Abstract
Background
Giving patients anti-osteoporotic agents peri-operatively is a well-accepted strategy to increase fusion rate and prevent complications. The purpose of this study was to investigate effectiveness of teriparatide and bisphosphonate on fusion surgery of thoracic and lumbar spine.
Methods
We searched EMBASE and PubMed for randomized clinical trials (RCTs) and prospective comparative studies using teriparatide or bisphosphonate in peri-operative spinal fusion surgery. Our synthesized data of fusion rate, Oswestry disability index (ODI), and adverse event in contrast-based network meta-analysis. Pooled results were presented in risk ratio (RR) or mean difference (MD) with 95% confidence interval (CI).
Results
Our search hit eight RCTs and three prospective studies with 676 patients receiving spinal surgery. Pooled result showed that teriparatide+Denosumab leads to significantly higher fusion rate than placebo (RR, 2.84; 95% CI: 1.22 to 6.60) and bisphosphonate (RR, 2.59; 95% CI: 1.13 to 5.96). We did not observe significant finding among placebo, teriparatide, and bisphosphonate in the two network models.
Conclusion
This is the first network meta-analysis providing an overview of the use of teriparatide and bisphosphonate for spinal fusion surgery. Teriparatide treatments are worth to be consider for spinal fusion surgery.
Introduction
Spinal fusion surgery is widely employed to treat lumbar stenosis, instability, intervertebral disc degeneration, deformity, and trauma of spine. In recent years, the number of patients undergoing the operation has been increasing in USA [1, 2]. The stability of spinal instrumentation relies on good bone quality and the pullout strength of pedicle screws is highly correlated with bone mineral density of spine [3]. Among patients undergoing the procedure, many are geriatrics with high prevalence of low bone mass and osteoporosis [1, 4]. Operation on an osteoporotic spine increases risk of complications, such as implant migration, instrumentation failure, adjacent compression fracture and pseudoarthrosis [5]. According to previous research, pseudoarthrosis after lumbar spine fusion is not rare, ranging from 5% to 35% [6, 7], and may be associated with poor outcomes [8]. As a result, successful treatment of osteoporosis and elevated fusion after spine surgery are important and challenging issues for surgeons. Giving patients anti-osteoporotic agents peri-operatively is a well-accepted strategy to increase fusion rate and prevent complications [9]. Among many anti-osteoporotic medicines, teriparatide [recombinant human PTH (1–34)] and bisphosphonate are most commonly used [9]. Teriparatide is an artificial synthetic parathyroid hormone. When given intermittently, it exhibits strong anabolic effect on skeleton and increases bone mineral density by stimulating new bone formation [10]. Bisphosphonate, on the other hand, is a derivative of inorganic pyrophosphate. It inhibits the activity of osteoclast and increases bone stock by decreasing bone absorption [11]. While there are studies supporting the use of both agents [12, 13], pooled evidence on their comparative efficacy is still lacking. To make up for such deficiency, this study performed a network meta-analysis to synthesize the current evidence on effectiveness of teriparatide and bisphosphonate in fusion surgery of thoracic and lumbar spine.
Methods
According to the Cochrane handbook and PRISMA guidelines, eligibility criteria were defined for this comprehensive synthesis and search strategy was developed. Databases and reference lists of relevant studies were searched and evidence was selected, followed by data extraction and quality assessment. The consistency model was then formed and network meta-analysis was conducted. This network meta-analysis was exempted from institutional review board approval because this study synthesized and analyzed only published data.
Evidence selection criteria
According to the proposed research question, this comprehensive synthesis selected evidence if (a) the study recruited patients undergoing spinal fusion; (b) the intervention involved the administration of teriparatide or bisphosphonate; and (c) the study design was randomized clinical trial or prospective comparative investigation with two or more arms. Exclusion criteria defined to enhance the validity of the comprehensive synthesis were as follows: (a) animal study; (b) studies recruited cervical spinal fusion; (c) gray literature without detailed information, data, or full text; and (d) studies without results on fusion rate, Oswestry disability index (ODI), bone mineral density (BMD), or overall adverse event.
Search strategy and study selection
The top two online databases in biomedical science, EMBASE and PubMed (including MEDLINE), were the main sources of this comprehensive synthesis. PubMed provides a well-established platform for building the primary search strategy. Relevant terms of spinal fusion, spinal arthrodesis, teriparatide, and bisphosphonate were identified in both free-text and medical subject heading (Emtree in EMBASE and MeSH in PubMed) with appropriate Boolean operator to form the search strategy. Boolean operator “OR” was used for combining the relevant terms of spinal fusion and spinal arthrodesis. As mentioned above, this analysis aims to provide an overview of the effects of two common anti-osteoporotic medicines (teriparatide and bisphosphonate) on patients undergoing spinal fusion procedure rather than making head-to-head comparison of the two anti-osteoporotic medicines. Thus, “OR” was also employed to combine relevant terms of teriparatide and bisphosphonate, thus increasing search sensitivity. Then, the spinal fusion part was combined with the anti-osteoporotic medicine part through Boolean operator “AND”. The search strategy developed had no restriction on language and publication date from each database inception until February 07, 2020 (S1 File in S1 Appendix).
After potential references were identified from EMBASE and PubMed, two research members started evidence selection in two steps, namely title and abstract screening and full-text review according to the eligibility criteria previously defined. In case of different judgements on a reference in the individual screening process of evidence selection, a meeting would be called to review the references till a consensus was reached.
Data extraction and quality assessment
Two research members independently extracted relevant information and outcome data. The relevant information covered the details of study design, location, number of patients, disease, types of spinal surgery, fusion segment, mean age, sex, and treatments. The outcome data included fusion rate, ODI, BMD, and overall adverse event. Fusion rate and overall adverse event rate were binary data, while the other two results were usually continuous data. Events were extracted for binary outcomes, and mean with standard deviation (SD) for continuous outcomes. When the original reports performed only standard error (SE), SD was estimated using the statistical formula SE = SD/√N.
According to the relevant information on details of trial design, two research members assessed the quality of each eligible study. About quality assessment of randomized clinical trials, selection bias, performance bias, we assessed detection bias, and attrition bias according to the Cochrane Risk of Bias Tool [14]. Relevant information for quality assessment involved evaluating randomization generation, allocation concealment, blinding (including healthcare providers, participants, and assessors), follow-up duration, loss to follow-up, and analysis type. On the other hand, we used the Newcastle-Ottawa Scale for non-randomized prospective comparative studies [15]. In case of disagreement on quality assessment, another research member would perform the third review and made the final judgement.
Evidence synthesis and statistical analysis
This study synthesized evidence in both qualitative and quantitative approach. The quantitative approach applied contrast-based network meta-analysis. Fusion rate and adverse event are binary data and hence synthesized in risk ratio (RR). On the other hand, ODI are continuous data and therefore pooled in weighted mean difference (WMD). Network meta-analysis was conducted using the random-effects model in view of conceptual heterogeneity among eligible evidence. We reported not only effect size (RR or WMD) but also 95% confidence interval (CI). To clarify the effects of teriparatide, bisphosphonate, combination of teriparatide and denosumab, and placebo, the network meta-analysis also performed surface under the cumulative ranking (SUCRA). This statistical method estimates the probability of each group among the most effective groups and shows group ranking of probability. Inconsistency and small study effect in consistency models of fusion rate, ODI, and adverse event rate were also examined, with inconsistency in each result detected using Lu-Ades’ loop inconsistency test and small study effects investigated using adjusted funnel plot and Egger’s regression intercept. Statistical significance was judged according to the common threshold (p < 0.05). All quantitative syntheses we mentioned above were completed using STATA version 14 for Microsoft Windows.
Results
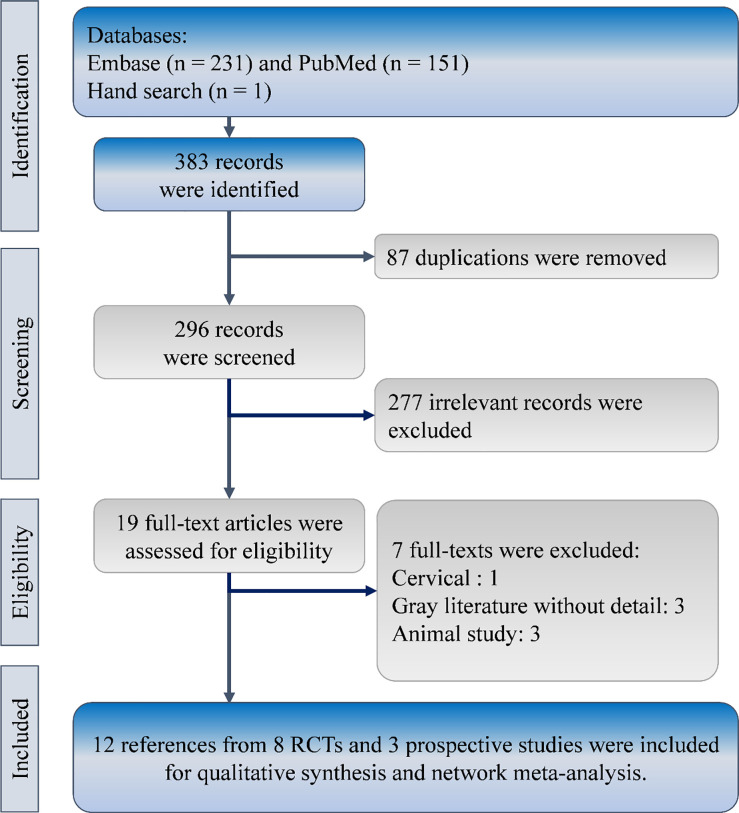
The developed search strategy obtained 382 references from the EMBASE (n = 231) and PubMed (n = 151), and one reference through reviewing relevant reference lists. After removing 87 duplications from the 383 references, titles and abstracts of the remaining 296 references were reviewed for eligibility. Then, 12 references from three prospective comparative studies and eight randomized clinical trials were eligible for the comprehensive synthesis (Fig 1) [16–27].
Fig 1. Flow diagram of study selection.
RCT, randomized clinical trial.
Characteristics of eligibility trials
The abovementioned 11 studies involved 676 patients receiving spinal surgery in China [16, 21, 25], Denmark [20], Japan [18, 19, 22–24, 26, 27], and Korea [17]. These patients were treated with placebo, teriparatide, combination of teriparatide and denosumab, and bisphosphonate. Mean age of patients in each study ranged from 60.7 to 78 years, and there were only 82 males (12.13%) in all these studies. Other details on study design, study location, surgical indication, and follow-up duration are shown in Table 1. S2 File in S1 Appendix displays quality of the studies.
Table 1. Characteristics of the included studies.
| Author | Location | Study Design | Surgical indication | Group | Patient number | Age Mean (SD) | Sex (M/F) | Follow up duration |
|---|---|---|---|---|---|---|---|---|
| Jespersen 2019 | Denmark | RCT | Spondylolisthesis | Teriparatide | 41 | 71(1.01) | 11/30 | 12 months |
| Placebo | 46 | 70(0.88) | 7/39 | |||||
| Sheng 2018 | China | RCT | Spondylolisthesis HIVD, Spinal stenosis | Zoledronic acid | 28 | 60.7(6.2) | 7/21 | 12 months |
| null | 28 | 63.1(4.9) | 10/18 | |||||
| Ide 2018 | Japan | RCT | Spinal stenosis | Teriparatide + denosumab | 8 | 73.2(2.7) | 3/5 | 12 months |
| Teriparatide | 8 | 75.0(2.4) | 0/8 | |||||
| Seki 2017 | Japan | Prospective | Vertebral fracture | Teriparatide | 33 | 72.5(5) | 0/33 | 24 months |
| Alendronate/ risedronate | 25 | 71.5(2) | 0/25 | |||||
| Ebata 2017 | Japan | RCT | Lumbar degenerative disease | Teriparatide | 36 | 72.6(7) | 0/36 | 6 months |
| null | 38 | 70.4(8) | 0/38 | |||||
| Cho 2017 | Korea | Prospective | Spinal stenosis, spondylolisthesis | Teriparatide | 23 | 71.0(4.9) | 0/23 | 24 months |
| Alendronate | 24 | 68.2(8.4) | 0/24 | |||||
| Yagi 2016 | Japan | Prospective | Posterior long instrumented fusion | Teriparatide | 43 | 68.6(6.9) | 0/43 | 24 months |
| null | 33 | 66.7(6.9) | 0/33 | |||||
| Chen 2016 | China | RCT | Spondylolisthesis | zoledronic acid | 33 | 65(8) | 6/27 | 12 months |
| Saline | 36 | 63(7) | 7/29 | |||||
| Ohtori 2013 | Japan | RCT | Spondylolisthesis with spinal stenosis | Teriparatide | 20 | 78(6.0) | 0/20 | 12 months |
| Risedronate | 20 | 75(5.0) | 0/20 | |||||
| Control | 22 | 77(5.8) | 0/22 | |||||
| Li 2012 | China | RCT | Non-specific | Zoledronic acid | 28 | 63.63(6.36) | 13/28 | 12 months |
| Saline | 25 | 63.83(5.7) | 16/25 | |||||
| Nagahama 2011 | Japan | RCT | Spondylolisthesis and spinal stenosis | Alendronate | 19 | 70.3(8.6) | 1/18 | 12 months |
| null | 17 | 67.4(7.6) | 1/16 |
HIVD, herniated intervertebral disc; RCT, randomized clinical trial.
Fusion rate
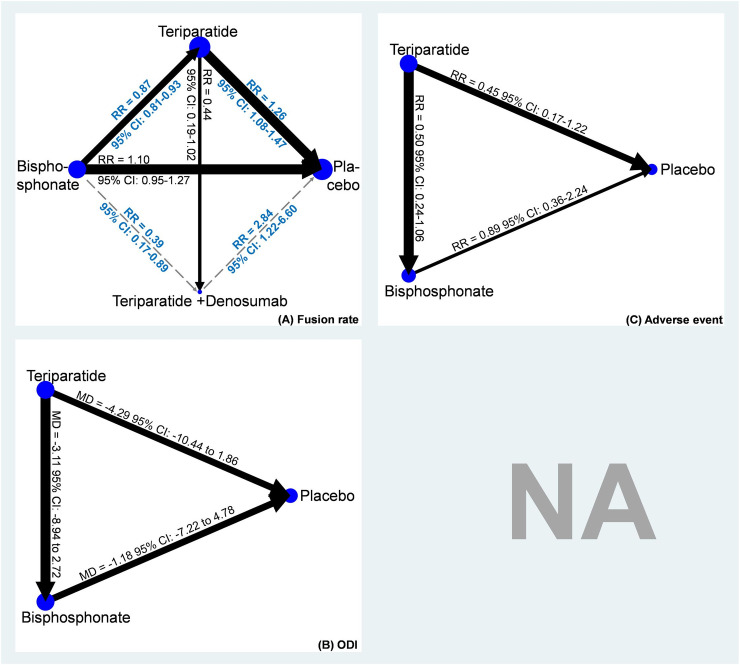
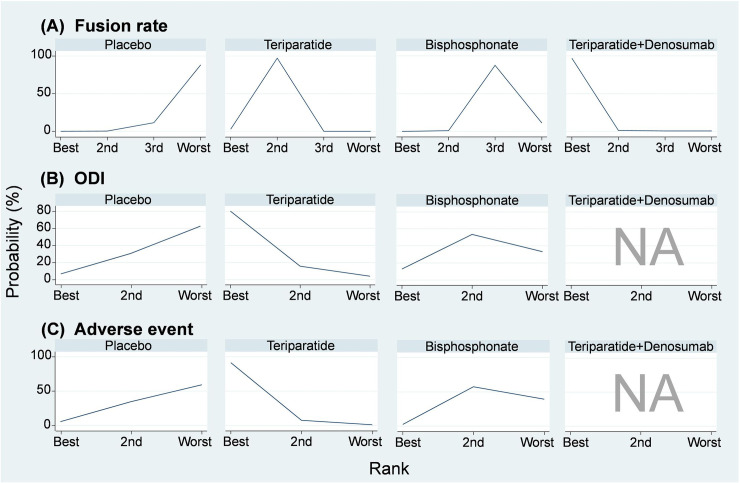
A total of nine studies using placebo, teriparatide, combination of teriparatide and denosumab, and bisphosphonate were included in the network meta-analysis of fusion rate (Fig 2A and S3 File in S1 Appendix) [16–22, 24, 25]. Results showed that compared with placebo, teriparatide (RR, 1.26, 95% CI: 1.08 to 1.47) and combination of teriparatide and denosumab (RR, 2.84, 95% CI: 1.22 to 6.60) achieved significantly higher fusion rate, but not bisphosphonate (RR, 1.10, 95% CI: 0.95 to 1.27). SUCRA demonstrated similar trends favoring combination of teriparatide and denosumab (Mean rank = 1; SUCRA = 98.4; Fig 3A and S4 File in S1 Appendix). In view of the closed loop formed by placebo, teriparatide, and bisphosphonate in the network meta-analysis of fusion rate, the loop inconsistency test was performed. The test did not detect inconsistency in the pooled fusion rate within the network model (Chi-square = 0.62, p = 0.43; S5 File in S1 Appendix). Moreover, Egger’s test did not detect serious small study effects (t = -0.66, 95% CI: -1.433 to 0.809, p = .531; S6 File in S1 Appendix).
Fig 2.
Network plots of (A) fusion rate, (B) Oswestry Disability Index (ODI), and (C) adverse event.
Fig 3.
Probability rank of (A) fusion rate, (B) Oswestry Disability Index (ODI), and (C) adverse event.
Oswestry disability index
Five studies reported data on ODI among teriparatide, bisphosphonate, and placebo (Fig 2B) [19, 22–25]. According to the available data, the network meta-analysis of ODI showed no significant differences among teriparatide, bisphosphonate, and placebo (S7 File in S1 Appendix). However, SUCRA indicated that teriparatide (Mean rank = 1.2; SUCRA = 88.2) may be a better treatment than bisphosphonate (Mean rank = 2.2; SUCRA = 39.8) and placebo (Mean rank = 2.6; SUCRA = 22.0; Fig 3B; S8 File in S1 Appendix). The loop inconsistency test for the network meta-analysis of ODI showed insignificance (chi-square = 2.22, p = 0.136; S9 File in S1 Appendix), and the Egger’s test did not detect small study effects in this consistency model (t = 1.22, 95% CI: -2.36 to 6.65, p = .276; S10 File in S1 Appendix).
Adverse event
Four of the eligible studies presented adverse event data on teriparatide, bisphosphonate, and placebo (Fig 2C) [17, 20, 23, 24]. The network meta-analysis of overall adverse event rate also showed insignificant differences among teriparatide, bisphosphonate, and placebo (S11 File in S1 Appendix). However, SUCRA still indicated that teriparatide (Mean rank = 1.1; SUCRA = 95.0) may be a better treatment than bisphosphonate (Mean rank = 2.4; SUCRA = 31.8) and placebo (Mean rank = 2.5; SUCRA = 23.2; Fig 3C; S12 File in S1 Appendix). The loop inconsistency test for the network meta-analysis of overall adverse event rate showed insignificance (chi-square = 0.06, p < .812; S13 File in S1 Appendix), and the Egger’s test also detected no small study effects (t = -0.30, 95% CI: -2.85 to 2.29, p = .779; S14 File in S1 Appendix).
Discussion
This study demonstrated higher fusion rate for the teriparatide group compared with the bisphosphonate and control groups. A trend of better clinical outcome and fewer adverse events were also observed in the teriparatide group, though the difference did not reach statistical significance.
Teriparatide and bisphosphonate are commonly used anti-osteoporotic agents involving completely different mechanisms and having different impacts on bone metabolism. Teriparatide given intermittently increases bone anabolism and stimulates new bone formation [28, 29]. Bisphosphonate, on the contrary, is an anti-resorptive drug that suppresses the activity of osteoclast and increases bone mineral density [30, 31]. The present results of superior fusion rate achieved by teriparatide after spinal surgery compared with bisphosphonate can be explained by their different drug mechanisms. Although both drugs can increase the strength of vertebral body [32] and provide better support to the pedicle screws, only teriparatide can act on osteoblast and osteocyte to accelerate new bone formation. This anabolic effect may be the key that leads to unequal impact on intervertebral fusion mass formation, and can explain why the benefit of teriparatide was also observed among the non-osteoporotic population [20]. In previous studies, nonunion of fracture or arthrodesis has been treated using teriparatide with promising results [33–36]. Similar effect was observed in spinal fusion surgery.
Risk factor for pseudoarthrosis after spinal fusion included old age, large spondylolisthesis slip angle, infection, smoking and excessive motion at the fusion site [37–40]. In this study, fusion levels, fusion methods, fusion devices, graft selection, surgical indications and surgical methods all show heterogeneity which would influence fusion rate. Cervical spine surgery is not included in the analysis due to fundamental difference in anatomy, surgical approach, endplate area and implant design in cervical spine, which should be discussed separately. Regarding diagnostic tools, there are different imaging modalities and grading systems for evaluating pseudoarthrosis [40, 41]. Currently, computed tomography and plain radiographies are most commonly used, but there are other tools including bone scan and positron emission tomography [40, 41]. The present review adopted stricter criteria for fusion; hence, “partial union” or “incomplete union” in the articles are not taken as solid fusion. Despite the abovementioned heterogeneous factors, all results had I-square values less than 50%, representing acceptable heterogeneity.
There is still no consensus toward the dose of teriparatide and duration of use for stimulating spinal fusion. Most studies adhered to the dose of subcutaneous 20 μg daily for osteoporotic treatment [17, 19, 23, 24, 27]. However, the same dose given weekly in the study of Ebata et al. also achieved outcome superior to that of the control group [18]. A previous study combined denosumab, an antibody of receptor activator of nuclear factor kappa-B ligand (RANKL), with teriparatide and demonstrated better fusion rate. Although there are other works supporting the combined use of denosumab and teriparatide for the treatment of osteoporosis [42], clinical evidence is insufficient because only one single study used such regiment. There is insignificant difference in ODI among the three groups despite of variations in fusion rate. This is compatible with previous study that radiographic union is not associated with better short-term clinical result [43]. However, in the long run, solid union still guarantees better functional outcome [8].
This study is the first network meta-analysis that discussed the use of teriparatide and bisphosphonate after spinal fusion surgery. There are some other systemic reviews focusing on the same issue. Frestes et al. reported insignificant difference in fusion rate between bisphosphonate and control group but bisphosphonate could reduce cage subsidence and vertebral fracture [12]. On the contrary, meta-analysis of Liu et al. suggested that bisphosphonate may improve fusion rate [44], and the discrepancy may be due to inclusion of retrospective studies by Liu et al. A recent meta-analysis comparing teriparatide, bisphosphate and control simultaneously concluded that teriparatide achieved better fusion rate than bisphosphonate and control, while there is no difference between bisphosphonate and control [13]. However, retrospective studies were also included and network meta-analysis was not performed. Moreover, three new studies by Sheng, Ide et al. and Jespersen et al. were not included [19, 20, 25]. The present analysis demonstrated similar results that teriparatide was better than bisphosphonate and control on the basis of latest and higher quality evidences.
Limitations
The study is limited by variations in follow-up duration and small number of included studies. Even without inconsistency and concerned heterogeneity detected, the evidence obtained may be not of high quality due to the mixed sample of randomized clinical trials and prospective comparative studies. Moreover, the consistency model of fusion rate used was an incomplete network meta-analysis. There was only one trial implementing combination of teriparatide and denosumab, and the estimates of the combination treatment relied only on this single trial. No randomized clinical trial or prospective comparative study comparing the combination therapy and bisphosphonate was found. To confirm the efficacy of teriparatide and bisphosphonate after spinal fusion, more well-designed randomized clinical trials on this topic with multiple arms should be examined. No recommendation on the dose of peri-operative teriparatide and duration of use can be given. Such would merit further exploration.
Conclusion
This is the very first network meta-analysis provides an overview of the use of teriparatide and bisphosphonate for spinal fusion surgery. Teriparatide treatments for spinal fusion surgery can significantly improve fusion rate while bisphosphonate cannot. Teriparatide tends to improve clinical symptoms or decrease adverse events, but the differences do not reach statistical significance. Combined use of denosumab and teriparatide may result in better fusion rate compared with using teriparatide alone, yet more evidence is necessary to support this combination therapy.
Supporting information
(DOC)
(PDF)
Abbreviations
- CI
confidence interval
- BMD
bone mineral density
- MD
mean difference
- ODI
Oswestry disability index
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT
randomized clinical trial
- RR
risk ratio
- SD
standard deviation
- SE
standard error
- SUCRA
surface under the cumulative ranking
Data Availability
The data underlying the results presented in the study are available from relevant studies: 1. Chen F, Dai Z, Kang Y, Lv G, Keller ET, Jiang Y. Effects of zoledronic acid on bone fusion in osteoporotic patients after lumbar fusion. Osteoporosis International. 2016;27(4):1469-76. doi: 10.1007/s00198-015-3398-1. 2. Cho PG, Ji GY, Shin DA, Ha Y, Yoon DH, Kim KN. An effect comparison of teriparatide and bisphosphonate on posterior lumbar interbody fusion in patients with osteoporosis: a prospective cohort study and preliminary data. European Spine Journal. 2017;26(3):691-7. doi: 10.1007/s00586-015-4342-y. PubMed Central PMCID: PMCLilly(United States). 3. Ebata S, Takahashi J, Hasegawa T, Mukaiyama K, Isogai Y, Ohba T, et al. Role of weekly teriparatide administration in osseous union enhancement within six months after posterior or transforaminal lumbar interbody fusion for osteoporosis-associated lumbar degenerative disorders: A multicenter, prospective randomized study. Journal of Bone and Joint Surgery - American Volume. 2017;99(5):365-72. doi: 10.2106/JBJS.16.00230. 4. Ide M, Yamada K, Kaneko K, Sekiya T, Kanai K, Higashi T, et al. Combined teriparatide and denosumab therapy accelerates spinal fusion following posterior lumbar interbody fusion. Orthopaedics and Traumatology: Surgery and Research. 2018;104(7):1043-8. doi: 10.1016/j.otsr.2018.07.015. 5. Jespersen AB, Andresen ADK, Jacobsen MK, Andersen MO, Carreon LY. Does Systemic Administration of Parathyroid Hormone After Noninstrumented Spinal Fusion Surgery Improve Fusion Rates and Fusion Mass in Elderly Patients Compared to Placebo in Patients With Degenerative Lumbar Spondylolisthesis? Spine (Phila Pa 1976). 2019;44(3):157-62. Epub 2018/07/14. doi: 10.1097/brs.0000000000002791. PubMed PMID: 30005049. 6. Li C, Wang HR, Li XL, Zhou XG, Dong J. The relation between zoledronic acid infusion and interbody fusion in patients undergoing transforaminal lumbar interbody fusion surgery. Acta Neurochirurgica. 2012;154(4):731-8. doi: 10.1007/s00701-012-1283-7. 7. Nagahama K, Kanayama M, Togawa D, Hashimoto T, Minami A. Does alendronate disturb the healing process of posterior lumbar interbody fusion? A prospective randomized trial. Journal of Neurosurgery: Spine. 2011;14(4):500-7. doi: 10.3171/2010.11.SPINE10245. 8. Ohtori S, Inoue G, Orita S, Yamauchi K, Eguchi Y, Ochiai N, et al. Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine. 2013;38(8):E487-E92. doi: 10.1097/BRS.0b013e31828826dd. PubMed Central PMCID: PMCEisai(Japan) Lilly(Japan). 9. Seki S, Hirano N, Kawaguchi Y, Nakano M, Yasuda T, Suzuki K, et al. Teriparatide versus low-dose bisphosphonates before and after surgery for adult spinal deformity in female Japanese patients with osteoporosis. European Spine Journal. 2017;26(8):2121-7. doi: 10.1007/s00586-017-4959-0. 10. Sheng J, Liu D, Zheng W, Zhou JJ, Wu HH, Xu W, et al. Zoledronic acid combined with bone cement augmented pedicle screw for osteoporotic lumbar fusion. Medical Journal of Chinese People's Liberation Army. 2018;43(12):1044-8. doi: 10.11855/j.issn.0577-7402.2018.12.09. 11. Ushirozako H, Hasegawa T, Ebata S, Oba H, Ohba T, Mukaiyama K, et al. Weekly Teriparatide Administration and Preoperative Anterior Slippage of the Cranial Vertebra Next to Fusion Segment < 2 mm Promote Osseous Union After Posterior Lumbar Interbody Fusion. Spine. 2019;44(5):E288-E97. doi: 10.1097/BRS.0000000000002833. 12. Yagi M, Ohne H, Konomi T, Fujiyoshi K, Kaneko S, Komiyama T, et al. Teriparatide improves volumetric bone mineral density and fine bone structure in the UIV+1 vertebra, and reduces bone failure type PJK after surgery for adult spinal deformity. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2016;27(12):3495-502. Epub 2016/06/28. doi: 10.1007/s00198-016-3676-6. PubMed PMID: 27341809.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS. Trends in Lumbar Fusion Procedure Rates and Associated Hospital Costs for Degenerative Spinal Diseases in the United States, 2004 to 2015. Spine (Phila Pa 1976). 2019;44(5):369–76. Epub 2018/08/04. 10.1097/BRS.0000000000002822 . [DOI] [PubMed] [Google Scholar]
- 2.Gray DT, Deyo RA, Kreuter W, Mirza SK, Heagerty PJ, Comstock BA, et al. Population-based trends in volumes and rates of ambulatory lumbar spine surgery. Spine (Phila Pa 1976). 2006;31(17):1957–63; discussion 64. Epub 2006/08/23. 10.1097/01.brs.0000229148.63418.c1 . [DOI] [PubMed] [Google Scholar]
- 3.Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS, 3rd, Cook SD. Effects of bone mineral density on pedicle screw fixation. Spine (Phila Pa 1976). 1994;19(21):2415–20. Epub 1994/11/01. 10.1097/00007632-199411000-00008 . [DOI] [PubMed] [Google Scholar]
- 4.Chin DK, Park JY, Yoon YS, Kuh SU, Jin BH, Kim KS, et al. Prevalence of osteoporosis in patients requiring spine surgery: incidence and significance of osteoporosis in spine disease. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2007;18(9):1219–24. Epub 2007/03/28. 10.1007/s00198-007-0370-8 . [DOI] [PubMed] [Google Scholar]
- 5.Bjerke BT, Zarrabian M, Aleem IS, Fogelson JL, Currier BL, Freedman BA, et al. Incidence of Osteoporosis-Related Complications Following Posterior Lumbar Fusion. Global Spine J. 2018;8(6):563–9. Epub 2018/09/12. 10.1177/2192568217743727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zdeblick TA. A prospective, randomized study of lumbar fusion. Preliminary results. Spine (Phila Pa 1976). 1993;18(8):983–91. Epub 1993/06/15. 10.1097/00007632-199306150-00006 . [DOI] [PubMed] [Google Scholar]
- 7.Madan SS, Boeree NR. Comparison of instrumented anterior interbody fusion with instrumented circumferential lumbar fusion. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2003;12(6):567–75. Epub 2003/12/16. 10.1007/s00586-002-0516-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bjarke Christensen F, Stender Hansen E, Laursen M, Thomsen K, Bunger CE. Long-term functional outcome of pedicle screw instrumentation as a support for posterolateral spinal fusion: randomized clinical study with a 5-year follow-up. Spine (Phila Pa 1976). 2002;27(12):1269–77. Epub 2002/06/18. 10.1097/00007632-200206150-00006 . [DOI] [PubMed] [Google Scholar]
- 9.McCoy S, Tundo F, Chidambaram S, Baaj AA. Clinical considerations for spinal surgery in the osteoporotic patient: A comprehensive review. Clin Neurol Neurosurg. 2019;180:40–7. Epub 2019/03/29. 10.1016/j.clineuro.2019.03.010 . [DOI] [PubMed] [Google Scholar]
- 10.Hodsman AB, Bauer DC, Dempster DW, Dian L, Hanley DA, Harris ST, et al. Parathyroid hormone and teriparatide for the treatment of osteoporosis: a review of the evidence and suggested guidelines for its use. Endocr Rev. 2005;26(5):688–703. Epub 2005/03/17. 10.1210/er.2004-0006 . [DOI] [PubMed] [Google Scholar]
- 11.Drake MT, Clarke BL, Khosla S. Bisphosphonates: mechanism of action and role in clinical practice. Mayo Clin Proc. 2008;83(9):1032–45. Epub 2008/09/09. 10.4065/83.9.1032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fretes N, Vellios E, Sharma A, Ajiboye RM. Radiographic and functional outcomes of bisphosphonate use in lumbar fusion: a systematic review and meta-analysis of comparative studies. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2019. Epub 2019/08/07. 10.1007/s00586-019-06090-2 . [DOI] [PubMed] [Google Scholar]
- 13.Buerba RA, Sharma A, Ziino C, Arzeno A, Ajiboye RM. Bisphosphonate and Teriparatide Use in Thoracolumbar Spinal Fusion: A Systematic Review and Meta-analysis of Comparative Studies. Spine (Phila Pa 1976). 2018;43(17):E1014–E23. Epub 2018/02/21. 10.1097/BRS.0000000000002608 . [DOI] [PubMed] [Google Scholar]
- 14.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stang AJEjoe. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. 2010;25(9):603–5. [DOI] [PubMed] [Google Scholar]
- 16.Chen F, Dai Z, Kang Y, Lv G, Keller ET, Jiang Y. Effects of zoledronic acid on bone fusion in osteoporotic patients after lumbar fusion. Osteoporosis International. 2016;27(4):1469–76. 10.1007/s00198-015-3398-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cho PG, Ji GY, Shin DA, Ha Y, Yoon DH, Kim KN. An effect comparison of teriparatide and bisphosphonate on posterior lumbar interbody fusion in patients with osteoporosis: a prospective cohort study and preliminary data. European Spine Journal. 2017;26(3):691–7. 10.1007/s00586-015-4342-y PubMed Central PMCID: PMCLilly(United States). [DOI] [PubMed] [Google Scholar]
- 18.Ebata S, Takahashi J, Hasegawa T, Mukaiyama K, Isogai Y, Ohba T, et al. Role of weekly teriparatide administration in osseous union enhancement within six months after posterior or transforaminal lumbar interbody fusion for osteoporosis-associated lumbar degenerative disorders: A multicenter, prospective randomized study. Journal of Bone and Joint Surgery—American Volume. 2017;99(5):365–72. 10.2106/JBJS.16.00230 [DOI] [PubMed] [Google Scholar]
- 19.Ide M, Yamada K, Kaneko K, Sekiya T, Kanai K, Higashi T, et al. Combined teriparatide and denosumab therapy accelerates spinal fusion following posterior lumbar interbody fusion. Orthopaedics and Traumatology: Surgery and Research. 2018;104(7):1043–8. 10.1016/j.otsr.2018.07.015 [DOI] [PubMed] [Google Scholar]
- 20.Jespersen AB, Andresen ADK, Jacobsen MK, Andersen MO, Carreon LY. Does Systemic Administration of Parathyroid Hormone After Noninstrumented Spinal Fusion Surgery Improve Fusion Rates and Fusion Mass in Elderly Patients Compared to Placebo in Patients With Degenerative Lumbar Spondylolisthesis? Spine (Phila Pa 1976). 2019;44(3):157–62. Epub 2018/07/14. 10.1097/brs.0000000000002791 . [DOI] [PubMed] [Google Scholar]
- 21.Li C, Wang HR, Li XL, Zhou XG, Dong J. The relation between zoledronic acid infusion and interbody fusion in patients undergoing transforaminal lumbar interbody fusion surgery. Acta Neurochirurgica. 2012;154(4):731–8. 10.1007/s00701-012-1283-7 [DOI] [PubMed] [Google Scholar]
- 22.Nagahama K, Kanayama M, Togawa D, Hashimoto T, Minami A. Does alendronate disturb the healing process of posterior lumbar interbody fusion? A prospective randomized trial. Journal of Neurosurgery: Spine. 2011;14(4):500–7. 10.3171/2010.11.SPINE10245 [DOI] [PubMed] [Google Scholar]
- 23.Ohtori S, Inoue G, Orita S, Yamauchi K, Eguchi Y, Ochiai N, et al. Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine. 2013;38(8):E487–E92. 10.1097/BRS.0b013e31828826dd PubMed Central PMCID: PMCEisai(Japan) Lilly(Japan). [DOI] [PubMed] [Google Scholar]
- 24.Seki S, Hirano N, Kawaguchi Y, Nakano M, Yasuda T, Suzuki K, et al. Teriparatide versus low-dose bisphosphonates before and after surgery for adult spinal deformity in female Japanese patients with osteoporosis. European Spine Journal. 2017;26(8):2121–7. 10.1007/s00586-017-4959-0 [DOI] [PubMed] [Google Scholar]
- 25.Sheng J, Liu D, Zheng W, Zhou JJ, Wu HH, Xu W, et al. Zoledronic acid combined with bone cement augmented pedicle screw for osteoporotic lumbar fusion. Medical Journal of Chinese People's Liberation Army. 2018;43(12):1044–8. 10.11855/j.issn.0577-7402.2018.12.09 [DOI] [Google Scholar]
- 26.Ushirozako H, Hasegawa T, Ebata S, Oba H, Ohba T, Mukaiyama K, et al. Weekly Teriparatide Administration and Preoperative Anterior Slippage of the Cranial Vertebra Next to Fusion Segment < 2 mm Promote Osseous Union After Posterior Lumbar Interbody Fusion. Spine. 2019;44(5):E288–E97. 10.1097/BRS.0000000000002833 [DOI] [PubMed] [Google Scholar]
- 27.Yagi M, Ohne H, Konomi T, Fujiyoshi K, Kaneko S, Komiyama T, et al. Teriparatide improves volumetric bone mineral density and fine bone structure in the UIV+1 vertebra, and reduces bone failure type PJK after surgery for adult spinal deformity. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2016;27(12):3495–502. Epub 2016/06/28. 10.1007/s00198-016-3676-6 . [DOI] [PubMed] [Google Scholar]
- 28.Greenspan SL, Bone HG, Ettinger MP, Hanley DA, Lindsay R, Zanchetta JR, et al. Effect of recombinant human parathyroid hormone (1–84) on vertebral fracture and bone mineral density in postmenopausal women with osteoporosis: a randomized trial. Ann Intern Med. 2007;146(5):326–39. Epub 2007/03/07. 10.7326/0003-4819-146-5-200703060-00005 . [DOI] [PubMed] [Google Scholar]
- 29.Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, et al. Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344(19):1434–41. Epub 2001/05/11. 10.1056/NEJM200105103441904 . [DOI] [PubMed] [Google Scholar]
- 30.Riggs BL, Parfitt AM. Drugs used to treat osteoporosis: the critical need for a uniform nomenclature based on their action on bone remodeling. Journal of bone and mineral research: the official journal of the American Society for Bone and Mineral Research. 2005;20(2):177–84. Epub 2005/01/14. 10.1359/JBMR.041114 . [DOI] [PubMed] [Google Scholar]
- 31.Orwoll E, Ettinger M, Weiss S, Miller P, Kendler D, Graham J, et al. Alendronate for the treatment of osteoporosis in men. N Engl J Med. 2000;343(9):604–10. Epub 2000/09/09. 10.1056/NEJM200008313430902 . [DOI] [PubMed] [Google Scholar]
- 32.Boivin GY, Chavassieux PM, Santora AC, Yates J, Meunier PJ. Alendronate increases bone strength by increasing the mean degree of mineralization of bone tissue in osteoporotic women. Bone. 2000;27(5):687–94. Epub 2000/11/04. 10.1016/s8756-3282(00)00376-8 . [DOI] [PubMed] [Google Scholar]
- 33.Oteo-Alvaro A, Moreno E. Atrophic humeral shaft nonunion treated with teriparatide (rh PTH 1–34): a case report. J Shoulder Elbow Surg. 2010;19(7):e22–8. Epub 2010/09/18. 10.1016/j.jse.2010.05.005 . [DOI] [PubMed] [Google Scholar]
- 34.Tamai K, Takamatsu K, Kazuki K. Successful treatment of nonunion with teriparatide after failed ankle arthrodesis for Charcot arthropathy. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2013;24(10):2729–32. Epub 2013/05/08. 10.1007/s00198-013-2367-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee YK, Ha YC, Koo KH. Teriparatide, a nonsurgical solution for femoral nonunion? A report of three cases. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2012;23(12):2897–900. Epub 2012/10/19. 10.1016/0006-2944(75)90084-8 . [DOI] [PubMed] [Google Scholar]
- 36.Pietrogrande L, Raimondo E. Teriparatide in the treatment of non-unions: scientific and clinical evidences. Injury. 2013;44 Suppl 1:S54–7. Epub 2013/02/13. 10.1016/S0020-1383(13)70013-5 . [DOI] [PubMed] [Google Scholar]
- 37.Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976). 2006;31(20):2329–36. Epub 2006/09/21. 10.1097/01.brs.0000238968.82799.d9 . [DOI] [PubMed] [Google Scholar]
- 38.Berman D, Oren JH, Bendo J, Spivak J. The Effect of Smoking on Spinal Fusion. Int J Spine Surg. 2017;11:29 Epub 2018/01/27. 10.14444/4029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Suda K, Ito M, Abumi K, Haba H, Taneichi H, Kaneda K. Radiological risk factors of pseudoarthrosis and/or instrument breakage after PLF with the pedicle screw system in isthmic spondylolisthesis. Journal of spinal disorders & techniques. 2006;19(8):541–6. Epub 2006/12/06. 10.1097/01.bsd.0000211226.97178.b9 . [DOI] [PubMed] [Google Scholar]
- 40.Raizman NM, O'Brien JR, Poehling-Monaghan KL, Yu WD. Pseudarthrosis of the spine. J Am Acad Orthop Surg. 2009;17(8):494–503. Epub 2009/08/05. 10.5435/00124635-200908000-00003 . [DOI] [PubMed] [Google Scholar]
- 41.Chun DS, Baker KC, Hsu WK. Lumbar pseudarthrosis: a review of current diagnosis and treatment. Neurosurg Focus. 2015;39(4):E10 Epub 2015/10/02. 10.3171/2015.7.FOCUS15292 . [DOI] [PubMed] [Google Scholar]
- 42.Leder BZ, Tsai JN, Uihlein AV, Burnett-Bowie SA, Zhu Y, Foley K, et al. Two years of Denosumab and teriparatide administration in postmenopausal women with osteoporosis (The DATA Extension Study): a randomized controlled trial. The Journal of clinical endocrinology and metabolism. 2014;99(5):1694–700. Epub 2014/02/13. 10.1210/jc.2013-4440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tsutsumimoto T, Shimogata M, Yoshimura Y, Misawa H. Union versus nonunion after posterolateral lumbar fusion: a comparison of long-term surgical outcomes in patients with degenerative lumbar spondylolisthesis. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2008;17(8):1107–12. Epub 2008/06/10. 10.1007/s00586-008-0695-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu WB, Zhao WT, Shen P, Zhang FJ. The effects of bisphosphonates on osteoporotic patients after lumbar fusion: a meta-analysis. Drug Des Devel Ther. 2018;12:2233–40. Epub 2018/07/27. 10.2147/DDDT.S164548 [DOI] [PMC free article] [PubMed] [Google Scholar]