Abstract
There are a number of medications which can serve as catalysts for drug-induced immune thrombocytopenia (DIPT). A minimum of six different mechanisms have been put forward as the means by which drug-induced antibodies can encourage platelet destruction, thus emphasising the complexity of the pathogenesis of DITP. Acyclovir, has been widely used because of its highly potent prohibitive properties for infections caused by HSV and VZV. The common adverse effects of this drug are well known, the severe adverse reactions are mostly related to high dose intravenous administrations. The immune thrombocytopenia induced by acyclovir is unusual. The authors present a rare clinical case of acyclovir-induced immune thrombocytopenia in a 72-year-old female patient with typical herpes zoster treated with acyclovir. The clinical and laboratory findings, taken together with the transitory relationship between acycolvir and the start of thrombocytopenia, combined with the elimination of the other know sources of thrombocytopenia, allowed us to reach the diagnosis of acyclovir-induced immune thrombocytopenia. An international database search was employed to complete an extensive review of the current literature. Contemporary information on acyclovir-induced immune thrombocytopenia was collected by the analysis of present day review articles and accessible case reports. The authors found five published cases of acyclovir-induced immune thrombocytopenia. Analyzing these articles it was concluded that immune thrombocytopenia induced by acyclovir is rare, and an unusual side effect, with good prognosis. Prompt diagnosis is vital to appropriate management, therefore clinicians need to be cognisant of this rare potential adverse reaction.
Keywords: acyclovir, herpes zoster, thrombocytopenia, drug induced, adverse reactions
Introduction
There are a number of medications which can serve as catalysts for drug-induced immune thrombocytopenia (DIPT) (1-3). The majority of DITP cases result in mild symptoms, but there have been documented instances of dangerous bleeding. A minimum of six different mechanisms have been put forward as the means by which drug-induced antibodies can encourage platelet destruction, thus emphasising the complexity of the pathogenesis of DITP. It is technically possible to identify the antibodies that react with platelets when they come in contact with the sensitising drug, but due to the complexity of the testing and the rarity of the necessary equipment and expertise, this is often not practical. Rather, in the vast majority of cases the decision to halt the suspected medication of subjects who experience DITP is better made on clinical grounds (4). Acyclovir, an acyclic purine nucleoside analogue, has been widely used because of its highly potent prohibitive properties for infections caused by HSV and VZV (5). Nausea, diarrhea, dizziness, headaches, and mental changes are the most common and well-known side effects of this drug. Severe adverse effects such as neurotoxicity, kidney disorders and psychiatric effects are not common, mostly related to high dose intravenous administrations (6-8). Immune thrombocytopenia induced by acyclovir is unusual.
Case report
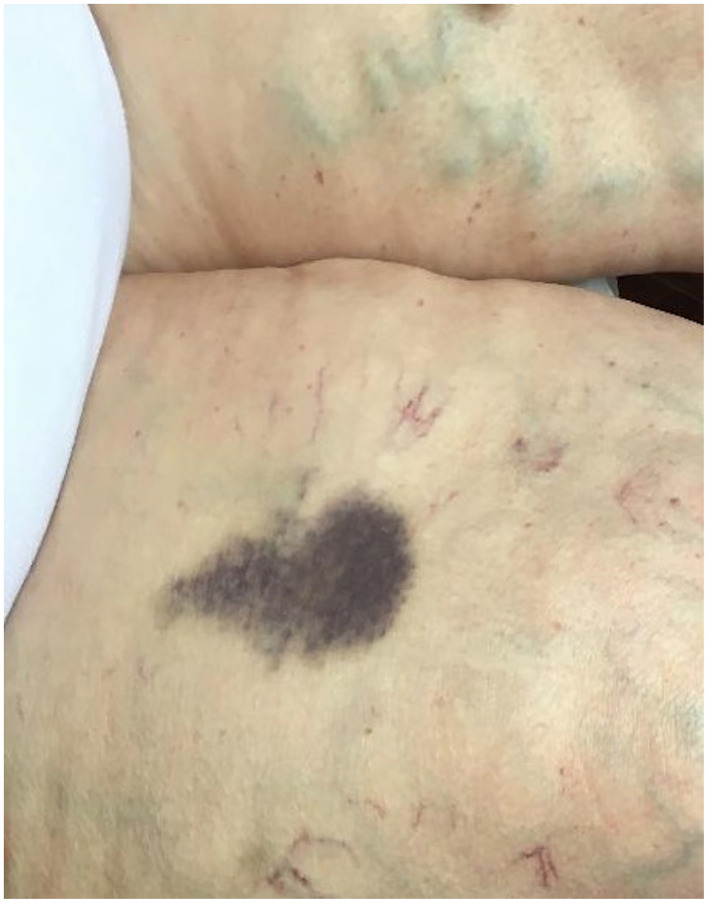
A 72-year-old woman was admitted to the Dermatology Clinic with a moderate clinical form of herpes zoster located on left thorax area. She was treated with acyclovir in an oral dose of 800 mg five times per day for a proposed period of 10 days with local treatment. On the seventh day of the treatment the patient presented two round ovalar hematomas. One with 10-cm diameters located on the left cubital area and another with 7-cm diameter situated on the right femoral area (Figs. 1 and 2). The patient denied any local trauma to these areas. She also denied fever, hematochezia, melena, hemoptysis, hematuria, or any neurologic symptoms. There was no history of smoking, systemic diseases, or drug allergy. The family and social history, were unremarkable. No other drugs were taken before and during the treatment of the herpes zoster virus infection. Laboratory tests: The performed laboratory tests on the day of presentation showed normal limits for hemoglobin, white blood cells and the platelet count was 15x109/l. Also the liver function, electrolyte profile, renal function and coagulation studies were in normal limits.
Figure 1.

Clinical aspect. Hematoma on the left cubital area.
Figure 2.
Clinical aspect. Hematoma on the right femoral area.
New laboratory tests were performed at the time of the appearance of the hematomas. The hematologic analysis showed normal limits except the platelet count which was lower at the value of 5x109/l. Tests for cytomegalovirus, hepatitis A, B and C viruses, and Epstein-Barr virus were performed and yielded negative results. The performed HIV test was also negative. The hematological consult excluded common known causes of thrombocytopenia. In order to prove a drug-induced immune thrombocytopenia, detection of acyclovir-dependent platelet antibodies was performed using enzyme-linked immunoassay (ELISA) which was positive. The clinical and laboratory findings, taken together with the transitory relationship between acyclovir and the start of thrombocytopenia, combined with the elimination of the other know sources of thrombocytopenia, allowed us to reach the diagnosis of acyclovir-induced immune thrombocytopenia. The administration of acyclovir was discontinued and oral prednisone treatment was introduced at 1 mg/kg body weight dose. The platelet count was checked every second day and began to rise 10 days after discontinuation of acyclovir and returned to normal values over a period of 15 days. After this period the dose of prednisone was decreased with 5 mg, every 3 days. The patient left the hospital clinically healed with normal levels of hematological laboratory findings including a normal platelet count level.
Discussion
Epidemiologic studies performed in the US and Europe suggest that ~10 persons per million are affected by DITP each year (9). The real incidence is unknown, but could be higher in elderly especially with associated severe co-morbidities and hospitalized persons, who are more likely to be exposed to different medications. The first report of DITP was published in 1865(10). Despite the low frequency, DITP is important to recognize because >200 drugs, including some herbal medicines, that have been reported to be causative (11). A minimum of six different mechanisms have been put forward as the means by which drug-induced antibodies can encourage platelet destruction, thus emphasising the complexity of the pathogenesis of DITP. The majority of DITPs are believed to have a drug-dependent immune mechanism as their source. How drugs induce platelet antibodies and how platelets are destroyed by these antibodies are still unclear (4). The clinical diagnosis of DITP is based on a few key features like: a) extensive petechiae, ecchymosis or hematomas appeared a few days after taking the putative drug, b) markedly low blood platelet levels appeared ~3-10 days after starting a putative medication, c) platelet counts return to normal at ~7 days after stopping the putative drug (usually in 1-10 days) and d) exclusion of common known causes of thrombocytopenia (12,13). In laboratory findings the presence of the specific drug-dependent platelet antibodies are crucial for the diagnosis. Also a careful, detailed personal and family history is important to patient evaluation. After examining methodologically and in detail the instances of drug-induced thrombocytopenia through 2008, George et al (14) constructed a database which catalogued the suspected drugs. The database is updated at regular intervals and can be accessed online at http://www.ouhsc.edu/platelets. They also devised a set of four clinical criteria and four levels of evidence to assess the likelihood that individual drugs are capable of causing DITP. In our case, the clinical aspect, the exclusion of other etiologies of thrombocytopenia, platelet count fluctuation, and the positive anti-platelet antibodies, and with the temporal relationship between the acyclovir and the start of thrombocytopenia allowed us to reach the diagnosis of acyclovir-induced immune thrombocytopenia. Based on the published clinical criteria we ranked the relationship between the drug and the disease on level 2 of evidence meeting three criteria of the four. The first step in the treatment is to discontinue medication in a patient with possible DITP. In many cases platelet levels start to increase without any medication. It is recommended as a common practice to administer corticosteroids, but whether they are beneficial in patients with DITP is not established. Other treatment options are mentioned in the literature i.e. platelet transfusion, intravenous IgG, or even plasma exchange with different results (15-17). Our patient was treated with oral corticosteroid with a good result. An international database search was employed to complete an extensive review of the current literature. Contemporary information on acyclovir-induced immune thrombocytopenia was further informed by the analysis of present day review articles and accessible case reports. Search of PubMed/MEDLINE, Google Scholar, and Web of Science databases found five published cases of acyclovir-induced immune thrombocytopenia (18-22). Acyclovir treatment was indicated for herpes simplex infection in three cases (18,20,22) and for zoster in two cases, similarly to our case (19,21). For the herpes simplex infections the treatment was oral, like in our case, in the other cases the administration of the drug was parenteral. All the cases were males aged between 20 and 81 years, except our presented case. The evolution in all the cases was similar, the clinical findings and the lower level of platelet count appeared after 4-8 days after starting the acyclovir treatment. In all the cases the specific drug-dependent platelet antibodies were done, with positive results. In all cases the treatment was stopped and different treatment options were used. Oral prednisone in one case, as in our case, intravenous IgG in one case, platelet mass transfusion in one case and in the others supportive treatment was used. In two cases the patients were without remarkable co-morbidities, similarly to our presented case (19,21). The other patients had severe co-morbidities such as systemic lupus, AIDS and chronic obstructive pulmonary disease, and were also treated for these diseases (18,20,22). In every case the evolution was good, platelet count levels became normal in 10-15 days (18-22). The immune thrombocytopenia induced by acyclovir is rare and an unusual side effect of a commonly used drug. Most DITPs are thought to be caused by, still unclear, drug-dependent immune mechanism. In elderly patients, and especially those with associated severe co-morbidities, who need to be treated with acyclovir, regular platelet count measurement should be considered. Prompt diagnosis is vital to appropriate management, therefore clinicians need to be cognisant of this rare potential adverse reaction (23,24).
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Authors' contributions
GLF was responsible for the clinical management of the patient, the evaluation and analysis of the data, and the writing of the manuscript. LF was involved in the conception of the study and was responsible for the preparation and revisions of the manuscript. RA, SLI, and MD were responsible for the literature research and the revisions of the manuscript. IB was involved in the conception of the study and contributed to the writing of the manuscript. The final version of the article was read and approved by all the authors.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Romanian College of Physicians of Mures County (Târgu Mureș, Romania).
Patient consent for publication
Written informed consent was obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
Authors' information
GLF: Associate Professor of Dermatology, Department of Dermatology, Dermatology Clinic, ‘George Emil Palade’ University of Medicine, Pharmacy, Science and Technology (Târgu Mureş, Romania).
References
- 1.Tatu AL, Elisei AM, Chioncel V, Miulescu M, Nwabudike LC. Immunologic adverse reactions of β-blockers and the skin (Review) Exp Ther Med. 2019;18:955–959. doi: 10.3892/etm.2019.7504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fekete GL, Fekete L. Cutaneous leukocytoclastic vasculitis associated with erlotinib treatment: A case report and review of the literature. Exp Ther Med. 2019;17:1128–1131. doi: 10.3892/etm.2018.6988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tatu AL, Ciobotaru OR, Miulescu M, Buzia OD, Elisei AM, Mardare N, Diaconu C, Robu S, Nwabudike LC. Hydrochlorothiazide: Chemical structure, therapeutic, phototoxic and carcinogenetic effects in dermatology. Rev Chim (Bucharest) 2018;69:2110–2114. [Google Scholar]
- 4.Aster RH, Curtis BR, McFarland JG, Bougie DW. Drug-induced immune thrombocytopenia: Pathogenesis, diagnosis, and management. J Thromb Haemost. 2009;7:911–918. doi: 10.1111/j.1538-7836.2009.03360.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dworkin RH, Johnson RW, Breuer J, Gnann JW, Levin MJ, Backonja M, Betts RF, Gershon AA, Haanpaa ML, McKendrick MW, et al. Recommendations for the management of herpes zoster. Clin Infect Dis. 2007;44 (Suppl 1):S1–S26. doi: 10.1086/510206. [DOI] [PubMed] [Google Scholar]
- 6.Busso M, Berman B. Antivirals in dermatology. J Am Acad Dermatol. 1995;32:1031–1040. doi: 10.1016/0190-9622(95)91344-0. [DOI] [PubMed] [Google Scholar]
- 7.Adair JC, Gold M, Bond RE. Acyclovir neurotoxicity: Clinical experience and review of the literature. South Med J. 1994;87:1227–1231. doi: 10.1097/00007611-199412000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Haefeli WE, Schoenenberger RA, Weiss P, Ritz RF. Acyclovir-induced neurotoxicity: Concentration - side effect relationship in acyclovir overdose. Am J Med. 1993;94:212–215. doi: 10.1016/0002-9343(93)90186-s. [DOI] [PubMed] [Google Scholar]
- 9.van den Bemt PM, Meyboom RH, Egberts AC. Drug-induced immune thrombocytopenia. Drug Saf. 2004;27:1243–1252. doi: 10.2165/00002018-200427150-00007. [DOI] [PubMed] [Google Scholar]
- 10.Vipan W. Quinine as a cause of purpura. Lancet. 1865;86(37) [Google Scholar]
- 11.Aster RH, Bougie DW. Drug-induced immune thrombocytopenia. N Engl J Med. 2007;357:580–587. doi: 10.1056/NEJMra066469. [DOI] [PubMed] [Google Scholar]
- 12.Chong BH. Drug-induced immune thrombocytopenia. Platelets. 1991;2:173–181. doi: 10.3109/09537109109005508. [DOI] [PubMed] [Google Scholar]
- 13.Visentin GP, Liu CY. Drug-induced thrombocytopenia. Hematol Oncol Clin North Am. 2007;21vi:685–696. doi: 10.1016/j.hoc.2007.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.George JN, Raskob GE, Shah SR, Rizvi MA, Hamilton SA, Osborne S, Vondracek T. Drug-induced thrombocytopenia: A systematic review of published case reports. Ann Intern Med. 1998;129:886–890. doi: 10.7326/0003-4819-129-11_part_1-199812010-00009. [DOI] [PubMed] [Google Scholar]
- 15.Crosby WH. Editorial: Wet purpura, dry purpura. JAMA. 1975;232:744–745. doi: 10.1001/jama.232.7.744. [DOI] [PubMed] [Google Scholar]
- 16.Ray JB, Brereton WF, Nullet FR. Intravenous immune globulin for the treatment of presumed quinidine-induced thrombocytopenia. DICP. 1990;24:693–695. doi: 10.1177/106002809002400706. [DOI] [PubMed] [Google Scholar]
- 17.Pourrat O. Treatment of drug-related diseases by plasma exchanges. Ann Med Interne (Paris) 1994;145:357–360. [PubMed] [Google Scholar]
- 18.Tsappa I, Missouris C, Psarellis S. Acyclovir-induced thrombocytopenia in a patient with SLE. BMJ Case Rep. 2018;2018(pii: bcr-2018-225118) doi: 10.1136/bcr-2018-225118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hong X, Wang X, Wang Z. A rare case report of acyclovir- induced immune thrombocytopenia with tongue hematomas as the first sign, and a literature review. BMC Pharmacol Toxicol. 2017;18(12) doi: 10.1186/s40360-017-0120-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kamboj J, Wu F, Kamboj R, Suzue K, Khosla P. A rare case of acyclovir-induced thrombocytopenia. Am J Ther. 2014;21:e159–162. doi: 10.1097/MJT.0b013e31826fc4be. [DOI] [PubMed] [Google Scholar]
- 21.Katsenos S, Gkolias D, Nikolopoulou M. Acyclovir-induced immune thrombocytopenia in a patient with herpes zoster of the trigeminal nerve. Pharmacotherapy. 2010;30:1085–1086. [Google Scholar]
- 22.Cersosimo RJ, Hankins MA, Hamrah SD. An unusual case of thrombocytopenia and leukopenia associated with diltiazem and acyclovir. J Pharm Technol. 2003;19:154–158. [Google Scholar]
- 23.Fekete GL, Cotoi OS, Fekete JE. Multiple nodular cutaneous metastasis as first clinical sign of signet ring cell gastric carcinoma - case report. Acta Dermatovenerol Croat. 2012;20:34–37. [PubMed] [Google Scholar]
- 24.Brănişteanu DE, Pintilie A, Andreş LE, Dimitriu A, Oanţă A, Stoleriu G, Brănişteanu DC. Ethiopatogenic hypotheses in lichen planus. Rev Med Chir Soc Med Nat Iasi. 2016;120:760–767. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.