Abstract
Objectives
The aim of this study was to report burnout time trends and describe the psychological effects of working as a Canadian emergency physician during the first weeks of the coronavirus disease 2019 (COVID‐19) pandemic.
Methods
This was a mixed‐methods study. Emergency physicians completed a weekly online survey. The primary outcome was physician burnout as measured by the emotional exhaustion and depersonalization items, from the Maslach Burnout Inventory. We captured data on work patterns, aerosolizing procedures, testing and diagnosis of COVID‐19. Each week participants entered free text explaining their experiences and well‐being.
Results
There were 468 participants who worked in 143 Canadian hospitals. Burnout levels did not significantly change over time (emotional exhaustion P = 0.632, depersonalization P = 0.155). Three participants were diagnosed with COVID‐19. Being tested for COVID‐19 (odds ratio [OR] 11.5, 95% confidence interval [CI] 3.1–42.5) and the number of shifts worked (OR 1.3, 95% CI 1.1–1.5 per additional shift) were associated with high emotional exhaustion. Having been tested for COVID‐19 (OR 4.3, 95% CI 1.1–17.8) was also associated with high depersonalization. Personal safety, academic and educational work, personal protective equipment, the workforce, patient volumes, work patterns, and work environment had an impact on physician well‐being. A new financial reality and contrasting negative and positive experiences affected participants’ psychological health.
Conclusion
Emergency physician burnout levels remained stable during the initial 10 weeks of this pandemic. The impact of COVID‐19 on the work environment and personal perceptions and fears about the impact on lifestyle have affected physician well‐being.
Keywords: COVID‐19, emergency physicians, physician burnout, physician wellness
1. INTRODUCTION
1.1. Background
Healthcare providers are at risk of negative psychological reactions after being exposed to stressful situations, ranging from symptoms such as fear and stress to posttraumatic stress disorder. 1 During the coronavirus disease 2019 (COVID‐19) pandemic, it is expected that some healthcare workers will experience moral injury, burnout, and mood disorders. Moral injury is the distress (shame or guilt) experienced after violating one's own moral code, 2 for example when rationing access to levels of health care. Burnout is a work‐related syndrome involving emotional exhaustion, depersonalization, and a sense of reduced personal accomplishment. 3 Burnout can lead to frustration, a sense of loss of control, and diminishing morale. 4 Burnout affects workforce retention and can lead to important mental health consequences including depression and suicide. 5
1.2. Importance
There are many reasons why the COVID‐19 pandemic has the potential to cause burnout among the emergency physician community. The job demands‐resources theory suggests that burnout results from increased physical or psychological work demands and reduced resources. 6 During a pandemic, reduced safety standards (personal protective equipment [PPE] shortages), increased workload (rising patient numbers, increased departmental staffing, covering for sick colleagues), and poor mental health (anxiety, fatigue, and depression) could all predispose physicians to burnout. 7 Psychological distress could result from repeated or prolonged exposure to distressing events, 8 death of a colleague, friend or family member, 9 being tasked with new or difficult roles beyond their normal remit, 8 being put into quarantine, 10 and deprioritizing treatment at triage. 11
1.3. Goals of this investigation
The aim of this study was to report burnout time trends and describe the psychological effects of working as an emergency physician in Canada during the first 10 weeks of the COVID‐19 pandemic.
2. METHODS
2.1. Study design and setting
This was a mixed‐methods study that follows the Good Reporting of A Mixed Methods Study guidance. 12 We followed a cohort of Canadian emergency physicians through the first 10 weeks of the COVID‐19 pandemic. The mixed‐methods approach allowed us to monitor burnout levels while simultaneously collecting both quantifiable risks for burnout and rich information on sources of psychological distress and participant experience.
2.2. Selection of participants
The population of interest was physicians working in Canadian emergency departments (EDs). We invited emergency physicians and trainees to participate in this study using 3 approaches (email, social media, and through professional societies). The survey was sent by email to 20 emergency physician groups in 7 provinces (via members of the Network of Canadian Emergency Researchers) on April 4, 2020, with 1 reminder sent a week later. The study was launched on Twitter (@EmergWell) and Facebook on April 13 and was disseminated through every Canadian association that registers emergency physicians: the Society of Rural Physicians of Canada (450 physicians), the Canadian Association of Emergency Physicians (1857 physicians), Association des médecins d'urgence du Québec (1358 physicians), and Association des spécialistes en médecine d'urgence du Québec (180 physicians).
2.3. Quantitative measurements
The study used a weekly online survey that was designed to be completed quickly, on a phone, tablet, or computer. Physicians were asked to complete the survey once a week for 10 weeks. The survey was designed to be as simple as possible to minimize loss to follow‐up as time progressed. Also, we were mindful that the burden of our survey could add to stress and burnout during this challenging time for participants; we wanted to minimize this impact. The participant could choose to receive survey reminders and links on their cellphone or else by email. Each week, an invitation was sent to a new survey, with 1 reminder 2 days later. The survey was initially piloted by the physician members of our investigator group, then refined further with feedback from 5 emergency physicians, to optimize clarity, brevity, layout, and simplicity.
The survey collected data relating to the period of March 9 to May 17, 2020. Details regarding the content of the survey are included in Appendix 1. The study was launched on April 4, 2020 (at the time of research ethics board approval), at which point physicians entered data on shifts worked in the previous 3 weeks (ie, between the weeks of March 9–15, 16–22, and 23–29). Burnout questions were first introduced on week 4 to ensure that participants entered their burnout responses prospectively.
2.4. Outcomes
Burnout, the most commonly used measure of physician mental health, 13 was our primary outcome. We measured physician burnout using the single item measures of emotional exhaustion and depersonalization from the Maslach Burnout Inventory, “I feel burned out from my work” and “I have become more callous toward people since I took this job,” with a 7‐point Likert scale response (never/a few times a year or less/once a month or less/a few times a month/once a week/a few times a week/every day). These items have been shown to correlate to the emotional exhaustion and depersonalization domains from the Maslach Burnout Inventory 14 and exhibit consistent association with key outcomes such as perceived major medical errors, unprofessional attitudes, and serious thoughts of dropping out in cohorts of medical students and physicians. 15 High levels of emotional exhaustion and depersonalization were defined as responses indicating occurrence at least weekly. 15 To minimize prior response recall, the Maslach Burnout Inventory items were included every 2 weeks (weeks 4, 6, 8, and 10). Our survey's secondary outcomes were shifts missed at short notice (with reasons for missing the shift) and participant COVID‐19 infection.
2.5. Explanatory variables
We hypothesized that working a higher number of shifts, additional shifts at short notice, and in unfamiliar settings could have detrimental effects on physician mental health, leading to burnout. We recorded the number of scheduled shifts participants worked every week, the number of shifts participants worked at short notice, and shifts worked in unfamiliar hospitals or areas other than the ED. We also tracked the number of aerosolizing procedures performed weekly because these procedures are thought to pose a high risk for hospital‐acquired COVID infection. We collected data on family circumstances including children, partners who worked in health care and other caregiver roles, as well as self‐identified immunosuppression.
The survey was anonymous; however, we collected age, genderhospital, province, and city of work, and prior experience of severe acute respiratory syndrome coronavirus or Middle East respiratory syndrome coronavirus.
2.6. Qualitative data collection
We asked participants to explain how they were feeling or else explain their survey answers in a free‐text box each week. There was no limit on text length. These qualitative comments were used adjunctively to augment our quantitative findings and to explore sources of psychological stress.
The Bottom Line
There are several threats to emergency physician psychological well‐being during this current pandemic, ranging from safety in the work environment to personal perceptions and fears about the impact on home life. The paper uses a mixed‐methods approach to explore psychological stressors and their association with physician burnout during the early stages of the coronavirus disease 2019 (COVID‐19) pandemic.
2.7. Analysis
The primary analysis was the time trend in emotional exhaustion and depersonalization burnout scores over the 10‐week study duration. Secondary analyses included associations with burnout and emerging themes from the participant free‐text communications.
Continuous data were reported as means with SDs or medians with interquartile range, where appropriate. Continuous and dichotomous measures were compared using analysis of variance and χ2 tests, respectively. Hierarchical models were developed to examine time trends and associations with burnout. For burnout, both emotional exhaustion and depersonalization were considered dependent variables. As every burnout score was included in these models, we accounted for clustering of effects of burnout scores within participants. The primary analysis (analysis of time trend) used hierarchical regression models to assess for an association between the pandemic week and burnout scores. Hierarchical logistic regression analyses evaluated associations with high emotional exhaustion and high depersonalization levels. Independent variables were chosen a priori, based on existing literature and plausibility. Independent variables for the models included age (years), gender (male vs non‐binary/female), tested for COVID‐19 in prior 7 days (yes/no), number of scheduled shifts in prior 7 days, number of extra shifts picked up at short notice in prior 7 days, number of aerosol procedures performed in prior 7 days, and whether some shifts were worked in a department other than the participant's usual one in prior 7 days (yes/no).
The goal of the qualitative analysis was to summarize emerging themes of important aspects for participant well‐being and distress. Limited by the types of free‐text data we acquired in our survey, we opted to complete a thematic analysis using interpretive description. 16 , 17 To capture the time course of emerging themes, we conducted a serial analysis of weekly data. Initially, 2 analysts (CW, TC) created a coding schema together using the first 4 weeks of data. These codes were then used to independently code each of the subsequent weeks. Analysts exchanged their remaining coding to ensure that they agreed upon final findings. To ensure further rigor, 3 members of our investigatory team (KR, CG, MM) conducted a further audit of the data trail. All study investigators reviewed the quantitative associations and qualitative data together to interpret the study findings.
Study data were collected and managed using REDCap electronic data capture tools hosted at McMaster University. 18 , 19 REDCap (Research Electronic Data Capture) is a secure, web‐based software platform designed to support data capture for research studies (REDCap Consortium, Nashville, TN). All analyses were performed using Stata/SE 13.1 (StataCorp, College Station, TX).
2.8. Ethics
The study was approved by Hamilton Integrated Research Board on April 3, 2020.
3. RESULTS
In total, 583 physicians consented to participate in the survey of whom, 468 participants entered data on their demographics. Overall, 461 participants completed at least 1 survey, and 231 completed all 10 weekly surveys (mean number of weekly surveys completed 7.7). Three participants unsubscribed from the survey, and 2 physicians reported they had stopped working in the ED during the pandemic.
Of the 1147 physicians working in 20 hospital groups, 345 (30%) consented to participate. A further 238 physicians gave consent to participate after the study was advertised on social media and distribution via medical society email lists. It is not possible to estimate response rates for social media and society distribution, and there was overlap between these methods of approach. In 2016, the Canadian Association of Emergency Physicians and Royal College of Physicians and Surgeon of Canada estimated there were 6500 physicians practicing as emergency physicians in Canada. 20
The median age was 41, and 49% of participants were female (Table 1). Approximately 9% were emergency medicine residents, the remainder being staff physicians. Every Canadian province and territory was represented with the exception of the Yukon. Participants worked at 143 different hospitals.
TABLE 1.
Participant demographics (n = 468)
| Age | Median 41 (interquartile range 35–50) |
|---|---|
| Gender | |
| Female | 227 (49%) |
| Male | 240 (51%) |
| Non‐binary | 1 (0%) |
| Position | |
| Emergency resident | 40 (9%) |
| Staff physician | 428 (91%) |
| Province/Territory | |
| British Columbia | 48 (10%) |
| Alberta | 19 (4%) |
| Saskatchewan | 15 (3%) |
| Manitoba | 20 (4%) |
| Ontario | 251 (54%) |
| Québec | 66 (14%) |
| New Brunswick | 12 (3%) |
| Prince Edward Island | 5 (1%) |
| Nova Scotia | 13 (3%) |
| Newfoundland and Labrador | 13 (3%) |
| Yukon | 0 |
| North West Territories | 3 (1%) |
| Nunavut | 1 (0%) |
| Other/not specified | 2 (0%) |
| Immunosuppressed | 15 (3%) |
| Lives with | |
| Partner | 400 (85%) |
| Children | 300 (64%) |
| Parents | 14 (3%) |
| Extended family | 12 (3%) |
| Roommate | 11 (2%) |
| Partner works in health care | 142 (30%) |
| Caregiver for friend or family member | 72 (15%) |
| Severe acute respiratory syndrome coronavirus or Middle East respiratory syndrome coronavirus experience | 147 (31%) |
| Typical shift pattern | |
| Even spread | 301 (64%) |
| More days | 57 (12%) |
| More evenings | 76 (16%) |
| More nights | 34 (7%) |
We did not find a time trend in burnout levels (P = 0.632 for emotional exhaustion and P = 0.155 for depersonalization). In week 4, 67/380 respondents (18%) scored high emotional exhaustion, 65/372 (17%) in week 6, 49/341 (14%) in week 8, and 47/297 (16%) in week 10. In week 4, 56/380 (15%) scored high depersonalization, 49/372 (13%) in week 6, 35/341 (10%) in week 8, and 39/296 (13%) in week 10. Of the 266 participants who completed both week 4 (first burnout survey) and week 10 (last burnout survey), 13 participants changed from low to high levels of emotional exhaustion, 21 moved from high to low emotional exhaustion, and 232 remained in the same category. For depersonalization, 12 moved from low to high, 15 high to low, and 239 remained static.
Three participants (0.6%) were diagnosed with COVID‐19. Of the 191 missed scheduled shifts, 124 (65% of missed shifts) were missed because the participant was in quarantine, 12 (6%) because of COVID illness, 6 (3%) because of childcare or family issues, and 49 (26%) for other reasons. Figure 1 shows time trends in number of shifts worked and missed.
FIGURE 1.
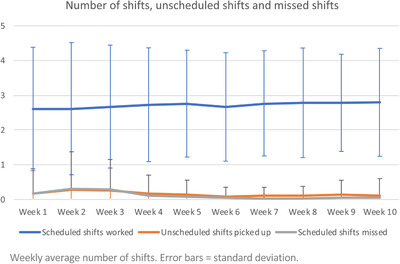
Time trends in scheduled, unscheduled, and missed work shifts
Being tested for COVID‐19 in the previous week (odds ratio [OR] 11.5, 95% confidence interval [CI] 3.1–42.5) and the number of shifts worked (OR 1.3, 95% CI 1.1–1.5 per additional shift, per week) were associated with high emotional exhaustion. Having been tested for COVID‐19 (OR 4.3, 95% CI 1.1–17.8) was also associated with high depersonalization. Table 2 shows the results of the multivariable hierarchical logistic regression models.
TABLE 2.
Associations between emergency physician characteristics, their work experience, and burnout levels (N = 436)
| Emotional exhaustion | Odds ratio | 95% confidence interval |
|---|---|---|
| Male gender | 0.54 | 0.22–1.35 |
| Age (years) | 1.03 | 0.98–1.09 |
| Tested for COVID‐19 | 11.48 | 3.10–42.46 |
| Number of shifts per week | 1.26 | 1.05–1.52 |
| Number of extra shifts per week, worked at short notice | 1.54 | 0.84–2.80 |
| Number of aerosol procedures | 0.90 | 0.68–1.19 |
| Working in usual department only | 0.75 | 0.13– 4.31 |
| Depersonalization | Odds ratio | 95% confidence interval |
|---|---|---|
| Male gender | 0.62 | 0.23–1.68 |
| Age (years) | 0.98 | 0.93–1.04 |
| Tested for COVID‐19 | 4.32 | 1.05–17.81 |
| Number of shifts per week | 1.13 | 0.93–1.39 |
| Number of extra shifts per week, worked at short notice | 1.54 | 0.81–2.93 |
| Number of aerosol procedures | 1.09 | 0.83–1.44 |
| Working in usual department only | 1.00 | 0.12–8.20 |
We analyzed a total of 516 qualitative comments over the 10‐week period from 213 different participants. A complete listing of the themes and their frequencies are found in Appendix 2. Broadly speaking there were 2 main categories of themes. The first category included themes about the impact of COVID‐19 on the work environment. We identified that personal safety, academic and educational work, PPE, the workforce, patient volumes, work patterns, and the work environment all had an impact on physician well‐being. Figure 2 lists these themes in full, with example quotes. The second category included themes concerning personal perceptions and fears about the ramifications of COVID‐19 on lifestyle. This category included a new financial reality and contrasting negative and positive experiences that affected participants' psychological health. Figure 3 outlines these themes in detail. Appendices 3 and 4 outline the thematic time trends relating to environmental impact and personal perceptions and fears relating to lifestyle.
FIGURE 2.
Themes relating to the impact of coronavirus disease 2019 (COVID‐19) on the workplace environment
FIGURE 3.
Personal perceptions and fears about the ramifications of coronavirus disease 2019 (COVID‐19) on lifestyle
4. LIMITATIONS
Our study had several limitations. Not all participants responded to the survey every week, meaning those who felt burned out may not have respond to the survey reminders. If this was the case, we would have underreported burnout rates. We did not directly measure burnout pre‐pandemic and are unable to report our findings in the context of “usual” burnout levels among this cohort. Our qualitative analysis was based on free text from the survey responses rather than interviews. We are still conducting in‐depth interviews with the same cohort and will report these results later, in relation to the findings from this survey.
5. DISCUSSION
In this Canadian emergency physician cohort, we did not detect a trend toward increasing physician burnout over time during the initial 10 weeks of the COVID‐19 pandemic. Our qualitative data suggest subsets of participants experienced significant distress relating to the pandemic, which affected both their work environment and lifestyle. The number of physicians unable to work (missing shifts at short notice) was exceedingly low, mostly a result of quarantine rather than illness, and only 3 out of 468 participants (0.6%) reported testing positive for COVID‐19.
Our findings suggest that emergency physician experiences are much broader and wide ranging than a simple burnout metric – their comments on the pandemic ranged from childrearing woes to finance to workplace safety issues. Although many participants commented on the burnout they were feeling, some found that the pandemic offered a new take on their professional lives, providing them with newfound purpose and resilience. This phenomenon has been previously described: after experiencing adversity, some people may develop mental health difficulties 21 whereas others develop self‐esteem and resilience. 22 Our study found that COVID‐19 testing and working more shifts in the prior week were associated with burnout. To our knowledge, the association with COVID‐19 testing has not previously been evaluated. Our qualitative data suggested COVID‐19 testing could be particularly stressful for an emergency physician because of stigma; having potentially exposed patients, coworkers, or family to the virus; and loss of income during illness or quarantine. However, it is also possible that those who felt burned out were more likely to be tested. Burnout and compassion fatigue are known to be associated with working longer hours. 23
There may be several reasons why we did not identify association between burnout and the progression of time during the first weeks of the pandemic. First, psychological distress is associated with high levels of exposure to traumatic events, 8 which may explain our lack of worsening burnout levels over time during the pandemic. It is possible that our cohort did not experience the concentrated numbers of sick patients seen in other parts of the world. Second, the mental health effects of a disaster or mass casualty are known to trail behind the initial trauma or event. 24 , 25 We may simply have measured burnout too soon after the start of this pandemic to detect changing burnout levels.
Our study has a number of strengths. Our reported burnout levels are comparable to those reported by an Italian cohort of nurses and physicians during the COVID‐19 pandemic 26 and those reported by the 2018 Canadian Medical Association National Physician Survey. 27 Our mixed‐methods approach allowed a rich exploration of the psychological stressors in addition to measuring participant burnout.
In conclusion, emergency physician burnout levels remained relatively stable during the initial 10 weeks of the COVID‐19 pandemic. Longer work hours and COVID‐19 testing were associated with burnout. There were several threats to emergency physician psychological well‐being including the impact of COVID‐19 on the work environment and personal perceptions and fears about the impact of COVID‐19 on lifestyle
CONFLICT OF INTEREST
Dr. Gérin‐Lajoie reports employment with the Canadian Medical Association and notes that the opinions and conclusions expressed are the writers’ own and are not those of the Canadian Medical Association.
AUTHOR CONTRIBUTIONS
Kerstin de Wit, Mathew Mercuri, Clare Wallner, Natasha Clayton, Kerri Ritchie, Caroline Gérin‐Lajoie, Lisa Schwartz, Sara Gray, and Teresa Chan planned and designed the study. Kerstin de Wit obtained research ethics approval and study funding. Kerstin de Wit, Clare Wallner, Natasha Clayton, Patrick Archambault, and Teresa Chan conducted the study, including designing the survey, disseminating study invitations, reviewing weekly survey responses, and resolving problems as they arose. Kerstin de Wit, Mathew Mercuri, Clare Wallner, Natasha Clayton, Kerri Ritchie, Caroline Gérin‐Lajoie, and Teresa Chan analyzed the data. All authors reviewed the study results and contributed to the interpretation. All study authors contributed to writing this manuscript and have approved the final version.
Supporting information
Supplementary information
Supplementary information
Supplementary information
Supplementary information
ACKNOWLEDGMENTS
We would like to acknowledge the support provided by the Network of Canadian Emergency Researchers, the Canadian Association of Emergency Physicians research committee, Dr Laurie Morrison, Dr Michelle Welsford, Dr Andrew Worster, Dr Shawn Mondoux, Mary Boulos, Robert Hill, and Anna Tran.
Biography
Kerstin de Wit, MBCHB, BSC, MSC, MD, MRCP, FRCEM, FRCPC is an Associate Professor at McMaster University.
de Wit K, Mercuri M, Wallner C, et al. Canadian emergency physician psychological distress and burnout during the first 10 weeks of COVID‐19: A mixed‐methods study. JACEP Open. 2020;1:1030–1038. 10.1002/emp2.12225
The study was endorsed by the Network of Canadian Emergency Researchers.
Supervising Editor: Theodore J. Gaeta, DO, MPH.
Funding Information: The Juravinski Research Institute and Hamilton Health Sciences.
[Correction added on 31 August 2020, after first online publication: “Caroline Gérin‐Lajoi” is corrected to “Caroline Gérin‐Lajoie” in two instances in the Author Contributions section.]
REFERENCES
- 1. Benedek DM, Fullerton C, Ursano RJ. First responders: mental health consequences of natural and human‐made disasters for public health and public safety workers. Annu Rev Public Health. 2007;28:55‐68. [DOI] [PubMed] [Google Scholar]
- 2. Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev. 2009;29(8):695‐706. [DOI] [PubMed] [Google Scholar]
- 3. Maslach C JS, Leiter MP. Maslach burnout inventory manual. Vol 3rd edn Palo Alto: Consulting Psychologists Pres; 1996. [Google Scholar]
- 4. Valent P. Diagnosis and treatment of helper stresses, traumas, and illnesses In: Figley CR, ed. Treating Compassion Fatigue. New York: Brunner‐Routledge; 2002;17‐37. [Google Scholar]
- 5. Dyrbye LN, Thomas MR, Massie FS, et al. Burnout and suicidal ideation among U.S. Medical Students. Ann Intern Med. 2008;149(5):334‐341. [DOI] [PubMed] [Google Scholar]
- 6. Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands‐resources model of burnout. J Appl Psychol. 2001;86:499–512. [PubMed] [Google Scholar]
- 7. Lee R, Seo B, Kladkyj S, Lovell BL, Schwarzmann L. Correlates of physician burnout across regions and specialties: a meta‐analysis. Hum Resour Health. 2013;11:48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Brooks SK, Rubin GJ, Greenberg N. Traumatic stress within disaster‐exposed occupations: overview of the literature and suggestions for the management of traumatic stress in the workplace. Br Med Bull. 2019;129(1):25‐34. [DOI] [PubMed] [Google Scholar]
- 9. Berninger A, Webber MP, Cohen HW, et al. Trends of elevated PTSD risk in firefighters exposed to the World Trade Center disaster: 2001–2005. Public Health Rep. 2010;125(4):556‐566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet North Am Ed. 2020;395(10227):912‐920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Thoresen S, Tønnessen A, Lindgaard CV, Andreassen AL, Weisaeth L. Stressful but rewarding: Norwegian personnel mobilised for the 2004 tsunami disaster. Disasters. 2009;33(3):353‐368. [DOI] [PubMed] [Google Scholar]
- 12. O'Cathain A, Murphy E, Nicholl J. The Quality of Mixed Methods Studies in Health Services Research. J Health Serv Res Policy. 2008;13(2):92‐98. [DOI] [PubMed] [Google Scholar]
- 13. Kinmna G, Teoh K. What could make a difference to the mental health of UK doctors? A review of the research evidence. London: Society of Occupational Medicine & The Louise Tebboth Foundation; https://eprints.bbk.ac.uk/24540/. Published 2018. Accessed. [Google Scholar]
- 14. West CP, Dyrbye LN, Sloan JA, Shanafelt TD. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. 2009;24(12):1318‐1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. West CP, Dyrbye LN, Satele DV, Sloan JA, Shanafelt TD. Concurrent validity of single‐item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. 2012;27(11):1445‐1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Thorne S. Interpretive Description. Qualitative research for applied practice. 2nd Edition ed: New York: Routledge Taylor and Francis Group; 2016. [Google Scholar]
- 17. Thorne S, Kirkham SR, O'Flynn‐Magee K. The analytic challenge in interpretive description. Int J Qual Methods. 2004;3(1):1‐11. [Google Scholar]
- 18. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Final Report of the Collaborative Working Group on the Future of Emergency Medicine in Canada. Emergency Medicine Training & Practice in Canada: Celebrating the Past & Evolving for the Future. Ottawa: Canadian Association of Emergency Physicians 2016. https://caep.ca/wp-content/uploads/2017/07/cwg0001_cwg-em_report_-_executive_summary_-_english_-_singles_-_web1.pdf
- 21. Williamson V, Stevelink SAM, Greenberg N. Occupational moral injury and mental health: systematic review and meta‐analysis. Br J Psychiatry. 2018;212(6):339‐346. [DOI] [PubMed] [Google Scholar]
- 22. Brooks S, Amlôt R, Rubin GJ, Greenberg N. Psychological resilience and post‐traumatic growth in disaster‐exposed organisations: overview of the literature. BMJ Mil Health. 2020;166(1):52‐56. [DOI] [PubMed] [Google Scholar]
- 23. Lynch SH, Lobo ML. Compassion fatigue in family caregivers: a Wilsonian concept analysis. J Adv Nurs. 2012;68(9):2125‐2134. [DOI] [PubMed] [Google Scholar]
- 24. Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397‐422. [DOI] [PubMed] [Google Scholar]
- 25. Morera LP, Gallea JI, Trógolo MA, Guido ME, Medrano LA. From work well‐being to burnout: a hypothetical phase model. Front Neurosci. 2020;14:360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Barello S, Palamenghi L, Graffigna G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID‐19 pandemic. Psychiatry Res. 2020;290:113129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Canadian Medical Association . CMA National Physician Health Survey. Ottawa: Canadian Medical Association; https://www.cma.ca/sites/default/files/2018-11/nph-survey-e.pdf. Published 2018. Accessed2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information
Supplementary information
Supplementary information
Supplementary information


