Abstract
Introduction:
Asian-Americans have been documented to have low human papillomavirus (HPV) vaccine initiation and completion. No research has attempted to examine underlying mechanisms of HPV vaccine uptake disparities among Asian-Americans. Using the P3 (practice, provider, and patient) model, this study aimed to identify practice-, provider-, and patient-level determinants of Asian-Americans’ HPV vaccine intention and uptake.
Methods:
We conducted a systematic review of published literature regarding practice-, provider- and patient-level determinants of vaccine intention (e.g., intention, willingness, or acceptability) and uptake (e.g., initiation or completion). Eligible studies were those presenting empirical/original data, focusing on Asian populations in the U.S., including outcomes related to HPV vaccine intention and uptake, and analyzing data on factors associated with these outcomes separately for Asian groups.
Results:
Twenty-six studies (19 quantitative and 7 qualitative studies) were included in the review. Most commonly studied subgroups were Koreans (n = 9), Chinese (n = 6), and Cambodians (n = 5). Studies showed varied prevalence across subgroups (intention: 23.4%–72%; initiation: 14%–67%; completion: 9%–63%). Only 3 studies included measurements of practice-level determinants (language services, insurance policy). Twelve studies measured provider-level determinants (most commonly documented: HPV vaccine recommendation). All studies measured patient-level determinants (most commonly documented: HPV and HPV vaccine knowledge, perceived safety, perceived susceptibility, and perceived relationship between HPV vaccine and sexual activity).
Conclusions:
Existing research on determinants of HPV vaccine intention and uptake among Asian-Americans currently lacks measurements of practice-level constructs and perspectives of clinic staff and providers, which are needed to guide system-level interventions and provider training. Data regarding patient-level determinants suggest that interventions for Asian-American populations can focus on providing educational information in culturally-appropriate manners, leveraging familial influences, and attending to access-related or cultural beliefs about HPV vaccine. Interventions should take into account varied vaccine intention and uptake prevalence in different Asian subgroups.
Keywords: Asian-Americans, HPV vaccine intention, HPV vaccine uptake, Systematic review, Multilevel factors
1. Introduction
Asian-Americans are extraordinarily heterogeneous, representing people from over 30 countries and speaking over 100 languages/dialects, with diverse immigration histories, socioeconomic status, religious/cultural beliefs, social norms, and patterns of health services utilization [1,2]. Numbering around 22 million, Asians are currently the fastest-growing racial/ethnic group in the U.S. [3–5]. Despite their growing number, Asians have traditionally been overlooked in health disparities research [6–8], partially due to the “model minority” stereotype (i.e., overemphasis on Asians’ ability to overcome hardship and succeed in America) [9].
One area that merits special attention is HPV vaccination among Asian adults and adolescents. The 2013–2016 National Health and Nutrition Examination Surveys (NHANES) indicated that Asians aged 9 to 26 have the lowest levels of HPV vaccine initiation among all racial/ethnic groups [10]. For example, the 2015–2016 NHANES wave showed that 39.6% of female Asians had initiated the vaccine, which was lower than female non-Hispanic Whites (48.4%), non-Hispanic Blacks (49.2%), Mexican-Americans (42.4%), and other Hispanic (42.6%). Among male Asians, prevalence of initiation was 26.4%, again lower than that of male non-Hispanic Whites (27.8%), non-Hispanic Blacks (28.1%), Mexican-Americans (28.0%), and other Hispanic (27.8%) [10].
The 2013–2015 National Health Interview Surveys (NHIS) also showed that Asian adult women have lower HPV vaccine initiation and completion coverage compared to non-Hispanic Whites [11,12]. For example, in the 2015 NHIS wave, the prevalence of Asian women’s HPV vaccine initiation and completion was 29.4% and 17.5%, respectively, in comparison to 37.9% and 26.7% for non-Hispanic Whites [11]. Furthermore, the 2018 National Immunization Teen – Survey demonstrated that 65.3% and 53.1% of Asian adolescents had initiated and completed the HPV vaccine series, respectively, both of which were lower than Black adolescents (72.8% and 53.3%) and Hispanic adolescents (75.5% and 56.6%) [13]. Research with college students also consistently reported that Asian students have lower HPV vaccination coverage compared to White students [14–17].
Despite this evidence, no research has attempted to examine underlying mechanisms of HPV vaccine uptake disparities among Asian-Americans. While a number of systematic reviews have focused on factors influencing HPV vaccine attitudes, acceptability, and uptake among general U.S. populations [18–21] and among minorities such as African-Americans and Latinos [22] or immigrants [23], to date no such review has focused on Asians. This gap in the literature makes it difficult for researchers interested in this population to understand and intervene on important determinants of HPV vaccine utilization. Indeed, to date, we are aware of only three published interventions targeting HPV vaccine among Asian-Americans: a text-messaging intervention for Korean-Americans [24] and two storytelling interventions for Korean-Americans and Vietnamese-Americans [25,26].
1.1. Theoretical framework and outcome measurements
Our guiding framework for this systematic review is the P3 (practice, provider, and patient) model [27]. The P3 model is a framework for understanding influences on preventive health behaviors (e.g., HPV vaccination) across three levels – the practice (e.g., vaccine supply, vaccine policy, use of standing orders), provider (e.g., clinical experiences, training, self-efficacy), and patient (e.g., sociodemographic characteristics, attitudes, access to care, social influences). Within each of the three levels, influences can be further categorized into different domains, such as healthcare delivery/organizational, communication style, predisposing, enabling, and reinforcing factors [28,29].
In using the P3 model, we aim to highlight possible multilevel influences on HPV vaccine intention and uptake. Increasingly, researchers recognize that health behaviors and outcomes are not just driven by individual-level factors, but are often results of interplays between factors at multiple socioecological levels, such as individuals’ physiological processes and behavioral patterns; the physical, social, cultural, and economic contexts; and larger social and systemic processes [30–32]. The Institute of Medicine recommends that interventions should target multilevel influences instead of focusing on one level of determinants [31].
Our systematic review focuses on two outcomes: HPV vaccine intention and HPV vaccine uptake. We characterize studies as capturing HPV vaccine intention if they measured intention to get the vaccine, willingness to get the vaccine, or acceptability of getting the vaccine. For example, studies capturing vaccine intention would include self-reported measurements such as “Are you willing to vaccinate your child against HPV?” or “How likely are you to get HPV vaccine?” We characterized studies as capturing constructs of HPV vaccine uptake if they measured vaccine initiation (i.e., getting 1 or more doses of the vaccine) or vaccine completion (i.e., getting 2 or 3 doses of the vaccine, depending on the age of initiation). For example, studies capturing vaccine uptake would include self-reported measurements such as “Have you ever received one or more doses of HPV vaccine?” or “How many doses of HPV vaccine has your child gotten?” Studies capturing vaccine uptake can also use verified measurements such as medical records.
1.2. Objective
Using the P3 model, this systematic review aims to identify practice, provider, and patient-level determinants of HPV vaccine intention and uptake among Asian-Americans.
2. Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [33] guided the design and reporting of this review (see Fig. 1).
Fig. 1.
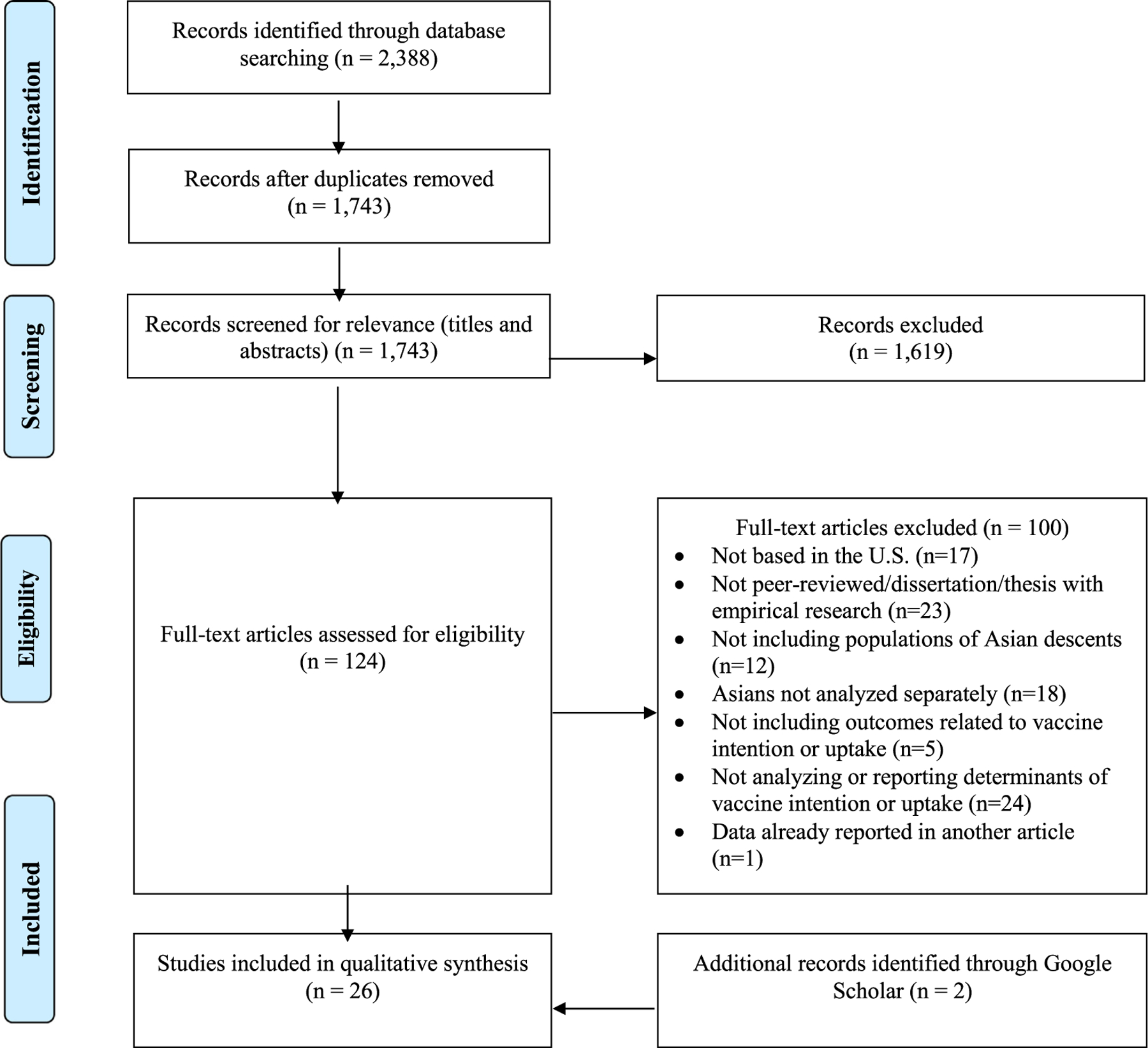
PRISMA flow chart of the searched, screened, identified, and included studies.
2.1. Search strategies
In May 2019, we performed systematic searches in five databases (PubMed, CINAHL, PsycINFO, ProQuest, and EMBASE). A trained health sciences librarian (LT) helped finalized the search terms and carried out the systematic searches. All search terms are included in Appendix A.
2.2. Inclusion and exclusion criteria
A study was included if it (a) was written in English, (b) was U. S.-based, (c) was a peer-reviewed article, dissertation, thesis, or report (e.g., research reports by the CDC or non-profit organizations) presenting empirical/original data, (d) was published between January 1994 and May 2019, (e) focused exclusively on Asian populations OR included Asian populations along with other racial/ethnic groups (e.g., Whites, Hispanic, Blacks) but analyzed data from Asian populations separately from other groups, (f) included outcomes related to HPV vaccine intention and uptake, and (g) analyzed data on factors associated with these outcomes.
2.3. Study selection
Two authors (HMJ and LT) independently screened titles and abstracts of records to select studies for full-text review. The lead author (MV) finalized the selection of studies for full-text review, reconciling any disagreements through discussions. Then, two authors (MV and HMJ) accessed full texts of these selected records and reviewed them to decide on studies included in the final analysis, resolving disagreements through discussions.
2.4. Data extraction
The lead author (MV) performed data extraction and two other authors (HMJ and TTN) reviewed these data to ensure accuracy. Information extracted from each article included: study design, data source, sample size, ethnic group, sex, and prevalence and determinants of HPV vaccine intention and uptake.
2.5. Data analysis
Using the P3 model as the framework, data were qualitatively synthesized. Determinants were organized into domains at each level (practice, provider, and patient). We further distinguished between outcomes of the studies (e.g., vaccine intention versus actual uptake). If studies reported both bivariate and multivariable analyses, we documented multivariable associations with p-values < 0.05 as influential determinants. If studies reported descriptive statistics (e.g., prevalence of reasons given for uptake), we documented categories reported at 20% or higher as influential determinants. In qualitative studies, main themes were documented as influential determinants.
2.6. Quality appraisal
We used the Quality Assessment Tool for Studies with Diverse Designs (QATSDD) [34] to critically appraise studies. The lead author (MV) scored each study; another author (HMJ) reviewed scoring to ensure accuracy. The QATSDD includes 16 criteria (e.g., theoretical framework, aims/objectives, data collection procedure, justification of analysis, and discussion of strengths and limitations), of which 12 apply to both quantitative and qualitative designs, 2 apply to only quantitative designs, and 2 apply to only qualitative designs. Each criterion was scored 0 to 3. A summary quality score was derived by summing scores and dividing by 14.
3. Results
Fig. 1 shows the selection process. We identified 2,388 records through database searches. After duplicates were removed, we screened the titles and abstracts of 1,743 articles for relevance, identifying 124 articles for full-text review. Of these 124 articles, 100 articles were excluded based on our criteria: not-based in the U.S. (n = 17), not peer-reviewed/dissertation/thesis with empirical research (n = 23), not including populations of Asians descents (n = 12), Asians not analyzed separately (n = 18), not including outcomes related to vaccine intention or uptake (n = 5), not analyzing or reporting determinants of vaccine intention or uptake (n = 24), and data already reported in another article (n = 1). Twenty-four articles were included in the final review. Additionally, through a Google Scholar search with the keywords “Asian Americans” and “HPV vaccine,” we identified 2 additional articles meeting criteria for inclusion in the review.
3.1. Study characteristics
Table 1 shows characteristics of the included 26 studies. Ethnic groups studied included: Koreans (n = 9; 35%), Chinese (n = 6; 23%), Cambodians (n = 5; 19%), South Asians (n = 2; 8%), Vietnamese (n = 2; 8%), Hmong (n = 2; 8%), Filipino (n = 1; 4%), and Japanese (n = 1; 4%). Three studies (12%) did not disaggregate participants by ethnic groups. Nineteen studies (73%) focused exclusively on Asian groups; the other 7 studies (27%) included other racial/ethnic groups in their analyses.
Table 1.
Characteristics of studies included in the systematic review (n = 26).
| Citation | Study design | Data source | Population | Gender | Quality rating (0–3) | Practice-level | Provider-level | Patient-level |
|---|---|---|---|---|---|---|---|---|
| [45]* | Cross-sectional survey | Mothers reporting vaccine uptake of teenage daughters | Chinese (n = 98) and Korean (n = 66) women of daughters aged 9–18 | 100% F | 2.36 | Assessed Influential | ||
| [43]* | Cross-sectional survey | Parents reporting vaccine uptake of children | Japanese (n = 200) and Filipino (n = 199) parents of children aged 11–18 | Not available for separate Asian subgroups | 2.50 | Assessed Influential | Assessed Influential | |
| [41] | Qualitative interviews and focus groups | Parents reporting vaccine uptake of teenage daughters | Cambodian community leaders (n = 13); Cambodian parents (n = 37) of daughters aged 9–26 | Community leaders: 54% F; Parents: 51% F |
1.79 | Assessed Influential | Assessed Influential | |
| [48]a | Cross-sectional survey | Participants reporting their own vaccine intention | Chinese international students (n = 350) aged 18–26 who had not received the vaccine | 48% F | 1.57 | Assessed | Assessed Influential | |
| [57] | Qualitative focus groups | Participants reporting their own vaccine intention | Chinese international students (n = 44) aged 18 or older | 52% F | 1.64 | Assessed Influential | ||
| [37]* | Qualitative interviews | Participants reporting their own vaccine uptake; Health center staff reporting their perspectives on clients’ vaccine uptake | Vietnamese women aged 18–26 (n = 24) Health center staff serving women (n = 2) |
Vietnamese: 100% F; Health center staff: N/A |
1.79 | Assessed Influential | Assessed Influential | Assessed Influential |
| [40] | Cross-sectional survey | Parents reporting intention to vaccinate children | South Asian parents (n = 136) of children aged 17 and below. The sample included Bangladeshis (n = 68), Indians (n = 40), Pakistanis (n = 15), Nepalese (n = 7) and Sri Lankans (n = 6). | 59% F | 1.71 | Assessed Influential | Assessed Influential | |
| [38] | Qualitative focus groups | Parents reporting intention to vaccinate children | Korean women aged 21–65 (n = 12) and community health workers (n = 14) | 100% F | 2.43 | Assessed Influential | Assessed Influential | |
| [36] | Qualitative focus groups | Participants reporting their own vaccine uptake | Korean female college students aged 18–26 (n = 20) | 100% F | 1.79 | Assessed Influential | Assessed Influential | Assessed Influential |
| [52] | Cross-sectional survey | Participants reporting their own vaccine intention and uptake | Korean female undergraduate and graduate students (n = 104) | 100% F | 2.07 | Assessed | Assessed Influential | |
| [55]* | Cross-sectional survey | Participants reporting their own vaccine uptake | Asian female students (n = 85) | 100% F | 1.57 | Assessed Influential | ||
| [35] | Qualitative focus groups | Participants reporting their own vaccine intention | Korean immigrant women (n = 16) | 100% F | 1.79 | Assessed Influential | Assessed Influential | Assessed Influential |
| [17]* | Cross-sectional survey | Participants reporting their own vaccine uptake | Asian and Pacific Islander female college students (n = 341). The sample included Chinese (n = 93), Hmong (n = 70), South Asians (n = 42), and Koreans (n = 40) | 100% F | 2.29 | Assessed Influential | ||
| [58] | Cross-sectional survey | Mothers reporting intention to vaccinate daughters; daughters reporting intention to get vaccinated | 19 dyads of Cambodian mothers and their teenage daughters (aged 14–17) (n = 38 in total); daughters have not received the vaccine | 100% F | 2.07 | Assessed Influential | ||
| [54] | Cross-sectional survey | Mothers reporting HPV vaccine uptake of teenage daughters | Cambodian mothers (n = 130) of teenage daughters aged 12–17 | 100% F | 2.50 | Assessed Influential | ||
| [39] | Qualitative focus groups | Parents reporting intention to vaccinate children | Korean parents (n = 20) of children aged 11–18 | 50% F | 2.57 | Assessed Influential | Assessed Influential | |
| [46] | Cross-sectional survey | Parents reporting vaccine uptake of children and their intention to vaccinate children | Korean parents (n = 74) of children aged 11–18 | 64% F | 2.50 | Assessed Influential | ||
| [50] | Cross-sectional survey | Self-reported; Mothers/grand-mothers reporting intention to vaccinate daughters/grand-daughters | Chinese women aged 18 or older (n = 158) | 100% F | 2.00 | Assessed Influential | ||
| [53]* | Cross-sectional survey | Adults reporting intention to vaccinate real or hypothetical daughter | Asian/Pacific Islander adults (weighted N: 8789113 or 5% of sample) | N/A for Asian groups | 1.64 | Assessed Influential | ||
| [82]b | Cross-sectional survey | Participants reporting their own vaccine uptake | Hmong women aged 21 to 65 (n = 104) | 100% F | 2.57 | Assessed | ||
| [42] | Cross-sectional survey | Mothers reporting HPV vaccine status of teenage daughters | Cambodian mothers (n = 86) of teenage daughters aged 9–17 | 100% F | 1.93 | Assessed Influential | Assessed Influential | |
| [44] | Cross-sectional survey | Mothers reporting HPV vaccine status of teenage daughters | Cambodian mothers (n = 96) of teenage daughters aged 9–18 | 100% F | 1.79 | Assessed Influential | Assessed | |
| [49]* | Cross-sectional survey | Participants reporting their own vaccine uptake | Asians aged 9 to 21 (n = 635) | N/A for Asian groups | 2.07 | Assessed Influential | ||
| [47] | Cross-sectional survey | Participants reporting their own vaccine uptake | Chinese college students aged 18 or older (n = 449) | 59% F | 2.14 | Assessed Influential | ||
| [51] | Cross-sectional survey | Participants reporting their own vaccine intention and uptake | Vietnamese women aged 18 or older (n = 113) | 100% F | 2.21 | Assessed Influential | ||
| [56] | Cross-sectional survey | Mothers reporting intention to vaccinate daughters | Korean women aged 25 to 45 (n = 165) | 100% F | 2.21 | Assessed Influential |
F: female; M: male.
N/A: Not available.
Assessed: determinant included in measurement; Influential: determinant documented to be influential.
The 2015 dissertation contained some similar data to the 2016 article by the same author. Only data not reported in the 2016 article are presented in this row.
This study reported no significant finding on influences on HPV vaccine intention or uptake, and thus is not included in Table 2a, 2b, 2c, or 2d.
Study includes not only Asians but also other racial/ethnic groups in their analyses.
The studies captured perspectives of the following participant groups: caregivers (e.g., parents; n = 14; 54%), college students (n = 7; 27%), general adult populations (n = 7; 27%), adolescents (n = 2; 8%), community leaders (n = 1; 4%), community health workers (n = 1; 4%), and health center staff (n = 1; 4%). Eighteen studies (69%) only included women in their sampling. Nineteen studies (73%) employed a quantitative design, all of which used cross-sectional surveys. The other seven studies (27%) used a qualitative design (interviews, n = 2 and focus groups, n = 6).
Ten studies (38%) reported prevalence of HPV vaccine intention and 11 studies (42%) reported determinants of HPV vaccine intention. Thirteen studies (50%) reported prevalence of HPV vaccine uptake (not including the 3 studies in which only unvaccinated participants were recruited), and 16 studies (62%) reported determinants of HPV vaccine uptake. Studies showed a considerable variation in prevalence of intention and uptake. Reported intention prevalence ranged from 23.4% to 72%. Reported initiation prevalence ranged from 14% to 67% and completion prevalence ranged from 9% to 63% (Table 2).
Table 2.
Prevalence of HPV vaccine intention and/or uptake reported in studies (n = 26).
| Citation | Population | N | % of HPV vaccine intention | % of HPV vaccine initiation | % of HPV vaccine completion | % of HPV vaccine uptake* |
|---|---|---|---|---|---|---|
| [45] | Daughters aged 9–18 of Chinese mothers | 97 | 25% | 9% | ||
| Daughters aged 9–18 of Korean mothers | 62 | 24% | 13% | |||
| [43] | Daughters aged 11–18 of Filipino parents | 122 | 45.1% | 21.3% | ||
| Daughters aged 11–18 of Japanese parents | 120 | 60.8% | 40.8% | |||
| Sons aged 11–18 of Filipino parents | 103 | 35.9% | 12.6% | |||
| Sons aged 11–18 of Japanese parents | 111 | 50.5% | 22.5% | |||
| [41] | Daughters of Cambodian community leaders | 7 | 42.9% | |||
| Daughters aged 9–26 of Cambodian parents | 37 | Only a couple of parents said their daughters had received the HPV vaccine. | ||||
| [48] | Female Chinese international students aged 18–26 | 169 | 10.1% unlikely, 20.7% undecided, 69.2% likely to get the vaccine | 0% (only those who had not initiated the vaccine were included for data analysis) | ||
| Male Chinese international students aged 18–26 | 179 | 41.1% unlikely, 24.2% undecided, 34.9% likely to get the vaccine | ||||
| [57] | Chinese international students aged 18 or older | 44 | ||||
| [37] | Vietnamese women aged 18–26 | 24 | 67% | 63% | ||
| [40] | South Asian parents with daughters aged 17 and below |
77 | 55.8% intended to vaccinate their daughters | |||
| South Asian parents with sons aged 17 and below | 80 | 41.3% intended to vaccinate their sons | ||||
| [38] | Korean women aged 21–65 | 12 | ||||
| [36] | Korean female college students aged 18–26 | 20 | ||||
| [52] | Korean female undergraduate and graduate students aged 18–26 | 104 | 34.6% intended to get the vaccine | 0% (only those who had not initiated the vaccine were recruited into the study) | ||
| [55] | Asian female students | 85 | ||||
| [35] | Korean immigrant women aged 21–29 | 16 | ||||
| [17] | Asian and Pacific Islander female college students aged 18–25 | 341 | 38.6% | |||
| [58] | Cambodian mothers of their daughters aged 14–17 | 19 | 68.4% of mothers intended to have their daughters vaccinated | |||
| Daughters aged 14–17 of Cambodian mothers | 19 | 36.8% of daughters intended to get vaccinated | 0% (only daughters who had not initiated the vaccine were recruited into the study) | |||
| [54] | Daughters aged 12–17 of Cambodian mothers | 129 | 32.6% | |||
| Sons of Cambodian mothers | 70 | 18.6% | ||||
| Cambodian mothers of teenage daughters aged 12–17 | 86 | 72% of mothers of unvaccinated daughters reported they would like their daughters to receive vaccinations | ||||
| [39] | Children aged 11–18 of Korean parents | 20 | ||||
| [46] | Children aged 11–18 of Korean parents | 74 | 73% | |||
| [50] | Chinese women aged 18 or older | 158 | 29.1% would like vaccine for self if cost involved, and 41.1% would like vaccine for self if no cost or little cost involved; 23.4% would like vaccine for daughter or granddaughter if cost involved; 31% would like vaccine for daughter or granddaughter if no cost or little cost involved |
|||
| [53] | Asian/Pacific Islander adults aged 18 and above | (weighted N: 8789113 or 5% of sample) | ||||
| [82] | Hmong women aged 21 to 65 | 104 | 14% | |||
| [42] | Daughters aged 9–17 of Cambodian mothers | 86 | 29% | 14% | ||
| [44] | Daughters of Cambodian mothers | 96 | 26% | |||
| [49] | Asians aged 9 to 21 | 635 | 27% | |||
| [47] | Chinese college students aged 18 or older | 449 | 38.3% | 22% | ||
| [51] | Vietnamese women aged 18 or older | 113 | Among those who were unvaccinated, 13.4% responded that they were not at all likely to receive HPV vaccine; 20.6% somewhat likely; 33% very or extremely likely | 14% | 10% | |
| [56] | Korean women aged 25 to 45 | 165 |
Studies that did not specify whether the reported uptake rate was for vaccine initiation or completion.
3.2. Quality appraisal
Study quality ranged from 1.57 to 2.57. Among all studies, most common issues encountered were a lack of sample size calculation (n = 19; 73%), user involvement in design (n = 19; 73%), and explicit theoretical framework (n = 14, 46%). Among quantitative studies, the most common issue encountered was a lack of assessment of reliability and validity (n = 10; 53%). Among qualitative studies, the most common issue encountered was a lack of reliability assessment for analytical procedures (n = 3; 43%).
3.3. Practice-level determinants of HPV vaccine intention and uptake
Only three studies (12%) measured practice-level determinants of HPV vaccine intention and uptake; all of them found influential practice-level determinants related to healthcare delivery or organizational factors (Table 3 and Appendix B). Two studies with Korean women highlighted the importance of language services at the clinic. Participants reported difficulties grasping English medical jargon [35] and worrying about going to the doctor due to difficulties understanding English [36]. One study interviewed clinicians at a Planned Parenthood clinic serving Vietnamese women and found that insurance policy of the clinic could be a barrier to vaccine uptake [37], as women could only get the vaccine at their primary care doctor and not at the Planned Parenthood.
Table 3.
Practice-level determinants of HPV vaccine intention and uptake.
3.4. Provider-level determinants of HPV vaccine intention and uptake
Twelve studies (46%) measured provider-level determinants of HPV vaccine intention and uptake. Ten studies found influential provider-level determinants. They were all measured through patients’ perceptions and all centered around communication between patients/caregivers and providers about HPV vaccine (i.e. communication style in the P3 model) (Table 4 and Appendix B).
Table 4.
Provider-level determinants of HPV vaccine intention and uptake.
| Domain | Provider-level determinant | Intention (reported by caregivers for their adolescents) | Intention (reported by participants for themselves) | Uptake (reported by caregivers for their adolescents) | Uptake (reported by participants for themselves) |
|---|---|---|---|---|---|
| Communication style | Recommendation from providers about HPV vaccine (n = 8) | [38–40] | [41–44] | [36] | |
| Discussion or conversation with providers about HPV vaccine (n = 3) | [39–40] | [37] | |||
| Providers’ advice regarding likelihood of getting cervical cancer (n = 2) | [35] | [36] | |||
| Hearing of HPV vaccine from providers (n = 1) | [42] | ||||
| Having asked providers for HPV vaccination (n = 1) | [44] |
Eight studies documented the role of HPV vaccine recommendations from providers. A provider’s recommendation was given as the reason why Korean college women got HPV vaccine for themselves [36]. Provider’s recommendation was also a reason influencing parents’ vaccine intention [38–40] or vaccine uptake [41–43] for their children. A study with Cambodian mothers of teenage daughters found a significant association between a provider’s recommendation and the teenage daughter’s HPV vaccine uptake [44]. Conversely, in four studies, caregivers also mentioned not having received a provider’s recommendation as a reason why they had not gotten HPV vaccine for their children [39,41–43].
Relatedly, discussion/conversation with providers about HPV vaccine was also important. Vietnamese women described conversations with providers about HPV vaccine as critical to vaccine uptake [37]. Korean parents reported limited communication with providers as a barrier to making informed decision about HPV vaccine [39]. South Asian parents cited a lack of discussion with providers as a reason for vaccination noncompliance [40].
Two studies with Korean women found that providers advised that Korean women were at lower risk for cervical cancer or that only “promiscuous” women would get cervical cancer, which factored into participants’ decision to not get the vaccine [35,36]. Finally, studies with Cambodian mothers found that daughters’ vaccine initiation was associated with mothers hearing of HPV vaccine from providers [42] or that daughters’ vaccine uptake was associated with mothers having asked providers for HPV vaccination [44].
3.5. Patient-level determinants of HPV vaccine intention and uptake
All 26 studies (100%) measured patient-level determinants. Twenty four out of 26 studies found influential patient-level determinants (Table 5 and Appendix B).
Table 5.
Patient-level determinants of HPV vaccine intention and uptake.
| Domain | Patient-level determinant | Intention (reported by caregivers for their adolescents) | Intention (reported by participants for themselves) | Uptake (reported by caregivers for their adolescents) | Uptake (reported by participants for themselves) |
|---|---|---|---|---|---|
| Healthcare delivery or organizational factors | Knowledge of where to get HPV vaccine (n = 1) | [45] | |||
| Knowledge of whether insurance covers HPV vaccine (n = 1) | [43] | ||||
| Access to clinics or providers with HPV vaccine (n = 1) | [46] | ||||
| Pap test receipt (n = 1) | [42] | ||||
| Level of familiarity with U.S. healthcare services (n = 1) | [35] | ||||
| Level of comfort with women’s health services (n = 1) | [35] | ||||
| Level of use of women’s health services (n = 1) | [17] | ||||
| Communication style | Parent-child discussion about HPV vaccine (n = 1) | [38] | |||
| Predisposing factors | Age (n = 3) | [40] | [17,47] | ||
| Child’s age (n = 2) | [39] | [43] | |||
| Sex (n = 4) | [40] | [48] | [47,49] | ||
| Language (n = 3) | [50] | [36,51] | |||
| HPV vaccine awareness (n = 4) | [41–43] | [52] | |||
| HPV or HPV vaccine knowledge (n = 9) | [40,53] | [35,52] | [54] | [17,36,47,51] | |
| General vaccine attitudes (n = 1) | [40] | ||||
| HPV vaccine attitudes (n = 2) | [40] | [47] | |||
| Belief about prevention (n = 1) | [41] | ||||
| Trust in Western medicine (n = 1) | [41] | ||||
| Medical mistrust (n = 1) | [55] | ||||
| Perceived HPV vaccine importance (n = 2) | [40,56] | ||||
| Perceived HPV vaccine effectiveness (n = 3) | [40] | [41,46] | |||
| Perceived HPV vaccine safety or side effect (n = 7) | [38–40] | [41,43,45] | [36] | ||
| HPV vaccine is too new (n = 3) | [39–40] | [43] | |||
| Perceived susceptibility (n = 5) | [35,57] | [43] | [36,52] | ||
| No need for HPV vaccine if not sexually active (n = 5) | [39–40] | [57] | [41] | [52] | |
| No need for HPV vaccine if practicing safe sex (n = 1) | [57] | ||||
| Trust in partner’s HPV status (n = 1) | [37] | ||||
| HPV vaccine promotes child’s sexual activity or promiscuity (n = 3) | [38] | [41,43] | |||
| American lifestyle increases susceptibility; thus should get vaccinated (n = 1) | [57] | ||||
| Get all vaccines for my child (n = 1) | [43] | ||||
| Worry about child’s health (n = 1) | [40] | ||||
| Belief regarding suitability of vaccine for Chinese people (n = 1) | [57] | ||||
| Too busy (n = 2) | [36,52] | ||||
| Enabling factors | Perceived costs (n = 4) | [38–39] | [41] | [36] | |
| School policy (n = 1) | [38] | ||||
| Not enough information or needing more information (n = 2) | [40] | [45] | |||
| Reinforcing factors | Influence from mother (n = 3) | [58] | [36–37] | ||
| HPV vaccine recommendation by parents (n = 1) | [52] | ||||
| Influence from family (n = 1) | [36] | ||||
| Influence from family and friends (n = 1) | [56] | ||||
| Influence from friends (n = 2) | [35,48] | ||||
| Influence from other parents (n = 1) | [38] | ||||
| Have friends whose children are HPV vaccinated (n = 1) | [43] | ||||
| Influence from social media (n = 1) | [36] | ||||
| Motivation to get protection from disease (n = 4) | [38] | [42–43] | [37] | ||
| Family stigma around sexual health (n = 1) | [37] | ||||
| Knowing someone with cancer (n = 1) | [17] | ||||
| Family history of cancer (n = 1) | [35] | ||||
| Interdependent self-construal (n = 1) | [56] | ||||
| Preventive activity | Having to get multiple doses (n = 1) | [36] | |||
| Belief regarding recommended ages (9–26) (n = 1) | [57] |
3.5.1. Healthcare delivery or organizational factors
Parents’ barriers to HPV vaccine uptake for adolescents included not knowing where to get HPV vaccine [45] and not knowing whether insurance covers HPV vaccine [43]. Additionally, a study found that Cambodian mothers’ receipt of a Pap test was associated with daughters’ vaccine initiation [42]. Interestingly, a study with Korean parents noted that compared to those who with vaccinated children, those with unvaccinated children perceived the ability to access providers or clinics with HPV vaccine as less of a barrier [46]. Among adult participants, unfamiliarity with U.S. healthcare services or discomfort in using women’s health services were barriers to seeing providers and receiving HPV vaccine [35]. Participant’s use of women’s health services was also associated with vaccine completion [17].
3.5.2. Communication style
A study with Korean women found that those with older children tended to engage in conversations and a collaborative decision-making about HPV vaccine with the children [38].
3.5.3. Predisposing factors
Regarding age, younger participants were more likely to have received the vaccine [17,47], and younger parents were more willing to get HPV vaccine for their children [40]. At the same time, parents’ belief that their children were too young to get the vaccine was a barrier to vaccine intention [39] and uptake [43] for children. Moreover, sex also influenced vaccine intention and uptake. Among South Asians, compared to fathers of daughters, mothers of daughters were more willing to get HPV vaccine for daughters [40]. Adult women also had higher vaccine intention [48] or vaccine uptake [47,49] compared to men. Additionally, English language fluency also played a role. Unfamiliarity with English medical terms was a barrier to seeing providers and receiving HPV vaccine for Korean women [36]. Adult women with higher English fluency were more supportive of getting HPV vaccine for their children and grandchildren [50] or more likely to have received HPV vaccine for themselves [51].
A lack of awareness of HPV vaccine was noted as a barrier to parents’ vaccine uptake for children [41–43] and adult women’s own vaccine uptake [52]. Relatedly, surveys found that higher parental knowledge of HPV or HPV vaccine was associated with higher parental vaccine intention [40,53] and uptake [54] for their children. Adult participants with higher knowledge of HPV or HPV vaccine were more supportive of getting HPV vaccine for themselves [52] or more likely to have received HPV vaccine [17,47,51].
A study with South Asian parents [40] measured general attitudes towards vaccination through a scale exploring effectiveness, side effects, and benefits for children’s health. It also measured HPV vaccine attitudes (i.e. thoughts on whether HPV vaccine was necessary for males). The study found that parents’ higher vaccine intention was associated with more positive general attitudes towards vaccination and thinking that HPV vaccine was necessary for males [40]. Another study using a scale to measure attitudes towards HPV vaccination among Chinese college students also found that more positive attitudes were associated with higher vaccine initiation [47].
In the Cambodian community, beliefs regarding disease prevention (e.g., priority placed on preventive health measures) could both negatively and positively impact vaccine uptake [41]. Additionally, those with lower trust in Western medicine may refuse to get the vaccine for their children [41]. Relatedly, a study with Asian college students noted that compared to vaccinated women, unvaccinated women had higher levels of medical mistrust (defined as “distrust and suspicion of medical personnel and institutions”) [55].
Parents with higher perceived importance of HPV vaccine had higher vaccine intention for their children [40,56]. Parents with higher perceived effectiveness of HPV vaccine also had higher vaccine intention [40] or uptake [41,46] for their children. Moreover, parents who had higher perceived side effects or low safety of HPV vaccine were less accepting of the vaccine [38–40] or chose not to get the vaccine for their children [41,43,45]. Korean women mentioned side effects of the vaccine as a barrier to vaccine uptake [36]. In addition, parental perception of HPV vaccine being too new was mentioned as a barrier to vaccine intention [39,40] and vaccine uptake [43] for adolescent children.
Perceived susceptibility played an important role in influencing vaccine intention and uptake. For example, Filipino and Japanese parents cited their children not being at risk for HPV as a reason why they did not vaccinate their children [43]. Qualitative studies found that Korean and Chinese adults did not think of themselves as susceptible to HPV infection, genital warts, or HPV-related cancers; some also believed that only those who were gay or those frequently engaged in sexual activity were at risk, leading to non-vaccination [35,36,52,57].
In several studies, parents believed that HPV vaccine was not necessary if their children were not sexually active [39–41]. This belief was also reported as a reason why Chinese students did not intent to get the vaccine for themselves [57] and why Korean female college students did not get vaccinated [52]. Chinese students also reported not intending to get the vaccine if they were practicing safe sex [57] and Vietnamese women reported not getting the vaccine because they trusted that their partners were HPV-free [37].
The belief that HPV vaccine promoted adolescents’ sexual activity was mentioned as a reason against parents’ vaccine intention [38] and vaccine uptake [41,43] for adolescent children. In a study with international Chinese students, participants were concerned about the fact that HPV vaccine was developed in “Western countries” and questioned the suitability of the vaccine for Chinese people [57]. Participants in the same study also mentioned how living in America and dating Americans increased one’s susceptibility to getting HPV and thus the vaccine seemed more needed once they left China [57]. Filipino and Japanese parents discussed “getting all vaccines” as a reason for vaccine uptake for their children [43]. South Asians cited worry about their children’s health as a reason for vaccine intention for their children [40]. Korean students mentioned being too busy as a reason for non-vaccination [36,52].
3.5.4. Enabling factors
Perceived high costs were a barrier to HPV vaccine intention and uptake among Cambodian and Korean parents [38,39,41] and Korean women [36]. In addition, Korean women reported receiving and following a recommendation from the school to get HPV vaccine for their daughters [38]. Parents discussed not having enough information or needing more information about HPV vaccine as a barrier to vaccine intention [40] and uptake [45] for their children.
3.5.5. Reinforcing factors
Vietnamese and Korean women discussed their mothers’ influences in vaccine decision-making for themselves [36,37]. A study of Cambodian mother-daughter pairs found an association between a daughter’s vaccine intention and her perception of her mother’s intention for her to get vaccinated [58]. Additionally, among Korean female college students, HPV vaccine recommendation by parents was associated with vaccine intention [52] while hearing negative messages about the vaccine through family members was a barrier to uptake [36].
A study with Korean women found that those with higher subjective norms (e.g., perceived approval of HPV vaccine from family and friends) had higher intention of getting their children vaccinated [56]. In a study with international Chinese students, influence from friends (i.e. having a friend who got vaccinated against HPV) was a predictor of vaccine intention [48]. Among Korean women, negative messages about HPV vaccine heard through friends played a role in vaccine intention [35].
Korean parents discussed how other parents’ opinions influenced their decision-making about HPV vaccine for their children [38]. Filipino and Japanese parents indicated having friends whose children who were vaccinated as a reason why they got the vaccine for their children [43]. Korean female students also discussed hearing negative messages about the vaccine through social media as a barrier to vaccination [36].
Knowing someone with cancer was significantly associated with vaccine completion among Asian female college students [17]. Moreover, Vietnamese women discussed motivation to get protection from diseases as a reason for getting the vaccine [37]. Studies also reported that motivation to protect their children from diseases was a reason underlying parents’ vaccine intention [38] as well as vaccine uptake [42,43] for their children.
Other barriers to vaccine intention and uptake included not having a family history of cervical cancer and thus not thinking of themselves as being at risk [35] and family stigma around discussing sex and sexual health [37]. In addition, a study with Korean women found that higher interdependent self-construal (defined as “an orientation of self in which individuals define themselves primarily through their relationships with others”) was associated with higher HPV vaccine intention [56].
3.5.6. Preventive activity
Having to get multiple doses of the vaccine was cited as a barrier to vaccine uptake for Korean female college students [36]. Additionally, a study with Chinese students discussed how participants disagreed with the recommended age of 9 to 26 for vaccination because they thought Chinese youths did not engage in sexual activity as early as their American counterparts [57].
4. Discussion
Our study represents the first effort to systematically examine multilevel determinants of HPV vaccine intention and uptake among Asian-Americans. Using the P3 model as the guiding framework, we documented findings across 26 studies. Only 3 studies included practice-level measurements, nearly half (12 studies) included provider-level measurements, and all studies included patient-level measurements. The prevalence of vaccine intention and uptake varied across studies.
One major finding is that only 3 studies assessed practice-level influences [35–37]. Furthermore, 2 of these 3 studies [35,36] only captured patients’ perspectives instead of clinic staff’s or providers’, limiting the ability to fully examine a range of aspects at healthcare practices that potentially impact vaccine intention or uptake. Systematic reviews have shown that healthcare system-based interventions can improve HPV vaccine coverage [59,60]. The Community Preventive Services Task Force also recommends the use of system-based interventions as well as the implementation of system-based interventions in combination to increase vaccination rates [62]. To inform these system-level interventions, future research on Asian populations should include additional measurements of practice-level determinants. Research can explore elements such as electronic health record-generated prompts, assessment and feedback strategies, or reminder and recall, which are associated with vaccine uptake in general U.S. populations [59,60]. The P3 model also provides useful blueprints for additional possible practice-level constructs to be measured, including supply, immunization champion, vaccine promotion culture, and communication regarding vaccination policies [27].
All 12 studies that examined provider-level influences focused on aspects of communication between patients/caregivers and providers [35–44,48,52]. Such communication was measured most commonly through a provider’s recommendation [36,38–44] but also included discussion/conversation with providers [37,39,40], hearing about the vaccine from providers [42], or asking providers about the vaccine [44]. The associations between a provider’s recommendation and HPV vaccine intention or uptake have also been demonstrated in studies with general U.S. populations [21,62,63]. Lacking from the studies in our review, however, is a deeper inquiry of the content and manner of vaccine recommendation.
In general U.S. populations, parents receiving a strong recommendation (i.e. recommendation that strongly endorses HPV vaccine, focuses on cancer prevention, and urges same-day vaccination) were more likely to get their children HPV vaccine [64]. It will be useful to explore whether such patterns hold true across Asian populations. This knowledge can also guide provider-level interventions, particularly with training providers on communication about HPV vaccine. Future research should also incorporate perspectives of providers serving Asian communities to further understand current practices around HPV vaccine recommendation (e.g., whether providers are adhering to “same day same way” recommendation) [65] as well as possible barriers and facilitators for providers.
Past research has demonstrated differences between Asians and Whites as well as differences across Asian groups regarding cancer health communication with providers. For example, in a survey, Asians were 0.67 times less likely to discuss breast cancer risks with providers compared to Whites [66]. In another study, Asians significantly differed from Whites regarding choice of healthcare providers as a cancer information source where they would look first in a time of need (33.2% for Asians versus 47.0% for Whites) [67]. In addition, differences across Asian subgroups also exist regarding having difficulties talking to a provider in the context of cancer screening [68].
At the patient level, influential determinants appearing in several studies (i.e., 5 or more studies) included HPV or HPV vaccine knowledge [17,35,36,40,47,51–54], perceived safety or side effect issues [36,38–41,43,45], perceived susceptibility [35,36,43,52,57], and beliefs regarding the relationship between HPV vaccine and sexual activity [37–41,43,52,57]. A systematic review on African-American and Latino parents’ HPV vaccine acceptance and uptake for their children documented similar influential factors with the exception of HPV or HPV vaccine knowledge [22]. Researchers designing programs to increase HPV vaccine uptake for minority communities should attend to these similarities and differences. Differences also exist in target audience for these determinants: in our review, HPV or HPV vaccine knowledge and beliefs regarding the relationship between HPV vaccine and sexual activity arose in studies with both Asian caregivers who discussed getting the vaccine for their children and Asian adults who discussed getting the vaccine for themselves. Meanwhile, perceived safety or side effects mainly came up in studies with caregivers (6 out of 7) [38–41,43,45], and perceived susceptibility mainly came up in studies with adult participants (4 out of 5) [35,36,52,57].
Altogether, these patient-level findings that emerged in our review are important targets for educational interventions on HPV vaccine, though research notes that educational interventions are more effective when implemented in conjunction with health system-based interventions [60,61]. For example, multilingual fact sheets incorporating culturally-relevant storytelling may help address issues related to knowledge and perceived susceptibility [25,69]. Moreover, caregivers can be provided with vaccine safety data from clinical trials, in addition to research showing no evidence of vaccinated individuals developing commonly-feared conditions (e.g., autoimmune and neurological conditions) [70]. It may also be useful to discuss risks associated with not receiving HPV vaccine [71]. Additionally, patients should be introduced to a strong body of evidence showing that no association exists between HPV vaccination and increased sexual activity [72,73]. Interventions should emphasize how given its preventive nature, HPV vaccine needs to be administered prior to exposure to HPV (e.g., sexual activity), and that getting the vaccine when one is not sexually active is actually the best strategy. More research should be done on how researchers or providers can present these data in a culturally appropriate manner that Asian caregivers and patients can easily understand.
Five studies in our review discussed familial influences on HPV vaccine intention and uptake [36,37,52,56,58], though measurements varied (e.g., influence from mothers, vaccine recommendation by parents, influence from family, influence from family and friends, or family stigma around sexual health). Previous research on familial influences among Asian-Americans has mainly focused on how familial influences act as barriers to healthy behaviors or health services utilization. For example, research has pointed to family stigma and lack of parent–child communication as barriers to sexual and mental health utilization [74–76] or patriarchal family structure as a reason why women underutilized cancer screening [77]. In our review, however, we found that familial influences can be both negatively and positively associated with HPV vaccination outcomes. Reviewed studies brought up family stigma around sexual health [37] as a barrier to vaccine uptake but also pointed to influences from mothers [36] and vaccine recommendation from parents [52] as facilitators of vaccine intention and uptake. Future research can explore methods to leverage familial influences to positively impact vaccine behaviors among Asian caregivers and patients.
Certain patient-level findings also emphasize a need for health systems to be more attentive to Asian patients’ backgrounds, beliefs, and practices. For example, the literature reviewed indicated language difficulties [36,50,51], unfamiliarity with or lack of comfort in using health services in the U.S. [35], and mistrust of medical systems or Western medicine [41,55]. Increasing availability of clinic language services (through on-site interpreters or Language Line) along with the use of patient navigators or community health workers may remedy these problems [78–81].
The designs of all reviewed studies were either cross-sectional surveys or qualitative designs, which can pose challenges in interpreting temporal relationships between variables. Most existing literature centered on Korean, Chinese, and Cambodian populations, leaving a gap of knowledge for other Asian subgroups. Due to the limited number of studies and different types of statistics (e.g., descriptive statistics versus associations/effect sizes) reported in them, we could neither perform a meta-analysis nor provide comparisons of determinants across subgroups of Asians. Note, however, that in studies included, the prevalence of intention and uptake varied greatly across communities (intention: 23.4% to 72%, initiation: 14% to 67%, and completion: 9% to 63%). Therefore, interventions should take into account the heterogeneity of Asian communities, particularly regarding socioeconomic status, religious/cultural beliefs, social norms, and patterns of health services utilization [1,2].
5. Conclusions
As the Asian populations in the U.S. increase, evidence suggests low utilization of HPV vaccine in these populations. Existing research on determinants of HPV vaccine intention and uptake in this population currently lacks measurements of practice-level constructs and perspectives of clinic staff and providers, all of which is needed to guide system-level interventions and provider training. Data regarding patient-level determinants indicate that interventions for Asian-American populations can focus on providing educational information in culturally-appropriate manners, leveraging familial influences, and attending to access-related or cultural beliefs about HPV vaccine. Interventions should take into account varied vaccine intention and uptake prevalence in different Asian subgroups.
Supplementary Material
Acknowledgments
Funding
M.V. is supported by the National Cancer Institute (F31 CA243220–01, PI: Vu). C.J.B. is supported by the US National Cancer Institute (R01CA215155–01A1, PI: Berg; R01CA179422–01, PI: Berg; R01CA239178–01A1, MPIs: Berg, Levine), the US Fogarty International Center/National Institutes of Health (1R01TW010664–01, MPIs: Berg, Kegler), and the US National Institute on Environmental Health Science/Fogarty International Center (D43ES030927–01, MPIs: Berg, Marsit, Sturua). C.E. is supported by the CDC Cancer Prevention and Control Research Network (CPCRN, U48 DP006377). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Footnotes
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethics approval
This manuscript is a systematic review of published literature; therefore, no human subjects approval is required.
Appendix A. Supplementary material
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2020.07.059.
References
- [1].Thompson CA, Gomez SL, Hastings KG, Kapphahn K, Yu P, Shariff-Marco S, et al. The burden of cancer in Asian Americans: a report of national mortality trends by Asian ethnicity. Cancer Epidemiol Biomark Prev 2016;25(10):1371–82. 10.1158/1055-9965.EPI-16-0167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Hamilton AS, Wu AH, Stram DO. Resources and methods for studying cancer among Asian Americans In: Wu AH, Stram DO, editors. Cancer epidemiology among Asian Americans. Springer International Publishing; 2016. p. 1–18. 10.1007/978-3-319-41118-7. [DOI] [Google Scholar]
- [3].Pew Research Center. Key facts about Asian Americans, a diverse and growing population. Retrieved March 22, 2020, from https://www.pewresearch.org/fact-tank/2017/09/08/key-facts-about-asian-americans/; 2017
- [4].Pew Research Center. Key facts about Asian origin groups in the U.S. Retrieved from https://www.pewresearch.org/fact-tank/2019/05/22/key-facts-about-asian-origin-groups-in-the-u-s/; 2019
- [5].United States Census Bureau. Asian-American and Pacific Islander Heritage Month: May 2019. Retrieved March 22, 2020, from https://www.census.gov/newsroom/facts-for-features/2019/asian-american-pacific-islander.html; 2019
- [6].Yi SS. Taking action to improve Asian American health. Am J Public Health 2020;110(4):435–7. 10.2105/AJPH.2020.305596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ghosh C A national health agenda for Asian Americans and Pacific islanders. JAMA 2010;304(12):1381 10.1001/jama.2010.1358. [DOI] [PubMed] [Google Scholar]
- [8].Ðoàn LN, Takata Y, Sakuma K-LK, Irvin VL. Trends in clinical research including Asian American, Native Hawaiian, and Pacific islander participants funded by the US national institutes of health, 1992 to 2018 e197432. JAMA Network Open 2019;2(7). 10.1001/jamanetworkopen.2019.7432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Yi SS, Kwon SC, Sacks R, Trinh-Shevrin C. Commentary: Persistence and health-related consequences of the model minority stereotype for Asian Americans. Ethn Dis 2016. [DOI] [PMC free article] [PubMed]
- [10].Patel EU, Grabowski MK, Eisenberg AL, Packman ZR, Gravitt PE, Tobian AAR. Increases in human papillomavirus vaccination among adolescent and young adult males in the United States, 2011–2016. J Infect Dis 2018;218(1):109–13. 10.1093/infdis/jiy165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Agénor M, Pérez AE, Peitzmeier SM, Borrero S. Racial/ethnic disparities in human papillomavirus vaccination initiation and completion among U.S. women in the post-affordable care act era. Ethnicity & Health 2018:1–15. 10.1080/13557858.2018.1427703. [DOI] [PubMed] [Google Scholar]
- [12].Cofie LE, Hirth JM, Guo F, Berenson AB, Markides K, Wong R. HPV vaccination among foreign-born women: examining the national health interview survey 2013–2015. Am J Prev Med 2018;54(1):20–7. 10.1016/j.amepre.2017.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Walker TY, Elam-Evans LD, Yankey D, Markowitz LE, Williams CL, Fredua B, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years — United States, 2018. MMWR Morb Mortal Wkly Rep 2019;68(33):718–23. 10.15585/mmwr.mm6833a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Licht AS, Murphy JM, Hyland AJ, Fix BV, Hawk LW, Mahoney MC. Is use of the human papillomavirus vaccine among female college students related to human papillomavirus knowledge and risk perception? Sexually Transmitted Infections 2010;86(1):74–8. 10.1136/sti.2009.037705. [DOI] [PubMed] [Google Scholar]
- [15].Cohen T, Legg JS, Hutchinson J, Levy J, Bosher W. Factors influencing HPV vaccine use among racially diverse female college students. J Health Disparities Res Practice 2015;8(2):75–88. [Google Scholar]
- [16].LaJoie AS, Kerr JC, Clover RD, Harper DM. Influencers and preference predictors of HPV vaccine uptake among US male and female young adult college students. Papillomavirus Res 2018;5:114–21. 10.1016/j.pvr.2018.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Lee HY, Kwon M, Vang S, Dewolfe J, Kim NK, Lee DK, et al. Disparities in human papillomavirus vaccine literacy and vaccine completion among Asian American pacific islander undergraduates: implications for cancer health equity. J Am Coll Health 2015;63(5):316–23. 10.1080/07448481.2015.1031237. [DOI] [PubMed] [Google Scholar]
- [18].Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: A theory-informed, systematic review. Prev Med 2007;45(2–3):107–14. 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- [19].Kessels SJM, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, Tooher RL. Factors associated with HPV vaccine uptake in teenage girls: A systematic review. Vaccine 2012;30(24):3546–56. 10.1016/j.vaccine.2012.03.063. [DOI] [PubMed] [Google Scholar]
- [20].Radisic G, Chapman J, Flight I, Wilson C. Factors associated with parents’ attitudes to the HPV vaccination of their adolescent sons: A systematic review. Prev Med 2017. 10.1016/j.ypmed.2016.11.019. [DOI] [PubMed]
- [21].Newman PA, Logie CH, Doukas N, Asakura K. HPV vaccine acceptability among men: A systematic review and meta-Analysis. Sexually Transmitted Infections 2013. 10.1136/sextrans-2012-050980. [DOI] [PMC free article] [PubMed]
- [22].Galbraith KV, Lechuga J, Jenerette CM, Moore LTCAD, Palmer MH, Hamilton JB. Parental acceptance and uptake of the HPV vaccine among African-Americans and Latinos in the United States: A literature review. Soc Sci Med 2016. 10.1016/j.socscimed.2016.04.028. [DOI] [PubMed]
- [23].Kim K, LeClaire A-R. A systematic review of factors influencing human papillomavirus vaccination among immigrant parents in the United States. Health Care Women Int 2017;00–00. 10.1080/07399332.2017.1404064. [DOI] [PubMed]
- [24].Lee HY, Koopmeiners JS, McHugh J, Raveis VH, Ahluwalia JS. MHealth pilot study: Text messaging intervention to promote HPV vaccination. Am J Health Behav 2016;40(1):67–76. 10.5993/AJHB.40.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Kim M, Lee H, Kiang P, Allison J. Development and acceptability of a peer-paired, cross-cultural and cross-generational storytelling HPV intervention for Korean American college women. Health Educ Res 2019;34(5):483–94. 10.1093/her/cyz022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Chen AC-C, Kim W (Sunny), Larkey L. Developing and pilot testing a digital storytelling intervention to promote HPV vaccination among Vietnamese American adolescents. GSTF J Nursing and Health Care (JNHC), 4(1); 2019. [Google Scholar]
- [27].Bednarczyk RA, Chamberlain A, Mathewson K, Salmon DA, Omer SB. Practice-, provider-, and patient-level interventions to improve preventive care: Development of the P3 Model. Preventive Med Rep 2018;11:131–8. 10.1016/j.pmedr.2018.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Walsh JME, Mcphee SJ. A systems model of clinical preventive care: an analysis of factors influencing patient and physician. Health Educ Behav 1992. 10.1177/109019819201900202. [DOI] [PubMed]
- [29].Green LW, Kreuter MW. Health promotion planning: An educational and ecological approach. New York: McGraw-Hill; 2005. [Google Scholar]
- [30].Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: Extending horizons, envisioning the future. Soc Sci Med 2006;62(7):1650–71. 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- [31].Smedley B, Syme S, editors. & Institute of Medicine. Promoting health. National Academies Press. Washington, D.C.: National Academies Press; 2000. 10.17226/9939 [DOI] [Google Scholar]
- [32].McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q 1988. 10.1177/109019818801500401. [DOI] [PubMed]
- [33].Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement e1000097. PLoS Med 2009;6(7). 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Sirriyeh R, Lawton R, Gardner P, Armitage G. Reviewing studies with diverse designs: the development and evaluation of a new tool. J Eval Clin Practice 2012;18(4):746–52. 10.1111/j.1365-2753.2011.01662.x. [DOI] [PubMed] [Google Scholar]
- [35].Lee HY, Lee MH. Barriers to cervical cancer screening and prevention in young Korean immigrant women: implications for intervention development. J Transcult Nurs 2017;28(4):353–62. 10.1177/1043659616649670. [DOI] [PubMed] [Google Scholar]
- [36].Kim M, Lee H, Kiang P, Kim D. Human papillomavirus: a qualitative study of Korean American female college students’ attitudes toward vaccination. Clin J Oncol Nursing 2017;21(5):E239–47. 10.1188/17.CJON.E239-E247. [DOI] [PubMed] [Google Scholar]
- [37].Hopfer S, Garcia S, Duong HT, Russo JA, Tanjasiri SP. A narrative engagement framework to understand HPV vaccination among latina and Vietnamese women in a planned parenthood setting. Health Educ Behav 2017;44 (5):738–47. 10.1177/1090198117728761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Kim K, Kim B, Choi E, Song Y, Han H-R. Knowledge, perceptions, and decision making about human papillomavirus vaccination among Korean American women: a focus group study. Women’s Health Issues: Official Publ Jacobs Inst Women’s Health 2015;25(2):112–9. 10.1016/j.whi.2014.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Lee Y-M, Mondragón E, Jeong YM, Lee HH, Aquino E, Shim K. Exploring the need of HPV education programs in Korean American communities. J Community Health Nurs 2019;36(1):19–30. 10.1080/07370016.2018.1555312. [DOI] [PubMed] [Google Scholar]
- [40].Khan SS. Parental acceptance of the Human Papillomavirus vaccination among South Asian immigrants living in the Midwest USA. Purdue University; 2014. [Google Scholar]
- [41].Do H, Seng P, Talbot J, Acorda E, Coronado GD, Taylor VM. HPV vaccine knowledge and beliefs among Cambodian American parents and community leaders. Asian Pacific J Cancer Prevention : APJCP 2009;10(3):339–44. [PMC free article] [PubMed] [Google Scholar]
- [42].Taylor VM, Burke NJ, Ko LK, Sos C, Liu Q, Do HH, et al. Understanding HPV vaccine uptake among Cambodian American girls. J Community Health 2014;39(5):857–62. 10.1007/s10900-014-9844-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Dela Cruz MRI, Braun KL, Tsark JAU, Albright CL, Chen JJ. HPV vaccination prevalence, parental barriers and motivators to vaccinating children in Hawai’i. Ethnicity and Health; 2018. p. 1–13. 10.1080/13557858.2018.1473556 [DOI] [PMC free article] [PubMed]
- [44].Taylor VM, Burke N, Do H, Liu Q, Yasui Y, Bastani R. HPV vaccination uptake among cambodian mothers. J Cancer Educ 2012;27(1):145–8. 10.1007/s13187-011-0269-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Bastani R, Glenn BA, Tsui J, Chang LC, Marchand EJ, Taylor VM, et al. Understanding sub-optimal HPV vaccine uptake among ethnic minority girls. Cancer Epidemiology, Biomarkers & Prevention : A Publ Am Assoc Cancer Res, Cosponsored by the Am Soc Preventive Oncol 2011. 10.1158/1055-9965.EPI-11-0267. [DOI] [PMC free article] [PubMed]
- [46].Lee Y-M, Riesche L, Lee H, Shim K. Parental HPV knowledge and perceptions of HPV vaccines among Korean American parents. Appl Nurs Res 2018;44:54–9. 10.1016/j.apnr.2018.09.008. [DOI] [PubMed] [Google Scholar]
- [47].Tung W-C, Lu M, Qiu X, Ervin S. Human papillomavirus knowledge, attitudes, and vaccination among Chinese college students in the United States. Vaccine 2019;37(24):3199–204. 10.1016/j.vaccine.2019.04.084. [DOI] [PubMed] [Google Scholar]
- [48].Gao H Exploring knowledge and beliefs of Human Papillomavirus (HPV) infection and HPV vaccination among U.S. Chinese international students. Purdue University; 2015. [Google Scholar]
- [49].Truong-Vu K-P. Gender and racial/ethnic differences in the timing of initiating the HPV vaccine. University of Colorado Boulder; 2018. [Google Scholar]
- [50].Nguyen GT, Chen B, Chan M. Pap testing, awareness, and acceptability of a human papillomavirus (HPV) vaccine among Chinese American women. J Immigr Minor Health 2012;14(5):803–8. 10.1007/s10903-012-9607-5. [DOI] [PubMed] [Google Scholar]
- [51].Yi JK, Anderson KO, Le YC, Escobar-Chaves SL, Reyes-Gibby CC. English proficiency, knowledge, and receipt of HPV vaccine in Vietnamese-American Women. J Community Health 2013;38(5):805–11. 10.1007/s10900-013-9680-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Kim M, Lee H, Kiang P, Aronowitz T, Sheldon LK, Shi L, et al. HPV vaccination and Korean American college women: cultural factors, knowledge, and attitudes in cervical cancer prevention. J Community Health 2019;44 (4):646–55. 10.1007/s10900-019-00634-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Otanez S, Torr BM. Ethnic and racial disparities in HPV vaccination attitudes. J Immigr Minor Health 2018;20(6):1476–82. 10.1007/s10903-017-0685-2. [DOI] [PubMed] [Google Scholar]
- [54].Lee H, Kim M, Kiang P, Shi L, Tan K, Chea P, et al. Factors associated with HPV vaccination among cambodian American teenagers. Public Health Nurs 2016;33(6):493–501. 10.1111/phn.12294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Kolar SK, Wheldon C, Hernandez ND, Young L, Romero-Daza N, Daley EM. Human papillomavirus vaccine knowledge and attitudes, preventative health behaviors, and medical mistrust among a racially and ethnically diverse sample of college women. J Racial Ethnic Health Disparities 2015;2(1):77–85. 10.1007/s40615-014-0050-2. [DOI] [PubMed] [Google Scholar]
- [56].Zhao N, Huh J, Murphy ST, Chatterjee JS, Baezconde-Garbanati L. Self-construal as a predictor of Korean American women’s intention to vaccinate daughters against human papillomavirus. Asian Am J Psychol 2014;5(2):96–105. 10.1037/a0036097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Gao H, Okoror TA, Hyner GC. Focus group study of Chinese international students’ knowledge and beliefs about HPV vaccination, before and after reading an informational pamphlet about Gardasil®. J Immigr Minor Health 2016;18(5):1085–92. 10.1007/s10903-016-0349-7. [DOI] [PubMed] [Google Scholar]
- [58].Lee H, Kim D, Kiang PN, Cooley ME, Shi L, Thiem L, et al. Awareness, knowledge, social norms, and vaccination intentions among Khmer mother– daughter pairs. Ethnicity & Health 2018;1–13. 10.1080/13557858.2018.1514455. [DOI] [PubMed]
- [59].Niccolai LM, Hansen CE. Practice- and community-based interventions to increase human papillomavirus vaccine coverage. JAMA Pediatrics 2015;169 (7):686 10.1001/jamapediatrics.2015.0310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Smulian EA, Mitchell KR, Stokley S. Interventions to increase HPV vaccination coverage: A systematic review. Hum Vaccines & Immunotherapeutics 2016;12 (6):1566–88. 10.1080/21645515.2015.1125055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Community preventive services task force. Increasing appropriate vaccination: evidence-based interventions for your community. The Community Guide - What Works. Retrieved March 23, 2020, from https://www.thecommunityguide.org/sites/default/files/assets/What-Works-Factsheet-Vaccination.pdf; 2017
- [62].Gilkey MB, McRee AL. Provider communication about HPV vaccination: A systematic review. Hum Vaccines Immunotherapeutics 2016. 10.1080/21645515.2015.1129090. [DOI] [PMC free article] [PubMed]
- [63].Newman PA, Logie CH, Lacombe-Duncan A, Baiden P, Tepjan S, Rubincam C, et al. Parents’ uptake of human papillomavirus vaccines for their children: a systematic review and meta-analysis of observational studies e019206. BMJ Open 2018;8(4). 10.1136/bmjopen-2017-019206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Gilkey MB, Calo WA, Moss JL, Shah PD, Marciniak MW, Brewer NT. Provider communication and HPV vaccination: The impact of recommendation quality. Vaccine 2016;34(9):1187–92. 10.1016/j.vaccine.2016.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Centers for disease control and prevention. Answering parents’ questions about HPV vaccine. Retrieved April 23, 2020, from https://www.cdc.gov/hpv/hcp/answering-questions.html; 2019
- [66].Kaplan CP. Breast cancer risk reduction options: awareness, discussion, and use among women from four ethnic groups. Cancer Epidemiol Biomark Prev 2006;15(1):162–6. 10.1158/1055-9965.EPI-04-0758. [DOI] [PubMed] [Google Scholar]
- [67].Nguyen GT, Bellamy SL. Cancer information seeking preferences and experiences: disparities between Asian Americans and whites in the health information national trends survey (HINTS). J Health Commun 2006;11 (sup001):173–80. 10.1080/10810730600639620. [DOI] [PubMed] [Google Scholar]
- [68].Shive SE, Ma GX, Tan Y, Toubbeh JI, Parameswaran L, Halowich J. Asian American subgroup differences in sources of health information and predictors of screening behavior. Californian J Health Promotion 2007;5(2):112–27. 10.32398/cjhp.v5i2.1237. [DOI] [Google Scholar]
- [69].Chan A, Brown B, Sepulveda E, Teran-Clayton L. Evaluation of fotonovela to increase human papillomavirus vaccine knowledge, attitudes, and intentions in a low-income Hispanic community. BMC Res Notes 2015;8(1):615 10.1186/s13104-015-1609-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Bednarczyk RA. Addressing HPV vaccine myths: practical information for healthcare providers. Hum Vaccines & Immunotherapeutics 2019;1–11. 10.1080/21645515.2019.1565267. [DOI] [PMC free article] [PubMed]
- [71].Zimet GD, Rosberger Z, Fisher WA, Perez S, Stupiansky NW. Beliefs, behaviors and HPV vaccine: Correcting the myths and the misinformation. Prev Med 2013;57(5):414–8. 10.1016/j.ypmed.2013.05.013. [DOI] [PubMed] [Google Scholar]
- [72].Petrosky EY, Liu G, Hariri S, Markowitz LE. Human papillomavirus vaccination and age at first sexual activity, national health and nutrition examination survey. Clin Pediatr 2017;56(4):363–70. 10.1177/0009922816660541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Bednarczyk RA, Davis R, Ault K, Orenstein W, Omer SB. Sexual activity-related outcomes after human papillomavirus vaccination of 11- to 12-year-olds. Pediatrics 2012;130(5):798–805. 10.1542/peds.2012-1516. [DOI] [PubMed] [Google Scholar]
- [74].Han M, Pong H. Mental health help-seeking behaviors among Asian American community college students: the effect of stigma, cultural barriers, and acculturation. J College Student Dev 2015;56(1):1–14. 10.1353/csd.2015.0001. [DOI] [Google Scholar]
- [75].Han C, Operario D, Choi K-H. If I was infected with HIV, I would be letting my family down: Family influences on risk and protective factors for unsafe sex among gay Asian Pacific Islander men. Health, Risk & Society 2011;13 (4):373–88. 10.1080/13698575.2011.575932. [DOI] [Google Scholar]
- [76].Okazaki S Influences of culture on Asian Americans’ sexuality. J Sex Res 2002;39(1):34–41. 10.1080/00224490209552117. [DOI] [PubMed] [Google Scholar]
- [77].Lee HY, Vang S. Barriers to cancer screening in Hmong Americans: the influence of health care accessibility, culture, and cancer literacy. J Community Health 2010;35(3):302–14. 10.1007/s10900-010-9228-7. [DOI] [PubMed] [Google Scholar]
- [78].Ali-Faisal SF, Colella TJF, Medina-Jaudes N, Benz Scott L. The effectiveness of patient navigation to improve healthcare utilization outcomes: A meta-analysis of randomized controlled trials. Patient Educ Couns 2017;100 (3):436–48. 10.1016/j.pec.2016.10.014. [DOI] [PubMed] [Google Scholar]
- [79].Genoff MC, Zaballa A, Gany F, Gonzalez J, Ramirez J, Jewell ST, et al. Navigating language barriers: a systematic review of patient navigators’ impact on cancer screening for limited english proficient patients. J Gen Intern Med 2016;31 (4):426–34. 10.1007/s11606-015-3572-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Jacobs EA, Lauderdale DS, Meltzer D, Shorey JM, Levinson W, Thisted RA. Impact of interpreter services on delivery of health care to limited-English-proficient patients. J Gen Intern Med 2001;16(7):468–74. 10.1046/j.1525-1497.2001.016007468.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Ku L, Flores G. Pay now or pay later: providing interpreter services in health care. Health Aff 2005;24(2):435–44. 10.1377/hlthaff.24.2.435. [DOI] [PubMed] [Google Scholar]
- [82].Shweta. Cervical cancer screening behavior of Hmong women: A social network analysis. Retrieved from: University of Minnesota; 2012. https://conservancy.umn.edu/handle/11299/143754. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


