Abstract
The nature and prevalence of combinations of mental disorders and their associations with premature mortality have never been reported in a comprehensive way. We describe the most common combinations of mental disorders and estimate excess mortality associated with these combinations. We designed a population‐based cohort study including all 7,505,576 persons living in Denmark at some point between January 1, 1995 and December 31, 2016. Information on mental disorders and mortality was obtained from national registers. A total of 546,090 individuals (10.5%) living in Denmark on January 1, 1995 were diagnosed with at least one mental disorder during the 22‐year follow‐up period. The overall crude rate of diagnosis of mental disorders was 9.28 (95% CI: 9.26‐9.30) per 1,000 person‐years. The rate of diagnosis of additional mental disorders was 70.01 (95% CI: 69.80‐70.26) per 1,000 person‐years for individuals with one disorder already diagnosed. At the end of follow‐up, two out of five individuals with mental disorders were diagnosed with two or more disorder types. The most prevalent were neurotic/stress‐related/somatoform disorders (ICD‐10 F40‐F48) and mood disorders (ICD‐10 F30‐F39), which – alone or in combination with other disorders – were present in 64.8% of individuals diagnosed with any mental disorder. Mortality rates were higher for people with mental disorders compared to those without mental disorders. The highest mortality rate ratio was 5.97 (95% CI: 5.52‐6.45) for the combination of schizophrenia (ICD‐10 F20‐F29), neurotic/stress‐related/somatoform disorders and substance use disorders (ICD‐10 F10‐F19). Any combination of mental disorders was associated with a shorter life expectancy compared to the general Danish population, with differences in remaining life expectancy ranging from 5.06 years (95% CI: 5.01‐5.11) to 17.46 years (95% CI: 16.86‐18.03). The largest excess mortality was observed for combinations that included substance use disorders. This study reports novel estimates related to the “force of comorbidity” and provides new insights into the contribution of substance use disorders to premature mortality in those with comorbid mental disorders.
Keywords: Mental disorders, comorbidity, mortality, life expectancy, substance use disorders, mood disorders, neurotic/stress‐related/somato‐form disorders, schizophrenia
It has long been recognized that individuals with a mental disorder are at increased risk of subsequently developing other mental disorders 1 . In a recent study based on comprehensive Danish registers, we demonstrated the pervasive nature of comorbidity within mental disorders by showing that individuals with any type of psychiatric diagnosis were at increased risk for subsequently developing all other types of mental disorders 2 . In that study, we restricted the analyses to pairs of disorders. This simplifying assumption made the analyses more tractable, but ignored the fact that some individuals will have three or more types of mental disorders.
While statistical methods have provided insights into the patterns of comorbidity (e.g., internalizing and externalizing disorders as defined by latent class analysis)3, 4, the nature and prevalence of combinations of mental disorders have not previously been described in a comprehensive way. Groups of disorders can be considered in temporally‐ordered sets (i.e., permutations) or sets that occurred during a period of observation regardless of temporal order (i.e., combinations). To keep the analysis of comorbidity tractable, we chose to explore combinations of mental disorders regardless of temporal order. Actually, our previous research 2 found that, for pairs of mental disorders with comparable ages of onset (e.g., depression and anxiety disorders) 5 , the risk of comorbidity was often symmetrical, regardless of which disorder came first.
It is clear that mental disorders are associated with premature mortality6, 7, 8. However, mortality‐related metrics such as mortality rate ratios are usually shown for single types of mental disorders9, 10, or broad categories of mental disorders 7 . While it is useful to compare these estimates across mental disorders, and some models adjust for prior mental disorders 11 , such studies have not captured the complex nature of comorbidity and its potential impact on mortality.
Based on the types of mental disorders included in the Global Burden of Disease study, we have recently demonstrated that those with two or more types of mental disorders have a shorter life expectancy (i.e., more life‐years lost) compared to those with one type of mental disorder 12 . There is a need to more precisely map the associations between specific combinations of mental disorders and excess mortality.
We had the opportunity to explore the above‐mentioned research questions using high quality Danish registers. The aims of the current study were to: a) describe the rate of accumulation of mental disorders over time; b) explore the prevalence and demographic correlates of combinations of mental disorders; c) estimate the mortality rate ratio for these combinations; and d) estimate the reduction in life expectancy for each mental disorder set.
Based on our previous observations that common disorders such as mood disorders, neurotic/stress‐related/somatoform disorders and substance use disorders were each associated with appreciable risks of developing a range of other disorders 2 , we predicted that these disorders would be found in many common combinations. Furthermore, since we estimated that substance use disorders were strongly associated with premature mortality (when looking both at mortality rates and life expectancy) 7 , and that life expectancy was shorter for those with two or more types of mental disorders 12 , we predicted that combinations including substance use disorders or a larger number of disorders would be associated with greater risk of premature mortality.
METHODS
Study population
We defined two population‐based cohorts – one dynamic and one fixed – in order to optimize the analyses of the key research questions in this study.
The dynamic cohort included all 7,505,576 persons younger than 95 years living in Denmark at some point between January 1, 1995 and December 31, 2016. Each individual in the study was followed from birth, immigration to Denmark, or January 1, 1995 (whichever happened last) until death, emigration from Denmark, 95th birthday, or December 31, 2016 (whichever happened first).
The fixed cohort comprised a subset of the dynamic cohort. More specifically, it included all 5,205,859 individuals living in Denmark on January 1, 1995 (thus, it did not include those born in or immigrating to Denmark after that date).
All data were obtained from the Danish Civil Registration System 13 , which has maintained information on all residents since 1968, including sex, date of birth, continuously updated information on vital status, and a unique personal identification number that can be used to link information from various national registries.
Assessment of mental disorders
Information on mental disorders was obtained from the Danish Psychiatric Central Research Register 14 , which contains data on all admissions to psychiatric inpatient facilities since 1969 and all visits to outpatient psychiatric departments and emergency departments since 1995.
The diagnostic system used was the Danish modification of the ICD‐8 from 1969 to 1993, and of the ICD‐10 from 1994 onwards. In order to make the analyses tractable, and to avoid identified comorbidity within broad domains (e.g., several types of anxiety disorders or substance use disorders), we used the ICD‐10 subchapter categories considered in previous publications based on Danish registers2, 3: organic, including symptomatic, mental disorders (F00‐F09); mental and behavioral disorders due to psychoactive substance use (substance use disorders) (F10‐F19); schizophrenia and related disorders (F20‐F29); mood disorders (F30‐F39); neurotic, stress‐related and somatoform disorders (F40‐F48); eating disorders (F50); personality disorders (F60); intellectual disabilities (F70‐F79); pervasive developmental disorders (F84); and behavioral and emotional disorders with onset usually occurring in childhood and adolescence (here abbreviated as “behavioral disorders”) (F90‐F98).
For each individual in the study, the date of onset for each disorder was defined as the date of first contact with the psychiatric care system.
Statistical analysis
Prevalence estimates and demographic correlates of all combinations of mental disorders were calculated using the fixed cohort of individuals living in Denmark on January 1, 1995, who had 22 years of follow‐up (unless censored due to death or emigration). This was done to allow for accumulation of comorbidity over time, and measurement of demographic correlates on the same date (which would not have been possible with the dynamic cohort).
We described the rate and number of different mental disorders diagnosed during the 22‐year period according to sex, country of birth (Denmark or others) and several baseline characteristics (each measured on January 1, 1995): age, gross yearly income, highest education achieved, and labour market affiliation 15 . Post‐hoc analyses compared the rate of diagnoses between different categories using Wald tests.
Results on mortality were based on the dynamic cohort (the fixed cohort of individuals living in Denmark on January 1, 1995 plus those born in or immigrating to Denmark between 1995 and 2016). We used the dynamic cohort to estimate mortality because time‐to‐event analyses can easily deal with dynamic cohorts, and the larger sample provided us with more precise estimates.
Each person was classified as experiencing a specific combination of mental disorders, with all disorders modelled as time‐varying variables 16 . Date of onset for a given combination of disorders was based on the date of diagnosis of the last of the disorders.
Mortality rate ratios (MRRs) with 95% confidence intervals (CIs) were estimated using Cox proportional hazards regression models, with age as the underlying time scale, and adjusting for sex and calendar time. Sex‐specific estimates were obtained by including an interaction term in the models.
In keeping with previous studies7, 8, 10, remaining life expectancy after onset of a combination of disorders compared to the general population of same sex and age was estimated as excess life‐years lost. The technical development of this method has recently been published8, 17, and a detailed account of how to implement it is available 18 . CIs for these estimates were obtained using non‐parametric bootstrap with 1,000 iterations.
All analyses were performed using R version 3.5.2. The Danish Data Protection Agency, Statistics Denmark, and the Danish Health Data Authority approved this study.
RESULTS
The fixed cohort of 5,205,859 Danish residents on January 1, 1995 (2,569,673 males and 2,636,186 females) was followed for 96.2 million person‐years, and the longest individual follow‐up period was 22 years (1995‐2016). Overall, 75% of persons were followed for at least 17.7 years.
During the follow‐up period, 546,090 persons (10.5%) were diagnosed with at least one mental disorder. The overall crude rate of diagnosis of mental disorders was 9.28 (95% CI: 9.26‐9.30) per 1,000 person‐years. The rate of mental disorders was lower among males compared to females, among individuals 45‐64 years old compared to other age groups, among those born in Denmark compared to those born elsewhere, among higher income vs. lower income and higher education vs. lower education groups, and among those employed vs. unemployed or otherwise outside the workforce (p<0.001 for all comparisons, see Table 1).
Table 1.
Diagnoses of mental disorders according to baseline characteristics of the fixed cohort (those living in Denmark on January 1, 1995)
| N | % | Follow‐up (millions of person‐years) | Rate of mental disorders per 1,000 person‐years | Number (%) of people receiving diagnoses of mental disorders in 1995‐2016 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Rate (95% CI) | p | No diagnosis | Exactly one | Exactly two | Exactly three | Four or more | ||||
| All persons | 5,205,859 | 100.0 | 96.2 | 9.28 (9.26‐9.30) | ‐ | 4,659,769 (89.5) | 322,715 (6.2) | 137,992 (2.7) | 57,052 (1.1) | 28,331 (0.5) |
| Gender | ||||||||||
| Females | 2,636,186 | 50.6 | 48.8 | 10.22 (10.19‐10.24) | Ref. | 2,329,457 (88.4) | 183,055 (6.9) | 76,453 (2.9) | 31,496 (1.2) | 15,725 (0.6) |
| Males | 2,569,673 | 49.4 | 47.4 | 8.32 (8.29‐8.34) | <0.001 | 2,330,312 (90.7) | 139,660 (5.4) | 61,539 (2.4) | 25,556 (1.0) | 12,606 (0.5) |
| Age in years | ||||||||||
| 0‐24 | 1,601,184 | 30.8 | 32.4 | 11.16 (11.13‐11.20) | Ref. | 1,400,078 (87.4) | 104,258 (6.5) | 54,490 (3.4) | 26,783 (1.7) | 15,575 (1.0) |
| 25‐44 | 1,546,373 | 29.7 | 31.7 | 8.15 (8.12‐8.18) | <0.001 | 1,397,201 (90.4) | 79,074 (5.1) | 42,451 (2.7) | 18,652 1.2) | 8,995 (0.6) |
| 45‐64 | 1,264,591 | 24.3 | 23.9 | 6.48 (6.45‐6.51) | <0.001 | 1,163,068 (92.0) | 64,262 (5.1) | 25,163 (2.0) | 8,834 (0.7) | 3,264 (0.3) |
| 65‐84 | 710,330 | 13.6 | 7.8 | 14.24 (14.15‐14.32) | <0.001 | 621,377 (87.5) | 70,455 (9.9) | 15,270 (2.1) | 2,739 (0.4) | 489 (0.1) |
| 85+ | 83,381 | 1.6 | 0.3 | 19.97 (19.47‐20.48) | <0.001 | 78,045 (93.6) | 4,666 (5.6) | 618 (0.7) | 44 (0.1) | 8 (0.0) |
| Country of birth | ||||||||||
| Denmark | 4,909,089 | 94.3 | 91.2 | 9.14 (9.12‐9.16) | Ref. | 4,398,470 (89.6) | 302,871 (6.2) | 128,048 (2.6) | 53,284 (1.1) | 26,416 (0.5) |
| Other | 279,953 | 5.4 | 4.8 | 11.96 (11.86‐12.06) | <0.001 | 246,092 (87.9) | 18,739 (6.7) | 9,563 (3.4) | 3,676 (1.3) | 1,883 (0.7) |
| Unknown | 16,817 | 0.3 | 0.2 | 9.45 (9.07‐9.85) | 0.109 | 15,207 (90.4) | 1,105 (6.6) | 381 (2.3) | 92 (0.5) | 32 (0.2) |
| Gross annual income | ||||||||||
| First tertile | 1,729,421 | 33.2 | 26.7 | 14.85 (14.80‐14.90) | Ref. | 1,482,786 (85.7) | 149,100 (8.6) | 61,036 (3.5) | 24,141 (1.4) | 12,358 (0.7) |
| Second tertile | 1,729,404 | 33.2 | 34.5 | 8.65 (8.62‐8.68) | <0.001 | 1,551,023 (89.7) | 101,624 (5.9) | 46,463 (2.7) | 20,268 (1.2) | 10,026 (0.6) |
| Third tertile | 1,729,407 | 33.2 | 34.6 | 5.58 (5.55‐5.60) | <0.001 | 1,610,373 (93.1) | 70,879 (4.1) | 29,868 (1.7) | 12,441 (0.7) | 5,846 (0.3) |
| No information | 17,627 | 0.30 | 0.2 | 14.00 (13.54‐14.48) | 0.001 | 15,587 (88.4) | 1,112 (6.3) | 625 (3.5) | 202 (1.1) | 101 (0.6) |
| Highest education achieved | ||||||||||
| Primary school | 1,501,845 | 28.8 | 27.9 | 11.63 (11.59‐11.67) | Ref. | 1,306,090 (87.0) | 113,138 (7.5) | 50,673 (3.4) | 21,054 (1.4) | 10,890 (0.7) |
| High school / vocational training | 2,044,183 | 39.3 | 40.9 | 8.10 (8.07‐8.13) | <0.001 | 1,846,787 (90.3) | 112,270 (5.5) | 51,436 (2.5) | 22,566 (1.1) | 11,124 (0.5) |
| Higher education | 1,161,094 | 22.3 | 22.9 | 7.20 (7.16‐7.23) | <0.001 | 1,062,171 (91.5) | 56,650 (4.9) | 25,734 (2.2) | 11,076 (1.0) | 5,463 (0.5) |
| No information | 498,737 | 9.6 | 4.4 | 16.12 (16.00‐16.24) | <0.001 | 444,721 (89.2) | 40,657 (8.2) | 10,149 (2.0) | 2,356 (0.5) | 854 (0.2) |
| Labour market affiliation | ||||||||||
| Employed | 3,197,123 | 61.4 | 65.2 | 6.41 (6.39‐6.43) | Ref. | 2,944,905 (92.1) | 145,423 (4.5) | 65,480 (2.0) | 28,088 (0.9) | 13,227 (0.4) |
| Unemployed | 324,286 | 6.2 | 6.5 | 12.80 (12.71‐12.88) | <0.001 | 277,111 (85.5) | 24,699 (7.6) | 13,152 (4.1) | 6,178 (1.9) | 3,146 (1.0) |
| Outside workforce for other reasons | 1,587,885 | 30.5 | 24.2 | 15.95 (15.90‐16.00) | <0.001 | 1,345,347 (84.7) | 149,862 (9.4) | 58,372 (3.7) | 22,492 (1.4) | 11,812 (0.7) |
| No information | 96,565 | 1.9 | 0.3 | 18.25 (17.80‐18.71) | <0.001 | 92,406 (95.7) | 2,731 (2.8) | 988 (1.0) | 294 (0.3) | 146 (0.2) |
The rate of diagnosis of additional mental disorders was 70.01 (95% CI: 69.80‐70.26) per 1,000 person‐years for individuals with one disorder already diagnosed. In those with two disorders, the rate of additional disorders was 63.70 (95% CI: 63.35‐64.06) per 1,000 person‐years. The rates of additional disorders dropped slightly to 55.33 (95% CI: 54.77‐55.89) and 45.48 (95% CI: 44.57‐46.42) for individuals diagnosed with three, or four or more disorders, respectively.
Mental disorders by count and type
During the 22‐year follow‐up period, the 546,090 persons with at least one disorder received in total 892,449 mental disorder diagnoses. At the end of follow‐up, there were 332,715 persons (6.2%) with exactly one disorder, 137,992 (2.7%) with exactly two, 57,052 (1.1%) with exactly three, and 28,331 (0.5%) with four or more mental disorders (see Table 1).
The 22‐year prevalence for all disorders is presented in Table 2 and Figure 1. The most prevalent mental disorders were neurotic/stress‐related/somatoform disorders (4.6% of the total population) and mood disorders (3.8% of the total population). Among individuals with at least one mental disorder, 43.5% had a neurotic/stress‐related/somatoform disorder and 36.6% had a mood disorder.
Table 2.
Mental disorders diagnosed in 1995‐2016 by type and count
| At least one (N=546,090; 10.5%) | Exactly one (N=322,715; 6.2%) | Exactly two (N=137,992; 2.6%) | Exactly three (N=57,052; 1.1%) | Four or more (N=28,331; 0.5%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diagnoses | % of total population | % of 1+ disorders | Diagnoses | % of 1 disorder | Diagnoses | % of 2 disorders | Diagnoses | % of 3 disorders | Diagnoses | % of 4+ disorders | ||
| Organic disorders | 111,575 | 2.1% | 20.4% | 76,503 | 23.7% | 22,694 | 16.4% | 7,694 | 13.5% | 4,684 | 16.5% | |
| Substance use disorders | 109,264 | 2.1% | 20.0% | 27,639 | 8.6% | 36,562 | 26.5% | 25,828 | 45.3% | 19,235 | 67.9% | |
| Schizophrenia | 73,131 | 1.4% | 13.4% | 19,884 | 6.2% | 22,852 | 16.6% | 15,654 | 27.4% | 14,741 | 52.0% | |
| Mood disorders | 199,701 | 3.8% | 36.6% | 67,267 | 20.8% | 71,825 | 52.1% | 38,356 | 67.2% | 22,253 | 78.5% | |
| Neurotic/stress‐related/somatoform disorders | 237,277 | 4.6% | 43.5% | 96,478 | 29.9% | 73,057 | 52.9% | 42,513 | 74.5% | 25,229 | 89.1% | |
| Eating disorders | 17,613 | 0.3% | 3.2% | 6,525 | 2.0% | 4,444 | 3.2% | 3,208 | 5.6% | 3,436 | 12.1% | |
| Personality disorders | 80,160 | 1.5% | 14.7% | 10,604 | 3.3% | 24,760 | 17.9% | 24,572 | 43.1% | 20,224 | 71.4% | |
| Intellectual disabilities | 15,387 | 0.3% | 2.8% | 3,200 | 1.0% | 5,963 | 4.3% | 3,352 | 5.9% | 2,872 | 10.1% | |
| Developmental disorders | 11,004 | 0.2% | 2.0% | 2,863 | 0.9% | 3,787 | 2.7% | 2,390 | 4.2% | 1,964 | 6.9% | |
| Behavioral disorders | 37,337 | 0.7% | 6.8% | 11,752 | 3.6% | 10,040 | 7.3% | 7,589 | 13.3% | 7,956 | 28.1% | |
| Total person‐diagnoses | 892,449 | 322,715 | 275,984 | 171,156 | 122,594 | |||||||
“Behavioral disorders” is an abbreviation for “behavioral and emotional disorders with onset usually occurring in childhood and adolescence”
Figure 1.
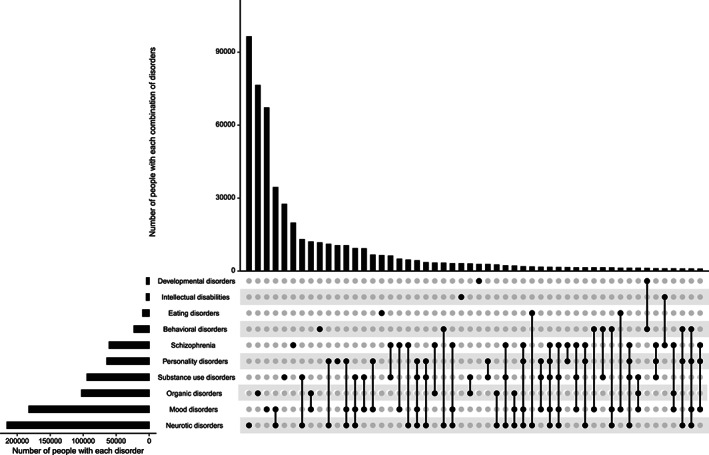
Combinations of mental disorders (with at least 1,000 people) diagnosed during the follow‐up period (1995‐2016); number of people diagnosed with each single disorder (horizontal bars); and number of people diagnosed with each combination of disorders (vertical bars). “Behavioral disorders” is an abbreviation for “behavioral and emotional disorders with onset usually occurring in childhood and adolescence”. “Neurotic disorders” is an abbreviation for “neurotic, stress‐related and somatoform disorders”.
Most common sets of mental disorders
We observed 616 out of 1,024 possible sets of disorders (210 combinations of disorders without considering time ordering). The 52 most common sets (with at least 1,000 individuals each), representing 92.8% of all persons with diagnosed mental disorders, are shown in Figure 1.
The three most common sets were composed of one disorder type (exactly‐one‐count sets): neurotic/stress‐related/somatoform disorders (N=96,478; 17.7% of the total 546,090 individuals with at least one diagnosis), organic disorders (N=76,503; 14.0%), and mood disorders (N=67,267; 12.3%).
The fourth most common set was comorbid mood and neurotic/stress‐related/somatoform disorders (which was also the most prevalent exactly‐two‐count set; N=34,504; 6.3%). The most common exactly‐three‐count set consisted of mood, neurotic/stress‐related/somatoform, and personality disorders (N=10,592; 1.9%). These three disorder types, in combination with substance use disorders, comprised the most common exactly‐four‐count set (N=4,414; 0.8%).
Indeed, mood and/or neurotic/stress‐related/somatoform disorders, alone or in combination with other disorders, were present in 64.8% of individuals diagnosed with any mental disorder. This percentage increased to 80.0% among individuals with exactly two disorders, 91.6% among those with three disorders, and 97.7% among those with four or more disorders.
Excess mortality associated with combinations of mental disorders
The dynamic cohort consisted of all 5,205,859 people from the fixed cohort along with an additional 2,299,717 people born in or immigrating to Denmark after January 1, 1995, resulting in a total of 7,505,576 individuals (3,742,852 males and 3,762,724 females) and 116.5 million person‐years of follow‐up.
Overall, 1,171,035 people (589,337 males and 581,698 females) died during the 22‐year observation period (15.6% of all males and females). Mortality rates were higher for people with any of the 52 most common combinations of mental disorders compared to those without mental disorders, except for those experiencing the combination of behavioral and pervasive developmental disorders (MRR 1.11, 95% CI: 0.67‐1.84). The highest MRR was 5.97 (95% CI: 5.52‐6.45) for the three‐disorder combination of schizophrenia, neurotic/stress‐related/somatoform disorders and substance use disorders (Figure 2).
Figure 2.
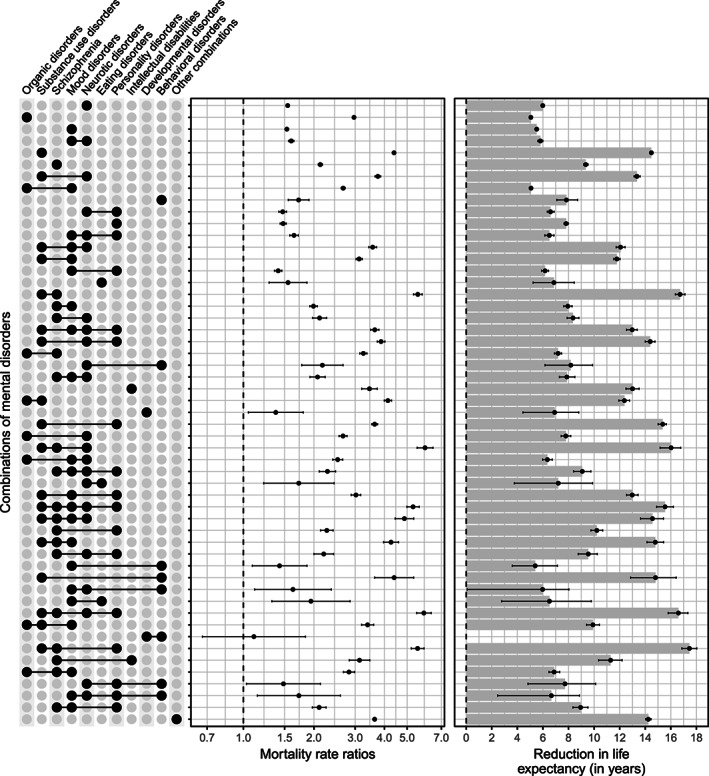
Mortality rate ratios comparing individuals experiencing each combination of mental disorders with individuals without any diagnosed disorder, adjusted for sex, age and calendar time; and reduction in life expectancy (in years) for individuals experiencing each combination of mental disorders compared to the general population of the same sex and age. The dashed line represents no excess mortality. “Behavioral disorders” is an abbreviation for “behavioral and emotional disorders with onset usually occurring in childhood and adolescence”. “Neurotic disorders” is an abbreviation for “neurotic, stress‐related and somatoform disorders”.
Each of the 52 combinations of mental disorders was associated with shorter life expectancy compared with the general population. The smallest difference in remaining life expectancy was observed for organic disorders: 5.06 years (95% CI: 5.01‐5.11). The largest difference in life expectancy was observed for those diagnosed with the three‐disorder combination of schizophrenia, personality disorders and substance use disorders: 17.46 years (95% CI: 16.86‐18.03) (see Figure 2).
Males had higher mortality rates and a larger reduction in life expectancy than females for several disorders (e.g., schizophrenia, mood disorders, neurotic/stress‐related/somatoform disorders, substance use disorders) and combinations of disorders (e.g., mood and neurotic/stress‐related/somatoform disorders; substance use and neurotic/stress‐related/somatoform disorders; mood and substance use disorders). Females did not have significantly higher mortality rates for any combination of disorders compared to males. However, among persons with pervasive developmental disorders alone, females had a larger reduction in life expectancy (see Figure 3).
Figure 3.
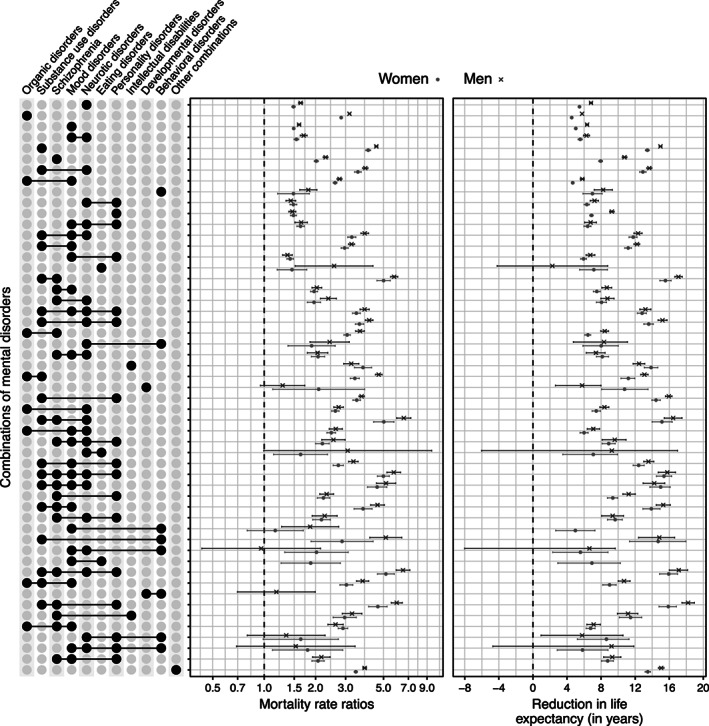
Sex‐specific mortality rate ratios comparing individuals experiencing each combination of mental disorders with individuals without any diagnosed disorder, adjusted for age and calendar time; and reduction in life expectancy (in years) for individuals experiencing each combination of mental disorders compared to the general population of the same sex and age. The dashed line represents no excess mortality. “Behavioral disorders” is an abbreviation for “behavioral and emotional disorders with onset usually occurring in childhood and adolescence”. “Neurotic disorders” is an abbreviation for “neurotic, stress‐related and somatoform disorders”.
The addition of comorbid schizophrenia and, especially, substance use disorders to any diagnosis or set of diagnoses was associated with increased mortality rates and reduced life expectancy across all combinations (see Figures 4 and 5). For example, individuals diagnosed with mood disorders alone experienced 1.5 times higher mortality rates than individuals without any diagnosis (MRR 1.53, 95% CI: 1.51‐1.55), while individuals diagnosed with mood and substance use disorders experienced three times higher mortality rates (MRR 3.12, 95% CI: 3.03‐3.22).
Figure 4.
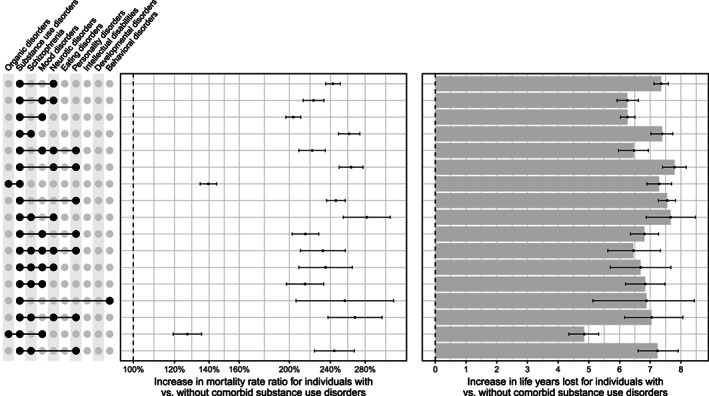
Increase in mortality rate ratio for individuals experiencing each combination of mental disorders with vs. without substance use disorders, adjusted for sex, age and calendar time; and increase in life years lost for individuals experiencing each combination of mental disorders with vs. without substance use disorders. The dashed line represents no excess mortality associated with the addition of substance use disorders to each combination of disorders. “Behavioral disorders” is an abbreviation for “behavioral and emotional disorders with onset usually occurring in childhood and adolescence”. “Neurotic disorders” is an abbreviation for “neurotic, stress‐related and somatoform disorders”.
Figure 5.
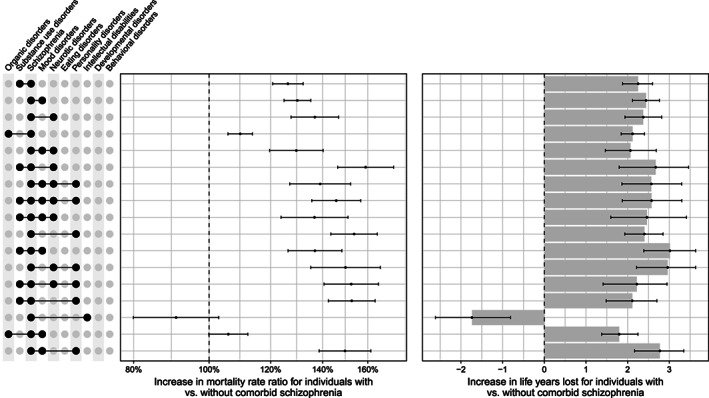
Increase in mortality rate ratio for individuals experiencing each combination of mental disorders with vs. without schizophrenia, adjusted for sex, age and calendar time; and increase in life years lost for individuals experiencing each combination of mental disorders with vs. without schizophrenia. The dashed line represents no excess mortality associated with the addition of schizophrenia to each combination of disorders. “Behavioral disorders” is an abbreviation for “behavioral and emotional disorders with onset usually occurring in childhood and adolescence”. “Neurotic disorders” is an abbreviation for “neurotic, stress‐related and somatoform disorders”.
DISCUSSION
In this study we describe the fine‐grained details of patterns of comorbidities within mental disorders, as well as the associations between these sets of mental disorders and subsequent mortality rates and life expectancy.
Overall, one in every 10 individuals received a diagnosis of at least one mental disorder during the 22‐year follow‐up period. Among those with mental disorders, about two out of five were diagnosed with two or more types. In keeping with prior studies based on latent class analyses4, 5, mood and neurotic/stress‐related/ somatoform disorders commonly co‐occurred, and contributed to many different sets of comorbid mental disorders.
Results regarding the accumulation of mental disorders showed that the rate of additional diagnoses after an initial diagnosis was higher than the overall rate of any diagnosis, demonstrating the “force of comorbidity”. The rates of additional diagnoses after two or more disorders was slightly lower, but still higher than the overall rate of any diagnosis.
Our study is the first to provide mortality estimates related to combinations of a comprehensive range of mental disorders. The associations between mental disorders and mortality highlight the prominent role of comorbid substance use disorders with respect to both elevated mortality rates and reduced life expectancy. These findings are in line with previous research9, 19, 20, 21 that observed higher mortality rates in patients with attention deficit/hyperactivity and other behavioral disorders, schizophrenia, bipolar disorder or depression, if they additionally experienced a comorbid substance use disorder.
Substance use disorders are relatively common3, 6, and we observed that these disorders often feature in combinations of mental disorders. Our previous research found that the risk of being diagnosed with substance use disorders was higher for those with other prior mental disorders 2 . For example, those diagnosed with a mood or neurotic/stress‐related/somatoform disorder were 10 and 12 times more likely to be subsequently diagnosed with substance use disorders, respectively; such that 13% were diagnosed with substance use disorders within 15 years after the first diagnosis of the mood or neurotic/stress‐related/somatoform disorder. In light of our new findings pointing to the substantial contribution of substance use also to premature mortality in those with mental disorders, efforts related to the prevention 22 and the early detection and prompt treatment 23 of this type of comorbidity warrant added emphasis.
Our study has several key strengths, the most important one being the use of population‐based registers, which allowed for the inclusion of the entire population with prospectively collected data. This design and analysis greatly reduce the potential for selection and/or immortal time biases (i.e., when some individuals cannot experience death during follow‐up because of the design of the study). Moreover, health care is free in Denmark, reducing the potential inequalities in access to care between people with different socio‐economic background. Additionally, as date of death was obtained from registers and is thought to be accurate 24 , mortality estimates were not affected by potential misclassification.
However, there are some limitations of the study that need to be taken into consideration. First, in order to make the analyses tractable and allow comparisons to related publications2, 3, 7, we considered broad diagnostic categories, rather than specific disorders. Second, we relied on clinical diagnoses rather than direct structured diagnostic interviews to identify mental disorders; however, several studies have confirmed that many register‐based mental disorder diagnoses have good validity25, 26, 27, 28, 29.
Third, although the study included the entire population, diagnosed individuals included only those with mental disorders registered in secondary care – individuals with untreated mental disorders, or treated solely by a general practitioner, were misclassified as having not experienced the mental disorder. While it is reasonable to assume that the most severe disorders will eventually be registered in secondary care, the identification of milder disorders could be underestimated30, 31. In addition, we did not identify remission through registers; the group of individuals with a mental disorder can therefore be interpreted as persons who have had a diagnosis of a mental disorder, irrespective of their potential subsequent recovery.
Fourth, the study period used to identify combinations of disorders comprised 22 years (from 1995 until 2016). While this is a long period to identify the most common sets of disorders, the estimates cannot be interpreted as lifetime prevalences of these combinations. With access to longer follow‐up times, we might have seen patterns of comorbidity linking disorders with early onset to those with late onset. Finally, patterns of mental disorders and their associated excess mortality in the Danish population may not generalize to other countries.
To the best of our knowledge, this study is the largest and most detailed to quantify the frequency of combinations of comorbid mental disorders to date. We report novel estimates related to the “force of comorbidity”. In addition, we provide new insights into the contribution of substance use disorders to the premature mortality in those with comorbid mental disorders. We hope that this research will motivate clinical research designed to identify ways to prevent the development of comorbidity within mental disorders, as well as early detection and prompt treatment.
ACKNOWLEDGEMENTS
The overall project was supported by the Danish National Research Foundation (Niels Bohr Professorship to J.J. McGrath). J.J. McGrath is also supported by a John Cade Fellowship (APP1056929) from National Health and Medical Research Council. O. Plana‐Ripoll has received funding from the European Union's Horizon 2020 Research and Innovation Programme under the Marie Sklodowska‐Curie grant agreement no. 837180. K.L. Musliner receives funding from Lundbeck Foundation (grant no. R303‐2018‐3551). S. Dalsgaard's research is supported by grants from Novo Nordisk Foundation (no. 22018), Helsefonden (no. 19‐8‐0260), and the European Union's Horizon 2020 Research and Innovation Programme (nos. 847879 and 667302). P.B. Mortensen is supported by Lundbeck Foundation (grant nos. R102‐A9118 and R155‐2014‐1724), the Stanley Medical Research Institute and the European Research Council (project no. 294838). The funding organizations did not participate in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication. Further details on the results of the study are available on an interactive visualization website (http://nbepi.com/sets).
REFERENCES
- 1. Kessler RC. Lifetime and 12‐month prevalence of DSM‐III‐R psychiatric disorders in the United States. Arch Gen Psychiatry 1994;51:8‐19. [DOI] [PubMed] [Google Scholar]
- 2. Plana‐Ripoll O, Pedersen CB, Holtz Y et al. Exploring comorbidity within mental disorders among a Danish national population. JAMA Psychiatry 2019;76:259‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kessler RC, Petukhova M, Zaslavsky AM. The role of latent internalizing and externalizing predispositions in accounting for the development of comorbidity among common mental disorders. Curr Opin Psychiatry 2011;24:307‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kessler RC, Cox BJ, Green JG et al. The effects of latent variables in the development of comorbidity among common mental disorders. Depress Anxiety 2011;28:29‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pedersen CB, Mors O, Bertelsen A et al. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry 2014;71:573‐81. [DOI] [PubMed] [Google Scholar]
- 6. Lawrence D, Hancock KJ, Kisely S. The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: retrospective analysis of population based registers. BMJ 2013;346:f2539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Plana‐Ripoll O, Pedersen CB, Agerbo E et al. A comprehensive analysis of mortality‐related health metrics associated with mental disorders: a nationwide, register‐based cohort study. Lancet 2019;394:1827‐35. [DOI] [PubMed] [Google Scholar]
- 8. Erlangsen A, Andersen PK, Toender A et al. Cause‐specific life‐years lost in people with mental disorders: a nationwide, register‐based cohort study. Lancet Psychiatry 2017;4:937‐45. [DOI] [PubMed] [Google Scholar]
- 9. Dalsgaard S, Østergaard SD, Leckman JF et al. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: a nationwide cohort study. Lancet 2015;385:2190‐6.25726514 [Google Scholar]
- 10. Laursen TM, Plana‐Ripoll O, Andersen PK et al. Cause‐specific life years lost among persons diagnosed with schizophrenia: is it getting better or worse? Schizophr Res 2019;206:284‐90. [DOI] [PubMed] [Google Scholar]
- 11. Meier SM, Mattheisen M, Mors O et al. Increased mortality among people with anxiety disorders: total population study. Br J Psychiatry 2016;209:216‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Weye N, Momen NC, Christensen MK et al. Association of specific mental disorders with premature mortality in the Danish population using alternative measurement methods. JAMA Netw Open 2020;3:e206646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pedersen CB. The Danish Civil Registration System. Scand J Public Health 2011;39(Suppl. 7):22‐5. [DOI] [PubMed] [Google Scholar]
- 14. Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Public Health 2011;39(Suppl. 7):54‐7. [DOI] [PubMed] [Google Scholar]
- 15. Agerbo E. High income, employment, postgraduate education, and marriage. Arch Gen Psychiatry 2007;64:1377. [DOI] [PubMed] [Google Scholar]
- 16. Clayton D, Hills M. Statistical models in epidemiology. Oxford: Oxford University Press, 1993. [Google Scholar]
- 17. Andersen PK. Life years lost among patients with a given disease. Stat Med 2017;36:3573‐82. [DOI] [PubMed] [Google Scholar]
- 18. Plana‐Ripoll O, Canudas‐Romo V, Weye N et al. Lillies: an R package for the estimation of excess life years lost among patients with a given disease or condition. PLoS One 2020;15:e0228073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Scott JG, Giørtz Pedersen M, Erskine HE et al. Mortality in individuals with disruptive behavior disorders diagnosed by specialist services – A nationwide cohort study. Psychiatry Res 2017;251:255‐60. [DOI] [PubMed] [Google Scholar]
- 20. Hjorthoj C, Ostergaard ML, Benros ME et al. Association between alcohol and substance use disorders and all‐cause and cause‐specific mortality in schizophrenia, bipolar disorder, and unipolar depression: a nationwide, prospective, register‐based study. Lancet Psychiatry 2015;2:801‐8. [DOI] [PubMed] [Google Scholar]
- 21. Meier SM, Dalsgaard S, Mortensen PB et al. Mortality risk in a nationwide cohort of individuals with tic disorders and with Tourette syndrome. Mov Disord 2017;32:605‐9. [DOI] [PubMed] [Google Scholar]
- 22. Kessler RC, Price RH. Primary prevention of secondary disorders: a proposal and agenda. Am J Community Psychol 1993;21:607‐33. [DOI] [PubMed] [Google Scholar]
- 23. Teesson M, Proudfoot H. (eds). Comorbid mental disorders and substance use disorders: epidemiology, prevention and treatment. Sydney: Australian Government Department of Health and Ageing, 2003. [Google Scholar]
- 24. Helweg‐Larsen K. The Danish register of causes of death. Scand J Public Health 2011;39(Suppl. 7):26‐9. [DOI] [PubMed] [Google Scholar]
- 25. Phung TKT, Andersen BB, Høgh P et al. Validity of dementia diagnoses in the Danish hospital registers. Dement Geriatr Cogn Disord 2007;24:220‐8. [DOI] [PubMed] [Google Scholar]
- 26. Kessing LV. Validity of diagnoses and other clinical register data in patients with affective disorder. Eur Psychiatry 1998;13:392‐8. [DOI] [PubMed] [Google Scholar]
- 27. Lauritsen MB, Jørgensen M, Madsen KM et al. Validity of childhood autism in the Danish Psychiatric Central Register: findings from a cohort sample born 1990‐1999. J Autism Dev Disord 2010;40:139‐48. [DOI] [PubMed] [Google Scholar]
- 28. Bock C, Bukh J, Vinberg M et al. Validity of the diagnosis of a single depressive episode in a case register. Clin Pract Epidemiol Ment Health 2009;5:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jakobsen KD, Frederiksen JN, Hansen T et al. Reliability of clinical ICD‐10 schizophrenia diagnoses. Nord J Psychiatry 2005;59:209‐12. [DOI] [PubMed] [Google Scholar]
- 30. Musliner KL, Liu X, Gasse C et al. Incidence of medically treated depression in Denmark among individuals 15‐44 years old: a comprehensive overview based on population registers. Acta Psychiatr Scand 2019;139:548‐57. [DOI] [PubMed] [Google Scholar]
- 31. Hansen SS, Munk‐Jørgensen P, Guldbaek B et al. Psychoactive substance use diagnoses among psychiatric in‐patients. Acta Psychiatr Scand 2000;102:432‐8. [DOI] [PubMed] [Google Scholar]


