Abstract
There is increasing concern globally about the enormity of the threats posed by antimicrobial resistance (AMR) to human, animal, plant and environmental health. A proliferation of international, national and institutional reports on the problems posed by AMR and the need for antibiotic stewardship have galvanised attention on the global stage. However, the AMR community increasingly laments a lack of action, often identified as an ‘implementation gap’. At a policy level, the design of internationally salient solutions that are able to address AMR’s interconnected biological and social (historical, political, economic and cultural) dimensions is not straightforward. This multidisciplinary paper responds by asking two basic questions: (A) Is a universal approach to AMR policy and antibiotic stewardship possible? (B) If yes, what hallmarks characterise ‘good’ antibiotic policy? Our multistage analysis revealed four central challenges facing current international antibiotic policy: metrics, prioritisation, implementation and inequality. In response to this diagnosis, we propose three hallmarks that can support robust international antibiotic policy. Emerging hallmarks for good antibiotic policies are: Structural, Equitable and Tracked. We describe these hallmarks and propose their consideration should aid the design and evaluation of international antibiotic policies with maximal benefit at both local and international scales.
Keywords: health policies and all other topics, infections, diseases, disorders, injuries, public health
Summary box.
The global crisis of antimicrobial resistance has led to a proliferation of expert reports and national and international antibiotic action plans.
Implementing international antibiotic policy that is meaningful in different social, cultural and economic contexts continues to prove challenging.
Our multidisciplinary analysis has identified four critical challenges of metrics, prioritisation, implementation and inequality for international antibiotic policy-making.
We propose a corresponding SET of basic hallmarks of good antibiotic policy, which we define as Structural, Equitable and Tracked.
Our SET of hallmarks can orientate disciplinary debates and provide a framework for developing robust international interventions.
Introduction: antimicrobial resistance as a biosocial problem
Since their introduction in the 1930s, antibiotics have acquired infrastructural importance in global health and food production.1 However, antibiotic reliance comes with a trade-off: using antibiotics accelerates the emergence of antimicrobial resistance (AMR), which diminishes their future effectiveness. This makes effective antibiotics a precious ‘global common-pool resource’,2–6 which can benefit humanity but will provide diminishing benefits if we fail to coordinate plans for preservation (a tragedy of the commons).
Over the past decade, rising concern about AMR has highlighted the need for collective action to protect our antibiotic ‘commons’.2 7–12 Governmental and non-governmental organisations have devoted substantial resources to tackling AMR and preserving antibiotic effectiveness on national and international stages.13 Increasing attention and funding have been accompanied by a proliferation of expert reports and policy proposals.14 While these AMR-focused initiatives have succeeded in achieving a clear international consensus on the need for action, many lament a lack of action in practice, dubbed an ‘implementation gap’. Substantial uncertainties also remain about the effects of different policy interventions, how international policies could be enforced globally, and who will pay in the long term. The main difficulty with managing the antibiotic commons seems to lie in jointly addressing the complex biological and social (understood here to be historical, political, economic and cultural) dimensions of AMR. Policy formation for the latter dimension is particularly challenging because it entails addressing different metrics, meanings and challenges in different settings.
We propose a new wide-angle approach to AMR-focused antibiotic regulation. Two basic questions guide our reflective process: (A) Is a universal approach to AMR policy and antibiotic stewardship possible? (B) If yes, what hallmarks characterise ‘good’ antibiotic policy?
To answer these questions, we have developed an innovative heuristic evaluation framework, which accounts both for AMR’s biological and social facets. Our approach was informed by the numerous national and international reports proposing various principles for antibiotic policy-making2 10 11 15–17 and the historical success of the 3Rs (Reduction, Refinement and Replacement) that restructured laboratory animal testing protocols. Developed as principles of ‘good animal experimentation’ in 1959, the 3Rs were concrete and aspirational enough to trigger a progressive evolution of protocols and dialogue in a contested policy arena.18(So et al have proposed three Rs for antimicrobial development).19
Applying this approach to AMR and antibiotic policy, our collaborative multidisciplinary analysis employed a three-stage evidence gathering, evaluation and consultation process (box 1), which consisted of: (1) asking selected medical humanities and sciences researchers whether they believe antibiotic policies could feasibly be guided by a universal set of guiding principles, and what they consider those guiding principles could be; (2) identifying possible hallmarks of good policy with a broad group of stakeholders from academia, medicine, animal/plant production, policy and funding bodies at an international workshop and (3) refining identified hallmarks in light of multidisciplinary feedback.
Box 1. Three stage evidence gathering, evaluation and consultation process.
Stage 1:
Following a 2018 Social Science and antimicrobial resistance (AMR) Research Symposium at the British Academy in London,162 a correspondence group of fourteen experts from the humanities, social, environmental and medical sciences reflected on whether there could be universal principles of international antibiotic policy making and hallmarks of ‘good’ policy.
Stage 2:
Identified policy challenges and core hallmarks of successful intervention informed a preliminary paper, which was circulated among correspondents and attendees of a multidisciplinary 2-day workshop in London in March 2019.
During presentations, small group breakout sessions, and group discussions, participants reflected on the preliminary paper’s four identified problem areas for antibiotic regulation: (A) metrics (defining and measuring AMR, antibiotic usage and performance indicators for interventions); (B) prioritisation (prioritising specific forms of antibiotic use over others); (C) implementation (developing and implementing interventions that are meaningful in high-income, medium-income and low-income settings); (D) inequality (formulating interventions that take into account global disparities of wealth, infectious disease and AMR burdens and access to antibiotics as well as effective health, water, sanitation and hygiene systems).
There was agreement on these interlinked problems but the four provisional hallmarks proved more contentious: (1) antibiotic policymaking should take into account antibiotics’ infrastructural relevance in medicine and food production; (2) should increase the microbial resilience of health and food systems to diminish the need for antibiotics; (3) be responsive to evolving knowledge regarding AMR and (4) relational in its acknowledgement of differing local challenges and capacities.
Participants agreed that there was no single solution to AMR but felt that hallmarks needed to be integrated and go beyond preserving the status quo. Key to more effective policymaking has to be an acknowledgement of antibiotics’ primary utility for global health and food production, which consists in their ability to reduce mortality and morbidity resulting from treatable infections. To preserve this utility, the overriding aim of any antibiotic policy must therefore be (1) to maximise and maintain access to effective treatments for infections, which includes the development of new treatments—while (2) reducing the need for antibiotic use by preventing infections, reducing antibiotic dependencies in healthcare and food systems, and minimising the environmental load of antibiotics and resistant bacteria.
Stage 3:
A refined version of new Structural, Equitable, Tracked Hallmarks was circulated among correspondents and participants, who were invited to be coauthors on the paper.
We believe that the resulting heuristic compass based first on the identification of central challenges of antibiotic policy-making (metrics, prioritisation, implementation, inequality) and second on the formulation of a corresponding Structural, Equitable and Tracked (SET) of hallmarks of good antibiotic policy, which we define as SET can orientate disciplinary debates and provide a framework for robust international interventions.10 20 21
The four central challenges of antibiotic regulation
Metrics
Despite long-standing regulation attempts, there remains substantial uncertainty about basic metrics surrounding antibiotic usage and AMR as well as about how to correlate measurements in a way that can inform meaningful policy formulation at the national and international levels.22
How to define resistance?
Since the first warnings about ‘drug fastness’ in microorganisms in 1907,23 24 there has been no clear transdisciplinary or international consensus on how to define AMR. The constantly evolving nature of AMR, the introduction of new drugs and the different availability and use of antibiotics means that terms like drug sensitive, intermediate resistant or resistant, mean different things in different regional contexts. There is also no transdisciplinary consensus on whether to define AMR according to predefined clinical breakpoints, minimum inhibitory concentrations, epidemiological cut-offs, pharmacokinectic/pharmacodynamic models, the presence or absence of resistance-conferring genetic elements or clinical impact on patients or animals. Disagreement over this latter point is highlighted by the common absence of drug-resistant infection as an official cause of death. Historically, the lack of consensus over AMR has led to differing microbiological and public health definitions of AMR with the former measuring incremental changes of microbial susceptibility and the latter measuring instances of treatment failure at predefined dosages.25–27
Whose methods count?
Internationally, the establishment of WHONET (est. 1989) and WHO’s Global Antimicrobial Resistance Surveillance System (GLASS, est. 2015) marked important efforts to standardise AMR reporting in humans and make data comparable.28 29 However, coordination problems remain: testing protocols by influential bodies like the European Committee on Antimicrobial Susceptibility Testing (EUCAST) and the US-based Clinical Laboratory Standards Institute (CLSI) occasionally diverge. Resulting international monitoring differences are exacerbated by issues of access (see problem area Inequality).30 EUCAST guidelines and updates are available free of charge. By contrast, CLSI guidelines and updates are often pay for use, which makes it difficult for resource poor laboratories to keep protocols up to date and feedback local AMR data into international databases.31 In low and middle income countries (LMICs), surveillance is often further complicated by lack of access to laboratory equipment, service contracts and paywalled literature.32 Ensuing disparities in global AMR reporting mean that international reports disproportionately reflect data from resource-rich settings and a limited number of well-studied low-income sentinel sites with international healthcare infrastructure investment.33 Resulting international stewardship and policy guidelines may, however, be of limited use in understudied resource-poor settings with different AMR ecologies and no access to key antibiotics.
What is relevant antibiotic use data for AMR?
Capturing relevant data on antibiotic use to inform AMR efforts has its own challenges. Starting in the 1990s, various high income countries (HICs) began to compile antibiotic usage data.34–37 However, data collection methods continue to vary. In the case of antibiotic usage in animals, the World Organisation of Animal Health (OIE) has begun to collect data on antibiotic sales intended to be used in animals and usage data since 2015. However, despite ongoing progress, data gaps remain with almost 25% of 182 OIE Member Countries not reporting quantitative and most reporting antibiotic sales and imports data but no data on use for the fourth OIE round of data collection.38 Reporting differences are also common among HICs. The EU developed a standardised metric to correlate antibiotic sales with the volume of animal production (mg/population correction unit) from 2010 onwards.39 Individual EU countries like Britain and Denmark publish not just sales but farm usage and prescription data for certain livestock categories.40 41 By contrast, the US Food and Drug Administration (FDA) publishes sales data only in broad categories of drug class by species but no usage data, which complicates AMR risk assessment.42
Correlating usage and AMR data is even more challenging. In its 2018–2019 report, the English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) showed a significant reduction in antibiotic prescriptions but an increase in antimicrobial-resistant infections for the seven priority bacterial pathogens reported.43 In 2017 and 2019, longitudinal studies of bloodstream infections in Malawi showed a long-term reduction of overall infections but a rise of antibiotic resistance in remaining infections.33 44 To be useful, aggregated metrics of antibiotic usage (including class of antibiotic) across infection types need to be contextualised with outcome and population health metrics, such as infection, resistance and morbidity/mortality rates.45–47
Understanding what the implications of specific forms of antibiotic usage (eg, prophylaxis, therapy, growth promotion) in different environments are for AMR and health outcomes is similarly crucial for policy formulation. Rising numbers of point prevalence studies and whole-genome sequencing are enhancing our knowledge of drivers and variations of AMR over time and in different areas across the world.48–51 However, our wider understanding of the evolutionary factors underlying AMR levels is still fragmentary as is our understanding of which stewardship interventions might make how much of a difference: in some cases like targeted 1950s antibiotic prescription bans at St Bartholomew’s Hospital in London52 or Denmark’s 1990s ban of lower-dosed avoparcin and tylosin animal growth promoters, reducing selection pressure by a specific type of drug usage led to a marked reduction, but not a complete disappearance, of correlating AMR.53 54 In other cases, antibiotic reductions may take years to manifest in terms of reduced AMR—as highlighted by the UK’s 2019 ESPAUR report and experiences in Scandinavian countries.43 53 55 Finally, some usage reductions may come too late to shift the evolutionary balance back in favour of microbial sensitivity as occurred with China banning the use of colistin growth promoters in 201656 following a report of the transferable mobilisable colistin resistance MCR-1 gene.57 Subsequent reports, however, showed that the gene was detectable in strain collections from more than 30 countries and was already circulating in Escherichia coli in China in the mid 1980s.58 The lack of uniformly comparable data makes it more difficult to evaluate trade-offs in various policy options.
How to develop meaningful key performance indicators?
While uncertainty remains about the degree to which interventions will be effective, reducing the overall amount of antibiotics used in health and animal and plant production systems is a key component of most AMR action plans.11 13 59 Over the past two decades, international bodies have attempted to decide which antibiotics to protect from overuse. Since 2004, WHO, OIE and the Food and Agriculture Organization (FAO) have begun using the categories of critically important antimicrobials (CIAs), highly important antimicrobials and important antimicrobials—although differences in the categorisation of the same drugs for veterinary and medical usages can remain.60 61 In 2019, the WHO’s Essential Medicines List added the AWaRe categorisation, to meet a need to recognise those medicines that should be Accessed as first-line narrow-spectrum treatment for particular conditions, and those with higher risks of becoming resistant that should be used Watchfully and those that should be Reserved for last-line treatment.62 This framework can be used as an index—the ratio of Access to Watch and Reserve medicines—to compare prescribing practices in different contexts, which goes some way to balancing the different challenges of improving access and restricting excess when setting targets.63 However, measurement of antibiotic usage remains a challenge. Although WHO and OIE have standardised methodologies to collect country-level antimicrobial usage in humans and animals for global reporting and consulting companies like IQVIA gather and sell additional proprietary data,64 65 more granular level detail about antibiotic usage on farms and in particular clinical and residential settings is required for targeted reduction strategies.66 67
Alongside improved usage data, deciding which microbes, resistance genes and AMR reservoirs to monitor in medical, animal and plant production, and environmental settings is similarly important for the formulation of meaningful policy interventions. For humans, WHO published a list of priority pathogens to monitor and target with antibiotic development efforts in 2017.68 For animals, the OIE Member Countries agreed on harmonised lists for both terrestrial and aquatic animals.69 70 However, it remains difficult to prioritise which sentinel organisms to survey and where potentially important AMR reservoirs are located due to different health threats in HICs, MICs and LICs, lacking clinical surveillance infrastructure in many LMICs and of environmental surveillance in the most countries, regionally skewed reporting that often centres on urban clinical settings, and limited diagnostic capabilities for non-classic pathogens.71 72 Furthermore, particular microbes such as Staphylococcus aureus and E. coli may or may not be causing disease, and therefore, their measurement without corresponding disease burden data might be misleading.
Discussed in more detail below (see Tracked), one recently proposed solution for human health might be to integrate AMR and infection burden measurements by tracking two priority organisms in bloodstream infections as part of United Nations (UN) Sustainable Development Goal (SDG) 3.d.1. This new AMR-specific SDG could help build laboratory capacity in resource-poor settings and spur the development of further integrated AMR-specific metrics. Another approach might be to strengthen point prevalence studies for specific sentinel organisms in LMIC settings.73 (Consultations on sentinel organisms and sentinel sites are ongoing by GLASS and the point prevalence survey).
The described temporal and contextual challenges of defining resistance, measuring antibiotic usage in relation to AMR and concerning which microbes to focus on also raise important questions when it comes to defining benchmarks or key performance indicators (KPIs) for policy initiatives: how far should antibiotic sensitivity be restored or preserved for a measure to be considered successful? Should the performance of a policy be linked to its reduction of antibiotic usage or should the KPI be demonstrated impact on human health? Should success be defined as the stabilisation or decline of AMR in specific culturable pathogens? Given the mobility of resistance genes and the One Health dimensions, should a metric of success be the abundance or prevalence of a particular resistance gene in the wider environment, determined through quantitative PCR methods74? How much time should policies have to achieve their goals?
Prioritisation
Overemphasis on surveillance data itself can serve to obscure different regional capabilities, underlying political interests and competing needs in animal and human medicine.75 In addition to defining meaningful metrics, a significant challenge facing international antibiotic regulation is which form of antibiotic use to prioritise in the face of time-limited microbial sensitivity to most drugs and heterogeneous epidemiological, social, economic and material contexts. The challenge of prioritisation comprises spatial and temporal components.
Spatial: since the 1940s, regulators have tried to protect important antibiotics by restricting their use,76 but this path-dependent prioritisation has been enacted differently across varying local, regional and national settings. Antibiotics’ infrastructural importance in global healthcare and food production means that a large number of sectors with different needs depend on routine antibiotic access.1 In the case of Europe and North America, historians have shown that distinct national antibiotic usage patterns have become socially entrenched over decades.77–81 To this day, antibiotic usage patterns vary across Europe and North America despite both regions' close economic, political and cultural ties.82 83 Differences of usage are even more substantial between HICs and LMICs with patients in the latter countries often depending to a much stronger degree on the efficacy of a limited number of locally available, affordable and easily administrable drugs—particularly in areas where there is no access to professional healthcare facilities.84–86 If different countries, sectors and even local healthcare facilities87 use different antibiotics for a variety of biological and social reasons, whose form of antibiotic use should receive priority?
The same problems of spatial prioritisation hold true in animal and plant production.34 88 One example of spatialised inequality of access are the polymyxin antibiotics (eg, colistin, discovered in 1949). After using the drugs to treat gram-negative infections in humans, HICs greatly reduced use of polymyxins in favour of less toxic carbapenems from 1980 onwards.89 Although limited use of ‘old’ colistin continued in HICs, their low cost and lacking HIC demand for human medicine led to aggressive pharmaceutical marketing and large-scale uptake for growth promotion and disease prevention in the industrialising animal production of LMICs like China and Brazil.88 When rising carbapenem resistance led to a resurgence of polymyxin use in human medicine around 2005, competing animal production and medical priorities meant that global regulators did not raise polymyxins’ status to that of CIAs. It was only after the discovery of the mcr-1 gene on transferable plasmids in bacterial isolates from Chinese pigs that polymyxins were recategorised as highest priority CIAs in 2016, received specific restriction recommendations from OIE, and were banned from use as growth promoters in China and Brazil.57 60 75
Temporal: another challenge of prioritisation regards the inevitable temporal conflict between acute healthcare needs and the future-focused dimensions of antibiotic stewardship.90 There is a well-evidenced ethical dilemma between preserving drugs’ future efficacy and using antibiotics to safe-guard vulnerable populations in the present. This is highlighted by studies on the rise of multidrug-resistant pathogens in itinerant and immunocompromised HIC and MIC populations91–94 or of AMR proliferation as a result of high levels of antibiotic use in prolonged crisis situations like the 2009 H1N1 influenza or the current COVID-19 pandemic.95–98 Similar dilemmas have also become apparent in campaigns of antimicrobial mass drug administration to prevent child stunting,99 100 against onchocerciasis, lymphatic filariasis or malaria,101 in the mass administration of azithromycin against drivers of childhood mortality in Tanzania, Niger and Malawi,102 103 and to prevent scabies and impetigo on the Solomon Islands.104
Answers to this temporal dilemma vary and reflect the perceived severity of need, cultural preferences for specific forms of use, and economic considerations. In some cases, the potential longer-term risk to public health of antibiotic resistance has been favoured over immediate clinical needs.105 However, in the main, present needs have overridden future-focused stewardship concerns. While there is no reason not to use antibiotics to save and improve lives, they have often been used as a ‘quick fix’106 to symptomatically control rather than eliminate underlying drivers of infection in human, animal health and plant production systems. The tendency to see antibiotics as ‘quick fixes’ has helped drive AMR and often distracted from investment in more sustainable forms of infection prevention like effective and affordable health, Water, Sanitation and Hygiene (WASH), and Infection Prevention Control (IPC) systems (see also Inequality below).85 Over-reliance on antibiotics has also been exacerbated by industry marketing of, in part, inappropriate antibiotic usage and targeted campaigning to undermine usage restrictions in high-income and low-income settings.34 77 107
Implementation
A third fundamental challenge for antibiotic policy-making concerns the formulation of binding international agreements that can still be implemented flexibly in different settings.17 108 Recent international agreements like the 2016 UN Paris Agreement on climate change remain based on the classic so-called Westphalian model of sovereign nation-states agreeing on a set of measures, which are then independently enacted within their borders without control by other actors.7 12 109 110 There are a number of challenges with this model: global trade flows are not easily regulated by nation-level policies; with few exceptions like the International Health Regulations on pandemics, international organisations like the WHO cannot enforce health agreements negotiated under their umbrella; the ability of governments to implement policies varies.8 20 110 111 Described implementation problems are exacerbated by the widespread absence of basic data and robust metrics (see above) to inform international policymaking. For example, while it may seem straightforward to define and evaluate policy success as reductions of drug usage in HICs, these metrics will likely fail in settings without reliable consumption/usage data and where informal grey market and unregulated over-the-counter sales account for a large part of the antibiotic supply.82 112 113
Using an integrated political, economic, sociological, technological, ecological, legislative and industry framework, reviews of national action plans proposed after the 2015 Global Action Plan on Antimicrobial Resistance have warned of continuing gaps in applying international concepts of stewardship at the national level.114 115 Focusing only on international and not on actual local policy alignment can foster the creation of ‘paper tiger’ initiatives, which are not enforced—as in the case of enacted but not enforced bans of over-the-counter antibiotic sales116—or obscure or relabel existing practices rather than reform underlying antibiotic infrastructures.13 117 118 Follow-up reports by WHO, UN and World Bank have proposed solutions including international investment in local IPC, antibiotic quality assurance and access schemes, AMR surveillance, vaccination, local stewardship champions and contextualised policy-making.10 20 21 111 In the case of animal production, experts have proposed using AMR monitoring in sentinel pathogens and technical support from HICs as tools to incentivise global reductions of antibiotic usage.119 Promising access to lucrative markets and using transnational integration to promote precautionary antibiotic policies is an additional tool that was used by the UK in the 1970s, Sweden in the 1990s, and is now being considered by the EU to reduce antibiotic growth promoter and prophylactic antibiotic use in non-European countries.34 120
However, so far, enactment of proposed measures has been fragmentary13 and it remains unclear how numerous national and international calls to action with complex interlayered principles of action can be translated into effective change in settings where antibiotic access is lacking and AMR is secondary (at best) to other health concerns. Looking beyond top-down nationstate alignment, by reemphasising municipal and community-based health initiatives as well as creating new metrics for antibiotic access before prioritising stewardship may be a solution. Recent social sciences research suggests the efficacy of adaptive value-driven bottom-up reforms. These reforms move from merely sanctioning inappropriate antibiotic use to identifying the sociostructural factors driving antibiotic use and devising targeted incentives for locally tailored shifts to more appropriate antibiotic use.121–123 However, it remains unclear whether relying on local or even regional solutions will be able to solve the global challenge posed by AMR. Calls for behavioural change, industry reform and individualised policymaking have often been ineffective.34 77
Inequality
One of the most significant challenges facing international antibiotic policy and global health frameworks more widely are significant levels of inequality between and within HICs and LMICs. These inequalities reflect historically uneven social and political opportunity as well as distribution of economic resources and disease burdens. Inequality has large implications for ways priorities are made and implemented in relation to antibiotics. Recognition of these inequalities challenges forms of policymaking that focus on metrics of drug reduction alone (see Metrics and Implementation above) or prioritise protection of HIC hospital antibiotics over LMIC needs for access to antibiotics and protein production.
The unevenness of social and political opportunities affects who can make or demand policies. At the international level, the historical dominance of HICs on relevant health bodies and many funders’ and high-level meetings’ location in HICs has led to a relative absence of the voices of some of the most affected LMIC stakeholders.124 There is a historically evidenced danger that this dominance of HIC voices can drown out LMIC concerns and lead to narrow policies centring on HIC concerns.125 126 Despite best intentions, motivations for international antibiotic policy initiatives must thus be considered uneven when framed with a health security lens—who is the ‘we’ in the need to act, and who is the ‘us’ being protected1?
Answering these questions is important. In the case of drug development, historical priority setting has been HIC-centric due to the greater profitability of high-income markets (with a particular emphasis on the most lucrative US market) and differing regional risk priorities.111 127 In the case of surveillance, antibiotic resistance and usage indicators emerge unevenly from particular locations, prioritise particular security concerns and carry particular interpretations. When shuttling between different contexts in which resistance and use might have a different significance, these abstracted numeric indicators can foster a contextual disconnect among decision-makers.128 The described surveillance disconnect is exacerbated by the relative lack of data from LICs and rural settings (see Metrics above). The result is a vicious circle: lacking access to equipment, current standards and scholarly literature means that disease and AMR burdens cannot be measured and published,32 which means that there are no data with which to build local expert capacity or inform international policy, which compounds the obscuring of difference between contexts.
Over time, decontextualised international decision making can result in policies that prioritise HIC-centric stewardship interventions like targeted drug restrictions that may prove deleterious in LMICs where infection risks are markedly higher and different.111 129 Limited data indicate an inverse correlation between countries' gross national income and invasive infections caused by WHO top-ranked antibiotic-resistant bacteria.71 Where resources are stretched thinly across health systems and infrastructure, other priorities than stewardship may be more pressing for investment. For example, IPC in health facilities and availability of effective WASH systems are essential. However, in 2017, ca. 785 million people worldwide had no access to safe drinking water, two of every seven people had no access to sanitation, and 22% of LIC health facilities had no water service.130 131 Indeed, investment in IPC and WASH is likely to be most effective for reducing AMR in many settings as a base on which stewardship might then be built.10 20 132 Furthermore, in many settings the ability to provide equitable access to essential medicines of sufficient quality, including antibiotics, remains elusive.10 112
Similar constraints are true for animal health which is related to issues such as food safety, food security and animal welfare. Many national and international action plans invoke enhanced biosecurity facilities, vaccination or good husbandry practices as a means to avoid unnecessary non-human antibiotic use, but they rarely set these measures as (funded) priorities contrary to raising awareness, developing surveillance or promoting responsible and prudent use, or they risk assuming inappropriate livestock production and disease management approaches in settings where economic and microbiological risks are manifestly different.133–135 While arguments for wider systems strengthening should not undermine statutory antibiotic reform, decontextualised policies focusing only on antibiotic stewardship and surveillance risk distracting from the even more important structural absence of adequate and situationally appropriate sanitary, veterinary and healthcare systems in many parts of the world.
Hallmarks of good antibiotic policy
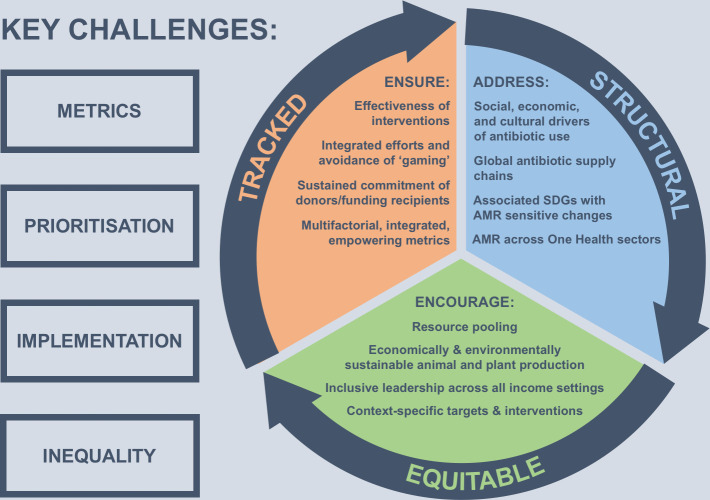
The four biosocial challenges of metrics, prioritisation, implementation and inequality require a holistic response from international antibiotic policy that is ambitious enough to improve the status quo but concrete and evocative enough to be an effective guide. Because such policies are enacted within a complex ecosystem, a broad perspective needs to inform their design and deployment to maximise effectiveness and minimise unintended consequences. It is this broad heuristic perspective, incorporating One Health, spatial, temporal and ethical dimensions that underlies the three interlinked SET hallmarks proposed here (figure 1).
Figure 1.
Interlinked hallmarks of successful antibiotic policy-making.
1. Structural: International antibiotic policies should recognise and respond to the multiple aspects of global antibiotic infrastructures.1 Since the 1930s, antibiotics have replaced older, more expensive forms of infection control in humans, animals and plants and enabled new medical interventions like organ transplants and prosthetic joint implants. Global health and food production systems rely on the comparatively cheap ‘work’ performed by antibiotics. Reforming antibiotic use cannot be separated from broader reforms of the infrastructures that have evolved around them.
Historically, there has been a tendency to make AMR manageable by compartmentalising problems and blaming individuals for drug overuse instead of the underlying social, political and economic factors driving antibiotic demand and dependencies (see Metrics and Prioritisation).34 77 136 137 In HICs, a long-standing focus on technical quick fixes and individual behavioural change meant that farmers and patients were routinely blamed for overuse without targeting wider infrastructural factors or the companies and experts supplying antibiotics.106 Bureaucratic divisions also meant that the same antibiotics could be subject to different regulations on farms and in clinics (see Implementation). The fact that most reforms stopped at national borders further fragmented international regulation.76 88 136 Since the adoption of One Health terminology by WHO and EU antibiotic regulators around 2010,138 nearly all international AMR initiatives have attempted to overcome described problems by integrating polices for drug regulation in human medicine, animal production and the environment. However, beyond surveillance, One Health was initially often narrowly applied to mean ‘animals’ rather than the wider environment—perhaps reflecting the absence of the UN Environmental Programme from the original Tripartite coalition of FAO, OIE and WHO. Recent European, Indian and private initiatives now explicitly target wastewaters and industrial wastes15 134 139 140 but implementing new standards remains challenging. Meanwhile, our scientific understanding of the relative effect of antibiotics, metals and biocides on environmental AMR burdens and of the efficacy of proposed interventions remains fragmentary.74 141 142
Successful antibiotic stewardship cannot be narrow and divorced from the social and environmental contexts in which use is taking place. More effective international policy requires the abandonment of regulatory silos, as well as the adoption of context-sensitive models. It requires a broad structural approach to reforming not only the international antibiotic supply chain (drug producers) but also wider contributing global and regional consumption patterns (eg, rising global demand for protein) as well as associated socio-structural factors (eg, fractured health and WASH infrastructures, time constraints on diagnosis, profit incentives to prescribe or sell drugs) and environmental factors (eg, infection burdens, drug residues in water systems).
As evidenced by recent successes in HIC animal production and health systems, jointly focusing on preventing disease with vaccines and improved welfare, updating the design of surveillance, hospital, animal housing systems and modifying antibiotic-seeking behaviour by patients and animal and plant producers can reduce antibiotic dependencies.143–145 However, high-income infrastructural starting points cannot be taken for granted elsewhere in the globe (see the Inequality section). To be effective internationally, the nature of ‘intervention’ must be less ‘AMR-specific’ and instead build up ‘AMR-sensitive’ changes20 which support wider UN SDGs including improved WASH, nutrition and access to affordable medical and veterinary healthcare.10 20 While we do not discount the importance of traditional regulatory tools like actively enforced bans of over-the-counter sales, understanding the work that antibiotics perform in non-HIC settings may also lead to an interlayering of old and new policy tools such as subsidised assurance and disease insurance schemes for farmers phasing out antibiotics, access to high-income markets for animal and plant products produced without antibiotics, public antibiotic production or certified antibiotic distribution schemes.20 127 146 147
2. Equitable: To be impactful globally, international antibiotic policies must recognise and respond to the unevenness in contributions towards and ability to tackle AMR while aiming for an equitable future for antibiotics regardless of where they are deployed. Historically, inequality and the difficulty of uniform policy implementation across HICs and LMICs have been major obstacles for international antibiotic reform (see the Inequality and Metrics section).
Because antibiotic effectiveness is a time-limited global common pool resource and even robust national responses offer little protection from the global circulation of AMR genes and organisms, the sustained pooling of international resources is an essential prerequisite to overcome identified challenges. Similar to climate change, some countries have a greater differentiated responsibility to contribute resources to this common pool than others.110 For decades, populations in HICs have had greater access to the antimicrobial commons than their counterparts in LMICs. High volumes of HIC usage facilitated the historical selection for and global circulation of resistant genes and organisms while HIC companies disproportionately profited from early antibiotic sales. HICs’ historical contribution to current AMR levels and role in spreading antibiotic dependent infrastructures to other parts of the world88 148 entail a moral obligation to bear a higher burden when it comes to mitigating resulting problems.110 Similarly, recent and projected high levels of antibiotic use and production in MICs create a comparable obligation to contribute resources to mitigate problems in poorer areas of the world and for future generations.48 119 149 150
Whether action is justified on the basis of historical usage, collective responsibility, obligations towards future generations, or enlightened self-interest, any international policy framework will have to include long-term financial and political HIC and MIC commitments to support antibiotic sensitive interventions in resource-poor communities. In LICs, antibiotic sensitive international support could centre on building human and infrastructural capacity by educating and employing more medical and veterinary professionals,20 enhancing laboratory provision and expanding access to effective, affordable, and safe vaccines, antibiotics, and WASH and health systems. From a One Health perspective, international policies should also promote economically and environmentally sustainable forms of animal and plant production as well as improve the management of waste containing antibiotics.
Well-designed structural and equitable international antibiotic policies can generate a global win-win.110 Building LMIC capacity for disease control and prevention and providing equitable access to effective treatments via market reforms, subsidies or public research and development127 151 152 will lower both local disease burdens and rising international AMR-related healthcare costs.10 20 111 127 In the case of animal and plant production, equitable policies will recognise that to ensure regional food security, targets for a sustainable antibiotic-controlled production system can only come after an infrastructural groundwork is in place to reduce reliance on these substances.119 123
Because of its structural dimensions, the lack of an easy target and a dysfunctional commercial research and development pipeline for new antibiotics,127 147 AMR has so far failed to attract the same degree of resources that organisations like the Global Vaccine Alliance (GAVI) (est. 2000) or the Global Fund (2002) have mobilised for individual diseases like HIV/AIDS, tuberculosis, malaria or polio. Achieving truly structural and equitable global AMR solutions will depend on the more effective generation and pooling of investment in safe antibiotic access, coordination of country-level policy responses and provision of effective WASH, IPC and educational resources.127 This role could be fulfilled by the existing Tripartite and a One Health Global Leadership Group on AMR.153 Another option suggested by some authors is creating a new dedicated international AMR body or pooled fund similar to GAVI.8 Ultimately, the structural challenges posed by AMR exceed the capabilities of any one nation. Overcoming the significant levels of inequality that have hampered previous responses will depend on intensifying international collaboration, equitably pooling resources and knowledge, and openly addressing the global disparities driving infectious disease burdens and the resulting need for antibiotics.
3. Tracked: Progress towards structural and equitable antibiotic policies has to be tracked to ensure ongoing effectiveness of interventions, promote integration of international efforts and motivate sustained commitment of donors and funding recipients. While a regular independent international stocktake could help ensure that policy interventions remain coordinated, equitable and up to date,12 the metrics informing global decision making need to be reviewed and carefully chosen.128 To avoid reifying existing inequalities and HIC biosecurity concerns (see the Metrics section), tracked policies should be based on and promote systems of contextual data gathering that are: multifactorial in their combination of existing and new metrics; integrated in their pooling of knowledge from different One Health and regional contexts; and empowering by conferring agency to local communities.
Multifactorial
Achieving effective tracked interventions requires a unifying global set of multifactorial metrics. To enable the rigorous evaluation of policies, multifactorial metrics need to simultaneously take into account antibiotic access, AMR and stewardship, but avoid rewarding short-termist gaming such as relabelling disease definitions, disincentivising healthcare-seeking behaviour and decontextualising surveillance (see the Inequality section).128 154 Standardised terminology and transparent AMR and drug usage surveillance are essential prerequisites for the design of meaningful international interventions. However, focusing too narrowly on reducing drug usage and misuse will not curb microbial threats (see Implementation section). Vice versa, focusing only on providing drugs without supporting additional means to reduce disease burdens will achieve little in the long term. Since 2018, several ways have been proposed to integrate AMR into the UN SDG framework. The most recent proposal is to ‘reduce the percentage of bloodstream infections due to selected antimicrobial resistant organisms’ and has been recommended to go forward to the UN Statistical Commission for inclusion in SDG 3 (Good Health and Well-being).73 This is one promising way to address stewardship without detracting from the goals of antibiotic access and disease prevention (see the Metrics section). There is, however, an additional need for new multifactorial metrics that also encompass AMR’s environmental and animal health dimensions as well as local access to drugs, WASH, vaccines and coselection for resistance by other antimicrobial substances. The new monitoring and evaluation framework proposed by FAO, OIE and WHO in 2019 is an important step in this direction.155
Integrated
In addition to drawing on multifactorial metrics, policy tracking should aim to integrate metrics across domains: taking into account the legacies of pre-existing interventions, improving knowledge integration across One Health sectors and incorporating knowledge generated in other geographical and social contexts. Enhancing the integration of international knowledge gathering will strengthen regionally nuanced decision making. Since the 1940s, successive generations of regulators have tried to manage the antibiotic commons by focusing on one form of intervention like ‘rational’ antibiotic use, reducing antibiotic use via statutory bans or non-statutory incentives and replacing antibiotics (eg, using metals in animal feeds). However, lack of cross-sectoral and international integration meant that benefits were often short-lived and had little effect on global drug usage or AMR.34 76 137 156 157 Regulatory silos at the national and international level have also repeatedly impeded the transmission of knowledge generated in one sector to other sectors—something that is exacerbated by the fact that animal health, medical and environmental regulators rarely interact on equal terms.158–160 In the case of AMR, the result was a lack of long-term strategic planning, a fragmentation of international policies and basic metrics (see the Metrics section)—and a tendency to reinvent the wheel—for example, the almost decennial recurrence of official warnings about post-antibiotic futures and ‘rational’ antibiotic use campaigns.77 161 Developing equitable structural policy frameworks thus not only depends on evaluating progress with multifactorial metrics but also on actively integrating knowledge throughout the One Health domains, leveraging existing national and regional policy frameworks and retaining institutional knowledge.
Empowering
Developing multifactorial and integrated metrics will achieve little if global AMR and usage data continues to be generated and made available unevenly. Equitably boosting laboratory and data analysis capacity is a prerequisite for strengthening the ability of those on the front lines of human, animal and plant health to devise their own solutions and generate accurate data for the global community. For example, in 2010, the Danish Yellow Card Initiative required farmers and veterinarians to track and record on farm antibiotic use. The initiative complemented low-granularity sales data and helped respective communities better understand what they were doing and grow support for stewardship efforts.54 In LMICs, enhancing national and local capacity to generate data can have similar effects. Being able to produce and wield robust surveillance data can increase the political weight of LMIC concerns at the international level. OIE, WHO and the UK Fleming Fund are already strengthening LIC usage and AMR surveillance capacity. However, organisations still lack sufficient resources to sustainably support laboratories and countries to enable them to publish accurate country-level data.29 New multifactorial and integrated metrics are also needed to produce data that is meaningful in settings without formal health and veterinary care systems. In the long term, reducing reliance on decontextualised data gathering like traveller surveillance and restructuring reporting formats to better reflect varying circumstances (see the Inequality section) will significantly enhance the evidence base for truly structural and equitable international antibiotic policy-making.
Conclusion
The past eight decades have seen antibiotic policy-makers struggle to overcome problematic metrics, narrow prioritisations, implementation deficits and global inequalities. The need for integrated architectures that act across existing silos to push evidence into action on AMR is being met through United Nations mandated mechanisms.10 To move beyond previous impasses, international policy will have to take seriously the infrastructural dimensions of antibiotic use, provide equitable solutions for communities across the globe and develop new forms of tracking progress that are multifactorial, integrated and empowering for the communities employing them.
Policies that take into account antibiotics’ SET have the greatest potential to sustainably adapt the way the global antibiotic commons are managed and accessed. As highlighted in our ideal-type example of multifactorial metrics and equitable capacity building in global food production (figure 2), SET policies have the potential to foster win-win situations for HIC and LMIC participants alike.
Figure 2.
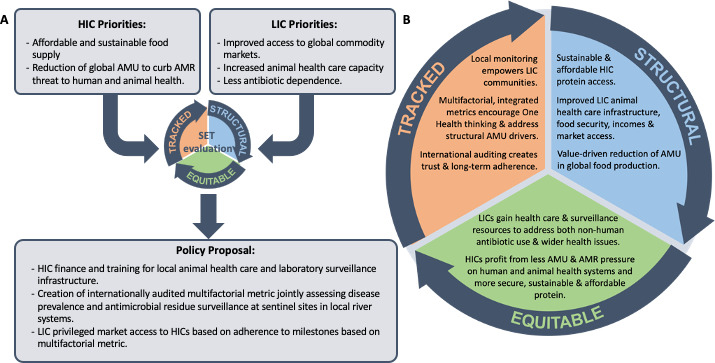
An ideal-type set of interventions for international food production. Ideal-type example of how using reflective policy-making in accordance with SET hallmarks could inform the design of equitable trade arrangements to: satisfy high income country demand for affordable sustainably produced protein; fulfil low income country calls for structural healthcare and surveillance capacity building and market access; encourage value driven. One health stewardship with multifactorial metrics integrating data on animal health with low-cost environmental sentinel monitoring for antimicrobial residues as a proxy for regional antimicrobial use (AMU). AMR, antimicrobial resistance; SET, Structural, Equitable and Tracked.
If the ultimate goal of antibiotic policy is to reduce mortality and morbidity resulting from treatable infections, then we need to adapt our food and health systems to provide optimal access to effective antibiotic interventions when they are needed—and simultaneously reduce the need for these interventions. This dual approach requires polices that not only focus on ‘quick fixes’106 for existing systems and behavioural modifications at the level of the individual. Instead, policies should consistently seek to adapt the wider physical and cultural infrastructures antibiotics are embedded in.
AMR is not a problem to be solved but a phenomenon to be continuously managed. Individual policies may not address all identified problem areas or integrate each of our three intervention hallmarks. However, we believe that our multidisciplinary SET of hallmarks can serve as a compass to critically evaluate and improve antibiotic policy in the present and for decades to come.
Acknowledgments
We are grateful to all correspondents and participants of the 2019 workshop for sharing their insights and expertise. The workshop and activity for this manuscript was supported by the Antimicrobials in Society (AMIS) programme (https://antimicrobialsinsociety.org/). The authors would like to thank Charlotte Kirchhelle for her help in preparing the figures of this article.
Footnotes
Handling editor: Seye Abimbola
Twitter: @Kirchhelle, @BroomAlex, @IsabelFrost19, @shoffmania, @koutterson, @anthroamr, @OxonAndrew
Contributors: CK and CC conceived the concept and cowrote this article with contributions from PA, AB, KC, JPF, NF, IF, CG, SH, SJH, JL, SN, KO, SHP, SR, APR, SRVK, ACS, ADS, LS, ET. CC acquired funding for the workshop and the articles.
Funding: AMIS is funded by The Antimicrobial Resistance Cross Council Initiative supported by the seven research councils in partnership with other funders. The lead funders are the Economic and Social Research Council (ESRC) with the Department of Health and the Arts and Humanities Research Council (AHRC). Kirchhelle’s work was supported by a Wellcome Trust University Award at University College Dublin and the Oxford Martin School. Fortané was supported by INRAE (ANR-18-CE03-001), Frost by CDDEP, Nayiga by ESRC, Taylor by the UK Fleming Fund. APR would like to acknowledge funding from the AMR Cross-Council Initiative through a grant from the Medical Research Council, a Council of UK Research and Innovation (Grant Number; MR/S004793/1)
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect those of CIHR, the Government of Canada, or WHO.
Competing interests: SH is Scientific Director of CIHR’s Institute of Population and Public Health and CIHR’s Scientific Co-Lead for Antimicrobial Resistance. He is Director of the WHO Collaborating Centre on Global Governance of Antimicrobial Resistance. KO in principal investigator of CARB-X, a project at Boston University (my employer), funded by three governments (US, UK and Germany) and two charitable foundations (Wellcome Trust and the Bill & Melinda Gates Foundation). CARB-X is a non-profit, making grants for preclinical antibacterial research. I do not view this as a conflict, but disclose in an abundance of caution. APR is the co-ordinator of the JPIAMR funded Network NEAR-AMR. ADS reports grants from ReAct-Action on Antibiotic Resistance and from Open Society Foundation during the conduct of the study. He served as Co-Convener of the UN Interagency Coordination Group on Antimicrobial Resistance (2018–2019), as a member of the Expert Commission on Addressing the Livestock Contribution to the Antibiotic Resistance Crisis (2016–2017), as a commissioned author to the UK Commission on AMR on 'A Framework for Costing the Lowering of Antimicrobial Use in Food Animal Production' (2016), as Head of the Secretariat of the Antibiotic Resistance Coalition, and as a Member of the Working Group on Antibiotic Resistance for the President’s Council of Advisors on Science and Technology (2013–2014).
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: There are no data in this work.
References
- 1.Chandler CIR, Hutchinson E, Hutchison C. Addressing antimicrobial resistance through social theory. An Anthropologically oriented report. London: London School of Hygiene & Tropical Medicine, 2016. [Google Scholar]
- 2.Hoffman SJ, Caleo GM, Daulaire N, et al. Strategies for achieving global collective action on antimicrobial resistance. Bull World Health Organ 2015;93:867–76. 10.2471/BLT.15.153171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hollis A, Maybarduk P. Antibiotic resistance is a tragedy of the commons that necessitates global cooperation. J Law Med Ethics 2015;43 Suppl 3:33–7. 10.1111/jlme.12272 [DOI] [PubMed] [Google Scholar]
- 4.Cars O, Högberg LD, Murray M, et al. Meeting the challenge of antibiotic resistance. BMJ 2008;337:a1438. 10.1136/bmj.a1438 [DOI] [PubMed] [Google Scholar]
- 5.Laxminarayan R, Malani A. Extending the cure: policy responses to the growing threat of antibiotic resistance: Earthscan, 2007. [Google Scholar]
- 6.Outterson K. The vanishing public domain: antibiotic resistance, pharmaceutical innovation and intellectual property law. Lawreview 2005;67:67 10.5195/LAWREVIEW.2005.70 [DOI] [Google Scholar]
- 7.Hoffman SJ, Outterson K. Introduction: what will it take to address the global threat of antibiotic resistance? J Law Med Ethics 2015;43 Suppl 3:6–11. 10.1111/jlme.12267 [DOI] [PubMed] [Google Scholar]
- 8.Rogers Van Katwyk S, Weldon I, Giubilini A, et al. Making use of existing international legal mechanisms to manage the global antimicrobial commons: identifying legal Hooks and institutional mandates. Health Care Anal 2020;105. 10.1007/s10728-020-00393-y. [Epub ahead of print: 31 Mar 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wernli D, Haustein T, Conly J, et al. A call for action: the application of the International health regulations to the global threat of antimicrobial resistance. PLoS Med 2011;8:e1001022. 10.1371/journal.pmed.1001022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.IACG No time to wait: securing the future from drug-resistant infections. Report to the Secretar-General of the United nations. New York: Interagency Coordination Group on Antimicrobial Resistance, 2019. [Google Scholar]
- 11.WHO/OIE/FAO Global action plan on antimicrobial resistance. Geneva: World Health Organisation, 2015. [Google Scholar]
- 12.Van Katwyk SR, Balasegaram M, Boriello P, et al. A roadmap for sustainably governing the global antimicrobial commons. Lancet 2019;394:1788–9. 10.1016/S0140-6736(19)32767-9 [DOI] [PubMed] [Google Scholar]
- 13.Rogers Van Katwyk S, Grimshaw JM, Nkangu M, et al. Government policy interventions to reduce human antimicrobial use: a systematic review and evidence MAP. PLoS Med 2019;16:e1002819. 10.1371/journal.pmed.1002819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kirchhelle C, Broom A, Chandler C, et al. The Informational Deluge - A Review of 72 years of antibiotic evaluation, surveillance, regulation, and calls to actionin preparation. [Google Scholar]
- 15.Tackling antimicrobial resistance 2019–2024 The UK’s five-year national action plan. London Her Majesty’s Government, 2019. [DOI] [PubMed] [Google Scholar]
- 16.WHO Who global principles for the containment of antimicrobial resistance in animals intended for food: report of a who consultation with the participation of the food and agriculture organization of the United nations and the office international des Epizooties, Geneva, Switzerland 5-9 June 2000. World Health Organization, 2000. [Google Scholar]
- 17.Hoffman SJ, Outterson K, Røttingen J-A, et al. An international legal framework to address antimicrobial resistance: SciELO public health, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kirk RGW. Recovering The Principles of Humane Experimental Technique: The 3Rs and the Human Essence of Animal Research. Sci Technol Human Values 2018;43:622–48. 10.1177/0162243917726579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.So AD, Ruiz-Esparza Q, Gupta N, et al. 3Rs for innovating novel antibiotics: sharing resources, risks, and rewards. BMJ 2012;344:e1782–4. 10.1136/bmj.e1782 [DOI] [PubMed] [Google Scholar]
- 20.Bank W. Pulling together to beat superbugs. knowledge and Implementaiton gaps in addressing antimicrobial resistance. Washington DC: World Bank, 2019. [Google Scholar]
- 21.WHO Turning plans into action for antimicrobial resistance (AMR). Working paper 2.0: implementation and coordination. Geneva: World Health Organization, 2019. [Google Scholar]
- 22.Dar OA, Hasan R, Schlundt J, et al. Exploring the evidence base for national and regional policy interventions to combat resistance. Lancet 2016;387:285–95. 10.1016/S0140-6736(15)00520-6 [DOI] [PubMed] [Google Scholar]
- 23.Summers WC. Microbial drug resistance: a historical perspective. Bacterial Resistance to Antimicrobials 2008;2:1–9. [Google Scholar]
- 24.Gradmann C. Magic bullets and moving targets: antibiotic resistance and experimental chemotherapy, 1900-1940. Dynamis 2001;31:305–21. 10.4321/S0211-95362011000200003 [DOI] [PubMed] [Google Scholar]
- 25.Fortané N, Dispositif-Frontière LSC. La triple ontologie des bactéries résistantes d’origine animale. Revue d'Anthropologie des Connaissances 2015;9:265–90. [Google Scholar]
- 26.Gradmann C. Sensitive matters: the world health organisation and antibiotic resistance testing, 1945-1975. Soc His Med 2013;26:555–74. 10.1093/shm/hkt018 [DOI] [Google Scholar]
- 27.Drlica K, Perlin DS, Resistance A. Understanding and responding to an emerging crisis. Upper Saddle River: Pearson Education, 2011. [Google Scholar]
- 28.WHO WHONET software platform. Geneva: World Health Organisation. [Google Scholar]
- 29.WHO Global antimicrobial resistance surveillance system (glass) report: early implementation 2017-2018. Geneva: WHO, 2019. [Google Scholar]
- 30.van der Bij AK, van Dijk K, Muilwijk J, et al. Clinical breakpoint changes and their impact on surveillance of antimicrobial resistance in Escherichia coli causing bacteraemia. Clin Microbiol Infect 2012;18:E466–72. 10.1111/j.1469-0691.2012.03996.x [DOI] [PubMed] [Google Scholar]
- 31.Kassim A, Omuse G, Premji Z, et al. Comparison of clinical laboratory Standards Institute and European Committee on antimicrobial susceptibility testing guidelines for the interpretation of antibiotic susceptibility at a university teaching hospital in Nairobi, Kenya: a cross-sectional study. Ann Clin Microbiol Antimicrob 2016;15:21. 10.1186/s12941-016-0135-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saha S, Saha S, Saha SK. Global science: barriers in Bangladesh. Elife 2018;7:e41926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Musicha P, Cornick JE, Bar-Zeev N, et al. Trends in antimicrobial resistance in bloodstream infection isolates at a large urban hospital in Malawi (1998-2016): a surveillance study. Lancet Infect Dis 2017;17:1042–52. 10.1016/S1473-3099(17)30394-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kirchhelle C. Pyrrhic progress: antibiotics in Anglo-American food production (1949-2018). New Brunswick: Rutgers University Press, 2020. [PubMed] [Google Scholar]
- 35.Hammerum AM, Heuer OE, Emborg H-D, et al. Danish integrated antimicrobial resistance monitoring and research program. Emerg Infect Dis 2007;13:1633–9. 10.3201/eid1311.070421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mölstad S, Löfmark S, Carlin K, et al. Lessons learnt during 20 years of the Swedish strategic programme against antibiotic resistance. Bull World Health Organ 2017;95:764–73. 10.2471/BLT.16.184374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tamura Y. The Japanese veterinary antimicrobial resistance monitoring system (JVARM). OIE international standards on Antimicrobial Resistance, 2003: 206–10. [Google Scholar]
- 38.OIE OIE annual report on antimicrobial agents intended for use in animals. better understanding of the global situation. third annual report. Paris: World Organisation for Animal Health (OIE), 2018. [Google Scholar]
- 39.EMA Trends in the sales of veterinary antimicrobal agents in nine European countries. reporting period: 2005-2009. Brussels: European Medicines Agency, 2011. [Google Scholar]
- 40.VMD Uk veterinary antibiotic resistance and sales surveillance report. UK-VARSS 2018. UK-VARSS new Haw veterinary medicines Directorate, 2019. [Google Scholar]
- 41.Statens Serum Institut, NF Institute DANMAP 2018 - Use of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from food animals, food and humans in Denmark. Copenhagen: Statens Serum Institut/ National Food Institute, 2019. [Google Scholar]
- 42.FDA 2018 summary report on antimicrobials sold or distributed for use in food-producing animals. Washington: Food and Drugs Administration, 2019. [Google Scholar]
- 43.English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2018-2019. London: Public Health England, 2019. [Google Scholar]
- 44.Iroh Tam P-Y, Musicha P, Kawaza K, et al. Emerging resistance to empiric antimicrobial regimens for pediatric bloodstream infections in Malawi (1998-2017). Clin Infect Dis 2019;69:61–8. 10.1093/cid/ciy834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schnall J, Rajkhowa A, Ikuta K, et al. Surveillance and monitoring of antimicrobial resistance: limitations and lessons from the gram project. BMC Med 2019;17:176. 10.1186/s12916-019-1412-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aarestrup FM. Monitoring of antimicrobial resistance among food animals: principles and limitations. J Vet Med B Infect Dis Vet Public Health 2004;51:380–8. 10.1111/j.1439-0450.2004.00775.x [DOI] [PubMed] [Google Scholar]
- 47.Van Boeckel TP, Gandra S, Ashok A, et al. Global antibiotic consumption 2000 to 2010: an analysis of national pharmaceutical sales data. Lancet Infect Dis 2014;14:742–50. 10.1016/S1473-3099(14)70780-7 [DOI] [PubMed] [Google Scholar]
- 48.Van Boeckel TP, Pires J, Silvester R, et al. Global trends in antimicrobial resistance in animals in low- and middle-income countries. Science 2019;365:eaaw1944. 10.1126/science.aaw1944 [DOI] [PubMed] [Google Scholar]
- 49.Giulieri SG, Tong SYC, Williamson DA. Using genomics to understand meticillin- and vancomycin-resistant Staphylococcus aureus infections. Microb Genom 2020;6:mgen000324. 10.1099/mgen.0.000324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Baker S, Thomson N, Weill F-X, et al. Genomic insights into the emergence and spread of antimicrobial-resistant bacterial pathogens. Science 2018;360:733–8. 10.1126/science.aar3777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bennett RJ, Baker KS. Looking backward to move forward: the utility of sequencing historical bacterial genomes. J Clin Microbiol 2019;57 10.1128/JCM.00100-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Barber M, Dutton AA, Beard MA, et al. Reversal of antibiotic resistance in hospital staphylococcal infection. Br Med J 1960;1:11–17. 10.1136/bmj.1.5165.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kahn LH. One health and the politics of antimicrobial resistance Baltimore. Johns Hopkins University Press, 2016. [Google Scholar]
- 54.FAO Tackling antimicrobial use and resistance in pig production. lessons learned in Denmark. Rome: Food and Agricultural Organisation/ Ministry of Environment and Food of Denmark, 2019. [Google Scholar]
- 55.Sørum M, Johnsen PJ, Aasnes B, et al. Prevalence, persistence, and molecular characterization of glycopeptide-resistant enterococci in Norwegian poultry and poultry farmers 3 to 8 years after the ban on avoparcin. Appl Environ Microbiol 2006;72:516–21. 10.1128/AEM.72.1.516-521.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Walsh TR, Wu Y. China bans colistin as a feed additive for animals. Lancet Infect Dis 2016;16:1102–3. 10.1016/S1473-3099(16)30329-2 [DOI] [PubMed] [Google Scholar]
- 57.Liu Y-Y, Wang Y, Walsh TR, et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis 2016;16:161–8. 10.1016/S1473-3099(15)00424-7 [DOI] [PubMed] [Google Scholar]
- 58.Shen Z, Wang Y, Shen Y, et al. Early emergence of mcr-1 in Escherichia coli from food-producing animals. Lancet Infect Dis 2016;16:293 10.1016/S1473-3099(16)00061-X [DOI] [PubMed] [Google Scholar]
- 59.WHO Library of national action plans. Geneva: World Health Organisation, 2020. [Google Scholar]
- 60.OIE OIE list of antimicrobial agents of veterinary importance: world organisation for animal health, 2019. [Google Scholar]
- 61.FAO/OIE/WHO Second joint FAO/OIE/WHO expert workshop on non-human antimicrobial usage and antimicrobial resistance: management options. Oslo, Norway. Geneva: World Health Organisation, 2004. [Google Scholar]
- 62.WHO Executive summary. The selection and use of essential medicines 2019. Report of the 22nd who expert Committee on the selection and use of essential medicines. Geneva: World Health Organisation, 2019. [Google Scholar]
- 63.Sharland M, Pulcini C, Harbarth S, et al. Classifying antibiotics in the who essential medicines list for optimal use-be aware. Lancet Infect Dis 2018;18:18–20. 10.1016/S1473-3099(17)30724-7 [DOI] [PubMed] [Google Scholar]
- 64.Góchez D, Raicek M, Pinto Ferreira J, et al. OIE annual report on antimicrobial agents intended for use in animals: methods used. Front Vet Sci 2019;6:317. 10.3389/fvets.2019.00317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.WHO Who methodology for a global programme on surveillance of antimicrobial consumption. Geneva: World Health Organisation, 2016. [Google Scholar]
- 66.Queenan K, Chandler CIR, Goodman C. A review of methods and metrics for studying human and livestock antibiotic use at the granular level. London LSHTM, 2017. [Google Scholar]
- 67.Queenan K, Chandler CIR, Goodman C. Meeting report: metrics and methods for assessing antibiotic use at the granular level in humans and livestock in LMICs. London: LSHTM, 2017. [Google Scholar]
- 68.WHO Global priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics. Geneva: World Health Organization, 2017. [Google Scholar]
- 69.OIE Development and harmonisation of national antimicrobial resistance surveillance and monitoring programmes for aquatic animals. aquatic animal health code. Paris: World Organisation For Animal Health, 2012. [Google Scholar]
- 70.OIE Harmonisation of national antimicrobial resistance surveillance and monitoring programmes. Terrestial animal health code. Paris: World Organisation for Animal health, 2018. [Google Scholar]
- 71.Savoldi A, Carrara E, Gladstone BP, et al. Gross national income and antibiotic resistance in invasive isolates: analysis of the top-ranked antibiotic-resistant bacteria on the 2017 who priority list. J Antimicrob Chemother 2019;74:3619–25. 10.1093/jac/dkz381 [DOI] [PubMed] [Google Scholar]
- 72.Pitzer VE, Meiring J, Martineau FP, et al. The invisible burden: diagnosing and Combatting typhoid fever in Asia and Africa. Clin Infect Dis 2019;69:S395–401. 10.1093/cid/ciz611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.So A, Sharma P. Tracking antimicrobial resistance in the sustainable development goals, 2019. Available: http://sdg.iisd.org/commentary/guest-articles/tracking-antimicrobial-resistance-in-the-sustainable-development-goals/
- 74.Singer AC, Shaw H, Rhodes V, et al. Review of antimicrobial resistance in the environment and its relevance to environmental regulators. Front Microbiol 2016;7:7. 10.3389/fmicb.2016.01728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.WHO Critically important antimicrobials for human medicine - 5th review. Geneva: WHO, 2017. [Google Scholar]
- 76.Podolsky SH. The evolving response to antibiotic resistance (1945–2018). Palgrave Commun 2018;4 10.1057/s41599-018-0181-x [DOI] [Google Scholar]
- 77.Podolsky SH. The antibiotic era. reform, resistance and the pursuit of a rational therapeutics. Baltimore: Johns Hopkins Press, 2015. [Google Scholar]
- 78.Gradmann C. Re-Inventing infectious disease: antibiotic resistance and drug development at the Bayer company 1945-80. Med Hist 2016;60:155–80. 10.1017/mdh.2016.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Schröter HG. Zwischen tradition und Fortschritt. AUS Der Geschichte Der Pharmabereiche von Bayer, Hoechst und Schering von 1935-1975. Frankfurter Historische Abhandlungen 2005;43. [Google Scholar]
- 80.Lie AK, Standards P. Producing Standards, producing the Nordic region: antibiotic susceptibility testing, from 1950-1970. Sci Context 2014;27:215–48. 10.1017/S0269889714000052 [DOI] [PubMed] [Google Scholar]
- 81.Hobaek B, Lie AK. Less Is More: Norwegian Drug Regulation, Antibiotic Policy, and the "Need Clause". Milbank Q 2019;97:762–95. 10.1111/1468-0009.12405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.WHO Who report on surveillance of antibiotic consumption. early implementation 2016-2018. Geneva: WHO, 2018. [Google Scholar]
- 83.ECDC Antimicrobial consumption in the EU/EEA. annual epidemiological report for 2018. Brussels: European Centre for Disease Control, 2019. [Google Scholar]
- 84.Krockow EM, Tarrant C. The International dimensions of antimicrobial resistance: contextual factors shape distinct ethical challenges in South Africa, Sri Lanka and the United Kingdom. Bioethics 2019;33:756–65. 10.1111/bioe.12604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kirchhelle C, Dyson ZA, Dougan G. A Biohistorical perspective of typhoid and antimicrobial resistance. Clin Infect Dis 2019;69:S388–94. 10.1093/cid/ciz556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Dyson ZA, Klemm EJ, Palmer S, et al. Antibiotic resistance and typhoid. Clin Infect Dis 2019;68:S165–70. 10.1093/cid/ciy1111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Huang SS, Labus BJ, Samuel MC, et al. Antibiotic resistance patterns of bacterial isolates from blood in San Francisco County, California, 1996-1999. Emerg Infect Dis 2002;8:195–201. 10.3201/eid0802.010102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kirchhelle C. Pharming animals: a global history of antibiotics in food production (1935–2017, 2018: 96. [Google Scholar]
- 89.Falagas ME, Kasiakou SK, Saravolatz LD. Colistin: the revival of polymyxins for the management of multidrug-resistant gram-negative bacterial infections. Clin Infect Dis 2005;40:1333–41. 10.1086/429323 [DOI] [PubMed] [Google Scholar]
- 90.Littmann J, Viens AM. The ethical significance of antimicrobial resistance. Public Health Ethics 2015;8:phv025–24. 10.1093/phe/phv025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.McMillen CW, Tuberculosis D, Global History A. To the present. New Haven and London: Yale University Press, 2015: 1900. [Google Scholar]
- 92.Neville K, Bromberg A, Bromberg R, et al. The third epidemic--multidrug-resistant tuberculosis. Chest 1994;105:45–8. 10.1378/chest.105.1.45 [DOI] [PubMed] [Google Scholar]
- 93.Young DM, Harris HW, Charlebois ED, et al. An epidemic of methicillin-resistant Staphylococcus aureus soft tissue infections among medically underserved patients. Arch Surg 2004;139:947–53. 10.1001/archsurg.139.9.947 [DOI] [PubMed] [Google Scholar]
- 94.Doron A, Broom A. The spectre of Superbugs: waste, structural violence and antimicrobial resistance in India. Worldwide Waste: Journal of Interdisciplinary Studies 2019;2 10.5334/wwwj.20 [DOI] [Google Scholar]
- 95.AAo S, Hindiyeh M, Sabateen AA. Embedding quality improvement through a learning collaborative to reduce and sustain hospital-acquired infections in the West bank. AMR Control, 2017: 96–8. [Google Scholar]
- 96.Davies M, Stockton B. Unseen enemy: doctors in Gaza. Bureau of Investigative Journalism, 2018. [Google Scholar]
- 97.Singer AC, Colizza V, Schmitt H, et al. Assessing the ecotoxicologic hazards of a pandemic influenza medical response. Environ Health Perspect 2011;119:1084–90. 10.1289/ehp.1002757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Rawson TM, Moore LSP, Castro-Sanchez E, et al. COVID-19 and the potential long-term impact on antimicrobial resistance. J Antimicrob Chemother 2020;75:1681–4. 10.1093/jac/dkaa194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Podolsky SH. Historical perspective on the rise and fall and rise of antibiotics and human weight gain. Ann Intern Med 2017;166:133–8. 10.7326/M16-1855 [DOI] [PubMed] [Google Scholar]
- 100.Millar M. Inequality and antibiotic resistance: a contractualist perspective. Bioethics 2019;33:749–55. 10.1111/bioe.12654 [DOI] [PubMed] [Google Scholar]
- 101.Poirot E, Skarbinski J, Sinclair D, et al. Mass drug administration for malaria. Cochrane Database Syst Rev 2013;44 10.1002/14651858.CD008846.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bogoch II, Utzinger J, Lo NC, et al. Antibacterial mass drug administration for child mortality reduction: opportunities, concerns, and possible next steps. PLoS Negl Trop Dis 2019;13:e0007315. 10.1371/journal.pntd.0007315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Keenan JD, Arzika AM, Maliki R, et al. Longer-Term assessment of azithromycin for reducing childhood mortality in Africa. N Engl J Med 2019;380:2207–14. 10.1056/NEJMoa1817213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Romani L, Marks M, Sokana O, et al. Efficacy of mass drug administration with ivermectin for control of scabies and impetigo, with coadministration of azithromycin: a single-arm community intervention trial. Lancet Infect Dis 2019;19:510–8. 10.1016/S1473-3099(18)30790-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Rid A, Littmann J, Buyx A. Evaluating the risks of public health programs: rational antibiotic use and antimicrobial resistance. Bioethics 2019;33:734–48. 10.1111/bioe.12653 [DOI] [PubMed] [Google Scholar]
- 106.Denyer Willis L, Chandler C. Quick fix for care, productivity, hygiene and inequality: reframing the entrenched problem of antibiotic overuse. BMJ Glob Health 2019;4:e001590. 10.1136/bmjgh-2019-001590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Pearson M, Chandler C. Knowing antmicrobial resistance in practice: a multi-country qualitative study with human and animal healthcare professionals. Glob Health Action 2019;12:1599560. 10.1080/16549716.2019.1599560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Rochford C, Sridhar D, Woods N, et al. Global governance of antimicrobial resistance. The Lancet 2018;391:1976–8. 10.1016/S0140-6736(18)31117-6 [DOI] [PubMed] [Google Scholar]
- 109.UN Paris agreement. New York: United Nations, 2016. [Google Scholar]
- 110.Rogers Van Katwyk S, Giubilini A, Kirchhelle C, et al. Exploring models for an international legal agreement on the global antimicrobial commons: lessons from climate agreements. Health Care Anal 2020;387. 10.1007/s10728-019-00389-3. [Epub ahead of print: 21 Jan 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Clift C. Review of progress on antimicrobial resistance: background and analysis. London: Chatham House: The Royal Institute of International Affairs, 2019. [Google Scholar]
- 112.Ozawa S, Evans DR, Bessias S, et al. Prevalence and estimated economic burden of substandard and Falsified medicines in low- and middle-income countries: a systematic review and meta-analysis. JAMA Netw Open 2018;1:e181662. 10.1001/jamanetworkopen.2018.1662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Morgan DJ, Okeke IN, Laxminarayan R, et al. Non-Prescription antimicrobial use worldwide: a systematic review. Lancet Infect Dis 2011;11:692–701. 10.1016/S1473-3099(11)70054-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ahmad R, Zhu NJ, Leather AJM, et al. Strengthening strategic management approaches to address antimicrobial resistance in global human health: a scoping review. BMJ Glob Health 2019;4:e001730. 10.1136/bmjgh-2019-001730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Pokharel S, Raut S, Adhikari B. Tackling antimicrobial resistance in low-income and middle-income countries. BMJ Glob Health 2019;4:e002104. 10.1136/bmjgh-2019-002104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Pokharel S, Adhikari B. Antimicrobial resistance and over the counter use of drugs in Nepal. J Glob Health 2020;10:010360. 10.7189/jogh.10.010360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.FAO/OIE/WHO Monitoring global progress for addressing antimicrobial resistance (AMR). analysis report of the second round of results of AMR country self-assessment survey. Geneva: FAO/ OIE/ WHO, 2018. [Google Scholar]
- 118.Goutard FL, Bordier M, Calba C, et al. Antimicrobial policy interventions in food animal production in South East Asia. BMJ 2017;358:j3544–41. 10.1136/bmj.j3544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.So AD, Shah TA, Roach S, et al. An integrated systems approach is needed to ensure the sustainability of antibiotic effectiveness for both humans and animals. J Law Med Ethics 2015;43 Suppl 3:38–45. 10.1111/jlme.12273 [DOI] [PubMed] [Google Scholar]
- 120.EU MEPs back plans to halt spread of drug resistance from animals to humans. Brussels: European Parliament, 2018. [Google Scholar]
- 121.Broom A, Kenny K, Kirby E, et al. Improvisation, therapeutic brokerage and antibiotic (mis)use in India: a qualitative interview study of Hyderabadi physicians and pharmacists. Crit Public Health 2020;30:16–27. 10.1080/09581596.2018.1516032 [DOI] [Google Scholar]
- 122.Broom J, Broom A, Kirby E. Context-Sensitive antibiotic optimization: a qualitative interviews study of a remote Australian hospital setting. J Hosp Infect 2018;100:265–9. 10.1016/j.jhin.2018.06.002 [DOI] [PubMed] [Google Scholar]
- 123.Hinchliffe S, Butcher A, Rahman MM. The AMR problem: demanding economies, biological margins, and co-producing alternative strategies. Palgrave Commun 2018;4 10.1057/s41599-018-0195-4 [DOI] [Google Scholar]
- 124.Figuié M. Towards a global governance of risks: international health organisations and the surveillance of emerging infectious diseases. J Risk Res 2014;17:469–83. 10.1080/13669877.2012.761277 [DOI] [Google Scholar]
- 125.Manton J, Gorsky M. Health planning in 1960s Africa: international health organisations and the post-colonial state. Med Hist 2018;62:425–48. 10.1017/mdh.2018.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Packard R. A history of global health: interventions into the lives of other peoples. Baltimore: Johns Hopkins Press, 2016. [Google Scholar]
- 127.Singer AC, Kirchhelle C, Roberts AP. (Inter)nationalising the antibiotic research and development pipeline. Lancet Infect Dis 2020;20:e54–62. 10.1016/S1473-3099(19)30552-3 [DOI] [PubMed] [Google Scholar]
- 128.Adams V. Metrics: what counts in global health. Duke University Press, 2016. [Google Scholar]
- 129.Bhutta ZA, Sommerfeld J, Lassi ZS, et al. Global burden, distribution, and interventions for infectious diseases of poverty. Infect Dis Poverty 2014;3:21. 10.1186/2049-9957-3-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.WHO Who Factsheet: drinking water. Geneva: World Health Organisation, 2019. [Google Scholar]
- 131.WHO Who Factsheet: sanitation. Geneva: World Health Organisation, 2019. [Google Scholar]
- 132.OIE, WHO FAO. Technical brief on water, sanitation, hygiene and wastewater management to prevent infections and reduce the spread of AMR. Rome, Paris, Geneva: Food and Agriculture Organization, World Organisation for Animal Health, World Health Organization, 2020. [Google Scholar]
- 133.FAO The Fao action plan on antimicrobial resistance 2016-2020. Rome: FAO, 2016. [Google Scholar]
- 134.EU A European one health action plan against antimicrobial resistance (AMR). Brussels: European Union, 2017. [Google Scholar]
- 135.OIE The OIE strategy on AMR and the prudent use of antibiotics. Paris: World Organisation for Animal Health/ OIE, 2016. [Google Scholar]
- 136.Podolsky SH, Bud R, Gradmann C, et al. History teaches us that confronting antibiotic resistance requires stronger global collective action. J Law Med Ethics 2015;43 Suppl 3:27–32. 10.1111/jlme.12271 [DOI] [PubMed] [Google Scholar]
- 137.Glover RE, Dangoor M, Mays N. Educating patients or blaming them? public education campaigns on antibiotic resistance. BMJ Opinion 2019. [Google Scholar]
- 138.Commission E Com (2011) 748 final communication from the Commission to the European Parliament and Council – action plan against the rising threats from antimicrobial resistance Brussels. European Commission, 2011. [Google Scholar]
- 139.Indian Ministry of Environment FaCC GSR 44 (E) Draft Notification. The Gazette of India 2020 (No. 41 Part II - Section 3 - Sub-section (i)), 2020: 1–11. [Google Scholar]
- 140.IFPMA AMR Industry Alliance - 2020 Progress Report, 2020. [Google Scholar]
- 141.Gov.UK Uk five year antimicrobial resistance strategy and action plan 2013-2018, 2013. [Google Scholar]
- 142.FAO/WHO Joint FAO/WHO meeting in collaboration with OIE on foodborne antimicrobial resistance: role of the environment, crops and biocides. microbiological risk assessment series. Rome, 2019. [Google Scholar]
- 143.EMA Sales of veterinary antimicrobial agents in 31 European countries in 2017. trends from 2010 to 2017 ninth ESVAC report. Brussels: European Medicines Agency, 2019. [Google Scholar]
- 144.Nuffield Trust Antibiotic prescribing UK. London; 2019. [Google Scholar]
- 145.FDA Summary report on antimicrobials sold or distributed for use in food-producing animals. Washington DC: Food and Drugs Administration, 2018. [Google Scholar]
- 146.Wellcome Trust News Five pioneering ways to stop superbugs. 23.05.2019 ED. London, 2019. [Google Scholar]
- 147.Roope LSJ, Smith RD, Pouwels KB, et al. The challenge of antimicrobial resistance: what economics can contribute. Science 2019;364:eaau4679. 10.1126/science.aau4679 [DOI] [PubMed] [Google Scholar]
- 148.Silbergeld EK. Chickenizing Farms & Food. How Industrial Meat Production Endangers Workers, Animals, and Consumers. Baltimore: Johns Hopkins University Press, 2016. [Google Scholar]
- 149.Klein EY, Van Boeckel TP, Martinez EM, et al. Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc Natl Acad Sci U S A 2018;115:E3463–70. 10.1073/pnas.1717295115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Van Boeckel TP, Brower C, Gilbert M, et al. Global trends in antimicrobial use in food animals. Proc Natl Acad Sci U S A 2015;112:5649–54. 10.1073/pnas.1503141112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Outterson K, Powers JH, Daniel GW, et al. Repairing the broken market for antibiotic innovation. Health Aff 2015;34:277–85. 10.1377/hlthaff.2014.1003 [DOI] [PubMed] [Google Scholar]
- 152.Outterson K. New business models for sustainable antibiotics. London Chatham House - Royal Institute of International Affairs, 2014. [Google Scholar]
- 153.IACG No time to wait: securing the future from drug-resistant infections. New York Interagency coordination group on antimicrobial resistance, 2019. [Google Scholar]
- 154.Reddy SG. Economics’ Biggest Success Story Is a Cautionary Tale. Foreign Policy, 2019. [Google Scholar]
- 155.FAO/OIE/WHO Monitoring and evaluation of the global action plan on antimicrobial resistance. framework and recommended indicators. Rome/ Paris/ Geneva: Food and Agricultural Organisation/ World Organisation for Animal Health/ World Health Organisation, 2019. [Google Scholar]
- 156.Gradmann C. From lighthouse to hothouse: Hospital hygiene, antibiotics and the evolution of infectious disease, 1950-1990. Hist Philos Life Sci 2017;40:8. 10.1007/s40656-017-0176-8 [DOI] [PubMed] [Google Scholar]
- 157.Kirchhelle C, Song S. Swann song: antibiotic regulation in British livestock production (1953-2006). Bull Hist Med 2018;92:317–50. 10.1353/bhm.2018.0029 [DOI] [PubMed] [Google Scholar]
- 158.Kirchhelle C. Between Bacteriology and Toxicology - Agricultural Antibiotics and US Risk Regulation : Creager ANH, Gaudilliere J-P, Risk on the table. New York: Berghahn, 2021. [Google Scholar]
- 159.Jerolmack C. Who's worried about turkeys? How 'organisational silos' impede zoonotic disease surveillance. Sociol Health Illn 2013;35:200–12. 10.1111/j.1467-9566.2012.01501.x [DOI] [PubMed] [Google Scholar]
- 160.Chien Y-J. How did international agencies perceive the avian influenza problem? The adoption and manufacture of the 'One World, One Health' framework. Sociol Health Illn 2013;35:213–26. 10.1111/j.1467-9566.2012.01534.x [DOI] [PubMed] [Google Scholar]
- 161.Podolsky SH, Lie AK. Futures and their uses: antibiotics and therapeutic revolutions. therapeutic revolutions: pharmaceuticals and social change in the twentieth century. Chicago: University of Chicago Press, 2016: 18–42. [Google Scholar]
- 162.Antimicrobials in Society [AMIS] Social Science and AMR Research Symposium - British Academy, London 2018. Available: https://antimicrobialsinsociety.org/events/social-science-and-amr-research-symposium/