Abstract
Background
Adverse childhood experiences (ACEs) are common among children. Little is known on how resilience factors and positive childhood experiences (PCEs) may moderate the relationship between ACEs and childhood depression.
Objective
Our study fills this gap by providing recent, nationally representative estimates of ACE and PCE exposure for ages 8-17 and examines the associations between ACE exposure and PCEs on the outcome of depression.
Participants and Setting
Data were drawn from the nationally representative 2016-2017 National Survey of Children’s Health (NSCH) and included a total sample of 40,302 children and adolescents.
Methods
Chi square analysis and multivariate logistic regressions were performed to assess associations of depression with 9 ACE and 6 PCE exposures. Additive and multiplicative interactions were examined between ACE exposure and PCEs (resiliency measures) on depression. Survey sampling weights and SAS survey procedures were used.
Results
Our study found that 4% of children had current depression and those with an ACE count greater than four had increased odds (aOR: 2.29; CI: 1.74-3.02). Multivariate regressions demonstrated associations between depression and low resiliency as well as significant interactions between ACE exposure and three PCEs. Children who were exposed to greater than four ACEs and did not exhibit resilience had 8.75 higher odds of depression (CI: 5.23-14.65) compared to those with less than four ACEs and some resilience.
Conclusions
These findings illustrate the need for the promotion of PCEs and the building of resiliency for combatting depression and reducing the impact of trauma in children and adolescents.
Keywords: Adverse childhood experiences, depression, resilience, positive childhood experiences, pediatrics
Introduction
Adverse childhood experiences (ACEs) are childhood events encompassing neglect, abuse, and household dysfunction that occur between birth and 17 years of age (Felitti et al., 2019). ACEs among children is highly prevalent in the United States, with 22% of children experiencing parental separation or divorce and 23% experiencing economic hardship (Crouch et al., 2019). Exposure to childhood trauma has long-term negative effects on the social-emotional and overall physical well-being of individuals into adulthood, as changes in brain structure and development may occur due to prolonged activation of the stress response (Fairbank & Fairbank, 2009, Shonkoff et al., 2012).
Depression is a common result of trauma for children and adolescents (Vibhakar et al., 2019), as childhood adversity has been associated with adult onset depression and has been linked to an increased likelihood of the reoccurrence of depression among adults (Hill et al., 2004, Shanahan et al., 2011, Gilman et al., 2013). Childhood adversity is more likely to be associated with chronic depression, versus non-chronic depression (Angst et al., 2011). Recently, research has begun to explore the short-term association between ACEs and mental health in childhood by examining the incidence of depression, finding that 4% of children and adolescents aged 8-17 had current depression and that multiple types of ACE exposures, as well as higher cumulative ACE counts, are associated with a higher odds of depression among ages 8-17 (Elmore & Crouch, 2020).
Depression among children and adolescents is a critical area of study, as depression, once experienced in childhood, has been shown to commonly reoccur in adults (Kovacs et al., 2016). Risk factors for depression and other mental health issues include various demographic variables. For example, as children get older, they have more time to be exposed to more ACEs and depression is more common for older children (Bethell et al., 2016). Furthermore, gender differences in depression are also to be noted, as females are more likely to experience depression than males (Salk et al., 2017).
Less is known on how resilience factors may moderate the relationship between ACEs and childhood depression. For children with ACE exposure, strong resilience levels are associated with healthier outcomes, including lower rates of maladaptive behaviors and stress symptomatology (Happer et al., 2017). Children with higher levels of resilience are less likely to exhibit emotional, mental, or behavioral conditions even when exposed to ACEs (Bethell et al., 2016). Thus, child resilience has been demonstrated to mediate the effects of ACEs on some mental health outcomes among children and adolescents.
A relatively new way of looking at ACEs is through the “HOPE: Health Outcomes from Positive Experiences” framework, which examines the role of positive childhood experiences (PCEs), such as being in nurturing relationships, living in a safe equitable environment, having opportunities for social engagement, and learning emotional competencies (Sege & Harper Browne, 2017). This evidence based framework, and the questions associated, have been previously used to measure the level of resiliency in an individual (Bethell et al., 2019). A small number of studies have examined the interaction between PCEs and ACEs (Chung et al., 2008, Hillis et al., 2010, Kosterman et al., 2011). The protective effects of PCEs for mental health problems in adulthood have been demonstrated among pregnant women and young adults with ACE exposure (Chung et al., 2008, Kosterman et al., 2011).
Yet, there has been limited research on the relationship between ACE exposure and PCEs (resilience factors) on the short-term outcome of depression during adolescence. Our study fills this gap by providing recent, nationally representative estimates of ACE exposure and resiliency for ages 8-17 and examines the associations between ACE exposure and resilience factors on the outcome of depression. In addition, we individually analyze how multiple types of resilience factors mediate cumulative ACE exposure on the outcome of depression among children and adolescents. We hypothesize that exposure to ACE’s and low resiliency is associated with an increased likelihood of depression and that high resiliency may reduce the impact of ACE exposure on the outcome of depression.
Methods
We drew our study sample from the 2016-2017 National Survey of Children’s Health (NSCH) which is a survey conducted by the Data Resource Center for Child and Adolescent Health (DRC) to assess children’s health and wellbeing. Across the United States, addresses from civilian, non-institutionalized households with at least one child between the ages of 0 and 17 were randomly selected for the survey. If the parent or caregiver had more than one child, the interviewer randomly chose a single child for the interview. A total of 71,811 surveys were completed for 2016 and 2017 with approximately 1,400 surveys per state and a response rate of 40.7% in 2016 and 37.4% in 2017. Both years were combined by the NSCH Data Resource Center for the final dataset. Further information on the NSCH’s sampling strategy can be found on the Data Resource Center website (Data Resource Center for Child and Adolescent Health, 2019).
To assess the associations between ACE exposure and resilience factors on the outcome of depression, ACE count and multiple resilience measures were included for analysis. The nine ACE exposures measured by the NSCH include: parental separation or divorce, parental death, witnessing household violence, witnessing neighborhood violence, household mental illness, household incarceration, household substance abuse, racial/ethnic mistreatment, and economic hardship. For our analysis, we examined the association using ACE count by individually tabulating all nine ACE survey questions and then categorizing ACE count into less than 4 ACES or 4 or more ACEs. This cut point is well-established for ACE research among children and has been demonstrated as a valid cut point using ACE screening tools including the NSCH, Family Map Inventories, and the Child Behavior Checklist (Kerker et al., 2015, McKelvey et al., 2017).
Based upon the categories of positive experiences outlined in the HOPE framework, we included five independent resilience factors to examine their association with depression and the interaction of resilience and ACEs (Sege & Harper Browne, 2017). We examined these factors individually because they represent different categories of PCEs. To reflect emotional competency, the variable ‘Child resilience’, defined as “staying calm and control when faced with a challenge” was dichotomized into ‘definitely true’ or ‘somewhat true and not true’. The HOPE framework also outlines the importance of having opportunities for constructive social engagement which we implemented as a combination variable for child participation in ‘After school activities’. The variable combined two survey questions, “During the past 12 months did this child participate in sports, clubs, lessons after school” and “During the past 12 months did this child volunteer at church, community, or school” into a dichotomous variable of ‘Yes’ for participation in either. Developing in a safe and stable environment, presented as the variables ‘Family problem solves together’ and ‘Family remains hopeful’, was assessed through two family resilience questions respectively: “When your family faces problems how likely are you to work together to solve problems” and “When your family faces problems how likely are you to stay hopeful even in difficult situations” which were both grouped into ‘almost all of the time or most of the time’ and ‘some of the time or none of the time’. Lastly, trusting relationships with adults other than guardians is included as a positive HOPE experience and a response of yes or no to the survey question, “Other than adults in your home, is there at least one other adult who they can rely on for guidance and support” was used for the response for the variable ‘Other adult mentor’ in our analysis.
The NSCH measures health conditions among children of survey caregivers through survey question, “Has a doctor ever told you this child has…”, for 26 independent health conditions including depression. If the caregiver answered yes, a secondary question “If yes, does this child CURRENTLY have this condition?” is answered. We restricted the outcome of depression to only cases of current depression to possibly reduce the temporal limitations of the cross-sectional study design.
Demographic information collected through caregiver reporting includes: child age, sex, and ethnicity; respondent’s relation to child, education level, insurance type; and family poverty/income level. All demographics were presented as sample descriptives through prevalence estimates and examined as possible confounders. Demographic variables are potential confounders of both ACE and resilience exposures, as well as mental health outcomes among children (Bethell et al., 2016). Age was categorized into 8-10, 11-13, and 14-17 years old for consistency with previous research (Elmore & Crouch, 2020). Insurance type is an also important predictor of the outcome as children without insurance may be less likely to be diagnosed with depression and children with public insurance have been found to be more likely to report depression (Elmore & Crouch, 2020). Also, caregiver mental health may impact ACE exposures, resilience factors, and may even contribute a genetic component to depression among children. Lastly, a variable identifying children with a special health care needs was included as a possible confounder of depression. The NSCH identifies the presence of a special health care need through five screening tool questions concerning elevated health services use, the utilization of prescription medication, functional limitations, specialized therapy, and ongoing emotional, developmental, or behavioral conditions. If the caregiver responded ‘Yes’ to any one of these five questions, the NSCH flagged the child as having special healthcare needs.
A total of 71,811 interviews were conducted during 2016 and 2017 and were eligible for inclusion in our study. First, we excluded 28,014 children of caregivers that were less than 8 years old (n=43,797) as children under 8 can’t adequately describe their own feelings and therefore clinicians rely on caregiver accounts of child behavior for diagnostic procedures (McGinnis et al., 2019). We also excluded 3,495 children of caregivers that did not answer survey questions related to depression, ACE exposure, or resilience factors. Our final sample size included 40,302 children.
Analyses were conducted for the outcome variable, current depression, and independent exposure variables including: ACE count, child resilience, family remains hopeful, family problem solves together, after school activities, and other adult mentor. First, sample characteristics were presented for the total sample and stratified by current depression. Next, ACE and resilience exposures were presented for the total study population and stratified by current depression. Both analyses were performed using PROC SURVEY FREQ and chi square analysis. Then, multivariate logistic regression models were conducted for each independent exposure variable separately predicting current depression. Lastly, resilience measures with statistically significant results were assessed for their interaction with ACE count on the outcome of depression through multivariate logistic regression. Dummy variables were created for each set of ACE exposure and resilience factor to examine additive and multiplicative interactions. After odds ratios were obtained, the additive interaction was evaluated using the relative excess risk due to interaction (RERIOR) calculation, OR11-OR10-OR01+1, and multiplicative interaction was assessed with the following formula: (OR11/OR10*OR01) (Knol & VanderWeele, 2012). Interaction results are presented using a template developed by Knol and Vanderweele for each set of interaction variables (VanderWeele & Knol, 2014). All logistic regression models were conducted using PROC SURVEY LOGISTIC. Logistic regression results are presented as adjusted odds ratios and wald confidence intervals including variables with statistically significant Pearson chi-square p-values (p<.01) when predicting depression (Table 1) for confounder adjustment.
Table 1.
Characteristics of caregivers to the 2016-2017 National Survey of Children’s Health, in total and stratified by current depression among children, N=40,302
| Characteristic | All N (%a) |
Currently Depressedb N (%) |
Not Currently Depressed N (%) |
P-valuec |
|---|---|---|---|---|
| Total sample | 40302 | 2174 (4.2) | 38128 (95.8) | |
| Sex of child | 0.02 | |||
| Male | 20566 (50.9) | 922 (45.9) | 19644 (51.2) | |
| Female | 19736 (49.1) | 1252 (54.1) | 18484 (48.8) | |
| Age of child | <.01 | |||
| 8 to 10 years old | 9956 (30.3) | 192 (12.2) | 9764 (31.1) | |
| 11 to 13 years old | 11360 (30.0) | 460 (23.9) | 10900 (30.3) | |
| 14 to 17 years old | 18986 (39.6) | 1522 (63.9) | 17464 (38.5) | |
| Race/ethnicity of child | <.01 | |||
| Non-Hispanic White | 28591 (52.3) | 1573 (58.3) | 27018 (52.0) | |
| Non-Hispanic Black | 2377 (13.3) | 129 (14.8) | 2248 (13.3) | |
| Hispanic | 4345 (24.5) | 234 (17.8) | 4111 (24.8) | |
| “Other” Non-Hispanic | 4989 (9.9) | 238 (9.0) | 4751 (9.9) | |
| Child with special healthcare needs | <.01 | |||
| Yes | 11341 (24.2) | 1877 (82.7) | 9464 (21.6) | |
| No | 28961 (75.8) | 297 (17.3) | 28664 (78.4) | |
| Caregiver’s relation to child | <.01 | |||
| Mother | 25791 (65.2) | 1511 (71.8) | 24280 (64.9) | |
| Father | 12560 (28.4) | 453 (16.5) | 12107 (29.0) | |
| Other | 1951 (6.3) | 210 (11.8) | 1741 (6.1) | |
| Caregiver mental health | <.01 | |||
| Excellent, very good, or good | 31865 (76.6) | 1224 (52.4) | 30641 (77.7) | |
| Fair or poor | 2441 (6.1) | 383 (18.6) | 2058 (5.6) | |
| No response | 5996 (17.2) | 567 (29.0) | 5429 (16.7) | |
| Insurance type | <.01 | |||
| Public only | 6999 (29.6) | 711 (45.7) | 6288 (28.9) | |
| Private only | 30330 (59.3) | 1213 (41.4) | 29117 (60.1) | |
| Public and private combination | 1462 (4.8) | 172 (8.3) | 1290 (4.7) | |
| Currently uninsured | 1511 (6.3) | 78 (4.6) | 1433 (6.3) | |
| Caregiver education | 0.30 | |||
| Less than high school/ high school diploma | 6101 (29.5) | 392 (31.8) | 5709 (29.4) | |
| Some college or more | 34201 (70.5) | 1782 (68.2) | 32419 (70.6) | |
| Poverty/income Level | <.01 | |||
| 0-99% Federal Poverty Level | 3918 (19.7) | 336 (28.5) | 3582 (19.3) | |
| 100%-199% Federal Poverty Level | 6000 (21.5) | 427 (23.3) | 5573 (21.5) | |
| 200%-399% Federal Poverty Level | 12235 (27.2) | 644 (23.1) | 11591 (27.4) | |
| 400% Federal Poverty Level or above | 18149 (31.6) | 767 (25.2) | 17382 (31.9) |
Weighted percentages to account for survey design
Respondents answered “Yes” to both questions for inclusion: “Has a health care provider ever told you this child has depression”, “If yes, does it child currently have this condition”
P-values were calculated using Chi-square analysis
To account for the complex survey design of NSCH, survey design features (sampling weights, cluster, and stratum) were used with SAS survey procedures to produce results nationally representative results. As indicated by the NSCH, results are reported in terms of the child rather than for the parent or caregiver, even in cases where the question refers to the caregiver or family. The guidance is based upon the NSCH population weights which are designed to reflect the child population rather than the population of caregivers or families (Data Resource Center for Child and Adolescent Health, 2019). All analyses were conducted using statistical software SAS 9.4 (SAS Institute, Cary, NC) and with a significance level of p <.01 to account for the large sample. This study was approved by the [name concealed for review] institutional review board as exempt.
Results:
The children in this study population were nearly equally divided between males (50.9%) and females (49.1%) and across the three age groups (30%, 30%, and 40% for ages 8-10, 11-13, and 14-17, respectively) (Table 1). The majority of the sample was non-Hispanic White (52.3%) and did not have special healthcare needs (75.8%). A small portion of children had a caregiver who self-reported their mental health as fair or poor (6.1%). Most children had a caregiver respondent who was their mother (65.2%) and who had some college or more (70.5%). Over one-quarter (29.6%) of children had public insurance and nearly twenty percent (19.7%) of children lived below the federal poverty line.
For the study sample, less than five percent of children (4.2%) had current depression and significant differences were found for the following characteristics: sex, age, race/ethnicity, presence of a special healthcare need, caregiver’s relation to child, caregiver mental health, insurance type, and poverty level (Table 2). Depression was more common for females (4.7%), ages 14-17 (6.8%), and non-Hispanic blacks and whites (4.7%, 4.7%, respectively). Children with special healthcare needs were more likely to experience depression (14.5%) than children with no special healthcare needs (1.0%). Children of respondents with fair or poor mental health were most likely to report depression (12.8%) but those who did not respond to the survey question were also more likely to report depression (7.1%) compared to those who reported excellent, very good, or good mental health. Children with public and private insurance combined were more likely to have depression (7.3%) than children with public insurance only (6.5%), those currently uninsured (3.1%), and those with private only (3.0%). Prevalence of depression decreased as poverty/income level increased. Children with a family income of 0-99% Federal Poverty Level were most likely to have current depression (6.1%) while those with family income 400% Federal Poverty Level of above were the least likely (3.4%).
Table 2.
Adverse Childhood Experiences (ACEs) and resilience factors among respondents to the 2016-2017 National Survey of Children’s Health, in total and stratified by current depression among children, N=40,302
| Characteristic | All N (%a) |
Currently Depressedb N (%) |
Not Currently Depressed N (%) |
P-valuec |
|---|---|---|---|---|
| Total sample | 40302 | 2174 (4.2) | 38128 (95.8) | |
| ACE Exposure | ||||
| ACE Countd | <.01 | |||
| Less than 4 | 37669 (92.3) | 1629 (72.2) | 36040 (93.2) | |
| 4 or more | 2633 (7.7) | 545 (27.8) | 2088 (6.8) | |
| Resilience Factors | ||||
| Child Resiliencee | <.01 | |||
| Definitely true or somewhat true | 37844 (93.2) | 1541 (66.3) | 36303 (94.4) | |
| Not true | 2458 (6.8) | 633 (33.7) | 1825 (5.6) | |
| Family Problem Solves Togetherf | <.01 | |||
| Almost all of the time or most of the time | 34677 (86.0) | 1535 (67.4) | 33142 (86.9) | |
| Some of the time or none of the time | 5625 (14.0) | 639 (32.6) | 4986 (13.1) | |
| Family Remains Hopefulg | <.01 | |||
| Almost all of the time or most of the time | 37452 (93.2) | 1708 (80.0) | 35744 (93.7) | |
| Some of the time or none of the time | 2850 (6.8) | 466 (20.0) | 2384 (6.3) | |
| After School Activitiesh | <.01 | |||
| Yes | 36223 (85.0) | 1702 (77.9) | 34521 (85.3) | |
| No | 4079 (15.0) | 472 (22.1) | 3607 (14.7) | |
| Other Adult Mentori | 0.03 | |||
| Yes | 37644 (89.7) | 1958 (86.5) | 35686 (89.9) | |
| No | 2658 (10.3) | 216 (13.5) | 2442 (10.1) | |
Weighted percentages to account for survey design
Respondents answered “Yes” to both questions for inclusion: “Has a health care provider ever told you this child has depression”, “If yes, does it child currently have this condition”
P-values were calculated using Chi-square analysis
ACE count includes all types of ACEs collected by survey: parental separation/divorce, parental death, household incarceration, witness household violence, witnessed neighborhood violence, household mental illness, household substance use, racial/ethnic mistreatment, and economic hardship
Respondents answer to “This child stays calm and control when faced with a challenge”
Respondents answer to “When your family faces problems how likely are you to work together to solve problems”
Respondents answer to “When your family faces problems how likely are you to stay hopeful even in difficult situations”
Respondents answer to “During the past 12 months did this child participate in sports, clubs, lessons after school” and or “volunteer at church, community, or school”
Respondents answer to “Other than adults in your home, is there at least 1 other adult who they can rely on for guidance and support”
Preliminary analysis using chi square tests, showed that ACE count and all resilience factors except the presence of an adult mentor were significantly associated with current depression among children ages 8-17. Among children who were currently depressed, almost 30% reported an ACE count of four or more compared to only 7% of children without current depression (Table 2). Children who were currently depressed were also less likely to report child resilience (66.3% vs. 94.4%), that the family problem solves together (67.4% vs. 86.9%), and their family remains hopeful (80.0% vs. 93.7%). After school activities were also report less often for children with current depression than those without depression (77.9% vs. 85.3%).
After adjusting for confounders, four exposures remained significantly associated with current depression including: ACE count, child resilience, family problem solves toether, and family remains hopeful (Table 3). Compared to children exposed to less than four ACEs, children exposed to four or more ACEs had higher odds of depression (aOR 2.29; CI: 1.74-3.02). The absence of child resilience was associated with almost four times greater odds of depression when compared to children with resilience (aOR 3.74; CI: 2.88-4.84). Compared to children whose family problem solves together often, children whose family problem solve together less often had a higher odds of depression (aOR 2.09; CI: 1.62-2.70). Lastly, children with a family that remains hopeful less often had a higher odds of depression (aOR 2.20; CI: 1.63-2.97) compared to children whose family remained hopeful more often.
Table 3.
Adjusted odds ratios and 95% Wald confidence intervals predicting current depression by Adverse Childhood Experiences (ACEs) and resilience factors, among respondents to 2016-2017 National Survey of Children’s Health survey, N=40,302
| Characteristic | Current Depressiona |
|---|---|
| aORb (95% CI)c | |
| Model 1: | |
| Ace Countd | |
| Less than four ACEs | Referent |
| Four or more ACEs | 2.29 (1.74-3.02) |
| Model 2: | |
| Child Resiliencee | |
| Definitely true or somewhat true | Referent |
| Not true | 3.74 (2.88-4.84) |
| Model 3: | |
| Family Problem Solves Togetherf | |
| Almost all of the time or some of the time | Referent |
| Some of the time or none of the time | 2.09 (1.62-2.70) |
| Model 4: | |
| Family Remains Hopefulg | |
| Almost all of the time or some of the time | Referent |
| Some of the time or none of the time | 2.20 (1.63-2.97) |
| Model 5: | |
| After School Activitiesh | |
| Yes | Referent |
| No | 1.08 (0.83-1.40) |
| Model 6: | |
| Other Adult Mentori | |
| Yes | Referent |
| No | 1.25 (0.86-1.83) |
Respondents answered “Yes” to both questions for inclusion: “Has a health care provider ever told you this child has depression”, “If yes, does it child currently have this condition”
Adjusted odds ratio adjusted for child and respondent characteristics: race, age, relation to child, insurance, adult education, special health care needs, and caregiver mental health
95% CI = 95% Wald confidence intervals; bold indicates significance at <.05 level
ACE count includes all types of ACEs collected by survey: parental separation/divorce, parental death, household incarceration, witness household violence, witnessed neighborhood violence, household mental illness, household substance use, racial/ethnic mistreatment, and economic hardship
Respondents answer to “This child stays calm and control when faced with a challenge”
Respondents answer to “When your family faces problems how likely are you to work together to solve problems”
Respondents answer to “When your family faces problems how likely are you to stay hopeful even in difficult situations”
Respondents answer to “During the past 12 months did this child participate in sports, clubs, lessons after school” and or “volunteer at church, community, or school”
Respondents answer to “Other than adults in your home, is there at least 1 other adult who they can rely on for guidance and support”
An assessment of interaction using multivariate logistic regression demonstrated significant interactions between ACE count and three resilience measures. Compared to children exposed to less than four ACEs with some resilience, children exposed to greater than four ACEs that don’t exhibit resilience had an 8.75 higher odds of depression (CI: 5.23-14.65) (Figure 1, Supplemental Table 1). The absence of child resilience also increased the odds of depression among children exposed to less than four ACEs (aOR 3.91; CI: 2.94-5.19). The interaction of child resilience and ACE count on depression showed a positive interaction on the additive scale and a negative interaction on the multiplicative scale (Figure 2). Compared to children exposed to less than four ACEs with a family that problem solves together often, a lack of family problem solving increased the odds of depression even among children exposed to less than four ACEs (aOR 2.48; CI 1.88-3.27) and more for those exposed to four or more ACEs (aOR 3.59; CI:2.06-6.25) (Figure 1, Supplemental Table 2). The interaction of family problem solving and ACE count on depression showed a negative interaction on both scales (Figure 2). Compared to children exposed to less than four ACEs with a family that remains hopeful most of the time, children exposed to greater than four ACEs with a family that remains hopeful less often had a greater odds of depression (aOR 3.74; CI: 2.11-6.63) (Figure 1, Supplemental Table 3). The interaction of family hopefulness and ACE count on depression showed a negative interaction on both scales (Figure 2).
Figure 1:
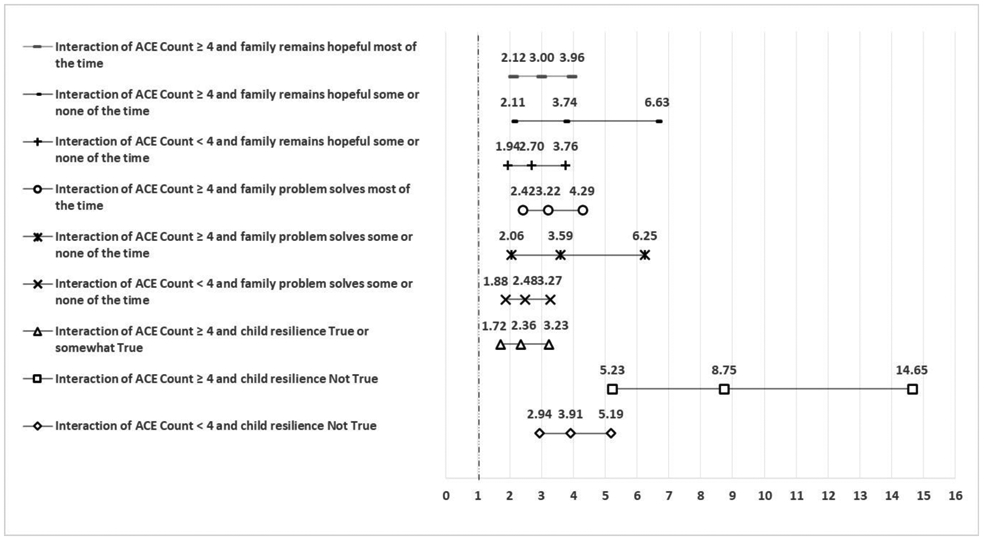
Interaction of Adverse Childhood Experiences (ACEs) and resilience factors predicting current depression, among respondents to 2016-2017 National Survey of Children’s Health survey, N=40,302. Values represent adjusted odds ratios (aORs) adjusted for child and respondent characteristics including: race, age, relation to child, insurance, adult education, special health care needs, and caregiver mental health.
Figure 2:
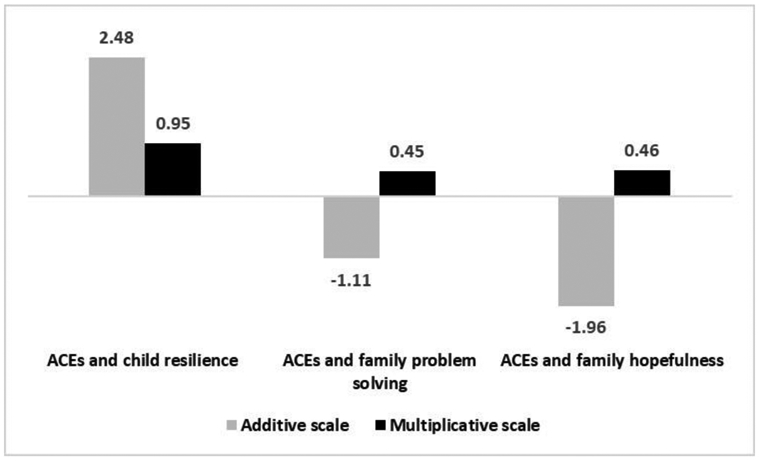
Additive and multiplicative interactions between Adverse Childhood Experiences (ACEs) and resilience factors predicting current depression, among respondents to 2016-2017 National Survey of Children’s Health survey, N=40,302. Values represent adjusted odds ratios (aORs) adjusted for child and respondent characteristics including: race, age, relation to child, insurance, adult education, special health care needs, and caregiver mental health.
Discussion:
There is a substantial body of evidence linking childhood ACE exposure to poor mental health during adulthood, with limited research on specific mental health outcomes among children and adolescents with ACE exposure. Prior studies examining the role of PCEs and other resilience measures in the prevention of poor mental health among children and adolescents exposed to ACEs focused on youth with substance abuse or adolescent pregnancy, not specifically depression (Hillis et al., 2010, Kosterman et al., 2011). The current study fills this gap by providing recent, nationally representative estimates of depression among children ages 8-17 and evaluates their association with ACE exposure and multiple measures of resiliency.
Our study found higher rates of current depression among children and adolescents than prior studies, with 4.2% of children with current depression, compared to a previous study using the NSCH 2011-2012 data among a similar age group which found 2.8% had depression (Porche et al., 2016). Consistent with a previous study among the same age group, we found that exposure to ACEs was common among children and adolescents and those with current depression were more likely to be exposed to ACEs than those without (Elmore & Crouch, 2020). Furthermore, we found the absence of resilience measures representing a child’s emotional competence (child resilience) and development in a safe, stable environment (family problem solves together and family remains hopeful) were significantly associated with depression in children and adolescents. Therefore, our study highlights the importance of these specific resilience factors because even if the burden of depression is not completely removed by PCEs, the presence of PCEs may lessen the severity of depression symptoms (Agenor et al., 2017).
Interaction analyses demonstrated that child resiliency and a safe, stable environment may be protective against ACE exposure. We found that among children and adolescents with ≥4 ACEs, the presence of child resiliency reduced the odds of depression fourfold. This finding is consistent with previous literature demonstrating child resilience and parental engagement attenuated the impact of ACEs on emotional, mental, or behavioral conditions among children (Bethell et al., 2016). Our study builds upon this knowledge specifically for the mental health outcome of depression and advances our understanding of this association by assessing interaction on an additive and multiplicative scale. The presence of interaction on the additive scale represents the public health significance on an individual level (VanderWeele & Knol, 2014). Therefore, our study demonstrates building child resiliency and ensuring children have a supportive environment can reduce the impact of ACEs on depression. The additive interaction scale also helps determine which groups would benefit the most from an intervention (VanderWeele & Knol, 2014). We found that intervention strategies to reduce depression for children exposed to ACEs are dependent upon the type of resilience measure. Based on the positive additive interaction between child resilience and ACE count exposure, our findings suggest interventions to prevent depression among children are most beneficial for those without child resilience. In contrast, the negative interaction between family problem solving and family hopefulness with ACE count exposure indicates interventions to reduce depression are best for children with these resilience factors present. This negative additive interaction indicates the combined effect of ACE exposure and a lack of family resilience was less than the sum of their separate effects. Future studies should further assess the mechanisms of this finding.
Our study illustrates the need for the promotion of PCEs and the building of child resiliency for combatting depression and reducing the impact of trauma in children and adolescents. The promotion of PCEs demonstrates the advancements in prevention science for reducing the consequences of ACEs but the creation of PCEs is necessary to build such resilience in the child and in their family (Shonkoff, 2016). Yet, the creation and promotion of PCEs is dependent on both the engagement of families and communities, as well as stakeholders in healthcare, education, and social services. Thus, new and continued efforts to measure current PCE in local communities, states, and nationally is needed. The measurement of PCEs and the role they may play in the mitigation of poor mental health outcomes among children and youth with ACEs helps to improve endeavors to identify intervention and engagement strategies (Leitch, 2017). State level measurement of both ACEs and PCEs, such as the recent California Medicaid program ACE and PCE screenings, is one strategy for developing targeted efforts in individual states (California Pan Ethnic Health Network, 2019).
Child service professionals and programs can find recommendations of policies and initiatives which foster PCEs in the National Bright Futures Guidelines for Health Supervision of Infants, Childs, and Adolescents (Hagan et al., 2017). These guidelines may assist child serving professionals and programs in determining which proposals for encouraging PCEs are most effective. Bright Futures highlights the importance of fostering open, supportive communication between the parent and child to develop shared goals and a joint plan of action based on the goals (Hagan et al., 2017). In addition, the Health Outcomes of Positive Experiences (HOPE) framework and the Prioritizing Possibilities agenda both purport the extension and implementation of evidence based proposals for PCE promotion in human service, clinical, and public health settings (Bethell et al., 2017, National Scientific Council on the Developing Child, 2019). Examples of these evidence based approaches include family focused prevention interventions and clinical pediatric practice guidelines (Leslie et al., 2016, Rayce et al., 2017, Traub & Boynton-Jarrett, 2017). Prior research has suggested that PCEs may reduce the burden of mental illness, such as depression, even if the mental illness is not completely gone (Bethell et al., 2019). Our results raise questions for further exploration on the mechanism by which PCEs promote social and emotional support in order to promote positive mental health.
Strengths and Weaknesses
This study is not without limitations. As a cross-sectional study, our results should not be used to form casual inferences and conclusions. Also, the NSCH asks caregivers about their children, so information on neglect and physical, emotional, or sexual abuse is not included. Due to caregiver bias, the report of ACE exposures may be underreported or overreported. The restriction of our outcome measure to current mental conditions was done to reduce the bias of temporality, but we cannot know whether the exposure or outcome occurred first. Also, secondary data analysis is subject to selective participation which could be related to both outcomes measures and ACE exposures. Thus, our findings may be under or overestimated based on non-response bias. Participation in the NSCH is limited to those with an address and transient or homeless children are not included in our sample. Lastly, our assessments of adverse experiences and resiliency are limited to the categories included in our study and may not be generalizable to other types of ACEs and PCEs.
Our study also has multiple strengths. To our knowledge, the NSCH is the first nationally representative study of children to measure depression, ACEs, and resiliency. By utilizing the combined 2016-2017 NSCH, we included a larger sample size allowing for the analysis of conditions with low prevalence. We also implemented a recently developed epidemiological assessment tool to measure interaction on both the additive and multiplicative scale. Lastly, caregiver report of ACE and resilience exposure provides more timely information to develop intervention efforts than retrospective interviews during adulthood.
Conclusion:
Our study adds to the growing body of literature demonstrating the positive relationship between PCEs and improved health outcomes among children with ACE exposure. By assessing the association between PCEs and depression among children and youth with ACEs, we expand the current literature while filling a critical gap. Our findings are important for the advancement and implementation of evidence-based approaches to build child and family resilience and may be used by policy makers and child serving professionals to target interventions to subgroups of children and youth who would most benefit.
Supplementary Material
Highlights:
Adverse childhood experiences are common and associated with childhood depression
Resilience factors may moderate the relationship between ACEs and childhood depression
Interaction analyses showed higher resilience may reduce the impact of ACEs on depression
New and continued efforts to develop and measure resiliency interventions are needed
Acknowledgments
This publication was made possible in part by Grant Number T32-GM081740 from NIH-NIGMS. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIGMS or NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of Interest: None
References
- Agenor C, Conner N, & Aroian K (2017). Flourishing: An Evolutionary Concept Analysis. Issues Ment Health Nurs, 35(11), 915–923. https://doi:10.1080/01612840.2017.1355945 [DOI] [PubMed] [Google Scholar]
- Angst J, Gamma A, Rossler W, Ajdacic V, Klein DN (2011). Childhood adversity and chronicity of mood disorders. Eur Arch Psychiatry Clin Neurosci, 261(1), 21–27. https://doi:10.1007/s00406-010-0120-3 [DOI] [PubMed] [Google Scholar]
- Bethell C, Gombojav N, Solloway M, Wissow L (2016). Adverse Childhood Experiences, Resilience and Mindfulness-Based Approaches: Common Denominator Issues for Children with Emotional, Mental, or Behavioral Problems. Child Adolesc Psychiatr Clin N Am, 25(2), 139–156. https://doi:10.1016/j.chc.2015.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bethell C, Jones J, Gombojav N, Linkenbach J, Sege R (2019). Positive Childhood Experiences and Adult Mental and Relational Health in a Statewide Sample: Associations Across Adverse Childhood Experiences Levels. JAMA Pediatr, e193007 https://doi:10.1001/jamapediatrics.2019.3007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bethell CD, Solloway MR, Guinosso S, Hassink S, Srivastav A, Ford D, Simpson LA (2017). Prioritizing Possibilities for Child and Family Health: An Agenda to Address Adverse Childhood Experiences and Foster the Social and Emotional Roots of Well-being in Pediatrics. Acad Pediatr, 17(7S), S36–S50. https://doi:10.1016/j.acap.2017.06.002 [DOI] [PubMed] [Google Scholar]
- National Scientific Council on the Developing Child. (2019). Supportive relationships and active skill-building strengthen the foundations of resilience: working paper 13. Center on the Developing Child Harvard University; https://developingchild.harvard.edu/wp-content/uploads/2015/05/The-Science-of-Resilience.pdf [Google Scholar]
- Chung EK, Mathew L, Elo IT, Coyne JC, Culhane JF (2008). Depressive symptoms in disadvantaged women receiving prenatal care: the influence of adverse and positive childhood experiences. Ambul Pediatr, 8(2), 109–116. https://doi:10.1016/j.ambp.2007.12.003 [DOI] [PubMed] [Google Scholar]
- Crouch E, Probst JC, Radcliff E, Bennett KJ, McKinney SH (2019). Prevalence of adverse childhood experiences (ACEs) among US children. Child Abuse Negl, 92, 209–218. https://doi:10.1016/j.chiabu.2019.04.010 [DOI] [PubMed] [Google Scholar]
- Elmore AL, & Crouch E (2020). The Association of Adverse Childhood Experiences with Anxiety and Depression for Children and Youth, 8 to 17 Years of Age. Acad Pediatr. https://doi:10.1016/j.acap.2020.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairbank JA, & Fairbank DW (2009). Epidemiology of child traumatic stress. Curr Psychiatry Rep, 11(4), 289–295. https://doi:10.1007/s11920-009-0042-9 [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS (2019). Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study. Am J Prev Med, 56(6), 774–786. https://doi:10.1016/j.amepre.2019.04.001 [DOI] [PubMed] [Google Scholar]
- Gilman SE, Trinh NH, Smoller JW, Fava M, Murphy JM, Breslau J (2013). Psychosocial stressors and the prognosis of major depression: a test of Axis IV. Psychol Med, 43(2), 303–316. https://doi:10.1017/S0033291712001080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan JF, Shaw JS, Duncan PM (2017). Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. (Third ed.). Elk Grove Village, IL: American Academy of Pediatrics. [Google Scholar]
- Happer K, Brown EJ, Sharma-Patel K (2017). Children's resilience and trauma-specific cognitive behavioral therapy: Comparing resilience as an outcome, a trait, and a process. Child Abuse Negl, 73, 30–41. https://doi:10.1016/j.chiabu.2017.09.021 [DOI] [PubMed] [Google Scholar]
- Data Resource Center for Child and Adolescent Health. (2019). The National Survey of Children's Health, 2019. https://www.childhealthdata.org/learn-about-the-nsch/NSCH
- Hill J, Pickles A, Rollinson L, Davies R, Byatt M (2004). Juvenile- versus adult-onset depression: multiple differences imply different pathways. Psychol Med, 34(8), 1483–1493. https://doi:10.1017/s0033291704002843 [DOI] [PubMed] [Google Scholar]
- Hillis SD, Anda RF, Dube SR, Felitti VJ, Marchbanks PA, Macaluso M, & Marks JS (2010). The Protective Effect of Family Strengths in Childhood against Adolescent Pregnancy and Its Long-Term Psychosocial Consequences. Perm J, 14(3), 18–27. https://doi:10.7812/tpp/10-028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerker BD, Zhang J, Nadeem E, Stein RE, Hurlburt MS, Heneghan A, Landsverk J, McCue Horwitz S (2015). Adverse Childhood Experiences and Mental Health, Chronic Medical Conditions, and Development in Young Children. Acad Pediatr, 15(5), 510–517. https://doi:10.1016/j.acap.2015.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knol MJ, & VanderWeele TJ (2012). Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol, 41(2), 514–520. https://doi:10.1093/ije/dyr218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosterman R, Mason WA, Haggerty KP, Hawkins JD, Spoth R, Redmond C (2011). Positive childhood experiences and positive adult functioning: prosocial continuity and the role of adolescent substance use. J Adolesc Health, 49(2), 180–186. https://doi:10.1016/j.jadohealth.2010.11.244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M, Obrosky S, George C (2016). The course of major depressive disorder from childhood to young adulthood: Recovery and recurrence in a longitudinal observational study. J Affect Disord, 203, 374–381. https://doi:10.1016/j.jad.2016.05.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leitch L (2017). Positive and Adverse Childhood Experiences Survey (PACES): threshold global works, https://www.thresholdglobalworks.com/portfolio-items/paces-survey/
- Leslie LK, Mehus CJ, Hawkins JD, Boat T, McCabe MA, Barkin S, Perrin EC, Metzler CW, Prado G, Tait VF, Brown R, Beardslee W (2016). Primary Health Care: Potential Home for Family-Focused Preventive Interventions. Am J Prev Med, 51(4 Suppl 2), S106–118. https://doi:10.1016/j.amepre.2016.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinnis RS, McGinnis EW, Hruschak J, Lopez-Duran NL, Fitzgerald K, Rosenblum KL, Muzik M (2019). Rapid detection of internalizing diagnosis in young children enabled by wearable sensors and machine learning. PLos One, e0210267 https://doi:10.1371/journal.pone.0210267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKelvey LM, Conners Edge NA, Fitzgerald S, Kraleti S, Whiteside-Mansell L (2017). Adverse childhood experiences: Screening and health in children from birth to age 5. Fam Syst Health, 35(4), 420–429. https://doi:10.1037/fsh0000301 [DOI] [PubMed] [Google Scholar]
- California Pan Ethnic Health Network. (2019). Governor Newsom’s budget makes important investments in health equity and prevention, https://cpehn.org/blog/201901/governor-newsom%E2%80%99s-budget-makes-important-investments-health-equity-and-prevention [Google Scholar]
- Porche MV, Costello DM, Rosen-Reynoso M (2016). Adverse Family Experiences, Child Mental Health, and Educational Outcomes for a National Sample of Students. School Mental Health, 8(1), 44–60. https://doi:10.1007/s12310-016-9174-3 [Google Scholar]
- Rayce SB, Rasmussen IS, Klest SK, Patras J, Pontoppidan M (2017). Effects of parenting interventions for at-risk parents with infants: a systematic review and meta-analyses. BMJ Open, 7(12), e015707 https://doi:10.1136/bmjopen-2016-015707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salk RH, Hyde JS, Abramson LY (2017). Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychol Bull, 143(8), 783–822. https://doi:10.1037/bu10000102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sege RD, & Harper Browne C (2017). Responding to ACEs With HOPE: Health Outcomes From Positive Experiences. Acad Pediatr, 17(7S), S79–S85. https://doi:10.1016/j.acap.2017.03.007 [DOI] [PubMed] [Google Scholar]
- Shanahan L, Copeland WE, Costello EJ, Angold A (2011). Child-, adolescent- and young adult-onset depressions: differential risk factors in development? Psychol Med, 41(11), 2265–2274. https://doi:10.1017/S0033291711000675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP (2016). Capitalizing on Advances in Science to Reduce the Health Consequences of Early Childhood Adversity. JAMA Pediatr, 170(10), 1003–1007. https://doi:10.1001/jamapediatrics.2016.1559 [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, Garner AS, The Committee on Psychosocial Aspects of Child and Family Health., Committee on Early Childhood, Adoption, and Dependent Care, and Section on Developmental and Behavioral Pediatrics., Siegel BS, Dobbins MI, Earls MF, Garner AS, McGuinn L, Pascoe J, Wood DL (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1), e232–246. https://doi:10.1542/peds.2011-2663 [DOI] [PubMed] [Google Scholar]
- Traub F, & Boynton-Jarrett R (2017). Modifiable Resilience Factors to Childhood Adversity for Clinical Pediatric Practice. Pediatrics, 139(5). https://doi:10.1542/peds.2016-2569 [DOI] [PubMed] [Google Scholar]
- VanderWeele TJ, & Knol MJ (2014). A Tutorial on Interaction. Epidemiologic Methods, 3(1). https://doi:10.1515/em-2013-0005 [Google Scholar]
- Vibhakar V, Allen LR, Gee B, Meiser-Stedman R (2019). A systematic review and meta-analysis on the prevalence of depression in children and adolescents after exposure to trauma. J Affect Disord, 255, 77–89. https://doi:10.1016/j.jad.2019.05.005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


