Abstract
Background
In 2011, the Accreditation Council for Graduate Medical Education (ACGME) instituted a 16-h limit on consecutive hours for first-year resident physicians. We sought to examine the effect of these work-hour regulations on physician safety.
Methods
All medical students matched to a United States residency program from 2002–2007 and 2014–2017 were invited to participate in prospective cohort studies. Each month participants reported hours of work, extended duration shifts, and adverse safety outcomes; including motor vehicle crashes , percutaneous injuries, and attentional failures. The incidence of each outcome was compared before and after the 2011 ACGME work-hour limit. Hypotheses were tested using generalized linear models adjusted for potential confounders.
Results
13% of all first-year resident physicians nationwide participated in the study, with 80,266 monthly reports completed by 15,276 first-year resident physicians. Following implementation of the 16-h 2011 ACGME work-hour limit, the mean number of extended duration (≥24-h) shifts per month decreased from 3.9 to 0.2. The risk of motor vehicle crash decreased 24% (RR 0.76; 0.67–0.85), percutaneous injury risk decreased more than 40% (RR 0.54; 0.48–0.61), and the rate of attentional failures was reduced 18% (IRR 0.82; 0.78–0.86). Extended duration shifts and prolonged weekly work hours were associated with an increased risk of adverse safety outcomes independent of cohort.
Conclusions
The 2011 ACGME work-hour limit was associated with meaningful improvements in physician safety and health. Surveillance is needed to monitor the ongoing impact of work hours on physician safety, health, and well-being.
Keywords: physicians, work hours, safety, sleep
BACKGROUND
The search for resident-physician work hours that are safe for both patients and physicians has continued for more than two decades.(1) In 2008, the National Academy of Medicine (NAM) synthesized the available evidence and recommended strategies to enhance sleep, supervision, and safety in this population.(2) The recommendations were intended to, “Promote conditions for safe medical care, improve the education of doctors in training, and increase the safety of residents and the general public.” In response, the Accreditation Council for Graduate Medical Education (ACGME) implemented a subset of the NAM recommendations in their 2011 guidelines that limited first-year resident physicians to work shifts of 16 or fewer consecutive hours and emphasized a commitment to patient safety and mitigation of fatigue-related risks (16-h 2011 ACGME work-hour limit).(3)
Evaluations of the 16-h 2011 ACGME work-hour limit focused on its impact on patient safety,(4–8) education,(5, 9–11) and resident well-being.(12–14) However, the critical issue of the safety of resident physicians themselves has been overlooked. Motor vehicle crashes represent the third leading cause of death among resident physicians.(15) Percutaneous injuries are common in some specialties, with recent single-center estimates reporting a career prevalence among surgical residents of 72%,(16) a prior-year prevalence among orthopedic residents of 42%,(17) and an increased risk for first-year residents across specialties.(18) Prior to the 2011 policy change, Barger et al. showed that residents who worked extended duration shifts had twice the risk of a motor vehicle crash on the drive from work.(19) Additional reports revealed that these extended duration shifts were also associated with a 61% increased risk of percutaneous injury,(20) and more than twice the incidence of attentional failures at night.(21) To our knowledge, no evaluations of the 16-h 2011 ACGME work-hour limit have reported on its effectiveness in reducing these adverse safety outcomes.
We sought to evaluate the impact of the 16-h 2011 ACGME work-hour limit on the safety and health of first-year resident physicians. We hypothesized that the restriction of extended duration shifts through the 16-h 2011 ACGME work-hour limit would be associated with reduced risk of motor vehicle crash, percutaneous injury, and attentional failures.
METHODS
We conducted a nationwide prospective cohort study of resident physicians for 5 academic years (2002–2007) prior to introduction of the 16-h 2011 ACGME work-hour limit, and for 3 academic years (2014–2017) post-implementation. All study procedures were approved by the Partners Human Research Committee and a Certificate of Confidentiality was issued by the Centers for Disease Control and Prevention. All variables utilized in this analysis were collected using identical methods in both cohorts. These methods have been described previously.(19, 20, 22)
Recruitment and Data Collection
Each April from 2002–2006, all United States (U.S.) medical school graduates and individuals who matched to a U.S. residency program through the Association of American Medical Colleges match process received an email informing them of the study, without detailing the study hypotheses. Similar recruitment methods were utilized in the subsequent cohort: In May of each year from 2014–2016, all medical school graduates who completed an application through the Electronic Residency Application Service (ERAS) were informed about the study via email. Those interested in participating were asked to complete an electronic informed consent process. In June of each year, individual password-coded links were sent via email to residents who consented to participate. The baseline survey collected individual demographic information, including age, gender, height, weight, medical history, and specialty program. Monthly reports collected work-hour information, including total hours of work, hours engaged in patient care, and additional work related to their residency program. The frequency of extended duration shifts was reported. Hours of sleep at work and away from work were reported. Respondents also reported on the frequency of adverse safety outcomes; including motor vehicle crashes and near-miss crashes. The instrument used to collect motor vehicle crash information has been previously validated.(19) We asked for documentation for all reported motor vehicle crashes (e.g., police reports, insurance claims). Similarly, we collected information on the frequency of occupational exposures, the source of the exposure, and factors which contributed to the exposure. We requested the occupational health report for each reported occupational exposure. We also queried how many times participants nodded off or fell asleep (attentional failures) during specific patient-care activities (during surgery and while talking to or examining patients), educational activities (during rounds with attending physicians and during lectures, seminars, or grand rounds), and while driving (either stopped at a light, or while the car was in motion).
Statistical Analysis
Data from both cohorts were pooled. We excluded months when: i) participants reported ≥14 work-free days; and ii) work-hour information was missing or exceeded 168 hours of work per week. The primary analysis tested the association between pre- and post-intervention cohorts and the outcomes of interest. Secondary analyses examined the association between weekly work hours, extended duration shifts, and the outcomes of interest across cohorts.
We compared demographics between exposed and unexposed groups using Wilcoxon rank sum and chi square tests. Weekly work hours were calculated as the sum of the number of hours spent physically awake in the hospital, classes, or workplace, plus the number of hours asleep in the hospital. Reports of work and sleep were compared using generalized linear models which accounted for clustering of respondents and the repeated-measures data structure.
We calculated the incidence of each adverse safety outcome before and after the 2011 policy change. Incidence rate ratios were constructed. The significance of the incidence rate ratio was tested using likelihood ratio tests in log-linear models (of note, similar results were obtained using Pearson- and deviance-based scaled Poisson models which accounted for overdispersion, conducted as sensitivity analyses). Rare outcomes were then dichotomized to reflect the presence or absence of at least one outcome during the month. We estimated the risk of each outcome using generalized linear mixed models with a binomial distribution and log-link function. Basic models for occupational exposures and percutaneous injuries were adjusted for hours spent in patient care that month. We identified potentially confounding variables a priori based on relevance to the research question and biologic plausibility. For example, body mass index (BMI) was identified as an important predictor for motor vehicle crashes, given its association with sleep apnea;(23) we controlled for BMI in all fully-adjusted models. We imputed data with the median for missing demographic information using the missing indicator method.(24) Fully-adjusted multivariable models controlled for age, gender, BMI, specialty program, and imputation indicator variables. Models examining occupational exposures and percutaneous injuries further controlled for the hours of patient care for that month. We then constructed mixed effects models to utilize data from both cohorts while testing extended duration shifts and weekly work hours as independent variables of interest. These analyses controlled for cohort using a conditional likelihood approach, in addition to the previously mentioned confounding variables. We conducted further sensitivity analyses that stratified by cohort and limited outcomes to those with supporting documentation.
Motor vehicle crash models were limited to participants who reported a valid driver’s license and months where they commuted to or from work. Occupational exposure models were limited to months where participants reported hours in patient care. SAS (version 9.4, Cary, NC) was used for statistical analysis. All tests were two-sided and p < 0.05 was considered statistically significant.
RESULTS
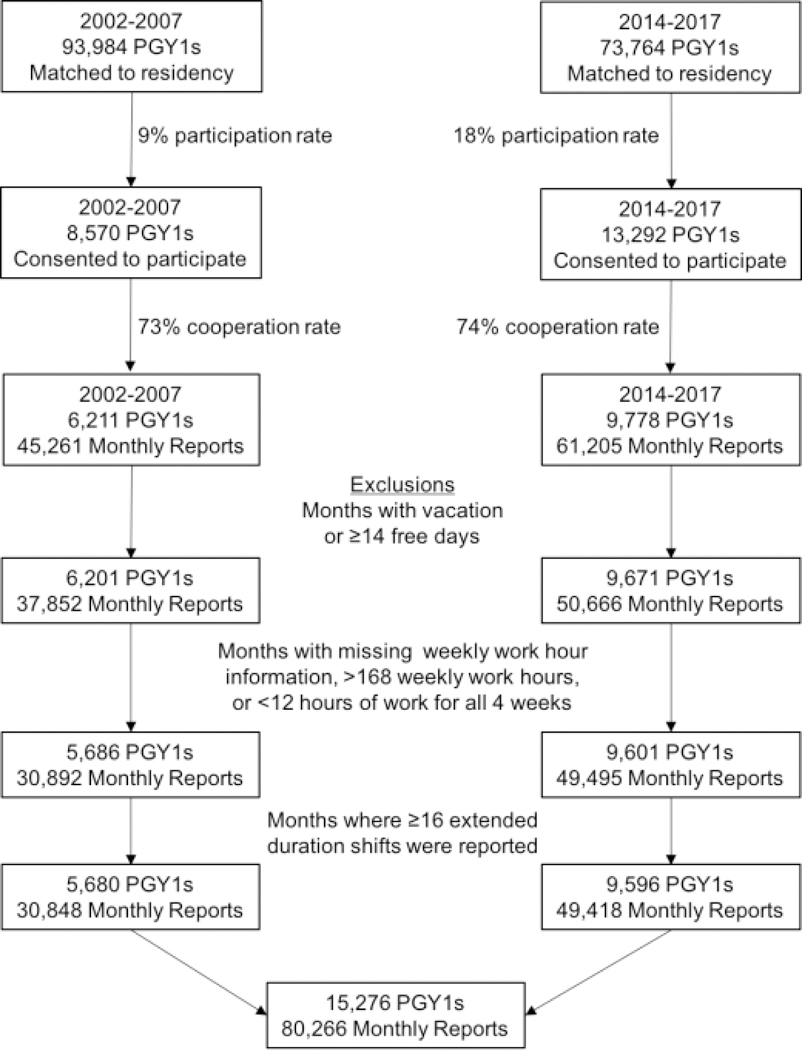
21,862 of 167,658 residents who matched to a United States residency program during the study interval consented to participate, representing 9% of all first-year residents nationally from 2002–2007 and 18% of all residents nationally from 2014–2017 (Figure 1). Approximately 75% of those who consented provided data and were included in the study cohort (cooperation rate). 6,211 first-year resident physicians completed 45,261 monthly reports between 2002 and 2007 and 9,778 first-year resident physicians completed 61,205 monthly reports between 2014 and 2017 (106,466 total monthly reports). After applying exclusion criteria, 80,266 monthly reports from 15,276 first-year resident physicians were available for analysis
Figure 1.
Participation in the study and exclusion criteria.
Characteristics of the Study Sample
Residents who contributed data after 2011 tended to be slightly younger and had a lower body mass index (Table 1). The composition of specialties was largely similar. Mean weekly hours of work decreased following the 16-h 2011 ACGME work-hour limit (71h vs. 62h), while hours engaged in patient care remained the same (Table 2). Participants reported fewer extended duration shifts per month (3.9 vs. 0.2). Nightly hours of sleep increased by 15 minutes of sleep per night (6.47h vs. 6.72h), despite less sleep obtained at work when extended-duration shifts were worked (2.52h vs. 1.86h). Nearly 1 in 3 extended-duration shifts (30%) were completed without sleep after 2011, compared to only 8% of extended duration shifts prior to 2011.
Table 1.
Demographic characteristics of the study sample
| Baseline Characteristics | 2002–2007 n=5,680 | 2014–2017 n=9,596 | p-value |
|---|---|---|---|
| Age | 28.9±3.9 | 28.7±3.2 | 0.01 |
| Female gender n(%) | 3,206 (56%) | 4,641 (48%) | <0.001 |
| Unknown | 32 (1%) | 668 (7%) | |
| Mean body mass index | 24.5±4.1 | 24.1±4.0 | <0.001 |
| Specialty n(%) * | <0.001 | ||
| Internal Medicine | 1,366 (24%) | 2,358 (25%) | |
| Family Practice | 643 (11%) | 1,125 (12%) | |
| Pediatrics | 790 (14%) | 1,080 (11%) | |
| General Surgery and surgical specialties | 643 (11%) | 934 (10%) | |
| Emergency Medicine | 369 (7%) | 687 (7%) | |
| Obstetrics/Gynecology | 364 (6%) | 509 (5%) | |
| Psychiatry | 251 (4%) | 422 (4%) | |
| Anesthesiology | 30 (1%) | 430 (4%) | |
| Other (including combined) | 1,129 (20%) | 1,402 (15%) | |
| Unknown | 95 (2%) | 649 (7%) | |
| Monthly Characteristics | n=30,848 | n=49,418 | |
| Weekly work hours | 71.1±18.5 | 62.1±17.0 | <0.001 |
| Hours engaged in patient care | 49.6±19.6 | 49.3±19.3 | 0.40 |
| Additional weekly work hours related to program | 3.7±4.3 | 5.0±6.3 | <0.001 |
| Extended duration shifts per month | 3.9±3.4 | 0.2±1.2 | <0.001 |
| Nightly sleep duration | 6.47±1.2 | 6.72±1.1 | <0.001 |
| Sleep duration on extended duration shifts | 2.52±1.5 | 1.86±1.9 | <0.001 |
Plus-minus values are means ± SD. Rank sum tests were used to compare age and body mass index. Wilcoxon chi square tests were used to compare gender and specialty. Univariate generalized linear regression models adjusted for clustering of individual responses were used to compare monthly characteristics.
Table 2.
The incidence of adverse safety outcomes before and after the 16-h 2011 ACGME work-hour limit.
| 2002–2007 | 2014–2017 | |||||||
|---|---|---|---|---|---|---|---|---|
| Months* | Outcomes | Rate per Person-Year | Months* | Outcomes | Rate per Person-Year | Incidence Rate Ratio | p-value | |
| Crashes | 28,428 | 565 | 0.238 | 47,241 | 736 | 0.187 | 0.78 | <0.001 |
| Police-Reported Crashes | 28,428 | 130 | 0.055 | 47,241 | 167 | 0.042 | 0.77 | 0.03 |
| Crashes on commute | 28,428 | 243 | 0.103 | 47,241 | 277 | 0.070 | 0.69 | <0.001 |
| Near-crashes | 28,428 | 7,999 | 3.377 | 47,241 | 7,813 | 1.985 | 0.59 | <0.001 |
| Occupational Exposures | 30,155 | 2,942 | 1.171 | 47,946 | 2,840 | 0.711 | 0.61 | <0.001 |
| Percutaneous Injuries |
30,155 | 884 | 0.352 | 47,946 | 682 | 0.173 | 0.49 | <0.001 |
| Attentional Failures | 30,848 | 92,557 | 36.005 | 49,418 | 123,070 | 29.885 | 0.83 | <0.001 |
Months where participants reported zero hours of patient care are excluded for assessment of outcomes occurring in the patient care setting (medical errors and occupational exposures). Crash and near-crash months are limited to participants who reported having a valid driver’s license and commuting to work. Attentional failures include all months of data. P-values were obtained from generalized log-linear regression models.
Incidence of Adverse Safety Outcomes Over Time
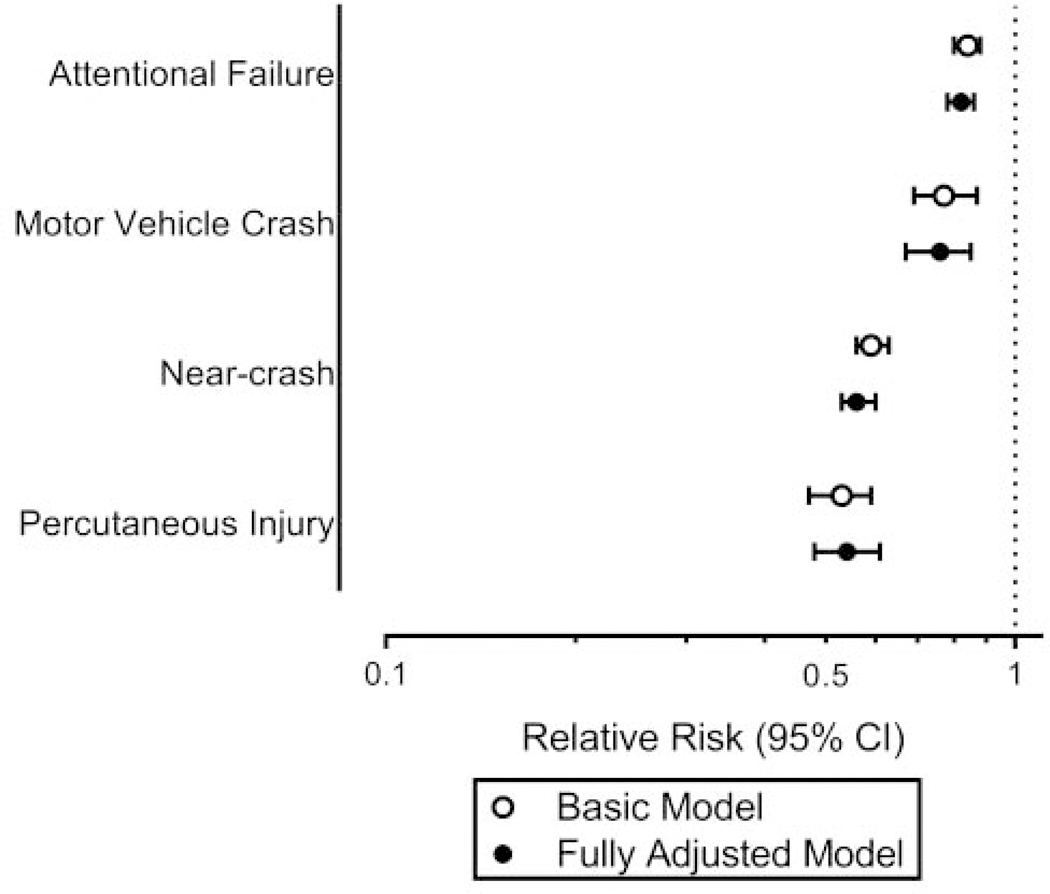
The incidence for each adverse outcome studied was significantly reduced following the 16-h 2011 ACGME work-hour limit (Table 2). After adjustment for potential confounders, the risk of motor vehicle crash decreased 24% (RR 0.76; 0.67–0.85), near-crashes decreased 44% (IRR 0.56; 0.53–0.60), percutaneous injury risk decreased 46% (RR 0.54; 0.48–0.61), and the rate of attentional failures was reduced 18% (IRR 0.82; 0.78–0.86) (Figure 2). Supporting documentation or additional detailed descriptions were provided for 81% of occupational exposures and 90% of reported motor vehicle crashes. Our results are similar or strengthened when limiting outcomes to those with supporting documentation (Table 3).
Figure 2.
The risk of adverse safety outcomes for first-year resident physicians who contributed data after implementation of the 16-h 2011 ACGME work-hour limit relative to first-year resident physicians who contributed data from 2002–2007.
Basic models for attentional failures, motor vehicle crash, and near crash include cohort as the only independent variable. The basic model for percutaneous injuries is adjusted for hours in patient care. The fully adjusted models for attentional failures, motor vehicle crash, and near crash are adjusted for age, gender, BMI, and specialty. The fully adjusted model for percutaneous injury is adjusted for all previously mentioned variables, as well as hours in patient care. All models are generalized linear models. Attentional failures and near-crashes use a Poisson distribution with a log link. All other models use a binomial distribution with a logit link function.
Table 3.
A sensitivity analysis comparing the relationship between the 2011 ACGME policy and resident safety outcomes overall compared to those with supporting documentation.
| Overall | p-value | With Supporting Documentation | p-value | |
|---|---|---|---|---|
| Crashes | RR 0.76 (0.67–0.85) | <0.0001 | RR 0.76 (0.67–0.87) | <0.0001 |
| Occupational Exposures^ | RR 0.57 (0.52–0.61) | <0.0001 | RR 0.46 (0.42–0.50) | <0.0001 |
All models are adjusted for age, gender, BMI, and specialty. P-values are obtained from likelihood ratio tests.
Also adjusted for hours of patient care in the month
Work Hours, Extended Duration Shifts, and Safety Outcomes
Participants in both cohorts reported exceeding 80 hours of work per week (averaged across 4 weeks) and working extended-duration shifts . Independent of cohort, working more than 80 hours per week and working extended duration shifts were each independently associated with an increased risk of adverse resident safety outcomes (Table 4). Compared with working no extended duration shifts, working even one extended duration shift in a month increased the risk of adverse outcomes; and working 5 or more extended duration shifts generally increased the risk of adverse outcomes to a greater degree. Similarly, compared with working up to 60 hours per week, increased risks of adverse outcomes were seen for those residents working >60–70 hours per week, those working >70–80 hours per week, and those working >80 hours per week in a dose-dependent fashion (Table 5). Stratified analyses are presented in the Supplemental Materials (Appendix Tables 1–3).
Table 4.
The adjusted association between weekly work hours, extended duration shifts, and adverse safety outcomes.
| Weekly Work Hours (WWH) | Extended Duration Shifts (EDS) | Combined categorical WWH and EDS | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n cases | n person months | ≤80 | >80 | None | 1–4 | ≥5 | ≤80 WWH No EDS | ≤80 WWH ≥1 EDS | >80 WWH No EDS | >80 WWH ≥1 EDS | ||||
| Crashes | 1,301 | 75,669 | Ref | 1.30 (1.12–1.51) | * | Ref | 1.20 (0.98–1.48) | 1.53 (1.27–1.86) | † | Ref | 1.37 (1.13–1.64) | 1.35 (1.06–1.73) | 1.56 (1.27–1.92) | † |
| Crashes leaving work | 520 | 75,669 | Ref | 1.59 (1.29–1.97) | * | Ref | 1.35 (0.99–1.84) | 1.91 (1.45–2.51) | † | Ref | 1.45 (1.10–1.92) | 1.35 (0.92–1.97) | 2.20 (1.64–2.95) | † |
| Near-crashes | 15,812 | 75,669 | Ref | 1.76 (1.67–1.87) | † | Ref | 1.37 (1.27–1.48) | 1.82 (1.70–1.95) | † | Ref | 1.42 (1.32–1.53) | 1.69 (1.52–1.88) | 2.27 (2.10–2.45) | † |
| Occupational Exposures | 5,782 | 78,101 | Ref | 1.50 (1.38–1.62) | † | Ref | 1.18 (1.05–1.33)^ | 1.25 (1.12–1.40)^ | * | Ref | 1.26 (1.13–1.41) | 1.67 (1.46–1.90) | 1.66 (1.48–1.86) | † |
| Percutaneous Injuries | 1,576 | 78,101 | Ref | 1.47 (1.30–1.66) | † | Ref | 1.14 (0.96–1.37)^ | 1.19 (1.00–1.41)^ | Ref | 1.20 (1.01–1.43) | 1.66 (1.36–2.02) | 1.57 (1.32–1.87) | † | |
| Attentional Failures | 215,627 | 80,266 | Ref | 1.68 (1.63–1.73) | † | Ref | 1.49 (1.42–1.56) | 2.05 (1.96–2.14) | † | Ref | 1.59 (1.52–1.67) | 1.54 (1.46–1.63) | 2.40 (2.29–2.50) | † |
All models are adjusted for age, gender, BMI, specialty, and cohort. P-values are obtained from likelihood ratio tests.
Also adjusted for hours of patient care in the month.
p-value<0.001
p-value=0.001.
Table 5.
The adjusted association between increasing weekly work hours and adverse safety outcomes.
| Weekly Work Hours | |||||
|---|---|---|---|---|---|
| ≤60 | >60 & ≤70 | >70 & ≤80 | >80 | p-valuve | |
| Crashes | Ref | 1.14 (0.97–1.33) | 1.17 (1.00–1.37) | 1.42 (1.20–1.68) | <0.001 |
| Crashes leaving work | Ref | 1.51 (1.16–1.95) | 1.56 (1.21–2.01) | 2.12 (1.64–2.76) | <0.001 |
| Near-crashes | Ref | 1.35 (1.27–1.45) | 1.59 (1.50–1.70) | 2.30 (2.14–2.47) | <0.001 |
| Occupational Exposures | Ref | 1.27 (1.15–1.41) | 1.66 (1.52–1.82) | 1.99 (1.80–2.19) | <0.001 |
| Percutaneous Injuries | Ref | 1.15 (0.98–1.36) | 1.41 (1.22–1.64) | 1.78 (1.53–2.07) | <0.001 |
| Attentional Failures | Ref | 1.39 (1.34–1.43) | 1.70 (1.65–1.75) | 2.27 (2.20–2.35) | <0.001 |
All models are adjusted for age, gender, BMI, specialty, and cohort. P-values are obtained from likelihood ratio tests
DISCUSSION
The 2011 ACGME work-hour restrictions were followed by marked improvements in resident safety. Residents reported lower rates of motor vehicle crashes on the commute, occupational exposures (including percutaneous injuries), and attentional failures. Following the policy change to eliminate extended-duration shifts in first-year resident physicians, average weekly work hours were reduced and nightly sleep duration increased. However, despite fears that the policy would limit hands-on training, reported hours spent in patient care remained unchanged.
Nationwide regulations that limited weekly work hours for residents and prohibited extended duration shifts were followed by improved safety. As reported elsewhere, compliance with the policy was not universal, (25, 26) and randomized trials of flexible hours permitted training programs at some institutions to exceed existing work hour limitations.(6, 8) Participants in both cohorts reporting exceeding 80 weekly work hours and working extended duration shifts. Sleep was obtained less frequently during extended duration shifts after the policy change, with a nearly 4-fold increase in the proportion of extended duration shifts without sleep (30% vs. 8%). The work hour limitations were not accompanied by an increased census of residency slots, which may have contributed to workload compression and reduced opportunity for sleep on-shift.(27) Independent of whether extended duration shifts were worked before or after the policy change, they were associated with significantly increased risk of adverse outcomes. Extended-duration shifts and prolonged weekly work hours were independent risk factors that acted synergistically to increase the risk of adverse outcomes. These findings are particularly important now, since the 2017 ACGME guidelines lifted the restrictions on extended duration shifts and again permit shifts of 24–28 consecutive hours of work for first-year resident physicians.(28) Several aspects of this issue, including physician safety, have been under-represented in the work hours debate. The pursuit of resident-physician work hours that are safe for patients and providers deserves further, more comprehensive, investigation.
Motor vehicle crashes are the third leading cause of death for medical residents, trailing only neoplastic disease and suicide.(15) Our findings reveal that elimination of extended duration shifts was associated with a significant reduction in the risk of crashes, particularly on the commute from work. Driving after extended duration shifts is known to be a high-risk activity.(19, 29) As the National Academy of Medicine recommended in their 2009 report,(2) some training programs have instituted safe transportation programs that enable residents to be reimbursed for ride-share or taxi costs following extended-duration shifts, however, the prevalence of such programs and their utilization by residents remains unclear. Installing alternative transport arrangements as the default following extended-duration shifts may be necessary for adoption of these habits as a cultural norm.
We found that average nightly sleep was increased following the 16-h 2011 ACGME work-hour limit, consistent with evidence that first-year resident physicians working overnight extended duration shifts achieve significantly less sleep than residents who do not work extended overnight shifts.(30) The FIRST trial found that first-year resident physicians assigned to programs which allowed extended-duration shifts were more than 8 times more likely to report that their work hours had a negative effect on their rest, and had a 7-fold increased risk of reporting that their work hours had a negative effect on their health, time for family and friends, and their hobbies.(31) Rosen et al. found a 7-fold increased odds of depression among first-year resident physicians who were not sleep deprived prior to their internship, but accumulated a chronic sleep debt over the course of their first postgraduate year.(32) Burnout is twice as common among physicians compared to the general population,(33) and sleep deficiency is a direct contributor to burnout.(34) Burnout, depression, sleepiness, and fatigue have also been associated with reported resident motor vehicle crashes.(35) Our findings suggest that work hour limitations may be an avenue to promote physician wellness.
Our data further reveal that the current ACGME standard of an average of 80 work hours per week is associated with an elevated risk of adverse outcomes. In the United States, resident physicians are allowed to work far longer hours than resident physicians in many other developed nations. The European Working Time Directive limits resident physicians throughout the European Union to 48 hours of work per week.(36) New Zealand has limited physicians-in-training to 16-hour shifts for more than 30 years, and the Province of Quebec in Canada recently cited the Canadian Charter of Rights and Freedoms in limiting resident physicians to 16 consecutive hours of work.(37) Australia does not restrict hours, but cautions that working more than 50 hours per week places the resident at risk, and exceeding 70 hours places the resident at higher risk.(38) Our data suggest that reducing weekly work hours would improve resident safety, and that cautions regarding the increased risk of long work weeks and extended-duration shifts should be made transparent to patients and providers.
Our study was observational, and we are unable to directly attribute the observed associations to the 16-h 2011 ACGME work-hour limit. The estimated associations could be affected by confounding bias. We controlled for multiple potential confounders, but residual confounding may persist through factors we did not collect or imprecise measurement of the confounders that were collected. We examined demographic characteristics for evidence of non-response bias. The demographic characteristics of participants in this sample are similar to the demographic characteristics of resident physicians nationally (Appendix Table 4). In total, 13% of all residents who matched to a United States residency program during the study interval participated in this study, including nearly 1 in 5 physicians entering residency from 2014–2017 (9% from 2002–2007 and 18% from 2014–2017) (Figure 1). Our findings have important policy implications for the more than 100,000 resident physicians in the US.
Some of the observed reductions in adverse safety outcomes may be attributable to secular trends. The national motor vehicle crash rate was reduced by 3% during our study interval (Appendix Table 5). Although the shift length limitations would have resulted in more commutes, the crash rate in our study sample was reduced by 22%, so it is unlikely that secular trends alone account for the observed improvement in vehicle crash rates in our study. The incidence of needlestick injuries among US health care workers has decreased approximately 1.4% per year since 2002.(39) We observed a 50% reduction in the incidence of needlestick injuries in our study population, exceeding the 20% reduction that would be expected over the time interval. In addition, our secondary analyses indicate that extended duration shifts are associated with an increased risk of adverse outcomes, independent of time period.
We collected outcomes via self-report. While this approach to the collection of adverse outcomes may be subject to social desirability bias, recall bias, and erroneous self-observation, the vast majority of reported occupational exposures and motor vehicle crashes were supported by additional documentation or detailed descriptions. Our results are similar or strengthened when limiting outcomes to those with supporting documentation (Table 3).
CONCLUSIONS
The 2011 ACGME guidelines that reduced work hours of first-year resident physicians was associated with improved resident safety and health. Extended-duration shifts and prolonged weekly work hours continue to adversely impact the safety and well-being of resident physicians. There is a pressing need to monitor changes in the rates of these adverse outcomes now that extended-duration shifts have been re-introduced.
CLINICAL SIGNIFICANCE.
First-year resident physician safety improved after the 2011 ACGME work hour limit.
The 2011 ACGME work hour limit was associated with increased sleep duration and significantly lower risk of motor vehicle crashes, near-crashes, percutaneous injuries, and attentional failures.
Extended duration shifts and prolonged weekly work hours were associated with an increased risk of adverse safety outcomes before and after work hour reform.
ACKNOWLEDGMENTS
We thank the resident physicians who took time from their busy work schedules to participate in this study; to the Association of American Medical Colleges, especially Marie Caulfield and Brianna Gunter, for their assistance with recruitment; to Steven W. Lockley for his assistance with the study design and data interpretation; to research assistants Michael Shreeve and Justin Buie, and students Kelly Racicot, Lars Johnsen, Erita Rothschild, Autumn Gertz, Niamh Mulrooney, Matthew Stewart, Jacob Stroud, Gregory Pavlov, Krystal Lipomi, Arlene Perez, and Julian Smith-Sparks for help with validating reported outcomes.
FUNDING
This project was supported by the National Institute for Occupational Safety and Health R01OH010300 and R01OH07567; National Heart, Lung and Blood Institute U01HL111478, T32HL007901 and F32HL134249. The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix Table 1.
The adjusted association between extended duration shifts and adverse safety outcomes stratified by cohort.
| Extended Duration Shifts (EDS) 2002–2007 | Extended Duration Shifts (EDS) 2014–2017 | |||||||
|---|---|---|---|---|---|---|---|---|
| None | 1–4 | ≥5 | p-value | None | 1–4 | ≥5 | p-value | |
| Crashes | Ref | 1.20 (0.94-1.54) | 1.46 (1.17-1.81) | 0.002 | Ref | 0.98 (0.65-1.49) | 2.02 (1.36-3.01) | 0.03 |
| Crashes leaving work | Ref | non-estimable | Ref | 1.05 (0.56- 1.96) |
1.64 (0.83- 3.23) |
0.51 | ||
| Near-crashes | Ref | 1.48 (1.35-1.62) | 1.95 (1.79-2.12) | <0.0001 | Ref | 1.20 (1.01-1.43) | 1.45 (1.19-1.76) | 0.0022 |
| Occupational Exposures^ | Ref | 1.11 (0.96-1.27) | 1.17 (1.03-1.33) | 0.05 | Ref | 1.44 (1.16-1.79) | 1.35 (1.02-1.79) | 0.0046 |
| Percutaneous Injuries^ | Ref | 0.97 (0.80-1.19) | 1.07 (0.89-1.29) | 0.53 | Ref | 1.50 (1.10-2.06) | 1.29 (0.85-1.97) | 0.07 |
| Attentional Failures | Ref | 1.59 (1.51-1.69) | 2.21 (2.09-2.33) | <0.0001 | Ref | 1.37 (1.25-1.49) | 1.71(1.51-1.93) | <0.0001 |
All models are adjusted for age, gender, BMI, specialty, and cohort. P-values are obtained from likelihood ratio tests.
Also adjusted for hours of patient care in the month.
Appendix Table 2.
The adjusted association between exceeding 80 weekly work hours and adverse safety outcomes stratified by cohort.
| Weekly Work Hours 2002–2007 | Weekly Work Hours 2014–2017 | |||||
|---|---|---|---|---|---|---|
| ≤80 | >80 | p-value | ≤80 | >80 | p-value | |
| Crashes | Ref | 1.24 (1.04–1.49) | 0.02 | Ref | 1.40 (1.09–1.79) | 0.001 |
| Crashes leaving work | Ref | non-estimable | Ref | 1.30 (0.88–1.94) | 0.19 | |
| Near-crashes | Ref | 1.80 (1.69–1.93) | <0.0001 | Ref | 1.68 (1.50–1.87) | <0.0001 |
| Occupational Exposures^ | Ref | 1.22 (1.10–1.35) | 0.0002 | Ref | 1.58 (1.38–1.82) | <0.0001 |
| Percutaneous Injuries^ | Ref | 1.21 (1.03–1.42) | 0.02 | Ref | 1.59 (1.28–1.96) | <0.0001 |
| Attentional Failures | Ref | 1.79 (1.73–1.85) | <0.0001 | Ref | 1.52 (1.44–1.60) | <0.0001 |
All models are adjusted for age, gender, BMI, and specialty. P-values are obtained from likelihood ratio tests.
Also adjusted for hours of patient care in the month.
Appendix Tables 3A and 3B:
The adjusted association between increasing weekly work hours and adverse safety outcomes stratified by cohort.
| Weekly Work Hours | |||||
|---|---|---|---|---|---|
| A: 2002–2007 | ≤60 | >60 & ≤70 | >70 & ≤80 | >80 | p-valuve |
| Crashes | Ref | 1.47 (1.12–1.94) | 1.42 (1.10–1.84) | 1.59 (1.24–2.02) | 0.0007 |
| Crashes leaving work | Ref | non-estimable | |||
| Near-crashes | Ref | 1.39 (1.25–1.53) | 1.72 (1.56–1.89) | 2.45 (2.23–2.69) | <0.0001 |
| Occupational Exposures | Ref | 1.25 (1.06–1.47) | 1.75 (1.52–2.01) | 1.88 (1.65–2.15) | <0.0001 |
| Percutaneous Injuries | Ref | 1.10 (0.85–1.43) | 1.45 (1.17–1.80) | 1.63 (1.33–2.00) | <0.0001 |
| Attentional Failures | Ref | 1.66 (1.56–1.76) | 2.12 (2.01–2.24) | 2.83 (2.68–2.98) | <0.0001 |
| Weekly Work Hours | |||||
|---|---|---|---|---|---|
| B: 2014–2017 | ≤60 | >60 & ≤70 | >70 & ≤80 | >80 | p-value |
| Crashes | Ref | 1.01 (0.83–1.22) | 1.05 (0.86–1.27) | 1.42 (1.09–1.85) | 0.13 |
| Crashes leaving work | Ref | 1.36 (1.00–1.86) | 1.37 (1.00–1.89) | 1.60 (1.04–2.46) | 0.07 |
| Near-crashes | Ref | 1.33 (1.22–1.45) | 1.52 (1.39–1.65) | 2.12 (1.88–2.40) | <0.0001 |
| Occupational Exposures | Ref | 1.29 (1.13-1.46) | 1.60 (1.41-1.81) | 2.23 (1.91-2.61) | <0.0001 |
| Percutaneous Injuries | Ref | 1.20 (0.97–1.49) | 1.36 (1.11–1.67) | 2.05 (1.61–2.61) | <0.0001 |
| Attentional Failures | Ref | 1.29 (1.25–1.34) | 1.52 (1.47–1.58) | 1.94 (1.83–2.05) | <0.0001 |
All models are adjusted for age, gender, BMI, and specialty. P-values are obtained from likelihood ratio tests
Appendix Tables 4A and 4B.
The demographics of the study sample compared to the characteristics of first-year residents nationally.
| A | Study Sample | ACGME National Data | ||
|---|---|---|---|---|
| 2014–2017 (n=9,778) | 2014–2015 (n=28,220) | 2015–2016 (n=29,074) | 2016–2017 (n=30,381) | |
| Age | 28.7±3.2 | 30.6 | 30.6 | 30.7 |
| Female Gender | 48% | 44% | 44% | 44% |
| Specialty* | ||||
| Internal Medicine | 25% | 34% | 34% | 34% |
| Family Medicine | 12% | 13% | 13% | 13% |
| Pediatrics | 11% | 11% | 11% | 10% |
| General Surgery and surgical specialties | 10% | 13% | 13% | 13% |
| Emergency Medicine | 7% | 7% | 7% | 7% |
| Obstetrics/Gynecology | 5% | 5% | 5% | 5% |
| Psychiatry | 4% | 5% | 5% | 5% |
| Anesthesiology | 4% | 3% | 4% | 3% |
| Other (including combined) | 15% | 9% | 8% | 10% |
| B | Study Sample | ACGME National Data |
|---|---|---|
| 2002–2007 (n=6,211) | 2007–2008 (n=36,012) | |
| Age | 28.9±3.9 | Not Reported |
| Female Gender | 56% | 41% |
| Specialty* | ||
| Internal Medicine | 24% | 31% |
| Family Medicine | 11% | 10% |
| Pediatrics | 14% | 10% |
| General Surgery and surgical specialties | 11% | 9% |
| Emergency Medicine | 7% | 4% |
| Obstetrics/Gynecology | 6% | 3% |
| Psychiatry | 4% | 5% |
| Anesthesiology | 1% | 4% |
| Other (including combined) | 20% | 22% |
Percentage of residents in each specialty. Percentages may not add to 100 due to rounding.
Reporting practices may explain some differences in the demographic characteristics of our study sample compared to residents nationally. Our baseline questionnaire was administered immediately upon entry of residency. The timing of age information in the national data is not known. The lower prevalence of reported internal medicine residents in our study may be explained by the reporting of planned specialty rather than preliminary or transitional year. National PGY-1 specific demographic information is not available for years prior to 2007.
Appendix Table 5.
Temporal trends in motor vehicle crashes in the USA.
| Year | Crashes | Licensed Drivers | Rate per Driver per Year |
|---|---|---|---|
| 2002 | 6,315,708 | 194,295,633 | 0.032505661 |
| 2003 | 6,327,955 | 196,165,667 | 0.032258219 |
| 2004 | 6,181,027 | 198,888,912 | 0.031077786 |
| 2005 | 6,159,350 | 200,548,972 | 0.030712449 |
| 2006 | 5,973,213 | 202,810,438 | 0.029452197 |
| 2007 | 6,024,008 | 205,741,845 | 0.02927945 |
| 2008 | 5,810,846 | 208,320,601 | 0.027893766 |
| 2009 | 5,505,180 | 209,618,386 | 0.026262868 |
| 2010 | 5,419,445 | 210,114,939 | 0.025792764 |
| 2011 | 5,337,829 | 211,874,649 | 0.025193335 |
| 2012 | 5,615,045 | 211,814,830 | 0.026509216 |
| 2013 | 5,686,891 | 212,159,728 | 0.026804762 |
| 2014 | 6,064,284 | 214,092,472 | 0.028325536 |
| 2015 | 6,296,134 | 218,084,465 | 0.028870163 |
| 2016 | 7,276,838 | 221,711,918 | 0.03282114 |
Average 2002–2007: 0.0308 crashes per driver per year.
Average 2014–2016: 0.0300 crashes per driver per year.
Footnotes
CONFLICTS OF INTEREST
Dr. Landrigan is supported in part by the Children’s Hospital Association for work as an executive council member of the Pediatric Research in Inpatient Settings (PRIS) network. He has served as a paid consultant to Virgin Pulse to help develop a Sleep and Health Program. He has consulted with and holds equity in the I-PASS Patient Safety Institute. In addition, he has received monetary awards, honoraria, and travel reimbursement from multiple academic and professional organizations for teaching and consulting on sleep deprivation, physician performance, handoffs, and safety, and has served as an expert witness in cases regarding patient safety and sleep deprivation.
Dr. Czeisler reports grants from Cephalon Inc., grants from Mary Ann & Stanley Snider via Combined Jewish Philanthropies, grants from National Football League Charities, grants from Optum, grants from Philips Respironics, Inc., grants from ResMed Foundation, grants from San Francisco Bar Pilots, grants from Schneider Inc., grants from Sysco, grants from Cephalon, Inc, grants from Jazz Pharmaceuticals, grants from Takeda Pharmaceuticals, grants from Teva Pharmaceuticals Industries, Ltd, grants from Sanofi-Aventis, Inc, grants from Sepracor, Inc, grants from Wake Up Narcolepsy, personal fees from Bose Corporation, personal fees from Boston Celtics, personal fees from Boston Red Sox, personal fees from Columbia River Bar Pilots, personal fees from Institute of Digital Media and Child Development, personal fees from Klarman Family Foundation, personal fees from Samsung Electronics, personal fees from Quest Diagnostics, Inc, personal fees from Vanda Pharmaceuticals, personal fees from Zurich Insurance Company, Ltd, personal fees from Purdue Pharma, LP, personal fees from McGraw Hill, personal fees from Houghton Mifflin Harcourt/Penguin, personal fees from Koninklijke Philips Electronics, N.V., personal fees from Cephalon, Inc, other from Vanda Pharmaceuticals, personal fees from Washington State Board of Pilotage Commissioners, personal fees from Ganésco Inc., grants from Jazz Pharmaceuticals Plc., Inc., grants from Regeneron Pharmaceuticals, grants from Sanofi S.A., and personal fees from New England Journal of Medicine, outside the submitted work; In addition, Dr. Czeisler holds a number of process patents in the field of sleep/circadian rhythms (e.g., photic resetting of the human circadian pacemaker). These are available to BWH upon request. Since 1985, Dr. Czeisler has also served as an expert on various legal and technical cases related to sleep and/or circadian rhythms including those involving the following commercial entities: Casper Sleep Inc., Complete General Construction Company, FedEx, Greyhound, HG Energy LLC, South Carolina Central Railroad Co., Steel Warehouse Inc., Stric-Lan Companies LLC, Texas Premier Resource LLC and United Parcel Service (UPS).
Dr. Czeisler’s interests were reviewed and managed by Brigham and Women’s Hospital and Partners HealthCare in accordance with their conflict of interest policies.
Dr. Barger is on the scientific advisory board for CurAegis Technologies. She has received consulting fees from University of Pittsburgh, Sygma, Insight and Puget Sound Pilots.
The other authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Steinbrook R The debate over residents’ work hours. N Engl J Med. 2002;347(16):1296–302. [DOI] [PubMed] [Google Scholar]
- 2.Johns MM, Wolman DM, Ulmer C. Resident duty hours: enhancing sleep, supervision, and safety: National Academies Press; 2009. [PubMed] [Google Scholar]
- 3.Nasca TJ, Day SH, Amis ES Jr., The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;363(2):e3. [DOI] [PubMed] [Google Scholar]
- 4.Patel MS, Volpp KG, Small DS, Hill AS, Even-Shoshan O, Rosenbaum L, et al. Association of the 2011 ACGME resident duty hour reforms with mortality and readmissions among hospitalized Medicare patients. Jama. 2014;312(22):2364–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rajaram R, Chung JW, Jones AT, Cohen ME, Dahlke AR, Ko CY, et al. Association of the 2011 ACGME resident duty hour reform with general surgery patient outcomes and with resident examination performance. Jama. 2014;312(22):2374–84. [DOI] [PubMed] [Google Scholar]
- 6.Bilimoria KY, Chung JW, Hedges LV, Dahlke AR, Love R, Cohen ME, et al. National Cluster-Randomized Trial of Duty-Hour Flexibility in Surgical Training. N Engl J Med. 2016;374(8):713–27. [DOI] [PubMed] [Google Scholar]
- 7.Choma NN, Vasilevskis EE, Sponsler KC, Hathaway J, Kripalani S. Effect of the ACGME 16-hour rule on efficiency and quality of care: duty hours 2.0. JAMA Intern Med. 2013;173(9):819–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silber JH, Bellini LM, Shea JA, Desai SV, Dinges DF, Basner M, et al. Patient Safety Outcomes under Flexible and Standard Resident Duty-Hour Rules. N Engl J Med. 2019;380(10):905–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DeLaroche A, Riggs T, Maisels MJ. Impact of the new 16-hour duty period on pediatric interns’ neonatal education. Clin Pediatr (Phila). 2014;53(1):51–9. [DOI] [PubMed] [Google Scholar]
- 10.Desai SV, Feldman L, Brown L, Dezube R, Yeh HC, Punjabi N, et al. Effect of the 2011 vs 2003 duty hour regulation-compliant models on sleep duration, trainee education, and continuity of patient care among internal medicine house staff: a randomized trial. JAMA Intern Med. 2013;173(8):649–55. [DOI] [PubMed] [Google Scholar]
- 11.Theobald CN, Stover DG, Choma NN, Hathaway J, Green JK, Peterson NB, et al. The effect of reducing maximum shift lengths to 16 hours on internal medicine interns’ educational opportunities. Acad Med. 2013;88(4):512–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Auger KA, Landrigan CP, Gonzalez del Rey JA, Sieplinga KR, Sucharew HJ, Simmons JM. Better rested, but more stressed? Evidence of the effects of resident work hour restrictions. Acad Pediatr. 2012;12(4):335–43. [DOI] [PubMed] [Google Scholar]
- 13.Sen S, Kranzler HR, Didwania AK, Schwartz AC, Amarnath S, Kolars JC, et al. Effects of the 2011 duty hour reforms on interns and their patients: a prospective longitudinal cohort study. JAMA Intern Med. 2013;173(8):657–62; discussion 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ripp JA, Bellini L, Fallar R, Bazari H, Katz JT, Korenstein D. The impact of duty hours restrictions on job burnout in internal medicine residents: a three-institution comparison study. Acad Med. 2015;90(4):494–9. [DOI] [PubMed] [Google Scholar]
- 15.Yaghmour NA, Brigham TP, Richter T, Miller RS, Philibert I, Baldwin DC, Jr., et al. Causes of Death of Residents in ACGME-Accredited Programs 2000 Through 2014: Implications for the Learning Environment. Acad Med. 2017;92(7):976–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choi LY, Torres R, Syed S, Boyle S, Ata A, Beyer TD, et al. Sharps and Needlestick Injuries Among Medical Students, Surgical Residents, Faculty, and Operating Room Staff at a Single Academic Institution. J Surg Educ. 2017;74(1):131–6. [DOI] [PubMed] [Google Scholar]
- 17.Bernard JA, Dattilo JR, Laporte DM. The incidence and reporting of sharps exposure among medical students, orthopedic residents, and faculty at one institution. J Surg Educ. 2013;70(5):660–8. [DOI] [PubMed] [Google Scholar]
- 18.Marnejon T, Gemmel D, Mulhern K. Patterns of Needlestick and Sharps Injuries Among Training Residents. JAMA Intern Med. 2016;176(2):251–2. [DOI] [PubMed] [Google Scholar]
- 19.Barger LK, Cade BE, Ayas NT, Cronin JW, Rosner B, Speizer FE, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352(2):125–34. [DOI] [PubMed] [Google Scholar]
- 20.Ayas NT, Barger LK, Cade BE, Hashimoto DM, Rosner B, Cronin JW, et al. Extended work duration and the risk of self-reported percutaneous injuries in interns. Jama. 2006;296(9):1055–62. [DOI] [PubMed] [Google Scholar]
- 21.Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP, et al. Effect of reducing interns’ weekly work hours on sleep and attentional failures. New England Journal of Medicine. 2004;351(18):1829–37. [DOI] [PubMed] [Google Scholar]
- 22.Barger LK, Ayas NT, Cade BE, Cronin JW, Rosner B, Speizer FE, et al. Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Med. 2006;3(12):e487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vgontzas AN, Tan TL, Bixler EO, Martin LF, Shubert D, Kales A. Sleep apnea and sleep disruption in obese patients. Arch Intern Med. 1994;154(15):1705–11. [PubMed] [Google Scholar]
- 24.Miettinen OS. Theoretical epidemiology: principles of occurrence research in medicine: Wiley; New York; 1985. [Google Scholar]
- 25.Landrigan CP, Barger LK, Cade BE, Ayas NT, Czeisler CA. Interns’ compliance with accreditation council for graduate medical education work-hour limits. Jama. 2006;296(9):1063–70. [DOI] [PubMed] [Google Scholar]
- 26.Drolet BC, Schwede M, Bishop KD, Fischer SA. Compliance and falsification of duty hours: reports from residents and program directors. J Grad Med Educ. 2013;5(3):368–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goitein L, Ludmerer KM. Resident workload-let’s treat the disease, not just the symptom. JAMA Intern Med. 2013;173(8):655–6. [DOI] [PubMed] [Google Scholar]
- 28.ACGME. Common Program Requirements. 2017. [Google Scholar]
- 29.Anderson C, Ftouni S, Ronda JM, Rajaratnam SMW, Czeisler CA, Lockley SW. Self-reported drowsiness and safety outcomes while driving after an extended duration work shift in trainee physicians. Sleep. 2017. [DOI] [PubMed] [Google Scholar]
- 30.Basner M, Dinges DF, Shea JA, Small DS, Zhu J, Norton L, et al. Sleep and Alertness in Medical Interns and Residents: An Observational Study on the Role of Extended Shifts. Sleep. 2017;40(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang AD, Chung JW, Dahlke AR, Biester T, Quinn CM, Matulewicz RS, et al. Differences in Resident Perceptions by Postgraduate Year of Duty Hour Policies: An Analysis from the Flexibility in Duty Hour Requirements for Surgical Trainees (FIRST) Trial. J Am Coll Surg. 2017;224(2):103–12. [DOI] [PubMed] [Google Scholar]
- 32.Rosen IM, Gimotty PA, Shea JA, Bellini LM. Evolution of sleep quantity, sleep deprivation, mood disturbances, empathy, and burnout among interns. Acad Med. 2006;81(1):82–5. [DOI] [PubMed] [Google Scholar]
- 33.Shanafelt TD, Hasan O, Dyrbye LN, Sinsky C, Satele D, Sloan J, et al. Changes in Burnout and Satisfaction With Work-Life Balance in Physicians and the General US Working Population Between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–13. [DOI] [PubMed] [Google Scholar]
- 34.Soderstrom M, Jeding K, Ekstedt M, Perski A, Akerstedt T. Insufficient sleep predicts clinical burnout. J Occup Health Psychol. 2012;17(2):175–83. [DOI] [PubMed] [Google Scholar]
- 35.West CP, Tan AD, Shanafelt TD. Association of resident fatigue and distress with occupational blood and body fluid exposures and motor vehicle incidents. Mayo Clin Proc. 2012;87(12):1138–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Axelrod L, Shah DJ, Jena AB. The European Working Time Directive: an uncontrolled experiment in medical care and education. Jama. 2013;309(5):447–8. [DOI] [PubMed] [Google Scholar]
- 37.Temple J Resident duty hours around the globe: where are we now? BMC Med Educ. 2014;14 Suppl 1:S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pattani R, Wu PE, Dhalla IA. Resident duty hours in Canada: past, present and future. Cmaj. 2014;186(10):761–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grimmond T, Good L. Exposure Survey of Trends in Occupational Practice (EXPO-S.T.O.P.) 2015: A national survey of sharps injuries and mucocutaneous blood exposures among health care workers in US hospitals. Am J Infect Control. 2017;45(11):1218–23. [DOI] [PubMed] [Google Scholar]