Abstract
Background
Studies show that by three months, over half of US infants receive formula and guidelines play a key role in formula feeding. The question then is, what might happen if caregivers follow guidelines and, more specifically, are there situations where following guidelines can result in infants who are overweight/have obesity?
Methods
We used our “Virtual Infant” agent-based model representing infant-caregiver pairs that allowed caregivers to feed infants each day according to guidelines put forth by Johns Hopkins Medicine(JHM), Children’s Hospital of Philadelphia(CHOP), Children’s Hospital of the King’s Daughters(CHKD), and WIC. The model simulated the resulting development of the infants from birth to six months. The two sets of guidelines vary in their recommendations, and do not provide studies that support amounts at given ages.
Results
Simulations identified several scenarios where caregivers followed JHM/CHOP/CHKD and WIC guidelines but infants still became overweight/with obesity by six months. For JHM/CHOP/CHKD guidelines, this occurred even when caregivers adjusted feeding based on infant’s weight. For WIC guidelines, when caregivers adjusted formula amounts, infants maintained healthy weight.
Conclusions
WIC guidelines may be a good starting point for caregivers who adjust as their infant grows, but the minimum amounts for JHM/CHKD/CHOP recommendations may be too high.
Introduction
In the United States, formula feeding infants is extremely common.(1) In fact, over half of infants have received some formula by three months,(2) and guidelines exist to guide caregivers about how much formula to give infants each day.(3) Though the counseling and guidance for infant feeding varies across clinics, guidelines do play an important role in infant feeding. Studies have shown that clinicians can influence caregivers’ infant feeding decisions,(4–6) and in 2017 90% of children under the age of 2 received a well-child check-up where they meet with a health care professional to check their growth and development. Clinicians may refer to and rely on recommendations put forth by reputable hospitals and institutions such as Johns Hopkins Medicine (JHM), Children’s Hospital of Philadelphia (CHOP) and Children’s Hospital of the King’s Daughters (CHKD). Additionally, 1.71 million infants receive benefits from the Women, Infants, and Children (WIC) program, which covers more than half of infants in the United States.(7) Studies estimate that infants participating in WIC consume over half of all formula sold in the US.(8) WIC implements a structured program to guide parents on infant feeding, where WIC staff are encouraged to provide resources such as the feeding recommendations listed in the WIC Infant Nutrition and Feeding handbook.(9)
The question then is, what happens if caregivers follow the guidelines? And more specifically, can following guidelines result in infants who are overweight or have obesity? This is important because overweight or obesity in infancy can affect a child’s risk later in childhood and adulthood.(10, 11) Therefore, we developed a virtual infant computational simulation model to see what happens to an infant’s body mass index (BMI) when their caregivers follow formula-feeding recommendations. Our infant model represents daily caloric intake, physical activity, metabolism, and the resulting changes in body size. In this study, the modeled scenarios allow for potential weekly changes to the amount of formula a caregiver feeds an infant, but each day of feeding is represented. The goal of this study is to use our computational simulation model to test formula feeding guidelines and observe whether or not they result in appropriate patterns of infant weight gain.
Computational simulation models help overcome the logistic and ethical challenges of testing feeding guidelines on a cohort of infants. Using computational simulation models, we can test different formula feeding recommendations in a virtual laboratory before implementing recommendations in real life. Computational models have been used previously to guide infant feeding. For example, in a previously published study, researchers used an agent-based model to test the impact of caregivers following complementary feeding guides on infants BMIs.(12) The model identified scenarios where following guidelines could lead to infants becoming overweight or developing obesity. Such models can help decisionmakers adjust existing guidelines and inform infant feeding practices.
Methods
Virtual Infant Model
We used our previously published Virtual Infant model to represent infant-caregiver pairs (e.g. pair consisting of an infant fed by a single caregiver) and infant feeding and growth from birth to six months in one-day time steps. In real life, caregivers can make his or her own decisions about feeding their infant, and can change their feeding decisions (e.g., how much formula to give) over time based on the daily growth and needs of their infant. Thus, in order to account for these we used an agent-based model.
Similar to infants in real life, each virtual infant has characteristics such as a sex and a starting weight, length, and body mass index (BMI). We sampled across a normal distribution of BMI percentiles centered around the 50th BMI percentile (varying the birthweight and length) from birth through six months. We simulated infants born at term without congenital abnormalities. Each infant also had an embedded metabolic model (adapted from previously published models (13, 14)) that represents the processes by which the infant’s body translates consumed and expended calories into daily changes in weight. This translation occurs in a series of steps. First, when a caregiver feeds an infant, the consumed calories enter the metabolic model. Ingested calories first satisfy energy needs for the basal metabolic rate (BMR), thermic effect of feeding (TEF), adaptive thermogenesis, and physical activity. BMR is the energy needed to keep a body functioning when at rest and is calculated for each virtual infant by summing the energy needs of the infant’s fat mass (FM), fat-free mass (FFM), and organs.(14) The thermic effect of feeding refers to the energy needed by the infant to process food.(14) Adaptive thermogenesis is the regulation of metabolic speed based on changes in energy intake.(14, 15) Studies conducted to derive these weight-specific energy needs were also conducted among infants.(16, 17) Values for specific components are in the Appendix. To obtain daily caloric expenditure from physical activity, we added calories from BMR, TEF, and thermogenesis and then subtracted them from the total energy requirements observed in Butte’s seminal study on infant energy needs.(18) When calculating the energy needs for each of these components, the model determines the energy needed to grow along the Centers for Disease Control (CDC) projection of the infant’s weight(19), meaning these caloric needs changed each day to account for growth as the infant aged. At the end of each day, if the caloric intake was greater than the calories needed to achieve desired growth, the infant would gain extra weight. If the total caloric intake does not meet the number of calories needed to maintain infant weight, the virtual infant metabolizes energy stores resulting in weight loss.
The model updates the virtual infant weight each day by calculating the changes in the FM and FFM. To calculate changes in FM and FFM, the model multiplies the energy surplus or energy deficit by the energy density of the particular tissue type. The model then adds the updated FM and FFM together (which captures the varying densities of different tissue types), which equals the weight of the virtual infant (in kg) for the start of the next time step/following day. We used the CDC definitions for overweight (85th BMI percentile) and obesity (95th BMI percentile) in this study.(20) This standard was used instead of the weight-for-length standard as recommended by the American Academy of Pediatrics(21) because of a previous study conducted by Roy et al. that concluded that BMI more accurately predicts future obesity risk.(22) Additionally, the weight-for-length standard is more pertinent to assessments of age-specific growth patterns, whereas BMI percentile better describes changes in FM and FFM. Each day, the infant’s caregiver decides the total number of feeds for the day by randomly selecting from a uniform distribution of the range of daily feeding frequencies in the recommendation. Then, the caregiver decides the amount for each feed by randomly selecting an amount from a uniform distribution with a range also based on the recommendations (see Table 1).
Table 1:
Infant formula-feeding recommendations
| Women Infants and Children/United States Department of Agriculture* | Children’s Hospital of Philadelphia/Johns Hopkins Medicine/Children’s Hospital of the King’s Daughters Recommendations* |
||||
|---|---|---|---|---|---|
| Age (months) | Daily Formula Milk (mL) | Ref | Age (months) | Daily Formula Milk (mL) | Ref |
| 0 | 414–1242.1 | (26) | 0 | 354.9–946.4 | (27), (28), (29) |
| 1 | 414–1242.1 | 1 | 354.9–946.4 | ||
| 2 | 414–1242.1 | 2 | 739.3–1064.7 | ||
| 3 | 414–1242.1 | 3 | 887.2–1242.1 | ||
| 4 | 768.9–1153.4 | 4 | 887.2–1242.1 | ||
| 5 | 768.9–1153.4 | 5 | 887.2–1242.1 | ||
we assume formula milk caloric density is 0.676 kcal/mL(37)
Each week, caregivers reassess the amount to feed their infant according to the recommendations in order to simulate caregivers adapting the amount they feed their infant based on the daily growth and needs of their infant. Specifically, if in the past week the infant has had a change in weight and has passed a major BMI percentile (5th, 10th, 25th, 50th, 75th, 90th and 95th), then the caregiver will adjust the feeding amounts to the lower end of the range (if BMI increases) or the upper end of the range (if BMI decreases). Depending on which scenario, the normal distribution is either truncated at the mean (when feeding from the upper half the mean is new minimum, or feeding from the lower half the mean is new maximum ) or truncated at the upper/lower quartile (75th percentile feeding amount is the new minimum for the upper quartile, and 25th percentile feeding amount is the new maximum for the lower quartile). For example, the WIC guidelines recommend between 414 and 1242.1 mL, (mean 828 mL) between 0 and 4 months. For a scenario where caregivers adjust to the upper/lower half, caregivers start off feeding an amount from the full range (normal distribution), and if the infant’s BMI increases and passes a major BMI percentile then the amount fed is pulled from the lower half of this distribution (e.g. the distribution is truncated at 828, new range, 414 to 828 mL). If an infant’s BMI continues to increase and crosses another major BMI percentile and they are already consuming the lower end of the range, then they will continue to consume portions at the lower end. If their BMI starts to decrease and crosses a major BMI percentile by the next week, the caregiver will adjust and feed from the full range. If after another week their BMI continues to decrease and crosses another major BMI percentile, the caregiver will adjust to the upper half. We allowed for only one adjustment per week, such that the portion size would not jump from the lower half to the upper half in one week or from the upper to the lower quartile in one week. The same is true for the scenario where they adjust to the upper/lower quartiles.
Validation
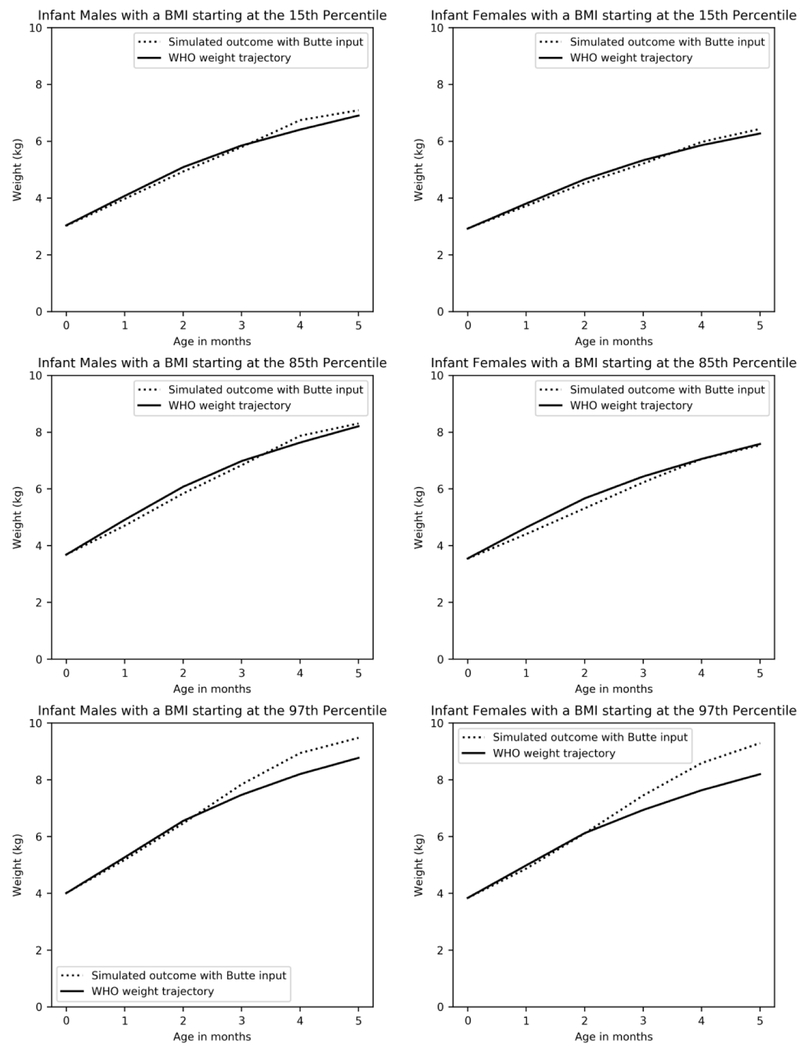
To validate our model, we compared infant BMIs generated from the metabolic model to the WHO growth standards for children under 24 months, which is based on the longitudinal component of the Multicentre Growth Reference Study which included cohorts of infants measured from birth through age 23.(23) This data was not used to build the model. The validation focused on energy intake and corresponding growth and did not distinguish between different types of calories (e.g., different macronutrients such as proteins, carbohydrate, etc.). We simulated caregivers feeding normal weight virtual infants (15th and 85th BMI percentile) calories equaling the necessary energy requirements for infants as derived in the study conducted by Butte.(24) This was the same study we used to derive the physical activity levels, another input described earlier in the Methods. Then, we plotted the resulting BMI percentile curves. Next, we compared these trajectories to the WHO reference BMI growth curves.(25) The difference between the BMI trajectories was not statistically significant. We conducted a z-test and found that the p-value was less than 0.05. For example, a virtual female infant at the 50th BMI percentile weighed 6.06 kg at three months of age and 7.37 kg at six months, 8.24 kg at nine months, compared to 5.84 kg and 7.29 kg at three and six months respectively on the WHO growth standard curve. As seen in Figure 1, we also validated the model for infants deviating from normal growth. We simulated caregivers feeding infants in the 97th BMI percentile calories equaling energy requirements to maintain 97th BMI percentile over the first sixth months, per Butte’s observed energy needs. When we compared this extreme scenario to the WHO growth standard curve, we observed that the BMI trajectory from the model output follows the same pattern as the WHO standard.
Figure 1. Validation of Simulation Model.
This figures compares outputs from the Virtual Infant model when infants were fed calories to meet required energy needs derived from Butte (24) (dotted line) to real world data from WHO reference curve (solid line).
Testing Different Feeding Guidelines
Next, we reviewed the literature for various formula-feeding guidelines and chose to test the sources that were detailed enough to derive calorie amounts. We tested two sets of formula-feeding recommendations over the first six months (Table 1): (1) Women Infants and Children (WIC)(26) (2) Children’s Hospital of Philadelphia (CHOP)(27)/the Johns Hopkins Medicine (JHM)(28)/Children’s Hospital of the King’s Daughters (CHKD).(29) The WIC recommendations are intended to guide low-income mothers involved in the WIC program, which provides supplemental food and formula and nutrition education to low-income pregnant women and mothers of infants and young children (0–5 years).(30) The CHOP/JHM/CHKD recommendations are plausibly meant to guide clinicians, patients, and others accessing their resources, though the intended audience is not clearly stated. The two sets of recommendations vary; thus, we conducted a literature search to determine how these guidelines were developed. This involved manually searching the literature on PubMed and Google Scholar using search terms including: infant formula feeding recommendations; deriving formula recommendations; feeding guidelines. Neither the guidelines nor the literature in our search cite any studies or explain how they derived the amounts. We considered recommendations from WHO and CDC, but they did not provide enough specificity to parameterize the model. Recommendations from WHO and CDC were considered but did not provide enough specificity to parameterize the model.
For the purposes of this paper, we only examined formula-fed infants.
To conduct a thorough exploration intended to identify if there are situations where growth deviates from a standard pattern of weight gain when adhering to formula feeding recommendations, we simulated the following scenarios for each feeding guideline : 1) Caregivers check BMI each week and adjust amount to the lower/upper half of the recommendation depending on their infant’s growth, 2) Caregivers check BMI each week and adjust amount to lower/upper quartile of the recommendation depending on their infant’s growth, 3) Caregivers feed infants according to the normal distribution of the full range, and they do not adjust the amount, and 4) Caregivers feed infants according to the lower quartile of the range, and they do not adjust the amount (most conservative feeding profile).
Each simulation experiment consisted of running the model 10,000 times to run 10,000 different infants. Mean daily BMI percentiles are reported in the results and figures, along with 95% uncertainty intervals.
Results
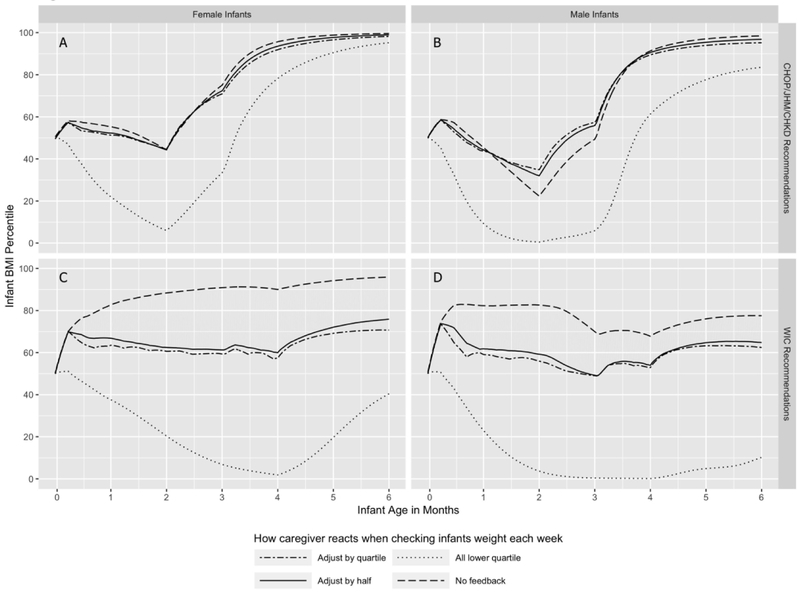
Caregivers feeding infants according to the WIC Formula-Feeding Recommendations for 6 months, Exclusive Formula-feeding
When caregivers were feeding infants according to the WIC formula-feeding recommendations, and could make adjustments, approximately 50% of male and female infants crossed the 75th BMI percentile within the first two weeks. At this point the caregivers adjusted the feed amounts and their BMIs remained healthy and relatively stable through six months, with an increase beginning in the fifth month. At six months, the female BMI was in the 74th percentile when caregivers adjusted to upper and lower half and 70th percentile when they adjusted to upper and lower quartile. The male BMI was at the 65th percentile when they adjusted to the upper and lower half and 62nd percentile when they adjusted to the upper and lower quartile. When caregivers follow the WIC recommendations without adjusting feeding amounts in response to infant weight trajectory, female infant BMIs reached overweight levels in the second month, which steadily increased to obese levels by six months. Male infant BMIs did not become unhealthy, though they did reach the 82nd percentile within the first month and ended at the 77th percentile. When caregivers always fed within the lowest quartile of feeding recommendations, infant BMIs reached underweight levels, by the fourth month for females and the second month for males. Female infant BMIs did reach healthy weights after the fourth month and the 40th BMI percentile by six months, and males reached the 10th BMI percentile by six months. See Figure 2.
Figure 2. Assessing impact of formula-feeding recommendations on infant BMI for 6 Months, Exclusive Formula-feeding.
Panel A: Food consumption based on Children’s Hospital of Philadelphia (CHOP)/Johns Hopkins Medicine (JHM)/Children’s Hospital of the King’s Daughters (CHKD) recommendations in female infants. Panel B: Food consumption based on Children’s Hospital of Philadelphia (CHOP)/Johns Hopkins Medicine (JHM)/Children’s Hospital of the King’s Daughters (CHKD) recommendations in male infants. Panel C: Food consumption based on Women Infants and Children (WIC) in female infants. Panel D: Food consumption based on Women Infants and Children (WIC) in male infants. Two-dashed lines (– – – –) represent virtual caregivers adjusting to the infants’ weight trajectory by feeding in the lower or upper quartile of feeding amounts in response to significant weight gain or loss, respectively. Solid lines (——) represent virtual caregivers adjusting to infants’ weight trajectory by feeding in the lower or upper half of feeding amounts in response to significant weight gain or loss, respectively. Dotted lines (·······) represent virtual caregivers feeding only within the bottom quartile of feeding amounts. Dashed lines (– – –) represent virtual caregivers feeding within the full range of feeding amounts with no adjustment responding to infant weight trajectories.
Caregivers feeding infants according to the CHOP/JHM/CHKD Formula-Feeding Recommendations for 6 months, Exclusive Formula-feeding
When caregivers adjusted feeding amounts by half or quartile in response to infant weight trajectory, infant BMIs reached overweight levels in the fourth month for all infants, and males maintained these overweight levels in both scenarios at six months and female infants reached obese BMI levels by six months in both scenarios where caregivers could adjust feeding amounts. When caregivers follow the CHOP/JHM/CHKD recommendations, drawing from the full recommended range of feeding amounts, without adjusting feeding amount in response to infant weight trajectory, female infant BMIs reached overweight levels in the fourth month, and obese levels by the fifth month. Male infant BMIs reached overweight in the fifth month and obese levels by the sixth month. When caregivers always fed within the lowest quartile of feeding recommendations, infant BMIs for both males and females reached underweight levels in the second month, and after two months the infant BMIs subsequently rapidly rebounded, with female infant BMIs reaching unhealthy overweight levels in the fifth month and males reaching the 83nd percentile by six months. See Figure 2.
Discussion
Our study identified a number of different situations in which caregivers followed JHM/CHOP/CHKD and WIC guidelines, yet infants still moved into the overweight/obese weight category by six months of age. This occurred for the JHM/CHOP/CHKD guidelines even when caregivers adjusted the amount of formula that they fed their infants based on their infant’s weekly weight. Such adjustments did help infants maintain healthy weight when the WIC guidelines were followed. However, there is evidence that caregivers don’t tend to make such feeding adjustments even when closely monitoring an infant’s weight.(31)
Our results suggest that the minimum amounts of daily formula recommended by JHM/CHOP/CHKD (which are 325 mL, 473 mL and 118 mL higher than WIC for the second, third, fourth/fifth month respectively) may be too high, not allowing caregivers the flexibility to adjust feed sizes low enough to prevent or move their infant out of the overweight/obese category. Further, caregivers may be introducing complementary foods during the four to six month window, which means that even smaller formula amounts may be needed by the infant, in order to account for the calories from solid foods.
Current infant feeding recommendations provide caregivers with ranges and estimates within which to feed their infants. However, further research must identify how infant feeding may change under varying circumstances and determine how best to respond to these variations. Since infant feeding guidelines offer a foundation for communication between nurses, doctors, and parents to help monitor infant health and encourage healthy diets, it is important to be able to demonstrate the impact of recommendations to caregivers. Feeding recommendations guide parents and health practitioners, and caregivers must know how to adjust the guidelines for individual infants. In order to understand how to adjust guidelines, we can use computational simulation models which serve as “virtual laboratories” to help overcome the logistical and ethical issues of clinical trials. Simulation models can iteratively test formula recommendations in the safety of a computer, to not only help clinicians and caregivers understand the impact of the guidelines on infant weight, but also help adapt the recommendations to fit the needs of the infant.
Limitations
Computational models are simplifications of reality and cannot include all possible factors that impact feeding in infants. Our simulations did not account for potential alterations in feeding during illnesses and sleep disturbances. We also did not represent different types of calories, such as different macronutrients which may vary between breastmilk and formula milk. One study found higher protein intake among breastfed infants which also resulted in more weight gain, which means we could be underestimating weight gain for formula fed infants.(32) Our study, similar to existing recommendations, assumed healthy infants over the first year of life. Similarly, our study assumed that feeding recommendations would have the same efficacy regardless of the mother’s health status, number of siblings, and economic status. Feeding guidelines from WIC, CHOP, JHM, and CHKD provide the flexibility of introducing solid foods between four and six months of age; however, we introduce at six months for each guideline because studies show that introducing solid foods too early can impact infant weight.(33) Because this paper sought to identify situations when following feeding recommendations could result in overweight or obese BMIs among infants, we did not model the impact of other cofounding factors, including sleep issues, medication, and growth-impacting medical conditions. We also acknowledge that there is likely a difference between an infant’s actual hunger and satiation and how hunger and satiety are understood by researchers and caregivers. This makes interpreting and responding to infant cues challenging. Therefore, we developed a model to track how infant growth follows standard patterns under specific feeding recommendations. We did not represent a caregiver’s level of responsiveness to an infant’s appetitive cues or behavior, nor did we represent caregivers misinterpreting cues ranging from restlessness to sucking on fists to excessive crying, which could be driven by an infant having a larger appetite or propensity for weight gain. Studies estimate about one in six infants displays excessive crying (e.g., any amount of crying that worries the caregivers or colic which may involve crying for least three hours a day, three times a week for three consecutive weeks and lasting three months (34)) which may result in more frequent feeding than we represented in our model for those infants.(35) Another study suggests that perceived fussiness may result in earlier introduction of solid foods, which we also did not model.(36) We did, however, include feedback due to infant weight changes.
Conclusion
Our study identified a number of different situations in which caregivers followed existing guidelines, yet infants still moved into the overweight/obese weight category by six months of age, even when caregivers adjusted the amount of formula they fed their infant based on their infant’s weekly changes in weight. This study suggests that the minimum amounts recommended by JHM/CHOP/CHKD may be too high. Lower minimum of the daily formula amounts better support responsive infant feeding, as the wider range gives caregivers more flexibility in responding to changes in growth.
Supplementary Material
CATEGORY OF STUDY: Population Study.
IMPACT
-
⚪
Our virtual infant simulation study answers the question: can caregivers follow current formula feeding guidelines and still end up with an infant who is overweight or has obesity?
-
⚪
Our study identified several situations in which unhealthy weight gain and/or weight loss could result from following established formula-feeding recommendations.
-
⚪
Our study also suggests that the minimum recommended amount of daily formula-feeding should be lower for Johns Hopkins Medicine/Children’s Hospital of Philadelphia/ Children’s Hospital of the King’s Daughters guidelines to give caregivers more flexibility in adjusting daily feeding levels in response to infant weight.
-
⚪
WIC guidelines may be a good starting point for caregivers who adjust as their infant grows.
-
⚪
In order to understand how to adjust guidelines, we can use computational simulation models which serve as “virtual laboratories” to help overcome the logistical and ethical issues of clinical trials.
Acknowledgments
FINANCIAL SUPPORT: Research reported in this publication was supported by the Global Obesity Prevention Center (GOPC) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the Office of the Director, National Institutes of Health (OD) under award number U54HD070725. It was also supported by NICHD via grant U01HD086861 and 5R01HD086013, and the Agency for Healthcare Research and Quality (AHRQ) via grant R01HS023317. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or Agency for Healthcare Research and Quality (AHRQ).
Footnotes
DISCLOSURE: The authors declare no conflict of interest.
Patient consent was not required.
References:
- 1.Grummer-Strawn LM, Scanlon KS, Fein SB 2008. Infant feeding and feeding transitions during the first year of life. Pediatrics 122 Suppl 2:S36–42. [DOI] [PubMed] [Google Scholar]
- 2.Division of Nutrition PA, and Obesity, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, 2018 Breastfeeding Report Card: United States, 2018. U.S. Department of Health and Human Services. [Google Scholar]
- 3.Odom EC, et al. 2014. Association of family and health care provider opinion on infant feeding with mother’s breastfeeding decision. Journal of the Academy of Nutrition and Dietetics 114:1203–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marchand L, Morrow M 1994. Infant feeding practices: understanding the decision-making process. Family medicine 26:319–324. [PubMed] [Google Scholar]
- 5.Cairney PA, Alder EM, Barbour RS 2006. Support for infant feeding: mothers’ perceptions. British Journal of Midwifery 14:694–700. [Google Scholar]
- 6.Heinig MJ, et al. 2006. Barriers to compliance with infant-feeding recommendations among low-income women. Journal of Human Lactation 22:27–38. [DOI] [PubMed] [Google Scholar]
- 7.United States Department of Agriculture The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC Program) Fact Sheet. https://fnsprod.azureedge.net/sites/default/files/wic/wic-fact-sheet.pdf.
- 8.Prell MA 2004. An economic model of WIC, the infant formula rebate program, and the retail price of infant formula. [Google Scholar]
- 9.Blum-Kemelor D LB, Christie L, Bartholomew A, Mitchell P, Singleton U, Salley T 2009. Infant Nutrition and Feeding: A Guide for Use in the WIC and CSF Programs. US Department of Agriculture, Food and Nutrition Service, Special Supplemental Nutrition Program for Women, Infants, and Children (WIC Program), https://wicworks.fns.usda.gov/wicworks/Topics/FG/CompleteIFG.pdf. [Google Scholar]
- 10.Druet C, et al. 2012. Prediction of childhood obesity by infancy weight gain: an individual‐level meta‐analysis. Paediatric and perinatal epidemiology 26:19–26. [DOI] [PubMed] [Google Scholar]
- 11.Reilly JJ, et al. 2005. Early life risk factors for obesity in childhood: cohort study. Bmj 330:1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferguson MC, et al. 2019. The Impact of Following Solid Food Feeding Guides on BMI Among Infants: A Simulation Study. American journal of preventive medicine 57:355–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hall KD, Butte NF, Swinburn BA, Chow CC 2013. Dynamics of childhood growth and obesity: development and validation of a quantitative mathematical model. The lancet Diabetes & endocrinology 1:97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rahmandad H 2014. Human growth and body weight dynamics: an integrative systems model. PLoS One 9:e114609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Doucet E, et al. 2001. Evidence for the existence of adaptive thermogenesis during weight loss. British Journal of Nutrition 85:715–723. [DOI] [PubMed] [Google Scholar]
- 16.Torun B 2005. Energy requirements of children and adolescents. Public Health Nutrition 8:968–993. [DOI] [PubMed] [Google Scholar]
- 17.Wang Z 2012. High ratio of resting energy expenditure to body mass in childhood and adolescence: a mechanistic model. American Journal of Human Biology 24:460–467. [DOI] [PubMed] [Google Scholar]
- 18.Butte NF 2005. Energy requirements of infants. Public health nutrition 8:953–967. [DOI] [PubMed] [Google Scholar]
- 19.Kuczmarski RJ, et al. 2000. CDC growth charts: United States advance data from vital and health statistics, no. 314. Hyattsville, MD: National Center for Health Statistics. [Google Scholar]
- 20.Barlow SE 2007. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 120:S164–S192. [DOI] [PubMed] [Google Scholar]
- 21.Daniels SR, Hassink SG 2015. The role of the pediatrician in primary prevention of obesity. Pediatrics 136:e275–e292. [DOI] [PubMed] [Google Scholar]
- 22.Roy SM, et al. 2016. Infant BMI or weight-for-length and obesity risk in early childhood. Pediatrics 137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grummer-Strawn L, Krebs NF, Reinold CM 2009. Use of World Health Organization and CDC growth charts for children aged 0–59 months in the United States. [PubMed] [Google Scholar]
- 24.Butte NF 2005. Energy requirements of infants. Public Health Nutr 8:953–967. [DOI] [PubMed] [Google Scholar]
- 25.Group WMGRS, de Onis M 2006. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatrica 95:76–85. [DOI] [PubMed] [Google Scholar]
- 26.U.S. Department of Agriculture 2009. Infant Nutrition and Feeding: A Guide for Use in the WIC and CSF Program. [Google Scholar]
- 27.Children’s Hospital of Philadelphia Feeding Guide for the First Year. Children’s Hospital of Philadelphia, Philadelphia, PA. [Google Scholar]
- 28.Johns Hopkins Medicine Feeding Guide for the First Year. The Johns Hopkins University, The Johns Hopkins Hospital, and Johns Hopkins Health System, Baltimore, MD. [Google Scholar]
- 29.Children’s Hospital of The King’s Daughters 2011. Infant Feeding Guide for the First Year. Norfolk, VA. [Google Scholar]
- 30.U.S. Department of Agriculture FaNS Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). [PubMed] [Google Scholar]
- 31.Kavanagh-Prochaska K, Cohen R, Heinig M, Dewey K 2006. Educational intervention to modify bottle-feeding behaviors among formula feeding mothers in the WIC Program: Impact on infant formula intake, weight gain and fatness. Federation of American Societies for Experimental Biology. [DOI] [PubMed] [Google Scholar]
- 32.Koletzko B, et al. 2005. Protein intake in the first year of life: a risk factor for later obesity? Early nutrition and its later consequences: new opportunities. Springer, pp 69–79. [Google Scholar]
- 33.Moorcroft KE, Marshall JL, McCormick FM 2011. Association between timing of introducing solid foods and obesity in infancy and childhood: a systematic review. Maternal & child nutrition 7:3–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Halpern R, Coelho R 2016. Excessive crying in infants. Jornal de pediatria 92:S40–S45. [DOI] [PubMed] [Google Scholar]
- 35.Morris S, St James-Roberts I, Sleep J, Gillham P 2001. Economic evaluation of strategies for managing crying and sleeping problems. Archives of disease in childhood 84:15–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wasser H, et al. 2011. Infants perceived as “fussy” are more likely to receive complementary foods before 4 months. Pediatrics 127:229–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O’Connor NR 2009. Infant formula. American family physician 79:565–570. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.