Abstract
Objective
To determine whether exogenously reduced psychological distress reduces reported low‐back pain (LBP) and is associated with reduced medical visits for LBP.
Data Sources
National Health Interview Survey, National Ambulatory Medical Care Survey, National Hospital Ambulatory Medical Care Survey, 1998‐2004.
Study Design
We estimate a fuzzy regression discontinuity model in which a discontinuity in the prevalence of psychological distress is identified by exogenous national events. We examine whether this discontinuity induced a corresponding discontinuity in the prevalence of LBP. We additionally estimate a regression discontinuity model to determine associated changes in medical visits with LBP as the primary complaint.
Principal Findings
The prevalence of LBP was discontinuously reduced by one‐fifth due to the exogenous national discontinuous reduction in psychological distress. This discontinuity in LBP cannot be explained by discontinuities in employment, insurance, injuries/poisoning, general health status, or other factors. We find an associated three‐fifth discontinuous reduction in medical visits with LBP as the primary complaint.
Conclusions
On a monthly basis, 2.1 million (P < .01) adults ceased to suffer LBP due to the national reduction in psychological distress, and associated medical visits with LBP as the primary complaint declined by 685 000 (P < .01).
Keywords: low‐back pain, medical visits, psychological distress, regression discontinuity
1. INTRODUCTION
Approximately 65‐80 percent of individuals will experience low‐back pain (LBP) during their lifetime, and there were approximately 2.5 million medical visits for neck and/or back pain each month (primary or secondary diagnoses), on average, from 1999 to 2000. 1 , 2 The cost of LBP is over $100 billion annually, two‐thirds being due to lowered productivity and lost wages. 3
Numerous longitudinal studies find that in samples of individuals without psychological distress at baseline, LBP predicts future psychological distress (mood/anxiety disorders). 4 , 5 , 6 In contrast, numerous additional longitudinal studies find the reverse: In samples of individuals without LBP at baseline, psychological distress (mood/anxiety disorders) predicts future LBP. 5 , 7
Significant light is shed on this latter phenomenon by neurobiological research, which has identified biological mechanisms linking psychological distress and pain. Consider one form of psychological distress, anxiety, defined as apprehension about potential future threats, where the outcomes of such threats are uncertain. 8 , 9 This can result in hypervigilance that initiates neurobiological changes that can result in increased sensitivity to pain. 8 , 9 Human studies find that experimentally induced anxiety, via the introduction of anxiety‐promoting information, can increase sensitivity to pain. 8 , 10 , 11 , 12 , 13 , 14 , 15 , 16 Not only can sensitivity to pain be induced by anxiety‐promoting information, but pain itself can also be induced in previously pain‐free individuals by increasing anxiety as demonstrated in human experiments. 8 , 17 , 18 , 19 , 20 Both increased sensitivity to pain and pain initiation may also occur in some types of depression due to the overlap between depression and anxiety. 9 , 16 , 21 , 22 , 23
These two lines of evidence, (1) longitudinal studies that establish psychological distress as a risk factor for LBP in samples of individuals without LBP at baseline, and (2) human experimental studies finding that psychological distress can initiate at least some pain experiences, suggest that at least some LBP, although not all, may be rooted in psychological distress. If the existence of this fraction of LBP implies that neurobiological effects have been set in motion by psychological distress, then reducing psychological distress should result in the reduction/cessation of this fraction of LBP. We thus hypothesize that an exogenous reduction of psychological distress would result in the cessation of at least some LBP. While the causes of LBP exist on a continuum, we propose a test of this hypothesis that should be able to determine what proportion of LBP may be largely rooted in psychological distress.
To examine our hypothesis, we use a design with high internal and external validity. Our approach is a regression discontinuity analysis applied to national data. Regression discontinuity models are increasingly used in economics, 24 , 25 , 26 epidemiology, 27 , 28 , 29 , 30 and medical research, 31 , 32 , 33 , 34 in contexts where randomized controlled trials are economically or ethically infeasible.
While this study should determine the extent to which a reduced prevalence of psychological distress reduces the prevalence of LBP, not all individuals with LBP seek medical attention. Thus, the implications of this phenomenon for health policy partially depend on the extent to which medical visits with LBP as the primary complaint are simultaneously reduced. We thus also use a regression discontinuity model to examine whether such visits were simultaneously reduced.
1.1. The impact of terrorist attacks and recessions on emotional well‐being
To determine whether a reduction in the prevalence of psychological distress results in a reduction in the prevalence of LBP, we exploit two co‐occurring exogenous national events that occurred in November of 2001 and would be expected to reduce psychological distress in November 2001: (a) the last of the three major governmental responses to the September 11, 2001 (9‐11), terrorist attacks, and (b) the ending of the 2001 recession. These events identify the timing of the discontinuity.
Evidence indicates that violent events are associated with reduced emotional well‐being. The impact of 9‐11 was found to increase negative affect among individuals in Britain. 35 Similar effects have also been found in young adults in the United States. 36 Related findings have also been found using data capturing the effect of the Charlie Hebdo terrorist attack in France and data capturing the effect of the 2011 riots in England. 37 , 38
Evidence also indicates that national economic downturns impact the prevalence of psychological/behavioral disorders. 39 The Great Recession of 2007‐2009 has been associated with increases in mental health issues. 40 , 41 , 42 This recession has also been associated with increases in proxies for psychological distress, such as mental health care utilization. 41 , 43 Studies examining earlier recessions find similar results. 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51
We suggest that not only do terrorism/violence and recession reduce emotional well‐being, but emotional well‐being would be improved by reducing terrorism/violence and quickly ending recessions. The extent to which these events occur in close time proximity to each other as well as the order in which they occur would be expected to impact the relative magnitude of their effects on psychological distress.
To frame our analysis, we note that the Index of Consumer Sentiment declined strongly starting in December 2000 and continued to decline through the formal beginning of the recession in March 2001. 52 This is consistent with the upward trend in psychological distress over approximately the same time period. See Figure 1, Panel A.
FIGURE 1.
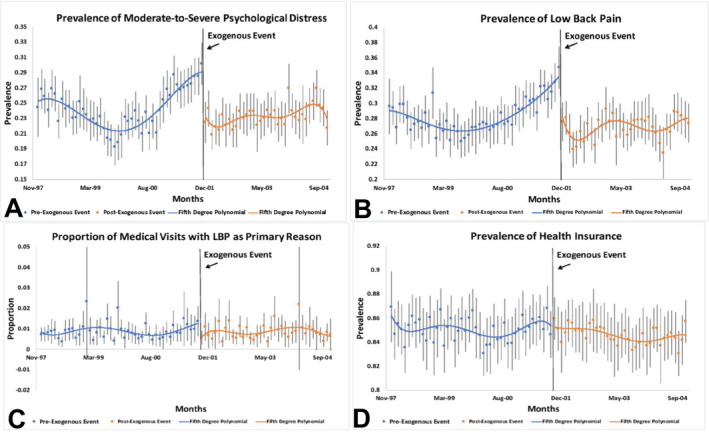
Panel A: prevalence of moderate‐to‐severe psychological distress (NHIS). Panel B: prevalence of low‐back pain (NHIS). Panel C: proportion of medical visits with LBP as primary reason (combined NAMCS and NHAMCS). Panel D: prevalence of health insurance (NHIS). All panels show January 1998 through December 2004 with 95% confidence intervals [Colour figure can be viewed at wileyonlinelibrary.com]
It was during this high prevalence of psychological distress that the 9‐11 terrorist attacks occurred, attacks associated with a continuing increase in psychological distress as shown in Figure 1, Panel A, but an increase that was likely smaller than would have been the case had there been no recession. The 9‐11 attacks were followed by three rapid government responses. On October 7, the United States invaded Afghanistan in an effort to dismantle Al‐Qaeda, the group identified as responsible for the 9‐11 attacks. 53 On October 26, Congress passed the Uniting and Strengthening America by Providing Appropriate Tools Required to Intercept and Obstruct Terrorism Act of 2001. 54 Finally, on November 19, Congress passed the Aviation and Security Act, creating the Transportation Security Administration. 55 Concomitantly, the economic recession also ended in November 2001. 56 The simultaneity of the end of the recession and the last of the three major governmental responses to 9‐11 would be expected to have a larger impact on psychological distress than either event occurring in isolation.
Any reduction in psychological distress occurring in the second half of November 2001 would not be fully reflected in the NHIS until the second half of December 2001, or more likely, the beginning of January 2002 because of the 30‐day look‐back period in the measure of psychological distress and because the NHIS is not collected during the winter holidays. Thus, the discontinuity in psychological distress occurring in November 2001 is likely to be picked up in these data between December 2001 and January 2002. The measure of self‐reported LBP in the NHIS looks back 90 days, and so is subject to a similar lag.
In contrast, any discontinuous reduction in medical visits for LBP in November 2001 would be reflected immediately in November 2001 in both the National Ambulatory Medical Care Survey (NAMCS) and the National Hospital Ambulatory Medical Care Survey (NHAMCS), which both provide the specific month of medical visits.
Although it is not reasonable to assume that the entire US population supported the US response to 9‐11, it is reasonable to assume that, on average, these events, combined with the end of recession, would reduce the national prevalence of psychological distress. The exogenous nature of these events allows us to evaluate rigorously the hypothesis that a reduction in the prevalence of psychological distress can induce a reduction in the prevalence of LBP. A concomitant reduction in medical visits for LBP should also be observed.
2. METHODS
2.1. Data
We use 84 months of repeated cross‐sectional data: 1998‐2004. Data on psychological distress and self‐reported LBP come from the NHIS. 57 The NHIS is an in‐person survey that collects information on health, health care access, and health behaviors of the civilian, noninstitutionalized US population. Data are collected across the calendar year using a complex survey design and are nationally representative by month. 58
We use the combined NAMCS and NHAMCS for the same period. The NAMCS is a survey of visits to office‐based physicians, and the NHAMCS is a survey of visits to hospital outpatient and emergency departments. Both are collected across the calendar year using a complex survey design and are nationally representative.
2.2. Outcome variable
Our primary outcome is LBP. Individuals in the NHIS were asked, “During the past three months, did you have low back pain?” Our secondary outcome is whether LBP was the most important reason for a given medical visit and is found in the NAMCS and NHAMCS. We omit medical visits for which LBP was not the primary complaint to avoid picking up visits where LBP was a peripheral concern and may not have influenced individuals to seek care.
2.3. Assignment variable
Individuals in the NHIS are implicitly assigned to treatment and control groups based on the interview schedule. There are approximately 2500 such observations per month. Individuals in the combined NAMCS and NHAMCS are implicitly assigned to treatment and control groups based on their medical treatment date. There are approximately 7300 such observations per month.
2.4. Treatment variable
“Treatment” is defined as a reduction in psychological distress to a level below moderate psychological distress. We use Kessler's K6, a reliable and valid measure of nonspecific psychological distress in the NHIS. 59 The components making up the K6 and its documented gender disparity suggest the K6 is capturing anxiety/mood disorders. 60 The components of the K6 are not linked to personal context (apart from time) or other health conditions, making the K6 a general measure. The K6 scale is derived by summing responses to six questions asking how often the respondent felt worthless, hopeless, restless, sad, nervous, or that everything was an effort, during the past 30 days. Answers are coded as 0 (none of the time), 1 (a little of the time), 2 (some of the time), 3 (most of the time), or 4 (all of the time) and are summed to yield a 0‐to‐24 scale. Scores ≥13 indicate severe psychological distress consistent with serious mental illness. 61 Scores of 5 to 12 indicate moderate psychological distress, a level sufficient to warrant clinical intervention. 62 , 63 However, the latter scoring was determined using only California data, where the optimal cut‐point for Hispanics was 6, while the optimal cut‐point for the overall population was 5. Since Hispanics made up approximately 39 percent of the California population but only 18 percent of the US population, we suggest that the appropriate cut‐point for moderate psychological distress for the national population is lower. Since the K6 is an ordinal measure, we cannot use fractional cut‐points and so conservatively use scores of 4 to 12 to capture moderate psychological distress. Thus, to capture moderate‐to‐severe levels of psychological distress, we use a binary indicator equal to one when K6 ≥ 4 and zero otherwise. We also construct versions capturing subclinical levels (K6 ≥ 3 and K6 ≥ 1) for sensitivity testing.
2.5. Covariates
Covariates from the NHIS include race/ethnicity, gender, marital status, education, general health status, family income, age, current health insurance, current employment status, and census region. An additional variable used for a placebo test is injuries/poisoning in the previous three months. Covariates available from the NAMCS and NHAMCS are limited and include race/ethnicity, gender, health insurance, and census region. We omit data from the northeast to avoid including 9‐11 victims and first responders as they may have sustained a physical injury to their low back. Each attack/crash on 9‐11 occurred in the northeast.
2.6. Regression discontinuity model
Regression discontinuity models can be conceptualized in two different ways. One is as a kind of randomized experiment, where subjects in the appropriate bandwidths to the right and left of the discontinuity are assumed to be as good as randomly allocated to treatment and control groups, ruling out selection bias. Treatment effects are measured by the difference in means between the two groups.
An alternative conceptualization posits that selection into treatment and control groups is not necessarily random, but is described by a regression line where there is equivalence in the pre‐and post‐functional form. Selection bias is ruled out by the assumption that in the absence of treatment, there would be no discontinuity in the functional form of the pre‐ and post‐regression line across the relevant regions. The untreated portion of the line serves as the counterfactual to treatment.
Regardless of the above conceptual choices, regression discontinuity analysis has two key assumptions. The first assumption is the continuity restriction: There is no discontinuity in potential outcomes at the cutoff. In other words, there should be no alternative interpretation for the existence of the discontinuity in the outcome apart from the hypothesis being tested. This implies that no alternative explanatory variables have a discontinuity that would serve as a causal confound. In contrast, the second assumption is that the probability of receiving treatment must be discontinuous at the cutoff and the position of the cutoff must be exogenously determined.
The discontinuity in the probability of receiving treatment can be assumed to be either sharp or fuzzy, 63 depending on how individuals are assumed to be allocated into treatment and control groups: with certainty or probabilistically. In the latter case, the fuzziness of the discontinuity is addressed by using the assignment variable at the cutoff as an instrumental variable for receiving treatment.
In this study, we are interested in the “treatment” of a reduction in psychological distress that occurs after the aforementioned co‐occurring national events. Not everyone would be expected to respond to these events in the same manner, making movement into or out of psychological distress probabilistic. Thus, a fuzzy regression discontinuity model, in which the probability of participation in “treatment” increases (or decreases) as one passes the cutoff threshold but can vary along the unit interval [0, 1], is appropriate.
Following Cattaneo, Idrobo, and Titiunike, 64 consider the assignment rule:
| (1) |
where treatment assignment is (experiencing the relevant events), is the assignment variable (months), and is the cutoff value of the assignment variable. The regression discontinuity estimator for the treatment assignment, , and the degree to which treatment is taken up, (experiencing moderate‐to‐severe psychological distress), can be written:
| (2) |
This is the first‐stage result: . The average treatment effect can be found by assuming local independence of (where is low‐back pain) and is close to 24
| (3) |
When we divide Equation (3) by Equation (2), we obtain
| (4) |
which is the local average treatment effect (LATE), , where the subscript, , indicates a fuzzy regression discontinuity, unit is the complier, and . In addition, our instrument in the first stage must meet the standard criteria: relevance/strength of the instrument, exclusion restriction, and monotonicity. 65
As noted above, for any regression discontinuity model to be valid, the assignment variable must be exogenously determined: Individuals must not manipulate the value of the assignment variable such that they are placed in the treatment or control group. The assignment variable, , is time measured in months. While individuals being interviewed for the NHIS have some choice as to their interview date, manipulation of the survey date with a view to avoid or ensure inclusion in the treatment group was not possible since the timing of the relevant exogenous events was not foreseeable. Similarly, while individuals whose medical visit is captured by the NAMCS or NHAMCS have some choice as to the day they receive care, manipulation of the survey date to avoid or ensure inclusion in the treatment group was not possible for the same reason.
We estimate our models using covariates. 63 , 66 Assuming that individuals are as good as randomly allocated to either side of the discontinuity, covariates will merely increase the precision of the estimate and should not yield estimates that are statistically different from the estimates not incorporating covariates.
To illustrate the addition of covariates formally, we assume a first‐degree polynomial. Assume that we possess a random sample:
| (5) |
to which we now add , a vector of covariates. Then, the regressions we wish we estimate are as follows:
| (6) |
| (7) |
Taking parameters and , we obtain covariate‐adjusted LATE, :
| (8) |
For the analysis of the combined NAMCS and NHAMCS, we use a sharp regression discontinuity model as these data do not contain the K6. Thus, the relevant model would be similar to Equation (6) where the treatment effect is τY.
The treatment effects described above will be sensitive to the sample weighting of the data. However, there are two types of weighting that occur in our models: kernel weights and sample weights. Kernel weights either weight each observation within the bandwidth equally, known as uniform weighting, or weight observations further away from the cutoff less using various formulas. 66 Sample weights reflect the probability that any individual selected participates in the survey. We include sample weights multiplied by uniform weights.
A number of additional issues arise in our analysis. The first is the discrete nature of the assignment variable. When the assignment variable is measured discretely, it is impossible to compute averages of arbitrarily small neighborhoods around the cutoff, producing an “irreducible gap” between the control group below the cutoff and the treatment group above the cutoff. 67 In this situation, a causal effect can only be identified via functional form assumptions. We take this approach.
This issue impacts questions of bandwidth size and the appropriate degree of polynomial to employ. Regression discontinuity models suffer from a bias‐variance trade‐off. Wide bandwidths include more data points resulting in lower variance, but can induce higher bias when estimating nonlinear relationships. In contrast, narrow bandwidths include fewer data points resulting in higher variance, but this smaller set of data points reduces bias.
Bias can also be impacted by the degree of polynomial used. Gelman and Imbens argue that in many cases, only local linear or quadratic polynomials should be used due to the unattractive properties of higher degree polynomials, these being the sensitivity of results to the order of the polynomial and the sensitivity of confidence intervals to the order the polynomial. 68 This suggests that relatively short bandwidths can be effectively analyzed using first‐degree polynomials under the assumption that the discontinuity is assumed to be occurring in a consistent functional form (eg, as described by Equations (6) and (7) across the pre‐ and post‐periods. This is the case as long as there are no significant nonlinearities occurring in the bandwidths used that would result in the local or quadratic linear regressions performing poorly at the boundary of the discontinuity.
Since we have a discrete assignment variable, we employ local linear regression and use a bandwidth of moderate length (9 months on the left and 9 months on the right of the discontinuity in addition to the discontinuity point) to ensure conservative performance at the boundaries of the discontinuity. We also incorporate bias correction. 63
All estimates are derived using Stata 15 and incorporate robust nonparametric confidence intervals. 63 , 66 , 69 In order to use the bias‐corrected standard errors as an approximation, we must and do have a sufficient number of mass points near the cutoff. 63 , 69 All estimates account for the probability weighting and clustering of the NHIS, NAMCS, and NHAMCS.
3. RESULTS
Table 1 presents descriptive statistics. If we adjust these data to reflect the total populations represented in each group, these data suggest that only 18 percent of individuals with self‐reported LBP have a medical visit in which LBP was the most important reason for the visit (assuming one medical visit per person with LBP [results not shown]).
TABLE 1.
Descriptive statistics
| NHIS | Combined NAMCS and NHAMCS | |||
|---|---|---|---|---|
| Before Discontinuity (9 months) | After Discontinuity (9 months) a | Before Discontinuity (9 months) | After Discontinuity (9 months) a | |
| K6 (moderate‐to‐severe psychological distress) | 0.210 | 0.168 | — | — |
| Self‐reported LBP | 0.317 | 0.260 | — | — |
| Proportion of medical visits with LBP as primary reason | — | — | 0.011 | 0.009 |
| Proportion of postoperative medical visits | 0.024 | 0.025 | ||
| Health insurance | 0.847 | 0.837 | 0.863 | 0.867 |
| Age (25‐34) | 0.185 | 0.187 | 0.104 | 0.107 |
| Age (35‐44) | 0.219 | 0.213 | 0.140 | 0.132 |
| Age (45‐54) | 0.187 | 0.188 | 0.145 | 0.148 |
| Age (55‐64) | 0.118 | 0.122 | 0.114 | 0.118 |
| Age (65+) | 0.154 | 0.154 | 0.243 | 0.226 |
| Female | 0.518 | 0.519 | 0.574 | 0.588 |
| Black | 0.116 | 0.118 | 0.099 | 0.115 |
| Hispanic | 0.111 | 0.115 | 0.072 | 0.078 |
| Asian and Pacific Islander | 0.034 | 0.034 | 0.036 | 0.034 |
| Other Race | 0.036 | 0.035 | 0.006 | 0.006 |
| Region—west | 0.239 | 0.240 | 0.315 | 0.249 |
| Region—south | 0.454 | 0.459 | 0.395 | 0.458 |
| Family income $15‐20 000 | 0.064 | 0.061 | — | — |
| Family income $20‐25 000 | 0.071 | 0.073 | — | — |
| Family income $25‐35 000 | 0.132 | 0.130 | — | — |
| Family income $35‐45 000 | 0.110 | 0.110 | — | — |
| Family income $45‐55 000 | 0.098 | 0.092 | — | — |
| Family income $55‐65 000 | 0.077 | 0.077 | — | — |
| Family income $65 000+ | 0.239 | 0.247 | — | — |
| Employed (working at a job) | 0.283 | 0.284 | — | — |
| Associate's degree | 0.094 | 0.094 | — | — |
| Bachelor's degree | 0.156 | 0.161 | — | — |
| Postgraduate | 0.077 | 0.077 | — | — |
| Married (spouse in home) | 0.576 | 0.575 | — | — |
| Married (spouse not in home) | 0.012 | 0.012 | ||
| Divorced | 0.129 | 0.126 | — | — |
| Separated | 0.024 | 0.023 | — | — |
| Widowed | 0.063 | 0.062 | — | — |
| Health status—excellent | 0.309 | 0.305 | — | — |
| Health status—very good | 0.333 | 0.321 | — | — |
| Health status—good | 0.238 | 0.254 | — | — |
| Health status—fair | 0.088 | 0.090 | — | — |
| Observations | 20 349 | 20 254 | 52 993 | 59 213 |
Nine months beyond the discontinuity point for a total of 10 months. Note that the northeast of the United States is omitted to avoid including victims, first responders, and similar individuals in the sample as these may have physically injured their low back.
The discontinuity in the prevalence of moderate‐to‐severe psychological distress is presented in Figure 1, Panel A, using a fifth‐degree polynomial to fit the entire series for illustrative purposes. There is a discontinuity between December 2001 and January 2002. While the actual discontinuity is experienced by individuals between October 2001 and November 2001, the discontinuity appears in data with a lag as noted above. Figure 1, Panel B, illustrates the corresponding data for LBP and shows a similar discontinuity. Figure 1, Panel C, shows medical visits for LBP and shows a discontinuity between October 2001 and November 2001 as these data are not subject to a reporting lag. Medical visits for LBP prior to the exogenous national event largely mirror the prevalence of health insurance, as shown in Figure 1, Panel D, albeit with a smaller amplitude.
Table 2 presents the fuzzy regression discontinuity results using a first‐degree polynomial with bias correction. Figure 2, Panels A and B, illustrates the intervals on either side of the exogenous event for the two relevant outcome variables. The estimate of the treatment effect, accounting for covariates, shows that every 1 percentage point reduction in moderate‐to‐severe psychological distress reduces the prevalence of LBP by 0.85 percentage points (P ≤ .05). The first‐stage estimate of ‐0.092 (P ≤ .01) is an approximate one‐third reduction in the 0.302 prevalence of moderate‐to‐severe psychological distress in the month before the discontinuity (Figure 2, Panel A). This resulted in a ‐7.8 percentage point (0.078 = ‐0.092 × 0.85) or approximate one‐fifth reduction in the 0.347 prevalence of LBP in the month before the discontinuity (Figure 2, Panel B). This reduction in LBP is equivalent to approximately 2.1 million (P < .01) individuals (excluding the northeast) no longer experiencing LBP. If we reduce the cut‐point of moderate‐to‐severe psychological distress to include subclinical levels of psychological distress, the estimated impact becomes smaller but remains statistically significant.
TABLE 2.
Impact of exogenous shock on reported prevalence of LBP and proportion of medical visits for LBP
| Fuzzy RD | Sharp RD | |||
|---|---|---|---|---|
| Self‐reported LBP | Medical visits | |||
| No Covariates Included | ||||
| Bins | ||||
| 9 months of observations to the left of the cutoff | 20 614 | 20 614 | 20 614 | 52 993 |
| 9 months of observations to the right of the cutoff a | 20 582 | 20 582 | 20 582 | 59 213 |
| First‐Stage Estimate of Psychological Distress (K6) | (K6 ≥ 4) | (K6 ≥ 3) | (K6 ≥ 1) | — |
| Coefficient | −0.089*** | −0.107*** | −0.134*** | — |
| Robust bias‐corrected standard error | 0.020 | 0.021 | 0.024 | — |
| Treatment effect | ||||
| Coefficient | 0.770** | 0.633** | 0.460 | −0.008** |
| Robust bias‐corrected standard error | 0.397 | 0.301 | 0.268 | 0.004 |
| Covariates included | ||||
| Bins | ||||
| 9 months of observations to the left of the cutoff | 20 349 | 20 349 | 20 349 | 52 993 |
| 9 months of observations to the right of the cutoff a | 20 254 | 20 254 | 20 254 | 59 213 |
| First‐stage Estimate of Psychological Distress (K6) | (K6 ≥ 4) | (K6 ≥ 3) | (K6 ≥ 1) | — |
| Coefficient | −0.092*** | −0.112*** | −0.140*** | — |
| Robust bias‐corrected standard error | 0.019 | 0.021 | 0.023 | — |
| Treatment effect | ||||
| Coefficient | 0.850** | 0.694*** | 0.496** | −0.008** |
| Robust bias‐corrected standard error | 0.361 | 0.274 | 0.253 | 0.004 |
Estimates of the effect of nonspecific psychological distress on the experience of LBP using fuzzy RD models and estimates of a concomitant effect on medical visits for LBP where the primary reason for the medical visit was LBP using a sharp RD model.
Abbreviation: RD, regression discontinuity.
**P ≤ .05, ***P ≤ .01.
Nine months beyond the discontinuity point for a total of 10 months.
FIGURE 2.
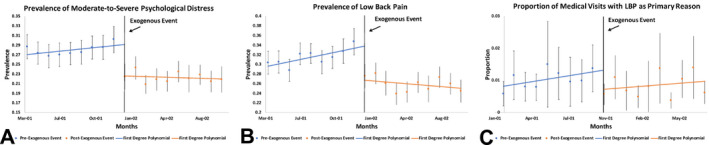
Panel A: prevalence of moderate‐to‐severe psychological distress (NHIS). Panel B: prevalence of low‐back pain (NHIS). Panel C: proportion of medical visits with LBP as primary reason (combined NAMCS and NHAMCS). All panels show monthly data with 95% confidence intervals [Colour figure can be viewed at wileyonlinelibrary.com]
A reduction in the proportion of medical visits with LBP as the primary complaint of 0.8 percentage points (P ≤ .05) from a baseline of 1.3 percent of all medical visits was found between November 2001 and December 2001, or approximately three‐fifths of all medical visits with LBP as the primary complaint. This represents a monthly reduction of approximately 685 000 (P < .01) visits (excluding the northeast) relative to those in the month immediately preceding the discontinuity.
3.1. Validity checks
We perform three categories of validity checks. We examine whether our models are consistent with the continuity restriction. We also examine whether our models are reasonable by subjecting them to a large set of placebo tests. Finally, we examine whether a test of a closely related alternative outcome yields findings consistent with those of LBP.
To evaluate the continuity restriction assumption, which implies that there should be no alternative interpretation for the existence of a specific discontinuity in the outcome apart from the hypothesis being tested, we examine alternative hypotheses in which a discontinuity would serve as a causal confound. In particular, we focus on three major alternative hypotheses for a national decrease in the prevalence of LBP, which would also be alternative hypotheses for the national decrease in the proportion of medical visits for which the reduction in self‐reported LBP was the primary reason.
The first alternative hypothesis is a discontinuity in the prevalence of health insurance. Any such discontinuity must occur in November of 2001 when the recession ended as this variable is not subject to a reporting lag. Changes in the prevalence of health insurance would mean changes in the proportion of people being treated for their health problems, including successfully treating episodes of LBP. Both Panel D of Figure 1 and the results of a sharp regression discontinuity model show that no discontinuity is present, resulting in a rejection of this alternative hypothesis [regression results not shown].
A second alternative hypothesis is a discontinuity in employment rates. Such a discontinuity must occur at the same time as the end of 2001 recession as this variable is not subject to a reporting lag. Such a discontinuity would show that more individuals became employed, possibly resulting in both better health and less LBP as their daily activities changed. Note that we do not use the economic definition of unemployment, but rather use the simple proportion of the adult population that was employed, a more appropriate measure in this context. Figure 3, Panel A, illustrates and a sharp regression discontinuity model shows that no discontinuity is present in employment, resulting in a rejection of this alternative hypothesis [regression results not shown].
FIGURE 3.
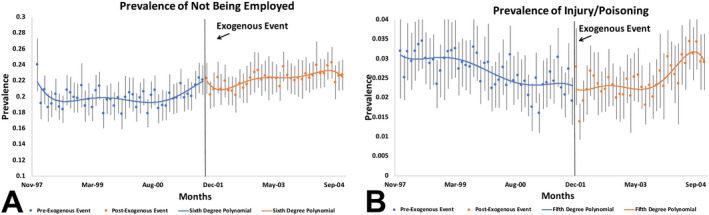
Panel A: prevalence of employment (NHIS). Panel B: prevalence of injury/poisoning (NHIS). Both using monthly data (January 1998 – December 2004) with 95% confidence intervals [Colour figure can be viewed at wileyonlinelibrary.com]
A third alternative hypothesis is a discontinuity in the rate of injuries/poisoning during the last three months, which could impact LBP. This discontinuity must occur in the data at the same time as LBP as this variable is subject to the same lag as LBP. Figure 3, Panel B, illustrates and a sharp regression discontinuity model shows that no discontinuity is present, resulting in a rejection of this alternative hypothesis [regression results not shown]. Note, that there is a clear discontinuity between January 2002 and February 2002, but this is not a concomitant discontinuity and is thus moot.
An additional category of validity checks is placebo tests that examine whether variables which would not be expected to exhibit a discontinuity actually do exhibit a discontinuity during the relevant time periods, indicating a problem with the model. Sharp regression discontinuity models conducted with each covariate as the dependent variables find no statistically significant discontinuities occurring during the relevant time periods [regression results not shown]. A final placebo test is whether medical visits that include an evaluation of pain that is objectively tied to surgical intervention—postoperative medical visits—exhibited a discontinuity during this time period. A sharp regression model finds no evidence of such a discontinuity [regression results not shown].
We conducted a final validity check to examine whether the prevalence of neck pain, another part of the spine, was also reduced in response to the reduction in the prevalence of psychological distress. We expect and find, using a fuzzy regression model identical to the model used for the main results, that the prevalence of neck pain is reduced [regression results not shown].
4. DISCUSSION
This is the first study, to our knowledge, to examine the hypothesis that an exogenous reduction in the prevalence of moderate‐to‐severe psychological distress will induce a reduction in the prevalence of LBP. There are three major findings. First, only a fraction of individuals with LBP access medical services where LBP is the primary reason for the medical visit, consistent with previous findings. 70 , 71 Second, we find that the prevalence of self‐reported LBP drops approximately 0.85 percentage points for every 1 percentage point reduction in the prevalence of moderate‐to‐severe psychological distress. Third, there was a concomitant reduction of approximately three‐fifths of medical visits where LBP was the primary complaint.
It is notable that these findings are consistent with the well‐known finding that as much as 85 percent of primary care patients with LBP have LBP that can be classified as nonspecific (no known pathoanatomical cause). 72 , 73 While our findings do not imply that all nonspecific LBP is rooted in psychological distress, as we do not know if our findings would be maintained for additional reductions in psychological distress, our findings do imply that approximately 85 percent of the observed reduction in LBP may be rooted in nonspecific psychological distress. Since LBP was reduced by approximately one‐fifth, this suggests that, at minimum, approximately 17 percent (0.17 = 0.20 × 0.85) of self‐reported LBP may be rooted in psychological distress.
These findings have significant implications for health care providers, specifically, to what degree might interventions for psychological distress (primarily mood and anxiety conditions) mimic the findings presented here? Note that such interventions may include, but would not necessarily be limited to, interventions focused specifically on LBP. 74 , 75 , 76 Potential interventions for LBP worth investigating may include those that focus generally on alleviating mood and anxiety conditions, which are the conditions primarily picked up by the measure of psychological distress used in this study. 77 If the findings of our study are accurate, such interventions, which have moderate effect sizes, may have a larger impact on LBP than psychological interventions focused specifically on LBP. While such interventions may not approach the size of the effect found in this study, such interventions may be highly appropriate for individuals whose LBP may be rooted in the neurobiological changes induced by psychological distress.
4.1. Limitations
This study is subject to at least three limitations. The first is that our finding of a concomitant three‐fifths reduction in medical visits with LBP as the primary complaint is only an association. Our methodology does not allow us to draw a causal inference from this finding. A second limitation is that while the natural experiment exploited here allowed us to determine the overall size of the impact of a reduction in the prevalence of psychological distress on the prevalence of reported low‐back pain, there is likely subgroup variation not captured in our analysis. A third limitation is that this paper does not discuss other relevant treatments for LBP, including exercise and treatments that impact adaptive factors such as self‐efficacy and positive coping. 78 , 79
5. CONCLUSIONS
The finding that an exogenous national reduction in the prevalence of moderate‐to‐severe psychological distress resulted in 2.1 million people (on a monthly basis) no longer having LBP suggests that a minimum of 17 percent of all LBP may be rooted in psychological distress. This is consistent with current neurobiological literature on the relationship between psychological distress and pain. The concomitant reduction in medical visits with a primary complaint of LBP of 685 000 per month suggests that this phenomenon may have an important impact on health care utilization. Investigation of whether clinical interventions aimed at reducing general mood/anxiety conditions in persons with LBP may have similar effects is warranted, even if such effects do not approach the same magnitude of the effect measured here.
Supporting information
Author Matrix
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: This work was a project for the MPH course, Analytic Methods for Health Policy and Management, at the University of California, Berkeley, a project initiated by the instructor, Timothy Brown, and which included project team members Christie Ahn, Haoyue Huang, and Zaidat Ibrahim. Timothy Brown was supported by the University of California, Berkeley, in his role as a faculty member, and Christie Ahn, Haoyue Huang, and Zaidat Ibrahim supported themselves in the role of students. All team members contributed time to update the project for publication after the conclusion of the course.
Disclosures: None.
Brown TT, Ahn C, Huang H, Ibrahim Z. Reducing the prevalence of low‐back pain by reducing the prevalence of psychological distress: Evidence from a natural experiment and implications for health care providers. Health Serv Res. 2020;55:631–641. 10.1111/1475-6773.13557
REFERENCES
- 1. Worsening Trends in the Management and Treatment of Back Pain | Guidelines | JAMA Internal Medicine | JAMA Network. https://jamanetwork.com/journals/jamainternalmedicine/article‐abstract/1722522. Accessed October 29, 2019
- 2. Manchikanti L. Epidemiology of low back pain. Pain Physician. 2000;3(2):167. [PubMed] [Google Scholar]
- 3. Katz JN. Lumbar disc disorders and low‐back pain: socioeconomic factors and consequences. JBJS. 2006;88:21‐24. [DOI] [PubMed] [Google Scholar]
- 4. de Heer EW, ten Have M, van Marwijk HWJ, et al. Pain as a risk factor for common mental disorders. Results from the Netherlands Mental Health Survey and Incidence Study‐2: a longitudinal, population‐based study. Pain. 2018;159(4):712‐718. [DOI] [PubMed] [Google Scholar]
- 5. Arola H‐M, Nicholls E, Mallen C, Thomas E. Self‐reported pain interference and symptoms of anxiety and depression in community‐dwelling older adults: can a temporal relationship be determined? Eur J Pain. 2010;14(9):966‐971. [DOI] [PubMed] [Google Scholar]
- 6. Hilderink PH, Burger H, Deeg DJ, Beekman AT, Oude Voshaar RC. The temporal relation between pain and depression: results from the longitudinal aging study Amsterdam. Psychosom Med. 2012;74(9):945. [DOI] [PubMed] [Google Scholar]
- 7. Pinheiro MB, Ferreira ML, Refshauge K, et al. Symptoms of depression and risk of low back pain: a prospective co‐twin study. Clin J Pain. 2017;33(9):777. [DOI] [PubMed] [Google Scholar]
- 8. Olango WM, Finn DP. Neurobiology of stress‐induced hyperalgesia In: Taylor B, Finn D, eds. Behavioral Neurobiology of Chronic Pain. Current Topics in Behavioral Neurosciences, Vol. 20. Berlin, Heidelberg: Springer; 2014:251‐280. 10.1007/7854_2014_302 [DOI] [PubMed] [Google Scholar]
- 9. Brown TT, Partanen J, Chuong L, Villaverde V, Griffin AC, Mendelson A. Discrimination hurts: the effect of discrimination on the development of chronic pain. Soc Sci Med. 2018;204:1‐8. [DOI] [PubMed] [Google Scholar]
- 10. Schumacher R, Velden M. Anxiety, pain experience, and pain report: a signal‐detection study. Percept Mot Skills. 1984;58(2):339‐349. [DOI] [PubMed] [Google Scholar]
- 11. Weisenberg M, Aviram O, Wolf Y, Raphaeli N. Relevant and irrelevant anxiety in the reaction to pain. Pain. 1984;20(4):371‐383. [DOI] [PubMed] [Google Scholar]
- 12. Dougher MJ. Sensory decision theory analysis of the effects of anxiety and experimental instructions on pain. J Abnorm Psychol. 1979;88(2):137. [DOI] [PubMed] [Google Scholar]
- 13. Cornwall A, Donderi DC. The effect of experimentally induced anxiety on the experience of pressure pain. Pain. 1988;35(1):105‐113. [DOI] [PubMed] [Google Scholar]
- 14. Rhudy JL, Meagher MW. Fear and anxiety: divergent effects on human pain thresholds. Pain. 2000;84(1):65‐75. [DOI] [PubMed] [Google Scholar]
- 15. Williams AE, Rhudy JL. The influence of conditioned fear on human pain thresholds: does preparedness play a role? J Pain. 2007;8(7):598‐606. [DOI] [PubMed] [Google Scholar]
- 16. Thompson T, Keogh E, French CC, Davis R. Anxiety sensitivity and pain: generalisability across noxious stimuli. Pain. 2008;134(1–2):187‐196. [DOI] [PubMed] [Google Scholar]
- 17. Schweiger A, Parducci A. Nocebo: the psychologic induction of pain. Pavlov J Biol Sci Off J Pavlov. 1981;16(3):140‐143. [DOI] [PubMed] [Google Scholar]
- 18. Bayer TL, Baer PE, Early C. Situational and psychophysiological factors in psychologically induced pain. Pain. 1991;44(1):45‐50. [DOI] [PubMed] [Google Scholar]
- 19. Leistad RB, Sand T, Westgaard RH, Nilsen KB, Stovner LJ. Stress‐induced pain and muscle activity in patients with migraine and tension‐type headache. Cephalalgia. 2006;26(1):64‐73. [DOI] [PubMed] [Google Scholar]
- 20. Colloca L, Benedetti F. Nocebo hyperalgesia: how anxiety is turned into pain. Curr Opin Anesthesiol. 2007;20(5):435‐439. [DOI] [PubMed] [Google Scholar]
- 21. Eysenck MW, Fajkowska M. Anxiety and depression: toward overlapping and distinctive features. Cogn Emot. 2018;32(7):1391‐1400. [DOI] [PubMed] [Google Scholar]
- 22. Trivedi MH. The Link between depression and physical symptoms. Prim Care Companion J Clin Psychiatry. 2004;6(suppl 1):12‐16. [PMC free article] [PubMed] [Google Scholar]
- 23. Tikàsz A, Tourjman V, Chalaye P, Marchand S, Potvin S. Increased spinal pain sensitization in major depressive disorder: a pilot study. Psychiatry Res. 2016;246:756‐761. [DOI] [PubMed] [Google Scholar]
- 24. Hahn J, Todd P, Van der Klaauw W. Identification and estimation of treatment effects with a regression‐discontinuity design. Econometrica. 2001;69(1):201‐209. [Google Scholar]
- 25. Imbens GW, Lemieux T. Regression discontinuity designs: a guide to practice. J Econom. 2008;142(2):615‐635. [Google Scholar]
- 26. Lee DS, Lemieux T. Regression discontinuity designs in economics. J Econ Lit. 2010;48(2):281‐355. [Google Scholar]
- 27. Bor J, Moscoe E, Mutevedzi P, Newell M‐L, Bärnighausen T. Regression discontinuity designs in epidemiology: causal inference without randomized trials. Epidemiol Camb Mass. 2014;25(5):729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Moscoe E, Bor J, Bärnighausen T. Regression discontinuity designs are underutilized in medicine, epidemiology, and public health: a review of current and best practice. J Clin Epidemiol. 2015;68(2):132‐143. [DOI] [PubMed] [Google Scholar]
- 29. Maas IL, Nolte S, Walter OB, et al. The regression discontinuity design showed to be a valid alternative to a randomized controlled trial for estimating treatment effects. J Clin Epidemiol. 2017;82:94‐102. [DOI] [PubMed] [Google Scholar]
- 30. Glymour MM, Hamad R. Causal thinking as a critical tool for eliminating social inequalities in health. Am Public Health Assoc. 2018;108(5):623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. O’Keeffe AG, Geneletti S, Baio G, Sharples LD, Nazareth I, Petersen I. Regression discontinuity designs: an approach to the evaluation of treatment efficacy in primary care using observational data. BMJ. 2014;349:g5293. [DOI] [PubMed] [Google Scholar]
- 32. Shoag J, Halpern J, Eisner B, et al. Efficacy of prostate‐specific antigen screening: use of regression discontinuity in the PLCO cancer screening trial. JAMA Oncol. 2015;1(7):984‐986. [DOI] [PubMed] [Google Scholar]
- 33. Venkataramani AS, Bor J, Jena AB. Regression discontinuity designs in healthcare research. BMJ. 2016;352:i1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Melamed A, Fink G, Wright AA, et al. Effect of adoption of neoadjuvant chemotherapy for advanced ovarian cancer on all cause mortality: quasi‐experimental study. BMJ. 2018;360:j5463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Metcalfe R, Powdthavee N, Dolan P. Destruction and distress: using a quasi‐experiment to show the effects of the September 11 attacks on mental well‐being in the United Kingdom. Econ J. 2011;121(550):F81‐F103. [Google Scholar]
- 36. Wang Y, Yang M. Crisis‐induced depression, physical activity and dietary intake among young adults: evidence from the 9/11 terrorist attacks. Econ Hum Biol. 2013;11(2):206‐220. [DOI] [PubMed] [Google Scholar]
- 37. Kim D, Albert Kim Y‐I. Mental health cost of terrorism: Study of the Charlie Hebdo attack in Paris. Health Econ. 2018;27(1):e1‐e14. [DOI] [PubMed] [Google Scholar]
- 38. Bencsik P. The non‐financial costs of violent public disturbances: Emotional responses to the 2011 riots in England. J Hous Econ. 2018;40:73‐82. [Google Scholar]
- 39. Catalano R, Goldman‐Mellor S, Saxton K, et al. The health effects of economic decline. Annu Rev Public Health. 2011;32:431‐450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Karanikolos M, Heino P, McKee M, Stuckler D, Legido‐Quigley H. Effects of the global financial crisis on health in high‐income OECD countries: a narrative review. Int J Health Serv. 2016;46(2):208‐240. [DOI] [PubMed] [Google Scholar]
- 41. Modrek S, Hamad R, Cullen MR. Psychological well‐being during the great recession: changes in mental health care utilization in an occupational cohort. Am J Public Health. 2015;105(2):304‐310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Burgard SA, Ailshire JA, Kalousova L. The great recession and health: people, populations, and disparities. Ann Am Acad Pol Soc Sci. 2013;650(1):194‐213. [Google Scholar]
- 43. Ayers JW, Althouse BM, Allem J‐P, et al. Novel surveillance of psychological distress during the great recession. J Affect Disord. 2012;142(1–3):323‐330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Currie J, Duque V, Garfinkel I. The great recession and mothers’ health. Econ J. 2015;125(588):F311‐F346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ruhm CJ. Are recessions good for your health? Q J Econ. 2000;115(2):617‐650. [Google Scholar]
- 46. Artazcoz L, Benach J, Borrell C, Cortes I. Unemployment and mental health: understanding the interactions among gender, family roles, and social class. Am J Public Health. 2004;94(1):82‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Charles KK, DeCicca P. Local labor market fluctuations and health: is there a connection and for whom? J Health Econ. 2008;27(6):1532‐1550. [DOI] [PubMed] [Google Scholar]
- 48. French MT, Davalos ME. This recession is wearing me out! Health‐related quality of life and economic downturns. J Ment Health Policy Econ. 2011;14(2):61‐72. [PubMed] [Google Scholar]
- 49. Dávalos ME, Fang H, French MT. Easing the pain of an economic downturn: macroeconomic conditions and excessive alcohol consumption. Health Econ. 2012;21(11):1318‐1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Browning M, Heinesen E. Effect of job loss due to plant closure on mortality and hospitalization. J Health Econ. 2012;31(4):599‐616. [DOI] [PubMed] [Google Scholar]
- 51. Tekin E, McClellan C, Minyard KJ. Health and Health Behaviors During the Worst of Times. Cambridge, MA: National Bureau of Economic ResOlangoearch; 2013. [Google Scholar]
- 52. University of Michigan . University of Michigan: Consumer Sentiment. FRED, Federal Reserve Bank of St. Louis. https://fred.stlouisfed.org/series/UMCSENT. Published November 1, 1952. Accessed October 29, 2019
- 53. Dixon R, Daniszewski J. U.S. Launches Attack; Missile Strikes Destroy Key Taliban Sites; Military: Bombers lead retaliatory assault against the regime that supports Bin Laden. Britain aids effort. “Today we focus on Afghanistan, but the battle is broader,” Bush says in global address: [Home Edition]. Los Angeles Times; Los Angeles, Calif. October 8, 2001:A.1. [Google Scholar]
- 54. https://www.govinfo.gov/content/pkg/PLAW‐107publ56/html/PLAW‐107publ56.htm. Accessed April 7, 2019
- 55. https://www.govinfo.gov/content/pkg/PLAW‐107publ71/html/PLAW‐107publ71.htm. Accessed October 29, 2019
- 56. Business Cycle Dating Committee, National Bureau of Economic Research . http://www.nber.org/cycles/july2003.html. Accessed October 29, 2019
- 57. Blewett LA, Rivera Drew JA, Griffin R, King ML, Williams KC. IPUMS Health Surveys: National Health Interview Survey, Version 6.3. Minneapolis, MN: IPUMS; 2018. [Google Scholar]
- 58. Botman S, Moriarity CL. Design and Estimation for the National Health Interview Survey, 1995‐2004. 2000. [PubMed] [Google Scholar]
- 59. Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non‐specific psychological distress. Psychol Med. 2002;32(6):959‐976. [DOI] [PubMed] [Google Scholar]
- 60. Pratt LA, Dey AN, Cohen AJ. Characteristics of adults with serious psychological distress as measured by the K6 scale, United States, 2001‐04. 2007. [PubMed]
- 61. Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184‐189. [DOI] [PubMed] [Google Scholar]
- 62. Prochaska JJ, Sung H‐Y, Max W, Shi Y, Ong M. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int J Methods Psychiatr Res. 2012;21(2):88‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Calonico S, Cattaneo MD, Titiunik R. Robust data‐driven inference in the regression‐discontinuity design. Stata J. 2014;14(4):909‐946. [Google Scholar]
- 64. Cattaneo MD, Idrobo N, Titiunik R. A Practical Introduction to Regression Discontinuity Designs: Volume I. Monograph Prepared for Cambridge Elements: Quantitative and Computational Methods for Social Science. Cambridge, UK: Cambridge University Press; 2018. [Google Scholar]
- 65. Imbens G, Angrist J. Identification and estimation of local average treatment effects. Econometrica. 1994;62(2):467‐475. [Google Scholar]
- 66. Calonico S, Cattaneo MD, Farrell MH, Titiunik R. Regression discontinuity designs using covariates. Rev Econ Stat. 2019;101(3):442‐451. [Google Scholar]
- 67. Lee DS, Card D. Regression discontinuity inference with specification error. J Econom. 2008;142(2):655‐674. [Google Scholar]
- 68. Gelman A, Imbens G. Why high‐order polynomials should not be used in regression discontinuity designs. J Bus Econ Stat. 2019;37(3):447‐456. [Google Scholar]
- 69. Calonico S, Cattaneo MD, Titiunik R. Robust nonparametric confidence intervals for regression‐discontinuity designs. Econometrica. 2014;82(6):2295‐2326. [Google Scholar]
- 70. Wieser S, Horisberger B, Schmidhauser S, et al. Cost of low back pain in Switzerland in 2005. Eur J Health Econ. 2011;12(5):455‐467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Picavet HSJ, Struijs JN, Westert GP. Utilization of health resources due to low back pain: survey and registered data compared. Spine. 2008;33(4):436. [DOI] [PubMed] [Google Scholar]
- 72. Chou R, Shekelle P. Will this patient develop persistent disabling low back pain? JAMA. 2010;303(13):1295‐1302. [DOI] [PubMed] [Google Scholar]
- 73. Balagué F, Mannion AF, Pellisé F, Cedraschi C. Non‐specific low back pain. The Lancet. 2012;379(9814):482‐491. [DOI] [PubMed] [Google Scholar]
- 74. Richmond H, Hall AM, Copsey B, et al. The effectiveness of cognitive behavioural treatment for non‐specific low back pain: a systematic review and meta‐analysis. PLoS One. 2015;10(8):e0134192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Hoffman BM, Papas RK, Chatkoff DK, Kerns RD. Meta‐analysis of psychological interventions for chronic low back pain. Health Psychol. 2007;26(1):1. [DOI] [PubMed] [Google Scholar]
- 76. Anheyer D, Haller H, Barth J, Lauche R, Dobos G, Cramer H. Mindfulness‐based stress reduction for treating low back pain: a systematic review and meta‐analysis. Ann Intern Med. 2017;166(11):799. [DOI] [PubMed] [Google Scholar]
- 77. Zhang A, Franklin C, Jing S, et al. The effectiveness of four empirically supported psychotherapies for primary care depression and anxiety: A systematic review and meta‐analysis. J Affect Disord. 2019;245:1168‐1186. [DOI] [PubMed] [Google Scholar]
- 78. Miyamoto GC, Lin C‐WC, Cabral CMN, van Dongen JM. Tulder MW van. Cost‐effectiveness of exercise therapy in the treatment of non‐specific neck pain and low back pain: a systematic review with meta‐analysis. Br J Sports Med. 2019;53(3):172‐181. [DOI] [PubMed] [Google Scholar]
- 79. Turner JA, Anderson ML, Balderson BH, Cook AJ, Sherman KJ, Cherkin DC. Mindfulness‐based stress reduction and cognitive‐behavioral therapy for chronic low back pain: similar effects on mindfulness, catastrophizing, self‐efficacy, and acceptance in a randomized controlled trial. Pain. 2016;157(11):2434‐2444. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author Matrix


