Abstract
In 1998, Ost published [One-session treatment of specific phobias–a rapid and effective method] [in Swedish] giving rise to the idea that brief, intensive, and concentrated psychosocial interventions could exhibit public health impact. At this juncture, and per criteria of the Society for Clinical Child and Adolescent Psychology, there are data supporting that brief, non-pharmacological intervention [prescriptions] for pediatric anxiety can be considered well-established or probably efficacious. In addition, data from 76 randomized controlled trials (N = 17,203 youth) yield an overall mean effect size of 0.19 on pediatric anxiety outcomes (pre-post). Note, however, that effect sizes vary significantly. These data point to the capacity for clinical change coming from in-vivo exposures for specific phobias (~3 h, one session), CBT with social skills training (~3 h, six sessions for indicated prevention and early intervention), and CBT-based parent training (~6 h, eight digital modules with clinician support). Given such evidence, we recommend efforts be made to establish ways to position such treatment innovations for rapid deployment facilitated by high-quality training, monitoring, technical assistance, and ongoing disclosures.
The past three decades of research show that non-pharmacological interventions are efficacious in the treatment and prevention of pediatric anxiety; however, few interventions are having public health impact (National Academies of Sciences, Engineering and Medicine, 2017). Conceptually, organizational/system-level factors (e.g., culture, implementation climate; readiness for change; Aarons et al., 2018; Aarons & Sawitzky, 2006; Powell et al., 2015) and the structural design features of most evidence-based psychosocial interventions (e.g., number, length, and frequency of sessions; type of provider training and supervision) have been cited as significant barriers to achieving uptake, sustainable implementation, and wide-scale dissemination in the United States. Ringle et al. (2015), Reid et al. (2017), and Salloum et al. (2016) reported, for example, barriers to transporting evidence-based psychosocial interventions into service delivery settings, including protocols designed to be delivered in too many sessions. As a result, when an evidence-based psychosocial intervention reaches the community, provider-driven adaptations occur (e.g., as much as two-thirds of the intervention is adapted for real-world delivery; Rhoades et al., 2012), which probably compromise clinical outcomes (e.g., from deviations in applying core change mechanisms with fidelity; Berkel et al., 2011).
To support evidence-based interventions in reaching the intended public health impact, a second wave of efficacy and effectiveness research has been slowly emerging with foci on “reengineering” evidence-based intervention (EBI) strategies. Herein, reengineering refers to modifying EBIs to maximize fit between interventions, the realities of delivery organizations, and the needs of end-users (e.g., service providers, youth, parents) to achieve more accessible, efficient, and cost-effective care (Brownson et al., 2018; Chiarchiaro et al., 2015). This is sensible (driven by evidence) based on meta-analytic findings suggesting that longer treatments do not necessarily equate to superior clinical outcomes in mental health, including EBIs for pediatric anxiety (Weisz et al., 2017). One approach to EBI reengineering, for example, has been via the modification of protocols on the basis of intervention length, session duration, and/or session frequency to be briefer. For example, in a recent review, Öst and Ollendick (2017) found initial support for what they termed “brief, intensive, and concentrated” (BIC) protocols for the treatment of pediatric phobias. For pediatric anxiety, Öst and Ollendick only found four studies and thus cautioned against making strong conclusions regarding efficacy or effectiveness of these protocols.
On the same spectrum as BIC is the idea that there might be a minimal intervention needed for change (Glasgow et al., 2014). Some view minimal interventions as intended to offer the smallest program dosage and intensity that can be delivered by an implementer with minimal expertise and resource set to achieve positive clinical outcomes. Ideally, these minimal interventions are theorized to work best by including only the strongest EBIs, while considering design features that yield consumer-friendly protocols (e.g., highly compatible with user needs, low application complexity). On the same spectrum, Rotheram-Borus et al.’s (2012) have placed their disruptive-innovations thesis. These are minimal interventions that could meet essential needs for the majority of consumers, while enabling more sustainable dissemination and implementation efforts, as previously articulated by the Knowledge to Action (Centers for Disease Control and Prevention; Wilson et al., 2011), the Diffusion of Innovations (Rogers, 2002, 2010), and more recently the RE-AIM (Harden et al., 2018; Kessler et al., 2013) conceptual frameworks. Here, on the spectrum, principles from entrepreneurial science are also found. That is, the minimal viable product (MVP) (Osterwalder & Pigneur, 2011) emphasizes the importance of developing innovations with the minimal set of features necessary to satisfy early adopters in order to gather feedback to iteratively develop “final” versions of products or services that are market-oriented, user-centered, and person-focused. To the spectrum, we introduce a metric: Non-pharmacological prescription [p]. [p] reflects the inscription and subscription (i.e., treatment name/type, amount in sessions/strength in session length to be dispensed). Ideally, [p] also reflects the signa [Sig], or directions to patient, such that individual-level instruction-compliance ratio for in-session and out-of-session skill application with quality can be considered. Our ideas to the conceptualization of [p] come from theory in Berkel et al. (2011), Gierisch et al. (2010), and Glasgow et al. (2014).
Brief, Non-Pharmacological, Interventions for Pediatric Anxiety
Since the initial work of Öst and colleagues, several randomized controlled trials (RCTs) targeting pediatric anxiety via brief, non-pharmacological, interventions have been published. In addition, about one-third of these brief-interventions deviate from cognitive and behavioral therapy theory, which is a positive step toward intervention innovation in pediatric anxiety. Armed with this knowledge, the time is ripe for shedding new light on progress made toward determining the evidence-based status of reengineered interventions in the pediatric anxiety area.
The focus on pediatric anxiety is important for several reasons. First, anxiety disorders are among the most prevalent psychiatric problems in youth, with rates ranging from 5% to 12% in children and as high as 31% in adolescents (Merikangas et al., 2010). Second, anxiety disorders are associated with significant impairments in functioning across several areas, including academic achievement, social competence, and self-esteem (e.g., Ezpeleta et al., 2001). Third, without intervention, anxiety disorders typically persist into adulthood and for some youth, are prospectively linked to negative sequela, including clinical depression, suicidal ideation, non-suicidal self-injury, conduct problems, and illegal substance use problems (Cummings et al., 2014). Fourth, pediatric anxiety disorders carry a significant societal cost, exceeding 17 USD billion per year, largely due to health-care expenditures, school absenteeism, and lost productivity due to parents or primary care-givers missing work (e.g., therapy appointments, staying home with the child, medical visits) (Bodden et al., 2008; Chisholm et al., 2016). Lastly, despite availability of several empirically supported psychosocial interventions for pediatric anxiety, real-world access is strikingly low (each year, 60% to 80% of youth with anxiety and its related impairments never receive services; Beesdo et al., 2009; Kohn et al., 2004; National Academies of Sciences, Engineering and Medicine, 2017). And, for youth who receive treatment services, recovery rates tend to average 60% with remission falling by 10% over time (Barrett & Turner, 2004; Chavira et al., 2004; Silverman et al., 2008).
The problem of pediatric anxiety is substantial and significant; so much that research efforts also have focused on advancing preventive interventions designed to interrupt the escalation of symptoms and the onset of anxiety disorders at the universal, selective, and indicated levels. Briefly, the Institute of Medicine classifies universal prevention as that which addresses the population at large; selective as that which targets those with an elevated vulnerability; and indicated as that which focuses on those with disorder levels that are subsyndromal or high and projected to develop into diagnoses (O’Connell et al., 2009). In the clinical child and adolescent area, the prevention of pediatric anxiety is as important as its treatment, particularly because prevention efforts appear to be promising in offering an additional avenue to maximize fit between the EBIs, its possible delivery settings (e.g., schools, summer camps), and the needs of end-users (e.g., youth, caregivers, lay implementers) to reduce the burden posed by pediatric anxiety. In fact, several studies show that pediatric anxiety can be prevented via brief, non-pharmacological, interventions; and like most treatments, preventive interventions draw on cognitive and behavioral therapy theory. Also, as it should be anticipated, preventive effects on clinical outcomes take time to emerge and are expected to vary by level (e.g., universal vs. indicated) (Fisak et al., 2011); while positive preventive effects also are relatively stable. For example, at the universal level, small effects are often found, followed by greater effects on clinical outcomes at the selective and then at the indicated prevention level. And, relative to treatment, prevention efforts offer strong promise in reducing anxiety symptom levels or risk for anxiety disorder development (e.g., effect sizes tend to range from 0.26 to 0.32 for indicated prevention and from 0.35 to 0.76 for treatment; Fisak et al., 2011; Reynolds et al., 2012; Stoll & Pina, 2016). Moreover, given that preventive interventions are typically shorter in duration compared to treatments, delivered in non-clinical community settings (e.g., schools, after-school settings), and increasingly implemented by non-mental health professionals (teachers, assistant principals), prevention offers another critical channel by which EBIs could be disseminated and sustained at-scale for adequate public health impact.
The Present Study: Meta-Analysis and Evidence Base Status
As such, this research sought to achieve two principal objectives. First, this study aimed at quantifying (via meta-analysis) the magnitude of effects produced by brief, non-pharmacological interventions on pediatric anxiety outcomes. Within this aim, program effects were examined in the contexts of moderation, such that variations were expected as a function of two categories of moderator variables relevant to intervention protocol (e.g., treatment versus prevention) and participant characteristics (e.g., youth age). Second, this study aimed at evaluating the evidence-based status of brief, non-pharmacological interventions, in an effort to draw conclusions that would inform clinical practice.
In terms of hypotheses, relevant to the first aim, it was expected (and desired) that the interventions of focal interest herein would produce small to medium effect sizes on pediatric anxiety outcomes, which would be consistent with findings from meta-analyses of several brief non-pediatric anxiety interventions – including multiple interventions designed to span just one session (e.g., Schleider & Weisz, 2017; Schleider et al., 2019b). Also expected (and desired) would be that larger effect sizes come from treatment, compared to prevention (indicated, selective, universal; Fisak et al., 2011; Reynolds et al., 2012). Clinically, one should desire large effects from treatment because this is the service often offered to youth that show the highest symptom levels and most severe impairment (empirically, higher risk levels tend to derive the earliest and greatest benefit from prevention; Spoth et al., 2014; Verdurmen et al., 2014). In an exploratory way, other putative moderators (i.e., provider type, modality, theoretical approach, youth age, ethnicity representation, gender) were considered and tested in terms of its relation to effect size. In the past, few studies have shown moderation effects. Reynolds et al. (2012) reported larger effect sizes by delivery modality with individual-based cognitive and behavioral therapy (CBT) for adolescents showing greater effects than group-based CBT, non-CBT, or nonspecific child-focused services (albeit formal sub-group analyses were not conducted to determine statistically significant variations). Fisak et al. (2011) reported larger effects for interventions delivered by mental health professionals compared to delivery by lay providers. We are not aware of any other type of known moderator of response for interventions targeting pediatric anxiety. In terms of the second aim, it was anticipated that certain brief, non-pharmacological interventions could emerge as well-established or probably efficacious. For example, CBT (with and without parent involvement or medication), in vivo exposure, behavior therapy, and family therapy (e.g., CBT for child and parent) are already earmarked as well-established or probably efficacious in the treatment of pediatric anxiety. These levels of empirical support refer to typical protocols (Higa-McMillan et al., 2016); but since many reengineered interventions (in both treatment and prevention) draw on the same efficacious components as typical protocols, some reengineered – as brief – could be brought to the attention of psychology training programs, practitioners, and third-party payers.
METHODS
Study Search Procedure
The principal source to select each study for evaluation was a computer index search using a combination of PsychINFO and Web of Science. Parameter selections were categories (psychology, psychiatry), topics (intervention, treatment, psychotherapy, training, modification), evaluation (clinical, randomized, comparison, effect, outcome), and population (child, youth, adolescent). In conjunction with selected parameter options, searches were carried out using combinations of the following keywords: anxiety, generalized anxiety, separation anxiety, social phobia, social anxiety, specific phobia, therapy, prevention, fears, phobic, worry, and panic. Auto-explode options were used in all computer searches to ensure that all relevant topics within the broader categories were included. The computer index search was supplemented with manual searches of studies cited in published meta-analyses, reviews, references in targeted studies citing other RCTs, and “in press” or “first online” studies recommended by the two search engines.
Study Selection
Studies were included for consideration based on the following criteria: (1) participants were selected and included in the original study on the basis of measures that had some degree of evidence of psychometric reliability (e.g., published Cronbach alpha reliability coefficients) due to: (1a) clinical anxiety as evidenced by diagnoses and/or symptoms, (1b) subsyndromal anxiety symptoms indicative of increased risk for disorder development, (1c) the presence of known risk factors associated with anxiety disorder development (e.g., parent with a diagnosed anxiety disorder), or (1d) universal prevention efforts specifically targeting anxiety disorders; (2) the mean age of child participants was 18 years or younger; (3) participants did not have a co-morbid neurodevelopmental disorder (e.g., autism spectrum disorder) or significant externalizing disorder; (4) random assignment to conditions used; (5) at least one condition evaluated a non-pharmacological intervention with a maximum intervention of 11 direct hours (including required booster sessions); and (6) condition protocols were clearly explained or specified. Studies of interventions involving medication only were excluded, as well as those focusing primarily on academic concerns, peer rejection or unpopularity, or “medical” problems (e.g., distress associated with a medical condition or procedure). Search efforts resulted in 76 studies meeting inclusion/exclusion criteria. Figure 1 shows the study search and inclusion flowchart.
FIGURE 1.
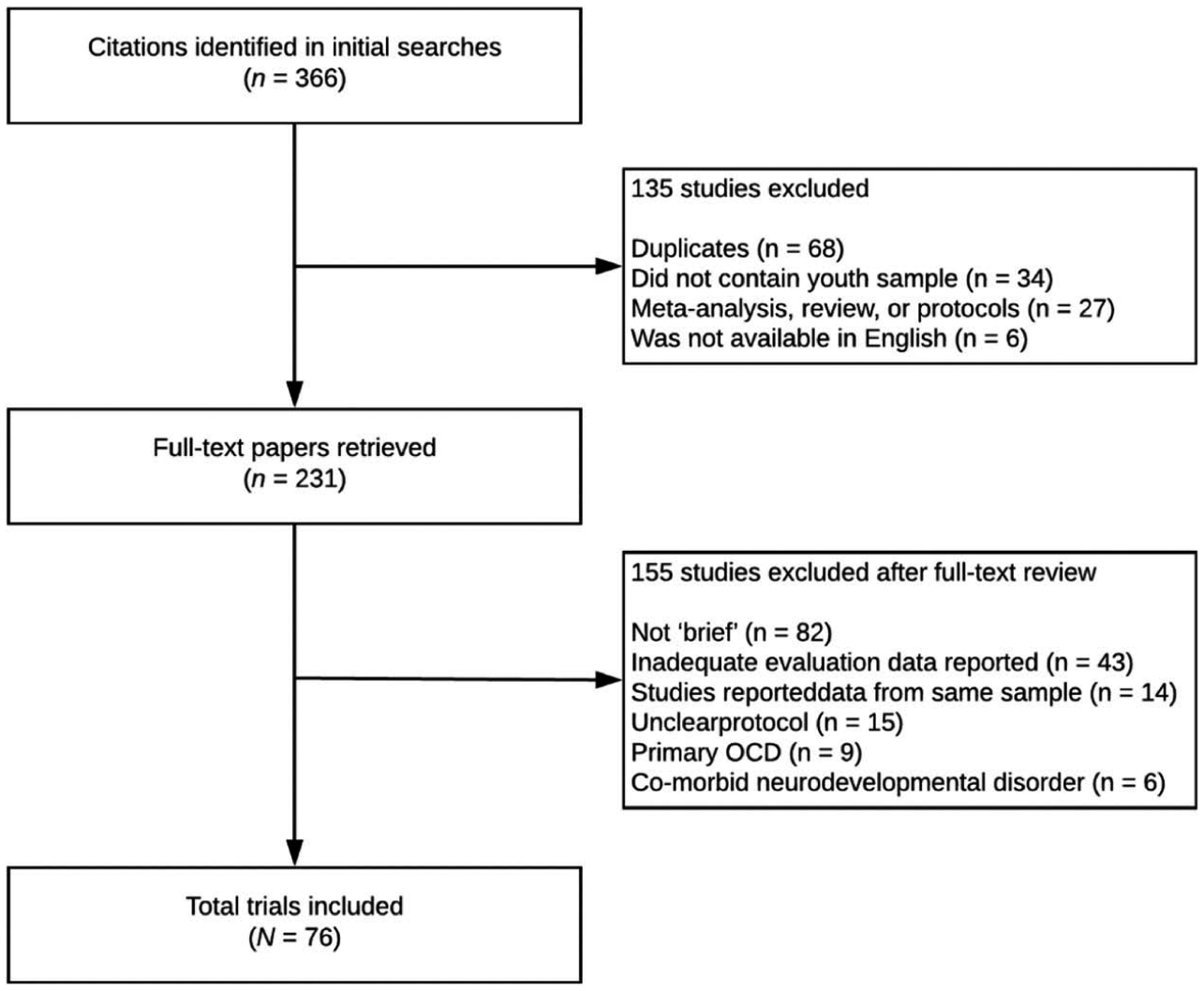
Flowchart for study identification, screening, and inclusion.
Study Coding Procedures
Studies were coded on variables relevant to quantitative characteristics used to calculate effect sizes. Anxiety outcome measures were included for effect size coding if the measure assessed anxiety symptoms, levels, or diagnoses using valid and reliable metrics (e.g., youth self-report, parent/caregiver report, behavioral observations, clinician assessments). For each eligible measure, the mean, standard deviation, and sample size was coded at each available assessment point.
Quantitative characteristics relevant to participant and intervention characteristics also were coded to evaluate effect size variations based on theory and published meta-analyses (Reynolds et al., 2012; Schleider & Weisz, 2017; Weisz et al., 2017). The variables were sex (female), race/ethnicity (minority representation), age (in years), primary/targeted anxiety problem (specific phobia vs. mixed anxiety vs. another specific anxiety disorder), intervention level (treatment, indicated prevention, selective prevention, universal prevention), focal intervention recipient or beneficiary (child, caregiver), primary delivery setting (research laboratory, community), provider (professional, nonprofessional or lay), training of providers (required vs. not required), supervision of providers (required vs. not required), intervention modality (individual, group, digital, attentional bias modification training), and comparator condition type (no-treatment or waitlist, placebo or attention control, another treatment). Two intervention design features relevant to our [p] calculation also were coded: intervention length (the total time in weeks as defined by the intervention [e.g., 10 weeks]) and session duration (average time per single session as defined by the intervention [e.g., 60 min]).
Quantitative data from measures assessing constructs of interest were entered into a Microsoft Excel (Microsoft Corp., Richmond, WA) database with algorithms programmed to calculate effect sizes. To ensure reliability, Lipsey and Wilson’s (2001) recommendations were implemented. First, approximately 3 weeks following the original coding of the studies, 100% of the studies were re-coded in a separate database without access to the original coding file. Double-entered data were checked against the original database by an independent and trained rater. Data corresponding to sample and intervention variables were coded by two independent and trained raters and verified by the first author. Inter-rater reliability between the two coded databases was moderate to high (0.86 >ICCs >0.94) for continuous effect size and moderator data and substantial to almost perfect (0.79 > κappas ≥1.0) for categorical variables.
Effect Size Calculation
To calculate between-group effect size estimates, the independent group pretest-posttest (IGPP) procedure was used. The IGPP procedure allows for comparisons between two independent groups (e.g., intervention vs. control) on their corresponding mean change scores on some dependent measure using different standardized instruments. This increases confidence that observed differences are truly attributable to the intervention condition and not a result of nonspecific epiphenomenal factors (e.g., passage of time, attention; Hedges, 1982; Morris & DeShon, 2002). Between-group effect sizes were calculated for all anxiety outcomes from pre to post-intervention, as well as pre-intervention to follow-up using the following equation:
In the first half of this equation, (MPre;Int − MPost;Int) is the mean difference for the intervention group, (MPre,Cont − MPost,Cont) is the mean difference for the control group, and SDpooled, pre is defined as:
Here, nG1 is the number of subjects in the intervention group, nG2 is the number of subjects in the control group, sG1 is the pre-intervention standard deviation for the intervention group, and sG2 is the pre-intervention standard deviation for the control group. Pre-intervention standard deviations were used as they were measured before any intervention has happened and are thus more likely to be consistent across studies (Becker, 1988).
As noted by the second half of the IGPP equation, effect sizes were adjusted to yield Hedge’s g estimates, which is recommended as to account for the potential upward bias of Cohen’s d effect sizes when based upon a collection of studies that include small sample sizes (e.g., N < 20; Lipsey & Wilson, 2001). Effect sizes also were weighted by the reciprocal of the standard error to account for differences among sample size and variances using the following equation (Lipsey & Wilson, 2001):
For all effect sizes reported herein, positive values reflect effects that are occurring in the expected direction (i.e., the intervention is related to the theorized clinical improvements) whereas a negative effect size value reflects continued clinical deterioration (i.e., the intervention seems unrelated to the theorized clinical improvements). A 95% confidence interval was derived for each effect size aggregate and labeled using the standards suggested by Cohen (1988): small (0.20 or less), medium (about 0.50), and large (0.80 or over); for communication purposes only.
Meta-Analytic Procedure
Individual studies frequently reported multiple measures of anxiety outcomes. The inclusion of multiple measures per singular construct violates assumptions of independence that underlie meta-analysis (Rosenthal & DiMatteo, 2001). When this assumption is violated, sample sizes are inflated and standard error estimates are distorted, producing biased effect size estimates. To maintain assumptions of independence, and per the recommendation of Lipsey and Wilson (2001), multiple effect sizes for a single construct within studies were averaged prior to synthesis with effect sizes from other studies to ensure that each study only contributed a single effect size estimate.
In terms of statistical approach, random effects models were used to calculate overall weighted effect sizes. Unlike a fixed effect approach that assumes between-study differences are due to sampling error alone, random effects models assume that between-study differences are the result of both sampling error and other sources of variability (e.g., putative moderators, study design, random differences). In this way, random effects models enable broader generalizability of meta-analytic findings to populations beyond those under investigation (Cooper et al., 2009; Hedges, 1983; Rosenthal & DiMatteo, 2001). To confirm the a priori decision to use a random effect model approach, and given the considerable methodological differences across studies, heterogeneity of effect sizes was determined using the Q-test.
The Q-test examines whether between-study variation could be completely explained by within-study sampling error or whether the variation among effect size values reflect real and important differences between studies. A significant Q-test value indicates there is significant variability in effect sizes beyond sampling error that should be examined via formal meta-moderation analyses. When the Q-test was significant, the I2 statistic also was calculated:
The I2 statistic provides an estimate of the proportion of observed variance that reflects true differences among effect sizes, with guidelines suggesting that 25%, 50%, and 75% values represent low, moderate, and high levels of heterogeneity, respectively (Higgins et al., 2003).
Validity Assessment
A byproduct of peer-reviewed publication standards and procedures is the “file-drawer problem,” which suggests that published studies are more likely to report statistically significant results than unpublished studies (Rosenthal, 1991). As such, meta-analytic reviews may yield a systematic upward bias due to the omission of null findings such that effect sizes may not accurately represent the “truth”. To address the file-drawer problem and potential publication bias, the fail-safe N (FSN; Rosenthal, 1991) was calculated using the following equation:
In this equation, K is the total number of studies assessing outcome or mediator variables in the meta-analysis and Z is mean effect size produced by the K studies. The FSN represents the number of studies with a mean effect size of zero that would be needed to reduce an effect size to non-significance. Thus, the FSN approximates how resistant calculated effect sizes are to null effects.
Moderators of Between-Group Effect Sizes
To ascertain the potential moderators of between-group effect sizes, a series of analog-to-ANOVA tests were conducted using the International Business Machines’ Statistical Package for the Social Sciences (IBM’s SPSS) with the MetaF macros provided by Wilson (2003). This macro uses a mixed effect model to test for moderation, whereby studies within subgroups are pooled using random effects approaches, while tests of significance between subgroups are conducted using fixed effect approaches (Borenstein et al., 2009). In addition, two approaches were taken to increase confidence in moderator findings. First, analyses were only conducted if the moderator category contained at least three studies per sub-group because meta-analytic moderation estimates have shown to be poor when the number of studies is very small (Weisz et al., 2017). Second, to maximize meta-analytic power in detecting significant moderation effects, separate analyses were conducted for each candidate moderator variable at each focal time point (i.e., pre- to post, pre to follow-up) (Raudenbush & Bryk, 2002; Van den Noortgate et al., 2013). To control for the increased possibility of Type I error due to the number of separate moderator analyses, a Holms-Bonferroni correction was applied. The Holms-Bonferroni adjusts p-values based on the total number of contrasts within a moderator category as to maintain experiment-wise error rates at a target alpha level while yielding more statistical power than a traditional Bonferroni correction. For example, focusing on one moderator category at a time (intervention, participant), analog-to-ANOVA tests were used (or meta-regression for continuous variables) to test for moderation. Then, the contrast with the smallest p-value was evaluated against an alpha of 0.05 divided by the total number of contrasts in the moderator category. If the contrast remained statistically significant, then the contrast with the next smallest p-value was tested using an alpha level of 0.05 divided by the number of remaining contrasts in the moderator category. This process continued until a nonsignificant difference within the category was observed; at which point, all remaining contrasts in the category were considered nonsignificant (for a more detailed discussion of the Holms-Bonferroni correction, see Jaccard & Guilamo-Ramos, 2002).
Non-Pharmacological Prescription [P] Calculation
For this research, [p] was calculated by multiplying intervention length by the product of session duration and session frequency. Session frequency was obtained by dividing a total number of intervention sessions by intervention length. In addition, the average number of days in-between sessions was calculated by multiplying the inverse of intervention session frequency by seven (representing the number of days in a week). For [p], in-between session time is considered an estimate of single dose/day (i.e., the time in which a single intervention dose – one session – has the potential to have effects on targeted outcomes (assuming beneficiary responsiveness is optimal, for example).
Evidence Base Status Evaluation
Evaluation criteria adopted by the Society of Clinical Child and Adolescent Psychology (SCCAP; Southam-Gerow & Prinstein, 2014) from the guidelines originally articulated by Chambless and colleagues (Chambless et al., 1998; Chambless & Hollon, 1998; Chambless et al., 1996) were used to determine the evidence-based status of brief, non-pharmacological, interventions for pediatric anxiety. Criteria are shown in Table 1. Using the M.1 to M.5 criteria listed in the table, two independent and trained evaluators rated the methodological robustness of each study, with coding verified by the first author. Initial agreement between evaluators was 98% with raters differing in their coding of the M.5 criterion for one study. The raters and first author discussed each discrepancy and then a 100% agreement between parties was reached.
TABLE 1.
Criteria for study selection and evidence-based status.
| Design and Methods (M) |
|---|
| M.1. Group design: Study involved a randomized controlled design |
| M.2. Independent variable: Intervention was manualized or logical equivalent |
| M.3. Population: Specified problems based on clearly delineated inclusion/exclusion criteria |
| M.4. Dependent variable: Reliable and valid measures used to ascertain outcomes |
| M.5. Analyses: Appropriate analytic approach with sufficient sample size to detect effects |
| Evidence-Based Status Criteria (Level 1 to 5) |
| Well-Established (Level 1) |
| Effects demonstrated on most primary outcomes by showing: |
| 1.1a. Statistically significant superiority to pill, psychological placebo, or another active intervention |
| OR |
| 1.1b. Equivalent (or not significantly different) to an already well-established intervention, |
| AND |
| 1.1c. In at least two independent research settings and by two independent investigatory teams, |
| AND |
| 1.2. M.1 to M.5 |
| Probably Efficacious (Level 2) |
| Effects demonstrated for the intervention by showing: |
| 2.1. Statistically significant superiority to a waitlist or no intervention control, in at least two good experiments, |
| OR |
| 2.2. Well-Established criteria except for 1.1c |
| AND |
| 2.3. M.1 to M.5 |
| Possibly Efficacious (Level 3) |
| Effects demonstrated for the intervention by showing: |
| 3.1 Statistically significant superiority to a waitlist or no intervention control, in at least one experiment, |
| AND |
| 3.2. M.1 to M.5 |
| OR |
| 3.3 Statistically significant effects, in at least two clinical studies, with two or more studies meeting the M.2 to M.5. |
| Experimental (Level 4) |
| Effects demonstrated for the intervention by showing: |
| 4.1. Statistically significant effects, but not tested in an experiment |
| OR |
| 4.2. Statistically significant effects, in at least one experiment, but no sufficient to meet Level 3 criteria |
| Questionable (Level 5) |
| Effects demonstrated for the intervention by showing: |
| 5.1. Inferiority to another intervention, waitlist, and/or control, |
| OR |
| 5.2. No beneficial effects. |
Relevant to R.1, Kazdin and Bass (1989) found that a sample size of 12 per condition, with treatment vs. no-treatment main effect comparisons, yielded large effects while intervention versus placebo main effect comparisons yielded small to medium effects. Criteria from Silverman and Hinshaw (2008), Division 12 Task Force on Psychological Interventions’ reports (Chambless et al., 1998, 1996), Chambless and Hollon (1998), and Chambless and Ollendick (2001). Editorial revisions were made to the M criteria and Levels 1 to 5 to expand the scope of interventions from treatments to also include preventive interventions; however, classification of interventions remained unaffected by our editorial revisions.
Upon establishing the methodological robustness of each study, “intervention families” were created to facilitate evidence-based status classification. Interventions were aggregated into distinct families when they shared most therapeutic elements with comparable theoretical foundations and prescribed the same intervention dosage (i.e., non-pharmacological prescription). When interventions had principally different theoretical underpinnings or shared comparable theoretical foundations but prescribed different intervention dosage amounts, they were separated into distinct intervention families. This approach was taken as to facilitate the ability to identify minimal intervention dosage thresholds necessary for clinically significant change in anxiety outcomes. Intervention families were then classified based on their empirical support into one of five “levels”, including well-established, probably efficacious, possibly efficacious, experimental, and questionable. Descriptions of each level, including evidentiary requirements, are presented in Table 1.
RESULTS
Characteristics of Included Studies
The final sample of studies consisted of 76 RCTs, including 40 that were prevention focused (13 indicated, 4 selective, and 17 universal) and 36 treatment focused. The total sample size was 17,203 youth between the ages of 3 to 18 years old (M = 10.61, SD = 2.75) with 55% being girls. Twenty-five studies evaluated interventions with samples consisting mostly of Caucasian youth, while only three studies evaluated interventions with majority non-Caucasian samples (Ginsburg & Drake, 2002; Kato & Shimizu, 2017; Pina et al., 2020). The remaining 48 studies did not report sample demographic information to ascertain ethnic minority representation. In terms of intervention characteristics, 114 independent intervention conditions were evaluated, with an overall average of 6 direct intervention hours (range = 1 to 10; SD = 2.64), delivered in about 8 sessions (range = 1 to 12; SD = 2.90), across 7.14 weeks (range = 1 to 16; SD = 3.47), with an average of 6 days between intervention sessions (range = 0 to 14; SD = 2.14). Approximately, 80% (n = 60) of interventions targeted pediatric anxiety broadly, without a focus on a particular disorder; of the remaining interventions, 13% (n = 10) targeted specific phobias and 8% (n = 6) focused on social anxiety. Most interventions were based on cognitive and/or behavioral therapy theory (63%), delivered by highly trained mental health professionals (67%), and largely focused on youth as the primary intervention recipient (91%). In terms of intervention modality, 48.5% (n = 32) of studies reported on protocols delivered in group format, 21.2% (n = 14) individual format, 21.2% (n = 14) used some form of technology in program delivery (e.g., internet, CD-ROMs, computer games). About 14% (n = 9) of studies used attention-bias modification training (ABMt) protocols and 4.5% (n = 3) were bibliotherapy. With regard to comparator conditions, 53% (n = 41) of studies used a waitlist or no treatment control, 22% (n = 17) compared an intervention to an active control condition (e.g., attention control, education support), and 8% (n = 6) used another proven intervention as the comparator.
Included studies are summarized in Table 2. Column 1 names the investigatory team and publication date. Column 2 reports participants’ characteristics (i.e., age, sex, clinical inclusion criteria) and randomization to condition and comparator. Column 3 describes significant program effects and condition comparison results. Finally, column 4 specifies Table 1 criteria relevant to the methodological robustness for each study. A total of 64 studies was considered methodologically robust in that they met M.1 to M.5 criteria. Twelve studies did not meet M.5 criterion because the sample size per condition/comparator was too small to detect reliable effects (i.e., Attwood et al., 2012; Barrett et al., 2001; Dewis et al., 2001; Gallagher et al., 2004; Ginsburg & Drake, 2002; Hains, 1992; Muris et al., 2002, 1998; Sheslow et al., 1983; Stallard et al., 2011; Tillfors et al., 2011; Whiteside et al., 2015).
TABLE 2.
RCTs contributing to the evidence-based status of brief, non-pharmacological interventions for anxiety and phobias in youth.
| Study | Sample characteristics | Significant program effects | Criteria |
|---|---|---|---|
| Anxiety (n = 66) | |||
| Hains (1992) | N = 25. Ages 15 to 16 years. Mean age not reported. 0% girls. Randomized to individual plus group cognitive-behavioral stress management intervention (CBSMI), individual plus group anxiety management training (AMS), or waitlist control. | Intervention conditions did not differ from one another. At posttest and 3-week FU, CBSMI and AMS led to lower STAIC state anxiety, STAIC trait anxiety, STAXI trait anger, STAXI state anger, and RCADS depression than control. | M.1 to M.4 |
| Kiselica et al. (1994) | N = 48. 9th grade students. Mean age not reported. 46% girls. Top 12 highest scores in classroom on STAIC-T anxiety. Randomized to stress inoculation training or usual care. | At posttest and 1-month FU, stress inoculation training led to lower STAIC trait anxiety than usual care. No other between-group differences emerged on SOSI stress or GPA. Stress inoculation training led to lower SOSI stress at posttest and FU. | M.1 to M.5 |
| Barrett et al. (2000) | N = 20. Ages 14 to 19 years (M = 16.30). Former Yugoslavian Refugee in Australia. Randomized to group cognitive behavior therapy (GCBT) or waitlist control. | At posttest, GCBT led to reduced YSR anxiety/depression than control. GCBT led to lower YSR internalizing, SCAS anxiety, and ASP cognitive styles but between-group differences were not evident. | M.1 to M.4 |
| Barrett et al. (2001) | N = 204. Ages 7 to 19 years (M = 12.50). Non-English-speaking Background in Australia. Randomized to GCBT or waitlist control. | At posttest, GCBT led to more improvements in BHS future outlook/hopelessness, SEI school self-esteem, RSES self-esteem, and reductions in RCMAS anxiety than control. | M.1 to M.5 |
| Ginsburg and Drake (2002) | N = 12. Ages 14 to 17 years (M = 15.60). 83% girls. DSM GAD, Specific Phobia, SoP, SAD. Randomized to GCBT or attention control. | At posttest, GCBT led to lower ADIS-C/P CSR severity and SCARED-C anxiety than control. GCBT led to lower SAS-A social anxiety, but between-group differences were not evident. | M.1 to M.4 |
| Heyne et al. (2002) | N = 61. Ages 7 to 14 years (M = 11.50). 46% girls. Met school refusal criteria as defined by Berg et al. (1969) and DSM GAD, Specific Phobia, SAD, SoP. Randomized to ICBT, ICBT plus parent teacher training (ICBT+PTT), or parent/teacher training (PTT) only. | At posttest, ICBT+PTT and PTT led to higher school attendance than ICBT. ICBT +PTT also led to lower CBCL internalizing symptoms than ICBT at posttest. In addition, PTT led to significantly less FSSC-R fear of the unknown, RCMAS worry and oversensitivity, and RCMAS physiological anxiety than ICBT. Additional between-group differences were not evident for any outcome at posttest or 4.5-month FU. All conditions led to lower FSSC-R fears, RCMAS anxiety, CDI depression, and higher SEQSS self-efficacy at posttest. At FU, ICBT+PTT led to lower FSSC-R fear and RCMAS worry/oversensitivity, ICBT led to lower FSSC-R fear, RCMAS physiological complaints and higher SEQSS self-efficacy. At FU, 69% (across all conditions) no longer met ADIS-C/P CSR diagnostic criteria for any anxiety disorder. | M.1 to M.5 |
| Muris et al. (2002) | N = 30. Ages 9 to 12 years (M = 10.00). 43% girls. RCADS ≥ 9 (boys) or 11 (girls) anxiety symptoms and DSM GAD, Specific Phobia, SAD, SoP. Randomized to ICBT, emotional disclosure treatment (ED), or no treatment control. | At posttest, ICBT led to lower RCADS anxiety, RCADS depression, STAIC trait anxiety than control and ED. At posttest, RCADS anxiety recovery rates were 80% in ICBT vs 40% in ED and 30% in control. | M.1 to M.4 |
| Gallagher et al. (2004) | N = 23. Ages 8 to 11 years. Mean age not reported. 52% girls. DSM SoP. Randomized to GCBT or waitlist control. | At posttest, GCBT led to lower CBCL anxiety/depression than control. At 3-week FU, GCBT led to lower SPAI-C social anxiety, RCMAS anxiety, CDI depression, and CBCL anxiety/depression than control. No other between-group differences emerged on SASC-R social anxiety, CBCL social competence, CBCL activities, or CBCL school problems. Both GCBT and control led to lower SASC-R social anxiety at posttest and FU. | M.1 to M.4 |
| Bernstein et al. (2005) | N = 61. Ages 7 to 11 years (M = 9.00). 66% girls. 53% girls. DSM GAD, Specific Phobia, SAD, SoP. Randomized to GCBT, GCBT plus parent training, or no-treatment control. | At posttest, 3-, and 6-month FU, GCBT and GCBT plus parent training led to lower MASC-P anxiety, SCARED-P anxiety, ADIS-C/P CSR severity, and CGI functioning than control. Stronger pre to posttest changes were found for GCBT plus parent training than GCBT for CGI functioning. At 12-month FU, GCBT and GCBT plus parent training led to lower CSR severity ratings than control, with improvements in CGI functioning being maintained at 3-year FU (Lee et al., 2017). | M.1 to M.5 |
| Mifsud and Rapee (2005) | N = 425. Ages 8 to 11 years (M = 9.5). 59% girls. RCMAS ≥ 18 RCMAS anxiety symptoms. Randomized to GCBT or waitlist control. | At posttest and 4-month FU, GCBT led to lower RCMAS anxiety, SCAS anxiety, SCAS-P anxiety, CATS automatic thoughts, and TRF emotional and behavioral problems than control. | M.1 to M.5 |
| Rapee et al. (2005) | N = 146. Ages 3 to 5 years (M = 3.9). 55% girls. STSC-approach subscale >30. Randomized to parent-education intervention or assessment only control. | Between-group differences were not evident for any outcome at posttest. Both parent-education intervention and control led to improvements in STSC-C/P temperament, TABC-R-P temperament, and behavioral inhibition measured via approach tasks. At 12-month FU, parent-education intervention had fewer ADIS-C/P CSR anxiety disorder diagnoses than control. At 11-year FU, girls in the parent-education intervention had lower SCAS-P anxiety, CALIS-C life interference, and fewer ADIS-C/P anxiety disorder diagnoses than control and boys in the intervention condition (Rapee, 2013). | M.1 to M.5 |
| Dadds and Roth (2008) | N = 734. Ages 3 to 7 years. Mean age not reported. 47% girls. Randomized to parent-focused ICBT or no intervention control. | At posttest, parent-focused CBT led to lower teacher reported SCBE child anxious-withdrawn and angry-aggressive behaviors and higher SCBE social competence than control. Between-group differences were not evident at 7-month FU. | M.1 to M.5 |
| Aune and Stiles (2009) | N = 1,439. Ages 12 to 14 years. Mean age not reported. 52% girls. Randomized to GCBT plus psychoeducation for parents, teachers, and community health workers or no intervention control. | At posttest, GCBT led to lower SPAI-C social anxiety and SCARED anxiety than control. | M.1 to M.5 |
| N = 190. Ages 12 to 14 years. Mean age not reported. 52% girls. Post-hoc subsample. SPAI-C ≥ 18 social anxiety symptoms. Randomized to GCBT plus psychoeducation for parents, teachers, and community health workers or no intervention control. | At posttest, GCBT led to lower SPAI-C social anxiety and SCARED anxiety than control. | M.1 to M.5 | |
| Calear et al. (2009) | N = 1,477. Ages 12 to 17 years. Mean age not reported. 56% girls. Randomized to internet-delivered CBT (iCBT) or waitlist control. | At posttest and 6-month FU, iCBT led to lower RCMAS anxiety than control. | M.1 to M.5 |
| Ginsburg (2009) | N = 40. Ages 7 to 12 years (M = 8.94). 45% girls. Parents met DSM criteria for GAD, Specific Phobia, SAD, SoP. Randomized to parent-focused ICBT or waitlist control. | At posttest, 6-month, and 12-month FU, family-focused ICBT led to lower ADIS-CSR severity and SCARED-P anxiety than control. At 12-month FU, family-focused ICBT led to fewer ADIS anxiety disorder diagnoses than control (0% vs. 30%). | M.1 to M.5 |
| Hunt et al. (2009) | N = 260. 9th grade students. Mean age and sex not reported. 43% girls. RCMAS >1SD above mean of a normative sample. Randomized to GCBT or assessment only control. | Between-group differences were not evident for any outcome at posttest, 2-year FU, and 4-year FU. Both GCBT and control led to lower RCMAS anxiety at 4-year FU. | M.1 to M.5 |
| Balle & Tortella-Feliu (2009) | N = 92. Ages 11 to 17 years. Mean age and sex not reported. CASI >80th percentile for anxiety sensitivity. Randomized to GCBT, waitlist, or no intervention control. | Between-group differences were not evident at posttest. Both GCBT and control conditions led to lower CASI anxiety sensitivity and SCAS-P anxiety symptoms. At 6-month FU, GCBT led to lower CASI anxiety sensitivity than controls. | M.1 to M.5 |
| Khanna and Kendall (2010) | N = 49. Ages 7 to 13 years (M = 10.10). 33% girls. DSM GAD, Specific Phobia, SAD, SoP. Randomized to computer-assisted CBT (CCAL), ICBT, or computer-assisted attention control. | Intervention conditions did not differ from one another. At posttest and 3-month FU, CCAL and ICBT led to lower ADIS-C/P CSR severity than control. No other between-group differences emerged on CGAS functioning, MASC-C anxiety, or CDI-C depression. CCAL and ICBT demonstrated reductions in MASC-C anxiety and CDI-C depression at posttest. | M.1 to M.5 |
| Miller et al. (2010) | N = 118. Ages 7 to 12 years (M = 9.75). 50% girls. Randomized to GCBT or waitlist control. | Between-group differences were not evident for any outcome at posttest. Both GCBT and control led to lower MASC anxiety and BASC-IC internalizing symptoms. | M.1 to M.5 |
| N = 33. Ages 7 to 12 years (M = 9.75). 50% girls. Post-hoc subsample. MASC anxiety >56. Randomized to GCBT or waitlist control. | At posttest, GCBT led to lower MASC anxiety than control. | M.1 to M.5 | |
| Pahl and Barrett (2010) | N = 263. Ages 4 to 6 years (M = 4.56). 48% girls. Randomized to GCBT or waitlist control. | At posttest, GCBT led to lower BIQ-T behavioral inhibition and higher BERS-T social-emotional competence than control. No other between-group differences emerged on PAS anxiety, BIQ-P behavioral inhibition, or BERS-P social-emotional competence. GCBT led to lower PAS anxiety, BIQ-P behavioral inhibition, and higher BERS-P social-emotional competence at posttest and 12-month FU. | M.1 to M.5 |
| Bar-Haim et al. (2011) | N = 34. Age 10 years (M = 10.10). 71% girls. SCARED >50th percentile for anxiety symptoms. Randomized to attention bias modification training (ABMt) or attention control training (ACT). | At posttest, ABMt led to higher rates of disengagement from threat and were less vulnerable to the stress induced by the stressor task than ACT. No additional between-group differences were evident, with both ABMt and ACT having led to lower STAIC trait anxiety at posttest. | M.1 to M.5 |
| Miller, Laye-Gindhu, Liu, et al. (2011) | N = 191. Ages 9 to 12 years (M = 10.1). 48% girls. MASC anxiety T-score of ≥ 56. Randomized to GCBT or attention control. | Between-group differences were not evident for any outcome at posttest, 5-month, or 17-month FU. | M.1 to M.5 |
| N = 42. Ages 9 to 12 years (M = 10.1). Post-hoc subsample. MASC anxiety T-score of >65. Randomized to GCBT or attention control. | Between-group differences were not evident for any outcome at posttest, 5-month, or 17-month FU. | M.1 to M.5 | |
| Miller, Laye-Gindhu, Liu, et al. (2011) | N = 253. Ages 9 to 12 years (M = 9.80). 54% girls. Randomized to GCBT or attention control. | Between-group differences were not evident for any outcome at posttest or 17-month FU. | M.1 to M.5 |
| N = 64. Ages 9 to 12 years (M = 9.80). Post-hoc subsample. MASC anxiety T-score of >65. Randomized to GCBT or attention control. | Between-group differences were not evident for any outcome at posttest or 17-month FU. | M.1 to M.5 | |
| Miller, Laye-Gindhu, Bennett, et al. (2011) | N = 553. Ages 9 to 12 years (M = 9.77). 50% girls. Randomized to GCBT or waitlist control. | Between-group differences were not evident. At posttest and 3-month FU, GCBT led to lower MASC anxiety. | M.1 to M.5 |
| Stallard et al. (2011) | N = 20. Ages 11 to 16 years. Mean age and sex not reported. Seeking services at Tier 3 Child and Adolescent Mental Health Services with DSM GAD, Specific Phobia, SAD, SoP or mild-moderate depression. Randomized to computer-assisted CBT or waitlist control. | No between-group analyses were conducted. Both computer-assisted CBT and control led to improved RSEI self-esteem and SQC cognitive schemas. Computer-assisted CBT also led to lower SCAS social phobia SDQ-P emotional difficulties, SDQ-P hyperactivity, AWS depression, and improved SDQ-P total strengths and difficulties. Control also led to lower SCAS physical injury fears. | M.1 to M.4 |
| Tillfors et al. (2011) | N = 19. Ages 15 to 21 years (M = 16.50). 89% girls. DSM SoP. Randomized to iCBT or waitlist control. | At posttest and 1-year FU, iCBT led to lower SPSQ-C social anxiety, LSAS-RS social anxiety, BAI anxiety, and MADRS-S depression than control. | M.1 to M.4 |
| Attwood et al. (2012) | N = 13. Ages 10 to 12 years (M = 10.6). 0% girls. Randomized to computer-assisted CBT or computer gaming control. | At posttest, computer-assisted CBT led to lower SCAS anxiety, SCAS social anxiety, and SCAS generalized anxiety than control. | M.1 to M.4 |
| Eldar et al. (2012) | N = 40. Ages 8 to 14 years (M = 9.84). 45% girls. DSM GAD, Specific Phobia, SAD, SoP. Randomized to ABMt away from threat, placebo attention control training using ABMt stimuli, or placebo attention training using neutral stimuli. | At posttest, ABMt led to greater reductions in dot-probe task attentional bias and ADIS-IV-C/P anxiety symptom counts compared to controls. At posttest, 33% of children in the ABMt condition no longer met ADIS-C/P CSR diagnostic criteria for any anxiety disorder, compared to 13.3% in the placebo condition, and 0% in the neutral placebo condition. No other between-group differences emerged on SCARED-anxiety or CDI-C depression, with all three conditions having led to lower SCARED-C anxiety and CDI-C depression. | M.1 to M.5 |
| Ginsburg et al. (2012) | N = 32. Ages 8 to 12 years (M = 10.28). 63% girls. DSM GAD, Specific Phobia, SAD, SoP. Randomized to modular ICBT or usual care. | Between-group differences were not evident for any outcome at posttest and 1-month FU. Both modular ICBT and usual care led to lower ADIS-C/P CSR anxiety severity, SCARED-C anxiety, and SDQ emotional difficulties, and higher CGAS functioning. | M.1 to M.5 |
| McLoone and Rapee (2012) | N = 152. Ages 7 to 12 years (M = 9.8). 62% girls. 10% of SCAS scores for their age group. Randomized to school-based GCBT, bibliotherapy w/o clinician support, or waitlist control. | At posttest and 12-month FU, school-based GCBT and bibliotherapy w/o clinician support led to lower SCAS-P anxiety and CALIS life interference than control. | M.1 to M.5 |
| Thirlwall et al. (2013) | N = 194. Ages 7 to 12 years. Mean age not reported. 52% girls. DSM GAD, Specific Phobia, SAD, SoP. Randomized to full guidance parent-delivered CBT, brief guidance parent-delivered CBT, or waitlist control. | At posttest, full guidance parent-delivered CBT led to lower CAIS-P interference and SMFQ low mood than brief guidance parent-delivered CBT and control. At posttest, participants in both treatment conditions were 85% more likely to have recovered from their ADIS-C/P CSR principal anxiety disorder than control, with full guided parent-delivered CBT leading to higher diagnostic recovery (50%) than brief guided parent-delivered CBT (39%). ADIS-C/P CSR diagnostic recovery rates at 6-month FU were comparable for both treatment conditions (76% for full guided, 71% for brief guided). Improvements for the intervention conditions were maintained at 3- to 5-year FU (Brown et al., 2017). | M.1 to M.5 |
| Waters et al. (2013) | N = 37. Ages 7 to 13 years (M = 9.60). 65% girls. DSM GAD, Specific Phobia, SAD, SoP. Randomized to ABMt-attention-toward-positive (ABMt-ATP) or ABMt attention training control (ABMt-ATC). | At posttest, ABMt-ATP led to lower ADIS-C/P CSR severity and higher attentional bias toward positive stimuli (via dot-probe task) than control. At posttest, 50% in ABMt-ATP no longer met ADIS-C/P CSR diagnostic criteria for principal anxiety disorder compared to 8% in control. No other between-group differences emerged on SCAS anxiety, SCAS-P anxiety, or CES-DC depression, with both conditions having led to lower SCAS anxiety, SCAS-P anxiety, and CES-DC depression at posttest. | M.1 to M.5 |
| Collins et al. (2014) | N = 317. Ages 9 to 10 years. Mean age not reported. 45% girls. Randomized to psychologist-led GCBT, teacher-led GCBT, or usual care. | Intervention conditions did not differ from one another at posttest. At posttest and 6-month FU, psychologist-led GCBT and teacher-led GCBT led to lower SCAS anxiety, CSI avoidance coping, and higher CSI problem solving coping and CSI social coping than control. At 6-month FU, psychologist-led GCBT led to lower SCAS anxiety than teacher-led GCBT and control, whereas teacher-led GCBT led to lower CSI avoidant coping was lower in teacher-led GCBT than psychologist-led GCBT and control. | M.1 to M.5 |
| Donovan and March (2014) | N = 52. Ages 3 to 6 years (M = 4.08). 54% girls. DSM GAD, Specific Phobia, SAD, SoP. Randomized to parent focused iCBT or waitlist control. | At posttest, 6-month, and 12-month FU, iCBT led to lower PAS anxiety, CBCL internalizing, and higher CGAS functioning than control. At posttest, ADIS-C/P CSR diagnostic recovery rates were 39.1% in iCBT and 25.9% in control; with iCBT ADIS-C/P CSR recovery rates improving to 70.6% in iCBT at 12-month FU. | M.1 to M.5 |
| Stallard et al. (2014) | N = 1,362. Ages 9 to 10 years. Mean age not reported. 51% girls. Randomized to school staff-led GCBT, health facilitator-led GCBT, or personal social and health education (PSHE) control. | At 12-month FU, health facilitator-led and school staff-led GCBT led to lower RCADS-C anxiety than control, with more pronounced changes occurring for those in school staff GCBT. At FU, health facilitator GCBT led to lower RCADS separation anxiety than school staff GCBT and control (Skryabina et al., 2016). | M.1 to M.5 |
| N = 99. Ages 9 to 10 years. Mean age not reported. Post-hoc subsample. ≥ 49 on RCADS anxiety. Randomized to school staff-led GCBT, health facilitator-led GCBT, or personal social and health education (PSHE) control. | Between-group differences were not evident for any outcome at posttest or 3-month FU. Both school staff-led and health facilitator-led GCBT led to lower RCADS-C anxiety. | M.1 to M.5 | |
| Wong et al. (2014) | N = 976. Ages 14 to 16 years. Mean age not reported. 70% girls. Randomized to iCBT for anxiety, iCBT for depression, or usual care. | Intervention conditions were not different from one another. At posttest, iCBT for anxiety led to reductions in GAD-7 generalized anxiety than control. iCBT for depression led to reductions in PHQ-5 depression than usual care. | M.1 to M.5 |
| Rodgers and Dunsmuir (2015) | N = 62. Ages 12 to 13 years. Mean age not reported. 69% girls. Randomized to GCBT or waitlist control. | At posttest and 4-month FU, GCBT led to lower SCAS and SCAS-P anxiety than control. No other between-group differences emerged on CRS school adjustment, with both GCBT and control having led to improvements in CRS school adjustment. | M.1 to M.5 |
| Ginsburg et al. (2015) | N = 136. Ages 6 to 13 years (M = 8.70). Parents met DSM criteria for GAD, Specific Phobia, SAD, SoP. Randomized to family-focused ICBT or information-monitoring control. | At posttest, 6-month, and 12-month FU, family-focused ICBT led to reduced ADIS-CSR severity than control. At 12-month FU, family-focused ICBT led to fewer ADIS anxiety disorder diagnoses than control (5.26% vs. 30.65%). Over time, family-focused ICBT also led to lower SCARED-P anxiety, CBCL anxiety/ depressive symptoms, and CBCL behavior problems than control (Pella et al., 2017). | M.1 to M.5 |
| Waters et al. (2015) | N = 59. Ages 6 to 17 years (M = 8.75). 53% girls. DSM GAD, Specific Phobia, SAD, SoP. Randomized to ABMt or waitlist control. | At posttest and 6-month FU, ABMt led to lower ADIS-C/P CSR severity, SCAS-P anxiety, SMFQ-P strengths and difficulties, CBCL internalizing, and higher CGAS functioning than control. At posttest, 35% no longer met ADIS-C/P CSR diagnostic criteria for principal anxiety disorder for ABMt vs. 7% in control. | M.1 to M.5 |
| Whiteside et al. (2015) | N = 14. Ages 7 to 14 (M = 10.20). 71% girls. DSM GAD, Specific Phobia, SAD, SoP. Randomized to ICBT or parent-coached exposure therapy (PC-Exp). | At posttest and 3-month FU, PC-Exp led to lower CBCL internalizing, CBCL externalizing, PARS anxiety, ADIS CSR severity, CGI severity, SCAS anxiety, SCAS-P anxiety, CSDS-P disability, and CATS negative cognitions than ICBT. | M.1 to M.4 |
| Calear et al. (2016) | N = 1,167. Ages 12 to 18 years (M = 14.86). 75% girls. Randomized to school supported iCBT, health service supported iCBT (e-GAD HS), or waitlist control. | Intervention conditions did not differ from one another. At posttest and 6-month FU, school supported iCBT led to lower SAS-A social anxiety, GAD-Y generalized anxiety, and higher WEMWBS psychological wellbeing than control. At 6-month FU, e-GAD HS led to higher WEMWBS wellbeing than control. No between-group differences were evident for any outcome at 12-month FU. | M.1 to M.5 |
| Calear et al. (2016) | N = 225. Ages 12 to 18 years (M = 14.86). 75% girls. Randomized to school-based iCBT or waitlist control. | No between-group differences were evident for any outcome at posttest or 3-month FU. | M.1 to M.5 |
| Fitzgerald et al. (2016) | N = 130. Ages 15 to 18 years (M = 15.94). 57% girls. SPAI-C ≥ 24. Randomized to ABMt or attention control training (ACT). | Between-group differences were not evident at posttest or 4-month FU. Both ABMt and ACT led to lower SPAI-C social anxiety and SCARED anxiety. | M.1 to M.5 |
| Infantino et al. (2016) | N = 24. Ages 5 to 11 years (M = 7.46). 54% girls. DSM GAD, Specific Phobia, SAD, SoP. Randomized to audio-based CBT or waitlist control. | At posttest and 3-month FU, audio-based CBT led to lower ADIS-C/P CSR severity, SCAS anxiety, and SCAS-P anxiety than control. At posttest, ADIS-C/P CSR diagnostic recovery rates for principal disorder were 58.3% for audio-based CBT and 16.7% for control. At FU, diagnostic recovery rates for audio-based CBT was 66.67%. | M.1 to M.5 |
| Morgan et al. (2016) | N = 51. Ages 3 to 6 years (M = 4.75). 49% girls. STSC >30. Randomized to parent-focused iCBT with clinician support or parent-focused iCBT without clinician support. | Intervention conditions did not differ from one another. At posttest, both conditions led to lower PAS-R anxiety, SDQ emotional difficulties, OAPA number of child anxiety diagnoses, and CALIS-PV life interference of anxiety. | M.1 to M.5 |
| Pergamin-Hight et al. (2016) | N = 67. Ages 6 to 18 years (M = 12.67). 57% girls. DSM SAD. Randomized to ABMt or ACT. | Between-group differences were not evident. Both ABMt and ACT led to lower ADIS-C/P social anxiety severity, SPAI-C social anxiety, dot probe response latencies, and higher dot probe accuracy at post and 3-month FU. | M.1 to M.5 |
| Pophillat et al. (2016) | N = 206. Ages 6 to 9 years. Mean age not reported. 51% girls. Randomized to GCBT or usual care control (health education classes). | At posttest, GCBT led to lower SCAS-P anxiety. No other between-group differences emerged. Both conditions led to lower ACES emotional skills. | M.1 to M.5 |
| Ruttledge et al. (2016) | N = 709. Ages 9 to 13 years (M = 10.83). 51% girls. Randomized to GCBT or usual care control (health education classes). | A posttest, GCBT led to improved BSC-Y self-concept, CES coping efficacy, and SCS school connectedness. GCBT also led to lower SCAS anxiety, however change was not significantly different than control. | M.1 to M.5 |
| Scholten et al. (2016) | N = 139. Ages 11 to 15 years (M = 13.27). 65% girls. SCAS ≥ 1 SD above the mean total anxiety symptoms or ≥ 1 SD above the mean on two SCAS subscales. Randomized to Biofeedback w/relaxation training video game (Dojo) or control video game. | Linear change of the top scoring SCAS subscale from pretest to posttest to FU was greater for Dojo than control. No between-group differences emerged for SCAS total anxiety. | M.1 to M.5 |
| Schoneveld et al. (2016) | N = 136. Ages 7 to 13 years (M = 9.95). 55% girls. SCAS ≥ 1 SD above the mean total anxiety symptoms or ≥ 1 SD above the mean on two SCAS subscales. Randomized to neurofeedback w/exposures and ABMt video game (Mindlight) or control video game. | Between-group differences were not evident at posttest and 3-month FU. Both Mindlight and control led to lower SCAS and SCAS-P anxiety. | M.1 to M.5 |
| Vigerland et al. (2016) | N = 93. Ages 8 to 12 years (M = 10.10). 51% girls. DSM GAD, PD, SAD, SoP, or Specific Phobia. Randomized to internet-delivered CBT with therapist-support or waitlist control. | At posttest, internet-delivered CBT led to lower ADIS-C/P CSR severity, SCAS-P anxiety, and improved CGAS functioning than control, with ADIS-C/P CSR severity and CGAS functioning improvements maintained at 3-month FU. No other between-group differences emerged on SCAS anxiety or QOLI-C quality of life. Internet-delivered CBT led to reduced SCAS anxiety and QOLI-C quality of life at posttest. | M.1 to M.5 |
| Ahlen et al. (2018) | N = 695. Ages 8 to 11 years (M = 9.60). 48% girls. Randomized to GCBT or waitlist control. | Between-group differences were not evident for any outcome at posttest and 12-month FU. | M.1 to M.5 |
| Cobham et al. (2017) | N = 61. Ages 7 to 14 years (M = 9.30). 49% girls. DSM Specific phobia, SAD, GAD, or SoP. Randomized to parent-focused GCBT or waitlist control. | At posttest, 3-, 6-, and 12-month FU, parent-focused intervention led to lower ADIS-C/P CSR severity, SCAS-P anxiety, SCAS anxiety, and CBCL internalizing than control. At posttest, 64.5% in parent-focused intervention were free from principal anxiety disorder vs. 16.2% in control based on ADIS-C/P CSR criterion. Parent-focused intervention ADIS-C/P CSR recovery rates improved to 84% at 12-month FU. | M.1 to M.5 |
| Creswell et al. (2017) | N = 136. Ages 5 to 12 (M = 9.21). 53% girls. Referred to mental health clinic for anxiety-related impairments. Randomized to brief guidance parent-delivered CBT or solution focused brief therapy (SFBT) | Between-group differences were not evident for any outcome at posttest or 3-month FU. Both brief guidance parent-delivered CBT and SFBT led to higher CGI improvement scores and lower KFQ-C fears, SCAS anxiety, SCAS-P anxiety, and ADIS-C/P CSR. | M.1 to M.5 |
| De Voogd et al. (2017) | N = 108. Ages 11 to 19 years (M = 14.45). 67% girls. SCARED >16 anxiety symptoms and/or CDI >7 depressive symptoms. Randomized to internet-based visual search ABMt (VS-ABMt), VS placebo-training, or no intervention control. | At posttest, VS-ABMt led to lower EVST attentional bias and Recognition Task interpretation bias than controls. No other between-group differences emerged on SCARED anxiety, CDI-C depression, RSES self-esteem, PTQ perseverative thinking, and SDQ-P strengths and difficulties, with all conditions having led to improvements in these outcomes at posttest and 6-month FU. | M.1 to M.5 |
| Kato and Shimizu (2017) | N = 74. Ages 8 to 9 years. Mean age not reported. 43% girls. Randomized to GCBT or no intervention control. | At posttest, GCBT led to lower SCAS-P anxiety. No other between-group differences emerged on SCAS anxiety, DSRS-depression, Hope, or SDQ-P total difficulties. | M.1 to M.5 |
| Morgan et al. (2017) | N = 433. Ages 3 to 6 years (M = 4.80). 53% girls. STSC >30. Randomized to parent-focused iCBT (with clinician support as needed) or waitlist control. | At posttest, parent-focused internet-based CBT led to lower PAS-R anxiety, CALIS life interference, and fewer PAS-R anxiety disorder diagnoses than control (40% vs. 54%, respectively). | M.1 to M.5 |
| Schoneveld et al. (2017) | N = 174. Ages 7 to 12 years (M = 9.97). 59% girls. Randomized to cognitive-behavioral neurofeedback training video game video game (Mindlight) or GCBT. SCAS ≥ 1 SD above the mean total anxiety symptoms or ≥ 1 SD above the mean on two SCAS subscales. | Between-group differences were not evident. Both Mindlight and GCBT led to lower SCAS and SCAS-P anxiety at posttest, 3-month and 6-month FU. | M.1 to M.5 |
| Weersing et al. (2017) | N = 185. Ages 8 to 17 (M = 11.30). 58% girls. DSM GAD, Specific Phobia, SAD, SoP. Randomized to brief behavioral therapy (BBT) or assisted referral to care (ARC). | At posttest, BBT led to lower CGI severity, PARS anxiety, improvements in CGAS functioning, and higher rates of CGI clinical improvement (56.8% vs. 28.2%) than ARC. | M.1 to M.5 |
| Bayer et al. (2018) | N = 545. Ages 3 to 6 years (M = 4.55). 48% girls. Australian Temperament Project approach/inhibition >30. Randomized to parent-focused GCBT or treatment as usual control (access to community mental health services). | Between-group differences were not evident. Both parent-focused GCBT and control led to lower SDQ internalizing symptoms and fewer DSM anxiety disorder diagnoses based on ADIS-C/P criteria. | M.1 to M.5 |
| Chavira et al. (2018) | N = 31. Ages 8 to 13 years (M= 11.25). Mean age and sex not reported. DSM Specific phobia, SAD, GAD, or SoP. Randomized to parent-mediated CBT bibliotherapy telephone-delivered, therapist-assisted bibliotherapy or parent-mediated CBT bibliotherapy minimal contact, self-directed. | At posttest, ADIS-C/P CSR recovery rates were 50% in telephone-therapist and 36% for self-directed. | M.1 to M.5 |
| Liu et al. (2018) | N = 84. Ages 9 to 12 years. Mean age and sex not reported. Met criteria for behavioral inhibition per BIQ. Randomized to ABMt or attention control training. | At posttest, ABMt led to lower C-DISC-IV separation anxiety than control. ABMt also led to reduced amygdala and insulate activation and enhanced activation in ventrolateral prefrontal cortex relative to control via fMRI data. | M.1 to M.5 |
| Ollendick et al. (2018) | N = 58. Ages 12 to 16 years (M = 14.29). 71% girls. DSM SAD. Randomized to ABMt or ACT. | At posttest, ABMt led to lower SCARED-C social anxiety than control. No other between-group differences emerged on SCARED-P social anxiety, EATQ-R-P attention control, or dot probe threat bias. Both ABMt and control led to lower SCARED-P social anxiety at posttest. | M.1 to M.5 |
| Schleider and Weisz (2018) | N = 96. Ages 12 to 15 years (M = 13.33) 55% girls. RCADS-P ≥ 84th percentile, has school-based accommodations for internalizing symptoms, or sought treatment for anxiety in past 3 years. Randomized to computer-based growth mind-set intervention (GMI) or computer-based supportive-therapy. | GMI led to lower CDI-P depression, SCARED-P anxiety, PCSC behavioral control, and CDI-C depression than computer-based supportive-therapy. | M.1 to M.5 |
| Suveg et al. (2018) | N = 92. Ages 7 to 12 years. Mean age not reported. 42% girls. DSM GAD, SAD, SoP. Randomized to emotion-focused CBT (ECBT) or ICBT. | Intervention conditions did not differ from one another. At posttest, both ECBT and ICBT led to lower ERC emotion regulation, ERC emotion dysregulation, ERC anger regulation, CEMS anger, sadness, and worry dysregulation, ADIS-C/P CSR severity, and CGI severity. At posttest, 72% in ECBT and 74% in ICBT no longer met ADIS-IV diagnostic criteria for their principal anxiety disorder. | M.1 to M.5 |
| Pina et al. (2020) | N = 109. Ages 8 to 12 (M = 9.64). 78% girls. SCAS ≥ 42 anxiety symptoms. Randomized to GCBT with social skills training or active control. | At 12-month FU, GCBT led to higher SEQSS self-efficacy for managing anxiety, SSIS-RS social competence, and lower CNCEQ cognitive interpretation biases than control. | M.1 to M.5 |
| Phobias (n = 10) | |||
| Sheslow et al. (1983) | N = 32. Ages 4 to 5 years. Mean age not reported. 50% girls. Darkness phobia as measure by <8 seconds of darkness tolerance. Randomized to graduated exposure, verbal coping skills, graduated exposure plus verbal coping skills, or contact-only control. | At posttest, graduated exposure condition and graduated exposure plus verbal coping skills conditions led to improved BAT dark tolerance than verbal coping skills and control, with more pronounced improvements occurring for graduated exposure condition. | M.1 to M.4 |
| Menzies and Clarke (1993) | N = 48. Ages 3 and 8 years (M = 5.50). BRS <15 and water phobic (no DSM diagnosis). Randomized to in vivo exposure plus vicarious exposure (IWE), vicarious exposure (VE), in vivo exposure (IVE), or assessment only control. | At posttest, IWE and IVE led to lower CWP water phobia, PCWP water phobia, OR phobic reactions, and greater improvements in BRS approach behavior and ability than control. At FU, IWE, VE, and IVE led to further reductions in OR phobic reactions, and improvements in BRS approach behavior and ability than control. At FU, IVE demonstrated poorer effect maintenance and improvement on all outcomes than IWE. | M.1 to M.5 |
| Cornwall et al. (1996) | N = 24. Ages 7 to 10 years (M = 8.25). DSM Specific Phobia (darkness). Randomized to individual emotive imagery therapy (EAT) or waitlist control. | At posttest and FU, EAT led to improvements in behavioral responses to darkness tolerance and lower FSSC-R fears, RCMAS anxiety, DFBQ darkness fear behavior than control. | M.1 to M.5 |
| Muris et al. (1998) | N = 28. Ages 8 to 17 years (M = 12.58). 100% girls. DSM Specific Phobia (spiders). Randomized to EMDR, in vivo exposure (IVE), or computerized exposure control. | At posttest and FU, IVE led to lower SPQ-C spider fear, SAM fear/arousal, BAT state anxiety, and BAT spider avoidance than EMDR and control. At posttest, EMDR led to lower SPQ-C spider fear than control. | M.1 to M.4 |
| Dewis et al. (2001) | N = 28. Ages 10 to 17 years. Mean age not reported. 64% girls. DSM Specific Phobia (spiders). Randomized to live graded exposure (LGE), computer-aided vicarious exposure (CAVE), or waitlist control. | At posttest and 1-month FU, LGE and CAVE had lower SPQ-C spider phobia, PT phobic severity, BAT approach avoidance, and SUDS than control. At posttest, LGE improved more than CAVE on SPQ-C and SUDS and led to greater reductions in SPQ-C spider phobia and PT phobic severity than CAVE at FU. | M.1 to M.4 |
| Öst et al. (2001) | N = 60. Ages 7 to 17 years (M = 11.70). 61% girls. DSM Specific Phobia. Randomized to child only one session treatment for specific phobia (OST), parent present OST, or waitlist control. | At posttest and 1-year FU, child only OST and parent present OST led to lower BAT avoidance than waitlist control, with greater improvements emerging for child only OST. No other between-group differences emerged on FSSC-R fears, RCMAS anxiety, CASI anxiety sensitivity, STAIC trait anxiety, STAIC state anxiety, and CDI depression. Both child-only OST and parent present OST led to lower FSSC-R fear, RCMAS anxiety, STAIC anxiety, and CASI anxiety sensitivity at post and FU. | M.1 to M.5 |
| Ollendick et al. (2009) | N = 196. Ages 7 to 16 years (M = 11.00). 55% girls. DSM Specific Phobia. Randomized to OST, education support treatment (EST), or waitlist control. | At posttest, OST led to lower BAT SUDS and ADIS-C/P CSR than EST and control. At 6-month FU, OST led to lower ADIS-C/P CSR severity than EST and control. Both OST and EST led to lower CBCL anxiety/depression, MASC anxiety, and FSSC-R fears than control at posttest and FU; OST and EST did not differ from one another for these outcomes. At posttest, ADIS-C/P CSR diagnostic recovery rates were 55% in OST, 23% in EST, and 2% in control; recovery rates were similar at FU (52% in OST and 21% in EST). | M.1 to M.5 |
| Flatt and King (2010) | N = 43. Ages 7 to 17 years (M = 11.23). 60% girls. DSM Specific Phobia. Randomized to OST, psychoeducation, or waitlist control. | Intervention conditions did not differ from one another. At posttest and 1-year FU, OST and Psychoeducation led to lower BAT approach avoidance and FSSC-II tearfulness, as well as higher SEQ-SP self-efficacy than control. | M.1 to M.5 |
| Waters et al. (2014) | N = 37. Ages 6 to 17 years (M = 10.56) 57% girls. DSM Specific Phobia. Randomized to Attention training toward positive stimuli plus OST (ATP+OST) or attention control training plus OST (ACT+OST). | At posttest and 3-month FU, ATP+OST led to lower danger expectancies to fear stimuli and greater bias toward positive stimuli at posttest than ACT+OST. No other between-group differences emerged on SCAS anxiety, SCAS-P anxiety, and SMFQ-C/P depression, with both ATP+OST and ACT+OST having led to lower SCAS anxiety, SCAS-P anxiety, and SMFQ-C/P depression at posttest and FU. | M.1 to M.5 |
| Ollendick et al. (2015) | N = 97. Ages 6 to 15 years. Mean age not reported. 52% girls. DSM Specific Phobia. Randomized to OST or parent-augmented OST (A-OST). | Intervention conditions did not differ from one another at posttest or 1-month FU. Both OST and A-OST led to lower ADIS-C/P CSR severity and higher PIR and CIR anxiety improvement. At 6-month FU, OST resulted in marginally superior ADIS-C/P diagnostic recovery ratings than A-OST (67.39% for OST and 49.02% for A-OST). | M.1 to M.5 |
ACES = Assessment of Children’s Emotional Skill; ADIS-C/P = Anxiety Disorders Interview Schedule for DSM-IV; ADIS-C/P CSR = Clinician Severity Rating; ASP = Ambiguous Situations Protocol; AWS = Adolescent Wellbeing Scale; BAI = Beck Anxiety Inventory; BASC-PRS = Behavior Assessment System for Children–Parent Rating Scales; BAT = Behavioral Assessment Test; BERS-P = Behavioral and Emotional Rating Scale (Parent); BERS-T = Behavioral and Emotional Rating Scale (Teacher); BHS = Beck Hopelessness Scale; BIQ = Behavioral Inhibition Questionnaire; BRS = Behavior Response Scale; BSC-Y = Beck Self-Concept Inventory for Youth; C-DISC-IV = Diagnostic Interview Schedule for Children; CALIS = Child Anxiety Life Interference Scale; CALIS-P = Child Anxiety Life Interference Scale (Parent); CALIS-PV-P = Child Anxiety Life Interference Scale – Preschool Version (Parent); CASI = Child Anxiety Sensitivity Index; CATS = Children’s Automatic Thoughts Scale; CBCL = Child Behavior Checklist; CDI = Children’s Depression Inventory; CEMS = Children’s Emotion Management Scales; CES = Coping Efficacy Scale; CES-DC = Center for Epidemiological Studies Depression Scale; CGAS = Children’s Global Assessment Scale; CGI = Clinical Global Impressions; CIR = Child Improvement Rating; CNCEQ = Children’s Negative Cognitive Error Questionnaire; CRS = Child Rating Scale; CSDS-P = Child Sheehan Disability Scale (Parent); CSI = Coping Strategy Indicator; CWP = Water Phobia Survey Schedule; DFBQ = Darkness Fear Behavior Questionnaire; DSRS-C = Depression Self Rating Scale for Children; EATQ-R-P = Early Adolescent Temperament Questionnaire-Revised Short Form; ERC = Emotion Regulation Checklist; FSSC-R = Fear Survey Schedule for Children-Revised; GAD = Generalized Anxiety Disorder; GAD-7 = Generalized Anxiety Disorder – Seven item scale; Hope = Children’s Hope Scale; KFQ-C = Koala Fear Questionnaire – child report; LSAS – RS = Liebowitz Social Anxiety Scale-Revised; MADRS-S = Montgomery-Asberg Depression Rating Scale-Self Report; MASC = Multidimensional Anxiety Scale for Children; MASC-P = Multidimensional Anxiety Scale for Children (Parent); MES = Motivation and Engagement Scale; OAPA = Online Assessment of Preschool Anxiety; OR = Overall Reaction; PAS = Preschool Anxiety Scale; PAS-R = Preschool Anxiety Scale-Revised; PCSC = Perceived Control Scale for Children; PCWP = Water Phobia Survey Schedule (Parent); PHQ = Patient Health Questionnaire; PIR = Parent Improvement Rating; PT = Phobic Target; PTQ = Perseverative Thinking Questionnaire; QOLI-C Quality of Life Inventory-Child Version; RCADS = Revised Children’s Anxiety and Depression Scale; RCMAS = Revised Children’s Manifest Anxiety Scale; RSEI = Rosenberg Self-Esteem Inventory; RSES = Rosenberg Self-Esteem Scale; RTAS = Revised Test Anxiety Scale; SAD = Separation Anxiety Disorder; SAM = Self-Assessment Manikin; SASA = Social Anxiety Scale for Adolescents-Avoidance; SASC-R = Social Anxiety Scale for Children-Revised; SCARED = Screen for Child Anxiety Related Emotional Disorders; SCARED-P = Screen for Child Anxiety Related Emotional Disorders (Parent); SCAS = Spence Children’s Anxiety Scale; SCAS-P = Spence Children’s Anxiety Scale SCAS-P (Parent); SCBE = Social Competence and Behavior Evaluation; SCS = School Connectedness Scale; SDQ-P = Strengths and Difficulties Questionnaire (Parent); SEI = Self Esteem Inventory; SEQ-SP Self-Efficacy Questionnaire for Specific Phobias; SEQSS = Self Efficacy Questionnaire for School Situations; SMFQ = Short Mood and Feelings Questionnaire; SMFQ-P = Short Mood and Feelings Questionnaire (Parent); SoP = Social Phobia; SOSI = Symptoms of Stress Inventory; SPAI-C = Social Phobia and Anxiety Inventory; SPQ-C = Spider Phobia Questionnaire for Children; SPSQ-C = Social Phobia Screening Questionnaire for Children; SQC = Schema Questionnaire for Children; SSIS-RS = Social Skills Improvement System-Rating Scales; STAIC = State-Trait Anxiety Inventory for Children; STAXI = State Trait Anger Expression Inventory; STSC = Short Temperament Scale for Children; STSC-P = Short Temperament Scale for Children (Parent); SUDS = Subjective Units of Distress; TABC-R-P = Temperament Assessment Battery for Children-Revised (Parent); TASC = Test Anxiety Scale for Children; TRF = Teacher’s Report Form; WEMWBS = Warwick-Edinburgh Mental Wellbeing Scale; YSR = Youth Self Report.
K = number of studies; N = sample size; g = weighted mean effect size; SDg = weighted standard deviation of g; 95% CI = 95% confidence interval; FSN = Fail-Safe N, which is the number of samples with an effect size of zero that should have been left out in order to reduce estimated effect size to non-significance; Qw = Variability among effect sizes; Pre to follow-up is average of 8.88 months; *p <.05, ** p <.01, ***p <.001.
Effect Sizes Produced by Brief, Non-Pharmacological Interventions
Of the total sample of 76 studies, 64 reported data necessary to calculate between-group effect sizes (i.e., raw means and standard deviations for outcomes measured at a minimum of two time points for an intervention and comparator). Calculated effect sizes are reported in Table 3. In the table, column 1 corresponds to the level of intervention. Column 2 shows the number of studies that contributed to the effect size calculation, and column 3 indicates the meta-analytic sample size. Column’s 4 through 7 report the weighted Hedge’s g effect sizes of anxiety outcomes and corresponding effect size standard deviations, 95% confidence intervals, and fail-safe N. Finally, column 8 reports Q-test statistics relevant to heterogeneity among effect sizes.
TABLE 3.
Estimates of pre to post and pre to follow-up between-group mean effect sizes for anxiety outcomes across brief EBIs.
| K | N | g | SDg | 95% Cl | FSN | Qw | ||
|---|---|---|---|---|---|---|---|---|
| Pre to Post | ||||||||
| Overall | 64 | 10,384 | 0.19 | 0.27 | 0.11 | 0.27 | 287 | 189.60 (63)*** |
| Treatment | 25 | 1,300 | 0.35 | 0.36 | 0.20 | 0.50 | 80 | 24.65 (24) |
| Prevention | 37 | 9,084 | 0.13 | 0.24 | 0.04 | 0.22 | 66 | 129.87 (38)*** |
| Targeted Prevention | 17 | 2,315 | 0.23 | 0.25 | 0.10 | 0.36 | 24 | 30.10 (16)* |
| Indicated Prevention | 13 | 1,915 | 0.22 | 0.24 | 0.10 | 0.30 | 14 | 22.56 (12)* |
| Selective Prevention | 4 | 400 | 0.31 | 0.27 | 0.06 | 0.46 | 2 | 7.22 (3) |
| Universal Prevention | 17 | 6,769 | 0.09 | 0.19 | −0.01 | 0.20 | - | 58.42 (16)*** |
| Pre to Follow-up | ||||||||
| Overall | 30 | 6,440 | 0.24 | 0.24 | 0.13 | 0.34 | 80 | 91.94 (29)*** |
| Treatment | 6 | 235 | 0.30 | 0.50 | 0.04 | 0.56 | 4 | 13.74 (5)* |
| Prevention | 23 | 5,855 | 0.22 | 0.23 | 0.12 | 0.33 | 43 | 77.45 (23)*** |
| Targeted Prevention | 15 | 2,057 | 0.29 | 0.28 | 0.14 | 0.44 | 24 | 17.94 (14) |
| Indicated Prevention | 13 | 1,881 | 0.30 | 0.29 | 0.13 | 0.47 | 18 | 17.01 (12) |
| Selective Prevention | 2 | 176 | 0.21 | 0.10 | −0.09 | 0.51 | - | 0.004 (1) |
| Universal Prevention | 8 | 3,798 | 0.17 | 0.17 | 0.03 | 0.32 | 4 | 26.70 (7)*** |
K = number of studies; N = sample size; g = weighted mean effect size; SDg = weighted standard deviation of g; 95% CI = 95% confidence interval; FSN = Fail-Safe N, which is the number of samples with an effect size of zero that should have been left out in order to reduce estimated effect size to non-significance; Qw = Variability among effect sizes; Pre to follow-up is average of 8.88 months;
p <.05,
p <.01,
p <.001.
Findings showed that brief-treatments produced a pre to post effect size of 0.35 (SDg = 0.36) whereas brief-prevention produced a pre to post effect size of 0.13 (SDg = 0.24). Within brief-prevention, there was some variability. Indicated and selective prevention produced effect sizes of 0.22 (SDg = 0.24) and 0.31 (SDg = 0.25), respectively. Analyses revealed no significant differences in pre to post effect sizes between indicated and selective prevention studies (Qb = 0.32, p < .57) and were thus combined into a singular targeted prevention category for remaining analyses. Universal prevention produced an effect size of 0.09 (SDg = 0.19); from pre to post. Overall, fail-safe N calculations were generally robust; however, the fail-safe N for selective prevention estimate was 2 suggesting that those effects would likely be altered by the presence of studies producing null effects or could simply be due to the small number of included studies (n = 4).
Results for pre to follow-up effect sizes were based on the 30 studies that reported follow-up data with continuation assessments ranging from 1 month to 4 years post-intervention. The meta-regression showed that follow-up duration did not account for significant differences in effect sizes (Q = 2.19 [1, 116], p = .14); accordingly, effects were averaged across assessments such that each study in the meta-analysis contributed a single estimate of pre to follow-up effects (M = 8.88 months; SD = 8.76). As shown in Table 3, the effect size for brief anxiety treatments decreased slightly (approximately 0.05 g-units) from pre-intervention to follow-up suggesting that these interventions could be mostly maintaining effects over time rather than showing growth in clinical outcome gains. Prevention produced an overall effect size from pre-intervention to follow-up of 0.22 (SD = 0.23) representing an increase of 0.09 g-units from pre to post-intervention effects. This suggests a slight growth in clinical outcome gains over time Indicated prevention produced a pre to follow-up effect size of 0.30 (SD = 0.29), universal prevention produced a pre to follow-up effect size of 0.17 (SD = 0.17), and lastly, selective prevention produced a pre to follow-up effect size of 0.21 (SD = 0.10).
Moderators of Brief, Non-Pharmacological Intervention Effects
There was moderate to a high degree of heterogeneity and thus moderation analyses were conducted as planned. That is, heterogeneity statistics indicated a significant degree of between-study variance in effect sizes from pre to post (Qw = 189.60 [63], p < .001) and pre to follow-up (Qw = 91.94 [29], p < .001). I2 statistics indicated that 46.80% to 70.30% was true between-study variation; pre to follow-up effect sizes had I2 rates of 68.40% to 73.77%.
From pre to post-intervention, only level of intervention emerged as a significant moderator of effect sizes (Qb = 28.11, p < .001), such that treatment yielded larger effect sizes (g = 0.26; 95% CI 0.16 to 0.37) than targeted prevention (g = 0.21; 95% CI 0.12 to 0.30). Universal prevention (g = 0.09; 95% CI −0.05 to 0.23) effects were non-significant. In terms of the levels of prevention, there was a significant difference in pre to post effect sizes between targeted and universal prevention (Qb = 3.84, p < .05). None of the participant traits and no other intervention level characteristic emerged as significant moderators of pre to post or pre to follow-up effect sizes.
Evidence-Based Status of Brief, Non-Pharmacological, Interventions for Pediatric Anxiety
As shown in Table 4, the well-established criteria applied to in vivo exposure treatment (in one/single session with three intervention hours) for specific phobias. Six reengineered interventions met the probably efficacious criteria: CBT (9 to 10 h), behavior therapy (8 h), stress inoculation training (8 h), clinician supported digital parent training (6 h), and exposure-based CBT with social skills training (3 h). Sixteen reengineered interventions were classified as possibly efficacious: CBT with or without parents (8 hr), clinician supported digital CBT (3 to 7 h), and clinician supported bibliotherapy (3 to 5 h). Also, ABMt met the possibly efficacious criteria in terms of: training away from threatening stimuli (1,920 trials across 4 sessions), training toward positive stimuli (640 trials across 4 sessions). There is a handful of additional reengineered interventions meeting the possibly efficacious criteria (include stress inoculation training; growth mind-set training, psychoeducation, in-vivo exposures in 1.5 h, and emotive imagery for specific phobias). Eleven interventions were classified as experimental. That is, neurofeedback with exposure and attention training (5 h), as well as biofeedback interventions with relaxation training (6 h) as delivered via immersive computer video games were classified as experimental. These experimental interventions produced significant within-group reductions in pediatric anxiety outcomes, but no between-group comparisons against active controls. Eye movement desensitization and reprocessing (EMDR) (2.5 h) was found to be no better (or equivalent) to in-vivo exposures.
TABLE 4.
Level of support designations for the brief, non-pharmacological interventions for anxiety and phobias in youth.
| Level 1 | Level 2 | Level 3 | Level 4 | Level 5 | |
|---|---|---|---|---|---|
| Well-Established | Probably Efficacious | Possibly Efficacious | Experimental | Questionable | |
| Anxiety | None | Exposure-based CBT w/social skills 3 hours [66] CBT 9 hours [9, 36] 10 hours [4, 33] Digital parent training w/clinician supporta, d 6 hours [34, 57] Behavioral therapy 8 hours [59] Stress inoculation training 8 hours [2] |
CBT 8 hours [10] CBT plus psychoeducation for parents, teachers, and community health workers 7.5 hours [13] Parent trainingd 6 hours [12] 9 hours [53] Digital CBT w/clinician supporta 3 hours [14] 5 hours [44] 6 hours [51] 7 hours [18] Growth mind-set training 0.5 hours [64] Family-based CBT 8 hours [15, 38] Parent and teacher trainingd, e 7 hours [6] Clinician-guided bibliotherapya,b 3 hours [31] 5 hours [31] ABMt (away from negative) 1920 trials [28] ABMt (toward positive) 640 trials [32] |
CBT 6 hours [7] Relaxation training 4 hours [1] Cognitive training 4 hours [1] Clinician-guided, parent-coached exposurea 6 hours [40] Digital biofeedback w/relaxation training 6 hours [49] Digital neurofeedback w/exposure and attention training 5 hours [50] ABMt (away from negative) 640 trials [43] 768 trials [21] 1152 trials [55] 1600 trials [63] Bibliotherapy w/no clinician supportc [30] |
None |
| Phobias | In vivo exposure 3 hours [72, 73] |
None | Psychoeducation 3 hours [74] In vivo exposure 1.5 hours [68] Emotive imagery 4 hours [69] |
None | Eye movement desensitization and reprocessing (EMDR) 2.5 hours [70] |
Level of Support Designations is described in Table 1. Number in [] refers to the studies as cited in Table 2. ABMt = Attention Bias Modification Training; CBT = Cognitive behavior therapy; dash indicates not enough data to meta-analyze (i.e., at least two studies).
Clinician here broadly refers to any person in a position in which they are delivering these interventions (e.g., clinical psychologists, counselors, social workers, nurses, prevention or behavior specialists, school psychologists).
Overcoming your Child’s Fears and Worries: A Self-help Guide using Cognitive-Behavioral Techniques (Creswell & Willetts, 2007). Helping Your Anxious Child: A Step-by-Step Guide (Rapee et al., 2008).
Focused on teaching cognitive-behavioral skills relevant to managing parent anxiety and/or supporting child in managing their anxiety. Teacher training occurred through in-person and telephone consultation with a clinician.
Non-Pharmacological Prescription [P]
To help inform clinical practice, between-group, pre to post-intervention effect sizes were calculated only for well-established and probably efficacious brief-interventions along with the corresponding [p] scores (from the number of sessions, length of session, frequency of sessions); given published data. In terms of treatment, approximately 3 h of intervention for a specific phobia is able to produce a mean effect size of 0.36 (SD = 0.43; 95% CI = 0.08 to 0.80; k studies = 5) when in-vivo exposures are implemented. In addition, about 7 h of CBT for pediatric anxiety disorders is able to produce a mean effect size of 0.50 (SD = 0.52; 95% CI = 0.02 to 0.97; k = 6). Furthermore, approximately 6 h of clinician supported digital parent training is able to produce a mean effect size of 0.32 (SD = 0.14; 95% CI = 0.11 to 0.47; k = 2) on pediatric anxiety outcomes. From pre to follow-up (about 5 months), the overall mean effect size for CBT was 0.33 (SD = 0.47; 95% CI = 0.04 to 0.71; k = 3) but there were insufficient studies to reliably calculate pre to follow-up effect sizes for parent training, behavior therapy, and in vivo exposures.
Turning to prevention, targeted (indicated and selective) efforts are able to produce a mean effect size of 0.41 (SD = 0.30; 95% CI = 0.13 to 0.69; k = 6) from about 8 h of EBIs. Interestingly, these 8 h of EBIs are producing almost twice the effect size as typical length EBIs (per Fisak et al., 2011 meta-analysis). In contrast, the effect size for universal prevention was small (0.09, SD = 0.15; 95% CI = 0.01 to 0.18; k = 12) and less than the corresponding universal prevention effect from non-reengineered ones. The pre to follow-up (about 9 months) effect size for targeted prevention was 0.45 (SD = 0.36; 95% CI = 0.08 to 0.82; k = 5) and for universal, it was 0.20 (SD = 0.17; 95% CI = 0.04 to 0.35; k = 7; an increase of 0.08 g-units from pre to post-intervention).
DISCUSSION
A new wave of brief, non-pharmacological, interventions for pediatric anxiety could soon reach community practice settings. Several reengineered interventions largely characterized by “brevity” are well-established or probably efficacious. Among the protocols that produced significant clinical changes with the least prescription [p], one is well-established: in-vivo exposures for the treatment of specific phobias (~3 h, one session); four are probably efficacious: CBT with social skills training (~3 h, six sessions for indicated prevention and early intervention), and CBT-based parent training (~6 h, eight digital modules with clinician support) (Barrett et al., 2001; Bernstein et al., 2005; Collins et al., 2014; Donovan & March, 2014; Morgan et al., 2017; Öst et al., 2001; Pina et al., 2020; Stallard et al., 2014; Ollendick et al., 2009; Weersing et al., 2017). Others might already be well into the pipeline toward becoming well-established with greater clinical precision (e.g., see NIH Reporter grants MH109601–03 [Attention training for underserved youth with anxiety]; MH115113–02 [Brain response associated with parent-based treatment for childhood anxiety disorders]; MH101118–05S1 [An efficacy-effectiveness trial of cognitive bias modification for youth anxiety]). Among probably and possibly efficacious interventions were those designed for delivery by clinicians, nonprofessionals, and by youths themselves – with no designated therapist (e.g., computer-based interventions), suggesting the possibility that a wide array of supports may help mitigate the burdens of child and adolescent anxiety.
In our evaluation of effect sizes, larger effect were evident from treatment than from prevention (also see Fisak et al., 2011; Reynolds et al., 2012). We attribute such effect size variations to clinical severity levels, for example, such that (compared to prevention) youth in treatment are more severe on the primary clinical index (or clinical inclusion criterion) at the entry point. Yet, we also know that prevention takes time to have an effect on reducing disorder onset (Trudeau et al., 2016); thus, relatively smaller effect sizes from prevention should not be surprising. Among the types of prevention, effect sizes for the “targeted” prevention (selective, indicated) show the most promise compared to universal prevention. Thus, in addition to reengineered treatments, reengineered preventive interventions might be an efficient and effective solution to interrupting pediatric anxiety disorder development.
Despite these positive findings, we have the concern that reengineering of pediatric anxiety treatments into briefer formats might lead to less clinical effectiveness for some youth (e.g., ES: ~0.70 for typical length treatments; Reynolds et al., 2012; compared to 0.35 for brief-treatments). As explained by Ost and Ollendick (2017), some reengineered interventions might lack robustness given the fewer and limited opportunities for testing catastrophic beliefs and assumptions; both of which are cornerstones of pediatric anxiety change theory in treatment. Some reengineered interventions also offer less time for in-session clinical processes (e.g., corrective feedback) and out-of-session practice (or application of EBIs with quality). Our concern is somewhat alleviated by findings from Weisz et al. (2017) who showed that the number of treatment weeks is significantly and negatively related to the magnitude of intervention effects at posttest (i.e., when the total duration of an intervention increases, then clinical effects tend to diminish). Thus, our question is: Who is most/least likely to benefit from reengineered interventions? The concern that reengineering of pediatric anxiety treatments into briefer formats might lead to less clinical effectiveness for some youth might not extend to prevention (e.g., ES: 0.17; Fisak et al., 2011; compared to 0.13 for brief-prevention in this research). The possibility that there is an advantage for prevention requires replication with additional studies because the fail-safe N estimates were low, and most protocols were universal or indicated. Even if replicated, we anticipate that several moderators may help explain the effect size heterogeneity between treatment and prevention. In this research, with the exception of intervention level, no other candidate moderator variable was statistically significant. Null moderation is often linked to low statistical power (only half of the identified studies reported data to afford moderation) and study design restrictions (little variability from data corresponding to controlled efficacy trials).
At this juncture, we feel it is important to persevere on facilitating the uptake of evidence-based treatment and preventive interventions – particularly those that are widely scalable, adaptable to diverse settings, low-cost. Such uptake efforts need to be inclusive of reengineered interventions. Looking ahead, three major barriers to uptake are obvious. One, some reengineered interventions are designed to be intensive (e.g., one session lasting several hours; see Öst et al., 2001) but providers in some locales (e.g., United States) only can submit insurance claims corresponding to one-hour session per day. It might be the case that insurance companies and other organizations paying for mental health services need to learn that some reengineered interventions are more cost-effective (long term) than typical length interventions. Thus, it is incumbent on the next generation of intervention science to tackle research questions relevant to cost. Two, few reengineered interventions have been tested in effectiveness settings or under natural delivery conditions – although some new trials have suggested their acceptability and utility (e.g., in rural U.S. public schools: Schleider, Burnette, et al., 2019a). Not knowing if reengineered interventions are clinically viable under natural delivery conditions elicits questions about whether interventions can serve youth who are underrepresented in such literature. For example, Latinx youth ethnicity moderated poorer outcomes in the Child Anxiety Multisite Study (Walkup et al., 2008), the largest pediatric anxiety RCT comparing three treatment modalities, two of which used the Coping Cat cognitive-behavioral treatment package (Version 1.4 with no culturally responsive approaches) (Taylor et al., 2018). Reengineered interventions should consider in what ways, if any, activation parameters can have an effect on clinical change in pediatric anxiety among Latinx youth. Three, very few reengineered interventions are deployment ready but commercialized programs are making headways to penetrate systems of mental health care (schools, community service clinics) perceived as the marketplace. In prevention science, for example, several interventions are embodied into user-friendly manuals, gamifications for youth, various training options for providers, surface or in-depth consultation arrangements, fidelity and quality monitoring tools, and ongoing clinical and performance reports with cost-saving data (see the Blueprints for Healthy Development). The same level of readiness needs to be achieved for pediatric anxiety treatments.
Limitations are mostly methodological and reflect published science. We are aware that meta-analysis is insufficient for making causal inferences and only provides intervention effect estimated averages that are as reliable as the data in the published studies that we included. Here, meta-analysis findings merely complement results from the evidence-based status classification. Thus, we agree that effect sizes were based on an aggregate of anxiety measures that met a minimum criterion of psychometric strength (i.e., at least one documented psychometric property [e.g., reliability coefficients ranged from 0.60 to 0.94]) such that measurement error could have attenuated study-level effect sizes. For example, measurement error from the instruments used in the studies included in this evaluation could have led to incorrect conclusions regarding null moderating variables. We also agree that most of the studies that included follow-up data we used in the meta-analysis came from assessments conducted at 12-month posttreatment or less, such that the long-term impact and durability of clinical gains is not known. Perhaps brief interventions produce outcomes that are as durable as typical length interventions but whether that is true and under what conditions remains to be established. In addition, we agree that the large majority of studies included in the meta-analysis (86%) evaluated interventions under efficacy conditions, not effectiveness. We know that intervention-related effect sizes tend to decrease when EBIs are transported into real-world conditions (Fixsen et al., 2018); thus, in anticipation of smaller clinical effects, there is a need for implementation theory and corresponding research, including mediation. In fact, no study relevant to a well-established or probably efficacious reengineered intervention has tested mediation using an analytic approach that emphasizes temporal order (a requirement for inferring causality and providing information about the theory of the intervention’s sequential, cascading, or delayed clinical change from intervention efforts; Carper et al., 2018; Kraemer et al., 2002; MacKinnon, 2008). Knowledge of mediation could translate into informing refinement of the reengineering process by pointing to behavior change elements that should be augmented in [p] to achieve better clinical outcomes.
CONCLUDING COMMENT
Earmarking an intervention as well-established or probably efficacious does not translate into policy or readiness for adoption, sustainability, or scaling-up. As articulated by Elliott and Mihalic (2004), Flay et al. (2005), Greenberg et al. (2005), and Lyon et al. (2018), there need to be resources for adequate dissemination and implementation; assuming evidence already supports the fit among the intervention, the realities of delivery organizations, and the needs of end-users (e.g., service providers, youth, parents). In part, reengineered interventions aim at improving such fit. With knowledge that some reengineered interventions are well established, probably, or possibly efficacious, emphasis needs to be placed on securing resources for high-quality training, monitoring, technical assistance, and disclosures about costs (e.g., staff training, on-site time, space, equipment, reproduction of materials; Chatterji et al., 2001; Foster et al., 2003). There also needs to be ongoing collaboration among researchers and providers about the conditions under which the intervention is working, maintenance of program effects, and availability of innovative efficiencies (e.g., single-session digitally administered interventions, which have a uniquely high potential for scalability; Schleider, Dobias, et al., 2019b). Therefore, in our view, reengineered interventions (treatment and prevention) require improved precision from iterations as well as state-of-the-art armamentaria so that public health impact can be realized.
ACKNOWLEDGMENTS
We gratefully acknowledge Drs. Nancy Gonzales, David MacKinnon, and Marisol Perez for their feedback on this article.
FUNDING
This work was supported in part by a prevention and implementation science fellowship awarded to R. Stoll, T32 DA039772 01 from the National Institute on Drug Abuse and grant number K01MH086687 awarded to A. Pina from the National Institute of Mental Health. The content is solely the responsibility of the authors and does not represent the official views of the funding agencies.
Footnotes
DISCLOSURE STATEMENT
The authors declare that they have no conflict of interest.
Contributor Information
Ryan D. Stoll, Department of Psychology, Arizona State University
Armando A. Pina, Department of Psychology, Arizona State University
Jessica Schleider, Department of Psychology, Stony Brook University.
REFERENCES
- Aarons GA, Moullin JC, & Ehrhart MG (2018). The role of organizational processes in dissemination and implementation research In Brownson RC, Colditz GA, & Proctor EK (Eds.), Dissemination and implementation research in health: Translating science to practice (pp. 121–142). Oxford University Press; 10.1093/oso/9780190683214.003.0008 [DOI] [Google Scholar]
- Aarons GA, & Sawitzky AC (2006). Organizational climate partially mediates the effect of culture on work attitudes and staff turnover in mental health services. Administration and Policy in Mental Health and Mental Health Services Research, 33(3), 289–301. 10.1007/s10488-006-0039-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett PM, & Turner CM (2004). Prevention of childhood anxiety and depression In Barrett PM & Ollendick TH (Eds.), Handbook of interventions that work with children and adolescents: Prevention and treatment (pp. 429–474). John Wiley & Sons Ltd. 10.1002/9780470753385.ch18 [DOI] [Google Scholar]
- Becker BJ (1988). Synthesizing standardized mean-change measures. British Journal of Mathematical and Statistical Psychology, 41(2), 257–278. 10.1111/j.2044-8317.1988.tb00901.x [DOI] [Google Scholar]
- Beesdo K, Knappe S, & Pine DS (2009). Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. The Psychiatric Clinics of North America, 32(3), 483–524. 10.1016/j.psc.2009.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg I, Nichols K, & Pritchard C (1969). School phobia—its classification and relationship to dependency. Journal of Child Psychology and Psychiatry, 10(2), 123–141. 10.1111/j.1469-7610.1969.tb02074.x [DOI] [PubMed] [Google Scholar]
- Berkel C, Mauricio AM, Schoenfelder E, & Sandler IN (2011). Putting the pieces together: An integrated model of program implementation. Prevention Science, 12(1), 23–33. 10.1007/s11121-010-0186-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodden DH, Dirksen CD, & Bögels SM (2008). Societal burden of clinically anxious youth referred for treatment: A cost-of-illness study. Journal of Abnormal Child Psychology, 36(4), 487–497. 10.1007/s10802-007-9194-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, & Rothstein HR (2009). Introduction to meta- analysis. John Wiley & Sons. [Google Scholar]
- Brownson R, Colditz G, & Proctor E (2018). Future issues in dissemination and implementation research In Brownson RC, Colditz GA, & Proctor EK (Eds.), Dissemination and implementation research in health: Translating science to practice (pp. 481–490). Oxford University Press; 10.1093/oso/9780190683214.003.0029 [DOI] [Google Scholar]
- Carper MM, Makover HB, & Kendall PC (2018). Future directions for the examination of mediators of treatment outcomes in youth. Journal of Clinical Child & Adolescent Psychology, 47(2), 345–356. 10.1080/15374416.2017.1359786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambless DL, Baker MJ, Baucom DH, Beutler LE, Calhoun KS, Crits-Christoph P, & Johnson SB (1998). Update on empirically validated therapies, II. The Clinical Psychologist, 51(1), 3–16. 10.1037/e619622010-001 [DOI] [Google Scholar]
- Chambless DL, & Hollon SD (1998). Defining empirically supported therapies. Journal of Consulting and Clinical Psychology, 66(1), 7–18. 10.1037/0022-006x.66.1.7 [DOI] [PubMed] [Google Scholar]
- Chambless DL, & Ollendick TH (2001). Empirically supported psychological interventions: Controversies and evidence. Annual Review of Psychology, 52(1), 685–716. 10.1146/annurev.psych.52.1.685 [DOI] [PubMed] [Google Scholar]
- Chambless DL, Sanderson WC, Shoham V, Bennett Johnson S, Pope KS, Crits Cristoph P, & McCurry S (1996). An update on empirically validated therapies. The Clinical Psychologist, 49, 5–18. 10.1037/e555332011-003 [DOI] [Google Scholar]
- Chatterji P, Caffray CM, Jones AS, Lillie-Blanton M, & Werthamer L (2001). Applying cost analysis methods to school-based prevention programs. Prevention Science, 2(1), 45–55. 10.1023/A:1010086928908 [DOI] [PubMed] [Google Scholar]
- Chavira DA, Stein MB, Bailey K, & Stein MT (2004). Child anxiety in primary care: Prevalent but untreated. Depression and Anxiety, 20(4), 155–164. 10.1002/da.20039 [DOI] [PubMed] [Google Scholar]
- Chiarchiaro J, Arnold RM, & White DB (2015). Reengineering advance care planning to create scalable, patient-and family-centered interventions. JAMA, 313(11), 1103–1104. 10.1001/jama.2015.0569 [DOI] [PubMed] [Google Scholar]
- Chisholm D, Sweeny K, Sheehan P, Rasmussen B, Smit F, Cuijpers P, & Saxena S (2016). Scaling-up treatment of depression and anxiety: A global return on investment analysis. The Lancet Psychiatry, 3(5), 415–424. 10.1016/s2215-0366(16)30024-4 [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences. Lawrence Erlbaum. [Google Scholar]
- Cooper H, Hedges LV, & Valentine JC (Eds.). (2009). The handbook of research synthesis and meta-analysis. Russell Sage Foundation. [Google Scholar]
- Creswell C, & Willetts L (2007). Overcoming your child’s fear and worries: A self-help guide using cognitive behavioral techniques. Constable & Robinson Ltd. [Google Scholar]
- Cummings CM, Caporino NE, & Kendall PC (2014). Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychological Bulletin, 140(3), 816–845. 10.1037/a0034733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott DS, & Mihalic S (2004). Issues in disseminating and replicating effective prevention programs. Prevention Science, 5(1), 47–53. 10.1023/B:PREV.0000013981.28071.52 [DOI] [PubMed] [Google Scholar]
- Ezpeleta L, Keeler G, Erkanli A, Costello EJ, & Angold A (2001). Epidemiology of psychiatric disability in childhood and adolescence. The Journal of Child Psychology and Psychiatry and Allied Disciplines, 42(7), 901–914. 10.1111/1469-7610.00786 [DOI] [PubMed] [Google Scholar]
- Fisak BJ Jr, Richard D, & Mann A (2011). The prevention of child and adolescent anxiety: A meta-analytic review. Prevention Science, 12(3), 255–268. 10.1007/s11121-011-0210-0 [DOI] [PubMed] [Google Scholar]
- Fixsen DL, Blase KA, & Van Dyke MK (2018). Assessing implementation stages. Active Implementation Research Network. www.activeimplementation.org/resources
- Flay BR, Biglan A, Boruch RF, Castro FG, Gottfredson D, Kellam S, Mościcki EK, Schinke S, Valentine JC, & Ji P (2005). Standards of evidence: Criteria for efficacy, effectiveness and dissemination. Prevention Science, 6(3), 151–175. 10.1007/s11121-005-5553-y [DOI] [PubMed] [Google Scholar]
- Foster EM, Dodge KA, & Jones D (2003). Issues in the economic evaluation of prevention programs. Applied Developmental Science, 7(2), 76–86. 10.1207/S1532480XADS0702_4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gierisch JM, DeFrank JT, Bowling JM, Rimer BK, Matuszewski JM, Farrell D, & Skinner CS (2010). Finding the minimal intervention needed for sustained mammography adherence. American Journal of Preventive Medicine, 39(4), 334–344. 10.1016/j.amepre.2010.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS (2009). The child anxiety prevention study: Intervention model and primary outcomes. Journal of Consulting and Clinical Psychology, 77(3), 580–587. 10.1037/a0014486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Fisher L, Strycker LA, Hessler D, Toobert DJ, King DK, & Jacobs T (2014). Minimal intervention needed for change: Definition, use, and value for improving health and health research. Translational Behavioral Medicine, 4(1), 26–33. 10.1007/s13142-013-0232-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg MT, Domitrovich CE, Graczyk PA, & Zins JE (2005). The study of implementation in school-based preventive interventions: Theory, research, and practice (Vol. 3). Center for Mental Health Services, Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Harden SM, Smith ML, Ory MG, Smith-Ray RL, Estabrooks PA, & Glasgow RE (2018). RE-AIM in clinical, community, and corporate settings: Perspectives, strategies, and recommendations to enhance public health impact. Frontiers in Public Health, 6, 71 10.3389/fpubh.2018.00071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedges LV (1982). Estimation of effect size from a series of independent studies. Psychological Bulletin, 92(2), 490–499. 10.1037/0033-2909.92.2.490 [DOI] [Google Scholar]
- Hedges LV (1983). A random effects model for effect sizes. Psychological Bulletin, 93(2), 388–395. 10.1037/0033-2909.93.2.388 [DOI] [Google Scholar]
- Higa-McMillan CK, Francis SE, Rith-Najarian L, & Chorpita BF (2016). Evidence base update: 50 years of research on treatment for child and adolescent anxiety. Journal of Clinical Child & Adolescent Psychology, 45(2), 91–113. 10.1080/15374416.2015.1046177 [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, & Altman DG (2003). Measuring inconsistency in meta-analyses. BMJ, 327(7414), 557–560. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaccard J, & Guilamo-Ramos V (2002). Analysis of variance frameworks in clinical child and adolescent psychology: Issues and recommendations. Journal of Clinical Child and Adolescent Psychology, 31 (1), 130–146. 10.1207/s15374424jccp3101_15 [DOI] [PubMed] [Google Scholar]
- Kazdin AE, & Bass D (1989). Power to detect differences between alternative treatments in comparative psychotherapy outcome research. Journal of Consulting and Clinical Psychology, 57(1), 138–147. 10.1037/0022-006x.57.1.138 [DOI] [PubMed] [Google Scholar]
- Kessler RS, Purcell EP, Glasgow RE, Klesges LM, Benkeser RM, & Peek CJ (2013). What does it mean to “employ” the RE-AIM model? Evaluation & the Health Professions, 36(1), 44–66. 10.1177/0163278712446066 [DOI] [PubMed] [Google Scholar]
- Kohn R, Saxena S, Levav I, & Saraceno B (2004). The treatment gap in mental health care. Bulletin of the World Health Organization, 82, 858–866. 11 https://doi.org//S0042-96862004001100011 [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, & Agras WS (2002). Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry, 59(10), 877–883. 10.1001/archpsyc.59.10.877 [DOI] [PubMed] [Google Scholar]
- Lipsey MW, & Wilson DB (2001). Practical meta-analysis. Sage Publications, Inc. [Google Scholar]
- Lyon AR, Stanick C, & Pullmann MD (2018). Toward high-fidelity treatment as usual: Evidence-based intervention structures to improve usual care psychotherapy. Clinical Psychology: Science and Practice, 25(4), e12265 10.1111/cpsp.12265 [DOI] [Google Scholar]
- MacKinnon DP (2008). Multivariate applications series Introduction to statistical mediation analysis. Taylor & Francis Group/Lawrence Erlbaum Associates; 10.4324/9780203809556 [DOI] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, & Swendsen J (2010). Lifetime prevalence of mental disorders in US adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 980–989. 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris SB, & DeShon RP (2002). Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychological Methods, 313(11), 105–125. 10.1001/jama.2015.0569 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2017). Advancing the science to improve population health: Proceedings of a workshop. National Academies Press. [PubMed] [Google Scholar]
- O’Connell ME, Boat T, & Warner KE (Eds.). (2009). Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. National Academies Press. [PubMed] [Google Scholar]
- Öst LG, & Ollendick TH (2017). Brief, intensive and concentrated cognitive behavioral treatments for anxiety disorders in children: A systematic review and meta-analysis. Behaviour Research and Therapy, 97, 134–145. 10.1016/j.brat.2017.07.008 [DOI] [PubMed] [Google Scholar]
- Osterwalder A, & Pigneur Y (2011). Aligning profit and purpose through business model innovation. In Responsible Management Practices for the 21st Century (pp. 61–76). [Google Scholar]
- Pina AA, Gonzales NA, Mazza GL, Gunn HJ, Holly LE, Stoll RD, & Tein JY (2020). Streamlined prevention and early intervention for pediatric anxiety disorders: A randomized controlled trial. Prevention Science. 10.1007/s11121-019-01066-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell BJ, Bosk EA, Wilen JS, Danko CM, Van Scoyoc A, & Banman A (2015). Evidence-based programs in “real world” settings: Finding the best fit In Daro D, Cohn Donnelly A, Huang L, Powell B (Eds.), Advances in child abuse prevention knowledge. Child maltreatment (contemporary issues in research and policy (Vol. 5). Springer; 10.1007/978-3-319-16327-7_7 [DOI] [Google Scholar]
- Rapee R, Wignall A, Spence S, Lyneham H, & Cobham V (2008). Helping your anxious child: A step-by-step guide for parents. New Harbinger Publications. [Google Scholar]
- Raudenbush S, & Bryk A (2002). Hierarchical linear models:Applications and data analysis methods. Sage. [Google Scholar]
- Reid AM, Bolshakova MI, Guzick AG, Fernandez AG, Striley CW, Geffken GR, & McNamara JP (2017). Common barriers to the dissemination of exposure therapy for youth with anxiety disorders. Community Mental Health Journal, 53(4), 432–437. 10.1007/s10597-017-0108-9 [DOI] [PubMed] [Google Scholar]
- Reynolds S, Wilson C, Austin J, & Hooper L (2012). Effects of psychotherapy for anxiety in children and adolescents: A meta-analytic review. Clinical Psychology Review, 32(4), 251–262. 10.1016/j.cpr.2012.01.005 [DOI] [PubMed] [Google Scholar]
- Rhoades BL, Bumbarger BK, & Moore JE (2012). The role of a state-level prevention support system in promoting high-quality implementation and sustainability of evidence-based programs. American Journal of Community Psychology, 50(3–4), 386–401. 10.1007/s10464-012-9502-1 [DOI] [PubMed] [Google Scholar]
- Ringle VA, Read KL, Edmunds JM, Brodman DM, Kendall PC, Barg F, & Beidas RS (2015). Barriers to and facilitators in the implementation of cognitive-behavioral therapy for youth anxiety in the community. Psychiatric Services, 66(9), 938–945. 10.1176/appi.ps.201400134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers EM (2002). Diffusion of preventive innovations. Addictive Behaviors, 27(6), 989–993. 10.1016/s0306-4603(02)00300-3 [DOI] [PubMed] [Google Scholar]
- Rogers EM (2010). Diffusion of innovations. Simon and Schuster. [Google Scholar]
- Rosenthal R (1991). Meta-analytic procedures for social research. Sage. [Google Scholar]
- Rosenthal R, & DiMatteo MR (2001). Meta-analysis: Recent developments in quantitative methods for literature reviews. Annual Review of Psychology, 52(1), 59–82. 10.1146/annurev.psych.52.1.59 [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Swendeman D, & Chorpita BF (2012). Disruptive innovations for designing and diffusing evidence-based interventions. American Psychologist, 67(6), 463–476. 10.1037/a0028180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salloum A, Johnco C, Lewin AB, McBride NM, & Storch EA (2016). Barriers to access and participation in community mental health treatment for anxious children. Journal of Affective Disorders, 196, 54–61. 10.1016/j.jad.2016.02.026 [DOI] [PubMed] [Google Scholar]
- Schleider JL, Burnette JL, Widman L, Hoyt C, & Prinstein MJ (2019a). Randomized trial of a single-session growth mind-set intervention for rural adolescents’ internalizing and externalizing problems. Journal of Clinical Child & Adolescent Psychology, 1–13. 10.1080/15374416.2019.1622123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleider JL, Dobias ML, Sung JY, & Mullarkey MC (2019b). Future directions in single-session youth mental health interventions. Journal of Clinical Child and Adolescent Psychology, 1–15. 10.1080/15374416.2019.1683852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleider JL, & Weisz JR (2017). Little treatments, promising effects? Meta-analysis of single-session interventions for youth psychiatric problems. Journal of the American Academy of Child & Adolescent Psychiatry, 56(2), 107–115. 10.1016/j.jaac.2016.11.007 [DOI] [PubMed] [Google Scholar]
- Silverman WK, & Hinshaw SP (2008). The second special issue on evidence-based psychosocial treatments for children and adolescents: A 10-year update. Journal of Clinical Child & Adolescent Psychology, 37(1), 1–7. 10.1080/15374410701817725 [DOI] [PubMed] [Google Scholar]
- Silverman WK, Pina AA, & Viswesvaran C (2008). Evidence-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. Journal of Clinical Child & Adolescent Psychology, 37(1), 105–130. 10.1080/15374410701817907 [DOI] [PubMed] [Google Scholar]
- Southam-Gerow MA, & Prinstein MJ (2014). Evidence base updates: The evolution of the evaluation of psychological treatments for children and adolescents. Journal of Clinical Child & Adolescent Psychology, 43(1), 1–6. 10.1080/15374416.2013.855128 [DOI] [PubMed] [Google Scholar]
- Spoth R, Trudeau L, Redmond C, & Shin C (2014). Replication RCT of early universal prevention effects on young adult substance misuse. Journal of Consulting and Clinical Psychology, 82(6), 949 10.1037/a0036840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoll RD, & Pina AA (2016). Using meta-analytic path analysis to identify mediators of youth anxiety and depression intervention effects. Presented as part of organized symposia (‘Modern Methods for Mediation Analysis in Prevention’) at the 24th Annual Meeting of the Society for Prevention Research, San Francisco, CA. [Google Scholar]
- Taylor JH, Lebowitz ER, Jakubovski E, Coughlin CG, Silverman WK, & Bloch MH (2018). Monotherapy insufficient in severe anxiety? Predictors and moderators in the child/adolescent anxiety multimodal study. Journal of Clinical Child & Adolescent Psychology, 47(2), 266–281. 10.1080/15374416.2017.1371028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trudeau L, Spoth R, Mason WA, Randall GK, Redmond C, & Schainker L (2016). Effects of adolescent universal substance misuse preventive interventions on young adult depression symptoms: Mediational modeling. Journal of Abnormal Child Psychology, 44(2), 257–268. 10.1007/s10802-015-9995-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Noortgate W, López-López JA, Marín-Martínez F, & Sánchez-Meca J (2013). Three-level meta-analysis of dependent effect sizes. Behavior Research Methods, 45(2), 576–594. 10.3758/s13428-012-0261-6 [DOI] [PubMed] [Google Scholar]
- Verdurmen JE, Koning IM, Vollebergh WA, van den Eijnden RJ, & Engels RC (2014). Risk moderation of a parent and student preventive alcohol intervention by adolescent and family factors: A cluster randomized trial. Preventive Medicine, 60, 88–94. 10.1016/j.ypmed.2013.12.027 [DOI] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, Ginsburg GS, Rynn MA, McCracken J, Waslick B, Iyengar S, March JS, & Kendall PC (2008). Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine, 359(26), 2753–2766. 10.1056/nejmoa0804633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz JR, Kuppens S, Ng MY, Eckshtain D, Ugueto AM, Vaughn-Coaxum R, Weersing VR, Krumholz Marchette LS, Chu BC, Weersing VR, Fordwood SR, & Jensen-Doss A (2017). What five decades of research tells us about the effects of youth psychological therapy: A multilevel meta-analysis and implications for science and practice. American Psychologist, 72(2), 79–117. 10.1037/a0040360 [DOI] [PubMed] [Google Scholar]
- Wilson DB (2003). Meta-analysis macros for SAS, SPSS, and Stata. Retrieved March 15, 2014, from http://mason.gmu.edu/~dwilsonb/ma.html
- Wilson KM, Brady TJ, & Lesesne C, & NCCDPHP Work Group on Translation. (2011). An organizing framework for translation in public health: The knowledge to action framework. Preventing Chronic Diseases, 8 (2), A46. [PMC free article] [PubMed] [Google Scholar]
References
Studies Included in Review References with an asterisk (*) indicate studies that will be included in the meta-analyses
- *.Ahlen J, Hursti T, Tanner L, Tokay Z, & Ghaderi A (2018). Prevention of anxiety and depression in Swedish school children: A cluster-randomized effectiveness study. Prevention Science, 19(2), 147–158. 10.1007/s11121-017-0821-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Attwood M, Meadows S, Stallard P, & Richardson T (2012). Universal and targeted computerised cognitive behavioural therapy (Think, Feel, Do) for emotional health in schools: Results from two exploratory studies. Child and Adolescent Mental Health, 17(3), 173–178. 10.1111/j.1475-3588.2011.00627.x [DOI] [PubMed] [Google Scholar]
- *.Aune T, & Stiles TC (2009). Universal-based prevention of syndromal and subsyndromal social anxiety: A randomized controlled study. Journal of Consulting and Clinical Psychology, 77(5), 867–879. 10.1037/a0015813 [DOI] [PubMed] [Google Scholar]
- *.Balle M, & Tortella-Feliu M (2009). Efficacy of a brief school-based program for selective prevention of childhood anxiety. Anxiety, Stress and Coping, 23(1), 71–85. 10.1080/10615800802590652 [DOI] [PubMed] [Google Scholar]
- *.Bar-Haim Y, Morag I, & Glickman S (2011). Training anxious children to disengage attention from threat: A randomized controlled trial. Journal of Child Psychology and Psychiatry and Allied Disciplines, 52(8), 861–869. 10.1111/j.1469-7610.2011.02368.x [DOI] [PubMed] [Google Scholar]
- *.Barrett PM, Moore AF, & Sonderegger R (2000). The FRIENDS program for young former-Yugoslavian refugees in Australia: A pilot study. Behaviour Change, 17(3), 124–133. 10.1375/bech.17.3.124 [DOI] [Google Scholar]
- *.Barrett PM, Sonderegger R, & Sonderegger NL (2001). Evaluation of an anxiety-prevention and positive-coping program (FRIENDS) for children and adolescents of non-english-speaking background. Behaviour Change, 18(2), 78–91. 10.1375/bech.18.2.78 [DOI] [Google Scholar]
- Bayer JK, Beatson R, Bretherton L, Hiscock H, Wake M, Gilbertson T, Mihalopoulos C, Prendergast LA, & Rapee RM (2018). Translational delivery of Cool Little Kids to prevent child internalizing problems: Randomized controlled trial. Australian and New Zealand Journal of Psychiatry, 52(2), 181–191. 10.1177/0004867417726582 [DOI] [PubMed] [Google Scholar]
- *.Bernstein GA, Bernat DH, Victor AM, & Layne AE (2008). School-based interventions for anxious children: 3-, 6-, and 12- month follow-ups. Journal of the American Academy of Child & Adolescent Psychiatry, 47(9), 1037–1047. 10.1097/CHI.ob013e31817eecco. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein GA, Layne AE, Egan EA, & Tennison DM (2005). School-based interventions for anxious children. Journal of the American Academy of Child & Adolescent Psychiatry, 44(11), 1118–1127. 10.1097/01.chi.0000177323.40005.a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Brown A, Creswell C, Barker C, Butler S, Cooper P, Hobbs C, & Thirlwall K (2017). Guided parent-delivered cognitive behaviour therapy for children with anxiety disorders: Outcomes at 3-to 5-year follow-up. British Journal of Clinical Psychology, 56(2), 149–159. 10.1111/bjc.12127 [DOI] [PubMed] [Google Scholar]
- *.Calear AL, Christensen H, Brewer J, Mackinnon, & Griffiths KM (2016). A pilot randomized controlled trial of the e-couch anxiety and worry program in schools. Internet Interventions, 6, 1–5. 10.1016/j.invent.2016.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Calear AL, Christensen H, Mackinnon A, Griffiths KM, & O’Kearney R (2009). The youthmood project: A cluster randomized controlled trial of an online cognitive behavioral program with adolescents. Journal of Consulting and Clinical Psychology, 77(6), 1021–1032. 10.1037/a0017391 [DOI] [PubMed] [Google Scholar]
- Chavira DA, Bustos C, Garcia M, Reinosa Segovia F, Baig A, Ng B, & Camacho A (2018). Telephone-assisted, parent-mediated CBT for rural Latino youth with anxiety: A feasibility trial. Cultural Diversity and Ethnic Minority Psychology, 24 (3),429 10.1037/cdp0000186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Cobham VE, Filus A, & Sanders MR (2017). Working with parents to treat anxiety-disordered children: A proof of concept RCT evaluating Fear-less Triple P. Behaviour Research and Therapy, 95, 128–138. 10.1016/j.brat.2017.06.004 [DOI] [PubMed] [Google Scholar]
- *.Collins S, Woolfson LM, & Durkin K (2014). Effects on coping skills and anxiety of a universal school-based mental health intervention delivered in Scottish primary schools. School Psychology International, 35(1), 85–100. 10.1177/0143034312469157 [DOI] [Google Scholar]
- *.Cornwall E, Spence SH, & Schotte D (1996). The effectiveness of emotive imagery in the treatment of darkness phobia in children. Behaviour Change, 13(4), 223–229. 10.1017/s0813483900004824 [DOI] [Google Scholar]
- *.Creswell C, Violato M, Fairbanks H, White E, Parkinson M, Abitabile G, & Cooper PJ (2017). Clinical outcomes and cost-effectiveness of brief guided parent-delivered cognitive behavioral therapy and solution-focused brief therapy for treatment of childhood anxiety disorders: A randomized controlled trial. The Lancet Psychiatry, 4(7), 529–539. 10.1016/S2215-0366(17)30149-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Dadds MR, & Roth JH (2008). Prevention of anxiety disorders: Results of a universal trial with young children. Journal of Child and Family Studies, 17(3), 320–335. 10.1007/s10826-007-9144-3 [DOI] [Google Scholar]
- *.De Voogd EL, Wiers RW, & Salemink E (2017). Online visual search attentional bias modification for adolescents with heightened anxiety and depressive symptoms: A randomized controlled trial. Behaviour Research and Therapy, 92, 57–67. 10.1016/j.brat.2017.02.006 [DOI] [PubMed] [Google Scholar]
- Dewis LM, Kirkby KC, Martin F, Daniels BA, Gilroy LJ, & Menzies RG (2001). Computer-aided vicarious exposure versus live graded exposure for spider phobia in children. Journal of Behavior Therapy and Experimental Psychiatry, 32(1), 17–27. 10.1375/bech.18.2.103 [DOI] [PubMed] [Google Scholar]
- *.Donovan CL, & March S (2014). Online CBT for preschool anxiety disorders: A randomised control trial. Behaviour Research and Therapy, 58, 24–35. 10.1016/j.brat.2014.05.001 [DOI] [PubMed] [Google Scholar]
- Eldar S Ph. D., Apter A, Lotan D, Edgar KP, Naim R, Fox NA, Pine DS, & Bar-haim Y (2012). Attention bias modification treatment for pediatric anxiety disorders: A randomized controlled trial. American Journal of Psychiatry, 169(2), 213–220. 10.1176/appi.ajp.2011.11060886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Fitzgerald A, Rawdon C, & Dooley B (2016). A randomized controlled trial of attention bias modification training for socially anxious adolescents. Behaviour Research and Therapy, 84, 1–8. 10.1016/j.brat.2016.06.003 [DOI] [PubMed] [Google Scholar]
- Flatt N, & King N (2010). Brief psycho-social interventions in the treatment of specific childhood phobias: A controlled trial and a 1-year follow-up. Behaviour Change, 27(3), 130–153. 10.1375/bech.27.3.130 [DOI] [Google Scholar]
- *.Gallagher HM, Rabian BA, & McCloskey MS (2004). A brief group cognitive-behavioral intervention for social phobia in childhood. Journal of Anxiety Disorders, 18(4), 459–479. 10.1016/S0887-6185(03)00027-6 [DOI] [PubMed] [Google Scholar]
- *.Ginsburg GS (2009). The child anxiety prevention study: Intervention model and primary outcomes. Journal of Consulting and Clinical Psychology, 77(3), 580–587. 10.1037/a0014486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Ginsburg GS, Becker KD, Drazdowski TK, & Tein J-Y (2012). Treating anxiety disorders in inner city schools: Results from a pilot randomized controlled trial comparing CBT and usual care Golda. Child & Youth Care Forum, 41(1), 1–19. 10.1007/s10566-011-9156-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Ginsburg GS, & Drake KL (2002). School-based treatment for anxious African American adolescents: A controlled pilot study. Journal of the American Academy of Child and Adolescent Psychiatry, 41(7), 768–775. 10.1097/00004583-200207000-00007 [DOI] [PubMed] [Google Scholar]
- Ginsburg GS, Drake KL, Tein JY, Teetsel R, & Riddle MA (2015). Preventing onset of anxiety disorders in offspring of anxious parents: A randomized controlled trial of a family-based intervention. American Journal of Psychiatry, 172(12), 1207–1214. 10.1176/appi.ajp.2015.14091178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Hains AA (1992). Comparison of cognitive-behavioral stress management techniques with adolescent boys. Journal of Counseling & Development, 70(5), 600–605. 10.1002/j.1556-6676.1992.tb01668.x [DOI] [Google Scholar]
- *.Heyne D, King NJ, Tonge BJ, Rollings S, Young D, Pritchard M, & Ollendick TH (2002). Evaluation of child therapy and caregiver training in the treatment of school refusal. Journal of the American Academy of Child & Adolescent Psychiatry, 41(6), 687–695. 10.1097/00004583-200206000-00008 [DOI] [PubMed] [Google Scholar]
- *.Hunt C, Andrews G, Sakashita C, Crino R, & Erskine A (2009). Randomized controlled trial of an early intervention programme for adolescent anxiety disorders. Australian & New Zealand Journal of Psychiatry, 43 (4), 300–304. 10.1080/00048670902721152 [DOI] [PubMed] [Google Scholar]
- *.Infantino A, Donovan CL, & March S (2016). A randomized controlled trial of an audio-based treatment program for child anxiety disorders. Behaviour Research and Therapy, 79, 35–45. 10.1016/j.brat.2016.02.007 [DOI] [PubMed] [Google Scholar]
- *.Kato S, & Shimizu E (2017). A pilot study on the effectiveness of a school-based cognitive-behavioral anxiety intervention for 8- and 9-year-old children: A controlled trial in Japan. Mental Health and Prevention, 8(October), 32–38. 10.1016/j.mhp.2017.10.001 [DOI] [Google Scholar]
- *.Kennedy SJ, Rapee RM, & Edwards SL (2009). A selective intervention program for inhibited preschool-aged children of parents with an anxiety disorder: Effects on current anxiety disorders and temperament. Journal of the American Academy of Child & Adolescent Psychiatry, 48(6), 602–609. 10.1097/chi.0b013e31819f6fa9 [DOI] [PubMed] [Google Scholar]
- *.Khanna MS, & Kendall PC (2010). Computer-assisted cognitive behavioral therapy for child anxiety: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology, 78(5), 737–745. 10.1037/a0019739 [DOI] [PubMed] [Google Scholar]
- *.Kiselica MS, Baker SB, Thomas RN, & Reedy S (1994). Effects of stress inoculation training on anxiety, stress, and academic performance among adolescents. Journal of Counseling Psychology, 41(3), 335–342. 10.1037/0022-0167.41.3.335 [DOI] [Google Scholar]
- *.Lee SS, Victor AM, James MG, Lauren E, & Bernstein GA (2017). School-based interventions for anxious children: Long-term follow-up. Child Psychiatry and Human Development, 47(2), 183–193. 10.1007/s10578-015-0555-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu P, Taber-Thomas BC, Fu X, & Pérez-Edgar KE (2018). Biobehavioral markers of attention bias modification in temperamental risk for anxiety: A randomized control trial. Journal of the American Academy of Child and Adolescent Psychiatry, 57(2), 103–110. 10.1016/j.jaac.2017.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.McLoone J, & Rapee RM (2012). Comparison of an anxiety management program for children implemented at home and school: Lessons learned. School Mental Health, 4(4), 231–242. 10.1007/s12310-012-9088-7 [DOI] [Google Scholar]
- Menzies RG, & Clarke JC (1993). A comparison of in vivo and vicarious exposure in the treatment of childhood water phobia. Behaviour Research and Therapy, 31(1), 9–15. 10.1016/0005-7967(93)90037-U [DOI] [PubMed] [Google Scholar]
- *.Mifsud C, & Rapee RM (2005). Early intervention for childhood anxiety in a school setting: Outcomes for an economically disadvantaged population. Journal of the American Academy of Child and Adolescent Psychiatry, 44(10), 996–1004. 10.1097/01.chi.0000173294.13441.87 [DOI] [PubMed] [Google Scholar]
- *.Miller LD, Short C, Garland EJ, & Clark S (2010). The ABCs of CBT (cognitive behavior therapy): Evidence-based approaches to child anxiety in public school settings. Journal of Counseling and Development, 88(4), 432–439. 10.1002/j.1556-6678.2010.tb00043.x [DOI] [Google Scholar]
- *.Miller LD, Laye-Gindhu A, Bennett JL, Liu Y, Gold S, March JS, Olson BF, & Waechtler VE (2011). An effectiveness study of a culturally enriched school-based CBT anxiety prevention program. Journal of Clinical Child and Adolescent Psychology, 40(4), 618–629. 10.1080/15374416.2011.581619 [DOI] [PubMed] [Google Scholar]
- *.Miller LD, Laye-Gindhu A, Liu Y, March JS, Thordarson DS, & Garland EJ (2011). Evaluation of a preventive intervention for child anxiety in two randomized attention-control school trials. Behaviour Research and Therapy, 49(5), 315–323. 10.1016/j.brat.2011.02.006 [DOI] [PubMed] [Google Scholar]
- *.Morgan AJ, Rapee RM, Salim A, Goharpey N, Tamir E, McLellan LF, & Bayer JK (2017). Internet-delivered parenting program for prevention and early intervention of anxiety problems in young children: Randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 56(5), 417–425. 10.1016/j.jaac.2017.02.010 [DOI] [PubMed] [Google Scholar]
- *.Morgan AJ, Rapee RM, & Bayer JK (2016). Prevention and early intervention of anxiety problems in young children: A pilot evaluation of Cool Little Kids online. Internet Interventions, 4, 105–112. 10.1016/j.invent.2016.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Muris P, Meesters C, & van Melick M (2002). Treatment of childhood anxiety disorders: A preliminary comparison between cognitive-behavioral group therapy and a psychological placebo intervention. Journal of Behavior Therapy and Experimental Psychiatry, 33(3–4), 143–158. 10.1016/s0005-7916(02)00025-3 [DOI] [PubMed] [Google Scholar]
- *.Muris P, Merckelbach H, Holdrinet I, & Sijsenaar M (1998). Treating phobic children: Effects of EMDR versus exposure. Journal of Consulting and Clinical Psychology, 66(1), 193–198. 10.1037/0022-006X.66.1.193 [DOI] [PubMed] [Google Scholar]
- Ollendick TH, Halldorsdottir T, Fraire MG, Austin KE, Noguchi RJP, Lewis KM, Jarrett MA, Cunningham NR, Canavera K, Allen KB, & Whitmore MJ (2015). Specific phobias in youth: A randomized controlled trial comparing one-session treatment to a parent-augmented one-session treatment. Behavior Therapy, 46(2), 141–155. 10.1016/j.beth.2014.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Ollendick TH, Öst LG, Reuterskiöld L, Costa N, Cederlund R, Sirbu C, Davis TE, & Jarrett MA (2009). One-session treatment of specific phobias in youth: A randomized clinical trial in the united states and Sweden. Journal of Consulting and Clinical Psychology, 77(3), 504–516. 10.1037/a0015158 [DOI] [PubMed] [Google Scholar]
- *.Öst LG, Svensson L, Hellström K, & Lindwall R (2001). One-session treatment of specific phobias in youths: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 69(5), 814–824. 10.1037/0022-006X.69.5.814 [DOI] [PubMed] [Google Scholar]
- *.Pahl KM, & Barrett PM (2010). Preventing anxiety and promoting social and emotional strength in preschool children: A universal evaluation of the fun FRIENDS program. Advances in School Mental Health Promotion, 3(3), 14–25. 10.1080/1754730x.2010.9715683 [DOI] [Google Scholar]
- *.Pella JE, Drake KL, Tein JY, & Ginsburg GS (2017). Child anxiety prevention study: Impact on functional outcomes. Child Psychiatry and Human Development, 48(3), 400–410. 10.1007/s10578-016-0667-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pergamin-Hight L, Pine DS, Fox NA, & Bar-Haim Y (2016). Attention bias modification for youth with social anxiety disorder. Journal of Child Psychology and Psychiatry and Allied Disciplines, 57(11), 1317–1325. 10.1111/jcpp.12599 [DOI] [PubMed] [Google Scholar]
- *.Pina AA, Gonzales NA, Mazza GL, Gunn HJ, Holly LE, Stoll R, Parker J, Chiapa A, Wynne H, & Tein JY (2020). Streamlined prevention and early intervention for youth anxiety disorders. Prevention Science. 10.1007/s11121-019-01066-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Pophillat E, Rooney RM, Nesa M, Davis MC, Baughman N, Hassan S, & Kane RT (2016). Preventing internalizing problems in 6–8 year old children: A universal school-based program. Frontiers in Psychology, 7(December), 1–13. 10.3389/fpsyg.2016.01928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putwain DW, & Pescod M (2018). Is reducing uncertain control the key to successful test anxiety intervention for secondary school students? Findings from a randomized control trial. School Psychology Quarterly, 33(2), 283–292. 10.1037/spq0000228 [DOI] [PubMed] [Google Scholar]
- Rapee RM (2013). The preventative effects of a brief, early intervention for preschool-aged children at risk for internalising: Follow-up into middle adolescence. Journal of Child Psychology and Psychiatry and Allied Disciplines, 54(7), 780–788. 10.1111/jcpp.12048 [DOI] [PubMed] [Google Scholar]
- Rapee RM, Kennedy S, Ingram M, Edwards S, & Sweeney L (2005). Prevention and early intervention of anxiety disorders in inhibited preschool children. Journal of Consulting and Clinical Psychology, 73(3), 488–497. 10.1037/0022-006X.73.3.488 [DOI] [PubMed] [Google Scholar]
- Reuland MM, & Teachman BA (2014). Interpretation bias modification for youth and their parents: A novel treatment for early adolescent social anxiety. Journal of Anxiety Disorders, 28(8), 851–864. 10.1016/j.janxdis.2014.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Rodgers A, & Dunsmuir S (2015). A controlled evaluation of the “FRIENDS for life” emotional resiliency programme on overall anxiety levels, anxiety subtype levels and school adjustment. Child and Adolescent Mental Health, 20(1), 13–19. 10.1111/camh.12030 [DOI] [PubMed] [Google Scholar]
- *.Ruttledge R, Devitt E, Greene G, Mullany M, Charles E, & Frehill J (2016). A randomised controlled trial of the FRIENDS for Life emotional resilience programme delivered by teachers in Irish primary schools. Educational & Child Psychology, 33(2), 69–89. [Google Scholar]
- Salemink E, & Wiers RW (2011). Modifying threat-related interpretive bias in adolescents. Journal of Abnormal Child Psychology, 39(7), 967–976. 10.1007/s10802-011-9523-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleider J, & Weisz J (2018). A single-session growth mindset intervention for adolescent anxiety and depression: 9-month outcomes of a randomized trial. Journal of Child Psychology and Psychiatry, 59(2), 160–170. 10.1111/jcpp.12811 [DOI] [PubMed] [Google Scholar]
- *.Scholten H, Malmberg M, Lobel A, Engels RCME, Granic I, & Jiménez-Murcia (2016). A randomized controlled trial to test the effectiveness of an immersive 3D video game for anxiety prevention among adolescents. PLoS ONE, 11(1), 1–24. 10.1371/journal.pone.0147763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Schoneveld EA, Lichtwarck-Aschoff A, & Granic I (2017). Preventing childhood anxiety disorders: Is an applied game as effective as a cognitive behavioral therapy-based program? Prevention Science, 19(2), 220–232. 10.1007/s11121-017-0843-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Schoneveld EA, Malmberg M, Lichtwarck-Aschoff A, Verheijen GP, Engels RCME, & Granic I (2016). A neurofeedback video game (MindLight) to prevent anxiety in children: A randomized controlled trial. Computers in Human Behavior, 63, 321–333. 10.1016/j.chb.2016.05.005 [DOI] [Google Scholar]
- Sheslow DV, Bondy AS, & Nelson RO (1983). A comparison of graduated exposure, verbal coping skills, and their combination in the treatment of children’s fear of the dark. Child & Family Behavior Therapy, 4(2–3), 33–45. 10.1300/J019v04n02_03 [DOI] [Google Scholar]
- *.Skryabina E, Taylor G, & Stallard P (2016). Effect of a universal anxiety prevention programme (FRIENDS) on children’s academic performance: Results from a randomized controlled trial. Journal of Child Psychology and Psychiatry and Allied Disciplines, 57(11), 1297–1307. 10.1111/jcpp.12593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stallard P, Richardson T, Velleman S, & Attwood M (2011). Computerized CBT (Think, Feel, Do) for depression and anxiety in children and adolescents: Outcomes and feedback from a pilot randomized controlled trial. Behavioural and Cognitive Psychotherapy, 39(3), 273–284. 10.1017/S135246581000086X [DOI] [PubMed] [Google Scholar]
- *.Stallard P, Skryabina E, Taylor G, Phillips R, Daniels H, Anderson R, & Simpson N (2014). Classroom-based cognitive behaviour therapy (FRIENDS): A cluster randomised controlled trial to Prevent Anxiety in Children through Education in Schools (PACES). The Lancet Psychiatry, 1(3), 185–192. 10.1016/S2215-0366(14)70244-5 [DOI] [PubMed] [Google Scholar]
- Ollendick TH, White SW, Richey J, Kim-Spoon J, Ryan SM, Wieckowski AT, Coffman MC, Elias R, Strege MV, Capriola-Hall NN, & Smith M (2018). Attention bias modification treatment for adolescents with social anxiety disorder. Behavior Therapy, 50(1), 126–139. 10.1016/j.beth.2018.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Suveg C, Jones A, Davis M, Jacob ML, Morelen D, Thomassin K, & Whitehead M (2018). Emotion-focused cognitive-behavioral therapy for youth with anxiety disorders: A randomized trial. Journal of Abnormal Child Psychology, 46(3), 569–580. 10.1007/s10802-017-0319-0 [DOI] [PubMed] [Google Scholar]
- *.Thirlwall K, Cooper PJ, Karalus J, Voysey M, Willetts L, & Creswell C (2013). Treatment of child anxiety disorders via guided parent-delivered cognitive-behavioural therapy: Randomised controlled trial. British Journal of Psychiatry, 203(6), 436–444. 10.1192/bjp.bp.113.126698 [DOI] [PubMed] [Google Scholar]
- *.Tillfors M, Andersson G, Ekselius L, Furmark T, Lewenhaupt S, Karlsson A, & Carlbring P (2011). A randomized trial of internet-delivered treatment for social anxiety disorder in high school students. Cognitive Behaviour Therapy, 40(2), 147–157. 10.1080/16506073.2011.555486 [DOI] [PubMed] [Google Scholar]
- *.Vigerland S, Ljótsson B, Thulin U, Öst LG, Andersson G, & Serlachius E (2016). Internet-delivered cognitive behavioural therapy for children with anxiety disorders: A randomised controlled trial. Behaviour Research and Therapy, 76, 47–56. 10.1016/j.brat.2015.11.006 [DOI] [PubMed] [Google Scholar]
- *.Waters AM, Farrell LJ, Zimmer-Gembeck MJ, Milliner E, Tiralongo E, Donovan CL, McConnell H, Bradley BP, Mogg K, & Ollendick TH (2014). Augmenting one-session treatment of children’s specific phobias with attention training to positive stimuli. Behaviour Research and Therapy, 62, 107–119. 10.1016/j.brat.2014.07.020 [DOI] [PubMed] [Google Scholar]
- Waters AM, Pittaway M, Mogg K, Bradley BP, & Pine DS (2013). Attention training towards positive stimuli in clinically anxious children. Developmental Cognitive Neuroscience, 4, 77–84. 10.1016/j.dcn.2012.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Waters AM, Zimmer-Gembeck MJ, Craske MG, Pine DS, Bradley BP, & Mogg K (2015). Look for good and never give up: A novel attention training treatment for childhood anxiety disorders. Behaviour Research and Therapy, 73, 111–123. 10.1016/j.brat.2015.08.005 [DOI] [PubMed] [Google Scholar]
- *.Weersing VR, Brent DA, Rozenman MS, Gonzalez A, Jeffreys M, Dickerson JF, Lynch FL, Porta G, & Iyengar S (2017). Brief behavioral therapy for pediatric anxiety and depression in primary care. JAMA Psychiatry, 74(6), 571 10.1001/jamapsychiatry.2017.0429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Whiteside SPH, Ale CM, Young B, Dammann JE, Tiede MS, & Biggs BK (2015). The feasibility of improving CBT for childhood anxiety disorders through a dismantling study. Behaviour Research and Therapy, 73, 83–89. 10.1016/j.brat.2015.07.011 [DOI] [PubMed] [Google Scholar]
- Wong N, Kady L, Mewton L, Sunderland M, & Andrews G (2014). Preventing anxiety and depression in adolescents: A randomised controlled trial of two school-based Internet-delivered cognitive behavioural therapy programmes. Internet Interventions, 1(2), 90–94. 10.1016/j.invent.2014.05.004 [DOI] [Google Scholar]


