Key Points
Question
Is administration of systemic corticosteroids associated with reduced 28-day mortality in critically ill patients with coronavirus disease 2019 (COVID-19)?
Findings
In this prospective meta-analysis of 7 randomized trials that included 1703 patients of whom 647 died, 28-day all-cause mortality was lower among patients who received corticosteroids compared with those who received usual care or placebo (summary odds ratio, 0.66).
Meaning
Administration of systemic corticosteroids, compared with usual care or placebo, was associated with lower 28-day all-cause mortality in critically ill patients with COVID-19.
Abstract
Importance
Effective therapies for patients with coronavirus disease 2019 (COVID-19) are needed, and clinical trial data have demonstrated that low-dose dexamethasone reduced mortality in hospitalized patients with COVID-19 who required respiratory support.
Objective
To estimate the association between administration of corticosteroids compared with usual care or placebo and 28-day all-cause mortality.
Design, Setting, and Participants
Prospective meta-analysis that pooled data from 7 randomized clinical trials that evaluated the efficacy of corticosteroids in 1703 critically ill patients with COVID-19. The trials were conducted in 12 countries from February 26, 2020, to June 9, 2020, and the date of final follow-up was July 6, 2020. Pooled data were aggregated from the individual trials, overall, and in predefined subgroups. Risk of bias was assessed using the Cochrane Risk of Bias Assessment Tool. Inconsistency among trial results was assessed using the I2 statistic. The primary analysis was an inverse variance–weighted fixed-effect meta-analysis of overall mortality, with the association between the intervention and mortality quantified using odds ratios (ORs). Random-effects meta-analyses also were conducted (with the Paule-Mandel estimate of heterogeneity and the Hartung-Knapp adjustment) and an inverse variance–weighted fixed-effect analysis using risk ratios.
Exposures
Patients had been randomized to receive systemic dexamethasone, hydrocortisone, or methylprednisolone (678 patients) or to receive usual care or placebo (1025 patients).
Main Outcomes and Measures
The primary outcome measure was all-cause mortality at 28 days after randomization. A secondary outcome was investigator-defined serious adverse events.
Results
A total of 1703 patients (median age, 60 years [interquartile range, 52-68 years]; 488 [29%] women) were included in the analysis. Risk of bias was assessed as “low” for 6 of the 7 mortality results and as “some concerns” in 1 trial because of the randomization method. Five trials reported mortality at 28 days, 1 trial at 21 days, and 1 trial at 30 days. There were 222 deaths among the 678 patients randomized to corticosteroids and 425 deaths among the 1025 patients randomized to usual care or placebo (summary OR, 0.66 [95% CI, 0.53-0.82]; P < .001 based on a fixed-effect meta-analysis). There was little inconsistency between the trial results (I2 = 15.6%; P = .31 for heterogeneity) and the summary OR was 0.70 (95% CI, 0.48-1.01; P = .053) based on the random-effects meta-analysis. The fixed-effect summary OR for the association with mortality was 0.64 (95% CI, 0.50-0.82; P < .001) for dexamethasone compared with usual care or placebo (3 trials, 1282 patients, and 527 deaths), the OR was 0.69 (95% CI, 0.43-1.12; P = .13) for hydrocortisone (3 trials, 374 patients, and 94 deaths), and the OR was 0.91 (95% CI, 0.29-2.87; P = .87) for methylprednisolone (1 trial, 47 patients, and 26 deaths). Among the 6 trials that reported serious adverse events, 64 events occurred among 354 patients randomized to corticosteroids and 80 events occurred among 342 patients randomized to usual care or placebo.
Conclusions and Relevance
In this prospective meta-analysis of clinical trials of critically ill patients with COVID-19, administration of systemic corticosteroids, compared with usual care or placebo, was associated with lower 28-day all-cause mortality.
This meta-analysis pools data from 7 randomized trials to estimate the association between administration of corticosteroids vs usual care or placebo and all-cause mortality at 28 days in patients with severe coronavirus disease 2019 (COVID-19).
Introduction
The role of corticosteroids in treating severe infections has been an enduring controversy.1,2,3 During the coronavirus disease 2019 (COVID-19) pandemic, rigorous data on the efficacy of corticosteroids have been limited.4,5 The pandemic has been a potent stimulus for clinical research addressing this controversy.
As of July 24, 2020, 55 studies of corticosteroids for the treatment of COVID-19 have been registered on ClinicalTrials.gov. Recognizing the urgency of generating reliable data on the efficacy of corticosteroids to guide clinical management, the Clinical Characterization and Management Working Group of the World Health Organization (WHO) developed a protocol for a prospective meta-analysis6 of ongoing randomized clinical trials.
While this initiative was in development, the UK-based Randomized Evaluation of COVID-19 Therapy (RECOVERY) trial reported its findings from 6425 patients randomized to 6 mg/d of dexamethasone or usual care. Overall, dexamethasone resulted in an absolute reduction in mortality of 2.8% (22.9% vs 25.7% for usual care; age-adjusted rate ratio, 0.83 [95% CI, 0.75-0.93]). The benefit was greatest for patients who were receiving invasive mechanical ventilation at the time of randomization with mortality of 29.3% for dexamethasone vs 41.4% for usual care (rate ratio, 0.64 [95% CI, 0.51-0.81]).7 The signal seen in this trial led most ongoing trials of corticosteroids to suspend recruitment.
The objective of this prospective meta-analysis of randomized trials was to estimate the association between administration of corticosteroids, compared with usual care or placebo, and 28-day all-cause mortality in hospitalized, critically ill patients with suspected or confirmed COVID-19.
Methods
Identification of Trials
Trials were identified through a comprehensive systematic search of ClinicalTrials.gov, the Chinese Clinical Trial Registry, and the EU Clinical Trials Register, from December 31, 2019, to April 6, 2020. All recruiting clinical trials related to COVID-19 that examined the therapeutic efficacy of corticosteroids were identified.
The search terms used to identify studies for the meta-analysis were COVID-19, corticosteroids, and steroids. Thirteen clinical trials were identified using these search terms. Three additional records not identified in the registries were identified through experts from the WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group. Three staff members at the W2O Group conducted the initial search, the results of which were presented to the protocol writing group. The protocol writing group determined by consensus whether trials met the inclusion criteria.
Development of Prospective Meta-analysis
Senior investigators of all trials identified as potentially eligible were asked to participate in weekly calls starting on May 14, 2020, during which plans for the prospective meta-analysis and drafts of the protocol were developed and reviewed. The protocol was registered and made publicly available on the PROSPERO database (CRD42020197242) on July 6, 2020, and has been published.8
Based on information from the published protocols and prior communications with trial investigators, the trials that had randomly assigned critically ill patients to a group in whom corticosteroids were administered and to a group in whom corticosteroids were not administered were invited by the WHO chief scientist on behalf of the Clinical Characterization and Management Working Group of the WHO to participate in the prospective meta-analysis. The protocol for the prospective meta-analysis stipulated that no additional trials would be included after outcome data were shared, but that if results from further eligible trials became available before the results of the prospective meta-analysis were published, additional meta-analyses including these results would be conducted and reported. Additional potentially eligible trials were identified through contact with experts and when published in peer-reviewed journals.
All trials secured institutional review board approval, but approval was not required for the secondary data analysis reported here. Informed consent for participation in each trial was obtained and was consistent with local institutional review board requirements. There were minor variations in the definitions of critically ill used to specify each trial’s eligibility criteria (Table 1).9 The RECOVERY trial recruited both critically ill and non–critically ill hospitalized patients. Because it was not possible to distinguish whether patients had been critically ill but not receiving invasive mechanical ventilation at the time of randomization, data were requested only for the patients in the RECOVERY trial who received invasive mechanical ventilation. Data were pooled from patients recruited to the participating trials through June 9, 2020, because patient management after that date was likely to be affected by the release of results of the RECOVERY trial on June 16, 2020.
Table 1. Characteristics of Included Trials.
| DEXA-COVID 19 | CoDEX | RECOVERY | CAPE COVID | COVID STEROID | REMAP-CAP | Steroids-SARIa | |
|---|---|---|---|---|---|---|---|
| ClinicalTrials.gov identifier | NCT04325061 | NCT04327401 | NCT04381936 | NCT02517489 | NCT04348305 | NCT02735707 | NCT04244591 |
| Planned sample size | 200 | 350 | NA | 290 | 1000 | NAb | 80 |
| Eligibility criteria |
|
|
|
|
|
|
|
| Corticosteroid | |||||||
| Drug name | Dexamethasone | Dexamethasone | Dexamethasone | Hydrocortisone | Hydrocortisone | Hydrocortisone | Methylprednisolone |
| Dosage and administration | 20 mg/d intravenously × 5 d and then 10 mg/d intravenously × 5 d | 20 mg/d intravenously × 5 d and then 10 mg/d intravenously × 5 d | 6 mg/d orally or intravenously | Continuous intravenous infusion × 8 d or 14 d (200 mg/d × 4 d or 7 d; 100 mg/d × 2 d or 4 d; 50 mg/d × 2 d or 3 d) | 200 mg/d intravenously × 7 d (continuous or bolus dosing every 6 h) | 50 mg intravenously every 6 h × 7 dd | 40 mg intravenously every 12 h × 5 d |
| Dose classification | High | High | Low | Low | Low | Low | High |
| Control intervention | Usual care | Usual care | Usual care | Placebo | Placebo | Usual care | Usual care |
| Primary outcome | 60-d mortality | Ventilator-free days | 28-d mortality | 21-d treatment failure (death or persistent requirement for mechanical ventilation or high-flow oxygen therapy) | Days alive without life support at 28 d | Composite of hospital mortality and ICU organ support–free days to 21 d | Lower lung injury score at 7 d and 14 d |
| Mortality outcome, d | 28 | 28 | 28 | 21 | 28 | 28 | 30 |
| Serious adverse event definitions |
|
|
|
|
|
|
|
| Location | Spain | Brazil | UK | France | Denmark | Australia, Canada, European Union, New Zealand, UK, US | China |
Abbreviations: ARDS, acute respiratory distress syndrome; CAPE COVID, Community-Acquired Pneumonia: Evaluation of Corticosteroids in Coronavirus Disease; CoDEX, COVID-19 Dexamethasone; COVID-19, coronavirus disease 2019; COVID STEROID, Hydrocortisone for COVID-19 and Severe Hypoxia; DEXA-COVID 19, Efficacy of Dexamethasone Treatment for Patients With ARDS Caused by COVID-19; Fio2, fraction of inspired oxygen; ICU, intensive care unit; NA, not applicable; RECOVERY, Randomized Evaluation of COVID-19 Therapy; REMAP-CAP, Randomized, Embedded, Multifactorial Adaptive Platform Trial for Community-Acquired Pneumonia; Sepsis-3, Third International Consensus Definitions for Sepsis and Septic Shock; Steroids-SARI, Glucocorticoid Therapy for COVID-19 Critically Ill Patients With Severe Acute Respiratory Failure.
Trial did not specify whether adverse events were serious or nonserious.
No sample size was specified at the start of the trial.
The RECOVERY trial also recruited hospitalized patients with suspected or confirmed COVID-19 who were not receiving invasive mechanical ventilation at randomization.
Too few patients were randomized to the high-dose group to permit separate analyses.
Outcomes
The primary outcome was all-cause mortality up to 30 days after randomization and was determined before any outcome data were available from any of the studies. Shorter-term mortality (eg, 21 days) was acceptable if longer-term mortality was not available. Five trials reported mortality at 28 days after randomization; therefore, the primary outcome is reported as 28-day all-cause mortality. The Community-Acquired Pneumonia: Evaluation of Corticosteroids in Coronavirus Disease (CAPE COVID; NCT02517489) trial10 reported mortality at 21 days and the Glucocorticoid Therapy for COVID-19 Critically Ill Patients With Severe Acute Respiratory Failure (Steroids-SARI; NCT04244591) trial reported mortality at 30 days.
The secondary outcome was serious adverse events. Details of the definitions and measurement of serious adverse events were collected in advance of the trials sharing outcome data.
Data Aggregation
Before sharing outcome data, trial investigators provided summary information on the characteristics of patients at the time of randomization and the numbers of patients lost to follow-up together with the age of each participant; these data were used to calculate the median age across trials. Trial investigators then provided summary tables showing the numbers of participants who did and did not experience each outcome according to intervention group, overall, and in the following patient subgroups based on status at randomization: (1) whether patients were receiving invasive mechanical ventilation, (2) whether patients were receiving vasoactive medication, (3) whether patients were aged 60 years or younger or were older than 60 years (the median across trials), (4) sex (male or female), and (5) whether patients had been symptomatic for 7 days or less or for more than 7 days. The fifth subgroup was specified post hoc based on results from the RECOVERY trial. All other subgroup analyses were prespecified before any outcome data became available.
Risk of Bias Assessment
For each trial, we assessed the risk of bias (“low risk,” “some concerns,” or “high risk” of bias) in the overall effect of corticosteroids on mortality and serious adverse events using version 2 of the Cochrane Risk of Bias Assessment Tool.11 We also assessed risk of bias for the effect of assignment to the intervention. Risk of bias assessments were based on the trial protocols and flowcharts following the Consolidated Standards of Reporting Trials together with this information supplied by the investigators of each trial: (1) the methods used to generate the allocation sequence and conceal randomized allocation; (2) whether patients and health professionals were blinded to assigned intervention; (3) the methods used to ensure that patients received their allocated intervention and the extent of deviations from the assigned intervention; and (4) the methods used to measure mortality and serious adverse events. Risk of bias assessments were done independently by 4 of the investigators (A.G., J.P.T.H., M.H.M., and J.S.), with disagreements resolved through discussion. We used the Grading of Recommendations Assessment, Development and Evaluation (GRADE)12 approach to assess the certainty of the evidence that corticosteroids reduce mortality in critically ill patients with COVID-19.
Data Analysis
We classified the trials according to the corticosteroid drug used in the intervention group and whether the trial used a low dose or a high dose of corticosteroids based on the following a priori–defined cutoffs: 15 mg/d of dexamethasone, 400 mg/d of hydrocortisone, and 1 mg/kg/d of methylprednisolone.13 The primary analysis was an inverse variance–weighted fixed-effect meta-analysis of odds ratios (ORs) for overall mortality, which was repeated after excluding results from the RECOVERY trial. We also conducted random-effects meta-analyses (with the Paule-Mandel estimate of heterogeneity)14,15 and an inverse variance–weighted fixed-effect analysis using risk ratios. We applied the Hartung-Knapp adjustment16,17 to account for uncertainty in the estimation of between-study variance in the random-effects meta-analysis. This variance is imprecisely estimated when few studies are included and when some studies are small (both of which are the case with this meta-analysis), leading to 95% CIs that are much wider than for the fixed-effect analysis.
We quantified inconsistency in associations among the trials using the I2 statistic and derived P values for heterogeneity using the Cochran Q statistic. We report precise P values. The protocol specified that a threshold for statistical significance would not be used. Odds ratios with 95% CIs were plotted for the association between corticosteroids, compared with usual care or placebo, and serious adverse events. Because the definitions of serious adverse events varied among the trials, a meta-analysis of this outcome was not conducted. Participants with missing outcome data were excluded from the analyses.
Evidence for differences in associations between the subgroups was quantified by ratios of ORs comparing associations in the subgroups and the corresponding P values for interaction. If the ratio of ORs is equal to 1, the estimated associations in the 2 subgroups are the same. The further the ratio of ORs is from 1, the greater is the difference between the estimated associations in the 2 subgroups. Comparisons between subgroups defined by trial characteristics were made using random-effects meta-regression and interpreted as exploratory because of the small number of trials and the potential for confounding by other characteristics. Comparisons between subgroups defined by patient characteristics were done by estimating the trial-specific ratios of ORs comparing associations between subgroups and then combining these in meta-analyses.18
A hybrid approach was adopted for the analysis relating to critically ill patients who were vs who were not receiving invasive mechanical ventilation at randomization because in some trials all patients were receiving invasive mechanical ventilation. For this analysis, we compared the overall associations among critically ill patients who were and who were not receiving invasive mechanical ventilation at randomization (including patients in the RECOVERY trial who received invasive mechanical ventilation) with the association among patients in the RECOVERY trial who required oxygen with or without noninvasive ventilation but were not receiving invasive mechanical ventilation at randomization.
To obtain illustrative estimates of absolute risks for the overall analysis and for different types of corticosteroids, we assumed a mortality risk without corticosteroids of 40% (approximately, the risk among all patients allocated to usual care or placebo) and applied the meta-analytic OR to obtain a mortality risk with corticosteroids. To obtain illustrative estimates of absolute risks for different patient subgroups, we assumed a mortality risk equal to the observed risk across patients in that subgroup who were randomized to usual care or placebo, and applied the subgroup meta-analytic OR to obtain a mortality risk with corticosteroids in the subgroup.
Because the Randomized, Embedded, Multifactorial Adaptive Platform Trial for Community-Acquired Pneumonia (REMAP-CAP; NCT02735707) trial19,20 assigned patients to both high-dose and low-dose corticosteroid interventions, we planned to use network meta-analysis to estimate associations between high-dose vs low-dose corticosteroids and mortality. However, too few patients in this trial were randomized to high-dose corticosteroids for such an analysis to be feasible.
All analyses were conducted using Stata statistical software version 16 (StataCorp) and new Stata commands to conduct and graph the results of meta-analyses.
Results
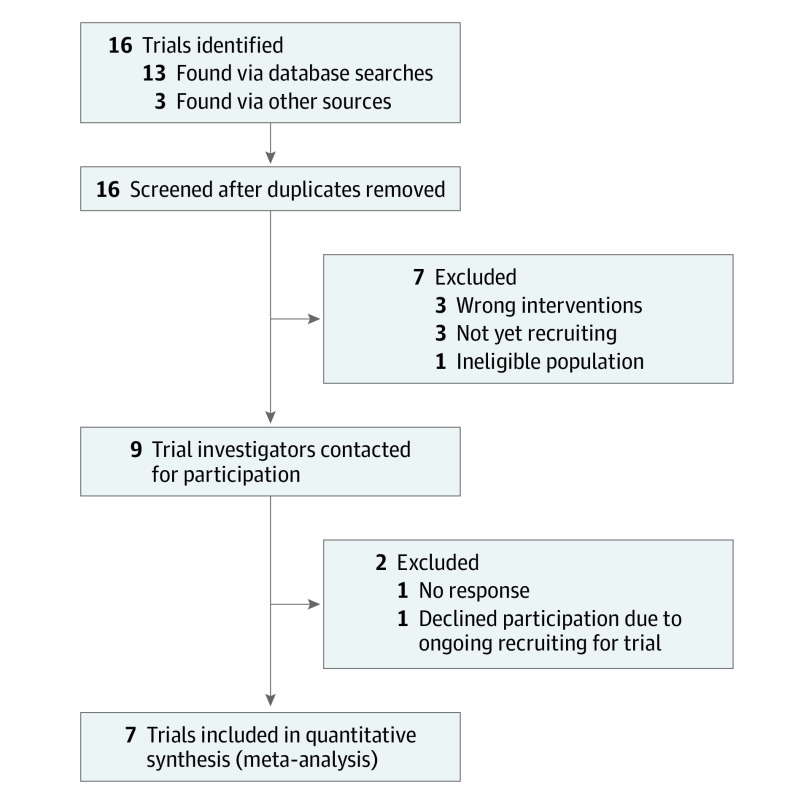
Sixteen trials that were recruiting critically patients with COVID-19 and had randomized patients to receive corticosteroids vs usual care or placebo were identified (Figure 1). One trial (NCT04273321) did not respond to requests to participate in the prospective meta-analysis and by May 2020 it had recruited 86 patients. Another trial (NCT04344730) declined participation because randomization was ongoing and by June 2020 it had recruited 14 patients. Other trials were excluded because their investigators confirmed that they had not recruited any patients (ChiCTR2000029656, ChiCTR2000030481, and 2020-002191-12 [no longer registered]), because they recruited patients with mild or moderate disease (NCT04329650), or because randomization did not include a group without corticosteroid treatment (NCT04330586, 2020-001306-35, and NCT04251871).
Figure 1. Flow Diagram Showing the Identification of Eligible Trials and Participating Trials.
Seven trials were included in the final meta-analysis (Table 1). Patients were recruited from Australia, Brazil, Canada, China, Denmark, France, Ireland, the Netherlands, New Zealand, Spain, the UK, and the US. Patients were recruited from February 26, 2020, to June 9, 2020, and the date of final follow-up was July 6, 2020. The corticosteroid groups included dexamethasone at low and high doses, low-dose hydrocortisone, and high-dose methylprednisolone. The Efficacy of Dexamethasone Treatment for Patients With ARDS Caused by COVID-19 (DEXA-COVID 19; NCT04325061) trial and the COVID-19 Dexamethasone (CoDEX; NCT04327401) trial21 only enrolled patients receiving invasive mechanical ventilation. For the RECOVERY trial,7 only patients who received invasive mechanical ventilation at randomization were included in the primary analysis. The REMAP-CAP trial19,20 (NCT02735707) and the Steroids-SARI (NCT04244591) trial only enrolled patients admitted to an intensive care unit. The CAPE COVID trial10 (NCT02517489) enrolled patients admitted to an intensive care unit or an intermediate care unit who were receiving a minimum of 6 L/min of supplemental oxygen. The Hydrocortisone for COVID-19 and Severe Hypoxia (COVID STEROID; NCT04348305) trial enrolled patients receiving a minimum of 10 L/min of supplemental oxygen. The definitions of serious adverse events varied between the trials, and mainly focused on secondary infections and sepsis (Table 1).
A total of 1703 patients were randomized (678 to corticosteroids and 1025 to usual care or placebo) in the 7 trials, the median age was 60 years (interquartile range, 52-68 years), and 488 patients (29%) were women (Table 2). The larger number of patients randomized to usual care or placebo was due to randomization in the RECOVERY trial (contributed 1007 [59.1%] patients to this analysis) in which patients were assigned to corticosteroid or usual care in a ratio of 1:2. Most patients had severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection confirmed by polymerase chain reaction; and the proportions of patients with SARS-CoV-2 infection confirmed by polymerase chain reaction ranged from 78.7% to 100% across trials. In all trials, the majority of patients were male. The extent of concurrent treatment with antiviral agents or azithromycin varied substantially among the trials (Table 2).
Table 2. Characteristics of Patients Included in the Prospective Meta-analysis.
| DEXA-COVID 19 | CoDEX | RECOVERY | CAPE COVID | COVID STEROID | REMAP-CAPa | Steroids-SARIb | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Steroid | No steroid | Steroid | No steroid | Steroid | No steroid | Steroid | No steroid | Steroid | No steroid | Steroid | No steroid | Steroid | No steroid | |
| Patients randomized by June 9, 2020 | 7 | 12 | 128 | 128 | 324 | 683 | 76 | 73 | 15 | 14 | 105 | 92 | 24 | 23 |
| Age, median (IQR), y | 62 (48-68) | 60 (52-69) | 62 (50-70) | 64 (57-73) | 59 (52-66) | 60 (52-68) | 63 (52-71) | 66 (54-73) | 57 (52-75) | 62 (55-71) | 59 (53-68) | 62 (50-72) | 67 (61-74) | 62 (54-68) |
| Female sex, No. (%) | 3 (42.9) | 3 (25) | 47 (36.7) | 44 (34.4) | 91 (28.1) | 182 (26.6) | 22 (28.9) | 23 (31.5) | 2 (13.3) | 4 (28.6) | 30 (28.6) | 25 (27.2) | 7 (29) | 5 (22) |
| PCR-confirmed SARS-CoV-2 infection, No. (%) | 7 (100) | 12 (100) | 120 (93.8) | 122 (95.3) | 301 (92.9) | 647 (94.7) | 72 (94.7) | 72 (98.6) | 15 (100) | 14 (100) | 80 (76.2) | 75 (81.5) | 24 (100) | 23 (100) |
| Treatments at randomization, No. (%) | ||||||||||||||
| Mechanical ventilation | 7 (100) | 12 (100) | 128 (100) | 128 (100) | 324 (100) | 683 (100) | 62 (81.6) | 59 (80.8) | 7 (46.7) | 8 (57.1) | 68 (64.8) | 49 (53.3) | 13 (54) | 14 (61) |
| Vasoactive | 3 (42.9) | 7 (58.3) | 83 (65.4) | 88 (68.8) | Not recorded | Not recorded | 18 (23.7) | 13 (17.8) | 5 (33.3) | 5 (35.7) | 46 (43.8) | 27 (29.3) | 14 (58) | 18 (78) |
| Any antiviralc | 6 (86) | 10 (83) | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | 24 (100) | 23 (100) |
| Remdesivir | Not recorded | Not recorded | 0 | 0 | 1 (0.3) | 0 | 1 (1.3) | 0 | 0 | 4 (28.6) | 1 (1.0) | 0 | Not recorded | Not recorded |
| Lopinavir or ritonavir | Not recorded | Not recorded | 0 | 1 (0.8) | 0 | 0 | 8 (10.5) | 9 (12.3) | 0 | 0 | 0 | 2 (2.2) | Not recorded | Not recorded |
| Favipravir | Not recorded | Not recorded | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | Not recorded | Not recorded |
| Hydroxychloroquine | 7 (100) | 12 (100) | 30 (23.4) | 22 (17.2) | 0 | 0 | 29 (38.2) | 32 (43.8) | 1 (6.7) | 0 | 5 (4.8) | 2 (2.2) | 0 | 0 |
| Azithromycin | 0 | 0 | 83 (64.8) | 81 (63.3) | 59 (18.2) | 81 (11.9) | 19 (25.0) | 24 (32.9) | Not recorded | Not recorded | 9 (8.6) | 6 (6.5) | Not recorded | Not recorded |
| Convalescent plasma | 0 | 0 | Not recorded | Not recorded | 0 | 0 | 0 | 0 | 0 | 2 (14.3) | 0 | 0 | Not recorded | Not recorded |
Abbreviations: CAPE COVID, Community-Acquired Pneumonia: Evaluation of Corticosteroids in Coronavirus Disease; CoDEX, COVID-19 Dexamethasone; COVID STEROID, Hydrocortisone for COVID-19 and Severe Hypoxia; DEXA-COVID 19, Efficacy of Dexamethasone Treatment for Patients With ARDS Caused by COVID-19; IQR, interquartile range; NA, not applicable; PCR, polymerase chain reaction; RECOVERY, Randomized Evaluation of COVID-19 Therapy; REMAP-CAP, Randomized, Embedded, Multifactorial Adaptive Platform Trial for Community-Acquired Pneumonia; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; Steroids-SARI, Glucocorticoid Therapy for COVID-19 Critically Ill Patients With Severe Acute Respiratory Failure.
Missing substantial data on antiviral use.
Missing data on PCR results.
Some of the trials did not provide information on individual antiviral drugs, which is indicated by “not recorded.” The trials with NA is this row provided data on individual antiviral drugs in the rows below.
There were minimal missing outcome data. Follow-up was complete for both mortality and serious adverse events for 4 of the 7 trials. In the RECOVERY trial (NCT04381936), 1 patient who received invasive mechanical ventilation (of 1007) in the corticosteroid group withdrew consent. In the CAPE COVID trial (NCT02517489), 1 patient (of 76) in the corticosteroid group withdrew consent. In the REMAP-CAP trial (NCT02735707), 5 patients (of 110) withdrew consent in the corticosteroid group and 6 patients (of 98) withdrew consent in the usual care group.
Association Between Corticosteroids and 28-Day All-Cause Mortality
Risk of bias was assessed as “low” for 6 of the 7 mortality results and as “some concerns” for the Steroids-SARI trial (NCT04244591; eTable 1 in the Supplement) because this trial used a fixed-randomization block size within centers and used text messages to implement randomization allocations. In the RECOVERY trial (NCT04381936), approximately 16% of patients in the control group received dexamethasone. This was regarded as reflecting usual practice,22 and was not considered to introduce a risk of bias in the effect of assignment to the intervention. Furthermore, any such bias would be toward the null.
There were 222 deaths among 678 patients randomized to corticosteroids and 425 deaths among 1025 patients randomized to usual care or placebo. Based on a fixed-effect meta-analysis, the summary OR was 0.66 (95% CI, 0.53-0.82; P < .001) for all-cause mortality comparing corticosteroids with usual care or placebo (Figure 2). This corresponds to an absolute mortality risk of 32% with corticosteroids compared with an assumed mortality risk of 40% with usual care or placebo. There was little inconsistency between the trial results (I2 = 15.6%; P = .31 for heterogeneity), and the summary OR was 0.70 (95% CI, 0.48-1.01; P = .053) based on a random-effects meta-analysis.
Figure 2. Association Between Corticosteroids and 28-Day All-Cause Mortality in Each Trial, Overall, and According to Corticosteroid Drug.

The area of the data marker for each trial is proportional to its weight in the fixed-effect meta-analysis. The Randomized Evaluation of COVID-19 Therapy (RECOVERY) trial result is for patients who were receiving invasive mechanical ventilation at randomization. CAPE COVID indicates Community-Acquired Pneumonia: Evaluation of Corticosteroids in Coronavirus Disease; CoDEX, COVID-19 Dexamethasone; COVID STEROID, Hydrocortisone for COVID-19 and Severe Hypoxia; DEXA-COVID 19, Efficacy of Dexamethasone Treatment for Patients With ARDS Caused by COVID-19; REMAP-CAP, Randomized, Embedded, Multifactorial Adaptive Platform Trial for Community-Acquired Pneumonia; Steroids-SARI, Glucocorticoid Therapy for COVID-19 Critically Ill Patients With Severe Acute Respiratory Failure.
aThe random-effects analysis estimates both the average and variability of effects across studies. The 95% CI for the average effect (shown here) is wide because there is a small number of studies, some of which have very small sample size. The prespecified primary analysis was the fixed-effect analysis, which should be used to guide clinical interpretation of the results.
In the analysis that excluded patients recruited to the RECOVERY trial, the OR was 0.77 (95% CI, 0.56-1.07) for all-cause mortality comparing corticosteroids with usual care or placebo, which was consistent with the corresponding result based on patients in the RECOVERY trial who were receiving invasive mechanical ventilation at randomization (OR, 0.59 [95% CI, 0.44-0.78]). This latter OR was not adjusted for age and therefore differs from the age-adjusted rate ratio in the report of the RECOVERY trial.7
The overall inverse variance–weighted fixed-effect risk ratio was 0.80 (95% CI, 0.70-0.91) for all-cause mortality comparing corticosteroids with usual care or placebo. The GRADE assessment of the certainty of the evidence that corticosteroids reduce all-cause mortality in critically ill patients with COVID-19 was moderate due to minor concerns across (1) imprecision, (2) a small amount of heterogeneity, and (3) a small risk of reporting bias due to some trials not responding to the requests for data.
For all-cause mortality comparing corticosteroids vs usual care or placebo, the fixed-effect summary OR was 0.64 (95% CI, 0.50-0.82; P < .001) for trials of dexamethasone (3 trials, 1282 patients, and 527 deaths; corresponding absolute risk of 30% for dexamethasone vs an assumed risk of 40% for usual care or placebo) and the OR was 0.69 (95% CI, 0.43-1.12; P = .13) for trials of hydrocortisone (3 trials, 374 patients, and 94 deaths; corresponding absolute risk of 32% for hydrocortisone vs an assumed risk of 40% for usual care or placebo). Using meta-regression to compare the associations for hydrocortisone and dexamethasone, the ratio of ORs was 1.06 (95% CI, 0.37-2.99). From the random-effects meta-analyses, the OR was 0.65 (95% CI, 0.36-1.17) for dexamethasone and the OR was 0.87 (95% CI, 0.072-10.5) for hydrocortisone; the wide 95% CIs reflect the imprecisely estimated between-trial variance because each analysis included only 3 trials. Only 1 trial (NCT04244591), which enrolled 47 patients of whom 26 died, evaluated methylprednisolone and the OR was 0.91 (95% CI, 0.29, 2.87; P = .87) for the association between methylprednisolone and all-cause mortality.
In trials that administered low doses of corticosteroids, the overall fixed-effect OR was 0.61 (95% CI, 0.48-0.78; P < .001) and the corresponding absolute risk was 29% for low-dose corticosteroids vs an assumed risk of 40% for usual care or placebo. In trials that administered high doses of corticosteroids, the fixed-effect OR was 0.83 (95% CI, 0.53-1.29; P = .46) and the corresponding absolute risk was 36% for high-dose corticosteroids vs an assumed risk of 40% for usual care or placebo. The ratio of ORs was 1.38 (95% CI, 0.69-2.79; P = .29). For trials that administered low-dose corticosteroids, the random-effects OR was 0.80 (95% CI, 0.063-10.32; P = .75). For trials that administered high-dose corticosteroids, the fixed-effect and random-effects estimates were identical (I2 = 0%).
We identified 1 additional trial, the Methylprednisolone in the Treatment of Patients With Signs of Severe Acute Respiratory Syndrome in Covid-19 (Metcovid; NCT04343729),23 when it was published on August 12, 2020 (eTables 2 and 3 in the Supplement); this trial had been registered after the searches of trial registries had been conducted. In this trial, 416 hospitalized patients with suspected SARS-CoV-2 infection were randomized to receive high-dose methylprednisolone or placebo. The risk of bias in the effect of assignment to intervention on 28-day mortality was assessed as “low” (eTable 4 in the Supplement). In an additional meta-analysis that included patients (71 in the steroid group and 70 in the no steroid group) from the Metcovid trial who were receiving invasive mechanical ventilation at randomization (based on an intention-to-treat analysis), the fixed-effect OR was 0.66 (95% CI, 0.54-0.82; P < .001) for the association between corticosteroids and 28-day mortality (eFigure 6 in the Supplement). There was little inconsistency among the trials (random-effects OR, 0.67 [95% CI, 0.51-0.87]; P = .009 and I2 = 2.4%). For the association between methylprednisolone and 28-day mortality, the fixed-effect OR was 0.80 (95% CI, 0.40-1.63; P = .54).
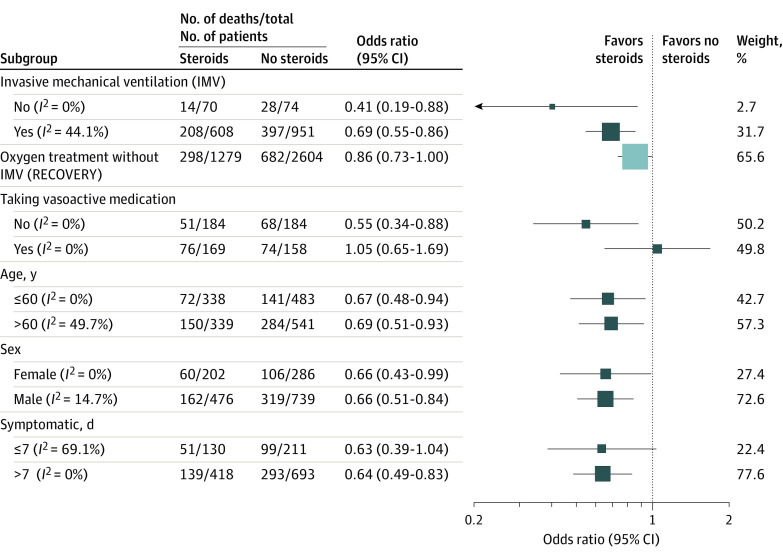
Association Between Corticosteroids and 28-Day All-Cause Mortality Within Subgroups
The estimated associations between corticosteroids vs usual care or placebo and mortality in the subgroups defined by patient characteristics at randomization appear in Figure 3. Among critically ill patients, many more were receiving invasive mechanical ventilation at randomization (1459 patients and 604 deaths) than were not (144 patients and 42 deaths). The overall fixed-effect OR was 0.69 (95% CI, 0.55-0.86) among patients who were receiving invasive mechanical ventilation at randomization (corresponding to an absolute risk of 30% for corticosteroids vs 38% for usual care or placebo) and the OR was 0.41 (95% CI, 0.19-0.88) among patients who were not receiving invasive mechanical ventilation at randomization (corresponding to an absolute risk of 23% for corticosteroids vs 42% for usual care or placebo). For comparison, the OR was 0.86 (95% CI, 0.73-1.00) among 3883 patients in the RECOVERY trial who required oxygen with or without noninvasive ventilation but were not receiving invasive mechanical ventilation at randomization.7
Figure 3. Association Between Corticosteroids and 28-Day All-Cause Mortality Within Subgroups Defined by Patient Characteristics at the Time of Randomization.
The area of the data markers is proportional to their weight in the meta-analysis. The estimated odds ratios were derived using fixed-effect meta-analyses across all trials for which data on the specified subgroup were available. The results for patients in the Randomized Evaluation of COVID-19 Therapy (RECOVERY) trial who required oxygen with or without noninvasive ventilation but were not receiving invasive mechanical ventilation at randomization is shown in a light blue box because these data were not otherwise included in this prospective meta-analysis.
Among the 4 trials that recruited critically ill patients who were and were not receiving invasive mechanical ventilation at randomization, the association between corticosteroids and lower mortality was less marked in patients receiving invasive mechanical ventilation (ratio of ORs, 4.34 [95% CI, 1.46-12.91]; P = .008 based on within-trial estimates combined across trials; eFigure 1 in the Supplement); however, only 401 patients (120 deaths) contributed to this comparison.
Among 695 patients from 6 trials for whom data were available, 327 (47.0%) were receiving vasoactive agents for blood pressure support at randomization. For the association between corticosteroids and mortality, the OR was 1.05 (95% CI, 0.65-1.69) among patients who were receiving vasoactive agents at randomization (an absolute risk of 48% for corticosteroids vs 47% for usual care or placebo) and the OR was 0.55 (95% CI, 0.34-0.88) among patients who were not receiving vasoactive agents at randomization (an absolute risk of 24% for corticosteroids vs 37% for usual care or placebo). The ratio of ORs was 1.90 (95% CI, 0.97-3.73, P = .06; eFigure 2 in the Supplement).
All trials contributed data according to age group and sex. For the association between corticosteroids and mortality, the OR was 0.69 (95% CI, 0.51-0.93) among 880 patients older than 60 years, the OR was 0.67 (95% CI, 0.48-0.94) among 821 patients aged 60 years or younger (ratio of ORs, 1.02 [95% CI, 0.63-1.65], P = .94; eFigure 3 in the Supplement), the OR was 0.66 (95% CI, 0.51-0.84) among 1215 men, and the OR was 0.66 (95% CI, 0.43-0.99) among 488 women (ratio of ORs, 1.07 [95% CI, 0.58-1.98], P = .84; eFigure 4 in the Supplement). For the association between corticosteroids and mortality based on data from 4 trials, the OR was 0.64 (95% CI, 0.49-0.83) among 1111 patients who were symptomatic for more than 7 days prior to randomization and the OR was 0.63 (95% CI, 0.39-1.04) among 341 patients who were symptomatic for 7 days or less prior to randomization (ratio of ORs, 1.07 [95% CI, 0.40-2.81], P = .90; eFigure 5 in the Supplement).
Serious Adverse Events
The RECOVERY trial did not record serious adverse events. The Steroids-SARI trial (NCT04244591) recorded adverse events but did not categorize them as serious or nonserious adverse events. Risk of bias was assessed as “low” in 2 of the 6 available trial results for serious adverse events (eTable 1 in the Supplement). In these trials, the study personnel were blinded to the intervention group. The other 4 trials had unblinded outcome assessment, and the risk of bias was assessed as “some concerns” based on subjectivity implying that classification of serious adverse events could differ between intervention groups.
The associations between corticosteroids vs usual care or placebo and serious adverse events in each trial appear in Figure 4. Among the 6 trials that reported serious adverse events, 64 events occurred among 354 patients randomized to corticosteroids and 80 events occurred among 342 patients randomized to usual care or placebo. Adverse events varied across trials but there was no suggestion that the risk of serious adverse events was higher in patients assigned to corticosteroids except for the 2 smallest trials, in which the total number of serious adverse events was 1 and 3.
Figure 4. Association Between Corticosteroids and Serious Adverse Events in Each Trial.

The area of the data markers is proportional to the inverse of the variance of the estimated odds ratio. CAPE COVID indicates Community-Acquired Pneumonia: Evaluation of Corticosteroids in Coronavirus Disease; CoDEX, COVID-19 Dexamethasone; COVID STEROID, Hydrocortisone for COVID-19 and Severe Hypoxia; DEXA-COVID 19, Efficacy of Dexamethasone Treatment for Patients With ARDS Caused by COVID-19; REMAP-CAP, Randomized, Embedded, Multifactorial Adaptive Platform Trial for Community-Acquired Pneumonia; Steroids-SARI, Glucocorticoid Therapy for COVID-19 Critically Ill Patients With Severe Acute Respiratory Failure. The Steroids-SARI trial recorded adverse events but did not categorize them as serious or nonserious.
Discussion
In this prospective meta-analysis of 7 randomized clinical trials that included 1703 critically ill patients with COVID-19 recruited from countries on 5 continents, administration of corticosteroids was associated with lower all-cause mortality at 28 days after randomization. There was no suggestion of an increased risk of serious of adverse events. The ORs for the association between corticosteroids and mortality were similar for dexamethasone and hydrocortisone. The comparison of the association between low-dose corticosteroids and mortality and the association between high-dose corticosteroids and mortality was imprecisely estimated.
Corticosteroids were associated with lower mortality among critically ill patients who were and were not receiving invasive mechanical ventilation at randomization, as well as in patients from the RECOVERY trial who required oxygen with or without noninvasive ventilation but were not receiving invasive mechanical ventilation at randomization. These results were consistent with the subgroup analysis suggesting that the association between corticosteroids and lower mortality was stronger in patients who were not receiving vasoactive medication at randomization than in those who were receiving vasoactive medication at randomization. The ORs for the association between corticosteroids and mortality appeared similar for older and younger individuals, men and women, and for longer and shorter durations of symptoms before randomization.
This analysis was expedited because of the release of results from the RECOVERY trial, which found that the absolute risk of death was reduced by 12.1% among those assigned to low-dose dexamethasone who were receiving invasive mechanical ventilation at randomization. Most ongoing trials of corticosteroids in critically ill patients with COVID-19 suspended enrollment after these results became publicly available because equipoise for withholding corticosteroids was no longer present. These trial results from diverse clinical and geographic settings suggest that in the absence of compelling contraindications, a corticosteroid regimen should be a component of standard care for critically ill patients with COVID-19.
The optimal dose and duration of treatment could not be assessed in this analysis, but there was no evidence suggesting that a higher dose of corticosteroids was associated with greater benefit than a lower dose of corticosteroids. Inclusion of data from the Metcovid trial did not materially change the results other than reducing the inconsistency among the trials. Data from the Metcovid trial were not included in the primary meta-analysis because this trial was registered after the searches of the trial registries were conducted.
All subgroup analyses other than that comparing longer with shorter duration of symptoms at randomization were prespecified. Although the benefit associated with corticosteroids appeared greater in critically ill patients who were not receiving invasive mechanical ventilation at randomization, this comparison was based on only 4 trials and 144 patients who were not receiving invasive mechanical ventilation at randomization, of whom 42 died. Corticosteroids were associated with lower mortality in critically ill patients who were and were not receiving invasive mechanical ventilation at randomization, as well as in patients in the RECOVERY trial who required oxygen with or without noninvasive ventilation but were not receiving invasive mechanical ventilation at randomization.7 It was not possible to classify this latter group according to whether they were critically ill at the time of randomization. These patients represented a spectrum of illness from patients receiving supplemental oxygen by nasal prongs to those receiving noninvasive ventilatory support in the form of high-flow oxygen or positive pressure by mask. Nonetheless, the substantial risk of death in these patients (682/2604 [26.1%] in the control group) is consistent with mortality in critically ill patients with COVID-19.24,25
The findings from this prospective meta-analysis provide evidence that treatment with corticosteroids is associated with reduced mortality for critically ill patients with COVID-19. The findings contrast with outcomes reported for the administration of corticosteroids among patients with influenza, for whom mortality and hospital-acquired infections may be increased by the administration of corticosteroids.26 In the current study, potential corticosteroid–induced complications could not be analyzed reliably because of limitations of the available data (serious adverse events were reported by only 6 of the 7 trials, and their definitions and methods of assessment varied among trials). However, serious adverse events were generally less likely in patients randomized to corticosteroids than to usual care or placebo.
This prospective meta-analysis was based on a relatively large number of critically ill patients with COVID-19 from geographically diverse sites who were randomized to receive corticosteroids or to receive usual care or placebo. The protocol and analysis plan, including specification of subgroup analyses, was registered and made publicly available on the PROSPERO database prior to data analysis or receipt of outcome data. The protocol also has been published along with a structured abstract.8 Provision of pooled data in prespecified subgroups facilitated rapid analysis and dissemination because a need for multiple data-sharing agreements was avoided. As is standard in meta-analyses, patients were compared only with other patients randomized in the same trial. Therefore, observed associations support a causal relationship between the administration of corticosteroids, compared with usual care or placebo, and reduced mortality.
Limitations
This study has several limitations. First, the prospective nature of this meta-analysis implies that there is little risk of selective reporting or of publication bias,6 but it is possible that lack of participation by some investigators of ongoing trials was based on their knowledge of their trial results. Nonetheless, the number of patients randomized in eligible trials who did not participate is likely to be smaller than the number of patients included in this meta-analysis.
Second, all but 1 of the included trials was assessed as “low risk” of bias for the effect of assignment to the intervention. The trial for which the risk of bias was assessed as “some concerns” (Steroids-SARI; NCT04244591) was relatively small (47 patients and 26 deaths) and contributed only 3.5% of the weight in the primary meta-analysis. It was the only trial that assessed the effect of methylprednisolone.
Third, there were only limited missing outcome data, but in many trials, follow-up was censored when participants were discharged from the hospital. We are aware of no reason that the effect of corticosteroids on postdischarge 28-day mortality would differ from that on predischarge mortality, but it will be important to report on longer-term mortality, including postdischarge mortality, in future analyses.
Fourth, the definitions and reporting of serious adverse events were not consistent across the trials and therefore a meta-analysis for this secondary end point was not conducted.
Fifth, the trials only recruited adults, and the effect of corticosteroids on children remains unclear. Similarly, the trials were mainly conducted in high-income settings.
Sixth, 1 trial reported mortality at 21 days and 1 trial reported mortality at 30 days after randomization, potentially leading to inconsistency between trial results.
Seventh, the RECOVERY trial contributed 57% of the weight in the primary meta-analysis of 28-day all-cause mortality, although there was little inconsistency between the effects of corticosteroids on 28-day mortality estimated by the different trials.
Conclusions
In this prospective meta-analysis of clinical trials of critically ill patients with COVID-19, administration of systemic corticosteroids, compared with usual care or placebo, was associated with lower 28-day all-cause mortality.
Lists of investigators and steering committee
eTable 1. Summary of assessments of the risk of bias in the estimated effect of corticosteroids on mortality and serious adverse events in each trial, with brief explanation of judgements
eTable 2. Characteristics of the METCOVID trial
eTable 3. Characteristics of patients included in the METCOVID trial
eTable 4. Summary of assessments of the risk of bias in the estimated effect of corticosteroids on mortality in the METCOVID trial
eFigure 1. Effects of corticosteroids on 28-day mortality according to whether patients received invasive mechanical ventilation (IMV) at the time of randomization
eFigure 2. Effects of corticosteroids on 28-day mortality according to whether patients received vasoactive medication at the time of randomization
eFigure 3. Effects of corticosteroids on 28-day mortality according to whether patients were aged ≤60 or >60 years at the time of randomization
eFigure 4. Effects of corticosteroids on 28-day mortality according to sex. Left plot: odds ratio (95% CI) in females and males in each trial
eFigure 5. Effects of corticosteroids on 28-day mortality according to duration of symptoms (≤7 days or >7 days) at the time of randomization, for the four trials that recorded this information
eFigure 6. Additional forest plot showing the association of corticosteroids with all-cause 28-day mortality in each trial including the METCOVID trial, overall and according to corticosteroid drug
References
- 1.Dale DC, Petersdorf RG. Corticosteroids and infectious diseases. Med Clin North Am. 1973;57(5):1277-1287. [DOI] [PubMed] [Google Scholar]
- 2.Annane D, Bellissant E, Bollaert PE, et al. . Corticosteroids in the treatment of severe sepsis and septic shock in adults. JAMA. 2009;301(22):2362-2375. [DOI] [PubMed] [Google Scholar]
- 3.Annane D, Bellissant E, Bollaert PE, et al. . Corticosteroids for treating sepsis in children and adults. Cochrane Database Syst Rev. 2019;12:CD002243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Russell CD, Millar JE, Baillie JK. Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury. Lancet. 2020;395(10223):473-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Villar J, Confalonieri M, Pastores SM, Meduri GU. Rationale for prolonged corticosteroid treatment in the acute respiratory distress syndrome caused by coronavirus disease 2019. Crit Care Explor. 2020;2(4):e0111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thomas J, Askie LM, Berlin JA, et al. Chapter 22: prospective approaches to accumulating evidence. Accessed August 24, 2020. http://www.training.cochrane.org/handbook doi: 10.1002/9781119536604.ch22 [DOI]
- 7.Horby P, Lim WS, Emberson JR, et al. ; RECOVERY Collaborative Group . Dexamethasone in hospitalized patients with Covid-19—preliminary report. N Engl J Med. Published online July 17, 2020. doi: 10.1056/NEJMoa2021436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sterne JAC, Diaz J, Villar J, et al. . Corticosteroid therapy for critically ill patients with COVID-19. Trials. Published online August 24, 2020. doi: 10.1186/s13063-020-04641-3 [DOI] [Google Scholar]
- 9.Ranieri VM, Rubenfeld GD, Thompson BT, et al. . Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526-2533. [DOI] [PubMed] [Google Scholar]
- 10.Dequin PF, Heming N, Meziani F, et al. . Effect of hydrocortisone on 21-day mortality or respiratory support among critically ill patients with COVID-19: a randomized clinical trial. JAMA. Published online September 2, 2020. doi: 10.1001/jama.2020.16761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sterne JAC, Savović J, Page MJ, et al. . RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 12.Guyatt GH, Oxman AD, Vist GE, et al. . GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924-926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Annane D, Pastores SM, Rochwerg B, et al. . Guidelines for the diagnosis and management of critical illness-related corticosteroid insufficiency (CIRCI) in critically ill patients (part I). Intensive Care Med. 2017;43(12):1751-1763. [DOI] [PubMed] [Google Scholar]
- 14.Paule RC, Mandel J. Consensus values and weighting factors. J Res. 1982;87(5):377–385. doi: 10.6028/jres.087.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Langan D, Higgins JPT, Simmonds M. Comparative performance of heterogeneity variance estimators in meta-analysis. Res Synth Methods. 2017;8(2):181-198. [DOI] [PubMed] [Google Scholar]
- 16.Hartung J, Knapp G. A refined method for the meta-analysis of controlled clinical trials with binary outcome. Stat Med. 2001;20(24):3875-3889. [DOI] [PubMed] [Google Scholar]
- 17.IntHout J, Ioannidis JP, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol. 2014;14:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fisher DJ, Carpenter JR, Morris TP, Freeman SC, Tierney JF. Meta-analytical methods to identify who benefits most from treatments. BMJ. 2017;356:j573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Angus DC, Berry S, Lewis RJ, et al. . The REMAP-CAP (Randomized Embedded Multifactorial Adaptive Platform for Community-acquired Pneumonia) study. Ann Am Thorac Soc. 2020;17(7):879-891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The Writing Committee for the REMAP-CAP Investigators Effect of hydrocortisone on mortality and organ support in patients with severe COVID-19: the REMAP-CAP COVID-19 Corticosteroid Domain randomized clinical trial. JAMA. Published online September 2, 2020. doi: 10.1001/jama.2020.17022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tomazini BM, Maia IS, Cavalcanti AB, et al. . Effect of dexamethasone on days alive and ventilator-free in patients with moderate or severe acute respiratory distress syndrome and COVID-19: the CoDEX randomized clinical trial. JAMA. Published online September 2, 2020. doi: 10.1001/jama.2020.17021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.International Severe Acute Respiratory and Emerging Infections Consortium COVID-19 report: 13 July 2020. Accessed August 11, 2020. https://media.tghn.org/medialibrary/2020/07/ISARIC_Data_Platform_COVID-19_Report_13JUL20.pdf
- 23.Jeronimo CMP, Farias MEL, Val FFA, et al. . Methylprednisolone as adjunctive therapy for patients hospitalized with COVID-19 (Metcovid). Clin Infect Dis. Published online August 12, 2020. doi: 10.1093/cid/ciaa1177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Docherty AB, Harrison EM, Green CA, et al. . Features of 20 133 UK patients in hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol. BMJ. 2020;369:m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abate SM, Ahmed Ali S, Mantfardo B, Basu B. Rate of intensive care unit admission and outcomes among patients with coronavirus. PLoS One. 2020;15(7):e0235653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lansbury LE, Rodrigo C, Leonardi-Bee J, et al. . Corticosteroids as adjunctive therapy in the treatment of influenza. Crit Care Med. 2020;48(2):e98-e106. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Lists of investigators and steering committee
eTable 1. Summary of assessments of the risk of bias in the estimated effect of corticosteroids on mortality and serious adverse events in each trial, with brief explanation of judgements
eTable 2. Characteristics of the METCOVID trial
eTable 3. Characteristics of patients included in the METCOVID trial
eTable 4. Summary of assessments of the risk of bias in the estimated effect of corticosteroids on mortality in the METCOVID trial
eFigure 1. Effects of corticosteroids on 28-day mortality according to whether patients received invasive mechanical ventilation (IMV) at the time of randomization
eFigure 2. Effects of corticosteroids on 28-day mortality according to whether patients received vasoactive medication at the time of randomization
eFigure 3. Effects of corticosteroids on 28-day mortality according to whether patients were aged ≤60 or >60 years at the time of randomization
eFigure 4. Effects of corticosteroids on 28-day mortality according to sex. Left plot: odds ratio (95% CI) in females and males in each trial
eFigure 5. Effects of corticosteroids on 28-day mortality according to duration of symptoms (≤7 days or >7 days) at the time of randomization, for the four trials that recorded this information
eFigure 6. Additional forest plot showing the association of corticosteroids with all-cause 28-day mortality in each trial including the METCOVID trial, overall and according to corticosteroid drug