Abstract
The aim of this study was to investigate the effect of the jaw opening exercise (JOE) on the thickness of the suprahyoid muscle and hyoid bone movement compared with the head lift exercise (HLE) in patients with dysphagia after stroke
This study recruited 30 patients with dysphagia after stroke. The JOE group performed a JOE using a resistance bar. The HLE group performed the traditional HLE. The total intervention duration was 6 weeks. We measured the thickness of the digastric and mylohyoid muscles using ultrasound. Two-dimensional motion analysis of the hyoid bone was performed using Image J software. The Borg rating of the perceived exertion scale was used to assess the intensity level of physical activity during the 2 exercises.
Both groups showed a significant increase in the thickness of the digastric and mylohyoid muscles (P < .05). Hyoid bone motion was significantly increased in the anterior and superior movement in both groups (P < .05). After the intervention, there was no significant difference between the 2 groups. The Borg rating of perceived exertion scale for the JOE group was significantly lower than that of the HLE group (P < .05).In conclusion, this study demonstrated that the JOE and the HLE had similar effects with respect to increasing suprahyoid muscle thickness and improving hyoid bone movement. However, the JOE required less perceived exertion than the HLE.
Keywords: dysphagia, head lift exercise, hyoid bone, jaw opening exercise, suprahyoid muscles
1. Introduction
The head lift exercise (HLE), also known as Shaker exercise, is commonly used to improve the swallowing function in dysphagia patients.[1] The HLE strengthens the suprahyoid muscles (e.g., the geniohyoid, mylohyoid, and digastrics muscles), which are the agonistic swallowing muscles located in the anterior region of the neck, by repeating or maintaining the head lifting and lowering motions from the floor in the supine position.[2]
The HLE stimulates the suprahyoid muscles and contributes to the increase in muscle activation.[3,4] As a result, the hyoid bone and larynx are sufficiently pulled toward the jaw tip of the mandible.[5] The movement of the hyoid bone during swallowing contributes to the normal swallowing mechanism through the downward rotation of the epiglottis and the upper esophageal sphincter opening.[6,7]
Previously, several studies have demonstrated that the HLE results in activation of the suprahyoid muscles in normal adults.[3,4,8] Park et al[5] reported that a 4-week HLE application to dysphagia patients after stroke showed increased movement of the hyoid bone and decreased aspiration. Choi et al[9] also reported that the HLE reduced aspiration and improved oral diet levels in patients with dysphagia after stroke.
Although the HLE is an effective exercise for improving the swallowing function in dysphagia patients, it is a very challenging exercise for physically vulnerable people such as the elderly and stroke patients. Because this exercise can only be performed in the supine position, it cannot be easily performed by a person who has difficulty in physically changing postures. It also causes fatigue of various muscles in the neck, especially the sternocleidomastoid muscle.[10,11] Repeated exposure to muscle fatigue can cause temporary pain and discomfort, which reduces compliance, which is one of the factors causing patients to drop out. Therefore, it is clinically important to demonstrate the effects of new or modified interventions that have similar effects to the HLE and address its limitations.
New exercises to replace the HLE have recently been introduced: the chin tuck against resistance exercise and the jaw opening exercise (JOE).[12,13] These 2 exercises have the same purpose as the HLE, but can be performed in a sitting position and impose less of a burden on the neck muscle. The chin tuck against resistance exercise consists of chin tucks downward against resistance, while the JOE consists of jaw opening against resistance.
Previous studies have demonstrated that the chin tuck against resistance exercise induces suprahyoid muscle activation in healthy adults to a similar degree as the HLE,[10,13] suggesting a potential therapeutic effect. Recently, some studies reported that the chin tuck against resistance exercise in patients with dysphagia after stroke improved the oropharyngeal swallowing function, including decreased aspiration.[14,15]
The JOE has also been reported to activate the suprahyoid muscle, similar to the HLE.[16] Moreover, Wada et al[17] demonstrated that when dysphagia patients performed the JOE for 4 weeks, it improved hyoid bone movement and opening of the upper esophageal sphincter. Nevertheless, the clinical effects of JOE remain unclear. So far, electromyographic evaluations for studying the effect of JOE have only been performed for normal adults, and no study has been conducted in patients with neurological diseases, such as stroke. Therefore, it is important to evaluate the effectiveness of the JOE through various evaluations such as ultrasound and hyoid bone motion analysis.
The purpose of this study was to investigate the effect of the JOE on the thickness of the suprahyoid muscle and hyoid bone movement compared with the HLE in patients with dysphagia after stroke.
2. Methods
2.1. Participants
This study recruited 30 patients with dysphagia after stroke from 2 hospitals in South Korea. The inclusion criteria were diagnosed as having had a stroke within 1 to 5 months post-onset; dysphagia confirmed by a videofluoroscopic swallowing study; ability to follow study instructions; ability to swallow voluntarily; liquid aspiration or penetration observed on a videofluoroscopic swallowing study; nasogastric tube; the ability to use at least 1 arm; and absence of any cognitive deficits (a score of >22 points in the Mini-mental Status Examination). The exclusion criteria were secondary stroke; brainstem stroke; presence of other neurologic diseases; pain in the disc, cervical spine, and jaw; limitations in jaw opening such as temporomandibular joint disc pain; cervical spine orthosis; history of cervical spine surgery; myelopathy; presence of a gastrostomy tube; and problems with the esophageal phase of dysphagia (e.g., achalasia or UES opening) confirmed by a videofluoroscopic swallowing study.
We explained the objectives and requirements of our study to all participants, and they voluntarily signed the informed consent form. Ethical approval was obtained from the Inje University Institutional Review Board before the experiment (INJE 2018-07-023-001).
2.2. Sample size estimation
The sample size was calculated using G-power 3.1 software (University of Dusseldorf, Dusseldorf, Germany). The power and alpha levels were set at 0.60 and 0.05, respectively, and the effective size was set at 0.8. According to prior analysis, each group required at least 12 subjects. Therefore, a total of 24 people were needed.
2.3. Methods
This study performed an open-label, parallel-group, comparative study randomized trial. In total, 30 patients were randomly allocated to either the JOE group or the HLE group by blocked randomization. The JOE group performed JOE using a resistance bar made of acrylonitrile-butadiene-styrene resin (LES 100; Cybermedic Inc., Iksan South Korea). Exercise types were divided into isometric exercises and isotonic exercises. The isometric exercise requires the jaw to be held open for 10 seconds against the resistance (10 seconds × 3 times). The isotonic exercise was repeated 30 times and required the jaw to be opened against resistance (30 times × 3 sets) (Fig. 1).
Figure 1.
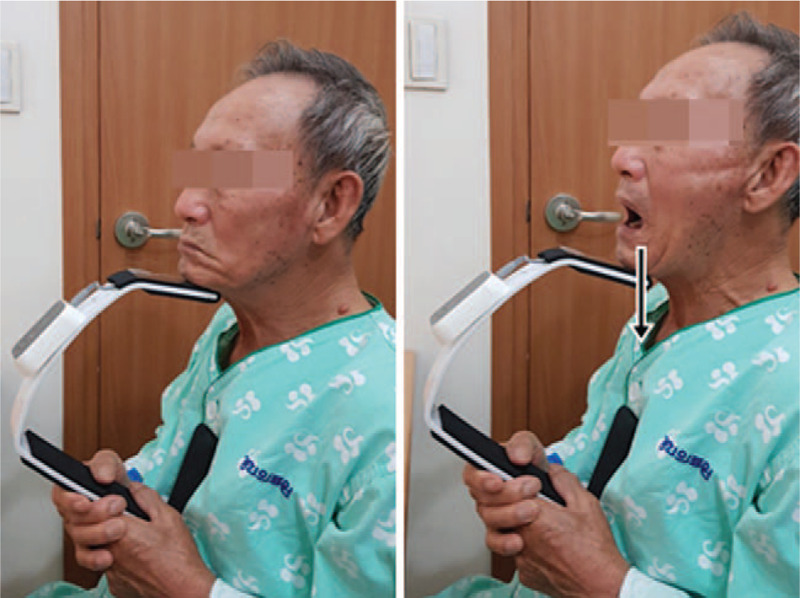
Jaw opening exericse (left) starting position, (right) jaw opening against resistance bar.
The HLE group performed HLEs that were of the same exercise type (isometric and isotonic type) and at the same frequency as the JOE. The HLE method refers to a previous study.[18] In addition, both groups received traditional dysphagia treatment by occupational therapists (30 minutes a day). Traditional dysphagia treatment included oral-facial massage, thermal-tactile stimulation, and various compensatory training exercises. The intervention took place 5 days a week for a 6 weeks period.
2.4. Outcome measurement
The primary outcome measurement of this study was the change in the thickness of the suprahyoid muscle. Muscle thickness was measured using a portable ultrasound device (SONON 300L; Healcerion, Seoul, Korea) with a 10 MHz linear- and convex-array transducer. To avoid tissue compression, ultrasound contact gel was applied to the probe. The evaluations were performed by a skilled investigator and were repeated 3 times, and the mean value was calculated to represent the suprahyoid muscles thickness for each subject. The participants were asked to sit upright in a chair with the Frankfurt plane parallel to the floor and without head support.
To measure the thickness of the suprahyoid muscles, the transducer was positioned between the hyoid bone and the chin and the image visualized through the tablet PC. The digastric muscle was measured from the upper to the lower boundary of the fascia at the broadest point perpendicular to the mylohyoid muscle. The mylohyoid muscle was measured from under the measurement point of the digastric muscle, from the upper to the lower boundary of the fascia[19] (Fig. 2).
Figure 2.
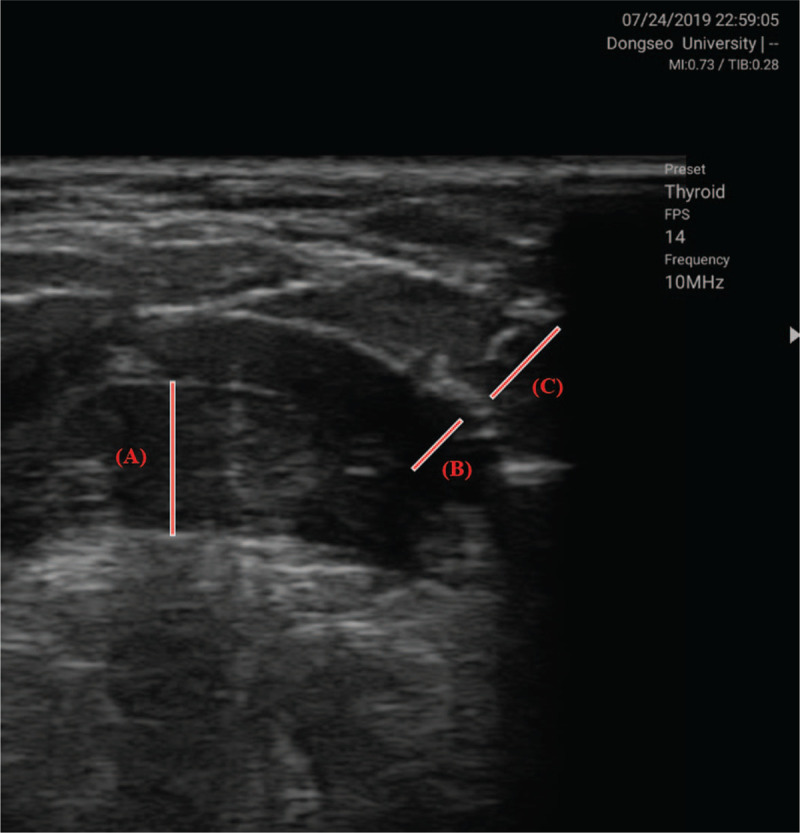
Thickness measure of suprahyoid muscles using ultrasound device geniohyoid muscle (B) mylohyoid muscle (C) anterior belly of digastric muscle.
The secondary outcome measurement of this study was the kinematic movement of the hyoid bone. We measured the spatial parameter of hyoid bone movement using computer software (Image J). Swallowing motion files were captured using a frame during videofluoroscopic swallowing study. Two picture frames of videofluoroscopic swallowing study were used for the analysis: one of the resting status of the hyoid and another of maximal excursion of the hyoid. The cervical 2 – 4 axis was used for the image rotation method. The cervical 2 – 4 axis line was rotated to the true vertical 90°, so that a straight line was drawn between the most anteroinferior points, cervical 2 and cervical 4. The anteroinferior corner of cervical 4 on each image (O; origin), which indicated a point in the resting status of the hyoid before swallowing, was used as an anchor point, and the most superoanterior point of the hyoid indicated maximum displacement after swallowing. Hyoid displacement was defined as the distance from the resting position to the maximal excursion position during swallowing. Horizontal and vertical displacements of the hyoid were calculated by the point values (x, y) on each image, which were measured on the resting position image (pre-swallow image) and the maximal excursion image. Anterior displacement (x2 - x1) - (Ox2 - Ox1) and vertical displacement (y2 - y1) - (Oy2 - Oy1) were measured: Pre-swallow image coordinates were x1, y1, and maximal excursion image coordinates were x2, y2. The coordinates of the anchor point of the pre-swallow image were Ox1, Oy1 and those of the excursion image were Ox2, Oy2.
The Borg Rating of Perceived Exertion Scale (BRPES) is a subjective method for measuring the intensity level of physical activity.[20] Perceived exertion is a measure of how hard the activity is for the subject during exercise and is based on the physical sensations (e.g., increased heart rate, respiration or breathing rate, sweating, and muscle fatigue) a person experiences during physical activity or exercise. The scale ranges from 6 (no exertion at all and/or very light) to 20 (maximal exertion and/or very hard). BRPES was measured immediately after each intervention (total 30 measurements) and the average value was recorded.
2.5. Statistical analysis
All statistical analyses were performed using SPSS version 15.0 (IBM Corporation, Armonk, NY). Descriptive statistics are presented as means with standard deviations. The Shapiro–Wilk test was used to check the normality of the outcome variables. To evaluate the intervention effects, the Wilcoxon signed-rank test was used to compare measures pre- and postintervention in each group. The Mann–Whitney U test was used to compare the intergroup changes in outcome measurements. A P-value of <.05 was deemed statistically significant.
3. Results
3.1. Participants
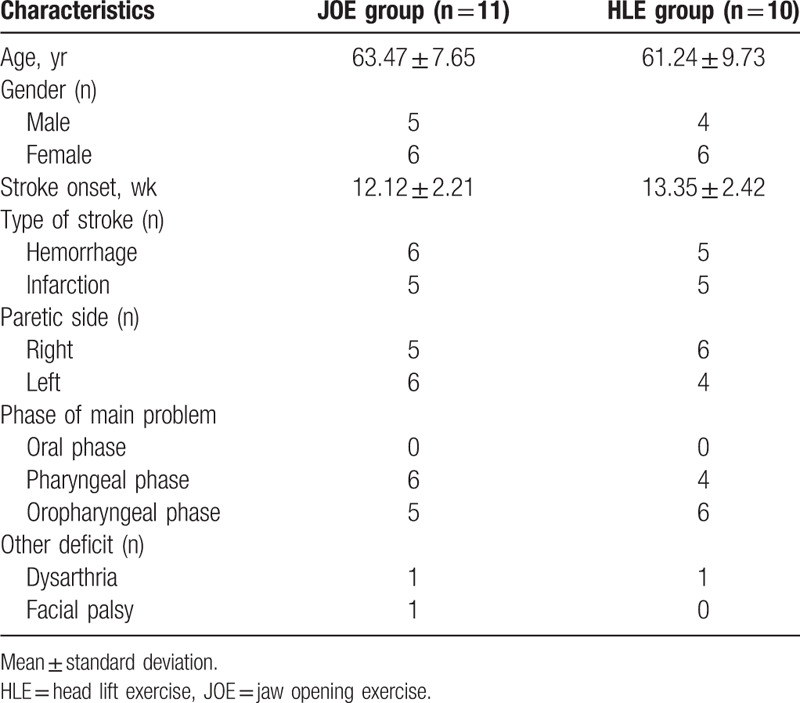
During the intervention period, 9 people were dropped out. Therefore, we analyzed the final 21 data. The homogeneity test for each measured item showed no significant differences in baseline clinical and demographic data between the groups (P > .05). A summary of the clinical and demographic features of the subjects is summarized in Table 1.
Table 1.
Characteristics of subjects.
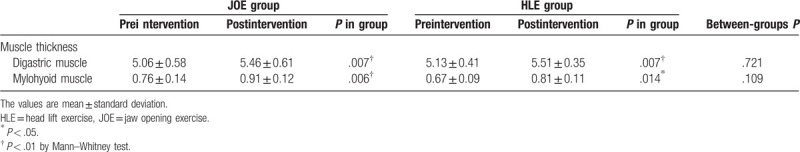
3.2. Effects on muscle thickness
The JOE group showed a statistically significant increase in the thickness of the digastric and mylohyoid muscles (P = .007 and .006, respectively). The HLE group also showed a statistically significant increase in the thickness of the digastric and mylohyoid muscles (P = .007 and .014, respectively). After the intervention, there was no significant difference in the thickness of the digastric and mylohyoid muscles between the 2 groups (P = .721 and .109, respectively) (Table 2).
Table 2.
Comparison of results between 2 groups (unit: mm).
3.3. Effects on hyoid movement
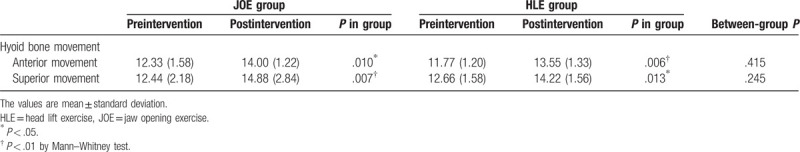
The JOE group showed a statistically significant increase in anterior and superior movement of the hyoid bone (P = .010 and .007, respectively). The HLE group also showed a statistically significant increase in anterior and superior movement of the hyoid bone (P = .006 and .013, respectively). After the intervention, there was no significant difference in anterior and superior movement of the hyoid bone between the 2 groups (P = .415 and .245, respectively) (Table 3).
Table 3.
Comparison of results between 2 groups (unit: mm).
3.4. Borg scale rating during therapeutic exercise
Borg scale rating showed an average of 10.5 ± 4.5 in the JOE group and the HLE group showed an average of 15.8 ± 5.3. There were statistically significant differences between the 2 groups (P < .05).
3.5. Dropout-rate related compliance
Three participants in the JOE group reported temporary temporomandibular joint fatigue and discomfort during exercise; however, only 1 dropped out of the study. As 2 participants had some discomfort in the temporomandibular joint, they wanted to continue exercising. Four participants in the HLE group reported neck or abdominal muscle fatigue and discomfort during exercise; 3 of them elected to drop out of the study. After the intervention, there were no side effects reported in either of the groups.
4. Discussion
During swallowing, the contraction of the suprahyoid muscles pulls the hyoid bone in the anterior-superior direction. As a result, it affects normal swallowing mechanisms such as epiglottis tilting and UES opening. Therefore, training to strengthen the suprahyoid muscle is important for safe swallowing. This study aimed to investigate the effects of the newly reported JOE on the thickness change of suprahyoid muscle, in comparison to the HLE.
This study measured the thickness of the digastric and mylohyoid muscles using ultrasonography. Both groups showed a significant increase in muscle thickness, but there was no significant difference between the 2 groups after intervention. This indicates that both the JOE and the HLE have similar effects with respect to increasing thickness of the digastric and mylohyoid muscles. Strength training that provides loading is known to be an effective method for increasing the thickness of skeletal muscles. This is associated with an increase in the number of myofibers and, as a result, an increase in thickness, which is known as muscle hypertrophy.[21,22] Resistance training of skeletal muscles causes immediate muscle activation, which indicates an increase in the number of recruited motor units.[23] Recently, Oh[24] investigated resistance training in the elderly through the head extension swallowing exercise and found significant muscle activation of the digastric and mylohyoid muscles as well as increased muscle thickness. These findings are similar to the results of this study. Therefore, it is possible that repeated induction of muscle activation through the JOE and the HLE may lead to an increase in muscle thickness.
An important factor in inducing muscle physiology changes, such as changes in muscle thickness through resistance training, is adequate resistance and exercise duration. Previous studies have reported that both the JOE and the HLE induce high muscle activation of the suprahyoid muscles using sEMG,[3,6,25] suggesting that these exercises have the potential for increasing the thickness of the suprahyoid muscle over a period of repeated training. In particular, training periods of at least 6 to 8 weeks are recommended to induce physiological changes in skeletal muscle, such as muscle hypertrophy.[26] This study also applied resistance training for 6 weeks and this period seems to be a somewhat appropriate period for increasing the thickness of the suprahyoid muscles.
One of the important roles of the suprahyoid muscle in normal swallowing is the kinematic effect of pulling the hyoid bone, as epiglottis rotation and UES opening are somewhat dependent on the hyoid bone movement. In this study, we showed significant improvement in hyoid bone movement in both the JOE and HLE groups, which is similar to previous results.[5,17] However, there was no significant difference between the 2 groups, suggesting that the 2 methods have similar effects on hyoid bone movement. A strong contractile force of the suprahyoid muscle is needed to pull the hyoid bone fully upwards during swallowing. One of the best options for this required increase in muscle strength is resistance training. Therefore, the increase in hyoid bone movement in this study can be explained by the increase in the thickness of the suprahyoid muscles through resistance training, as muscle contractile force is closely related to muscle thickness. In other words, the results of the study assume that an increase in muscle thickness results in an increase in muscle contractile force and, therefore, an increase in hyoid bone movement. Previous studies have demonstrated that resistance training of the suprahyoid muscles, through the HLE, is effective in increasing hyoid bone movement.[5,12]
Finally, we measured the intensity level of physical activity for both exercise methods using BRPES. It was found that the JOE group had a significantly lower BRPES score than the HLE group. This finding implies that the JOE is a less demanding and rigorous exercise than the HLE, which is important for ensuring patient compliance. In this study, 1 patient (5%) in the JOE exercise group and 3 patients (10%) in the HLE group dropped out due to problems such as muscle fatigue and tolerance, which means that the JOE requires less physical effort than the HLE. However, 3 patients in the JOE group reported muscles fatigue or discomfort in the temporomandibular joint. In other words, the repetitive JOE has the potential to cause temporomandibular joint pain and dislocation problems. Therefore, this study does not recommend the JOE for patients with serious temporomandibular joint problems. In addition, special attention should be paid to the discomfort and fatigue of the temporomandibular joint during exercise.
This study has some limitations. First, we cannot generalize the results of this study due to the limited number of subjects. Second, the intensity of the JOE could not be controlled objectively. Third, despite efforts to minimize the bias of ultrasound measurements, there may have been some errors in the measurements. Further studies are needed to overcome these limitations.
5. Conclusion
This study demonstrated that both the JOE and the HLE had similar effects with respect to increasing the thickness of the suprahyoid muscles and improving hyoid bone movement. However, the JOE may require less overall physical effort than the HLE, but may cause discomfort in the temporomandibular joint. Therefore, it is recommended that these 2 exercises be selected based on the condition of the patient.
Author contributions
Conceptualization: Jong-Bae Choi.
Data curation: Jong-Bae Choi.
Funding acquisition: Young-Jin Jung.
Investigation: Jong-Bae Choi.
Methodology: Ji-Su Park.
Writing – original draft: Young-Jin Jung, Ji-Su Park.
Writing – review & editing: Ji-Su Park.
Glossary
Abbreviations: HLE = head lift exercise, JOE = jaw opening exercise.
References
- [1].Antunes EB, Lunet N. Effects of the head lift exercise on the swallow function: a systematic review. Gerodontology 2012;29:247–57.. [DOI] [PubMed] [Google Scholar]
- [2].Easterling C, Grande B, Kern M, et al. Attaining and maintaining isometric and isokinetic goals of the Shaker exercise. Dysphgia 2005;20:133–8.. [DOI] [PubMed] [Google Scholar]
- [3].Koshi N, Matsumoto H, Hiramatsu T, et al. Influence of backrest angle on swallowing musculature activity and physical strain during the head lift exercise in elderly women compared with young women. J Oral Rehabil 2018;45:532–8.. [DOI] [PubMed] [Google Scholar]
- [4].Woo HS, Won SY, Chang KY. Comparison of muscle activity between two adult groups according to the number of Shaker exercise. J Oral Rehabil 2014;41:409–15.. [DOI] [PubMed] [Google Scholar]
- [5].Park JS, Hwang NK, Oh DH, et al. Effect of head lift exercise on kinematic motion of the hyolaryngeal complex and aspiration in patients with dysphagic stroke. J Oral Rehabil 2017;44:385–91.. [DOI] [PubMed] [Google Scholar]
- [6].Pearson WG, Langmore SE, Yu LB, et al. Structural analysis of muscles elevating the hyolaryngeal complex. Dysphagia 2012;27:445–51.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Pearson WG, Hindson DF, Langmore SE, et al. Evaluating swallowing muscles essential for hyolaryngeal elevation by using muscle functional magnetic resonance imaging. Int J Radiat Oncol Biol Phys 2013;85:735–40.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Mishra A, Rajappa A, Tipton E, et al. The recline exercise: comparisons with the head lift exercise in healthy adults. Dysphagia 2015;30:707–30.. [DOI] [PubMed] [Google Scholar]
- [9].Choi JB, Shim SH, Yang JE, et al. Effects of Shaker exercise in stroke survivors with oropharyngeal dysphagia. NeuroRehabilitation 2017;41:753–7.. [DOI] [PubMed] [Google Scholar]
- [10].Sze WP, Yoon WL, Escoffier N, et al. Evaluating the training effects of two swallowing rehabilitation therapies using surface electromyography: chin tuck against resistance (CTAR) exercise and the shaker exercise. Dysphagia 2016;31:195–205.. [DOI] [PubMed] [Google Scholar]
- [11].White KT, Easterling C, Roberts N, et al. Fatigue analysis before and after shaker exercise: physiologic tool for exercise design. Dysphagia 2008;23:385–91.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Koyama Y, Sugimoto A, Hamano T, et al. Proposal for a modified jaw opening exercise for dysphagia: a randomized, controlled trial. Tokai J Exp Clin Med 2017;42:71–8.. [PubMed] [Google Scholar]
- [13].Yoon WL, Khoo JK, Rickard Liow SJ. Chin tuck against resistance (CTAR): new method for enhancing suprahyoid muscle activity using a Shaker-type exercise. Dysphagia 2014;29:243–8.. [DOI] [PubMed] [Google Scholar]
- [14].Gao J, Zhang HJ. Effects of chin tuck against resistance exercise versus Shaker exercise on dysphagia and psychological state after cerebral infarction. Eur J Phys Rehabil Med 2017;53:426–32.. [DOI] [PubMed] [Google Scholar]
- [15].Park JS, An DH, Oh DH, et al. Effect of chin tuck against resistance exercise on patients with dysphagia following stroke: a randomized pilot study. NeuroRehabilitation 2018;42:191–7.. [DOI] [PubMed] [Google Scholar]
- [16].Hughes T, Watts CR. Effects of 2 resistive exercises on electrophysiological measures of submandibular muscle activity. Arch Phys Med Rehabil 2016;97:1552–7.. [DOI] [PubMed] [Google Scholar]
- [17].Wada S, Tohara H, Iida T, et al. Jaw-opening exercise for insufficient opening of upper esophageal sphincter. Arch Phys Med Rehabil 2012;93:1995–9.. [DOI] [PubMed] [Google Scholar]
- [18].Park JS, Lee G, Jung YJ. Effects of game-based chin tuck against resistance exercise vs head-lift exercise in patients with dysphagia after stroke: an assessor-blind, randomized controlled trial. J Rehabil Med 2019;51:749–54.. [DOI] [PubMed] [Google Scholar]
- [19].Park JS, Lee SH, Jung SH, et al. Tongue strengthening exercise is effective in improving the oropharyngeal muscles associated with swallowing in community-dwelling older adults in South Korea: a randomized trial. Medicine (Baltimore) 2019;98:17304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982;14:377–81.. [PubMed] [Google Scholar]
- [21].Schoenfeld BJ, Ogborn DI, Krieger JW. Effect of repetition duration during resistance training on muscle hypertrophy: a systematic review and meta-analysis. Sports Med 2015;45:577–85.. [DOI] [PubMed] [Google Scholar]
- [22].Schoenfeld BJ, Ogborn D, Krieger JW. Effects of resistance training frequency on measures of muscle hypertrophy: a systematic review and meta-analysis. Sports Med 2016;46:1689–97.. [DOI] [PubMed] [Google Scholar]
- [23].Wheeler KM, Chiara T, Sapienza CM. Surface electromyographic activity of the submental muscles during swallow and expiratory pressure threshold training tasks. Dysphagia 2007;22:108–16.. [DOI] [PubMed] [Google Scholar]
- [24].Oh JC. Effect of the head extension swallowing exercise on suprahyoid muscle activity in elderly individuals. Exp Gerontol 2018;110:133–8.. [DOI] [PubMed] [Google Scholar]
- [25].Oh JC, Kwon JS. Effects of resistive jaw-opening exercise with elastic bands on suprahyoid muscle activation in normal subjects. Folia Phoniatr Logop 2018;70:101–8.. [DOI] [PubMed] [Google Scholar]
- [26].Borde R, Hortobágyi T, Granacher U. Dose-response relationships of resistance training in healthy old adults: a systematic review and meta-analysis. Sports Med 2015;45:1693–720.. [DOI] [PMC free article] [PubMed] [Google Scholar]


