Abstract
Introduction:
So-called “deaths of despair”—those involving drug overdoses, alcohol-related liver disease, and suicide—have been rising in the U.S. among middle-aged non-Hispanic white adults without a college degree. Premature deaths (ages 25–69) from alcoholic liver disease were examined specifically in this study from 1999 to 2018, by sex, race/Hispanic origin, and age group.
Methods:
Data were drawn from the 1999–2018 Multiple Cause of Death database and bridged-race estimates of the U.S. resident population, including 281,243 alcoholic liver disease deaths or an average of eight deaths per 100,000 population. Analyses examined alcoholic liver disease death rates for sex differences among three age groups (25–49, 50–59, and 60–69 years), by race/Hispanic origin, from 1999 to 2018, as well as age-adjusted and age-specific annual percentage changes (accounted for cohorts), years of potential life lost, and age of death for sociodemographic backgrounds, alcoholic liver disease clinical courses, and comortalities.
Results:
Non-Hispanic whites increasingly experienced greater alcoholic liver disease mortality than non-Hispanic blacks and Hispanics, confirming the racial/ethnic crossover observed in previous studies. Although men consistently had higher rates of mortality, male-to-female ratios decreased in the past 2 decades and were the lowest among ages 25–49 years and especially among ages 25–34 years. Although women generally had longer life expectancies, women died of alcoholic liver disease on average about 2–3 years earlier than men.
Conclusions:
Prevention and intervention efforts are imperative to address the narrowing sex gap and widening racial disparities in alcoholic liver disease premature deaths.
INTRODUCTION
Premature mortality, or unfulfilled life expectancy, has increased in recent years.1–4 Life expectancy in the U.S. has not kept pace with other industrialized nations5,6 and has declined since 2015.6–8 Kochanek et al.9 reported that increasing death rates from drug overdoses, suicides, and alcoholic (alcohol-associated) liver disease (ALD) were responsible for the increased all-cause death rate among non-Hispanic whites. Case and Deaton2 referred to these three causes as “deaths of despair,” which stemmed from cumulative disadvantages to some people (e.g., middle-aged non-Hispanic whites with a high school or less education) as a result of economic stagnation and social disintegration since the 1970s. Rehm and Probst10,11 suggested that alcohol use was a direct or indirect cause of these deaths. Increasing social inequality may have exacerbated alcohol use problems, thereby increasing premature mortality.10–14
With defining characteristics including alcoholic fatty liver (i.e., steatosis), alcoholic hepatitis, and fibrosis/liver cirrhosis, ALD is a significant burden on health in the U.S. and substantially contributes to premature mortality.15,16 ALD is associated with greater premature mortality than all causes.17 In 2018, the percentage of premature deaths from all causes was 33%, which paled in comparison to the 87% for ALD. Premature deaths from overall chronic liver disease and cirrhosis are projected to increase until 2030 for all racial and ethnic groups except non-Hispanic black men.18 ALD risk is determined by the interaction of alcohol consumption with both host factors (e.g., sex, race, genetic variants, SES) and comorbidities (e.g., metabolic syndrome, hepatitis C virus [HCV], malnutrition, hemochromatosis).19 Concurrent unhealthy behaviors or conditions (e.g., smoking, drug use, poor dietary habits, obesity) often exacerbate the extent and severity of ALD, thereby contributing to mortality.16,20
Expanding upon the “deaths of despair” literature,21–25 this study examines ALD premature mortality trends from 1999 to 2018. In light of the narrowing sex gap in alcohol-related emergency department visits,26 hospitalizations,27 and mortality6,28–30 in recent years, this study focuses on sex differences in ALD, by race/Hispanic origin, with respect to age-specific death rates, annual percentage changes (APCs), years of potential life lost (YPLL), and age of death. Age-specific death rates are compared across three age groups (25–49, 50–59, and 60–69 years).
METHODS
Analyses were based on 1999–2018 Multiple Cause of Death data (www.cdc.gov/nchs/data_access/Vitalstatsonline.htm) and bridged-race estimates of the U.S. resident population (www.cdc.gov/nchs/nvss/bridged_race.htm) from the National Center for Health Statistics (NCHS). Multiple Cause of Death data compiled by the NCHS’s National Vital Statistics System from death certificates for U.S. residents provided information on ALD deaths. Mid-year population data produced by the U.S. Census Bureau for NCHS provided denominators in rate calculations. Each death certificate contains a single underlying cause of death, up to 20 additional contributing causes, and sociodemographic data. During 1999–2018, causes of death were coded in accordance with ICD-10.31 However, the coding rule change discontinuing the use of ICD-10: F10.0 (mental and behavioral disorders due to use of alcohol, acute intoxication) contributed to an unusually large increase in ALD deaths from 2006 to 2007.32
According to the underlying cause of death, “the disease or injury which initiated the train of morbid events leading directly or indirectly to death or circumstances of the accident or violence which produced the fatal injury,”33 a total of 281,243 decedents died prematurely of ALD at ages 25–69 years, ranging from 10,210 in 1999 to 20,180 in 2018. Premature mortality was defined as death before age 70 years, following the age threshold used by the UN Sustainable Development Goals for health.34 The lower age threshold was set at 25 years because decedents rarely died of ALD at younger ages.
Measures
This study identified decedents with ALD reported as the underlying cause of death; co-occurring conditions reported as contributing causes of death; and sociodemographic characteristics, which acted as covariates (e.g., education, marital status) or stratifiers (e.g., sex, race/Hispanic origin, age group) depending on the analysis. ALD included ICD-10 codes for alcoholic fatty liver (K70.0); alcoholic hepatitis (K70.1); alcoholic fibrosis and sclerosis of liver (K70.2); alcoholic cirrhosis of liver (K70.3); alcoholic hepatic failure (K70.4); and alcoholic liver disease, unspecified (K70.9). Selected co-occurring conditions included alcohol use disorder (AUD) (F10), tobacco use disorder (F17), HCV infection (B17.1 and B18.2), diabetes (E10–E14), hypertension (I10–I13), and unnatural death (V01–Y89).
Statistical Analysis
Data were initially analyzed for 1999–2017 in 2019 and reanalyzed for 1999–2018 in March 2020. Descriptive analyses graphically examined trends in sex-specific ALD death rates and male-to-female rate ratios from 1999 to 2018, by race/Hispanic origin (i.e., [non-Hispanic] whites and blacks and Hispanics), comparing three age groups (25–49, 50–59, and 60–69 years); trendlines were fitted using generalized additive models implemented in R, version 3.5.3 mgcv.35 Age-period-cohort analyses, implemented in R code provided by the National Cancer Institute,36 examined age-adjusted and age-specific APCs (i.e., net and local drifts, respectively) accounting for cohorts. Stata, version 15.1 was used to calculate YPLL and mean age of ALD death (the latter is a complement to average YPLL per decedent such that the two measures sum to 70 years). For YPLL, the total number and the age-adjusted rate in each year using APCs derived from Poisson models quantified the magnitude of change from 1999 to 2006 and 2007 to 2018. Mean ages of death for each covariate adjusted for other covariates were based on predictive margins derived from truncated Poisson regression with robust variance and truncations at ages 24 and 70 years.37
RESULTS
From 1999 to 2018, age-specific ALD death rates were consistently lower for women than men and lower for ages 25–49 years than ages 50–59 and 60–69 years (Figure 1). However, male-to-female rate ratios decreased during the period, particularly among those aged 25–49 years. According to the age-period-cohort analysis (Figure 2), the ALD death rate increased more rapidly for women. The respective age-adjusted APCs (net drifts) for women versus men were 4.91 vs 2.70 for whites, 2.20 vs −0.24 for Hispanics, and −0.13 vs −2.61 for blacks. Despite wide 95% CIs, increases in ALD death rates (local drifts) were notable among people aged <35 years. Both the total number and rate of YPLL increased from 2007 to 2018 and increased more rapidly for women than men (Table 1). For example, the respective APCs in YPLL rate for women versus men were 5.6 vs 2.9 for whites, 3.7 vs −0.1 for blacks, and 3.3 vs 0.7 for Hispanics.
Figure 1.
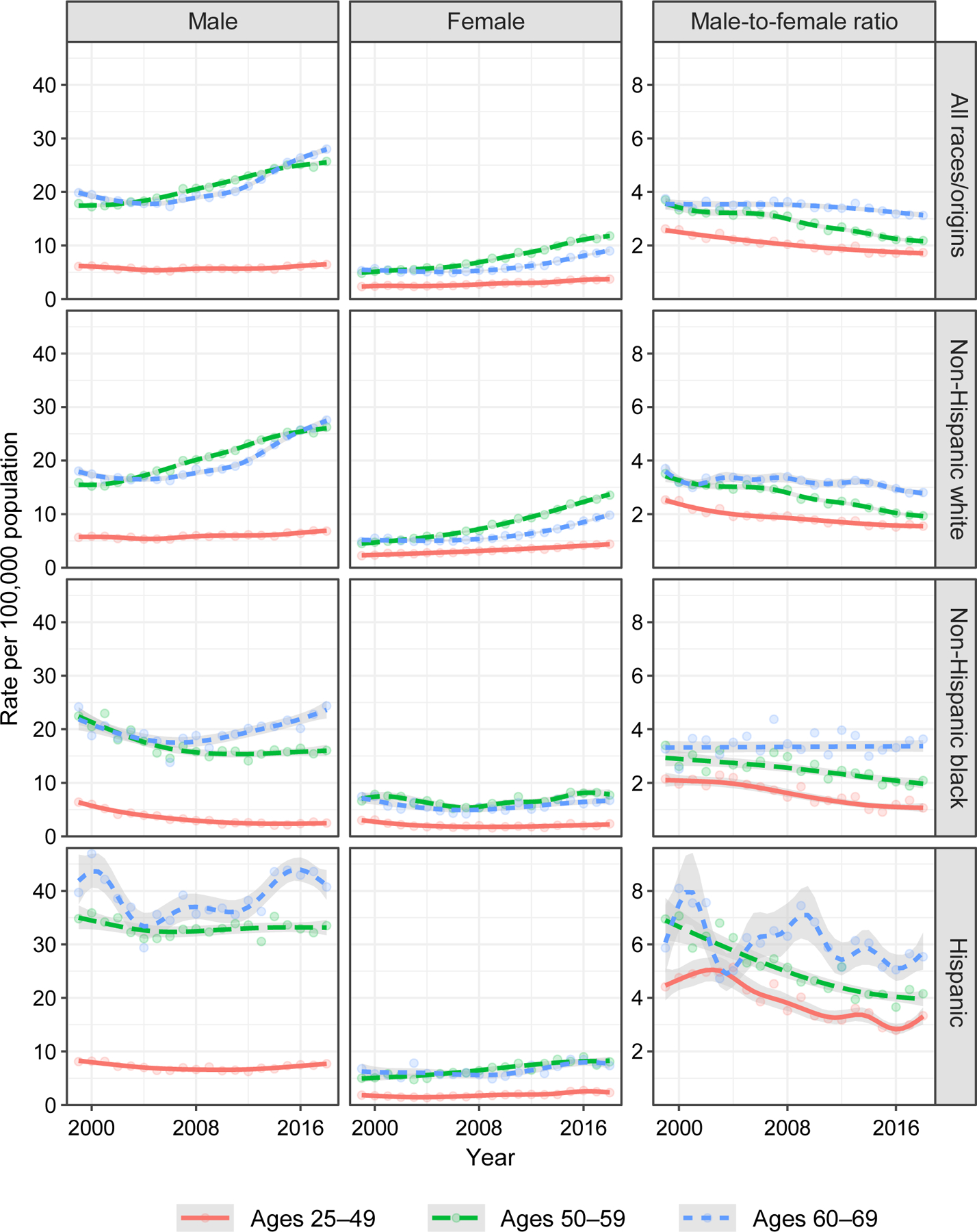
Sex-specific death rate (per 100,000 population) and male-to-female rate ratio for alcoholic liver disease, by age group and race/Hispanic origin, in the U.S., 1999–2018.
Note: Gray areas indicate 95% CIs.
Figure 2.
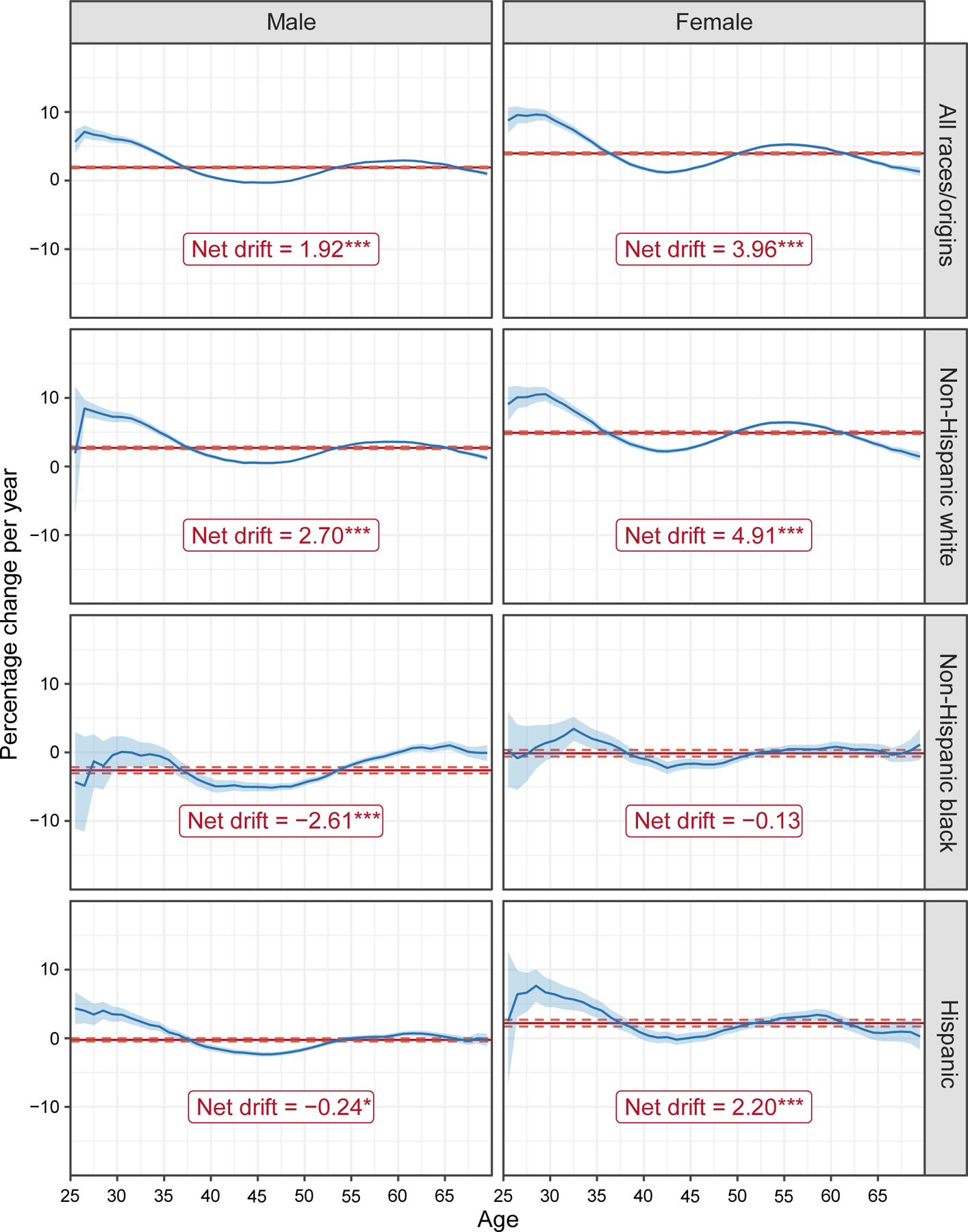
Age-adjusted (net drift) and age-specific annual percentage changes (APC) for alcoholic liver disease mortality, by sex and race/Hispanic origin, in the U.S., 1999–2018.
Note: Dashed lines and gray areas indicate 95% CIs for age-adjusted and age-specific APC, respectively (*p<0.05; ***p<0.001).
Table 1.
Years of Potential Life Lost (YPPL) to Alcoholic Liver Disease, 1999–2018
| Year | All races, both sexes | Non-Hispanic white | Non-Hispanic black | Hispanic | |||
|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | ||
| Total YPLL (Rate)a | YPLL (Rate)a | YPLL (Rate)a | YPLL (Rate)a | YPLL (Rate)a | YPLL (Rate)a | YPLL (Rate)a | |
| 1999 | 186,630 (123) | 92,415 (163) | 33,797 (59) | 16,250 (212) | 7,887 (86) | 22,208 (332) | 4,397 (63) |
| 2000 | 191,404 (123) | 93,765 (163) | 35,341 (61) | 15,540 (194) | 8,409 (89) | 24,265 (339) | 4,345 (59) |
| 2001 | 194,048 (122) | 93,433 (160) | 39,127 (67) | 15,063 (184) | 7,232 (75) | 24,837 (328) | 4,564 (60) |
| 2002 | 187,834 (116) | 91,312 (154) | 38,661 (66) | 12,309 (146) | 6,593 (67) | 24,000 (304) | 4,233 (53) |
| 2003 | 193,366 (118) | 95,642 (160) | 38,587 (65) | 13,602 (157) | 6,085 (61) | 24,625 (294) | 4,457 (52) |
| 2004 | 192,773 (115) | 94,148 (156) | 41,491 (69) | 12,282 (139) | 5,906 (57) | 24,415 (278) | 4,334 (49) |
| 2005 | 196,164 (115) | 96,278 (157) | 41,113 (68) | 11,741 (128) | 6,203 (59) | 24,511 (266) | 5,152 (55) |
| 2006 | 197,638 (114) | 96,578 (156) | 42,338 (70) | 10,481 (111) | 5,561 (52) | 25,717 (266) | 5,862 (59) |
| APC | 0.6** (−1.2**) | 0.6** (−0.7**) | 3.0** (2.1**) | −5.7** (−8.4**) | −5.5** (−7.4**) | 1.2* (−3.8**) | 3.6** (−1.4) |
| 2007 | 219,359 (125) | 107,289 (173) | 47,182 (78) | 11,939 (123) | 5,849 (53) | 28,708 (284) | 5,736 (56) |
| 2008 | 224,086 (127) | 110,161 (178) | 47,374 (79) | 11,387 (115) | 6,244 (56) | 28,879 (272) | 6,876 (64) |
| 2009 | 230,054 (129) | 110,121 (177) | 51,424 (85) | 11,117 (110) | 5,904 (51) | 30,902 (276) | 6,989 (62) |
| 2010 | 238,725 (133) | 114,026 (183) | 53,720 (89) | 10,940 (105) | 6,515 (56) | 30,566 (265) | 7,694 (66) |
| 2011 | 247,184 (136) | 114,614 (183) | 57,290 (95) | 11,720 (110) | 7,373 (62) | 31,813 (267) | 8,480 (70) |
| 2012 | 253,814 (139) | 121,365 (196) | 57,986 (97) | 11,162 (104) | 6,436 (54) | 32,461 (262) | 8,242 (66) |
| 2013 | 262,459 (143) | 123,682 (200) | 59,109 (100) | 11,947 (109) | 6,875 (58) | 33,878 (263) | 8,803 (68) |
| 2014 | 273,779 (149) | 124,003 (201) | 64,786 (111) | 11,547 (104) | 7,889 (66) | 37,580 (283) | 9,443 (71) |
| 2015 | 296,736 (162) | 133,336 (221) | 70,029 (120) | 11,894 (106) | 9,242 (76) | 39,692 (288) | 11,559 (84) |
| 2016 | 303,942 (165) | 133,389 (221) | 73,949 (129) | 12,592 (111) | 8,514 (70) | 41,582 (291) | 12,737 (90) |
| 2017 | 307,210 (167) | 135,261 (229) | 74,821(131) | 13,256 (117) | 8,604 (70) | 41,922 (286) | 11,633 (80) |
| 2018 | 315,951 (172) | 136,712 (232) | 76,803 (136) | 13,364 (117) | 9,370 (78) | 44,388 (293) | 11,588 (77) |
| APC | 3.7** (3.2**) | 2.4** (2.9**) | 4.9** (5.6**) | 1.4** (−0.1) | 4.6** (3.7**) | 4.4** (0.7**) | 6.8** (3.3**) |
Note: Boldface indicates statistical significance
p<0.05;
p<0.01.
Age-adjusted YPLL rate per 100,000 population.
APC, annual percentage change.
With some fluctuations, mean age of ALD death steadily increased between 1999 and 2018 and increased more among men (Table 2). On average, decedents died of alcoholic fatty liver disease at a younger age than other types of ALD. Women died of ALD about 2–3 years earlier than men, but the sex difference was smaller among Hispanics, who died younger than whites and blacks, and much larger for blacks who died of alcoholic fatty liver and alcoholic hepatitis and who died in 2012–2018. Having a college degree tended to raise the mean age of death, except among Hispanic women. Co-occurring AUD reduced the mean age of death among white and Hispanic men; co-occurring injury (unnatural death) reduced the mean age of death among Hispanic men. By contrast, co-occurring tobacco use disorder, diabetes, and hypertension were generally associated with older mean ages of death.
Table 2.
Predictive Margins for Mean Age of Death From Alcoholic Liver Disease, 1999–2018
| Predictors for mean age of death | Non-Hispanic white | Non-Hispanic black | Hispanic | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Dif. | Male | Female | Dif. | Male | Female | Dif. | |
| Alcoholic liver disease | 55.2 | 52.4 | 2.8** | 55.4 | 52.5 | 3.0** | 52.6 | 51.1 | 1.5** |
| K70.0 Alcoholic fatty liver | 50.0** | 47.8** | 2.2** | 50.3** | 45.4** | 4.9** | 45.8** | 47.1** | −1.3 |
| K70.1 Alcoholic hepatitis | 52.4** | 49.7** | 2.7** | 54.0** | 50.0** | 4.0** | 49.0** | 46.7** | 2.3** |
| K70.2 Alcoholic fibrosis and sclerosis of liver | 53.2** | 50.2 | 3.0 | 51.4 | 51.5 | −0.2 | 54.6 | - | - |
| K70.3 Alcoholic cirrhosis of liver (ref) | 55.9 | 53.1 | 2.8** | 55.8 | 53.2 | 2.6** | 53.2 | 51.8 | 1.5** |
| K70.4 Alcoholic hepatic failure | 54.1** | 51.4** | 2.7** | 54.8** | 51.6** | 3.2** | 51.1** | 48.8** | 2.3** |
| K70.9 Alcoholic liver disease, unspecified | 55.0** | 52.2** | 2.8** | 55.7 | 52.2** | 3.5** | 52.0** | 50.8** | 1.3** |
| Educational achievement | |||||||||
| High school or less (ref) | 54.8 | 51.9 | 2.9** | 55.4 | 52.3 | 3.1** | 52.5 | 51.3 | 1.2** |
| Some college | 54.9 | 52.3** | 2.6** | 55.1 | 52.3 | 2.9** | 52.2 | 49.6** | 2.6** |
| College | 56.8** | 54.5** | 2.3** | 56.2* | 54.3** | 1.9** | 54.0** | 50.2* | 3.8** |
| Unknown | 56.6** | 52.7** | 3.9** | 56.1 | 53.2 | 2.9** | 54.6** | 52.4 | 2.2** |
| Marital status | |||||||||
| Never married (ref) | 49.5 | 47.1 | 2.4** | 51.7 | 49.2 | 2.5** | 48.0 | 46.9 | 1.1** |
| Married | 56.5** | 53.4** | 3.2** | 56.6** | 52.6** | 4.0** | 54.1** | 52.3** | 1.8** |
| Widowed | 61.9** | 59.9** | 2.0** | 62.3** | 60.0** | 2.2** | 60.8** | 58.9** | 1.9** |
| Divorced | 55.7** | 52.9** | 2.8** | 57.2** | 54.6** | 2.6** | 54.2** | 52.7** | 1.5** |
| Unknown | 54.7** | 53.4** | 1.3** | 55.8** | 52.7** | 3.0** | 51.4** | 51.3** | 0.1 |
| Co-occurring condition | |||||||||
| Alcohol use disorder | |||||||||
| No (ref) | 55.2 | 52.4 | 2.8** | 55.4 | 52.5 | 2.9** | 52.7 | 51.1 | 1.6** |
| Yes | 54.8** | 52.3 | 2.5** | 55.4 | 52.2 | 3.2** | 51.9** | 51.1 | 0.8* |
| Tobacco use disorder | |||||||||
| No (ref) | 55.0 | 52.3 | 2.7** | 55.3 | 52.3 | 3.0** | 52.6 | 51.1 | 1.5** |
| Yes | 56.9** | 53.0** | 3.8** | 56.6** | 54.6** | 2.0** | 53.8** | 51.8 | 2.0** |
| Hepatitis C virus infection | |||||||||
| No (ref) | 55.2 | 52.5 | 2.7** | 55.3 | 52.3 | 3.0** | 52.6 | 51.1 | 1.5** |
| Yes | 54.7** | 51.5** | 3.2** | 56.5** | 53.7** | 2.7** | 53.1** | 51.3 | 1.9** |
| Diabetes | |||||||||
| No (ref) | 55.1 | 52.3 | 2.8** | 55.4 | 52.4 | 3.0** | 52.5 | 50.9 | 1.6** |
| Yes | 57.4** | 55.7** | 1.8** | 56.6** | 53.9** | 2.7** | 55.1** | 55.0** | 0.1 |
| Hypertension | |||||||||
| No (ref) | 55.1 | 52.2 | 2.9** | 55.3 | 52.3 | 3.1** | 52.5 | 50.9 | 1.6** |
| Yes | 56.8** | 55.8** | 0.9** | 56.6** | 54.9** | 1.8** | 55.1** | 55.1** | 0.0 |
| Unnatural death | |||||||||
| No (ref) | 55.2 | 52.4 | 2.8** | 55.4 | 52.5 | 3.0** | 52.7 | 51.1 | 1.5** |
| Yes | 54.9 | 52.4 | 2.5** | 55.0 | 53.7 | 1.3 | 51.3** | 49.6 | 1.7 |
| Year | |||||||||
| 1999 | 53.3** | 50.7** | 2.6** | 52.3** | 50.0** | 2.3** | 51.1* | 49.4 | 1.7* |
| 2000 | 53.2** | 51.3 | 1.9** | 51.4** | 50.4* | 1.1* | 51.6 | 49.8 | 1.9* |
| 2001 | 53.2** | 51.0** | 2.2** | 52.6** | 50.6* | 2.1** | 51.5 | 49.8 | 1.7* |
| 2002 | 53.7** | 51.2* | 2.5** | 53.1** | 51.1 | 2.0** | 51.7 | 50.5 | 1.2 |
| 2003 | 53.6** | 51.3* | 2.4** | 53.2** | 51.9 | 1.2* | 51.3* | 51.6 | −0.3 |
| 2004 | 54.0* | 51.3 | 2.7** | 53.9 | 52.2 | 1.7** | 50.9** | 51.2 | −0.2 |
| 2005 | 54.2 | 51.6 | 2.5** | 53.8* | 51.3 | 2.5** | 51.8 | 50.6 | 1.2 |
| 2006 | 54.3 | 51.8 | 2.6** | 54.1 | 51.3 | 2.8** | 52.0 | 50.2 | 1.8** |
| 2007 (ref) | 54.5 | 51.8 | 2.7** | 54.7 | 51.9 | 2.8** | 52.0 | 50.8 | 1.2* |
| 2008 | 54.7 | 52.1 | 2.6** | 55.4 | 52.3 | 3.1** | 52.1 | 50.3 | 1.8** |
| 2009 | 55.0** | 52.2 | 2.7** | 55.2 | 53.2 | 2.0** | 52.1 | 50.8 | 1.3* |
| 2010 | 55.2** | 52.5** | 2.7** | 56.2** | 52.5 | 3.8** | 52.5 | 50.4 | 2.1** |
| 2011 | 55.4** | 52.6** | 2.8** | 56.0** | 53.8** | 2.3** | 53.0** | 51.3 | 1.7** |
| 2012 | 55.5** | 52.9** | 2.7** | 56.8** | 53.1 | 3.7** | 53.5** | 52.1 | 1.4** |
| 2013 | 55.9** | 53.0** | 2.9** | 56.9** | 53.1 | 3.9** | 52.9** | 51.0 | 1.8** |
| 2014 | 56.3** | 53.0** | 3.3** | 57.7** | 54.0** | 3.7** | 53.5** | 52.6** | 0.9 |
| 2015 | 56.2** | 53.3** | 2.9** | 58.1** | 53.6** | 4.5** | 53.6** | 51.6 | 2.0** |
| 2016 | 56.6** | 53.4** | 3.2** | 57.7** | 53.7** | 4.0** | 53.3** | 51.6 | 1.6** |
| 2017 | 56.5** | 53.5** | 3.0** | 57.7** | 54.1** | 3.5** | 53.8** | 51.5 | 2.3** |
| 2018 | 56.9** | 53.7** | 3.1** | 58.5** | 53.8** | 4.8** | 53.6** | 52.0 | 1.6** |
Note: Boldface indicates statistical significance
p<0.05;
p<0.01.
DISCUSSION
This study documented and confirmed an upward trend in premature deaths from ALD by sex and race/Hispanic origin from 1999–2018. As suggested in a previous study,6 ALD death rates were higher among men, but relative increases were greater among women, resulting in narrowing sex gaps. Accounted for cohort effects, premature mortality mainly increased among whites and Hispanic women, as indicated by net drift in Figure 2 and confirmed by age-adjusted YPLL rates in Table 1. The narrowing sex gaps in ALD death rates reflect the increasing trends in women’s drinking, high-risk drinking, and AUD38 and possible relatively higher occurrence of alcoholic hepatitis in women at younger ages. Similar sex differences in alcohol-related harms have been observed globally.39
The impact of ALD on women was further reflected in lower mean ages of ALD death than men regardless of sociodemographics, clinical courses of ALD, and comortalities. Although women are known to have longer life expectancies than men, women die of ALD at younger ages, presumably because women are at greater risk for developing ALD at lower lifetime alcohol intakes and shorter drinking histories. Women are more susceptible to ALD because of differences in hepatic ethanol metabolism and in mechanisms by which the body reacts to alcohol, such as endotoxin levels,40 gut permeability to endotoxins,41–46 effects of estrogen and androgens on endotoxin- and alcohol-mediated liver injury,44,47 and alcohol elimination rates.48,49 These variations are due to differences in first-pass metabolism, enzymatic activities,44,50–54 volumes of distribution, and peak blood alcohol levels.41,44,53 Given greater vulnerability to physiological consequences of high-risk drinking for women, narrowing sex gaps in prevalence of high-risk drinking may have contributed to the increasing sex disparity in mean age of ALD death over time. The rising trends in ALD deaths also coincide with those in severe obesity, which is more prevalent in women.55
Because of few symptoms at early disease stages and stigma attached to heavy alcohol use, most people with ALD are not diagnosed until later stages, when symptoms appear.16 Consequently, ALD is usually diagnosed among middle-aged adults, and survival rates are quite low once diagnosed.56 The finding of higher prevalence of ALD death among people aged 50 years and older reflects disease progression from morbidity to mortality. This age trend also parallels recent increases in alcohol use and binge drinking among middle-aged adults.57 Larger increases in binge and heavy drinking among older Americans57–59 may account for rising ALD death rates among black and Hispanic men from the mid-2000s for ages 60–69 years.
Unexpectedly, adults aged 25–34 years showed faster growth in ALD mortality (from 259 deaths in 1999 to 832 deaths in 2018) than older counterparts, as indicated by net drift (Figure 2) and rising death rates since 2007.60 Because it usually takes 10 or more years of drinking to develop liver diseases, premature mortality before age 35 years is quite unusual and cause for serious public health concerns. Cholankeril et al.61 reported that young adults (aged 18–39 years) on the liver transplantation waiting list had significantly greater severity of liver disease compared with their older counterparts. Increasing ALD mortality rates among young adults could be attributed to increases in extreme binge drinking, or high-intensity drinking, among heavy drinkers.62–69 One study found that certain birth cohorts aged younger than 50 years (men born between 1976 and 1985 and women born between 1981 and 1985) had the highest alcohol consumption.70 Changes in drinking patterns and more pronounced sex convergence in alcohol consumption among younger age cohorts38,39,57,71–75 contribute to the narrowing sex gap in ALD deaths. The hypothesis also is consistent with the same phenomenon observed in alcohol-related emergency department visits26 and hospitalization.27
Historically, sex disparities in drinking were more pronounced in Hispanics than other racial/ethnic groups. Hispanic women typically had much lower ALD death rates than men because heavy and binge drinking were male-dominated activities, whereas abstention and infrequent light drinking were common patterns among women.76–79 In this study, despite Hispanics’ lower all-cause mortality, Hispanic men maintained higher ALD death rates than their non-Hispanic counterparts. Lower SES, as reflected in lower educational attainment, might be a contributing factor to the higher ALD death rates observed in Hispanic men.80 Heightened rates among Hispanic women may be attributed to increases in female drinking associated with acculturation.81,82
The ALD death rates for whites surpassed those for blacks in the early 2000s. For several prior decades, blacks had much higher rates of cirrhosis mortality than whites.83,84 Scholars attributed these earlier racial disparities to differences in drinking behaviors. Compared with whites, blacks had a greater propensity for continued heavy drinking into their 30s and 40s despite later onset,85–87 as well as greater consumption of spirits.88,89 However, the higher rates in earlier years could also be due to the “alcohol harm paradox,” in which drinkers with lower SES experience more alcohol-related harms because of harmful alcohol consumption patterns, other unhealthy behaviors, and lack of access to healthcare resources.90 Increases in educational attainment among blacks could be one potential factor besides changes in drinking patterns. Higher college completion rates may have improved economic, social, and behavioral circumstances, leading to healthier lifestyles, better access to quality health care, and ultimately reductions in premature deaths from ALD. Yoon and colleagues91 found that college-educated blacks were less likely to drink beyond daily or weekly drinking limits than their counterparts with a high school education or less. Recent declines in mortality from HIV, HCV, and tobacco-related conditions, which are cofactors of ALD, also likely contributed to decreases in ALD deaths among blacks.3
In this study, middle-aged whites with lower educational attainment contributed to increases in premature mortality from ALD, as Case and Deaton2 suggested. However, middle-aged Hispanics with lower educational attainment also contributed to this increase. Educational attainment was inversely associated with ALD death rates overall. The ALD death rate escalated more rapidly after the economic recession in 2008 for all those with a high school or less education, and the associated male-to-female ratio of ALD death rates was higher for this educational group and decreased more drastically than for other groups after 2008 (Appendix Figure 1). Education was positively associated with mean age of death among whites, blacks, and Hispanic men, but not necessarily among female Hispanics, who received no beneficial effect of college education on health. Similar to a lack of education, never being married was associated with death at younger ages compared with other marital statuses, partly because lack of social integration increases mortality risks.92,93
Age-specific death rates and age-adjusted YPLL rates showed changes in direction (i.e., from modest declines to significant increases) in the mid-2000s. The first change from 2006 to 2007 was due to an ICD-10 coding rule change.32 Accelerated increases in ALD death rates after 2007, however, could be a lingering consequence of heavy drinking associated with economic hardship during the 2008–2009 recession. Previous studies reported that rising foreclosures, unemployment, and poverty coincided with an increase in heavy drinking occasions among heavy drinkers.94–96 Furthermore, resources to finance AUD treatment may have been depleted, adversely impacting ALD treatment options for financially vulnerable individuals.
The opioid epidemic beginning around 2010 and the new era of direct-acting antivirals for HCV infection beginning in 2011 have affected ALD mortality trends. Alcohol may interact with certain drugs to accentuate liver injury because the liver metabolizes, eliminates, and detoxifies both substances.97 Further analysis confirmed that the percentage of ALD deaths with drug-induced causes increased considerably during the study period and was greater among non-Hispanics (Appendix Figure 2). Alcohol use, in combination with coinfections with HIV-1 or hepatitis B virus, fosters progression of HCV infection in the development and severity of liver cirrhosis and mortality.98,99 Successful antiviral treatments for HCV have reduced the contribution of HCV to ALD deaths and prolonged longevity, particularly for non-Hispanic blacks. However, drug-induced causes (8.5%) and HCV (7.8%) are not very prevalent among ALD deaths.
Limitations
This study has several limitations, including use of death certificates, which are subject to under-reporting100–106; misclassification of race/ethnicity107,108; and lack of information on ALD onset, drinking histories, and treatment experiences and effectiveness. The high degree of selectivity in liver transplantation based on many psychosocial criteria, including 6-month abstinence from alcohol, may have prevented survival of ALD patients on the waiting list and those who had AUD but could not abstain from alcohol.61,109 Moreover, as in other observational studies, inferences are subject to measurement bias and confounding, and a cross-sectional study cannot investigate differential ALD progression among subgroups with various drinking patterns and durations. Large-scale prospective studies are needed to follow patients from diagnosis to death.
It is not clear whether there has been any improvement in under-reporting in general or due to stigma, as the NCHS medical examiners’ and coroners’ handbook110 has always encouraged reporting alcohol use on death certificates when it is believed to be a contributory cause. In the extreme scenario in which all the non-alcoholic liver disease deaths were indeed ALD deaths and were misclassified due to underreporting, the narrowing sex gaps would have been less pronounced. To accurately identify the pathologies associated with ALD deaths, a thorough macroscopic and microscopic post-mortem examination is desired. However, autopsies were performed on only a small percentage (8.9%) of ALD decedents and disproportionately on decedents with alcoholic fatty liver disease.
CONCLUSIONS
Although some studies have evaluated sex differences in alcohol consumption and cirrhosis mortality,111–117 this study examined ALD mortality directly by drawing upon all death certificates in the U.S. spanning 2 decades. Findings reported here provide empirical evidence of increases in premature mortality from ALD and demonstrate that longevity of men and women with ALD could be affected by demographic factors (e.g., race/Hispanic origin, marital status, and education) and comortalities. These findings encourage future research to examine whether environmental factors or alcohol policies may reduce premature mortality from ALD by reducing alcohol consumption or eliminating socioeconomic inequalities that imperil the health of economically disadvantaged populations. Destigmatizing AUD will also increase treatment utilization and prevent death from ALD. Future studies analyzing ALD mortality by sex and race/ethnicity should also take genetic and environmental risk factors into consideration, as they affect alcohol metabolism and subsequent liver injury.99,118–120 To address narrowing sex gaps in premature death from ALD, greater emphasis must be placed on implementation of abstinence programs, early detection of ALD, and education about hazardous drinking levels for women, as Saunders et al.121 suggested a few decades ago.
Supplementary Material
ACKNOWLEDGMENTS
The findings and conclusions in this report are those of the authors and do not reflect the official position of the National Institute on Alcohol Abuse and Alcoholism.
This article is based on a study conducted for the Alcohol Epidemiologic Data System project funded by the National Institute on Alcohol Abuse and Alcoholism, NIH, through Contract No. HHSN275201800004C to CSR, Incorporated. The views and opinions expressed in this article are those of the authors and should not be construed to represent the views of the sponsoring agency or the federal government.
Y-HY, CMC, MES, and AMW conceptualized the study. Y-HY led the drafting of the article. CMC performed data analysis. All authors (including MKJ) interpreted the findings, reviewed and edited drafts of the article, and approved the final version. Susanne Hiller-Sturmhöfel and Hunter Barret provided editorial support.
No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078-15083. 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Case A, Deaton A. Mortality and morbidity in the 21st century. Brookings Pap Econ Act. 2017;2017:397–476. 10.1353/eca.2017.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shiels MS, Chernyavskiy P, Anderson WF, et al. Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: an analysis of death certificate data. Lancet. 2017;389(10073):1043–1054. 10.1016/s0140-6736(17)30187-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.United Health Foundation. America’s Health Rankings Annual Report 2017. Minnetonka MN: United Health Foundation; 2017. https://assets.americashealthrankings.org/app/uploads/ahrannual17_complete-121817.pdf. Accessed September 18, 2019. [Google Scholar]
- 5.Woolf SH, Aron L, eds. U.S. Health in International Perspective: Shorter Lives, Poorer Health Washington, DC: National Academies Press; 2013. [PubMed] [Google Scholar]
- 6.Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959–2017. JAMA. 2019;322(20):1996–2016. 10.1001/jama.2019.16932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kochanek KD, Murphy SL, Xu J, Arias E. Deaths: Final Data for 2017. Natl Vital Stat Rep. 2019;68(9):1–77. [PubMed] [Google Scholar]
- 8.Murphy SL, Xu J, Kochanek KD, Curtin SC, Arias E. Deaths: Final Data for 2015. Natl Vital Stat Rep. 2017;66(6):1–75. [PubMed] [Google Scholar]
- 9.Kochanek KD, Arias E, Bastian BA. The effect of changes in selected age-specific causes of death on non-Hispanic white life expectancy between 2000 and 2014. NCHS Data Brief. 2016;(250):1–8. [PubMed] [Google Scholar]
- 10.Rehm J, Probst C. What about drinking is associated with shorter life in poorer people? PLoS Med. 2018;15(1):e1002477 10.1371/journal.pmed.1002477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rehm J, Probst C. Decreases of life expectancy despite decreases in non-communicable disease mortality: the role of substance use and socioeconomic status. Eur Addict Res. 2018;24(2):53–59. 10.1159/000488328. [DOI] [PubMed] [Google Scholar]
- 12.Imtiaz S, Probst C, Rehm J. Substance use and population life expectancy in the USA: interactions with health inequalities and implications for policy. Drug Alcohol Rev. 2018;37(suppl 1):S263–S267. 10.1111/dar.12616. [DOI] [PubMed] [Google Scholar]
- 13.Probst C, Rehm J. Alcohol use, opioid overdose and socioeconomic status in Canada: a threat to life expectancy? CMAJ. 2018;190(44):E1294–E1295. 10.1503/cmaj.180806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Probst C, Roerecke M, Behrendt S, Rehm J. Socioeconomic differences in alcohol-attributable mortality compared with all-cause mortality: a systematic review and meta-analysis. Int J Epidemiol. 2014;43(4):1314–1327. 10.1093/ije/dyu043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rehm J, Samokhvalov AV, Shield KD. Global burden of alcoholic liver diseases. J Hepatol. 2013;59(1):160–168. 10.1016/j.jhep.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 16.Singal AK, Bataller R, Ahn J, Kamath PS, Shah VH. ACG clinical guideline: alcoholic liver disease. Am J Gastroenterol. 2018;113(2):175–194. 10.1038/ajg.2017.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.CDC. Multiple Cause of Death 1999–2017 on CDC WONDER Online Database, released December, 2018. Data are from the Multiple Cause of Death Files, 1999–2017, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. https://wonder.cdc.gov/mcd.html. Accessed June 9, 2019. [Google Scholar]
- 18.Best AF, Haozous EA, Berrington de Gonzalez A, et al. Premature mortality projections in the USA through 2030: a modelling study. Lancet Public Health. 2018;3(8):e374–e384. 10.1016/S2468-2667(18)30114-2. Erratum in: Lancet Public Health. 2018;3(8):e364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singal AK, Anand BS. Recent trends in the epidemiology of alcoholic liver disease. Clin Liver Dis (Hoboken). 2013;2(2):53–56. 10.1002/cld.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Streba LA, Vere CC, Streba CT, Ciurea ME. Focus on alcoholic liver disease: from nosography to treatment. World J Gastroenterol. 2014;20(25):8040–8047. 10.3748/wjg.v20.i25.8040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brown L, Tucker-Seeley R. Commentary: will ‘Deaths of despair’ among whites change how we talk about racial/ethnic health disparities? Ethn Dis. 2018;28(2):123–128. 10.18865/ed.28.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gaydosh L, Hummer RA, Hargrove TW, et al. The depths of despair among US adults entering midlife. Am J Public Health. 2019;109(5):774–780. 10.2105/ajph.2019.305002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Glei DA, Goldman N, Weinstein M. A growing socioeconomic divide: effects of the great recession on perceived economic distress in the United States. PLoS One. 2019;14(4):e0214947 10.1371/journal.pone.0214947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shanahan L, Hill SN, Gaydosh LM, et al. Does despair really kill? A roadmap for an evidence-based answer. Am J Public Health. 2019;109(6):854–858. 10.2105/ajph.2019.305016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stein EM, Gennuso KP, Ugboaja DC, Remington PL. The epidemic of despair among white Americans: trends in the leading causes of premature death, 1999–2015. Am J Public Health. 2017;107(10):1541–1547. 10.2105/ajph.2017.303941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.White AM, Slater ME, Ng G, Hingson R, Breslow R. Trends in alcohol-related emergency department visits in the United States: results from the Nationwide Emergency Department Sample, 2006 to 2014. Alcohol Clin Exp Res. 2018;42(2):352–359. 10.1111/acer.13559. [DOI] [PubMed] [Google Scholar]
- 27.Chen CM, Yoon Y-H. Trends in alcohol-related morbidity among community hospital discharges, United States, 2000–2014 Surveillance Report #106. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism, Division of Epidemiology and Prevention Research; 2017. [Google Scholar]
- 28.Moon AM, Yang JY, Barritt AS 4th, Bataller R, Peery AF. Rising mortality from alcohol-associated liver disease in the United States in the 21st century. Am J Gastroenterol. 2020;115(1):79–87. 10.14309/ajg.0000000000000442. [DOI] [PubMed] [Google Scholar]
- 29.Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999–2016: observational study. BMJ. 2018;362:k2817 10.1136/bmj.k2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.White AM, Castle I-JP, Hingson RW, Powell PA. Using death certificates to explore changes in alcohol-related mortality in the United States, 1999 to 2017. Alcohol Clin Exp Res. 2020;44(1):178–187. 10.1111/acer.14239. [DOI] [PubMed] [Google Scholar]
- 31.WHO. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 32.Xu J, Kochanek KD, Murphy SL, Tejada-Vera B. Deaths: final data for 2007. Natl Vital Stat Rep. 2010;58(19):1–19. [PubMed] [Google Scholar]
- 33.National Center for Health Statistics. Instructions for classifying the underlying cause of death. Hyattsville, MD: National Center for Health Statistics; 1992. [Google Scholar]
- 34.Norheim OF, Jha P, Admasu K, et al. Avoiding 40% of the premature deaths in each country, 2010–30: review of national mortality trends to help quantify the UN sustainable development goal for health. Lancet. 2015;385(9964):239–252. 10.1016/S0140-6736(14)61591-9. Erratum in: Lancet. 2015;30;385(9983):2152. [DOI] [PubMed] [Google Scholar]
- 35.Wood SN. Generalized Additive Models: An Introduction with R. 2nd ed Boca Raton, FL: CRC Press; 2017. [Google Scholar]
- 36.Rosenberg PS, Check DP, Anderson WF. A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev. 2014;23(11):2296–2302. 10.1158/1055-9965.epi-14-0300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Williams R Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J. 2012;12(2):308–331. . [DOI] [Google Scholar]
- 38.Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001–2002 to 2012–2013: results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74(9):911–923. 10.1001/jamapsychiatry.2017.2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Slade T, Chapman C, Swift W, et al. Birth cohort trends in the global epidemiology of alcohol use and alcohol-related harms in men and women: systematic review and metaregression. BMJ Open. 2016;6(10):e011827 10.1136/bmjopen-2016-011827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bala S, Marcos M, Gattu A, Catalano D, Szabo G. Acute binge drinking increases serum endotoxin and bacterial DNA levels in healthy individuals. PLoS One. 2014;9(5):e96864 10.1371/journal.pone.0096864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Day CP. Who gets alcoholic liver disease: nature or nurture? J R Coll Physicians Lond. 2000;34(6):557–562. [PMC free article] [PubMed] [Google Scholar]
- 42.Kirpich IA, McClain CJ, Vatsalya V, et al. Liver injury and endotoxemia in male and female alcohol-dependent individuals admitted to an alcohol treatment program. Alcohol Clin Exp Res. 2017;41(4):747–757. 10.1111/acer.13346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Parlesak A, Schäfer C, Schütz T, Bode JC, Bode C. Increased intestinal permeability to macromolecules and endotoxemia in patients with chronic alcohol abuse in different stages of alcohol-induced liver disease. J Hepatol. 2000;32(5):742–747. 10.1016/s0168-8278(00)80242-1. [DOI] [PubMed] [Google Scholar]
- 44.Sato N, Lindros KO, Baraona E, et al. Sex difference in alcohol-related organ injury. Alcohol Clin Exp Res. 2001;25(5 suppl 1):40S–45S. 10.1111/j.1530-0277.2001.tb02371.x. [DOI] [PubMed] [Google Scholar]
- 45.Szabo G Gut-liver axis in alcoholic liver disease. Gastroenterology. 2015;148(1):30–36. 10.1053/j.gastro.2014.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Szabo G Women and alcoholic liver disease - warning of a silent danger. Nat Rev Gastroenterol Hepatol. 2018;15(5):253–254. 10.1038/nrgastro.2018.8. [DOI] [PubMed] [Google Scholar]
- 47.Ikejima K, Enomoto N, Iimuro Y, et al. Estrogen increases sensitivity of hepatic Kupffer cells to endotoxin. Am J Physiol. 1998;274(4):G669–G676. 10.1152/ajpgi.1998.274.4.g669. [DOI] [PubMed] [Google Scholar]
- 48.Mumenthaler MS, Taylor JL, O’Hara R, Yesavage JA. Gender differences in moderate drinking effects. Alcohol Res Health. 1999;23(1):55–64. [PMC free article] [PubMed] [Google Scholar]
- 49.Taylor JL, Dolhert N, Friedman L, Mumenthaler M, Yesavage JA. Alcohol elimination and simulator performance of male and female aviators: a preliminary report. Aviat Space Environ Med. 1996;67(5):407–413. [PubMed] [Google Scholar]
- 50.DiPadova C, Worner TM, Julkunen RJ, Lieber CS. Effects of fasting and chronic alcohol consumption on the first-pass metabolism of ethanol. Gastroenterology. 1987;92(5 Pt 1):1169–1173. 10.1016/s0016-5085(87)91073-0. [DOI] [PubMed] [Google Scholar]
- 51.Frezza M, di Padova C, Pozzato G, et al. High blood alcohol levels in women. The role of decreased gastric alcohol dehydrogenase activity and first-pass metabolism. N Engl J Med. 1990;322(2):95–99. 10.1056/nejm199001113220205. Erratum in: N Engl J Med. 1990;323(8):553. N Engl J Med. 1990;322(21):1540. [DOI] [PubMed] [Google Scholar]
- 52.Li TK, Beard JD, Orr WE, et al. Variation in ethanol pharmacokinetics and perceived gender and ethnic differences in alcohol elimination. Alcohol Clin Exp Res. 2000;24(4):415–416. 10.1111/j.1530-0277.2000.tb02002.x. [DOI] [PubMed] [Google Scholar]
- 53.Schenker S Medical consequences of alcohol abuse: is gender a factor? Alcohol Clin Exp Res. 1997;21(1):179–181. 10.1111/j.1530-0277.1997.tb03746.x. [DOI] [PubMed] [Google Scholar]
- 54.Thomasson HR. Gender differences in alcohol metabolism. Physiological responses to ethanol In: Galanter M, Beglieiter H, Deitrich R, et al. , eds. Recent Developments in Alcoholism-1995: Alcoholism and Women. New York, NY: Springer; 1995;12:163–179. 10.1007/0-306-47138-8_9. [DOI] [PubMed] [Google Scholar]
- 55.Fryar CD, Carroll MD, Ogden CL. Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2015–2016. Health E-Stats. National Center for Health Statistics. 2018. www.cdc.gov/nchs/data/hestat/obesity_adult_15_16/obesity_adult_15_16.pdf. Revised November 21, 2019 Accessed March 9, 2020. [Google Scholar]
- 56.Jepsen P, Lash TL, Vilstrup H. The clinical course of alcoholic cirrhosis: development of comorbid diseases. A Danish nationwide cohort study. Liver Int. 2016;36(11):1696–1703. 10.1111/liv.13151. [DOI] [PubMed] [Google Scholar]
- 57.Grucza RA, Sher KJ, Kerr WC, et al. Trends in adult alcohol use and binge drinking in the early 21st-Century United States: a meta-analysis of 6 national survey series. Alcohol Clin Exp Res. 2018;42(10):1939–1950. 10.1111/acer.13859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Breslow RA, Castle IP, Chen CM, Graubard BI. Trends in alcohol consumption among older Americans: National Health Interview Surveys, 1997 to 2014. Alcohol Clin Exp Res. 2017;41(5):976–986. 10.1111/acer.13365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Han BH, Moore AA, Ferris R, Palamar JJ. Binge drinking among older adults in the United States, 2015 to 2017. J Am Geriatr Soc. 2019;67(10):2139–2144. 10.1111/jgs.16071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yoon Y-H, Chen CM. Liver cirrhosis mortality in the United States: national, state, and regional trends, 2000–2017 Surveillance Report #114. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism, Division of Epidemiology and Prevention Research; 2019. [Google Scholar]
- 61.Cholankeril G, Gadiparthi C, Yoo ER, et al. Temporal trends associated with the rise in alcoholic liver disease-related liver transplantation in the United States. Transplantation. 2019;103(1):131–139. 10.1097/tp.0000000000002471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hingson RW, White A. Trends in extreme binge drinking among US high school seniors. JAMA Pediatr. 2013;167(11):996–998. 10.1001/jamapediatrics.2013.3083. [DOI] [PubMed] [Google Scholar]
- 63.Hingson R, White A. One-fifth of high-school seniors participate in binge drinking. J Pediatr. 2014;164(3):672–676. 10.1016/j.jpeds.2013.12.023. [DOI] [PubMed] [Google Scholar]
- 64.Jang JB, Patrick ME, Keyes KM, Hamilton AD, Schulenberg JE. Frequent binge drinking among US adolescents, 1991 to 2015. Pediatrics. 2017;139(6):e20164023 10.1542/peds.2016-4023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Patrick ME, Azar B. High-intensity drinking. Alcohol Res. 2018;39(1):49–55. [PMC free article] [PubMed] [Google Scholar]
- 66.Patrick ME, Schulenberg JE, Martz ME, et al. Extreme binge drinking among 12th-grade students in the United States: prevalence and predictors. JAMA Pediatr. 2013;167(11):1019–1025. 10.1001/jamapediatrics.2013.2392. Erratum in: JAMA Pediatr. 2013;167(12):1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Patrick ME, Terry-McElrath YM, Miech RA, et al. Age-specific prevalence of binge and high-intensity drinking among U.S. young adults: changes from 2005 to 2015. Alcohol Clin Exp Res. 2017;41(7):1319–1328. 10.1111/acer.13413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Patrick ME, Terry-McElrath YM. Prevalence of high-intensity drinking from adolescence through young adulthood: national data from 2016–2017. Subst Abuse. 2019;13:1178221818822976 10.1177/1178221818822976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.White A, Hingson R. The burden of alcohol use: excessive alcohol consumption and related consequences among college students. Alcohol Res. 2013;35(2):201–218. [PMC free article] [PubMed] [Google Scholar]
- 70.Kerr WC, Greenfield TK, Ye Y, Bond J, Rehm J. Are the 1976–1985 birth cohorts heavier drinkers? Age-period-cohort analyses of the National Alcohol Surveys 1979–2010. Addiction. 2013;108(6):1038–1048. 10.1111/j.1360-0443.2012.04055.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dwyer-Lindgren L, Flaxman AD, Ng M, et al. Drinking patterns in US counties from 2002 to 2012. Am J Public Health. 2015;105(6):1120–1127. 10.2105/ajph.2014.302313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Keyes KM, Grant BF, Hasin DS. Evidence for a closing gender gap in alcohol use, abuse, and dependence in the United States population. Drug Alcohol Depend. 2008;93(1–2):21–29. 10.1016/j.drugalcdep.2007.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Keyes KM, Jager J, Mal-Sarkar T, et al. Is there a recent epidemic of women’s drinking? A critical review of national studies. Alcohol Clin Exp Res. 2019;43(7):1344–1359. 10.1111/acer.14082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.McCaul ME, Roach D, Hasin DS, Weisner C, Chang G, Sinha R. Alcohol and women: a brief overview. Alcohol Clin Exp Res. 2019;43(5):774–779. 10.1111/acer.13985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.White A, Castle IJ, Chen CM, et al. Converging patterns of alcohol use and related outcomes among females and males in the United States, 2002 to 2012. Alcohol Clin Exp Res. 2015;39(9):1712–1726. 10.1111/acer.12815. [DOI] [PubMed] [Google Scholar]
- 76.Yoon Y-H, Yi HY, Thomson PC. Alcohol-related and viral hepatitis C-related cirrhosis mortality among Hispanic subgroups in the United States, 2000–2004. Alcohol Clin Exp Res. 2011;35(2):240–249. 10.1111/j.1530-0277.2010.01340.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Caetano R Alcohol use among Hispanic groups in the United States. Am J Drug Alcohol Abuse. 1988;14(3):293–308. 10.3109/00952998809001552. [DOI] [PubMed] [Google Scholar]
- 78.Canino G Alcohol use and misuse among Hispanic women: selected factors, processes, and studies. Int J Addict. 1994;29(9):1083–1100. 10.3109/10826089409047930. [DOI] [PubMed] [Google Scholar]
- 79.Gilbert MJ, Cervantes RC. Patterns and practices of alcohol use among Mexican-Americans: a comprehensive review. Hisp J Behav Sci. 1986;8(1):1–60. 10.1177/07399863860081001. [DOI] [Google Scholar]
- 80.U.S. Census Bureau. CPS Historical Time Series Tables. Table A-2 Percent of People 25 Years and Over Who Have Completed High School or College, by Race, Hispanic Origin and Sex: Selected Years 1940 to 2018. Washington, DC: U.S. Census Bureau; 2019. www.census.gov/data/tables/time-series/demo/educational-attainment/cps-historical-time-series.html. Accessed March 13, 2020. [Google Scholar]
- 81.Chartier KG, Vaeth PA, Caetano R. Focus on: ethnicity and the social and health harms from drinking. Alcohol Res. 2013;35(2):229–237. [PMC free article] [PubMed] [Google Scholar]
- 82.Vaeth PA, Caetano R, Rodriguez LA. The Hispanic Americans Baseline Alcohol Survey (HABLAS): the association between acculturation, birthplace and alcohol consumption across Hispanic national groups. Addict Behav. 2012;37(9):1029–1037. 10.1016/j.addbeh.2012.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kerr WC, Karriker-Jaffe KJ, Ye Y. Examining alcohol’s contribution to the US African-American/White cirrhosis mortality differential from 1950 to 2002. Alcohol. 2013;48(5):605–612. 10.1093/alcalc/agt031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mandayam S, Jamal MM, Morgan TR. Epidemiology of alcoholic liver disease. Semin Liver Dis. 2004;24(3):217–232. 10.1055/s-2004-832936. [DOI] [PubMed] [Google Scholar]
- 85.Ethnicity Caetano R. and drinking in northern California: a comparison among whites, blacks and Hispanics. Alcohol Alcohol. 1984;19(1):31–44. 10.1093/oxfordjournals.alcalc.a044398. [DOI] [PubMed] [Google Scholar]
- 86.Caetano R, Kaskutas LA. Changes in drinking problems among whites, blacks, and Hispanics, 1984–1992. Subst Use Misuse. 1996;31(11–12):1547–1571. 10.3109/10826089609063991. [DOI] [PubMed] [Google Scholar]
- 87.Johnson RA, Larison C, Gerstein DR, Greenblatt J. Prevalence of Substance Use Among Racial and Ethnic Subgroups in the United States 1991–1993. Rockville, MD: Substance Abuse and Mental Health Services Administration; 1998. [Google Scholar]
- 88.Migration Herd D., cultural transformation and the rise of black liver cirrhosis mortality. Br J Addict. 1985;80(4):397–410. 10.1111/j.1360-0443.1985.tb03011.x. [DOI] [PubMed] [Google Scholar]
- 89.Kerr WC, Greenfield TK. Distribution of alcohol consumption and expenditures and the impact of improved measurement on coverage of alcohol sales in the 2000 National Alcohol Survey. Alcohol Clin Exp Res. 2007;31(10):1714–1722. 10.1111/j.1530-0277.2007.00467.x. [DOI] [PubMed] [Google Scholar]
- 90.Bellis MA, Hughes K, Nicholls J, et al. The alcohol harm paradox: using a national survey to explore how alcohol may disproportionately impact health in deprived individuals. BMC Public Health. 2016;16:111 10.1186/s12889-016-2766-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Yoon Y-H, Yi H, Chen CM, Breslow RA. Education level and drinking behavior among racial/ethnic groups: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Poster presented at the 133rd Annual Meeting of the American Public Health Association, Philadelphia, PA, December 10–14; 2005. [Google Scholar]
- 92.Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979;109(2):186–204. 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 93.Berkman LF, Melchior M, Chastang JF, et al. Social integration and mortality: a prospective study of French employees of Electricity of France-Gas of France: the GAZEL Cohort. Am J Epidemiol. 2004;159(2):167–174. 10.1093/aje/kwh020. [DOI] [PubMed] [Google Scholar]
- 94.Kerr WC, Mulia N, Zemore SE. U.S. trends in light, moderate, and heavy drinking episodes from 2000 to 2010. Alcohol Clin Exp Res. 2014;38(9):2496–2501. 10.1111/acer.12521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kerr WC, Kaplan MS, Huguet N, et al. Economic recession, alcohol, and suicide rates: comparative effects of poverty, foreclosure, and job loss. Am J Prev Med. 2017;52(4):469–475. 10.1016/j.amepre.2016.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mulia N, Zemore SE, Murphy R, Liu H, Catalano R. Economic loss and alcohol consumption and problems during the 2008 to 2009 U.S. recession. Alcohol Clin Exp Res. 2014;38(4):1026–1034. 10.1111/acer.12301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ding W-X, Yang Li. Alcohol and drug-induced liver injury: metabolism, mechanisms, pathogenesis and potential therapies. Liver Res. 2019;3(3–4):129–131. 10.1016/j.livres.2019.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lauer GM, Walker BD. Hepatitis C virus infection. N Engl J Med. 2001;345(1):41–52. 10.1056/nejm200107053450107. [DOI] [PubMed] [Google Scholar]
- 99.Zakhari S, Li TK. Determinants of alcohol use and abuse: impact of quantity and frequency patterns on liver disease. Hepatology. 2007;46(6):2032–2039. 10.1002/hep.22010. [DOI] [PubMed] [Google Scholar]
- 100.Hanzlick R Death certificates, natural death, and alcohol. The problem of underreporting. Am J Forensic Med Pathol. 1988;9(2):149–150. 10.1097/00000433-198806000-00011. [DOI] [PubMed] [Google Scholar]
- 101.Kircher T, Nelson J, Burdo H. The autopsy as a measure of accuracy of the death certificate. N Engl J Med. 1985;313(20):1263–1269. 10.1056/nejm198511143132005. [DOI] [PubMed] [Google Scholar]
- 102.Nashold RD, Naor EM. Alcohol-related deaths in Wisconsin: the impact of alcohol on mortality. Am J Public Health. 1981;71(11):1237–1241. 10.2105/ajph.71.11.1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Nelson DE, Sacks JJ, Parrish RG, et al. Sensitivity of multiple-cause mortality data for surveillance of deaths associated with head or neck injuries. MMWR Surveill Summ. 1993;42(5):29–35. [PubMed] [Google Scholar]
- 104.Petersson B, Krantz P, Kristensson H, Trell E, Sternby NH. Alcohol-related death: a major contributor to mortality in urban middle-aged men. Lancet. 1982;2(8307):1088–1090. 10.1016/s0140-6736(82)90015-0. [DOI] [PubMed] [Google Scholar]
- 105.Pollock DA, Boyle CA, DeStefano F, Moyer LA, Kirk ML. Underreporting of alcohol-related mortality on death certificates of young US Army veterans. JAMA. 1987;258(3):345–348. 10.1001/jama.1987.03400030061032. [DOI] [PubMed] [Google Scholar]
- 106.Romelsjö A, Karlsson G, Henningsohn L, Jakobsson SW. The prevalence of alcohol-related mortality in both sexes: variation between indicators, Stockholm, 1987. Am J Public Health. 1993;83(6):838–844. 10.2105/ajph.83.6.838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Arias E, Schauman WS, Eschbach K, Sorlie PD, Backlund E. The validity of race and Hispanic origin reporting on death certificates in the United States. Vital Health Stat 2. 2008;(148):1–23. [PubMed] [Google Scholar]
- 108.Rosenberg HM, Maurer JD, Sorlie PD, et al. Quality of death rates by race and Hispanic origin: a summary of current research, 1999. Vital Health Stat 2. 1999;(128):1–13. [PubMed] [Google Scholar]
- 109.Singh S, Osna NA, Kharbanda KK. Treatment options for alcoholic and non-alcoholic fatty liver disease: a review. World J Gastroenterol. 2017;23(36):6549–6570. 10.3748/wjg.v23.i36.6549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.National Center for Health Statistics. Medical Examiners’ and Coroners’ Handbook on Death Registration and Fetal Death Reporting. Hyattsville, MD: National Center for Health Statistics; 2003. www.cdc.gov/nchs/data/misc/hb_me.pdf. Published 2003. Accessed March 9, 2020. [Google Scholar]
- 111.Becker U, Deis A, Sørensen TI, et al. Prediction of risk of liver disease by alcohol intake, sex, and age: a prospective population study. Hepatology. 1996;23(5):1025–1029. 10.1002/hep.510230513. [DOI] [PubMed] [Google Scholar]
- 112.Becker U, Grønbaek M, Johansen D, Sørensen TI. Lower risk for alcohol-induced cirrhosis in wine drinkers. Hepatology. 2002;35(4):868–875. 10.1053/jhep.2002.32101. [DOI] [PubMed] [Google Scholar]
- 113.Corrao G, Aricò S, Lepore R, et al. Amount and duration of alcohol intake as risk factors of symptomatic liver cirrhosis: a case-control study. J Clin Epidemiol. 1993;46(7):601–607. 10.1016/0895-4356(93)90032-v. [DOI] [PubMed] [Google Scholar]
- 114.Gordon T, Kannel WB. Drinking and mortality: the Framingham Study. Am J Epidemiol. 1984;120(1):97–107. 10.1093/oxfordjournals.aje.a113879. [DOI] [PubMed] [Google Scholar]
- 115.Klatsky AL, Friedman GD, Armstrong MA, Kipp H. Wine, liquor, beer, and mortality. Am J Epidemiol. 2003;158(6):585–595. 10.1093/aje/kwg184. [DOI] [PubMed] [Google Scholar]
- 116.Rehm J, Taylor B, Mohapatra S, et al. Alcohol as a risk factor for liver cirrhosis: a systematic review and meta-analysis. Drug Alcohol Rev. 2010;29(4):437–445. 10.1111/j.1465-3362.2009.00153.x. [DOI] [PubMed] [Google Scholar]
- 117.Thun MJ, Peto R, Lopez AD, et al. Alcohol consumption and mortality among middle-aged and elderly U.S. adults. N Engl J Med. 1997;337(24):1705–1714. 10.1056/nejm199712113372401. [DOI] [PubMed] [Google Scholar]
- 118.Day CP. Genes or environment to determine alcoholic liver disease and non-alcoholic fatty liver disease. Liver Int. 2006;26(9):1021–1028. 10.1111/j.1478-3231.2006.01323.x. [DOI] [PubMed] [Google Scholar]
- 119.Kemmer N, Neff GW. Ethnic variations in chronic liver diseases. Dig Dis Sci. 2008;53(5):1339–1344. 10.1007/s10620-007-9992-0. [DOI] [PubMed] [Google Scholar]
- 120.Reuben A Alcohol and the liver. Curr Opin Gastroenterol. 2008;24(3):328–338. 10.1097/MOG.0b013e3282fbceca. [DOI] [PubMed] [Google Scholar]
- 121.Saunders JB, Davis M, Williams R. Do women develop alcoholic liver disease more readily than men? Br Med J (Clin Res Ed). 1981;282(6270):1140–1143. 10.1136/bmj.282.6270.1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


