Abstract
Objectives:
Hospital-associated disability (HAD), defined as loss of independence in activities of daily living (ADL) following acute hospitalization, is observed among older adults. The study objective is to determine overall prevalence of HAD among older adults hospitalized in acute care, and to assess the impact of study initiation year in moderation of prevalence.
Design:
Meta-analysis of data collected from randomized trials, quasi-experimental and prospective cohort studies. English-language searches to identify included studies were completed February 2018 and updated May 2018 of electronic databases and reference lists of studies and reviews. Included studies were human subjects investigations that measured ADL ≥ 2 time points before/during and after hospitalization and reported prevalence of ADL decline among older adults.
Setting:
Acute care hospital units.
Participants:
Adults aged ≥ 65 years hospitalized in medical-surgical acute care. Total sample size across all included studies was 7,375.
Methods:
Independence in ADL was assessed using the Katz Index of Independence in Activities of Daily Living and Barthel Index of Independence in Activities of Daily Living.
Results:
Random effects meta-analysis across included studies identified combined prevalence of HAD as 30% (95% CI: 24%, 33%; p < 0.001). The effect of study initiation year on prevalence rate was minimal. A large amount of heterogeneity was observed between studies, which may be due in part to non-standardized measurement of ADL impairment or other methodological differences.
Conclusions and Implications:
Hospitalization in acute care poses a significant risk to functional independence of older adults and this risk is unchanged despite shorter lengths of stay. The evidence supports the continued need for hospital-based programs that provide assessment of functional ability and identification of at risk older adults in order to better treat and prevent HAD.
Keywords: hospitalization, disability, activities of daily living, older adult
Brief Summary:
Prevalence of hospital-associated disability in acute care older patients is 30%, which has remained consistent overtime despite shorter lengths of stay. Hospitalization is a sentinel event leading to older adult disability.
INTRODUCTION
Mounting evidence now exists to indicate the negative impact of acute care hospitalization on health outcomes among older adults. Chief among the adverse consequences is increased risk for loss of functional independence and chronic disability.1–6 This phenomenon, often referred to as hospital-associated disability (HAD), is frequently defined as loss of independence in activities of daily living (ADL) following hospitalization.7
The World Health Organization’s International Classification of Functioning, Disability, and Health (ICF) describes functional impairments in activities as having a limitation in independent execution of daily tasks including self-care (bathing, dressing, using the toilet, and eating) and mobility (transferring from bed or a chair, walking across the room).8 Investigation of changes in ADL from before hospitalization to during and following hospitalization showed that longer length of stay in acute care is associated with greater likelihood of functional impairment;6,9,10 and led to seminal findings about the short and long-term consequences of hospitalization for many older adults. For example, Gill and colleagues have reported that hospitalization places older adults at risk for new or worsening disability, and reduces the likelihood of recovery from disability.2,3 Additionally, Fortinsky et al. and Brown et al. independently reported that older hospitalized patients who experience a loss of functional independence are at increased risk for nursing home admission at discharge.1,11 Brown et al. showed that these patients are also at increased risk for death.1
Change in ADL independence has been used as a marker of functional changes in various studies, including studies characterizing HAD and those testing the efficacy of interventions designed to reduce HAD. The main objective of this meta-analysis is to provide a systematic and thorough examination of the literature to identify the overall prevalence that older adults develop HAD, as exhibited by a clinical decline in ADL (i.e. ADL impairment) from pre-hospitalization to post-hospitalization. Additionally, considering that length of stay has decreased over time across the USA and Europe,12,13 a secondary objective assesses the effect of year of study initiation on the prevalence of HAD in this population.
METHODS
This meta-analysis is registered with PROSPERO14, protocol number: CRD42018091097.
Data Sources and Searches
Articles were identified through English-language searches of human subjects research in February 2018 and updated in May of 2018 using the following electronic databases: PubMed, Embase, CINAHL, Scopus, Proquest (PsychINFO & ProQuest Dissertations & Theses Global), NICHSR ONESearch, and ClinicalTrials.gov. List A1 contains lists of search terms used for online databases. Terms were deliberately wide-ranging to capture many different aspects of disability (e.g. cognition), but we restricted this analysis to change in activities of daily living. The reference lists of enrolled articles were also reviewed by hand to improve the integrity of this study. Our search was not limited to a specified time-period.
Study Selection
Using a two-step process, two investigators independently screened abstracts and evaluated full-text articles to identify studies meeting pre-specified eligibility criteria (Table A1). Decision disagreements were resolved by a third investigator to establish consensus. The results were tracked in an electronic database using the web application Rayyan (Qatar Computing Research Institute; Doha, Qatar).15
Eligible studies included randomized controlled trials, prospective cohort and quasi-experimental studies. The target population was adults, aged ≥ 65 years, hospitalized in acute care on medical-surgical units. Studies that included patients from psychiatry, cardiology, and neurology units in addition to patients from general medical-surgical units were included in the analysis. In the studies that used experimental study design, the target population for this review consisted only of patients in the control group. All studies assessed patient functional independence at ≥ two time points (e.g. 1] prior to hospitalization or at hospital admission, and 2] at discharge or following the index hospitalization).
We excluded studies that only admitted older adults to rehabilitative or restorative care in acute care settings such as inpatient rehabilitation units or geriatric-specialty units. Geriatric-specialty, or Acute Care for Elders (ACE) units are specifically designed to improve functional outcomes for older patients using an interdisciplinary model and were recently the subject of a different systematic review and meta-analysis.16,17
Data Extraction and Quality Assessment
A team of investigators individually extracted data on characteristics of study populations, interventions, comparators, outcomes (including findings related to population subgroups), study designs, settings, and methods including study time-points when ADL data was collected before and after hospitalization. An independent investigator verified the completeness and accuracy of the extracted data. Two independent investigators rated the quality of the individual studies as good, fair, or poor using the National Institute of Health’s Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies and the Cochrane Risk of Bias Tool or the Jadad Scale for reporting randomized controlled trials.
Data Synthesis and Analysis
Evidence tables containing study characteristics, results, and quality bias ratings were developed and synthesized into one database. Studies were organized chronologically based on publication year. Included studies used the Katz Index of Independence in Activities of Daily Living or Barthel Index to measure ADL.18,19 The Katz index is scored 0 – 6 points, with higher scores indicating greater ADL dependence.18 The Barthel index is scored 0 – 100 points, with higher scores indicating greater ADL independence.19 Modifications to the Katz and Barthel Indices have been made over time including changes in the ADLs that are included and changes to the level of independence assessed (e.g. independent, needs some assistance, needs total assistance). All studies examined change in ADL score between data collection time points, including how many patients experienced a clinically significant decline in ADL score at or after discharge. The primary outcome used in the meta-analysis was prevalence of ADL decline from pre-hospitalization to post-hospitalization. To minimize the effect of pre-hospitalization illness on ADL decline, we completed a sensitivity analysis assessing prevalence restricted to studies that reported changes in ADL independence from 2 weeks prior to admission (PTA) to discharge or within a month of discharge of the index hospitalization.
Statistical Analysis
For each study, the prevalence (number of participants that experienced ADL decline/total participants in the control group or in the study) with 95% confidence intervals (95% CI) were collected and entered into the study database. The scores on the Katz and Barthel Indices were converted to effect sizes to make them comparable across studies. The scores in the individual studies were combined using random effects meta-analysis to determine overall effect of hospitalization on ADL decline. The random effects model was utilized because it better accounts for heterogeneity between studies.20 Heterogeneity between studies was assessed using Cochran’s Q.21 Weighting by sample size was used to avoid excessive influence of smaller studies. Funnel plots and Fail Safe N were used to assess presence of study bias and robustness of results.22,23 Additional analyses included the year of study initiation as a moderator of the effect on prevalence rates of ADL decline to examine changes in rates over time. All analyses were conducted using the metafor package24 in R Studio (R Development Core Team, Auckland, New Zealand).
RESULTS
Study Characteristics
The initial literature search yielded 802 study titles and abstracts for screening. After discarding duplicate titles and abstracts and applying the inclusion and exclusion criteria, 164 study full texts were identified and screened. Of these, 15 studies fit the review criteria and were used for meta-analysis (Figure 1).
Figure 1.
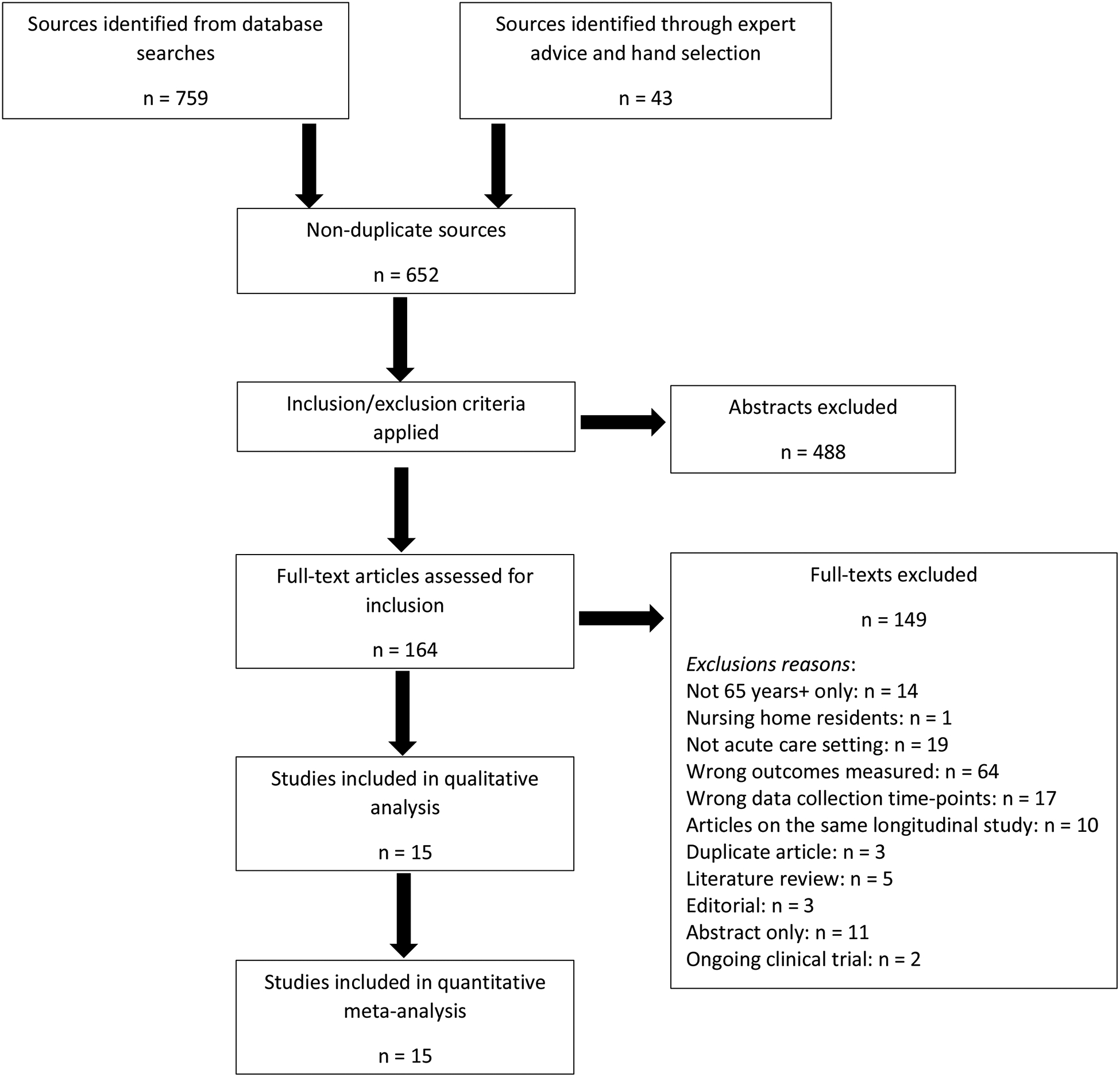
PRISMA flow diagram for included studies.
A summary of sample characteristics of included studies is presented in Table 1. These studies occurred during the years of 1983 to 2013. Eleven studies were based in the USA and 4 in other countries (2 in Italy, 1 in France, and 1 in Israel). Sample sizes ranged from 71 to 1,279 participants, and the total sample size across all included studies was 7,375. Thirteen prospective studies were categorized as hospital-based, i.e. participants were recruited upon admission to acute care hospitalization and followed throughout the index hospitalization and, often, during the post-discharge period. The hospital-based studies included 9 studies based in the USA and 4 based in other countries with a mean age range from 73.9 to 84.1 years. Seven of the hospital-based studies were completed at a teaching hospital, 2 at VA hospitals, 2 at large hospital centers, and 1 at a safety net hospital. Of the hospital-based studies, 8 assessed ADL change from 2 weeks prior to admission to discharge, 1 assessed ADL change from 2 weeks prior to admission to 1-week post-discharge, 3 assessed ADL change from admission to discharge, and 1 assessed ADL change from admission to 3 months post-discharge. Of the 15 included studies, 2 USA-based cohort studies were categorized as community-based, i.e. participants were recruited from the community and followed over multiple years during which time acute care hospitalization data was collected. The community-based studies collected information on participants at 6-month intervals, so that pre-hospitalization assessment of ADL could occur up to 6 months prior to hospitalization and post-hospitalization assessment of ADL could occur up to 6 months after hospitalization depending on when the participant was interviewed. The determination of HAD varied considerably among investigations. The studies used either the Katz or Barthel index to assess ADL; however all but two studies used a modified version of these tools (Table 1). Of note, 9 studies excluded the ADL assessment of continence independence,1,3,6,10,25–29 10 studies added assessments of independence in walking,1,3,4,6,10,25,27,29–32 and 2 studies added assessment of independence in grooming.29,32
Table 1.
Studies Included in Meta-Analyses
| 1st Author (Journal) | Study Period | Country | Study design | Sample size | Mean age, Y (SD) | Hospital setting (unit type) | Tool | Pre- to Post-assessment | Prevalence of HAD | Quality (poor, fair, good) |
|---|---|---|---|---|---|---|---|---|---|---|
| McVey (Ann Int Med)4 | 1983–1984 | USA | Randomized controlled trial | 178 (Control, 90) | 81.5 (5.8) | VA hospital (med, surg, psych) | *Katz | Admission – Discharge | 33/90 | good |
| Hirsch (J Am Geron Soc)30 | 1987 | USA | Prospective cohort study | 71 | 84 (NR) | Teaching hospital (med) | *Katz, CNA | 2 week PTA – 1 week PD | 30/49 | fair |
| Murray (J Geron Med Sci)25 | 1987–1989 | USA | Prospective cohort study | 291 (Control, 143) | 80.5 (7.6) | Teaching hospital (med, surg) | *Katz | Admission – 3 month PD | 41/143 | good |
| Inouye (J Am Geron Soc)26 | 1990–1991 | USA | Controlled trial | 216 (Control, 131) | 78.8 (6.2) | Teaching hospital (med) | *Katz | 2 week PTA – Discharge | 44/131 | good |
| Landefeld (New Eng J Med)27 | 1990–1992 | USA | Randomized controlled trial | 651 (Control, 324) | 80.2 (6.8) | Teaching hospital (med) | *Katz | 2 week PTA – Discharge | 64/300 | fair |
| Sager (Arch Int Med)10 | 1990–1992 | USA | Prospective cohort study | 1279 | 79 (6.3) | Teaching hospital (med) | *Katz | 2 week PTA – Discharge | 320/1072 | fair |
| Brown (J Am Geriatr Soc)1 | 1989–1991 | USA | Prospective cohort study | 498 | 78.7 (6.1) | Teaching hospital (med) | *Katz | 2 week PTA – Discharge | 135/474 | good |
| Zaslavsky (J Geron Med Sci)31 | 2009–2011 | Israel | Prospective cohort study | 691 | 78.8 (5.7) | Hospital center (med) | ^Barthel | 2 week PTA – Discharge | 286/691 | fair |
| Sourdet (J Am Med Dir Assoc)42 | 2011–2012 | France | Prospective cohort study | 503 | 84.1 (5.7) | Teaching hospital (med, surg) | Katz | Admission – Discharge | 91/503 | good |
| Chodos (J Gen Intern Med)28 | 2010–2012 | USA | Prospective cohort study | 583 (65+ years, 245) | 66.1 (8.8) | Safety net hospital (med, cardio, neuro) | *Katz | 2 week PTA – Discharge | 82/245 | good |
| Palese (J Ger Nurs)43 | 2012–2013 | Italy | Prospective cohort study | 1464 | 74.4 (1.3) | Hospital center (med) | Barthel | Admission – Discharge | 251/1464 | good |
| Brown (JAMA Intern Med)29 | 2010–2011 | USA | Randomized controlled trial | 100 (Control, 50) | 73.9 (7) | VA hospital (med) | *Katz | 2 week PTA – Discharge | 20/46 | good |
| Fimognari (J geron Med Sci)32 | 2004–2006 | Italy | Prospective cohort study | 675 | 82.6 (8.1) | Hospital center (med) | ^Barthel | 2 week PTA – Discharge | 126/675 | fair |
| Gill (J Am Med Assoc)3 | 1998–2003 | USA | Prospective cohort study | 754 | 78.4 (5.3) | Community | *Katz | a | 417/754 | fair |
| Boyd (J Am Geriatr soc)6 | 1992–1994 | USA | Prospective cohort study | 457 | NR | Community | ^Katz | b | 130/394 | good |
Control = sample size of control group in intervention study; CNA = Care Nursing Assessment;
Katz = modified Katz Index of Independence in Activities of Daily Living;
Barthel = modified Barthel Index of Independence in Activities of Daily Living.
Assessed hospitalization in the prior month and compared ADL from before hospitalization to after the hospitalization over the one month period
Assessed hospitalization every 6 months and compared ADL from before hospitalization to after over the course of the 6 months
Prevalence of Hospital-Associated Disability
Prevalence among all hospital-based studies ranged from 17% to 61% (Figure 2). Random effects meta-analysis showed the combined prevalence across studies was 30% (95% CI: 24%, 36%; p<0.001). Sensitivity analysis of only studies assessing ADL decline from 2 weeks prior to admission to discharge or within a month of discharge showed a combined prevalence of 33% (95% CI: 26%, 41%; Figure A1). Analysis including the 2 community-based studies did not appreciably change the prevalence rates (Figure A2). Removal of the 2 studies that included patients from psychiatry, cardiology, and neurology units in addition to patients from general medical-surgical units did not change the combined prevalence (data not shown).
Figure 2. Forest plot of the prevalence of hospital-associated disability (HAD): hospital-based studies only.
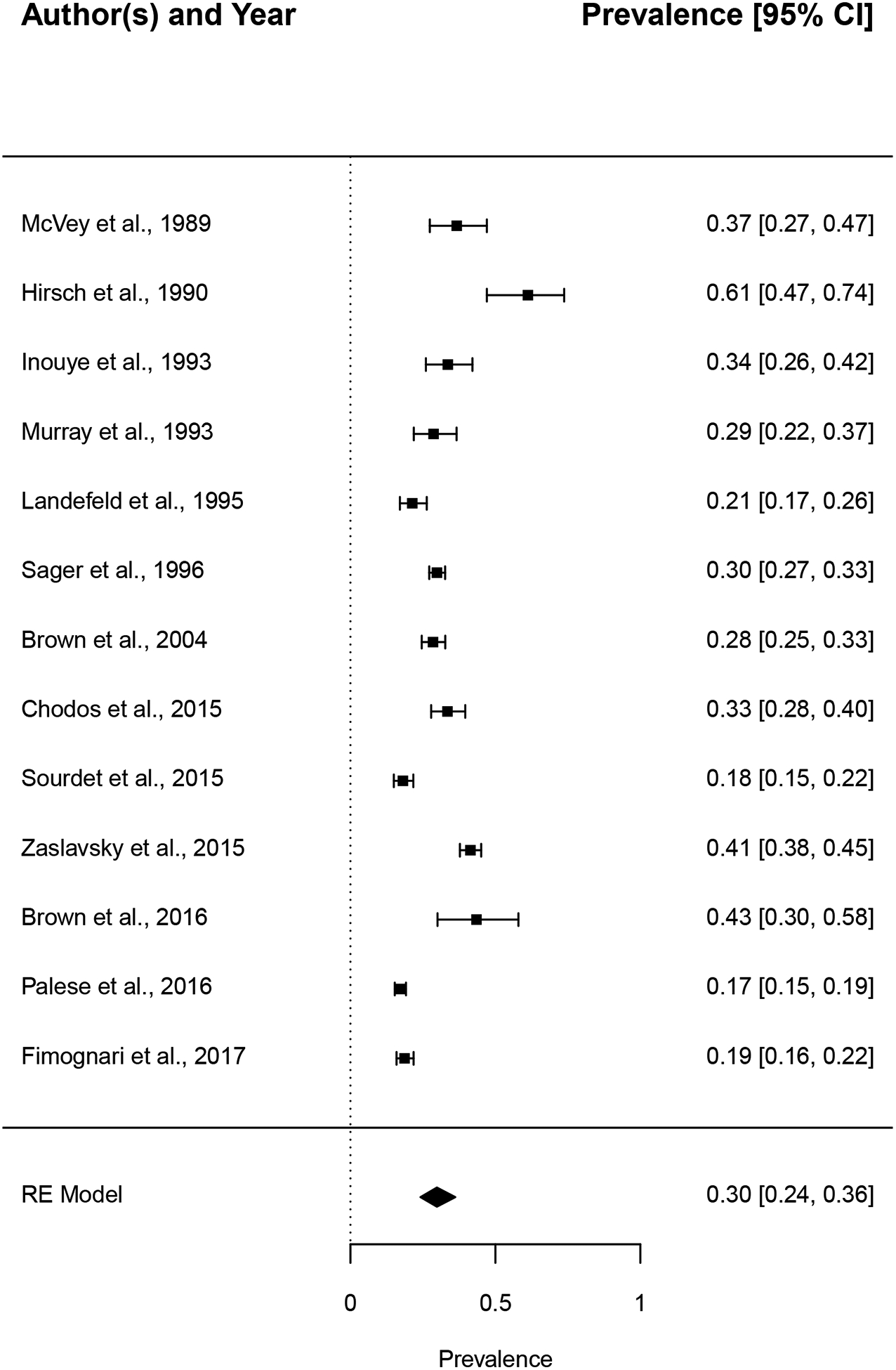
Prevalence rates from 13 individual hospital-based studies were combined using random-effects meta-analysis with a generalized linear mixed model. Vertical reference line indicates prevalence rate of 0 (no HAD); size of squats is proportional to the weight of the study in the analysis. CI=confidence interval.
Moderator Effect of Time
Moderation analyses using year of study initiation among hospital-based studies did not show any significant effects of time (QM = 1.32, p = 0.25). The cumulative meta-analysis also showed no significant change in the prevalence rate over time (Figure 3). Although the earliest studies did report the highest prevalence of HAD, there was still considerable overlap of the 95% confidence intervals with later studies. Similarly, among only studies that reported ADL decline from 2 weeks prior to admission to post-hospitalization, there was no significant effects of time on moderation of prevalence (QM = 0.01, p = 0.92) and the cumulative meta-analysis did not show significant change in prevalence rate over time (Figure A3).
Figure 3. Cumulative meta-analysis of all included studies showing time as a moderator of prevalence of hospital-associated disability (HAD).
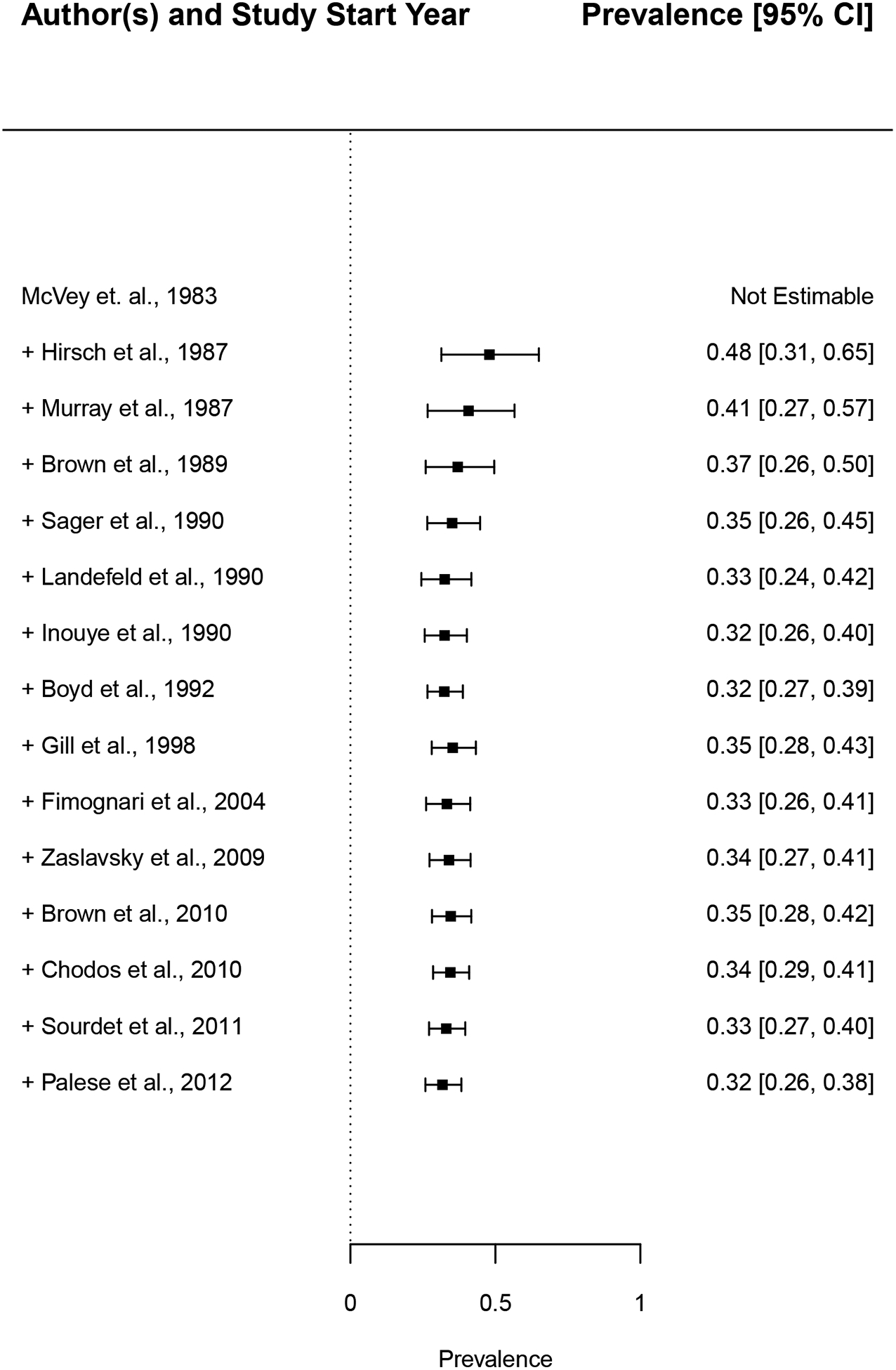
Prevalence rates were estimated after the addition of each study in chronological order of study initiation year to examine changes in prevalence over time. Vertical reference line indicates prevalence rate of 0 (no HAD).
Quality of Studies
All studies received a quality bias score of fair or good (Table 1). Studies that received a score of fair often failed to report whether study assessors and interviewers were blinded or reported that the assessors were not blinded to participant grouping. Additionally, these studies often failed to report participation rates and the justification for sample size used via power analysis.
Funnel plots for the prevalence showed substantial heterogeneity across the studies, which was confirmed by Cochran’s Q test (Figure A4, hospital-based studies only: Q=242.5, df=12, p<0.0001; Figure A5, 2 week PTA only: Q=123.7, df=8, p<0.0001; Figure A6, all studies: Q=499.5, df=14, p<0.0001). In addition, the funnel plots showed that many studies (even those with large sample sizes) lacked precision in their estimates, as shown by the wide horizontal spread in the plot. The funnel plots showed skew in the lower part of the plot, suggesting potential publication bias among smaller studies.
Despite these limitations, the Fail-Safe N analysis showed a strong effect for HAD prevalence (average effect size: −1.03, p < 0.0001). Among hospital-based studies, the Fail-Safe N for prevalence estimates indicated that 561,016 negative unpublished studies would need to be added to change meta-analysis results to be non-significant.
DISCUSSION
This meta-analysis identified that among older adults hospitalized in acute care the overall prevalence rate of HAD was 30%. In light of evidence that hospital-associated ADL impairment puts older adults at increased risk for nursing home placement and death,1 these results support that nearly one-third of hospitalized older adults could be at elevated risk of institutionalization and mortality after leaving the hospital. Furthermore, the number of cases of HAD is likely to rise as the older adult population continues to expand in the coming years,33 placing increased burden on global health care systems through increased costs and overloading of systems that provide post-hospital services such as nursing homes and home health care agencies. Thus, there is a continued need for elevated awareness of HAD in hospitalized older adults, improved systematic assessment of hospital-associated functional decline, and implementation of effective HAD prevention and treatment efforts such as hospital programs centered on maintenance of functional independence.
To the best of our knowledge, the study presented herein is the first meta-analysis of prevalence of functional disability among older adults hospitalized in acute care. Another very important systematic review and meta-analysis was published in 2012 assessing hospital-associated disability and related health outcomes and the effectiveness of Acute Care for Elders (ACE) model of hospital care, however the ACE study did not present prevalence of functional outcomes but rather focused on weighted mean differences and risk ratios for functional decline between usual care and intervention groups.17 Thus, our findings are novel and build on the findings of Fox et al. by illustrating that ACE models of care, which prevent and reduce HAD, are greatly needed.
Implications for Clinical Practice
Hospital-based programs have been designed that are cost-effective solutions to preventing and reducing HAD for older patients. Specifically, the ACE model focuses on preventing functional decline and other hospital-related issues among hospitalized older adults in acute care settings.34–36 Fox et al. showed that in-patient care of older adults that included ACE model components was beneficial for reducing ADL impairment from pre-hospitalization baseline function to hospital discharge functional status. This analysis also showed that ACE decreased discharge to the skilled nursing facility and increased discharge to home.17 Furthermore, the ACE unit is cost-effective and reduces 30-day readmission, which is essential for the sustainability of a program targeting a rapidly growing older adult population.37 The findings of our meta-analysis support that programs such as ACE, which use a systematic assessment or intervention for preventing HAD are greatly needed, thus clinicians should be supported and encouraged to develop and implement them in their hospitals.
Strengths and Limitations
This study has notable strengths. First, to our knowledge, it is the first meta-analysis conducted examining HAD among older adults hospitalized in acute care. Secondly, we were able to include a large number of studies encompassing a range of geographic areas and populations, thus increasing generalizability of the results. However, there are also limitations to acknowledge. First, many articles published on this subject were excluded due to non-standardized and poorly described evaluation processes or outcome measurement for ADL decline. Secondly, it is recognized that some clinical diagnoses such as stroke or hip fracture may lead to functional dependence that would be attributed to HAD. However, many older adults are admitted with diagnoses that do not directly impact on function. Thirdly, included studies showed a large amount of heterogeneity. Heterogeneity could be the result of methodological differences between studies or clinical differences in the populations, as well as potential publication bias. Additionally, despite including two studies that derived a portion of the study samples from specialty units, this meta-analysis was largely focused on HAD among patients in general acute care hospital settings. Therefore, the results presented may not apply to patients cared for on various types of hospital units and in facilities with specialty care such as rehabilitation. Finally, despite the wide range of search terms, such searches inevitably miss some studies. We are aware of 3 studies that examined ADL impairment following acute care hospitalization in older adults that were not identified in our search: Covinsky et al.38, Volpato et al.39 and Mudge et al.40 Reanalysis including these studies did not appreciably change the results (data not shown), indicating that omission of a small number of studies is unlikely to change our conclusions. This is further supported by the large Fail-Safe N for the prevalence estimates.
Conclusions and Implications
This meta-analysis shows that hospital associated disability remains a common problem among older adults hospitalized in acute care. Overall, the findings illustrate the continued need for hospital-based programs with function-focused care such as Acute Care for Elders.
This work also highlights a need for research aimed at establishing a standardized methodology for assessing and characterizing HAD. The lack of standardized methods for assessing ADL among hospitalized patients observed in this meta-analysis suggests that our use of functional disability as an outcome measure is not consistent. An important negative consequences of this is the inability to assess the effectiveness of quality patient care in the hospital. Furthermore, the results show a need for standardization of the timing of HAD assessment before and after hospitalization. In light of evidence supporting the important role of pre-hospitalization illness on ADL impairment,11,38 it is recommended that clinicians determine patient ADL status upon admission and follow up with patients at discharge or after hospitalization to assess for HAD. Another meta-analysis suggested a similar approach for evidence collection to increase the possibility that conclusions could be made about the effectiveness of treatments for patients.41 Ultimately, standardizing methods for assessing ADL status will assist in further characterizing HAD and in testing new interventions for mitigating the negative effects of hospitalization for older adults in the future.
Supplementary Material
Table A1. Eligibility criteria for included studies.
List A1. Electronic database search terms.
Figure A6. Funnel plot of estimates (estimated prevalence of HAD) vs precision (standard error) across all studies. This analysis assessed the level of heterogeneity across all studies.
Figure A5. Funnel plot of estimates (estimated prevalence of HAD) vs precision (standard error) across studies assessing ADL decline from 2 weeks prior to admission to post-hospitalization. This analysis assessed the level of heterogeneity across only studies assessing ADL decline from 2 weeks prior to admission to discharge or after discharge.
Figure A4. Funnel plot of estimates (estimated prevalence of HAD) vs precision (standard error) across hospital-based studies only. This analysis assessed the level of heterogeneity across only hospital-based studies.
Figure A2. Forest plot of the prevalence of hospital-associated disability (HAD) among older adults across all studies. Prevalence rates from 15 individual studies were combined using random-effects meta-analysis with a generalized linear mixed model. Studies were grouped into hospital- or community-based, respectively, based on where the sample was originally recruited. The vertical reference line indicates prevalence rate of 0 (no HAD); size of squares is proportional to the weight of the study in the analysis. CI=confidence interval.
Figure A3. Cumulative meta-analysis of studies assessing ADL decline from 2 weeks prior to admission to post-hospitalization showing time as a moderator of prevalence of hospital-associated disability (HAD). Prevalence rates were estimated after the addition of each study in chronological order of study initiation year to examine changes in prevalence over time. Vertical reference line indicates prevalence rate of 0 (no HAD).
Figure A1. Forest plot of the prevalence of hospital-associated disability (HAD) among older adults among studies assessing ADL decline from 2 weeks prior to admission to post-hospitalization. Prevalence rates from 8 individual studies were combined using random-effects meta-analysis with a generalized linear mixed model. The vertical reference line indicates prevalence rate of 0 (no HAD); size of squares is proportional to the weight of the study in the analysis. CI=confidence interval.
Acknowledgements
The funders/sponsors had no role in the design and conduct of the study; the collection, management, analysis and interpretation of the data; the preparation, review, or approval manuscript; nor the decision to submit the manuscript for publication.
Funding Sources:
University of Alabama at Birmingham- 2018 AMC21 Multi-Investigator Pilot Award partially supported effort on this project. CL is partially supported by NIH grant K12 GM088010; ADM is partially supported by NIH and VA grants; TWB is partially supported by NIH grant P2CHD086851; NCW is partially supported by NIH grant K01 NIAMS 1K01AR068400. REK is partially supported by multiple NIH and VA grants. CJB is partially supported by a VA Rehabilitation R&D Merit Award I01 RX001995.
Footnotes
Conflicts of Interest
CL, MEF, YZ, MF, SH, NCW, CSC, TWB, CHS, REK, and CJB have no perceived conflicts of interest to declare.
REFERENCES
- 1.Brown CJ, Friedkin RJ, Inouye SK. Prevalence and outcomes of low mobility in hospitalized older patients. J Am Geriatr Soc. 2004;52(8):1263–1270. [DOI] [PubMed] [Google Scholar]
- 2.Gill TM, Allore HG, Gahbauer EA, Murphy TE. Change in disability after hospitalization or restricted activity in older persons. JAMA. 2010;304(17):1919–1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292(17):2115–2124. [DOI] [PubMed] [Google Scholar]
- 4.McVey LJ, Becker PM, Saltz CC, Feussner JR, et al. Effect of a geriatric consultation team on functional status of elderly hospitalized patients. A randomized, controlled clinical trial. Ann Intern Med. 1989;110(1):79–84. [DOI] [PubMed] [Google Scholar]
- 5.Lamont CT, Sampson S, Matthias R, Kane R. The outcome of hospitalization for acute illness in the elderly. J Am Geriatr Soc. 1983;31(5):282–288. [DOI] [PubMed] [Google Scholar]
- 6.Boyd CM, Ricks M, Fried LP, Guralnik JM, et al. Functional decline and recovery of activities of daily living in hospitalized, disabled older women: the Women’s Health and Aging Study I. J Am Geriatr Soc. 2009;57(10):1757–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure”. JAMA. 2011;306(16):1782–1793. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. International Classification of Functioning, Disability and Health: ICF. In. Geneva: WHO; 2001. [Google Scholar]
- 9.Buurman BM, Hoogerduijn JG, van Gemert EA, de Haan RJ, et al. Clinical characteristics and outcomes of hospitalized older patients with distinct risk profiles for functional decline: a prospective cohort study. PLoS One. 2012;7(1):e29621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sager MA, Franke T, Inouye SK, Landefeld CS, et al. Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med. 1996;156(6):645–652. [PubMed] [Google Scholar]
- 11.Fortinsky RH, Covinsky KE, Palmer RM, Landefeld CS. Effects of functional status changes before and during hospitalization on nursing home admission of older adults. J Gerontol A Biol Sci Med Sci. 1999;54(10):M521–526. [DOI] [PubMed] [Google Scholar]
- 12.Burke RE, Juarez-Colunga E, Levy C, Prochazka AV, et al. Rise of post-acute care facilities as a discharge destination of US hospitalizations. JAMA Intern Med. 2015;175(2):295–296. [DOI] [PubMed] [Google Scholar]
- 13.OECD, Union E. Health at a Glance: Europe 2016. 2016.
- 14.NIH. PROSPERO International prospective register of systematic reviews. https://www.crd.york.ac.uk/prospero/. Accessed March 13, 2018. [DOI] [PMC free article] [PubMed]
- 15.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fox MT, Sidani S, Persaud M, Tregunno D, et al. Acute care for elders components of acute geriatric unit care: systematic descriptive review. J Am Geriatr Soc. 2013;61(6):939–946. [DOI] [PubMed] [Google Scholar]
- 17.Fox MT, Persaud M, Maimets I, O’Brien K, et al. Effectiveness of acute geriatric unit care using acute care for elders components: a systematic review and meta-analysis. J Am Geriatr Soc. 2012;60(12):2237–2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Katz S, Ford AB, Moskowitz RW, Jackson BA, et al. Studies of Illness in the Aged. The Index of Adl: A Standardized Measure of Biological and Psychosocial Function. JAMA. 1963;185:914–919. [DOI] [PubMed] [Google Scholar]
- 19.Mahoney FI, Barthel DW. Functional Evaluation: The Barthel Index. Md State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 20.Vevea LHJ. Fixed- and random-effects models in meta-analysis. Psychological Methods. 1998;3(4):486–504. [Google Scholar]
- 21.Hedges L Statistical methods for meta-analysis. Academic Press, Orlando, FL: 1985. [Google Scholar]
- 22.Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. [DOI] [PubMed] [Google Scholar]
- 23.Rosenberg MS. The file-drawer problem revisited: a general weighted method for calculating fail-safe numbers in meta-analysis. Evolution. 2005;59(2):464–468. [PubMed] [Google Scholar]
- 24.Viechtbauer W Conducting Meta-Analyses in R with the metafor Package. Journal of Statistical Software. 2010;36(3):1–48. [Google Scholar]
- 25.Murray AM, Levkoff SE, Wetle TT, Beckett L, et al. Acute delirium and functional decline in the hospitalized elderly patient. J Gerontol. 1993;48(5):M181–186. [DOI] [PubMed] [Google Scholar]
- 26.Inouye SK, Wagner DR, Acampora D, Horwitz RI, et al. A controlled trial of a nursing-centered intervention in hospitalized elderly medical patients: the Yale Geriatric Care Program. J Am Geriatr Soc. 1993;41(12):1353–1360. [DOI] [PubMed] [Google Scholar]
- 27.Landefeld CS, Palmer RM, Kresevic DM, Fortinsky RH, et al. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332(20):1338–1344. [DOI] [PubMed] [Google Scholar]
- 28.Chodos AH, Kushel MB, Greysen SR, Guzman D, et al. Hospitalization-Associated Disability in Adults Admitted to a Safety-Net Hospital. J Gen Intern Med. 2015;30(12):1765–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown CJ, Foley KT, Lowman JD Jr., MacLennan PA, et al. Comparison of Posthospitalization Function and Community Mobility in Hospital Mobility Program and Usual Care Patients: A Randomized Clinical Trial. JAMA Intern Med. 2016;176(7):921–927. [DOI] [PubMed] [Google Scholar]
- 30.Hirsch CH, Sommers L, Olsen A, Mullen L, et al. The natural history of functional morbidity in hospitalized older patients. J Am Geriatr Soc. 1990;38(12):1296–1303. [DOI] [PubMed] [Google Scholar]
- 31.Zaslavsky O, Zisberg A, Shadmi E. Impact of functional change before and during hospitalization on functional recovery 1 month following hospitalization. J Gerontol A Biol Sci Med Sci. 2015;70(3):381–386. [DOI] [PubMed] [Google Scholar]
- 32.Fimognari FL, Pierantozzi A, De Alfieri W, Salani B, et al. The Severity of Acute Illness and Functional Trajectories in Hospitalized Older Medical Patients. J Gerontol A Biol Sci Med Sci. 2017;72(1):102–108. [DOI] [PubMed] [Google Scholar]
- 33.Older People Projected to Outnumber Children for First Time in U.S. History [press release]. 2018.
- 34.Covinsky KE, Palmer RM, Kresevic DM, Kahana E, et al. Improving functional outcomes in older patients: lessons from an acute care for elders unit. Jt Comm J Qual Improv. 1998;24(2):63–76. [DOI] [PubMed] [Google Scholar]
- 35.Amador LF, Reed D, Lehman CA. The acute care for elders unit: taking the rehabilitation model into the hospital setting. Rehabil Nurs. 2007;32(3):126–132. [DOI] [PubMed] [Google Scholar]
- 36.Palmer RM. The Acute Care for Elders Unit Model of Care. Geriatrics (Basel). 2018;3(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Flood KL, Maclennan PA, McGrew D, Green D, et al. Effects of an acute care for elders unit on costs and 30-day readmissions. JAMA Intern Med. 2013;173(11):981–987. [DOI] [PubMed] [Google Scholar]
- 38.Covinsky KE, Palmer RM, Fortinsky RH, Counsell SR, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51(4):451–458. [DOI] [PubMed] [Google Scholar]
- 39.Volpato S, Onder G, Cavalieri M, Guerra G, et al. Characteristics of nondisabled older patients developing new disability associated with medical illnesses and hospitalization. J Gen Intern Med. 2007;22(5):668–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mudge AM, O’Rourke P, Denaro CP. Timing and risk factors for functional changes associated with medical hospitalization in older patients. J Gerontol A Biol Sci Med Sci. 2010;65(8):866–872. [DOI] [PubMed] [Google Scholar]
- 41.Talevski J, Sanders KM, Duque G, Connaughton C, et al. Effect of Clinical Care Pathways on Quality of Life and Physical Function After Fragility Fracture: A Meta-analysis. J Am Med Dir Assoc. 2019;20(7):926 e921–926 e911. [DOI] [PubMed] [Google Scholar]
- 42.Sourdet S, Lafont C, Rolland Y, Nourhashemi F, et al. Preventable Iatrogenic Disability in Elderly Patients During Hospitalization. J Am Med Dir Assoc. 2015;16(8):674–681. [DOI] [PubMed] [Google Scholar]
- 43.Palese A, Gonella S, Moreale R, Guarnier A, et al. Hospital-acquired functional decline in older patients cared for in acute medical wards and predictors: Findings from a multicentre longitudinal study. Geriatr Nurs. 2016;37(3):192–199. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table A1. Eligibility criteria for included studies.
List A1. Electronic database search terms.
Figure A6. Funnel plot of estimates (estimated prevalence of HAD) vs precision (standard error) across all studies. This analysis assessed the level of heterogeneity across all studies.
Figure A5. Funnel plot of estimates (estimated prevalence of HAD) vs precision (standard error) across studies assessing ADL decline from 2 weeks prior to admission to post-hospitalization. This analysis assessed the level of heterogeneity across only studies assessing ADL decline from 2 weeks prior to admission to discharge or after discharge.
Figure A4. Funnel plot of estimates (estimated prevalence of HAD) vs precision (standard error) across hospital-based studies only. This analysis assessed the level of heterogeneity across only hospital-based studies.
Figure A2. Forest plot of the prevalence of hospital-associated disability (HAD) among older adults across all studies. Prevalence rates from 15 individual studies were combined using random-effects meta-analysis with a generalized linear mixed model. Studies were grouped into hospital- or community-based, respectively, based on where the sample was originally recruited. The vertical reference line indicates prevalence rate of 0 (no HAD); size of squares is proportional to the weight of the study in the analysis. CI=confidence interval.
Figure A3. Cumulative meta-analysis of studies assessing ADL decline from 2 weeks prior to admission to post-hospitalization showing time as a moderator of prevalence of hospital-associated disability (HAD). Prevalence rates were estimated after the addition of each study in chronological order of study initiation year to examine changes in prevalence over time. Vertical reference line indicates prevalence rate of 0 (no HAD).
Figure A1. Forest plot of the prevalence of hospital-associated disability (HAD) among older adults among studies assessing ADL decline from 2 weeks prior to admission to post-hospitalization. Prevalence rates from 8 individual studies were combined using random-effects meta-analysis with a generalized linear mixed model. The vertical reference line indicates prevalence rate of 0 (no HAD); size of squares is proportional to the weight of the study in the analysis. CI=confidence interval.


