Abstract
Heart failure exhibits remarkable pathophysiologic heterogeneity. A large body of evidence suggests that regardless of the underlying etiology, heart failure is associated with induction of cytokines and chemokines that may contribute to the pathogenesis of adverse remodeling, and systolic and diastolic dysfunction. The pro-inflammatory cytokines tumor necrosis factor (TNF)-α, interleukin (IL)-1, and IL-6 have been extensively implicated in the pathogenesis of heart failure. Inflammatory cytokines modulate phenotype and function of all myocardial cells, suppressing contractile function in cardiomyocytes, inducing inflammatory activation in macrophages, stimulating microvascular inflammation and dysfunction, and promoting a matrix-degrading phenotype in fibroblasts. Moreover, cytokine-induced growth factor synthesis may exert chronic fibrogenic actions contributing to the pathogenesis of heart failure with preserved ejection fraction (HFpEF). In addition to their role in adverse cardiac remodeling, some inflammatory cytokines may also exert protective actions on cardiomyocytes under conditions of stress. Chemokines, such as CCL2, are also upregulated in failing hearts and may stimulate recruitment of pro-inflammatory leukocytes, promoting myocardial injury, fibrotic remodeling, and dysfunction. Although experimental evidence suggests that cytokine and chemokine targeting may hold therapeutic promise in heart failure, clinical translation remains challenging. This review manuscript summarizes our knowledge on the role of TNF-α, IL-1, IL-6, and CCL2 in the pathogenesis of heart failure, and discusses the promises and challenges of targeted anti-cytokine therapy. Dissection of protective and maladaptive cellular actions of cytokines in the failing heart, and identification of patient subsets with overactive or dysregulated myocardial inflammatory responses are required for design of successful therapeutic approaches.
Keywords: Heart failure, Cytokine, Chemokine, Inflammation, Interleukin-1, TNF-α
Introduction
Heart failure is a condition in which the heart either cannot pump enough blood to meet the needs of various tissues or can do so only at the cost of increased filling pressures [1, 2]. Based on the ejection fraction, the most commonly used indicator of systolic function, heart failure patients can be classified into two major groups. Heart failure patients with reduced ejection fraction (HFrEF) exhibit depressed systolic function. On the other hand, the term heart failure with preserved ejection fraction (HFpEF) is used for patients who have the same heart failure symptoms, in the absence of significant reductions in ejection fraction. Elevated filling pressures in HFpEF patients are caused predominantly by perturbations in diastolic function. Epidemiologic studies have demonstrated that HFpEF accounts for almost half of all incident heart failure [3]. Both HFrEF and HFpEF have a poor prognosis. Although approaches targeting neurohumoral pathways have shown beneficial effects in patients with HFrEF, effective therapeutic strategies for HFpEF are lacking.
A major obstacle that hampers development of new therapeutics in heart failure is the pathophysiologic heterogeneity of the disease. The clinical syndrome of heart failure can be triggered by a wide range of pathophysiologic changes, including myocardial ischemia and infarction, pressure or volume overload, metabolic dysregulation, genetic perturbations in sarcomeric protein function, and responses to viral infections. Regardless of underlying etiology, heart failure is associated with both local and systemic activation of inflammatory signaling cascades [4]. In patients with myocarditis or inflammatory cardiomyopathies, inflammation is the primary cause of heart failure [5]. Moreover, cytokine-mediated inflammation has been implicated in acute stress-induced cardiomyopathy [6], an enigmatic entity that may be associated with major emotional or physical stress [7], and may also be a rare cause of myocardial injury in patients with coronavirus disease 2019 (COVID-19) [8, 9]. In most other cases, activation of an inflammatory program reflects a reparative or protective response to other primary injurious processes. Regardless of the underlying etiology, excessive, unrestrained, or dysregulated inflammation may exacerbate myocardial injury, thus contributing to the progression of heart failure. The inflammatory response in the failing heart is characterized by induction and activation of a wide range of pleiotropic cytokines and chemokines that modulate phenotype and function of all myocardial cells. The complexity and pleiotropy of inflammatory mediators have hampered therapeutic implementation of therapeutic strategies targeting the inflammatory response.
This review manuscript discusses the potential role of the best-studied and most promising pro-inflammatory cytokines and chemokines as therapeutic targets in heart failure, We focus on the prototypic inflammatory cytokines tumor necrosis factor (TNF)-α, interleukin (IL)-1 and IL-6, and on the CC chemokine CCL2/monocyte chemoattractant protein (MCP)-1. We summarize the cell biological actions of these mediators in the failing heart and their potential contribution to dysfunction and heart failure progression. Finally, we discuss the promises and challenges of cytokine and chemokine targeting in heart failure patients.
Inflammatory Cytokines in the Pathogenesis of Chronic Heart Failure
A large body of evidence, derived through both experimental and clinical studies, supports an important role for inflammatory cytokines and chemokines in the pathogenesis of myocardial dysfunction and adverse cardiac remodeling. Marked elevations of circulating pro-inflammatory cytokines are consistently noted in heart failure patients, in both HFrEF and HFpEF subpopulations [10, 11]. Cytokine levels are further increased in patients exhibiting an acute decompensation [12] and seem to predict clinical outcome [13]. Patients with ischemic cardiomyopathy in the absence of myocardial infarction exhibit induction of chemokines in chronically ischemic myocardial segments, accompanied by recruitment of inflammatory leukocytes [14]. Moreover, several studies using experimental animal models of heart failure induced through a wide range of pathophysiologic perturbations showed that disruption of pro-inflammatory cytokine signaling may exert beneficial actions [15–17]. However, this evidence should not be interpreted as suggestive of unidimensional deleterious effects of inflammatory cytokine signaling in failing hearts. Inflammatory cytokines are highly pleiotropic and multifunctional. Several members of the cytokine and chemokine families are upregulated in response to myocardial injury and may exert important protective actions on cardiomyocytes [18], while activating reparative programs [19]. Although there is little doubt that dysregulated, excessive, or prolonged inflammatory responses precipitate or worsen heart failure in human patients, the relative contribution of inflammatory signaling likely depends on the underlying etiology of the disease. In patients developing heart failure due to viral myocarditis, inflammatory injury may be the primary cause of dysfunction and adverse remodeling [5, 20]. In contrast, in other heart failure etiologies, the role of inflammatory cytokines is less convincingly documented. All types of myocardial injury result in secondary activation of an immune response. Several lines of evidence support the notion that regardless of the underlying etiology of heart failure, cytokine and chemokine induction promote dysfunction and progressive remodeling of the myocardium. First, inflammatory cytokines have negative inotropic effects [21]. Second, inflammatory cytokines may promote cardiomyocyte apoptosis [22]. Third, pro-inflammatory cytokines may activate a matrix-degrading program, inducing matrix metalloproteinases, and triggering extracellular matrix degradation [23], thus depriving cardiomyocytes from key matrix-driven signals that preserve homeostatic function. Fourth, chronic pro-inflammatory cytokine activation may stimulate a fibrogenic program, leading to induction of fibrogenic growth factors, expansion of activated fibroblasts, and subsequent deposition of extracellular matrix (ECM) proteins in the cardiac interstitium. Inflammation-mediated interstitial fibrosis may increase myocardial stiffness, contributing to the pathogenesis of HFpEF [24, 25]. To what extent these detrimental actions outweigh any protective effects of the inflammatory mediators is dependent on the pathophysiologic context and on the cytokine-specific patterns of inflammatory activation.
Pro-Inflammatory Cytokines in Heart Failure
TNF-α
The multifunctional cytokine TNF-α is the best-studied inflammatory mediator in heart failure. In the early 1990s, observations suggesting that HFrEF patients have markedly elevated circulating TNF-α levels [10] triggered a large body of experimental work to investigate the effects of TNF-α in the failing heart. Although clinical trials showed that anti-TNF approaches do not benefit human heart failure patients, the insights gained by studying the role of TNF-α in the myocardium contributed significantly to our understanding of the complex role of inflammation in heart disease, and the clinical investigations highlighted the challenges of therapeutic translation.
Expression and Role of TNF-α in Heart Failure
Increased myocardial expression of TNF-α has been consistently documented in experimental models of heart failure [26, 27] and in human patients with cardiomyopathic conditions [28]. Several different cell types contribute to the increased expression of TNF-α in injured and failing hearts, including cardiomyocytes [27], macrophages [29], vascular cells [29], and mast cells [30]. The mechanisms of TNF-α induction may involve activation of mechanosensitive signaling cascades [27], neurohumoral signaling, or responses to damage-associated molecular patterns (DAMPs) released by injured cardiomyocytes. Several lines of evidence support the notion that TNF-α may play a causative role in heart failure. First, mice with cardiac-specific overexpression of TNF-α develop dilated cardiomyopathy [22, 31, 32] and infusion of TNF-α impairs LV systolic and diastolic function in dogs [33]. Second, TNF deletion attenuated dysfunction in a model of left ventricular pressure overload [15], and TNF-α antagonism reduced adverse remodeling and improved hemodynamics in models of volume overload and post-infarction heart failure [34, 35]. Third, in human heart failure patients, higher circulating levels of TNF-α were associated with increased mortality rates in both HFrEF and HFpEF subpopulations [36].
Cell Biological Mechanisms Responsible for the Effects of TNF-α in Heart Failure
TNF-α-mediated adverse remodeling and heart failure progression may involve effects on cardiomyocytes, macrophages, and the extracellular matrix (Fig. 1). In cardiomyocytes, TNF-α exerts negative inotropic actions by perturbing calcium homeostasis [37] and may trigger an apoptotic response by activating intrinsic cell death pathways [38]. In macrophages, TNF-α may stimulate synthesis of other pro-inflammatory cytokines with pro-apoptotic, negative inotropic, and matrix-degrading properties [39], and may upregulate expression of inducible nitric oxide synthase (iNOS) [40]. In fibroblasts, TNF-α may disrupt the balance between matrix metalloproteinases (MMPs) and their inhibitors, leading to ECM degradation [41, 42]. Finally, in the microvasculature, TNF-α increases permeability through modulation of endothelial cyclooxygenase-2, [43] and induces expression of endothelial adhesion molecules, such as intercellular adhesion molecule (ICAM)-1 and vascular cell adhesion molecule (VCAM)-1 [44], thus enhancing adhesive interactions between circulating leukocytes and the endothelial lining. Neutrophils or pro-inflammatory monocytes may be trapped in the cardiac microcirculation, thus contributing to tissue injury and cardiac dysfunction.
Fig. 1.
Cellular actions of TNF-α and IL-1 in heart failure. The pleiotropic cytokines TNF-α and IL-1 have been implicated in both post-infarction heart failure (HF) and in non-ischemic HF by modulating phenotype and function of cardiomyocytes, immune cells, fibroblasts, and vascular cells. Both TNF-α and IL-1 have negative inotropic actions and induce apoptosis in cardiomyocytes. Moreover, both TNF-α and IL-1 induce MMP expression, promoting degradation of the cardiac extracellular matrix (ECM), and stimulate inflammatory signaling in leukocytes and vascular endothelial cells. However, several studies have suggested that TNF-α may exert protective actions on cardiomyocytes under conditions of stress, by regulating calcium homeostasis and by preserving mitochondrial function. The cartoon was designed using Servier Medical Art (https://smart.servier.com/)
Several studies have suggested that in addition to its effects in progression and accentuation of adverse remodeling and dysfunction, TNF-α may also exert protective actions on injured or stressed cardiomyocytes. In a model of non-reperfused MI, global deletion of TNF receptors (TNFRs) was associated with increased infarct size, suggesting that TNF-α signaling may transduce cytoprotective signals [18]. In a genetic model of cardiomyopathy due to desmin loss, TNF-α was found to have cytoprotective actions by promoting formation of an alternative cytoskeletal network that prevents deterioration of cardiac function [45]. Whether this mechanism can be generalized in other models of heart failure remains unknown. In isolated rat hearts, low-dose TNF-α improved hemodynamics; the favorable actions were attributed to the inhibitory effect of TNF-α on cardiomyocyte calcium influx that may have reduced intracellular calcium overload [46]. In addition, TNF-α protected mitochondrial respiratory function following anoxia/reoxygenation injury presumably due to modulation of reactive oxygen species (ROS) and sphingolipids [47]. The conflicting findings suggesting both protective and injurious effects of TNF-α in vivo may reflect dose-dependent effects or differences in the balance between TNFR1 versus TNFR2 signaling in various cell types and experimental models. It has been suggested that the deleterious effects of TNF-α on cardiac remodeling may be mediated through TNFR1 signaling; in contrast, TNFR2 actions may be beneficial [39]. However, the cell-specific actions of TNFR signaling in vivo and their role in mediating cardiac remodeling have not been systematically investigated.
TNF-α Antagonism in Patients with Heart Failure
The in vivo evidence on the deleterious effects of TNF-α in the failing myocardium, and early clinical studies suggesting attenuated dysfunction in small groups of patients receiving TNF-α antagonists [48] fueled large clinical trials to investigate the effectiveness of TNF-α blockade in HFrEF patients. Unfortunately, the results were disappointing [49]. The Randomized Etanercept North AmerIcan Strategy to Study AntagoNism of CytokinEs (RENAISSANCE) and Research into Etanercept CytOkine antagonism in VEntriculaR dysfunction (RECOVER) trials tested the effects of TNF-α antagonism through administration of soluble TNFR (etanercept) in patients with heart failure and systolic dysfunction. Both trials were halted prematurely due to the lack of clinical benefit. In addition, the data from both trials were combined in the Randomized Etanercept Worldwide Evaluation (RENEWAL) trial; however, again etanercept had no effect on the primary endpoint of death or heart failure hospitalization in HFrEF patients [50]. The phase II Anti-TNF-α in Congestive Heart Failure (ATTACH) trial examined the effects of infliximab, a chimeric monoclonal anti-TNF-α antibody in HFrEF patients. TNF-α antagonism using infliximab had adverse effects, increasing all-cause mortality and heart failure hospitalizations in comparison with conventional treatment [51]. The conflicting findings between the highly promising animal model investigations and early clinical studies, and the disappointing large clinical trials are frustrating, but may be explained considering the heterogeneity of heart failure and the pleiotropic effects of the cytokines. First, in human patients the (well-described) protective effects of TNF-α on cardiomyocytes may be more prominent than any deleterious actions. Second, human heart failure populations are pathophysiologically heterogeneous. Thus, TNF-α antagonism may afford benefit in a yet unidentified subset of patients with prominent cytokine-mediated injury. Third, dose-dependent effects of the cytokine may complicate design of effective therapy. Failing hearts may require an optimal level of TNF-α activity to preserve function and to prevent excessive remodeling. In addition, intrinsic biological actions of the anti-TNF agents may have contributed to the adverse effects of the treatment in some clinical trials. TNFR antagonists may also act as agonists (referred to as “stimulating antagonists”) and may stabilize the cytokine under certain conditions [52].
IL-1
The IL-1 family has 11 cytokine members and 10 receptors [53]; IL-1α/IL-1β, IL-18, and the IL-33/ST2 axis are the best-studied members of the family in the cardiovascular system. A large body of experimental evidence supports the notion that members of the IL-1 family may play an important role in progression of heart failure and in the pathogenesis of systolic dysfunction [54, 55]. However, the potential effectiveness of IL-1 targeting in patients with heart failure has not been established.
Expression and Role of IL-1 in Heart Failure
IL-1 is consistently upregulated in experimental models of heart failure due to a wide range of etiologies, including myocardial infarction [56], left ventricular pressure overload [57, 58], transgenic overexpression of calcineurin [59], and diabetic cardiomyopathy [60]. Moreover, myocardial IL-1β induction has been reported in patients with cardiomyopathic conditions [61]. Heart failure is also associated with activation of the inflammasome [62], a molecular platform of several components that is involved in caspase-1-mediated processing of pro-IL-1β into its active form. Several cell types may contribute to IL-1 synthesis and activation in injured and failing hearts, including immune cells, fibroblasts, vascular cells, and cardiomyocytes [57, 62–64].
Extensive experimental evidence suggests an important role for IL-1 signaling in the pathogenesis of cardiac dysfunction and adverse remodeling associated with heart failure. Mice with genetic disruption of IL-1 signaling due to loss of IL1R1, the signaling receptor for IL-1, had attenuated adverse remodeling after myocardial infarction, exhibiting suppressed inflammatory responses [16]. Pharmacologic targeting of IL-1 cascades also showed protective effects in experimental models. Administration of recombinant IL-1Ra (anakinra) protected the heart from adverse remodeling in rodent models of post-infarction and non-ischemic heart failure [65, 66]. Treatment with anti-IL-1β antibodies was also effective in heart failure models. In both diabetic and non-diabetic rats with post-infarction heart failure, administration of the anti-IL-1β antibody gevokizumab attenuated dilative remodeling and improved ventricular function, reducing hypertrophy and fibrosis [67]. However, some studies have suggested that endogenous activation of sub-inflammatory levels of IL-β may also play an adaptive role following pressure overload mediating growth factor-induced compensatory hypertrophy [68].
What Are the Cellular Mechanisms of IL-1-Mediated Heart Failure?
As the prototypical pleiotropic pro-inflammatory cytokine, IL-1 acts on many different cell types (Fig. 1). Although the cellular basis for IL-1-driven cardiac remodeling and dysfunction has not been systematically studied, associative data and in vitro experiments suggest several potential mechanisms. First, much like TNF-α, IL-1 suppresses systolic cardiomyocyte function through effects that may involve disruption of calcium handling [69] or suppression of β-adrenergic responses [70]. Second, IL-1 exerts pro-apoptotic actions on cardiomyocytes [71]. Third, IL-1 induces leukocyte mobilization and activation, thus stimulating downstream inflammatory responses [72, 73]. Fourth, IL-1 may stimulate adhesion molecule expression in endothelial cells [74], promoting adhesive interactions with circulating leukocytes and increasing recruitment of inflammatory cells in the myocardium. Fifth, IL-1 promotes a matrix-degrading phenotype in fibroblasts, contributing to disruption of critical matrix–cardiomyocyte interactions required for cell survival [73]. Sixth, IL-1-driven matrix degradation may ultimately activate fibroblast-mediated matrix protein synthesis, resulting in accentuated fibrosis [75] through increased expression of fibrogenic growth factors. Seventh, IL-1 may increase arterial stiffness [76] and microvascular inflammation, thus contributing to the pathogenesis of HFpEF. Finally, in heart failure associated with autoimmune myocarditis, the effects of IL-1 may involve dendritic cell activation and subsequent stimulation of autoreactive CD4+ T cells [77].
Targeting the IL-1 System in Human Heart Failure Patients
In the Canakinumab Anti-Inflammatory Thrombosis Outcomes Study (CANTOS) trial, treatment of patients with prior myocardial infarction and evidence of active inflammation (suggested by elevated high sensitivity C-reactive protein (hsCRP)) with the anti-IL1β monoclonal antibody canakinumab had modest favorable effects, reducing the risk of the composite endpoint (non-fatal myocardial infarction, non-fatal stroke or death) by 15% in comparison with standard treatment [78]. The study supported the role of IL-1β in the pathogenesis of atherothrombotic disease and also generated observations that may be important in understanding and treating heart failure. A pre-specified exploratory analysis of the CANTOS data showed that IL-1β inhibition reduced the rate of heart failure hospitalizations or heart failure–related death in a dose-dependent manner [79]. Although the CANTOS trial was not designed to examine the effectiveness of IL-1β targeting in heart failure, the findings are consistent with animal model experiments and suggest that canakinumab may have therapeutic benefit in subsets of heart failure patients. Animal model studies also support protective actions of gevokizumab, another anti-IL-1β antibody, in patients with post-infarction heart failure [67]. In addition, other smaller studies further support this concept. In two small clinical studies in HFrEF patients, anakinra treatment improved indicators of systolic function [80]. In a small group of patients with HFpEF and elevated hsCRP, treatment with anakinra reduced NT-proBNP, but failed to improve indicators of cardiorespiratory fitness [81]. Moreover, in patients with rheumatoid arthritis, treatment with anakinra improved indicators of left ventricular and vascular function [76, 82]. Thus, IL-1 inhibition may hold promise as therapy for subpopulations of heart failure patients exhibiting prominent pro-inflammatory activation.
IL-6
IL-6 is the prototypical member of the gp130 cytokine family of cytokines that also includes several other cytokines that have been implicated in the pathogenesis of cardiovascular diseases, such as IL-11, leukemia inhibitory factor (LIF), cardiotrophin-1, and oncostatin-M. These cytokines transduce signals through the common signaling receptor subunit gp130 [83], activating Janus kinases and triggering STAT3 phosphorylation.
Expression and Role of IL-6 in Heart Failure
IL-6 is consistently upregulated in experimental models of cardiac injury and heart failure regardless of the underlying etiology, and is expressed by cardiomyocytes, infiltrating mononuclear cells, and fibroblasts [30, 84–86]. Moreover, in pressure-overloaded hearts, IL-6 induction is accompanied by upregulation of the IL-6 receptor (IL-6Rα) [86]. Increased IL-6 expression may reflect the stimulatory effects of neurohumoral pathways, Toll-like receptor (TLR) agonists, or other pro-inflammatory cytokines (such as TNF-α and IL-1) on myocardial cells, or infiltrating leukocytes. During heart failure progression, negative regulatory mechanisms may be activated to restrain expression of IL-6 and other pro-inflammatory cytokines. Degradation of IL-6 mRNA by the RNAse regnase-1 has been suggested as a mechanism restraining IL-6 expression and pro-inflammatory actions in the pressure-overloaded myocardium [87]. Although several clinical studies have demonstrated that failing hearts have increased myocardial IL-6 expression in comparison with non-failing myocardium [88], other investigations failed to show increased IL-6 synthesis in heart failure [89], but reported increased levels of downstream components of the IL-6 signaling cascade, such as gp130. The conflicting findings may reflect sampling at different stages of the disease, study of different subsets of heart failure patients, or activation of the IL-6/IL-6R axis [90] in rejected donor hearts, typically used as controls in many studies.
Experimental studies on the role of IL-6 in heart failure have produced conflicting findings, dependent on the model, the pathophysiologic context, and the type of interventions used to study the effects of IL-6 signaling. The bulk of the evidence suggests that the effects of IL-6 signaling in the failing heart are primarily pro-inflammatory and may accentuate dysfunction. Persistent gp130/STAT3 signaling enhanced inflammation in remodeling infarcted hearts [91]. Moreover, in the pressure-overloaded myocardium, genetic loss of IL6 improved cardiac function and attenuated hypertrophy through actions attributed to abrogation of CaMKII-dependent effects on cardiomyocytes [92]. However, other investigations using similar genetic approaches found no significant effects of IL6 deletion on the pressure-overloaded heart [93]. Pharmacologic blockade of IL-6 through administration of an anti-IL6R antibody attenuated dilation and improved function in a model of post-infarction heart failure [94].
The Pleiotropic Actions of IL-6 in the Failing Heart: The Impact of Cell-Specific Effects and Trans-Signaling
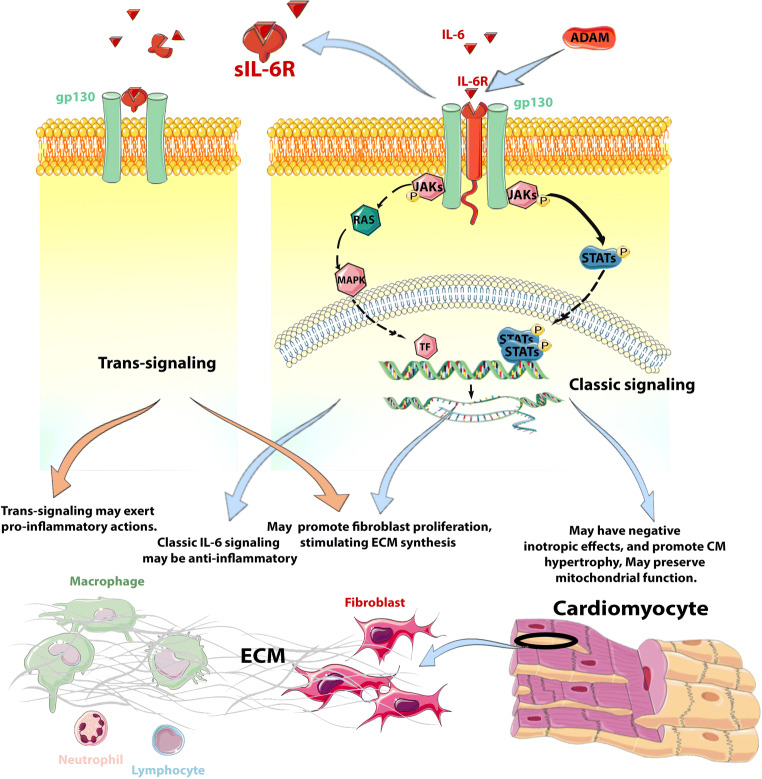
IL-6 is notorious for its pleiotropic actions on many different cell types involved in heart failure, including macrophages, lymphocytes, cardiomyocytes, fibroblasts, and vascular cells. Moreover, the concept of IL-6 trans-signaling contributes an additional layer of complexity to IL-6-mediated actions. Classic IL-6 signaling involves binding of the cytokine to the IL-6R on the cell surface, and subsequent association of the IL-6/IL-6R complex with gp130, which dimerizes and initiates signaling. However, IL-6 can also signal in the absence of cell surface IL-6R. A Disintegrin and Metalloprotease (ADAM) proteases can cleave IL-6R from the cells, generating soluble IL-6R (sIL-6R), which may associate with IL-6, stimulating gp130 signaling on cells that do not express IL-6R on their surface [95]. This mechanism called “trans-signaling” significantly expands the cellular repertoire of IL-6 and complicates interpretation of its cellular actions (Fig. 2) [83]. Unfortunately, very little is known regarding the relative in vivo role of classic and trans IL-6 signaling in the failing heart.
Fig. 2.
IL-6 signaling and cellular actions in the failing heart. The wide range of cellular targets of IL-6 and the complexity of IL-6 signaling may explain its pleiotropic actions in heart failure. IL-6 has been reported to exert both pro- and anti-inflammatory actions, stimulates fibroblast proliferation and ECM synthesis, and promotes cardiomyocyte hypertrophy. The potential role of trans-signaling adds a layer of complexity to IL-6 actions. Classically, IL-6 signals through binding to the IL-6 receptor (IL-6R) which in turn associates with the dimerized gp130 receptor subunit gp130 to form a receptor complex that activates Janus kinases and triggers STAT3 phosphorylation. Cells lacking the IL-6R may also be affected by IL-6 through trans-signaling. ADAM proteases can cleave IL-6R from cell surface, generating soluble IL-6R (sIL-6R), which may associate with IL-6, stimulating gp130/STAT3 signaling on cells lacking IL-6R. While classic IL-6 signaling may be anti-inflammatory, trans-signaling has been suggested to exert pro-inflammatory actions. The relative contributions of canonical and trans IL-6 signaling in heart failure have not been systematically studied. This cartoon was designed using Servier Medical Art (https://smart.servier.com/)
In heart failure, IL-6 has important modulatory effects on several different cell types. In cardiomyocytes, IL-6 exerts negative inotropic effects [96] and promotes a hypertrophic response [97–99] through the gp130/STAT3 pathway, but may also exert protective actions, mediated through preservation of mitochondrial function [100]. In fibroblasts, IL-6 promotes proliferation and stimulates ECM synthesis [101–103]. The combined effects of IL-6 on cardiomyocytes and fibroblasts may play an important role in the pathogenesis of HFpEF. In experimental mouse studies, infusion of IL-6 caused concentric hypertrophy and fibrosis, and increased myocardial stiffness [97]. IL-6 also has potent modulatory effects on macrophages and lymphocytes. Both pro- and anti-inflammatory effects of IL-6 have been reported [104–107]; trans-signaling has been suggested to exert pro-inflammatory actions, whereas canonical IL-6 signaling may be anti-inflammatory [108]. The in vivo role of IL-6 in inflammation is likely dependent on the relative contribution of macrophage and lymphocyte subsets, and on the relative role of classic versus trans-signaling in each specific inflammatory condition. In the absence of cell-specific dissection in vivo, it is impossible to define the role of inflammatory signaling in mediating the in vivo effects of IL-6 in failing hearts.
Targeting IL-6 in Human Heart Failure
Extensive evidence suggests that IL-6 plays a crucial role in the post-inflammatory hepatic acute phase response and is implicated in autoimmunity. Based on this evidence, IL-6 has been considered an attractive therapeutic target in many conditions associated with inflammation. The IL-6 receptor neutralizing antibody tocilizumab has been approved as effective therapy for patients with moderate to severe rheumatoid arthritis and temporal arteritis, and for the treatment of the cytokine release syndrome associated with CAR-T cell therapies. Experimental evidence demonstrating involvement of IL-6 signaling in the pathogenesis of heart failure suggests that treatment with tocilizumab may also be effective in heart failure patients. However, clinical studies supporting this notion are lacking. In patients with rheumatoid arthritis in the absence of cardiovascular disease, tocilizumab reduced the circulating levels of N-terminal pro-B-type natriuretic peptide (NT-proBNP) [109]; this finding may reflect cardioprotective actions that may attenuate heart failure development. A phase II clinical trial tested the effectiveness of tocilizumab in reducing ischemic myocardial injury in acute coronary syndromes. In non-ST elevation myocardial infarction (non-STEMI) patients, a single dose of tocilizumab administered prior to coronary angiography was safe and attenuated troponin T release and systemic inflammation [110]. Although IL-6 blockade reduced serum CRP, levels of the chemokines CXCL10 and CCL4 were increased, highlighting the complexity of IL-6 actions on inflammatory cascades [111].
It should be noted that the use of anti-IL-6 therapeutics is complicated by the classic versus trans-signaling actions of the cytokine. Anti-IL-6R antibodies block all modes of IL-6 signaling, whereas soluble gp130 selectively inhibits IL-6 trans-signaling by binding to the IL-6–sIL-6R complex. The effects of various IL-6 targeting strategies on the failing heart have not been systematically investigated.
CCL2 and the Chemokines
Chemokines are small (8–12 kDa) chemotactic cytokines that regulate cell migration and positioning in development, homeostasis, and inflammation [112]. On a structural basis, chemokines can be subclassified into four subfamilies: the XC, CC, CXC, and CX3C chemokines. From a functional perspective, chemokines can be “homeostatic” (constitutively expressed in certain tissues and involved in basal leukocyte trafficking and formation of lymphoid organs), “inflammatory” (members inducible following injury with effects in leukocyte recruitment and activation) [113–115], or may exhibit both homeostatic and inflammatory roles. The inflammatory CC chemokine CCL2/MCP-1 is the best-studied member of the family in heart failure and has been suggested as a therapeutic target in conditions associated with myocardial injury and adverse remodeling [116].
Expression and Role of CCL2 in Failing Hearts
CCL2 is markedly and consistently upregulated in experimental models of cardiac injury, remodeling and heart failure [19, 57, 117–119]. In infarcted and in failing hearts, CCL2 has been localized in endothelial cells [117], vascular smooth muscle cells [120], mononuclear cells [17], and cardiomyocytes [119]; its induction may involve activation of TLR signaling, neurohumoral cascades, or pro-inflammatory cytokine-mediated pathways [115]. Studies in human patients also demonstrated CCL2 upregulation in failing hearts. CCL2 was overexpressed in myocardial samples from patients with ischemic [14], dilated [121], or hypertrophic cardiomyopathy [122].
Extensive experimental evidence suggests that CCL2 contributes to adverse remodeling, dysfunction, and fibrosis in models of infarctive and non-infarctive heart failure (Table 1). In models of myocardial infarction, CCL2 deletion and anti-CCL2 gene therapy improved adverse remodeling [124], at the expense of delayed phagocytosis of dead cardiomyocytes with granulation tissue [19]. In a model of ischemic fibrotic cardiomyopathy induced through brief repetitive ischemia followed by reperfusion, CCL2 contributed to macrophage recruitment, fibrotic remodeling, and systolic dysfunction [17]. Moreover, in a model of left ventricular pressure overload, CCL2 neutralization attenuated diastolic dysfunction, reducing fibrosis [120]. Clinical studies have also generated associative data consistent with an important role of CCL2 in heart failure. In HFrEF patients, high circulating CCL2 levels were associated with more severe symptoms and worse systolic dysfunction [130]. Moreover, in patients with advanced heart failure, high circulating levels of CCL2 were associated with increased mortality [131].
Table 1.
Experimental studies investigating the role of the CCL2/CCR2 axis in heart failure
| Heart failure model | Intervention | Effects on cardiac function and remodeling | Cellular target and molecular mechanism | Reference |
|---|---|---|---|---|
| Rat model of pressure overload through suprarenal aortic constriction | Anti-CCL2 neutralizing antibody | Anti-CCL2 antibody ameliorated diastolic dysfunction. | Decreased macrophage recruitment, fibroblast proliferation and TGF-β production associated with attenuated myocardial fibrosis | [120] |
| Mouse model of left ventricular pressure overload | CCR2 antagonist and antibody-mediated CCR2+ cell depletion | CCR2 antagonist and depletion of CCR2+ cells attenuated LV dilation and systolic dysfunction | Attenuated CCR2+ macrophage recruitment, cardiomyocyte hypertrophy, and cardiac fibrosis | [123] |
| Mouse model of non-reperfused myocardial infarction | Anti-CCL2 gene therapy | Anti-CCL2 therapy attenuated LV dilatation and systolic dysfunction, and increased post-MI survival | Attenuated interstitial fibrosis, macrophage infiltration, and TNF-α and TGF-β1 levels | [124] |
| Mouse model of reperfused myocardial infarction | CCL2 KO and antibody neutralization | CCL2 KO mice had reduced post-infarction dilative remodeling | Attenuated myofibroblast proliferation, reduced macrophage recruitment and activation, associated with reduced fibrosis and delayed granulation tissue formation | [19] |
| Mouse model of ischemic cardiomyopathy induced through brief repetitive ischemia/reperfusion | CCL2 KO and antibody neutralization | CCL2 KO mice had improved systolic function, evidenced by increased fractional shortening | Reduced fibroblast proliferation and macrophage recruitment associated with attenuated interstitial fibrosis | [17] |
| Mouse model of ischemia/reperfusion | Depletion of CCR2+ macrophages (by injecting DT in CCR2-DTR mice) | Depletion of CCR2+ macrophages improved LV systolic function, and reduced LV dilation | Reduced infarct size and attenuated cardiomyocyte hypertrophy | [125] |
| Mouse model of angiotensin II-induced cardiac remodeling | CCL2 KO | CCL2 loss did not affect systolic function, but attenuated fibrosis | Attenuated fibrogenic effects of Ang-II, and the expression of TNF-α and TGF-β1 | [126] |
| Mouse model of aging | CCL2 KO | Aged CCL2 KO mice had attenuated diastolic dysfunction | Reduced leukocyte infiltration, associated with attenuated fibrosis | [127] |
| Mouse model of streptozotocin-induced diabetes |
CCR2 KO CCR2 inhibitor |
CCR2 KO and inhibitor improved cardiac function and reduced LV dilation in diabetic mice | Attenuated cardiomyocyte apoptosis and induced polarization of M2 macrophages. In addition, CCR2 KO reduced myocardial fibrosis presumably due to decreased macrophage-driven inflammation and oxidative stress | [128] |
| N/A | Transgenic Cardiomyocyte-specific CCL2 overexpression | Cardiomyocyte-specific CCL2 overexpression in mice induced cardiac hypertrophy and dilation | Induced myocardial inflammation and fibrotic changes attributed to inflammatory cell recruitment and activation | [129] |
KO knockout
What Is the Cellular Basis for the Effects of CCL2 on Cardiac Remodeling and Dysfunction?
Immune cells are the most likely major cellular targets of CCL2 in failing hearts. As an inducible inflammatory CC chemokine, CCL2 is markedly upregulated following injury, binds to proteoglycans on the endothelium or the ECM, and promotes recruitment of pro-inflammatory CCR2+ monocytes. In the infarcted and remodeling myocardium, CCR2+ monocytes may promote injury and exacerbate dysfunction by secreting pro-inflammatory cytokines and matrix-degrading proteases. CCL2-driven pro-inflammatory signaling may accentuate cardiomyocyte death; disruption of the CCL2/CCR2 axis in experimental models of myocardial infarction was reported to reduce infarct size in many [132–135] but not in all studies [19].
CCL2 may also exert potent fibrogenic actions on the remodeling myocardium [17]. CCL2-mediated fibrosis has been attributed primarily to recruitment and activation of monocytes and macrophages, resulting in increased synthesis of fibrogenic mediators, such as TGF-β and osteopontin [17, 19, 136]. Whether CCL2 may also exert direct fibrogenic actions through effects on resident cardiac fibroblasts or their progenitors remains controversial. Although CCL2 has been reported to stimulate pro-fibrotic signaling in skin, liver, and lung fibroblasts [137–139], in cardiac fibroblasts, CCL2 did not affect matrix gene synthesis or proliferative activity [17]. It has also been suggested that CCL2 may exert fibrogenic actions through recruitment of circulating fibroblast progenitors [126, 140]. However, the evidence supporting this notion is associative, based on co-localization of relatively non-specific hematopoietic cell and fibroblast markers in the same cells. Lineage tracing studies have consistently demonstrated that most activated fibroblasts in failing hearts are derived from resident fibroblast populations, and not from circulating hematopoietic cells [141–143] Thus, the potential role of CCL2-mediated recruitment of fibroblast progenitors in cardiac fibrosis remains unclear [144].
It has also been suggested that CCL2 may exert direct actions on cardiomyocytes, increasing injury-associated death and promoting dysfunction. Some studies have suggested that CCL2 may promote cardiomyocyte apoptosis through induction of the ribonuclease monocyte chemoattractant protein-1-induced protein (MCPIP, originally proposed to function as a transcription factor), also known as regnase-1 [145, 146]. However, regnase-1/MCPIP can be induced by a wide range of inflammatory mediators, and is known to restrain inflammation by degrading cytokine RNAs in immune and non-immune cells [147]. Although the bulk of the experimental evidence suggests that CCL2 contributes to adverse remodeling (while playing a role in cardiac repair), some studies using CCL2-overexpressing mice have suggested cardioprotective actions of CCL2 in ischemia/reperfusion, mediated through effects that may involve attenuation of oxidative stress [148]. These findings may reflect the consequences of baseline alterations in the cardiac microenvironment in CCL2-overexpressing mice undergoing ischemia protocols, rather than direct protective actions of CCL2 on cardiomyocytes.
CCL2 as a Therapeutic Target in Heart Failure
Considering the extensive evidence suggesting a causative role for CCL2 in cardiac remodeling and dysfunction, antagonism of the CCL2:CCR2 axis holds promise as heart failure therapy. Other CC chemokines may also be involved in recruitment of pro-inflammatory leukocytes; thus, combined targeting of several CC chemokine receptors may increase the effectiveness of the approach. Despite decades of experimental work on the biology of the chemokines, implementation of chemokine-targeting therapeutics in inflammatory conditions remains at an early stage. In a phase II clinical trial, treatment with an anti-CCR2 antibody failed to improve symptoms in patients with rheumatoid arthritis [149]. Another phase II trial using the dual CCR2/CCR5 inhibitor cenicriviroc in patients with non-alcoholic steatohepatitis showed promise, suggesting attenuation of inflammation-driven fibrosis [150]. The effectiveness of CC chemokine targeting in human patients with heart failure has not been tested. Despite the established role of the CCL2/CCR2 axis in cardiac remodeling, several concerns are raised regarding the potential effects of CC chemokine inhibition. First, macrophages do not exert solely pro-inflammatory actions, but also serve to downregulate inflammation and to stimulate angiogenesis. Experimental studies have suggested that CCL2 may play a role in arteriogenesis [151], a process that may be important for preservation of myocardial perfusion in patients with heart failure. Targeting CCR2 may not selectively inhibit recruitment of pro-inflammatory macrophages, but may also perturb downstream inflammatory responses that recruit protective leukocyte subsets in the remodeling myocardium. Second, use of dual CC chemokine inhibitors to target inflammation in heart failure may also reduce recruitment of lymphocyte subpopulations involved in suppression of inflammation, such as regulatory T cells (Tregs) [152].
The Challenges of Clinical Translation
Therapeutic translation is always challenging, especially when dealing with a pathophysiologically heterogeneous condition, such as heart failure. Despite the promising experimental findings in animal models, targeting pro-inflammatory chemokines and cytokines has not yet produced therapeutic benefit in patients with heart failure. Several major challenges have hampered therapeutic translation. First, documentation of clinical benefits in human heart failure populations requires well-designed and very expensive clinical trials with long follow-up. Thus, the pace of testing candidate agents in clinical trials is predictably slow. Second, animal models are inherently suboptimal tools for prediction of therapeutic efficacy. The strength of animal model studies lies in the provision of cell biological insights using reductionist approaches and standardized protocols. No animal model can recapitulate the pathophysiologic heterogeneity of human heart failure. Thus, a major priority in clinical heart failure research is the pathophysiologic stratification of human patient populations and the identification of patient subsets with excessive or dysregulated inflammatory responses. Use of inflammatory biomarkers and imaging strategies may contribute to identification of patients that may benefit from targeted cytokine therapeutics [153]. Third, the need for chronic administration of cytokine or chemokine inhibitors to delay progression of heart failure is a major concern. Pro-inflammatory signaling plays an important role in the defense against infections, in reparative responses to injury, and in control of tumors. Moreover, some members of the cytokine family have been suggested to exert important protective actions on cardiomyocytes under conditions of stress. Considering the perils of chronic administration of anti-cytokine therapeutics, it may be preferable to focus on clinical settings associated with rapid inflammation-driven cardiac remodeling, such as post-infarction heart failure [154] or acute myocarditis. In these conditions, brief cytokine inhibition may have lasting effects on the remodeling process, protecting from the development of heart failure.
Conclusions
Over the last 30 years, experimental and clinical studies have greatly contributed to our understanding of the role of inflammation in the pathogenesis of heart failure. Despite early disappointments in clinical translation, targeting inflammatory mediators remains a promising and attractive direction in heart failure therapeutics. Successful implementation of cytokine targeting approaches in heart failure patients will require dissection of specific pro-inflammatory pathways with a critical role in dysfunction and progression of adverse remodeling, and identification of patient subpopulations with dysregulated or overactive inflammatory responses that may derive maximal benefit from targeted cytokine or chemokine inhibition.
Acknowledgments
Availability of Data and Material
N/A
Code Availability
N/A
Funding
N.G.F.’s laboratory is supported by NIH grants R01 HL76246, R01 HL85440, and R01 HL149407 and by U.S. Department of Defense grants PR151029 and PR181464.
Compliance with Ethical Standards
Conflicts of Interest/Competing Interests
None.
Ethics Approval
N/A
Consent to Participate
N/A
Consent for Publication
N/A
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pfeffer MA, Shah AM, Borlaug BA. Heart failure with preserved ejection fraction in perspective. Circ Res. 2019;124:1598–1617. doi: 10.1161/CIRCRESAHA.119.313572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Braunwald E. Heart disease. A textbook of cardiovascular medicine. 4th Ed. Philadelphia: WB Saunders; 1992. [Google Scholar]
- 3.Senni M, Tribouilloy CM, Rodeheffer RJ, Jacobsen SJ, Evans JM, Bailey KR, Redfield MM. Congestive heart failure in the community: a study of all incident cases in Olmsted County, Minnesota, in 1991. Circulation. 1998;98:2282–2289. doi: 10.1161/01.cir.98.21.2282. [DOI] [PubMed] [Google Scholar]
- 4.Dick SA, Epelman S. Chronic heart failure and inflammation: what do we really know? Circ Res. 2016;119:159–176. doi: 10.1161/CIRCRESAHA.116.308030. [DOI] [PubMed] [Google Scholar]
- 5.Trachtenberg BH, Hare JM. Inflammatory cardiomyopathic syndromes. Circ Res. 2017;121:803–818. doi: 10.1161/CIRCRESAHA.117.310221. [DOI] [PubMed] [Google Scholar]
- 6.Wilson HM, Cheyne L, Brown PAJ, Kerr K, Hannah A, Srinivasan J, Duniak N, Horgan G, Dawson DK. Characterization of the myocardial inflammatory response in acute stress-induced (Takotsubo) cardiomyopathy. JACC Basic Transl Sci. 2018;3:766–778. doi: 10.1016/j.jacbts.2018.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scally C, Abbas H, Ahearn T, Srinivasan J, Mezincescu A, Rudd A, Spath N, Yucel-Finn A, Yuecel R, Oldroyd K, Dospinescu C, Horgan G, Broadhurst P, Henning A, Newby DE, Semple S, Wilson HM, Dawson DK. Myocardial and systemic inflammation in acute stress-induced (Takotsubo) cardiomyopathy. Circulation. 2019;139:1581–1592. doi: 10.1161/CIRCULATIONAHA.118.037975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Giustino G, Croft LB, Oates CP, Rahman K, Lerakis S, Reddy VY, Goldman M. Takotsubo cardiomyopathy in COVID-19. J Am Coll Cardiol. 2020;76:628–629. doi: 10.1016/j.jacc.2020.05.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jabri A, Kalra A, Kumar A, Alameh A, Adroja S, Bashir H, Nowacki AS, Shah R, Khubber S, Kanaa’N A, Hedrick DP, Sleik KM, Mehta N, Chung MK, Khot UN, Kapadia SR, Puri R, Reed GW. Incidence of stress cardiomyopathy during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3:e2014780. doi: 10.1001/jamanetworkopen.2020.14780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levine B, Kalman J, Mayer L, Fillit HM, Packer M. Elevated circulating levels of tumor necrosis factor in severe chronic heart failure. N Engl J Med. 1990;323:236–241. doi: 10.1056/NEJM199007263230405. [DOI] [PubMed] [Google Scholar]
- 11.Sanders-van Wijk S, van Empel V, Davarzani N, Maeder MT, Handschin R, Pfisterer ME, Brunner-la Rocca HP, for the TIME-CHF investigators Circulating biomarkers of distinct pathophysiological pathways in heart failure with preserved vs. reduced left ventricular ejection fraction. Eur J Heart Fail. 2015;17:1006–1014. doi: 10.1002/ejhf.414. [DOI] [PubMed] [Google Scholar]
- 12.Abernethy A, Raza S, Sun JL, Anstrom KJ, Tracy R, Steiner J, et al. Pro-inflammatory biomarkers in stable versus acutely decompensated heart failure with preserved ejection fraction. J Am Heart Assoc. 2018;7. 10.1161/JAHA.117.007385. [DOI] [PMC free article] [PubMed]
- 13.Chirinos JA, Orlenko A, Zhao L, Basso MD, Cvijic ME, Li Z, Spires TE, Yarde M, Wang Z, Seiffert DA, Prenner S, Zamani P, Bhattacharya P, Kumar A, Margulies KB, Car BD, Gordon DA, Moore JH, Cappola TP. Multiple plasma biomarkers for risk stratification in patients with heart failure and preserved ejection fraction. J Am Coll Cardiol. 2020;75:1281–1295. doi: 10.1016/j.jacc.2019.12.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frangogiannis NG, Shimoni S, Chang SM, Ren G, Shan K, Aggeli C, Reardon MJ, Letsou GV, Espada R, Ramchandani M, Entman ML, Zoghbi WA. Evidence for an active inflammatory process in the hibernating human myocardium. Am J Pathol. 2002;160:1425–1433. doi: 10.1016/S0002-9440(10)62568-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun M, Chen M, Dawood F, Zurawska U, Li JY, Parker T, Kassiri Z, Kirshenbaum LA, Arnold M, Khokha R, Liu PP. Tumor necrosis factor-alpha mediates cardiac remodeling and ventricular dysfunction after pressure overload state. Circulation. 2007;115:1398–1407. doi: 10.1161/CIRCULATIONAHA.106.643585. [DOI] [PubMed] [Google Scholar]
- 16.Bujak M, Dobaczewski M, Chatila K, Mendoza LH, Li N, Reddy A, Frangogiannis NG. Interleukin-1 receptor type I signaling critically regulates infarct healing and cardiac remodeling. Am J Pathol. 2008;173:57–67. doi: 10.2353/ajpath.2008.070974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frangogiannis NG, Dewald O, Xia Y, Ren G, Haudek S, Leucker T, Kraemer D, Taffet G, Rollins BJ, Entman ML. Critical role of monocyte chemoattractant protein-1/CC chemokine ligand 2 in the pathogenesis of ischemic cardiomyopathy. Circulation. 2007;115:584–592. doi: 10.1161/CIRCULATIONAHA.106.646091. [DOI] [PubMed] [Google Scholar]
- 18.Kurrelmeyer KM, Michael LH, Baumgarten G, Taffet GE, Peschon JJ, Sivasubramanian N, Entman ML, Mann DL. Endogenous tumor necrosis factor protects the adult cardiac myocyte against ischemic-induced apoptosis in a murine model of acute myocardial infarction. Proc Natl Acad Sci U S A. 2000;97:5456–5461. doi: 10.1073/pnas.070036297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dewald O, Zymek P, Winkelmann K, Koerting A, Ren G, Abou-Khamis T, Michael LH, Rollins BJ, Entman ML, Frangogiannis NG. CCL2/monocyte chemoattractant protein-1 regulates inflammatory responses critical to healing myocardial infarcts. Circ Res. 2005;96:881–889. doi: 10.1161/01.RES.0000163017.13772.3a. [DOI] [PubMed] [Google Scholar]
- 20.Zhao L, Fu Z. Roles of host immunity in viral myocarditis and dilated cardiomyopathy. J Immunol Res. 2018;2018:5301548. doi: 10.1155/2018/5301548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Finkel MS, Oddis CV, Jacob TD, Watkins S, Hattler B, Simmons R. Negative inotropic effects of cytokines on the heart mediated by nitric oxide. Science. 1992;257:387–389. doi: 10.1126/science.1631560. [DOI] [PubMed] [Google Scholar]
- 22.Kubota T, McTiernan CF, Frye CS, et al. Dilated cardiomyopathy in transgenic mice with cardiac-specific overexpression of tumor necrosis factor-alpha. Circ Res. 1997;81:627–635. doi: 10.1161/01.res.81.4.627. [DOI] [PubMed] [Google Scholar]
- 23.Siwik DA, Chang DL, Colucci WS. Interleukin-1beta and tumor necrosis factor-alpha decrease collagen synthesis and increase matrix metalloproteinase activity in cardiac fibroblasts in vitro. Circ Res. 2000;86:1259–1265. doi: 10.1161/01.res.86.12.1259. [DOI] [PubMed] [Google Scholar]
- 24.Packer M, Kitzman DW. Obesity-related heart failure with a preserved ejection fraction: the mechanistic rationale for combining inhibitors of aldosterone, neprilysin, and sodium-glucose cotransporter-2. JACC Heart Fail. 2018;6:633–639. doi: 10.1016/j.jchf.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 25.Frangogiannis NG. The extracellular matrix in ischemic and nonischemic heart failure. Circ Res. 2019;125:117–146. doi: 10.1161/CIRCRESAHA.119.311148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kapadia S, Lee J, Torre-Amione G, Birdsall HH, Ma TS, Mann DL. Tumor necrosis factor-alpha gene and protein expression in adult feline myocardium after endotoxin administration. J Clin Invest. 1995;96:1042–1052. doi: 10.1172/JCI118090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kapadia SR, Oral H, Lee J, Nakano M, Taffet GE, Mann DL. Hemodynamic regulation of tumor necrosis factor-alpha gene and protein expression in adult feline myocardium. Circ Res. 1997;81:187–195. doi: 10.1161/01.res.81.2.187. [DOI] [PubMed] [Google Scholar]
- 28.Torre-Amione G, Kapadia S, Lee J, Durand JB, Bies RD, Young JB, Mann DL. Tumor necrosis factor-alpha and tumor necrosis factor receptors in the failing human heart. Circulation. 1996;93:704–711. doi: 10.1161/01.cir.93.4.704. [DOI] [PubMed] [Google Scholar]
- 29.Shioi T, Matsumori A, Sasayama S. Persistent expression of cytokine in the chronic stage of viral myocarditis in mice. Circulation. 1996;94:2930–2937. doi: 10.1161/01.cir.94.11.2930. [DOI] [PubMed] [Google Scholar]
- 30.Frangogiannis NG, Lindsey ML, Michael LH, Youker KA, Bressler RB, Mendoza LH, Spengler RN, Smith CW, Entman ML. Resident cardiac mast cells degranulate and release preformed TNF-alpha, initiating the cytokine cascade in experimental canine myocardial ischemia/reperfusion. Circulation. 1998;98:699–710. doi: 10.1161/01.cir.98.7.699. [DOI] [PubMed] [Google Scholar]
- 31.Janczewski AM, Kadokami T, Lemster B, Frye CS, McTiernan CF, Feldman AM. Morphological and functional changes in cardiac myocytes isolated from mice overexpressing TNF-alpha. Am J Physiol Heart Circ Physiol. 2003;284:H960–H969. doi: 10.1152/ajpheart.0718.2001. [DOI] [PubMed] [Google Scholar]
- 32.Bryant D, Becker L, Richardson J, Shelton J, Franco F, Peshock R, Thompson M, Giroir B. Cardiac failure in transgenic mice with myocardial expression of tumor necrosis factor-alpha. Circulation. 1998;97:1375–1381. doi: 10.1161/01.cir.97.14.1375. [DOI] [PubMed] [Google Scholar]
- 33.Pagani FD, Baker LS, Hsi C, Knox M, Fink MP, Visner MS. Left ventricular systolic and diastolic dysfunction after infusion of tumor necrosis factor-alpha in conscious dogs. J Clin Invest. 1992;90:389–398. doi: 10.1172/JCI115873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jobe LJ, Melendez GC, Levick SP, et al. TNF-alpha inhibition attenuates adverse myocardial remodeling in a rat model of volume overload. Am J Physiol Heart Circ Physiol. 2009;297:H1462–H1468. doi: 10.1152/ajpheart.00442.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berry MF, Woo YJ, Pirolli TJ, Bish LT, Moise MA, Burdick JW, Morine KJ, Jayasankar V, Gardner TJ, Sweeney HL. Administration of a tumor necrosis factor inhibitor at the time of myocardial infarction attenuates subsequent ventricular remodeling. J Heart Lung Transplant. 2004;23:1061–1068. doi: 10.1016/j.healun.2004.06.021. [DOI] [PubMed] [Google Scholar]
- 36.Dunlay SM, Weston SA, Redfield MM, Killian JM, Roger VL. Tumor necrosis factor-alpha and mortality in heart failure: a community study. Circulation. 2008;118:625–631. doi: 10.1161/CIRCULATIONAHA.107.759191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yokoyama T, Vaca L, Rossen RD, Durante W, Hazarika P, Mann DL. Cellular basis for the negative inotropic effects of tumor necrosis factor-alpha in the adult mammalian heart. J Clin Invest. 1993;92:2303–2312. doi: 10.1172/JCI116834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haudek SB, Taffet GE, Schneider MD, Mann DL. TNF provokes cardiomyocyte apoptosis and cardiac remodeling through activation of multiple cell death pathways. J Clin Invest. 2007;117:2692–2701. doi: 10.1172/JCI29134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hamid T, Gu Y, Ortines RV, Bhattacharya C, Wang G, Xuan YT, Prabhu SD. Divergent tumor necrosis factor receptor-related remodeling responses in heart failure: role of nuclear factor-kappaB and inflammatory activation. Circulation. 2009;119:1386–1397. doi: 10.1161/CIRCULATIONAHA.108.802918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sanders DB, Larson DF, Hunter K, Gorman M, Yang B. Comparison of tumor necrosis factor-alpha effect on the expression of iNOS in macrophage and cardiac myocytes. Perfusion. 2001;16:67–74. doi: 10.1177/026765910101600110. [DOI] [PubMed] [Google Scholar]
- 41.Sivasubramanian N, Coker ML, Kurrelmeyer KM, MacLellan WR, DeMayo FJ, Spinale FG, Mann DL. Left ventricular remodeling in transgenic mice with cardiac restricted overexpression of tumor necrosis factor. Circulation. 2001;104:826–831. doi: 10.1161/hc3401.093154. [DOI] [PubMed] [Google Scholar]
- 42.Li YY, Feng YQ, Kadokami T, McTiernan CF, Draviam R, Watkins SC, Feldman AM. Myocardial extracellular matrix remodeling in transgenic mice overexpressing tumor necrosis factor alpha can be modulated by anti-tumor necrosis factor alpha therapy. Proc Natl Acad Sci U S A. 2000;97:12746–12751. doi: 10.1073/pnas.97.23.12746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mark KS, Trickler WJ, Miller DW. Tumor necrosis factor-alpha induces cyclooxygenase-2 expression and prostaglandin release in brain microvessel endothelial cells. J Pharmacol Exp Ther. 2001;297:1051–1058. [PubMed] [Google Scholar]
- 44.Mattila P, Majuri ML, Mattila PS, Renkonen R. TNF alpha-induced expression of endothelial adhesion molecules, ICAM-1 and VCAM-1, is linked to protein kinase C activation. Scand J Immunol. 1992;36:159–165. doi: 10.1111/j.1365-3083.1992.tb03087.x. [DOI] [PubMed] [Google Scholar]
- 45.Papathanasiou S, Rickelt S, Soriano ME, Schips TG, Maier HJ, Davos CH, Varela A, Kaklamanis L, Mann DL, Capetanaki Y. Tumor necrosis factor-alpha confers cardioprotection through ectopic expression of keratins K8 and K18. Nat Med. 2015;21:1076–1084. doi: 10.1038/nm.3925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rathi SS, Xu YJ, Dhalla NS. Mechanism of cardioprotective action of TNF-alpha in the isolated rat heart. Exp Clin Cardiol. 2002;7:146–150. [PMC free article] [PubMed] [Google Scholar]
- 47.Lacerda L, McCarthy J, Mungly SF, et al. TNFalpha protects cardiac mitochondria independently of its cell surface receptors. Basic Res Cardiol. 2010;105:751–762. doi: 10.1007/s00395-010-0113-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Deswal A, Bozkurt B, Seta Y, Parilti-Eiswirth S, Hayes FA, Blosch C, Mann DL. Safety and efficacy of a soluble P75 tumor necrosis factor receptor (Enbrel, etanercept) in patients with advanced heart failure. Circulation. 1999;99:3224–3226. doi: 10.1161/01.cir.99.25.3224. [DOI] [PubMed] [Google Scholar]
- 49.Adamo L, Rocha-Resende C, Prabhu SD, Mann DL. Reappraising the role of inflammation in heart failure. Nat Rev Cardiol. 2020;17:269–285. doi: 10.1038/s41569-019-0315-x. [DOI] [PubMed] [Google Scholar]
- 50.Mann DL, McMurray JJ, Packer M, et al. Targeted anticytokine therapy in patients with chronic heart failure: results of the randomized etanercept worldwide evaluation (RENEWAL) Circulation. 2004;109:1594–1602. doi: 10.1161/01.CIR.0000124490.27666.B2. [DOI] [PubMed] [Google Scholar]
- 51.Chung ES, Packer M, Lo KH, Fasanmade AA, Willerson JT, Anti-TNF Therapy Against Congestive Heart Failure Investigators Randomized, double-blind, placebo-controlled, pilot trial of infliximab, a chimeric monoclonal antibody to tumor necrosis factor-alpha, in patients with moderate-to-severe heart failure: results of the anti-TNF therapy against congestive heart failure (ATTACH) trial. Circulation. 2003;107:3133–3140. doi: 10.1161/01.CIR.0000077913.60364.D2. [DOI] [PubMed] [Google Scholar]
- 52.Klein B, Brailly H. Cytokine-binding proteins: stimulating antagonists. Immunol Today. 1995;16:216–220. doi: 10.1016/0167-5699(95)80161-8. [DOI] [PubMed] [Google Scholar]
- 53.Dinarello CA. Overview of the IL-1 family in innate inflammation and acquired immunity. Immunol Rev. 2018;281:8–27. doi: 10.1111/imr.12621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bujak M, Frangogiannis NG. The role of IL-1 in the pathogenesis of heart disease. Arch Immunol Ther Exp. 2009;57:165–176. doi: 10.1007/s00005-009-0024-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Abbate A, Toldo S, Marchetti C, Kron J, van Tassell BW, Dinarello CA. Interleukin-1 and the Inflammasome as therapeutic targets in cardiovascular disease. Circ Res. 2020;126:1260–1280. doi: 10.1161/CIRCRESAHA.120.315937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dewald O, Ren G, Duerr GD, Zoerlein M, Klemm C, Gersch C, Tincey S, Michael LH, Entman ML, Frangogiannis NG. Of mice and dogs: species-specific differences in the inflammatory response following myocardial infarction. Am J Pathol. 2004;164:665–677. doi: 10.1016/S0002-9440(10)63154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Shioi T, Matsumori A, Kihara Y, Inoko M, Ono K, Iwanaga Y, Yamada T, Iwasaki A, Matsushima K, Sasayama S. Increased expression of interleukin-1 beta and monocyte chemotactic and activating factor/monocyte chemoattractant protein-1 in the hypertrophied and failing heart with pressure overload. Circ Res. 1997;81:664–671. doi: 10.1161/01.res.81.5.664. [DOI] [PubMed] [Google Scholar]
- 58.Xia Y, Lee K, Li N, Corbett D, Mendoza L, Frangogiannis NG. Characterization of the inflammatory and fibrotic response in a mouse model of cardiac pressure overload. Histochem Cell Biol. 2009;131:471–481. doi: 10.1007/s00418-008-0541-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bracey NA, Beck PL, Muruve DA, Hirota SA, Guo J, Jabagi H, Wright Jr JR, MacDonald JA, Lees-Miller JP, Roach D, Semeniuk LM, Duff HJ. The Nlrp3 inflammasome promotes myocardial dysfunction in structural cardiomyopathy through interleukin-1beta. Exp Physiol. 2013;98:462–472. doi: 10.1113/expphysiol.2012.068338. [DOI] [PubMed] [Google Scholar]
- 60.Luo B, Li B, Wang W, Liu X, Xia Y, Zhang C, Zhang M, Zhang Y, An F. NLRP3 gene silencing ameliorates diabetic cardiomyopathy in a type 2 diabetes rat model. PLoS One. 2014;9:e104771. doi: 10.1371/journal.pone.0104771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Francis SE, Holden H, Holt CM, Duff GW. Interleukin-1 in myocardium and coronary arteries of patients with dilated cardiomyopathy. J Mol Cell Cardiol. 1998;30:215–223. doi: 10.1006/jmcc.1997.0592. [DOI] [PubMed] [Google Scholar]
- 62.Suetomi T, Willeford A, Brand CS, Cho Y, Ross RS, Miyamoto S, Brown JH. Inflammation and NLRP3 inflammasome activation initiated in response to pressure overload by Ca(2+)/calmodulin-dependent protein kinase II delta signaling in cardiomyocytes are essential for adverse cardiac remodeling. Circulation. 2018;138:2530–2544. doi: 10.1161/CIRCULATIONAHA.118.034621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mezzaroma E, Toldo S, Farkas D, Seropian IM, van Tassell BW, Salloum FN, Kannan HR, Menna AC, Voelkel NF, Abbate A. The inflammasome promotes adverse cardiac remodeling following acute myocardial infarction in the mouse. Proc Natl Acad Sci U S A. 2011;108:19725–19730. doi: 10.1073/pnas.1108586108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kawaguchi M, Takahashi M, Hata T, Kashima Y, Usui F, Morimoto H, Izawa A, Takahashi Y, Masumoto J, Koyama J, Hongo M, Noda T, Nakayama J, Sagara J, Taniguchi S', Ikeda U. Inflammasome activation of cardiac fibroblasts is essential for myocardial ischemia/reperfusion injury. Circulation. 2011;123:594–604. doi: 10.1161/CIRCULATIONAHA.110.982777. [DOI] [PubMed] [Google Scholar]
- 65.Abbate A, Salloum FN, Vecile E, Das A, Hoke NN, Straino S, Biondi-Zoccai GGL, Houser JE, Qureshi IZ, Ownby ED, Gustini E, Biasucci LM, Severino A, Capogrossi MC, Vetrovec GW, Crea F, Baldi A, Kukreja RC, Dobrina A. Anakinra, a recombinant human interleukin-1 receptor antagonist, inhibits apoptosis in experimental acute myocardial infarction. Circulation. 2008;117:2670–2683. doi: 10.1161/CIRCULATIONAHA.107.740233. [DOI] [PubMed] [Google Scholar]
- 66.Zhu J, Zhang J, Xiang D, Zhang Z, Zhang L, Wu M, Zhu S, Zhang R, Han W. Recombinant human interleukin-1 receptor antagonist protects mice against acute doxorubicin-induced cardiotoxicity. Eur J Pharmacol. 2010;643:247–253. doi: 10.1016/j.ejphar.2010.06.024. [DOI] [PubMed] [Google Scholar]
- 67.Harouki N, Nicol L, Remy-Jouet I, Henry JP, Dumesnil A, Lejeune A, Renet S, Golding F, Djerada Z, Wecker D, Bolduc V, Bouly M, Roussel J, Richard V, Mulder P. The IL-1beta antibody gevokizumab limits cardiac remodeling and coronary dysfunction in rats with heart failure. JACC Basic Transl Sci. 2017;2:418–430. doi: 10.1016/j.jacbts.2017.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Honsho S, Nishikawa S, Amano K, Zen K, Adachi Y, Kishita E, Matsui A, Katsume A, Yamaguchi S, Nishikawa K, Isoda K, Riches DWH, Matoba S, Okigaki M, Matsubara H. Pressure-mediated hypertrophy and mechanical stretch induces IL-1 release and subsequent IGF-1 generation to maintain compensative hypertrophy by affecting Akt and JNK pathways. Circ Res. 2009;105:1149–1158. doi: 10.1161/CIRCRESAHA.109.208199. [DOI] [PubMed] [Google Scholar]
- 69.Kumar A, Thota V, Dee L, Olson J, Uretz E, Parrillo JE. Tumor necrosis factor alpha and interleukin 1beta are responsible for in vitro myocardial cell depression induced by human septic shock serum. J Exp Med. 1996;183:949–958. doi: 10.1084/jem.183.3.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gulick T, Chung MK, Pieper SJ, Lange LG, Schreiner GF. Interleukin 1 and tumor necrosis factor inhibit cardiac myocyte beta-adrenergic responsiveness. Proc Natl Acad Sci U S A. 1989;86:6753–6757. doi: 10.1073/pnas.86.17.6753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ing DJ, Zang J, Dzau VJ, Webster KA, Bishopric NH. Modulation of cytokine-induced cardiac myocyte apoptosis by nitric oxide, Bak, and Bcl-x. Circ Res. 1999;84:21–33. doi: 10.1161/01.res.84.1.21. [DOI] [PubMed] [Google Scholar]
- 72.Sager HB, Heidt T, Hulsmans M, Dutta P, Courties G, Sebas M, Wojtkiewicz GR, Tricot B, Iwamoto Y, Sun Y, Weissleder R, Libby P, Swirski FK, Nahrendorf M. Targeting interleukin-1beta reduces leukocyte production after acute myocardial infarction. Circulation. 2015;132:1880–1890. doi: 10.1161/CIRCULATIONAHA.115.016160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Saxena A, Chen W, Su Y, Rai V, Uche OU, Li N, Frangogiannis NG. IL-1 induces proinflammatory leukocyte infiltration and regulates fibroblast phenotype in the infarcted myocardium. J Immunol. 2013;191:4838–4848. doi: 10.4049/jimmunol.1300725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Leszczynski D, Josephs MD, Foegh ML. IL-1 beta-stimulated leucocyte-endothelial adhesion is regulated, in part, by the cyclic-GMP-dependent signal transduction pathway. Scand J Immunol. 1994;39:551–556. doi: 10.1111/j.1365-3083.1994.tb03412.x. [DOI] [PubMed] [Google Scholar]
- 75.Bageghni SA, Hemmings KE, Yuldasheva NY, Maqbool A, Gamboa-Esteves FO, Humphreys NE, et al. Fibroblast-specific deletion of interleukin-1 receptor-1 reduces adverse cardiac remodeling following myocardial infarction. JCI Insight. 2019;5. 10.1172/jci.insight.125074. [DOI] [PMC free article] [PubMed]
- 76.Ikonomidis I, Tzortzis S, Lekakis J, Paraskevaidis I, Andreadou I, Nikolaou M, Kaplanoglou T, Katsimbri P, Skarantavos G, Soucacos P, Kremastinos DT. Lowering interleukin-1 activity with anakinra improves myocardial deformation in rheumatoid arthritis. Heart. 2009;95:1502–1507. doi: 10.1136/hrt.2009.168971. [DOI] [PubMed] [Google Scholar]
- 77.Eriksson U, Kurrer MO, Sonderegger I, Iezzi G, Tafuri A, Hunziker L, Suzuki S, Bachmaier K, Bingisser RM, Penninger JM, Kopf M. Activation of dendritic cells through the interleukin 1 receptor 1 is critical for the induction of autoimmune myocarditis. J Exp Med. 2003;197:323–331. doi: 10.1084/jem.20021788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, Kastelein JJP, Cornel JH, Pais P, Pella D, Genest J, Cifkova R, Lorenzatti A, Forster T, Kobalava Z, Vida-Simiti L, Flather M, Shimokawa H, Ogawa H, Dellborg M, Rossi PRF, Troquay RPT, Libby P, Glynn RJ. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377:1119–1131. doi: 10.1056/NEJMoa1707914. [DOI] [PubMed] [Google Scholar]
- 79.Everett BM, Cornel JH, Lainscak M, Anker SD, Abbate A, Thuren T, Libby P, Glynn RJ, Ridker PM. Anti-inflammatory therapy with canakinumab for the prevention of hospitalization for heart failure. Circulation. 2019;139:1289–1299. doi: 10.1161/CIRCULATIONAHA.118.038010. [DOI] [PubMed] [Google Scholar]
- 80.Buckley LF, Carbone S, Trankle CR, Canada JM, Erdle CO, Regan JA, Viscusi MM, Kadariya D, Billingsley H, Arena R, Abbate A, van Tassell BW. Effect of Interleukin-1 blockade on left ventricular systolic performance and work: a post hoc pooled analysis of 2 clinical trials. J Cardiovasc Pharmacol. 2018;72:68–70. doi: 10.1097/FJC.0000000000000591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Van Tassell BW, Trankle CR, Canada JM, et al. IL-1 blockade in patients with heart failure with preserved ejection fraction. Circ Heart Fail. 2018;11:e005036. doi: 10.1161/CIRCHEARTFAILURE.118.005036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ikonomidis I, Lekakis JP, Nikolaou M, Paraskevaidis I, Andreadou I, Kaplanoglou T, Katsimbri P, Skarantavos G, Soucacos PN, Kremastinos DT. Inhibition of interleukin-1 by anakinra improves vascular and left ventricular function in patients with rheumatoid arthritis. Circulation. 2008;117:2662–2669. doi: 10.1161/CIRCULATIONAHA.107.731877. [DOI] [PubMed] [Google Scholar]
- 83.Rose-John S. Interleukin-6 family cytokines. Cold Spring Harb Perspect Biol. 2018;10. 10.1101/cshperspect.a028415. [DOI] [PMC free article] [PubMed]
- 84.Yue P, Massie BM, Simpson PC, Long CS. Cytokine expression increases in nonmyocytes from rats with postinfarction heart failure. Am J Phys. 1998;275:H250–H258. doi: 10.1152/ajpheart.1998.275.1.H250. [DOI] [PubMed] [Google Scholar]
- 85.Gwechenberger M, Mendoza LH, Youker KA, Frangogiannis NG, Smith CW, Michael LH, Entman ML. Cardiac myocytes produce interleukin-6 in culture and in viable border zone of reperfused infarctions. Circulation. 1999;99:546–551. doi: 10.1161/01.cir.99.4.546. [DOI] [PubMed] [Google Scholar]
- 86.Baumgarten G, Knuefermann P, Kalra D, Gao F, Taffet GE, Michael L, Blackshear PJ, Carballo E, Sivasubramanian N, Mann DL. Load-dependent and -independent regulation of proinflammatory cytokine and cytokine receptor gene expression in the adult mammalian heart. Circulation. 2002;105:2192–2197. doi: 10.1161/01.cir.0000015608.37608.18. [DOI] [PubMed] [Google Scholar]
- 87.Omiya S, Omori Y, Taneike M, Murakawa T, Ito J, Tanada Y, Nishida K, Yamaguchi O, Satoh T, Shah AM, Akira S, Otsu K. Cytokine mRNA degradation in cardiomyocytes restrains sterile inflammation in pressure-overloaded hearts. Circulation. 2020;141:667–677. doi: 10.1161/CIRCULATIONAHA.119.044582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kubota T, Miyagishima M, Alvarez RJ, et al. Expression of proinflammatory cytokines in the failing human heart: comparison of recent-onset and end-stage congestive heart failure. J Heart Lung Transplant. 2000;19:819–824. doi: 10.1016/s1053-2498(00)00173-x. [DOI] [PubMed] [Google Scholar]
- 89.Eiken HG, Oie E, Damas JK, Yndestad A, Bjerkeli V, Aass H, Simonsen S, Geiran OR, Tonnessen T, Christensen G, Froland SS, Gullestad L, Attramadal H, Aukrust P. Myocardial gene expression of leukaemia inhibitory factor, interleukin-6 and glycoprotein 130 in end-stage human heart failure. Eur J Clin Investig. 2001;31:389–397. doi: 10.1046/j.1365-2362.2001.00795.x. [DOI] [PubMed] [Google Scholar]
- 90.Plenz G, Eschert H, Erren M, Wichter T, Böhm M, Flesch M, Scheld HH, Deng MC. The interleukin-6/interleukin-6-receptor system is activated in donor hearts. J Am Coll Cardiol. 2002;39:1508–1512. doi: 10.1016/s0735-1097(02)01791-6. [DOI] [PubMed] [Google Scholar]
- 91.Hilfiker-Kleiner D, Shukla P, Klein G, Schaefer A, Stapel B, Hoch M, Müller W, Scherr M, Theilmeier G, Ernst M, Hilfiker A, Drexler H. Continuous glycoprotein-130-mediated signal transducer and activator of transcription-3 activation promotes inflammation, left ventricular rupture, and adverse outcome in subacute myocardial infarction. Circulation. 2010;122:145–155. doi: 10.1161/CIRCULATIONAHA.109.933127. [DOI] [PubMed] [Google Scholar]
- 92.Zhao L, Cheng G, Jin R, Afzal MR, Samanta A, Xuan YT, Girgis M, Elias HK, Zhu Y, Davani A, Yang Y, Chen X, Ye S, Wang OL, Chen L, Hauptman J, Vincent RJ, Dawn B. Deletion of interleukin-6 attenuates pressure overload-induced left ventricular hypertrophy and dysfunction. Circ Res. 2016;118:1918–1929. doi: 10.1161/CIRCRESAHA.116.308688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lai NC, Gao MH, Tang E, Tang R, Guo T, Dalton ND, Deng A, Tang T. Pressure overload-induced cardiac remodeling and dysfunction in the absence of interleukin 6 in mice. Lab Investig. 2012;92:1518–1526. doi: 10.1038/labinvest.2012.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kobara M, Noda K, Kitamura M, Okamoto A, Shiraishi T, Toba H, Matsubara H, Nakata T. Antibody against interleukin-6 receptor attenuates left ventricular remodelling after myocardial infarction in mice. Cardiovasc Res. 2010;87:424–430. doi: 10.1093/cvr/cvq078. [DOI] [PubMed] [Google Scholar]
- 95.Mackiewicz A, Schooltink H, Heinrich PC, Rose-John S. Complex of soluble human IL-6-receptor/IL-6 up-regulates expression of acute-phase proteins. J Immunol. 1992;149:2021–2027. [PubMed] [Google Scholar]
- 96.Kinugawa K, Takahashi T, Kohmoto O, Yao A, Aoyagi T, Momomura S, Hirata Y, Serizawa T. Nitric oxide-mediated effects of interleukin-6 on [Ca2+]i and cell contraction in cultured chick ventricular myocytes. Circ Res. 1994;75:285–295. doi: 10.1161/01.res.75.2.285. [DOI] [PubMed] [Google Scholar]
- 97.Melendez GC, McLarty JL, Levick SP, et al. Interleukin 6 mediates myocardial fibrosis, concentric hypertrophy, and diastolic dysfunction in rats. Hypertension. 2010;56:225–231. doi: 10.1161/HYPERTENSIONAHA.109.148635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sano M, Fukuda K, Kodama H, Pan J, Saito M, Matsuzaki J, Takahashi T, Makino S, Kato T, Ogawa S. Interleukin-6 family of cytokines mediate angiotensin II-induced cardiac hypertrophy in rodent cardiomyocytes. J Biol Chem. 2000;275:29717–29723. doi: 10.1074/jbc.M003128200. [DOI] [PubMed] [Google Scholar]
- 99.Kunisada K, Tone E, Fujio Y, Matsui H, Yamauchi-Takihara K, Kishimoto T. Activation of gp130 transduces hypertrophic signals via STAT3 in cardiac myocytes. Circulation. 1998;98:346–352. doi: 10.1161/01.cir.98.4.346. [DOI] [PubMed] [Google Scholar]
- 100.Smart N, Mojet MH, Latchman DS, et al. IL-6 induces PI 3-kinase and nitric oxide-dependent protection and preserves mitochondrial function in cardiomyocytes. Cardiovasc Res. 2006;69:164–177. doi: 10.1016/j.cardiores.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 101.Chou CH, Hung CS, Liao CW, Wei LH, Chen CW, Shun CT, Wen WF, Wan CH, Wu XM, Chang YY, Wu VC, Wu KD, Lin YH, The TAIPAI Study Group IL-6 trans-signalling contributes to aldosterone-induced cardiac fibrosis. Cardiovasc Res. 2018;114:690–702. doi: 10.1093/cvr/cvy013. [DOI] [PubMed] [Google Scholar]
- 102.Leicht M, Briest W, Zimmer HG. Regulation of norepinephrine-induced proliferation in cardiac fibroblasts by interleukin-6 and p42/p44 mitogen activated protein kinase. Mol Cell Biochem. 2003;243:65–72. doi: 10.1023/a:1021655023870. [DOI] [PubMed] [Google Scholar]
- 103.Mir SA, Chatterjee A, Mitra A, Pathak K, Mahata SK, Sarkar S. Inhibition of signal transducer and activator of transcription 3 (STAT3) attenuates interleukin-6 (IL-6)-induced collagen synthesis and resultant hypertrophy in rat heart. J Biol Chem. 2012;287:2666–2677. doi: 10.1074/jbc.M111.246173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Mitani H, Katayama N, Araki H, Ohishi K, Kobayashi K, Suzuki H, Nishii K, Masuya M, Yasukawa K, Minami N, Shiku H. Activity of interleukin 6 in the differentiation of monocytes to macrophages and dendritic cells. Br J Haematol. 2000;109:288–295. doi: 10.1046/j.1365-2141.2000.02020.x. [DOI] [PubMed] [Google Scholar]
- 105.Mauer J, Chaurasia B, Goldau J, Vogt MC, Ruud J, Nguyen KD, Theurich S, Hausen AC, Schmitz J, Brönneke HS, Estevez E, Allen TL, Mesaros A, Partridge L, Febbraio MA, Chawla A, Wunderlich FT, Brüning JC. Signaling by IL-6 promotes alternative activation of macrophages to limit endotoxemia and obesity-associated resistance to insulin. Nat Immunol. 2014;15:423–430. doi: 10.1038/ni.2865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sackett SD, Otto T, Mohs A, Sander LE, Strauch S, Streetz KL, Kroy DC, Trautwein C. Myeloid cells require gp130 signaling for protective anti-inflammatory functions during sepsis. FASEB J. 2019;33:6035–6044. doi: 10.1096/fj.201802118R. [DOI] [PubMed] [Google Scholar]
- 107.Scheller J, Chalaris A, Schmidt-Arras D, Rose-John S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim Biophys Acta. 1813;2011:878–888. doi: 10.1016/j.bbamcr.2011.01.034. [DOI] [PubMed] [Google Scholar]
- 108.Kraakman MJ, Kammoun HL, Allen TL, Deswaerte V, Henstridge DC, Estevez E, Matthews VB, Neill B, White DA, Murphy AJ, Peijs L, Yang C, Risis S, Bruce CR, du XJ, Bobik A, Lee-Young RS, Kingwell BA, Vasanthakumar A, Shi W, Kallies A, Lancaster GI, Rose-John S, Febbraio MA. Blocking IL-6 trans-signaling prevents high-fat diet-induced adipose tissue macrophage recruitment but does not improve insulin resistance. Cell Metab. 2015;21:403–416. doi: 10.1016/j.cmet.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 109.Yokoe I, Kobayashi H, Kobayashi Y, Giles JT, Yoneyama K, Kitamura N, Takei M. Impact of tocilizumab on N-terminal pro-brain natriuretic peptide levels in patients with active rheumatoid arthritis without cardiac symptoms. Scand J Rheumatol. 2018;47:364–370. doi: 10.1080/03009742.2017.1418424. [DOI] [PubMed] [Google Scholar]
- 110.Kleveland O, Kunszt G, Bratlie M, Ueland T, Broch K, Holte E, Michelsen AE, Bendz B, Amundsen BH, Espevik T, Aakhus S, Damås JK, Aukrust P, Wiseth R, Gullestad L. Effect of a single dose of the interleukin-6 receptor antagonist tocilizumab on inflammation and troponin T release in patients with non-ST-elevation myocardial infarction: a double-blind, randomized, placebo-controlled phase 2 trial. Eur Heart J. 2016;37:2406–2413. doi: 10.1093/eurheartj/ehw171. [DOI] [PubMed] [Google Scholar]
- 111.Kleveland O, Ueland T, Kunszt G, Bratlie M, Yndestad A, Broch K, Holte E, Ryan L, Amundsen BH, Bendz B, Aakhus S, Espevik T, Halvorsen B, Mollnes TE, Wiseth R, Gullestad L, Aukrust P, Damås JK. Interleukin-6 receptor inhibition with tocilizumab induces a selective and substantial increase in plasma IP-10 and MIP-1beta in non-ST-elevation myocardial infarction. Int J Cardiol. 2018;271:1–7. doi: 10.1016/j.ijcard.2018.04.136. [DOI] [PubMed] [Google Scholar]
- 112.Sokol CL, Luster AD. The chemokine system in innate immunity. Cold Spring Harb Perspect Biol. 2015;7. 10.1101/cshperspect.a016303. [DOI] [PMC free article] [PubMed]
- 113.Clark-Lewis I, Kim KS, Rajarathnam K, Gong JH, Dewald B, Moser B, Baggiolini M, Sykes BD. Structure–activity relationships of chemokines. J Leukoc Biol. 1995;57:703–711. doi: 10.1002/jlb.57.5.703. [DOI] [PubMed] [Google Scholar]
- 114.Zlotnik A, Morales J, Hedrick JA. Recent advances in chemokines and chemokine receptors. Crit Rev Immunol. 1999;19:1–47. [PubMed] [Google Scholar]
- 115.Chen B, Frangogiannis NG. Chemokines in myocardial infarction. J Cardiovasc Transl Res. 2020. 10.1007/s12265-020-10006-7. [DOI] [PubMed]
- 116.Xia Y, Frangogiannis NG. MCP-1/CCL2 as a therapeutic target in myocardial infarction and ischemic cardiomyopathy. Inflamm Allergy Drug Targets. 2007;6:101–107. doi: 10.2174/187152807780832265. [DOI] [PubMed] [Google Scholar]
- 117.Kumar AG, Ballantyne CM, Michael LH, Kukielka GL, Youker KA, Lindsey ML, Hawkins HK, Birdsall HH, MacKay CR, LaRosa GJ, Rossen RD, Smith CW, Entman ML. Induction of monocyte chemoattractant protein-1 in the small veins of the ischemic and reperfused canine myocardium. Circulation. 1997;95:693–700. doi: 10.1161/01.cir.95.3.693. [DOI] [PubMed] [Google Scholar]
- 118.Dewald O, Frangogiannis NG, Zoerlein M, Duerr GD, Klemm C, Knuefermann P, Taffet G, Michael LH, Crapo JD, Welz A, Entman ML. Development of murine ischemic cardiomyopathy is associated with a transient inflammatory reaction and depends on reactive oxygen species. Proc Natl Acad Sci U S A. 2003;100:2700–2705. doi: 10.1073/pnas.0438035100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Behr TM, Wang X, Aiyar N, Coatney RW, Li X, Koster P, Angermann CE, Ohlstein E, Feuerstein GZ, Winaver J. Monocyte chemoattractant protein-1 is upregulated in rats with volume-overload congestive heart failure. Circulation. 2000;102:1315–1322. doi: 10.1161/01.cir.102.11.1315. [DOI] [PubMed] [Google Scholar]
- 120.Kuwahara F, Kai H, Tokuda K, Takeya M, Takeshita A, Egashira K, Imaizumi T. Hypertensive myocardial fibrosis and diastolic dysfunction: another model of inflammation? Hypertension. 2004;43:739–745. doi: 10.1161/01.HYP.0000118584.33350.7d. [DOI] [PubMed] [Google Scholar]
- 121.Lehmann MH, Kuhnert H, Muller S, Sigusch HH. Monocyte chemoattractant protein 1 (MCP-1) gene expression in dilated cardiomyopathy. Cytokine. 1998;10:739–746. doi: 10.1006/cyto.1998.0354. [DOI] [PubMed] [Google Scholar]
- 122.Iwasaki J, Nakamura K, Matsubara H, Nakamura Y, Nishii N, Banba K, Murakami M, Ohta-Ogo K, Kimura H, Toh N, Nagase S, Oka T, Morita H, Kusano KF, Ohe T. Relationship between circulating levels of monocyte chemoattractant protein-1 and systolic dysfunction in patients with hypertrophic cardiomyopathy. Cardiovasc Pathol. 2009;18:317–322. doi: 10.1016/j.carpath.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 123.Patel B, Bansal SS, Ismahil MA, Hamid T, Rokosh G, Mack M, Prabhu SD. CCR2(+) monocyte-derived infiltrating macrophages are required for adverse cardiac remodeling during pressure overload. JACC Basic Transl Sci. 2018;3:230–244. doi: 10.1016/j.jacbts.2017.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hayashidani S, Tsutsui H, Shiomi T, Ikeuchi M, Matsusaka H, Suematsu N, Wen J, Egashira K, Takeshita A. Anti-monocyte chemoattractant protein-1 gene therapy attenuates left ventricular remodeling and failure after experimental myocardial infarction. Circulation. 2003;108:2134–2140. doi: 10.1161/01.CIR.0000092890.29552.22. [DOI] [PubMed] [Google Scholar]
- 125.Bajpai G, Bredemeyer A, Li W, Zaitsev K, Koenig AL, Lokshina I, Mohan J, Ivey B, Hsiao HM, Weinheimer C, Kovacs A, Epelman S, Artyomov M, Kreisel D, Lavine KJ. Tissue resident CCR2− and CCR2+ cardiac macrophages differentially orchestrate monocyte recruitment and fate specification following myocardial injury. Circ Res. 2019;124:263–278. doi: 10.1161/CIRCRESAHA.118.314028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Haudek SB, Cheng J, Du J, et al. Monocytic fibroblast precursors mediate fibrosis in angiotensin-II-induced cardiac hypertrophy. J Mol Cell Cardiol. 2010;49:499–507. doi: 10.1016/j.yjmcc.2010.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Trial J, Heredia CP, Taffet GE, Entman ML, Cieslik KA. Dissecting the role of myeloid and mesenchymal fibroblasts in age-dependent cardiac fibrosis. Basic Res Cardiol. 2017;112:34. doi: 10.1007/s00395-017-0623-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Tan X, Hu L, Shu Z, Chen L, Li X, du M, Sun D, Mao X, Deng S, Huang K, Zhang F. Role of CCR2 in the development of streptozotocin-treated diabetic cardiomyopathy. Diabetes. 2019;68:2063–2073. doi: 10.2337/db18-1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kolattukudy PE, Quach T, Bergese S, Breckenridge S, Hensley J, Altschuld R, Gordillo G, Klenotic S, Orosz C, Parker-Thornburg J. Myocarditis induced by targeted expression of the MCP-1 gene in murine cardiac muscle. Am J Pathol. 1998;152:101–111. [PMC free article] [PubMed] [Google Scholar]
- 130.Stumpf C, Lehner C, Raaz D, Yilmaz A, Anger T, Daniel WG, Garlichs CD. Platelets contribute to enhanced MCP-1 levels in patients with chronic heart failure. Heart. 2008;94:65–69. doi: 10.1136/hrt.2007.115006. [DOI] [PubMed] [Google Scholar]
- 131.Hohensinner PJ, Rychli K, Zorn G, Hülsmann M, Berger R, Mörtl D, Richter B, Huber K, Wojta J, Pacher R, Niessner A. Macrophage-modulating cytokines predict adverse outcome in heart failure. Thromb Haemost. 2010;103:435–441. doi: 10.1160/TH09-06-0399. [DOI] [PubMed] [Google Scholar]
- 132.Grisanti LA, Traynham CJ, Repas AA, Gao E, Koch WJ, Tilley DG. beta2-adrenergic receptor-dependent chemokine receptor 2 expression regulates leukocyte recruitment to the heart following acute injury. Proc Natl Acad Sci U S A. 2016;113:15126–15131. doi: 10.1073/pnas.1611023114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wang J, Seo MJ, Deci MB, Weil BR, Canty JM, Nguyen J. Effect of CCR2 inhibitor-loaded lipid micelles on inflammatory cell migration and cardiac function after myocardial infarction. Int J Nanomedicine. 2018;13:6441–6451. doi: 10.2147/IJN.S178650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Leuschner F, Dutta P, Gorbatov R, Novobrantseva TI, Donahoe JS, Courties G, Lee KM, Kim JI, Markmann JF, Marinelli B, Panizzi P, Lee WW, Iwamoto Y, Milstein S, Epstein-Barash H, Cantley W, Wong J, Cortez-Retamozo V, Newton A, Love K, Libby P, Pittet MJ, Swirski FK, Koteliansky V, Langer R, Weissleder R, Anderson DG, Nahrendorf M. Therapeutic siRNA silencing in inflammatory monocytes in mice. Nat Biotechnol. 2011;29:1005–1010. doi: 10.1038/nbt.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Lu W, Xie Z, Tang Y, Bai L, Yao Y, Fu C, Ma G. Photoluminescent mesoporous silicon nanoparticles with siCCR2 improve the effects of mesenchymal stromal cell transplantation after acute myocardial infarction. Theranostics. 2015;5:1068–1082. doi: 10.7150/thno.11517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Sakai N, Wada T, Furuichi K, Shimizu K, Kokubo S, Hara A, Yamahana J, Okumura T, Matsushima K, Yokoyama H, Kaneko S. MCP-1/CCR2-dependent loop for fibrogenesis in human peripheral CD14-positive monocytes. J Leukoc Biol. 2006;79:555–563. doi: 10.1189/jlb.0305127. [DOI] [PubMed] [Google Scholar]
- 137.Kruglov EA, Nathanson RA, Nguyen T, Dranoff JA. Secretion of MCP-1/CCL2 by bile duct epithelia induces myofibroblastic transdifferentiation of portal fibroblasts. Am J Physiol Gastrointest Liver Physiol. 2006;290:G765–G771. doi: 10.1152/ajpgi.00308.2005. [DOI] [PubMed] [Google Scholar]
- 138.Yamamoto T, Eckes B, Mauch C, Hartmann K, Krieg T. Monocyte chemoattractant protein-1 enhances gene expression and synthesis of matrix metalloproteinase-1 in human fibroblasts by an autocrine IL-1 alpha loop. J Immunol. 2000;164:6174–6179. doi: 10.4049/jimmunol.164.12.6174. [DOI] [PubMed] [Google Scholar]
- 139.Gharaee-Kermani M, Denholm EM, Phan SH. Costimulation of fibroblast collagen and transforming growth factor beta1 gene expression by monocyte chemoattractant protein-1 via specific receptors. J Biol Chem. 1996;271:17779–17784. doi: 10.1074/jbc.271.30.17779. [DOI] [PubMed] [Google Scholar]
- 140.Haudek SB, Xia Y, Huebener P, Lee JM, Carlson S, Crawford JR, Pilling D, Gomer RH, Trial J, Frangogiannis NG, Entman ML. Bone marrow-derived fibroblast precursors mediate ischemic cardiomyopathy in mice. Proc Natl Acad Sci U S A. 2006;103:18284–18289. doi: 10.1073/pnas.0608799103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Moore-Morris T, Cattaneo P, Guimaraes-Camboa N, et al. Infarct fibroblasts do not derive from bone marrow lineages. Circ Res. 2018;122:583–590. doi: 10.1161/CIRCRESAHA.117.311490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Moore-Morris T, Guimaraes-Camboa N, Banerjee I, et al. Resident fibroblast lineages mediate pressure overload-induced cardiac fibrosis. J Clin Invest. 2014;124:2921–2934. doi: 10.1172/JCI74783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kanisicak O, Khalil H, Ivey MJ, Karch J, Maliken BD, Correll RN, Brody MJ, J. Lin SC, Aronow BJ, Tallquist MD, Molkentin JD. Genetic lineage tracing defines myofibroblast origin and function in the injured heart. Nat Commun. 2016;7:12260. doi: 10.1038/ncomms12260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Alex L, Frangogiannis NG. The cellular origin of activated fibroblasts in the infarcted and remodeling myocardium. Circ Res. 2018;122:540–542. doi: 10.1161/CIRCRESAHA.118.312654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Zhou L, Azfer A, Niu J, Graham S, Choudhury M, Adamski FM, Younce C, Binkley PF, Kolattukudy PE. Monocyte chemoattractant protein-1 induces a novel transcription factor that causes cardiac myocyte apoptosis and ventricular dysfunction. Circ Res. 2006;98:1177–1185. doi: 10.1161/01.RES.0000220106.64661.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Zhang W, Zhu T, Chen L, Luo W, Chao J. MCP-1 mediates ischemia–reperfusion-induced cardiomyocyte apoptosis via MCPIP1 and CaSR. Am J Physiol Heart Circ Physiol. 2020;318:H59–H71. doi: 10.1152/ajpheart.00308.2019. [DOI] [PubMed] [Google Scholar]
- 147.Mao R, Yang R, Chen X, Harhaj EW, Wang X, Fan Y. Regnase-1, a rapid response ribonuclease regulating inflammation and stress responses. Cell Mol Immunol. 2017;14:412–422. doi: 10.1038/cmi.2016.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Morimoto H, Hirose M, Takahashi M, Kawaguchi M, Ise H, Kolattukudy PE, Yamada M, Ikeda U. MCP-1 induces cardioprotection against ischaemia/reperfusion injury: role of reactive oxygen species. Cardiovasc Res. 2008;78:554–562. doi: 10.1093/cvr/cvn035. [DOI] [PubMed] [Google Scholar]
- 149.Vergunst CE, Gerlag DM, Lopatinskaya L, Klareskog L, Smith MD, van den Bosch F, Dinant HJ, Lee Y, Wyant T, Jacobson EW, Baeten D, Tak PP. Modulation of CCR2 in rheumatoid arthritis: a double-blind, randomized, placebo-controlled clinical trial. Arthritis Rheum. 2008;58:1931–1939. doi: 10.1002/art.23591. [DOI] [PubMed] [Google Scholar]
- 150.Ratziu V, Sanyal A, Harrison SA, Wong VWS, Francque S, Goodman Z, et al. Cenicriviroc treatment for adults with nonalcoholic steatohepatitis and fibrosis: final analysis of the phase 2b CENTAUR study. Hepatology. 2020. 10.1002/hep.31108. [DOI] [PubMed]
- 151.Scholz D, Ito W, Fleming I, Deindl E, Sauer A, Wiesnet M, Busse R, Schaper J, Schaper W. Ultrastructure and molecular histology of rabbit hind-limb collateral artery growth (arteriogenesis) Virchows Arch. 2000;436:257–270. doi: 10.1007/s004280050039. [DOI] [PubMed] [Google Scholar]
- 152.Dobaczewski M, Xia Y, Bujak M, Gonzalez-Quesada C, Frangogiannis NG. CCR5 signaling suppresses inflammation and reduces adverse remodeling of the infarcted heart, mediating recruitment of regulatory T cells. Am J Pathol. 2010;176:2177–2187. doi: 10.2353/ajpath.2010.090759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Frangogiannis NG. The inflammatory response in myocardial injury, repair, and remodelling. Nat Rev Cardiol. 2014;11:255–265. doi: 10.1038/nrcardio.2014.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Christia P, Frangogiannis NG. Targeting inflammatory pathways in myocardial infarction. Eur J Clin Investig. 2013;43:986–995. doi: 10.1111/eci.12118. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
N/A