target in alveolar rhabdomyosarcoma. Oncogene 27, 6550–6560 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ehnman M, et al. Distinct Effects of Ligand-Induced PDGFRalpha and PDGFRbeta Signaling in the Human Rhabdomyosarcoma Tumor Cell and Stroma Cell Compartments. Cancer Res 73, 2139–2149 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Shern JF, et al. Targeted resequencing of pediatric rhabdomyosarcoma: report from the Children's Oncology Group, The Children's Cancer and Leukemia Group, The Institute of Cancer Research UK, and the National Cancer Institute. J Clin Oncol 36, (suppl; abstract 10515) (2018). [Google Scholar]
- 104.Naini S, et al. Defining the cooperative genetic changes that temporally drive alveolar rhabdomyosarcoma. Cancer Res 68, 9583–9588 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hayes MN & Langenau DM Discovering novel oncogenic pathways and new therapies using zebrafish models of sarcoma. Methods Cell Biol 138, 525–561 (2017). [DOI] [PubMed] [Google Scholar]
- 106.Annavarapu SR, et al. Characterization of Wnt/beta-catenin signaling in rhabdomyosarcoma. Lab Invest 93, 1090–1099 (2013). [DOI] [PubMed] [Google Scholar]
- 107.Chen EY, et al. Glycogen synthase kinase 3 inhibitors induce the canonical WNT/beta-catenin pathway to suppress growth and self-renewal in embryonal rhabdomyosarcoma. Proc Natl Acad Sci U S A 111, 5349–5354 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Satheesha S, et al. Targeting hedgehog signaling reduces self-renewal in embryonal rhabdomyosarcoma. Oncogene (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zibat A, et al. Activation of the hedgehog pathway confers a poor prognosis in embryonal and fusion gene-negative alveolar rhabdomyosarcoma. Oncogene 29, 6323–6330 (2010). [DOI] [PubMed] [Google Scholar]
- 110.Almazan-Moga A, et al. Ligand-dependent Hedgehog pathway activation in Rhabdomyosarcoma: the oncogenic role of the ligands. Br J Cancer 117, 1314–1325 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Conti B, Slemmons KK, Rota R & Linardic CM Recent Insights into Notch Signaling in Embryonal Rhabdomyosarcoma. Curr Drug Targets (2015). [DOI] [PubMed] [Google Scholar]
- 112.Mohamed AD, Tremblay AM, Murray GI & Wackerhage H The Hippo signal transduction pathway in soft tissue sarcomas. Biochim Biophys Acta 1856, 121–129 (2015). [DOI] [PubMed] [Google Scholar]
- 113.Crose LE, et al. Alveolar rhabdomyosarcoma-associated PAX3-FOXO1 promotes tumorigenesis via Hippo pathway suppression. The Journal of Clinical Investigation 124, 285–296 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Slemmons KK, Crose LE, Rudzinski E, Bentley RC & Linardic CM Role of the YAP Oncoprotein in Priming Ras-Driven Rhabdomyosarcoma. PLoS One 10, e0140781 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Roma J, Almazan-Moga A, Sanchez de Toledo J & Gallego S Notch, wnt, and hedgehog pathways in rhabdomyosarcoma: from single pathways to an integrated network. Sarcoma 2012, 695603 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kohsaka S, et al. A recurrent neomorphic mutation in MYOD1 defines a clinically aggressive subset of embryonal rhabdomyosarcoma associated with PI3K-AKT pathway mutations. Nat Genet 46, 595–600 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Van Antwerp ME, Chen DG, Chang C & Prochownik EV A point mutation in the MyoD basic domain imparts c-Myc-like properties. Proc Natl Acad Sci U S A 89, 9010–9014 (1992). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.MacQuarrie KL, et al. Comparison of genome-wide binding of MyoD in normal human myogenic cells and rhabdomyosarcomas identifies regional and local suppression of promyogenic transcription factors. Molecular and Cellular Biology 33, 773–784 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lee MH, Jothi M, Gudkov AV & Mal AK Histone methyltransferase KMT1A restrains entry of alveolar rhabdomyosarcoma cells into a myogenic differentiated state. Cancer Res 71, 3921–3931 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Walters ZS, et al. JARID2 is a direct target of the PAX3-FOXO1 fusion protein and inhibits myogenic differentiation of rhabdomyosarcoma cells. Oncogene (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ciarapica R, et al. The Polycomb group (PcG) protein EZH2 supports the survival of PAX3-FOXO1 alveolar rhabdomyosarcoma by repressing FBXO32 (Atrogin1/MAFbx). Oncogene (2013). [DOI] [PubMed] [Google Scholar]
- 122.Huynh KD, Fischle W, Verdin E & Bardwell VJ BCoR, a novel corepressor involved in BCL-6 repression. Genes Dev 14, 1810–1823 (2000). [PMC free article] [PubMed] [Google Scholar]
- 123.Missiaglia E, et al. MicroRNA and gene co-expression networks characterize biological and clinical behavior of rhabdomyosarcomas. Cancer Lett 385, 251–260 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hanahan D & Weinberg RA Hallmarks of cancer: the next generation. Cell 144, 646–674 (2011). [DOI] [PubMed] [Google Scholar]
- 125.Marshall AD, Lagutina I & Grosveld GC PAX3-FOXO1 induces cannabinoid receptor 1 to enhance cell invasion and metastasis. Cancer Res 71, 7471–7480 (2011). [DOI] [PubMed] [Google Scholar]
- 126.Yu Y, Davicioni E, Triche TJ & Merlino G The homeoprotein six1 transcriptionally activates multiple protumorigenic genes but requires ezrin to promote metastasis. Cancer Res 66, 1982–1989 (2006). [DOI] [PubMed] [Google Scholar]
- 127.Zheng H & Kang Y Multilayer control of the EMT master regulators. Oncogene 33, 1755–1763 (2014). [DOI] [PubMed] [Google Scholar]
- 128.Thiery JP, Acloque H, Huang RY & Nieto MA Epithelial-mesenchymal transitions in development and disease. Cell 139, 871–890 (2009). [DOI] [PubMed] [Google Scholar]
- 129.Skrzypek K, et al. SNAIL is a key regulator of alveolar rhabdomyosarcoma tumor growth and differentiation through repression of MYF5 and MYOD function. Cell Death Dis 9, 643 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ignatius MS, et al. The NOTCH1/SNAIL1/MEF2C Pathway Regulates Growth and Self-Renewal in Embryonal Rhabdomyosarcoma. Cell Rep 19, 2304–2318 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Khan J, et al. cDNA microarrays detect activation of a myogenic transcription program by the PAX3-FKHR fusion oncogene. Proc.Natl.Acad.Sci.U.S.A 96, 13264–13269 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Xu L, et al. Integrative Bayesian Analysis Identifies Rhabdomyosarcoma Disease Genes. Cell Rep 24, 238–251 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Soleimani VD, et al. Snail regulates MyoD binding-site occupancy to direct enhancer switching and differentiation-specific transcription in myogenesis. Mol Cell 47, 457–468 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lopez-Soto A, Gonzalez S, Smyth MJ & Galluzzi L Control of Metastasis by NK Cells. Cancer Cell 32, 135–154 (2017). [DOI] [PubMed] [Google Scholar]
- 135.Eichmuller SB, Osen W, Mandelboim O & Seliger B Immune Modulatory microRNAs Involved in Tumor Attack and Tumor Immune Escape. J Natl Cancer Inst 109(2017). [DOI] [PubMed] [Google Scholar]
- 136.Tran E, Robbins PF & Rosenberg SA 'Final common pathway' of human cancer immunotherapy: targeting random somatic mutations. Nat Immunol 18, 255–262 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Davicioni E, Anderson JR, Buckley JD, Meyer WH & Triche TJ Gene expression profiling for survival prediction in pediatric rhabdomyosarcomas: a report from the children's oncology group. J Clin Oncol 28, 1240–1246 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Rodeberg DA, et al. Prognostic significance and tumor biology of regional lymph node disease in patients with rhabdomyosarcoma: a report from the Children's Oncology Group. J.Clin.Oncol. 29, 1304–1311 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Mackall CL, et al. A pilot study of consolidative immunotherapy in patients with high-risk pediatric sarcomas. Clin Cancer Res 14, 4850–4858 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Qualman SJ, et al. Intergroup Rhabdomyosarcoma Study: update for pathologists. Pediatr Dev Pathol 1, 550–561 (1998). [DOI] [PubMed] [Google Scholar]
- 141.Oberlin O, et al. Prognostic factors in metastatic rhabdomyosarcomas: results of a pooled analysis from United States and European cooperative groups. J.Clin.Oncol 26, 2384–2389 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Miser JS & Pizzo PA Soft tissue sarcomas in childhood. Pediatr Clin North Am 32, 779–800 (1985). [DOI] [PubMed] [Google Scholar]
- 143.Haussler SM, et al. Head and neck rhabdomyosarcoma in children: a 20-year retrospective study at a tertiary referral center. J Cancer Res Clin Oncol 144, 371–379 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Sachedina A, Chan K, MacGregor D, Campbell M & Grover SR More than Grapes and Bleeding: An Updated Look at Pelvic Rhabdomyosarcoma in Young Females. J Pediatr Adolesc Gynecol (2018). [DOI] [PubMed] [Google Scholar]
- 145.Fernandez-Pineda I, et al. Vaginal tumors in childhood: the experience of St. Jude Children's Research Hospital. J Pediatr Surg 46, 2071–2075 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Karcioglu ZA, Hadjistilianou D, Rozans M & DeFrancesco S Orbital rhabdomyosarcoma. Cancer Control 11, 328–333 (2004). [DOI] [PubMed] [Google Scholar]
- 147.Doyle LA Sarcoma classification: an update based on the 2013 World Health Organization Classification of Tumors of Soft Tissue and Bone. Cancer 120, 1763–1774 (2014). [DOI] [PubMed] [Google Scholar]
- 148.Dziuba I, Kurzawa P, Dopierala M, Larque AB & Januszkiewicz-Lewandowska D Rhabdomyosarcoma in children - current pathologic and molecular classification. Pol J Pathol 69, 20–32 (2018). [DOI] [PubMed] [Google Scholar]
- 149.Parham D Rhabdomyosarcoma and related tumors in Pediatric Neoplasia: Morphology and Biology (ed. Parham D) 87–104 (Lippincott-Raven Publishers, Philadelphia, 1996). [Google Scholar]
- 150.Rudzinski ER, et al. Dense pattern of embryonal rhabdomyosarcoma, a lesion easily confused with alveolar rhabdomyosarcoma: a report from the Soft Tissue Sarcoma Committee of the Children's Oncology Group. Am J Clin Pathol 140, 82–90 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Rudzinski ER Histology and fusion status in rhabdomyosarcoma. Am Soc Clin Oncol Educ Book, 425–428 (2013). [DOI] [PubMed] [Google Scholar]
- 152.Arnold MA, et al. Histology, Fusion Status, and Outcome in Alveolar Rhabdomyosarcoma With Low-Risk Clinical Features: A Report From the Children's Oncology Group. Pediatr Blood Cancer 63, 634–639 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Ruiz-Mesa C, Goldberg JM, Coronado Munoz AJ, Dumont SN & Trent JC Rhabdomyosarcoma in adults: new perspectives on therapy. Curr Treat Options Oncol 16, 27 (2015). [DOI] [PubMed] [Google Scholar]
- 154.Noujaim J, et al. Adult Pleomorphic Rhabdomyosarcoma: A Multicentre Retrospective Study. Anticancer Res 35, 6213–6217 (2015). [PubMed] [Google Scholar]
- 155.Goldstein M, Meller I, Issakov J & Orr-Urtreger A Novel genes implicated in embryonal, alveolar, and pleomorphic rhabdomyosarcoma: a cytogenetic and molecular analysis of primary tumors. Neoplasia 8, 332–343 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Arnold MA & Barr FG Molecular diagnostics in the management of rhabdomyosarcoma. Expert Rev Mol Diagn 17, 189–194 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Nishio J, et al. Use of a novel FISH assay on paraffin-embedded tissues as an adjunct to diagnosis of alveolar rhabdomyosarcoma. Lab Invest 86, 547–556 (2006). [DOI] [PubMed] [Google Scholar]
- 158.Missiaglia E, et al. PAX3/FOXO1 fusion gene status is the key prognostic molecular marker in rhabdomyosarcoma and significantly improves current risk stratification. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 30, 1670–1677 (2012). [DOI] [PubMed] [Google Scholar]
- 159.Skapek SX, et al. PAX-FOXO1 fusion status drives unfavorable outcome for children with rhabdomyosarcoma: a children's oncology group report. Pediatric blood & cancer 60, 1411–1417 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Rudzinski ER, et al. Myogenin, AP2beta, NOS-1, and HMGA2 Are Surrogate Markers of Fusion Status in Rhabdomyosarcoma: A Report From the Soft Tissue Sarcoma Committee of the Children's Oncology Group. Am J Surg Pathol (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Villani A, et al. Biochemical and imaging surveillance in germline TP53 mutation carriers with Li-Fraumeni syndrome: 11 year follow-up of a prospective observational study. Lancet Oncol 17, 1295–1305 (2016). [DOI] [PubMed] [Google Scholar]
- 162.Kratz CP, et al. Cancer Screening Recommendations for Individuals with Li-Fraumeni Syndrome. Clin Cancer Res 23, e38–e45 (2017). [DOI] [PubMed] [Google Scholar]
- 163.Malkin D, Nichols KE, Schiffman JD, Plon SE & Brodeur GM The Future of Surveillance in the Context of Cancer Predisposition: Through the Murky Looking Glass. Clin Cancer Res 23, e133–e137 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Phallen J, et al. Direct detection of early-stage cancers using circulating tumor DNA. Sci Transl Med 9(2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Ferrari A, et al. Adult-type soft tissue sarcomas in pediatric-age patients: experience at the Istituto Nazionale Tumori in Milan. J.Clin.Oncol 23, 4021–4030 (2005). [DOI] [PubMed] [Google Scholar]
- 166.Blakely ML, et al. Prognostic factors and surgical treatment guidelines for children with rhabdomyosarcoma of the perineum or anus: a report of Intergroup Rhabdomyosarcoma Studies I through IV, 1972 through 1997. J Pediatr Surg 38, 347–353 (2003). [DOI] [PubMed] [Google Scholar]
- 167.Crist WM, et al. Prognosis in children with rhabdomyosarcoma: a report of the intergroup rhabdomyosarcoma studies I and II. Intergroup Rhabdomyosarcoma Committee. J Clin Oncol 8, 443–452 (1990). [DOI] [PubMed] [Google Scholar]
- 168.Malempati S & Hawkins DS Rhabdomyosarcoma: review of the Children's Oncology Group (COG) Soft-Tissue Sarcoma Committee experience and rationale for current COG studies. Pediatric blood & cancer 59, 5–10 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Ferrari A, et al. Access to clinical trials for adolescents with soft tissue sarcomas: Enrollment in European pediatric Soft tissue sarcoma Study Group (EpSSG) protocols. Pediatr Blood Cancer 64(2017). [DOI] [PubMed] [Google Scholar]
- 170.Dantonello TM, et al. Survival following disease recurrence of primary localized alveolar rhabdomyosarcoma. Pediatr Blood Cancer 60, 1267–1273 (2013). [DOI] [PubMed] [Google Scholar]
- 171.Heyn RM, et al. The role of combined chemotherapy in the treatment of rhabdomyosarcoma in children. Cancer 34, 2128–2142 (1974). [DOI] [PubMed] [Google Scholar]
- 172.Gallego S, et al. Detection of bone marrow micrometastasis and microcirculating disease in rhabdomyosarcoma by a real-time RT-PCR assay. J Cancer Res Clin Oncol 132, 356–362 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Meza JL, Anderson J, Pappo AS & Meyer WH Analysis of prognostic factors in patients with nonmetastatic rhabdomyosarcoma treated on intergroup rhabdomyosarcoma studies III and IV: the Children's Oncology Group. J Clin Oncol 24, 3844–3851 (2006). [DOI] [PubMed] [Google Scholar]
- 174.Lawrence W Jr., Anderson JR, Gehan EA & Maurer H Pretreatment TNM staging of childhood rhabdomyosarcoma: a report of the Intergroup Rhabdomyosarcoma Study Group. Children's Cancer Study Group. Pediatric Oncology Group. Cancer 80, 1165–1170 (1997). [PubMed] [Google Scholar]
- 175.Maurer HM, et al. The Intergroup Rhabdomyosarcoma Study-I. A final report. Cancer 61, 209–220 (1988). [DOI] [PubMed] [Google Scholar]
- 176.Hingorani P, et al. Clinical Application of Prognostic Gene Expression Signature in Fusion Gene-Negative Rhabdomyosarcoma: A Report from the Children's Oncology Group. Clin Cancer Res 21, 4733–4739 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Bisogno G, et al. Addition of dose-intensified doxorubicin to standard chemotherapy for rhabdomyosarcoma (EpSSG RMS 2005): a multicentre, open-label, randomised controlled, phase 3 trial. Lancet Oncol 19, 1061–1071 (2018). [DOI] [PubMed] [Google Scholar]
- 178.Bisogno G, et al. The role of doxorubicin in the treatment of rhabdomyosarcoma: preliminary results from the EpSSG RMS 2005 randomized trial. Pediatr Blood Cancer 61, S133–S134 (2014). [Google Scholar]
- 179.Casanova M, et al. Vinorelbine and low-dose cyclophosphamide in the treatment of pediatric sarcomas: pilot study for the upcoming European Rhabdomyosarcoma Protocol. Cancer 101, 1664–1671 (2004). [DOI] [PubMed] [Google Scholar]
- 180.Bisogno G, et al. Maintenance low-dose chemotherapy in patients with high-risk (HR) rhabdomyosarcoma (RMS): A report from the European Paediatric Soft Tissue Sarcoma Study Group (EpSSG). Journal of Clinical Oncology 36, LBA2–LBA2 (2018). [Google Scholar]
- 181.Pappo AS, et al. Two consecutive phase II window trials of irinotecan alone or in combination with vincristine for the treatment of metastatic rhabdomyosarcoma: the Children's Oncology Group. J Clin Oncol 25, 362–369 (2007). [DOI] [PubMed] [Google Scholar]
- 182.Hawkins D, et al. Vincristine, dactinomycin, cyclophosphamide (VAC) versus VAC/V plus irinotecan (VI) for intermediate-risk rhabdomyosarcoma (IRRMS): A report from the Children's Oncology Group Soft Tissue Sarcoma Committee. Proceedings of the American Society of Clinical Oncology, Abstract 10004 (2014). [Google Scholar]
- 183.Hawkins DS, et al. Addition of Vincristine and Irinotecan to Vincristine, Dactinomycin, and Cyclophosphamide Does Not Improve Outcome for Intermediate-Risk Rhabdomyosarcoma: A Report From the Children's Oncology Group. J Clin Oncol, JCO2018779694 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Bisogno G, et al. Sequential high-dose chemotherapy for children with metastatic rhabdomyosarcoma. Eur.J Cancer 45, 3035–3041 (2009). [DOI] [PubMed] [Google Scholar]
- 185.Weigel BJ, et al. Intensive Multiagent Therapy, Including Dose-Compressed Cycles of Ifosfamide/Etoposide and Vincristine/Doxorubicin/Cyclophosphamide, Irinotecan, and Radiation, in Patients With High-Risk Rhabdomyosarcoma: A Report From the Children's Oncology Group. J Clin Oncol 34, 117–122 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Walterhouse DO, et al. Shorter-duration therapy using vincristine, dactinomycin, and lower-dose cyclophosphamide with or without radiotherapy for patients with newly diagnosed low-risk rhabdomyosarcoma: a report from the Soft Tissue Sarcoma Committee of the Children's Oncology Group. J Clin Oncol 32, 3547–3552 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Walterhouse DO, et al. Reduction of cyclophosphamide dose for patients with subset 2 low-risk rhabdomyosarcoma is associated with an increased risk of recurrence: A report from the Soft Tissue Sarcoma Committee of the Children's Oncology Group. Cancer 123, 2368–2375 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Dasgupta R, Fuchs J & Rodeberg D Rhabdomyosarcoma. Semin Pediatr Surg 25, 276–283 (2016). [DOI] [PubMed] [Google Scholar]
- 189.Kieran K & Shnorhavorian M Current standards of care in bladder and prostate rhabdomyosarcoma. Urol Oncol 34, 93–102 (2016). [DOI] [PubMed] [Google Scholar]
- 190.Maurer HM, et al. The Intergroup Rhabdomyosarcoma Study-II. Cancer 71, 1904–1922 (1993). [DOI] [PubMed] [Google Scholar]
- 191.Terezakis SA & Wharam MD Radiotherapy for rhabdomyosarcoma: indications and outcome. Clin Oncol (R Coll Radiol) 25, 27–35 (2013). [DOI] [PubMed] [Google Scholar]
- 192.Saltzman AF & Cost NG Current Treatment of Pediatric Bladder and Prostate Rhabdomyosarcoma. Curr Urol Rep 19, 11 (2018). [DOI] [PubMed] [Google Scholar]
- 193.Casey DL & Wolden SL Rhabdomyosarcoma of the Head and Neck: A Multimodal Approach. J Neurol Surg B Skull Base 79, 58–64 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Ferrari A, et al. Rhabdomyosarcoma in infants younger than one year old: a report from the Italian Cooperative Group. Cancer 97, 2597–2604 (2003). [DOI] [PubMed] [Google Scholar]
- 195.Malempati S, et al. Rhabdomyosarcoma in infants younger than 1 year: a report from the Children's Oncology Group. Cancer 117, 3493–3501 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Alaggio R, et al. A Molecular Study of Pediatric Spindle and Sclerosing Rhabdomyosarcoma: Identification of Novel and Recurrent VGLL2-related Fusions in Infantile Cases. Am J Surg Pathol 40, 224–235 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Pappo AS, et al. Survival after relapse in children and adolescents with rhabdomyosarcoma: A report from the Intergroup Rhabdomyosarcoma Study Group. J Clin Oncol. 17, 3487–3493 (1999). [DOI] [PubMed] [Google Scholar]
- 198.Pappo AS, et al. A phase 2 trial of R1507, a monoclonal antibody to the insulin-like growth factor-1 receptor (IGF-1R), in patients with recurrent or refractory rhabdomyosarcoma, osteosarcoma, synovial sarcoma, and other soft tissue sarcomas: results of a Sarcoma Alliance for Research Through Collaboration study. Cancer 120, 2448–2456 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Kim A, et al. Phase 2 trial of sorafenib in children and young adults with refractory solid tumors: A report from the Children's Oncology Group. Pediatr Blood Cancer 62, 1562–1566 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Wagner LM, et al. Phase II study of cixutumumab in combination with temsirolimus in pediatric patients and young adults with recurrent or refractory sarcoma: a report from the Children's Oncology Group. Pediatr Blood Cancer 62, 440–444 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Mascarenhas L, et al. Randomized phase II trial of bevacizumab and temsirolimus in combination with vinorelbine (V) and cyclophosphamide (C) for first relapse/disease progression of rhabdomyosarcoma (RMS): A report from the Children’s Oncology Group (COG). J Clin Oncol 32, 5s (suppl; abstr 10003) (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Wolfe J, et al. Symptoms and Distress in Children With Advanced Cancer: Prospective Patient-Reported Outcomes From the PediQUEST Study. J Clin Oncol 33, 1928–1935 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Gupta AA, et al. Patterns of chemotherapy-induced toxicities and outcome in children and adolescents with metastatic rhabdomyosarcoma: A report from the Children's Oncology Group. Pediatr Blood Cancer 64(2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Cotter SE, et al. Proton radiotherapy for pediatric bladder/prostate rhabdomyosarcoma: clinical outcomes and dosimetry compared to intensity-modulated radiation therapy. Int J Radiat Oncol Biol Phys 81, 1367–1373 (2011). [DOI] [PubMed] [Google Scholar]
- 205.Macedo A Jr., et al. Sexual function in teenagers after multimodal treatment of pelvic rhabdomyosarcoma: A preliminary report. Journal of pediatric urology 6, 605–608 (2010). [DOI] [PubMed] [Google Scholar]
- 206.Frees S, et al. Erectile function after treatment for rhabdomyosarcoma of prostate and bladder. Journal of pediatric urology 12, 404 e401–404 e406 (2016). [DOI] [PubMed] [Google Scholar]
- 207.Martelli H, et al. Quality of life and functional outcome of male patients with bladder-prostate rhabdomyosarcoma treated with conservative surgery and brachytherapy during childhood. Brachytherapy 15, 306–311 (2016). [DOI] [PubMed] [Google Scholar]
- 208.Raney B, et al. Late effects in 164 patients with rhabdomyosarcoma of the bladder/prostate region: a report from the international workshop. J Urol 176, 2190–2194; discussion 2194-2195 (2006). [DOI] [PubMed] [Google Scholar]
- 209.Shapiro DD, Harel M, Ferrer F & McKenna PH Focusing on organ preservation and function: paradigm shifts in the treatment of pediatric genitourinary rhabdomyosarcoma. International urology and nephrology 48, 1009–1013 (2016). [DOI] [PubMed] [Google Scholar]
- 210.Rodeberg DA, et al. Delayed primary excision with subsequent modification of radiotherapy dose for intermediate-risk rhabdomyosarcoma: a report from the Children's Oncology Group Soft Tissue Sarcoma Committee. Int J Cancer 137, 204–211 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Chen S, et al. Genome-wide CRISPR screen in a mouse model of tumor growth and metastasis. Cell 160, 1246–1260 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Stewart E, et al. Orthotopic patient-derived xenografts of paediatric solid tumours. Nature 549, 96–100 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Langenau DM, et al. Effects of RAS on the genesis of embryonal rhabdomyosarcoma. Genes Dev. 21, 1382–1395 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Amatruda JF, Shepard JL, Stern HM & Zon LI Zebrafish as a cancer model system. Cancer Cell 1, 229–231 (2002). [DOI] [PubMed] [Google Scholar]
- 215.Galindo RL, Allport JA & Olson EN A Drosophila model of the rhabdomyosarcoma initiator PAX7-FKHR. Proc.Natl.Acad.Sci.U.S.A 103, 13439–13444 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Linardic CM & Counter CM Genetic modeling of Ras-induced human rhabdomyosarcoma. Methods Enzymol 438, 419–427 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Linardic CM, Downie DL, Qualman S, Bentley RC & Counter CM Genetic modeling of human rhabdomyosarcoma. Cancer Res. 65, 4490–4495 (2005). [DOI] [PubMed] [Google Scholar]
- 218.Sharp R, et al. Synergism between Ink4a/Arf inactivation and aberrrant HGF/SF signaling in rhabdomyosarcomagenesis. Nature Medicine 8, 1276–1280 (2002). [DOI] [PubMed] [Google Scholar]
- 219.Merchant MS, et al. Adjuvant Immunotherapy to Improve Outcome in High-Risk Pediatric Sarcomas. Clin Cancer Res 22, 3182–3191 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Merchant MS, et al. Phase I Clinical Trial of Ipilimumab in Pediatric Patients with Advanced Solid Tumors. Clin Cancer Res 22, 1364–1370 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Chicas-Sett R, Morales-Orue I, Rodriguez-Abreu D & Lara-Jimenez P Combining radiotherapy and ipilimumab induces clinically relevant radiation-induced abscopal effects in metastatic melanoma patients: A systematic review. Clin Transl Radiat Oncol 9, 5–11 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Allen CE, et al. Target and Agent Prioritization for the Children's Oncology Group-National Cancer Institute Pediatric MATCH Trial. J Natl Cancer Inst 109(2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Volchenboum SL, et al. Data Commons to Support Pediatric Cancer Research. Am Soc Clin Oncol Educ Book 37, 746–752 (2017). [DOI] [PubMed] [Google Scholar]
- 224.Ren YX, et al. Mouse mesenchymal stem cells expressing PAX-FKHR form alveolar rhabdomyosarcomas by cooperating with secondary mutations. Cancer Res. 68, 6587–6597 (2008). [DOI] [PubMed] [Google Scholar]
- 225.Hahn H, et al. Rhabdomyosarcomas and radiation hypersensitivity in a mouse model of Gorlin syndrome. Nature Medicine 4, 619–622 (1998). [DOI] [PubMed] [Google Scholar]
- 226.Hatley ME, et al. A mouse model of rhabdomyosarcoma originating from the adipocyte lineage. Cancer Cell 22, 536–546 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Nyagetuba JKM & Hansen EN Pediatric solid tumors in Africa: different biology? Curr Opin Pediatr 29, 354–357 (2017). [DOI] [PubMed] [Google Scholar]
- 228.Gupta S, et al. Treating Childhood Cancer in Low- and Middle-Income Countries in Cancer: Disease Control Priorities, Third Edition (Volume 3) (eds. Gelband H, Jha P, Sankaranarayanan R & Horton S) (Washington (DC: ), 2015). [Google Scholar]
- 229.Antillon F, et al. Treating Pediatric soft tissue sarcomas in a country with limited resources: the experience of the Unidad Nacional de Oncologia Pediatrica in Guatemala. Pediatr Blood Cancer 51, 760–764 (2008). [DOI] [PubMed] [Google Scholar]
- 230.Sultan I, Qaddoumi I, Yaser S, Rodriguez-Galindo C & Ferrari A Comparing adult and pediatric rhabdomyosarcoma in the surveillance, epidemiology and end results program, 1973 to 2005: an analysis of 2,600 patients. J Clin Oncol 27, 3391–3397 (2009). [DOI] [PubMed] [Google Scholar]
- 231.Ferrari A, et al. Rhabdomyosarcoma in adults. A retrospective analysis of 171 patients treated at a single institution. Cancer 98, 571–580 (2003). [DOI] [PubMed] [Google Scholar]
- 232.Davis LE, et al. Clinical trial enrollment of adolescents and young adults with sarcoma. Cancer 123, 3434–3440 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Wexler LH, S.S., Helman LJ. Rhabdomyosarcoma in Principles and Practice of Pediatric Oncology (ed. Pizzo PA, P.D.) 798–826 (Wolters Kluwer, Philadelphia, PA, 2016). [Google Scholar]
- 234.Grufferman S, et al. Parental military service, agent orange exposure, and the risk of rhabdomyosarcoma in offspring. J Pediatr 165, 1216–1221 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


