Abstract
Background
Traumatic brain injury (TBI) is characterized by high prevalence, morbidity, and mortality. Diffuse axonal injury (DAI) is a specific type of TBI leading to prolonged consciousness impairment and disability. There is still no standard treatment for DAI, so we introduced traditional Chinese medicine into the treatment of these patients.
Case summaries
Three patients had TBI after traffic accidents. Their Glasgow Coma Scale (GCS) scores in the intensive care unit (ICU) were E1VEM2-3, E1VEM2-3, and E1VEM2 respectively. All of them were diagnosed with DAI based on magnetic resonance imaging (MRI). Because of continuing consciousness disturbances, their families agreed to combine traditional Chinese medicine and modern medicine treatments through inpatient consultation in Taoyuan General hospital. Two patients took Buyang Huanwu Decoction, and one Tianma Gouteng Decoction twice a day. All of them received 20 min of acupuncture treatments 5 times per week. Acupuncture points included Baihui (GV20), Sishencong (EX-HN1), Shuigou (GV26), Hegu (LI4), and Taichong (LR3). All of them started Traditional Chinese medicine treatment within 2 weeks after TBI. The GCS of all three patients recovered to E4M5V6.
Conclusions
The early addition of traditional Chinese medicine treatments to Western medical care can improve the prognosis of patients with diffuse axonal injury.
Keywords: Diffuse axonal injury, Traumatic brain injury, Traditional Chinese medicine
Abbreviations: TBI, Traumatic brain injury; DAI, Diffuse axonal injury; GCS, Glasgow Coma Scale; ICU, intensive care unit; MRI, magnetic resonance imaging; BHD, Buyang Huanwu Decoction; TGD, Tianma Gouteng Decoction
Graphical abstract
Highlights
-
•
Traumatic brain injury diagnosed with diffuse axonal injury, the lower GCS, the poorer outcome. This article points out that combining Chinese medicine and modern medicine can lead to better outcome(motor, speech function and GCS score).
-
•
Chinese medicine has neuroprotective effect and it’s safe when combining with modern medicine in severe traumatic brain injury in this cases report.
1. Introduction
Traumatic brain injury (TBI) results in mortality and disability around the world. In 2013, there were approximately 2.5 million emergency department visits, 282,000 hospitalizations, and 56,000 deaths related to TBI in the United States.1 The incidence of TBI varies greatly across countries and regions, and its incidence in countries such as Sweden, Italy, France, and Norway appears to have decreased over time, while it might have increased in Spain and Taiwan.2 TBI prevalence in Taiwan is 52,000 cases per year, up to 25% of which are fatal.3
Diffuse axonal injury (DAI) is defined as a prolonged consciousness disturbance, more than 6 h after head injury, without demonstrable swelling or ischemic brain lesions.4,5 Up to 75% of the patients with moderate to severe head injury who survive the acute phase are diagnosed with DAI.6
DAI comes from high energy shearing forces and it is the main cause of continued consciousness disturbances, mortality, and cognitive impairment after TBI.7, 8, 9 The magnetic resonance imaging (MRI) of DAI cases usually shows lesions in the junction of cerebral white and grey matter, the corpus callosum, and the brain stem.6, 7, 8, 9, 10
With the progress of medicine, many severe traumatic brain injury patients can now survive, but their consciousness and activity of daily living function are still damaged. After the acute stage, TBI has long term sequelae, such as impaired consciousness, anesthesia, speech impediments, severe disability, and post-traumatic seizures and epilepsy. DAI often results in cognitive, physical and behavioral impairment, and the patients have difficulties returning to work and to a good quality of life. Since a satisfactory standard treatment is not available, we tried traditional Chinese medicine as an alternative therapeutic approach. The purpose of this report is to show that the treatment of DAI patients with a combination of traditional Chinese medicine and modern medicine is safe and effective.
2. Chinese medicine treatments
2.1. Acupuncture points and protocol
Acupuncture was performed with Casoon stainless steel needles (0.30 × 25 mm, 0.35 × 40 mm). Acupuncture points included the Baihui (GV20 on the head, 5 B-cun superior to the anterior hairline, on the median line), Sishencong (EX-HN1, four points at the vertex, one cun from GV20 in a cross formation), Shuigou (GV26, on the face, at the midpoint of the philtrum midline), Hegu (LI4, on the dorsum of the hand, radial to the midpoint of the second metatarsal bone, bilaterally), Taichong (LR3, on the dorsum of the foot, between the first and second metatarsal bones, in the depression distal to the junction of the bases of the two bones, over the dorsalis pedis artery, bilaterally).11, 12 We used 2% Chlorhexidine Gluconate for local disinfection, and avoided applying acupuncture near traumatic wounds. Needles were left in place for 20 min without any manipulation or electro stimulation. We performed acupuncture five times per week.
2.2. Decoction selection method
According to previous studies, traditional Chinese medicine decoctions or compound recipes may be safe and effective for TBI.13 The Buyang Huanwu Decoction (BHD) is a well-known traditional Chinese medicine prescription, used clinically for stroke-induced disability. BHD is composed of Astragalus membranaceus Bunge, Angelica sinensis, Paeonia lactiflora, Ligusticum chuanxiong, Prunus persica, Carthamus tinctorius and Pheretima aspergillum.14 BHD is prescribed for patients with hemiplegia and paraplegia, and several experimental studies indicate that it can improve the recovery of behavioral scores.14, 15, 16
The Tianma Gouteng Decoction (TGD) is prescribed to patients with headaches, dizziness, hypertension, and insomnia.17 Tianma Gouteng Decoction contains Rhizoma Gastrodiae, Ramulus cum Uncis Uncariae, Concha Haliotidis, Fructus Gardeniae, Radix Scutellariae, Eucommia ulmoides Oliver, Radix Cyathulae officinalis, Ramulus Loranthi, Poria cum Radix Pini, Caulis Polygoni Multiflori, and Herba Leonuri.
We used different decoctions according to the patient’s clinical presentation.
2.3. Case report no. 1
2.3.1. Patient information, examination and diagnostic assessment
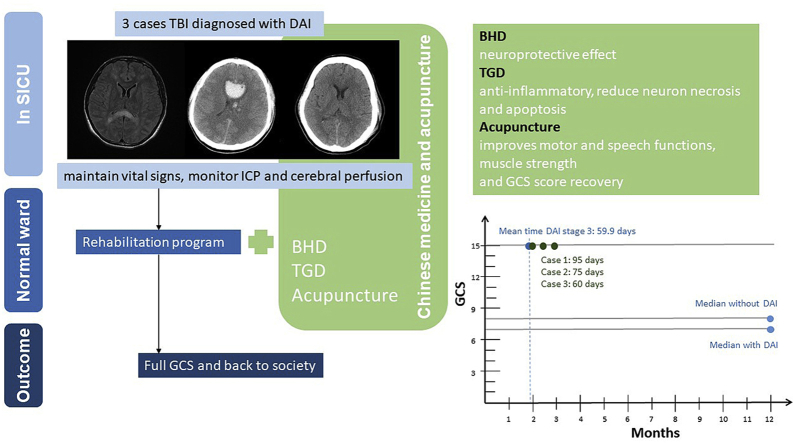
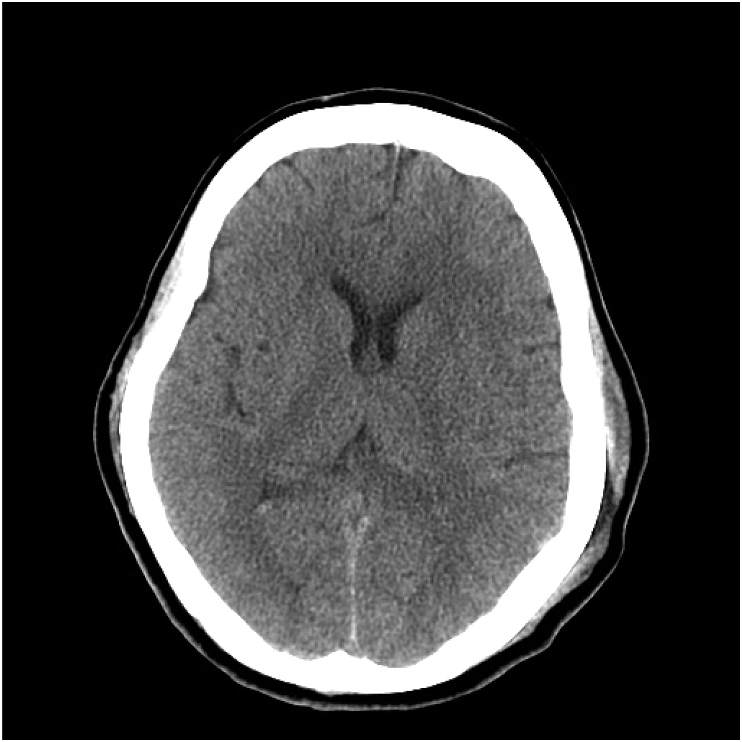
A 23-year-old man without any past medical history had a traffic accident and was sent to our emergency room on June 22, 2014. The GCS was E4V5M2 initially and worsened to E3M4V2. The patient had bilateral tibia and left femur fractures, and bruises over his trunk and limbs. Computed tomography (CT) showed a right subarachnoid hemorrhage. After surgery of the lower limb fractures, the patient was sent to the ICU for further treatment and care. Because of persisting consciousness disturbances (E1VEM2-3), the patient received an MRI examination which revealed stage 3 diffuse axonal injury (Fig. 1).
Fig. 1.
Image of case no.1. (A)CT of case no. 1, taken on June 22, 2014: minimal subarachnoid hemorrhage (SAH), right frontotemporal region. (B) MRI (T2 FLAIR) of case no. 1, taken on July 3, 2014: Diffuse axonal injury, grade III (involving the cerebral hemisphere, corpus callosum and brain stem), and subacute intracerebral hematoma in the right parietal lobe can be appreciated.
2.3.2. Intervention: acupuncture and decoction therapies
Traditional Chinese medicine (BHD) treatment started on July 3, 2014. The pulse condition of the patient was string-like and we could not obtain a tongue diagnosis due to endotracheal intubation. Acupuncture treatment started on July 4. The patient’s GCS was E2VEM2-3 at the start of traditional Chinese medicine therapy.
2.3.3. Outcome
The patient recovered to a full GCS score in Oct 2014: He could just pronounce sentences consisting of 3–4 words, and his voice was not clear. He continued receiving traditional Chinese medicine treatments together with rehabilitation treatments. The patient came to our Chinese Medicine outpatient department for follow up on July 3, 2015: His verbal speed and responses were somewhat slow, but his voice was clear and smooth. He felt lower extremities and low back tightness, and he sometimes chocked when drinking water. He could take care of himself without any assistance.
2.4. Case report no. 2
2.4.1. Patient information, examination and diagnostic assessment
A 20-year-old male without any past medical history had a traffic accident on Nov 11, 2014, and was sent to the emergency room. His GCS on arrival to the ER was E1V1M4. His pupil size was 2.5 mm (right) and 3.0 mm (left) with positive light reflex. When he stayed at our ER, his body temperature increased to 40 °C with tremors of the upper extremities. CT showed left thalamus hemorrhage, intraventricular hemorrhage, falx subdural hematoma, and subarachnoid hemorrhage. The patient was then transferred to the Surgical Intensive Care Unit (SICU) for further treatment.
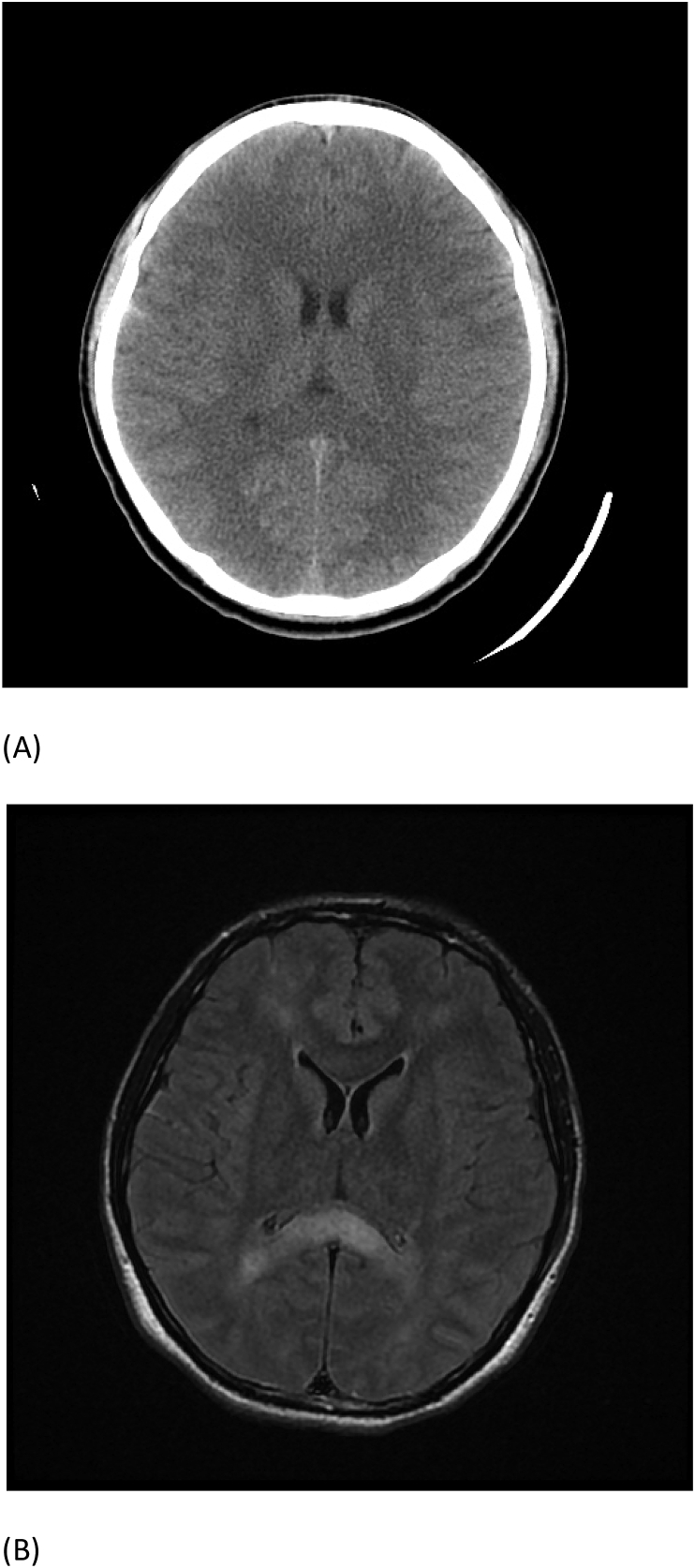
The patient’s consciousness became worse after admission (E1VEM2-3), so a new brain CT was performed on Nov 28 (Fig. 2), which showed a delayed hemorrhage of the corpus callosum and the bilateral frontal lobes. An intracranial pressure (ICP) monitor was inserted on the same day. After surgery, the patient’s ICP was kept below 20 mmHg and cerebral perfusion pressure (CPP) higher by mannitol and sedation.
Fig. 2.
CT of case no. 2, taken on Nov 28, 2014: Note the multiple intracranial hemorrhage (ICHs) in the left thalamus.
The patient consciousness was still poor. His GCS was around E1VEM2-3. The patient had intermittent fever up to 38 °C and persisting tremor of the extremities. The Chinese Medicine Department was consulted due to persisted poor conscious status (E1VEM2-3) on Dec 3, 2014.
2.4.2. Intervention: acupuncture and decoction therapies
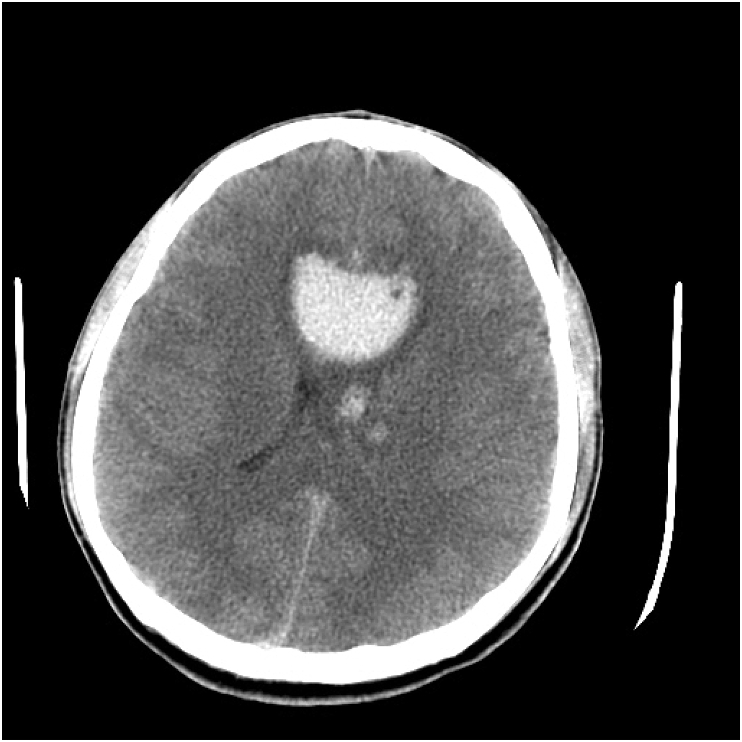
We noticed red acne on his face, and sweat around his head. The pulse condition of the patient was string-like and rapid. We could not obtain a tongue diagnosis due to endotracheal intubation. We started TGD treatment on Dec 3, and the fever subsided from Dec 5. An MRI exam was performed on Dec 8 (Fig. 3) and showed stage 3 diffuse axonal injury, explaining the persisting poor GCS level, which returned to E1-2VEM4. Acupuncture treatment started on Dec 16.
Fig. 3.
MRI (Flair2) of case no. 2, taken on Dec 18, 2014: Suspect diffuse axonal injury. Multiple ICHs, with the largest ones at the corpus callosum and bifrontal lobes, intraventricular hemorrhage (IVH), and SAH can be detected.
2.4.3. Outcome
The patient’s GCS recovered to E4VEM4 progressively. His facial acne was healed but a few scars were left. The tremor of the upper extremities stopped on Jan 2, 2015.
The endotracheal tube was removed on Jan 6, and he was transferred to the regular neurosurgery ward on Jan 13 and to the rehabilitation ward on Jan 26. We adjusted the administration of Chinese medicine decoction from TGD to BHD on Jan 26. He could say simple words on Feb 26. The patient continued the rehabilitation program alongside traditional Chinese medicine treatment and was discharged on July 10, 2015 with a GCS of E4V5M6. He could perform all his daily activities by himself and return to school without problems.
2.5. Case report no. 3
2.5.1. Patient information, examination and diagnostic assessment
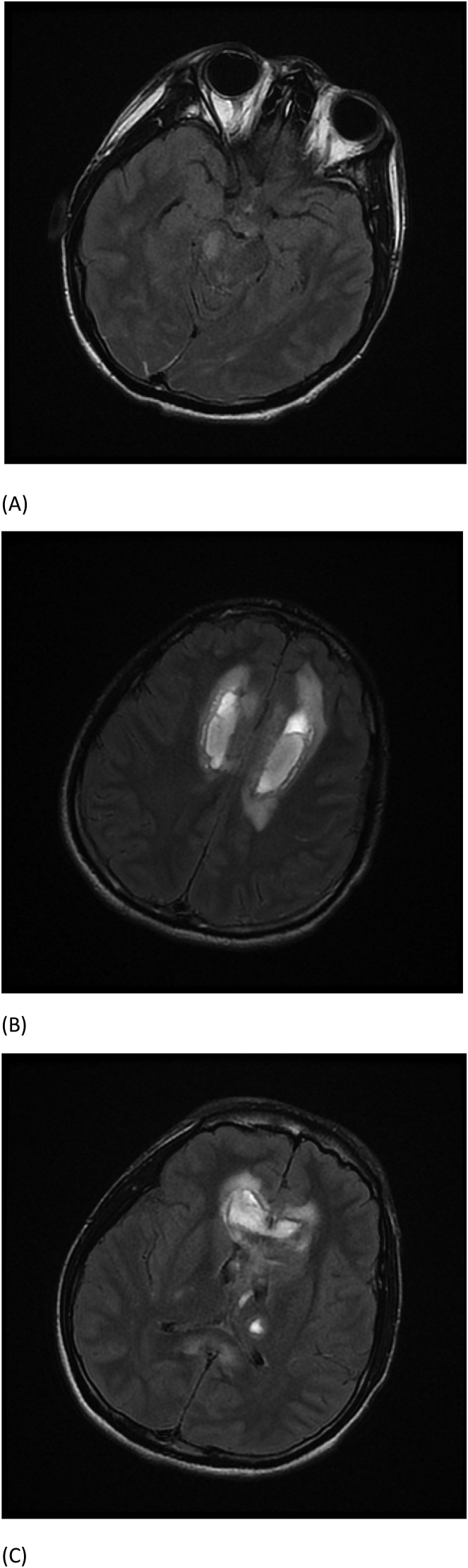
A 58 year-old woman with a history of hypertension under regular medication control was hit by a vehicle when riding a motorbike. She was sent to our ER on Nov 23, 2015 with multiple bruises. Her GCS was E1V2M1. Brain CT showed diffuse subarachnoid hemorrhage in the bilateral cerebral hemispheres and basal cisterns (Fig. 4). X-rays showed left pulmonary atelectasis and fractures of the left ribs. After endotracheal intubation, an ICP monitor was inserted in the operating room. The patient was then admitted to the SICU for further treatment guided by ICP and CPP levels.
Fig. 4.
CT of case no. 3, taken on Nov 23, 2015: Diffuse bilateral SAH and right contusional hemorrhage can be appreciated.
2.5.2. Intervention: acupuncture and decoction therapies
The patient’s poor consciousness (GCS: E1VEM1) persisted, and traditional Chinese medicine was started. Pulse condition of the patient was string-like and we could not obtain a tongue diagnosis due to endotracheal intubation. BHD use started on Nov 26, and acupuncture treatment started on Dec 1. MRI on Dec 7 showed acute infarction of the right thalamus, left parietal lobe, and corpus callosum, and stage 3 diffuse axonal injury was diagnosed (see Fig. 5).
Fig. 5.
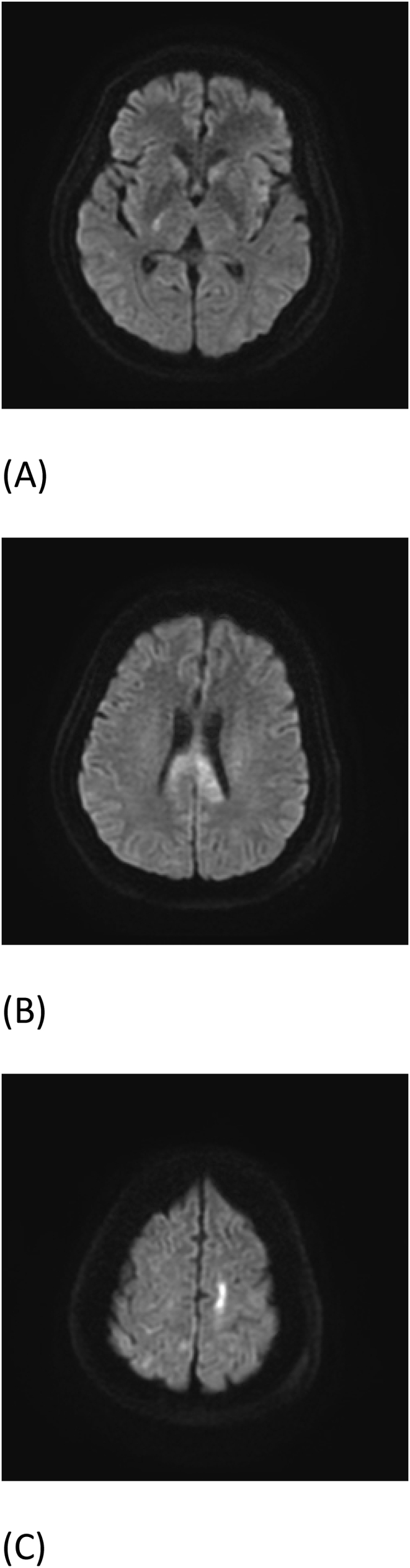
MRI (DWI1) of case no. 3, taken on Dec 17, 2015: Hyperdiffusion in the right thalamus, splenium of corpus callosum (more severe on left), and left parietal subcortical white matter.
2.5.3. Outcome
The patient was transferred to the respiratory care centrer for ventilation weaning. Her consciousness recovered to E4VEM5 on Jan 8, 2016. Her GCS progressively recovered to E4V3-4M6 and her endotracheal tube was removed on Jan 22. She was transferred to the general ward on Jan 26, and her GCS was fully recovered to E4V5M6 on Jan 29. She was discharged on Feb 4.
2.6. Adverse effect and safety
Neither complications nor adverse effects were reported by the patients during the course of treatment in Taoyuan General Hospital; however, further observation would be necessary to determine possible adverse effects and general long term follow-up.
3. Discussion
We gathered three cases receiving traditional Chinese medicine interventions after traumatic brain injury, and all of them had good recovery. Combining traditional Chinese medicine (decoctions and acupuncture) with Western medicine treatments is thus another therapeutic choice for diffuse axonal injury caused by severe traumatic brain injury.
3.1. Diffuse axonal injury
According to previous reports, DAI is found in 65–72% of the patients with moderate to severe head injury who survive the acute phase.17,18 The injuries are caused by shearing forces due to acceleration and deceleration. The damage usually appears in several locations. The most common sites are the junction of cerebral white and grey matter, the corpus callosum and the brain stem. The outcome of DAI was reported to be associated with injury location and number.6,10
According to Salazar et al., patients with DAI have lower GCS scores, worse outcomes and poorer prognosis than patients with other lesions.19 The median Glasgow Outcome Scale-Extended (GOSE) score measured after 12 months post-injury in patients with DAI is 7, compared with 8 without DAI. Skandsen et al. classified DAI into three stages (Table 1). There were no significant differences in outcome between stage 1 and 2, but stage 3 was associated with a higher rate of disability.6 According to Park et al., higher DAI grades are associated with slower consciousness recovery: The mean time of GCS recovery to E4V5M6 was 3.7 days in stage 1 patients and 59.9 days in stage 3 patients.20
Table 1.
Magnetic resonance imaging-based classification of DAI.
| Stage | Definition |
|---|---|
| 1a | Confirmed traumatic lesions to the lobar white matter or cerebellum only |
| 2 | Traumatic lesions is the corpus callosum, with or without lesions in the lobar white matter |
| 3b | Traumatic lesions in the brainstem in areas typical of DAI (dorsolateral quadrant of the upper brainstem, superior cerebellar peduncles) with or without lesions in the lobar white matter or corpus callosum |
Signal loss compatible with microbleeds (in the gradient echo sequence) or increased signal intensity compatible with tissue edema (in the FLAIR sequence).
In cases with unilateral superficial brain stem lesions, the lesion was interpreted as a contusion rather than DAI.
In brain trauma injury with DAI, the standard medical treatment aims to maintain stable vital signs, and monitor intracranial pressure and cerebral perfusion. The ICP and CPP were kept within normal range by sedation and osmotherapy. If ICP progressively increased after suitable medicine treatment, decompressive craniotomy was performed.21
3.2. Pathophysiology
Trauma and stroke are difficult insults sharing similar molecular and cellular mechanisms leading to brain cell death, as shown in previous studies.22, 23, 24, After stroke damage, local brain tissue swelling leads to moderate to severe reduction of cerebral blood flow, which in turn results in oxygen and glucose deprivation. These phenomena induce metabolic stress, energy failure, ionic imbalance, and ischemic injury.24,25 In severe TBI, cerebral blood flow reduction also occurs due to brain swelling, causing secondary ischemia. Cells in an ischemic environment will die within minutes.26, 27,
3.3. Traditional Chinese medicine
In the Chinese medicine literature, there is no specific discussion and treatment for DAI, possibly because there was no appropriate vital sign supportive care system and treatment for severe brain trauma patients until recent times, and the mortality rate was high. Given the similarities between TBI secondary injuries and stroke, we combined stroke-related traditional Chinese medicine treatments with modern medicine.
Several published clinical trials indicate that traditional Chinese medicine improves the treatment of experimental TBI or cerebral ischemic injury.29,31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42 The evidence of the beneficial effects of traditional Chinese medicine for TBI is increasing, and involves Chinese medicine decoctions, Chinese medical extracts and acupuncture. A systematic review suggested, as possible mechanisms, that Chinese medicine decoctions may reduce brain water content, improve the blood-brain barrier permeability, and decrease tumor necrosis factor alpha/nitric oxide (TNF-α/NO) expression.12
3.3.1. Buyang Huanwu Decoction (BHD)
BHD was the primary prescription for hemiplegia and paraplegia in the past. Today, it is extensively used for cerebral ischemic injury such as stroke and TBI.14 Many experimental studies indicate that BHD can improve the recovery of behavioral scores and decrease ischemia-reperfusion injury. The extract of Astragalus, the main herb in BHD, has protective effects on cerebral ischemia injury when used with Panax notoginseng saponins extract. Its mechanism may be based on the improvement of the early energy metabolism and the prevention of delayed apoptosis by inhibition of the mitochondrial apoptosis pathway.28 Based on a study by Mu et al., BHD exerts its neuroprotective effect by improving blood circulation, reducing calcium overload, inhibiting excitotoxicity, promoting angiogenesis and the migration of neural precursor cells to the infarct zone, reducing the inflammatory response, and inhibiting neuronal apoptosis.29
3.3.2. Tianma Gouteng Decoction (TGD)
TGD is often prescribed in China as an experimental treatment for stroke and neurodegenerative diseases. A study showed that TGD prevents the onset of hypertension and alters its development.30 Five major compound groups are contained in TGD: alkaloids, flavonoids, iridoids, carotenoids and natural phenols. These compounds exert strong anti-inflammatory effects by reducing the production of cytokines, chemokines and proteases in neuronal cells. They also reduce neuron necrosis and apoptosis by antioxidative and antiapoptotic effects.31
BHD and TGD can interrupt the biochemical cascades occurred in TBI and stroke, and are therefore potential therapeutic candidates for TBI and ischemic brain injury.
3.3.3. Acupuncture
All patients were treated with acupuncture a few days after Chinese decoctions were administered. The acupuncture points were: Baihui (GV20), Sishencong (EX-HN1), Shuigou (GV26), Hegu (LI4), and Taichong (LR3).32
Baihui (GV20)-based scalp acupuncture can improve infarct volume and neurological function scores, exerting neuroprotective effects in experimental ischemic brain injury.33 Sishencong (EX-HN1), Taichong (LR3), and other acupuncture points could improve cognitive performance, as observed by functional magnetic resonance imaging (fMRI), by strengthening the connections between cognition-related regions such as the insula, dorsal prefrontal cortex, hippocampus, thalamus, inferior parietal lobule and anterior cingulate cortex.34
The Baihui (GV20), Shuigou (GV26), and Hegu (LI4) acupuncture point regimens can significantly increase the number of neural stem cells, neurons and astrocytes cells in TBI rats, and acupuncture can also improve neurogenesis by stimulating the proliferation and differentiation of brain neural stem cells.33 By activating the brain-derived neurotrophic factor/tropomyosin receptor kinase B (BNDF/TrkB) signaling pathway, Baihui (GV20), Shuigou (GV26), Hegu (LI4), and other acupuncture point regimens promote the recovery of neurological impairment in rabbits after TBI.34, 35
In the Taiwan’s National Health Insurance Research Database’s cohort study, patients with TBI receiving acupuncture treatment returned to the emergency room and were re-hospitalized in the first year after injury less often than those who did not receive acupuncture.36 In another study by the same group, TBI patients undergoing acupuncture treatment were shown to have lower risk of stroke than patients who did not receive the treatment.37
Acupuncture improves motor and speech functions and GCS score recovery.38 In the rehabilitation stage, acupuncture can further improve motor function and muscle strength.39, 40 However, a review article indicated that many studies on this subject showed low methodological quality and varying acupuncture modalities, strategies, and outcome measurements.41
Modern medicine allows patients to survive the acute stage of TBI, but the treatment options are limited to ICP and CPP. Traditional Chinese medicine includes decoctions, acupuncture, blood-letting or their various combinations. The main purpose of traditional Chinese medicine in this context is to facilitate weaning from mechanical ventilation, improving consciousness, and shortening hospitalization. Traditional Chinese medicine treatments in TBI, and in particular in DAI, can compensate the insufficiency of modern medicine. Cheng et al. reported a case of early Chinese medicine intervention, 4 days after traumatic brain injury. That case had full recovery of consciousness (from E1VtM4 to a GCS score of 15) and was discharged in 2 months. The experience of traditional Chinese medicine can significantly improve our approach to this disease.42
3.3.4. Selecting decoction criteria
We chose BHD as our decoction according to previous literature and our experience. In traditional Chinese medicine, TBI leads to qi deficiency, qi, and blood stasis in the body. The mechanism of BHD in traditional Chinese medicine is to supplement the qi and remove stasis to promote blood circulation, thus aligning with the treatment direction for TBI. Hence, we did not see cause to add or subtract other herb medicines in the treatment course.
Case no. 2 presented as fever and persisting tremor in the beginning of the treatment course. According to the theory of traditional Chinese medicine, Liver yang flamed up and internal wind may have led to high body temperature and tremor. After considering previous literature, we administered TGD to subside the Liver yang and extinguish internal wind. We replaced TGD with BHD when the patient started the rehabilitation program (Table 2).
Table 2.
Summary of the cases.
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Age, sex | 23, Male | 20, Male | 58, Female |
| TBI date | June 22, 2014 | Nov 11, 2014 | Nov 23, 2015 |
| Decoction | BHD | TGD (Dec 3, 2014–Jan 25, 2015) | BHD |
| BHD (Jan 26, 2015) | |||
| TCM start date | July 3, 2014(11th) | Dec 3, 2014(22nd) | Dec 1, 2015(8th) |
| GCS at TCM start date | E2VEM2-3 | E1VEM2-3 | E1VEM1 |
| Acupuncture start date | July 4, 2014(12th) | Dec 16, 2014(35th) | Dec 1, 2015(8th) |
TBI, traumatic brain injury; TCM, traditional Chinese medicine; GCS, Glasgow Coma Scale.
4. Conclusions
This report described two Chinese medicine decoctions combined with acupuncture treatment in three cases with DAI from severe traumatic brain injury, all resulting in good outcomes. According to previous literature, DAI has poor prognosis. In this report, we demonstrate that traditional Chinese medicine and acupuncture may be safe and effective alternative treatments for TBI with DAI, though the consequences derived from the natural course of DAI cannot be ruled out. More rigorous studies are still needed to prove the effectiveness of traditional Chinese medicine, and the appropriate treatment protocol in TBI and DAI.
Ethics considerations
We have obtained written informed consent from the patients for publication of this cases report in print form for scientific purposes. This study was approved by the Institutional Review Board of Taoyuan General Hospital (TYGH109-01).
Declaration of interest
The authors declare that there are no conflicts of interest.
Funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that there are no conflicts of interest. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jtcme.2020.02.012.
Contributor Information
Yu-Chang Hou, Email: houyc0115@gmail.com.
Yuan-Yi Chang, Email: c3312@ms7.hinet.net.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Taylor C.A., Bell J.M., Breiding M.J., Xu L. Traumatic brain injury-related emergency department visits, hospitalizations, and deaths - United States, 2007 and 2013. MMWR Surveill Summ. 2017;66:1–16. doi: 10.15585/mmwr.ss6609a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li M., Zhao Z., Yu G., Zhang J. Epidemiology of traumatic brain injury over the world: a systematic review. Austin Neurol & Neurosci. 2016;1:1007. doi: 10.4172/2327-5146.1000275. [DOI] [Google Scholar]
- 3.Tung Y.C., Tu H.P., Tsai W.C. Increased incidence of herpes zoster and postherpetic neuralgia in adult patients following traumatic brain injury: a nationwide population-based study in Taiwan. PLoS One. 2015;10 doi: 10.1371/journal.pone.0129043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alberico A.M., Ward J.D., Choi S.C., Marmarou A., Young H.F. Outcome after severe head injury. Relationship to mass lesions, diffuse injury, and ICP course in pediatric and adult patients. J Neurosurg. 1987;67:648–656. doi: 10.3171/jns.1987.67.5.0648. [DOI] [PubMed] [Google Scholar]
- 5.Eum S.W., Lim D.J., Kim B.R. Prognostic factors in patients with diffuse axonal injury. J Korean Neurosurg So. 1998;27:1668–1674. [Google Scholar]
- 6.Skandsen T., Kvistad K.A., Solheim O., Strand I.H., Folvik M., Vik A. Prevalence and impact of diffuse axonal injury in patients with moderate and severe head injury: a cohort study of early magnetic resonance imaging findings and 1-year outcome. J Neurosurg. 2010;113:556–563. doi: 10.3171/2009.9.JNS09626. [DOI] [PubMed] [Google Scholar]
- 7.Maas A.I., Stocchetti N., Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7:728–741. doi: 10.1016/S1474-4422(08)70164-9. [DOI] [PubMed] [Google Scholar]
- 8.Weiss N., Galanaud D., Carpentier A., Naccache L., Puybasset L. Clinical review: prognostic value of magnetic resonance imaging in acute brain injury and coma. Crit Care. 2007;11:230. doi: 10.1186/cc6107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scheid R., Walther K., Guthke T., Preul C., von Cramon D.Y. Cognitive sequelae of diffuse axonal injury. Arch Neurol. 2006;63:418–424. doi: 10.1001/archneur.63.3.418. [DOI] [PubMed] [Google Scholar]
- 10.Adams J.H., Doyle D., Ford I., Gennarelli T.A., Graham D.I., McLellan D.R. Diffuse axonal injury in head injury: definition, diagnosis and grading. Histopathology. 1989;15:49–59. doi: 10.1111/j.1365-2559.1989.tb03040.x. [DOI] [PubMed] [Google Scholar]
- 11.WHO Regional Office for the Western Pacific . World Health Organization Press; 2008. WHO Standard Acupuncture Point Locations in the Western Pacific Region. [Google Scholar]
- 12.Yang B., Wang Z., Sheng C. Evidence-based review of oral traditional Chinese medicine compound recipe administration for treating weight drop-induced experimental traumatic brain injury. BMC Compl Alternative Med. 2016;16:95. doi: 10.1186/s12906-016-1076-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang H.W., Liou K.T., Wang Y.H. Deciphering the neuroprotective mechanisms of Bu-yang Huan-Wu decoction by an integrative neurofunctional and genomic approach in ischemic stroke mice. J Ethnopharmacol. 2011;38:22–33. doi: 10.1016/j.jep.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 14.Wang L., Jiang D.M. Neuroprotective effect of Buyang Huanwu Decoction on spinal ischemia/reperfusion injury in rats. J Ethnopharmacol. 2009;124:219–223. doi: 10.1016/j.jep.2009.04.045. [DOI] [PubMed] [Google Scholar]
- 15.Zhao L.D., Wang J.H., Jin G.R., Zhao Y., Zhang H.J. Neuroprotective effect of Buyang Huanwu decoction against focal cerebral ischemia/reperfusion injury in rats--time window and mechanism. J Ethnopharmacol. 2012;140:339–344. doi: 10.1016/j.jep.2012.01.026. 2012. [DOI] [PubMed] [Google Scholar]
- 16.Fruehauf H. Prevention and treatment by Chinese herbal medicine, stroke and post-stroke syndrome. J Chin Med. 1994;44:22–35. [Google Scholar]
- 17.Skandsen T., Kvistad K.A., Solheim O., Strand I.H., Folvik M., Vik A. Prevalence and impact of diffuse axonal injury in patients with moderate and severe head injury: a cohort study of early magnetic resonance imaging findings and 1-year outcome. J Neurosurg. 2010;113:556–563. doi: 10.3171/2009.9.JNS09626. [DOI] [PubMed] [Google Scholar]
- 18.Lagares A., Ramos A., Pérez-Nuñez A. The role of MR imaging in assessing prognosis after severe and moderate head injury. Acta Neurochir (Wien) 2009;151:341–356. doi: 10.1007/s00701-009-0194-8. [DOI] [PubMed] [Google Scholar]
- 19.Salazar A.M., Grafman J.H., Vance S.C., Weingartner H., Dillon J.D., Ludlow C. Consciousness and amnesia after penetrating head injury: neurology and anatomy. Neurology. 1986;36:178–187. doi: 10.1212/wnl.36.2.178. [DOI] [PubMed] [Google Scholar]
- 20.Park S.J., Hur J.W., Kwon K.Y., Rhee J.J., Lee J.W., Lee H.K. Time to recover consciousness in patients with diffuse axonal injury: assessment with reference to magnetic resonance grading. J Korean Neurosurg Soc. 2009;46:205–209. doi: 10.3340/jkns.2009.46.3.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carney N., Totten A.M., O’Reilly C. fourth ed. vol. 80. 2017. pp. 6–15. (Guidelines for the Management of Severe Traumatic Brain Injury). Neurosurgery. [DOI] [PubMed] [Google Scholar]
- 22.Dirnagl U., Iadecola C., Moskowitz M.A. Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci. 1999;22:391–397. doi: 10.1016/s0166-2236(99)01401-0. [DOI] [PubMed] [Google Scholar]
- 23.Smith D.H., Chen X.H., Pierce J.E. Progressive atrophy and neuron death for one year following brain trauma in the rat. J Neurotrauma. 1997;14:715–727. doi: 10.1089/neu.1997.14.715. [DOI] [PubMed] [Google Scholar]
- 24.Wiegand F., Liao W., Busch C. Respiratory chain inhibition induces tolerance to focal cerebral ischemia. J Cerebr Blood Flow Metabol. 1999;19:1229–1237. doi: 10.1097/00004647-199911000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Folbergrová J., Smith M.L., Inamura K., Siesjö B.K. Decrease of glutamate decarboxylase activity in substantia nigra and caudoputamen following transient hyperglycemic ischemia in the rat. J Cerebr Blood Flow Metabol. 1989;9:897–901. doi: 10.1038/jcbfm.1989.124. [DOI] [PubMed] [Google Scholar]
- 26.Marion D.W., Bouma G.J. The use of stable xenon-enhanced computed tomographic studies of cerebral blood flow to define changes in cerebral carbon dioxide vasoresponsivity caused by a severe head injury. Neurosurgery. 1991;29:869–873. doi: 10.1097/00006123-199112000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Bouma G.J., Muizelaar J.P., Choi S.C., Newlon P.G., Young H.F. Cerebral circulation and metabolism after severe traumatic brain injury: the elusive role of ischemia. J Neurosurg. 1991;75:685–693. doi: 10.3171/jns.1991.75.5.0685. [DOI] [PubMed] [Google Scholar]
- 28.Huang X.P., Tan H., Chen B.Y., Deng C.Q. Combination of total Astragalus extract and total Panax notoginseng saponins strengthened the protective effects on brain damage through improving energy metabolism and inhibiting apoptosis after cerebral ischemia-reperfusion in mice. Chin J Integr Med. 2017;23:445–452. doi: 10.1007/s11655-015-1965-0. [DOI] [PubMed] [Google Scholar]
- 29.Mu Q., Liu P., Hu X., Gao H., Zheng X., Huang H. Neuroprotective effects of Buyang Huanwu decoction on cerebral ischemia-induced neuronal damage. Neural Regen Res. 2014;9:1621–1627. doi: 10.4103/1673-5374.141791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang T.-X., Zhang T.X., Wang Y.F., Ciriello J. The herbal medicine tian ma gou teng yen alters the development of high blood pressure in the spontaneously hypertensive rat. Am J Chin Med. 1989;17:211–219. doi: 10.1142/S0192415X89000309. [DOI] [PubMed] [Google Scholar]
- 31.Chik S.C., Or T.C., Luo D., Yang C.L., Lau A.S. Pharmacological effects of active compounds on neurodegenerative disease with gastrodia and uncaria decoction, a commonly used poststroke decoction. ScientificWorldJournal. 2013;2013:896873. doi: 10.1155/2013/896873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang Y.M., Zhang Y.Q., Cheng S.B., Chen S.X., Chen A.L., Tang C.Z. Effect of acupuncture on proliferation and differentiation of neural stem cells in brain tissues of rats with traumatic brain injury. Chin J Integr Med. 2013;19:132–136. doi: 10.1007/s11655-013-1353-6. [DOI] [PubMed] [Google Scholar]
- 33.Wang W.W., Xie C.L., Lu L., Zheng G.Q. A systematic review and meta-analysis of Baihui (GV20)-based scalp acupuncture in experimental ischemic stroke. Sci Rep. 2014;4:3981. doi: 10.1038/srep03981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tan T.T., Wang D., Huang J.K. Modulatory effects of acupuncture on brain networks in mild cognitive impairment patients. Neural Regen Res. 2017;12:250–258. doi: 10.4103/1673-5374.200808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li X., Chen C., Yang X. Acupuncture improved neurological recovery after traumatic brain injury by activating BDNF/TrkB pathway. Evid Based Complement Alternat Med. 2017;2017:8460145. doi: 10.1155/2017/8460145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shih C.C., Lee H.H., Chen T.L. Reduced use of emergency care and hospitalization in patients with traumatic brain injury receiving acupuncture treatment. Evid Based Complement Alternat Med. 2013;2013:262039. doi: 10.1155/2013/262039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shih C.C., Hsu Y.T., Wang H.H. Decreased risk of stroke in patients with traumatic brain injury receiving acupuncture treatment: a population-based retrospective cohort study. PLoS One. 2014;9 doi: 10.1371/journal.pone.0089208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ding J., Dong G.F., Song Y.X., Xu Y.C. Control observation on therapeutic effects of acupuncture treatment on acute severe craniocerebral injury. Chin Acupunct Moxibustion. 2002;22:445–447. [Google Scholar]
- 39.Cao W.S., Qin Y.X., Hou Q.X. Acupuncture combined with hyperbaric oxygen treatment for post-traumatic brain injury syndrome (Translation). Modern Rehabilitation. Journal of Clinical Rehabilitative Tissue Engineering. 2001;5:110. [Google Scholar]
- 40.Chang Z.J., Liu P. Rehabilitation and acupuncture treatment for patients with traumatic brain injury (Translation) Chin J Med Device. 2005;18:38–39. [Google Scholar]
- 41.Wong V., Cheuk D.K., Lee S., Chu V. Acupuncture for acute management and rehabilitation of traumatic brain injury. Cochrane Database Syst Rev. 2013;3:CD007700. doi: 10.1002/14651858.CD007700.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cheng K.W., Huang C.T., Chang Y.Y., Hou Y.C. Early intervention with integrated Chinese and Western medicine in severe traumatic brain injury-A case report. J Chin Med. 2015;26:73–82. doi: 10.3966/101764462015062601007. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.