Abstract
Objectives
Smoking has many deleterious consequences on health, one of which can be sleep-related issues. Therefore, a meta-analysis was performed with the aim of pooling results from studies on the relationship between smoking and sleep-related issues.
Methods
The present study follows PRISMA guidelines. Databases were searched by both researchers to find the articles. The review was done up to December 2018. In order to analyze the results of the screened articles, statistical indexes were converted to logarithms and the studies were combined with each other. Finally, several analyses were conducted with respect to various subgroups. In the subgroup analysis, the pool index of the studies was determined and the degree of heterogeneity in each subgroup was presented. Meta-regression was also used.
Results
Smoking is associated with a risk of developing sleep-related issues. Risk ratio (1.47; 1.20–1.79) for smokers was higher than for non-smokers. Egger’s test and Begg’s test indicated publication bias.
Conclusions
Smoking is associated with sleep-related issues. Informing smokers about the effects of smoking on sleep issues can be effective in reducing and preventing its consequences.
Keywords: Smoking, Sleep, Sleep-related issues, Sleep disturbances, Systematic review, Meta-analysis
Résumé
Objectifs
Le tabagisme a de nombreuses conséquences délétères sur la santé, et les problèmes liés au sommeil peuvent en faire partie. Nous avons effectué une méta-analyse en vue de regrouper les résultats d’études sur la relation entre le tabagisme et les problèmes liés au sommeil.
Méthode
Notre étude suit les lignes directrices PRISMA. Les deux chercheurs ont interrogé des bases de données pour trouver les articles. La revue a été menée jusqu’en décembre 2018. Pour analyser les résultats des articles filtrés, des indices statistiques ont été convertis en logarithmes, et les études ont été combinées entre elles. Enfin, plusieurs analyses ont été effectuées pour divers sous-groupes. Dans les analyses des sous-groupes, nous avons déterminé l’indice des études regroupées et présenté le degré d’hétérogénéité dans chaque sous-groupe. Nous avons aussi utilisé la méta-régression.
Résultats
Le tabagisme est associé à un risque de contracter des problèmes liés au sommeil. Le risque relatif (1,47; 1,20-1,79) des fumeurs était supérieur à celui des non-fumeurs. Le test d’Egger et le test de Begg ont montré un biais de publication.
Conclusions
Le tabagisme est associé à des problèmes liés au sommeil. Informer les fumeurs des effets du tabagisme sur les problèmes de sommeil peut être un moyen efficace d’en réduire et d’en prévenir les conséquences.
Mots-clés: Fumer, Sommeil, Problèmes liés au sommeil, Perturbations du sommeil, Revue systématique, Méta-analyse
Introduction
Sleeping is one of the most important aspects of life and any disruption in it can have deleterious consequences (Roberts et al. 2009). Sleep disturbance, especially insomnia disorder, is an important health problem (Pandi-Perumal et al. 2006). Sleep disorders are associated with poor quality of life and the important aspects of physical and mental problems (Hertenstein et al. 2018; Kim et al. 2016; Milojevich and Lukowski 2016; Sivertsen et al. 2014; Thomas et al. 2017; Troxel et al. 2007) such as obesity, diabetes and depression (Anothaisintawee et al. 2016; Baglioni et al. 2011; Beccuti and Pannain 2011; Hargens et al. 2013; Li et al. 2016; Martinez-Gomez et al. 2013; Sakamoto et al. 2017; Sivertsen et al. 2012). One of the sleep problems is insomnia (Thorpy 2012) which is visible in the general population (Ford and Kamerow 1989; Ohayon and Bader 2010), and its prevalence in the elderly population is reported to be between 20% and 40% (Foley et al. 1995; Liu and Liu 2005; Maggi et al. 1998; Ohayon et al. 2001).
In 2015, smoking was one of the major risk agents of death and disability worldwide (Forouzanfar et al. 2016). Smoking plays an important role in increasing the burden of disease, especially in low-income countries (Forouzanfar et al. 2016). Age-standardized prevalence of daily smoking has been reported as 25% for men and 5.4% for women (Reitsma et al. 2017). 11.5% of global deaths were due to smoking in 2015 (Reitsma et al. 2017). Smoking is associated with an increased risk of various diseases, including cancer (O’Keeffe et al. 2018; Sugawara et al. 2018), diabetes (Liu et al. 2018a, b), respiratory health (Jayes et al. 2016), stroke (Haheim et al. 1996; Peters et al. 2013) and coronary heart disease (Huxley and Woodward 2011).
Review studies also address the risk factors of sleep-related issues (Al Lawati et al. 2009; Bartel et al. 2015; Jaehne et al. 2009; Smagula et al. 2016; Taveira et al. 2018; van de Wouw et al. 2012; Xiaolin Gu 2017; Yang et al. 2017). A recent published meta-analysis on obstructive sleep apnea and tobacco did not report a significant association (Taveira et al. 2018). Insomnia carries the risk of being unable to quit smoking (Short et al. 2017) and nicotine can also affect sleep via neurotransmitters (Jaehne et al. 2015) and it can increase arousal and the difficulty in initiating sleep (Kishimoto and Domino 1998). The studies have examined the role of smoking in relation to sleep-related issues, especially insomnia disorder and poor sleep quality. But most studies which have been conducted on the effects of smoking on sleep disorders are based on cross-sectional studies (Ban and Lee 2001; Cohen et al. 2018; Conway et al. 2008; Fritsch Montero et al. 2010; Gomes Felden et al. 2017; Harma et al. 1998; Kageyama et al. 2017; Zhang et al. 2017). Cross-sectional studies are not very desirable for researchers due to not providing a complete understanding of the research design, fear of bias, and ambiguity about the relationship between the dimensions being measured (Reichenheim and Coutinho 2010; Shahar and Shahar 2013). The systematic review, along with meta-analysis, is considered the best method of synthesizing the scientific evidence (Haddaway and Watson 2016) and can provide more reliable findings (Antman et al. 1992; Oxman and Guyatt 1993). On the other hand, studies on the effects of smoking on sleep-related issues have not yet been pooled to clarify the ambiguities. The purpose of the current study was to determine the effects of smoking on sleep-related issues based on systematic review and meta-analysis.
Materials and methods
The PRISMA (Moher et al. 2009) checklist was used to examine the risk of sleep-related issues among smokers. This checklist contains a collection of items needed for meta-analysis.
Search in databases
Four databases were searched by the researchers (current study authors SA and SB) to find articles related to the research topic. The databases include PubMed, Scopus, ResearchGate and Google Scholar, which were searched according to the keywords. The words used for this purpose are listed in Table 1. The researchers prospectively and independently searched the databases up to December 2018. SA searched two databases (PubMed, ResearchGate) and SB searched two other databases (Scopus, Google Scholar) to find articles. The researchers screened articles they found on their own searched databases; in cases where there was a difference of opinion between them with regard to whether or not the article in question met the inclusion criteria, the matter was discussed until agreement was reached. After independent screening of the papers, the researchers finally reached a consensus on each article.
Table 1.
Keywords used for search up to December 2018
| #1 | Sleep Disorders [Mesh] OR Sleep Disorders [Text Word] OR Sleep Disorder [Mesh] OR Sleep Disorder [Text Word] OR Insomnia [Mesh] OR Insomnia [Text Word] OR Sleeplessness [Mesh] OR Sleeplessness [Text Word] OR Sleep disturbance [Mesh] OR Sleep disturbance [Text Word] OR Narcolepsy [Mesh] OR Narcolepsy [Text Word] OR Narcoleptic Syndrome [Mesh] OR Narcoleptic Syndrome [Text Word] OR Hypersomnia [Mesh] OR Hypersomnia [Text Word] OR Apnea [Mesh] OR Apnea [Text Word] OR restless legs syndrome [Text Word] OR restless legs syndrome [Mesh] OR Obstructive sleep apnea [Mesh] OR Obstructive sleep apnea [Text Word] OR Snoring [Mesh] OR Snoring [Text Word] sleep related breathing disorders [Text Word] OR Central sleep apnea [Text Word] OR Parasomnias [Text Word] OR Sleepwalking [Text Word] OR Sleep terrors [Text Word] OR Sleep Eating Disorder [Text Word] OR Sleep paralysis [Text Word] OR nightmares [Text Word] OR Sleep talking [Text Word] OR Circadian Rhythm Sleep-Wake Disorders |
| #2 | Cigarette smoking [Mesh] OR Cigarette smoking [Text Word] OR Tobacco Smoking [Mesh] OR Tobacco Smoking [Text Word] OR Tobacco Use [Mesh] OR Tobacco Use [Text Word] OR Pipe Smoking [Mesh] OR Pipe Smoking [Text Word] OR Cigar Smoking [Mesh] OR Cigar Smoking [Text Word] OR Cigarette consumption [Mesh] OR Cigarette consumption [Text Word] OR nicotine [Mesh] OR nicotine [Text Word] |
Selection criteria
Only studies with prospective designs were considered eligible for inclusion. Studies that measured baseline smoking and also assessed sleep-related issues at the end of the line were eligible for the current study as well. Smoking includes cigarette smoking, nicotine dependence and smoking habits; it also involves the following classes: ever-smokers, chronic smokers, heavy smokers, moderate smokers, experimenter smokers, established smokers, current smokers and former smokers. Smoking was considered as an exposure variable. All of the studies that measured smoking based on self-report or clinical evaluation were eligible for inclusion. Outcome variables included in this research were sleep-related issues. Sleep-related issues must be measured at the finishing line in eligible studies. This category of sleep problems included insomnia, sleep disturbances, sleep complaints, daytime sleepiness, sleep apnea, narcolepsy, and sleep difficulty. Age greater than or equal to 12 was considered. In articles with the same database, only one article with the highest quality was selected and other articles were excluded.
Extraction
Both researchers independently extracted all of the papers’ information and the differences were resolved by discussion. This checklist relates to the data extraction along with the details which are presented in Table 2.
Table 2.
Studies included in the meta-analysis
| First author and year of publication | Country | Population | Follow-up time | Age range | Sex | Sample size | Smoking | Sleep-related issues | Quality assessment: risk of bias | Results | Adjustment for other covariates | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Selection | Confounders | Performance bias | Data collection method | Withdrawals and dropouts | |||||||||||
| Chen et al. 2017 | Taiwan | General population | 7 years | ≥ 18 | 46.6% women | 12,728 | Self-reported | Clinically diagnosed (insomnia) | Low | Moderate | Moderate | Low | Low |
Hazard ratio Ever-smoker 1.45 (CI 1.20–1.76) |
Socio-demographic, health-related variables |
| Haario et al. 2013 | Finland | General population | 5 years | 40–60 at baseline | 81.3% women | 6458 | Unknown | Four-item Jenkins Sleep Questionnaire (insomnia) | Low | Low | Moderate | Moderate | Low |
Odds ratio 1.06 (CI 0.91–1.23) |
Age, gender, baseline insomnia symptoms, marital status, occupational class, sleep duration, common mental disorders |
| Lee et al. 2016 | USA | General population | 23 years | 14–32 | 60% women | 674 | Self-reported |
Insomnia Severity Index measure (insomnia) |
High | Moderate | Moderate | Moderate | Low |
Odds ratio Chronic smokers 2.69 (CI 1.06–6.82) Moderate smokers 5.33 (CI 1.94–14.64) |
Sex, ethnicity, depressive symptoms, age, educational level, partner status, BMI |
| Nordmann et al. 2016 | France | Opiate dependence | 1 year | 31.9–34.3 | 16.05% women | 162 | Nicotine dependence | Center for Epidemiological Studies Depression; Opiate Treatment Index (OTI) questionnaire (sleep disturbance) | High | High | Moderate | Moderate | Low |
Odds ratio Nicotine dependence Moderate Sleep disturbance 3.44 (CI 1.46–8.11) Severe sleep disturbance 5.46 (CI 2.29–13.03) |
Multivariate analysis |
| Patten et al. 2000 | USA | General population | 4 years | 12–18 | 49.3% women | 7960 | Standard question | TAPS questionnaire (sleep disturbance) | Low | High | Moderate | Moderate | Low |
Odds ratio Experimenter 1.20 (CI 1.03–1.40) Established smoker 1.47 (CI 1.16–1.87) |
Multivariate analysis |
| Phillips and Mannino 2005 | USA | General population | 9 years | 45–69 | 55.2% women | 13,564 | Self-reported |
Maastricht Questionnaire (sleep complaints) |
Low | Low | Moderate | Moderate | Low |
Odds ratio Current smoking 1.20 (CI 1.04–1.30) 0.80 (CI 0.70–0.90) 1.00 (CI 0.90–1.20) Former smoking 0.90 (CI 0.80–0.96) 1.00 (CI 0.90–1.10) 0.90 (CI 0.80–1.01) |
Age, sex, menopausal status, race, education level, income, body mass index, depression, presence of cardiac disease, lung function status, presence of hypertension, alcohol intake, diabetes, and hypnotic use |
| Theorell-Haglow et al. 2015 | Sweden | General population | 10 years | 43.7 ± 15.2 | Women | 7051 | Six questions | Uppsala Sleep Inventory; Self-reported (excessive daytime; sleepiness) | Low | High | Moderate | Moderate | Low |
Odds ratio Current smoking 7.27 (CI 2.57–20.5) |
Age, development in all covariates, somatic disease |
| Janson et al. 2001 | Sweden | General population | 10 years | 30–69 | Men | 2602 | questions | Questionnaire (sleep disturbances) | Moderate | Moderate | Moderate | Moderate | Moderate |
Odds ratio Ever-smoker 1.06 (CI 0.92–1.71) |
Medical disorder, BMI, physically inactive, alcohol dependent |
| Tom et al. 2010 | UK | General population | Unknown | 48–54 | Women | 962 | Unknown | Self-reported (sleep difficulty) | High | High | Moderate | High | Moderate |
Odds ratio Ever smoked Moderate sleep disturbances 1.14 (CI 0.93–1.39) Severe sleep disturbances 1.35 (CI 1.02–1.80) |
Age |
| Brook et al. 2012 | USA | General population | 25 years | Mean 40–65 | Women | 498 | Self-reported | Five questions (insomnia) | High | Moderate | Moderate | Moderate | Moderate |
Odds ratio Heavy Smokers 2.76 (CI 1.10–6.92) Moderate Smokers 2.24 (CI 0.74–6.77) |
Age, marital status, body mass index, health conditions, depressed mood and educational level |
Quality measure
The Effective Public Health Practice Project Quality Assessment Tool (EPHPP) (Armijo-Olivo et al. 2012) is a valid tool in qualitative evaluations. For the current study, an adapted version was used. The EPHPP has quantitative and qualitative dimensions (Armijo-Olivo et al. 2012). Its dimensions include sample size and sampling method, the design of the study, the method of variables assessment and controlled variables (Armijo-Olivo et al. 2012). At the psychometric level, the study also shows that this tool is desirable (Armijo-Olivo et al. 2012).
Analysis strategy
According to the systematic review and meta-analysis methodology, several analytical methods have been used for this study. These were done as follows: (1) The results of each of the studies were transformed into a single index, i.e., if multiple subgroup results were reported in one study, the subgroups were pooled together using the fixed effects method. (2) Subgroup results also became a single index for pooling the subgroups. (3) Once the results of the studies have been combined, the overall estimation time has been achieved. (4) These indices and their confidence interval were converted to an index using logarithms. (5) Finally, all studies were pooled initially in the overall level. The dimensions of qualitative evaluation were also analyzed separately. In the subgroup analysis, the pool index of the studies was determined and the degree of heterogeneity in each subgroup was presented. Meta-regression was also used in this study to investigate the results of the relationship between smoking and sleep-related issues in quality assessment (Al Lawati et al. 2009). In addition, two other issues were examined. First, the bias was measured with tests which are common in meta-analysis (Begg and Mazumdar 1994; Duval and Tweedie 2000; Egger et al. 1997) and then the heterogeneity of the studies in the relationship between smoking and sleep-related issues was investigated (Q test and I2) (Higgins and Thompson 2002; Ioannidis et al. 2007) using STATA software.
Results
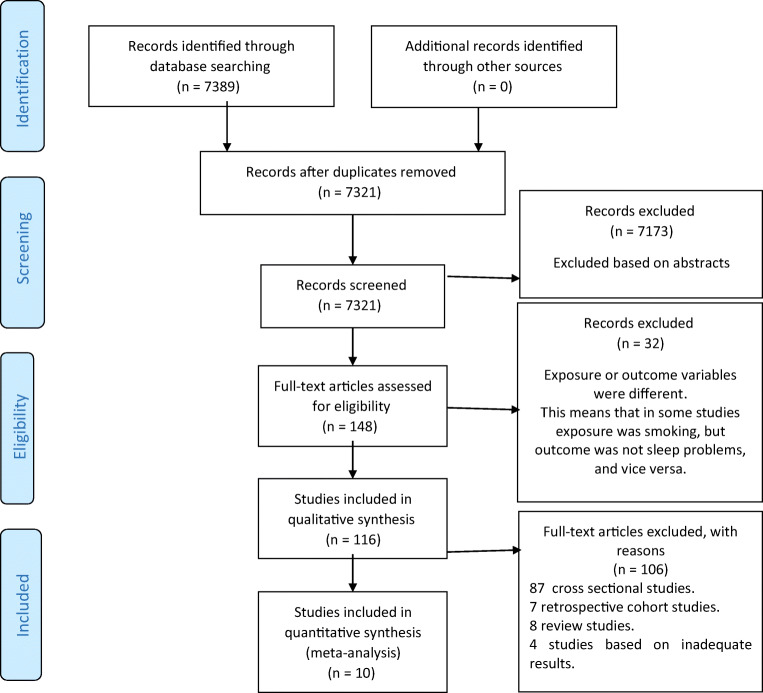
Flow chart of screen
The articles were screened according to the principles of PRISMA (Fig. 1). Ten cohort studies (Brook et al. 2012; Chen et al. 2017; Haario et al. 2013; Janson et al. 2001; Lee et al. 2016; Nordmann et al. 2016; Patten et al. 2000; Phillips and Mannino 2005; Theorell-Haglow et al. 2015; Tom et al. 2010) were found eligible and the information in these articles is shown in Table 2.
Fig. 1.
Selection flow diagram (Moher et al. 2009)
Quality of eligible cohort studies
The results are reported in Table 1. In the first dimension (selection), half of the articles were of good quality and the other half were of poor and moderate quality. In the second dimension (confounders), most of the studies were of poor and moderate quality. From the standpoint of variable exposure assessment, 10 studies have moderate bias. In the dimension of measuring the outcome variables, most of the studies were of moderate quality. In the last dimension, all articles were of good and moderate quality and poor quality was not seen in any of the articles.
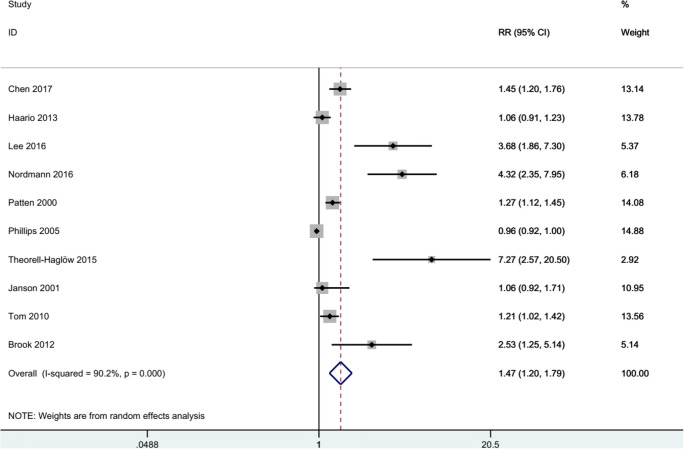
Smoking and sleep-related issues
In Fig. 2, the results indicate that smoking is associated with a risk of development of sleep-related issues: RR = 1.47. For this relation, the confidence interval was as follows: 1.20–1.79 with p value < 0.001.
Fig. 2.
Forest plot of smoking and sleep-related issues
Based on the results of Table 3, it can be shown that there is no difference between the studies in low (Chen et al. 2017; Haario et al. 2013; Patten et al. 2000; Phillips and Mannino 2005; Theorell-Haglow et al. 2015) and moderate (Janson et al. 2001) selection bias, but in high selection bias (Brook et al. 2012; Lee et al. 2016; Nordmann et al. 2016; Tom et al. 2010) the result was significant. In dimension of controlling the confounders, high (Nordmann et al. 2016; Patten et al. 2000; Theorell-Haglow et al. 2015; Tom et al. 2010) and moderate (Brook et al. 2012; Chen et al. 2017; Janson et al. 2001; Lee et al. 2016) studies had significant results. In both methods of measuring exposure variable, results were statistically significant. Results were significant in all three dimensions of low (Chen et al. 2017), moderate (Brook et al. 2012; Janson et al. 2001) and high (Tom et al. 2010) in the outcome measurement method. The fifth dimension results also showed that the results were significant in low bias, but in moderate bias the result was not significant.
Table 3.
Smoking and sleep-related issues based on quality assessment
| Quality assessment | Pooled RR | Lower CI | Upper CI | Weight | Heterogeneity (I-squared) | P value | Meta-regression (p value) |
|---|---|---|---|---|---|---|---|
| Selection bias | |||||||
| Low | 1.24 | 1.00 | 1.55 | 58.80 | 91.3 | 0.50 | p = 0.433 |
| Moderate | 1.06 | 0.78 | 1.45 | 10.95 | 0 | 0.713 | |
| High | 2.55 | 1.20 | 5.38 | 30.25 | 88.6 | 0.014 | |
| Confounders bias | |||||||
| Low | 0.98 | 0.91 | 1.06 | 28.67 | 35.2 | 0.648 | p = 0.172 |
| Moderate | 1.73 | 1.14 | 2.64 | 34.59 | 77.7 | 0.011 | |
| High | 1.93 | 1.28 | 2.90 | 36.74 | 88.6 | 0.002 | |
| Performance bias | |||||||
| Moderate | 1.27 | 1.12 | 1.45 | 14.08 | 0 | 0.001 | p = 0.621 |
| High | 1.54 | 1.22 | 1.94 | 85.92 | 90.1 | 0.001 | |
| Data collection method bias | |||||||
| Low | 1.45 | 1.20 | 1.76 | 13.14 | 0 | 0.001 | p = 0.518 |
| Moderate | 1.56 | 1.22 | 2.00 | 73.30 | 90.6 | 0.001 | |
| High | 1.21 | 1.03 | 1.43 | 13.56 | 0 | 0.024 | |
| Withdrawals and dropouts bias | |||||||
| Low | 1.58 | 1.22 | 2.04 | 70.35 | 92.6 | 0.001 | p = 0.553 |
| Moderate | 1.28 | 0.95 | 1.72 | 29.65 | 59.0 | 0.109 | |
Publication bias
The results of Egger’s test (p = 0.001) and Begg’s test (p = 0.060) revealed publication bias. Examining the publication bias graph (trim-and-fill in Fig. 3) (Duval and Tweedie 2000) indicated that six studies were missed. As the test results show (I2 = 90.2%), there is a high degree of heterogeneity (Higgins et al. 2003). In most analyses based on qualitative evaluation, the level of heterogeneity was still high (Table 2). In addition, χ2 was also examined (91.53; df = 9; p < 0.001). Accordingly, Fig. 3 demonstrates a lack of symmetry.
Fig. 3.
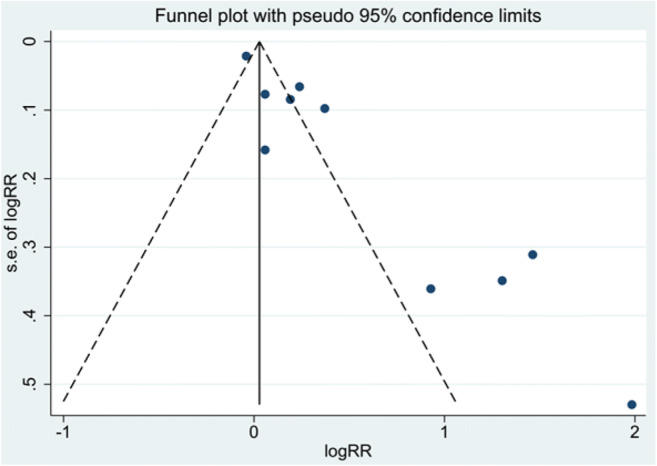
Funnel plot of smoking and sleep-related issues
Meta-regression
Evaluation of meta-regression results shows that the relationship between smoking and risk of sleep-related issue is not related to any quality dimension (Table 2).
Discussion
It was found that smoking increases the risk of developing sleep-related issues. This rate was 1.47%. In other words, smokers are 47% more likely to experience sleep-related issues than non-smokers. As the research literature in this area indicates, smoking has a negative effect on sleep and its quality (Janson et al. 1995; Revicki et al. 1991; Townsend et al. 1991). The possible mechanism that has been stated about the effects of smoking on sleep-related issues is that smoking triggers depression or health-related issues (Brook et al. 2012; Jaehne et al. 2012; Lee et al. 2016; Wetter and Young 1994). According to the mechanism of smoking effects on depression, obesity, diabetes and diseases (Baglioni et al. 2011; Beccuti and Pannain 2011; Hargens et al. 2013; L. Li et al. 2016; Liu et al. 2018a, b; Martinez-Gomez et al. 2013; Sakamoto et al. 2017; Sivertsen et al. 2012), it is stated that there is comorbidity between smoking and depression, obesity, diabetes and other disorders and diseases that can also be involved in sleep-related issues. Smoking is also associated with sleep-related breathing problems, which results in poor sleep quality and sleepiness (Jaehne et al. 2009) which is also associated with the reduction in rapid eye movement sleep (Davila et al. 1994; Gillin et al. 1994). As mentioned, nicotine can cause arousal and thus make sleeping difficult (Kishimoto and Domino 1998). Also, smoking has been recognized as a mechanism to deal with chronic pain and emotional problems (Ditre et al. 2010; Patterson et al. 2012). This is important because smoking affects mental distress and pain intensity and through this mechanism, it causes sleep problems (Custodio et al. 2015). Another approach claims that there is an inverse relationship, in that sleep problems are associated with increased pain perception (Smith et al. 2009) and this itself increases the risk of smoking (Hamidovic and de Wit 2009). Evaluating the qualitative results of the studies included in the meta-analysis of the 5 dimensions indicated that there were some differences in the dimensions of the quality assessment.
The strengths that can be mentioned about this study are as follows: This meta-analysis somehow sought to summarize studies of the relationship between smoking and sleep-related issues and it is a pioneering study with a review perspective, and no other meta-analysis studies have been done before. Second, compared with the research background in this area, our study is the only one that has examined the longitudinal researches, and it leads to the inference of causal relationships. Third, in the studies included in the meta-analysis, confounders were adjusted to some extent. Therefore, the role of other variables in relation to smoking and sleep-related issues was adjusted as much as possible. Limitations: The study of sex differences was not carried out, because studies entered into the meta-analysis did not provide adequate results about this issue. But there are some differences between men and women in terms of sleep (Mong and Cusmano 2016). For example, sleep problems may have more negative consequences for women’s health than for men’s (Mong and Cusmano 2016) and in this regard, it has been found that girls are twice as likely as boys to experience sleep problems (Mong et al. 2011). Also, sleep-related issues studied in this article included insomnia, sleep quality, and sleeplessness; therefore, this limitation has to be considered in generalizations and interpretations. Another limitation of the present study is that, with a few exceptions, other studies are based on self-report evaluation of sleep-related issues and smoking. Another limitation in this study is the bias of publication which can affect the results and findings. Therefore, in interpreting the results, this restriction should be considered. The investigation of the relationship between smoking and other sleep problems is recommended. This can be possible with the growth of research literature. The study involved different age groups. This can be a reason for heterogeneity. Therefore, age differences in the relationship between smoking and sleep-related issues cannot be ignored. As sleep in different age groups can have different quality, sleep patterns change with aging (Li et al. 2018) and aging accompanies quantitative and qualitative changes in sleep (Espiritu 2008; Vitiello 2006). Heterogeneity has made limitations for this meta-analysis as well. There were differences in the present study with regard to smoking, type of smoking, sleep problems, population size and type of population, socio-economic and other differences. The heterogeneity is due to two sources: clinical and methodological differences (Higgins and Green 2011).
In summary, according to the current research results, smoking can have adverse effects on sleep quality and it can also increase the risk of sleep-related issues. Taking advantage of smoking prevention techniques can reduce the negative consequences of smoking on sleeping health.
Public health implications
Smoking is considered an important public health issue (Jaehne et al. 2009) that has significant effects on adverse health dimensions, including mortality (Doll et al. 2004), chronic diseases (Office of the Surgeon General, Office on Smoking and Health 2004) and other health consequences (Newcomb and Carbone 1992). Therefore, studying the different health dimensions associated with smoking is an important public health issue. On the other hand, the present study showed that smoking was a risk factor for sleep problems. Sleep disturbances are also associated with mental health (Hestetun et al. 2018). Therefore, increasing attention to smoking and sleep-related problems is a matter of public health priority, because stopping smoking is associated with reduced sleep disturbance (Patten et al. 2000) and it can increase sleep quality by itself (Wetter et al. 1995).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Al Lawati NM, Patel SR, Ayas NT. Epidemiology, risk factors, and consequences of obstructive sleep apnea and short sleep duration. Progress in Cardiovascular Diseases. 2009;51(4):285–293. doi: 10.1016/j.pcad.2008.08.001. [DOI] [PubMed] [Google Scholar]
- Anothaisintawee T, Reutrakul S, Van Cauter E, Thakkinstian A. Sleep disturbances compared to traditional risk factors for diabetes development: systematic review and meta-analysis. Sleep Medicine Reviews. 2016;30:11–24. doi: 10.1016/j.smrv.2015.10.002. [DOI] [PubMed] [Google Scholar]
- Antman EM, Lau J, Kupelnick B, Mosteller F, Chalmers TC. A comparison of results of meta-analyses of randomized control trials and recommendations of clinical experts. Treatments for myocardial infarction. Jama. 1992;268(2):240–248. doi: 10.1001/jama.1992.03490020088036. [DOI] [PubMed] [Google Scholar]
- Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. Journal of Evaluation in Clinical Practice. 2012;18(1):12–18. doi: 10.1111/j.1365-2753.2010.01516.x. [DOI] [PubMed] [Google Scholar]
- Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. Journal of Affective Disorders. 2011;135(1–3):10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Ban DJ, Lee TJ. Sleep duration, subjective sleep disturbances and associated factors among university students in Korea. Journal of Korean Medical Science. 2001;16(4):475–480. doi: 10.3346/jkms.2001.16.4.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartel KA, Gradisar M, Williamson P. Protective and risk factors for adolescent sleep: a meta-analytic review. Sleep Medicine Reviews. 2015;21:72–85. doi: 10.1016/j.smrv.2014.08.002. [DOI] [PubMed] [Google Scholar]
- Beccuti G, Pannain S. Sleep and obesity. Current Opinion in Clinical Nutrition and Metabolic Care. 2011;14(4):402–412. doi: 10.1097/MCO.0b013e3283479109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- Brook DW, Rubenstone E, Zhang C, Brook JS. Trajectories of cigarette smoking in adulthood predict insomnia among women in late mid-life. Sleep Medicine. 2012;13(9):1130–1137. doi: 10.1016/j.sleep.2012.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen LJ, Steptoe A, Chen YH, Ku PW, Lin CH. Physical activity, smoking, and the incidence of clinically diagnosed insomnia. Sleep Medicine. 2017;30:189–194. doi: 10.1016/j.sleep.2016.06.040. [DOI] [PubMed] [Google Scholar]
- Cohen, A., Ben Abu, N., & Haimov, I. (2018). The interplay between tobacco dependence and sleep quality among young adults. Behavioral Sleep Medicine, 1–14. 10.1080/15402002.2018.1546707. [DOI] [PubMed]
- Conway SG, Roizenblatt SS, Palombini L, Castro LS, Bittencourt LR, Silva RS, Tufik S. Effect of smoking habits on sleep. Brazilian Journal of Medical and Biological Research. 2008;41(8):722–727. doi: 10.1590/S0100-879X2008000800014. [DOI] [PubMed] [Google Scholar]
- Custodio L, Carlson CR, Upton B, Okeson JP, Harrison AL, de Leeuw R. The impact of cigarette smoking on sleep quality of patients with masticatory myofascial pain. Journal of Oral & Facial Pain and Headache. 2015;29(1):15–23. doi: 10.11607/ofph.1266. [DOI] [PubMed] [Google Scholar]
- Davila DG, Hurt RD, Offord KP, Harris CD, Shepard JW., Jr Acute effects of transdermal nicotine on sleep architecture, snoring, and sleep-disordered breathing in nonsmokers. American Journal of Respiratory and Critical Care Medicine. 1994;150(2):469–474. doi: 10.1164/ajrccm.150.2.8049831. [DOI] [PubMed] [Google Scholar]
- Ditre JW, Heckman BW, Butts EA, Brandon TH. Effects of expectancies and coping on pain-induced motivation to smoke. Journal of Abnormal Psychology. 2010;119(3):524–533. doi: 10.1037/a0019568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ (Clinical research ed.) 2004;328(7455):1519. doi: 10.1136/bmj.38142.554479.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–463. doi: 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espiritu JR. Aging-related sleep changes. Clinics in Geriatric Medicine. 2008;24(1):1–14. doi: 10.1016/j.cger.2007.08.007. [DOI] [PubMed] [Google Scholar]
- Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep. 1995;18(6):425–432. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? Jama. 1989;262(11):1479–1484. doi: 10.1001/jama.1989.03430110069030. [DOI] [PubMed] [Google Scholar]
- Forouzanfar, M. H., Afshin, A., Alexander, L. T., Anderson, H. R., Bhutta, Z. A., Biryukov, S., et al. (2016). Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet, 388(10053), 1659–1724. 10.1016/S0140-6736(16)31679-8. [DOI] [PMC free article] [PubMed]
- Fritsch Montero R, Lahsen Martinez P, Romeo Gomez R, Araya Baltra R, Rojas Castillo G. Sleep disorders in the adult population of Santiago of Chile and its association with common psychiatric disorders. Actas Españolas de Psiquiatría. 2010;38(6):358–364. [PubMed] [Google Scholar]
- Gillin JC, Lardon M, Ruiz C, Golshan S, Salin-Pascual R. Dose-dependent effects of transdermal nicotine on early morning awakening and rapid eye movement sleep time in nonsmoking normal volunteers. Journal of Clinical Psychopharmacology. 1994;14(4):264–267. doi: 10.1097/00004714-199408000-00006. [DOI] [PubMed] [Google Scholar]
- Gomes Felden EP, Barbosa DG, Junior GJF, Santos MO, Pelegrini A, Silva DAS. Factors associated with sleep duration in Brazilian high school students. Chronobiology International. 2017;34(6):773–781. doi: 10.1080/07420528.2017.1323759. [DOI] [PubMed] [Google Scholar]
- Haario P, Rahkonen O, Laaksonen M, Lahelma E, Lallukka T. Bidirectional associations between insomnia symptoms and unhealthy behaviours. Journal of Sleep Research. 2013;22(1):89–95. doi: 10.1111/j.1365-2869.2012.01043.x. [DOI] [PubMed] [Google Scholar]
- Haddaway, N. R., & Watson, M. J. (2016). On the benefits of systematic reviews for wildlife parasitology. International Journal for Parasitology, 5(2), 184–191. 10.1016/j.ijppaw.2016.05.002. [DOI] [PMC free article] [PubMed]
- Haheim LL, Holme I, Hjermann I, Leren P. Smoking habits and risk of fatal stroke: 18 years follow up of the Oslo Study. Journal of Epidemiology and Community Health. 1996;50(6):621–624. doi: 10.1136/jech.50.6.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamidovic A, de Wit H. Sleep deprivation increases cigarette smoking. Pharmacology, Biochemistry, and Behavior. 2009;93(3):263–269. doi: 10.1016/j.pbb.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hargens TA, Kaleth AS, Edwards ES, Butner KL. Association between sleep disorders, obesity, and exercise: a review. Nature and Science of Sleep. 2013;5:27–35. doi: 10.2147/NSS.S34838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harma M, Tenkanen L, Sjoblom T, Alikoski T, Heinsalmi P. Combined effects of shift work and life-style on the prevalence of insomnia, sleep deprivation and daytime sleepiness. Scandinavian Journal of Work, Environment & Health. 1998;24(4):300–307. doi: 10.5271/sjweh.324. [DOI] [PubMed] [Google Scholar]
- Hertenstein E, Feige B, Gmeiner T, Kienzler C, Spiegelhalder K, Johann A, et al. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Medicine Reviews. 2018;43:96–105. doi: 10.1016/j.smrv.2018.10.006. [DOI] [PubMed] [Google Scholar]
- Hestetun I, Svendsen MV, Oellingrath IM. Sleep problems and mental health among young Norwegian adolescents. Nordic Journal of Psychiatry. 2018;72(8):578–585. doi: 10.1080/08039488.2018.1499043. [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. T., & Green, S. (2011). Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration.
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Statistics in Medicine. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet. 2011;378(9799):1297–1305. doi: 10.1016/s0140-6736(11)60781-2. [DOI] [PubMed] [Google Scholar]
- Ioannidis JP, Patsopoulos NA, Evangelou E. Uncertainty in heterogeneity estimates in meta-analyses. Bmj. 2007;335(7626):914–916. doi: 10.1136/bmj.39343.408449.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaehne A, Loessl B, Barkai Z, Riemann D, Hornyak M. Effects of nicotine on sleep during consumption, withdrawal and replacement therapy. Sleep Medicine Reviews. 2009;13(5):363–377. doi: 10.1016/j.smrv.2008.12.003. [DOI] [PubMed] [Google Scholar]
- Jaehne A, Unbehaun T, Feige B, Lutz UC, Batra A, Riemann D. How smoking affects sleep: a polysomnographical analysis. Sleep Medicine. 2012;13(10):1286–1292. doi: 10.1016/j.sleep.2012.06.026. [DOI] [PubMed] [Google Scholar]
- Jaehne A, Unbehaun T, Feige B, Cohrs S, Rodenbeck A, Schutz AL, et al. Sleep changes in smokers before, during and 3 months after nicotine withdrawal. Addiction Biology. 2015;20(4):747–755. doi: 10.1111/adb.12151. [DOI] [PubMed] [Google Scholar]
- Janson C, Gislason T, De Backer W, Plaschke P, Bjornsson E, Hetta J, et al. Prevalence of sleep disturbances among young adults in three European countries. Sleep. 1995;18(7):589–597. [PubMed] [Google Scholar]
- Janson C, Lindberg E, Gislason T, Elmasry A, Boman G. Insomnia in men-a 10-year prospective population based study. Sleep. 2001;24(4):425–430. doi: 10.1093/sleep/24.4.425. [DOI] [PubMed] [Google Scholar]
- Jayes L, Haslam PL, Gratziou CG, Powell P, Britton J, Vardavas C, et al. SmokeHaz: systematic reviews and meta-analyses of the effects of smoking on respiratory health. Chest. 2016;150(1):164–179. doi: 10.1016/j.chest.2016.03.060. [DOI] [PubMed] [Google Scholar]
- Kageyama M, Odagiri K, Mizuta I, Yamamoto M, Yamaga K, Hirano T, et al. Health-related behaviors associated with subjective sleep insufficiency in Japanese workers: a cross-sectional study. Journal of Occupational Health. 2017;59(2):139–146. doi: 10.1539/joh.16-0038-OA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim TK, Lee HC, Lee SG, Han KT, Park EC. The combined effect of sleep duration and quality on mental health among Republic of Korea Armed Forces. Military Medicine. 2016;181(11):e1581–e1589. doi: 10.7205/milmed-d-15-00538. [DOI] [PubMed] [Google Scholar]
- Kishimoto T, Domino EF. Effects of tobacco smoking and abstinence on middle latency auditory evoked potentials. Clinical Pharmacology and Therapeutics. 1998;63(5):571–579. doi: 10.1016/s0009-9236(98)90108-4. [DOI] [PubMed] [Google Scholar]
- Lee JY, Brook JS, Finch SJ, Brook DW. Trajectories of cigarette smoking beginning in adolescence predict insomnia in the mid thirties. Substance Use & Misuse. 2016;51(5):616–624. doi: 10.3109/10826084.2015.1126747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Wu C, Gan Y, Qu X, Lu Z. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry. 2016;16(1):375. doi: 10.1186/s12888-016-1075-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Vitiello MV, Gooneratne NS. Sleep in normal aging. Sleep Medicine Clinics. 2018;13(1):1–11. doi: 10.1016/j.jsmc.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X, Liu L. Sleep habits and insomnia in a sample of elderly persons in China. Sleep. 2005;28(12):1579–1587. [PubMed] [Google Scholar]
- Liu X, Bragg F, Yang L, Kartsonaki C, Guo Y, Du H, et al. Smoking and smoking cessation in relation to risk of diabetes in Chinese men and women: a 9-year prospective study of 0.5 million people. The Lancet Public Health. 2018;3(4):e167–e176. doi: 10.1016/s2468-2667(18)30026-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, X., Bragg, F., Yang, L., Kartsonaki, C., Guo, Y., Du, H., et al. (2018b). Smoking and smoking cessation in relation to risk of diabetes in Chinese men and women: a 9-year prospective study of 0·5 million people. The Lancet Public Health, 3(4), e167–e176. 10.1016/S2468-2667(18)30026-4. [DOI] [PMC free article] [PubMed]
- Maggi S, Langlois JA, Minicuci N, Grigoletto F, Pavan M, Foley DJ, Enzi G. Sleep complaints in community-dwelling older persons: prevalence, associated factors, and reported causes. Journal of the American Geriatrics Society. 1998;46(2):161–168. doi: 10.1111/j.1532-5415.1998.tb02533.x. [DOI] [PubMed] [Google Scholar]
- Martinez-Gomez D, Guallar-Castillon P, Leon-Munoz LM, Lopez-Garcia E, Rodriguez-Artalejo F. Combined impact of traditional and non-traditional health behaviors on mortality: a national prospective cohort study in Spanish older adults. BMC Medicine. 2013;11:47. doi: 10.1186/1741-7015-11-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milojevich HM, Lukowski AF. Sleep and mental health in undergraduate students with generally healthy sleep habits. PLoS One. 2016;11(6):e0156372. doi: 10.1371/journal.pone.0156372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mong JA, Cusmano DM. Sex differences in sleep: impact of biological sex and sex steroids. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 2016;371(1688):20150110–20150110. doi: 10.1098/rstb.2015.0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mong JA, Baker FC, Mahoney MM, Paul KN, Schwartz MD, Semba K, Silver R. Sleep, rhythms, and the endocrine brain: influence of sex and gonadal hormones. The Journal of Neuroscience. 2011;31(45):16107–16116. doi: 10.1523/jneurosci.4175-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb PA, Carbone PP. The health consequences of smoking. Cancer Medical Clinics of North America. 1992;76(2):305–331. doi: 10.1016/s0025-7125(16)30355-8. [DOI] [PubMed] [Google Scholar]
- Nordmann S, Lions C, Vilotitch A, Michel L, Mora M, Spire B, et al. A prospective, longitudinal study of sleep disturbance and comorbidity in opiate dependence (the ANRS Methaville study) Psychopharmacology. 2016;233(7):1203–1213. doi: 10.1007/s00213-016-4202-4. [DOI] [PubMed] [Google Scholar]
- O’Keeffe LM, Taylor G, Huxley RR, Mitchell P, Woodward M, Peters SAE. Smoking as a risk factor for lung cancer in women and men: a systematic review and meta-analysis. BMJ Open. 2018;8(10):e021611. doi: 10.1136/bmjopen-2018-021611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the Surgeon General, Office on Smoking and Health. (2004). Reports of the surgeon general. In The health consequences of smoking: a report of the surgeon general. Atlanta (GA): Centers for Disease Control and Prevention (US).
- Ohayon MM, Bader G. Prevalence and correlates of insomnia in the Swedish population aged 19-75 years. Sleep Medicine. 2010;11(10):980–986. doi: 10.1016/j.sleep.2010.07.012. [DOI] [PubMed] [Google Scholar]
- Ohayon MM, Zulley J, Guilleminault C, Smirne S, Priest RG. How age and daytime activities are related to insomnia in the general population: consequences for older people. Journal of the American Geriatrics Society. 2001;49(4):360–366. doi: 10.1046/j.1532-5415.2001.49077.x. [DOI] [PubMed] [Google Scholar]
- Oxman AD, Guyatt GH. The science of reviewing research. Annals of the New York Academy of Sciences. 1993;703:125–133. doi: 10.1111/j.1749-6632.1993.tb26342.x. [DOI] [PubMed] [Google Scholar]
- Pandi-Perumal SR, Verster JC, Kayumov L, Lowe AD, Santana MG, Pires ML, et al. Sleep disorders, sleepiness and traffic safety: a public health menace. Brazilian Journal of Medical and Biological Research. 2006;39(7):863–871. doi: 10.1590/S0100-879X2006000700003. [DOI] [PubMed] [Google Scholar]
- Patten CA, Choi WS, Gillin JC, Pierce JP. Depressive symptoms and cigarette smoking predict development and persistence of sleep problems in US adolescents. Pediatrics. 2000;106(2):E23. doi: 10.1542/peds.106.2.e23. [DOI] [PubMed] [Google Scholar]
- Patterson AL, Gritzner S, Resnick MP, Dobscha SK, Turk DC, Morasco BJ. Smoking cigarettes as a coping strategy for chronic pain is associated with greater pain intensity and poorer pain-related function. The Journal of Pain. 2012;13(3):285–292. doi: 10.1016/j.jpain.2011.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters SA, Huxley RR, Woodward M. Smoking as a risk factor for stroke in women compared with men: a systematic review and meta-analysis of 81 cohorts, including 3,980,359 individuals and 42,401 strokes. Stroke. 2013;44(10):2821–2828. doi: 10.1161/strokeaha.113.002342. [DOI] [PubMed] [Google Scholar]
- Phillips B, Mannino D. Correlates of sleep complaints in adults: the ARIC study. Journal of Clinical Sleep Medicine. 2005;1(3):277–283. doi: 10.5664/jcsm.26344. [DOI] [PubMed] [Google Scholar]
- Reichenheim ME, Coutinho ES. Measures and models for causal inference in cross-sectional studies: arguments for the appropriateness of the prevalence odds ratio and related logistic regression. BMC Medical Research Methodology. 2010;10:66. doi: 10.1186/1471-2288-10-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reitsma MB, Fullman N, Ng M, Salama JS, Abajobir A, Abate KH, et al. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet. 2017;389(10082):1885–1906. doi: 10.1016/S0140-6736(17)30819-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Revicki D, Sobal J, DeForge B. Smoking status and the practice of other unhealthy behaviors. Family Medicine. 1991;23(5):361–364. [PubMed] [Google Scholar]
- Roberts RE, Roberts CR, Duong HT. Sleepless in adolescence: prospective data on sleep deprivation, health and functioning. Journal of Adolescence. 2009;32(5):1045–1057. doi: 10.1016/j.adolescence.2009.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakamoto, N., Gozal, D., Smith, D. L., Yang, L., Morimoto, N., Wada, H., et al. (2017). Sleep duration, snoring prevalence, obesity, and behavioral problems in a large cohort of primary school students in Japan. Sleep, 40(3). 10.1093/sleep/zsw082. [DOI] [PubMed]
- Shahar E, Shahar DJ. Causal diagrams and the cross-sectional study. Clinical Epidemiology. 2013;5:57–65. doi: 10.2147/CLEP.S42843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short NA, Mathes BM, Gibby B, Oglesby ME, Zvolensky MJ, Schmidt NB. Insomnia symptoms as a risk factor for cessation failure following smoking treatment. Addiction Research and Theory. 2017;25(1):17–23. doi: 10.1080/16066359.2016.1190342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivertsen B, Salo P, Mykletun A, Hysing M, Pallesen S, Krokstad S, et al. The bidirectional association between depression and insomnia: the HUNT study. Psychosomatic Medicine. 2012;74(7):758–765. doi: 10.1097/PSY.0b013e3182648619. [DOI] [PubMed] [Google Scholar]
- Sivertsen B, Lallukka T, Salo P, Pallesen S, Hysing M, Krokstad S, Simon O. Insomnia as a risk factor for ill health: results from the large population-based prospective HUNT Study in Norway. Journal of Sleep Research. 2014;23(2):124–132. doi: 10.1111/jsr.12102. [DOI] [PubMed] [Google Scholar]
- Smagula SF, Stone KL, Fabio A, Cauley JA. Risk factors for sleep disturbances in older adults: evidence from prospective studies. Sleep Medicine Reviews. 2016;25:21–30. doi: 10.1016/j.smrv.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith MT, Wickwire EM, Grace EG, Edwards RR, Buenaver LF, Peterson S, et al. Sleep disorders and their association with laboratory pain sensitivity in temporomandibular joint disorder. Sleep. 2009;32(6):779–790. doi: 10.1093/sleep/32.6.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugawara, Y., Tsuji, I., Mizoue, T., Inoue, M., Sawada, N., Matsuo, K., et al. (2018). Cigarette smoking and cervical cancer risk: an evaluation based on a systematic review and meta-analysis among Japanese women. Japanese Journal of Clinical Oncology. 10.1093/jjco/hyy158. [DOI] [PubMed]
- Taveira KVM, Kuntze MM, Berretta F, de Souza BDM, Godolfim LR, Demathe T, et al. Association between obstructive sleep apnea and alcohol, caffeine and tobacco: a meta-analysis. Journal of Oral Rehabilitation. 2018;45(11):890–902. doi: 10.1111/joor.12686. [DOI] [PubMed] [Google Scholar]
- Theorell-Haglow J, Akerstedt T, Schwarz J, Lindberg E. Predictors for development of excessive daytime sleepiness in women: a population-based 10-year follow-up. Sleep. 2015;38(12):1995–2003. doi: 10.5665/sleep.5258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas KM, Redd LA, Wright JD, Hartos JL. Sleep and mental health in the general population of elderly women. The Journal of Primary Prevention. 2017;38(5):495–503. doi: 10.1007/s10935-017-0484-5. [DOI] [PubMed] [Google Scholar]
- Thorpy MJ. Classification of sleep disorders. Neurotherapeutics. 2012;9(4):687–701. doi: 10.1007/s13311-012-0145-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tom SE, Kuh D, Guralnik JM, Mishra GD. Self-reported sleep difficulty during the menopausal transition: results from a prospective cohort study. Menopause. 2010;17(6):1128–1135. doi: 10.1097/gme.0b013e3181dd55b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend J, Wilkes H, Haines A, Jarvis M. Adolescent smokers seen in general practice: health, lifestyle, physical measurements, and response to antismoking advice. BMJ (Clinical research ed.) 1991;303(6808):947–950. doi: 10.1136/bmj.303.6808.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel WM, Robles TF, Hall M, Buysse DJ. Marital quality and the marital bed: examining the covariation between relationship quality and sleep. Sleep Medicine Reviews. 2007;11(5):389–404. doi: 10.1016/j.smrv.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Wouw E, Evenhuis HM, Echteld MA. Prevalence, associated factors and treatment of sleep problems in adults with intellectual disability: a systematic review. Research in Developmental Disabilities. 2012;33(4):1310–1332. doi: 10.1016/j.ridd.2012.03.003. [DOI] [PubMed] [Google Scholar]
- Vitiello MV. Sleep in normal aging. Sleep Medicine Clinics. 2006;1(2):171–176. doi: 10.1016/j.jsmc.2006.04.007. [DOI] [Google Scholar]
- Wetter DW, Young TB. The relation between cigarette smoking and sleep disturbance. Preventive Medicine. 1994;23(3):328–334. doi: 10.1006/pmed.1994.1046. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Fiore MC, Baker TB, Young TB. Tobacco withdrawal and nicotine replacement influence objective measures of sleep. Journal of Consulting and Clinical Psychology. 1995;63(4):658–667. doi: 10.1037//0022-006x.63.4.658. [DOI] [PubMed] [Google Scholar]
- Xiaolin Gu MM. Risk factors of sleep disorder after stroke: a meta-analysis. Topics in Stroke Rehabilitation. 2017;24(1):34–40. doi: 10.1080/10749357.2016.1188474. [DOI] [PubMed] [Google Scholar]
- Yang Y, Shin JC, Li D, An R. Sedentary behavior and sleep problems: a systematic review and meta-analysis. International Journal of Behavioral Medicine. 2017;24(4):481–492. doi: 10.1007/s12529-016-9609-0. [DOI] [PubMed] [Google Scholar]
- Zhang HS, Li Y, Mo HY, Qiu DX, Zhao J, Luo JL, et al. A community-based cross-sectional study of sleep quality in middle-aged and older adults. Quality of Life Research. 2017;26(4):923–933. doi: 10.1007/s11136-016-1408-1. [DOI] [PubMed] [Google Scholar]