Abstract
Objective:
Previous studies have demonstrated associations between race-based residential segregation, neighborhood socioeconomic and physical environmental characteristics, and mortality. Relatively few studies have examined independent and joint effects of these multiple neighborhood characteristics and mortality, including potential mediating pathways. In this study we examine the extent to which associations between race-based residential segregation and all-cause mortality may be explained by multiple socioeconomic indicators and exposure to air pollutants.
Methods:
Drawing on data from multiple sources, we assessed bivariate associations between race-based residential segregation (operationalized as percent non-Hispanic Black), education (percent with graduate equivalency degree), poverty (percent below poverty), income inequality (GINI coefficient) and air pollution (ambient PM2.5) and age adjusted all-cause, all race mortality (henceforth all cause mortality) at the census tract level in the Detroit Metropolitan Area. We used inequality curves to assess the (in)equitable distribution of economic and environmental characteristics by census tract racial composition. Finally, we used generalized estimating equations (GEE) to examine independent and joint associations among percent NHB, education, income inequality, and air pollution to all-cause mortality, and test for mediating effects.
Results:
Bivariate associations between racial composition, education, poverty, income inequality, PM2.5 and all-cause mortality were statistically significant. Census tracts with higher concentrations of NHB residents had significantly lower educational attainment, higher poverty, and greater exposure to PM2.5. In multivariate models, education, income inequality and PM2.5 fully attenuated associations between racial composition and all-cause mortality.
Conclusions:
Results are consistent with the hypothesis that race-based residential segregation is associated with heightened all-cause mortality, and that those effects are mediated by education, income inequality, and exposure to air pollution at the census tract level. Public health and cross-sector interventions to eliminate race-based residential segregation or to eliminate the maldistribution of educational and economic resources, and environmental exposures, across census tracts could substantially reduce regional inequities in all-cause mortality.
Keywords: Race-based residential segregation and mortality, joint effects of socioeconomic status and physical environment on mortality, Cumulative risk
INTRODUCTION
Race-based residential segregation has been inversely associated with economic and educational opportunities (Logan, Minca, & Adar, 2012; Massey, Gross, & Eggers, 1991; S. R. Reardon, Fox, & Townsend, 2015) and positively associated with air pollutant levels, proximity to hazardous waste facilities and other hazardous land uses (Jones et al., 2014; L. J. Rice et al., 2014). The unequal distribution of multiple risk factors associated with adverse health outcomes has contributed to interest in examining how these risks combine or accumulate to shape health outcomes across geographic areas (Sexton & Linder, 2011; Solomon, Morello-Frosch, Zeise, & Faust, 2016). Much of the literature examining the accumulation of risks conceptualizes social and economic indicators as indicators of population vulnerability, defined as population characteristics associated with heightened probability of exposure to physical environmental threats, or as population susceptibility, defined as characteristics associated with greater health impacts at any given level of exposure (Callahan et al., 2003; Moretto et al., 2016). Race-based residential segregation in the context of the United States is conceptualized here as an indicator of the social environment, reflecting historical as well as contemporary policies that inequitably shape access to housing across geographic areas. Segregation, in turn, shapes access to resources such as education and employment opportunities, as well as the ability to avoid exposures that are inimical to health, such as air pollution (Phelan & Link, 2015; Schulz, Williams, Israel, & Lempert, 2002; Williams & Collins, 2001; Williams & Mohammed, 2013). Relatively few studies have examined the combined implications for health of these multiple pathways through which segregation may impact health outcomes. In this paper, we examine the independent and joint contributions of race-based residential segregation, indicators of the economic environment, and exposure to air pollutants to all-cause mortality, in the Detroit Metropolitan Area (DMA).
Conceptual Framework
In the century since W.E.B. DuBois documented the physical and social environments in which “the Philadelphia Negro” lived, worked and sought to maintain health and well-being (Du Bois, 1899), a body of work has emerged examining associations between neighborhood racial composition, neighborhood economic and physical environmental characteristics and health. Building on prior models of segregation and health (Schulz et al., 2016, 2002; Williams & Collins, 2001), we conceptualize racial residential segregation as a manifestation of racist ideologies that shape health outcomes through multiple pathways, encompassing both health protective and health eroding impacts. These include systematic impacts on the social, economic and physical contexts in which people live, shaping opportunities for health. Below we briefly review the evidence linking racial or ethnic composition of neighborhoods, as one indicator of segregation, with socioeconomic and physical environmental contexts, and with all-cause mortality.
Race-based residential segregation.
Racial residential segregation can be conceptualized as an indicator of historical and contemporary social and political environments, and as one manifestation of ideologies of white supremacy, a political, economic and cultural system that rests upon the systematic devaluation of Black and Brown lives (Ansley, 1997). Historically in the U.S., housing policies and practices explicitly created and reinforced racial segregation (Rothstein, 2017), assuring separation of non-Hispanic Whites (NHW) from racialized groups (Charles, 2003; Rothstein, 2017). The Fair Housing Act of 1968 provided protections against housing discrimination on the basis of race, color, religion or national origin. However, racial segregation has remained high in many areas of the country, in particular for non-Hispanic Black (NHB) Americans (Reibel & Regelson, 2011). The geographic separation of NHB Americans from, in particular, NHW is reflective of, and reinforces, deeply embedded ideologies of white supremacy that structure social relationships in the U.S. (Kendi, 2017; Rothstein, 2017).
Socioeconomic inequalities.
There is substantial evidence that residential racial segregation contributes to economic divestment, limited educational and employment opportunities, as well as foreclosure risk (Bell & Lee, 2011; Morello-Frosch & Jesdale, 2006; Rugh & Massey, 2010; Sugrue, 2014). Socioeconomic characteristics of neighborhoods, including opportunity structures, economic resources and income inequalities, are associated with health inequities. Across various measures of socioeconomic position (SEP), incremental increases in social standing largely correlate with improved community health outcomes (Andersen et al., 2018; Meijer, Röhl, Bloomfield, & Grittner, 2012). NHBs and Hispanics in the United States are disproportionately likely to reside in communities with reduced access to quality education and employment opportunities (Logan et al., 2012; Massey et al., 1991; S. R. Reardon et al., 2015) and to benefit less in terms of occupational and economic returns on educational attainment (Phelan & Link, 2015; Williams & Mohammed, 2013). Several studies have linked neighborhood level characteristics such as educational attainment and economic indicators to racial and ethnic health inequities (Denney, Saint Onge, & Dennis, 2018; LaVeist, Pollack, Thorpe, Fesahazion, & Gaskin, 2011; Mode, Evans, & Zonderman, 2016; Yao & Robert, 2011). Lower economic status contributes to adverse health effects through multiple mechanisms including, for example, poor quality housing (Camacho-Rivera, Kawachi, Bennett, & Subramanian, 2014; Evans & Kantrowitz, 2002; Evans & Kim, 2010) and reduced access to healthcare (Kirby & Kaneda, 2005). Residents of areas with limited economic opportunities and access to resources (e.g., transportation, health and social services) which can buffer adverse effects of poverty (Dinwiddie, Gaskin, Chan, Norrington, & McCleary, 2013; Haley et al., 2017; Kirby & Kaneda, 2005; Meijer et al., 2012; White, Haas, & Williams, 2012) face particular challenges.
Physical environment.
Exposure to ambient air pollution is an important risk factor in the physical environment. It is associated with increased risk of multiple adverse health outcomes, including cardiovascular mortality (Brook et al., 2010; Jerrett et al., 2013; Ostro et al., 2015), respiratory hospitalization (Neupane et al., 2010), asthma exacerbation (Fan, Li, Fan, Bai, & Yang, 2016; Li et al., 2011; Strickland et al., 2010), incidence and duration of respiratory symptoms (Johannson et al., 2014; Stern et al., 2013), declines in lung function (Gehring et al., 2013; M. B. Rice et al., 2013; Urman et al., 2014), preterm delivery and low birth weights (Pedersen et al., 2013; Shah, Balkhair, & Knowledge Synthesis Group on Determinants of Preterm/LBW Birth, 2011; Stieb, Chen, Eshoul, & Judek, 2012), and restricted activity (Fann et al., 2012; Nam, Selin, Rielly, & Paltsev, 2010). Fine particulate matter (PM2.5) is more strongly associated with morbidity and mortality than coarse particulate matter (PM10) (U.S Environmental Protection Agency, 2002). Adverse health effects are observed at pollution levels below current U.S. National Ambient Air Quality Standards (NAAQS) and common to many U.S. cities (Lepeule, Laden, Dockery, & Schwartz, 2012; Shi et al., 2016).
Combined socioeconomic and physical environmental factors and health.
In addition to the social and economic vulnerabilities described above, NHB and Hispanic communities, and those with low to moderate incomes, are disproportionately exposed to air pollutants (Clark, Quinn, Dodge, & Nelson, 2014; Collins, Grineski, Chakraborty, Montgomery, & Hernandez, 2015; Gray, Edwards, & Miranda, 2013; Huang & London, 2012; Jones et al., 2014; Mohai, Lantz, Morenoff, House, & Mero, 2009; Schulz et al., 2016). Low to moderate economic status contributes to challenges avoiding exposure and may exacerbate adverse health effects of exposures (Sadd, Pastor, Morello-Frosch, Scoggins, & Jesdale, 2011). Mechanisms include, for example, poorer quality housing (Adamkiewicz et al., 2014; Jacobs, 2011) and reduced access to health care (Forno & Celedon, 2009). Children and older adults are more susceptible to adverse health effects of exposure (Bell & Lee, 2011; Kelishadi & Poursafa, 2010; National Environmental Justice Advisory Council, 2014; Sacks et al., 2011; Solomon et al., 2016). Yet, relatively few studies have examined combined effects of exposure to air pollution in conjunction with population social and economic vulnerabilities, or quantified the health impacts associated with reductions in air pollution in communities as these may vary with characteristics of exposed populations. Using data from the Detroit Metropolitan Area (DMA), we examine the independent and joint contributions of air pollution exposure and social and economic characteristics of neighborhoods to all-cause mortality. Despite evidence linking racial residential segregation to circumscribed access to resources necessary to maintain health (e.g., educational opportunity, economic opportunity) and to excess exposure to environments detrimental to health (e.g., air pollutants), results from studies examining associations between neighborhood racial composition and mortality have been mixed. In a recent review article, Bécares and colleagues (2012) found that several studies reported positive associations between percent black residents and all-cause mortality (Erwin, Fitzhugh, Brown, Looney, & Forde, 2010; Jackson, Anderson, Johnson, & Sorlie, 2000; LeClere, Rogers, & Peters, 1997), while others reported null or negative associations (Blanchard, Cossman, & Levin, 2004; Hutchinson et al., 2009; Inagami et al., 2006).
There are a number of potential explanations for these mixed results. The reported findings may be influenced by differences across studies in the extent to which they account for potential mediating pathways as well as neighborhood level correlations between racial composition, restricted economic and educational opportunities, and adverse physical environmental exposures (Huang & London, 2012; Sadd et al., 2011; Schulz et al., 2018, 2016; Su et al., 2009). Researchers have sought increasingly to examine joint effects of physical environmental exposures with social and economic characteristics on health (Collins et al., 2015; Mohai et al., 2009) in order to understand unique and joint effects of these correlated pathways. To the extent that adverse physical environmental exposures cluster in communities with limited social and economic resources, effects may accumulate, compounding implications for racial and socioeconomic health inequities (Bell & Lee, 2011; Callahan et al., 2003; Commission on the Social Determinants of Health, 2008; Dankwa-Mullan et al., 2010; Kelishadi & Poursafa, 2010; Mujahid et al., 2008; Sacks et al., 2011; Solomon et al., 2016).
Understanding joint effects of multiple, often linked, social, economic and physical environmental factors thus remains an important challenge (Alvarez, Appleton, Fuller, Belcourt, & Kubzansky, 2018; Huang & London, 2012; Sadd et al., 2011; Su et al., 2009). This research examines hypothesized relationships between multiple area level characteristics and all-cause mortality, using specific measures that may be relevant to developing local policies, to address this important gap (Markevych et al., 2017).
Overarching goal.
The primary research question addressed in this paper is the extent to which area level social, economic and physical environmental characteristics contribute to geographic variations in mortality in the DMA. Relationships are modeled at the census tract level to examine contributions to census tract level all-cause, all race mortality. Understanding the factors that drive the racial and socioeconomic patterning of risk within and across the DMA, including processes through which cumulative advantage and disadvantage accrue, is essential to understand the drivers of poor health outcomes and health inequities and to address them. Among these potential pathways are synergistic effects of the physical environment with social and economic characteristics.
Context.
Historically, the DMA, made up of Macomb, Oakland, and Wayne Counties, has been among the most racially segregated regions in the nation (Farley, 2011; Fry & Taylor, 2012). Numerous factors contributed to this segregation, including housing agreements prominent prior to 1948 that restricted home-ownership in areas of the city of Detroit to whites only (Sugrue, 2014). Despite Detroit’s major contributions to the Civil Rights Movement, discrimination in the real estate market, including federally-backed home mortgages available to NHWs but not NHBs, perpetuated segregation and reduced NHBs’ access to suburban employment opportunities (Farley, 2015; Farley, Danziger, & Holzer, 2000; Sugrue, 2014). Today’s DMA reflects these historical and contemporary processes (see Figure 1). NHB populations in Wayne, Oakland, and Macomb counties are clustered in older, urban areas (“2015 Data Release New and Notable,” 2016). Eighty-five percent of Wayne County’s NHB population is located in Detroit city (“2015 Data Release New and Notable,” 2016). Detroit city is also home to an Hispanic community whose roots extend back nearly a century (Rodriguez, Bowie, Frattaroli, & Gielen, 2009). NHBs and Hispanics across the DMA are disproportionately represented in households below the federal poverty line (Jargowsky, 2015). Over 57% of Detroit’s children (Annie E. Casey Foundation, 2015; New Detroit Coalition, 2014), compared to 37%, 20%, and 13% of children in Wayne, Macomb, and Oakland counties, respectively, live in households below the poverty line (“2015 Data Release New and Notable,” 2016).
Fig. 1.
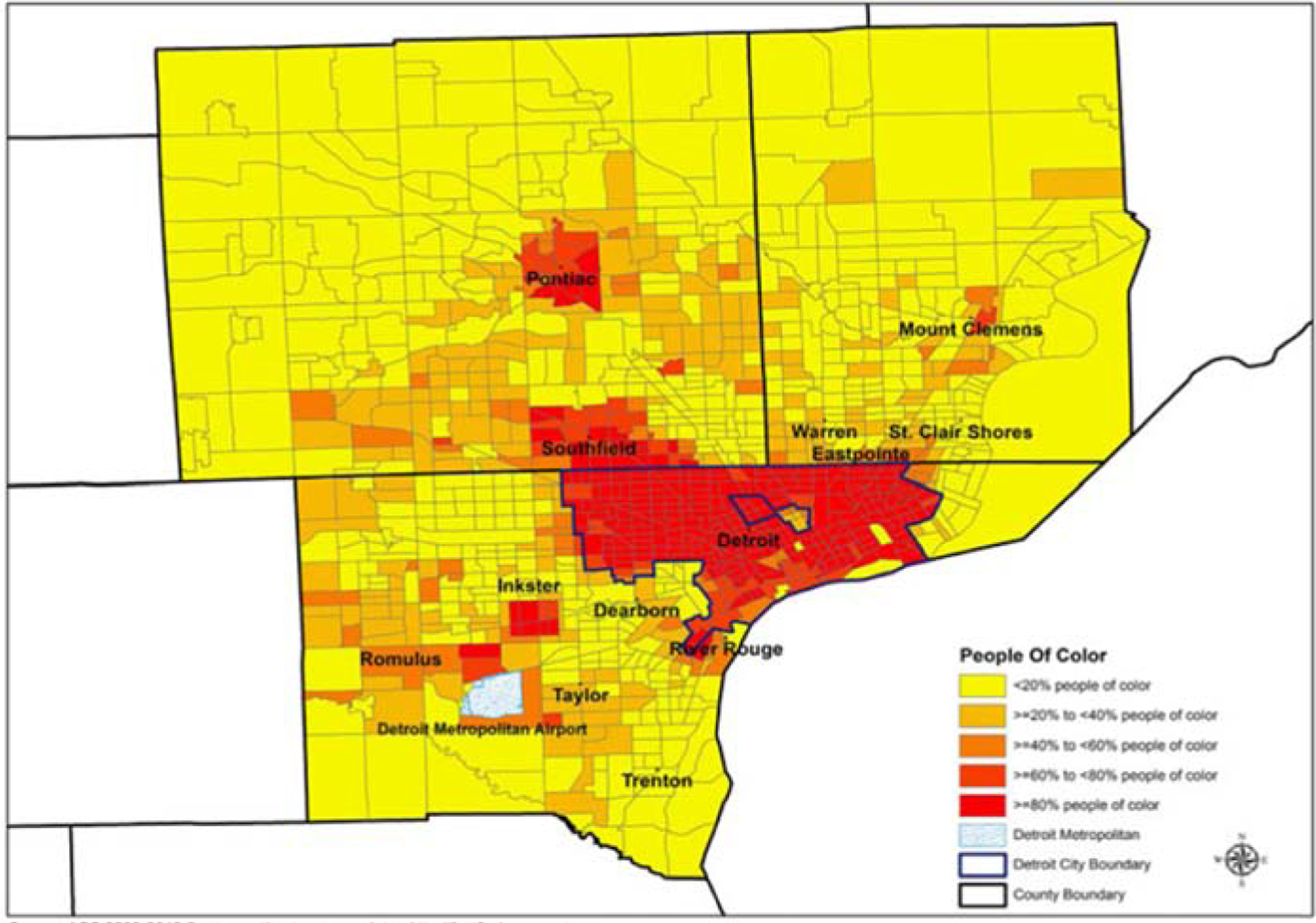
Proportion people of color at the Census track level-Detroit Metropolitan Area.
DMA census tracts with greater concentrations of NHB and Hispanic residents, households below the poverty line, and residents who have not completed high school are more likely to have higher levels of exposure to diesel PM (a component of air pollution more broadly) and associated cancer and respiratory health risks (Schulz et al., 2016). This study extends previous research in the DMA by examining the independent and joint associations between racial composition, physical environmental exposures (fine particulate matter or PM2.5), social and economic characteristics (education, poverty, income inequality) and all-cause mortality in the DMA.
DATA AND METHODS
The study was conducted as part of Community Action to Promote Healthy Environments, a community-based participatory research partnership designed to equitably engage community, academic, and health service provider organizations in research, and to translate results from that research into action to promote health equity (see Acknowledgments). The University of Michigan granted institutional review board approval for this study on 24 January, 2013.
Data.
Data for the analyses described below were drawn from multiple sources. Demographic data were drawn from the 2009–2013 American Community Survey, aggregated over a 5-year period in keeping with ACS recommendation (U.S. Census Bureau, 2018, 2020). Mortality data were provided by the Michigan Department of Health and Human Services (MDHHS) and include records of all deaths that occurred in the Detroit metropolitan area (Wayne, Oakland, and Macomb Counties) between the 2009–2013 period. Information on fine particulate matter was drawn from the EPA’s National-Scale Fused Air Quality Surfaces Using Downscaling Tool and the Community Multiscale Air Quality (CMAQ) model, for the calendar years 2009–2013. The downscaler model combines air quality monitoring and modeling data to provide better fine-scale predictions of air pollutant levels at local and community scales (Berrocal, Gelfand, & Holland, 2010b, 2010a, 2012). Tests of this model indicate that predictions are better calibrated and offer improved predictive intervals compared with either Bayesian melding or ordinary kriging (Berrocal et al., 2010b). Additional information about the construction of CMAQ data is available from the EPA website (https://www.epa.gov/air-research/downscaler-model-predicting-daily-air-pollution): It is downloadable at the census tract level.
Measures.
All measures are constructed at the census tract level.
Dependent variable:
Age adjusted all-cause mortality at the census tract level. This variable is calculated using mortality data obtained from the MDHHS, as described above, and including all deaths from the DMA area during the period 2009–2013. Deaths were geocoded and linked to the census tract in which the decedent resided. Age adjusted all-cause mortality was calculated for each census tract by calculating age-specific mortality within the tract and multiplying it by the proportion of the total population in that age group, then summing across all age groups for each census tract (Curtin & Klein, 1995). This method adjusts for the different age structures of populations across census tracts. Age adjusted all-cause mortality is reported as deaths per 100,000 population. Because deaths are rare events, they can fluctuate over time: using broader periods of time will allow for more stable estimates. Therefore, we used the five-year average (2009–2013) to calculate the 2013 mortality rate at the census tract level (IOM, 1997), aligned with multi-year averaging used by prior ecological studies of area mortality (Erwin et al., 2010; Hutchinson et al., 2009).
Independent variables are listed here.
Percent Non-Hispanic Black (NHB), derived from American Community Survey (ACS) data (2009–2013), was measured as the percent of the total population in each census tract that identified as non-Hispanic Black or African American, which was used as a proxy for race-based residential segregation. Education was assessed as the percent of census tract residents aged 25 and older with less than high school education or Graduate Equivalency Degree (GED), drawing on ACS data, 2009–2013. Income was assessed as the percent of households in a census tract with incomes below the federal poverty level, 2009–2013 (Mooney, Richards, & Rundle, 2014). Income inequality was measured using the GINI coefficient (Kondo et al., 2009), derived from the ACS at the census tract level, 2009–2013 (U.S. Census Bureau, n.d.). Air pollution was assessed as PM2.5 concentration, calculated at the census tract level, using 2009–2013 PM2.5 24-hour annual average concentrations.
For each of the census tract level independent variables above, models were run using continuous variables, and also using scores calculated based on their percentile distribution, in quintiles ranging from 1 (<P20) to 5 (>P80). Each tract in the study area was rank ordered, and assigned a quintile score for each of the above variables using this ranking system. Quintiles were entered into the models using Q1 as the referent: A positive coefficient indicates that the value for the quintile in question is higher than for the referent, and a negative coefficient indicates that the value is lower than the referent. Results presented use the rank ordered quintiles, which allow for non-linear associations.
Analysis.
To estimate the extent to which education, poverty, income inequality and PM2.5 are (in)equitably distributed across census tracts by percent NHB, the cumulative proportion of the population, ordered by area-based percentages of racial concentration was plotted against the cumulative share of poverty, education, income inequality and PM2.5, respectively. In the case for which each population group has the same share of the impact of the environmental hazard or vulnerability, the curve coincides with the equality line. If the curve lies above the equality line, the inequality index is negative, indicating that more disadvantaged groups encounter greater environmental exposure or vulnerability burdens. If the curve lies below the equality line, then more advantaged groups carry a higher proportion of cumulative environmental exposure or vulnerability burdens. A summary measure of inequality is defined as twice the area between the curve and the equality line:
This measure gives a quantitative summary of inequality among groups. In order to assess the integral we used the “trapezoidal rule” (Atkinson, 1989) to approximate the region under the graph of the function e(s). The value of 0 is the lowest level of inequality where all groups have the same exposure to the variable of interest. When the inequality score is negative, it indicates that less advantaged groups bear a disproportionate burden of exposure: The highest level of inequality, where disadvantaged groups bear the burden of all the exposure is −1 (Kakwani, Wagstaff, & van Doorslaer, 1997).
To examine the independent and joint associations of indicators of social, economic and physical environments to all-cause mortality at the census tract level, we used the generalized estimating equation (GEE) modeling approach with identity link and exchangeable correlation matrix (Hardin & Hilbe, 2003; Liang & Zeger, 1986). This approach allows us to somewhat control the spatial clustering of the outcome with the appropriate selection of the block-exchangeable correlation matrix and thus any possible spatial correlations were then taken into account (Hardin & Hilbe, 2003; Zeger, Liang, & Albert, 1988).
Different model configurations were considered to assess the individual and multivariate associations between each independent variable and all-cause mortality. Models examine single-social factor-response and multi-social factor-response relationships. To assess the most correct specification of the models, in addition to additive models, we considered multiplicative models assessing interactions between independent variables data (Maddala & Lahiri, 2009). Although there were some statistically significant (p < 0.05) interaction terms, they were few in number and patterns were inconsistent. Based on these results, and assessment of the goodness of fit statistics (QIC and BIC), we were unable to conclude that the interaction models were a better fit than the main effect models. As a result, the final models reported in this paper report main effect models. To assess the sensitivity of models to varying specifications of the variables, we ran models using the rank-ordered quintile versions of each variable as described above and their binary versions using the third quartile as the threshold or cut point. Patterns were similar: Findings are reported using the rank-ordered quintile versions, 95% confidence intervals, and p-value for each coefficient of interest.
RESULTS
Table 1 shows descriptive statistics for each of the indicators included in the models. At the census tract level, the mean proportion of residents who identified as NHB was 29.7 (SD=36.9). The mean proportion of residents 25 and older with less than a high school education was 14.1 (SD=10.2). The mean proportion of households with incomes below the poverty line was 17.9 (SD=15.4), and the mean annual level of PM2.5 for census tracts in the DMA was 10.2 μg/m3 (SD = 0.4). The age-adjusted mean number of deaths per year at the census tract level was 648.5 (SD=235.9).
Table 1.
Descriptive Statistics for census tracts reporting mortality (n=1,141) in the Detroit Metropolitan Area (DMA)
| Measures | N | % | Mean | StdDev | Min | Max |
|---|---|---|---|---|---|---|
| (continuous) | ||||||
| All-cause mortality | 1141 | 648.5 | 235.9 | 113.0 | 1418.5 | |
| % Non-Hispanic Black (NHB) | 1141 | 29.7 | 36.9 | 0.0 | 100.0 | |
| % 25 years and older with <HS education | 1141 | 14.1 | 10.2 | 0.0 | 68.0 | |
| % below poverty | 1141 | 17.9 | 15.4 | 0.0 | 69.2 | |
| Gini Coefficient | 1141 | 0.4 | 0.1 | 0.0 | 0.7 | |
| PM25 concentration | 1141 | 10.2 | 0.4 | 9.2 | 10.8 | |
| (categorical) | ||||||
| %NHB, Quintiles | ||||||
| 1 | 229 | 20.1 | 0.0 | 1.7 | ||
| 2 | 229 | 20.1 | 1.7 | 4.8 | ||
| 3 | 229 | 20.1 | 4.8 | 14.8 | ||
| 4 | 229 | 20.1 | 14.8 | 83.6 | ||
| 5 | 225 | 19.7 | 83.6 | 100.0 | ||
| % 25 years and older with <HS education, Quintiles | ||||||
| 1 | 229 | 20.1 | 0.0 | 5.6 | ||
| 2 | 230 | 20.2 | 5.6 | 9.6 | ||
| 3 | 230 | 20.2 | 9.6 | 14.3 | ||
| 4 | 230 | 20.2 | 14.3 | 21.9 | ||
| 5 | 222 | 19.5 | 21.9 | 68.0 | ||
| % below poverty, Quintiles | ||||||
| 1 | 230 | 20.2 | 0.0 | 5.1 | ||
| 2 | 228 | 20.0 | 5.1 | 8.6 | ||
| 3 | 229 | 20.1 | 8.6 | 16.0 | ||
| 4 | 230 | 20.2 | 16.0 | 33.6 | ||
| 5 | 224 | 19.6 | 33.6 | 69.2 | ||
| Income inequality (GINI) (xl0) | ||||||
| 1 | 229 | 20.1 | 0.0 | 3.6 | ||
| 2 | 231 | 20.3 | 3.7 | 3.9 | ||
| 3 | 228 | 20.0 | 4.0 | 4.3 | ||
| 4 | 228 | 20.0 | 4.3 | 4.7 | ||
| 5 | 224 | 19.6 | 4.7 | 7.0 | ||
| PM2.5 Concentration, Quintiles | ||||||
| 1 | 231 | 20.2 | 9.2 | 9.9 | ||
| 2 | 230 | 20.2 | 9.9 | 10.3 | ||
| 3 | 333 | 29.2 | 10.3 | 10.5 | ||
| 4 | 124 | 10.9 | 10.5 | 10.5 | ||
| 5 | 223 | 19.5 | 10.5 | 10.8 | ||
As shown in Model 2, all-cause mortality rates were significantly greater for those residing in census tracts with larger proportions of adults who did not have a high school diploma, households below the poverty line (Model 3), and greater income inequality (Model 4), respectively. For education and income inequality, odds of mortality were significantly higher in each of quintiles 2–5 compared with mortality in the referent (lowest) quintile. For poverty, those in the 3rd (B=63.5, p=0.003) and 4th (B=62.6, p=0.003) quintiles showed comparable increases in all-cause mortality rates, while those in the 5th quintile experienced rates of all-cause mortality that were 114.6 per 100,000 population greater than those in the lowest poverty quintile (p=0.000).
Finally, for PM2.5, residents of census tracts in the second (B=142.6, p=0.000), third (B=156.1, p = 0.000), fourth (B= 183.2, p = 0.004), and fifth (B=206.5, p < 0.001) quintiles experienced significantly higher rates of all-cause mortality compared to residents of census tracts in the first quintile.
Table 3 presents results from analyses of inequality indices. Census tracts with higher percentage of NHB residents are significantly more likely to have a higher proportion of residents aged 25 and older who have not completed high school, to have a higher proportion of residents living below the poverty line, and to have higher proportions of high PM2.5 exposure. A trend toward greater income inequality in census tracts with a greater percentage of NHB residents was not statistically significant.
Table 3:
Significance tests of inequality in distribution of neighborhood poverty, education, income inequality, and PM2.5 by neighborhood racial composition in the Detroit Metropolitan Area (census tract n=1144)
| Index | 95%CI | ||
|---|---|---|---|
| Proportion over age 25 and older without high school completion | −0.437 | (−0.406,−0.467)*** | |
| Proportion residents living below poverty | −0.580 | (−0.536,−0.625)*** | |
| Census tract Percent | Proportion of residents living in neighborhood with high | ||
| Non-Hispanic Black | income inequality (GINI) | −0.410 | (−0.382,−0.438) |
| Proportion resident living in neighborhoods with high PM25 exposure | −0.485 | (−0.451,−0.52)*** | |
| Proportion residents living below poverty | −0.091 | (−0.08,−0.101)** |
These results are consistent with prior research that has demonstrated that areas with greater percentages of NHB residents have reduced education (Bennett, 2011; Reskin, 2012), higher rates of poverty (Krieger, Waterman, Gryparis, & Coull, 2015), and exposure to airborne pollutants (Jones et al., 2014; Krieger et al., 2015; Rice et al., 2014). Our next research question assessed the individual and joint contributions of racial composition, socioeconomic position and airborne particulate matter. Models including both poverty and education simultaneously were unstable. Examination of variance inflation factors (VIF) identified multicollinearity concerns for poverty (VIF=4.06). VIF for other variables did not approach levels of concern, with VIF =2.89 for education, and VIF< 2 for percent NHB, income inequality, and PM2.5. Thus models for which results are reported in Table 4 include percent NHB, percent of adults without a high school diploma, income inequality and PM2.5.
Table 4:
Census tract all cause mortality regressed on percent non-Hispanic Black, percent adult population with less than high school education, income inequality, and fine airborne particulate matter (PM2.5)
| Model 1 | Model 2 | Model 3 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable (Census tract quintiles, 1=ref) | Estimate | Stderr | 95%CI | p-value | Estimate | Stderr | 95%CI | p-value | Estimate | Stderr | 95%CI | p-value |
| Intercept | 608.3 | 14.4 | (580.1,636.5) | 0.000 | 527.5 | 20.1 | (488, 567) | <.0001 | 448.4 | 20.2 | (408.9 , 487.9) | <.0001 |
| Percent non-Hispanic Black | ||||||||||||
| 1 | Ref | Ref | Ref | |||||||||
| 2 | −7.2 | 21.5 | (−49.5, 35.0) | 0.737 | −16.7 | 20.8 | (−57.5, 24.2) | 0.424 | −29.4 | 19.9 | (−68.4 , 9.6) | 0.140 |
| 3 | 28.1 | 20.7 | (−12.4, 68.6) | 0.173 | 1.7 | 20.9 | (−39.3, 42.6) | 0.936 | −22.1 | 20.6 | (−62.4 , 18.2) | 0.283 |
| 4 | 40.8 | 21.3 | (−0.9, 82.5) | 0.055 | −8.8 | 23.3 | (−54.4, 36.8) | 0.706 | −36.5 | 23.5 | (−82.5 , 9.6) | 0.120 |
| 5 | 139.9 | 20.9 | (99.0,180.8) | 0.000 | 68.6 | 25.7 | (18.1,119.1) | 0.008 | 32.5 | 27.5 | (−21.3 , 86.3) | 0.237 |
| Percent >age 24 with <HS education | ||||||||||||
| 1 | Ref | Ref | ||||||||||
| 2 | 64.9 | 20.9 | (24,105.8) | 0.002 | 66.4 | 20.3 | (26.5 , 106.2) | 0.001 | ||||
| 3 | 117.0 | 20.4 | (77, 157.1) | <.0001 | 104.6 | 20.2 | (65.0, 144.1) | <.0001 | ||||
| 4 | 122.4 | 22.1 | (79.2, 165.7) | <.0001 | 102.4 | 23.5 | (56.4 , 148.4) | <.0001 | ||||
| 5 | 105.7 | 25.8 | (55.1, 156.3) | <.0001 | 87.3 | 27.9 | (32.6 , 141.9) | 0.002 | ||||
| Income Inequality (GINI Coefficient) | ||||||||||||
| 1 | Ref | Ref | ||||||||||
| 2 | 24.4 | 18.6 | (−12.1,60.9) | 0.190 | 24.5 | 17.5 | (−9.9 , 58.8) | 0.162 | ||||
| 3 | 38.4 | 21.1 | (−3, 79.8) | 0.069 | 40.9 | 20.3 | (1.1 , 80.7) | 0.044 | ||||
| 4 | 19.4 | 22.5 | (−24.7,63.5) | 0.388 | 28.5 | 21.9 | (−14.5 , 71.6) | 0.193 | ||||
| 5 | 69.7 | 24.9 | (21, 118.4) | 0.005 | 76.7 | 25.1 | (27.4 , 125.9) | 0.002 | ||||
| PM2.5 | ||||||||||||
| 1 | Ref | |||||||||||
| 2 | 144.6 | 20.4 | (104.5 , 184.7) | <.0001 | ||||||||
| 3 | 129.9 | 19.2 | (92.2 , 167.7) | <.0001 | ||||||||
| 4 | 115.2 | 26.2 | (63.8 , 166.5) | <.0001 | ||||||||
| 5 | 131.4 | 25.5 | (81.5 , 181.4) | <.0001 | ||||||||
Results presented in Table 4 show that initially significant positive associations between percent NHB and all-cause mortality (presented in Table 2 and replicated here in Model 1 for ease of comparison) are attenuated with the inclusion of education, income inequality and air quality variables. In Model 1, mortality rates in census tracts in the 4th (B=40.8, p=.055) and 5th (B=139.9, p<.001) quintiles of %NHB are greater than those in the 1st quintile. After accounting for socioeconomic indicators (percent high school completion, income inequality) in Model 2, mortality rates remain significant higher in census tracts in the 5th quintile for percent NHB (B=68.6, p=.008). In Model 3, which accounts for both socioeconomic and air pollutant indicators, mortality rates in census tracts in the 2nd (B=−29.4, p=0.140), 3rd (B=−22.1, p=0.283), 4th (B=−26.5.3, p=0.120) and 5th (B=32.5, p=0.237) quintile of percent NHB are not significantly different from those in the first quintile.
Table 2.
presents results from analyses examining the first research question: what are the associations between all-cause mortality and racial composition (percent NHB), socioeconomic status (percent of residents aged 25 and older without a high school education, percent below poverty, income inequality), and air pollution (PM2.5). In general, all-cause mortality increased for census tracts with greater proportions of NHB residents, greater proportions of residents with lower socioeconomic status, and census tracts with greater exposure to particulate matter. As shown in Model 1, residents of census tracts in the 4th and 5th quintile experienced 40.8 (p=0.055) and 139.9 (p=0.000) more deaths per 100,000 population, compared to those in the first quintile. Mortality rates in the 2nd and 3rd quintiles were not significantly different from those in the lowest quintile of NHB residents.
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable (Census tract quintiles, 1 =ref) | Estimate | Stderr | 95%CI | P− value | Estimate | Stdesrr | 95%CI | P−value | Estimate | Stderr | 95%CI | P− value | Estimate | Ssderr | 90%CI | P−value | Estimate | Stderr | 95%CI | P− value |
| Intercept | 608.3 | 14.4 | 1580.1636.5) | 0.000 | 550.1 | 13.8 | (523.577.1) | 0.00 | 592.1 | 15.2 | (562.3622) | 0.000 | 591.6 | 14.4 | (563.3619.8) | 0.000 | 513.8 | 13.1 | (488.1,39.5) | 0.000 |
| Percent non−Hispanic Black | ||||||||||||||||||||
| 1 | ref | |||||||||||||||||||
| 2 | −7.2 | 21.5 | (−49.5. 35.0) | 0.737 | ||||||||||||||||
| 3 | 28.1 | 20.7 | (−12.4. 68.6) | 0.173 | ||||||||||||||||
| 4 | 40.8 | 21.3 | (−0.9. 82.5) | 0.055 | ||||||||||||||||
| 5 | 139.9 | 20.9 | (99.0,180.8) | 0.000 | ||||||||||||||||
| Percent > age 24 with < HS education | ||||||||||||||||||||
| 1 | ref | |||||||||||||||||||
| 2 | 61.7 | 20.6 | (21.4,102.1) | 0.003 | ||||||||||||||||
| 3 | 122.0 | 20.0 | (82.9.161.1) | 0.000 | ||||||||||||||||
| 4 | 150.8 | 19.7 | (112.3, 189.4) | 0.000 | ||||||||||||||||
| 5 | 158.7 | 22.6 | (114.5, 202.9) | 0.000 | ||||||||||||||||
| Percent households below poverty | ||||||||||||||||||||
| 1 | ref | |||||||||||||||||||
| 2 | 41.8 | 21.3 | (0. 83. 5) | 0.050 | ||||||||||||||||
| 3 | 63.5 | 21.2 | (22.0, 105.0) | 0.003 | ||||||||||||||||
| 4 | 62.6 | 20.8 | (21.9,103.3) | 0.003 | ||||||||||||||||
| 5 | 114.6 | 23.5 | (68.5,160.8) | 0.000 | ||||||||||||||||
| Income Inequality | ||||||||||||||||||||
| 1 | ref | |||||||||||||||||||
| 2 | 39.3 | 19.4 | (1.4. 77.3) | 0.042 | ||||||||||||||||
| 3 | S9.2 | 21.7 | (16.7, 101.7) | 0.006 | ||||||||||||||||
| 4 | 65.8 | 20.8 | (25.0,106.6) | 0.002 | ||||||||||||||||
| 5 | 121.2 | 23.1 | (75.8,166.5) | 0.000 | ||||||||||||||||
| PM2.5 | ||||||||||||||||||||
| 1 | ref | |||||||||||||||||||
| 2 | 142.6 | 20.9 | (101.5, 183.6) | 0.000 | ||||||||||||||||
| 3 | 156.1 | 17.3 | (122.2, 190.0) | 0.000 | ||||||||||||||||
| 4 | 183.2 | 22.2 | (139.7, 226.6) | 0.000 | ||||||||||||||||
| 5 | 206.5 | 21.9 | (163.5, 249.5) | 0.000 | ||||||||||||||||
Associations between education and all-cause mortality are attenuated somewhat from results shown in Table 2, but remain statistically significant for each quintile. Rates of all-cause mortality are significantly higher in census tracts with greater proportions of adults who have not completed high school compared with those in the lowest quintile, as follows: 2nd (B=66.4, p=0.001), 3rd (B=104.6, p<0.001), 4th (B=102.4, p<0.001) and 5th (B=87.3, p=0.002) quintiles. Substantial overlap in the confidence intervals for quintiles 2–5 does not allow distinctions to be drawn across those quintiles.
In the full model, associations between income inequality and all-cause mortality remain in the expected direction, but are attenuated with the inclusion of other variables: 2nd (B=24.5, p=0.162) , 3rd (B=40.0, p=0.044), 4th (B=28.5, p=0.193) and 5th (B=76.7, p=0.002). As noted above, while quintiles 2–5 show rates of mortality that are significantly greater than the referent (quintile 1, lowest level of income inequality), the overlap in confidence intervals across quintiles 2–5 does not warrant distinctions across those quintiles. These results are generally consistent with the hypothesis that greater income inequality is associated with heightened all-cause mortality.
Finally, associations between exposure to PM2.5 and all-cause mortality remain statistically significant for each quintile, compared to those in the lowest quintile of exposure. Mortality rates in the 2nd (B=144.6, p<0.001), 3rd (B=129.9, p<0.001), 4th (B=115.2, p<0.001) and 5th (B=131.4, p<0.001) quintiles are significantly greater than those in the first quintile: These effects are evident after accounting for the effects of racial composition and socioeconomic indicators.
A formal test (MacKinnon, Fairchild, & Fritz, 2007) indicates that associations between percent NHB and all cause, all race mortality are fully attenuated in models including census tract level percentage over age 24 who have completed high school education or equivalent, income inequality and PM2.5 exposure (p<0.001) (results not shown).
DISCUSSION
Findings reported here indicate that census tract level racial composition, proportion of adults with less than a high school education, proportion of households below the poverty line, income inequality, and exposure to PM2.5 are each associated with age-adjusted all-cause, all-race mortality at the census tract level in bivariate models. Census tracts with higher proportions of NHB residents are disproportionately likely to have greater proportions of adults who have not completed high school, households with incomes below the poverty line, and higher levels of exposure to PM2.5. After accounting for census tract level indicators of education, income inequality and particulate matter, associations between census tract percent NHB and all-cause mortality are no longer statistically insignificant: Formal tests indicate that racial composition is attenuated in the full model. Associations between education, income inequality and fine particulate matter remain significant predictors of mortality in the full model. We discuss each of these findings below.
Percent non-Hispanic Black.
Our finding that the percent NHB at the census tract level was positively associated with all-cause mortality in bivariate models, and not significantly associated with all-cause mortality in multivariate models joins mixed findings reported previously in the literature (Bécares et al., 2012; Blanchard et al., 2004; Erwin et al., 2010; Hutchinson et al., 2009; Inagami et al., 2006; Jackson et al., 2000), and suggests the importance of guiding theoretical frameworks and controls for potential mediators in multivariate models. Specifically, our findings suggest that associations between percent NHB and all-cause mortality in bivariate models may be explained by heightened exposure to adverse socioeconomic contexts (circumscribed educational opportunities, poverty, income inequality) and physical environmental exposures (PM2.5). These patterns are consistent with the conceptual framework guiding this analysis, which suggests that the physical separation of NHBs in geographically distinct neighborhoods contributes to inequities in the distribution of opportunities for education and economic inequalities, shaping access to resources that are essential for the maintenance of health. Furthermore, associations between the racial composition of census tracts and levels of PM2.5 also suggest disproportionate exposure among residents of neighborhoods with high concentrations of NHB residents to physical environmental conditions that are inimical to health.
Results reported here suggest that excess mortality associated with the concentration of NHB residents at census tract level is attenuated by circumscribed access to educational opportunities and heightened exposure to air pollution. Previous studies using ecological models have reported mixed results, with some finding positive associations between racial composition and mortality (Erwin et al., 2010) and others reporting inverse associations between racial composition and black mortality (Hutchinson et al., 2009). Our finding of an initially significant association of percent NHB with all-cause, all-race mortality (Table 2) which is attenuated after inclusion of potential mediating pathways (socioeconomic indicators, environmental pollutants) suggests one potential reason for the mixed findings previously reported may be linked to the analytic and conceptual models that inform that previous work. The inclusion or exclusion of variables that represent potential mediating pathways may influence reported findings.
Furthermore, variations in findings across local areas may also reflect regional and local variations in the patterning of racial segregation and its implications. While ideologies of white supremacy are a national phenomenon, imbedded in national policies and practices, local expressions of those policies and practices, and local community responses to them may contribute to variations in patterns and outcomes. Specifically, associations between percent NHB and health outcomes may vary with the distribution of percent NHB, poverty characteristics (Kershaw et al., 2011), social characteristics of the neighborhood (e.g., social capital, histories of resistance and political organization) (Minkler & Freudenberg, 2010), and access to countervailing identities that may be health protective (Geronimus et al., 2016). These local variations may be obscured through the use of national datasets, as well as local datasets in which key variables may be unavailable, contributing to mixed findings reported in the literature. Close attention to local histories, contemporary political, social and economic dynamics, model specification and theoretical and empirical pathways is critical to development of a more nuanced understanding of these associations and pathways, as they emerge within local contexts. Such analyses can be importantly enhanced by engaging community residents and leaders in the process of framing and interpreting the research findings (Israel, Eng, Schulz, & Parker, 2013). Findings from the cross-sectional analyses reported here are consistent with the proposition that adverse associations between percent NHB and all-cause, all-race mortality in the DMA are mediated through socioeconomic indicators (e.g., education) and physical environmental exposures (e.g., air pollutants). Future studies using longitudinal analyses are warranted to more specifically assess mediation effects.
Socioeconomic Status.
The proportion of the population aged 24 and older with less than a high school education remained significantly associated with all-cause mortality in multivariate models accounting for racial composition, income inequality and PM2.5. The direction of associations between income inequality and all-cause mortality remained consistent although effect sizes were substantially attenuated in the full models. It is plausible that the associations between income inequality and all-cause mortality may be at least partially explained by other variables included in the model. For example, income inequality has been linked to widening gaps in educational achievement (Reardon, 2014). Individuals with low socioeconomic status who live in areas with higher income inequality are more likely to attend poorer resourced schools (Reardon, 2014) and drop out of high school, perhaps due to a perception that an investment in education will have a low economic return (Kearney & Levine, 2016). Income inequality has also been associated with lower levels of investment in public educational systems within poorer communities (Reardon, 2014). Such disinvestment in educational systems has been previously reported to be associated with lower educational attainment (Duncan & Murname, 2011) and linked with growing levels of income inequality resulting from this opportunity gap. Similarly, associations between income inequality and pollution have been documented (see Cushing, Morello-Frosch, Wander, & Pastor, 2015 for a recent review), with more equitable states (assessed variously as voter turnout, educational attainment, energy prices, employment opportunities) associated with reduced pollution (Boyce, Klemer, Templet, & Willis, 1999; Cushing et al., 2015; Templet, 1995). Further examination of associations among the mediating pathways posited in our conceptual model, for which this analysis provides some cross-sectional support, is warranted.
Particulate Matter.
Our finding that PM2.5 remains significantly associated with all-cause mortality in the full model is consistent with the hypothesis that PM2.5 exerts independent effects on health, above and beyond those captured with the social and economic indicators included in the models presented here. This finding is consistent with the conceptual model that underlies this analysis, which suggests that residents of more segregated neighborhoods are more likely to be exposed to toxic physical environments (in this case, operationalized as PM2.5), and that those exposures are associated with all-cause mortality even after accounting for racial composition and socioeconomic indicators. Thus, they suggest that race-based residential segregation operates not only through its impact on social and economic resources such as education and economic opportunities (reflected in income inequalities) but also through additional exposure to risk factors in the physical environment, such as heightened exposure to air pollutants.
Joint effects:
The results described above are derived from multivariate models that assess the joint effects of racial composition, socioeconomic indicators (educational attainment, income inequality) and exposure to air pollution. They begin to address the question of the extent to which these variables, which often cluster spatially, are independently and jointly associated with adverse health outcomes. Results reported here are consistent with the hypothesis that census tracts with higher concentrations of NHB residents experience higher levels of all-cause, all-race mortality. They also indicate that access to educational and economic resources are unequally distributed across census tracts in the DMA, with lower levels of educational attainment and higher levels of poverty in census tracts with higher concentrations of NHB residents. Similarly, exposure to poor air quality is unequally distributed, with higher levels of PM2.5 in census tracts with higher concentrations of NHB residents.
Multivariate models suggest that educational attainment, income inequality, and exposure to PM2.5 attenuate bivariate associations between racial composition and all-cause, all-race mortality. Further, significant associations between each of these pathways and mortality in the multivariate models suggest that each pathway may help to explain the initial associations between racial composition and mortality. These findings are consistent with the conceptual framework described above, and with literature linking segregation to adverse health outcomes through multiple mediating pathways.
Limitations: There are well known limitations of ecological analyses such as those used here, which examine data aggregated at the census tract level. These include what is commonly termed the ‘ecological fallacy’ in which relationships observed for populations or groups are interpreted as if they are true for individuals within that population (Levin, 2006). Results from the analyses reported here are interpretable as applicable to understanding population risk of mortality and should not be inferred to individual risk of mortality. In addition, the outcome used in this analysis of all-cause mortality for all racial groups combined does not examine, for example, specific causes of mortality or variations between racial groups on the impact of the factors considered.
Our use of cross-sectional analysis allows us to describe associations, including the attenuation of NHB associations with mortality, but does not allow causal attribution nor formal tests of mediation. The use of longitudinal models to more explicitly assess associations over time, lag times to mortality, and test mediational pathways will be critical next steps to more formally test the conceptual model presented in this paper.
There are several limitations of our use of percent non-Hispanic Black (NHB) as a proxy for race-based residential segregation. First, although it is easily operationalized, this measure does not account for the clustering of racial groups within census tracts (Kramer & Hogue, 2009). For example, a neighborhood that is 80% NHB means something different in a city that is 20% NHB compared to a city that is 79% NHB, such as Detroit. Commonly used measures of segregation such as the dissimilarity index and isolation index assess more specifically the distribution of racial groups within and across neighborhoods. A recent analysis reported significant correlations between percent NHB and black/white isolation, using the isolation index (Yang & Matthews, 2015). A second study reported significant associations between both racial composition and segregation measured using the dissimilarity index, and mortality (Nuru-Jeter & LaVeist, 2011), suggesting that these measures may capture different constructs. A second important criticism of the use of percent NHB is the failure to contextualize the measure within the larger area, that is, as an absolute, rather than a relative indicator of racial segregation. The conversion of raw percent NHB in our measure into an ordinal variable reflecting quintiles of census tract level percent NHB partially addresses this concern. Specifically, the lowest quintile (Q1) of our measure includes the 20% of all census tracts in the DMA with the smallest proportion of NHBs, ranging from 0.0%-1.7% NHB. The highest quintile (Q5) captures the 20% of rank ordered census tracts in the DMA with the highest proportion of NHB residents, ranging from 83.0–100.0% NHB. Thus, findings reported here reflect the associations with mortality of residing in census tracts within the DMA with relatively higher proportions of NHB residents, compared with those census tracts in the lowest 20% of percent NHB in the DMA. Finally, our focus in this paper on percent NHB does not account for effects of segregation of Hispanic or Latinx households in census tracts within the tri-county area. Several studies have found evidence of disproportionate exposure to pollutants among communities with higher proportions of Hispanic residents (Jones et al., 2014; Martenies, Milando, Williams, & Batterman, 2017). Further analyses examining segregation across multiple racial and ethnic groups would importantly extend this analysis.
This analysis used data aggregated over a 5-year period and is cross sectional rather than longitudinal. This methodology does not allow us to capture effects over time or to determine causality. Such temporal effects have been established through previous studies, and the cross-sectional techniques used in this analysis may underestimate health impacts that emerge over time as the effects of exposure accumulate (e.g. associations with cancer, which may become visible over longer time periods than are captured in our analysis). In that regard, these estimates may be conservative. The strength of the analytic method lies in its ability to capture geographic variation of multiple variables with variant units of analysis, and is described in greater detail in the “Strengths” section that follows.
Given limitations of available data, we are unable to specifically include potentially protective pathways or mechanisms in the models, for example, measure of social capital or social support. Given protective effects of social cohesion reported elsewhere (Bécares, Nazroo, & Stafford, 2009; Hutchinson et al., 2009), future studies assessing positive social relationships as potential pathways linking racial or ethnic density to reduced mortality are critical to understanding local variations in associations between racial composition and health outcomes.
Our measure of PM was derived from downscaler models with estimates linked to census tracts. The use of aggregated data over a five-year period obscures temporal variations in the data that are likely linked to variations in mortality. Modeled data used for these estimates is derived from data captured by monitors at specific locations, and is affected by uncertainty in the estimates. Finally, PM2.5 is just one of many potential physical environmental risk factors to which residents of racially segregated communities may be disproportionately exposed. Others include excess exposure to lead through disproportionate older or poorly maintained housing stock, toxics through increased proximity to hazardous land uses, and poor-quality infrastructure (e.g., sidewalk maintenance), documented extensively in the literature. As a result of these limitations in our measure of physical environmental exposures, the findings reported here are likely conservative.
Strengths.
Despite the limitations of ecological studies described above, there is increasing recognition that population level studies play an important role in studying important public health problems, particularly for problems that operate at the population level (Levin, 2006; Pearce, 2000; Susser, 1994). As argued by Geoffrey Rose (2001) in his classic work on the determinants of population rates, as opposed to determinants of individual cases, it is essential to study the characteristics of populations rather than the characteristics of individuals in order to understand mechanisms of intervention with the potential to shift the mean risk for the group, rather than simply affecting individual risk factors (Rose, 2001). A further strength of the ecological analyses presented here is that they may be well-suited to development of policy recommendations that mitigate population level, rather than individual level risks, or maximize population level benefits.
Our focus in this analysis is on geographic variations in multiple social, economic and physical environmental exposures - what has been termed a “riskscape” (Morello-Frosch & Shenassa, 2006) - and their associations with the geographic patterning of mortality outcomes. The methodology used in this analysis, adapted from Su and colleagues (2009), does not lend itself to interpretation of point estimates per unit of change. Rather, its strength lies in the transformation of measures captured with very different units (e.g., percent below poverty, microns per cubic meter for air pollution) into quintiles distributed over a common geographic region. It allows for analysis of the relative distribution of risk across multiple indicators within a defined geographic area (the DMA) and the independent and joint contributions of those variations in relative risk to variations in mortality.
To our knowledge, this is one of only a handful of papers that have examined multiple characteristics of neighborhoods both individually and collectively, using models that examine their unique contributions to mortality. In doing so, they enable identification of potential mediating pathways and also help to discern potential points of population level intervention that can be useful in identifying priorities for public health intervention and policy change. In the multivariate model presented here (Table 4), indicators of socioeconomic variation (education, income inequality) and exposure to PM2.5 retain consistent and statistically significant associations with all-cause mortality, suggesting that interventions to improve educational access and success, reduce income inequality, and interventions to reduce PM2.5 have the potential to yield substantial population level reductions in mortality. The findings reported here suggest that, in this DMA analysis, reduced access to education and excess exposure to air pollutants in areas with higher concentrations of NHB residents, substantially attenuate initially observed cross-sectional associations between census tract racial composition and mortality. These findings suggest the importance of further, longitudinal analyses to further examine these associations, and suggest health benefits of efforts to address the maldistribution of educational opportunities and environmental exposures in communities of color.
IMPLICATIONS
In 2001, David Williams and Chiquita Collins (2001) suggested that race-based residential segregation be considered a fundamental cause of health inequities between racial groups, and outlined multiple pathways through which such segregation may contribute to disparities in health outcomes. They concluded that public health interventions focused on reducing racial inequities in health should focus on elimination of race-based residential segregation, or on eliminating the effects of such segregation on access to resources (Williams & Collins, 2001). Our finding that, after accounting for socioeconomic and physical environmental characteristics of neighborhoods, the positive association between proportion NHB residents and mortality is no longer statistically significant joins a body of evidence suggesting that economic divestment and environmental exposures in segregated communities contribute to excess mortality. These results suggest that adverse impacts of race-based residential segregation travel, in part, through impacts of divestment in predominantly black communities for educational and economic opportunities, as well as through the disproportionate exposure of NHB communities to noxious physical environments such as high concentrations of PM2.5.
Writing over a decade ago, Frohlich and Potvin (2008) described what they called the “inequality paradox”, in which well-intentioned efforts to improve population health may inadvertently contribute to increases in health disparities as more privileged or well-resourced communities benefit disproportionately compared to structurally marginalized communities. As a result, these population health interventions can inadvertently serve to increase health inequities. One example is the Clean Air Act, passed in the 1970s, which has led to overall reductions in national levels of air pollutants and associated mortality (Holladay, 2011). However, substantial evidence indicates that, despite these overall reductions in air pollution, communities of color and low income communities remain disproportionately exposed to, and adversely affected by, air pollution and associated health impacts (Ruffin, 2011; Schulz et al., 2018). The inequality paradox, then, is that despite overall reductions in mortality attributable to the Clean Air Act, substantial inequalities in exposure and health remain.
To address this paradox, Frohlich and Potvin suggest that interventions must also recognize and address factors that place marginalized populations “at risk of risk.” Such efforts may include, for example, investments in public education in order to promote educational and economic equity, and to reduce income inequality while simultaneously working to reduce the inequitable distribution of air pollutants. Additional strategies include addressing race-based housing discrimination as a fundamental driver of racial segregation (Sharkey, 2013), reducing income inequalities (e.g. increases in minimum wage), and promoting more equitable political and economic power to influence land use decisions.
Recognizing that segregation, housing and lending policies in the 20th century were fundamental drivers of today’s inequalities in income, education and wealth (Mitchell & Franco, 2018), substantive and concerted efforts to address the contemporary effects of those policies are necessary components of efforts to attain health equity. Examples include community driven community reinvestment strategies that focus on schools, community-based organizations and other anchor institutions located in predominantly Black and Brown areas, which remain more subject to economic inequality (Mitchell and Franco, 2018). It is critical that local development be driven by community insights, values and priorities in order to most effectively address poverty and racism, and avoid unanticipated effects such as gentrification and displacement (National Academies of Sciences Engineering and Medicine, 2017). Specific efforts to address excess exposure to air pollutants in predominantly non-Hispanic Black and Hispanic communities are also essential. Such efforts must be community led (Heaney, Wilson, & Wilson, 2007), and supported with legal, economic and other resources beyond the community, with explicit attention to strategies that avoid, for example, green gentrification and the displacement of current residents as neighborhoods become more desirable to more affluent individuals (Rigolon & Christiansen, 2019). Evidence that countries and states with greater political and economic equity in general generate lower levels of pollution, with more equitable distribution of pollutants, suggest the importance of continued vigilance to protect voting rights and the power to influence land use and other decisions affecting the health and well-being of low income communities and communities of color (Cushing et al., 2015; Wilson, Hutson, & Mujahid, 2008). These and related strategies to promote political, racial and economic equity offer critical pathways toward social and environmental justice and more equitable health outcomes.
White supremacy is a political, economic and cultural system that rests upon the systematic devaluation of Black and Brown lives (Ansley, 1997). We have argued here that it underlies the creation and maintenance of racially segregated communities, economic disinvestment from those communities, and permitting of the emission of excess pollutants affecting those communities. As such, efforts to reduce racial and ethnic health inequities must address ideologies of white racial superiority imbedded in legal codes, development and permitting processes, policing, and decisions about the geographic distribution of investment in public infrastructure (Rothstein, 2017). These ideologies fundamentally determine the distribution of risk that results in the unnecessary and unjust deaths of thousands of Black and Brown Americans annually (Thakrar, Forrest, Maltenfort, & Forrest, 2018) and must be addressed if we are to attain racial, ethnic and socioeconomic equity in health.
Highlights:
Previous studies have demonstrated associations between race-based residential segregation, neighborhood socioeconomic and physical environmental characteristics, and mortality. Few studies have examined independent and joint effects of these multiple neighborhood characteristics and mortality, including potential mediating pathways.
We find significant associations between census tract race-based residential segregation (operationalized as percent non-Hispanic Black), education (percent with graduate equivalency degree), poverty (percent below poverty), air pollution (ambient PM2.5) and age adjusted all-cause, all race mortality (henceforth all cause mortality) , in the Detroit Metropolitan Area. Income inequality was not significantly associated with race-based residential segregation.
In multivariate models, education, income inequality and PM2.5 fully attenuated associations between racial composition and all-cause mortality.
Results are consistent with the hypothesis that race-based residential segregation is associated with heightened all-cause mortality, and that those effects are mediated by education, income inequality, and exposure to air pollution at the census tract level.
Public health and cross-sector interventions to eliminate race-based residential segregation or to eliminate the maldistribution of educational and economic resources, and environmental exposures, across census tracts could substantially reduce regional inequities in all-cause mortality.
ACKNOWEDGEMENTS
We thank the members of the CAPHE Steering Committee for their contributions to the work presented here, including representatives from: Community Action Against Asthma (CAAA), the Detroit Healthy Environments Partnership (www.hepdetroit.org), the Detroit Community-Academic Urban Research Center (www.detroiturc.org), Detroit Hispanic Development Corporation, Detroit Future Cities, Detroiters Working for Environmental Justice, Green Door Initiative, Michigan Department of Environmental Quality, Sierra Club Detroit, Southwest Detroit Environmental Vision, Southwest Detroit Community Benefits Coalition, University of Michigan School of Public Health, and the Wayne State University Transnational Environmental Law Clinic. The study and analysis were supported by the National Institute of Environmental Health Sciences (NIEHS) (R01 ES022616 and P30ES017885) and the Fred A. and Barbara M. Erb Family Foundation. The results presented here are solely the responsibility of the authors and do not necessarily represent the views of NIEHS, its directors, officers, or staff. We thank our funders for support for this manuscript. Finally, we acknowledge those whose seminal work on race and environment have paved the way for this research, including W. E. B. Du Bois and the United Church of Christ Justice and Witness Ministries (UCC), Toxic Wastes and Race at Twenty, 1987-2007 (Bullard, Mohai, Saha, & Wright, 2007).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: None
REFERENCES
- 2015 Data Release New and Notable. (2016). Retrieved August 24, 2017, from https://www.census.gov/programs-surveys/acs/news/data-releases/2015/release.html
- Adamkiewicz G, Spengler JD, Harley AE, Stoddard A, Yang M, Alvarez-Reeves M, & Sorensen G (2014). Environmental conditions in low-income urban housing: Clustering and associations with self-reported health. American Journal of Public Health, 104(9), 1650–1656. 10.2105/AJPH.2013.301253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez HAO, Appleton AA, Fuller CH, Belcourt A, & Kubzansky LD (2018). An Integrated Socio-Environmental Model of Health and Well-Being: A Conceptual Framework Exploring the Joint Contribution of Environmental and Social Exposures to Health and Disease Over the Life Span. Current Environmental Health Reports, 1–11. [DOI] [PubMed] [Google Scholar]
- Andersen SW, Blot WJ, Shu X-O, Sonderman JS, Steinwandel M, Hargreaves MK, & Zheng W (2018). Associations between neighborhood environment, health behaviors, and mortality. American Journal of Preventive Medicine, 54(1), 87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annie E Casey Foundation. (2015). Kids Count Data Book.
- Ansley FL (1997). White Supremacy (And What We Should Do About It) In Delgado R & Stefancic J (Eds.), Critical White Studies: Looking Behind the Mirror (pp. 592–595). Philadelphia, PA: Temple University Press. [Google Scholar]
- Atkinson KE (1989). An Introduction to Numerical Analysis (2nd ed.). John Wiley and Sons, Inc. [Google Scholar]
- Bécares L, Nazroo J, & Stafford M (2009). The buffering effects of ethnic density on experienced racism and health. Health & Place, 15, 700–708. [DOI] [PubMed] [Google Scholar]
- Bécares L, Shaw R, Nazroo J, Stafford M, Albor C, Atkin K, … Pickett K (2012). Ethnic Density Effects on Physical Morbidity, Mortality, and Health Behaviors: A Systematic Review of the Literature. American Journal of Public Health, 102(12), e33–e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell J, & Lee MM (2011). Impacting health through a focus on race and place. Oakland, CA: Retrieved from https://www.policylink.org/sites/default/files/WHY_PLACE_AND_RACEMATTER_FULLREPORT_WEB.PDF [Google Scholar]
- Bennett PR (2011). The relationship between neighborhood racial concentration and verbal ability: An investigation using the institutional resources model. Social Science Research, 40, 1124–1141. 10.1016/j.ssresearch.2011.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrocal VJ, Gelfand AE, & Holland DM (2010a). A bivariate space-time downscalar under space and time misalignment. Ann. Appl. Stat, 4, 1942–1975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrocal VJ, Gelfand AE, & Holland DM (2010b). A spatiotemporal downscaler for output from numerical models. J. Agric. Biol. Environ. Stat, 15, 176–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrocal VJ, Gelfand AE, & Holland DM (2012). Space-Time Data Fusion Under Error in Computer Model Output: An Application to Modeling Air Quality. Biometrics, 68, 837–848. 10.1111/j.1541-0420.2011.01725.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard TC, Cossman JS, & Levin ML (2004). Multiple Meanings of Minority Concentration: Incorporating Contextual Explanations into the Analysis of Individual-Level U.S. Black Mortality Outcomes. Population Research and Policy Review, 23(3), 309–326. [Google Scholar]
- Boyce JK, Klemer AR, Templet PH, & Willis CE (1999). Power distribution, the environment, and public health: a state-level analysis. Ecol. Econ, 29, 127–140. [Google Scholar]
- Brook RD, Rajagopalan S, Pope CA, Brook JR, Bhatnagar A, Diez-Roux AV, … Kaufman JD (2010). Particulate Matter Air Pollution and Cardiovascular Disease: An Update to the Scientific Statement From the American Heart Association. Circulation, 121(21), 2331–2378. 10.1161/CIR.0b013e3181dbece1 [DOI] [PubMed] [Google Scholar]
- Bullard RD, Mohai P, Saha R, & Wright B (2007). Toxic Wastes and Race at Twenty 1987–2007: A Report Prepared for the United Church of Christ Justice & Witness Ministries. [Google Scholar]
- Callahan MA, Bender ES, Bollweg GL, Dellarco VL, Delpire VL, Halper MP, … Victery W (2003). Framework for Cumulative Risk Assessment. Washington, D.C. [Google Scholar]
- Camacho-Rivera M, Kawachi I, Bennett GG, & Subramanian SV (2014). Associations of Neighborhood Concentrated Poverty, Neighborhood Racial/Ethnic Composition, and Indoor Allergen Exposures: a Cross-Sectional Analysis of Los Angeles Households, 2006–2008. Journal of Urban Health : Bulletin of the New York Academy of Medicine, 91(4), 661–676. 10.1007/s11524-014-9872-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles CZ (2003). The Dynamics of Racial Residential Segregation. Annual Review of Sociology, 29, 167–207. [Google Scholar]
- Clark NM, Quinn M, Dodge JA, & Nelson BW (2014). Alliance system and policy change: Necessary ingredients for improvement in diabetes care and reduction of disparities. Health Promotion Practice, 15(2 Suppl), 11S–22S. 10.1177/1524839914543829 [DOI] [PubMed] [Google Scholar]
- Collins TW, Grineski SE, Chakraborty J, Montgomery MC, & Hernandez M (2015). Downscaling Environmental Justice Analysis: Determinants of Household-Level Hazardous Air Pollutant Exposure in Greater Houston. Annals of the Association of American Geographers, 105(4), 684–703. [Google Scholar]
- Commission on the Social Determinants of Health. (2008). Closing the gap in a generation: Health equity through action on the social determinants of health Geneva. Retrieved from https://www.who.int/social_determinants/thecommission/finalreport/en/ [Google Scholar]
- Curtin LR, & Klein RJ (1995). Age Adjusted Death Rates (DHHS Publication No. (PHS) 95–1237). Retrieved from https://www.cdc.gov/nchs/data/statnt/statnt06rv.pdf [PubMed]
- Cushing L, Morello-Frosch R, Wander M, & Pastor M (2015). The haves, the have-nots, and the health of everyone: The relationship between social inequality and environmental quality. Annual Review of Public Health, 36, 193–209. [DOI] [PubMed] [Google Scholar]
- Dankwa-Mullan I, Rhee KB, Williams K, Sanchez I, Sy FS, Stinson N Jr., & Ruffin J (2010). The science of eliminating health disparities: Summary and analysis of the NIH summit recommendations. American Journal of Public Health, 100(S1), S12–S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denney JT, Saint Onge JM, & Dennis JA (2018). Neighborhood concentrated disadvantage and adult mortality: insights for racial and ethnic differences. Popul Res Policy Rev, 37, 301–321. [Google Scholar]
- Dinwiddie GY, Gaskin DJ, Chan KS, Norrington J, & McCleary R (2013). Residential segregation, geographic proximity and type of services used: Evidence for racial/ethnic disparities in mental health. Social Science & Medicine, 80, 67–75. 10.1016/j.socscimed.2012.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Bois WEB (1899). The Philadelphia Negro: A Social Study. Philadelphia, PA: The University of Pennsylvania. [Google Scholar]
- Duncan GJ, & Murname RJ (2011). Whither Opportunity: Rising inequality, schools and children’s life chances New York, NY: Russell Sage Foundation. [Google Scholar]
- Erwin PC, Fitzhugh EC, Brown KC, Looney S, & Forde T (2010). Health Disparities in Rural Areas: The Interaction of Race, Socioeconomic Status, and Geography. Journal of Health Care for the Poor and Underserved, 21(3), 931–945. [DOI] [PubMed] [Google Scholar]
- Evans GW, & Kantrowitz E (2002). Socioeconomic Status and Health: The Potential Role of Environmental Risk Exposure. Annual Review of Public Health, 23, 303–331. [DOI] [PubMed] [Google Scholar]
- Evans GW, & Kim P (2010). Multiple risk exposure as a potential explanatory mechanism for the socioeconomic status-health gradient. Annals of the New York Academy of Sciences, 1186, 174–189. 10.1111/j.1749-6632.2009.05336 [DOI] [PubMed] [Google Scholar]
- Fan J, Li S, Fan C, Bai Z, & Yang K (2016). The impact of PM2.5 on asthma emergency department visits: A systematic review and meta-analysis. Environmental Science and Pollution Research International, 23(1), 843–850. 10.1007/s11356-015-5321-x [DOI] [PubMed] [Google Scholar]
- Fann N, Lamson AD, Anenberg SC, Wesson K, Risley D, & Hubbell BJ (2012). Estimating the national public health burden associated with exposure to ambient PM2.5 and ozone. Risk Analysis, 32(1), 81–95. 10.1111/j.1539-6924.2011.01630.x [DOI] [PubMed] [Google Scholar]
- Farley R (2011). The Waning of American Apartheid? Contexts, 10(3), 36–43. 10.1177/1536504211418452 [DOI] [Google Scholar]
- Farley R (2015). The Bankruptcy of Detroit: What Role Did Race Play? City & Community, 14(2), 118–137. 10.1111/cico.12106 [DOI] [Google Scholar]
- Farley R, Danziger S, & Holzer HJ (2000). Detroit Divided. New York, NY: Russell Sage Foundation. [Google Scholar]
- Forno E, & Celedon JC (2009). Asthma and ethnic minorities: Socioeconomic status and beyond. Current Opinion in Allergy and Clinical Immunology, 9(2), 154–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frohlich KL, & Potvin L (2008). Transcending the known in public health practice: The inequality paradox: The population approach and vulnerable populations. American Journal of Public Health, 98(2), 216–221. 10.2105/AJPH.2007.114777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fry R, & Taylor P (2012). The Rise of Residential Segregation by Income. [Google Scholar]
- Gehring U, Gruzieva O, Agius RM, Beelen R, Custovic A, Cyrys J, … Brunekreef B (2013). Air Pollution Exposure and Lung Function in Children: The ESCAPE Project. Environmental Health Perspectives, 121(11–12), 1357–1364. 10.1289/ehp.1306770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, James SA, Destin M, Graham LA, Hatzenbuehler ML, Pearson JA, … Thompson JP (2016). Jedi Public Health: Co-Creating an Identity-Safe Culture to Promote Healthy Equity. SSM Popul Health, 2, 105–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray SC, Edwards SE, & Miranda ML (2013). Race, socioeconomic status, and air pollution in North Carolina. Environmental Research, 126, 152–158. 10.1016/j.envres.2013.06.005 [DOI] [PubMed] [Google Scholar]
- Haley DF, Linton S, Luo R, Hunter-Jones J, Adimora AA, Wingood GM, … Cooper HL (2017). Public Housing Relocations and Relationships of Changes in Neighborhood Disadvantage and Transportation Access to Unmet Need for Medical Care. Journal of Health Care for the Poor and Underserved, 28(1), 315–328. 10.1353/hpu.2017.0026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardin J, & Hilbe J (2003). Generalized Estimating Equations. London: Chapman and Hall/CRC. [Google Scholar]
- Heaney CD, Wilson SMM, & Wilson OR (2007). The West End Revitalization Association’s Community-Owned and -Managed Research Model: Development Implementation, and Action. Progress in Community Health Partnerships: Research, Education, and Action, 1(4). 10.1353/cpr.2007.0037 [DOI] [PubMed] [Google Scholar]
- Holladay JS (2011). Valuing the Clean Air Act: How Do We Know How Much Clean Air is Worth? [Google Scholar]
- Huang G, & London J (2012). Mapping cumulative effects, social vulnerability, and health in the San Joaquin Valley, California. American Journal of Public Health, 102(5), 830–832. 10.2105/AJPH.2011.300466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchinson RN, Putt MA, Dean LT, Long JA, Montagnet CA, & Armstrong K (2009). Neighborhood racial composition, social capital, and black all-cause mortality in Philadelphia. Social Science & Medicine, 68, 1859–1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inagami S, Borrell LN, Wong MD, Fang J, Shapiro MF, & Asch SM (2006). Residential Segregation and Latino, Black, and White Mortality in New York City. Journal of Urban Health : Bulletin of the New York Academy of Medicine, 83(3), 406–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel BA, Eng E, Schulz AJ, & Parker E (Eds.). (2013). Methods for Community-Based Participatory Research for Health. San Francisco: Jossey-Bass. [Google Scholar]
- Jackson SA, Anderson RT, Johnson NJ, & Sorlie PD (2000). The Relation of Residential Segregation to All-Cause Mortality: A Study in Black and White. American Journal of Public Health, 90(4), 615–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs DE (2011). Environmental Health Disparities in Housing. American Journal of Public Health, 101(S1), S115–S122. 10.2105/AJPH.2010.300058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jargowsky PA (2015). Architecture of segregation: Civil unrest: the concentration of poverty, and public policy. Retrieved from https://tcf.org/content/report/architecture-of-segregation/
- Jerrett M, Burnett RT, Beckerman BS, Turner MC, Krewski D, Thurston G, … Pope CA (2013). Spatial analysis of air pollution and mortality in California. American Journal of Respiratory and Critical Care Medicine, 188(5), 593–599. 10.1164/rccm.201303-0609OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johannson KA, Vittinghoff E, Lee K, Balmes JR, Ji W, Kaplan GG, … Collard HR (2014). Acute exacerbation of idiopathic pulmonary fibrosis associated with air pollution exposure. European Respiratory Journal, 43(4), 1124–1131. 10.1183/09031936.00122213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones MR, Diez-Roux AV, Hajat A, Kershaw K, O’Neill MS, Guallar E, … Navas-Acien A (2014). Race/Ethnicity, Residential Segregation, and Exposure to Ambient Air Pollution: The Multi-Ethnic Study of Atherosclerosis (MESA). American Journal of Public Health, 104(11), 2130–2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakwani N, Wagstaff A, & van Doorslaer E (1997). Socioeconomic inequalities in health: Measurement, computation, and statistical inference. Journal of Econometrics, 77(1), 87–103. 10.1016/S0304-4076(96)01807-6 [DOI] [Google Scholar]
- Kearney MS, & Levine PB (2016). Income inequality, social mobility, and the decision to drop out of high school. Brookings Papers on Economic Activity, 333–380. [Google Scholar]
- Kelishadi R, & Poursafa P (2010). Air pollution and non-respiratory health hazards for children. Archives of Medical Science, 6(4), 483–495. 10.5114/aoms.2010.14458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendi IX (2017). Stamped from the Beginning: The Definitive History of Racist Ideas in America. New York, NY: Bold Type Books. [Google Scholar]
- Kershaw KN, Diez-Roux AV, Burgard SA, Lisabeth LD, Mujahid MS, & Schulz AJ (2011). Metropolitan-level Racial Residential Segregation and Black-White Disparities in Hypertension. Am J Epidemiol, 174(5), 537–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby JB, & Kaneda T (2005). Neighborhood socioeconomic disadvantage and access to health care. Journal of Health and Social Behavior, 46(1), 15–31. 10.1177/002214650504600103 [DOI] [PubMed] [Google Scholar]
- Kondo N, Sembajwe G, Kawachi I, van Dam RM, Subramanian SV, & Yamagata Z (2009). Income inequality, mortality, and self rated health: meta-analysis of multilevel studies. BMJ, 339(7731), 1178–1181. 10.1136/bmj.b4471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer MR, & Hogue CR (2009). Is Segregation Bad for Your Health? Epidemiologic Reviews, 31(1), 178–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Waterman PD, Gryparis A, & Coull BA (2015). Black carbon exposure, socioeconomic and racial/ethnic spatial polarization, and the Index of Concentration at the Extremes (ICE). Health & Place, 34, 215–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist T, Pollack K, Thorpe R, Fesahazion R, & Gaskin D (2011). Place, not race: Disparities dissipate in southwest Baltimore when blacks and whites live under similar conditions. Health Affairs, 30(10), 1880–1887. 10.1377/hlthaff.2011.0640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeClere F, Rogers R, & Peters K (1997). Ethnicity and mortality in the United States: individual and community correlates. Social Forces, 76(1), 169–198. [Google Scholar]
- Lepeule J, Laden F, Dockery D, & Schwartz J (2012). Chronic exposure to fine particles and mortality: An extended follow-up of the Harvard Six Cities study from 1974–2009. Environmental Health Perspectives, 120(7), 965–970. 10.1289/ehp.1104660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin KA (2006). Study design VI - Ecological Studies. Evidence-Based Dentistry, 7(4), 108. [DOI] [PubMed] [Google Scholar]
- Li S, Batterman S, Wasilevich E, Wahl R, Wirth J, Su F, & Mukherjee B (2011). Associations of daily asthma emergency department visits and hospital admissions with ambient air pollutants among the pediatric Medicaid population in Detroit: Time-series and time-stratified case-crossover analyses with threshold effects. Environmental Research, 111(8), 1137–1147. 10.1016/j.envres.2011.06.002 [DOI] [PubMed] [Google Scholar]
- Liang K-L, & Zeger S (1986). Longitudinal data analysis using generalized linear models. Biometrika, 73(1), 13–22. 10.1093/biomet/73.1.13 [DOI] [Google Scholar]
- Logan JR, Minca E, & Adar S (2012). The Geography of Inequality: Why Separate Means Unequal in American Public Schools. Sociology of Education, 85 10.1177/0038040711431588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, & Fritz MS (2007). Mediation Analysis. Annual Review of Psychology, 58, 593–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddala GS, & Lahiri K (2009). Diagnostic checking, model selection, and specification testing In Introduction to Econometrics (Fourth, pp. 401–449). Wiley. [Google Scholar]
- Markevych I, Schoierer J, Hartig T, Chudnovsky A, Hystad P, Dzhambov AM, … Fuertes E (2017). Exploring pathways linking greenspace to health: Theoretical and methodological guidance. Environmental Research, 158, 301–317. 10.1016/j.envres.2017.06.028 [DOI] [PubMed] [Google Scholar]
- Martenies SE, Milando CW, Williams GO, & Batterman SA (2017). Disease and Health Inequalities Attributable to Air Pollutant Exposure in Detroit, Michigan. Int J Environ Res Public Health, 14(10), 1243 10.3390/ijerph14101243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey DS, Gross AB, & Eggers ML (1991). Segregation, the concentration of poverty, and the life chances of individuals. Social Science Research, 20(4), 397–420. 10.1016/0049-089X(91)90020-4 [DOI] [Google Scholar]
- Meijer M, Röhl J, Bloomfield K, & Grittner U (2012). Do neighborhoods affect individual mortality? A systematic review and meta-analysis of multilevel studies. Social Science & Medicine, 74(1204–1212). [DOI] [PubMed] [Google Scholar]
- Minkler M, & Freudenberg N (2010). From Community-Based Participatory Research to Policy Change. In Burack C, Seifer SD, & Fitzgerald HE (Eds.), Handbook of Engaged Scholarship: Contemporary Landscapes, Future Directions: Volume 2: Community-Campus Partnerships (pp. 275–294). Michigan State University Press. [Google Scholar]
- Mitchell B, & Franco J (2018). Segregation and Economic Inequality. [Google Scholar]
- Mode NA, Evans MK, & Zonderman AB (2016). Race, Neighborhood Economic Status, Income Inequality and Mortality. PLOS ONE, 11(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohai P, Lantz PM, Morenoff J, House JS, & Mero RP (2009). Racial and socioeconomic disparities in residential proximity to polluting industrial facilities: Evidence from the Americans’ Changing Lives Study. American Journal of Public Health, 99(S3), S649–S656. 10.2105/AJPH.2007.131383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney SJ, Richards CA, & Rundle AG (2014). There Goes the Neighborhood Effect: Bias Owing to Nondifferential Measurement Error in the Construction of Neighborhood Contextual Measures. Epidemiology, 25(4), 528–535. 10.1097/eDe.0000000000000113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morello-Frosch R, & Jesdale BM (2006). Separate and Unequal: Residential Segregation and Estimated Cancer Risks Associated with Ambient Air Toxics in U.S. Metropolitan Areas. Environmental Health Perspectives, 114(3), 386–393. 10.1289/ehp.8500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morello-Frosch R, & Shenassa ED (2006). The environmental “riskscape” and social inequality: implications for explaining maternal and child health disparities. Environ Health Perspect, 114(8), 1150–1153. https://doi.org/doi: 10.1289/ehp.8930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moretto A, Bachman A, Boobis A, Solomon KR, Pastoor TP, Wilks MF, & Embry MR (2016). A framework for cumulative risk assessment in the 21st century. Critical Reviews in Toxicology, 47(2), 85–97. 10.1080/10408444.2016.1211618 [DOI] [PubMed] [Google Scholar]
- Mujahid MS, Diez-Roux AV, Morenoff JD, Raghunathan TE, Cooper RS, Ni H, & Shea S (2008). Neighborhood characteristics and hypertension. Epidemiology, 19(4), 590–598. [DOI] [PubMed] [Google Scholar]
- Nam KM, Selin NE, Rielly JM, & Paltsev S (2010). Measuring welfare loss caused by air pollution in Europe: A CGE analysis. Energy Policy, 38(9), 5059–5071. 10.1016/j.enpol.2010.04.034 [DOI] [Google Scholar]
- National Academies of Sciences Engineering and Medicine. (2017). Communities in Action: Pathways to Health Equity. (Weinstein N, Geller A, Negussie Y, & Baciu A, Eds.). Washington, DC: The National Academies Press; 10.17226/24624 [DOI] [PubMed] [Google Scholar]
- National Environmental Justice Advisory Council. (2014). Recommendations for Integrating [Google Scholar]
- Environmental Justice into the EPA’s Research Enterprise. Retrieved from https://www.epa.gov/sites/production/files/2015-02/documents/nejac-research-recommendations-2014.pdf
- Neupane B, Jerret M, Burnett RT, Marrie T, Arain A, & Loeb M (2010). Long-term exposure to ambient air pollution and risk of hospitalization with community-acquired pneumonia in older adults. American Journal of Respiratory and Critical Care Medicine, 181(1), 47–53. 10.1164/rccm.200901-0160OC [DOI] [PubMed] [Google Scholar]
- New Detroit Coalition. (2014). Metropolitan Detroit Race Equity Report. Retrieved from https://www.newdetroit.org/wp-content/uploads/2017/05/MetropolitanDetroit_RaceEquity_Report_NewDetroit.pdf
- Nuru-Jeter AM, & LaVeist TA (2011). Racial Segregation, Income Inequality, and Mortality in US Metropolitan Areas. Journal of Urban Health : Bulletin of the New York Academy of Medicine, 88(2), 270–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostro B, Hu J, Goldberg D, Reynolds P, Hertz A, Bernstein L, & Kleeman MJ (2015). Associations of mortality with long-term exposures to fine and ultrafine particles, species, and sources: Results from the California Teachers Study Cohort. Environmental Health Perspectives, 123(6), 549–556. 10.1289/ehp.1408565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce N (2000). The ecological fallacy strikes back. Journal of Epidemiology and Community Health, 54(5), 326–327. 10.1136/jech.54.5.326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen M, Giorgis-Allemand L, Bernard C, Aquilera I, Andersen AMN, Ballester F, … Slama R (2013). Ambient air pollution and low birthweight: A European cohort study (ESCAPE). Lancet Resipr Med, 1(9), 695–704. 10.1016/S2213-2600(13)70192-9 [DOI] [PubMed] [Google Scholar]
- Phelan JC, & Link BG (2015). Is Racism a Fundamental Cause of Inequalities in Health? Annu. Rev. Sociol, 41, 311–330. [Google Scholar]
- Reardon S (2014). Income inequality affects our children’s educational opportunities. Retrieved June 3, 2020, from https://equitablegrowth.org/income-inequality-affects-our-childrens-educational-opportunities/
- Reardon SR, Fox L, & Townsend J (2015). Neighborhood Income Composition by Household Race and Income, 1990–2009. The Annals of the American Academy of Political and Social Science, 660(1), 78–97. 10.1177/0002716215576104 [DOI] [Google Scholar]
- Reibel M, & Regelson M (2011). Neighborhood Racial and Ethnic Change: The Time Dimension in Segregation. Urban Geography, 32(3), 360–382. 10.2747/0272-3638.32.3.360 [DOI] [Google Scholar]
- Reskin B (2012). The Race Discrimination System. Annu. Rev. Sociol, 38, 17–35. 10.1146/annurev-soc-071811-145508 [DOI] [Google Scholar]
- Rice LJ, Jiang C, Wilson SM, Burwell-Naney K, Samantapudi A, & Zhang H (2014). Use of Segregation Indices, Townsend Index, and Air Toxics Data to Assess Lifetime Cancer Risk Disparities in Metropolitan Charleston, South Carolina, USA. Int. J. Environ. Res. Public Health, 11, 5510–5526. 10.3390/ijerph110505510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice MB, Ljungman PL, Wilker EH, Schwartz JD, Koutrakis P, Washko GR, … Mittleman MA (2013). Short-term exposure to air pollution and lung function in the Framingham Heart Study. American Journal of Respiratory and Critical Care Medicine, 188(11), 1351–1357. 10.1164/rccm.201308-1414OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigolon A, & Christiansen J (2019). Greening without Gentrification: Learning from Parks-Related Anti-Displacement Strategies Nationwide. Retrieved June 13, 2020, from https://www.ioes.ucla.edu/wp-content/uploads/Greening-without-Gentrification-report-2019.pdf
- Rodriguez EM, Bowie JV, Frattaroli S, & Gielen A (2009). A qualitative exploration of the community partner experience in a faith-based breast cancer educational intervention. Health Education Research, 24(5), 760–771. 10.1093/her/cyp010 [DOI] [PubMed] [Google Scholar]
- Rose G (2001). Sick individuals and sick populations. International Journal of Epidemiology, 30(3), 427–432. 10.1093/ije/30.3.427 [DOI] [PubMed] [Google Scholar]
- Rothstein R (2017). The Color of Law: A Forgotten History of How Our Government Segregated America. New York, NY: Liveright Publishing Corporation. [Google Scholar]
- Ruffin J (2011). A Renewed Commitment to Environmental Justice in Health Disparities Research. Am J Public Health, 101, S12–S14. 10.2105/AJPH.2011.300480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rugh JS, & Massey DS (2010). Racial Segregation and the American Foreclosure Crisis. American Sociological Review, 75(5), 629–651. 10.1177/0003122410380868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks JD, Stanek LW, Luben TJ, Johns DO, Buckley BJ, Brown JS, & Ross M (2011). Particulate matter-induced health effects: Who is susceptible? Environmental Health Perspectives, 119(4), 446–454. 10.1289/ehp.1002255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadd JL, Pastor M, Morello-Frosch R, Scoggins J, & Jesdale B (2011). Playing it safe: Assessing cumulative impact and social vulnerability through an environmental justice screening method in the South Coast Air Basin, California. International Journal of Environmental Research and Public Health, 8(5), 1441–1459. 10.3390/ijerph8051441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz AJ, Mentz G, Sampson M, Ward M, Dvonch J, de Majo R, … Wilkins D (2018). Independent and Joint Contributions of Fine Particle Matter Exposure and Population Vulnerabilty to Mortality in the Detroit Metropolitan Area. International Journal of Environmental Research and Public Health, 15(6), 1209 10.3390/ijerph15061209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz AJ, Mentz G, Sampson N, Ward M, Anderson R, de Majo R, … Wilkins D (2016). Race and the distribution of social and physical environmental risk: A case example from the Detroit metropolitan area. Du Bois Review, 13(2), 285–304. 10.1017/S1742058X16000163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz AJ, Williams DR, Israel BA, & Lempert LB (2002). Racial and spatial relations as fundamental determinants of health in Detroit. The Milbank Quarterly, 80(4), 677–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sexton K, & Linder SH (2011). Cumulative Risk Assessment for Combined Health Effects from Chemical and Nonchemical Stressors. American Journal of Public Health, 101(S1), S81–S88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah PS, Balkhair T, & Knowledge Synthesis Group on Determinants of Preterm/LBW Birth. (2011). Air pollution and birth outcomes: A systematic review. Environmental International, 37(2), 498–516. [DOI] [PubMed] [Google Scholar]
- Sharkey P (2013). Stuck in Place: Urban Neighborhoods and the End of Progress Toward Racial Equality. Chicago and London: The University of Chicago Press. [Google Scholar]
- Shi L, Zanobetti A, Kloog I, Coull BA, Koutrakis P, Melly SJ, & Schwartz JD (2016). Low-concentration PM2.5 and Mortality: Estimating acute and chronic effects in a population-based study. Environmental Health Perspectives, 124(1), 46–52. 10.1289/ehp.1409111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon GM, Morello-Frosch R, Zeise L, & Faust JB (2016). Cumulative environmental impacts: Science and policy to protect communities. Annual Review of Public Health, 37, 83–96. 10.1146/annurev-publhealth-032315-021807 [DOI] [PubMed] [Google Scholar]
- Stern G, Latzin P, Roosli M, Fuchs O, Proietti E, Kuehni C, & Frey U (2013). A prospective study of the impact of air pollution on respiratory symptoms and infections in infants. American Journal of Respiratory and Critical Care Medicine, 187(12), 1341–1348. 10.1164/rccm.201211-2008OC [DOI] [PubMed] [Google Scholar]
- Stieb DM, Chen L, Eshoul M, & Judek S (2012). Ambient air pollution, birth weight, and preterm birth: A systematic review and meta-analysis. Environmental Research, 117, 100–111. 10.1016/j.envres.2012.05.007 [DOI] [PubMed] [Google Scholar]
- Strickland MJ, Darrow LA, Klein M, Flanders WD, Sarnat JA, Waller LA, … Tolbert PE (2010). Short-term associations between ambient air pollutants and pediatric asthma emergency department visits. American Journal of Respiratory and Critical Care Medicine, 182(3), 307–316. 10.1164/rccm.200908-1201OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su JG, Morello-Frosch R, Jesdale BM, Kyle AD, Shamasunder B, & Jerret M (2009). An index for assessing demographic inequalities in environmental hazards with application to Los Angeles, California. Environ Sci Technol, 43(20), 7626–7634. 10.1021/es901041p [DOI] [PubMed] [Google Scholar]
- Sugrue TJ (2014). The Origins of Urban Crisis: Race and Inequality in Postwar Detroit. Princeton, NJ: Princeton University Press. [Google Scholar]
- Susser M (1994). The logic in ecological: I. The logic of analysis. American Journal of Public Health, 84(5), 825–829. 10.2105/ajph.84.5.825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Templet PH (1995). Equity and sustainability: an empirical analysis. Soc. Nat. Resour, 8(6), 509–523. [Google Scholar]
- Thakrar AP, Forrest AD, Maltenfort MG, & Forrest CB (2018). Child Mortality in the US and 19 OECD Comparator Nations: A 50-Year Time-Trend Analysis. Health Affairs, 37(1). 10.1377/hlthaff.2017.0767 [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau (n.d.). Income Inequality Data Tables. Retrieved from https://www.census.gov/topics/income-poverty/income-inequality/data/data-tables.html
- U.S. Census Bureau. (2018). Understanding and Using American Community Survey Data: What All Data Users Need to Know. Government Printing Office. Washington, D.C. [Google Scholar]
- U.S. Census Bureau. (2020). American Community Survey: Guidance for Users. When to use 1-year, 3-year, and 5-year estimates. [Google Scholar]
- U.S. Environmental Protection Agency. (2002). Health assessment document for diesel engine exhaust (Final 2002). Washington, D.C: Retrieved from https://cfpub.epa.gov/ncea/risk/recordisplay.cfm?deid=29060 [Google Scholar]
- Urman R, McConnell R, Islam T, Avol EL, Lurmann FW, Vora H, … Gauderman WJ (2014). Associations of children’s lung function with ambient air pollution: Joint effects of regional and near-roadway pollutants. Thorax, 69(6), 540–547. 10.1136/thoraxjnl-2012-203159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White K, Haas JS, & Williams DR (2012). Elucidating the Role of Place in Health Care Disparities: The Example of Racial/Ethnic Residential Segregation. Health Services Research, 47(3), 1278–1299. 10.1111/j.1475-6773.2012.01410.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Collins C (2001). Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health. Public Health Reports, 116, 404–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Mohammed SA (2013). Racism and Health I: Pathways and Scientific Evidence. American Behavioral Scientist, 57(8), 1152–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson S, Hutson M, & Mujahid M (2008). How Planning and Zoning Contribute to Inequitable Development, Neighborhood Health, and Environmental Injustice. Environmental Justice, 1(4). 10.1089/env.2008.0506 [DOI] [Google Scholar]
- Yang T-C, & Matthews SA (2015). Death by Segregation: Does the Dimension of Racial Segregation Matter? PLoS One, 10(9). 10.1371/journal.pone.0138489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao L, & Robert SA (2011). Examining the Racial Crossover in Mortality between African American and White Older Adults: A Multilevel Survival Analysis of Race, Individual Socioeconomic Status, and Neighborhood Socioeconomic Context. Journal of Aging Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeger SL, Liang K-L, & Albert PS (1988). Models for Longitudinal Data: A Generalized Estimating Equation Approach. Biometrics: International Biometric Society, 44(4), 1049–1060. 10.2307/2531734 [DOI] [PubMed] [Google Scholar]


