Key Points
Question
Are dance-based mind-motor activities associated with benefits for fall prevention and better physical functions, such as balance, mobility, and strength, in healthy adults 65 years and older?
Findings
This systematic review and meta-analysis of 29 randomized clinical trials found that dance-based mind-motor interventions were associated with a statistically significant reduction (37%) in fall risk and a statistically significant reduced rate (31%) of falls. There was a statistically significant association between favorable physical function outcomes and dance-based mind-motor activities for participants in the dance-based mind-motor intervention groups compared with those in the control groups.
Meaning
Dance-based mind-motor activities may help fall prevention efforts in healthy older adults.
Abstract
Importance
Falls increase morbidity and mortality in adults 65 years and older. The role of dance-based mind-motor activities in preventing falls among healthy older adults is not well established.
Objective
To assess the effectiveness of dance-based mind-motor activities in preventing falls.
Data Sources
Systematic search included the PubMed, Embase, Cochrane Library, Web of Science, CINAHL, PsychINFO, Abstracts in Social Gerontology, AgeLine, AMED, and Scopus databases from database inception to February 18, 2018, using the Medical Subject Headings aged 65 and older, accidental falls, and dancing.
Study Selection
This systematic review and meta-analysis included 29 randomized clinical trials that evaluated a dance-based mind-motor activity in healthy older adults with regard to fall risk, fall rate, or well-established measures of physical function in the domains of balance, mobility, and strength. The included studies targeted participants without comorbidities associated with higher fall risk. Dance-based mind-motor activities were defined as coordinated upright mind-motor movements that emphasize dynamic balance, structured through music or an inner rhythm (eg, breathing) and distinctive instructions or choreography, and that involve social interaction.
Data Extraction and Synthesis
Standardized independent screening, data extraction, and bias assessment were performed. Data were pooled using random-effects models. The study followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guideline.
Main Outcomes and Measures
Primary outcomes were risk of falling and rate of falls. For the secondary end points of physical function (balance, mobility, and strength), standardized mean differences (SMDs) were estimated and pooled (Hedges g).
Results
In this systematic review and meta-analysis of 29 randomized clinical trials, dance-based mind-motor activities were significantly associated with reduced (37%) risk of falling (risk ratio, 0.63; 95% CI, 0.49-0.80; 8 trials, 1579 participants) and a significantly reduced (31%) rate of falls (incidence rate ratio, 0.69; 95% CI, 0.53-0.89; 7 trials, 2012 participants). In addition, dance-based mind-motor activities were significantly associated with improved physical function in the domains of balance (standardized mean difference [SMD], 0.62; 95% CI, 0.33-0.90; 15 trials, 1476 participants), mobility (SMD, −0.56; 95% CI, −0.81 to −0.31; 13 trials, 1379 participants), and lower body strength (SMD, 0.57; 95% CI, 0.23-0.91; 13 trials, 1613 participants) but not upper body strength (SMD, 0.18; 95% CI, −0.03 to 0.38; 4 trials, 414 participants).
Conclusion and Relevance
Among healthy older adults, dance-based mind-motor activities were associated with decreased risk of falling and rate of falls and improved balance, mobility, and lower body strength. This type of activity may be useful in preventing falls in this population.
This systematic review and meta-analysis assesses the association of dance-based mind-motor activities with falls and physical function among healthy older adults.
Introduction
In industrialized countries, life expectancy and the number of age-related chronic diseases are increasing.1 Currently, approximately 30% of community-dwelling adults 65 years and older experience a fall per year, increasing up to approximately 50% of adults 80 years and older.2,3,4 Notably, more than 30% of falls among older adults need medical attention, and approximately 5% to 7% of falls result in a fracture.4,5 Consequently, falls are costly6 and carry a high risk of functional decline and loss of autonomy for the individual.4
On the other hand, exercise interventions are effective in improving strength, balance, and gait and reducing falls and related injuries among older adults.7,8 Dance-based mind-motor activities have been suggested as physical exercise9,10,11 with extended benefits beyond the physical on cognition,12,13 social interaction,14,15 quality of life,16 and motivation to be physically active.17,18 Mechanistically, these benefits may be explained by the multidimensional nature of these activities, which combine sensorimotor and cognitive engagement,19,20 relevant to fall prevention.
To our knowledge, no prior meta-analysis of randomized clinical trials (RCTs) has reported on associations between dance-based mind-motor activities and the risk of falling, the rate of falls, and physical function outcomes (balance, mobility, and strength). Therefore, we conducted a systematic review and meta-analysis to summarize the current evidence from RCTs among healthy adults 65 years and older.
Methods
Data Sources and Searches
For this systematic review and meta-analysis, we conducted a systematic search in PubMed, Embase, the Cochrane Library, Web of Science, CINAHL, PsychINFO, Abstracts in Social Gerontology, AgeLine, AMED, and Scopus databases from database inception to February 18, 2018, using thesaurus terms and key words (eAppendix in the Supplement for search terms used in PubMed). In addition, we performed lateral screening of the bibliographies of reviewed publications. We contacted authors of articles without sufficient information for complete data.
Study Selection
Screening and data extraction were predefined and standardized and followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline.21 At every stage, 2 independent researchers (from among M.M., M.F., U.M., and R.M.) screened each article. Disagreements were solved by consensus and, if necessary, by the consultation of a third independent reviewer (P.O.B.-C.). We included only RCTs that analyzed the effect of dance-based mind-motor activities on the number of persons who fell (risk of falling) or on the number of falls (rate of falls) as primary outcomes or at least 1 of the selected secondary outcomes related to physical function (balance, mobility, or strength) compared with an active (exercise not related to dance-based mind-motor activities) or a passive control group.
We defined dance-based mind-motor activities as coordinated upright mind-motor movements that emphasize dynamic balance, structured through music or an inner rhythm (eg, breathing) and distinctive instructions or choreography, and involve social interaction. Mind-motor activities are activities that combine cognitive and physical tasks (dual tasking or multitasking activities) that involve working memory and deliberate motor control. Dance-based mind-motor activities can be performed solo, in a pair, or in group formations. In addition to several styles of well-known dance-based mind-motor activities, such as folk or ballroom dancing, tai chi fulfills the above definition. Contrarily, most yoga styles focus on static body postures rather than dynamic movements and therefore were excluded. Furthermore, we excluded stepping exercises on so-called dance platforms because of the lack of social interaction.
We only considered RCTs that included healthy and ambulatory older adults (mean age, ≥65 years) living in the community or in independent living facilities. We excluded studies involving participants with comorbidities that directly affect the risk of falling (eg, Parkinson disease, type 2 diabetes, and cognitive decline). Only articles in the English language fulfilled the eligibility criteria. Two reviewers (from among M.M., M.F., U.M., and P.O.B.-C.) independently assessed potential sources of bias using the Cochrane Collaboration’s tool for assessing risk of bias.22 All included studies had been approved by an ethics committee and informed consent of participants had been obtained.
Statistical Analysis
To determine the strength of associations between a dance-based mind-motor activity and risk of falling and rate of falls, we pooled risk ratios (RRs) for risk of falling and Poisson-derived incidence rate ratios (IRRs) for the rate of falls using random-effects models based on intention-to-treat analysis. We estimated the IRRs based on reported incident falls and person-years in trials that did not directly report IRRs.
For the secondary outcomes, only trials that reported standardized, validated, and clinically used tests to measure balance, mobility, or strength were included: the Berg Balance Scale,23,24 the 1-leg test,25,26 and the functional reach test27 for balance; Timed Up and Go test28 for mobility; and sit to stand tests29,30 for lower body strength and the handgrip strength test31 for upper body strength. To determine the strength of associations between a dance-based mind-motor activity and physical function measures, we calculated a pooled Hedges g standardized mean difference (SMD) using a random-effects model.32 If a study reported outcomes stratified or by 2 tests that assessed the same outcome, we pooled the reported effect sizes before entering them into the meta-analysis. We weighted stratified outcomes by the inverse of the variance, assumed dependency between the assessments, and used a conservative correlation coefficient of 0.8.32 To interpret the effect of the intervention, we followed the guideline suggested by Cohen: equivalent effect size (SMD of 0), small effect size (SMD of 0.2), medium effect size (SMD of 0.5), and large effect size (SMD of 0.8).33
Heterogeneity was quantified by the I2 statistic as suggested by Borenstein et al.32 We performed prespecified subgroup analyses by type of dance-based mind-motor intervention (non–tai chi vs tai chi), frequency (<3 vs ≥3 times per week), duration (<12 vs ≥12 weeks), type of dwelling (community dwelling vs independent living facilities), and type of randomization (participants randomized vs cluster randomization). In addition, we performed a random-effects meta-regression by intervention frequency and intervention duration if more than 10 RCTs were included.
Small-study effects were assessed for each outcome if more than 10 RCTs were available. We conducted the Harbord modified test for the primary outcome of RR of falls34 and the Egger test for balance, mobility, and lower body strength.32 We used the Egger publication bias plot and funnel plots to visually assess indication of publication bias.35 We used Stata software, version 15 (StataCorp LLC) for data analysis.36 Statistical assessment was 2 sided and considered statistically significant at P < .05.
Results
Study Characteristics
From 4627 screened publications, 29 RCTs that fulfilled the inclusion criteria were identified (eAppendix in the Supplement). Eight trials37,38,39,40,41,42,43,44 reported on the risk of falling, 7 trials40,41,42,43,45,46,47 reported on the rate of falls, and 4 trials reported on both. A total of 15 trials37,38,39,40,41,44,48,49,50,51,52,53,54,55,56 reported on balance, 13 trials39,40,41,45,48,50,54,57,58,59,60,61,62 reported on mobility, 13 trials38,45,46,50,55,56,58,59,60,61,63,64,65 reported on lower body strength, and 4 trials44,47,55,59 reported on upper body strength. Table 1 gives an overview of all included trials. Table 2 lists the main descriptive statistics by outcome.
Table 1. Characteristics of Included Trialsa.
| Source | Populationb | Activity (No. of participants) | Female, %/age, mean (SD), y | Intervention group | Allocation/blinding of assessors | End point assessment | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention group | Control group | Total | Intervention group | Control group | Frequency, times per wk/class time, min | Duration of intervention | Adherence, mean, % | ||||
| Alves et al,48 2013 | Community dwelling; members of a dance project sponsored by the government; no further statement about socioeconomic status or race/ethnicity | Ballroom dance (25) | Control (25) | 50 | 84/69 (7) | 96/68 (8) | 2/120 | 16 wk | 90 | Participants randomized/NR or unclear | Balance: BBS; mobility: TUG test |
| Bennett et al,49 2018 | Community dwelling; recruited from the northwest Florida community via local senior centers; 91% White, 8.7% Black; most participants with grades 11-12 education | Line dancing (12) | Usual care/no exercise (11) | 23 | 83/73 (8) (total, both groups combined) | 91 | 2/60 | 8 wk | 80 | Participants randomized/no blinding of assessors | Balance: BBS |
| Cepeda et al,57 2015 | Community dwelling; no further statement about socioeconomic status or race/ethnicity | Ballroom dance (19) | Control (15) | 24 | 100/69 (7) | 100/72 (7) | 3/60 | 8 wk | 91 | Participants randomized/NR or unclear | Mobility: TUG test |
| Choi et al,37 2004 | Institutionalized; no further statement about socioeconomic status or race/ethnicity | Tai chi with music (29) | Control (30) | 59 | 79/77 (8) | 70/79 (7) | 3/35 | 12 wk | 70 | Facilities randomized (cluster randomization)/no blinding of assessors | Falls: risk of falling (RR); weekly monitoring of fall episodes during 12 wk of intervention; balance: OLS eyes open/eyes closed combined |
| Chyu et al,45 2010 | Community dwelling; postmenopausal women; no further statement about socioeconomic status or race/ethnicity | Tai chi (26) | Control (28) | 54 | 100/72 (6) | 100/71 (6) | 3/60 | 24 wk | 94 | Participants randomized/assessors blinded | Falls: rate of falls (IRR); self-reported at baseline, 12 and 24 wk; mobility: TUG test; lower body strength: 5 times STS test |
| Cruz-Ferreira et al,58 2015 | Community dwelling; women recruited from a local health center; no further statement about socioeconomic status or race/ethnicity | Creative dance (32) | Control (25) | 57 | 100/71 (4) | 100/73 (5) | 3/50 | 24 wk | 85 | Participants randomized/assessors blinded | Mobility: TUG test; lower body strength: 30-s STS test |
| Eyigor et al,38 2009 | Community dwelling; recruited in outpatient clinics; in the intervention group 64.7% had primary school education, in the control group 38.5%; most participants were housewives | Turkish folk dance (19) | Control (18) | 37 | 100/74 (8) | 100/71 (6) | 3/60 | 8 wk | NR | Participants randomized/assessors blinded | Falls: risk of falling (RR); unpublished data, reported by author on request; balance: BBS; lower body strength: 5 times STS test |
| Frye et al,59 2007 | Community dwelling; 94.4% White/non-Hispanic, 2.8% Black/non-Hispanic, 2.8% Asian/Pacific Islander; well-educated sample: 18.1% with postcollege degree, 20.8% with 4-y college degree, 26.4% with some college degree, 18.1% with high school diploma, 2.8% some high school | Tai chi (23) | Control (21) | 44 | 64/69 (9) (total, both groups combined) | 3/60 | 12 wk | 91.4% Of participants attended at least 80% of classes | Participants randomized/PI, project coordinator, and instructors not blinded, unclear if assessors were blinded | Mobility: TUG test; lower body strength: 30-s STS test; upper body strength: HGS | |
| Hopkins et al,53 1990 | Community dwelling; no further statement about socioeconomic status or race/ethnicity | Low-impact aerobic dance (30) | Control (23) | 53 | 100/65 (4) | 100/66 (4) | 3/50 | 12 wk | NR | Participants randomized/NR or unclear | Balance: OLS; mobility: TUG test; lower body strength: 30-s STS test |
| Huang et al,39 2010 | Community dwelling; 35.5% in tai chi group and 68.1% in the control group had ≤6 y of education | Tai chi (31) | Control (47) | 78 | 29/71 (0) | 40/72 (1) | 3/40 | 5 mo (21 wk) | NR | Villages randomized (cluster randomization)/NR or unclear | Falls: risk of falling (RR); assessed during follow-up, means of assessment NR; balance: FR; mobility: TUG test |
| Hui et al,60 2009 | Community dwelling; no further statement about socioeconomic status or race/ethnicity | Low-impact aerobic dance (52) | Control (45) | 97 | 96/68 (5) | 98/69 (4) | Approximately 2 (total 23 sessions)/50-60 | 12 wk | 91.3 | Social centers randomized (cluster randomization)/assessors blinded | Mobility: TUG test; lower body strength: 10-s STS test (treated same way in meta-analysis as trials reporting 30-s STS test) |
| Janyacharoen et al,63 2013 | Community dwelling; no further statement about socioeconomic status or race/ethnicity | Traditional Thai dance (20) | General aerobic exercises in daily life (18) | 38 | 100/67 (6) | 100/65 (4) | 3/40 | 6 wk | NR | Participants randomized/assessors blinded | Lower body strength: 5 times STS test |
| Li et al,40 2005 | Community dwelling; recruited from the pool of patients enrolled in the Legacy Health System in Portland, Oregon; 90% in tai chi group and 91% in control group were White; 94% in tai chi group and 90% in control group had high school degree or higher; annual household income was <$35 000 for 64% in the tai chi group and for 70% in the control group | Tai chi (125) | Seated stretching exercises (131) | 256 | 70/77 (5) | 70/78 (5) | 3/60 | 26 wk | Median adherence rate for both groups: 61 of approximately 72 sessions scheduled | Participants randomized/assessors blinded | Falls: risk of falling (RR), fall rate (IRR); means of falls assessment NR; balance: BBS, OLS, FR, combined; mobility: TUG test |
| Li et al,51 2008 | Community dwelling; participating in social and recreational activities outside their home on a minimum of 2 occasions per week; no further statement about socioeconomic status or race/ethnicity | Tai chi (22) | Discussion meetings (18) | 40 | 50/65 (3) | 50/66 (4) | 4/60 | 16 wk | 92 | Participants randomized/NR or unclear | Balance: OLS |
| Logghe et al,52 2009 | Community dwelling; identified through the patient registration files of participating GPs; GPs invited participants to participate; 71% in tai chi group and 65.5% in control group had high school education or more; 96.2% in the tai chi group and 91.3% in the control group were born in the Netherlands | Tai chi (138) | Control (131) | 269 | 70/78 (5) | 73/77 (5) | 2/60 | 13 wk | 47% Of participants attended at least 80% of classes | Participants randomized/assessors blinded | Balance: BBS |
| McKinley et al,64 2008 | Community dwelling; no further statement about socioeconomic status or race/ethnicity | Tango dance program (14) | Walking (11) | 25 | 78/78 (8) | 72/75 (8) | 2/120 | 10 wk | >90 (Both groups) | Participants randomized/assessors blinded | Lower body strength: 5 times STS test |
| Merom et al,46 2016 | Residents of self-care retirement villages; 17% non-English speaking, 73% born in Australia; 36% with ≤10 y of education | Folk or ballroom dance (275) | Delayed intervention (247) | 522 | 83/43% >80 y; all participants at least 60 y | 86/35% >80 y; all participants at least 60 y | 2/60 | 12 mo (52 wk/total of 80 lessons) | 51 | Retirement villages randomized (cluster randomization)/assessors were not blinded at follow-up assessments | Falls: rate of falls (IRR); daily self-report in diaries that were sent to study center on monthly basis; if a fall happened or the diary was not sent in, participants were called to assess details; strength: 5 times STS test |
| Merom et al,65 2016 | Community dwelling; 45.0% in the dance group and 52.7% in the control group had primary/high school as highest education level, 21.7% in the dance group and 20.0% in the control group had TAFE apprenticeship and 33.3% in the dance group, and 27.3% in the control group had university degrees | Ballroom dance (40) | Walking program (39) | 79 | 85/60-69 y: 50%; 70-74 y: 25%; ≥75 y: 25% | 85/60-69 y: 62%; 70-74 y: 18%; ≥75 y: 21% | 2/60 | 8 mo (34 wk; approximately 69 sessions) | 66 | Participants randomized/assessors only at baseline blinded, but not on follow-up assessments | Lower body strength: 5 times STS test |
| Noradechanunt et al,61 2017 | Community dwelling; 76.9% in tai chi group and 92.3% in control group had high school or higher education | Tai chi (9) | Telephone counseling (10) | 19 | 69/67 (8) | 77/65 (7) | 2/90 | 12 wk | 85 | Participants randomized/assessors blinded | Mobility: TUG test; lower body strength: 30-s STS test |
| Pereira et al,53 2008 | Community dwelling; women registered in the university’s physical activity program for elderly people; no further statement about socioeconomic status or race/ethnicity | Tai chi (38) | Control (39) | 77 | 100/68 (5) | 100/69 (7) | 3/50 | 12 wk | NR | Participants randomized/NR or unclear | Balance: OLS |
| Serano-Guzmann et al,54 2016 | Community dwelling; White postmenopausal women attending a primary care clinic and referred to the clinical laboratory of the physiotherapy department at the University of Granada, Spain | Flamenco and sevillanas (27) | Self-care treatment advice (25) | 52 | 100/69 (4) | 100/69 (3) | 3/50 | 8 wk | 100 | Participant randomized/assessors blinded | Balance: OLS; mobility: TUG test |
| Sun et al,55 2015 | Community dwelling; recruited via public announcement, 55.5% in the tai chi group and 72.8% in the control group had ≥12 y of education | Tai chi (72) | Social activities (66) | 138 | 81/68 (6) | 70/70 (6) | 2/60 | 6 mo (26 wk) | NR | Participant randomized/NR or unclear | Balance: OLS; upper body strength: HGS (results were combined for right and left hand before entering the meta-analysis) |
| Taylor et al,62 2012 | Community dwelling; recruited in Auckland, Dunedin, and Christchurch, New Zealand; 12 participants identified as Māori or Pacific Islander | Group 1: Tai chi (233); group 2: tai chi (220) | Group 1: low-level exercise (231); group 2: low-level exercise (231) | Group 1: 264; group 2: 251 | Group 1: 69/75 (7); group 2: 76/74 (6) | Group 1: 76; 74 (6); group 2: 76/74 (6) | Group 1: 1/60; group 2: 2/60 | Group 1: 20 wk; group 2: 20 wk | Group 1: 79; group 2: 72 | Participants randomized/assessors blinded | Mobility: TUG test (results were combined for groups 1 and 2 before entering the meta-analysis); lower body strength: 30-s STS test (results were combined for groups 1 and 2 before entering the meta-analysis) |
| Taylor-Piliae et al,56 2010 | Community dwelling; recruited in Santa Clara County or San Mateo County in California; college educated, 85% White | Tai chi (37) | Attendance control/no exercise (56) | 93 | 65/71 (6) | 73/68 (6) | 2/45 | 6 mo (26 wk) | 77 | Participants randomized/assessors blinded | Balance: OLS, FR; lower body strength: 30-s STS test |
| Trombetti et al,41 2011 | Community dwelling; 11% in early intervention and 19% in delayed intervention had primary school education, 66% in early intervention and 68% in delayed intervention had middle school education, and 21% in early intervention and 15% in delayed intervention had high school education | Dalcroze eurhythmics (66) | Delayed intervention (68) | 134 | 97/75 (8) | 96/76 (6) | 1/60 | 25 wk | 83 | Participants randomized/assessors blinded | Falls: risk of falling (RR), rate of falls (IRR); prospectively monitored daily with falls diaries that were mailed monthly to study coordinator; balance: OLS; mobility: TUG test |
| Voukelatos et al,42 2007 | Community dwelling in Central and Southeastern Sydney, Australia; 14% in the tai chi group and 17% in the control group had university education, 43% in the tai chi group and 41% in the control group had intermediate-level education, 16% in the tai chi group and 12% in the control group had below intermediate-level education; remaining participants had secondary education or technical college education | Tai chi (347) | Wait-list control (337) | 684 | 85/69 (7) (total, both groups combined) | 83 | 1/60 | 16 wk | 71 | Participants randomized/assessors blinded | Falls: risk of falling (RR), rate of falls (IRR); prospectively monitored daily during 24 wk with a falls calendar that was mailed back to study center monthly; if participants did not send back falls calendars, they were called within 2 wk to assess fall status |
| Wolf et al,47 1996 | Community dwelling; 20.8% in tai chi group and 20.3% in the wellness education group had elementary or high school education, 56.9% in the tai chi group and 51.6% in the wellness education group had college education, and 22.2% in the tai chi group and 28.1% in the wellness education group had graduate school education | Tai chi (72) | Wellness education (64) | 137 | 81/77 (5) | 84/75 (4) | 2/Minimum of 45 (individual); instructor time, unclear how much time in group setting; participants were asked to perform the exercises 2 times daily for 15 min | 15 wk | NR | Participants randomized/assessors blinded | Falls: rate of falls (IRR); monthly calendars or monthly telephone calls by project staff; nurse coordinator verified all fall reports requiring medical attention; upper body strength: HGS |
| Wolf et al,43 2003 | Institutionalized; 80.0% in the tai chi group and 81.6% in the wellness group were White; 80.0% in the tai chi group and 78.0% in the wellness group had high school and beyond education | Tai chi (145) | Wellness education (141) | 286 | 95/81 (7) | 94/81 (6) | 2/60-90 | 48 wk | 76 | Facilities randomized (cluster randomization)/assessors blinded | Falls: risk of falling (RR), rate of falls (IRR); participants reported if they experienced a fall (1) to identify the day and (2) to give details about circumstances and if medical attention was needed; forms were sent to instructor weekly and reviewed by study staff monthly; participants who fell were called to confirm the fall within 1 wk after reviewing of the forms; participants who did not hand in their forms were called for confirmation within 1-2 wk |
| Woo et al,44 2007 | Community dwelling, recruited from community centers in Shatin, Hong Kong; no further statement about socioeconomic status or race/ethnicity | Tai chi (60) | Control (60) | 120 | 50/Men: 68 (2); women: 70 (3) | 50/Men: 68 (3); women: 70 (3) | 3/NR | 12 mo (52 wk) | 81 | Participants randomized/assessors blinded | Falls: risk of falling (RR); means of assessment NR; balance: OLS (reported average of both legs); upper body strength: HGS (dominant hand, results were combined for men and women before entering the meta-analysis) |
Abbreviations: BBS, Berg Balance Scale; FR, functional reach; GP, general practitioner; HGS, handgrip strength; IRR, incidence rate ratio; NR, not reported; OLS, 1-leg stance; RR, risk ratio; SMD, standardized mean difference (Hedges g); STS, sit to stand; TAFE, Technical and Further Education; TUG, Timed Up and Go.
Numbers are rounded to whole numbers.
Type of dwelling, statements about socioeconomic status (income and education level), and race/ethnicity as reported by the authors.
Table 2. Characteristics of Included Trials.
| Source | Intervention | Adherence, % | Sample size, median (IQR) [range] | Age, weighted mean (SD), y | Intervention duration (follow-up time), median (IQR) [range], wk | Session duration, median (IQR) [range], min |
|---|---|---|---|---|---|---|
| Risk of falling (RR) (n = 8 trials including 1579 participants)a | ||||||
| Choi et al,37 2004 | Tai chi with music | 70 | 127 (73.25-212.50) [30-684] | 73.19 (4.94) | 22 (15-30) [8-48] | 60 (42.4-60) [35-60]b |
| Eyigor et al,38 2009 | Turkish folk dance | Not reported | ||||
| Huang et al,39 2010 | Tai chi | Not reported | ||||
| Li et al,40 2005 | Tai chi | 61 of 72 lessons scheduled | ||||
| Trombetti et al,41 2011 | Dalcroze eurhythmics | 83 | ||||
| Voukelatos et al,42 2007 | Tai chi | 71 | ||||
| Wolf et al,43 2003 | Tai chi | 76 | ||||
| Woo et al,44 2007 | Tai chi | 81 | ||||
| Rate of falls (IRR) (n = 7 trials including 2012 participants)a | ||||||
| Chyu et al,45 2010 | Tai chi | 94 | 188 (135-408) [54-702] | 74.40 (4.33)c | 24 (20-36) [15-52] | 60 (60-60) [45-70] |
| Li et al,40 2005 | Tai chi | 61 of 72 lessons scheduled | ||||
| Merom et al,46 2016 | Folk or ballroom dance | 51 | ||||
| Trombetti et al,41 2011 | Dalcroze eurhythmics | 83 | ||||
| Voukelatos et al,42 2007 | Tai chi | 71 | ||||
| Wolf et al,47 1996 | Tai chi | Not reported | ||||
| Wolf et al43 2003 | Tai chi | 76 | ||||
| Balance (SMD) (n = 15 trials including 1476 participants)a | ||||||
| Alves et al,48 2013 | Ballroom dance | 90 | 77 (51-125.5) [23-269] | 72.90 (4.2) | 16 (21-24) [8-48] | 60 (50-60) [35-120]b |
| Bennett et al,49 2018 | Line dancing | 80 | ||||
| Choi et al,37 2004 | Tai chi with music | 70 | ||||
| Eyigor et al,38 2009 | Turkish folk dance | Not reported | ||||
| Hopkins et al,53 1990 | Aerobic dance | Not reported | ||||
| Huang et al,39 2010 | Tai chi | Not reported | ||||
| Li et al,40 2005 | Tai chi | 85 (61 of 72 lessons scheduled) | ||||
| Li et al,51 2008 | Tai chi | 92 | ||||
| Logghe et al,52 2009 | Tai chi | 47% Of participants attended at least 80% of classes | ||||
| Pereira et al,53 2008 | Tai chi | Not reported | ||||
| Serano-Guzmann et al,54 2016 | Flamenco and sevillanas | 100 | ||||
| Sun et al,55 2015 | Tai chi | Not reported | ||||
| Taylor-Piliae et al,56 2010 | Tai chi | 77 | ||||
| Trombetti et al,41 2011 | Dalcroze eurhythmics | 83 | ||||
| Woo et al,44 2007 | Tai chi | 81 | ||||
| Mobility (SMD) (n = 13 trials including 1379 participants)a | ||||||
| Alves et al,48 2013 | Ballroom dance | 90 | 54 (50-97) [19-451] | 73.02 (3.25) | 16 (12-24) [8-52] | 60 (40-60) [40-120] |
| Cepeda et al,57 2015 | Ballroom dance | 91 | ||||
| Chyu et al,45 2010 | Tai chi | 94 | ||||
| Cruz-Ferreira et al,58 2015 | Creative dance | 85 | ||||
| Frye et al,59 2007 | Tai chi | 91.4% Of participants attended at least 80% of classes | ||||
| Hopkins et al,53 1990 | Low-impact aerobic dance | Not reported | ||||
| Huang et al,39 2010 | Tai chi | Not reported | ||||
| Hui et al,60 2009 | Low-impact aerobic dance | 91.3 | ||||
| Li et al,40 2005 | Tai chi | 85 (61 of 72 lessons scheduled) | ||||
| Noradechanunt et al,61 2017 | Tai chi | 85 | ||||
| Serano-Guzmann et al,54 2016 | Flamenco and sevillanas | 100 | ||||
| Taylor et al,62 2012 | Tai chi | 1 Time per week: 79; 2 times per week: 72 | ||||
| Trombetti et al,41 2011 | Dalcroze eurhythmics | 83 | ||||
| Lower body strength (SMD) (n = 13 trials including 1613 participants)a | ||||||
| Chyu et al,45 2010 | Tai chi | 94 | 54 (38-97) [19-530] | 73.14 (3.30)c | 12 (12-24) [6-52] | 60 (50-60) [40-120] |
| Cruz-Ferreira et al,58 2015 | Creative dance | 85 | ||||
| Eyigor et al,38 2009 | Turkish folk dance | Not reported | ||||
| Frye et al,59 2007 | Tai chi | 91.4% Of participants attended at least 80% of classes | ||||
| Hopkins et al,53 1990 | Low-impact aerobic dance | Not reported | ||||
| Hui et al,60 2009 | Low-impact aerobic dance | 91.3 | ||||
| Janyacharoen et al,53 2013 | Thai dance | Not reported | ||||
| McKinley et al,63 2008 | Adapted tango | >90 | ||||
| Merom et al,46 2016 | Folk or ballroom dance | 51 | ||||
| Merom et al,65 2016 | Ballroom dance | 66 | ||||
| Noradechanunt et al,61 2017 | Tai chi | 85 | ||||
| Taylor et al,62 2012 | Tai chi | 1 Time per week: 79; 2 times per week: 72 | ||||
| Taylor-Piliae et al,56 2010 | Tai chi | 77 | ||||
| Upper body strength (SMD) (n = 4 trials including 414 participants)a | ||||||
| Frye et al,59 2007 | Tai chi | 91.4% Of participants attended at least 80% of classes | 116 (95-124.5) [44-138] | 70.78 (3.3) | 20.5 (14.25-32.5) [12-52] | 60 (52.5-60) [45-60]b |
| Sun et al,55 2015 | Tai chi | Not reported | ||||
| Wolf et al,47 1996 | Tai chi | Not reported | ||||
| Woo et al,44 2007 | Tai chi | 81 | ||||
| Total | ||||||
| All 29 included trials | NA | NA | 77 (44-136) [19-702] | 73.10 (4.22)c | 16 (12-24) [6-52] | 60 (50-60) [35-120]b |
Abbreviations: IQR, interquartile range; IRR, incidence rate ratio; NA, not applicable; RR, risk ratio; SMD, standardized mean difference (Hedges g).
Total sum of participants of all trials included within specific outcome.
Woo et al44 do not report on session duration; therefore, numbers were calculated without this study.
Overall, the sample size of the trials varied greatly, from 19 up to 684 participants. Most trials38,39,40,41,42,44,45,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65 included community-dwelling older adults, with most participants being women. Seven trials37,40,41,43,47,52,64 reported the mean age of their population being at least 70 years. Three trials37,43,46 were conducted among participants living in independent living facilities. Five trials37,39,43,46,60 used cluster randomization.
Within the 29 trials, the interventions lasted between 6 weeks and 12 months, and the duration of intervention sessions ranged from 35 to 120 minutes. The frequency of the study intervention varied between once per week41,42 and 4 times per week,51 with most trials reporting 2 times per week43,46,47,48,49,52,55,56,60,61,62,64,65 or 3 times per week.37,38,39,40,44,45,50,53,54,57,58,59,63 Adherence was at least 80% in 15 of the 22 trials40,41,44,45,48,49,51,52,54,57,58,59,60,61,64 that reported adherence.
In terms of type of dance-based mind-motor activity, 13 trials38,41,46,48,49,50,54,57,58,60,63,64,65 investigated activities that involved dance styles, such as ballroom or folk dances, and 16 trials37,39,40,42,43,44,45,47,51,52,53,55,56,59,61,62 investigated tai chi.
More than half of the trials were conducted in North America40,43,45,47,48,49,50,56,59,64 (10 trials) or Asia37,44,51,55,60,63 (7 trials). Five trials each were from Europe38,41,52,54,58 and Oceania,42,46,61,62,65 and 2 trials53,57 were from South America.
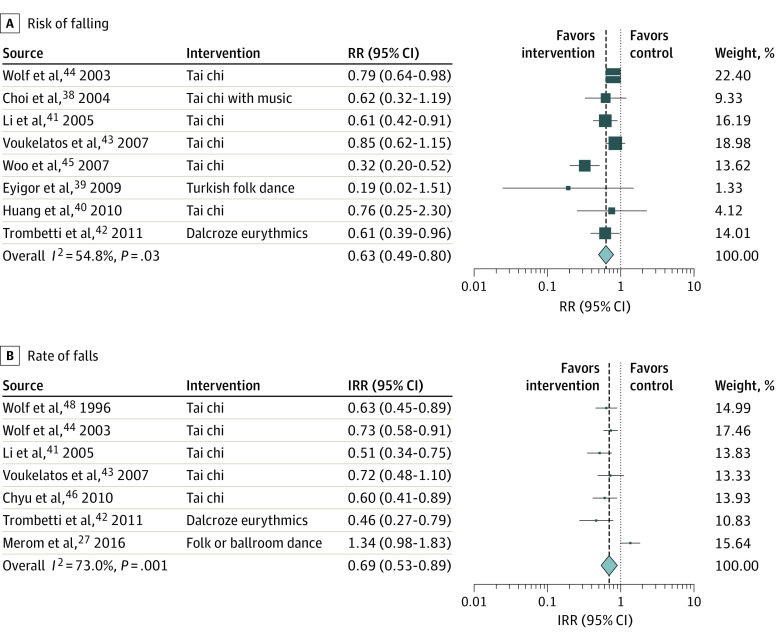
Primary Outcomes: Risk of Falling and Rate of Falls
Dance-based mind-motor activities were associated with 37% reduction in risk of falling (RR, 0.63; 95% CI, 0.49-0.80) (Figure 1A) based on 8 trials37,38,39,40,41,42,43,44 of 1579 participants, with a weighted mean (SD) age of 73.2 (4.9) years, a median sample size of 127 (range, 30-684), and median intervention duration of 22 weeks (range, 8-48 weeks).
Figure 1. Association of Dance-Based Mind-Motor Activities With Falls .
For risk of falling, the total sample size by pooling 8 trials was 1579. For rate of falls, the total sample size by pooling 7 trials was 2012. Weights are from random-effects analysis. Box sizes correspond to precision; the bigger the box, the more precise. Precision was determined as the inverse of the variance. IRR indicates incidence rate ratio; RR, risk ratio.
Prespecified subgroup analyses revealed a significant association with reduction of risk of falling for trials that conducted interventions 3 times per week or more (RR, 0.47; 95% CI, 0.31-0.72) and for trials with durations between 12 and 24 weeks (RR, 0.71; 95% CI, 0.58-0.86 (eAppendix in the Supplement).
Two sensitivity analyses were performed for risk of falling, one excluding the trial by Woo et al,44 which was driving the pooled result, and one excluding the trial by Eyigor et al,38 from which unpublished results were taken. For both sensitivity analyses, the pooled RR remained statistically significant in favor of the intervention groups (RR, 0.74; 95% CI, 0.64-0.86 for the analysis excluding the trial by Woo et al,44 and RR, 0.64; 95% CI, 0.50-0.82 for the analysis excluding the trial by Eyigor et al38) (eAppendix in the Supplement).
For rate of falls, dance-based mind-motor activities were associated with a reduction by 31% (IRR, 0.69; 95% CI, 0.53-0.89; 7 trials) (Figure 1B) based on 7 trials of 2012 participants with a weighted mean (SD) age of 74.4 (4.3) years, a median sample size of 188 (range, 54-684), and a median intervention duration of 24 weeks (range, 15-52 weeks).
Subgroup analyses suggested this association was most pronounced in trials that conducted the intervention 3 times per week or more (IRR, 0.55; 95% CI, 0.42-0.73) and for trials that lasted between 12 and 24 weeks (IRR, 0.59; 95% CI, 0.49-0.71) (eAppendix in the Supplement).
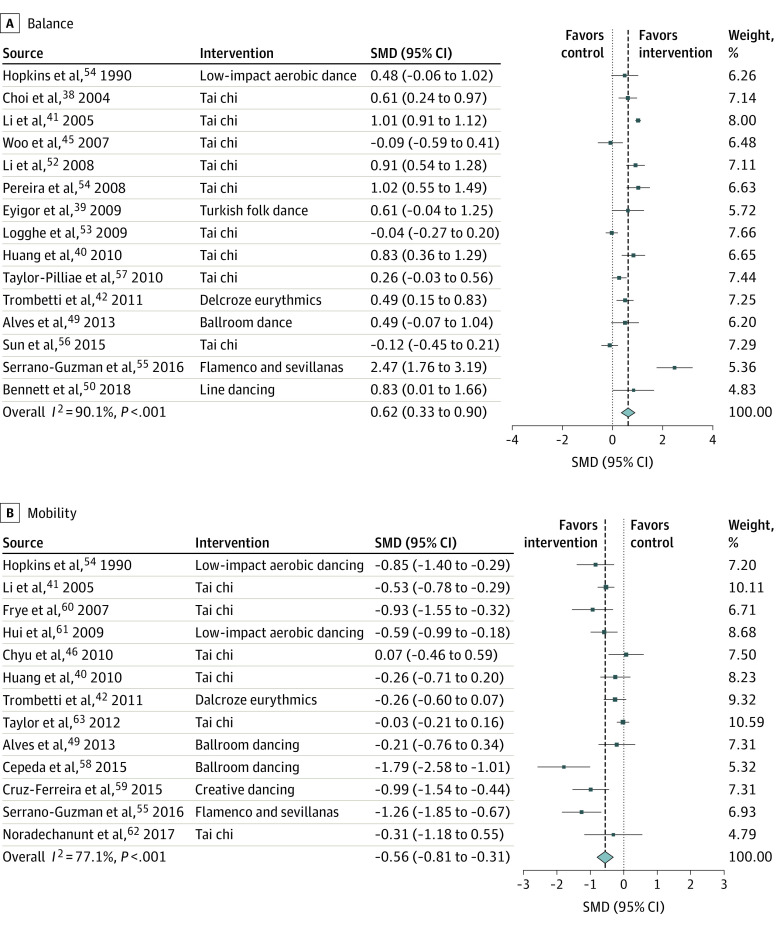
Secondary Outcome: Physical Function
An association was found between dance-based mind-motor activities and improved balance (SMD, 0.62; 95% CI, 0.33-0.90) (Figure 2A) in 15 trials37,38,39,40,41,44,48,49,50,51,52,53,54,55,56 of 1476 participants, with a weighted mean (SD) age of 72.3 (4.3) years, a median sample size of 77 (range, 23-269), and a median intervention duration of 16 weeks (range, 8-48 weeks). Subgroup analyses by intervention type found a higher SMD for non–tai chi (SMD, 0.86; 95% CI, 0.33-1.39) activities. Interventions performed 3 times per week or more were associated with a higher SMD (SMD, 0.84; 95% CI, 0.54, 1.14). Sensitivity analyses excluding the trial by Hopkins et al50 (published much earlier than the others) or the trial by Serrano-Guzman et al54 (driving the result) also found an association between dance-based mind-motor and improved balance (SMD, 0.63; 95% CI, 0.33-0.93 for the analysis excluding the trial by Hopkins et al50 and SMD, 0.51; 95% CI, 0.24-0.78 for the analysis excluding the trial by Serrano-Guzman et al54).
Figure 2. Association of Dance-Based Mind-Motor Activities With Balance and Mobility.
Effect sizes are Hedges g standardized mean differences (SMDs). Weights are from random-effects analysis. Box sizes correspond to precision; the bigger the box, the more precise. Precision was determined as the inverse of the variance for each estimate. For balance (A), assessments included the Berg Balance Scale, 1-leg stance, and functional reach. For the Berg Balance Scale and 1-leg stance, an increase of time indicates an improvement in the test result. For functional reach, an increase in reached distance indicates an improvement. Hence, positive values would favor the intervention groups over the control groups. For mobility (B), all included trials assessed mobility with the Timed Up and Go test. Decreased completion time indicated improvement in the Time Up and Go Test result. Hence, negative values would favor the intervention groups over the control groups.
An association was also found between dance-based mind-motor activities and improved mobility (SMD, –0.56; 95% CI, –0.81 to –0.31) (Figure 2B) based on 13 trials39,40,41,45,48,50,54,57,58,59,60,61,62 of 1379 participants, with a weighted mean (SD) age of 73.0 (3.3 years), a median sample size of 54 (range, 19-451), and a median intervention duration of 16 weeks (range, 8-52 weeks). For mobility, decreased completion time indicated improvement in Timed Up and Go test results. Hence, negative values would favor the intervention groups over control groups. Subgroup analyses found positive associations for non–tai chi activities (SMD, –0.79; 95% CI, –1.16 to –0.42) and for activities with 3 sessions or more per week (SMD, –0.76; 95% CI, –1.10 to 0.42). The results remained positively associated within sensitivity analyses that excluded the trial by Hopkins et al50 or the trial driving the results by Cepeda et al57 (SMD, –0.54; 95% CI, –0.80 to –0.28 for the analysis excluding the trial by Hopkins et al50 and SMD, –0.48; 95% CI, –0.71 to –0.25 for the analysis excluding the trial by Cepeda et al57).
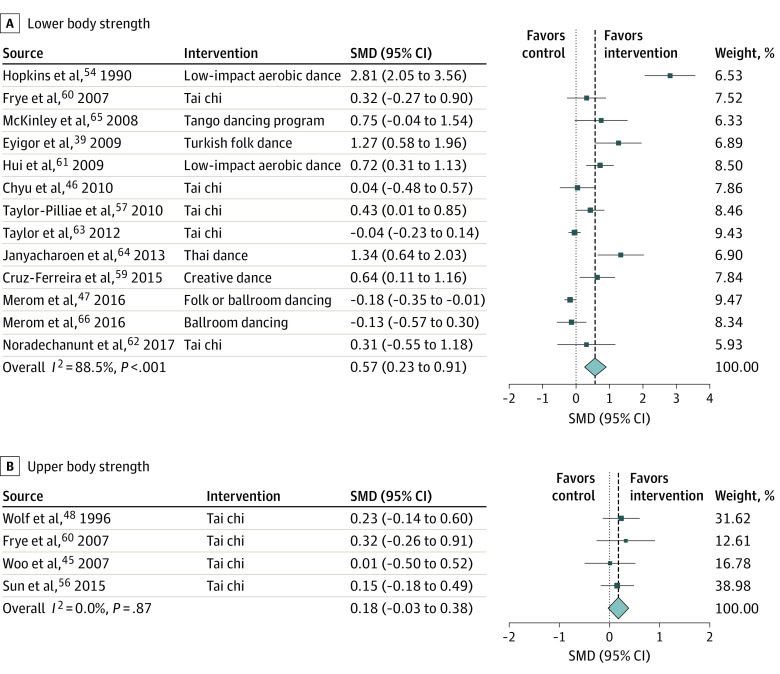
Dance-based mind-motor activities were associated with improved lower body strength (SMD, 0.57; 95% CI, 0.23-0.91) (Figure 3A), based on 13 trials38,45,50,56,58,59,60,61,62,63,64,65 with 1613 participants with a weighted mean (SD) age of 73.1 (3.3) years, a median sample size of 54 (range, 19-530), and a median intervention duration of 12 weeks (range, 6-52 weeks). Subgroup analyses supported a positive association with improved lower body strength for non–tai chi activities (SMD, 0.86; 95% CI, 0.25-1.47) and intervention frequencies of 3 times per week or more (SMD, 1.04; 95% CI, 0.31-1.77). In a sensitivity analysis excluding the early trial by Hopkins et al,50 the SMD remained significant (SMD, 0.39; 95% CI, 0.12-0.65). No significant association was found between dance-based mind-motor activities and upper body strength (SMD, 0.18; 95% CI, −0.03 to 0.38) (Figure 3B) based on 4 trials44,47,55,59 with 414 participants. For subgroup and sensitivity analyses of physical function outcomes, see the eAppendix in the Supplement.
Figure 3. Association of Dance-Based Mind-Motor Activities With Body Strength.
Effect sizes are Hedges g standardized mean differences (SMDs). Weights are from random-effects analysis. Box sizes correspond to precision; the bigger the box, the more precise. Precision was determined as the inverse of the variance for each estimate. For lower body strength (A), assessments included the 5 times sit to stand (STS) test (the time to complete 5 stands is measured) and the 30-second STS test (number of stands completed within 30 seconds is measured). Effect sizes of the 5 times STS test were multiplied by −1 to achieve same direction signaling improvement as the effect sizes of the 30-second STS test. Hence, positive values would favor the intervention groups over the control groups. For upper body strength (B), all included trials assessed UBS using handgrip strength. Increasing values indicate an improvement in the test result. Hence, positive values would favor the intervention groups over the control groups.
Assessment of Small-Study Effects
The limited number of trials did not allow for the assessment of small-study effects for the risk of falling, rate of falls, and upper body strength.22 For balance, visual inspection of the funnel plot suggested asymmetry, but there was no evidence of small-study effects based on the Egger test (intercept, −1.59; SE, 1.45; P = .29). For mobility and lower body strength, the funnel plots showed asymmetry, and the Egger test result was statistically significant (intercept, −2.87; SE, 1.04; P = .02 for mobility and intercept, 4.04; SE, 1.05; P = .003 for lower body strength), suggesting that small-study effects cannot be ruled out.
Assessment of Heterogeneity
Moderate heterogeneity was found for the primary outcomes (risk of falling: I2 = 54.8%, P = .03; rate of falls: I2 = 73.0%, P = .001). For secondary outcomes, substantial heterogeneity was found in all domains except upper body strength (balance: I2 = 90.1%, P < .001; mobility: I2 = 77.1%, P < .001; lower body strength: I2 = 88.5%, P < .001; upper body strength: I2 = 0.0%, P = .87).
Assessment of Bias
Based on the Cochrane tool of bias,66 a high risk of bias was found for at least 1 domain in 10 trials37,38,39,46,49,51,58,59,60,65 and an unclear risk of bias in at least 1 domain for every included trial (eAppendix in the Supplement).66
Discussion
In this systematic review and meta-analysis, which included 29 trials of 4239 healthy older adults, there was a significant association between dance-based mind-motor activities, including both tai chi and non–tai chi activities, and reductions in the risk of falling and the rate of falls. The association of dance-based mind-motor activities with consistent improvements in balance, mobility, and lower body strength supports these findings. Notably, the predefined subgroup analyses suggest that greater frequency (≥3 times per week) and a duration of the intervention between 12 and 24 weeks are associated with greater benefits from these interventions with regard to fall and functional outcomes.
For fall prevention, the analysis of dance-based mind-motor interventions are in alignment with findings of prior meta-analyses67,68 of multicomponent physical exercise interventions or tai chi alone. Although the analyses for the primary outcomes included more trials that investigated tai chi than non–tai chi dance-based mind-motor activities, the results by subgroups of type of dance-based mind-motor activities suggest that non–tai chi trials might have similar associations with risk of falls and fall rate reductions. In particular, there was a consistently stronger association with improvement of function and non–tai chi dance-based mind-motor interventions for balance, mobility, and lower body strength, and the results therefore extend and strengthen the evidence base of exercise trials that focus on multitasking skills for fall prevention among healthy older adults.
To our knowledge, this meta-analysis is the first that aims to summarize the associations of dance-based mind-motor activities beyond tai chi with the risk of falling and the rate of falls among healthy older adults. Earlier systematic reviews that investigated dance-based mind-motor activities among healthy older adults suggested a beneficial effect for fall prevention solely based on the improvement of balance or strength9,10,11,69 or included tai chi interventions only.68 Other meta-analyses on the effect of dance-based mind-motor activities preselected on cardiovascular risk,70 Parkinson disease,71 or cognitive12,72 function. Sheldon et al67 report subgroup analyses only for 1 trial in the category dance, whereas the present study additionally included 2 trials that investigated non–tai chi activities for each outcome (risk of falling38,41 and rate of falls41,46).
Furthermore, the present meta-analysis supports benefits of dance-based mind-motor activities for several dimensions of physical function, including balance, mobility, and lower body strength. The observed nonsignificant association on upper body strength may be explained by the fact that the upper extremities in dance-based mind-motor activities are used for expression and partnering rather than building strength or body weight support.
Strengths and Limitations
This study has strengths and limitations. Strengths include the comprehensive search strategy within 10 different databases, which incorporated unpublished information from authors38 and was built on the conceptual framework established by the Prevention of Falls Network Europe (ProFaNE).67 In addition to ProFaNE’s definition of 3-dimensional training, this study combined mind and motor abilities, as well as the domain of social interaction. In this meta-analysis, 13 of 29 trials38,41,46,48,49,50,54,57,58,60,63,64,65 tested dance styles.
This study found consistent associations between dance-based mind-motor activities and improvement for falls and physical function, and the associations remained significant for all sensitivity analyses performed with influential studies excluded. Finally, relevant to implementation of dance-based mind-motor activities into public health strategies, most trials included in this meta-analysis reported at least 80% adherence, which may be better than previously reported adherence rates for other structured exercise interventions.25,67
This meta-analysis also has limitations. Because of the limited number of non–tai chi trials, several of these trials had to be excluded, giving a stronger weight to the tai chi interventions. However, subgroup analyses excluding the tai chi trials support a similar positive association of non–tai chi activities with balance, mobility, and lower body strength as tai chi. Although data for risk of falling and fall rate were collected with sufficient quality, aspects of physical function, such as balance and strength, were evaluated in part with nonstandardized and noncomparable assessment devices, such as balance platforms or isokinetic machines, which led to the exclusion of several trials that reported on physical function. Finally, these results might not be generalizable to older men because all but 1 trial included mainly women.39,44,51
Conclusions
Although these results found significant positive associations across risk of falling, rate of falls, and 3 of 4 investigated functional measures and are therefore promising in their consistency and effect size for fall prevention, the study also documented limitations in the quality of individual trials. This is true especially for the non–tai chi interventions. Tai chi is among the best-studied activities for older adults.68 However, additional high-quality trials investigating other types of dance-based mind-motor activities are needed to evaluate options for populations who do not have a tradition of tai chi practice but do have strong cultural bonds to activities such as folk and ballroom dancing or eurhythmics. Additional trials are needed to investigate dance-based mind-motor activities, considering optimal duration and frequency for most effective fall prevention among healthy older adults.
eAppendix. Supplementary Material
References
- 1.Salomon JA, Wang H, Freeman MK, et al. Healthy life expectancy for 187 countries, 1990-2010: a systematic analysis for the Global Burden Disease Study 2010. Lancet. 2012;380(9859):2144-2162. doi: 10.1016/S0140-6736(12)61690-0 [DOI] [PubMed] [Google Scholar]
- 2.Inouye SK, Brown CJ, Tinetti ME. Medicare nonpayment, hospital falls, and unintended consequences. N Engl J Med. 2009;360(23):2390-2393. doi: 10.1056/NEJMp0900963 [DOI] [PubMed] [Google Scholar]
- 3.Schweizerische Eidgenossenschaft Gesundheit im Alter Gehvermögen und Stürze. Accessed September 22, 2019. https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/gesundheitszustand/alter.html
- 4.Peel NM. Epidemiology of falls in older age. Can J Aging. 2011;30(1):7-19. doi: 10.1017/S071498081000070X [DOI] [PubMed] [Google Scholar]
- 5.Morrison A, Fan T, Sen SS, Weisenfluh L. Epidemiology of falls and osteoporotic fractures: a systematic review. Clinicoecon Outcomes Res. 2013;5:9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults—United States. J Safety Res. 2016;58:99-103. doi: 10.1016/j.jsr.2016.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Caban-Martinez AJ, Courtney TK, Chang W-R, et al. Leisure-time physical activity, falls, and fall injuries in middle-aged adults. Am J Prev Med. 2015;49(6):888-901. doi: 10.1016/j.amepre.2015.05.022 [DOI] [PubMed] [Google Scholar]
- 8.de Souto Barreto P, Rolland Y, Vellas B, Maltais M. Association of long-term exercise training with risk of falls, fractures, hospitalizations, and mortality in older adults: a systematic review and meta-analysis. JAMA Intern Med. 2019;179(3):394-405. doi: 10.1001/jamainternmed.2018.5406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fernández-Argüelles EL, Rodríguez-Mansilla J, Antunez LE, Garrido-Ardila EM, Muñoz RP. Effects of dancing on the risk of falling related factors of healthy older adults: a systematic review. Arch Gerontol Geriatr. 2015;60(1):1-8. doi: 10.1016/j.archger.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 10.Hwang PW, Braun KL. The effectiveness of dance interventions to improve older adults’ health: a systematic literature review. Altern Ther Health Med. 2015;21(5):64-70. [PMC free article] [PubMed] [Google Scholar]
- 11.Keogh JWL, Kilding A, Pidgeon P, Ashley L, Gillis D. Physical benefits of dancing for healthy older adults: a review. J Aging Phys Act. 2009;17(4):479-500. doi: 10.1123/japa.17.4.479 [DOI] [PubMed] [Google Scholar]
- 12.Meng X, Li G, Jia Y, et al. Effects of dance intervention on global cognition, executive function and memory of older adults: a meta-analysis and systematic review. Aging Clin Exp Res. 2020;32(1):7-19. doi: 10.1007/s40520-019-01159-w [DOI] [PubMed] [Google Scholar]
- 13.Zhang Y, Li C, Zou L, Liu X, Song W. The effects of mind-body exercise on cognitive performance in elderly: a systematic review and meta-analysis. Int J Environ Res Public Health. 2018;15(12):E2791. doi: 10.3390/ijerph15122791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murrock CJ, Graor CH. Depression, social isolation, and the lived experience of dancing in disadvantaged adults. Arch Psychiatr Nurs. 2016;30(1):27-34. doi: 10.1016/j.apnu.2015.10.010 [DOI] [PubMed] [Google Scholar]
- 15.Lima MMS, Vieira AP. Ballroom dance as therapy for the elderly in Brazil. Am J Dance Ther. 2007;29(2):129-142. doi: 10.1007/s10465-007-9040-9 [DOI] [Google Scholar]
- 16.Koch S, Kunz T, Lykou S, Cruz R. Effects of dance movement therapy and dance on health-related psychological outcomes: a meta-analysis. Arts Psychother. 2014;41(1):46-64. doi: 10.1016/j.aip.2013.10.004 [DOI] [Google Scholar]
- 17.Kaltsatou AC, Kouidi EI, Anifanti MA, Douka SI, Deligiannis AP. Functional and psychosocial effects of either a traditional dancing or a formal exercising training program in patients with chronic heart failure: a comparative randomized controlled study. Clin Rehabil. 2014;28(2):128-138. doi: 10.1177/0269215513492988 [DOI] [PubMed] [Google Scholar]
- 18.Nadasen K. “Life without line dancing and the other activities would be too dreadful to imagine”: an increase in social activity for older women. J Women Aging. 2008;20(3-4):329-342. doi: 10.1080/08952840801985060 [DOI] [PubMed] [Google Scholar]
- 19.Ballesteros S, Kraft E, Santana S, Tziraki C. Maintaining older brain functionality: a targeted review. Neurosci Biobehav Rev. 2015;55:453-477. doi: 10.1016/j.neubiorev.2015.06.008 [DOI] [PubMed] [Google Scholar]
- 20.Rehfeld K, Lüders A, Hökelmann A, et al. Dance training is superior to repetitive physical exercise in inducing brain plasticity in the elderly. PLoS One. 2018;13(7):e0196636. doi: 10.1371/journal.pone.0196636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1-e34. doi: 10.1016/j.jclinepi.2009.06.006 [DOI] [PubMed] [Google Scholar]
- 22.Higgins JPT, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, eds. Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed John Wiley & Sons; 2019. doi: 10.1002/9781119536604 [DOI] [Google Scholar]
- 23.Veronese N, Maggi S, Schofield P, Stubbs B. Dance movement therapy and falls prevention. Maturitas. 2017;102:1-5. doi: 10.1016/j.maturitas.2017.05.004 [DOI] [PubMed] [Google Scholar]
- 24.Berg KO, Wood-Dauphinee SL, Williams JI, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(suppl 2):S7-S11. [PubMed] [Google Scholar]
- 25.Fong Yan A, Cobley S, Chan C, et al. The effectiveness of dance interventions on physical health outcomes compared to other forms of physical activity: a systematic review and meta-analysis. Sports Med. 2018;48(4):933-951. doi: 10.1007/s40279-017-0853-5 [DOI] [PubMed] [Google Scholar]
- 26.Jonsson E, Seiger A, Hirschfeld H. One-leg stance in healthy young and elderly adults: a measure of postural steadiness? Clin Biomech (Bristol, Avon). 2004;19(7):688-694. doi: 10.1016/j.clinbiomech.2004.04.002 [DOI] [PubMed] [Google Scholar]
- 27.Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. J Gerontol. 1990;45(6):M192-M197. doi: 10.1093/geronj/45.6.M192 [DOI] [PubMed] [Google Scholar]
- 28.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142-148. doi: 10.1111/j.1532-5415.1991.tb01616.x [DOI] [PubMed] [Google Scholar]
- 29.Bohannon RW. Reference values for the five-repetition sit-to-stand test: a descriptive meta-analysis of data from elders. Percept Mot Skills. 2006;103(1):215-222. doi: 10.2466/pms.103.1.215-222 [DOI] [PubMed] [Google Scholar]
- 30.Jones CJ, Rikli RE, Beam WCA. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport. 1999;70(2):113-119. doi: 10.1080/02701367.1999.10608028 [DOI] [PubMed] [Google Scholar]
- 31.Rantanen T, Guralnik JM, Foley D, et al. Midlife hand grip strength as a predictor of old age disability. JAMA. 1999;281(6):558-560. doi: 10.1001/jama.281.6.558 [DOI] [PubMed] [Google Scholar]
- 32.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Effect sizes based on means In: Introduction to Beta-analysis. John Wiley & Sons; 2011:21-32. [Google Scholar]
- 33.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Academic Press; 2013. doi: 10.4324/9780203771587 [DOI] [Google Scholar]
- 34.Harbord RM, Egger M, Sterne JA. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med. 2006;25(20):3443-3457. doi: 10.1002/sim.2380 [DOI] [PubMed] [Google Scholar]
- 35.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629-634. doi: 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stata Statistical Software : Release 15 [computer program]. StataCorp LLC; 2017.
- 37.Choi JH, Moon JS, Song R. Effects of sun-style tai chi exercise on physical fitness and fall prevention in fall-prone older adults. J Adv Nurs. 2005;51(2):150-157. doi: 10.1111/j.1365-2648.2005.03480.x [DOI] [PubMed] [Google Scholar]
- 38.Eyigor S, Karapolat H, Durmaz B, Ibisoglu U, Cakir S. A randomized controlled trial of Turkish folklore dance on the physical performance, balance, depression and quality of life in older women. Arch Gerontol Geriatr. 2009;48(1):84-88. doi: 10.1016/j.archger.2007.10.008 [DOI] [PubMed] [Google Scholar]
- 39.Huang HC, Liu CY, Huang YT, Kernohan WG. Community-based interventions to reduce falls among older adults in Taiwan: long time follow-up randomised controlled study. J Clin Nurs. 2010;19(7-8):959-968. doi: 10.1111/j.1365-2702.2009.02834.x [DOI] [PubMed] [Google Scholar]
- 40.Li F, Harmer P, Fisher KJ, et al. Tai Chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2005;60(2):187-194. doi: 10.1093/gerona/60.2.187 [DOI] [PubMed] [Google Scholar]
- 41.Trombetti A, Hars M, Herrmann FR, Kressig RW, Ferrari S, Rizzoli R. Effect of music-based multitask training on gait, balance, and fall risk in elderly people: a randomized controlled trial. Arch Intern Med. 2011;171(6):525-533. doi: 10.1001/archinternmed.2010.446 [DOI] [PubMed] [Google Scholar]
- 42.Voukelatos A, Cumming RG, Lord SR, Rissel C. A randomized, controlled trial of tai chi for the prevention of falls: the Central Sydney tai chi trial. J Am Geriatr Soc. 2007;55(8):1185-1191. doi: 10.1111/j.1532-5415.2007.01244.x [DOI] [PubMed] [Google Scholar]
- 43.Wolf SL, Sattin RW, Kutner M, O’Grady M, Greenspan AI, Gregor RJ. Intense tai chi exercise training and fall occurrences in older, transitionally frail adults: a randomized, controlled trial. J Am Geriatr Soc. 2003;51(12):1693-1701. doi: 10.1046/j.1532-5415.2003.51552.x [DOI] [PubMed] [Google Scholar]
- 44.Woo J, Hong A, Lau E, Lynn H. A randomised controlled trial of Tai Chi and resistance exercise on bone health, muscle strength and balance in community-living elderly people. Age Ageing. 2007;36(3):262-268. doi: 10.1093/ageing/afm005 [DOI] [PubMed] [Google Scholar]
- 45.Chyu M-C, James CR, Sawyer SF, et al. Effects of tai chi exercise on posturography, gait, physical function and quality of life in postmenopausal women with osteopaenia: a randomized clinical study. Clin Rehabil. 2010;24(12):1080-1090. doi: 10.1177/0269215510375902 [DOI] [PubMed] [Google Scholar]
- 46.Merom D, Mathieu E, Cerin E, et al. Social dancing and incidence of falls in older adults: a cluster randomised controlled trial. PLoS Med. 2016;13(8):e1002112. doi: 10.1371/journal.pmed.1002112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: an investigation of tai chi and computerized balance training. J Am Geriatr Soc. 1996;44(5):489-497. doi: 10.1111/j.1532-5415.1996.tb01432.x [DOI] [PubMed] [Google Scholar]
- 48.Alves H. Dancing and the Aging Brain: The Effects of a 4-Month Ballroom Dance Intervention on the Cognition of Healthy Older Adults, University of Illinois at Urbana-Champaign; 2013. [Google Scholar]
- 49.Bennett CG, Hackney ME. Effects of line dancing on physical function and perceived limitation in older adults with self-reported mobility limitations. Disabil Rehabil. 2018;40(11):1259-1265. doi: 10.1080/09638288.2017.1294207 [DOI] [PubMed] [Google Scholar]
- 50.Hopkins DR, Murrah B, Hoeger WW, Rhodes RC. Effect of low-impact aerobic dance on the functional fitness of elderly women. Gerontologist. 1990;30(2):189-192. doi: 10.1093/geront/30.2.189 [DOI] [PubMed] [Google Scholar]
- 51.Li JX, Xu DQ, Hong Y. Effects of 16-week Tai Chi intervention on postural stability and proprioception of knee and ankle in older people. Age Ageing. 2008;37(5):575-578. doi: 10.1093/ageing/afn109 [DOI] [PubMed] [Google Scholar]
- 52.Logghe IH, Zeeuwe PE, Verhagen AP, et al. Lack of effect of Tai Chi Chuan in preventing falls in elderly people living at home: a randomized clinical trial. J Am Geriatr Soc. 2009;57(1):70-75. doi: 10.1111/j.1532-5415.2008.02064.x [DOI] [PubMed] [Google Scholar]
- 53.Pereira M, Oliveira R, Silva M, Souza L, Vianna L.. Effects of Tai Chi Chuan on knee extensor muscle strength and balance in elderly women. Braz J Phys Ther. 2008;12(2):121-126. doi: 10.1590/S1413-35552008000200008 [DOI] [Google Scholar]
- 54.Serrano-Guzmán M, Aguilar-Ferrándiz ME, Valenza CM, Ocaña-Peinado FM, Valenza-Demet G, Villaverde-Gutiérrez C. Effectiveness of a flamenco and sevillanas program to enhance mobility, balance, physical activity, blood pressure, body mass, and quality of life in postmenopausal women living in the community in Spain: a randomized clinical trial. Menopause. 2016;23(9):965-973. doi: 10.1097/GME.0000000000000652 [DOI] [PubMed] [Google Scholar]
- 55.Sun J, Kanagawa K, Sasaki J, Ooki S, Xu H, Wang L. Tai chi improves cognitive and physical function in the elderly: a randomized controlled trial. J Phys Ther Sci. 2015;27(5):1467-1471. doi: 10.1589/jpts.27.1467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Taylor-Piliae RE, Newell KA, Cherin R, Lee MJ, King AC, Haskell WL. Effects of Tai Chi and Western exercise on physical and cognitive functioning in healthy community-dwelling older adults. J Aging Phys Act. 2010;18(3):261-279. doi: 10.1123/japa.18.3.261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cepeda CC, Lodovico A, Fowler N, Rodacki AL. Effect of an eight-week ballroom dancing program on muscle architecture in older adults females. J Aging Phys Act. 2015;23(4):607-612. doi: 10.1123/japa.2014-0101 [DOI] [PubMed] [Google Scholar]
- 58.Cruz-Ferreira A, Marmeleira J, Formigo A, Gomes D, Fernandes J. Creative dance improves physical fitness and life satisfaction in older women. Res Aging. 2015;37(8):837-855. doi: 10.1177/0164027514568103 [DOI] [PubMed] [Google Scholar]
- 59.Frye B, Scheinthal S, Kemarskaya T, Pruchno R. Tai chi and low impact exercise: effects on the physical functioning and psychological well-being of older people. J Appl Gerontol. 2007;26(5):433-453. doi: 10.1177/0733464807306915 [DOI] [Google Scholar]
- 60.Hui E, Chui BT, Woo J. Effects of dance on physical and psychological well-being in older persons. Arch Gerontol Geriatr. 2009;49(1):e45-e50. doi: 10.1016/j.archger.2008.08.006 [DOI] [PubMed] [Google Scholar]
- 61.Noradechanunt C, Worsley A, Groeller H. Thai yoga improves physical function and well-being in older adults: a randomised controlled trial. J Sci Med Sport. 2017;20(5):494-501. doi: 10.1016/j.jsams.2016.10.007 [DOI] [PubMed] [Google Scholar]
- 62.Taylor D, Hale L, Schluter P, et al. Effectiveness of tai chi as a community-based falls prevention intervention: a randomized controlled trial. J Am Geriatr Soc. 2012;60(5):841-848. doi: 10.1111/j.1532-5415.2012.03928.x [DOI] [PubMed] [Google Scholar]
- 63.Janyacharoen T, Laophosri M, Kanpittaya J, Auvichayapat P, Sawanyawisuth K. Physical performance in recently aged adults after 6 weeks traditional Thai dance: a randomized controlled trial. Clin Interv Aging. 2013;8:855-859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.McKinley P, Jacobson A, Leroux A, Bednarczyk V, Rossignol M, Fung J. Effect of a community-based Argentine tango dance program on functional balance and confidence in older adults. J Aging Phys Act. 2008;16(4):435-453. doi: 10.1123/japa.16.4.435 [DOI] [PubMed] [Google Scholar]
- 65.Merom D, Grunseit A, Eramudugolla R, Jefferis B, Mcneill J, Anstey KJ. Cognitive benefits of social dancing and walking in old age: the dancing mind randomized controlled trial. Front Aging Neurosci. 2016;8:26. doi: 10.3389/fnagi.2016.00026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Higgins JPT, Altman DG, Gøtzsche PC, et al. ; Cochrane Bias Methods Group; Cochrane Statistical Methods Group . The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sherrington C, Fairhall NJ, Wallbank GK, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;1:CD012424. doi: 10.1002/14651858.CD012424.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Huang ZG, Feng YH, Li YH, Lv CS. Systematic review and meta-analysis: Tai Chi for preventing falls in older adults. BMJ Open. 2017;7(2):e013661. doi: 10.1136/bmjopen-2016-013661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liu X, Shen PL, Tsai YS. Dance intervention effects on physical function in healthy older adults: a systematic review and meta-analysis. Aging Clin Exp Res. 2020. doi: 10.1007/s40520-019-01440-y [DOI] [PubMed] [Google Scholar]
- 70.Rodrigues-Krause J, Farinha JB, Krause M, Reischak-Oliveira Á. Effects of dance interventions on cardiovascular risk with ageing: systematic review and meta-analysis. Complement Ther Med. 2016;29:16-28. doi: 10.1016/j.ctim.2016.09.004 [DOI] [PubMed] [Google Scholar]
- 71.Sharp K, Hewitt J. Dance as an intervention for people with Parkinson’s disease: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2014;47:445-456. doi: 10.1016/j.neubiorev.2014.09.009 [DOI] [PubMed] [Google Scholar]
- 72.Wu C, Yi Q, Zheng X, et al. Effects of mind-body exercises on cognitive function in older adults: a meta-analysis. J Am Geriatr Soc. 2019;67(4):749-758. doi: 10.1111/jgs.15714 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Supplementary Material