Abstract
The COVID-19 pandemic is a global health crisis that requires the application of interdisciplinary research to address numerous knowledge gaps including molecular strategies to prevent viral reproduction in affected individuals. In response to the Frontiers Research Topic, “Coronavirus disease (COVID-19): Pathophysiology, Epidemiology, Clinical Management, and Public Health Response,” this Hypothesis article proposes a novel therapeutic strategy to repurpose metabotropic glutamate 5 receptor (mGluR5) inhibitors to interfere with viral hijacking of the host protein synthesis machinery. We review pertinent background on SARS-CoV-2, fragile X syndrome (FXS) and metabotropic glutamate receptor 5 (mGluR5) and provide a mechanistic-based hypothesis and preliminary data to support testing mGluR5 inhibitors in COVID-19 research.
Keywords: coronavirus, COVID-19, fragile X mental retardation protein, metabotropic glutamate receptor 5, protein synthesis
Introduction
In December of 2019, an outbreak of respiratory disease began in Wuhan, China. The causative agent was a novel betacoronavirus of the same subgenus as severe acute respiratory syndrome (SARS) coronavirus (CoV) and was named SARS-CoV-2, a.k.a. novel CoV (nCoV-2019), which causes the disease coronavirus-19 (COVID-19) (Zhu et al., 2020). COVID-19 quickly spread worldwide with clinical manifestations ranging from mild respiratory symptoms to severe pneumonia and fatality. We submit this Hypothesis paper as an interdisciplinary research approach supporting a molecular-based therapeutic strategy to reduce virus reproduction in individuals infected with SARS-CoV-2. Specifically, we provide the conceptional framework to support testing metabotropic glutamate receptor 5 (mGluR5) inhibitors to attenuate virus reproduction. Inhibitors of mGluR5 have been extensively studied in the neurodevelopmental disorder fragile X syndrome (FXS) as well as other psychiatric disorders (Gravius et al., 2010; Michalon et al., 2012; Scharf et al., 2015; Berry-Kravis et al., 2017). Inhibition of mGluR5 represses exaggerated protein synthesis that occurs in the absence of the RNA binding protein fragile X mental retardation protein (FMRP) (Bear et al., 2004; Osterweil et al., 2010). Work by Soto-Acosta and colleagues in 2018 demonstrates that FMRP represses Zika virus (ZIKV) infection by blocking viral RNA translation (Soto-Acosta et al., 2018). Thus, we propose that mGluR5 inhibitors may be a viable therapeutic strategy to interfere with the ability of SARS-CoV-2 to hijack the host cell translational machinery.
Conceptual Framework
SARS-CoV-2
SARS-CoV-2 is a betacoronavirus of the same family as Middle East Respiratory Syndrome (MERS-CoV) and SARS-CoV (Zhu et al., 2020). Betacoronaviruses are enveloped, non-segmented, positive-sense, single-stranded RNA [ssRNA(+)] viruses of zoonotic origin that replicate in the host cell cytoplasm and induce fever and respiratory symptoms. Infection starts by attachment of the receptor binding domain of the spike protein to host cell receptors, which mediates endocytosis of the virus into the cell and release of the ssRNA(+) viral genome into the cytoplasm. The SARS-CoV-2 and SARS-CoV receptor binding domains of spike protein share angiotensin-converting enzyme 2 (ACE2) as the host cell receptor (Li et al., 2003; Li, 2015; Wan et al., 2020). Protein-protein docking experiments and molecular dynamics (MD) simulations indicate that SARS-CoV-2 binds to ACE2 with a higher affinity than SARS-CoV, but the interaction is more temperature sensitive (He et al., 2020). These data may explain why SARS-CoV-2 is more infectious than SARS-CoV and suggest that the infection ability of SARS-CoV-2 will decline faster. Once inside the host cell, the coronavirus ssRNA(+) viral genome is used as a template to synthesize viral proteins. The viral RNA (vRNA) appears to evade the host immune system by mimicking cellular mRNA. When a critical mass of new virions are manufactured, they bud at membranes of the endoplasmic reticulum and/or Golgi apparatus and are released by exocytosis.
Regarding post-transcriptional regulation of CoV RNAs, the ∼30 kb viral RNA includes a 5′-leader sequence, 5′-untranslated region (UTR), coding sequences for viral proteins, 3′-UTR and poly(A) tail (Fehr and Perlman, 2015). The 5′-proximal two-thirds of the RNA encodes the replicase mRNA that contains 2 open reading frames, ORF1a and ORF1b. The 3′ third of CoV RNA encodes structural and accessory proteins. First, the viral RNA is translated to generate viral proteins required for transcription. Translation of ORF1a yields polyprotein 1a (pp1a), and a −1 ribosomal frame shift translates ORB1b to yield pp1ab. Together these polyproteins are processed into 16 non-structural proteins, which drive viral RNA replication and subgenomic mRNA (sgmRNA) synthesis. Specifically, the ssRNA(+) viral genome is a template for synthesis of double stranded (dsRNA), which is transcribed, thereby providing new ssRNA(+) viral genomes as well as nested sets of subgenomic mRNAs (sgmRNA) that encode structural proteins. The sgmRNA, like the RNA genome, can function as a template for negative strand RNA synthesis (Wu and Brian, 2010).
Of relevance to our hypothesis, the virus needs to commandeer the host cell protein synthesis machinery in order to propagate. Protein synthesis is dependent on the interactions between trans factors (RNA binding proteins, RBP) and cis-regulatory RNA elements. Specifically, cis-regulatory elements in CoV RNA need to interact with host cell RBP to translate viral mRNA. The detailed RNA-protein interactions that mediate the post-transcriptional gene regulation of SARS-CoV-2 RNA remain to be determined; however, we can predict pivotal players based on current literature. We hypothesize that FMRP, which functions as a protein synthesis inhibitor, is a pivotal molecular player and that drugs under investigation to reduce exaggerated protein synthesis in FXS may be applicable to attenuate viral protein synthesis.
Fragile X Syndrome, FMRP and ZIKV Subgenomic RNA
Fragile X syndrome is a neurodevelopmental disorder clinically characterized by low IQ, autistic-like behaviors and seizures (Hagerman and Hagerman, 2002). FXS results from a mutation in the FMR1 gene on the X chromosome, which is associated with transcriptional silencing of the FMR1 promoter and loss of expression of FMRP (Verkerk et al., 1991). FMRP is a mRNA binding protein that associates with polysomes or non-translating ribonucleoprotein (RNP) particles and is involved in the transport, localization and translational repression of hundreds of mRNAs (Feng et al., 1997a, b; Weiler et al., 1997; Brown et al., 2001; Darnell et al., 2001; Laggerbauer et al., 2001; Li et al., 2001; Mazroui et al., 2002; Miyashiro et al., 2003; Bagni and Greenough, 2005).
In 2018, Soto-Acosta and colleagues published an article, “Fragile X mental retardation protein is a Zika virus restriction factor that is antagonized by subgenomic flaviviral RNA” (Soto-Acosta et al., 2018). Briefly, FMRP is a host factor that inhibits ZIKV translation by binding to the 3′-UTR of ZIKV subgenomic flavivirus RNAs (sfRNAs). The flavivirus life cycle is completely dependent on the cytoplasmic fate of one RNA species, namely the genomic vRNA, whose replication occurs entirely in the cytoplasm and does not generate any DNA intermediates. To create an environment favorable to infection, flaviviruses have evolved mechanisms to dampen antiviral processes, notably through the production of specific vRNA degradation products termed subgenomic flavivirus RNA (sfRNA). sfRNAs are RNAs produced by the viral replication machinery but do not contribute to synthesizing viral proteins and are non-infectious (Mazeaud et al., 2018; Berthoux, 2020). These sfRNAs bind to and inhibit the activity of host proteins that would normally block virus multiplication. FMRP is one of those proteins that binds to Zika sfRNA and inhibits the production of viral proteins. In the absence of FMRP, both the rate of infection and translation of viral protein increase per cell; i.e., knockdown of FMRP increases the infection rate ∼50–80%. Soto-Acosta and colleagues hypothesized that because FMRP is a known repressor of cellular mRNA translation, that translation of ZIKV is inhibited by FMRP early after infection thus reducing ZIKV infection, but as infection progresses, sfRNA antagonizes FMRP function leading to increased expression of FMRP target genes. Overall, the findings by Soto-Acosta et al. strongly suggest that FMRP plays a pivotal role in ZIKV infection and pathogenesis through regulation of protein synthesis.
Over two decades of studies elucidating the function of FMRP demonstrate that this RBP regulates cellular protein synthesis through multiple mechanisms including stalling polyribosomes, associating with miRNA and mRNA ribonucleoprotein complexes, and regulating the formation of RNA granules including processing (P)-bodies and stress granules (Lai et al., 2020). FMRP interacts with at least 180 other proteins of which 30% are ribosomal assembly factors (Taha et al., 2020). Thus, lack of expression of this pivotal translation regulator in FXS, or sequestration of FMRP by viral RNA, is expected to have large effects on cellular protein synthesis. Negative allosteric modulation of mGluR5 rescues elevated protein synthesis in mouse models of FXS and tuberous sclerosis (Michalon et al., 2012; Kelly et al., 2018).
Fragile X Syndrome, FMRP and the Immune System
Interestingly, FXS is associated with dysregulation of the immune system, with an over-representation of infectious diseases and an under-representation of autoimmune disorders (Yu et al., 2020). Patients with FXS exhibit a significantly altered cytokine profile compared to controls. Plasma protein levels of the cytokine IL-1α are elevated and numerous serum chemokines are reduced (Ashwood et al., 2010; Van Dijck et al., 2020). The reduced levels of pro-inflammatory chemokines may indicate that the FXS immune system has a decreased capacity to respond to infection. Of importance, activation of peripheral blood mononuclear cells (PBMC) from patients with FXS with a group 1 mGluR agonist results in increased production of pro-inflammatory cytokines compared to PBMC from control subjects (Careaga et al., 2014a). The increase in cytokine production can be blocked with an mGluR5 antagonist. In addition to cytokine profiles, patients with FXS have an increased propensity to exhibit elevated serum anti-neuronal antibodies (43% of males) (Lisik et al., 2015). Non-human FXS models also exhibit dysregulation of the immune system. Drosophila melanogaster Fmr1 mutants are defective in controlling bacterial infection by S. pneumoniae or S. marcescens compared to wild type flies (O’Connor et al., 2017). Peripheral immune system function appears normal in Fmr1KO mice, but the mutant mice exhibit elevated hippocampal IL-1β and IL-6 mRNA compared to wild type controls at 4 h post-stimulation with lipopolysaccharide (Yuskaitis et al., 2010; Hodges et al., 2020). In contrast to full-mutation FXS, women carriers with the FXS premutation have an increased comorbidity of immune-mediated disorders and decreased cytokine production of GM-CSF and IL-12 (p40) compared to controls (Winarni et al., 2012; Careaga et al., 2014b; Jalnapurkar et al., 2015). Overall, these studies suggest that altered FMRP levels are associated with aberrant immune system function. It remains to be determined if persons with FXS are more susceptible to infection by SARS-CoV-2 and other viruses, and conversely, if the FMR1 premutation is protective against viral infection.
SARS-CoV-2 Negative Sense RNA Contains a Canonical FMRP Binding Site
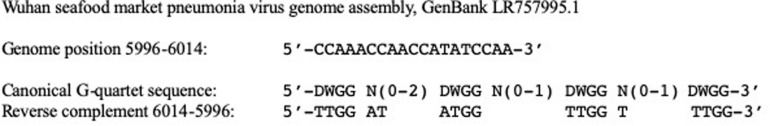
Fragile X mental retardation protein binds to hundreds of cellular target mRNAs and predominantly functions to reversibly stall ribosomal translocation of messages (Darnell et al., 2011). It is of interest to determine if FMRP is a host cell factor that binds to SARS-CoV-2 genomic RNA or sgRNA as part of a regulatory mechanism involved in SARS-CoV-2 mRNA translation. FMRP binds to target RNAs via G-quartet cis-regulatory elements through the consensus sequence 5′-DWGG N(0–2) DWGG N(0–1) DWGG N(0–1) DWGG-3′ where D = A, G or U and W = A or U (Darnell et al., 2001). Based on sequence analysis of the whole genome of the Wuhan seafood market pneumonia virus genome assembly (GenBank LR757995.1), we predict that FMRP binds to negative sense of SARS-CoV-2 RNA. Specifically, there is a canonical G-quartet sequence from nucleotides 6014-5996 (Figure 1). FMRP also binds to target RNA through kissing complex cis-elements with the consensus site 5′-GGGCKAAGGARK……. KAGCGRCUGG-3′ where K = G or U and R = G or A (Darnell et al., 2005). We did not find any kissing complex sequences in the positive or negative sense of SARS-Cov-2 RNA. We predict that binding of FMRP to negative sense of SARS-CoV-2 RNA sequesters FMRP such that it cannot act as a translational brake for vRNA synthesis, similar to the role sfRNA plays in antagonizing FMRP function in ZIKV.
FIGURE 1.
SARS-Cov-2 negative sense RNA contains a canonical G-quartet FMRP binding site. FMRP binds to target RNAs via G-quartet cis-regulatory elements through the consensus sequence 5′-DWGG N(0–2) DWGG N(0–1) DWGG N(0–1) DWGG-3′ where D = any nucleotide except C and W = A or U. The whole genome sequence of the Wuhan seafood market pneumonia virus genome assembly (GenBank LR757995.1) contains a canonical G-quartet sequence at nucleotides 6014-5996 of negative sense of SARS-CoV-2 RNA. The corresponding negative sense sequence is: 5′-TTGG-AT-ATGG-TTGG-T-TTGG-3′.
Molecular Modeling Predicts That FMRP Binds to SARS-CoV-2 Positive and Negative Sense RNAs
Understanding how SARS-CoV-2 interferes with RNA-related posttranscriptional processes could identify novel therapies (Maranon et al., 2020). We utilized the catRAPID algorithm1 to predict RNA/protein interactions relevant to SARS-CoV-2 RNA (GenBank LR757995.1). This algorithm identifies potential interactions between protein and RNA molecules by combining the contributions of secondary structure, hydrogen binding and van der Waal’s forces to generate an interaction profile (Bellucci et al., 2011; Agostini et al., 2013; Cirillo et al., 2013). First, we utilized catRAPID omics to compute which RBP are predicted to bind to positive and negative sense SARS-CoV-2 RNAs. Top-ranked RBP included several splicing and heterogeneous nuclear ribonucleoproteins (Table 1). FMRP exhibited an average interaction strength of 0.30 (range 0–0.95) with an average star value of 2.58 (range 2.35–2.75) for positive sense SARS-CoV-2 RNA based on 242 predicted interactions where 57 of those interactions had an intensity ≥0.5, which is indicative of high specificity for the interaction. FMRP exhibited an average interaction strength of 0.27 (range 0–0.99) with an average star value of 2.54 (range 2.34–2.74) for negative sense SARS-CoV-2 RNA based on 42 predicted interactions where 8 interactions had an intensity ≥0.5. The interaction strength (enrichment with respect to random interactions) was computed using a reference set of 100 random protein and 100 random RNA sequences having the same lengths as the molecules under investigation, and the star rating system is a score representing the sum of the catRAPID normalized propensity, the presence of RNA/DNA binding domains and disordered regions, and the presence of known RNA-binding motifs with the range of 0–3 (Agostini et al., 2013; Cirillo et al., 2013).
TABLE 1.
Top catRAPID hits for RBP that bind to SARS-CoV-2 RNA.
| Positive Strand | |
| CSTF2 | Cleavage stimulation factor subunit 2 |
| ESRP2 | Epithelial splicing regulatory protein 2 |
| FUS | RNA-binding protein FUS |
| SRSF3 | Serine/arginine-rich splicing factor 3 |
| SRSF4 | Serine/arginine-rich splicing factor 4 |
| SRSF5 | Serine/arginine-rich splicing factor 5 |
| SRS10 | Serine/arginine-rich splicing factor 10 |
| SSB | Lupus La protein |
| YBX1 | Y-box-binding protein 1 |
| Negative Strand | |
| ESRP2 | Epithelial splicing regulatory protein 2 |
| HNRNPF | Heterogeneous nuclear ribonucleoprotein F |
| HNRNPH1 | Heterogeneous nuclear ribonucleoprotein H |
| HNRNPH2 | Heterogeneous nuclear ribonucleoprotein H2 |
| QK1 | Protein quaking |
| SFPQ | Splicing factor, proline- and glutamine-rich |
| SRSF3 | Serine/arginine-rich splicing factor 3 |
| SRSF5 | Serine/arginine-rich splicing factor 5 |
| TIA1 | Nucleolysin TIA-1 isoform p40 |
| TRA2B | Transformer-2 protein homolog beta |
Second, we utilized catRAPID Global Score with uniform fragmentation to predict FMRP (GenBank AAH86957.1)/SARS-CoV-2 interactions. The Global Score predicts the overall interaction ability of a protein-RNA pair based on an algorithm trained on data generated by photoactivatable ribonucleoside-enhanced, high-throughput sequencing of RNA isolated by crosslinking and immunoprecipitation (PAR/HITS-CLIP) (Hafner et al., 2010). The Global Scores were 0.97 for positive sense and 0.84 for negative sense SARS-CoV-2 RNA and FMRP. The top 20 predicted interaction sites were between nucleotides 11,365–12,560 for both positive and negative sense SARS-CoV-2 RNA (interaction propensity range 279–417). Additional RNA fragments with the highest interaction propensities are listed in Table 2. The fragment of FMRP with the highest binding activity for both positive and negative sense SARS-CoV-2 RNA encompassed amino acids 311–362, which partially overlaps with a known KH RNA binding domain in FMRP (amino acids 283–325) (Siomi et al., 1994). Other FMRP protein regions with high predicted binding affinity for nucleotides 11,365–12,560 for both positive and negative sense SARS-CoV-2 RNA overlapped or partially overlapped with known Agenet (63–120) KH1 (221–280), KH2 (283–325), C-terminal (C1, 399–526), and C2 (504–586) domains as well as intervening FMRP protein sequences.
TABLE 2.
Top catRAPID hits of SARS-CoV-2 that bind to FMRP.
| Fragment | Interaction Propensity |
| Positive Strand | |
| 11365–12560 | 416.94 |
| 7783–8978 | 274.98 |
| 1216–2411 | 267.13 |
| 3007–4002 | 265.21 |
| 3604–4799 | 264.88 |
| 4798–5993 | 263.82 |
| 8380–9575 | 263.65 |
| 7186–8381 | 262.81 |
| 4201–5396 | 256.57 |
| 2410–3605 | 253.78 |
| Negative Strand | |
| 11365–12560 | 413.11 |
| 7186–8381 | 272.08 |
| 4798–5993 | 268.10 |
| 7783–8978 | 267.37 |
| 10171–11366 | 261.15 |
| 5992–7187 | 259.99 |
| 5395–6590 | 257.13 |
| 9574–10769 | 255.20 |
| 8380–9575 | 254.77 |
| 4201–5396 | 254.30 |
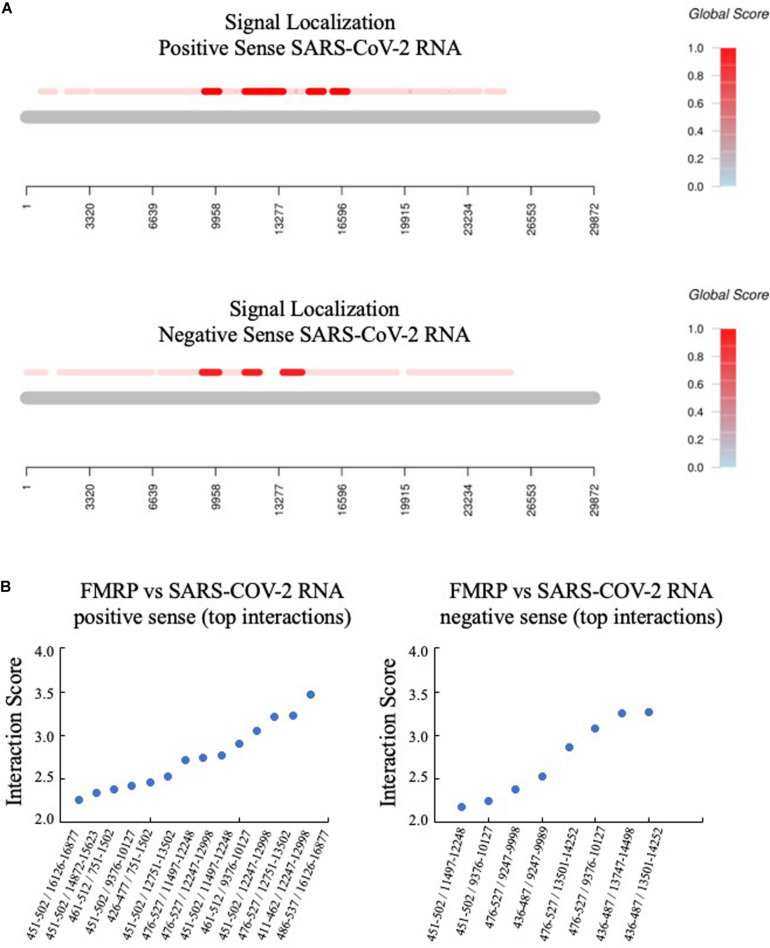
Third, the catRAPID signal localization algorithm predicted the top interactions for positive and negative sense SARS-CoV-2 RNA (Figure 2). The protein region of FMRP implicated in binding overlapped with the C1 region, which is an arginine-glycine-rich (RG-rich) region that participates in non-specific RNA binding (Adinolfi et al., 1999).
FIGURE 2.
FMRP is predicted to bind to multiple regions of SARS-CoV-2 RNA. (A) The catRAPID Global Score algorithm with uniform fragmentation and signal localization predicts multiple FMRP binding sites in both positive and negative sense SARS-CoV-2 RNA, with the strongest predicted binding in the region of nucleotides 9,000–17,000 (positive sense) and nucleotides 9,000–15,000 (negative sense). (B) The top specific interactions are graphed by protein/RNA sequence positions (x-axis) versus interaction score (y-axis). Protein and RNA coordinates are reported relative to the NCBI database.
And fourth, we utilized catRAPID Global Score with weighted fragmentation to predict FMRP/SARS-CoV-2 interactions. The fragmentation weighted option generates interaction predictions using intact RBP (FMRP) and fragments of the RNA (100–200 nucleotides of positive or negative SARS-CoV-2 RNA), and is useful for the study of RNAs, which are larger than 1,000 nucleotides. FMRP and SARS-CoV-2 RNA are predicted to interact with propensities of 0.93 (positive sense) and 0.87 (negative sense). The top predicted interaction sites for positive and negative sense SARS-COV-2 are provided in the Supplementary Figure S1. Of note, 8 negative sense SARS-CoV-2 RNA fragments spanned the putative G-quartet region and exhibited an average interaction propensity of 5.8 ± 1.2 with FMRP. For comparison of interaction propensities, FMRP interacts with human mRNAs including CAMK2A (BC040457.1), PSD-95 (U83192.1) and APP (BC065529.1) with global scores of 0.54, 0.68 and 0.71, respectively, using the weighted algorithm.
Overall, these molecular modeling studies indicate an overwhelming plentitude of potential interactions between FMRP and SARS-CoV-2 RNA, which remain to be experimentally validated. FMRP is predicted to bind along 25 kB of the 29.8 kB length of positive and negative sense SARS-CoV-2 RNAs such that the RNA could act as a sink for FMRP and other RBP and prevent their normal function. The predicted interaction propensities of FMRP with SARS-CoV-2 positive and negative sense RNAs are stronger than known FMRP target mRNAs.
Repurposing mGluR5 Inhibitors for Treatment of COVID-19
The leading drug target to date for FXS is the glutamate-activated, G-protein-coupled receptor mGluR5, which signals through FMRP (Bear et al., 2004; Stoppel et al., 2017). The mGluRs contain a large extracellular amino terminal domain, a heptahelical transmembrane region, and an intracellular carboxy terminal domain. Negative allosteric modulators (NAMs) of mGluR5 bind to the transmembrane heptahelical domain. These drugs are potent, non-competitive, selective and systematically active allosteric antagonists that are under study for a range of indications including anxiety, epilepsy, pain, depression, Parkinson’s disease, gastroesophageal reflux disease, FXS, autism, and addiction (Westmark, 2014). There has been a concerted effort to repurpose mGluR5 NAMs for the treatment of FXS where these drugs rescue disease phenotypes in multiple preclinical models and have been safely tested in clinical trials (Gravius et al., 2010; Michalon et al., 2012; Scharf et al., 2015; Berry-Kravis et al., 2017). Although mGluR5 expression is enriched in brain tissue, the receptor is ubiquitously expressed in the body including the lungs2. We hypothesize that mGluR5 NAMs could be a prophylactic treatment to slow viral protein synthesis in patients infected with SARS-CoV-2.
Treatment of COVID-19 will likely require a therapeutic cocktail approach. Lead candidate drugs have been reviewed and include angiotensin receptor blockers, statins, remdesivir, chloroquine, hydroxychloroquine, lopinavir-ritonavir and interferon-beta (Kupferschmidt and Cohen, 2020). Angiotensin receptor blockers and statins upregulate ACE2, the SARS-CoV-2 host receptor, and are expected to increase the host response to infection allowing the patient to recover on their own (Fedson et al., 2020). Remdesivir shuts down viral replication by inhibiting viral RNA polymerase and has been shown to inhibit both the SARS and MERS viruses but not Ebola. Remdesivir must be given intravenously and is expensive. Chloroquine and hydroxychloroquine decrease the acidity of cellular endosomes compartments, which are involved in the degradation of foreign material. These drugs require high doses that could cause severe toxicity and many side effects. Lopinavir-ritonavir inhibits the HIV protease and has been shown effective in marmosets infected with the MERS-CoV virus. Interferon-beta regulates inflammation. A combination of lopinavir-ritonavir with interferon-beta has lessened disease severity in marmosets with MERS-CoV but could be risky for patients with severe COVID-19 and lead to more tissue damage. Other drugs under investigation for COVID-19 include corticosteroids and baricitinib, which reduce inflammation in the treatment of rheumatoid arthritis; camostat mesylate, which inhibits a human protein involved with infection; anti-viral drugs including the influenza drug favipiravir; and additional HIV antivirals (Kupferschmidt and Cohen, 2020). An alternative therapeutic strategy is to boost immunity with plasma from convalesced COVID-19 patients or monoclonal antibodies directed at SARS-CoV-2.
We propose that inclusion of mGluR5 NAMs as part of a drug cocktail approach to combat COVID-19 offers the advantages of: (1) extensive preclinical research regarding its mechanism of action; (2) prior safety testing in human clinical trials of FXS; (3) numerous mGluR5 NAMs available from multiple pharmaceutical countries worldwide; (4) orally dosed; (5) protein target ubiquitously expressed including the lungs; (6) less expensive to produce small molecule drugs; and (7) targets a post-transcriptional gene regulatory step in viral production not addressed by other therapies under investigation. In addition, blockade of mGluR5 activity prevents an increase in proinflammatory cytokines and chemokines (Shah et al., 2012), which may quell the cytokine storm elicited by SARS-CoV-2 infection.
Preclinical Testing Strategy of mGluR5 Inhibitors in SARS-COVID-2 Models
Proposed experiments to validate our hypothesis include: (1) gel mobility shift and co-immunoprecipitation assays to identify FMRP/SARS-Cov-2 RNA interactions, (2) in vitro translation assays to quantitate viral and cellular protein synthesis levels in the presence and absence of FMRP and mGluR5 inhibitors, (3) in vitro assays in SARS-CoV-2 RNA-infected cells that under- and over-express FMRP to assess protein synthesis levels and virus production with/without mGluR5 inhibitors, and (4) in vivo testing of disease outcomes in a COVID-19 animal model in response to mGluR5 inhibitors. An important caveat to this hypothesis is that viruses can differentially affect the host translational machinery. It will be important to test both mGluR5 NAMs and positive allosteric modulators (PAMs) in preclinical studies to ascertain effects on SARS-CoV-2 RNA and protein synthesis. To our knowledge, the only study testing mGluR5 drugs in a virus model was in a virus-induced temporal lobe epilepsy (TMEV) model where treatment with the PAM VU0360172 reduced acute seizures, while blocking mGluR5 did not make seizure phenotypes worse (Hanak et al., 2019).
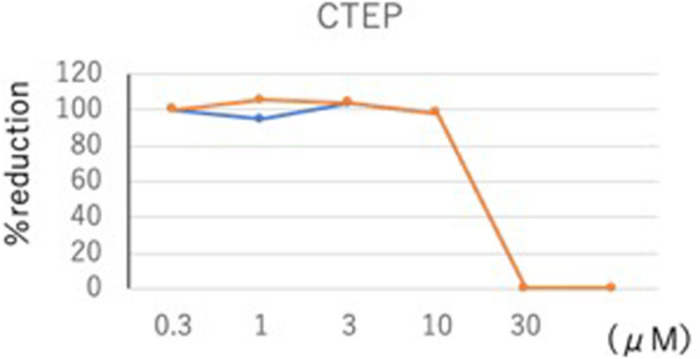
Toward validation of our model, we tested the mGluR5 inhibitor 2-chloro-4-((2,5-dimethyl-1-(4-(trifluoro- methoxy)phenyl)-1H-imidazol-4-yl)ethynyl)pyridine (CTEP) in an in vitro SARS-CoV-2 assay (Figure 3). CTEP is a commercially available, research-grade mGluR5 inhibitor developed by Hoffmann-La Roche. This negative allosteric modulator of mGluR5 acts with nanomolar affinity and greater than 1,000-fold selectivity when tested against 103 targets (Lindemann et al., 2011). CTEP has high oral bioavailability and long duration of action in animal models with a single dose lasting 18 h. CTEP reduced viral plaque load with an IC50 of 13.1 μM in a VeroE6/TMPRSS2 cell assay. In vivo testing of CTEP in a hamster COVID-19 model is in progress.
FIGURE 3.
CTEP reduces SARS-CoV-2 viral plaque load. SARS-CoV-2 virus titer was assessed in response to a 100-fold concentration range (0.3–30 μM) of the mGluR5 inhibitor CTEP. Confluent VeroE6/TPMRSS2 cells seeded at a density of 5 × 105 cells per well in 6-well plates were infected with SARS-CoV-2 [approximately 80 plaque-forming units of SARS-CoV-2/UT-NCGM02/Human/2020/Tokyo (UT-NCGM02) isolated from a mild case in Tokyo]. After 30 min infection, viral inoculum was removed and cells were washed three times to remove any unbound virus before being overlaid with MEM containing a final concentration of 5% fetal bovine serum and 1.0% methyl cellulose (Sigma-Aldrich; to allow for plaque formation) along with various concentrations of CTEP. After an incubation of 2 days, the number of plaques were counted and IC50 values were calculated using Graphpad Prism software (Graphpad Software, La Jolla, CA, United States). CTEP reduced virus titer with an IC50 of 13.1 μM.
Clinical Feasibility
The old adage, “feed a cold, starve a fever,” may apply to treating COVID-19. Starving a fever is medical folklore for normalizing metabolism that is in overdrive. Metabolism is dependent on protein synthesis. Because virus translation dominates host cell translation at later time points of infection due to the high level of viral transcripts (Irigoyen et al., 2016), reducing protein synthesis after the onset of symptoms would be predicted to starve virus translation more than host cell translation leading to reduced virus production and affording the adaptive immune system more time to generate a response.
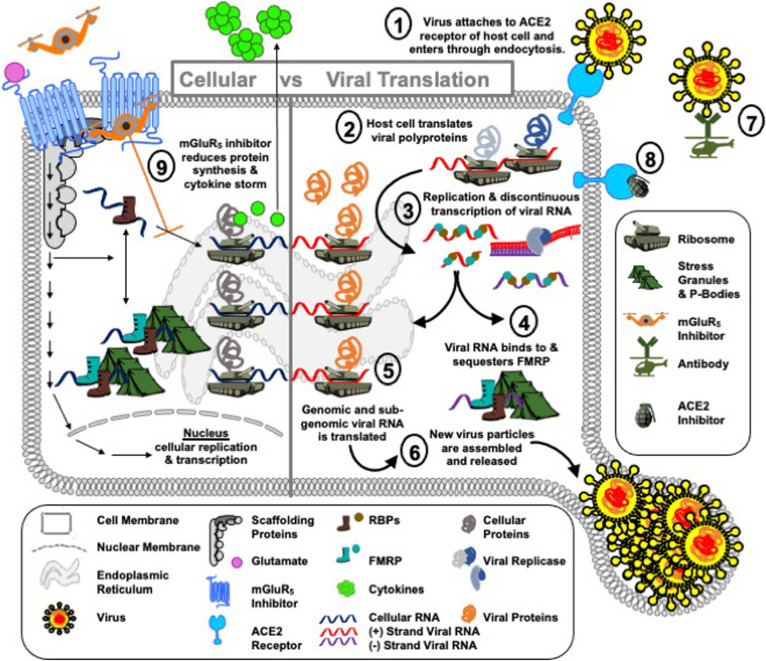
Inhibitors of mGluR5, which have been extensively studied in both preclinical research and in clinical trials, particularly as regards FXS and Parkinson’s disease (PD) (Gravius et al., 2010; Michalon et al., 2012; Scharf et al., 2015; Tison et al., 2016; Berry-Kravis et al., 2017), offer a potential repurposing strategy for COVID-19 (Figure 4). The FXS field has three decades of experience in mobilizing academic, pharmaceutical, biotechnology and clinical partners to repurpose drugs for a rare disorder through the efforts of FRAXA Research Foundation, the National Fragile X Foundation (NFXF) and other advocacy groups. There have been over 3,000 publications by the biomedical community to understand the role of FMRP in FXS and to test promising drugs with mGluR5 as the leading drug target. This experience could be rapidly extrapolated to COVID-19. Of most importance, multiple clinical trials have been conducted in both children and adults with FXS as well as adults with PD with minimal adverse effects.
FIGURE 4.
Operation mGluR5. COVID-19 is a global pandemic, i.e., a Blitzkrieg attack by SARS-CoV-2 on the human population. The port of attack for SARS-CoV-2 is the cell surface receptor angiotensin-converting enzyme 2 (ACE2) in the cells of the lungs ➀. Once SARS-CoV-2 lands and breaches the cell border, the virus injects positive-sense, single-stranded RNA [ssRNA(+)] into the cell cytoplasm and immediately takes hostage of the host cell protein synthesis machinery ➁ to replicate and transcribe new viral RNA ➂. This is accomplished by a swift and effective disarmament of the cell’s shock troops, RNA binding proteins (RBPs). Shock troops is a military term for infantry formations created to lead an attack. In the RNA world, RBPs bind to RNA to either degrade, localize, store or translate messages. RBPs can bind to viral as well as cellular mRNA. In the case of viral infection, viral RNA recruits cellular RBPs to translate viral proteins at ribosomes, or sequesters cellular RBPs at other cell encampments, such as stress granules and P-bodies, to block their normal cellular function. We hypothesize that FMRP is a shock troop that is sequestered by SARS-CoV-2 RNA to prevent its normal function of acting as a brake on protein synthesis ➃. In the absence of FMRP, it is predicted that the rate of viral protein synthesis ➄ and hence further infection ➅ are increased. Public surveillance policies and on-site diagnostics (i.e., equivalent to wartime communications and intelligence reports) to inform the public and health care professionals on viral spread are in place. Vaccines, which can mediate a rapid immune response to fight infection are in progress (i.e., cell airborne attack) ➆. Drugs to target ACE2, the port of infection, are identified and under study (i.e., cell naval response) ➇. What we lack in the fight against SARS-CoV-2 are drugs that support the boots on the ground, i.e., RBPs, and protect their encampments, i.e., ribosomes, stress granules and P-bodies. We propose that mGluR5 inhibitors ➈ are a potential drug therapy to combat viral hijack of the host translational infrastructure (i.e., the cell army) by slowing down protein synthesis to afford the innate immune system time to identify a viral infection and mediate an adaptive response as well as to afford the cell degradation machinery (i.e., cell marines) time to recruit and degrade viral proteins. It is anticipated that reduced protein synthesis could have negative consequences for the host cell as well as the virus; however, similar to chemotherapy that kills both healthy and cancer cells, this defensive strategy to delay advance of the stealth virus invader could buy time until the enemy can be eradicated by flanking troops. An additional potential benefit of mGluR5 inhibition is reduced cytokine production, which could attenuate the COVID-19 cytokine storm.
Limitations regarding repurposing mGluR5 inhibitors for COVID-19 include: (1) the need for key supporting experiments regarding the mechanism, i.e., linking mGluR5, FMRP and viral protein production; (2) FMRP is not the only downstream target of mGluR5; (3) viral protein production is not exclusively regulated by FMRP and/or mGluR5; (4) caution is required in the interpretation of the in vitro virus titer data in response to CTEP as weak activity is indicated by an IC50 of 13.1 μM; and (5) it is unknown if an effective serum concentration can be achieved in patients and if therapeutic doses will induce adverse reactions. Nonetheless, considering the dearth of therapeutic options for COVID-19 and the established safety profile of mGluR5 NAMs, it is worthwhile to test clinical grade mGluR5 NAMs, such as AFQ056, basimglurant and dipraglurant, in in vitro and in vivo models of COVID-19.
Conclusion
In conclusion, public surveillance and vaccine development for COVID-19 are on-going, but we have limited knowledge of SARS-CoV-2 post-transcriptional gene regulation and a dearth of therapeutic options. Thus, there is a critical need for the research community to rapidly mobilize to address these knowledge gaps related to COVID-19. In addition, viral infections will remain a serious threat even after COVID-19 passes. Viruses are constantly mutating and have the capacity to transmit between species. It is imperative to identify an arsenal of therapeutic options. Evidence-based research to support vaccine and drug development requires time and money to conduct rigorous and reproducible studies in preclinical models to support a hypothesis followed by extensive clinical trial validation. Thus, when currently available drugs can be repurposed for a rare disorder, or a global epidemic, it can greatly reduce the cost and time of drug validation. Targeting protein synthesis as part of a therapeutic arsenal may be a feasible broad-spectrum option to target viruses, which depend on, and cannot replicate without, the host cell translational machinery.
It remains to be determined if FMRP plays a role in protein synthesis in response to SARS-CoV-2 infection, and if mGluR5 NAMs are a viable therapeutic strategy to modulate viral protein production. From a post-transcriptional gene regulation perspective, research questions that need to be addressed include: which RBP bind to and regulate synthesis of SARS-CoV-2 genomic and subgenomic RNA? Does SARS-Cov-2 RNA sequester and thereby inactivate host cell RBP such as FMRP to promote viral RNA production? Do drugs that target RBP attenuate viral replication? How do those drugs affect the immune response? Nonetheless, mGluR5 NAMs have been extensively studied in non-viral models, have proven relatively safe, and may provide a rapid repurposing strategy. Similar to physical distancing and the temporary shutdown of our economy at the national level to allow public surveillance and prevent viral spread, temporary attenuation of protein synthesis at the cellular level may afford the immune system time to find and fight SARS-Cov-2.
Data Availability Statement
All datasets presented in this study are included in the article/Supplementary Material.
Author Contributions
CW: conceptualization and original draft preparation. CW and MK: data collection. CW, PH, PW, and YK: review and editing. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the Frontiers journals for their rapid mobilization of a COVID-19 initiative including organization of this Research Topic and the reviewers for their insightful critiques, which significantly improved the manuscript. We also thank Dr. Michael Tranfaglia (FRAXA Research Foundation), Dr. David Brown (Healx), Dr. Elizabeth Berry-Kravis (Rush University Medical Center), Dr. Fabrizio Gasparini (Novartis), Dr. Andrzej Dekundy (Merz Pharmaceuticals), and Dr. Debomoy Lahiri (Indiana University) for helpful discussions.
Funding. CW was funded by USDA grant number 2018-67001-28266 and NIH grant number R03 HD097067. YK was funded by a grant (HHSN272201400008C) from the Center for Research on Influenza Pathogenesis, funded by the National Institute of Allergy and Infectious Diseases, and by a Research Program on Emerging and Re-emerging Infectious Disease grant (19fk0108113) from the Japan Agency for Medical Research and Development (AMED).
The Human Protein Atlas, accessed 04/02/20 at https://www.proteinatlas.org/ENSG00000168959-GRM5.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcell.2020.00856/full#supplementary-material
References
- Adinolfi S., Bagni C., Musco G., Gibson T., Mazzarella L., Pastore A. (1999). Dissecting FMR1, the protein responsible for fragile X syndrome, in its structural and functional domains. RNA 5 121448–121258. 10.1017/S1355838299990647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agostini F., Zanzoni A., Klus P., Marchese D., Cirillo D., Tartaglia G. G. (2013). catRAPID omics: a web server for large-scale prediction of protein-RNA interactions. Bioinformatics 29 2928–2930. 10.1093/bioinformatics/btt495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashwood P., Nguyen D. V., Hessl D., Hagerman R. J., Tassone F. (2010). Plasma cytokine profiles in Fragile X subjects: is there a role for cytokines in the pathogenesis? Brain Behav. Immun. 24 898–902. 10.1016/j.bbi.2010.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagni C., Greenough W. T. (2005). From mRNP trafficking to spine dysmorphogenesis: the roots of fragile X syndrome. Nat. Rev. Neurosci. 6 376–387. 10.1038/nrn1667 [DOI] [PubMed] [Google Scholar]
- Bear M. F., Huber K. M., Warren S. T. (2004). The mGluR theory of fragile X mental retardation. Trends Neurosci. 27 370–377. 10.1016/j.tins.2004.04.009 [DOI] [PubMed] [Google Scholar]
- Bellucci M., Agostini F., Masin M., Tartaglia G. G. (2011). Predicting protein associations with long noncoding RNAs. Nat. Methods 8 444–445. 10.1038/nmeth.1611 [DOI] [PubMed] [Google Scholar]
- Berry-Kravis E. M., Lindemann L., Jonch A. E., Apostol G., Bear M. F., Carpenter R. L., et al. (2017). Drug development for neurodevelopmental disorders: lessons learned from fragile X syndrome. Nat. Rev. Drug Discov. 17 280–299. 10.1038/nrd.2017.221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berthoux L. (2020). The restrictome of flaviviruses. Virol. Sin. 10.1007/s12250-020-00208-3. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown V., Jin P., Ceman S., Darnell J. C., O’Donnell W. T., Tenenbaum S. A., et al. (2001). Microarray identification of FMRP-associated brain mRNAs and altered mRNA translational profiles in fragile X syndrome. Cell 107 477–487. 10.1016/s0092-8674(01)00568-2 [DOI] [PubMed] [Google Scholar]
- Careaga M., Noyon T., Basuta K., Van de Water J., Tassone F., Hagerman R. J., et al. (2014a). Group I metabotropic glutamate receptor mediated dynamic immune dysfunction in children with fragile X syndrome. J. Neuroinflammation 11:110. 10.1186/1742-2094-11-110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Careaga M., Rose D., Tassone F., Berman R. F., Hagerman R., Ashwood P. (2014b). Immune dysregulation as a cause of autoinflammation in fragile X premutation carriers: link between FMRI CGG repeat number and decreased cytokine responses. PLoS One 9:e94475. 10.1371/journal.pone.0094475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cirillo D., Agostini F., Klus P., Marchese D., Rodriguez S., Bolognesi B., et al. (2013). Neurodegenerative diseases: quantitative predictions of protein-RNA interactions. RNA 19 129–140. 10.1261/rna.034777.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darnell J. C., Fraser C. E., Mostovetsky O., Stefani G., Jones T. A., Eddy S. R., et al. (2005). Kissing complex RNAs mediate interaction between the Fragile-X mental retardation protein KH2 domain and brain polyribosomes. Genes Dev. 19 903–918. 10.1101/gad.1276805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darnell J. C., Jensen K. B., Jin P., Brown V., Warren S. T., Darnell R. B. (2001). Fragile X mental retardation protein targets G quartet mRNAs important for neuronal function. Cell 107 489–499. 10.1016/s0092-8674(01)00566-9 [DOI] [PubMed] [Google Scholar]
- Darnell J. C., Van Driesche S. J., Zhang C., Hung K. Y., Mele A., Fraser C. E., et al. (2011). FMRP stalls ribosomal translocation on mRNAs linked to synaptic function and autism. Cell 146 247–261. 10.1016/j.cell.2011.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fedson D. S., Opal S. M., Rordam O. M. (2020). Hiding in plain sight: an approach to treating patients with severe COVID-19 infection. mBio 11:e00398-20. 10.1128/mBio.00398-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fehr A. R., Perlman S. (2015). Coronaviruses: an overview of their replication and pathogenesis. Methods Mol. Biol. 1282 1–23. 10.1007/978-1-4939-2438-7_1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Y., Absher D., Eberhart D. E., Brown V., Malter H. E., Warren S. T. (1997a). FMRP associates with polyribosomes as an mRNP, and the I304N mutation of severe fragile X syndrome abolishes this association. Mol. Cell 1 109–118. 10.1016/s1097-2765(00)80012-x [DOI] [PubMed] [Google Scholar]
- Feng Y., Gutekunst C. A., Eberhart D. E., Yi H., Warren S. T., Hersch S. M. (1997b). Fragile X mental retardation protein: nucleocytoplasmic shuttling and association with somatodendritic ribosomes. J. Neurosci. 17 1539–1547. 10.1523/jneurosci.17-05-01539.1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravius A., Pietraszek M., Dekundy A., Danysz W. (2010). Metabotropic glutamate receptors as therapeutic targets for cognitive disorders. Curr. Top. Med. Chem. 10 187–206. 10.2174/156802610790411018 [DOI] [PubMed] [Google Scholar]
- Hafner M., Landthaler M., Burger L., Khorshid M., Hausser J., Berninger P., et al. (2010). Transcriptome-wide identification of RNA-binding protein and microRNA target sites by PAR-CLIP. Cell 141 129–141. 10.1016/j.cell.2010.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagerman R. J., Hagerman P. J. (2002). Physical and Behavioral Phenotype. Baltimore: John Hopkins University Press. [Google Scholar]
- Hanak T. J., Libbey J. E., Doty D. J., Sim J. T., DePaula-Silva A. B., Fujinami R. S. (2019). Positive modulation of mGluR5 attenuates seizures and reduces TNF-alpha(+) macrophages and microglia in the brain in a murine model of virus-induced temporal lobe epilepsy. Exp. Neurol. 311 194–204. 10.1016/j.expneurol.2018.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He J., Tao H., Yan Y., Huang S.-Y., Yi X. (2020). Molecular mechanism of evolution and human infection with SARS-CoV-2. Viruses. 12:428. 10.3390/v12040428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodges S. L., Nolan S. O., Tomac L. A., Muhammad I. D. A., Binder M. S., Taube J. H., et al. (2020). Lipopolysaccharide-induced inflammation leads to acute elevations in pro-inflammatory cytokine expression in a mouse model of Fragile X syndrome. Physiol. Behav. 215:112776. 10.1016/j.physbeh.2019.112776 [DOI] [PubMed] [Google Scholar]
- Irigoyen N., Firth A. E., Jones J. D., Chung B. Y., Siddell S. G., Brierley I. (2016). High-resolution analysis of coronavirus gene expression by RNA sequencing and ribosome profiling. PLoS Pathog. 12:e1005473. 10.1371/journal.ppat.1005473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalnapurkar I., Rafika N., Tassone F., Hagerman R. (2015). Immune mediated disorders in women with a fragile X expansion and FXTAS. Am. J. Med. Genet. A. 167A 190–197. 10.1002/ajmg.a.36748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly E., Schaeffer S. M., Dhamne S. C., Lipton J. O., Lindemann L., Honer M., et al. (2018). mGluR5 modulation of behavioral and epileptic phenotypes in a mouse model of tuberous sclerosis complex. Neuropsychopharmacology 43 1457–1465. 10.1038/npp.2017.295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kupferschmidt K., Cohen J. (2020). Race to find COVID-19 treatments accelerates. Science 367 1412–1413. 10.1126/science.367.6485.1412 [DOI] [PubMed] [Google Scholar]
- Laggerbauer B., Ostareck D., Keidel E. M., Ostareck-Lederer A., Fischer U. (2001). Evidence that fragile X mental retardation protein is a negative regulator of translation. Hum. Mol. Genet. 10 329–338. 10.1093/hmg/10.4.329 [DOI] [PubMed] [Google Scholar]
- Lai A., Valdez-Sinon A. N., Bassell G. J. (2020). Regulation of RNA granules by FMRP and implications for neurological diseases. Traffic 21 454–462. 10.1111/tra.12733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F. (2015). Receptor recognition mechanisms of coronaviruses: a decade of structural studies. J. Virol. 89 1954–1964. 10.1128/jvi.02615-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Moore M. J., Vasilieva N., Sui J., Wong S. K., Berne M. A., et al. (2003). Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature 426 450–454. 10.1038/nature02145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z., Zhang Y., Ku L., Wilkinson K. D., Warren S. T., Feng Y. (2001). The fragile X mental retardation protein inhibits translation via interacting with mRNA. Nucleic Acids Res. 29 2276–2283. 10.1093/nar/29.11.2276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindemann L., Jaeschke G., Michalon A., Vieira E., Honer M., Spooren W., et al. (2011). CTEP: a novel, potent, long-acting, and orally bioavailable metabotropic glutamate receptor 5 inhibitor. J. Pharmacol. Exp. Ther. 339 474–486. 10.1124/jpet.111.185660 [DOI] [PubMed] [Google Scholar]
- Lisik M. Z., Gutmajster E., Sieron A. L. (2015). Anti-neuronal antibodies in patients with fragile X syndrome: is there a role of autoimmunity in its pathogenesis? Neurodegener. Dis. 15 45–49. 10.1159/000369215 [DOI] [PubMed] [Google Scholar]
- Maranon D. G., Anderson J., Maranon A. G., Wilusz J. (2020). The interface between coronaviruses and host cell RNA biology: novel potential insights for future therapeutic intervention. WIREs RNA. 10.1002/wrna.1614. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazeaud C., Freppel W., Chatel-Chaix L. (2018). The multiples fates of the flavivirus RNA genome during pathogenesis. Front. Genet. 9:595. 10.3389/fgene.2018.00595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazroui R., Huot M. E., Tremblay S., Filion C., Labelle Y., Khandjian E. W. (2002). Trapping of messenger RNA by Fragile X Mental Retardation protein into cytoplasmic granules induces translation repression. Hum. Mol. Genet. 11 3007–3017. 10.1093/hmg/11.24.3007 [DOI] [PubMed] [Google Scholar]
- Michalon A., Sidorov M., Ballard T. M., Ozmen L., Spooren W., Wettstein J. G., et al. (2012). Chronic pharmacological mGlu5 inhibition corrects fragile X in adult mice. Neuron 74 49–56. 10.1016/j.neuron.2012.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyashiro K. Y., Beckel-Mitchener A., Purk T. P., Becker K. G., Barret T., Liu L., et al. (2003). RNA cargoes associating with FMRP reveal deficits in cellular functioning in Fmr1 null mice. Neuron 37 417–431. 10.1016/s0896-6273(03)00034-5 [DOI] [PubMed] [Google Scholar]
- O’Connor R. M., Stone E. F., Wayne C. R., Marcinkevicius E. V., Ulgherait M., Delventhal R., et al. (2017). A Drosophila model of Fragile X syndrome exhibits defects in phagocytosis by innate immune cells. J. Cell Biol. 216 595–605. 10.1083/jcb.201607093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osterweil E. K., Krueger D. D., Reinhold K., Bear M. F. (2010). Hypersensitivity to mGluR5 and ERK1/2 leads to excessive protein synthesis in the hippocampus of a mouse model of fragile X syndrome. J. Neurosci. 30 15616–15627. 10.1523/jneurosci.3888-10.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scharf S. H., Jaeschke G., Wettstein J. G., Lindemann L. (2015). Metabotropic glutamate receptor 5 as drug target for Fragile X syndrome. Curr. Opin. Pharmacol. 20 124–134. 10.1016/j.coph.2014.11.004 [DOI] [PubMed] [Google Scholar]
- Shah A., Silverstein P. S., Singh D. P., Kumar A. (2012). Involvement of metabotropic glutamate receptor 5, AKT/PI3K signaling and NF-kappaB pathway in methamphetamine-mediated increase in IL-6 and IL-8 expression in astrocytes. J. Neuroinflammation 9:52. 10.1186/1742-2094-9-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siomi H., Choi M., Siomi M. C., Nussbaum R. L., Dreyfuss G. (1994). Essential role of KH domains in RNA binding: impaired RNA binding by a mutation in the KH domain of FMR1 that causes fragile X syndrome. Cell 77 33–39. 10.1016/0092-8674(94)90232-1 [DOI] [PubMed] [Google Scholar]
- Soto-Acosta R., Xie X., Shan C., Baker C. K., Shi P. Y., Rossi S. L., et al. (2018). Fragile X mental retardation protein is a Zika virus restriction factor that is antagonized by subgenomic flaviviral RNA. Elife 7:e39023. 10.7554/eLife.39023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoppel L. J., Osterweil E. K., Bear M. F. (2017). “Chapter 9: the mGluR theory of fragile X: from mice to men,” in Fragile X Syndrome from Genetics to Targeted Treatment, eds Willemsen R., Kooy F. (Amsterdam: Elsevier; ). [Google Scholar]
- Taha M. S., Haghighi F., Stefansik A., Nakhaei-Rad S., Kazemein Jaemi N. S., Aghyad Al Kabbani M., et al. (2020). Novel FMRP interaction networks linked to cellular stress. FEBS J. 10.1111/febs.15443 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Tison F., Keywood C., Wakefield M., Durif F., Corvol J. C., Eggert K., et al. (2016). A phase 2A trial of the novel mGluR5-negative allosteric modulator dipraglurant for levodopa-induced dyskinesia in Parkinson’s disease. Mov. Disord. 31 1373–1380. 10.1002/mds.26659 [DOI] [PubMed] [Google Scholar]
- Van Dijck A., Barbosa S., Bermudez-Martin P., Khalfallah O., Gilet C., Martinuzzi E., et al. (2020). Reduced serum levels of pro-inflammatory chemokines in fragile X syndrome. BMC Neurol. 20:138. 10.1186/s12883-020-01715-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verkerk A. J., Pieretti M., Sutcliffe J. S., Fu Y. H., Kuhl D. P., Pizzuti A., et al. (1991). Identification of a gene (FMR-1) containing a CGG repeat coincident with a breakpoint cluster region exhibiting length variation in fragile X syndrome. Cell 65 905–914. 10.1016/0092-8674(91)90397-h [DOI] [PubMed] [Google Scholar]
- Wan Y., Shang J., Graham R., Baric R. S., Li F. (2020). Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J. Virol. 94:e00127-20. 10.1128/JVI.00127-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiler I. J., Irwin S. A., Klintsova A. Y., Spencer C. M., Brazelton A. D., Miyashiro K., et al. (1997). Fragile X mental retardation protein is translated near synapses in response to neurotransmitter activation. Proc. Natl. Acad. Sci. U.S.A. 94 5395–5400. 10.1073/pnas.94.10.5395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westmark C. (2014). “Chapter: group 1 metabotropic glutamate receptors: a potential therapeutic target for amyloidogenic disorders,” in Metabotropic Glutamate Receptors: Molecular Mechanisms, Role in Neurological Disorders, and Pharmacological Effects, ed. Foster Olive M. (Hauppauge, NY: Nova Science Publishers; ). [Google Scholar]
- Winarni T. I., Chonchaiya W., Sumekar T. A., Ashwood P., Morales G. M., Tassone F., et al. (2012). Immune-mediated disorders among women carriers of fragile X premutation alleles. Am. J. Med. Genet. A. 158A 2473–2481. 10.1002/ajmg.a.35569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu H. Y., Brian D. A. (2010). Subgenomic messenger RNA amplification in coronaviruses. Proc. Natl. Acad. Sci. U.S.A. 107 12257–12262. 10.1073/pnas.1000378107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu K. H., Palmer N., Fox K., Prock L., Mandl K. D., Kohane I. S., et al. (2020). The phenotypical implications of immune dysregulation in fragile X syndrome. Eur. J. Neurol. 27 590–593. 10.1111/ene.14146 [DOI] [PubMed] [Google Scholar]
- Yuskaitis C. J., Beurel E., Jope R. S. (2010). Evidence of reactive astrocytes but not peripheral immune system activation in a mouse model of Fragile X syndrome. Biochim. Biophys. Acta 1802 1006–1012. 10.1016/j.bbadis.2010.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., et al. (2020). A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382 727–733. 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All datasets presented in this study are included in the article/Supplementary Material.