Abstract
Severe acute respiratory syndrome coronavirus-2 and the related coronavirus disease-19 (COVID-19) is a worldwide emerging situation, which was initially reported in December 2019 in Wuhan, China. Currently, more than 7258842 new cases, and more than 411879 deaths have been reported globally. This new highly transmitted coronavirus is responsible for the development of severe acute respiratory distress syndrome. Due to this disorder, a great number of patients are hospitalized in the intensive care unit followed by connection to extracorporeal membrane oxygenation for breath supporting and survival. Severe acute respiratory distress syndrome is mostly accompanied by the secretion of proinflammatory cytokines, including interleukin (IL)-2, IL-6, IL-7, granulocyte colony-stimulating factor (GSCF), interferon-inducible protein 10 (IP10), monocyte chemotactic protein-1 (MCP1), macrophage inflammatory protein 1A (MIP1A), and tumor necrosis factor alpha (TNF-α), an event which is known as “cytokine storm”. Further disease pathology involves a generalized modulation of immune responses, leading to fatal multiorgan failure. Currently, no specific treatment or vaccination against severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has been developed. Mesenchymal stromal cells (MSCs), which are known for their immunosuppressive actions, could be applied as an alternative co-therapy in critically-ill COVID-19 patients. Specifically, MSCs can regulate the immune responses through the conversion of Th1 to Th2, activation of M2 macrophages, and modulation of dendritic cells maturation. These key immunoregulatory properties of MSCs may be exerted either by produced soluble factors or by cell-cell contact interactions. To date, several clinical trials have been registered to assess the safety, efficacy, and therapeutic potential of MSCs in COVID-19. Moreover, MSC treatment may be effective for the reversion of ground-glass opacity of damaged lungs and reduce the tissue fibrosis. Taking into account the multifunctional properties of MSCs, the proposed stem-cell-based therapy may be proven significantly effective in critically-ill COVID-19 patients. The current therapeutic strategy may improve the patient’s overall condition and in parallel may decrease the mortality rate of the current disease.
Keywords: SARS-CoV-2, COVID-19, Respiratory syndrome, Cytokine storm, Mesenchymal stromal cells, Immunoregulation, Lungs, Th2 response, Dendritic cells, Natural killer cells
Core tip: In this review, the therapeutic potential of mesenchymal stromal cells (MSCs) towards coronavirus disease-19 (COVID-19), will be highlighted. Importantly, MSCs exert key immunoregulatory/immunosuppressive properties that can alter significantly the immune responses. Also, MSCs share regenerative abilities, reducing in this way the lung tissue damage. These unique MSCs features, which may significantly improve the overall condition of COVID-19 patients, will be presented in the following article.
INTRODUCTION
In December 2019, a new highly transmitted coronavirus, which was provisionally named 2019-novel coronavirus, was spread in Wuhan, China[1]. In March 2020, the International Committee on Taxonomy of Viruses (ICTV) has renamed it as severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2)[2]. The zoonotic transmission in a seafood market of Wuhan is speculated until now as the initial route of transmission to humans[2,3]. By the time that this publication is prepared, more than 7258842 cases have been reported, and more than 411879 deaths have been occurred worldwide. Due to the global transmission of SARS-CoV-2, the World Health Organization recognized it as a serious public health issue and in January 2020 declared coronavirus disease-19 (COVID-19) as pandemic[1]. Despite the fact that China was initially affected by COVID-19, accounting more than 80000 cases and 77000 deaths, the United States is now the leading country in confirmed SARS-CoV-2 cases[4]. It is estimated that more than 1979893 people have been infected in the United States[4]. The European Union, Italy, and Spain have been stricken hard by COVID-19, accounting for more than 32500 deaths[4].
Epidemiological studies have shown that SARS-CoV-2 infection and disease severity vary between the two genders. Currently, it has been reported that males are more susceptible to COVID-19 infection than females[5,6]. In addition, SARS-CoV-2 can affect all group ages, while 15% of patients may suffer from the severe form of this disorder[3]. Moreover, the probability for severe disorder occurrence increases dramatically in those aged over 65 years[3,5,7]. The average mortality of COVID-19 is under 3%, however, in highly affected countries such as Italy, Spain and France, the mortality rate may exceed 6%[4]. Additionally, mortality rate can be varied and is dependent on underlying disease and age[3]. Recently, a mortality rate of 10%-27% was reported in patients aged over 85 years, 3%-11% in ages of 65-84 years, 1%-3% in ages of 55-64 years, and below 1% in ages of 20-54 years[3,5,7].
SARS-CoV-2 is responsible for inducing severe acute respiratory distress syndrome (ARDS) in infected patients, which promotes further lung damage and tissue fibrosis[8,9]. Its pathophysiology is related with elevated levels of inflammatory cytokines such as IL-2, IL-6, IL-7, GSCF, IP10, MCP1, MIP1A, and TNF-α, an event which is known as “cytokine storm”[9-11]. Except for lung damage, SARS-CoV-2 may infiltrate other organs such as heart, kidney, and brain, causing cardiomyopathy, arrhythmias, kidney failure, and encephalitis, respectively[3,12,13]. Also, the placental transmission of SARS-CoV-2 from mothers to their fetuses is currently being investigated[13,14]. In the study of Schwartz[13], no SARS-CoV-2 intrauterine transmission from infected mothers to their fetuses was reported. Additionally, no maternal deaths from SARS-CoV-2 has been reported to date, which is in contrast to previous related viruses such as SARS and Middle East respiratory syndrome (MERS)[13-15].
Until now, several treatments have been tested, including prophylactic hydroxychloroquine and colchicine administration, antiviral agents, monoclonal antibodies against SARS-CoV-2, and transfusion of convalescent plasma[16-19]. The majority of the above treatments have Food and Drug Administration (FDA) approval for their application to other diseases, while their use in COVID-19 patients is still under investigation. Remdesivir, an experimental drug to treat Ebola, has been tested in clinical trials for its efficacy in SARS-CoV-2 infection, while globally a great effort has been performed for the production of satisfactory vaccines against the current virus[19-24]. Recently, remdesivir was approved by the FDA for application in COVID-19 patients.
Knowing that COVID-19 can cause significant modifications to the patient’s immune system, alternative strategies should also be tested. In this way, the mesenchymal stromal cells (MSCs), a mesodermal cellular population originated mostly from bone marrow (BM), Wharton’s Jelly tissue (WJ-tissue), and adipose tissue (AT), could be potentially applied in COVID-19 patients[25-28]. MSCs are known for their immunoregulatory/immunosuppressive properties, which are exerted in several ways[25]. MSCs are currently applied in severe autoimmune disorders such as multiple sclerosis (MS), amyotrophic lateral sclerosis (ALS), Crohn’s disease, diabetes mellitus, etc., thus reducing disease manifestations[29]. In this way, MSCs can be applied mostly as cotherapy in combination with the above pharmaceutical agents to reverse the severe manifestations induced by SARS-CoV-2 infections. In this review, we will highlight the specific immunomodulation aspects of MSCs and their potential application in patients infected by SARS-CoV-2. Furthermore, the immune response against COVID-19, MSCs origin, immunoregulatory properties, and their possible application in COVID-19 will be presented. For the purposes of the current review article, we searched initially over 300 published articles focused on COVID-19 pathogenesis and MSC biology. During the eligibility process, 166 studies were excluded and the remaining 134 articles were finally included in this review. Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram describes the methodological framework that was followed in the current article (Supplementary Figure 1). Based on the above data, the scientific community might consider the broad use of MSCs in critically ill patients, improving their overall condition.
INVASION MECHANISM OF SARS-COV-2
SARS-CoV-2, according to the ICTV, is placed within the Coronaviridae and specifically is a member of the subgenus Sarbecovirus[2,30]. SARS-CoV-2 consists of four structural proteins, spike (S), envelope (E), membrane (M), and nucleocapsid (N), and its diameter is approximately 50-150 nm[31,32]. It is a positive-sense single-stranded RNA virus (++ssRNA), while its genome contains 29903 bases[33]. The use of molecular methods has revealed that SARS-CoV-2 (Genbank accession No. NC_045512) is similar to bat -SL-CoVZC45 (88% similarity, Genbank accession No. MG772933.1) and bat-SL-CoVZXC21 (89% similarity, Genbank accession No. MG772934.1)[33-35]. Also, it is related more with the original SARS-CoV (80% similarity, Genbank accession No. FJ588686) than the MERS coronavirus (MERS-CoV, 50% similarity, Genbank accession No. NC_019843)[36].
The infection of SARS-CoV-2 begins with its proper adaption to the angiotensin I converting enzyme 2 receptor (ACE2), a process where the S protein is involved[17]. Zhou et al[37] showed with the use of reverse genetics that ACE2 is the main receptor that SARS-CoV-2 uses for its fusion with the cellular membrane. Moreover, Wrapp et al[38,39] showed that SARS-CoV-2 can bind ACE2 with higher affinity than the original SARS-CoV. Furthermore, the entrance of the virus to host cells is performed by the S protein primed by transmembrane protease serine 2 (TMPRSS2)[40]. TMPRSS2 is a cysteine-rich protease domain, and its expression is regulated by androgenic hormones[41]. Overexpression of TMPRSS2 is mostly observed in prostate cancer[41]. Its relation with the pathophysiological mechanism of SARS-Cov-2 led researchers to associate possibly its function with lung damage severity and tumorigenesis.
ACE2 and TMPRSS2 are mostly found in alveolar type II cells[42]. Additionally, capillary endothelial cells (ECs) of other tissues such as heart, liver, kidney, and intestine also express the above proteins[43]. For this reason, patients suffering from COVID-19, besides pneumonia, which is the most common manifestation, may exhibit other disorders such as cardiomyopathy, impaired liver and kidney function, and encephalitis.
IMMUNE SYSTEM AND COVID-19
After the infiltration of SARS-CoV-2 to the host cells, a specific series of events occur. COVID-19 is characterized by three-phase immunopathology, where the patient’s immune system has a central role. Among patients, fever (92.8% of the patients), cough (69.8%), dyspnea (34.5%), myalgia (27%), headache (7%), and diarrhea (6%) were the most common symptoms[3]. Additionally, there is an increasing tendency that younger persons (ages < 20-years-old) can be asymptomatic carriers of SARS-CoV-2, who can transmit effectively the virus to others[5,7].
The first phase is the incubation – non-severe stage, where the virus is recognized by the immune system[5,44]. In this way, the innate immune response is performed to limit the virus infection. If the virus escapes the host’s defense, then the second phase is initiated[44,45]. For this reason, immunocompromised patients or patients with underlying disorders characterized by impaired immune function, may have increased probabilities for severe disease occurrence. Chen et al[5] showed that the most common underlying diseases, which were related with the severe outcome, were cardiovascular disease, hypertension, and diabetes mellitus.
In the second phase, the virus induces severe damage to the infected cells through its replication cycle[46]. This event leads to the activation of dendritic cells (DCs), epithelial cells, and macrophages, which are producing IL-1β, IL-2, IL-6, IL-8, interferon (IFN)-α/β, TNF-α, C-C motif chemokine 3 (CCL3), CCL5, CCL2, and IP-10. These inflammatory molecules can efficiently stimulate T helper cell (Th)1, Th2, and Th17 responses. Indeed, the overactivation of CXCR3+CD4+ T cells, CXCR3+CD8+ T cells, and CXCR3+ natural killer (NK) cells has been observed in COVID-19[47]. These cells are responsible for the production of inflammatory cytokines. Previous studies in COVID-19 patients have shown increased levels of IL-1B, IL-1RA, IL-7, IL-8, IL-9, fibroblast growth factor, granulocyte-macrophage colony-stimulating factor (GM-CSF), IFN-γ, G-CSF, IP10, MCP1, MIP1A, platelet-derived growth factor (PDGF), TNF-α, vascular endothelial growth factor (VEGF)[48]. Among them, IL-2, IL-6, IL-7, G-CSF, IP10, MCP1, MIP1A, and TNF-α were significantly higher in severely conditioned patients[9-11,47,49]. In addition, thrombocytopenia, lymphopenia, respiratory failure, pneumonitis, shock, and organ failure have been observed in COVID-19 patients[11]. In addition, Wan et al[50] reported that COVID-19 patients were characterized by overactivated lymphocytes despite the occurred lymphocytopenia that was evident in the peripheral blood. This study showed that CD8+ T cells were reduced at a percentage of 28.4% and 61.9% in mild and severe group patients, respectively. Also, NK cell reduction was evident in both groups (34.1% in mild, 47.6% in severe)[50]. These findings were accompanied by significantly high IL-6 levels in both mild and severe groups. Additionally, Xu et al[51] reported the substantial reduction of CD4+ and CD8+ T cells in peripheral blood of COVID-19 patients, although it appeared that lymphocytes were overactivated due to high expression of human leukocyte antigen DR-isotype (HLA-DR) (34.7%) in CD4+ and CD38 (39.4%) in CD8+ T cells[51].
The third phase involves the prolonged lung damage that can cause severe ARDS. These patients must enter the intensive care unit (ICU), followed by connection to extracorporeal membrane oxygenation in order to survive[46]. It has been reported in COVID-19 patients that hyaluronan (HA) is produced due to the “cytokine storm”, thus promoting pneumonia accompanied by pulmonary ground-glass opacity[52]. Indeed, IL1 and TNF-α can strongly induce the HA production through overactivation of HA-synthase-2 of CD31+ cells and lung alveolar epithelial cells. A series of studies showed that damaged lungs are infiltrated mostly by macrophages, monocytes, and giant cells, while few overactivated CD4+ and CD8+ T cells were present[52,53]. Furthermore, inflammatory cytokines can activate fibroblasts, which in turn can overproduce collagen, promoting even more lung fibrosis[53,54].
Currently, the satisfactory administration of COVID-19 is a great challenge. Th1 and Th2 responses are playing a central role in disease severity of SARS-CoV-2 in the same way as MERS-CoV and SARS-CoV. Moreover, from previous experience, it is known that most neutralizing antibodies are against the S and E proteins[11,55]. However, the manufacturing of COVID-19 specific drugs and vaccines is still an ongoing process. Alternative strategies should also be tested for the suppression of the hyperacute immune response, which can lead to patient survival. To date, a great number of pharmaceutical agents, including antiviral agents, monoclonal antibodies against inflammatory cytokines, and convalescent plasma, are under investigation for COVID-19 (Table 1). The majority of these agents have current FDA approval for other diseases, including treatment of hepatitis C and rheumatic disease, while they are under evaluation for the safety, tolerability, and efficacy in COVID-19 patients. Most of these pharmaceutical agents have specific targets (e.g., S protein, IL-6R, and IL-6) but also are accompanied by adverse reactions. Moderate adverse effects may be observed in patients, including fever, headache, nausea, skin rash, diarrhea, and impairment of liver function. In addition to the use of pharmaceutical agents, it has been suggested that MSCs can effectively suppress the patient’s overactivated immune system by utilizing their immunoregulatory properties. MSCs have been used extensively in a wide number of registered clinical trials, supporting their tolerability, safety, and efficacy[56]. No severe adverse reactions have been observed after MSCs infusion to patients. In this way, MSCs could be employed as an alternative therapeutic strategy or as cotherapy in severely conditioned COVID-19 patients.
Table 1.
Most common therapeutic compounds used for the treatment of coronavirus disease-19
| Agents | Mechanism of action | Approval | |
| Antimalarial agent | Chloroquine/hydroxychloroquine | Inhibition of RNA-dependent RNA polymerase, Increase of endosomal and lysosomal pH | FDA approved (under investigation for COVID-19) |
| Antiviral agent | Ribavirin | Inducing mutations in RNA-dependent replication in RNA viruses, stop viral RNA synthesis | FDA approved (under investigation for COVID-19) |
| Nelfinavir | Inhibitor of viral proteases | FDA approved (under investigation for COVID-19) | |
| Remdesivir | Inhibition of viral RNA-dependent RNA polymerase and proofreading | FDA approved (for COVID-19) | |
| Anti-rheumatic agent | Baricitinib/ruxolitinib | JAK inhibitor/suppression of immune cells | Clinical Trial phase III |
| Monoclonal antibody | Tocilizumab | Humanized monoclonal antibody against the interleukin-6 receptor (IL-6R) and IL-6 | FDA approved (under investigation for COVID-19) |
| Anakinra | Humanized monoclonal antibody against IL-1R | FDA approved (under investigation for COVID-19) | |
| Vaccination | Ad5-nCoV | Recombinant adenovirus type 5 | Clinical Trials Phase II |
| ChAdOx1 nCoV-19 | Adenovirus vector | Clinical Trials Phase I-II | |
| INO-4800 | DNA plasmid delivered by electroporation | Clinical Trials Phase I-II | |
| NVX-CoV2373 | Recombinant S protein of SARS-CoV-2 | Clinical Trial Phase I | |
| LV-SMENP-DC | Minigene vaccination in combination with modified DCs | Clinical Trial Phase I | |
| Human antibodies | Convalescent plasma | Plasma enriched with antibodies specific to SARS-CoV-2, derived from convalescent patients | Clinical Trials Phase I |
| Stem cells | MSCs and derivatives (exosomes) | Suppression of the overactivated immune response through cell-cell contact and secretion of soluble factors | Clinical Trials Phase I |
COVID-19: Coronavirus disease-19; MSCs: Mesenchymal stromal cells; SARS-CoV-2: Severe acute respiratory syndrome coronavirus-2; DCs: Dendritic cells; FDA: Food and Drug Administration.
ORIGIN AND PROPERTIES OF MSCS
MSCs, a mesodermal multipotent cellular population, can mostly be derived from BM, WJ-tissue, umbilical cord blood, AT, amniotic fluid (AF), and dental pulp[57]. MSCs also have been isolated from solid organs such as the liver, lungs and kidney. Friedenstein, 40 years ago, was the first to isolate a fibroblastic-like cell population from BM with plastic adherent and differentiation properties[58]. In 2006, the International Society for Cellular Therapy (ISCT) provided the minimum criteria for the proper identification of MSCs[59]. Based on ISCT, the following criteria must be fulfilled to define MSCs: (1) Spindle-shaped plastic adherent cells; (2) Expression of specific antigens. Specifically, positive expression (≥ 95%) of CD73, CD90, CD105, and low expression (≤ 2%) of CD34, CD45, CD11a, CD19 and HLA-DR; and (3) Mesodermal multilineage differentiation abilities towards “osteocytes”, “adipocytes”, and “chondrocytes”.
Additionally, ISCT proposed the term “multipotent mesenchymal stromal cells” be used when this cellular population is applied in experimental approaches[59]. In 2019, the ISCT’s MSC committee reported that “mesenchymal stromal cells” have specific secretory, immunomodulatory, and homing properties and are distinguished from “mesenchymal stem cells”, which have restricted properties focused on self-renewal and differentiation[60].
Until date, BM is the most common source for MSCs isolation, estimating that MSCs represent 0.01%-0.001% of total nucleated cells[25]. BM-MSCs are located to the abluminal surface of sinusoidal blood vessels in BM. These cells represent the stroma, where can efficiently regulate the differentiation of the resident hematopoietic stem cells (HSCs)[25]. Specifically, MSCs support HSC differentiation through the expression of c-Kit, CXCR4, and Tie2. It has been shown in the literature that CXCR4/CXCL12, and CXCR7/CXCL12 interplay has a significant impact on the regulation of HSC homing and differentiation[61]. Additionally, the Notch-Delta, Wnt, Shh signaling pathways have been reported to be involved in this differentiation process[61].
Unlike BM harvesting, MSCs can be non-invasively isolated from other sources, including the umbilical cord’s WJ-tissue, a discarded material after gestation[62]. In recent years, there is a tendency to use MSCs derived from the stromal vascular fraction (SVF) of liposuction aspirates or subcutaneous AT in regenerative medicine applications[63]. Typically, MSCs represents 1%-10% of AT resident cells, making AT a greater source than BM. MSCs originated from AT are known as adipose derived stem cells or adipose derived MSCs (AD-MSCs) and exhibit similar immunophenotypic, differentiation potential and immunoregulatory properties as MSCs from other sources[63].
MSCs have been used in a great number of approaches, including tissue engineering and regenerative medicine applications, graft vs host disease (GvHD), co-transplantation with HSCs, and administration of autoimmune disorders such as MS, ALS, and Crohn’s disease[64-66]. MSCs can exert their functions through the production of cytokines, chemokines, exosomes, and miRNAs, which can act in a paracrine manner on targeted cellular populations[25]. Moreover, MSCs have proven their regenerative properties when applied to injured lungs, liver, kidney, and heart[67]. Recently, it is under evaluation the beneficial regenerative effect of MSCs in erectile dysfunction[68,69]. MSCs, due to their plasticity, have been differentiated successfully to ECs, vascular smooth muscle cells, hepatocytes, insulin-producing cells, etc. Much effort has been put into the transdifferentiation of MSCs to ectodermal cell lineages, such as neurons, by utilizing the induced pluripotent stem cell technology[70].
MSCs are immune privileged cells, and thus can be used either allogeneically or autologously in large scale clinical trials. Most often, a great number of clinical grade MSCs is required, which has been proven a quite demanding task. In this way, the autologous isolation and expansion of MSCs in significant numbers may be hampered by an individual’s characteristics, such as age and disease severity. On the other hand, allogeneic pooled MSCs may be a better option for regenerative medicine approaches. Le Blanc et al[71] have reported that MSCs expressed low levels of HLA class II intracellularly, which can be presented to their membrane surface after IFN-γ induction. However, MSCs do not express the costimulatory molecules B7-1, B7-2, CD40, and CD40L. Studies in non-human primates have revealed that MSCs escape T cell recognition and are well tolerated[71,72]. Besides the above properties, MSCs have unique immunoregulatory properties. Specifically, there is evidence that MSCs have a role in the antigen presentation process and are actively involving in organism homeostasis[29].
IMMUNOMODULATORY PROPERTIES OF MSCS
Despite the therapeutic potential of MSCs in regenerative medicine applications, these cells have shown promising results in the regulation of immune responses[25,29]. MSCs can act both in immune activation and immune suppression, depending on the microenvironment stimuli (Figure 1). The significant immunoregulatory/ immunosuppressive abilities of MSCs have been exploited for therapeutic applications in autoimmune disorders and GvHD[65,66]. Taking into account that SARS-CoV-2 can induce significant alterations to innate and adaptive immune responses, leading to the “cytokine storm”, the transfusion of MSCs to COVID-19 patients may be beneficial.
Figure 1.
Immunomodulatory properties of activated MSCs against overactivated immune cells during SARS-CoV-2 infection. MSCs efficiently suppress the immune responses through the secretion of soluble molecules or cell-cell contact interactions. MSCs have a broad effect on the immune responses exerted by macrophages, dendritic cells, natural killer cells, and T and B cells. SARS-CoV-2: Severe acute respiratory syndrome coronavirus-2; MSCs: Mesenchymal stromal cells; NK cells: Natural killer cells; NO: Nitric oxide; IDO: Indoleamine-2,3-dioxygenase; EVs: Extracellular vesicles.
It has been described in the literature that MSCs can effectively modulate DC maturation, T cells (naïve and effector T cells – Th1/ Th2/ Th17 cells), and NK cell responses[25,29]. In the presence of low IFN-γ levels, MSCs can translocate the intracellular HLA class II to their membrane, thus playing a role in innate immunity. On the other hand, high IFN-γ levels can induce MSCs to exert their immunoregulatory properties, mostly through paracrine signaling pathways. In addition, there is evidence that MSCs under specific circumstances may act as antigen-presenting cells[25]. The immunomodulation abilities of MSCs can be exerted by delivered soluble factors (cytokines, chemokines, growth factors, modulators of enzyme function), direct cell-cell contact, or a combination of those (Table 2)[29].
Table 2.
Immunomodulation mechanisms of mesenchymal stromal cells
| Implicated biomolecules | Mechanism of action | Implicated immune cells | Result | |
| Cell-cell contact | Fas/fas ligand | Fas/fas ligand death signaling pathway/FADD/caspases activation or TRAIL signaling pathway | Macrophages, DCs, T and B cells | Apoptosis |
| PD-L1/ PD-1 | PD-L1 induced death through binding with the inhibitory checkpoint protein PD-1 | T and B cells | Reducing cell proliferation, reducing apoptosis of T reg | |
| HLA-G/LIRB2 (ILT4/CD85d) and KIR2DL4 (CD158d) | HLA-G/LIRB2 interaction /phosphorylation of TIMS/SHP phosphatases activation/ MAPK downregulation | DCs, NK cells and T cells | Inhibition of cellular proliferation | |
| Soluble factors | PGE2 | PGE2/cAMP production/ downregulation of IL-2, IL-2R expression. PGE2/ downregulation of PtdIn/ suppression of T cell receptor signaling | Macrophages, DCs, T and B cells | M2 macrophages switching; Prevention of DCs maturation, T and B cell inactivation |
| IDO | IDO blocks the conversion of tryptophan to kyneurenin/in combination with TGF-β1 and HGF | DCs NK cells, T and B cells | G0/G1 cell cycle arrest | |
| NO | NO/suppression of STAT5 phosphorylation | Macrophages, T and B cells | Inhibition of cellular proliferation | |
| Galectins | Crosslinking with TCR/clustering prevention | T and B cells | Inhibition of T and B cell proliferation | |
| Soluble HLA-G isoforms | Similar interaction mechanism as membrane bound HLA-G isoforms | DCs, NK cells and T cells | Inhibition of cellular proliferation | |
| ΕVs | miR-21-5p, miR-142-3p, miR-223-3p, and miR-126-3p | Interaction with JAG1, PDCD4, IL-12p35, downregulation of IL-6 expression | DCs | Inhibition of DC maturation |
| miR-145, miR-146 and miR-155 | Suppression of TRAF6 and IL-1 IRAK1 expression/down-regulation of NF-κB p65 phosphorylation/decrease in TNF- α, ΙL-1β and IL-6 production | Macrophages, T cells | Inactivation of M1 macrophages; Switching from Th1 to Th2 responses |
FADD: Fas-associated death domain; PtdIn: Phosphatidylinositol; DCs: Dendritic cells; NK cells: Natural killer cells; PGE2: Prostaglandin E2; IL: Interleukin; TNF: Tumor necrosis factor; NO: Nitric oxide; STAT5: signal transducer and activator of transcription 5; TCR: T cell receptor; TRAIL: TNF-related apoptosis-inducing ligand; IDO: Indoleamine-2,3-dioxygenase; EVs: Extracellular vesicles; SHP: Src-homology 2 domain-containing protein tyrosine phosphatases; TRAF6: TNF receptor-associated factor 6; IRAK1: IL-1 receptor-associated kinase 1.
Interplay between MSCs and macrophages
MSCs can effectively modulate the responses of neutrophils and macrophages. Both cells are playing central roles to the antigen presentation process to DCs, leading to specific immune responses by the cells of innate immunity[73]. Macrophages are distinguished to M1 (classically activated) and M2 (alternatively activated) macrophages[29]. M1 macrophages are responsible for pathogen phagocytosis and presentation of antigen epitopes to DCs. In this process, a set of inflammatory cytokines are produced by M1 macrophages, such as TNF-α, ΙL-1α/β, IL-6, and IL-12, thus activating and promoting Th1 responses. On the other hand, M2 macrophages promote Th2 responses and are considered immunosuppressive cells[74]. These cells exhibit low expression of inflammatory cytokines and high production of anti-inflammatory IL-10, which is associated with tissue remodeling, wound repair, and clearance of apoptotic cells[74]. It has been reported that MSCs can modulate the M1/ M2 macrophage phenotype through cell-cell or paracrine interactions[29,75].
Activation of MSCs with IFN-γ leads to the production of TNF-α, MCP1, and IL-1β, which can further promote the M1 macrophage phenotype. Alternatively, MSCs, through the expression of prostaglandin E2 (PGE2), can induce M2 macrophage phenotype switch[29]. Further evidence for the role of MSCs in promoting the M2 macrophage phenotype arises from the study of Wahnon et al[76]. Specifically, they reported that signal transducer activators of transcription-3 (STAT3) is activated through cell-cell interactions between MSCs and macrophages[76]. Moreover, the same study showed that the STAT3 transcription factor is responsible for IL-10 production by macrophages and DCs, promoting further their immunosuppressive functions[76].
Regulation of DC maturation
Immature DCs (imDCs), the immune sentinels of the periphery, can be activated after inflammatory cytokine production by macrophages. Cleaved antigenic epitopes are loaded to HLA molecules of imDCs, followed by the presentation to T cells of the draining lymph nodes[77]. Then, DCs undergo maturation, which can induce specific Th1 and Th2 responses against specific antigenic epitopes. It has been found that TNF-α, IL-1β, and IL-6, produced either by M1 macrophages or IFN-γ activated MSCs, can drive DC maturation[78]. The prevention of DC maturation is of great importance, especially when this leads to prolonged T cell responses, causing host cell and tissue damage. Several studies have shown that MSCs can interfere with DCs maturation through the production of soluble factors[29,78,79]. Mostly, it has been suggested that secreted PGE2 by activated MSCs plays an important role in the inhibition of DCs maturation[29]. This has been confirmed by results from co-culture studies using MSCs and DCs[80]. These studies, were characterized by low expression of CD38, CD80, CD86, IL-6, and IL-12, which are significant molecules for T cell activation[81]. Moreover, DCs exhibited low migratory ability, exerted by CCR7-CCL21 interaction. Liu et al[82] suggested that the production of TNF-α-stimulating gene 6 by MSCs can suppress DCs maturation though the inactivation of signaling cascades mediated by mitogen activated protein kinase (MAPK) and nuclear factor-kappa B (NF-κB).
The inhibitory effect of MSCs in DC maturation can be increased by the production of specific miRNAs, including miR-21-5p, miR-142-3p, miR-223-3p, and miR-126-3p[83]. In this process, extracellular vesicles (EVs) of MSCs are enriched with the above miRNAs, suggesting an additional way of regulating DC maturation[84].
MSCs and T cell responses
Immunomodulation of T cell responses can be exerted by MSCs in several ways. MSCs secrete a set of molecules that can act either positively or negatively to the T cell responses. Also, inhibition of T cell proliferation can be performed via cell-cell contact with MSCs[85].
Dependent on the microenvironment stimuli, MSCs can effectively inhibit T cell proliferation through the production of PGE2, indoleamine-2,3-dioxygenase (IDO), TGF-β, and hepatocyte growth factor (HGF)[25,29]. The effect of PGE2 inhibition of T cell proliferation was reported for the first time in 1971[86]. Several years later, the specific mechanism of action by which PGE2 can exert its immunosuppressive effects on T cells was revealed. PGE2 is a prostanoid, which is synthesized by arachidonic acid through the action of cycloxygenase-1[87]. PGE2 is responsible for the production of cAMP in activated T cells. CAMP plays a key role in the downregulation of IL-2 and IL-2R expression and abrogation of Ca2+ after T cell receptor (TCR) activation. Also, PGE2 negatively regulates the hydrolysis of phosphatidylinositol and the production of diacylglycerol and inositol phosphate (IP), resulting in T cell inactivation[87]. Recently, it was reported that PGE2 may be involved in T cell polarization, promoting further Th2 responses. In addition, PGE2 produced by MSCs can orchestrate the CD4+ CD25+FOXP3 T reg responses, influencing even more the immunosuppression of hyperactivated T cells[29].
IDO also is a strong immunosuppressive agent of T cell responses[85]. Specifically, IDO blocks the metabolism of tryptophan to kynurenine in T cells. Kynurenine is an essential amino acid for the cell cycle of T cells, and its absence leads to G0/G1 cell cycle arrest. In addition, Ryan et al[88] reported that IFN-γ activated MSCs can produce TGF-β1 and HGF and, in combination with IDO, can significantly suppress alloreactive T cell proliferation. MSCs via the secretion of nitric oxide (NO) can inhibit T cell proliferation[89]. NO is another potent immunosuppressive agent that can effectively downregulate immune responses. Specifically, NO is responsible for the suppression of signal transducer and activator of transcription 5 phosphorylation, which further results in the inhibition of TCR-mediated T cell proliferation and inflammatory cytokine production. Additionally, it was found that galectins 1 and 3 secreted by MSCs can effectively suppress T cell proliferation by preventing TCR clustering through a crosslink interaction mechanism[89].
Additionally, MSCs can exert their immunosuppressive properties through T cell apoptosis mediated by cell-cell interactions[90]. In this way, the Fas/Fas ligand death signaling pathway can induce apoptosis to T cells, through downstream activation of Fas-associated death domain and caspases. It has been found that MSCs, upon inflammatory stimuli, can express the Fas ligand, binding in this way to Fas receptor of hyperactivated T cells[90,91]. Another potential activator of Fas-associated death domain is the TNF-related apoptosis-inducing ligand (TRAIL)/death receptor (DR) signaling pathway. IFN-γ activated MSCs produce high amounts of TRAIL, which binds to DRs expressed in T cells, thus leading to their apoptosis. Also, MSCs can reduce T cell proliferation via programmed death ligand-1 (PD-L1)/programmed death-1 (PD-1) interaction. Specifically, PD-L1 expressed by MSCs binds to the inhibitory checkpoint molecule PD-1 of T cells, followed by Src-homology 2 domain-containing protein tyrosine phosphatases (SHP)-1 and SHP-2 phosphorylation. Finally, inhibition of MAPK is performed, which leads to inhibition of cellular proliferation. The PD-L1 can inhibit cellular proliferation and may have a broad effect on T cell subpopulations, including CD4+, CD8+, and Th17 cells[91]. Remarkably, Luz-Crawford et al[92] showed that the PD-L1/PD-1 interaction also could induce inhibition of Th17 cells via cell-cell contact. On the other hand, this mechanism has a positive association with CD4+ CD25+FOXP3 T reg proliferation.
MSCs and B cell responses
Similarly, to T cell modulation, B cell responses can be regulated by MSCs via the secretion of soluble factors and through cell-cell contact interactions. IDO and PGE2 alongside the production of TGF-β1 and HGF can lead to cell cycle arrest of B cells (G0/G1)[93]. Additionally, direct cell contact interactions, mostly utilizing the Fas/Fas ligand, TRAIL/DR death signaling, and PD-L1/PD-1 pathways, can promote apoptosis in B cells[94,95]. Recent evidence also showed that coculture of MSCs with B cells resulted in downregulation of CXCR4 and CXCR5, thus preventing the migratory ability and homing of B cells towards CXCL12 and CXCL13 chemoattractant agents. It has been shown that BM-MSCs via secretion of GM-CSF can inhibit the production of CXCR4, CXR5, IL-6, and IL-7 by activated B cells[95]. Indeed, the MSC interaction with plasma B cells results in impaired secretion of immunoglobulin (Ig)M, IgG, and IgA by plasma B cells. However, MSCs cannot downregulate the expression of the costimulatory molecules CD80, CD86, and HLA-DR in activated B cells[96]. Additionally, MSCs did not cause any negative effect on IFN-γ, TNF-α, IL-4, and IL-10 expression by B cells[96].
Modulation of NK responses
NK cells are the responsible cellular population for the elimination of virus-infected and tumorigenic cells. In addition, these cells of the innate immunity bear inhibitory and activating receptors to their surface[97]. Killer cell immunoglobulin-like receptors (KIRs) exert inhibitory effects, while natural cytotoxicity receptors, NKp46, NKp30, and NKp44, are responsible for NK activation[98]. Due to virus infection or malignant transformation, the affected cells initially decrease the expression of HLA class I, thus becoming susceptible by NK cells. In this way, NK cells are activated to exhibit their strong cytolytic activity against their targets[98].
A remarkably complex interplay between NK cells and MSCs has been reported[99]. Indeed, NK cells can exert cytolytic actions against MSCs due to the low expression of HLA class I[100]. Alternatively, activation of MSCs with IFN-γ leads to upregulation of HLA class I expression, which can strongly interact with KIRs, inhibiting in this way the MSCs cytolysis mediated by NK cells[100]. In this context, toll-like receptors (TLRs), presented in MSCs, seem to play a significant role. Activation of TLR3 in MSCs leads to increased immunosuppression against NK cells[101].
Further immunosuppression of NK cells is mediated by the secretion of soluble factors from MSCs[29]. Indeed, IDO and PGE2 can inhibit IL-2 induced NK responses, while TGF-β1 and HGF act cooperatively with the above-described molecules[29,102]. Depending on the microenvironment stimuli, MSCs can either activate or inhibit the action of NK cells. It has been shown that WJ-MSCs can stimulate the proliferation of NK cells via the production of inflammatory cytokines, including TNF-α, IL1α / β, ΙL-6, and others[103]. More research is required regarding the interplay of MSCs and NK cells in order to understand better their association.
HLA-G and immune responses
The HLA system has an essential key role in immune responses[104]. The HLA system includes the HLA class I and class II molecules, which are located within chromosome 6p21[105]. In this complex system, the HLA class I involves the classical A, B, and C genes and the non-classical genes E, F, and G, while the HLA class II involves the genes DP, DQ, DM, DO, and DR. Both, HLA class I and II are expressed in all cells, particularly in immune cells, and thus play a significant role in antigen recognition and presentation. On the other hand, the exact role of non-classical HLA genes has not yet been completely elucidated. Among them, HLA-G seems to share key immunoregulatory properties[104,105].
For the first time, the role of HLA-G was investigated in pregnancy. The placental and fetus region of the umbilical cord express significant amounts of HLA-G, thus preventing the rejection of the semi-allogeneic fetus by the mother[104,106]. HLA-G involves the non-secreted membrane bound isoforms HLA-G1-4 and the soluble isoforms HLA-G5-7. It is speculated that HLA-G5 occurs after specific cleavage of membrane-bound HLA-G1 mediated by metalloproteinase-2. It seems that HLA-G exerts its anti-inflammatory and immunoregulatory properties in a wide variety of immune cells, including monocytes, DCs, NK cells, and T cells[104].
Importantly, the HLA-G isoforms can interact with leukocyte immunoglobulin like receptor B1 (LILRB1, ILT2/CD88j), LIRB2 (ILT4/CD85d), and KIR2DL4 (CD158d), which are expressed in monocytes, DCs, T cells, and NK cells[104,107]. Indeed, the interaction of HLA-G with LILRB1 and LIRB2 induces the phosphorylation of the immunoreceptor tyrosine-base inhibitory motifs, followed by activation of SHP phosphatases, which lead to downregulation of MAPK and inhibition of cell proliferation[107]. Alongside IDO and IL10, HLA-G can suppress the proliferation of hyperacute T cells and can prevent the differentiation of monocytes to DCs[80,85]. In this way, the secreted cytokines, including TNF-α, ΙL1-α, β, IL-6, IL-7, IL-8, IL-9, GM-CSF, and IFN-γ, can be blocked indirectly via the HLA-G mediated inhibition of DCs and T cells. In a high inflammatory environment, HLA-G interactions can mediate the recruitment and the expansion of CD4+CD25+FOXP3+ T cells (T reg), which in turn can inhibit effectively the proliferation of allocytotoxic T cells. Additionally, soluble HLA-G5-7 isoforms, can induce the secretion of IL-10 and TGF-β1, which further promotes the inhibition of CD8+ T cell proliferation[104,108]. Several reports have indicated that HLA-G can influence the Th2 response, leading to increased production of anti-inflammatory cytokine IL-10, TGF-β1, and HGF. HLA-G can also modulate the function of NK cells by interacting with KIR2DL4. It has been described in the literature that endocytosis of soluble HLA-G with KIR2DL4 is required for the inhibition of NK cells and cytokine production[109]. On the other hand, it has been reported that HLA-G homodimers are required for the secretion of TNF-α, ΙL-4, and IL-6[110]. This specific set of cytokines is required for successful trophoblast implantation. In this way, more experiments must be performed in order to elucidate better the interplay between HLA-G and NK cells.
MSCs, as part of their immunomodulation, are capable of producing both the membrane bound and soluble HLA-G isoforms. MSCs can be derived efficiently from placental and WJ-tissue, which is located within umbilical cord. Also, it has been shown that placental and WJ-MSCs may exert advanced immunoregulatory/ immunosuppressive properties compared to BM or AD -MSCs due to their embryonic origin[106]. Evidence from our previous work confirmed the expression of HLA-G isoforms by WJ-MSCs[106]. Moreover, HLA-G expression was retained after long term storage of WJ-MSCs with the vitrification approach. Vitrified WJ-MSCs after 1 year of storage at -196 °C successfully inhibited monocyte proliferation in mixed lymphocyte reaction studies[106]. In this way, MSCs can be isolated, expanded and stored long term without any negative effect to their immunomodulatory properties. Thus, they can be ready for use on demand.
MSCS AND COVID-19
Until date, MSCs have been applied in large scale cell based therapies, where safety and treatment efficacy have been well documented[56]. Their unique role in immune modulation led to the use of MSCs as potential treatment in immunological based diseases, including GvHD, MS, ALS, SLE, etc[25,29]. Currently, no specific drugs against COVID-19 exist, while the development of satisfactory vaccines is a challenging process. Therefore, a safe and effective treatment is still under investigation. Taking into consideration that SARS-CoV-2 is responsible for an extended immunomodulation, caused by “cytokine storm”, the administration of MSCs may have a considerable therapeutic benefit, especially in patients with increased COVID-19 severity[8,9]. In addition, MSCs are negative for ACE2 receptor and TMPRSS2, and thus cannot be a target for SARS-CoV-2, making their application even safer[47].
Currently, over 30 clinical trials, where MSCs can be potentially applied in COVID-19 as therapeutic agents, have been officially registered (www.clinicaltrials.gov)[111]. The majority of the clinical trials involve intravenous administration of MSCs to COVID-19 patients, but most of them are currently under the recruitment phase (Table 3 ).
Table 3.
Clinical trials associated with the use of mesenchymal stromal cells in coronavirus disease-19
| NCT number | Title | Status | MSCs origin | Route of infusion |
| NCT04252118 | Mesenchymal stem cell treatment for pneumonia patients infected with COVID-19 | Recruiting | Not specified | Intravenously |
| NCT04313322 | Treatment of COVID-19 patients using Wharton's Jelly-mesenchymal stem cells | Recruiting | Wharton’s Jelly MSCs | Intravenously |
| NCT04336254 | Safety and efficacy study of allogeneic human dental pulp mesenchymal stem cells to treat severe COVID-19 patients | Recruiting | Allogeneic human dental pulp stem cells | Intravenously |
| NCT04288102 | Treatment with mesenchymal stem cells for severe COVID-19 | Recruiting | Not specified | Intravenously |
| NCT04346368 | Bone marrow-derived mesenchymal stem cell treatment for severe patients with COVID-19 | Not yet recruiting | BM-MSCs | Intravenously |
| NCT04366323 | Clinical trial to assess the safety and efficacy of intravenous administration of allogeneic adult mesenchymal stem cells of expanded adipose tissue in patients with severe pneumonia due to COVID-19 | Not yet recruiting | Allogeneic and expanded adipose tissue-derived MSCs | Intravenously |
| NCT04276987 | A pilot clinical study on inhalation of mesenchymal stem cells exosomes treating severe novel coronavirus pneumonia | Not yet recruiting | MSCs-derived exosomes | 5 times aerosol inhalation of MSCs derived exosomes |
| NCT04269525 | Umbilical cord (UC)-derived mesenchymal stem cells (MSCs) treatment for the 2019-novel coronavirus (nCOV) pneumonia | Recruiting | UC-MSCs | Intravenously |
| NCT04348461 | Battle against COVID-19 using mesenchymal stromal cells | Not yet recruiting | Allogeneic and expanded adipose tissue-derived MSCs | Intravenously |
| NCT03042143 | Repair of acute respiratory distress syndrome by stromal cell administration (REALIST) (COVID-19) | Recruiting | Human umbilical cord derived CD362 enriched MSCs | Intravenously |
| NCT04333368 | Cell therapy using umbilical cord-derived mesenchymal stromal cells in SARS-CoV-2-related ARDS | Recruiting | Umbilical cord Wharton's jelly-derived human | Intravenously |
| NCT04352803 | Adipose mesenchymal cells for abatement of SARS-CoV-2 respiratory compromise in COVID-19 disease | Not yet recruiting | Autologous adipose MSC's | Intravenously |
COVID-19: Coronavirus disease-19; MSCs: Mesenchymal stromal cells; SARS-CoV-2: Severe acute respiratory syndrome coronavirus-2; ARDS: Acute respiratory distress syndrome; UC-MSCs: Umbilical cord-derived mesenchymal stem cells; BM-MSCs: Bone marrow-derived mesenchymal stem cells.
Among them, a study of Leng et al[47] showed promising results in severe diseased COVID-19 patients. This study was conducted in a great number of hospitals, mostly in China, and was approved by the National Health Commission of China. In this study, clinical grade MSCs were intravenously infused in seven patients diagnosed with SARS-CoV-2. Importantly, one patient was in critical condition and entered the ICU, four patients exhibited severe type of the disease, and the last two were in better condition. Also, a placebo group was used, consisting of three severe type patients. The MSCs were administrated in a number of 1 × 106 cells/kg with an infusion rate of 40 drops/min. After 2-4 d of MSC administration, the severe symptoms, including fever, oxygen saturation, and cough, were improved, and the majority of the patients were discharged. Also, the critically severe patients exited the ICU and successfully recovered. On the other hand, one patient from the placebo group was died, one developed ARDS, and one was in stable condition[47].
Leng et al[47] showed that MSCs exerted their immunoregulatory properties and were capable of tolerating the hyperacute immune responses of patients, thus improving significantly the patients’ overall condition (Figure 1). Indeed, the levels of C-reactive protein in the study group were declined, accompanied by a decrease in the TNF-α concentration. Mass cytometry analysis revealed that the overactivated CXCR3+CD4+ T cells, CXCR3+CD8+ T cells, and CXCR3+NK cells disappeared and that the CD14+CD11c+CD11bmid DCs reversed to normal conditions. Leukopenia was also reversed in all patients within 1 or 2 wk after MSCs administration. Furthermore, the ground glass opacity of lungs seemed to have subsided in patients[47].
Another important issue that should be mentioned is the time point of MSC administration to COVID-19 patients. The exact time point for MSC administration varied among the studies. In a number of clinical trials, the MSCs are infused at specific time points (0, 2, 6, 10, 14 wk) after disease onset. In other studies, MSCs are infused in severe conditioned COVID-19 patients as a co-therapy alongside with their primary therapeutic protocol. Severe COVID-19 condition is established through the determination of specific clinical manifestations. Severe clinical manifestations include fever, respiratory distress (respiratory rate ≥ 30/min), low oxygen saturation (≤ 93% at rest state), low arterial partial pressure of oxygen/fraction of inspiration O2 ≤ 300 mmHg, while respiratory failure (connection of patients to extracorporeal membrane oxygenation), shock, and organ failure compromise the critically severe manifestations. The cytokine levels of IL-2, IL-6, IL-7, G-CSF, IP10, MCP1, MIP1A, and TNF-α are also determined and were mostly found to be elevated when patients are suffering from the severe manifestations and critically severe manifestations.
MSCs can exert their immunoregulatory properties by activating inflammatory cytokines, including IL-1, IL-6, IFN-γ and TNF-α. At disease onset, patients are not characterized by increased alveolar epithelium damage due to the low virus replication. On the other hand, when virus load is high, severe alveolar epithelium damage can occur due to the production of inflammatory cytokines and the initiation of “cytokine storm”. MSCs can now be activated (by inflammatory cytokines), which can lead to immunoregulation of the overactivated immune system. Besides these facts, MSCs could also have a prophylactic effect, and this could be the primary reason for their use at disease onset. Taking into consideration the above data, the specific time point for the administration of MSCs should be established that leads to patients’ condition improvement.
Similar results regarding the immunomodulatory benefits of MSCs have been reported by other research groups around the world. Indeed, in the study of Petrou et al[112] the ALS severity score was decreased in all patients after MSCs infusion, while the treatment was proven safe and well tolerated.
In this way, MSCs can modulate effectively a series of immune responses, including macrophages, DCs, NK, T, and B cells. Especially in COVID-19, the latest evidence supports that IL-6 is the main inflammatory cytokine for the immune system overactivation, and MSCs may be used as potential immunoregulatory players and inhibitors of IL-6 production[113]. MSCs can secrete anti-inflammatory cytokines, including IL-10. In addition, MSCs can induce apoptosis to overactivate T and B cells, promote Th2 responses, and activate M2 macrophages, regulating even more the inflammation.
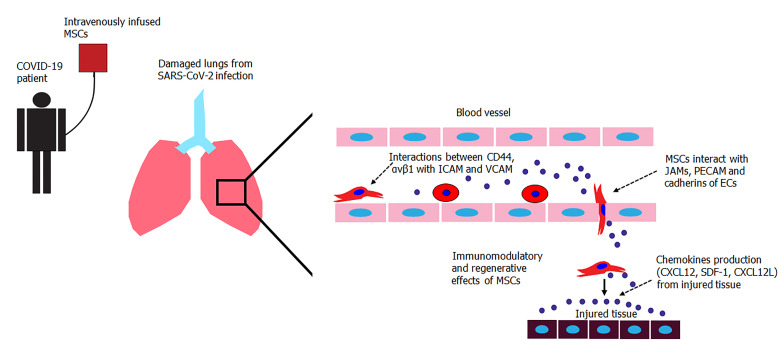
Besides its well documented immunoregulatory properties, MSCs may exert key regenerative properties towards damaged alveolar epithelium and lung fibrosis[114]. In previous studies, it has been shown that MSCs accumulate in lung capillary vessels after intravenous injections[115]. MSCs engraft to the injury site in a chemokine-gradient dependent manner. Upon chemokine detection (CXCL12, SDF-1, CXCL12L), MSCs can upregulate CD44 and ανβ1 integrins, and through the interaction with P/E selectins, vascular adhesion molecule-1 (VCAM-1) and intracellular adhesion molecule-1 (I-CAM-1) can perform the rolling adhesion to endothelium surface until reaching the injury site[25]. Then, transendothelial migration of MSCs occurs in a process mediated by junctional adhesion molecules, platelet-EC adhesion molecule-1, and cadherins (Figure 2). MSCs produce several growth factors, such as TGF-β1, VEGF, HGF, EGF, and IGF, that could induce the differentiation of alveolar epithelial cells from progenitor cells, attracting the M2 macrophages while reducing the scar tissue formation process[25]. This has been further confirmed by evidence regarding the reversion of ground glass opacity in lungs of COVID-19 patients after MSC infusion[47].
Figure 2.
Transendothelial migration of intravenously infused MSCs in COVID-19 patients. Proposed mechanism of MSCs trafficking towards to chemokine stimuli produced from affected cells. MSCs perform endothelial rolling through interactions of CD44 and ανβ1 with intercellular cell adhesion molecule and vascular cell adhesion molecule. Transendothelial migration of MSCs is mediated through interactions of junctional adhesion molecular, platelet endothelial cell adhesion molecule PECAM, and cadherins. Upon arrival to their destination, MSCs exert their immunomodulatory and regenerative potential to the damaged tissue. COVID-19: Coronavirus disease-19; ICAM: Intercellular cell adhesion molecule; MSCs: Mesenchymal stromal cells; VCAM: Vascular cell adhesion molecule; PECAM: Platelet endothelial cell adhesion molecule; JAM: Junctional adhesion molecular; ECs: Endothelial cells.
The safe and tolerability of allogeneically infused MSCs have been reported in the past. There was evidence that intravenously infused MSCs could be accumulated in capillary vessels of lungs, thus raising the possibility of pulmonary embolism occurrence. In a phase I clinical trial performed by Iacobaeus et al[115], no long-term engraftment of MSCs was performed in patients with MS. MSCs were further cleared from the circulation through the secondary lymphoid organs[115]. In another phase I clinical trial evaluating the possible treatment of ARDS, allogeneic BM-MSCs were well tolerated by the patients, and no infusion or treatment related adverse events were reported[116]. Moreover, Matthay et al[117] reported that intravenous injection of MSCs in a number of 10 × 106 cells/kg was safe in patients with moderate ARDS. In both studies, after MSC infusion, the levels of IL-6 and IL-8 and the in-hospital mortality of patients were critically decreased, promoting even more the therapeutic potential of MSCs[47,117]. In recent years, AD-MSCs have gained significant interest by the scientific society for their regenerative and immunoregulatory properties. Recently, Gentile et al[26,27] reported that AD-MSCs exert key immunosuppressive properties via the secretion of TGF-β1, HGF, and IFN-γ and remarkable regenerative properties through the secretion of VEGF and PDGF[26,27]. Indeed, besides their immunosuppressive properties, AD-MSCs can secrete pro-angiogenic factors such as VEGF and PDGF, which can stimulate the ECs, promoting in this way the vascularization and the regeneration of damaged lung tissue[26-28]. Moreover, a phase I clinical trial using autologous or allogenic AD-MSCs was conducted since April 2020 in COVID-19 patients, determining the safety and tolerability of these cells[26].
Moreover, MSCs, upon environmental stimuli, are able to secrete EVs containing biomolecules, which effectively can promote key function processes, such as local immunomodulation and tissue regeneration[118]. EVs are composed of lipid bilayer membranes and can be classified into exosomes (microvesicles (MVs) with diameter of 30-100 nm), apoptotic bodies, and the recently described nanovesicles with diameter of 8-12 nm[119,120]. MVs mostly contain mRNAs, microRNAs, cytokines, and chemokines that can regulate a wide number of biological processes, including the function and homing of immune cells[121,122]. It has been shown that MVs derived from BM-MSCs suppress the expression of IL-1β and TNF-α and can promote the conversion of Th1 to Th2 responses[120,123]. Also, MVs contain the miRNAs miR-145, miR-146, and miR-155, which can effectively suppress the expression of TNF receptor-associated factor 6 and IL-1 receptor-associated kinase 1, followed by down-regulation of NF-κB p65 phosphorylation[120,122,124]. These events further lead to the impaired production of TNF- α, ΙL-1β, and IL-6 and is accompanied by inhibition of proliferation of M1 macrophages[120,122]. To date, a clinical trial that involves the application of inhaled exosomes derived from MSCs in patients with COVID-19 has been registered (NCT04276987). Moreover, MSC derived exosomes have been used as therapeutic agents in lung inflammatory diseases and tissue protection from fibrosis. In this context, WJ-MSCs derived exosomes significantly suppressed TGF-β1 expression and its downstream signaling pathway involving the inactivation of SMAD4 and SMAD5, leading to decreased collagen production and attenuation of scar tissue formation[120,125]. Exosomes can be produced under large scale good manufacturing practices (GMPs) conditions and could act beneficially in COVID-19 patients.
CURRENT LEGISLATION DESCRIBING THE USE OF MSCS
The use of MSCs in COVID-19 patients is categorized as stem cell-based therapies, and therefore the guidelines of International Society for Stem Cell Research must be strictly followed[126]. Moreover, International Society for Stem Cell Research released the “The Guidelines for the Clinical Translation of Stem Cells”, which involves the current standards for the development of stem cell-based therapies, leading to proven therapeutic potential for the patient[126].
To promote the therapeutic outcome for the patients, MSC based therapies must overcome a great number of challenges, including expansion time, required cell number-dosage, cell cultivation, and cell exposure to animal-derived products, which can affect significantly the safety and efficacy. Furthermore, prolonged in vitro cultured stem cells may lose their key function characteristics such as stemness and plasticity, or even more could undergo malignant tumorigenic transformation[126].
According to the “Guidance of Human Somatic Cell therapy and Gene Therapy” established for human cells, tissues, and cellular, tissue-based products (HCT/Ps), stem cell-based products must be developed under GMPs conditions. Also, additional regulations exist depending on the cell manipulation or either if HCT/Ps are intended to be used in homologous or allogeneic setting[126]. FDA has defined the minimal manipulation as the process, which is not altering the biological characteristics of stem cells. Moreover, processes including density-gradient separation, cell selection, centrifugation, and cryopreservation are defined as minimal manipulation HCT/Ps[126].
All other processes involving cell cultivation, expansion, exposure to animal derived substances, activation, and gene modifications are considered as more-than-minimal-manipulated HCT/Ps[126]. Furthermore, the use of MSCs in allogeneic setting must fulfill donor eligibility (donor screening and testing for communicable diseases), Quality Assurance program (GMPs conditions and Quality Control system), proper storage conditions (long-term stem cell stability under cryopreserved conditions), and distributing–release criteria. The aforementioned information must be specifically defined in Standard Operation Procedure documentation in order to reduce the risk occurrence for the patient. Trials regarding the homologous or allogeneic use of MSCs must be approved by the corresponding national health commission[126].
All MSC based therapies performed in United States must be registered to the FDA. Accordingly, the European Medicines Agency and the Therapeutic Goods Administration is responsible for the cell-based therapies performed in Europe and in Australia, respectively. According to Committee for Advanced Therapies, which has been established by the European Medicines Agency, all MSC-based products in the European Union will be defined as Advanced Therapeutical Medicinal Products, with the only exception being the aforementioned minimally manipulated stem cells[126]. The above requirements and the developed authorities make the MSC based therapies even safer for the patients, bringing stem cell based therapy one step closer to broad clinical utility.
CONCLUDING REMARKS
The above evidence clearly indicate that MSCs could be used as potential therapeutic agents in patients suffering from COVID-19. MSCs can modulate effectively the overactivated immune responses caused by SARS-CoV-2 through inactivation of macrophages and NK, T, and B cells, while at the same time could promote the Th2 response and the activation of M2 macrophages[25,29]. In addition, MSCs could have a beneficial regenerative effect in damaged lungs and alveolar epithelial cells, reversing in this way the ground glass opacity in patient’s lungs[67].
Until now, several treatment protocols have been proposed, such as the administration of remdesivir, hydrochoriquine, colchicine, and vaccination of high risk patients[20,22]. However, most of these treatments are accompanied by significant adverse reactions, limiting their application to patients. The induced “cytokine storm” by SARS-CoV-2 infection has attracted the attention of the scientific society. This phenomenon, and specifically IL-6, may be responsible for the immune system overactivation and also is associated with poor prognosis in critically ill patients.
On the other hand, MSCs, which are negative for ACE2 receptor and TMPRSS2, could be effective in regulating the “cytokine storm”[47]. Moreover, WJ-MSCs may possess better immunoregulatory properties through the elevated expression of HLA-G, the existence of longer telomeres, and fewer epigenetic modifications compared to MSCs from the other sources[106]. AD-MSCs that are extensively used in a great series of personalized regenerative medicine applications, including breast reconstruction with fat graft, androgenic alopecia, etc, exhibited similar properties as the MSCs from other sources[127-133].
Recently, the application of AD-MSCs as immunoregulatory agents in COVID-19 patients is gaining day by day more attention by the scientific society, worldwide[26,27]. AD-MSCs can be efficiently isolated in great quantities from SVF or subcutaneous AT, expanded under clinical grade GMP conditions, and applied through intravenously infusion to critically-ill COVID-19 patients[26,27]. AD-MSCs exert equal immunoregulatory properties as MSCs from BM and WJ tissue through secretion of soluble factors or cell–cell contact interactions, as has been described previously[26,27]. Furthermore, AD-MSCs can be efficiently differentiated towards “chondrogenic” and “osteogenic” lineages and can produce significant amounts of proangiogenic factors, indicating their significant regenerative potential[26,27,127]. These regenerative properties of AD-MSCs may prove to be of great importance in restoration of lung alveolar epithelium and reversion of ground-glass opacity in critically-ill COVID-19 patients. Taking into account the above data, AD-MSCs may also represent a safe and effective therapeutic strategy for COVID-19 patients, and may be the best cellular population option when a great number of MSCs are required for immediate use.
CONCLUSION
MSCs can be potentially applied in COVID-19 as co-therapy without having severe adverse reactions. The exact time point of MSCs administration should be established in order to obtain the best outcome for patients[134]. It has been shown in literature that MSCs can suppress the overactivated immune system of severe and critically severe patients. Simultaneously, MSCs may also possess a prophylactic effect if used at disease onset. Existing evidence suggest that MSCs are important immunoregulatory players, but more research is needed, in order to obtain safer conclusions. The ultimate goal will be to decrease the COVID-19 mortality rate, and this is where MSCs can assist significantly.
Footnotes
Conflict-of-interest statement: The authors declare no conflict of interest.
Manuscript source: Invited manuscript
Peer-review started: May 15, 2020
First decision: June 3, 2020
Article in press: July 19, 2020
Specialty type: Cell and tissue engineering
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Gentile P, Ullah M S-Editor: Yan JP L-Editor: Filipodia P-Editor: Wu YXJ
Contributor Information
Panagiotis Mallis, Hellenic Cord Blood Bank, Biomedical Research Foundation Academy of Athens, Athens 11527, Greece. pmallis@bioacademy.gr.
Efstathios Michalopoulos, Hellenic Cord Blood Bank, Biomedical Research Foundation Academy of Athens, Athens 11527, Greece.
Theofanis Chatzistamatiou, Hellenic Cord Blood Bank, Biomedical Research Foundation Academy of Athens, Athens 11527, Greece.
Catherine Stavropoulos-Giokas, Hellenic Cord Blood Bank, Biomedical Research Foundation Academy of Athens, Athens 11527, Greece.
References
- 1.Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J Med Virol. 2020;92:401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents. 2020;55:105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johns Hopkins University of Medicine. COVID-19 Map. 2020 [cited 7 May 2020] Available from: https://coronavirus.jhu.edu/map.html. [Google Scholar]
- 5.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yuan S, Liao Z, Huang H, Jiang B, Zhang X, Wang Y, Zhao M. Comparison of the Indicators of Psychological Stress in the Population of Hubei Province and Non-Endemic Provinces in China During Two Weeks During the Coronavirus Disease 2019 (COVID-19) Outbreak in February 2020. Med Sci Monit. 2020;26:e923767. doi: 10.12659/MSM.923767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang, Lin M, Wei L, Xie L, Zhu G, Dela Cruz CS, Sharma L. Epidemiologic and Clinical Characteristics of Novel Coronavirus Infections Involving 13 Patients Outside Wuhan, China. JAMA. 2020;323:1092–1093. doi: 10.1001/jama.2020.1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ye Q, Wang B, Mao J. The pathogenesis and treatment of the `Cytokine Storm' in COVID-19. J Infect. 2020;80:607–613. doi: 10.1016/j.jinf.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ HLH Across Speciality Collaboration, UK. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Law HK, Cheung CY, Ng HY, Sia SF, Chan YO, Luk W, Nicholls JM, Peiris JS, Lau YL. Chemokine up-regulation in SARS-coronavirus-infected, monocyte-derived human dendritic cells. Blood. 2005;106:2366–2374. doi: 10.1182/blood-2004-10-4166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prompetchara E, Ketloy C, Palaga T. Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic. Asian Pac J Allergy Immunol. 2020;38:1–9. doi: 10.12932/AP-200220-0772. [DOI] [PubMed] [Google Scholar]
- 12.Li T, Lu H, Zhang W. Clinical observation and management of COVID-19 patients. Emerg Microbes Infect. 2020;9:687–690. doi: 10.1080/22221751.2020.1741327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwartz DA. An Analysis of 38 Pregnant Women with COVID-19, Their Newborn Infants, and Maternal-Fetal Transmission of SARS-CoV-2: Maternal Coronavirus Infections and Pregnancy Outcomes. Arch Pathol Lab Med. 2020 doi: 10.5858/arpa.2020-0901-SA. [DOI] [PubMed] [Google Scholar]
- 14.Chen D, Yang H, Cao Y, Cheng W, Duan T, Fan C, Fan S, Feng L, Gao Y, He F, He J, Hu Y, Jiang Y, Li Y, Li J, Li X, Li X, Lin K, Liu C, Liu J, Liu X, Pan X, Pang Q, Pu M, Qi H, Shi C, Sun Y, Sun J, Wang X, Wang Y, Wang Z, Wang Z, Wang C, Wu S, Xin H, Yan J, Zhao Y, Zheng J, Zhou Y, Zou L, Zeng Y, Zhang Y, Guan X. Expert consensus for managing pregnant women and neonates born to mothers with suspected or confirmed novel coronavirus (COVID-19) infection. Int J Gynaecol Obstet. 2020;149:130–136. doi: 10.1002/ijgo.13146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lu Q, Shi Y. Coronavirus disease (COVID-19) and neonate: What neonatologist need to know. J Med Virol. 2020;92:564–567. doi: 10.1002/jmv.25740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gendelman O, Amital H, Bragazzi NL, Watad A, Chodick G. Continuous hydroxychloroquine or colchicine therapy does not prevent infection with SARS-CoV-2: Insights from a large healthcare database analysis. Autoimmun Rev. 2020;19:102566. doi: 10.1016/j.autrev.2020.102566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou G, Zhao Q. Perspectives on therapeutic neutralizing antibodies against the Novel Coronavirus SARS-CoV-2. Int J Biol Sci. 2020;16:1718–1723. doi: 10.7150/ijbs.45123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dzik S. COVID-19 Convalescent Plasma: Now Is the Time for Better Science. Transfus Med Rev. 2020 doi: 10.1016/j.tmrv.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ullah M. Novel coronavirus (covid-19) treatment options. 2020. [Google Scholar]
- 20.Sheahan TP, Sims AC, Leist SR, Schäfer A, Won J, Brown AJ, Montgomery SA, Hogg A, Babusis D, Clarke MO, Spahn JE, Bauer L, Sellers S, Porter D, Feng JY, Cihlar T, Jordan R, Denison MR, Baric RS. Comparative therapeutic efficacy of remdesivir and combination lopinavir, ritonavir, and interferon beta against MERS-CoV. Nat Commun. 2020;11:222. doi: 10.1038/s41467-019-13940-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, Shi Z, Hu Z, Zhong W, Xiao G. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30:269–271. doi: 10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agostini ML, Andres EL, Sims AC, Graham RL, Sheahan TP, Lu X, Smith EC, Case JB, Feng JY, Jordan R, Ray AS, Cihlar T, Siegel D, Mackman RL, Clarke MO, Baric RS, Denison MR. Coronavirus Susceptibility to the Antiviral Remdesivir (GS-5734) Is Mediated by the Viral Polymerase and the Proofreading Exoribonuclease. mBio. 2018;9:e00221–18. doi: 10.1128/mBio.00221-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tseng CT, Sbrana E, Iwata-Yoshikawa N, Newman PC, Garron T, Atmar RL, Peters CJ, Couch RB. Immunization with SARS coronavirus vaccines leads to pulmonary immunopathology on challenge with the SARS virus. PLoS One. 2012;7:e35421. doi: 10.1371/journal.pone.0035421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ahn DG, Shin HJ, Kim MH, Lee S, Kim HS, Myoung J, Kim BT, Kim SJ. Current Status of Epidemiology, Diagnosis, Therapeutics, and Vaccines for Novel Coronavirus Disease 2019 (COVID-19) J Microbiol Biotechnol. 2020;30:313–324. doi: 10.4014/jmb.2003.03011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salem HK, Thiemermann C. Mesenchymal stromal cells: current understanding and clinical status. Stem Cells. 2010;28:585–596. doi: 10.1002/stem.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gentile P, Sterodimas A. Adipose-derived stromal stem cells (ASCs) as a new regenerative immediate therapy combating coronavirus (COVID-19)-induced pneumonia. Expert Opin Biol Ther. 2020;20:711–716. doi: 10.1080/14712598.2020.1761322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gentile P, Sterodimas A. Adipose Stem Cells (ASCs) and Stromal Vascular Fraction (SVF) as a Potential Therapy in Combating (COVID-19)-Disease. Aging Dis. 2020;11:465–469. doi: 10.14336/AD.2020.0422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rogers CJ, Harman RJ, Bunnell BA, Schreiber MA, Xiang C, Wang FS, Santidrian AF, Minev BR. Rationale for the clinical use of adipose-derived mesenchymal stem cells for COVID-19 patients. J Transl Med. 2020;18:203. doi: 10.1186/s12967-020-02380-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yagi H, Soto-Gutierrez A, Parekkadan B, Kitagawa Y, Tompkins RG, Kobayashi N, Yarmush ML. Mesenchymal stem cells: Mechanisms of immunomodulation and homing. Cell Transplant. 2010;19:667–679. doi: 10.3727/096368910X508762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.International Committee on Taxonomy of Viruses. 2020 [cited 7 May 2020]. Available from: https://talk.ictvonline.org/information/w/news/1300/page. [Google Scholar]
- 31.Wang Q, Zhang Y, Wu L, Niu S, Song C, Zhang Z, Lu G, Qiao C, Hu Y, Yuen KY, Wang Q, Zhou H, Yan J, Qi J. Structural and Functional Basis of SARS-CoV-2 Entry by Using Human ACE2. Cell. 2020;181:894–904.e9. doi: 10.1016/j.cell.2020.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell. 2020;181:281–292.e6. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen L, Liu W, Zhang Q, Xu K, Ye G, Wu W, Sun Z, Liu F, Wu K, Zhong B, Mei Y, Zhang W, Chen Y, Li Y, Shi M, Lan K, Liu Y. RNA based mNGS approach identifies a novel human coronavirus from two individual pneumonia cases in 2019 Wuhan outbreak. Emerg Microbes Infect. 2020;9:313–319. doi: 10.1080/22221751.2020.1725399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jiang S, Du L, Shi Z. An emerging coronavirus causing pneumonia outbreak in Wuhan, China: calling for developing therapeutic and prophylactic strategies. Emerg Microbes Infect. 2020;9:275–277. doi: 10.1080/22221751.2020.1723441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, Chen J, Meng Y, Wang J, Lin Y, Yuan J, Xie Z, Ma J, Liu WJ, Wang D, Xu W, Holmes EC, Gao GF, Wu G, Chen W, Shi W, Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ren LL, Wang YM, Wu ZQ, Xiang ZC, Guo L, Xu T, Jiang YZ, Xiong Y, Li YJ, Li XW, Li H, Fan GH, Gu XY, Xiao Y, Gao H, Xu JY, Yang F, Wang XM, Wu C, Chen L, Liu YW, Liu B, Yang J, Wang XR, Dong J, Li L, Huang CL, Zhao JP, Hu Y, Cheng ZS, Liu LL, Qian ZH, Qin C, Jin Q, Cao B, Wang JW. Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study. Chin Med J (Engl) 2020;133:1015–1024. doi: 10.1097/CM9.0000000000000722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wrapp D, De Vlieger D, Corbett KS, Torres GM, Wang N, Van Breedam W, Roose K, van Schie L VIB-CMB COVID-19 Response Team, Hoffmann M, Pöhlmann S, Graham BS, Callewaert N, Schepens B, Saelens X, McLellan JS. Structural Basis for Potent Neutralization of Betacoronaviruses by Single-Domain Camelid Antibodies. Cell. 2020;181:1004–1015.e15. doi: 10.1016/j.cell.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, Graham BS, McLellan JS. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367:1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, Müller MA, Drosten C, Pöhlmann S. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181:271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen YW, Lee MS, Lucht A, Chou FP, Huang W, Havighurst TC, Kim K, Wang JK, Antalis TM, Johnson MD, Lin CY. TMPRSS2, a serine protease expressed in the prostate on the apical surface of luminal epithelial cells and released into semen in prostasomes, is misregulated in prostate cancer cells. Am J Pathol. 2010;176:2986–2996. doi: 10.2353/ajpath.2010.090665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Song H, Seddighzadeh B, Cooperberg MR, Huang FW. Expression of ACE2, the SARS-CoV-2 receptor, and TMPRSS2 in prostate epithelial cells. 2020 Preprint. Available from: bioRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vaarala MH, Porvari KS, Kellokumpu S, Kyllönen AP, Vihko PT. Expression of transmembrane serine protease TMPRSS2 in mouse and human tissues. J Pathol. 2001;193:134–140. doi: 10.1002/1096-9896(2000)9999:9999<::AID-PATH743>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 44.Lin L, Lu L, Cao W, Li T. Hypothesis for potential pathogenesis of SARS-CoV-2 infection-a review of immune changes in patients with viral pneumonia. Emerg Microbes Infect. 2020;9:727–732. doi: 10.1080/22221751.2020.1746199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen Y, Li L. SARS-CoV-2: virus dynamics and host response. Lancet Infect Dis. 2020;20:515–516. doi: 10.1016/S1473-3099(20)30235-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R. COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020;24:91–98. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Leng Z, Zhu R, Hou W, Feng Y, Yang Y, Han Q, Shan G, Meng F, Du D, Wang S, Fan J, Wang W, Deng L, Shi H, Li H, Hu Z, Zhang F, Gao J, Liu H, Li X, Zhao Y, Yin K, He X, Gao Z, Wang Y, Yang B, Jin R, Stambler I, Lim LW, Su H, Moskalev A, Cano A, Chakrabarti S, Min KJ, Ellison-Hughes G, Caruso C, Jin K, Zhao RC. Transplantation of ACE2- Mesenchymal Stem Cells Improves the Outcome of Patients with COVID-19 Pneumonia. Aging Dis. 2020;11:216–228. doi: 10.14336/AD.2020.0228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Conti P, Ronconi G, Caraffa A, Gallenga CE, Ross R, Frydas I, Kritas SK. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVI-19 or SARS-CoV-2): anti-inflammatory strategies. J Biol Regul Homeost Agents. 2020;34:1. doi: 10.23812/CONTI-E. [DOI] [PubMed] [Google Scholar]
- 49.Rahmati M, Moosavi MA. Cytokine-targeted therapy in severely ill covid-19 patients: Options and cautions. E. ur J Med Oncol. 2020;4:179–180. [Google Scholar]
- 50.Wan S, Yi Q, Fan S, Lv J, Zhang X, Guo L, Lang C, Xiao Q, Xiao K, Yi Z, Qiang M, Xiang J, Zhang B, Chen Y. Characteristics of lymphocyte subsets and cytokines in peripheral blood of 123 hospitalized 3 patients with 2019 novel coronavirus pneumonia (NCP). 2020 Preprint. Available from: medRxiv. [Google Scholar]
- 51.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Liu S, Zhao P, Liu H, Zhu L, Tai Y, Bai C, Gao T, Song J, Xia P, Dong J, Zhao J, Wang FS. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shi Y, Wang Y, Shao C, Huang J, Gan J, Huang X, Bucci E, Piacentini M, Ippolito G, Melino G. COVID-19 infection: the perspectives on immune responses. Cell Death Differ. 2020;27:1451–1454. doi: 10.1038/s41418-020-0530-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bell TJ, Brand OJ, Morgan DJ, Salek-Ardakani S, Jagger C, Fujimori T, Cholewa L, Tilakaratna V, Östling J, Thomas M, Day AJ, Snelgrove RJ, Hussell T. Defective lung function following influenza virus is due to prolonged, reversible hyaluronan synthesis. Matrix Biol. 2019;80:14–28. doi: 10.1016/j.matbio.2018.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Collum SD, Chen NY, Hernandez AM, Hanmandlu A, Sweeney H, Mertens TCJ, Weng T, Luo F, Molina JG, Davies J, Horan IP, Morrell NW, Amione-Guerra J, Al-Jabbari O, Youker K, Sun W, Rajadas J, Bollyky PL, Akkanti BH, Jyothula S, Sinha N, Guha A, Karmouty-Quintana H. Inhibition of hyaluronan synthesis attenuates pulmonary hypertension associated with lung fibrosis. Br J Pharmacol. 2017;174:3284–3301. doi: 10.1111/bph.13947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jiang S, Hillyer C, Du L. Neutralizing Antibodies against SARS-CoV-2 and Other Human Coronaviruses. Trends Immunol. 2020;41:355–359. doi: 10.1016/j.it.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kabat M, Bobkov I, Kumar S, Grumet M. Trends in mesenchymal stem cell clinical trials 2004-2018: Is efficacy optimal in a narrow dose range? Stem Cells Transl Med. 2020;9:17–27. doi: 10.1002/sctm.19-0202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mushahary D, Spittler A, Kasper C, Weber V, Charwat V. Isolation, cultivation, and characterization of human mesenchymal stem cells. Cytometry A. 2018;93:19–31. doi: 10.1002/cyto.a.23242. [DOI] [PubMed] [Google Scholar]
- 58.Bianco P, Robey PG, Simmons PJ. Mesenchymal stem cells: revisiting history, concepts, and assays. Cell Stem Cell. 2008;2:313–319. doi: 10.1016/j.stem.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop Dj, Horwitz Z. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8:315–317. doi: 10.1080/14653240600855905. [DOI] [PubMed] [Google Scholar]
- 60.Viswanathan S, Shi Y, Galipeau J, Krampera M, Leblanc K, Martin I, Nolta J, Phinney DG, Sensebe L. Mesenchymal stem versus stromal cells: International Society for Cell & Gene Therapy (ISCT®) Mesenchymal Stromal Cell committee position statement on nomenclature. Cytotherapy. 2019;21:1019–1024. doi: 10.1016/j.jcyt.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 61.Saleh M, Shamsasanjan K, Movassaghpourakbari A, Akbarzadehlaleh P, Molaeipour Z. The Impact of Mesenchymal Stem Cells on Differentiation of Hematopoietic Stem Cells. Adv Pharm Bull. 2015;5:299–304. doi: 10.15171/apb.2015.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Troyer DL, Weiss ML. Wharton's jelly-derived cells are a primitive stromal cell population. Stem Cells. 2008;26:591–599. doi: 10.1634/stemcells.2007-0439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Baer PC, Geiger H. Adipose-derived mesenchymal stromal/stem cells: tissue localization, characterization, and heterogeneity. Stem Cells Int. 2012;2012:812693. doi: 10.1155/2012/812693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Marion NW, Mao JJ. Mesenchymal stem cells and tissue engineering. Methods Enzymol. 2006;420:339–361. doi: 10.1016/S0076-6879(06)20016-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Galipeau J. Mesenchymal Stromal Cells for Graft-versus-Host Disease: A Trilogy. Biol Blood Marrow Transplant. 2020;26:e89–e91. doi: 10.1016/j.bbmt.2020.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Figueroa FE, Carrión F, Villanueva S, Khoury M. Mesenchymal stem cell treatment for autoimmune diseases: a critical review. Biol Res. 2012;45:269–277. doi: 10.4067/S0716-97602012000300008. [DOI] [PubMed] [Google Scholar]
- 67.Han Y, Li X, Zhang Y, Han Y, Chang F, Ding J. Mesenchymal Stem Cells for Regenerative Medicine. Cells. 2019;8:886. doi: 10.3390/cells8080886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Protogerou V, Beshari SE, Michalopoulos E, Mallis P, Chrysikos D, Samolis AA, Stavropoulos-Giokas C, Troupis T. The Combined Use of Stem Cells and Platelet Lysate Plasma for the Treatment of Erectile Dysfunction: A Pilot Study-6 Months Results. Medicines (Basel) 2020;7:14. doi: 10.3390/medicines7030014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Protogerou V, Michalopoulos E, Mallis P, Gontika I, Dimou Z, Liakouras C, Stavropoulos-Giokas C, Kostakopoulos N, Chrisofos M, Deliveliotis C. Administration of Adipose Derived Mesenchymal Stem Cells and Platelet Lysate in Erectile Dysfunction: A Single Center Pilot Study. Bioengineering (Basel) 2019;6:21. doi: 10.3390/bioengineering6010021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Steens J, Klein D. Current Strategies to Generate Human Mesenchymal Stem Cells In Vitro. Stem Cells Int. 2018;2018:6726185. doi: 10.1155/2018/6726185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Le Blanc K, Tammik C, Rosendahl K, Zetterberg E, Ringdén O. HLA expression and immunologic properties of differentiated and undifferentiated mesenchymal stem cells. Exp Hematol. 2003;31:890–896. doi: 10.1016/s0301-472x(03)00110-3. [DOI] [PubMed] [Google Scholar]
- 72.Devine SM, Bartholomew AM, Mahmud N, Nelson M, Patil S, Hardy W, Sturgeon C, Hewett T, Chung T, Stock W, Sher D, Weissman S, Ferrer K, Mosca J, Deans R, Moseley A, Hoffman R. Mesenchymal stem cells are capable of homing to the bone marrow of non-human primates following systemic infusion. Exp Hematol. 2001;29:244–255. doi: 10.1016/s0301-472x(00)00635-4. [DOI] [PubMed] [Google Scholar]
- 73.Németh K, Leelahavanichkul A, Yuen PS, Mayer B, Parmelee A, Doi K, Robey PG, Leelahavanichkul K, Koller BH, Brown JM, Hu X, Jelinek I, Star RA, Mezey E. Bone marrow stromal cells attenuate sepsis via prostaglandin E(2)-dependent reprogramming of host macrophages to increase their interleukin-10 production. Nat Med. 2009;15:42–49. doi: 10.1038/nm.1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shapouri-Moghaddam A, Mohammadian S, Vazini H, Taghadosi M, Esmaeili SA, Mardani F, Seifi B, Mohammadi A, Afshari JT, Sahebkar A. Macrophage plasticity, polarization, and function in health and disease. J Cell Physiol. 2018;233:6425–6440. doi: 10.1002/jcp.26429. [DOI] [PubMed] [Google Scholar]
- 75.Bernardo ME, Fibbe WE. Mesenchymal stromal cells: sensors and switchers of inflammation. Cell Stem Cell. 2013;13:392–402. doi: 10.1016/j.stem.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 76.Gur-Wahnon D, Borovsky Z, Beyth S, Liebergall M, Rachmilewitz J. Contact-dependent induction of regulatory antigen-presenting cells by human mesenchymal stem cells is mediated via STAT3 signaling. Exp Hematol. 2007;35:426–433. doi: 10.1016/j.exphem.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 77.Mellman I, Steinman RM. Dendritic cells: specialized and regulated antigen processing machines. Cell. 2001;106:255–258. doi: 10.1016/s0092-8674(01)00449-4. [DOI] [PubMed] [Google Scholar]
- 78.Djouad F, Charbonnier LM, Bouffi C, Louis-Plence P, Bony C, Apparailly F, Cantos C, Jorgensen C, Noël D. Mesenchymal stem cells inhibit the differentiation of dendritic cells through an interleukin-6-dependent mechanism. Stem Cells. 2007;25:2025–2032. doi: 10.1634/stemcells.2006-0548. [DOI] [PubMed] [Google Scholar]
- 79.English K, Barry FP, Mahon BP. Murine mesenchymal stem cells suppress dendritic cell migration, maturation and antigen presentation. Immunol Lett. 2008;115:50–58. doi: 10.1016/j.imlet.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 80.Spaggiari GM, Abdelrazik H, Becchetti F, Moretta L. MSCs inhibit monocyte-derived DC maturation and function by selectively interfering with the generation of immature DCs: central role of MSC-derived prostaglandin E2. Blood. 2009;113:6576–6583. doi: 10.1182/blood-2009-02-203943. [DOI] [PubMed] [Google Scholar]
- 81.van Megen KM, van 't Wout ET, Lages Motta J, Dekker B, Nikolic T, Roep BO. Activated Mesenchymal Stromal Cells Process and Present Antigens Regulating Adaptive Immunity. Front Immunol. 2019;10:694. doi: 10.3389/fimmu.2019.00694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Liu Y, Yin Z, Zhang R, Yan K, Chen L, Chen F, Huang W, Lv B, Sun C, Jiang X. MSCs inhibit bone marrow-derived DC maturation and function through the release of TSG-6. Biochem Biophys Res Commun. 2014;450:1409–1415. doi: 10.1016/j.bbrc.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 83.Scalavino V, Liso M, Serino G. Role of microRNAs in the Regulation of Dendritic Cell Generation and Function. Int J Mol Sci. 2020;21:1319. doi: 10.3390/ijms21041319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chen W, Huang Y, Han J, Yu L, Li Y, Lu Z, Li H, Liu Z, Shi C, Duan F, Xiao Y. Immunomodulatory effects of mesenchymal stromal cells-derived exosome. Immunol Res. 2016;64:831–840. doi: 10.1007/s12026-016-8798-6. [DOI] [PubMed] [Google Scholar]
- 85.Haddad R, Saldanha-Araujo F. Mechanisms of T-cell immunosuppression by mesenchymal stromal cells: what do we know so far? Biomed Res Int. 2014;2014:216806. doi: 10.1155/2014/216806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sreeramkumar V, Fresno M, Cuesta N. Prostaglandin E2 and T cells: friends or foes? Immunol Cell Biol. 2012;90:579–586. doi: 10.1038/icb.2011.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ricciotti E, FitzGerald GA. Prostaglandins and inflammation. Arterioscler Thromb Vasc Biol. 2011;31:986–1000. doi: 10.1161/ATVBAHA.110.207449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ryan JM, Barry F, Murphy JM, Mahon BP. Interferon-gamma does not break, but promotes the immunosuppressive capacity of adult human mesenchymal stem cells. Clin Exp Immunol. 2007;149:353–363. doi: 10.1111/j.1365-2249.2007.03422.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ren G, Zhang L, Zhao X, Xu G, Zhang Y, Roberts AI, Zhao RC, Shi Y. Mesenchymal stem cell-mediated immunosuppression occurs via concerted action of chemokines and nitric oxide. Cell Stem Cell. 2008;2:141–150. doi: 10.1016/j.stem.2007.11.014. [DOI] [PubMed] [Google Scholar]
- 90.Wang L, Zhao Y, Shi S. Interplay between mesenchymal stem cells and lymphocytes: implications for immunotherapy and tissue regeneration. J Dent Res. 2012;91:1003–1010. doi: 10.1177/0022034512460404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Davies LC, Heldring N, Kadri N, Le Blanc K. Mesenchymal Stromal Cell Secretion of Programmed Death-1 Ligands Regulates T Cell Mediated Immunosuppression. Stem Cells. 2017;35:766–776. doi: 10.1002/stem.2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Luz-Crawford P, Noël D, Fernandez X, Khoury M, Figueroa F, Carrión F, Jorgensen C, Djouad F. Mesenchymal stem cells repress Th17 molecular program through the PD-1 pathway. PLoS One. 2012;7:e45272. doi: 10.1371/journal.pone.0045272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Franquesa M, Hoogduijn MJ, Bestard O, Grinyó JM. Immunomodulatory effect of mesenchymal stem cells on B cells. Front Immunol. 2012;3:212. doi: 10.3389/fimmu.2012.00212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Fan L, Hu C, Chen J, Cen P, Wang J, Li L. Interaction between Mesenchymal Stem Cells and B-Cells. Int J Mol Sci. 2016;17:650. doi: 10.3390/ijms17050650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Asari S, Itakura S, Ferreri K, Liu CP, Kuroda Y, Kandeel F, Mullen Y. Mesenchymal stem cells suppress B-cell terminal differentiation. Exp Hematol. 2009;37:604–615. doi: 10.1016/j.exphem.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Machado Cde V, Telles PD, Nascimento IL. Immunological characteristics of mesenchymal stem cells. Rev Bras Hematol Hemoter. 2013;35:62–67. doi: 10.5581/1516-8484.20130017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Biassoni R. Natural killer cell receptors. Adv Exp Med Biol. 2008;640:35–52. doi: 10.1007/978-0-387-09789-3_4. [DOI] [PubMed] [Google Scholar]
- 98.Finton KA, Strong RK. Structural insights into activation of antiviral NK cell responses. Immunol Rev. 2012;250:239–257. doi: 10.1111/j.1600-065X.2012.01168.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Casado JG, Tarazona R, Sanchez-Margallo FM. NK and MSCs crosstalk: the sense of immunomodulation and their sensitivity. Stem Cell Rev Rep. 2013;9:184–189. doi: 10.1007/s12015-013-9430-y. [DOI] [PubMed] [Google Scholar]
- 100.Najar M, Fayyad-Kazan M, Meuleman N, Bron D, Fayyad-Kazan H, Lagneaux L. Mesenchymal stromal cells of the bone marrow and natural killer cells: cell interactions and cross modulation. J Cell Commun Signal. 2018;12:673–688. doi: 10.1007/s12079-018-0448-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sangiorgi B, Panepucci RA. Modulation of Immunoregulatory Properties of Mesenchymal Stromal Cells by Toll-Like Receptors: Potential Applications on GVHD. Stem Cells Int. 2016;2016:9434250. doi: 10.1155/2016/9434250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Holt D, Ma X, Kundu N, Fulton A. Prostaglandin E(2) (PGE (2)) suppresses natural killer cell function primarily through the PGE(2) receptor EP4. Cancer Immunol Immunother. 2011;60:1577–1586. doi: 10.1007/s00262-011-1064-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Najar M, Fayyad-Kazan M, Meuleman N, Bron D, Fayyad-Kazan H, Lagneaux L. Immunological impact of Wharton's Jelly mesenchymal stromal cells and natural killer cell co-culture. Mol Cell Biochem. 2018;447:111–124. doi: 10.1007/s11010-018-3297-9. [DOI] [PubMed] [Google Scholar]
- 104.Alegre E, Rizzo R, Bortolotti D, Fernandez-Landázuri S, Fainardi E, González A. Some basic aspects of HLA-G biology. J Immunol Res. 2014;2014:657625. doi: 10.1155/2014/657625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Shiina T, Hosomichi K, Inoko H, Kulski JK. The HLA genomic loci map: expression, interaction, diversity and disease. J Hum Genet. 2009;54:15–39. doi: 10.1038/jhg.2008.5. [DOI] [PubMed] [Google Scholar]
- 106.Mallis P, Boulari D, Michalopoulos E, Dinou A, Spyropoulou-Vlachou M, Stavropoulos-Giokas C. Evaluation of HLA-G Expression in Multipotent Mesenchymal Stromal Cells Derived from Vitrified Wharton's Jelly Tissue. Bioengineering (Basel) 2018;5:95. doi: 10.3390/bioengineering5040095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Rajagopalan S, Long EO. KIR2DL4 (CD158d): An activation receptor for HLA-G. Front Immunol. 2012;3:258. doi: 10.3389/fimmu.2012.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Rizzo R. Immunosupressive properties of hla-g molecules produced by mesenchymal stromal cells. J Transplant Technol Res. 2013 [Google Scholar]
- 109.Rajagopalan S, Bryceson YT, Kuppusamy SP, Geraghty DE, van der Meer A, Joosten I, Long EO. Activation of NK cells by an endocytosed receptor for soluble HLA-G. PLoS Biol. 2006;4:e9. doi: 10.1371/journal.pbio.0040009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Roussev RG, Coulam CB. HLA-G and its role in implantation (review) J Assist Reprod Genet. 2007;24:288–295. doi: 10.1007/s10815-007-9148-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.ClinicalTrials.gov. Available from: https://clinicaltrials.gov/ [Google Scholar]
- 112.Petrou P, Gothelf Y, Argov Z, Gotkine M, Levy YS, Kassis I, Vaknin-Dembinsky A, Ben-Hur T, Offen D, Abramsky O, Melamed E, Karussis D. Safety and Clinical Effects of Mesenchymal Stem Cells Secreting Neurotrophic Factor Transplantation in Patients With Amyotrophic Lateral Sclerosis: Results of Phase 1/2 and 2a Clinical Trials. JAMA Neurol. 2016;73:337–344. doi: 10.1001/jamaneurol.2015.4321. [DOI] [PubMed] [Google Scholar]
- 113.Zhang C, Wu Z, Li JW, Zhao H, Wang GQ. Cytokine release syndrome in severe COVID-19: interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality. Int J Antimicrob Agents. 2020;55:105954. doi: 10.1016/j.ijantimicag.2020.105954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lee JW, Fang X, Krasnodembskaya A, Howard JP, Matthay MA. Concise review: Mesenchymal stem cells for acute lung injury: role of paracrine soluble factors. Stem Cells. 2011;29:913–919. doi: 10.1002/stem.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Iacobaeus E, Kadri N, Lefsihane K, Boberg E, Gavin C, Törnqvist Andrén A, Lilja A, Brundin L, Blanc KL. Short and Long Term Clinical and Immunologic Follow up after Bone Marrow Mesenchymal Stromal Cell Therapy in Progressive Multiple Sclerosis-A Phase I Study. J Clin Med. 2019;8:2102. doi: 10.3390/jcm8122102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wilson JG, Liu KD, Zhuo H, Caballero L, McMillan M, Fang X, Cosgrove K, Vojnik R, Calfee CS, Lee JW, Rogers AJ, Levitt J, Wiener-Kronish J, Bajwa EK, Leavitt A, McKenna D, Thompson BT, Matthay MA. Mesenchymal stem (stromal) cells for treatment of ARDS: a phase 1 clinical trial. Lancet Respir Med. 2015;3:24–32. doi: 10.1016/S2213-2600(14)70291-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Matthay MA, Calfee CS, Zhuo H, Thompson BT, Wilson JG, Levitt JE, Rogers AJ, Gotts JE, Wiener-Kronish JP, Bajwa EK, Donahoe MP, McVerry BJ, Ortiz LA, Exline M, Christman JW, Abbott J, Delucchi KL, Caballero L, McMillan M, McKenna DH, Liu KD. Treatment with allogeneic mesenchymal stromal cells for moderate to severe acute respiratory distress syndrome (START study): a randomised phase 2a safety trial. Lancet Respir Med. 2019;7:154–162. doi: 10.1016/S2213-2600(18)30418-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Gowen A, Shahjin F, Chand S, Odegaard KE, Yelamanchili SV. Mesenchymal Stem Cell-Derived Extracellular Vesicles: Challenges in Clinical Applications. Front Cell Dev Biol. 2020;8:149. doi: 10.3389/fcell.2020.00149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Raposo G, Stoorvogel W. Extracellular vesicles: exosomes, microvesicles, and friends. J Cell Biol. 2013;200:373–383. doi: 10.1083/jcb.201211138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Harrell CR, Jovicic N, Djonov V, Arsenijevic N, Volarevic V. Mesenchymal Stem Cell-Derived Exosomes and Other Extracellular Vesicles as New Remedies in the Therapy of Inflammatory Diseases. Cells. 2019;8:1605. doi: 10.3390/cells8121605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hulsmans M, Holvoet P. MicroRNA-containing microvesicles regulating inflammation in association with atherosclerotic disease. Cardiovasc Res. 2013;100:7–18. doi: 10.1093/cvr/cvt161. [DOI] [PubMed] [Google Scholar]
- 122.Yin K, Wang S, Zhao RC. Exosomes from mesenchymal stem/stromal cells: a new therapeutic paradigm. Biomark Res. 2019;7:8. doi: 10.1186/s40364-019-0159-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Xie M, Xiong W, She Z, Wen Z, Abdirahman AS, Wan W, Wen C. Immunoregulatory Effects of Stem Cell-Derived Extracellular Vesicles on Immune Cells. Front Immunol. 2020;11:13. doi: 10.3389/fimmu.2020.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Saba R, Sorensen DL, Booth SA. MicroRNA-146a: A Dominant, Negative Regulator of the Innate Immune Response. Front Immunol. 2014;5:578. doi: 10.3389/fimmu.2014.00578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zhao T, Sun F, Liu J, Ding T, She J, Mao F, Xu W, Qian H, Yan Y. Emerging Role of Mesenchymal Stem Cell-derived Exosomes in Regenerative Medicine. Curr Stem Cell Res Ther. 2019;14:482–494. doi: 10.2174/1574888X14666190228103230. [DOI] [PubMed] [Google Scholar]
- 126.Deasy BM, Anderson JE, Zeli S. Regulatory issues in the therapeutic use of stem cells. Regen Med Tissue Eng. 2013 [Google Scholar]
- 127.Scioli MG, Bielli A, Gentile P, Cervelli V, Orlandi A. Combined treatment with platelet-rich plasma and insulin favours chondrogenic and osteogenic differentiation of human adipose-derived stem cells in three-dimensional collagen scaffolds. J Tissue Eng Regen Med. 2017;11:2398–2410. doi: 10.1002/term.2139. [DOI] [PubMed] [Google Scholar]
- 128.Gentile P, Scioli MG, Bielli A, Orlandi A, Cervelli V. Concise Review: The Use of Adipose-Derived Stromal Vascular Fraction Cells and Platelet Rich Plasma in Regenerative Plastic Surgery. Stem Cells. 2017;35:117–134. doi: 10.1002/stem.2498. [DOI] [PubMed] [Google Scholar]
- 129.Gentile P. Autologous Cellular Method Using Micrografts of Human Adipose Tissue Derived Follicle Stem Cells in Androgenic Alopecia. Int J Mol Sci. 2019;20:3446. doi: 10.3390/ijms20143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Gentile P, Kothari A, Casella D, Calabrese C. Fat Graft Enhanced With Adipose-Derived Stem Cells in Aesthetic Breast Augmentation: Clinical, Histological, and Instrumental Evaluation. Aesthet Surg J. 2019 doi: 10.1093/asj/sjz292. [DOI] [PubMed] [Google Scholar]
- 131.Gentile P, Casella D, Palma E, Calabrese C. Engineered Fat Graft Enhanced with Adipose-Derived Stromal Vascular Fraction Cells for Regenerative Medicine: Clinical, Histological and Instrumental Evaluation in Breast Reconstruction. J Clin Med. 2019;8:504. doi: 10.3390/jcm8040504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Gentile P, De Angelis B, Pasin M, Cervelli G, Curcio CB, Floris M, Di Pasquali C, Bocchini I, Balzani A, Nicoli F, Insalaco C, Tati E, Lucarini L, Palla L, Pascali M, De Logu P, Di Segni C, Bottini DJ, Cervelli V. Adipose-derived stromal vascular fraction cells and platelet-rich plasma: basic and clinical evaluation for cell-based therapies in patients with scars on the face. J Craniofac Surg. 2014;25:267–272. doi: 10.1097/01.scs.0000436746.21031.ba. [DOI] [PubMed] [Google Scholar]
- 133.Cervelli V, Bocchini I, Di Pasquali C, De Angelis B, Cervelli G, Curcio CB, Orlandi A, Scioli MG, Tati E, Delogu P, Gentile P. P.R.L. platelet rich lipotransfert: our experience and current state of art in the combined use of fat and PRP. Biomed Res Int. 2013;2013:434191. doi: 10.1155/2013/434191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Ullah M. The pandemic of novel coronavirus disease 2019 (covid-19): Need for an immediate action. OAJBS. 2020;2:301–302. [Google Scholar]