Abstract
This review article addresses the various aspects of nano-biomaterials used in or being pursued for the purpose of promoting bone regeneration. In the last decade, significant growth in the fields of polymer sciences, nanotechnology, and biotechnology has resulted in the development of new nano-biomaterials. These are extensively explored as drug delivery carriers and as implantable devices. At the interface of nanomaterials and biological systems, the organic and synthetic worlds have merged over the past two decades, forming a new scientific field incorporating nano-material design for biological applications. For this field to evolve, there is a need to understand the dynamic forces and molecular components that shape these interactions and influence function, while also considering safety. While there is still much to learn about the bio-physicochemical interactions at the interface, we are at a point where pockets of accumulated knowledge can provide a conceptual framework to guide further exploration and inform future product development. This review is intended as a resource for academics, scientists, and physicians working in the field of orthopedics and bone repair.
Keywords: bone regeneration, biomaterials, nanomaterials, delivery systems, stem cells
Introduction
Bone undergoes self-repair of small defects due to the synergistic actions of mesenchymal cells, osteogenic cells, and cells of the immune system (Marsell and Einhorn, 2011). This self-repaired bone contains physico-chemical and mechanical properties that recapitulate the bone which was replaced (Dimitriou et al., 2011). However, larger defects are unable to undergo the same level of self-healing, and regenerative medicine approaches are paramount in addressing these clinical challenges (Ho-Shui-Ling et al., 2018).
Autologous and allograft bone are generally considered the clinical standard-of-care for bone repair (Grabowski and Cornett, 2013; Gupta et al., 2015), despite critical limitations such as supply and quality of host bone, donor site morbidity (Angevine et al., 2005; Gruskay et al., 2014), and immunogenicity, respectively (Stevenson and Horowitz, 1992; Bauer and Muschler, 2000). Osteoinductive growth factors, in particular recombinant human bone morphogenetic protein-2 (rhBMP-2), have demonstrated remarkable efficacy, but a number of concerns and controversies exist regarding the safety of their clinical use and high cost (Burkus et al., 2002, 2003; Carragee et al., 2011; Singh K. et al., 2014; Vavken et al., 2016; Zadegan et al., 2017). Although numerous synthetic bone graft substitutes are available, the problem of delayed and/or compromised healing remains a significant clinical challenge (Zura et al., 2016; Fernandez et al., 2020).
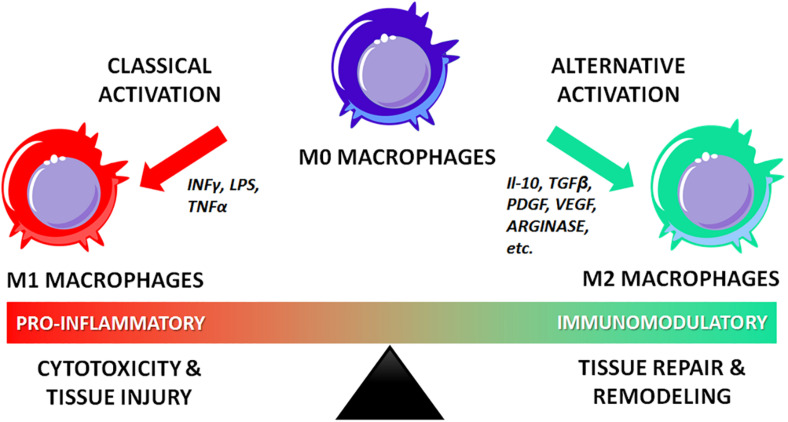
The ideal biomaterials for bone regeneration should not only be biocompatible and osteoconductive but also osteoinductive. They should be able to leverage the self-healing capabilities of the bone by (i) providing the main structural, compositional, and biochemical cues for the formation of new tissue; (ii) engaging the host’s resident immune cells in the regenerative response; (iii) promoting the recruitment, proliferation, and differentiation of progenitor cells; and (iv) recovering an adequate local blood supply to support healing and remodeling (Schmidt-Bleek et al., 2014; Minardi et al., 2015a).
Recently, nanotechnology has become a domain with breakthrough potential to further propel the field of bone regeneration. Nanostructured biomaterials have proven superior at enhancing bone regeneration due to their unique chemical and physical properties (e.g., magnetic, electrical) that are uniquely different from their bulk counterparts (Perez et al., 2013; Wang Q. et al., 2016). These differences stem from an ability to be engineered to precisely mimic the composition and nanoarchitecture of bone, while allowing for the recapitulation of crucial characteristics of its biochemical milieu at the nanoscale (Minardi et al., 2016b). This translates in improved ability to engage the host’s immune and progenitor cells at the nanoscale, resulting in enhanced outcomes (Cheng et al., 2013).
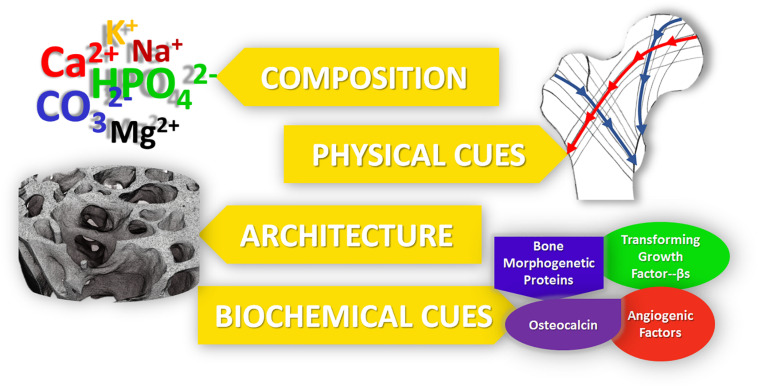
In the rational design of regenerative nanotechnologies for bone regeneration, four crucial elements of bone should be considered and recapitulated as closely as possible: (i) composition, (ii) physical stimuli, (iii) architecture and (iv) biochemical cues, as summarized in Figure 1. Inspired by mimicking these 4 fundamental characteristics of bone, a plethora of nanostructured materials have been developed over the last decade to elicit bone regeneration. Technologies that recapitulate more than one of these four fundamental elements have been shown to lead to superior outcomes. This review highlights such ongoing work in the field of nanostructured materials for bone regeneration and their potential in clinical practice.
FIGURE 1.
The five main properties of bone, which should be recapitulated into bone regenerative strategies for improved outcomes.
Mimicking Bone Composition: Bioceramics and Composite Nanostructured Biomaterials
Bioceramics
Bone is a natural nanostructured composite, consisting of approximately 60% (dry weight) mineral, mostly nano-apatite—which is a calcium phosphate (CaP) ceramic (Minardi et al., 2015a). Accordingly, a number of bioceramics containing calcium and phosphorous have been proposed for bone regeneration (Hench et al., 2014; Jones et al., 2016). Of these, CaP materials most closely mimic the mineral phase of bone and have demonstrated relatively greater osteoinductivity, making CaP a common material of choice for bone grafts. A number of bioceramics have been used clinically for several decades (Szpalski and Gunzburg, 2002; Giannoudis et al., 2005; Campana et al., 2014; Fernandez de Grado et al., 2018), both for load- and non-load- bearing applications (Roberts and Rosenbaum, 2012). While conventional bioceramics had poor mechanical properties and unfavorable biodegradability and porosity (Fielding and Bose, 2013; Wen et al., 2017), the latest generation of bioceramics are structured at the nanoscale and have significantly improved bioactivity, biodegradation and mechanical properties, and are reviewed below. Their advantages and disadvantages are summarized in Table 1.
TABLE 1.
Summary of the main nanostructured calcium-phosphate based materials for bone regeneration, with their respective advantages and disadvantages.
| Advantages | Disadvantages | References | |
| Nanostructured Bioceramics | |||
| Nano-bioglasses | Biocompatible | Suboptimal Biodegradation | Vallet-Regí et al., 2003; Izquierdo-Barba et al., 2013; Ducheyne, 2015; Islam et al., 2017; Mancuso et al., 2017 |
| Enhanced bone integration | Poor mechanical properties | ||
| Improved biodegradation | |||
| Hydroxyapatite | High biocompatibility | Poor mechanical properties | Liou et al., 2004; Capuccini et al., 2008; Boanini et al., 2010; Tampieri et al., 2012; Zofková et al., 2013 |
| Resembles mineral phase of bone | |||
| Can be doped with multiple ions to closely mimic bone mineral | Slow degradation rates in vivo | ||
| Osteoconductive | |||
| Can be used in a plethora of formulations (e.g., powder, solid scaffold, cement, coatings) | Limited osteoinductivity | ||
| High biocompatibility | |||
| Tricalcium phosphate | Provides main bulding blocks for new matrix deposition | Poor mechanical properties | Shepherd and Best, 2011; Sadat-Shojai et al., 2013; Vahabzadeh and Bose, 2017; Sergi et al., 2018 |
| Can be doped with multiple ions to tune bioactivity and degradation | |||
| Osteoconductive | |||
| Can be used in a plethora of formulations (e.g., powder, solid scaffold, cement, coatings) | |||
| Faster in vivo degradation | |||
| Nanocomposites | |||
| Ceramic/polymer composites (e.g., HA/PLGA, HA/Alginate) | High biocompatibility | May have limited osteoinductivity | Kim et al., 2005; Miao et al., 2005; Tampieri et al., 2005; Heo et al., 2009; Akman et al., 2010; Bernstein et al., 2010; Cruz, 2010; Bhumiratana et al., 2011; Wang Z. et al., 2016; Zhu et al., 2017; Bian et al., 2019 |
| Ease of fabrication | Fabrication requires organic solvents | ||
| Can be used to prepare scaffolds with complex 3D architecture | |||
| Improved mechanical properties of scaffolds | |||
| Tunable degradation rate | |||
| Bio-hybrid composites | High biocompatibility | Poor mechanical properties (not load bearing) | Tampieri et al., 2008; Tampieri et al., 2011; Minardi et al., 2015a; Minardi et al., 2019 |
| Fabrication not requiring organic solvents | |||
| Highly biomimetic | |||
| Excellent bioactivity | |||
Hydroxyapatite-Based Ceramics
Among CaP ceramic phases, synthetic hydroxyapatite (HA) has been the one most extensively studied due to its biocompatibility and resemblance to the composition of natural bone mineral (Sadat-Shojai et al., 2013; Šupová, 2015). First generation materials were fabricated with stoichiometric HA [Ca10(PO4)6(OH)], which has been successfully synthesized and mass produced through several synthesis strategies, including hydrothermal reactions, sol–gel syntheses, and mechanochemical syntheses (Kalita and Bhatt, 2007). However, natural bone mineral is produced in a very dynamic environment with numerous ions present (e.g., Mg2+, K+, Na+, CO, HPO), which frequently substitute ions in the apatite lattice. The apatite present in natural bone is calcium deficient and is characterized by a Ca/P ratio lower than the typical 1.67 of stoichiometric HA (Kalita and Verma, 2010; Dziadek et al., 2017). Ion substitution plays an important role in maintaining the low crystallinity of bone apatite, which is crucial for bone metabolism. This low crystallinity may correspond to higher reactivity in vivo, resulting in faster bone formation and remodeling (Minardi et al., 2015a). In contrast, stoichiometric HA is more crystalline and stable in aqueous solutions, resulting in a less biodegradable material that could impede the formation of new bone through the entirety of a defect space or osteointegration with the surrounding matrix (Liou et al., 2004; Tampieri et al., 2012). To overcome these limitations, numerous biomimetic multi-substituted nano HAs have been developed to mimic the natural mineral phase of bone and enhance bioactivity and solubility (Boanini et al., 2010; Zofková et al., 2013).
Various substituted nanostructured HAs have been proposed, some of which have been used as tools to fine-tune or stimulate specific biological functions. For example, Mg2+ plays a vital role in osteogenesis and is present in young and newly formed bone (De Bruijn et al., 1992). Landi et al. (2006) found that Mg-substituted HA showed enhanced cell adhesion, proliferation, and metabolic activity compared to HA. Due to the smaller ionic radius of Mg2+ relative to Ca2+, the Mg-substituted structure is more unstable when incorporated into the crystal lattice (Fadeev et al., 2003). Mg is also thought to induce nitric oxide production in endothelial cells, a critical component of angiogenesis (Maier et al., 2004). Sr acts to enhance bone formation in vivo by inhibiting osteoclast-mediated bone resorption while upregulating osteoblast activity (Li et al., 2009; Ozturan et al., 2011), which is why Sr-based drugs have been long used to treat osteoporosis (e.g., strontium renelate; Capuccini et al., 2008). Thus, Sr-doped nano-HA has also been extensively used in bone regenerative strategies (Wong et al., 2004; Frasnelli et al., 2017; Neves et al., 2017; Ratnayake et al., 2017). Similarly, substitution with Zn has been shown to enhance osteogenic activity (Ren et al., 2009), with a proposed mechanism of inhibiting osteoclast resorption and upregulating osteoblastic activity (Hadley et al., 2010; Yamaguchi and Weitzmann, 2011). More recently, Tampieri et al. (2010) proposed a conceptually new type of nanostructured calcium-deficient HA, by substituting it with Fe2+ and Fe3+ to endow the HA with superparamagnetic properties. This magnetic behavior may potentially be exploited for bone regeneration purposes to enhance osteogenesis (Tampieri et al., 2012).
Alternatively, a common anionic substitution involves CO replacement of the phosphate group within nano-HA, which may influence bone turnover and metabolism (Du et al., 2019). When incorporated in HA, it showed enhanced osteoconductive potential compared to pure HA (Du et al., 2019), while increasing its solubility due to its decreased crystallinity (Wang and Nancollas, 2008). In contrast to these effects, F– doped HA results in decreased solubility (Kim et al., 2004) and increased strength, therefore reducing the brittleness of the CaP (Bianco et al., 2010). Si-HA showed instead improved osteoblast attachment and differentiation, and decreased osteoclast differentiation in vivo (Matesanz et al., 2014).
Tricalcium Phospohate-Based Ceramics
Another popular type of CaP ceramic used extensively in orthopedics is tricalcium phosphate (TCP). Two types of TCP have been pursued for bone regeneration: α-TCP and β-TCP. They differ in their atomic arrangements (Wen et al., 2017), but both have a Ca/P ratio of 1.5 (Wen et al., 2017). β-TCP has become the TCP of choice, given its superior rate of degradation and bioactivity over α-TCP (Kamitakahara et al., 2008; Ghanaati et al., 2010). Hydroxyapatite and TCP can also be combined in varying ratios within composite scaffolds to tune degradation and potentially enhance osteoconductive and osteoinductive properties (Daculsi, 1998; Arinzeh et al., 2005; Samavedi et al., 2013). Similar to HA, TCPs can also undergo ion-substitution as a tool to create ceramic-based materials that target specific biological pathways in vivo. For example, Mg-doped β-TCP and Sr-doped β-TCP-based materials have shown improved bone healing through accelerated osteogenesis and angiogenesis in a large animal model (Bose et al., 2011; Tarafder et al., 2015), with improved mechanical strength compared to the pure TCP scaffolds (Tarafder et al., 2015). Similar to Fe-doped HA, Fe-doped TCP stabilized the β-TCP phase, and osteoblasts showed enhanced cell adhesion to doped-TCP relative to pure TCP (Vahabzadeh and Bose, 2017). Moreover, cell proliferation was reportedly enhanced in TCP doped with other ions, such as Mg2+, Zn2+, Sr2+, and Li+ (Vahabzadeh and Bose, 2017).
Using these ceramic phases, numerous types of nanostructured 3D scaffolds (and bone cements) have been prepared through a variety of ways, including dry methods, wet methods, and high temperature methods (Sadat-Shojai et al., 2013). Dry methods include solid-state and mechanochemical reactions. The solid-state and mechanochemical technique have the advantage of a simple procedure for large scale production, whereas the mechanochemical technique reliably produces a specific nanostructure (Sadat-Shojai et al., 2013). Wet methods are commonly used and include techniques including but not limited to sol–gel synthesis and hydrothermal synthesis. These methods have the advantage of producing nanoparticles with a consistent morphology and size (Shepherd and Best, 2011; Sadat-Shojai et al., 2013). The downfall of these techniques is that the products can often have multiple phases present (Sadat-Shojai et al., 2013). High temperature processes such as combustion and pyrolysis are capable of bypassing the problem of multiple phases, however control over the byproducts limits this method’s applications (Sadat-Shojai et al., 2013). Moreover, there a numerous techniques to introduce porosity within 3D CaP scaffolds, including a polymeric sponge technique (Monmaturapoj and Yatongchai, 2011), foaming technique (Sopyan et al., 2007), supercritical foaming technique (Diaz-Gomez et al., 2017), gel casting of foams (Sopyan et al., 2007), and slip casting (Sopyan et al., 2007). Although all of these nanostructured ceramics are limited by poor mechanical properties, their strong osteoconductive potential makes them attractive for use as coating materials for load bearing implants, where such use may enhance osteointegration or even have antibacterial properties (Sergi et al., 2018).
Although nanostructured calcium-deficient CaP materials have provided enhanced biomimicry of the mineral phase of native bone, they have not proven capable of recapitulating all of its subtle and complex physiochemical properties. Thus, strategies based on nanostructured composites have been developed to fulfill this goal.
Nanostructured Composites
Biomimicry is an increasingly popular strategy in regenerative medicine, aiming to engineer materials that closely resemble the target tissue (Nandakumar et al., 2013). Since bone is a natural composite—made of an inorganic component (mostly multi-substituted HA) and an organic component (mostly type I collagen)—researchers have long focused on developing nanostructured ceramic/polymer composite materials with the purpose of recreating the composition and function of natural bone. Nanostructured composites for bone regeneration leverage the osteoconductivity of synthetic CaP ceramic phases and the unique mechanical properties of polymers. For example, both synthetic polymers like poly(L-lactic acid) (PLLA; Cruz, 2010; Zhu et al., 2017), poly(e-caprolactone) (PCL; Heo et al., 2009; Bernstein et al., 2010), poly(lactic-co-glycolic acid) (PLGA; Miao et al., 2005; Wang Z. et al., 2016) as well as naturally occurring polymers such as gelatin (Kim et al., 2005), silk (Bhumiratana et al., 2011), chitosan (Akman et al., 2010), alginate (Tampieri et al., 2005), and collagen (Bian et al., 2019) have been combined with HA and TCP to fabricate a plethora of composite materials over the past three decades. These composites have been fabricated in a myriad of ways: electrospinning, gas foaming, solvent casting and particulate leaching, phase separation, and melt mixing have been widely used to fabricate scaffolds (Alizadeh-Osgouei et al., 2019). The major drawback, common to all these approaches in the manufacturing of porous structures is the inability of conventional methods to completely control the architecture of scaffolds, such as pore size and interconnections. Furthermore, the use of solvents required by some of these methods can impact scaffold biocompatibility (Alizadeh-Osgouei et al., 2019). Additive manufacturing is a new and modern technique that shows great potential to offer complete control of architectural details such as pore size, which significantly affects the properties of ceramic-based scaffolds. 3D-printing techniques have received much attention due to the capacity to fabricate specific and complex structures (further discussed in paragraph 4) (Kumar et al., 2019).
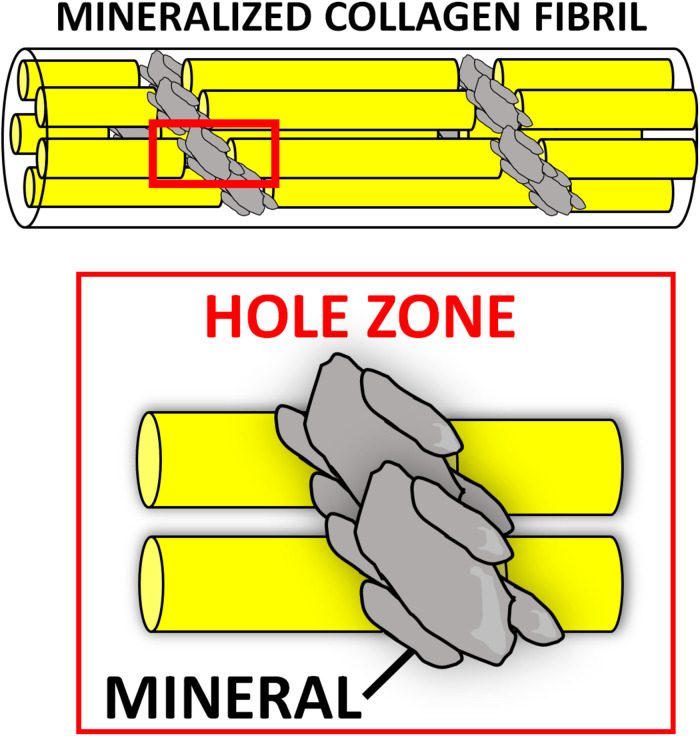
Numerous composite materials have been fabricated with natural polymers, with the underlying hypothesis that mimicking natural bone matrix would harness regeneration. A plethora of CaP/natural polymer composites have been described. The first generation of such composites was prepared by blending the desired ceramic phase with the natural polymer of choice in aqueous solutions (Ridi et al., 2017). Although these materials contained the two main components of bone matrix, they lacked vital chemical, physical, and topographical information at the nanoscale, which cells need to repair bone (Tampieri et al., 2011). The organic matrix (mostly type I collagen) of natural bone acts as a template for the nucleation of the mineral phase, directing its deposition, and guiding the growth of the mineral crystals along its fibers via interaction of its functional groups (e.g., carbonyl groups) with the apatite crystals. It is believed that the mineralization begins in correspondence of the hole zones of the collagen fibrils (intrafibrillar mineralization) (Figure 2). This highly regulated chemical-physical interaction between the inorganic and organic phase not only directs the orientation of the forming apatite crystals, but also limits their crystallinity, which is paramount to the formation of a nanocomposite material (i.e., bone extracellular matrix [ECM]) (Kim D. et al., 2018). The unique characteristics of both stiffness and flexibility of the bone result from this intimate interaction between these two components (Nair et al., 2014). Thus, several groups have focused on the development of biologically inspired synthesis methods to mineralize natural polymers by mimicking the process of bone biomineralization. In these syntheses, the ceramic phase is deposited onto the organic template during its self-assembly through a pH-driven process which resembles that of bone biomineralization. Using this synthetic approach, the mineral phase is not simply mixed with the organic template, but nucleated directly onto it and intimately bonded to the organic matrix, resulting in nanostrustured “bio-hybrid composites” (Minardi et al., 2015a). Accordingly, many studies have described the bio-inspired mineralization with nanoapatite phases of several natural polymers, such as chitosan (Palazzo et al., 2015), alginate (Tampieri et al., 2005), gelatin (Landi et al., 2008), and type I collagen (Tampieri et al., 2008). The main advantages of these materials are: (i) their ability to mimic bone matrix at the nanoscale, storing the crucial nano-compositional and topographical information necessary for cell migration, proliferation and osteogenic differentiation (Minardi et al., 2015a); (ii) their high degree of interconnected porosity, conventionally achieved by freeze-drying (Wu et al., 2010a), which facilitates cell infiltration and neovascularization (O’Brien et al., 2004); (iii) their syntheses do not require harsh conditions, allowing for the incorporation of a variety of delivery systems and bioactive molecules (Minardi et al., 2016b). This class of nano bone substitutes has shown great promise in a plethora of in vitro studies as well as in non-load bearing in vivo models. More recently, increasingly sophisticated bio-hybrid composites were developed, which appear able to incorporate multi-substituted biomimetic apatite phases. For example, a Mg-doped apatite/type I collagen nanocomposite was shown to closely resemble the structure and composition of the human trabecular bone niche, significantly improving the osteogenic differentiation of human mesenchymal stem cells (MSCs) in vitro and bone regeneration in both ectopic (Minardi et al., 2015a) and orthotopic large animal models (Minardi et al., 2019). Using this biologically inspired synthesis method, some researchers are currently working to develop bio-inspired hybrid nanocomposites with enhanced osteogenic features endowed with magnetic properties (D’Amora et al., 2016; Tampieri et al., 2016). Their potential for bone regeneration will be discussed further in section “Magnetically Responsive Materials” of this review.
FIGURE 2.
Intrafibrillar mineralization occurring during bone biomineralization. The nucleation of the mineral (gray) is thought to begin at the “hole zones” of the collagen fibrils (in red box), between single collagen molecules (yellow), as depicted in this schematic.
Nanostructured Bio-Glasses
Bioactive glasses are mainly comprised of calcium oxide, silicate, borate, and phosphorous (Hench et al., 2014). By varying the relative amounts of these components, different bioactive glasses can be manufactured and, over the past three decades, many variants have been proposed for bone regenerative applications (van Vugt et al., 2017). Several are available clinically (Jones et al., 2016), and have demonstrated biocompatibility, osteoconductivity, and biodegradability (Kong et al., 2018).
Bioglasses can be prepared by melt–quench or sol–gel process (Vichery and Nedelec, 2016). While the first generations of bioglasses were solid or macroporous, the latest nanostructured versions, synthesized through the sol–gel approach, have unique nanostructural features, including improved nanotextural properties, highly ordered structure, and controlled pore size and pore interconnectivity (Islam et al., 2017; Mancuso et al., 2017). Such nano-features greatly enhance osseointegration compared to first generation bulk bioglasses. The graft-bone integration begins with the solubilization of surface ions resulting in a silica gel layer. A nanostructured calcium phosphate phase (i.e., hydroxyapatite) starts to nucleate on this layer, activating local osteoblasts to form new bone (Ducheyne, 2015). This mechanism contributes to the nano-bioglass degradation, while promoting bone formation. Even their degradation depends on their composition and nanostructure and can be tailored from days to months; for example, borate-based bioglasses have been shown to degrade much faster than silicate varieties (Balasubramanian et al., 2018; Furlan et al., 2018). Recent studies showed that increasing the surface area and porosity of nanostructured bioglasses can greatly accelerate their biodegradation, as well as biointegration (Kong et al., 2018).
The ability to release bioactive ions during degradation is one of the most important features of these bioglasses (Mouriño et al., 2019). For instance, it is known that the early vascularization of biomaterials plays an essential role in bone regeneration (Almubarak et al., 2016). Toward this end, numerous nanoparticles and mesoporous bioactive glasses have been specifically developed to enhance not only osteogenesis but also early angiogenesis through the release of pro-angiogenic ions (Kim J.-J. et al., 2017). Namely, strontium-doped bioglass nanoparticles have shown to increase both osteoblast activity (Fiorilli et al., 2018; Leite et al., 2018; Zhao et al., 2018), as well as induce osteoblasts to secrete angiogenesis-associated cytokines for early vascularization, ultimately resulting in improved bone repair (Zarins et al., 2016; Zhao et al., 2018). Similarly, bioglasses releasing copper or cobalt ions have also been proposed, due to their angiogenic properties (Bari et al., 2017; Weng et al., 2017; Kargozar et al., 2018; Zheng et al., 2018). Silver- (Kaya et al., 2018) or manganese-doped nanobioglasses (Nawaz et al., 2018) have instead been developed to deliver antimicrobial activity, and to aid in the healing process by preventing infections.
Due to their highly ordered mesopores and surface area, nanobioglasses can also be excellent delivery vehicles for bioactive molecules (e.g., drugs and proteins) to further boost bone repair (Baino et al., 2017; Wang et al., 2019; Lalzawmliana et al., 2020). For example, Lee J.-H. et al. (2017) reported a significant enhancement in osteoblast activity, secretion of ECM molecules and calcification through the controlled release of phenamil (a drug known as a potent BMP signaling activator) and strontium ions from mesoporous bioglass nanoparticles. In recent proof-of-concept in vivo studies, others have demonstrated how mesoporous nanobioglasses can also be an ideal delivery system for growth factors, such as IGF (Lalzawmliana et al., 2019) or FGF (Kang et al., 2015), with significantly imporved regenerative outcomes in preclinical animal models.
Mimicking the Electrical Environment of Bone: Nanomaterials Harnessing Piezoelectricity, Conductivity and Magnetism
The field of bone mechanobiology has vastly improved since the advent of nanotechnology, expanding our fundamental knowledge of how mechanical forces regulate the process of bone homeostasis and remodeling (Chen et al., 2010). Although the origin remains a topic of debate, mechanical stress-generated electric potentials are known to be important in modulating cellular behavior to control growth and the remodeling process (Perez et al., 2015; Ribeiro et al., 2015b; Zhang et al., 2016). In addition to stress-generated potentials, electric fields present endogenously in living tissues, as well as electrical stimulation applied externally have also been shown to influence cell behavior and promote tissue growth (McCaig et al., 2005; Balint et al., 2013; Kang et al., 2014; Reid and Zhao, 2014; Funk, 2015). Accordingly, manipulation of the electrical environment has emerged as a promising strategy to enhance bone regeneration, with nanotechnological approaches offering tremendous potential for achieving this aim. Collectively, the nanomaterials recapitulating or leveraging the physical stimuli naturally present in the bone can be categorized as (i) piezoelectric, (ii) electrically conductive, and (iii) magnetic materials and are briefly summarized in Table 2. The impact of nanotechnology on their development and rational design is reviewed below.
TABLE 2.
Advantages and disadvantages of nanostructured materials harnessing physical stimuli for bone regeneration.
| Advantages | Disadvantages | References | |
| Nanostructured piezoelectic materials | |||
| Piezoelectric Ceramics (e.g., BT, BN, ZnO) | Robust piezoelectric characteristics Desirable osteoinductive potential |
Potential for cytotoxicity | Maeder et al., 2004; Boccaccini and Blaker, 2005; Opoku et al., 2015; Panda and Sahoo, 2015; Rocca et al., 2015; Fernandes et al., 2016; Li X. et al., 2016; Zhang et al., 2016; Bramhill et al., 2017; Damaraju et al., 2017; Ribeiro et al., 2017; Tajbakhsh and Hajiali, 2017; Ehterami et al., 2018; Kao et al., 2019 |
| Piezoelectric Polymers (e.g., PVDF and its copolymers, PLLA, PHBV) | Biocompatibility and non-toxicity Manufacturing flexibility High strength and impact resistance |
Unfavorable biodegradability | |
| Piezoelectric Polymer-Ceramic Composites | Ability to tailor and enhance several properties of the composite construct: mechanical properties, piezoelectric coefficient, biodegradability, bioactivity | Lack of data regarding the piezoelectric properties of certain composite materials | |
| Nanostructured electrically conductive materials | |||
| Conductive Nanomaterials (non-polymeric, e.g., graphene, gold nanoparticles) | Excellent mechanical properties High electrical conductivity ensuring reliable delivery of bioelectric signals |
Non-degradability Questions/concerns regarding biocompatibility and long-term safety |
Kim S. et al., 2011; Otero et al., 2012; Bitounis et al., 2013; Liu et al., 2013; Nurunnabi et al., 2015; Sridhar et al., 2015; Assaf et al., 2017; Kim J.W. et al., 2017; Silva et al., 2017; Wang et al., 2017; Zhou et al., 2017; Chan et al., 2018; Cheng et al., 2018; Lalegul-Ulker et al., 2018 |
| Conductive Nanopolymers (e.g., polyheterocycle family of conductive polymers) | Improved biocompatibility and biodegradability Manufacturing flexibility |
Unfavorable mechanical properties and processability Relative lack of animal studies evaluating in vivo performance |
|
| Nanostructured Magnetically Responsive Materials | |||
| Magnetic Nanoparticles (MNPs) and Magnetoelectric Composites | Superparamagnetic properties Ability to deliver cues via remote (external) stimulation |
Uncertain biocompatibility and long-term safety | Pisanic et al., 2007; Häfeli et al., 2009; Huang et al., 2009; Bock et al., 2010; Wu et al., 2010b; Wu Y. et al., 2010; Wei et al., 2011; Zhu et al., 2011; Panseri et al., 2012; Tampieri et al., 2012; Alarifi et al., 2014; Singh R.K. et al., 2014; Shen et al., 2015; Li X. et al., 2016; Ribeiro et al., 2016; Yun et al., 2016 |
Piezoelectric Materials
Piezoelectricity is observed when a mechanical deformation causes the formation of a net dipole moment and subsequent polarization of the material (Tichý, 2010). Bone is a piezoelectric nanostructured material, and this property was invoked as a potential mechanism by which cells could detect and respond to mechanical stress (Fukada and Yasuda, 1957). The role for piezoelectricity in bone remodeling continues to be debated, and there has been renewed appeal for its physiologic importance in the process of bone mechanosensation (Halperin et al., 2004; Noris-Suarez et al., 2007). As such, with the emergence of nanotechnological approaches there has been a rapid increase in the number of publications on piezoelectric materials for bone regeneration (Tandon et al., 2018). They can be thought of as sensitive mechano-electrical transducers, and as such, they are typically applied to the implantation areas which are exposed to mechanical loads (Zhang K. et al., 2018; Chorsi et al., 2019). A number of different piezoelectric materials have been investigated for bone regeneration applications, which are briefly reviewed here.
Inorganic Piezoelectric Materials: Piezoelectric Ceramics
Nanopiezoceramic materials investigated for bone regeneration applications include barium titanate (BT), boron nitride (BN), and zinc oxide (ZnO). While these materials possess a high piezoelectric coefficient, some of them display lower biocompatibility at high doses, which can represent a major limitation for their use in tissue engineering applications (Maeder et al., 2004; Opoku et al., 2015; Panda and Sahoo, 2015; Kao et al., 2019). Nevertheless, each of these piezoceramics has shown osteoinductive capabilities in vitro, supporting their use in the development of bone regenerative biomaterials, where they are often incorporated in a variety of ways into 3D scaffolds in order to impart piezoelectric characteristics to augment bone formation. For example, BT nanoparticles have been shown to enhance the osteogenic differentiation of MSCs, and osteoblastic cells demonstrated superior adhesion, proliferation, and migration into the pores of scaffolds comprised of BT, while BN nanotubes (BNNTs) demonstrate high protein adsorption ability and promotion of enhanced MSC attachment, proliferation, and osteogenic differentiation (Rocca et al., 2015; Li X. et al., 2016; Tajbakhsh and Hajiali, 2017; Ehterami et al., 2018). Finally, the incorporation of ZnO nanoparticles has proven capable of enhancing both the bioactivity and even the mechanical properties of such composite materials (Shalumon et al., 2011; Feng et al., 2014; Kao et al., 2019).
Organic Piezoelectric Materials: Piezoelectric Polymers
Piezoelectric polymers have also received increasing attention for bone regeneration applications in recent years (Tichý, 2010). Typically fabricated either as films, rods, or tubes/fibers (Ribeiro et al., 2015b), they exhibit sound mechanical properties, including superior strength and impact resistance when compared to inorganic materials. Biocompatibility, piezoelectric activity, and significant osteogenic capacity have also been demonstrated both in vitro and in vivo (Zhang et al., 2016; Damaraju et al., 2017; Ribeiro et al., 2017; Kao et al., 2019). Among these, PVDF [poly(vinylidene fluoride)] and its copolymers, PLLA, and PHBV (poly-3-hydroxybutyrate-3-hydroxy valerate) are the most studied.
Poly(vinylidene fluoride) and its copolymers can provide the necessary electromechanical stimulation for the differentiation of human MSCs into the osteogenic lineage in vitro (Damaraju et al., 2013, 2017; Nunes-Pereira et al., 2015; Ribeiro et al., 2015a; Zhang et al., 2016), as well as the capacity to effectively promote bone regeneration in vivo in rodent models (Zhang et al., 2016; Ribeiro et al., 2017). In addition to its potential utility as a bone graft substitute, PVDF has also shown promise as a suitable coating for existing implant materials in order to enhance osteogenesis (Zhou Z. et al., 2016). The primary concern with PVDF and its copolymers is the lack of biodegradability, which limits clinical potential. This limitation is being addressed with the development of newer-generation piezoelectric polymer-based materials with tailorable degradation properties. Poly-3-hydroxybutyrate-3-hydroxy valerate and PLLA, both of which are biodegradable, have emerged as promising candidates (Duan et al., 2011), demonstrating osteogenic capacity both in vitro and in vivo (Ikada et al., 1996; Sultana and Wang, 2012; Wang et al., 2013). PLLA has also been explored for bone regeneration utility beyond its use as a bone graft substitute. Due to its biodegradability, non-toxicity, and advantageous mechanical properties, PLLA is an attractive material for clinical application in the fabrication of biodegradable fixation devices such as screws, pins, and suture anchors, where a bioresorbable implant is desirable to avoid the risk of complicating revision surgery or the requirement for an additional procedure for implant removal (Bucholz et al., 1994; Barber et al., 1995; Prokop et al., 2005; Gkiokas et al., 2012).
Piezoelectric Polymer – Ceramic Composite Materials
Piezoelectric polymers and ceramics have also been used in combination to fabricate a variety of composite materials (Boccaccini and Blaker, 2005; Bramhill et al., 2017). Polymer matrix composites harness the manufacturing flexibility afforded by polymers and the substantial piezoelectric properties of otherwise brittle ceramics to produce complex forms ideally suited to support bone formation, including porous scaffolds (Zhang et al., 2014; Liu et al., 2016), layered structures (Dubey et al., 2015), nanoparticles (Marino et al., 2015, 2017; Niskanen et al., 2016), and dense disks (Dubey et al., 2013). Of the polymer matrix composites, PLLA-based composites have been used most extensively in the field of bone regeneration (Fernandes et al., 2016; Tajbakhsh and Hajiali, 2017). Composite membranes incorporating PVDF-TrFE and BT have also been found to support bone formation in several investigations (Gimenes et al., 2004; Scalize et al., 2016; Zhang et al., 2016), suggesting significant potential for clinical application owing to the improved osteogenic capability demonstrated in vitro and in vivo in rodent bone defect models. Of the ceramic matrix composites, HA/BT-based materials are the most studied, with a number of studies demonstrating the osteoinductive capability of such composites (Jianqing et al., 1997; Baxter et al., 2009; Dubey et al., 2014; Jiao et al., 2017; Ehterami et al., 2018).
The emergence of piezoelectric materials and their rapidly increasing usage has motivated investigators to adopt new and innovative approaches to create biomaterials with desirable properties. Techniques which are gaining interest include 3D printing (Kim et al., 2014; Schult et al., 2016; Bodkhe et al., 2017), fabrication of piezoelectric nanofibers using solution blow spinning (Bolbasov et al., 2014, 2016; Daristotle et al., 2016), and the development of systems capable of applying controlled mechanical stimulation to piezoelectric scaffolds (Trumbull et al., 2016; Zhou X. et al., 2016).
A lack of quantitative data on the piezoelectric coefficient of many composite materials is a limitation to this newly emerging class of materials. However, although this area of research remains in its relative infancy, nanopiezoelectric materials show tremendous promise for bone regeneration.
Electrically Conductive Materials
In cases when the patient is immobilized, whether due to a fracture or other health condition, or in a non-load bearing healing setting, the natural mechanical stimulus does not occur and the effectiveness of piezoelectric materials is subsequently diminished (Mehta et al., 2012). Such limitations call for the development of new approaches capable of delivering electrical cues via alternative means, either by remote stimulation or through innovative nanomaterials activated by micromotion. Electrically conductive materials provide such an innovative tool, serving as the substrate through which external electrical stimulation is converted into bioelectric signals and delivered to the site (Chen et al., 2019).
Electrical stimulation therapy has occasionally been attempted as a supplement to promote bone healing in the case of fractures and spinal arthrodesis, although with arguable success, for decades (Gan and Glazer, 2006; Goldstein et al., 2010; Einhorn and Gerstenfeld, 2015). Researchers have more recently begun to explore conductive materials capable of propagating electrical signals to the site of repair in order to accelerate bone regeneration. Unlike piezoelectric materials, these require an externally applied power source to produce electrical signals. On one hand, this approach requires optimization of a number of different parameters including the frequency, amplitude, duration, and nature (alternating/direct) of the signal which may complicate assessment of efficacy (Dubey et al., 2011). On the other hand, it affords a great degree of control over the stimulus which cannot be achieved with the use of piezoelectric materials, allowing the functionality of the material to be tailored to its specific application.
One method for producing electroactive biomaterials capable of serving as conduits for the delivery of external electrical stimulation to cells involves the use of a polymer matrix incorporating conductive nanomaterials such as graphene (Assaf et al., 2017), carbon nanofibers (Whulanza et al., 2013), or metallic particles (e.g., gold nanoparticles) (Sridhar et al., 2015). Of these, graphene family materials have been found to possess excellent mechanical and conductive properties (Kim S. et al., 2011; Bitounis et al., 2013; Kim J.W. et al., 2017), support proliferation (Kalbacova et al., 2010) and osteogenic differentiation of MSCs (Nayak et al., 2011; Bressan et al., 2014), yield high degrees of mineralization (Lee et al., 2011; Xie et al., 2015), and even exert antimicrobial action (Pang et al., 2017). A number of graphene-based materials have been developed in the form of scaffolds, scaffold reinforcement materials, and surface coatings for existing materials, with demonstrated capacity to promote and enhance new bone formation in vivo (Silva et al., 2017; Wang et al., 2017; Zhou et al., 2017). Significant limitations to graphene and other similar electroactive materials include their non-degradability and uncertain biocompatibility, as well as questions regarding their long-term safety (Nurunnabi et al., 2015; Cheng et al., 2018).
To address these limitations, other methods of obtaining electroactive biomaterials which utilize intrinsically conductive polymers (CPs) have been explored. Such an approach offers the advantages of improved biocompatibility and biodegradability, in addition to manufacturing flexibility allowing incorporation of other components (Lalegul-Ulker et al., 2018). Among several CPs in use, the polyheterocycle family, including polypyrrole (PPy), polyaniline (PANI), and polythiophene (PTh) and its derivative poly(3,4-ethylenedioxythiophene) (PEDOT), are the most extensively studied for bone regeneration applications (Otero et al., 2012). These materials exhibit desirable electrical conductivity sufficient to promote cell proliferation and osteogenic differentiation (Liu et al., 2013), but are limited by inherently poor mechanical properties and processability (Chan et al., 2018), prompting the development of conductive polymeric composites. For example, CPs can be blended with various other natural and/or synthetic non-CPs to fine-tune degradation and mechanical properties (Kaur et al., 2015). Conductive copolymers incorporating other electroactive polymeric components provide for further enhancement of biocompatibility, biodegradability, and electroactivity (Cui et al., 2012). Conductive polymer-based conducting nanofibers, conducting hydrogels, and 3D conductive composite scaffolds are additional examples of electroactive biomaterials being explored for bone regeneration applications (Sajesh et al., 2013; Li L. et al., 2016; Guex et al., 2017; Chen et al., 2018). While numerous investigations have generated exciting results supporting the osteogenic capabilities of conducting polymers and their composites in vitro, there remains a need for more animal studies to validate the performance of this promising family of electroactive biomaterials.
Magnetically Responsive Materials
Magnetic stimulation therapy, like electrical stimulation therapy, has been used clinically for a number of years (Assiotis et al., 2012). While the underlying mechanisms of action are unclear, in vitro studies suggest that pulsed and static magnetic fields are capable of enhancing osteoblast differentiation (Jansen et al., 2010; Wang et al., 2014; Marędziak et al., 2016), and animal studies have shown promise for promoting bony healing and integration into graft materials (Fredericks et al., 2000; Puricelli et al., 2006).
When describing the magnetic behavior of a material, ferro- and ferrimagnetism refer to a material’s ability to be magnetized by an external magnetic field and remain magnetized upon its removal. Paramagnetism, on the other hand, is defined by a material’s lack of retained magnetism upon removal of the external magnetic field, a desirable property in tissue engineering applications, as aggregation of the material’s magnetic particles in vivo could lead to local toxicity (Balavijayalakshmi et al., 2014). Of particular interest are magnetic nanoparticles (MNPs) owing to their special superparamagnetic properties. Superparamagnetic behavior, exhibited by small ferro- or ferrimagnetic nanoparticles, do not retain magnetism in the absence of external magnetic fields; however, their magnetic susceptibility is much greater than that of standard paramagnetic materials, permitting precise magnetic control and functionalization for a given application (Reddy et al., 2012). Among MNPs, iron oxide nanoparticles, typically maghemite (Fe2O3) or magnetite (Fe3O4), have been the most commonly used (Liu et al., 2016), as they have demonstrated osteoinductive capacity in vitro, even in the absence of external magnetic stimulation (Huang et al., 2009; Bock et al., 2010; Wei et al., 2011). Thus, MNPs have been incorporated into conventional bioceramic or polymeric scaffolds, adding intrinsic magnetic properties capable of enhancing osteogenic potential. Results from in vivo studies suggest that the magnetic field resulting from the presence of incorporated MNPs, albeit small, can indeed drive the formation of new bone, even without external magnetic stimulation. Wu and colleagues incorporated iron oxide MNPs into a CaP bioceramic scaffold and found this material capable of enhancing osteogenesis in a rodent model of ectopic bone formation (Wu Y. et al., 2010), while Singh and associates produced a PCL biopolymeric nanofibrous scaffold incorporating iron oxide MNPs, which demonstrated the ability to enhance bone formation in a rodent segmental bone defect model (Singh R.K. et al., 2014).
MNP incorporation provides further functionality by rendering the biomaterial magnetically responsive, permitting the use of controlled external magnetic field stimulation to potentially regulate and direct cellular behavior toward osteogenesis and even angiogenesis (Sapir et al., 2012). Yun et al. (2016) studied the effects of external magnetic stimulation applied to magnetic PCL/MNP scaffolds on osteoblast differentiation and bone formation and found that external stimulation not only promoted in vitro osteoblastic differentiation, but also significantly enhanced new bone formation, compared to the magnetic scaffold alone, in mouse calvarium defects.
New and innovative methods in this arena continue to emerge. In a combined approach, magnetoelectric composite materials bridge the magnetic and piezoelectric properties of bone to produce a potentially synergistic regenerative effect. Such materials respond to magnetic stimulation with mechanical deformation (due to the magnetostriction of one component, that is the change in shape occurring during magnetization), resulting in electrical polarization (due to the piezoelectric behavior of the other component). Thus, bioelectrical cues can be delivered to a desired cellular environment with precise remote control (Ribeiro et al., 2016).
Since their introduction, concerns regarding the cytotoxic effects of iron oxides have justifiably arisen, with a documented relationship between their clinical use and the outbreak of acute adverse events, such as nephrogenic systemic fibrosis, formation of apoptotic bodies, inflammation, and other toxic effects (Pisanic et al., 2007; Häfeli et al., 2009; Wu et al., 2010b; Zhu et al., 2011; Alarifi et al., 2014; Shen et al., 2015). This has provoked efforts to produce magnetic biomaterials with improved biological features, such as doping well-known biocompatible nanomaterials with a magnetic phase to replace magnetite and the other iron oxides. Recently, Tampieri and colleagues reported fabrication of biocompatible FeHA nanoparticles with a superparamagnetic-like phase by doping HA with iron (Fe2+/Fe3+) ions (Tampieri et al., 2012). In vitro studies showed that these FeHA nanoparticles were capable of enhancing cell proliferation to a greater degree than HA particles alone, without reducing cell viability. Furthermore, the in vivo biocompatibility of FeHA was demonstrated in a pilot animal study of a rabbit critical bone defect (Panseri et al., 2012). While approaches to bone regeneration based on magnetic stimulation and magnetically responsive biomaterials are in the early stages of development, the results to date suggest promise for such strategies in bone regeneration applications going forward.
Materials Mimicking Bone Architecture: 3D Printed and Biomorphic Ceramics
Native bone displays structural features with levels of organization spanning several orders of magnitude (nm to cm scale) (Chen et al., 2008). This multiscale hierarchical structure, as well as the interactions between its organic and mineral components at the molecular level, contribute significantly to biological and mechanical properties of bone (Gupta et al., 2005). Thus, utilization of these features to guide the hierarchical design of biomaterials represents a potential strategy to promote bone regeneration. This section focuses on nanostructured scaffold materials designed to recapitulate native nanocues by providing mimicry of the structural features of the natural bone matrix.
Architectural Considerations
For bone tissue engineering applications, a scaffold should possess appropriate structural and mechanical properties to sustain physiological loads in order to preserve weight-bearing function, while also possessing intrinsic biocompatibility in order to facilitate favorable biomaterial-native bone interactions, which serve to enhance tissue regeneration and implant integration (Ikeda et al., 2009). Many early bone tissue engineering designs sought to accomplish this goal through synthetic structures which imparted bulk properties to the constructs, such as adequate mechanical strength and sufficient transport properties for cell infiltration and tissue organization (Christenson et al., 2007). These designs, although successful in replicating many of the macroscopic properties of native bone, often failed prior to full healing (Burdick and Anseth, 2002; Murugan and Ramakrishna, 2005). A key factor identified in these failures was inadequate tissue regeneration around the material shortly after implantation, owing to poor interaction of the biomaterial with the host tissue (Christenson et al., 2007). In fact, the process of bone formation is governed by interactions and informational cues derived from structural features spanning multiple length scales from nanoscale to macroscale (Gusic et al., 2014). Nanoscale interactions in particular have been shown to be crucial in controlling cell functions such as proliferation, migration, and adhesion in native tissues (Benoit and Anseth, 2005). Indeed, all living systems are governed by molecular behavior at nanometer scales (Zhang et al., 2012). As in other tissues, the cellular organization and corresponding tissue properties of bone are highly dependent on the nanostructural features of the ECM, since cells are predisposed to interact with nanostructured surfaces (Kaplan et al., 1994; Taton, 2001; Liu et al., 2006). This may help to explain why early generation tissue substitutes—produced through macro- and microfabrication techniques that were unable to recreate sophisticated structures that mimic the subtleties of the ECM—showed suboptimal performance. Recent paradigm shifts to nanoscience-enabled techniques have resulted in the emergence of novel nanotechnological approaches that enable more precise recapitulation of the architectural features of native bone, offering greater potential for modulating cellular behavior and enhancing bone regeneration (Webster et al., 2000; Murphy et al., 2010; Saiz et al., 2013; Tang et al., 2016).
Native bone is characterized by unique topological features derived from its micro- and nanostructured surfaces and interfaces, which are crucial to its function and growth and therefore promising targets for biomimicry (Nadeem et al., 2015). Nanotechnology offers new opportunities to capitalize on the structure-function relationships in bone by replicating a number of these integral features. By providing the substrate upon which cells attach and proliferate, surface topography can modulate cellular behavior and function (Boyan et al., 2002). Native bone is composed of collagen fibrils with rod or needle-like HA deposits scattered across their surface. These deposits produce surface roughness which has been shown to promote both adhesion of osteoblasts as well as differentiation of MSCs to the osteogenic lineage (Nadeem et al., 2015). Based on this, researchers have developed approaches to introduce surface roughness onto scaffold materials in order to more effectively mimic the mineralized interface encountered by cells adhering to native bone ECM (Henkel et al., 2013). Farshid and colleagues (Farshid et al., 2017), for instance, introduced microscale surface roughness onto polymeric scaffolds through the incorporation of boron nitride nanotubes and nanoplatelets, which resulted in greater collagen deposition and cell attachment by pre-osteoblasts in vitro. In another approach, Shakir et al. (2018) utilized nano-HA to enhance the surface roughness of a resin-based chitosan scaffold, which they found capable of promoting superior bone regeneration in vivo in a rat calvarium defect model.
Given that the HA deposits producing surface roughness in native bone have dimensions in the nanoscale, fabrication of surfaces with nanostructured topography can prove even more beneficial to inducing osteogenesis than simply producing roughness at the microscale (Lim et al., 2005). Indeed, Lim and colleagues (Lim et al., 2005) generated nanoscale surface roughness by introducing “nanoislands” of varying size to a polymeric substrate and investigated their effects on osteoblastic cell behavior. They found that a smaller island height produced greater cell adhesion and spreading as well as increased alkaline phosphatase activity, demonstrating the advantages of down-scaling the dimensions of topographical features. Other surface nanotopographies, such nanogrooves and nanopits, have also been shown to enhance osteoblast differentiation and osteogenic cell function in several studies (Dalby et al., 2007; Liu et al., 2014; Gong, 2015; Xu et al., 2017).
In addition to surface topography, cell and ECM alignment within the native bone represents a structural feature integral to its growth and function, and is thus a promising target for biomimicry (Takano et al., 1999). The anisotropic characteristics of bone tissue—a result of its unique adaptive response to external forces—is due to the longitudinal alignment of its collagen fibers, and there is evidence that MSCs more readily differentiate to an osteogenic phenotype when confined into such an alignment (Ber et al., 2005; Li et al., 2007). This phenomenon is thought to be mediated by contact guidance mechanisms whereby instructive physical cues, generated through the local interactions which occur in specific cellular orientations and alignment, act to regulate cell morphology and function (Boyan, 1996; Badami et al., 2006). Tissue engineering strategies which are capable of exploiting these mechanisms may therefore allow cell fate to be precisely directed for its intended application. For the purposes of bone tissue engineering, simulation of the alignment found in the native bone may potentially promote bone regeneration by driving stem cells toward an osteogenic lineage and enhancing their functions through the recapitulation of the native cues (Ber et al., 2005; Nadeem et al., 2015).
To achieve the desired alignment, one approach involves the creation of micron and/or nanoscale grooves on the substrate material, which allows cells to grow and spontaneously elongate along the direction of groove alignment (Perizzolo et al., 2001; Zhu et al., 2005; Badami et al., 2006). Nadeem et al. (2015) utilized such an approach through the introduction of integrated surface micropatterns to their 3D CaP/gelatin biomaterials, producing cell-instructive scaffolds which were osteoinductive in vitro and promoted greater bone formation and osseointegration in vivo in a rabbit radial segmental defect model. A more direct approach toward biomimicry is to simply replicate the aligned fibers seen in the native collagenous architecture of bone. Innovative techniques utilizing aligned nanofibers created, for example, by electrospinning, have made it possible to accomplish this form of biomimicry with extraordinary precision (Jose et al., 2009; Anjaneyulu et al., 2017). By replicating the morphological and chemical structure of the natural ECM at the nanoscale level, nanofibrous scaffold materials offer greater potential to modulate cellular function and guide cell growth (Murugan and Ramakrishna, 2005; Leung and Ko, 2011; Pas̨cu et al., 2013). Additionally, such materials provide increased surface area-to-volume ratios and porosity, thereby enhancing osteoconductivity, as well as desirable biocompatibility, biodegradability, and mechanical strength (Haider et al., 2018).
3D Printing
The internal porosity of native bone is yet another important structural feature which bone regenerative engineering approaches have targeted for biomimicry. The presence of an interconnected, 3D, porous architecture is a critical requirement for any bone tissue engineering strategy in order to allow for cell migration and the transport of nutrients and waste (Lee et al., 2014). Nanofibrous scaffolds prove especially advantageous in this regard, as the small fiber diameter creates a highly porous matrix enabling effective cell migration and proliferation throughout the scaffold (Rezwan et al., 2006; Zhang et al., 2008; Xu et al., 2017). In addition to overall porosity, average pore size is another significant consideration. Although the optimal pore size to promote bone regeneration within engineered scaffolds has not been definitively established, in general, smaller pore sizes will promote initial cell adhesion due to higher substrate surface area, while larger pores will enable greater cellular infiltration from surrounding tissue, a critical requirement for vascular ingrowth and subsequent tissue maintenance (Kenar et al., 2006; Murphy et al., 2010; Cox et al., 2015). While nanofibrous scaffolds provide a high overall porosity, nanofibers created by electrospinning tend to produce constructs with reduced average pore size compared to larger fiber scaffolds, resulting in decreased cell penetration depth (Badami et al., 2006). The need for more precise control of porosity and pore size within scaffold materials has prompted the implementation of novel 3D printing systems which may offer such capabilities. 3D printing technologies such as fused deposition modeling, stereolithography, and selective laser sintering have enabled the production of scaffolds with greater spatial resolution and fidelity than traditional fabrication methods, while also offering the ability to introduce precise pore gradients which more effectively mimic the physical cues for growth found in native bone tissue (Bracaglia et al., 2017; Alehosseini et al., 2018; Malikmammadov et al., 2018; Babilotte et al., 2019). While 3D printing approaches to the design of scaffolds for bone tissue engineering are quite new and still being explored for their utility, they also offer strong potential for the 3D patterning of surface roughness and other key physical features, providing even further recapitulation of the native cues present in bone (Murphy and Atala, 2014).
Mimicking the architecture of native bone is an essential component of material design for bone regeneration applications. These materials must provide an environment suitable for cellular recruitment, adhesion, proliferation, and pro-osteogenic differentiation. There is an abundance of technologies that provide tight control over topography, porosity, and mechanical properties of various materials that have proven useful for bone regeneration. Providing a suitable environment for osteogenesis is a crucial aspect of material design for bone regeneration, but it is not the only consideration. These materials must also be durable, biocompatible, and capable of integrating with surrounding tissues, among other properties, to be relevant for clinical applications.
Scaffolds Synthesized Through Biomorphic Transformation
Long bone and critical-sized defects caused by trauma, non-union, or tumors represent a difficult clinical challenge in need of more reliable solutions (Berner et al., 2012; Roffi et al., 2017). Most currently available synthetic scaffolds have not proven capable of providing the necessary osteo- and vascular conductivity within the innermost portions of the scaffold. This could be attributed to a disorganized and tortuous porosity impeding cell penetration into the scaffold and subsequent tissue development; sufficient mechanical strength to promote integration with host tissues can also be a challenge (Mastrogiacomo et al., 2006).
In the attempt to overcome these limitations, “biomorphic transformations” have been developed. These synthetic approaches consist of a series of steps involving pyrolysis and complex chemical reactions (mainly liquid or gas infiltration processes), allowing for the chemical transformation of natural substrates into ceramic scaffolds, while preserving their original fine architecture from the nano up to the macro scale. Among natural templates, one is particularly advantageous as a solution to long bone defect healing—wood. Wood presents a unique hierarchical architecture on a cellular micro and nano-structure scale (Fratzl and Weinkamer, 2007). The pattern of fiber bundles and channel-like porous areas of selected types of wood (e.g., rattan) is surprisingly similar to that found in long bone (Tampieri et al., 2009). There have been a few remarkable attempts to utilize wood as a scaffold for the synthesis of biomimetic hierarchically organized load bearing scaffolds for long bone repair. In 2009, a biomimetic HA bone scaffold from natural wood with highly organized multiscale porosity was first proposed (Tampieri et al., 2009). The resulting material was a porous nanostructured apatite scaffold with a hierarchical structure, representing an inorganic substitute for bone graft that allowed for cellular invasion while providing space for vascularization (Tampieri et al., 2009). Recently, they used a similar approach of bio-ceramization of a wood template to prepare a hollow cylindrical ceramic scaffold to resemble cortical bone, and filled it with a spongy HA/collagen bio-hybrid scaffold to resemble spongy bone. They assessed the osteoconductivity of the construct in a sheep critical size load bearing model (2 cm metatarsus defect), finding significant osteointegration at the bone/scaffold interface (Filardo et al., 2014). Using the same large animal model, in a follow-up study, they increased the diameter of the lumen of the external cortical-like biomorphic scaffold (Filardo et al., 2019). Osteointegration was observed in all samples, but the group with the largest internal diameter (11 mm) showed the best results in terms of bone-to-implant contact and new bone growth inside the scaffold. Additionally, the investigators posited that scaffold degradation in the cortical area—which induced osteointegration and new bone formation—is possible evidence of activation of load-induced biochemical signaling within the bone healing cascade.
Bigoni et al. (2020) reported that the mechanical properties of these biomorphic HA scaffolds have superior mechanical properties (higher strength, stiffness, and toughness at low density) when compared to usual porous ceramics obtained through sintering; probably due to the unique hierarchically organized multiscale resolution down to the nano-scale, which is not yet present in common ceramics.
While there is much potential for wood-based scaffolds and biomorphic transformation, certain drawbacks exist in comparison with other approaches. For instance, the process of biomorphic synthesis requires complex and strict control of reaction kinetics to avoid deformations and structural defects and to maintain the multiscale porosity (i.e., down to the nanoporosity) (Tampieri et al., 2018). Further, it relies on gas-solid reactions that are strongly affected by different phenomena relating to adsorption of the gaseous reactant by the solid, kinetics of nucleation and growth of synthesized inorganic phase at the surface, and the penetration of the gaseous reactant within the innermost portion of the structure (Szekely, 2012). This control is vital when fabricating larger pieces, since diffusive phenomena affect the rate of phase transformation (Bigoni et al., 2020). Without strict control of this process, the advantages of wood as a template cannot be capitalized upon.
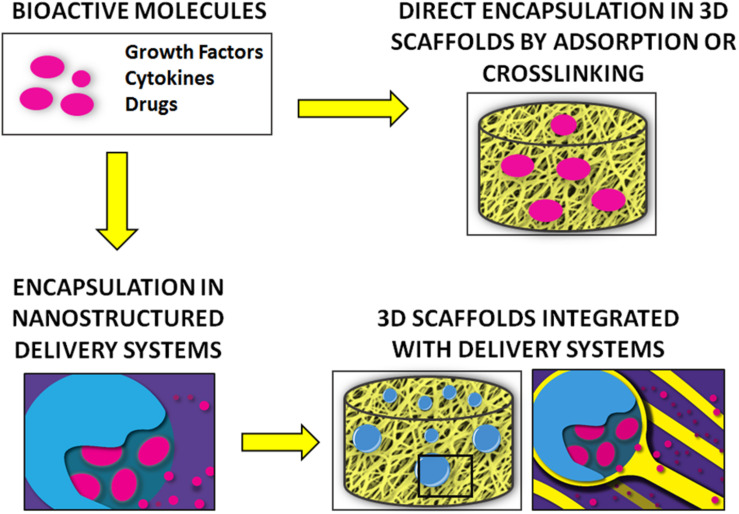
Mimicking Bone’s Biochemical Niche: Delivery of Bioactive Molecules
A variety of bioactive molecules compose the biochemical milieu of bone (Minardi et al., 2020). Several strategies have been proposed to deliver biochemical cues (e.g., growth factors, cytokines) to recapitulate this environment and enhance bone regeneration, as summarized in Figure 3. Initial attempts consisted of the direct adsorption or crosslinking of biomolecules to implants, which resulted in suboptimal outcomes, mostly due to burst release and molecule denaturation (Fan et al., 2012).
FIGURE 3.
Summary of the main strategies for the delivery of bioactive molecules for bone regeneration.
Delivery systems offer more effective and precise control over release (Minardi et al., 2014). Among delivery systems, nanostructured varieties have proven superior, as they can be finely tuned to provide a higher yield of loading and sustained release over time, while allowing for complex temporally controlled release kinetics (Minardi et al., 2016b). The most common nanostructured delivery systems developed for bone regeneration are reviewed below and summarized in Table 3.
TABLE 3.
Main types of nanostructured delivery systems used in bone regeneration, with their respective advantages and disadvantages.
| Advantages | Disadvantages | References | |
| Inorganic nanostructured delivery systems | |||
| Ceramics (e.g., HA, TCP) | Intrinsic osteoconductivity Surface functionalization Widely available |
Unfavorable biodegradability profile Low yield of payload loading |
Matsumoto et al., 2004; Dong et al., 2007; Habraken et al., 2007; LeGeros, 2008; Yuan et al., 2010; Xie et al., 2010; Bose and Tarafder, 2012; Jeon et al., 2012; Fielding and Bose, 2013; Fan et al., 2014; Wen et al., 2017 |
| Metallic or metalloid oxides (e.g., silica) | Tailorable mesoporous structure Surface functionalization with and/or encapsulation of bioactive molecules Modifiable architecture and topography Optimization of cell adhesion and proliferation |
Cytotoxicity at certain particle sizes and/or concentrations | Oh et al., 2005; Raja et al., 2005; Magrez et al., 2009; Lai et al., 2011; Lallana et al., 2012; Portan et al., 2012; Tang et al., 2012; Setyawati et al., 2013; Shadjou and Hasanzadeh, 2015; Zhou et al., 2015; Cui et al., 2018; Tang et al., 2014; Hu et al., 2012; Huang et al., 2014; Kwon et al., 2017; Liu et al., 2017 |
| Organic nanostructured delivery systems | |||
| Synthetic polymers (e.g., PLA, PLGA) | Widely available Overall favorable biocompatibility Many modifiable properties: e.g., L/G ratio, molecular weight. Modifiable with cross-linkers or surface functionalization |
Low yield of payload loading Burst release Difficulty in accomplishing sustained release Certain polymers have cytotoxic degradation products |
Alcantar et al., 2000; Habraken et al., 2007; Lü et al., 2009; Puppi et al., 2010; Anderson and Shive, 2012; Makadia and Siegel, 2011; Jacob et al., 2018 |
| Natural polymers (e.g., gelatin, chitosan) | Widely available Favorable biocompatibility and biodegradability Biomimetic properties Modifiable with cross-linkers or surface functionalization |
Low yield of payload loading Rapid degradation in vivo Burst release Difficulty in accomplishing sustained release |
Friess, 1998; Aframian et al., 2002; Malafaya et al., 2007; Niu et al., 2009; He et al., 2011; Vo et al., 2012; Farokhi et al., 2014; Amjadian et al., 2016; Cai et al., 2016; Ding et al., 2016; Shen et al., 2016; Jacob et al., 2018; Oliveira et al., 2019 |
| Composite nanostructured delivery systems | |||
| Composites | High loading efficiency Highly tunable release kinetics Sustained release Optimization of unique properties of each material |
Generally require more complex syntheses | Li et al., 2006; Liu et al., 2009; Niu et al., 2009; Reves et al., 2011; Fan et al., 2012; Singh et al., 2015; Minardi et al., 2015b; Kim B.-S. et al., 2018; Wang et al., 2018; Zhang Q. et al., 2018; Minardi et al., 2020 |
Nanostructured Delivery Systems
Osteogenic growth factors, including bone morphogenetic proteins (BMP-2 and BMP-7), or the transforming growth factor-β (TGF-β) family, are known to play a crucial role in cell proliferation, differentiation, and ultimately osteogenesis (Chen et al., 2004). As FDA-approved in 2002, BMP-2 is delivered with an absorbable collagen sponge (ACS) [INFUSETM] for clinical applications (McKay et al., 2007). Although efficacious, supraphysiologic doses of the growth factor are required, which have been associated with a number of adverse side effects (Tannoury and An, 2014). Given these challenges, there is significant research interest in the development of novel delivery systems to provide controlled release of lower doses of BMP-2 and other bioactive molecules important for bone regeneration. Toward this end, a wide array of nano-structured systems capable of delivering bioactive signals and molecules have been proposed.
Inorganic Nanostructured Delivery Systems
Utilizing ceramic materials for drug delivery in the field of bone regeneration presents advantages, as these materials themselves have osteoconductive properties (Habraken et al., 2007; LeGeros, 2008; Yuan et al., 2010). Commonly used ceramics include CaPs, such as HA and TCP. In the first generation of HA-based delivery systems, HA was directly adsorbed with bioactive molecules such as BMP-2 (Matsumoto et al., 2004; Dong et al., 2007; Xie et al., 2010), however, side effects associated with their burst release quickly demanded alternative strategies (Xie et al., 2010), such as chemically bonding bioactive molecules to the surface of the ceramic particles, which provides a more controlled and sustained release over time (Fan et al., 2014). The surface of CaP particles can be functionalized to bind a wide array of bioactive molecules for bone regeneration (Bose and Tarafder, 2012). For example, nano-HA particles can be functionalized to bind to and provide sustained release of BMP-2 to stimulate osteogenesis in vitro (Jeon et al., 2012).
Metallic or metalloid oxide nanomaterials such as silica (SiO2) and titanium oxide (TiO2) nanotubes have also been functionalized into nano-structured delivery systems for different bioactive molecules for bone regenerative applications (Lai et al., 2011; Shadjou and Hasanzadeh, 2015; Zhou et al., 2015). Silica-based nanomaterials (e.g., mesoporous silica) have been engineered to provide controlled release of different biomolecules (Shadjou and Hasanzadeh, 2015). These materials are generally biocompatible and can be easily functionalized with a number of different linker molecules (Lallana et al., 2012). Zhou et al. (2015) utilized silica nanoparticles to enable dual-delivery of BMP-2 and dexamethasone, and Cui et al. (2018) have utilized a silica-based nanomaterial delivery system for controlled release of BMP-2-related peptide both in vitro and in vivo. The tailorable mesoporous structure and the ability to bind a variety of different molecules are notable advantages of these silica-based materials (Tang et al., 2012). Additionally, the architecture and topography of these compounds can be engineered to promote cell adhesion, proliferation, and differentiation—all critical requirements for in vivo applications (Tang et al., 2014).
TiO2 nanotubes for delivery of drugs and other biomolecules have also been described (Hu et al., 2012; Huang et al., 2014; Kwon et al., 2017). These can be designed to both encapsulate and display the molecule of interest on the material surface (Huang et al., 2014). One group directly functionalized the surface of TiO2 nanotubes with BMP-2, which promoted osteogenic differentiation in vitro (Lai et al., 2011). In addition to biomolecule delivery, the surface of TiO2 nanotubes can be activated and coated with ceramics like CaP or HA (Oh et al., 2005; Raja et al., 2005). However, concerns have arisen regarding the toxicity of TiO2-based nanomaterials, with one study suggesting that the strong adherence of osteoblasts to the metallic material may induce apoptosis (Portan et al., 2012; Setyawati et al., 2013; Liu et al., 2017). Dose-dependent cytotoxic effects of TiO2 nanofilaments have also been described elsewhere (Magrez et al., 2009).
Organic Nanostructured Delivery Systems
Alternatively, polymer-based delivery systems have been fabricated using both synthetic and natural materials (Jacob et al., 2018). Commonly used synthetic polymers include polyethylene glycol (PEG), poly(L-lactic acid) (PLA), PCL, PLGA, and poly(L-lactic acid) fumarate (PLAF). Polyethylene glycol and PLA are comprised of single monomers, while PCL, PLGA, and PLAF are copolymers. There has been extensive use of synthetic polymers as delivery systems for bone regeneration applications, including delivery of BMP-2, dexamethasone, antibiotics, and other pharmacologics (Puppi et al., 2010). Polyethylene glycol, PCL, and PLGA are all biocompatible (Alcantar et al., 2000; Anderson and Shive, 2012), although PLGA is generally favored, because it is FDA-approved and has been demonstrated to be non-inflammatory in various studies (Habraken et al., 2007; Lü et al., 2009; Makadia and Siegel, 2011). Additionally, various properties of PLGA—the L/G ratio, molecular weight, and stereochemistry—can be modified to control the polymer’s properties and degradation rate (Habraken et al., 2007). Polymers such as PLA and PLGA can yield cytotoxic acidic degradation products (Habraken et al., 2007). Therefore, controlled degradation is important for both drug delivery and to minimize toxicity.
Natural polymers used for the controlled release of bioactive molecules to promote bone regeneration include gelatin, chitosan, alginate, collagen, silk fibroin, hyaluronic acid, and fibrin, among others (Jacob et al., 2018). These materials are advantageous given their biocompatibility and biomimetic properties, which result from a close resemblance of native ECM, and are also fully biodegradable (Malafaya et al., 2007; Vo et al., 2012). Natural polymers have been described in systems delivering BMP-2 (Niu et al., 2009; Shen et al., 2016), vascular endothelial growth factor (VEGF; Farokhi et al., 2014), antibiotics (Cai et al., 2016), and immunomodulators (Amjadian et al., 2016). However, there are known limitations to using natural polymers as the foundation for delivery systems. For example, controlling the release of molecules from these polymers is challenging. Collagen is known to degrade rapidly in vivo through protease action (Friess, 1998); however, various chemical modifications—including cross-linking (Aframian et al., 2002; He et al., 2011; Oliveira et al., 2019) or combination with other compounds (e.g., composite materials) (Niu et al., 2009; Ding et al., 2016)—have enabled researchers to significantly prolong the degradation rates of these natural polymers. Other limitations of natural polymers include fabrication costs, batch variability, and harvesting (Vo et al., 2012).
Composite Nanostructured Delivery Systems
Composite materials are often developed to overcome specific limitations of a given material, such as those described above. The optimal properties of each individual material can be leveraged when combining multiple components into one delivery system. Contributing to the sustained release of osteogenic factors, which is critical for in vivo outcomes, composite materials provide additional functionality that can be used to fine-tune the temporal release profile of a given compound. Some common examples include ceramic/polymer composites, polymer blends, and silica/polymer composites. Several different polymer and HA composite materials for controlled delivery of BMP-2 have been described, including silk fibroin/poly(ethylene oxide)/nano-HA (Li et al., 2006), gelatin/fibrin/nano-HA (Liu et al., 2009), collagen/poly(L-lactic acid)/nano-HA (Niu et al., 2009), chitosan/nano-HA (Reves et al., 2011), and ε-polycaprolactone/HA (Kim B.-S. et al., 2018). The polymer components can be cross-linked and functionalized, whereas the ceramic components provide osteoconductive properties. Multiple polymers have been combined to create polymer blends, which provide further control of degradation rates (Wang et al., 2018). Metal/metalloid and polymer composites for drug delivery are a popular and expanding area of research in bone tissue engineering. Although metallic oxides like silica can be engineered to provide burst release of biomolecules, further functionalization with polymers can provide sustained release over time. Poly(lactic-co-glycolic acid)-mesoporous silicon composites have also gained significant traction as a delivery system. For example, PLGA-mesoporous silicon microspheres have been engineered to deliver therapeutics, including BMP-2 (Minardi et al., 2020) and other bioactive molecules (Minardi et al., 2015b); these have demonstrated excellent release profiles, biocompatibility, and osteogenic profiles both in vitro and in vivo. Other groups have utilized similar composite systems for bone tissue engineering applications (Fan et al., 2012; Zhang Q. et al., 2018). In another study, Singh et al. (2015) created a composite of PCL nanofibers coated with a mesoporous silica shell that was capable of binding to and providing sustained release of several bioactive molecules, with a subsequent upregulation of osteogenic differentiation in vitro.
Biomaterials Functionalized With Nanostructured Delivery Systems
Scaffolds can be engineered to provide both spatially- and temporally controlled release of important biomolecules that facilitate bone regeneration and healing (Minardi et al., 2014, 2016b). While temporally controlled release is important to orchestrate the cascade of molecular and cellular events necessary to bone healing, the spatial release of biomolecules in vivo ensures that it occurs at the defect or desired area of interest for clinical applications (Minardi et al., 2016b). The most popular types of scaffolds (hydrogels (Nguyen and West, 2002), ceramics (Habraken et al., 2007), 3D-printed materials (Yi et al., 2016), and various composite materials (Yi et al., 2016) have all been proposed in combination with nanostructured delivery systems. These scaffolds can be functionalized with various bioactive components and molecules (Minardi et al., 2016b), including growth factors, peptides and mimicker molecules, immunomodulatory molecules, antibiotics, and even entire cells. Well-established as a potent stimulator of osteogenesis, incorporation of BMP-2 or BMP-2 mimetics into scaffolds is understandably an active area of research. Angiogenic factors such as VEGF, platelet derived growth factor (PDGF), and fibroblast growth factor (FGF) have also been shown to play an important role in bone regeneration and to support the maturation of the newly formed bone (David Roodman, 2003; Kaigler et al., 2006; De la Riva et al., 2010).
In addition to growth factors, systems can be functionalized to deliver other important bioactive molecules for bone healing, including immunomodulatory therapeutics and antibiotics to optimize bone healing. The host inflammatory response plays a critical role in osteogenesis and bone healing (Walsh et al., 2006; Guihard et al., 2012, 2015; Corradetti et al., 2015), and incorporation of immunomodulatory molecules within scaffolds provides another means to optimize bone healing and scaffold integration. Given that the risk of infection, including osteomyelitis, is significant after placement of implants (Lucke et al., 2003), the controlled release of antibiotics has the potential to provide a huge advantage to implanted devices and subsequent bone healing (Adams et al., 2009). Functionalization with these various molecules can occur via several different mechanisms, including incorporation of nanostructured systems within the scaffold, cross-linking and surface modifications, adsorption, direct loading of cells, among others. For example, various types of scaffolds—fibrous gelatin, poly(L-lactide), and HA particle composite (Amjadian et al., 2016) and electrospun nanofiber disks (Li et al., 2015)—have been functionalized to deliver local dexamethasone to improve osteogenesis. Herein, we list and review the most common and successful strategies for incorporation of delivery systems into 3-dimensional implants for bone regeneration.
Direct Incorporation of Nano-Delivery Systems in 3D Constructs
Direct incorporation of bioactive molecules and nanostructured delivery systems has been accomplished using a number of different techniques. One common modality is the hydrogel. Numerous polymeric hydrogels have been developed (Hoare and Kohane, 2008), as they can be engineered to both control the release of biomolecules (Gibbs et al., 2016) and enhance cellular adhesion and differentiation (Tibbitt and Anseth, 2009). These hydrogels are typically biocompatible and can be easily functionalized with cell adhesion ligands by modification of their surface (Hoffman, 2012). Some challenges persist, including their fabrication and clinical deployment (Hoare and Kohane, 2008). Hydrogels also inherently lack a solid framework, can be difficult to handle, and they may be difficult to sterilize, which can limit the clinical utility of these materials (Hoffman, 2012). Madl et al. (2014) engineered alginate hydrogels functionalized with a peptide mimetic of BMP-2, which were shown to upregulate markers of osteogenic differentiation and increase mineralization in vitro. Delivery systems of angiogenic factors such as VEGF have also been incorporated into polymeric hydrogel scaffolds for delivery in vivo (Kempen et al., 2009).
Surface Modification and Cross-Linking of Nano-Delivery Systems to 3D Constructs
Surface modification and cross-linking are other modes of biomaterials functionalization. Surface chemistries can facilitate stable, covalent binding of molecules, with the potential to provide tightly controlled release (Nie et al., 2007). Heparin-based linkers, for example, are commonly used to link growth factors to surfaces (Liang and Kiick, 2014). Various examples of these linkers have been described for local delivery of BMP-2 (Kim S.E. et al., 2011; Yun et al., 2013) and angiogenic factors like VEGF (Lode et al., 2008; Singh et al., 2011) and PDGF (Lee et al., 2012). Delivery systems of BMP-2 have also been incorporated directly onto the surface of 3D-printed ceramic scaffolds using polymer emulsion (Kim B.-S. et al., 2018).
Surface modification with immunomodulatory molecules has also been described. For example, Spiller et al. (2015) functionalized a decellularized scaffold with IL-4 via biotin-streptavidin binding and/or IFN-γ via adsorption, to facilitate rapid release of IFN-γ to promote pro-inflammatory M1 macrophages and sustained release of IL-4 to promote pro-healing M2 macrophages. Other groups have functionalized scaffolds with immunomodulatory molecules, including IL-4 (Minardi et al., 2016a), IL-10 (Rodell et al., 2015), and IL-33 (Liu et al., 2018) for various applications. The delivery of immunomodulatory molecules is relatively novel, particularly for bone tissue engineering, and this area of research is at a pivotal stage. Notably, scaffolds functionalized with IFN-γ have demonstrated increased vascularization relative to controls (Spiller et al., 2015).
Many other scaffolds have been engineered to provide a more sustained release of encapsulated BMP-2 (Yang et al., 2013; Rahman et al., 2014; Gan et al., 2015; Kim B.-S. et al., 2018; Mohammadi et al., 2018). Sun et al. (2018) fabricated a porous scaffold comprised of sintered HA nanoparticles, functionalized with either BMP-2 or BMP-2-related peptide, and both options provided significant osteogenic potential when assessed in a critical-size cranial defect model in rats. Hu et al. (2012) anodized a titanium substrate to form TiO2 nanotubes that were loaded with BMP-2 for sustained release, which showed promising upregulation of osteogenic differentiation in vitro.
Multifunctional Nanofiber Scaffolds as Drug Delivery Systems
Some nanostructured materials can simultaneously be used for the loading and release of bioactive molecules or to bind endogenous growth factors as well as to fabricate 3D scaffolds. A prime example is the use of peptide amphiphiles. Stupp and coworkers engineered a heparin-binding peptide amphiphile (HBPA) nanogel capable of binding and mimicking physiologic BMP-2 signaling (Lee et al., 2013). This BMP-2-binding PA promoted bone regeneration in a rat critical size femoral defect model with 10-fold lower doses than typically required (Lee et al., 2013). Additional approaches by this group have shown that BMP-2-binding PA nanogels provide significant bone regenerative capacity in an established pre-clinical posterolateral lumbar fusion (PLF) model with 10-fold lower doses of BMP-2 than typically required (Lee et al., 2015). In another study, hydrogels were designed with BMP-2 mimicking peptides that were capable of inducing osteogenic differentiation of rat MSCs in vitro. This osteogenic capacity was confirmed in vivo using a rat cranial defect model (Liang et al., 2019). In a recent study, peptide amphiphiles were functionalized with supramolecular glycopeptide nanostructures containing sulfated monosaccharides (Lee S. S. et al., 2017), given that heparan sulfate chains are a critical motif for the binding of many osteogenic growth factors under physiologic conditions (Xu and Esko, 2014). When assessed in vivo using an established rat PLF model, the PA nanostructures combined with a 100-fold lower dose of BMP-2 than typically required (100 ng of BMP-2 per animal) yielded an impressive 100% fusion rate (Lee S. S. et al., 2017). PA nanostructures combined with an even lower dose of BMP-2 (10 ng/animal, or 5 ng/scaffold) or without BMP-2 did not yield fusion, although PA nanofibers alone were minimally bioactive when assessed in vitro in C2C12 cells (Lee S. S. et al., 2017). The pre-clinical data regarding the use of PA-based materials for bone regeneration are promising. Although it is possible to control the nano-scale properties of the PAs, functionalize with different binding motifs, and gel the material into a macrostructure for in vivo applications, some future challenges include optimizing these materials for different clinical applications, ensuring minimal batch-to-batch variability, and large-scale fabrication of these materials.
These studies are but a few examples of the surface chemistries that can be employed to functionalize scaffolds with bioactive molecules. Given the multitude of variables that can be manipulated, the potential for drug delivery and bone regeneration applications are ever-expanding.
Discussion and Conclusion
While each of the previously discussed approaches to bone regeneration show promise, bone defects are not all alike. For instance, the repair of large bone defects resulting from trauma requires a mechanically competent scaffold (Masquelet et al., 2000). Arthroplasty, on the other hand, calls for strategies that improve implant lifespan, as the longevity of conventional materials remains a major limitation in this setting (Smith et al., 2018). For this application, the key to success lies in improving the osseointegration of existing implants through surface modifications (Serra et al., 2013; Puertolas and Kurtz, 2014). Orthopedic infection is another major challenge to implant-based bone healing, and additional material characteristics, such as antimicrobial properties, should be considered.
Even so, the biological environment for bone healing may also be compromised as a result of numerous patient-related factors, local and/or systemic, including advanced age, gender, tobacco, and/or alcohol use, pre-existing chronic illness, and the use of certain medications (Andrzejowski and Giannoudis, 2019). For example, the bone healing deficiencies observed in older patients or smokers may require cell-based approaches or growth factors such as rhBMP-2, which may reliably stimulate healing but can be associated with significant adverse effects. Another example is the use of biologics, which is a strategy of choice in several orthopedic procedures, but that remains inappropriate in oncologic patients, where this may potentially exert local or even systemic tumor-promoting effects (Serakinci et al., 2014; Holzapfel et al., 2016). Together, these influences act through a variety of mechanisms to predispose some patients to impaired bone regeneration, which can only be overcome by personalized regenerative strategies. By providing more precise and individualized treatment modalities, nanotechnological approaches to bone regeneration may provide more effective and longer-lasting implants, decreased infection rates, and improved bony healing, which could ultimately translate to improved patient outcomes. In particular, nanotechnology has allowed for the design of materials that can approach the challenge of augmenting bone regeneration from different angles, such as simultaneously mimicking the bone nano-composition and structure, while serving as a delivery vehicle for bioactive molecules and/or cells (Zhao et al., 2011). Nano-biomaterials that are able to recapitulate more than one of the aspects of bone as reviewed herein may certainly offer superior performances in challenging clinical settings. For example, nanotechnology offers oncologic patients novel means of integrating drug delivery functions into osteoinductive biomaterials which in turn can be used for both the regeneration of bone defects as well as the targeted treatment of the cancer (Acharya and Sahoo, 2011; Gu et al., 2013; Rawat et al., 2015).
Given that each bone defect and combination of pre-existing conditions may call for different regenerative strategies or a combination of them, it is also crucial not to overlook the role of the host’s immune system in bone healing. In fact, the immune system not only protects the body from pathogens but also orchestrates the response to foreign materials, and monitors for possible alterations in tissue homeostasis through a mechanism known as inflammation (Taraballi et al., 2018). While many researchers have investigated methods to minimize the immune response to materials to preserve their regenerative potential, in recent years there has been a shift toward the development of technologies able to preferentially engage the host’s immune cells. In fact, inflammation and the subsequent recruitment of immune cells to the diseases site are paramount to initiate healing (Taraballi et al., 2018). Nonetheless, while inflammation is desirable due to its key role in initiating tissue repair, it does need to be controlled in order to avoid the initiation of a foreign body response against bone regenerative materials (Franz et al., 2011).
Inflammation consists of the infiltration, proliferation, and polarization of hematopoietic and non-hematopoietic cells, that are recruited and activated by specific bioactive factors produced within the lesion (Taraballi et al., 2018). Among the cells involved in this highly orchestrated process, macrophages have been found to be the primary players (Wynn and Vannella, 2016; Michalski and McCauley, 2017). Classically activated macrophages (M1) are the first to be recruited to the site of injury and are gradually replaced by the alternatively activated macrophages (M2) if a regenerative response is initiated (Minardi et al., 2016a). M2 macrophages are immunomodulatory and coordinate tissue repair-producing anti-inflammatory molecules such as IL-10 and TGF-β; this triggers angiogenesis and matrix remodeling, while suppressing the M1-mediated inflammation (Figure 4; Minardi et al., 2016a).
FIGURE 4.
Role of classically and alternatively activated macrophages in inflammation, tissue injury and regeneration.
Currently, the two main strategies to modulate the macrophage-driven inflammatory response are through (i) materials functionalized with nanodelivery systems for the release of immunomodulatory mediators (Spiller et al., 2015); (ii) materials engineered at the nanoscale so that their composition and structure itself may induce macrophage polarization toward the M2 lineage (Vasconcelos et al., 2016; Zhang R. et al., 2018; Lee et al., 2019). Compared to classical cell-based regenerative strategies, immunomodulatory strategies leverage on the self-healing capabilities of the body, thus resulting less technically challenging, since they do not require the direct encapsulation or delivery of live cells.
Although the field of immunomodulatory materials is still in its relative infancy, nanostructured materials have proven to have the necessary level of sophistication to address the challenges of this new arena. Nanostructured immunomodulatory materials will be amongst the most disruptive bone regenerative technologies, as the future of bone regeneration is clearly headed toward increasingly personalized approaches.
Author Contributions
SM, EH, and WH conceived and outlined the review. All authors wrote and edited the manuscript and designed the schematics.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Parker Marsh and Jonathan Paul for assisting with the collection and review of some of the references cited in this manuscript.
Footnotes
Funding. Partial salary support was provided for the authors through the NIH grants 5R01AR069580 and 5R01AR072721.
References
- Acharya S., Sahoo S. K. (2011). PLGA nanoparticles containing various anticancer agents and tumour delivery by EPR effect. Adv. Drug Deliv. Rev. 63 170–183. 10.1016/j.addr.2010.10.008 [DOI] [PubMed] [Google Scholar]
- Adams C. S., Antoci V., Jr., Harrison G., Patal P., Freeman T. A., Shapiro I. M., et al. (2009). Controlled release of vancomycin from thin sol−gel films on implant surfaces successfully controls osteomyelitis. J. Orthopaedic Res. 27 701–709. 10.1002/jor.20815 [DOI] [PubMed] [Google Scholar]
- Aframian D., Redman R., Yamano S., Nikolovski J., Cukierman E., Yamada K., et al. (2002). Tissue compatibility of two biodegradable tubular scaffolds implanted adjacent to skin or buccal mucosa in mice. Tissue Eng. 8 649–659. 10.1089/107632702760240562 [DOI] [PubMed] [Google Scholar]
- Akman A. C., Tığlı R. S., Gümüşderelioğlu M., Nohutcu R. M. (2010). bFGF−loaded HA−chitosan: a promising scaffold for periodontal tissue engineering. J. Biomed. Mater. Res. Part A 92 953–962. [DOI] [PubMed] [Google Scholar]
- Alarifi S., Ali D., Alkahtani S., Alhader M. S. (2014). Iron oxide nanoparticles induce oxidative stress, DNA damage, and caspase activation in the human breast cancer cell line. Biol. Trace Elem. Res. 159 416–424. 10.1007/s12011-014-9972-0 [DOI] [PubMed] [Google Scholar]
- Alcantar N. A., Aydil E. S., Israelachvili J. N. (2000). Polyethylene glycol–coated biocompatible surfaces. J. Biomed. Mater. Res. 51 343–351. [DOI] [PubMed] [Google Scholar]
- Alehosseini M., Golafshan N., Kharaziha M., Fathi M., Edris H. (2018). Hemocompatible and bioactive heparin-loaded PCL-α-TCP fibrous membranes for bone tissue engineering. Macromol. Biosci. 18:1800020. 10.1002/mabi.201800020 [DOI] [PubMed] [Google Scholar]
- Alizadeh-Osgouei M., Li Y., Wen C. (2019). A comprehensive review of biodegradable synthetic polymer-ceramic composites and their manufacture for biomedical applications. Bioactive Mater. 4 22–36. 10.1016/j.bioactmat.2018.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almubarak S., Nethercott H., Freeberg M., Beaudon C., Jha A., Jackson W., et al. (2016). Tissue engineering strategies for promoting vascularized bone regeneration. Bone 83 197–209. 10.1016/j.bone.2015.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amjadian S., Seyedjafari E., Zeynali B., Shabani I. (2016). The synergistic effect of nano-hydroxyapatite and dexamethasone in the fibrous delivery system of gelatin and poly (l-lactide) on the osteogenesis of mesenchymal stem cells. Int. J. Pharm. 507 1–11. 10.1016/j.ijpharm.2016.04.032 [DOI] [PubMed] [Google Scholar]
- Anderson J. M., Shive M. S. (2012). Biodegradation and biocompatibility of PLA and PLGA microspheres. Adv. Drug Deliv. Rev. 64 72–82. 10.1016/j.addr.2012.09.004 [DOI] [PubMed] [Google Scholar]
- Andrzejowski P., Giannoudis P. V. (2019). The ‘diamond concept’ for long bone non-union management. J. Orthop. Traumatol. 20:21. 10.1186/s10195-019-0528-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angevine P. D., Zivin J. G., McCormick P. C. (2005). Cost-effectiveness of single-level anterior cervical discectomy and fusion for cervical spondylosis. Spine (Phila Pa 1976) 30 1989–1997. 10.1097/01.brs.0000176332.67849.ea [DOI] [PubMed] [Google Scholar]
- Anjaneyulu U., Priyadarshini B., Nirmala Grace A., Vijayalakshmi U. (2017). Fabrication and characterization of Ag doped hydroxyapatite-polyvinyl alcohol composite nanofibers and its in vitro biological evaluations for bone tissue engineering applications. J. Sol-Gel Sci. Technol. 81 750–761. 10.1007/s10971-016-4243-5 [DOI] [Google Scholar]
- Arinzeh T. L., Tran T., Mcalary J., Daculsi G. (2005). A comparative study of biphasic calcium phosphate ceramics for human mesenchymal stem-cell-induced bone formation. Biomaterials 26 3631–3638. 10.1016/j.biomaterials.2004.09.035 [DOI] [PubMed] [Google Scholar]
- Assaf K., Leal C. V., Derami M. S., de Rezende Duek E. A., Ceragioli H. J., de Oliveira A. L. R. (2017). Sciatic nerve repair using poly(epsilon-caprolactone) tubular prosthesis associated with nanoparticles of carbon and graphene. Brain Behav. 7:e00755. 10.1002/brb3.755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assiotis A., Sachinis N. P., Chalidis B. E. (2012). Pulsed electromagnetic fields for the treatment of tibial delayed unions and nonunions. A prospective clinical study and review of the literature. J. Orthop. Surg. Res. 7:24. 10.1186/1749-799X-7-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babilotte J., Guduric V., Le Nihouannen D., Naveau A., Fricain J. C., Catros S. (2019). 3D printed polymer–mineral composite biomaterials for bone tissue engineering: fabrication and characterization. J. Biomed. Mater. Res. 107 2579–2595. 10.1002/jbm.b.34348 [DOI] [PubMed] [Google Scholar]
- Badami A. S., Kreke M. R., Thompson M. S., Riffle J. S., Goldstein A. S. (2006). Effect of fiber diameter on spreading, proliferation, and differentiation of osteoblastic cells on electrospun poly(lactic acid) substrates. Biomaterials 27 596–606. 10.1016/j.biomaterials.2005.05.084 [DOI] [PubMed] [Google Scholar]
- Baino F., Fiorilli S., Vitale-Brovarone C. (2017). Composite biomaterials based on sol-gel mesoporous silicate glasses: a review. Bioengineering 4:15. 10.3390/bioengineering4010015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balasubramanian P., Buettner T., Pacheco V. M., Boccaccini A. R. (2018). Boron-containing bioactive glasses in bone and soft tissue engineering. J. Eur. Ceramic Soc. 38 855–869. 10.1016/j.jeurceramsoc.2017.11.001 [DOI] [Google Scholar]
- Balavijayalakshmi J., Suriyanarayanan N., Jayaprakash R. (2014). Effects of sintering on structural and magnetic properties of Cu substituted cobalt–nickel mixed ferrite nano particles. J. Magn. Magn. Mater. 362 135–140. 10.1016/j.jmmm.2014.03.005 [DOI] [Google Scholar]
- Balint R., Cassidy N. J., Cartmell S. H. (2013). Electrical stimulation: a novel tool for tissue engineering. Tissue Eng. Part B Rev. 19 48–57. 10.1089/ten.TEB.2012.0183 [DOI] [PubMed] [Google Scholar]
- Barber F. A., Elrod B. F., McGuire D. A., Paulos L. E. (1995). Preliminary results of an absorbable interference screw. Arthroscopy 11 537–548. 10.1016/0749-8063(95)90129-9 [DOI] [PubMed] [Google Scholar]
- Bari A., Bloise N., Fiorilli S., Novajra G., Vallet-Regí M., Bruni G., et al. (2017). Copper-containing mesoporous bioactive glass nanoparticles as multifunctional agent for bone regeneration. Acta Biomater. 55 493–504. 10.1016/j.actbio.2017.04.012 [DOI] [PubMed] [Google Scholar]
- Bauer T. W., Muschler G. F. (2000). Bone graft materials. An overview of the basic science. Clin. Orthop. Relat. Res. 371 10–27. 10.1097/00003086-200002000-00003 [DOI] [PubMed] [Google Scholar]
- Baxter F. R., Turner I. G., Bowen C. R., Gittings J. P., Chaudhuri J. B. (2009). An in vitro study of electrically active hydroxyapatite-barium titanate ceramics using Saos-2 cells. J. Mater. Sci. 20 1697–1708. 10.1007/s10856-009-3734-0 [DOI] [PubMed] [Google Scholar]
- Benoit D. S., Anseth K. S. (2005). The effect on osteoblast function of colocalized RGD and PHSRN epitopes on PEG surfaces. Biomaterials 26 5209–5220. 10.1016/j.biomaterials.2005.01.045 [DOI] [PubMed] [Google Scholar]
- Ber S., Torun Kose G., Hasirci V. (2005). Bone tissue engineering on patterned collagen films: an in vitro study. Biomaterials 26 1977–1986. 10.1016/j.biomaterials.2004.07.007 [DOI] [PubMed] [Google Scholar]
- Berner A., Reichert J. C., Müller M. B., Zellner J., Pfeifer C., Dienstknecht T., et al. (2012). Treatment of long bone defects and non-unions: from research to clinical practice. Cell Tissue Res. 347 501–519. 10.1007/s00441-011-1184-8 [DOI] [PubMed] [Google Scholar]
- Bernstein M., Gotman I., Makarov C., Phadke A., Radin S., Ducheyne P., et al. (2010). Low temperature fabrication of β–TCP–PCL nanocomposites for bone implants. Adv. Eng. Mater. 12 B341–B347. 10.1002/adem.201080027 [DOI] [Google Scholar]
- Bhumiratana S., Grayson W. L., Castaneda A., Rockwood D. N., Gil E. S., Kaplan D. L., et al. (2011). Nucleation and growth of mineralized bone matrix on silk-hydroxyapatite composite scaffolds. Biomaterials 32 2812–2820. 10.1016/j.biomaterials.2010.12.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bian T., Zhao K., Meng Q., Tang Y., Jiao H., Luo J. (2019). The construction and performance of multi-level hierarchical hydroxyapatite (HA)/collagen composite implant based on biomimetic bone Haversian motif. Mater. Design 162 60–69. 10.1016/j.matdes.2018.11.040 [DOI] [Google Scholar]
- Bianco A., Cacciotti I., Lombardi M., Montanaro L., Bemporad E., Sebastiani M. (2010). F-substituted hydroxyapatite nanopowders: thermal stability, sintering behaviour and mechanical properties. Ceram. Int. 36 313–322. 10.1016/j.ceramint.2009.09.007 [DOI] [Google Scholar]
- Bigoni D., Cavuoto R., Misseroni D., Paggi M., Ruffini A., Sprio S., et al. (2020). Ceramics with the signature of wood: a mechanical insight. Mater. Today Bio 5:100032. 10.1016/j.mtbio.2019.100032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitounis D., Ali-Boucetta H., Hong B. H., Min D. H., Kostarelos K. (2013). Prospects and challenges of graphene in biomedical applications. Adv. Mater. 25 2258–2268. 10.1002/adma.201203700 [DOI] [PubMed] [Google Scholar]
- Boanini E., Gazzano M., Bigi A. (2010). Ionic substitutions in calcium phosphates synthesized at low temperature. Acta Biomater. 6 1882–1894. 10.1016/j.actbio.2009.12.041 [DOI] [PubMed] [Google Scholar]
- Boccaccini A. R., Blaker J. J. (2005). Bioactive composite materials for tissue engineering scaffolds. Expert Rev. Med. Devices 2 303–317. 10.1586/17434440.2.3.303 [DOI] [PubMed] [Google Scholar]
- Bock N., Riminucci A., Dionigi C., Russo A., Tampieri A., Landi E., et al. (2010). A novel route in bone tissue engineering: magnetic biomimetic scaffolds. Acta Biomater. 6 786–796. 10.1016/j.actbio.2009.09.017 [DOI] [PubMed] [Google Scholar]
- Bodkhe S., Turcot G., Gosselin F. P., Therriault D. (2017). One-step solvent evaporation-assisted 3D printing of piezoelectric PVDF nanocomposite structures. ACS Appl. Mater. Interf. 9 20833–20842. 10.1021/acsami.7b04095 [DOI] [PubMed] [Google Scholar]
- Bolbasov E. N., Anissimov Y. G., Pustovoytov A. V., Khlusov I. A., Zaitsev A. A., Zaitsev K. V., et al. (2014). Ferroelectric polymer scaffolds based on a copolymer of tetrafluoroethylene with vinylidene fluoride: fabrication and properties. Mater. Sci. Eng. 40 32–41. 10.1016/j.msec.2014.03.038 [DOI] [PubMed] [Google Scholar]
- Bolbasov E. N., Stankevich K. S., Sudarev E. A., Bouznik V. M., Kudryavtseva V. L., Antonova L. V., et al. (2016). The investigation of the production method influence on the structure and properties of the ferroelectric nonwoven materials based on vinylidene fluoride – tetrafluoroethylene copolymer. Mater. Chem. Phys. 182 338–346. 10.1016/j.matchemphys.2016.07.041 [DOI] [Google Scholar]
- Bose S., Tarafder S. (2012). Calcium phosphate ceramic systems in growth factor and drug delivery for bone tissue engineering: a review. Acta Biomater. 8 1401–1421. 10.1016/j.actbio.2011.11.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bose S., Tarafder S., Banerjee S. S., Davies N. M., Bandyopadhyay A. (2011). Understanding in vivo response and mechanical property variation in MgO, SrO and SiO2 doped β-TCP. Bone 48 1282–1290. 10.1016/j.bone.2011.03.685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyan B. (1996). Role of material surfaces in regulating bone and cartilage cell response. Biomaterials 17 137–146. 10.1016/0142-9612(96)85758-9 [DOI] [PubMed] [Google Scholar]
- Boyan B. D., Bonewald L. F., Paschalis E. P., Lohmann C. H., Rosser J., Cochran D. L., et al. (2002). Osteoblast-mediated mineral deposition in culture is dependent on surface microtopography. Calcified Tissue Int. 71 519–529. 10.1007/s00223-001-1114-y [DOI] [PubMed] [Google Scholar]
- Bracaglia L. G., Smith B. T., Watson E., Arumugasaamy N., Mikos A. G., Fisher J. P. (2017). 3D printing for the design and fabrication of polymer-based gradient scaffolds. Acta Biomater. 56 3–13. 10.1016/j.actbio.2017.03.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bramhill J., Ross S., Ross G. (2017). Bioactive nanocomposites for tissue repair and regeneration: a review. Int. J. Environ. Res. Public Health 14:66. 10.3390/ijerph14010066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bressan E., Ferroni L., Gardin C., Sbricoli L., Gobbato L., Ludovichetti F. S., et al. (2014). Graphene based scaffolds effects on stem cells commitment. J. Transl. Med. 12:296. 10.1186/s12967-014-0296-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucholz R. W., Henry S., Henley M. B. (1994). Fixation with bioabsorbable screws for the treatment of fractures of the ankle. J. Bone Joint Surg. Am. 76 319–324. 10.2106/00004623-199403000-00001 [DOI] [PubMed] [Google Scholar]
- Burdick J. A., Anseth K. S. (2002). Photoencapsulation of osteoblasts in injectable RGD-modified PEG hydrogels for bone tissue engineering. Biomaterials 23 4315–4323. 10.1016/s0142-9612(02)00176-x [DOI] [PubMed] [Google Scholar]
- Burkus J. K., Gornet M. F., Dickman C. A., Zdeblick T. A. (2002). Anterior lumbar interbody fusion using rhBMP-2 with tapered interbody cages. J. Spinal Disord. Tech. 15 337–349. 10.1097/00024720-200210000-00001 [DOI] [PubMed] [Google Scholar]
- Burkus J. K., Heim S. E., Gornet M. F., Zdeblick T. A. (2003). Is INFUSE bone graft superior to autograft bone? An integrated analysis of clinical trials using the LT-CAGE lumbar tapered fusion device. J. Spinal Disord. Tech. 16 113–122. 10.1097/00024720-200304000-00001 [DOI] [PubMed] [Google Scholar]
- Cai Y., Yu J., Kundu S. C., Yao J. (2016). Multifunctional nano-hydroxyapatite and alginate/gelatin based sticky gel composites for potential bone regeneration. Mater. Chem. Phys. 181 227–233. 10.1016/j.matchemphys.2016.06.053 [DOI] [Google Scholar]
- Campana V., Milano G., Pagano E., Barba M., Cicione C., Salonna G., et al. (2014). Bone substitutes in orthopaedic surgery: from basic science to clinical practice. J. Mater. Sci. Mater. Med. 25 2445–2461. 10.1007/s10856-014-5240-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capuccini C., Torricelli P., Sima F., Boanini E., Ristoscu C., Bracci B., et al. (2008). Strontium-substituted hydroxyapatite coatings synthesized by pulsed-laser deposition: in vitro osteoblast and osteoclast response. Acta Biomater. 4 1885–1893. 10.1016/j.actbio.2008.05.005 [DOI] [PubMed] [Google Scholar]
- Carragee E. J., Hurwitz E. L., Weiner B. K. (2011). A critical review of recombinant human bone morphogenetic protein-2 trials in spinal surgery: emerging safety concerns and lessons learned. Spine J. 11 471–491. 10.1016/j.spinee.2011.04.023 [DOI] [PubMed] [Google Scholar]
- Chan E. W. C., Bennet D., Baek P., Barker D., Kim S., Travas-Sejdic J. (2018). Electrospun polythiophene phenylenes for tissue engineering. Biomacromolecules 19 1456–1468. 10.1021/acs.biomac.8b00341 [DOI] [PubMed] [Google Scholar]
- Chen C., Bai X., Ding Y., Lee I. S. (2019). Electrical stimulation as a novel tool for regulating cell behavior in tissue engineering. Biomater. Res. 23:25. 10.1186/s40824-019-0176-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen D., Zhao M., Mundy G. R. (2004). Bone morphogenetic proteins. Growth Factors 22 233–241. 10.1080/08977190412331279890 [DOI] [PubMed] [Google Scholar]
- Chen J., Yu M., Guo B., Ma P. X., Yin Z. (2018). Conductive nanofibrous composite scaffolds based on in-situ formed polyaniline nanoparticle and polylactide for bone regeneration. J. Colloid Interface Sci. 514 517–527. 10.1016/j.jcis.2017.12.062 [DOI] [PubMed] [Google Scholar]
- Chen J. H., Liu C., You L., Simmons C. A. (2010). Boning up on Wolff’s Law: mechanical regulation of the cells that make and maintain bone. J. Biomech. 43 108–118. 10.1016/j.jbiomech.2009.09.016 [DOI] [PubMed] [Google Scholar]
- Chen P. Y., Lin A. Y., Lin Y. S., Seki Y., Stokes A. G., Peyras J., et al. (2008). Structure and mechanical properties of selected biological materials. J. Mech. Behav. Biomed. Mater. 1 208–226. 10.1016/j.jmbbm.2008.02.003 [DOI] [PubMed] [Google Scholar]
- Cheng L.-C., Jiang X., Wang J., Chen C., Liu R.-S. (2013). Nano–bio effects: interaction of nanomaterials with cells. Nanoscale 5 3547–3569. 10.1039/c3nr34276j [DOI] [PubMed] [Google Scholar]
- Cheng X., Wan Q., Pei X. (2018). Graphene family materials in bone tissue regeneration: perspectives and challenges. Nanoscale Res. Lett. 13:289. 10.1186/s11671-018-2694-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorsi M. T., Curry E. J., Chorsi H. T., Das R., Baroody J., Purohit P. K., et al. (2019). Piezoelectric biomaterials for sensors and actuators. Adv. Mater. 31:e1802084. 10.1002/adma.201802084 [DOI] [PubMed] [Google Scholar]
- Christenson E. M., Anseth K. S., van den Beucken J. J., Chan C. K., Ercan B., Jansen J. A., et al. (2007). Nanobiomaterial applications in orthopedics. J. Orthop. Res. 25 11–22. 10.1002/jor.20305 [DOI] [PubMed] [Google Scholar]
- Corradetti B., Taraballi F., Powell S., Sung D., Minardi S., Ferrari M., et al. (2015). Osteoprogenitor cells from bone marrow and cortical bone: understanding how the environment affects their fate. Stem Cells Dev. 24 1112–1123. 10.1089/scd.2014.0351 [DOI] [PubMed] [Google Scholar]
- Cox S. C., Thornby J. A., Gibbons G. J., Williams M. A., Mallick K. K. (2015). 3D printing of porous hydroxyapatite scaffolds intended for use in bone tissue engineering applications. Mater. Sci. Eng. 47 237–247. 10.1016/j.msec.2014.11.024 [DOI] [PubMed] [Google Scholar]
- Cruz F. (2010). Fabrication of HA/PLLA composite scaffolds for bone tissue engineering using additive manufacturing technologies. Biopolymers 11 227–242. 10.5772/10264 [DOI] [Google Scholar]
- Cui H., Liu Y., Deng M., Pang X., Zhang P., Wang X., et al. (2012). Synthesis of biodegradable and electroactive tetraaniline grafted poly(ester amide) copolymers for bone tissue engineering. Biomacromolecules 13 2881–2889. 10.1021/bm300897j [DOI] [PubMed] [Google Scholar]
- Cui W., Liu Q., Yang L., Wang K., Sun T., Ji Y., et al. (2018). Sustained delivery of BMP-2-related peptide from the true bone ceramics/hollow mesoporous silica nanoparticles scaffold for bone tissue regeneration. ACS Biomater. Sci. Eng. 4 211–221. 10.1021/acsbiomaterials.7b00506 [DOI] [PubMed] [Google Scholar]
- D’Amora U., Russo T., De Santis R., Gloria A., Ambrosio L. (2016). “Hybrid nanocomposites with magnetic activation for advanced bone tissue engineering,” in Bio-Inspired Regenerative Medicine: Materials, Processes, and Clinical Applications, ed. Tampieri A. (New York, NY: Pan Stanford publishing; ), 179 10.1201/b19914-8 [DOI] [Google Scholar]
- Daculsi G. (1998). Biphasic calcium phosphate concept applied to artificial bone, implant coating and injectable bone substitute. Biomaterials 19 1473–1478. 10.1016/S0142-9612(98)00061-1 [DOI] [PubMed] [Google Scholar]
- Dalby M. J., Gadegaard N., Tare R., Andar A., Riehle M. O., Herzyk P., et al. (2007). The control of human mesenchymal cell differentiation using nanoscale symmetry and disorder. Nat. Mater. 6 997–1003. 10.1038/nmat2013 [DOI] [PubMed] [Google Scholar]
- Damaraju S. M., Shen Y., Elele E., Khusid B., Eshghinejad A., Li J., et al. (2017). Three-dimensional piezoelectric fibrous scaffolds selectively promote mesenchymal stem cell differentiation. Biomaterials 149 51–62. 10.1016/j.biomaterials.2017.09.024 [DOI] [PubMed] [Google Scholar]
- Damaraju S. M., Wu S., Jaffe M., Arinzeh T. L. (2013). Structural changes in PVDF fibers due to electrospinning and its effect on biological function. Biomed. Mater. 8:045007 10.1088/1748-6041/8/4/045007 [DOI] [PubMed] [Google Scholar]
- Daristotle J. L., Behrens A. M., Sandler A. D., Kofinas P. (2016). A review of the fundamental principles and applications of solution blow spinning. ACS Appl. Mater. Interfaces 8 34951–34963. 10.1021/acsami.6b12994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- David Roodman G. (2003). Role of stromal−derived cytokines and growth factors in bone metastasis. Cancer 97 733–738. 10.1002/cncr.11148 [DOI] [PubMed] [Google Scholar]
- De Bruijn J., Klein C., De Groot K., Van Blitterswijk C. (1992). The ultrastructure of the bone−hydroxyapatite interface in vitro. J. Biomed. Mater. Res. 26 1365–1382. 10.1002/jbm.820261008 [DOI] [PubMed] [Google Scholar]
- De la Riva B., Sánchez E., Hernández A., Reyes R., Tamimi F., López-Cabarcos E., et al. (2010). Local controlled release of VEGF and PDGF from a combined brushite–chitosan system enhances bone regeneration. J. Controlled Release 143 45–52. 10.1016/j.jconrel.2009.11.026 [DOI] [PubMed] [Google Scholar]
- Diaz-Gomez L., García-González C. A., Wang J., Yang F., Aznar-Cervantes S., Cenis J. L., et al. (2017). Biodegradable PCL/fibroin/hydroxyapatite porous scaffolds prepared by supercritical foaming for bone regeneration. Int. J. Pharma. 527 115–125. 10.1016/j.ijpharm.2017.05.038 [DOI] [PubMed] [Google Scholar]
- Dimitriou R., Jones E., McGonagle D., Giannoudis P. V. (2011). Bone regeneration: current concepts and future directions. BMC Med. 9:66. 10.1186/1741-7015-9-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding Z., Fan Z., Huang X., Lu Q., Xu W., Kaplan D. L. (2016). Silk–hydroxyapatite nanoscale scaffolds with programmable growth factor delivery for bone repair. ACS Appl. Mater. Interf. 8 24463–24470. 10.1021/acsami.6b08180 [DOI] [PubMed] [Google Scholar]
- Dong X., Wang Q., Wu T., Pan H. (2007). Understanding adsorption-desorption dynamics of BMP-2 on hydroxyapatite (001) surface. Biophys. J. 93 750–759. 10.1529/biophysj.106.103168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Y., Guo J. L., Wang J., Mikos A. G., Zhang S. (2019). Hierarchically designed bone scaffolds: from internal cues to external stimuli. Biomaterials 218:119334. 10.1016/j.biomaterials.2019.119334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan B., Cheung W. L., Wang M. (2011). Optimized fabrication of Ca-P/PHBV nanocomposite scaffolds via selective laser sintering for bone tissue engineering. Biofabrication 3:015001 10.1088/1758-5082/3/1/015001 [DOI] [PubMed] [Google Scholar]
- Dubey A. K., Basu B., Bandyopadhyay A. (2014). Pulsed electrical stimulation and surface charge induced cell growth on multistage spark plasma sintered hydroxyapatite-barium titanate piezobiocomposite. J. Am. Ceram. Soc. 97 481–489. 10.1111/jace.12647 [DOI] [Google Scholar]
- Dubey A. K., Ea A., Balani K., Basu B., Bandyopadhyay A. (2013). Multifunctional properties of multistage spark plasma sintered HA-BaTiO 3 -based piezobiocomposites for bone replacement applications. J. Am. Ceramic Soc. 96 3753–3759. 10.1111/jace.12566 [DOI] [Google Scholar]
- Dubey A. K., Gupta S. D., Basu B. (2011). Optimization of electrical stimulation parameters for enhanced cell proliferation on biomaterial surfaces. J. Biomed. Mater. Res. 98 18–29. 10.1002/jbm.b.31827 [DOI] [PubMed] [Google Scholar]
- Dubey A. K., Kinoshita R., Kakimoto K.-I. (2015). Piezoelectric sodium potassium niobate mediated improved polarization and in vitro bioactivity of hydroxyapatite. RSC Adv. 5 19638–19646. 10.1039/C5RA00771B [DOI] [Google Scholar]
- Ducheyne P. (2015). Comprehensive Biomaterials. Amsterdam: Elsevier. [Google Scholar]
- Dziadek M., Stodolak-Zych E., Cholewa-Kowalska K. (2017). Biodegradable ceramic-polymer composites for biomedical applications: a review. Mater. Sci. Eng. C 71 1175–1191. 10.1016/j.msec.2016.10.014 [DOI] [PubMed] [Google Scholar]
- Ehterami A., Kazemi M., Nazari B., Saraeian P., Azami M. (2018). Fabrication and characterization of highly porous barium titanate based scaffold coated by Gel/HA nanocomposite with high piezoelectric coefficient for bone tissue engineering applications. J. Mech. Behav. Biomed. Mater. 79 195–202. 10.1016/j.jmbbm.2017.12.034 [DOI] [PubMed] [Google Scholar]
- Einhorn T. A., Gerstenfeld L. C. (2015). Fracture healing: mechanisms and interventions. Nat. Rev. Rheumatol. 11 45–54. 10.1038/nrrheum.2014.164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fadeev I. V., Shvorneva L. I., Barinov S. M., Orlovskii V. P. (2003). Synthesis and structure of magnesium-substituted hydroxyapatite. Inorganic Mater. 39 947–950. 10.1023/A:1025509305805 [DOI] [Google Scholar]
- Fan D., De Rosa E., Murphy M. B., Peng Y., Smid C. A., Chiappini C., et al. (2012). Mesoporous silicon−PLGA composite microspheres for the double controlled release of biomolecules for orthopedic tissue engineering. Adv. Funct. Mater. 22 282–293. 10.1002/adfm.201100403 [DOI] [Google Scholar]
- Fan R., Deng X., Zhou L., Gao X., Fan M., Wang Y., et al. (2014). Injectable thermosensitive hydrogel composite with surface-functionalized calcium phosphate as raw materials. Int. J. Nanomed. 9:615. 10.2147/IJN.S52689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farokhi M., Mottaghitalab F., Shokrgozar M. A., Ai J., Hadjati J., Azami M. (2014). Bio-hybrid silk fibroin/calcium phosphate/PLGA nanocomposite scaffold to control the delivery of vascular endothelial growth factor. Mater. Sci. Eng. C 35 401–410. 10.1016/j.msec.2013.11.023 [DOI] [PubMed] [Google Scholar]
- Farshid B., Lalwani G., Shir Mohammadi M., Simonsen J., Sitharaman B. (2017). Boron nitride nanotubes and nanoplatelets as reinforcing agents of polymeric matrices for bone tissue engineering. J. Biomed. Mater. Res. B Appl. Biomater. 105 406–419. 10.1002/jbm.b.33565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng P., Wei P., Shuai C., Peng S. (2014). Characterization of mechanical and biological properties of 3-D scaffolds reinforced with zinc oxide for bone tissue engineering. PLoS One 9:e87755. 10.1371/journal.pone.0087755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandes J. S., Gentile P., Martins M., Neves N. M., Miller C., Crawford A., et al. (2016). Reinforcement of poly-l-lactic acid electrospun membranes with strontium borosilicate bioactive glasses for bone tissue engineering. Acta Biomater. 44 168–177. 10.1016/j.actbio.2016.08.042 [DOI] [PubMed] [Google Scholar]
- Fernandez de Grado G., Keller L., Idoux-Gillet Y., Wagner Q., Musset A.-M., Benkirane-Jessel N., et al. (2018). Bone substitutes: a review of their characteristics, clinical use, and perspectives for large bone defects management. J. Tissue Eng. 9:204173141877681. 10.1177/2041731418776819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez F., Babu S. S., Komath M., Varma H. (2020). “Biointegration of bone graft substiutes from osteointegration to osteotranduction,” in Biointegration of Medical Implant Materials, ed. Sharma C. P. (Amsterdam: Elsevier; ), 245–261. 10.1016/B978-0-08-102680-9.00010-X [DOI] [Google Scholar]
- Fielding G., Bose S. (2013). SiO2 and ZnO dopants in three-dimensionally printed tricalcium phosphate bone tissue engineering scaffolds enhance osteogenesis and angiogenesis in vivo. Acta Biomater. 9 9137–9148. 10.1016/j.actbio.2013.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filardo G., Kon E., Tampieri A., Cabezas-Rodríguez R., Di Martino A., Fini M., et al. (2014). New bio-ceramization processes applied to vegetable hierarchical structures for bone regeneration: an experimental model in sheep. Tissue Eng. Part A 20 763–773. 10.1089/ten.TEA.2013.0108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filardo G., Roffi A., Fey T., Fini M., Giavaresi G., Marcacci M., et al. (2019). Vegetable hierarchical structures as template for bone regeneration: new bio−ceramization process for the development of a bone scaffold applied to an experimental sheep model. J. Biomed. Mater. Res. Part B 108 600–611. 10.1002/jbm.b.34414 [DOI] [PubMed] [Google Scholar]
- Fiorilli S., Molino G., Pontremoli C., Iviglia G., Torre E., Cassinelli C., et al. (2018). The incorporation of strontium to improve bone-regeneration ability of mesoporous bioactive glasses. Materials 11:678. 10.3390/ma11050678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franz S., Rammelt S., Scharnweber D., Simon J. C. (2011). Immune responses to implants–a review of the implications for the design of immunomodulatory biomaterials. Biomaterials 32 6692–6709. 10.1016/j.biomaterials.2011.05.078 [DOI] [PubMed] [Google Scholar]
- Frasnelli M., Cristofaro F., Sglavo V. M., Dirè S., Callone E., Ceccato R., et al. (2017). Synthesis and characterization of strontium-substituted hydroxyapatite nanoparticles for bone regeneration. Mater. Sci. Eng. C 71 653–662. 10.1016/j.msec.2016.10.047 [DOI] [PubMed] [Google Scholar]
- Fratzl P., Weinkamer R. (2007). Nature’s hierarchical materials. Prog. Mater. Sci. 52 1263–1334. 10.1016/j.pmatsci.2007.06.001 [DOI] [Google Scholar]
- Fredericks D. C., Nepola J. V., Baker J. T., Abbott J., Simon B. (2000). Effects of pulsed electromagnetic fields on bone healing in a rabbit tibial osteotomy model. J. Orthop. Trauma 14 93–100. 10.1097/00005131-200002000-00004 [DOI] [PubMed] [Google Scholar]
- Friess W. (1998). Collagen–biomaterial for drug delivery. Eur. J. Pharm. Biopharm. 45 113–136. 10.1016/S0939-6411(98)00017-4 [DOI] [PubMed] [Google Scholar]
- Fukada E., Yasuda I. (1957). On the piezoelectric effect of bone. J. Phys. Soc. Japan 12 1158–1162. 10.1143/JPSJ.12.1158 29347132 [DOI] [Google Scholar]
- Funk R. H. W. (2015). Endogenous electric fields as guiding cue for cell migration. Front. Physiol. 6:143. 10.3389/fphys.2015.00143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furlan R. G., Correr W. R., Russi A. F. C., da Costa Iemma M. R., Trovatti E., Pecoraro É. (2018). Preparation and characterization of boron-based bioglass by sol- gel process. J. Sol-Gel Sci. Technol. 88 181–191. 10.1007/s10971-018-4806-8 [DOI] [Google Scholar]
- Gan J. C., Glazer P. A. (2006). Electrical stimulation therapies for spinal fusions: current concepts. Eur. Spine J. 15 1301–1311. 10.1007/s00586-006-0087-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan Q., Zhu J., Yuan Y., Liu H., Qian J., Li Y., et al. (2015). A dual-delivery system of pH-responsive chitosan-functionalized mesoporous silica nanoparticles bearing BMP-2 and dexamethasone for enhanced bone regeneration. J. Mater. Chem. B 3 2056–2066. 10.1039/C4TB01897D [DOI] [PubMed] [Google Scholar]
- Ghanaati S., Barbeck M., Orth C., Willershausen I., Thimm B. W., Hoffmann C., et al. (2010). Influence of β-tricalcium phosphate granule size and morphology on tissue reaction in vivo. Acta Biomater. 6 4476–4487. 10.1016/j.actbio.2010.07.006 [DOI] [PubMed] [Google Scholar]
- Giannoudis P. V., Dinopoulos H., Tsiridis E. (2005). Bone substitutes: an update. Injury 36 S20–S27. 10.1016/j.injury.2005.07.029 [DOI] [PubMed] [Google Scholar]
- Gibbs D. M., Black C. R., Dawson J. I., Oreffo R. O. (2016). A review of hydrogel use in fracture healing and bone regeneration. J. Tissue Eng. Regen. Med. 10 187–198. 10.1002/term.1968 [DOI] [PubMed] [Google Scholar]
- Gimenes R., Bar-Cohen Y., Zaghete M. A., Bertolini M., Varela J. A., Coelho L. O., et al. (2004). “Composites PVDF-TrFE/BT used as bioactive membranes for enhancing bone regeneration,” in Proceedings of the Smart Structures and Materials 2004: Electroactive Polymer Actuators and Devices (EAPAD) 5385, San Diego, CA, 539 10.1117/12.548647 [DOI] [Google Scholar]
- Gkiokas A., Morassi L. G., Kohl S., Zampakides C., Megremis P., Evangelopoulos D. S. (2012). Bioabsorbable pins for treatment of osteochondral fractures of the knee after acute patella dislocation in children and young adolescents. Adv. Orthop. 2012:249687. 10.1155/2012/249687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein C., Sprague S., Petrisor B. A. (2010). Electrical stimulation for fracture healing: current evidence. J. Orthop. Trauma 24(Suppl. 1) S62–S65. 10.1097/BOT.0b013e3181cdde1b [DOI] [PubMed] [Google Scholar]
- Gong T. (2015). Nanomaterials and Regenrative Medicine, Vol. 10 Zagreb: IAPC Publishing. [Google Scholar]
- Grabowski G., Cornett C. A. (2013). Bone graft and bone graft substitutes in spine surgery: current concepts and controversies. J. Am. Acad. Orthop. Surg. 21 51–60. 10.5435/JAAOS-21-01-51 [DOI] [PubMed] [Google Scholar]
- Gruskay J. A., Basques B. A., Bohl D. D., Webb M. L., Grauer J. N. (2014). Short-term adverse events, length of stay, and readmission after iliac crest bone graft for spinal fusion. Spine (Phila Pa 1976) 39 1718–1724. 10.1097/BRS.0000000000000476 [DOI] [PubMed] [Google Scholar]
- Gu W., Wu C., Chen J., Xiao Y. (2013). Nanotechnology in the targeted drug delivery for bone diseases and bone regeneration. Int. J. Nanomedicine 8 2305–2317. 10.2147/IJN.S44393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guex A. G., Puetzer J. L., Armgarth A., Littmann E., Stavrinidou E., Giannelis E. P., et al. (2017). Highly porous scaffolds of PEDOT:PSS for bone tissue engineering. Acta Biomater. 62 91–101. 10.1016/j.actbio.2017.08.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guihard P., Boutet M.-A., Brounais-Le Royer B., Gamblin A.-L., Amiaud J., Renaud A., et al. (2015). Oncostatin m, an inflammatory cytokine produced by macrophages, supports intramembranous bone healing in a mouse model of tibia injury. Am. J. Pathol. 185 765–775. 10.1016/j.ajpath.2014.11.008 [DOI] [PubMed] [Google Scholar]
- Guihard P., Danger Y., Brounais B., David E., Brion R., Delecrin J., et al. (2012). Induction of osteogenesis in mesenchymal stem cells by activated monocytes/macrophages depends on oncostatin M signaling. Stem Cells 30 762–772. 10.1002/stem.1040 [DOI] [PubMed] [Google Scholar]
- Gupta A., Kukkar N., Sharif K., Main B. J., Albers C. E., El-Amin Iii S. F. (2015). Bone graft substitutes for spine fusion: a brief review. World J. Orthop. 6 449–456. 10.5312/wjo.v6.i6.449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta H. S., Wagermaier W., Zickler G. A., Raz-Ben Aroush D., Funari S. S., Roschger P., et al. (2005). Nanoscale deformation mechanisms in bone. Nano Lett. 5 2108–2111. 10.1021/nl051584b [DOI] [PubMed] [Google Scholar]
- Gusic N., Ivkovic A., VaFaye J., Vukasovic A., Ivkovic J., Hudetz D., et al. (2014). Nanobiotechnology and bone regeneration: a mini-review. Int. Orthop. 38 1877–1884. 10.1007/s00264-014-2412-0 [DOI] [PubMed] [Google Scholar]
- Habraken W., Wolke J., Jansen J. (2007). Ceramic composites as matrices and scaffolds for drug delivery in tissue engineering. Adv. Drug Deliv. Rev. 59 234–248. 10.1016/j.addr.2007.03.011 [DOI] [PubMed] [Google Scholar]
- Hadley K. B., Newman S. M., Hunt J. R. (2010). Dietary zinc reduces osteoclast resorption activities and increases markers of osteoblast differentiation, matrix maturation, and mineralization in the long bones of growing rats. J. Nutr. Biochem. 21 297–303. 10.1016/j.jnutbio.2009.01.002 [DOI] [PubMed] [Google Scholar]
- Häfeli U. O., Riffle J. S., Harris-Shekhawat L., Carmichael-Baranauskas A., Mark F., Dailey J. P., et al. (2009). Cell uptake and in vitro toxicity of magnetic nanoparticles suitable for drug delivery. Mol. Pharma. 6 1417–1428. 10.1021/mp900083m [DOI] [PubMed] [Google Scholar]
- Haider A., Haider S., Kang I.-K. (2018). A comprehensive review summarizing the effect of electrospinning parameters and potential applications of nanofibers in biomedical and biotechnology. Arabian J. Chem. 11 1165–1188. 10.1016/j.arabjc.2015.11.015 [DOI] [Google Scholar]
- Halperin C., Mutchnik S., Agronin A., Molotskii M., Urenski P., Salai M., et al. (2004). Piezoelectric effect in human bones studied in nanometer scale. Nano Lett. 4 1253–1256. 10.1021/nl049453i [DOI] [Google Scholar]
- He Q., Zhao Y., Chen B., Xiao Z., Zhang J., Chen L., et al. (2011). Improved cellularization and angiogenesis using collagen scaffolds chemically conjugated with vascular endothelial growth factor. Acta Biomater. 7 1084–1093. 10.1016/j.actbio.2010.10.022 [DOI] [PubMed] [Google Scholar]
- Hench L. L., Roki N., Fenn M. B. (2014). Bioactive glasses: importance of structure and properties in bone regeneration. J. Mol. Struct. 1073 24–30. 10.1016/j.molstruc.2014.03.066 [DOI] [Google Scholar]
- Henkel J., Woodruff M. A., Epari D. R., Steck R., Glatt V., Dickinson I. C., et al. (2013). Bone regeneration based on tissue engineering conceptions-A 21st century perspective. Bone Res. 1 216–248. 10.4248/BR201303002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heo S. J., Kim S. E., Wei J., Hyun Y. T., Yun H. S., Kim D. H., et al. (2009). Fabrication and characterization of novel nano−and micro−HA/PCL composite scaffolds using a modified rapid prototyping process. J. Biomed. Mater. Res. Part A 89 108–116. 10.1002/jbm.a.31726 [DOI] [PubMed] [Google Scholar]
- Ho-Shui-Ling A., Bolander J., Rustom L. E., Johnson A. W., Luyten F. P., Picart C. (2018). Bone regeneration strategies: engineered scaffolds, bioactive molecules and stem cells current stage and future perspectives. Biomaterials 180 143–162. 10.1016/j.biomaterials.2018.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoare T. R., Kohane D. S. (2008). Hydrogels in drug delivery: progress and challenges. Polymer 49 1993–2007. 10.1016/j.polymer.2008.01.027 [DOI] [Google Scholar]
- Hoffman A. S. (2012). Hydrogels for biomedical applications. Adv. Drug Deliv. Rev. 64 18–23. 10.1016/j.addr.2012.09.010 [DOI] [PubMed] [Google Scholar]
- Holzapfel B. M., Wagner F., Martine L. C., Reppenhagen S., Rudert M., Schuetz M., et al. (2016). Tissue engineering and regenerative medicine in musculoskeletal oncology. Cancer Metastasis Rev. 35 475–487. 10.1007/s10555-016-9635-z [DOI] [PubMed] [Google Scholar]
- Hu Y., Cai K., Luo Z., Xu D., Xie D., Huang Y., et al. (2012). TiO2 nanotubes as drug nanoreservoirs for the regulation of mobility and differentiation of mesenchymal stem cells. Acta Biomater. 8 439–448. 10.1016/j.actbio.2011.10.021 [DOI] [PubMed] [Google Scholar]
- Huang D. M., Hsiao J. K., Chen Y. C., Chien L. Y., Yao M., Chen Y. K., et al. (2009). The promotion of human mesenchymal stem cell proliferation by superparamagnetic iron oxide nanoparticles. Biomaterials 30 3645–3651. 10.1016/j.biomaterials.2009.03.032 [DOI] [PubMed] [Google Scholar]
- Huang P., Wang J., Lai S., Liu F., Ni N., Cao Q., et al. (2014). Surface modified titania nanotubes containing anti-bacterial drugs for controlled delivery nanosystems with high bioactivity. J. Mater. Chem. B 2 8616–8625. 10.1039/C4TB01281J [DOI] [PubMed] [Google Scholar]
- Ikada Y., Shikinami Y., Hara Y., Tagawa M., Fukada E. (1996). Enhancement of bone formation by drawn poly(L-lactide). J. Biomed. Mater. Res. 30 553–558. [DOI] [PubMed] [Google Scholar]
- Ikeda R., Fujioka H., Nagura I., Kokubu T., Toyokawa N., Inui A., et al. (2009). The effect of porosity and mechanical property of a synthetic polymer scaffold on repair of osteochondral defects. Int. Orthop. 33 821–828. 10.1007/s00264-008-0532-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam M. T., Felfel R. M., Abou Neel E. A., Grant D. M., Ahmed I., Hossain K. M. Z. (2017). Bioactive calcium phosphate–based glasses and ceramics and their biomedical applications: a review. J. Tissue Eng. 8:2041731417719170. 10.1177/2041731417719170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izquierdo-Barba I., Salinas A. J., Vallet-Regí M. (2013). Bioactive glasses: from macro to nano. Int. J. App. Glass Sci. 4, 149–161. 10.1111/ijag.12028 [DOI] [Google Scholar]
- Jacob J., Haponiuk J. T., Thomas S., Gopi S. (2018). Biopolymer based nanomaterials in drug delivery systems: a review. Mater. Today Chem. 9 43–55. 10.1016/j.mtchem.2018.05.002 [DOI] [Google Scholar]
- Jansen J. H., van der Jagt O. P., Punt B. J., Verhaar J. A., van Leeuwen J. P., Weinans H., et al. (2010). Stimulation of osteogenic differentiation in human osteoprogenitor cells by pulsed electromagnetic fields: an in vitro study. BMC Musculoskelet Disord. 11:188. 10.1186/1471-2474-11-188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeon B. J., Jeong S. Y., Koo A. N., Kim B.-C., Hwang Y.-S., Lee S. C. (2012). Fabrication of porous PLGA microspheres with BMP-2 releasing polyphosphate-functionalized nano-hydroxyapatite for enhanced bone regeneration. Macromol. Res. 20 715–724. 10.1007/s13233-012-0103-5 [DOI] [Google Scholar]
- Jianqing F., Huipin Y., Xingdong Z. (1997). Promotion of osteogenesis by a piezoelectric biological ceramic. Biomaterials 18 1531–1534. 10.1016/S0142-9612(97)80004-X [DOI] [PubMed] [Google Scholar]
- Jiao H., Zhao K., Ma L., Tang Y., Liu X., Bian T. (2017). Preparation and characterization of BaTiO3/HA nanocomposite materials by hydrothermal synthesis. J. Alloys Compounds 693 221–225. 10.1016/j.jallcom.2016.09.175 [DOI] [Google Scholar]
- Jones J. R., Brauer D. S., Hupa L., Greenspan D. C. (2016). Bioglass and bioactive glasses and their impact on healthcare. Int. J. Appl. Glass Sci. 7 423–434. 10.1111/ijag.12252 [DOI] [Google Scholar]
- Jose M., Thomas V., Johnson K., Dean D., Nyairo E. (2009). Aligned PLGA/HA nanofibrous nanocomposite scaffolds for bone tissue engineering. Acta Biomater. 5 305–315. 10.1016/j.actbio.2008.07.019 [DOI] [PubMed] [Google Scholar]
- Kaigler D., Wang Z., Horger K., Mooney D. J., Krebsbach P. H. (2006). VEGF scaffolds enhance angiogenesis and bone regeneration in irradiated osseous defects. J. Bone Mineral Res. 21 735–744. 10.1359/jbmr.060120 [DOI] [PubMed] [Google Scholar]
- Kalbacova M., Broz A., Kong J., Kalbac M. (2010). Graphene substrates promote adherence of human osteoblasts and mesenchymal stromal cells. Carbon 48 4323–4329. 10.1016/j.carbon.2010.07.045 [DOI] [Google Scholar]
- Kalita S. J., Bhatt H. A. (2007). Nanocrystalline hydroxyapatite doped with magnesium and zinc: synthesis and characterization. Mater. Sci. Eng. C 27 837–848. 10.1016/j.msec.2006.09.036 [DOI] [Google Scholar]
- Kalita S. J., Verma S. (2010). Nanocrystalline hydroxyapatite bioceramic using microwave radiation: synthesis and characterization. Mater. Sci. Eng. C 30 295–303. 10.1016/j.msec.2009.11.007 [DOI] [PubMed] [Google Scholar]
- Kamitakahara M., Ohtsuki C., Miyazaki T. (2008). Behavior of ceramic biomaterials derived from tricalcium phosphate in physiological condition. J. Biomater. Appl. 23 197–212. 10.1177/0885328208096798 [DOI] [PubMed] [Google Scholar]
- Kang K. S., Hong J. M., Jeong Y. H., Seol Y. J., Yong W. J., Rhie J. W., et al. (2014). Combined effect of three types of biophysical stimuli for bone regeneration. Tissue Eng. Part A 20 1767–1777. 10.1089/ten.TEA.2013.0157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang M. S., Kim J.-H., Singh R. K., Jang J.-H., Kim H.-W. (2015). Therapeutic-designed electrospun bone scaffolds: mesoporous bioactive nanocarriers in hollow fiber composites to sequentially deliver dual growth factors. Acta Biomater. 16 103–116. 10.1016/j.actbio.2014.12.028 [DOI] [PubMed] [Google Scholar]
- Kao F. C., Chiu P. Y., Tsai T. T., Lin Z. H. (2019). The application of nanogenerators and piezoelectricity in osteogenesis. Sci. Technol. Adv. Mater. 20 1103–1117. 10.1080/14686996.2019.1693880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan F., Hayes W., Keaveny T., Boskey A., Einhorn T., Iannotti J. (1994). Orthopedic basic science. Am. Acad. Orthop. Surg. 1 127–145. [Google Scholar]
- Kargozar S., Baino F., Hamzehlou S., Hill R. G., Mozafari M. (2018). Bioactive glasses: sprouting angiogenesis in tissue engineering. Trends Biotechnol. 36 430–444. 10.1016/j.tibtech.2017.12.003 [DOI] [PubMed] [Google Scholar]
- Kaur G., Adhikari R., Cass P., Bown M., Gunatillake P. (2015). Electrically conductive polymers and composites for biomedical applications. RSC Adv. 5 37553–37567. 10.1039/C5RA01851J [DOI] [Google Scholar]
- Kaya S., Cresswell M., Boccaccini A. R. (2018). Mesoporous silica-based bioactive glasses for antibiotic-free antibacterial applications. Mater. Sci. Eng. C 83 99–107. 10.1016/j.msec.2017.11.003 [DOI] [PubMed] [Google Scholar]
- Kempen D. H., Lu L., Heijink A., Hefferan T. E., Creemers L. B., Maran A., et al. (2009). Effect of local sequential VEGF and BMP-2 delivery on ectopic and orthotopic bone regeneration. Biomaterials 30 2816–2825. 10.1016/j.biomaterials.2009.01.031 [DOI] [PubMed] [Google Scholar]
- Kenar H., Kose G., Hasirci V. (2006). Tissue engineering of bone on micropatterned biodegradable polyester films. Biomaterials 27 885–895. 10.1016/j.biomaterials.2005.07.001 [DOI] [PubMed] [Google Scholar]
- Kim B.-S., Yang S.-S., Kim C. S. (2018). Incorporation of BMP-2 nanoparticles on the surface of a 3D-printed hydroxyapatite scaffold using an ε-polycaprolactone polymer emulsion coating method for bone tissue engineering. Colloids Surf. B Biointerf. 170 421–429. 10.1016/j.colsurfb.2018.06.043 [DOI] [PubMed] [Google Scholar]
- Kim D., Lee B., Thomopoulos S., Jun Y.-S. (2018). The role of confined collagen geometry in decreasing nucleation energy barriers to intrafibrillar mineralization. Nat. Commun. 9 1–9. 10.1038/s41467-018-03041-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H. W., Li L. H., Koh Y. H., Knowles J. C., Kim H. E. (2004). Sol–Gel preparation and properties of fluoride−substituted hydroxyapatite powders. J. Am. Ceramic Soc. 87 1939–1944. 10.1111/j.1151-2916.2004.tb06344.x [DOI] [Google Scholar]
- Kim H. W., Song J. H., Kim H. E. (2005). Nanofiber generation of gelatin–hydroxyapatite biomimetics for guided tissue regeneration. Adv. Funct. Mater. 15 1988–1994. 10.1002/adfm.200500116 [DOI] [Google Scholar]
- Kim J.-J., El-Fiqi A., Kim H.-W. (2017). Synergetic cues of bioactive nanoparticles and nanofibrous structure in bone scaffolds to stimulate osteogenesis and angiogenesis. ACS Appl. Mater. Interf. 9 2059–2073. 10.1021/acsami.6b12089 [DOI] [PubMed] [Google Scholar]
- Kim J. W., Shin Y. C., Lee J. J., Bae E. B., Jeon Y. C., Jeong C. M., et al. (2017). The effect of reduced graphene oxide-coated biphasic calcium phosphate bone graft material on osteogenesis. Int. J. Mol. Sci. 18:1725. 10.3390/ijms18081725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim K., Zhu W., Qu X., Aaronson C., McCall W. R., Chen S., et al. (2014). 3D optical printing of piezoelectric nanoparticle–polymer composite materials. ACS Nano 8 9799–9806. 10.1021/nn503268f [DOI] [PubMed] [Google Scholar]
- Kim S., Ku S. H., Lim S. Y., Kim J. H., Park C. B. (2011). Graphene-biomineral hybrid materials. Adv. Mater. 23 2009–2014. 10.1002/adma.201100010 [DOI] [PubMed] [Google Scholar]
- Kim S. E., Song S.-H., Yun Y. P., Choi B.-J., Kwon I. K., Bae M. S., et al. (2011). The effect of immobilization of heparin and bone morphogenic protein-2 (BMP-2) to titanium surfaces on inflammation and osteoblast function. Biomaterials 32 366–373. 10.1016/j.biomaterials.2010.09.008 [DOI] [PubMed] [Google Scholar]
- Kong C. H., Steffi C., Shi Z., Wang W. (2018). Development of mesoporous bioactive glass nanoparticles and its use in bone tissue engineering. J. Biomed. Mater. Res. Part B 106 2878–2887. 10.1002/jbm.b.34143 [DOI] [PubMed] [Google Scholar]
- Kumar A., Kargozar S., Baino F., Han S. S. (2019). Additive manufacturing methods for producing hydroxyapatite and hydroxyapatite-based composite scaffolds: a review. Front. Mater. 6:313 10.3389/fmats [DOI] [Google Scholar]
- Kwon D. H., Lee S. J., Wikesjö U. M., Johansson P. H., Johansson C. B., Sul Y. T. (2017). Bone tissue response following local drug delivery of bisphosphonate through titanium oxide nanotube implants in a rabbit model. J. Clin. Periodontol. 44 941–949. 10.1111/jcpe.12776 [DOI] [PubMed] [Google Scholar]
- Lai M., Cai K., Zhao L., Chen X., Hou Y., Yang Z. (2011). Surface functionalization of TiO2 nanotubes with bone morphogenetic protein 2 and its synergistic effect on the differentiation of mesenchymal stem cells. Biomacromolecules 12 1097–1105. 10.1021/bm1014365 [DOI] [PubMed] [Google Scholar]
- Lalegul-Ulker O., Elcin A. E., Elcin Y. M. (2018). Intrinsically conductive polymer nanocomposites for cellular applications. Adv. Exp. Med. Biol. 1078 135–153. 10.1007/978-981-13-0950-2_8 [DOI] [PubMed] [Google Scholar]
- Lallana E., Sousa-Herves A., Fernandez-Trillo F., Riguera R., Fernandez-Megia E. (2012). Click chemistry for drug delivery nanosystems. Pharm. Res. 29 1–34. 10.1007/s11095-011-0568-5 [DOI] [PubMed] [Google Scholar]
- Lalzawmliana V., Anand A., Kumar V., Das P., Devi K. B., Mukherjee J., et al. (2019). Potential of growth factor incorporated mesoporous bioactive glass for in vivo bone regeneration. J. Mech. Behav. Biomed. Mater. 91 182–192. 10.1016/j.jmbbm.2018.12.012 [DOI] [PubMed] [Google Scholar]
- Lalzawmliana V., Anand A., Roy M., Kundu B., Nandi S. K. (2020). Mesoporous bioactive glasses for bone healing and biomolecules delivery. Mater. Sci. Eng. C 106:110180. 10.1016/j.msec.2019.110180 [DOI] [PubMed] [Google Scholar]
- Landi E., Tampieri A., Mattioli-Belmonte M., Celotti G., Sandri M., Gigante A., et al. (2006). Biomimetic Mg- and Mg, CO3-substituted hydroxyapatites: synthesis characterization and in vitro behaviour. J. Eur. Ceramic Soc. 26 2593–2601. 10.1016/j.jeurceramsoc.2005.06.040 [DOI] [Google Scholar]
- Landi E., Valentini F., Tampieri A. (2008). Porous hydroxyapatite/gelatine scaffolds with ice-designed channel-like porosity for biomedical applications. Acta Biomater. 4 1620–1626. 10.1016/j.actbio.2008.05.023 [DOI] [PubMed] [Google Scholar]
- Lee E. J., Kasper F. K., Mikos A. G. (2014). Biomaterials for tissue engineering. Ann. Biomed. Eng. 42 323–337. 10.1007/s10439-013-0859-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.-H., Mandakhbayar N., El-Fiqi A., Kim H.-W. (2017). Intracellular co-delivery of Sr ion and phenamil drug through mesoporous bioglass nanocarriers synergizes BMP signaling and tissue mineralization. Acta Biomater. 60 93–108. 10.1016/j.actbio.2017.07.021 [DOI] [PubMed] [Google Scholar]
- Lee J., Byun H., Madhurakkat Perikamana S. K., Lee S., Shin H. (2019). Current advances in immunomodulatory biomaterials for bone regeneration. Adv. Healthcare Mater. 8:1801106. 10.1002/adhm.201801106 [DOI] [PubMed] [Google Scholar]
- Lee J., Yoo J. J., Atala A., Lee S. J. (2012). The effect of controlled release of PDGF-BB from heparin-conjugated electrospun PCL/gelatin scaffolds on cellular bioactivity and infiltration. Biomaterials 33 6709–6720. 10.1016/j.biomaterials.2012.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S. S., Fyrner T., Chen F., Álvarez Z., Sleep E., Chun D. S., et al. (2017). Sulfated glycopeptide nanostructures for multipotent protein activation. Nature Nanotechnol. 12 821–829. 10.1038/nnano.2017.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S. S., Hsu E. L., Mendoza M., Ghodasra J., Nickoli M. S., Ashtekar A., et al. (2015). Gel scaffolds of BMP−2−binding peptide amphiphile nanofibers for spinal arthrodesis. Adv. Healthcare Mater. 4 131–141. 10.1002/adhm.201400129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S. S., Huang B. J., Kaltz S. R., Sur S., Newcomb C. J., Stock S. R., et al. (2013). Bone regeneration with low dose BMP-2 amplified by biomimetic supramolecular nanofibers within collagen scaffolds. Biomaterials 34 452–459. 10.1016/j.biomaterials.2012.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee W. C., Lim C. H., Shi H., Tang L. A., Wang Y., Lim C. T., et al. (2011). Origin of enhanced stem cell growth and differentiation on graphene and graphene oxide. ACS Nano 5 7334–7341. 10.1021/nn202190c [DOI] [PubMed] [Google Scholar]
- LeGeros R. Z. (2008). Calcium phosphate-based osteoinductive materials. Chem. Rev. 108 4742–4753. 10.1021/cr800427g [DOI] [PubMed] [Google Scholar]
- Leite A. I. J., Gonçalves A. I., Rodrigues M. R. T., Gomes M. E., Mano J. O. F. (2018). Strontium-doped bioactive glass nanoparticles in osteogenic commitment. ACS Appl. Mater. Interf. 10 23311–23320. 10.1021/acsami.8b06154 [DOI] [PubMed] [Google Scholar]
- Leung V., Ko F. (2011). Biomedical applications of nanofibers. Polym. Adv. Technol. 22 350–365. 10.1002/pat.1813 [DOI] [Google Scholar]
- Li C., Vepari C., Jin H.-J., Kim H. J., Kaplan D. L. (2006). Electrospun silk-BMP-2 scaffolds for bone tissue engineering. Biomaterials 27 3115–3124. 10.1016/j.biomaterials.2006.01.022 [DOI] [PubMed] [Google Scholar]
- Li L., Yu M., Ma P. X., Guo B. (2016). Electroactive degradable copolymers enhancing osteogenic differentiation from bone marrow derived mesenchymal stem cells. J. Mater. Chem. 4 471–481. 10.1039/C5TB01899D [DOI] [PubMed] [Google Scholar]
- Li L., Zhou G., Wang Y., Yang G., Ding S., Zhou S. (2015). Controlled dual delivery of BMP-2 and dexamethasone by nanoparticle-embedded electrospun nanofibers for the efficient repair of critical-sized rat calvarial defect. Biomaterials 37 218–229. 10.1016/j.biomaterials.2014.10.015 [DOI] [PubMed] [Google Scholar]
- Li W.-J., Mauck R. L., Cooper J. A., Yuan X., Tuan R. S. (2007). Engineering controllable anisotropy in electrospun biodegradable nanofibrous scaffolds for musculoskeletal tissue engineering. J. Biomech. 40 1686–1693. 10.1016/j.jbiomech.2006.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Wang X., Jiang X., Yamaguchi M., Ito A., Bando Y., et al. (2016). Boron nitride nanotube-enhanced osteogenic differentiation of mesenchymal stem cells. J. Biomed. Mater. Res. B Appl. Biomater. 104 323–329. 10.1002/jbm.b.33391 [DOI] [PubMed] [Google Scholar]
- Li Z., Lu W. W., Chiu P. K. Y., Lam R. W. M., Xu B., Cheung K. M. C., et al. (2009). Strontium-calcium coadministration stimulates bone matrix osteogenic factor expression and new bone formation in a large animal model. J. Orthopaedic Res. 27 758–762. 10.1002/jor.20818 [DOI] [PubMed] [Google Scholar]
- Liang P., Zheng J., Zhang Z., Hou Y., Wang J., Zhang C., et al. (2019). Bioactive 3D scaffolds self-assembled from phosphorylated mimicking peptide amphiphiles to enhance osteogenesis. J. Biomater. Sci. Polym. Ed. 30 34–48. 10.1080/09205063.2018.1505264 [DOI] [PubMed] [Google Scholar]
- Liang Y., Kiick K. L. (2014). Heparin-functionalized polymeric biomaterials in tissue engineering and drug delivery applications. Acta Biomater. 10 1588–1600. 10.1016/j.actbio.2013.07.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim J. Y., Hansen J. C., Siedlecki C. A., Runt J., Donahue H. J. (2005). Human foetal osteoblastic cell response to polymer-demixed nanotopographic interfaces. J. R. Soc. Interface 2 97–108. 10.1098/rsif.2004.0019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liou S.-C., Chen S.-Y., Lee H.-Y., Bow J.-S. (2004). Structural characterization of nano-sized calcium deficient apatite powders. Biomaterials 25 189–196. 10.1016/S0142-9612(03)00479-4 [DOI] [PubMed] [Google Scholar]
- Liu B., Chen L., Shao C., Zhang F., Zhou K., Cao J., et al. (2016). Improved osteoblasts growth on osteomimetic hydroxyapatite/BaTiO3 composites with aligned lamellar porous structure. Mater. Sci. Eng. C Mater. Biol. Appl. 61 8–14. 10.1016/j.msec.2015.12.009 [DOI] [PubMed] [Google Scholar]
- Liu H., Slamovich E. B., Webster T. J. (2006). Increased osteoblast functions among nanophase titania/poly(lactide-co-glycolide) composites of the highest nanometer surface roughness. J. Biomed. Mater. Res. A 78 798–807. 10.1002/jbm.a.30734 [DOI] [PubMed] [Google Scholar]
- Liu J. M., Zhang X., Joe S., Luo X., Shea L. D. (2018). Evaluation of biomaterial scaffold delivery of IL-33 as a localized immunomodulatory agent to support cell transplantation in adipose tissue. J. Immunol. Regen. Med. 1 1–12. 10.1016/j.regen.2018.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L., Bhatia R., Webster T. J. (2017). Atomic layer deposition of nano-TiO2 thin films with enhanced biocompatibility and antimicrobial activity for orthopedic implants. Int. J. Nanomed. 12:8711. 10.2147/IJN.S148065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L., Li P., Zhou G., Wang M., Jia X., Liu M., et al. (2013). Increased proliferation and differentiation of pre-osteoblasts MC3T3-E1 cells on nanostructured polypyrrole membrane under combined electrical and mechanical stimulation. J. Biomed. Nanotechnol. 9 1532–1539. 10.1166/jbn.2013.1650 [DOI] [PubMed] [Google Scholar]
- Liu X.-Y., Qiu G.-X., Weng X.-S., Yu B., Wang Y.-P. (2014). What is the optimum fusion technique for adult spondylolisthesis—PLIF or PLF or PLIF Plus PLF? A meta-analysis from 17 comparative studies. Spine 39 1887–1898. 10.1097/BRS.0000000000000549 [DOI] [PubMed] [Google Scholar]
- Liu Y., Lu Y., Tian X., Cui G., Zhao Y., Yang Q., et al. (2009). Segmental bone regeneration using an rhBMP-2-loaded gelatin/nanohydroxyapatite/fibrin scaffold in a rabbit model. Biomaterials 30 6276–6285. 10.1016/j.biomaterials.2009.08.003 [DOI] [PubMed] [Google Scholar]
- Lode A., Reinstorf A., Bernhardt A., Wolf−Brandstetter C., König U., Gelinsky M. (2008). Heparin modification of calcium phosphate bone cements for VEGF functionalization. J. Biomed. Mater. Res. Part A 86 749–759. 10.1002/jbm.a.31581 [DOI] [PubMed] [Google Scholar]
- Lü J.-M., Wang X., Marin-Muller C., Wang H., Lin P. H., Yao Q., et al. (2009). Current advances in research and clinical applications of PLGA-based nanotechnology. Expert Rev. Mol. Diagnost. 9 325–341. 10.1586/erm.09.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucke M., Schmidmaier G., Sadoni S., Wildemann B., Schiller R., Haas N., et al. (2003). Gentamicin coating of metallic implants reduces implant-related osteomyelitis in rats. Bone 32 521–531. 10.1016/S8756-3282(03)00050-4 [DOI] [PubMed] [Google Scholar]
- Madl C. M., Mehta M., Duda G. N., Heilshorn S. C., Mooney D. J. (2014). Presentation of BMP-2 mimicking peptides in 3D hydrogels directs cell fate commitment in osteoblasts and mesenchymal stem cells. Biomacromolecules 15 445–455. 10.1021/bm401726u [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeder M. D., Damjanovic D., Setter N. (2004). Lead free piezoelectric materials. J. Electroceram. 13 385–392. 10.1007/s10832-004-5130-y [DOI] [Google Scholar]
- Magrez A., Horváth L., Smajda R., Salicio V., Pasquier N., Forro L., et al. (2009). Cellular toxicity of TiO2-based nanofilaments. ACS Nano 3 2274–2280. 10.1021/nn9002067 [DOI] [PubMed] [Google Scholar]
- Maier J. A., Bernardini D., Rayssiguier Y., Mazur A. (2004). High concentrations of magnesium modulate vascular endothelial cell behaviour in vitro. Biochim. Biophys. Acta (BBA) 1689 6–12. 10.1016/j.bbadis.2004.02.004 [DOI] [PubMed] [Google Scholar]
- Makadia H. K., Siegel S. J. (2011). Poly lactic-co-glycolic acid (PLGA) as biodegradable controlled drug delivery carrier. Polymers 3 1377–1397. 10.3390/polym3031377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malafaya P. B., Silva G. A., Reis R. L. (2007). Natural–origin polymers as carriers and scaffolds for biomolecules and cell delivery in tissue engineering applications. Adv. Drug Deliv. Rev. 59 207–233. 10.1016/j.addr.2007.03.012 [DOI] [PubMed] [Google Scholar]
- Malikmammadov E., Tanir T. E., Kiziltay A., Hasirci V., Hasirci N. (2018). PCL-TCP wet spun scaffolds carrying antibiotic-loaded microspheres for bone tissue engineering. J. Biomater. Sci. Polym. Ed. 29 805–824. 10.1080/09205063.2017.1354671 [DOI] [PubMed] [Google Scholar]
- Mancuso E., Bretcanu O. A., Marshall M., Birch M. A., McCaskie A. W., Dalgarno K. W. (2017). Novel bioglasses for bone tissue repair and regeneration: effect of glass design on sintering ability, ion release and biocompatibility. Mater. Design 129 239–248. 10.1016/j.matdes.2017.05.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marędziak M., Śmieszek A., Tomaszewski K. A., Lewandowski D., Marycz K. (2016). The effect of low static magnetic field on osteogenic and adipogenic differentiation potential of human adipose stromal/stem cells. J. Magn. Magn. Mater. 398 235–245. 10.1016/j.jmmm.2015.09.004 [DOI] [Google Scholar]
- Marino A., Arai S., Hou Y., Sinibaldi E., Pellegrino M., Chang Y.-T., et al. (2015). Piezoelectric nanoparticle-assisted wireless neuronal stimulation. ACS Nano 9 7678–7689. 10.1021/acsnano.5b03162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marino A., Genchi G. G., Mattoli V., Ciofani G. (2017). Piezoelectric nanotransducers: the future of neural stimulation. Nano Today 14 9–12. 10.1016/j.nantod.2016.12.005 [DOI] [Google Scholar]
- Marsell R., Einhorn T. A. (2011). The biology of fracture healing. Injury 42 551–555. 10.1016/j.injury.2011.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masquelet A. C., Fitoussi F., Begue T., Muller G. P. (2000). [Reconstruction of the long bones by the induced membrane and spongy autograft]. Ann. Chir. Plast. Esthet. 45 346–353. [PubMed] [Google Scholar]
- Mastrogiacomo M., Scaglione S., Martinetti R., Dolcini L., Beltrame F., Cancedda R., et al. (2006). Role of scaffold internal structure on in vivo bone formation in macroporous calcium phosphate bioceramics. Biomaterials 27 3230–3237. 10.1016/j.biomaterials.2006.01.031 [DOI] [PubMed] [Google Scholar]
- Matesanz M. C., Linares J., Lilue I., Sánchez-Salcedo S., Feito M. J., Arcos D., et al. (2014). Nanocrystalline silicon substituted hydroxyapatite effects on osteoclast differentiation and resorptive activity. J. Mater. Chem. B 2 2910–2919. 10.1039/c3tb21697g [DOI] [PubMed] [Google Scholar]
- Matsumoto T., Okazaki M., Inoue M., Yamaguchi S., Kusunose T., Toyonaga T., et al. (2004). Hydroxyapatite particles as a controlled release carrier of protein. Biomaterials 25 3807–3812. 10.1016/j.biomaterials.2003.10.081 [DOI] [PubMed] [Google Scholar]
- McCaig C. D., Rajnicek A. M., Song B., Zhao M. (2005). Controlling cell behavior electrically: current views and future potential. Physiol. Rev. 85 943–978. 10.1152/physrev.00020.2004 [DOI] [PubMed] [Google Scholar]
- McKay W. F., Peckham S. M., Badura J. M. (2007). A comprehensive clinical review of recombinant human bone morphogenetic protein-2 (INFUSE® Bone Graft). Int. Orthop. 31 729–734. 10.1007/s00264-007-0418-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta M., Schmidt-Bleek K., Duda G. N., Mooney D. J. (2012). Biomaterial delivery of morphogens to mimic the natural healing cascade in bone. Adv. Drug Deliv. Rev. 64 1257–1276. 10.1016/j.addr.2012.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miao X., Lim W.-K., Huang X., Chen Y. (2005). Preparation and characterization of interpenetrating phased TCP/HA/PLGA composites. Materials Lett. 59 4000–4005. 10.1016/j.matlet.2005.07.062 [DOI] [Google Scholar]
- Michalski M. N., McCauley L. K. (2017). Macrophages and skeletal health. Pharmacol. Ther. 174 43–54. 10.1016/j.pharmthera.2017.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minardi S., Corradetti B., Taraballi F., Byun J. H., Cabrera F., Liu X., et al. (2016a). IL-4 release from a biomimetic scaffold for the temporally controlled modulation of macrophage response. Ann. Biomed. Eng. 44 2008–2019. 10.1007/s10439-016-1580-z [DOI] [PubMed] [Google Scholar]
- Minardi S., Corradetti B., Taraballi F., Sandri M., Van Eps J., Cabrera F. J., et al. (2015a). Evaluation of the osteoinductive potential of a bio-inspired scaffold mimicking the osteogenic niche for bone augmentation. Biomaterials 62 128–137. 10.1016/j.biomaterials.2015.05.011 [DOI] [PubMed] [Google Scholar]
- Minardi S., Fernandez-Moure J. S., Fan D., Murphy M. B., Yazdi I. K., Liu X., et al. (2020). Biocompatible PLGA-mesoporous silicon microspheres for the controlled release of BMP-2 for bone augmentation. Pharmaceutics 12:118. 10.3390/pharmaceutics12020118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minardi S., Pandolfi L., Taraballi F., De Rosa E., Yazdi I. K., Liu X., et al. (2015b). PLGA-mesoporous silicon microspheres for the in vivo controlled temporospatial delivery of proteins. ACS Appl. Mater. Interf. 7 16364–16373. 10.1021/acsami.5b03464 [DOI] [PubMed] [Google Scholar]
- Minardi S., Sandri M., Martinez J. O., Yazdi I. K., Liu X., Ferrari M., et al. (2014). Multiscale patterning of a biomimetic scaffold integrated with composite microspheres. Small 10 3943–3953. 10.1002/smll.201401211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minardi S., Taraballi F., Cabrera F., Van Eps J., Wang X., Gazze S., et al. (2019). Biomimetic hydroxyapatite/collagen composite drives bone niche recapitulation in a rabbit orthotopic model. Materials Today Bio 2:100005. 10.1016/j.mtbio.2019.100005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minardi S., Taraballi F., Pandolfi L., Tasciotti E. (2016b). Patterning biomaterials for the spatiotemporal delivery of bioactive molecules. Front. Bioeng. Biotechnol. 4:45. 10.3389/fbioe.2016.00045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammadi M., Alibolandi M., Abnous K., Salmasi Z., Jaafari M. R., Ramezani M. (2018). Fabrication of hybrid scaffold based on hydroxyapatite-biodegradable nanofibers incorporated with liposomal formulation of BMP-2 peptide for bone tissue engineering. Nanomed. Nanotechnol. Biol. Med. 14 1987–1997. 10.1016/j.nano.2018.06.001 [DOI] [PubMed] [Google Scholar]
- Monmaturapoj N., Yatongchai C. (2011). Influence of preparation method on hydroxyapatite porous scaffolds. Bull. Mater. Sci. 34 1733–1737. 10.1007/s12034-011-0384-x [DOI] [Google Scholar]
- Mouriño V., Vidotto R., Cattalini J., Boccaccini A. (2019). Enhancing biological activity of bioactive glass scaffolds by inorganic ion delivery for bone tissue engineering. Curr. Opin. Biomed. Eng. 10 23–34. 10.1016/j.cobme.2019.02.002 [DOI] [Google Scholar]
- Murphy C. M., Haugh M. G., O’Brien F. J. (2010). The effect of mean pore size on cell attachment, proliferation and migration in collagen–glycosaminoglycan scaffolds for bone tissue engineering. Biomaterials 31 461–466. 10.1016/j.biomaterials.2009.09.063 [DOI] [PubMed] [Google Scholar]
- Murphy S. V., Atala A. (2014). 3D bioprinting of tissues and organs. Nat. Biotechnol. 32 773–785. 10.1038/nbt.2958 [DOI] [PubMed] [Google Scholar]
- Murugan R., Ramakrishna S. (2005). Development of nanocomposites for bone grafting. Composites Sci. Technol. 65 2385–2406. 10.1016/j.compscitech.2005.07.022 [DOI] [Google Scholar]
- Nadeem D., Smith C.-A., Dalby M. J., Dominic Meek R. M., Lin S., Li G., et al. (2015). Three-dimensional CaP/gelatin lattice scaffolds with integrated osteoinductive surface topographies for bone tissue engineering. Biofabrication 7:015005 10.1088/1758-5090/7/1/015005 [DOI] [PubMed] [Google Scholar]
- Nair A. K., Gautieri A., Buehler M. J. (2014). Role of intrafibrillar collagen mineralization in defining the compressive properties of nascent bone. Biomacromolecules 15 2494–2500. 10.1021/bm5003416 [DOI] [PubMed] [Google Scholar]
- Nandakumar A., Cruz C., Mentink A., Birgani Z. T., Moroni L., van Blitterswijk C., et al. (2013). Monolithic and assembled polymer–ceramic composites for bone regeneration. Acta Biomater. 9 5708–5717. 10.1016/j.actbio.2012.10.044 [DOI] [PubMed] [Google Scholar]
- Nawaz Q., Rehman M. A. U., Burkovski A., Schmidt J., Beltrán A. M., Shahid A., et al. (2018). Synthesis and characterization of manganese containing mesoporous bioactive glass nanoparticles for biomedical applications. J. Mater. Sci. Mater. Med. 29:64. 10.1007/s10856-018-6070-4 [DOI] [PubMed] [Google Scholar]
- Nayak T. R., Andersen H., Makam V. S., Khaw C., Bae S., Xu X., et al. (2011). Graphene for controlled and accelerated osteogenic differentiation of human mesenchymal stem cells. ACS Nano 5 4670–4678. 10.1021/nn200500h [DOI] [PubMed] [Google Scholar]
- Neves N., Linhares D., Costa G., Ribeiro C., Barbosa M. (2017). In vivo and clinical application of strontium-enriched biomaterials for bone regeneration: a systematic review. Bone Joint Res. 6 366–375. 10.1302/2046-3758.66.BJR-2016-0311.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen K. T., West J. L. (2002). Photopolymerizable hydrogels for tissue engineering applications. Biomaterials 23 4307–4314. 10.1016/S0142-9612(02)00175-8 [DOI] [PubMed] [Google Scholar]
- Nie T., Baldwin A., Yamaguchi N., Kiick K. L. (2007). Production of heparin-functionalized hydrogels for the development of responsive and controlled growth factor delivery systems. J. Controlled Release 122 287–296. 10.1016/j.jconrel.2007.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niskanen J., Zhang I., Xue Y., Golberg D., Maysinger D., Winnik F. M. (2016). Boron nitride nanotubes as vehicles for intracellular delivery of fluorescent drugs and probes. Nanomedicine 11 447–463. 10.2217/nnm.15.214 [DOI] [PubMed] [Google Scholar]
- Niu X., Feng Q., Wang M., Guo X., Zheng Q. (2009). Porous nano-HA/collagen/PLLA scaffold containing chitosan microspheres for controlled delivery of synthetic peptide derived from BMP-2. J. Controlled Release 134 111–117. 10.1016/j.jconrel.2008.11.020 [DOI] [PubMed] [Google Scholar]
- Noris-Suarez K., Lira-Olivares J., Ferreira A. M., Feijoo J. L., Suarez N., Hernandez M. C., et al. (2007). In vitro deposition of hydroxyapatite on cortical bone collagen stimulated by deformation-induced piezoelectricity. Biomacromolecules 8 941–948. 10.1021/bm060828z [DOI] [PubMed] [Google Scholar]
- Nunes-Pereira J., Ribeiro S., Ribeiro C., Gombek C. J., Gama F. M., Gomes A. C., et al. (2015). Poly(vinylidene fluoride) and copolymers as porous membranes for tissue engineering applications. Polymer Testing 44 234–241. 10.1016/j.polymertesting.2015.05.001 [DOI] [Google Scholar]
- Nurunnabi M., Parvez K., Nafiujjaman M., Revuri V., Khan H. A., Feng X., et al. (2015). Bioapplication of graphene oxide derivatives: drug/gene delivery, imaging, polymeric modification, toxicology, therapeutics and challenges. RSC Adv. 5 42141–42161. 10.1039/C5RA04756K [DOI] [Google Scholar]
- O’Brien F. J., Harley B. A., Yannas I. V., Gibson L. (2004). Influence of freezing rate on pore structure in freeze-dried collagen-GAG scaffolds. Biomaterials 25 1077–1086. 10.1016/S0142-9612(03)00630-6 [DOI] [PubMed] [Google Scholar]
- Oh S.-H., Finones R. R., Daraio C., Chen L.-H., Jin S. (2005). Growth of nano-scale hydroxyapatite using chemically treated titanium oxide nanotubes. Biomaterials 26 4938–4943. 10.1016/j.biomaterials.2005.01.048 [DOI] [PubMed] [Google Scholar]
- Oliveira P., Montembault A., Sudre G., Alcouffe P., Marcon L., Gehan H., et al. (2019). Self-crosslinked fibrous collagen/chitosan blends: processing, properties evaluation and monitoring of degradation by bi-fluorescence imaging. Int. J. Biol. Macromol. 131 353–367. 10.1016/j.ijbiomac.2019.02.134 [DOI] [PubMed] [Google Scholar]
- Opoku C., Dahiya A. S., Oshman C., Cayrel F., Poulin-Vittrant G., Alquier D., et al. (2015). Fabrication of ZnO nanowire based piezoelectric generators and related structures. Phys. Proc. 70 858–862. 10.1016/j.phpro.2015.08.176 [DOI] [Google Scholar]
- Otero T. F., Martinez J. G., Arias-Pardilla J. (2012). Biomimetic electrochemistry from conducting polymers. A review. Electrochim. Acta 84 112–128. 10.1016/j.electacta.2012.03.097 [DOI] [Google Scholar]
- Ozturan K. E., Demir B., Yucel I., Cakıcı H., Yilmaz F., Haberal A. (2011). Effect of strontium ranelate on fracture healing in the osteoporotic rats. J. Orthop. Res. 29 138–142. 10.1002/jor.21204 [DOI] [PubMed] [Google Scholar]
- Palazzo B., Izzo D., Scalera F., Cancelli A., Gervaso F. (2015). Bio-hybrid scaffolds for bone tissue engineering: nano-hydroxyapatite/chitosan composites. Key Eng. Mater. 631 300–305. 10.4028/www.scientific.net/KEM.631.300 [DOI] [Google Scholar]
- Panda P. K., Sahoo B. (2015). PZT to lead free piezo ceramics: a review. Ferroelectrics 474 128–143. 10.1080/00150193.2015.997146 [DOI] [Google Scholar]
- Pang L., Dai C., Bi L., Guo Z., Fan J. (2017). Biosafety and antibacterial ability of graphene and graphene oxide in vitro and in vivo. Nanoscale Res. Lett. 12:564. 10.1186/s11671-017-2317-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panseri S., Cunha C., D’Alessandro T., Sandri M., Giavaresi G., Marcacci M., et al. (2012). Intrinsically superparamagnetic Fe-hydroxyapatite nanoparticles positively influence osteoblast-like cell behaviour. J. Nanobiotechnol. 10:32. 10.1186/1477-3155-10-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pas̨cu E. I., Stokes J., McGuinness G. B. (2013). Electrospun composites of PHBV, silk fibroin and nano-hydroxyapatite for bone tissue engineering. Mater. Sci. Eng. 33 4905–4916. 10.1016/j.msec.2013.08.012 [DOI] [PubMed] [Google Scholar]
- Perez R. A., Seo S.-J., Won J.-E., Lee E.-J., Jang J.-H., Knowles J. C., et al. (2015). Therapeutically relevant aspects in bone repair and regeneration. Mater. Today 18 573–589. 10.1016/j.mattod.2015.06.011 [DOI] [Google Scholar]
- Perez R. A., Won J.-E., Knowles J. C., Kim H.-W. (2013). Naturally and synthetic smart composite biomaterials for tissue regeneration. Adv. Drug Deliv. Rev. 65 471–496. 10.1016/j.addr.2012.03.009 [DOI] [PubMed] [Google Scholar]
- Perizzolo D., Lacefield W. R., Brunette D. M. (2001). Interaction between topography and coating in the formation of bone nodules in culture for hydroxyapatite- and titanium-coated micromachined surfaces. J. Biomed. Mater. Res. 56 494–503. [DOI] [PubMed] [Google Scholar]
- Pisanic T. R., II, Blackwell J. D., Shubayev V. I., Finones R. R., Jin S. (2007). Nanotoxicity of iron oxide nanoparticle internalization in growing neurons. Biomaterials 28 2572–2581. 10.1016/j.biomaterials.2007.01.043 [DOI] [PubMed] [Google Scholar]
- Portan D. V., Kroustalli A. A., Deligianni D. D., Papanicolaou G. C. (2012). On the biocompatibility between TiO2 nanotubes layer and human osteoblasts. J. Biomed. Mater. Res. Part A 100 2546–2553. 10.1002/jbm.a.34188 [DOI] [PubMed] [Google Scholar]
- Prokop A., Jubel A., Hahn U., Dietershagen M., Bleidistel M., Peters C., et al. (2005). A comparative radiological assessment of polylactide pins over 3 years in vivo. Biomaterials 26 4129–4138. 10.1016/j.biomaterials.2004.10.031 [DOI] [PubMed] [Google Scholar]
- Puertolas J. A., Kurtz S. M. (2014). Evaluation of carbon nanotubes and graphene as reinforcements for UHMWPE-based composites in arthroplastic applications: a review. J. Mech. Behav. Biomed. Mater. 39 129–145. 10.1016/j.jmbbm.2014.06.013 [DOI] [PubMed] [Google Scholar]
- Puppi D., Chiellini F., Piras A., Chiellini E. (2010). Polymeric materials for bone and cartilage repair. Prog. Polym. Sci. 35 403–440. 10.1016/j.progpolymsci.2010.01.006 [DOI] [Google Scholar]
- Puricelli E., Ulbrich L. M., Ponzoni D., Filho J. J. (2006). Histological analysis of the effects of a static magnetic field on bone healing process in rat femurs. Head Face Med. 2:43. 10.1186/1746-160X-2-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman C. V., Ben−David D., Dhillon A., Kuhn G., Gould T. W., Müller R., et al. (2014). Controlled release of BMP−2 from a sintered polymer scaffold enhances bone repair in a mouse calvarial defect model. J. Tissue Eng. Regen. Med. 8 59–66. 10.1002/term.1497 [DOI] [PubMed] [Google Scholar]
- Raja K., Misra M., Paramguru K. (2005). Deposition of calcium phosphate coating on nanotubular anodized titanium. Mater. Lett. 59 2137–2141. 10.1016/j.matlet.2005.01.084 [DOI] [Google Scholar]
- Ratnayake J. T., Mucalo M., Dias G. J. (2017). Substituted hydroxyapatites for bone regeneration: a review of current trends. J. Biomed. Mater. Res. Part B Appl. Biomater. 105 1285–1299. 10.1002/jbm.b.33651 [DOI] [PubMed] [Google Scholar]
- Rawat P., Manglani K., Gupta S., Kalam A., Vohora D., Ahmad F. J., et al. (2015). Design and development of bioceramic based functionalized PLGA nanoparticles of risedronate for bone targeting: in-vitro characterization and pharmacodynamic evaluation. Pharma. Res. 32 3149–3158. 10.1007/s11095-015-1692-4 [DOI] [PubMed] [Google Scholar]
- Reddy L. H., Arias J. L., Nicolas J., Couvreur P. (2012). Magnetic nanoparticles: design and characterization, toxicity and biocompatibility, pharmaceutical and biomedical applications. Chem. Rev. 112 5818–5878. 10.1021/cr300068p [DOI] [PubMed] [Google Scholar]
- Reid B., Zhao M. (2014). The electrical response to injury: molecular mechanisms and wound healing. Adv. Wound Care 3 184–201. 10.1089/wound.2013.0442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren F., Xin R., Ge X., Leng Y. (2009). Characterization and structural analysis of zinc-substituted hydroxyapatites. Acta Biomater. 5 3141–3149. 10.1016/j.actbio.2009.04.014 [DOI] [PubMed] [Google Scholar]
- Reves B. T., Jennings J. A., Bumgardner J. D., Haggard W. O. (2011). Osteoinductivity assessment of BMP-2 loaded composite chitosan-nano-hydroxyapatite scaffolds in a rat muscle pouch. Materials 4 1360–1374. 10.3390/ma4081360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rezwan K., Chen Q. Z., Blaker J. J., Boccaccini A. R. (2006). Biodegradable and bioactive porous polymer/inorganic composite scaffolds for bone tissue engineering. Biomaterials 27 3413–3431. 10.1016/j.biomaterials.2006.01.039 [DOI] [PubMed] [Google Scholar]
- Ribeiro C., Correia D. M., Rodrigues I., Guardão L., Guimarães S., Soares R., et al. (2017). In vivo demonstration of the suitability of piezoelectric stimuli for bone reparation. Mater. Lett. 209 118–121. 10.1016/j.matlet.2017.07.099 [DOI] [Google Scholar]
- Ribeiro C., Correia V., Martins P., Gama F. M., Lanceros-Mendez S. (2016). Proving the suitability of magnetoelectric stimuli for tissue engineering applications. Colloids Surf. 140 430–436. 10.1016/j.colsurfb.2015.12.055 [DOI] [PubMed] [Google Scholar]
- Ribeiro C., Parssinen J., Sencadas V., Correia V., Miettinen S., Hytonen V. P., et al. (2015a). Dynamic piezoelectric stimulation enhances osteogenic differentiation of human adipose stem cells. J. Biomed. Mater. Res. A 103 2172–2175. 10.1002/jbm.a.35368 [DOI] [PubMed] [Google Scholar]
- Ribeiro C., Sencadas V., Correia D. M., Lanceros-Mendez S. (2015b). Piezoelectric polymers as biomaterials for tissue engineering applications. Colloids Surf. B Biointerf. 136 46–55. 10.1016/j.colsurfb.2015.08.043 [DOI] [PubMed] [Google Scholar]
- Ridi F., Meazzini I., Castroflorio B., Bonini M., Berti D., Baglioni P. (2017). Functional calcium phosphate composites in nanomedicine. Adv. Colloid Interf. Sci. 244 281–295. 10.1016/j.cis.2016.03.006 [DOI] [PubMed] [Google Scholar]
- Roberts T. T., Rosenbaum A. J. (2012). Bone grafts, bone substitutes and orthobiologics: the bridge between basic science and clinical advancements in fracture healing. Organogenesis 8 114–124. 10.4161/org.23306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocca A., Marino A., Rocca V., Moscato S., de Vito G., Piazza V., et al. (2015). Barium titanate nanoparticles and hypergravity stimulation improve differentiation of mesenchymal stem cells into osteoblasts. Int. J. Nanomed. 10 433–445. 10.2147/IJN.S76329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodell C. B., Rai R., Faubel S., Burdick J. A., Soranno D. E. (2015). Local immunotherapy via delivery of interleukin-10 and transforming growth factor β antagonist for treatment of chronic kidney disease. J. Controlled Release 206 131–139. 10.1016/j.jconrel.2015.03.025 [DOI] [PubMed] [Google Scholar]
- Roffi A., Krishnakumar G. S., Gostynska N., Kon E., Candrian C., Filardo G. (2017). The role of three-dimensional scaffolds in treating long bone defects: evidence from preclinical and clinical literature-a systematic review. BioMed Res. Int. 2017:8074178. 10.1155/2017/8074178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadat-Shojai M., Khorasani M.-T., Dinpanah-Khoshdargi E., Jamshidi A. (2013). Synthesis methods for nanosized hydroxyapatite with diverse structures. Acta Biomater. 9 7591–7621. 10.1016/j.actbio.2013.04.012 [DOI] [PubMed] [Google Scholar]
- Saiz E., Zimmermann E. A., Lee J. S., Wegst U. G. K., Tomsia A. P. (2013). Perspectives on the role of nanotechnology in bone tissue engineering. Dental Mater. 29 103–115. 10.1016/j.dental.2012.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sajesh K. M., Jayakumar R., Nair S. V., Chennazhi K. P. (2013). Biocompatible conducting chitosan/polypyrrole-alginate composite scaffold for bone tissue engineering. Int. J. Biol. Macromol. 62 465–471. 10.1016/j.ijbiomac.2013.09.028 [DOI] [PubMed] [Google Scholar]
- Samavedi S., Whittington A. R., Goldstein A. S. (2013). Calcium phosphate ceramics in bone tissue engineering: a review of properties and their influence on cell behavior. Acta Biomater. 9 8037–8045. 10.1016/j.actbio.2013.06.014 [DOI] [PubMed] [Google Scholar]
- Sapir Y., Cohen S., Friedman G., Polyak B. (2012). The promotion of in vitro vessel-like organization of endothelial cells in magnetically responsive alginate scaffolds. Biomaterials 33 4100–4109. 10.1016/j.biomaterials.2012.02.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scalize P. H., Bombonato-Prado K. F., de Sousa L. G., Rosa A. L., Beloti M. M., Semprini M., et al. (2016). Poly(Vinylidene Fluoride-Trifluorethylene)/barium titanate membrane promotes de novo bone formation and may modulate gene expression in osteoporotic rat model. J. Mater. Sci. 27:180. 10.1007/s10856-016-5799-x [DOI] [PubMed] [Google Scholar]
- Schmidt-Bleek K., Petersen A., Dienelt A., Schwarz C., Duda G. N. (2014). Initiation and early control of tissue regeneration - bone healing as a model system for tissue regeneration. Expert Opin. Biol. Ther. 14 247–259. 10.1517/14712598.2014.857653 [DOI] [PubMed] [Google Scholar]
- Schult M., Buckow E., Seitz H. (2016). Experimental studies on 3D printing of barium titanate ceramics for medical applications. Curr. Directions Biomed. Eng. 2 95–99. 10.1515/cdbme-2016-0024 [DOI] [Google Scholar]
- Serakinci N., Fahrioglu U., Christensen R. (2014). Mesenchymal stem cells, cancer challenges and new directions. Eur. J. Cancer 50 1522–1530. 10.1016/j.ejca.2014.02.011 [DOI] [PubMed] [Google Scholar]
- Sergi R., Bellucci D., Candidato R. T., Lusvarghi L., Bolelli G., Pawlowski L., et al. (2018). Bioactive Zn-doped hydroxyapatite coatings and their antibacterial efficacy against Escherichia coli and Staphylococcus aureus. Surf. Coa. Technol. 352 84–91. 10.1016/j.surfcoat.2018.08.017 [DOI] [Google Scholar]
- Serra G., Morais L., Elias C. N., Semenova I. P., Valiev R., Salimgareeva G., et al. (2013). Nanostructured severe plastic deformation processed titanium for orthodontic mini-implants. Mater. Sci. Eng. C Mater. Biol. Appl. 33 4197–4202. 10.1016/j.msec.2013.06.012 [DOI] [PubMed] [Google Scholar]
- Setyawati M. I., Khoo P. K. S., Eng B. H., Xiong S., Zhao X., Das G. K., et al. (2013). Cytotoxic and genotoxic characterization of titanium dioxide, gadolinium oxide, and poly (lactic−co−glycolic acid) nanoparticles in human fibroblasts. J. Biomed. Mater. Res. Part A 101 633–640. 10.1002/jbm.a.34363 [DOI] [PubMed] [Google Scholar]
- Shadjou N., Hasanzadeh M. (2015). Bone tissue engineering using silica-based mesoporous nanobiomaterials: recent progress. Mater. Sci. Eng. C 55 401–409. 10.1016/j.msec.2015.05.027 [DOI] [PubMed] [Google Scholar]
- Shakir M., Jolly R., Khan A. A., Ahmed S. S., Alam S., Rauf M. A., et al. (2018). Resol based chitosan/nano-hydroxyapatite nanoensemble for effective bone tissue engineering. Carbohydr. Polym. 179 317–327. 10.1016/j.carbpol.2017.09.103 [DOI] [PubMed] [Google Scholar]
- Shalumon K. T., Anulekha K. H., Nair S. V., Nair S. V., Chennazhi K. P., Jayakumar R. (2011). Sodium alginate/poly(vinyl alcohol)/nano ZnO composite nanofibers for antibacterial wound dressings. Int. J. Biol. Macromol. 49 247–254. 10.1016/j.ijbiomac.2011.04.005 [DOI] [PubMed] [Google Scholar]
- Shen X., Zhang Y., Gu Y., Xu Y., Liu Y., Li B., et al. (2016). Sequential and sustained release of SDF-1 and BMP-2 from silk fibroin-nanohydroxyapatite scaffold for the enhancement of bone regeneration. Biomaterials 106 205–216. 10.1016/j.biomaterials.2016.08.023 [DOI] [PubMed] [Google Scholar]
- Shen Y., Huang Z., Liu X., Qian J., Xu J., Yang X., et al. (2015). Iron-induced myocardial injury: an alarming side effect of superparamagnetic iron oxide nanoparticles. J. Cell Mol. Med. 19 2032–2035. 10.1111/jcmm.12582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepherd J. H., Best S. M. (2011). Calcium phosphate scaffolds for bone repair. JOM 63 83–92. 10.1007/s11837-011-0063-9 [DOI] [Google Scholar]
- Silva E., Vasconcellos L. M. R., Rodrigues B. V. M., Dos Santos D. M., Campana-Filho S. P., Marciano F. R., et al. (2017). PDLLA honeycomb-like scaffolds with a high loading of superhydrophilic graphene/multi-walled carbon nanotubes promote osteoblast in vitro functions and guided in vivo bone regeneration. Mater. Sci. Eng. C Mater. Biol. Appl. 73 31–39. 10.1016/j.msec.2016.11.075 [DOI] [PubMed] [Google Scholar]
- Singh K., Ahmadinia K., Park D. K., Nandyala S. V., Marquez-Lara A., Patel A. A., et al. (2014). Complications of spinal fusion with utilization of bone morphogenetic protein: a systematic review of the literature. Spine (Phila Pa 1976) 39 91–101. 10.1097/BRS.0000000000000004 [DOI] [PubMed] [Google Scholar]
- Singh R. K., Jin G.-Z., Mahapatra C., Patel K. D., Chrzanowski W., Kim H.-W. (2015). Mesoporous silica-layered biopolymer hybrid nanofibrous scaffold: a novel nanobiomatrix platform for therapeutics delivery and bone regeneration. ACS Appl. Mater. Interf. 7 8088–8098. 10.1021/acsami.5b00692 [DOI] [PubMed] [Google Scholar]
- Singh R. K., Patel K. D., Lee J. H., Lee E.-J., Kim J.-H., Kim T.-H., et al. (2014). Potential of magnetic nanofiber scaffolds with mechanical and biological properties applicable for bone regeneration. PLoS One 9:e91584. 10.1371/journal.pone.0091584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S., Wu B. M., Dunn J. C. (2011). The enhancement of VEGF-mediated angiogenesis by polycaprolactone scaffolds with surface cross-linked heparin. Biomaterials 32 2059–2069. 10.1016/j.biomaterials.2010.11.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith W. R., Hudson P. W., Ponce B. A., Rajaram Manoharan S. R. (2018). Nanotechnology in orthopedics: a clinically oriented review. BMC Musculoskelet Disord. 19:67. 10.1186/s12891-018-1990-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sopyan I., Mel M., Ramesh S., Khalid K. (2007). Porous hydroxyapatite for artificial bone applications. Sci. Technol. Adv. Mater. 8:116 10.1016/j.stam.2006.11.017 [DOI] [Google Scholar]
- Spiller K. L., Nassiri S., Witherel C. E., Anfang R. R., Ng J., Nakazawa K. R., et al. (2015). Sequential delivery of immunomodulatory cytokines to facilitate the M1-to-M2 transition of macrophages and enhance vascularization of bone scaffolds. Biomaterials 37 194–207. 10.1016/j.biomaterials.2014.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sridhar S., Venugopal J. R., Sridhar R., Ramakrishna S. (2015). Cardiogenic differentiation of mesenchymal stem cells with gold nanoparticle loaded functionalized nanofibers. Colloids Surf. 134 346–354. 10.1016/j.colsurfb.2015.07.019 [DOI] [PubMed] [Google Scholar]
- Stevenson S., Horowitz M. (1992). The response to bone allografts. J. Bone Joint Surg. Am. 74 939–950. 10.2106/00004623-199274060-00017 [DOI] [PubMed] [Google Scholar]
- Sultana N., Wang M. (2012). PHBV/PLLA-based composite scaffolds fabricated using an emulsion freezing/freeze-drying technique for bone tissue engineering: surface modification and in vitro biological evaluation. Biofabrication 4:015003 10.1088/1758-5082/4/1/015003 [DOI] [PubMed] [Google Scholar]
- Sun T., Zhou K., Liu M., Guo X., Qu Y., Cui W., et al. (2018). Loading of BMP−2−related peptide onto three−dimensional nano−hydroxyapatite scaffolds accelerates mineralization in critical−sized cranial bone defects. J. Tissue Eng. Regen. Med. 12 864–877. 10.1002/term.2371 [DOI] [PubMed] [Google Scholar]
- Šupová M. (2015). Substituted hydroxyapatites for biomedical applications: a review. Ceram. Int. 41 9203–9231. 10.1016/j.ceramint.2015.03.316 [DOI] [Google Scholar]
- Szekely J. (2012). Gas-solid Reactions. Amsterdam: Elsevier. [Google Scholar]
- Szpalski M., Gunzburg R. (2002). Applications of calcium phosphate-based cancellous bone void fillers in trauma surgery. Orthopedics 25 S601–S609. [DOI] [PubMed] [Google Scholar]
- Tajbakhsh S., Hajiali F. (2017). A comprehensive study on the fabrication and properties of biocomposites of poly(lactic acid)/ceramics for bone tissue engineering. Mater. Sci. Eng. 70 897–912. 10.1016/j.msec.2016.09.008 [DOI] [PubMed] [Google Scholar]
- Takano Y., Turner C. H., Owan I., Martin R. B., Lau S. T., Forwood M. R., et al. (1999). Elastic anisotropy and collagen orientation of osteonal bone are dependent on the mechanical strain distribution. J. Orthop. Res. 17 59–66. 10.1002/jor.1100170110 [DOI] [PubMed] [Google Scholar]
- Tampieri A., D’Alessandro T., Sandri M., Sprio S., Landi E., Bertinetti L., et al. (2012). Intrinsic magnetism and hyperthermia in bioactive Fe-doped hydroxyapatite. Acta Biomater. 8 843–851. 10.1016/j.actbio.2011.09.032 [DOI] [PubMed] [Google Scholar]
- Tampieri A., Landi E., Valentini F., Sandri M., d’Alessandro T., Dediu V., et al. (2010). A conceptually new type of bio-hybrid scaffold for bone regeneration. Nanotechnology 22:015104 10.1088/0957-4484/22/1/015104 [DOI] [PubMed] [Google Scholar]
- Tampieri A., Ruffini A., Ballardini A., Montesi M., Panseri S., Salamanna F., et al. (2018). Heterogeneous chemistry in the 3-D state: an original approach to generate bioactive, mechanically-competent bone scaffolds. Biomater. Sci. 7 307–321. 10.1039/c8bm01145a [DOI] [PubMed] [Google Scholar]
- Tampieri A., Sandri M., Landi E., Celotti G., Roveri N., Mattioli-Belmonte M., et al. (2005). HA/alginate hybrid composites prepared through bio-inspired nucleation. Acta Biomater. 1 343–351. 10.1016/j.actbio.2005.01.001 [DOI] [PubMed] [Google Scholar]
- Tampieri A., Sandri M., Landi E., Sprio S., Valentini F., Boskey A. (2008). Synthetic biomineralisation yielding HA/collagen hybrid composite. Adv. Appl. Ceramics 107 298–302. 10.1179/174367608X314163 [DOI] [Google Scholar]
- Tampieri A., Sandri M., Panseri S., Adamiano A., Montesi M., Sprio S. (2016). “Biologically inspired nanomaterials and nanobiomagnetism: a synergy among new emerging concepts in regenerative medicine,” in Bio-inspired Regenerative Medicine: Materials, Processes and Clinical Applications, (Singapore: PAN Stanford Publishing; ), 1–20. 10.1201/b19914-2 [DOI] [Google Scholar]
- Tampieri A., Sprio S., Ruffini A., Celotti G., Lesci I. G., Roveri N. (2009). From wood to bone: multi-step process to convert wood hierarchical structures into biomimetic hydroxyapatite scaffolds for bone tissue engineering. J. Mater. Chem. 19 4973–4980. 10.1039/B900333A [DOI] [Google Scholar]
- Tampieri A., Sprio S., Sandri M., Valentini F. (2011). Mimicking natural bio-mineralization processes: a new tool for osteochondral scaffold development. Trends Biotechnol. 29 526–535. 10.1016/j.tibtech.2011.04.011 [DOI] [PubMed] [Google Scholar]
- Tandon B., Blaker J. J., Cartmell S. H. (2018). Piezoelectric materials as stimulatory biomedical materials and scaffolds for bone repair. Acta Biomater. 73 1–20. 10.1016/j.actbio.2018.04.026 [DOI] [PubMed] [Google Scholar]
- Tang F., Li L., Chen D. (2012). Mesoporous silica nanoparticles: synthesis, biocompatibility and drug delivery. Adv. Mater. 24 1504–1534. 10.1002/adma.201104763 [DOI] [PubMed] [Google Scholar]
- Tang W., Lin D., Yu Y., Niu H., Guo H., Yuan Y., et al. (2016). Bioinspired trimodal macro/micro/nano-porous scaffolds loading rhBMP-2 for complete regeneration of critical size bone defect. Acta Biomater. 32 309–323. 10.1016/j.actbio.2015.12.006 [DOI] [PubMed] [Google Scholar]
- Tang Y., Zhao Y., Wang X., Lin T. (2014). Layer−by−layer assembly of silica nanoparticles on 3D fibrous scaffolds: enhancement of osteoblast cell adhesion, proliferation, and differentiation. J. Biomed. Mater. Res. Part A 102 3803–3812. 10.1002/jbm.a.35050 [DOI] [PubMed] [Google Scholar]
- Tannoury C. A., An H. S. (2014). Complications with the use of bone morphogenetic protein 2 (BMP-2) in spine surgery. Spine J. 14 552–559. 10.1016/j.spinee.2013.08.060 [DOI] [PubMed] [Google Scholar]
- Taraballi F., Sushnitha M., Tsao C., Bauza G., Liverani C., Shi A., et al. (2018). Biomimetic tissue engineering: tuning the immune and inflammatory response to implantable biomaterials. Adv. Healthcare Mater. 7:1800490. 10.1002/adhm.201800490 [DOI] [PubMed] [Google Scholar]
- Tarafder S., Dernell W. S., Bandyopadhyay A., Bose S. (2015). SrO−and MgO−doped microwave sintered 3D printed tricalcium phosphate scaffolds: mechanical properties and in vivo osteogenesis in a rabbit model. J. Biomed. Mater. Res. Part B Appl. Biomater. 103 679–690. 10.1002/jbm.b.33239 [DOI] [PubMed] [Google Scholar]
- Taton T. A. (2001). Nanotechnology, boning up on biology. Nature 412 491–492. 10.1038/35087687 [DOI] [PubMed] [Google Scholar]
- Tibbitt M. W., Anseth K. S. (2009). Hydrogels as extracellular matrix mimics for 3D cell culture. Biotechnol. Bioeng. 103 655–663. 10.1002/bit.22361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tichý J. A. (2010). Fundamentals of Piezoelectric Sensorics : Mechanical, Dielectric, and Thermodynamical Properties of Piezoelectric Materials. Springer-Verlag: Berlin: 10.1007/978-3-540-68427-5 [DOI] [Google Scholar]
- Trumbull A., Subramanian G., Yildirim-Ayan E. (2016). Mechanoresponsive musculoskeletal tissue differentiation of adipose-derived stem cells. Biomed. Eng. Online 15:43. 10.1186/s12938-016-0150-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahabzadeh S., Bose S. (2017). Effects of iron on physical and mechanical properties, and osteoblast cell interaction in β-tricalcium phosphate. Ann. Biomed. Eng. 45 819–828. 10.1007/s10439-016-1724-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallet-Regí M., Ragel C. V., Salinas A. J. (2003). Glasses with medical applications. Eur. J. Inorg. Chem. 6, 1029–1042. 10.1002/ejic.200390134 [DOI] [Google Scholar]
- van Vugt T. A., Geurts J. A. P., Arts J. J., Lindfors N. C. (2017). “3 - Biomaterials in treatment of orthopedic infections,” in Management of Periprosthetic Joint Infections (PJIs), eds Arts J. J. C., Geurts J. (Sawston: Woodhead Publishing; ), 41–68. 10.1016/B978-0-08-100205-6.00003-3 [DOI] [Google Scholar]
- Vasconcelos D. M., Gonçalves R. M., Almeida C. R., Pereira I. O., Oliveira M. I., Neves N., et al. (2016). Fibrinogen scaffolds with immunomodulatory properties promote in vivo bone regeneration. Biomaterials 111 163–178. 10.1016/j.biomaterials.2016.10.004 [DOI] [PubMed] [Google Scholar]
- Vavken J., Mameghani A., Vavken P., Schaeren S. (2016). Complications and cancer rates in spine fusion with recombinant human bone morphogenetic protein-2 (rhBMP-2). Eur. Spine J. 25 3979–3989. 10.1007/s00586-015-3870-9 [DOI] [PubMed] [Google Scholar]
- Vichery C., Nedelec J.-M. (2016). Bioactive glass nanoparticles: from synthesis to materials design for biomedical applications. Materials 9:288. 10.3390/ma9040288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vo T. N., Kasper F. K., Mikos A. G. (2012). Strategies for controlled delivery of growth factors and cells for bone regeneration. Adv. Drug Deliv. Rev. 64 1292–1309. 10.1016/j.addr.2012.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh M. C., Kim N., Kadono Y., Rho J., Lee S. Y., Lorenzo J., et al. (2006). Osteoimmunology: interplay between the immune system and bone metabolism. Annu. Rev. Immunol. 24 33–63. 10.1146/annurev.immunol.24.021605.090646 [DOI] [PubMed] [Google Scholar]
- Wang B., Guo Y., Chen X., Zeng C., Hu Q., Yin W., et al. (2018). Nanoparticle-modified chitosan-agarose-gelatin scaffold for sustained release of SDF-1 and BMP-2. Int. J. Nanomed. 13:7395. 10.2147/IJN.S180859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., An Y., Li F., Li D., Jing D., Guo T., et al. (2014). The effects of pulsed electromagnetic field on the functions of osteoblasts on implant surfaces with different topographies. Acta Biomater. 10 975–985. 10.1016/j.actbio.2013.10.008 [DOI] [PubMed] [Google Scholar]
- Wang L., Nancollas G. H. (2008). Calcium orthophosphates: crystallization and dissolution. Chem. Rev. 108 4628–4669. 10.1021/cr0782574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang N., Zhou Z., Xia L., Dai Y., Liu H. (2013). Fabrication and characterization of bioactive beta-Ca2SiO4/PHBV composite scaffolds. Mater. Sci. Eng. C Mater. Biol. Appl. 33 2294–2301. 10.1016/j.msec.2013.01.059 [DOI] [PubMed] [Google Scholar]
- Wang Q., Yan J., Yang J., Li B. (2016). Nanomaterials promise better bone repair. Mater. Today 19 451–463. 10.1016/j.mattod.2015.12.003 [DOI] [Google Scholar]
- Wang Y., Hu X., Dai J., Wang J., Tan Y., Yang X., et al. (2017). A 3D graphene coated bioglass scaffold for bone defect therapy based on the molecular targeting approach. J. Mater. Chem. 5 6794–6800. 10.1039/C7TB01515A [DOI] [PubMed] [Google Scholar]
- Wang Y., Pan H., Chen X. (2019). The preparation of hollow mesoporous bioglass nanoparticles with excellent drug delivery capacity for bone tissue regeneration. Front. Chem. 7:283. 10.3389/fchem.2019.00283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Chen L., Wang Y., Chen X., Zhang P. (2016). Improved cell adhesion and osteogenesis of op-HA/PLGA composite by poly (dopamine)-assisted immobilization of collagen mimetic peptide and osteogenic growth peptide. ACS Appl. Mater. Interf. 8 26559–26569. 10.1021/acsami.6b08733 [DOI] [PubMed] [Google Scholar]
- Webster T. J., Ergun C., Doremus R. H., Siegel R. W., Bizios R. (2000). Enhanced functions of osteoblasts on nanophase ceramics. Biomaterials 21 1803–1810. 10.1016/s0142-9612(00)00075-2 [DOI] [PubMed] [Google Scholar]
- Wei Y., Zhang X., Song Y., Han B., Hu X., Wang X., et al. (2011). Magnetic biodegradable Fe3O4/CS/PVA nanofibrous membranes for bone regeneration. Biomed. Mater. 6:055008 10.1088/1748-6041/6/5/055008 [DOI] [PubMed] [Google Scholar]
- Wen Y., Xun S., Haoye M., Baichuan S., Peng C., Xuejian L., et al. (2017). 3D printed porous ceramic scaffolds for bone tissue engineering: a review. Biomater. Sci. 5 1690–1698. 10.1039/C7BM00315C [DOI] [PubMed] [Google Scholar]
- Weng L., Boda S. K., Teusink M. J., Shuler F. D., Li X., Xie J. (2017). Binary doping of strontium and copper enhancing osteogenesis and angiogenesis of bioactive glass nanofibers while suppressing osteoclast activity. ACS Appl. Mater. Interf. 9 24484–24496. 10.1021/acsami.7b06521 [DOI] [PubMed] [Google Scholar]
- Whulanza Y., Battini E., Vannozzi L., Vomero M., Ahluwalia A., Vozzi G. (2013). Electrical and mechanical characterisation of single wall carbon nanotubes based composites for tissue engineering applications. J. Nanosci. Nanotechnol. 13 188–197. 10.1166/jnn.2013.6708 [DOI] [PubMed] [Google Scholar]
- Wong C., Lu W., Chan W., Cheung K., Luk K., Lu D., et al. (2004). In vivo cancellous bone remodeling on a strontium−containing hydroxyapatite (sr−HA) bioactive cement. J. Biomed. Mater. Res. Part A 68 513–521. 10.1002/jbm.a.20089 [DOI] [PubMed] [Google Scholar]
- Wu X., Liu Y., Li X., Wen P., Zhang Y., Long Y., et al. (2010a). Preparation of aligned porous gelatin scaffolds by unidirectional freeze-drying method. Acta Biomater. 6 1167–1177. 10.1016/j.actbio.2009.08.041 [DOI] [PubMed] [Google Scholar]
- Wu X., Tan Y., Mao H., Zhang M. (2010b). Toxic effects of iron oxide nanoparticles on human umbilical vein endothelial cells. Int. J. Nanomedicine 5 385–399. 10.2147/ijn.s10458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., Jiang W., Wen X., He B., Zeng X., Wang G., et al. (2010). A novel calcium phosphate ceramic-magnetic nanoparticle composite as a potential bone substitute. Biomed. Mater. 5:15001 10.1088/1748-6041/5/1/015001 [DOI] [PubMed] [Google Scholar]
- Wynn T. A., Vannella K. M. (2016). Macrophages in tissue repair, regeneration, and fibrosis. Immunity 44 450–462. 10.1016/j.immuni.2016.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie G., Sun J., Zhong G., Liu C., Wei J. (2010). Hydroxyapatite nanoparticles as a controlled-release carrier of BMP-2: absorption and release kinetics in vitro. J. Mater. Sci. Mater. Med. 21 1875–1880. 10.1007/s10856-010-4038-0 [DOI] [PubMed] [Google Scholar]
- Xie H., Cao T., Gomes J. V., Castro Neto A. H., Rosa V. (2015). Two and three-dimensional graphene substrates to magnify osteogenic differentiation of periodontal ligament stem cells. Carbon 93 266–275. 10.1016/j.carbon.2015.05.071 [DOI] [Google Scholar]
- Xu D., Esko J. D. (2014). Demystifying heparan sulfate–protein interactions. Annu. Rev. Biochem. 83 129–157. 10.1146/annurev-biochem-060713-035314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu T., Yang H., Yang D., Yu Z.-Z. (2017). Polylactic acid nanofiber scaffold decorated with chitosan islandlike topography for bone tissue engineering. ACS Appl. Mater. Interf. 9 21094–21104. 10.1021/acsami.7b01176 [DOI] [PubMed] [Google Scholar]
- Yamaguchi M., Weitzmann M. N. (2011). Zinc stimulates osteoblastogenesis and suppresses osteoclastogenesis by antagonizing NF-κB activation. Mol. Cell. Biochem. 355:179. 10.1007/s11010-011-0852-z [DOI] [PubMed] [Google Scholar]
- Yang F., Wang J., Hou J., Guo H., Liu C. (2013). Bone regeneration using cell-mediated responsive degradable PEG-based scaffolds incorporating with rhBMP-2. Biomaterials 34 1514–1528. 10.1016/j.biomaterials.2012.10.058 [DOI] [PubMed] [Google Scholar]
- Yi H., Rehman F. U., Zhao C., Liu B., He N. (2016). Recent advances in nano scaffolds for bone repair. Bone Res. 4 1–11. 10.1038/boneres.2016.50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan H., Fernandes H., Habibovic P., de Boer J., Barradas A. M., de Ruiter A., et al. (2010). Osteoinductive ceramics as a synthetic alternative to autologous bone grafting. Proc. Natl. Acade. Sci. U.S.A. 107 13614–13619. 10.1073/pnas.1003600107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yun H.-M., Ahn S.-J., Park K.-R., Kim M.-J., Kim J.-J., Jin G.-Z., et al. (2016). Magnetic nanocomposite scaffolds combined with static magnetic field in the stimulation of osteoblastic differentiation and bone formation. Biomaterials 85 88–98. 10.1016/j.biomaterials.2016.01.035 [DOI] [PubMed] [Google Scholar]
- Yun Y.-P., Kim S. E., Kang E. Y., Kim H.-J., Park K., Song H.-R. (2013). The effect of bone morphogenic protein-2 (BMP-2)-immobilizing heparinized-chitosan scaffolds for enhanced osteoblast activity. Tissue Eng. Regen. Med. 10 122–130. 10.1007/s13770-013-0386-4 [DOI] [Google Scholar]
- Zadegan S. A., Abedi A., Jazayeri S. B., Nasiri Bonaki H., Jazayeri S. B., Vaccaro A. R., et al. (2017). Bone morphogenetic proteins in anterior cervical fusion: a systematic review and meta-analysis. World Neurosurg. 104 752–787. 10.1016/j.wneu.2017.02.098 [DOI] [PubMed] [Google Scholar]
- Zarins J., Pilmane M., Sidhoma E., Salma I. (2016). Does local application of strontium increase osteogenesis and biomaterial osteointegration in osteoporotic and other bone tissue conditions: review of literature. Acta Chirurgica Latviensis 16:17 10.1515/chilat-2017-0004 [DOI] [Google Scholar]
- Zhang K., Wang S., Zhou C., Cheng L., Gao X., Xie X., et al. (2018). Advanced smart biomaterials and constructs for hard tissue engineering and regeneration. Bone Res. 6:31. 10.1038/s41413-018-0032-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Q., Qin M., Zhou X., Nie W., Wang W., Li L., et al. (2018). Porous nanofibrous scaffold incorporated with S1P loaded mesoporous silica nanoparticles and BMP-2 encapsulated PLGA microspheres for enhancing angiogenesis and osteogenesis. J. Mater. Chem. B 6 6731–6743. 10.1039/C8TB02138D [DOI] [PubMed] [Google Scholar]
- Zhang R., Liu X., Xiong Z., Huang Q., Yang X., Yan H., et al. (2018). The immunomodulatory effects of Zn-incorporated micro/nanostructured coating in inducing osteogenesis. Artif. Cells Nanomed. Biotechnol. 46(Suppl. 1) 1123–1130. 10.1080/21691401.2018.1446442 [DOI] [PubMed] [Google Scholar]
- Zhang X., Zhang C., Lin Y., Hu P., Shen Y., Wang K., et al. (2016). Nanocomposite membranes enhance bone regeneration through restoring physiological electric microenvironment. ACS Nano 10 7279–7286. 10.1021/acsnano.6b02247 [DOI] [PubMed] [Google Scholar]
- Zhang X. Q., Xu X., Bertrand N., Pridgen E., Swami A., Farokhzad O. C. (2012). Interactions of nanomaterials and biological systems: implications to personalized nanomedicine. Adv. Drug Deliv. Rev. 64 1363–1384. 10.1016/j.addr.2012.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Chen L., Zeng J., Zhou K., Zhang D. (2014). Aligned porous barium titanate/hydroxyapatite composites with high piezoelectric coefficients for bone tissue engineering. Mater. Sci. Eng. 39 143–149. 10.1016/j.msec.2014.02.022 [DOI] [PubMed] [Google Scholar]
- Zhang Y., Venugopal J. R., El-Turki A., Ramakrishna S., Su B., Lim C. T. (2008). Electrospun biomimetic nanocomposite nanofibers of hydroxyapatite/chitosan for bone tissue engineering. Biomaterials 29 4314–4322. 10.1016/j.biomaterials.2008.07.038 [DOI] [PubMed] [Google Scholar]
- Zhao F., Lei B., Li X., Mo Y., Wang R., Chen D., et al. (2018). Promoting in vivo early angiogenesis with sub-micrometer strontium-contained bioactive microspheres through modulating macrophage phenotypes. Biomaterials 178 36–47. 10.1016/j.biomaterials.2018.06.004 [DOI] [PubMed] [Google Scholar]
- Zhao X., Kim J., Cezar C. A., Huebsch N., Lee K., Bouhadir K., et al. (2011). Active scaffolds for on-demand drug and cell delivery. Proc. Natl. Acad. Sci. U.S.A. 108 67–72. 10.1073/pnas.1007862108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng K., Wu J., Li W., Dippold D., Wan Y., Boccaccini A. R. (2018). Incorporation of Cu-containing bioactive glass nanoparticles in gelatin-coated scaffolds enhances bioactivity and osteogenic activity. ACS Biomater. Sci. Eng. 4 1546–1557. 10.1021/acsbiomaterials.8b00051 [DOI] [PubMed] [Google Scholar]
- Zhou T., Li G., Lin S., Tian T., Ma Q., Zhang Q., et al. (2017). Electrospun poly(3-hydroxybutyrate-co-4-hydroxybutyrate)/graphene oxide scaffold: enhanced properties and promoted in vivo bone repair in rats. ACS Appl. Mater. Interfaces 9 42589–42600. 10.1021/acsami.7b14267 [DOI] [PubMed] [Google Scholar]
- Zhou X., Castro N. J., Zhu W., Cui H., Aliabouzar M., Sarkar K., et al. (2016). Improved human bone marrow mesenchymal stem cell osteogenesis in 3D bioprinted tissue scaffolds with low intensity pulsed ultrasound stimulation. Sci. Rep. 6:32876. 10.1038/srep32876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou X., Feng W., Qiu K., Chen L., Wang W., Nie W., et al. (2015). BMP-2 derived peptide and dexamethasone incorporated mesoporous silica nanoparticles for enhanced osteogenic differentiation of bone mesenchymal stem cells. ACS Appl. Mater. Interf. 7 15777–15789. 10.1021/acsami.5b02636 [DOI] [PubMed] [Google Scholar]
- Zhou Z., Li W., He T., Qian L., Tan G., Ning C. (2016). Polarization of an electroactive functional film on titanium for inducing osteogenic differentiation. Sci. Rep. 6:35512. 10.1038/srep35512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu B., Lu Q., Yin J., Hu J., Wang Z. (2005). Alignment of osteoblast-like cells and cell-produced collagen matrix induced by nanogrooves. Tissue Eng. 11 825–834. 10.1089/ten.2005.11.825 [DOI] [PubMed] [Google Scholar]
- Zhu M. T., Wang B., Wang Y., Yuan L., Wang H. J., Wang M., et al. (2011). Endothelial dysfunction and inflammation induced by iron oxide nanoparticle exposure: risk factors for early atherosclerosis. Toxicol. Lett. 203 162–171. 10.1016/j.toxlet.2011.03.021 [DOI] [PubMed] [Google Scholar]
- Zhu W., Guo D., Peng L., Chen Y. F., Cui J., Xiong J., et al. (2017). Repair of rabbit cartilage defect based on the fusion of rabbit bone marrow stromal cells and Nano-HA/PLLA composite material. Artif. Cells Nanomed. Biotechnol. 45 115–119. 10.3109/21691401.2016.1138482 [DOI] [PubMed] [Google Scholar]
- Zofková I., Nemcikova P., Matucha P. (2013). Trace elements and bone health. Clin. Chem. Lab. Med. 51 1555–1561. 10.1515/cclm-2012-0868 [DOI] [PubMed] [Google Scholar]
- Zura R., Xiong Z., Einhorn T., Watson J. T., Ostrum R. F., Prayson M. J., et al. (2016). Epidemiology of fracture nonunion in 18 human bones. JAMA Surg. 151:e162775. 10.1001/jamasurg.2016.2775 [DOI] [PubMed] [Google Scholar]