Abstract
Purpose of the Review
To discuss tear- and patient-related factors that influence the healing potential of rotator cuff tears and to clarify the terminology surrounding this topic.
Recent Findings
Over the last few years, further insight has been gained regarding rotator cuff tear features that are associated with poor healing rates after rotator cuff repair. Some of these features have been incorporated in prediction models developed to accurately predict rotator cuff healing rates utilizing preoperative risk factors weighted by importance.
Summary
Rotator cuff tears may be considered functionally irreparable based on their size, chronicity, absence of adequate tendon length, atrophy, and fatty infiltration. Furthermore, advanced age, use of tobacco products, diabetes, and other patient-related factors may impair tendon healing. Careful analysis and discussion of all these factors with patients is essential to determine if surgical repair of a rotator cuff tear should be recommended, or if it is best to proceed with one of the several salvage procedures reviewed in this topical collection, including augmentation of the repair, superior capsular reconstruction, tendon transfers, and other.
Keywords: Rotator cuff, Rotator cuff repair, Re-tear, Non-healing, Irreparable, Factors
Introduction
The ultimate goal of rotator cuff repair surgery is to eliminate pain and restore function. Healing of the rotator cuff tendons after rotator cuff repair has been shown to best achieve these goals, with worse functional outcomes seen in those patients whose rotator cuff tears do not heal [1, 2]. Therefore, most would agree that maximizing the likelihood of rotator cuff healing is desirable in order to optimize patient outcomes [3].
Unfortunately, a substantial percentage of rotator cuff repairs do not result in tendon healing [4]. A recent meta-analysis reported a mean rotator cuff repair surgery non-healing rate of 26.6% [5]. Tendon healing rates have been found to be highly dependent upon multiple tear- and patient-related factors, and, accordingly, a great deal of research has been performed to better elucidate and understand the relative contributions of these factors to successful healing [6]. Broadly speaking, factors that influence rotator cuff tear reparability and healing fall into one of three categories: factors related to the nature of the tear, factors related to the patient, and factors related to the surgical repair technique and postoperative rehabilitation.
In this review, we focus on the preoperative factors—those related to the tear and the patient—that are thought to affect rotator cuff repair healing rates. Additionally, we present evidence to support or negate the influence of these factors on rotator cuff healing. In this regard, we have chosen to focus on studies that specifically report rotator cuff repair healing rates as opposed to relying on clinical outcomes as a surrogate for healing.
Defining Terms
Before discussing the tear- and patient-related factors that influence rotator cuff repair healing rates, it is important to clarify the terminology related to irreparable rotator cuff tears and rotator cuff repair healing (Table 1).
Table 1.
Definitions of important terms
| Term | Description | |
|---|---|---|
| Preoperative reparability | Irreparable RCT | RCT which is physically unable to be restored to its native footprint |
| Massive RCT | RCT of a certain size, typically > 5 cm2 or involving 3 or more tendons | |
| Functionally irreparable RCT | RCT which either cannot be restored to its native footprint or would result in poor functional outcomes if repaired | |
| Postoperative healing | RCR failure | Poor outcome after RCR, regardless of etiology |
| RCR non-healing | Failure of tendon healing after RCR | |
| RCR re-tear | Recurrent tendon tear following a healed RCR |
RCT, rotator cuff tear; RCR, rotator cuff repair
What Is an Irreparable Rotator Cuff Tear?
Though in general terms the phrase irreparable rotator cuff tear means that a tendon tear cannot be physically approximated and held securely to its anatomic footprint, with regard to rotator cuff tears, the entity we are trying to define needs to be expanded to include also those rotator cuff tears where meaningful improvements in pain and function will not be achieved even if a primary repair is physically feasible. Many refer to these more severe tears as massive irreparable rotator cuff tears, but the term massive only captures size: although many three-tendon tears are irreparable, some actually are (e.g., acute tears). Mayo Clinic surgeons have coined the term functionally irreparable rotator cuff tear reflecting the fact that some of these tears will just not reach the anatomic footprint (irreparable) whereas others may reach but still will not heal (functionally irreparable) due to several of the reasons discussed in this review [7••].
What Defines Failure of a Rotator Cuff Repair?
Rotator cuff repair failure is a broad term that may include not just lack of healing of the rotator cuff repair but also other complications, such as infection or postoperative stiffness, that lead to a poor outcome. When discussing lack of continuity of the muscle-tendon-bone unit after an attempted rotator cuff repair, the terms non-healing and re-tear are most often used. Mall and colleagues astutely observed that, while the terms re-tear and non-healing are often used interchangeably, very rarely do authors truly document rotator cuff tear healing followed by a subsequent recurrent tear [8]. The exception may be a repair that heals at the tendon to bone interface and unfortunately fails by tearing later on at the muscle-tendon junction. Our preference is to use the terms non-healing or incomplete healing for the typical clinical situation, and reserve the term re-tear or recurrent tear for either secondary tears at the muscle-tendon junction with documented healing at the tendon-bone junction or tear of a different tendon of the rotator cuff following documented healing of the tendons that were repaired.
How Is Rotator Cuff Repair Healing Measured?
Rotator cuff repair healing refers to the biologic restoration of physical continuity of the rotator cuff muscle-tendon-bone unit, reconstituting continuous tissue from the muscle belly origin to the anatomic footprint in bone [7••]. The methods used to assess healing vary widely [8]. Outside of research, surgeons may consider the repair clinically healed when strength is restored to normal. However, without an imaging modality—such as magnetic resonance imaging (MRI), CT arthrogram (CTA), or ultrasonography (US)—or a second-look arthroscopy, healing cannot be documented. Debate continues regarding the ideal imaging modality to assess cuff healing. CTA demonstrates for sure if there is lack of continuity anywhere in the muscle-tendon-bone unit, but it is invasive and requires radiation. MRI avoids invasiveness and radiation but, in some cases, it may be difficult to interpret, especially in the presence of anchor interference. US allows for dynamic evaluation but is operator-dependent and, even in the best of hands, has a sensitivity of 91%, specificity of 86%, and 89% accuracy in evaluating rotator cuff integrity postoperatively [9].
Tear-Related Factors
Tear Size
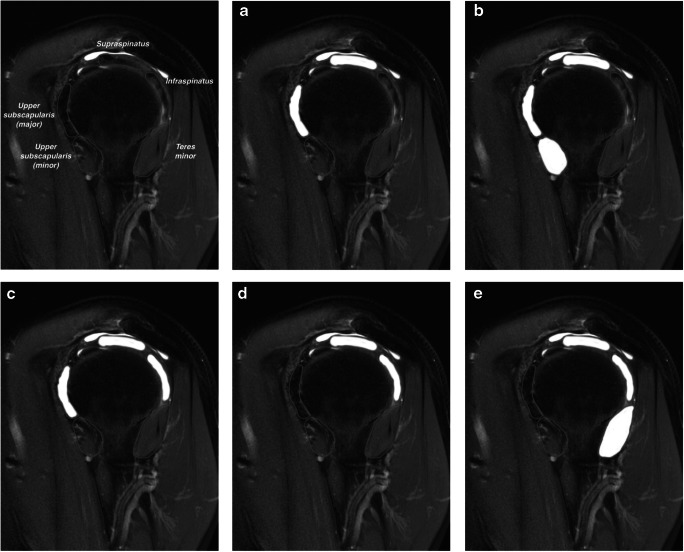
Rotator cuff tear size can be defined in many ways. The most commonly used systems in the literature include Drs. DeOrio and Cofield’s definition, which is based on measuring the size of the tear in centimeters (small 1, medium 1–3, large 3–5, massive > 5 cm2), and Dr. Gerber’s definition, which is based on the number of tendons involved in the tear [10]. Dr. Patte defined tear size based on the location of the tendon stump in reference to the equator of the humeral head and glenoid rim on coronal oblique imaging [11]. Additionally, Dr. Collin refined Dr. Gerber’s concept, proposing a geographical definition of tear size to predict the presence of shoulder pseudoparalysis (Fig. 1) [12].
Fig. 1.
Collin classification of rotator cuff tear size. T2 MRI sagittal oblique images demonstrating the Collin classification of rotator cuff tear size. The rotator cuff is divided into five sections: lower subscapularis, upper subscapularis, supraspinatus, infraspinatus, and teres minor. The classification system consists of five rotator cuff tear types: type A involves upper subscapularis and supraspinatus; type B involves the entire subscapularis and supraspinatus; type C involves upper subscapularis, supraspinatus, and infraspinatus; type D involves supraspinatus and infraspinatus; and type E involves supraspinatus, infraspinatus, and teres minor
Regardless of the specific size definition used, tear size has repeatedly been shown to correlate with non-healing after rotator cuff repair [2, 13–21]. Furthermore, in studies that have used statistical methods such as multivariate analyses to separate confounding variables, a larger tear size has consistently been found to be an independent risk factor for non-healing [14, 15, 18–20].
Tear size is one of the few tear- and patient-related factors that does not have contradictory evidence in the literature regarding its significant influence on rotator cuff repair healing rates. Most surgeons agree that tears that are massive (over 5 cm2) and/or involve three or more tendons (especially when extending into to the lower third of subscapularis or teres minor) fall into the category of FIRCT. However, as mentioned previously, it is important to recognize that size in and of itself does not definitely define tendon reparability as massive but acute tears often have good healing rates when repaired in a timely fashion, despite their size [22].
Fatty Infiltration
Fatty infiltration, or fatty degeneration, refers to the replacement of muscle tissue with adipose tissue within the confines of the epimysium. Fatty infiltration may be neurogenic or occur as a consequence of a chronic rotator cuff tear, where lack of muscle tension and contractility lead to degenerative changes with loss of muscle cells and an increase in fat cells [4]. Some prefer the term fatty degeneration to fatty infiltration, as animal studies have demonstrated that the causative progenitor cells reside within the muscle tissue prior to tissue injury, rather than infiltrating from a distant site after injury occurs [23].
Fatty degeneration is largely considered to be an irreversible and progressive process even after successful rotator cuff repair [24]. Therefore, quantifying the amount of fatty degeneration represents a key factor for the timing of surgery and in predicting expected functional outcomes following rotator cuff repair [20, 21]. The first classification of fatty infiltration was developed by Dr. Goutallier and was based on CT imaging [25]. Drs. Fuchs and Gerber studied fatty infiltration on MRI and developed a simplified MRI-based classification system (Table 2, Fig. 2) [26].
Table 2.
Fuchs-Gerber classification of rotator cuff fatty degeneration on MRI
| Grade | Description* | Goutallier grade equivalent |
|---|---|---|
| Normal | No fat present | 0 |
| Moderate | More muscle than fat | 1 or 2 |
| Severe | Equal or more fat than muscle | 3 or 4 |
*Based the amount of fat within the rotator cuff muscle epimysium on the most lateral T1 MRI sagittal oblique image where the scapular spine is still in continuity with the scapular body
Fig. 2.

Example of fatty degeneration on MRI. T1 MRI sagittal oblique image demonstrating moderate fatty degeneration of the supraspinatus and infraspinatus muscle bellies, according to the Fuchs-Gerber classification. Note that only fat (white) within the confines of the muscle parenchyma, as opposed to the fat surrounding the muscle belly, is considered true fatty degeneration
Many studies have evaluated the relationship between fatty degeneration and rotator cuff repair non-healing and have found routinely that increasing fatty degeneration is a strong independent risk factor for non-healing [2, 14, 16, 17•, 18, 20, 27–29, 30•, 31]. In fact, a recent meta-analysis of 18 studies concluded that fatty degeneration, with an odds ratio of 9.3, had the most significant negative effect on rotator cuff healing of all patient- and tear-related factors [32•]. Most surgeons would agree that fatty infiltration grade 3 or 4 in the Goutallier classification or advanced in the Fuchs-Gerber classification falls into the category of FIRCT. For posterosuperior rotator cuff tears, fatty infiltration of the infraspinatus is particularly relevant; a severe tear of the supraspinatus may be compensated for by the presence of well-balanced subscapularis and infraspinatus force couples. However, once the infraspinatus is severely compromised and develops advanced fatty infiltration, the prognosis of rotator cuff repair surgery seems to be substantially worse.
Suprascapular Neuropathy
Neuropathy may be associated with compression or stretching of the suprascapular nerve at the suprascapular or spinoglenoid notch secondary to severe retraction of a rotator cuff tear, and may result in the development of fatty degeneration [33, 34]. Goutallier noted that infraspinatus fatty degeneration often is more severe than that in the supraspinatus [25], and this may be due to compression on the suprascapular nerve at the spinoglenoid notch. Suprascapular neuropathy has not been evaluated as an independent risk factor for rotator cuff repair non-healing.
Muscle Atrophy
Muscle atrophy is another term that lends itself to confusion. It purely means that a muscle has lost bulk. Accurate quantification of the overall muscle bulk is difficult, however, since we tend to assess three-dimensional muscle volume on two-dimensional MRI or CT scan images. Additionally, muscle and tendon retraction can lead to a false impression of increased muscle atrophy. For example, let us take the supraspinatus muscle: since it is fusiform, when the muscle retracts secondary to a rotator cuff tear, the cross-sectional area will appear to have decreased on parasagittal imaging, even though the muscle may have not lost that much bulk overall. The only methods that would allow accurate assessment of muscle bulk would require manual or automatic segmentation of the muscles to render three-dimensional structures. This methodology exists today but is only used for research purposes. Another common error is to mislabel atrophy as fatty infiltration. As the muscle atrophies, the periscapular space previously occupied by muscle becomes occupied by connective tissue with a large content of fat. More fatty tissue outside of the outline of the epimysium (Fig. 2) is mistaken by some as true fatty degeneration within the confines of the muscle.
Nonetheless, supraspinatus atrophy has been assessed with methods such as the occupation ratio (ratio of the supraspinatus circumference to the supraspinatus fossa circumference) [20] and the tangent sign (failure of the supraspinatus muscle to cross a line between the superior coracoid process and the superior scapular spine; Fig. 3) [35]. Supraspinatus muscle atrophy, as measured by the tangent sign, has been found to be an independent risk factor for non-healing in one retrospective study [16]. Additionally, retrospective reviews using the occupation ratio have found that a ratio of < 53.5% [20] or < 43% [30•] is predictive of rotator cuff repair non-healing. Tangent lines can also be traced for the subscapularis (from the edge of the coracoid to the inferior scapular tip) and infraspinatus and teres minor (from the scapular spine to the inferior scapular tip).
Fig. 3.
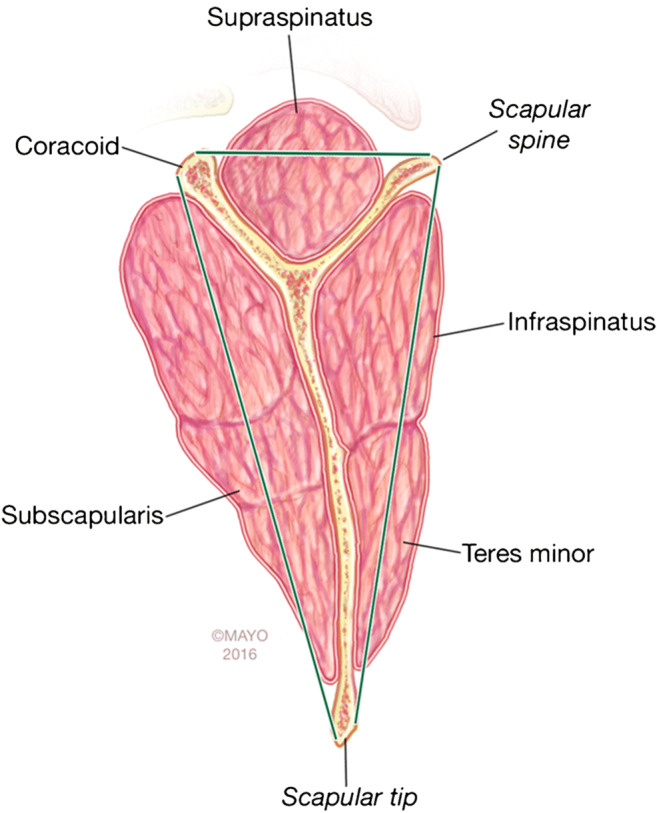
Tangent lines used to evaluate for muscle atrophy. Tangent lines can be used to evaluate muscle atrophy in the setting of a rotator cuff tear. Lines are drawn between the coracoid tip and scapular spine (supraspinatus), the coracoid and the scapular tip (subscapularis), and scapular spine and scapular tip (infraspinatus and teres minor) on sagittal oblique images. A positive tangent sign is present when the respective muscle bellies do not cross their tangent line. “Used with permission of Mayo Foundation for Medical Education and Research. All rights reserved”
Tendon Delamination and Tissue Quality
Tendon delamination and tissue quality are related but distinct terms. Tendon delamination refers to the separation of the tendon in layers (Fig. 4), typically between layers 2 and 3 as described by Drs. Clark and Harryman [36]. Delamination is often used as a surrogate for poor tissue quality, which refers to chronic degenerative changes within the tendon substance that result in a thin or fragile tendon with compromised suture-holding properties [37]. Delamination is reported to occur in 32 to 82% of rotator cuff tears, depending on the definition used [37].
Fig. 4.

Tendon delamination may correlate with decreased chance of tendon healing arthroscopic images from lateral viewing portal demonstrating delamination of the supraspinatus tendon
Dr. Boileau and colleagues have studied the effect of rotator cuff tendon delamination on healing rates extensively. According to their studies, delamination correlates with tear size, retraction, and rotator cuff repair non-healing [37]. Additionally, they found that patient age and delamination of the supraspinatus or infraspinatus were correlated with worse rotator cuff repair healing rates in a prospective study of patients undergoing arthroscopic rotator cuff repair for chronic supraspinatus tears [1].
Whether tendon delamination is an independent risk factor or not is debated. A prospective study of 1043 patients found that delamination was associated with non-healing but, after multivariate analysis, it was not considered to be an independent risk factor [38]. Another study, however, did find delamination to be an independent risk factor [20].
In terms of tissue quality’s role in rotator cuff repair healing, one retrospective study of 55 patients with high grade partial or small full-thickness rotator cuff tears found that increasing tendinopathic changes as assessed on MRI was associated with non-healing [39]. The subjective evaluation of tendon quality by the surgeon at the time of rotator cuff repair is felt by some to correlate with healing, but the influence of this factor is difficult to analyze.
Tendon Retraction and Length
Tendon retraction on imaging may be due to muscle retraction and/or shortening of the residual tendon stump (Fig. 5) [3]. One study found that > 22.2 mm of tendon retraction from the anatomic footprint, along with muscle atrophy, was highly predictive of rotator cuff repair non-healing [20]. Another retrospective study also found tendon retraction to be an independent risk factor for non-healing [31]. It is likely that both muscle retraction and short residual tendon stump length are associated with negative healing outcomes [3]. Meyer and colleagues reported that less than 15 mm of residual tendon length represented a risk factor for non-healing [40].
Fig. 5.
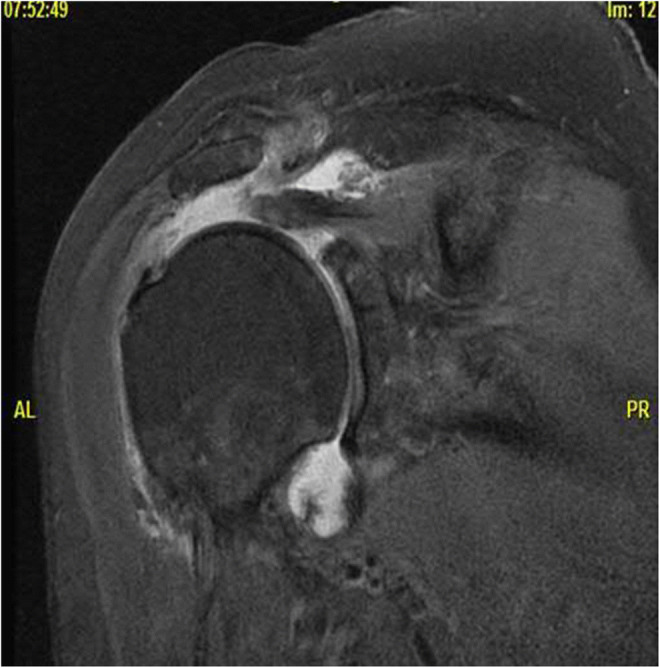
Measurement of residual tendon length. T2 MRI coronal oblique image demonstrating decreased supraspinatus tendon length in the setting of a rotator cuff tear. Note that tendon retraction in and of itself will cause muscle belly cross-sectional area to appear decreased, regardless of the presence of true muscle atrophy, due to the fusiform nature of supraspinatus
Tear Location
The location of tears within the rotator cuff may influence rotator cuff repair healing rates. One study found that isolated supraspinatus tears, without involvement of other cuff tendons, the biceps, or acromioclavicular joint, have better healing rates than those that do involve other structures [41]. Other authors have stated that tears disrupting the rotator cable are at increased risk for non-healing [10]. Additionally, while the majority of rotator cuff tears occur at the bone-tendon interface [4], a rare but notable exception is when the tear instead occurs at the musculotendinous junction. These tears, which are most commonly seen in infraspinatus, rapidly and predictably undergo fatty degeneration and are associated with poor surgical outcomes when repaired primarily [42, 43]. However, tear location has not been evaluated in multivariate studies as an independent risk factor for tendon non-healing.
Shoulder Stiffness
The influence of preoperative and postoperative shoulder stiffness on rotator cuff healing is particularly interesting. Multiple studies have found that patients with preoperative stiffness have equal, or better, healing rates than patients without preoperative stiffness [44, 45, 46•]. Notably, in each of these studies, patients with preoperative stiffness were treated with simultaneous capsular release or manipulation under anesthesia at the same time as rotator cuff repair to regain their postoperative motion [44, 45, 46•]. Regarding postoperative stiffness, one study reported that patients with postoperative stiffness had much higher non-healing rates (89.5%) than those patients without postoperative shoulder stiffness (18.2%) [47]. On the contrary, in a retrospective cohort study of patients who had stiffness preoperatively compared with those that did not, the non-healing rates were actually better in the group of patients with stiffness (2.6%) than the group without stiffness (14.7%) [46•].
Patient-Related Factors
Age
Many studies have evaluated the effect of patient age on rotator cuff repair healing rates, the majority of which have found that age negatively correlates with rotator cuff repair healing [2, 16, 17•, 18, 19, 21, 41, 48•, 49]. A prospective study of patients with large to massive rotator cuff tears evaluated factors that predict reparability, as defined by the intraoperative ability to repair a tear to at least 50% of the anatomic footprint, and found that age correlated with irreparability [16]. A prospective study of 256 rotator cuff repairs in the UK, assessed at 12 months postoperatively by MRI, found that increasing age independently and negatively influenced rotator cuff repair healing rates after controlling for tear size [19]. In an evaluation of 1600 consecutive rotator cuff repairs, all of whom received postoperative US at 6 months, patient age was an independent risk factor on multiple logistic regression analysis, with rotator cuff repair non-healing rates increasing by approximately 5% per decade [48•].
However, a few studies have actually failed to demonstrate that age is an independent risk factor for rotator cuff repair non-healing [15, 27, 30•]. A retrospective review of 177 rotator cuff repair patients who had CTA at 1 year postoperatively found that older patients had worse rotator cuff repair healing rates but, on multivariate analysis, that age was in fact not an independent risk factor [27]. Some have suggested that patient age is perhaps simply a proxy for other negative prognostic factors, and not an independent risk factor per se [3, 30•].
Smoking
Nicotine is a potent vasoconstrictor, decreasing oxygen delivery to soft tissues and bone, and smoking tobacco has been demonstrated to be a risk factor for developing degenerative rotator cuff tears in a dose- and time-dependent manner [50]. Studies have also shown that the severity of rotator cuff tears is greater in smokers than in non-smokers [51].
With respect to rotator cuff repair healing rates, the evidence is conflicting. A retrospective analysis of 249 patients who underwent rotator cuff repair found that non-healing rates were significantly higher in smokers (29.4%) than in a group of non-smokers matched for age, tear size, and fatty degeneration (5.9%) [52]. Another study, which evaluated postoperative outcome scores but not healing rates, found that smokers had worse improvements in ASES score than the non-smoking cohort at 2 years [53]. However, three studies evaluating preoperative predictors of rotator cuff repair healing have concluded that smoking is not correlated with non-healing [21, 32•, 54].
Body Mass Index
Obesity has been associated with fatty degeneration of the rotator cuff, even in the absence of a rotator cuff tear [55], and therefore is thought to potentially be a risk factor for rotator cuff repair non-healing. In a retrospective review of 146 patients who underwent rotator cuff repair, the authors found that patients with a body mass index (BMI) > 30 kg/m2 had greater non-healing rates (28.6%) than those with BMI < 25 kg/m2 (15.8%) as assessed on postoperative US [56]. Additionally, multiple studies that have evaluated clinical outcomes, but not healing rates, have found that obese patients have worse outcomes after rotator cuff repair than non-obese patients [57–59]. However, retrospective review studies with multivariate analyses have at times found that BMI was and at other times was not an independent risk factor for non-healing [16–19].
Diabetes Mellitus
In a retrospective review of 264 patients undergoing rotator cuff repair and postoperative MRI at 3 months, there was no significant difference in non-healing rates between the diabetic (23.3%) and non-diabetic (15.1%) patients [54]. However, this study may have been underpowered with just 30 diabetic patients, all of whom were hospitalized preoperatively for intensive glycemic control [60]. Another retrospective study matched diabetic patients with non-diabetic patients according the patient age, gender, comorbidities, and tear size and found that diabetic patients did not improve as significantly as their non-diabetic matches postoperatively [61]. However, in this study, rotator cuff repair healing was not specifically assessed [61].
Two database studies have evaluated the effect of diabetes mellitus (DM) on rotator cuff repair surgery. In one study, DM was a risk factor for postoperative infection but not for revision surgery [62]. In the other study, DM was a risk factor for requiring rotator cuff repair surgery [63]. However, in neither study were rotator cuff repair healing rates evaluated. In retrospective studies with multivariate analyses, DM has at times been identified as an independent risk factor, and at other times has not, for rotator cuff repair non-healing [17•, 25].
Dyslipidemia
Animal studies have demonstrated that hypercholesterolemia increases fatty degeneration and inhibits tendon healing in a rotator cuff tear model, and that correcting hypercholesterolemia reverses these changes [64]. Therefore, authors have evaluated whether dyslipidemia decreases rotator cuff repair healing rates in humans.
In a retrospective review of 85 patients who had ultrasound evaluation after rotator cuff repair, patients with a diagnosis of dyslipidemia, all of whom were on statins, had much greater risk of non-healing (45.5%) than those without dyslipidemia diagnosis (11.3%) [65]. Similarly, a database study found that rotator cuff repair revision rates were increased in patients with moderate or high total cholesterol levels [66]. However, in this study, the use of statins appeared to be protective of this increased revision surgery risk [66].
Like with many of the patient-related factors, there is conflicting evidence as to whether dyslipidemia is actually an independent risk factor for rotator cuff repair non-healing. A retrospective review of 180 patients who had medium to large rotator cuff repairs and 2-year follow-up with MRI found that dyslipidemia was a significant and independent risk factor [20]; however, another study found that dyslipidemia was not an independent risk factor for rotator cuff repair non-healing on multivariate analysis [30•].
Vitamin D
Vitamin D has been shown to influence bone and tendon healing in general [67] and a study performed on rats found that low vitamin D levels negatively affect early tendon to bone healing in a rotator cuff tear model [68].
In human studies, a low vitamin D level has variably been associated with poor outcomes after rotator cuff repair surgery. In a database study, low vitamin D levels were associated with greater rates of revision rotator cuff repair surgery (5.9%) compared with those with sufficient vitamin D levels (3.7%) [69]. Additionally, a multivariate linear regression analysis demonstrated that a low serum 25-vitamin D level was an independent risk factor for fatty degeneration of the supraspinatus and infraspinatus muscles in patients with full-thickness rotator cuff tears [70].
However, in a retrospective evaluation of 92 consecutive patients who underwent rotator cuff repair and had serum 25-vitamin D levels measured, deficiency was not found to correlate with tear size, extent of retraction, or fatty degeneration [71]. 25-Vitamin D deficiency (< 20 ng/mL) was found in 88% of the patients studied, which may have caused the study to be underpowered. A low serum 25-vitamin D level has not been evaluated as an independent risk factor for rotator cuff repair non-healing.
Osteoporosis
Due to the need for strong tendon-to-bone fixation via suture anchors or alternative devices in bone, authors have evaluated whether osteoporosis and low bone mineral density (BMD) can lead to worse rotator cuff repair healing rates.
In a retrospective review of 272 patients who underwent rotator cuff repair and had tendon healing assessed via US or CTA, low bone mineral density, along with fatty degeneration of infraspinatus and increased tendon retraction, was found to be an independent risk factor for non-healing on multivariate analysis [31]. Additionally, in a large database study, rotator cuff repair revision rates were found to be greater for osteoporotic patients (6.6%) than for non-osteoporotic controls (4.5%) [72]. However, this study did not evaluate rotator cuff repair healing specifically [72].
NSAID Use
Despite the frequent concern over the negative influence of NSAIDs on postoperative tendon healing rates, studies have demonstrated that perioperative NSAID use does not have a deleterious effect on rotator cuff healing [8, 73, 74]. A systematic review did find that postoperative celecoxib use after rotator cuff repair was associated with a greater rate of non-healing (37%) than ibuprofen use (7%), but it did not evaluate causality [74].
Other Factors
Several other patient-related factors may have an influence on rotator cuff repair healing rates but have not been investigated definitively to date. These include malnutrition (low preoperative albumin level), alcoholism, behavioral abnormalities that might lead to poor compliance, bone morphometry (e.g., glenoid inclination, acromion shape and size, critical shoulder angle), hypermobility syndromes (e.g., Ehlers-Danlos syndrome), inflammatory arthritides such as rheumatoid arthritis, use of anticoagulants or platelet inhibitors, and others.
Multiple database studies have evaluated the relationship of steroid injections and rotator cuff repair outcomes and have found that steroid injections prior to rotator cuff repair have an increased risk of requiring revisions surgery compared with matched controls in a dose- and time-dependent manner [75••, 76, 77]. The influence of preoperative steroid injections on rotator cuff repair healing rates has not been assessed.
Future Directions
Recently, researchers have attempted to create predictive models, using the tear- and patient-related factors that are thought to influence rotator cuff healing rates preoperatively, to improve rotator cuff repair non-healing risk stratification.
Dr. Kwon and colleagues performed a retrospective review of 603 patients who underwent arthroscopic rotator cuff repair and had MRI evaluation at 1 year postoperatively. In their cohort, the non-healing rate was 24%. Using multivariate analysis, the authors found that age > 70, increasing tear size in anterior to posterior direction, tendon retraction, infraspinatus fatty degeneration Goutallier grade > 2, low BMD scores, and high work activity level were all independent risk factors for tendon non-healing. Using these risk factors, the authors developed a preoperative scoring system, called the Rotator Cuff Healing Index, which is based on these risk factors and weighted according to their individual risk odds ratios [78].
Similarly, Dr. Jeong and colleagues performed a case-control study of 112 rotator cuff repair patients, 51 of whom did not have successful tendon healing, with MRI evaluation at 9 months postoperatively. While many factors were associated with non-healing on univariate analysis, only supraspinatus muscle atrophy and infraspinatus fatty degeneration were independent risk factors. Using just these two variables, with cutoffs of < 43% for supraspinatus occupation ratio and Goutallier grade ≥ 2 for infraspinatus fatty degeneration, the authors had a sensitivity of 98%, specificity of 83.6%, and accuracy of 90.2% when used on their cohort for predicting rotator cuff non-healing [30•].
Although neither of these predictive models have yet been prospectively validated, they represent an important step forward in using this wealth of information to appropriately counsel individual patients on their personal risk of non-healing after rotator cuff repair surgery. Future validation studies with large patient cohorts will hopefully confirm the accuracy of these tools.
Conclusions
Many tear- and patient-related factors have been implicated as risk factors for rotator cuff tear irreparability and rotator cuff repair non-healing. Factors such as tear size, fatty degeneration, muscle atrophy, and tendon retraction have been clearly identified as independent risk factors, while the evidence to date regarding other factors is conflicting (Table 3). The relative influence of these factors on rotator cuff repair non-healing deserves further investigations. Predictive models of rotator cuff healing, based on these factors, have recently been developed that may help surgeons better individualize preoperative consultation with their patients.
Table 3.
Tear- and patient-related risk factors for rotator cuff repair non-healing
| Tear-related factor | Evidence | Patient-related factor | Evidence |
|---|---|---|---|
| Tear size | Supportive evidence, multiple studies | Increased age | Conflicting evidence |
| Fatty degeneration | Supportive evidence, multiple studies | Smoking | Conflicting evidence |
| Suprascapular neuropathy | Not evaluated as an independent risk factor | BMI | Conflicting evidence |
| Muscle atrophy | Supportive evidence, multiple studies | DM | Conflicting evidence |
| Tendon delamination | Conflicting evidence | Dyslipidemia | Conflicting evidence |
| Tendon retraction | Supportive evidence, few studies | Low Serum Vitamin D | Not evaluated as an independent risk factor |
| Tear location | Not evaluated as an independent risk factor | Osteoporosis | Supportive evidence, few studies |
| Stiffness (preop) | Protective, few studies | NSAID use | No supportive evidence |
Compliance with Ethical Standards
Conflict of Interest
Andrew Jensen and Adam Taylor declare that they have no conflicts of interest. Joaquin Sanchez-Sotelo reports receiving research grants and royalties from Stryker, consulting fees from Wright Medical and Exactech, speaking engagement fees from Wright Medical and Acumed, publication royalties from Elsevier and Oxford University Press, and is a board member for ASES and an associate editor for JSES JOT and JSEA.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Surgical Management of Massive Irreparable Cuff Tears
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Andrew R. Jensen, Email: Jensen.Andrew@mayo.edu
Adam J. Taylor, Email: ATaylor4@dhs.lacounty.gov
Joaquin Sanchez-Sotelo, Email: Sanchezsotelo.Joaquin@mayo.edu.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87(6):1229–1240. doi: 10.2106/00004623-200506000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Cho NS, Rhee YG. The factors affecting the clinical outcome and integrity of arthroscopically repaired rotator cuff tears of the shoulder. Clin Orthop Surg. 2009;1(2):96–104. doi: 10.4055/cios.2009.1.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abtahi AM, Granger EK, Tashjian RZ. Factors affecting healing after arthroscopic rotator cuff repair. World J Orthop. 2015;6(2):211–220. doi: 10.5312/wjo.v6.i2.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sanchez-Sotelo J. Mayo Clinic principles of shoulder surgery. New York: Oxford University Press; 2018. [Google Scholar]
- 5.McElvany MD, McGoldrick E, Gee AO, Neradilek MB, Matsen FA., 3rd Rotator cuff repair: published evidence on factors associated with repair integrity and clinical outcome. Am J Sports Med. 2015;43(2):491–500. doi: 10.1177/0363546514529644. [DOI] [PubMed] [Google Scholar]
- 6.Charousset C, Bellaiche L, Kalra K, Petrover D. Arthroscopic repair of full-thickness rotator cuff tears: is there tendon healing in patients aged 65 years or older? Arthroscopy. 2010;26(3):302–309. doi: 10.1016/j.arthro.2009.08.027. [DOI] [PubMed] [Google Scholar]
- 7.Burnier M, Elhassan BT, Sanchez-Sotelo J. Surgical management of irreparable rotator cuff tears: what works, what does not, and what is coming. J Bone Joint Surg Am. 2019;101(17):1603–1612. doi: 10.2106/JBJS.18.01392. [DOI] [PubMed] [Google Scholar]
- 8.Mall NA, Tanaka MJ, Choi LS, Paletta GA., Jr Factors affecting rotator cuff healing. J Bone Joint Surg Am. 2014;96(9):778–788. doi: 10.2106/JBJS.M.00583. [DOI] [PubMed] [Google Scholar]
- 9.Prickett WD, Teefey SA, Galatz LM, Calfee RP, Middleton WD, Yamaguchi K. Accuracy of ultrasound imaging of the rotator cuff in shoulders that are painful postoperatively. J Bone Joint Surg Am. 2003;85(6):1084–1089. doi: 10.2106/00004623-200306000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Ladermann A, Denard PJ, Collin P. Massive rotator cuff tears: definition and treatment. Int Orthop. 2015;39(12):2403–2414. doi: 10.1007/s00264-015-2796-5. [DOI] [PubMed] [Google Scholar]
- 11.Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990;254:81–86. doi: 10.1097/00003086-199005000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Collin P, Matsumura N, Ladermann A, Denard PJ, Walch G. Relationship between massive chronic rotator cuff tear pattern and loss of active shoulder range of motion. J Shoulder Elb Surg. 2014;23(8):1195–1202. doi: 10.1016/j.jse.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 13.Bishop J, Klepps S, Lo IK, Bird J, Gladstone JN, Flatow EL. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elb Surg. 2006;15(3):290–299. doi: 10.1016/j.jse.2005.09.017. [DOI] [PubMed] [Google Scholar]
- 14.Gasbarro G, Ye J, Newsome H, Jiang K, Wright V, Vyas D, et al. Morphologic risk factors in predicting symptomatic structural failure of arthroscopic rotator cuff repairs: tear size, location, and atrophy matter. Arthroscopy. 2016;32(10):1947–1952. doi: 10.1016/j.arthro.2016.01.067. [DOI] [PubMed] [Google Scholar]
- 15.Gwark JY, Sung CM, Na JB, Park HB. Outcomes of arthroscopic rotator cuff repair in patients who are 70 years of age or older versus under 70 years of age: a sex- and tear size-matched case-control study. Arthroscopy. 2018;34(7):2045–2053. doi: 10.1016/j.arthro.2018.02.047. [DOI] [PubMed] [Google Scholar]
- 16.Kuptniratsaikul V, Laohathaimongkol T, Umprai V, Yeekian C, Prasathaporn N. Pre-operative factors correlated with arthroscopic reparability of large-to-massive rotator cuff tears. BMC Musculoskelet Disord. 2019;20(1):111. doi: 10.1186/s12891-019-2485-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee YS, Jeong JY, Park CD, Kang SG, Yoo JC. Evaluation of the risk factors for a rotator cuff retear after repair surgery. Am J Sports Med. 2017;45(8):1755–1761. doi: 10.1177/0363546517695234. [DOI] [PubMed] [Google Scholar]
- 18.Park JS, Park HJ, Kim SH, Oh JH. Prognostic factors affecting rotator cuff healing after arthroscopic repair in small to medium-sized tears. Am J Sports Med. 2015;43(10):2386–2392. doi: 10.1177/0363546515594449. [DOI] [PubMed] [Google Scholar]
- 19.Rashid MS, Cooper C, Cook J, Cooper D, Dakin SG, Snelling S, et al. Increasing age and tear size reduce rotator cuff repair healing rate at 1 year. Acta Orthop. 2017;88(6):606–611. doi: 10.1080/17453674.2017.1370844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim YK, Jung KH, Kim JW, Kim US, Hwang DH. Factors affecting rotator cuff integrity after arthroscopic repair for medium-sized or larger cuff tears: a retrospective cohort study. J Shoulder Elb Surg. 2018;27(6):1012–1020. doi: 10.1016/j.jse.2017.11.016. [DOI] [PubMed] [Google Scholar]
- 21.Tashjian RZ, Hollins AM, Kim HM, Teefey SA, Middleton WD, Steger-May K, et al. Factors affecting healing rates after arthroscopic double-row rotator cuff repair. Am J Sports Med. 2010;38(12):2435–2442. doi: 10.1177/0363546510382835. [DOI] [PubMed] [Google Scholar]
- 22.Cvetanovich GL, Waterman BR, Verma NN, Romeo AA. Management of the irreparable rotator cuff tear. J Am Acad Orthop Surg. 2019. 10.5435/JAAOS-D-18-00199. [DOI] [PubMed]
- 23.Jensen AR, Kelley BV, Mosich GM, Ariniello A, Eliasberg CD, Vu B, et al. Neer Award 2018: platelet-derived growth factor receptor alpha co-expression typifies a subset of platelet-derived growth factor receptor beta-positive progenitor cells that contribute to fatty degeneration and fibrosis of the murine rotator cuff. J Shoulder Elb Surg. 2018;27(7):1149–1161. doi: 10.1016/j.jse.2018.02.040. [DOI] [PubMed] [Google Scholar]
- 24.Deniz G, Kose O, Tugay A, Guler F, Turan A. Fatty degeneration and atrophy of the rotator cuff muscles after arthroscopic repair: does it improve, halt or deteriorate? Arch Orthop Trauma Surg. 2014;134(7):985–990. doi: 10.1007/s00402-014-2009-5. [DOI] [PubMed] [Google Scholar]
- 25.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83. doi: 10.1097/00003086-199407000-00014. [DOI] [PubMed] [Google Scholar]
- 26.Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elb Surg. 1999;8(6):599–605. doi: 10.1016/S1058-2746(99)90097-6. [DOI] [PubMed] [Google Scholar]
- 27.Oh JH, Kim SH, Kang JY, Oh CH, Gong HS. Effect of age on functional and structural outcome after rotator cuff repair. Am J Sports Med. 2010;38(4):672–678. doi: 10.1177/0363546509352460. [DOI] [PubMed] [Google Scholar]
- 28.Collin P, Thomazeau H, Walch G, Gerber C, Mansat P, Favard L, et al. Clinical and structural outcome twenty years after repair of isolated supraspinatus tendon tears. J Shoulder Elb Surg. 2019;28(1):196–202. doi: 10.1016/j.jse.2018.07.023. [DOI] [PubMed] [Google Scholar]
- 29.Iijima Y, Matsuki K, Hoshika S, Ueda Y, Hamada H, Tokai M, et al. Relationship between postoperative retear and preoperative fatty degeneration in large and massive rotator cuff tears: quantitative analysis using T2 mapping. J Shoulder Elb Surg. 2019;28(8):1562–1567. doi: 10.1016/j.jse.2019.04.036. [DOI] [PubMed] [Google Scholar]
- 30.Jeong HY, Kim HJ, Jeon YS, Rhee YG. Factors predictive of healing in large rotator cuff tears: is it possible to predict retear preoperatively? Am J Sports Med. 2018;46(7):1693–1700. doi: 10.1177/0363546518762386. [DOI] [PubMed] [Google Scholar]
- 31.Chung SW, Oh JH, Gong HS, Kim JY, Kim SH. Factors affecting rotator cuff healing after arthroscopic repair: osteoporosis as one of the independent risk factors. Am J Sports Med. 2011;39(10):2099–2107. doi: 10.1177/0363546511415659. [DOI] [PubMed] [Google Scholar]
- 32.Raman J, Walton D, MacDermid JC, Athwal GS. Predictors of outcomes after rotator cuff repair-a meta-analysis. J Hand Ther. 2017;30(3):276–292. doi: 10.1016/j.jht.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 33.Shi LL, Boykin RE, Lin A, Warner JJ. Association of suprascapular neuropathy with rotator cuff tendon tears and fatty degeneration. J Shoulder Elb Surg. 2014;23(3):339–346. doi: 10.1016/j.jse.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 34.Kong BY, Kim SH, Kim DH, Joung HY, Jang YH, Oh JH. Suprascapular neuropathy in massive rotator cuff tears with severe fatty degeneration in the infraspinatus muscle. Bone Joint J. 2016;98-b(11):1505–1509. doi: 10.1302/0301-620X.98B11.37928. [DOI] [PubMed] [Google Scholar]
- 35.Kissenberth MJ, Rulewicz GJ, Hamilton SC, Bruch HE, Hawkins RJ. A positive tangent sign predicts the repairability of rotator cuff tears. J Shoulder Elb Surg. 2014;23(7):1023–1027. doi: 10.1016/j.jse.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 36.Clark JM, Harryman DT., 2nd Tendons, ligaments, and capsule of the rotator cuff. Gross and microscopic anatomy. J Bone Joint Surg Am. 1992;74(5):713–725. doi: 10.2106/00004623-199274050-00010. [DOI] [PubMed] [Google Scholar]
- 37.Boileau P, Andreani O, Schramm M, Baba M, Barret H, Chelli M. The effect of tendon delamination on rotator cuff healing. Am J Sports Med. 2019;47(5):1074–1081. doi: 10.1177/0363546519835491. [DOI] [PubMed] [Google Scholar]
- 38.Kwon J, Lee YH, Kim SH, Ko JH, Park BK, Oh JH. Delamination does not affect outcomes after arthroscopic rotator cuff repair as compared with nondelaminated rotator cuff tears: a study of 1043 consecutive cases. Am J Sports Med. 2019;47(3):674–681. doi: 10.1177/0363546518817764. [DOI] [PubMed] [Google Scholar]
- 39.Chung SW, Kim JY, Yoon JP, Lyu SH, Rhee SM, Oh SB. Arthroscopic repair of partial-thickness and small full-thickness rotator cuff tears: tendon quality as a prognostic factor for repair integrity. Am J Sports Med. 2015;43(3):588–596. doi: 10.1177/0363546514561004. [DOI] [PubMed] [Google Scholar]
- 40.Meyer DC, Wieser K, Farshad M, Gerber C. Retraction of supraspinatus muscle and tendon as predictors of success of rotator cuff repair. Am J Sports Med. 2012;40(10):2242–2247. doi: 10.1177/0363546512457587. [DOI] [PubMed] [Google Scholar]
- 41.Nho SJ, Brown BS, Lyman S, Adler RS, Altchek DW, MacGillivray JD. Prospective analysis of arthroscopic rotator cuff repair: prognostic factors affecting clinical and ultrasound outcome. J Shoulder Elb Surg. 2009;18(1):13–20. doi: 10.1016/j.jse.2008.05.045. [DOI] [PubMed] [Google Scholar]
- 42.Lunn JV, Castellanos-Rosas J, Tavernier T, Barthelemy R, Walch G. A novel lesion of the infraspinatus characterized by musculotendinous disruption, edema, and late fatty infiltration. J Shoulder Elb Surg. 2008;17(4):546–553. doi: 10.1016/j.jse.2007.11.016. [DOI] [PubMed] [Google Scholar]
- 43.Millett PJ, Hussain ZB, Fritz EM, Warth RJ, Katthagen JC, Pogorzelski J. Rotator cuff tears at the musculotendinous junction: classification and surgical options for repair and reconstruction. Arthrosc Tech. 2017;6(4):e1075–e1e85. doi: 10.1016/j.eats.2017.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McGrath JP, Lam PH, Tan MT, Murrell GA. The effect of concomitant glenohumeral joint capsule release during rotator cuff repair--a comparative study. J Shoulder Elb Surg. 2016;25(5):714–722. doi: 10.1016/j.jse.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 45.Zhang K, de Sa D, Kanakamedala A, Sheean AJ, Vyas D. Management of concomitant preoperative rotator cuff pathology and adhesive capsulitis: a systematic review of indications, treatment approaches, and outcomes. Arthroscopy. 2019;35(3):979–993. doi: 10.1016/j.arthro.2018.10.126. [DOI] [PubMed] [Google Scholar]
- 46.Kim IB, Jung DW. A rotator cuff tear concomitant with shoulder stiffness is associated with a lower retear rate after 1-stage arthroscopic surgery. Am J Sports Med. 2018;46(8):1909–1918. doi: 10.1177/0363546518768813. [DOI] [PubMed] [Google Scholar]
- 47.Chung SW, Huong CB, Kim SH, Oh JH. Shoulder stiffness after rotator cuff repair: risk factors and influence on outcome. Arthroscopy. 2013;29(2):290–300. doi: 10.1016/j.arthro.2012.08.023. [DOI] [PubMed] [Google Scholar]
- 48.Diebold G, Lam P, Walton J, Murrell GAC. Relationship between age and rotator cuff retear: a study of 1,600 consecutive rotator cuff repairs. J Bone Joint Surg Am. 2017;99(14):1198–1205. doi: 10.2106/JBJS.16.00770. [DOI] [PubMed] [Google Scholar]
- 49.Shim SB, Jeong JY, Yum TH, Yoo JC. A comparative study to evaluate the risk factors for medium-sized rotator cuff tear in patients younger than 50 years of age. Arthroscopy. 2018;34(11):2971–2979. doi: 10.1016/j.arthro.2018.06.031. [DOI] [PubMed] [Google Scholar]
- 50.Baumgarten KM, Gerlach D, Galatz LM, Teefey SA, Middleton WD, Ditsios K, et al. Cigarette smoking increases the risk for rotator cuff tears. Clin Orthop Relat Res. 2010;468(6):1534–1541. doi: 10.1007/s11999-009-0781-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Djerbi I, Chammas M, Mirous MP, Lazerges C, Coulet B. Impact of cardiovascular risk factor on the prevalence and severity of symptomatic full-thickness rotator cuff tears. Orthop Traumatol Surg Res. 2015;101(6 Suppl):S269–S273. doi: 10.1016/j.otsr.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 52.Park JH, Oh KS, Kim TM, Kim J, Yoon JP, Kim JY, et al. Effect of smoking on healing. Am J Sports Med. 2018;46(12):2960–8. 10.1177/0363546518789691. [DOI] [PubMed]
- 53.Naimark M, Robbins CB, Gagnier JJ, Landfair G, Carpenter J, Bedi A, et al. Impact of smoking on patient outcomes after arthroscopic rotator cuff repair. BMJ Open Sport Exerc Med. 2018;4(1):e000416. doi: 10.1136/bmjsem-2018-000416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nho SJ, Shindle MK, Adler RS, Warren RF, Altchek DW, MacGillivray JD. Prospective analysis of arthroscopic rotator cuff repair: subgroup analysis. J Shoulder Elb Surg. 2009;18(5):697–704. doi: 10.1016/j.jse.2008.11.018. [DOI] [PubMed] [Google Scholar]
- 55.Matson AP, Kim C, Bajpai S, Green CL, Hash TW, Garrigues GE. The effect of obesity on fatty infiltration of the rotator cuff musculature in patients without rotator cuff tears. Should Elb. 2019;11(1 Suppl):30–38. doi: 10.1177/1758573217736008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ateschrang A, Eggensperger F, Ahrend MD, Schroter S, Stockle U, Kraus TM. Obesity causes poorer clinical results and higher re-tear rates in rotator cuff repair. Arch Orthop Trauma Surg. 2018;138(6):835–842. doi: 10.1007/s00402-018-2921-1. [DOI] [PubMed] [Google Scholar]
- 57.Kessler KE, Robbins CB, Bedi A, Carpenter JE, Gagnier JJ, Miller BS. Does increased body mass index influence outcomes after rotator cuff repair? Arthroscopy. 2018;34(3):754–761. doi: 10.1016/j.arthro.2017.08.248. [DOI] [PubMed] [Google Scholar]
- 58.Namdari S, Baldwin K, Glaser D, Green A. Does obesity affect early outcome of rotator cuff repair? J Shoulder Elb Surg. 2010;19(8):1250–1255. doi: 10.1016/j.jse.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 59.Warrender WJ, Brown OL, Abboud JA. Outcomes of arthroscopic rotator cuff repairs in obese patients. J Shoulder Elb Surg. 2011;20(6):961–967. doi: 10.1016/j.jse.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 60.Miyatake K, Takeda Y, Fujii K, Suzue N, Kawasaki Y, Omichi Y, et al. Comparable clinical and structural outcomes after arthroscopic rotator cuff repair in diabetic and non-diabetic patients. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3810–3817. doi: 10.1007/s00167-018-4994-3. [DOI] [PubMed] [Google Scholar]
- 61.Clement ND, Hallett A, MacDonald D, Howie C, McBirnie J. Does diabetes affect outcome after arthroscopic repair of the rotator cuff? J Bone Joint Surg (Br) 2010;92(8):1112–1117. doi: 10.1302/0301-620X.92B8.23571. [DOI] [PubMed] [Google Scholar]
- 62.Cancienne JM, Deasey MJ, Kew ME, Werner BC. The association of perioperative glycemic control with adverse outcomes within 6 months after arthroscopic rotator cuff repair. Arthroscopy. 2019;35(6):1771–1778. doi: 10.1016/j.arthro.2019.01.035. [DOI] [PubMed] [Google Scholar]
- 63.Huang SW, Wang WT, Chou LC, Liou TH, Chen YW, Lin HW. Diabetes mellitus increases the risk of rotator cuff tear repair surgery: a population-based cohort study. J Diabetes Complicat. 2016;30(8):1473–1477. doi: 10.1016/j.jdiacomp.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 64.Chung SW, Park H, Kwon J, Choe GY, Kim SH, Oh JH. Effect of hypercholesterolemia on fatty infiltration and quality of tendon-to-bone healing in a rabbit model of a chronic rotator cuff tear: electrophysiological, biomechanical, and histological analyses. Am J Sports Med. 2016;44(5):1153–1164. doi: 10.1177/0363546515627816. [DOI] [PubMed] [Google Scholar]
- 65.Garcia GH, Liu JN, Wong A, Cordasco F, Dines DM, Dines JS, et al. Hyperlipidemia increases the risk of retear after arthroscopic rotator cuff repair. J Shoulder Elb Surg. 2017;26(12):2086–2090. doi: 10.1016/j.jse.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 66.Cancienne JM, Brockmeier SF, Rodeo SA, Werner BC. Perioperative serum lipid status and statin use affect the revision surgery rate after arthroscopic rotator cuff repair. Am J Sports Med. 2017;45(13):2948–2954. doi: 10.1177/0363546517717686. [DOI] [PubMed] [Google Scholar]
- 67.Dougherty KA, Dilisio MF, Agrawal DK. Vitamin D and the immunomodulation of rotator cuff injury. J Inflamm Res. 2016;9:123–131. doi: 10.2147/JIR.S106206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Angeline ME, Ma R, Pascual-Garrido C, Voigt C, Deng XH, Warren RF, et al. Effect of diet-induced vitamin D deficiency on rotator cuff healing in a rat model. Am J Sports Med. 2014;42(1):27–34. doi: 10.1177/0363546513505421. [DOI] [PubMed] [Google Scholar]
- 69.Cancienne JM, Brockmeier SF, Kew ME, Werner BC. Perioperative serum 25-hydroxyvitamin d levels affect revision surgery rates after arthroscopic rotator cuff repair. Arthroscopy. 2019;35(3):763–769. doi: 10.1016/j.arthro.2018.09.032. [DOI] [PubMed] [Google Scholar]
- 70.Oh JH, Kim SH, Kim JH, Shin YH, Yoon JP, Oh CH. The level of vitamin D in the serum correlates with fatty degeneration of the muscles of the rotator cuff. J Bone Joint Surg (Br) 2009;91(12):1587–1593. doi: 10.1302/0301-620X.91B12.22481. [DOI] [PubMed] [Google Scholar]
- 71.Ryu KJ, Kim BH, Lee Y, Dan J, Kim JH. Low serum vitamin d is not correlated with the severity of a rotator cuff tear or retear after arthroscopic repair. Am J Sports Med. 2015;43(7):1743–1750. doi: 10.1177/0363546515578101. [DOI] [PubMed] [Google Scholar]
- 72.Cancienne JM, Brockmeier SF, Kew ME, Deasey MJ, Werner BC. The association of osteoporosis and bisphosphonate use with revision shoulder surgery after rotator cuff repair. Arthroscopy. 2019;35(8):2314–2320. doi: 10.1016/j.arthro.2019.03.036. [DOI] [PubMed] [Google Scholar]
- 73.Duchman KR, Lemmex DB, Patel SH, Ledbetter L, Garrigues GE, Riboh JC. The effect of non-steroidal anti-inflammatory drugs on tendon-to-bone healing: a systematic review with subgroup meta-analysis. Iowa Orthop J. 2019;39(1):107–119. [PMC free article] [PubMed] [Google Scholar]
- 74.Constantinescu DS, Campbell MP, Moatshe G, Vap AR. Effects of perioperative nonsteroidal anti-inflammatory drug administration on soft tissue healing: a systematic review of clinical outcomes after sports medicine orthopaedic surgery procedures. Orthop J Sports Med. 2019;7(4):2325967119838873. doi: 10.1177/2325967119838873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Weber AE, Trasolini NA, Mayer EN, Essilfie A, Vangsness CT, Jr, Gamradt SC, et al. Injections prior to rotator cuff repair are associated with increased rotator cuff revision rates. Arthroscopy. 2019;35(3):717–724. doi: 10.1016/j.arthro.2018.10.116. [DOI] [PubMed] [Google Scholar]
- 76.Traven SA, Brinton D, Simpson KN, Adkins Z, Althoff A, Palsis J, et al. Preoperative shoulder injections are associated with increased risk of revision rotator cuff repair. Arthroscopy. 2019;35(3):706–713. doi: 10.1016/j.arthro.2018.10.107. [DOI] [PubMed] [Google Scholar]
- 77.Desai VS, Camp CL, Boddapati V, Dines JS, Brockmeier SF, Werner BC. Increasing numbers of shoulder corticosteroid injections within a year preoperatively may be associated with a higher rate of subsequent revision rotator cuff surgery. Arthroscopy. 2019;35(1):45–50. doi: 10.1016/j.arthro.2018.07.043. [DOI] [PubMed] [Google Scholar]
- 78.Kwon J, Kim SH, Lee YH, Kim TI, Oh JH. The rotator cuff healing index: a new scoring system to predict rotator cuff healing after surgical repair. Am J Sports Med. 2019;47(1):173–180. doi: 10.1177/0363546518810763. [DOI] [PubMed] [Google Scholar]