Abstract
Background
This study sought to characterize cognitive outcomes among Latino survivors of childhood acute lymphoblastic leukemia (ALL) and lymphoblastic lymphoma (LL).
Procedure
In this cross-sectional cohort study, Latino survivors of ALL (n = 57) and LL (n = 5) aged 6–16 years were pooled and evaluated using validated measures of cognitive, academic, and behavioral function and English language proficiency. Performance was compared with norms using single-sample t-tests.
Results
In this cohort (n = 62, 50% male), mean ages at diagnosis and testing were 4.5 and 10.8 years, respectively; mean time off treatment was 44.7 months. All participants spoke English and over half (57%) identified Spanish as the primary language in the home. Forty-two families (68%) placed in the two lowest Hollingshead socioeconomic status categories. Participants were below average for working memory (P < 0.001). Overall, participants were in the average range, but significantly lower than published norms on domain-specific measures of verbal comprehension (P < 0.001); perceptual reasoning (P = 0.033); processing speed (P = 0.003); visual memory (P < 0.001); visuomotor attention, scanning, and sequencing (P = 0.005); and reading comprehension (P = 0.001). Parents reported concerns with working memory (P < 0.001) and metacognition (P = 0.014).
Conclusions
Similar to other childhood ALL/LL survivors, overall cognitive function in this Latino sample was relatively preserved but selected deficits were observed. Routine cognitive screening is indicated in this population.
Keywords: acute lymphoblastic leukemia, cancer, cognitive, late effects, Latino, sociodemographics
1 |. INTRODUCTION
Long-term survival for children with acute lymphoblastic leukemia (ALL) and lymphoblastic lymphoma (LL) treated using contemporary regimens now approaches 85–90%.1–3 Unfortunately, long-term survivors commonly develop clinically significant cognitive deficits resulting from treatment-related factors including intrathecal chemotherapy, systemic high-dose methotrexate, and cranial irradiation, as well as host-related factors, such as younger age at diagnosis and female sex.4–7 Two recent meta-analyses suggest that even in the context of modern regimens where routine use of cranial irradiation is sharply reduced, ALL survivors treated only with chemotherapy still show cognitive impairment, particularly in attention and executive functioning.8,9 Due to similarities in their biology, clinical behavior, effective treatment regimens, and long-term sequelae, distinction between ALL and LL is made on the basis of bone marrow involvement and is considered arbitrary.2 Consequently, survivors of ALL and LL are typically analyzed as a single group in research concerning neurocognitive outcomes.7
Clinically apparent cognitive dysfunction among long-term survivors of childhood ALL typically has a subtle, protracted onset and often manifests years after treatment.10 Deficits in working memory, attention, executive functioning, and processing speed are commonly detected.4,5,11–13 These deficits impede learning and have been associated with declines in general cognitive ability and academic achievement. Long-term consequences of such deficits are significant, including educational and economic disparities among young adult survivors.13–15
Survivors of childhood ALL from racial/ethnic minorities and those with lower socioeconomic status (SES) have reason to be at even higher risk. In typically developing children, strong relationships have been documented between SES, cognitive abilities, and academic achievement.16–18 This is particularly important in Latino samples, as research has consistently found lower performance by Latinos when assessed with the Wechsler Intelligence Scale for Children–Fourth Edition (WISC-IV) relative to standardization samples.19 This pattern may reflect the multiple areas of difficulties assessing Latinos and other minorities, such as test construction, standardization samples, and language, particularly effects of language proficiency on test performance.19 Domains most affected by SES disparities include language abilities (i.e., vocabulary, phonological awareness, syntax, and reading comprehension skills), executive functioning (i.e., planning, cognitive flexibility, working memory), attention, and memory.16–18 Although these risk factors are well established in the general population, there is limited information about how they might modify outcomes of childhood ALL survivors. For example, in two recent meta-analyses that summarized sociodemographic characteristics, only one-third of the studies reported the racial/ethnic composition of their samples, and nearly 80% of the participants identified as White/Caucasian; SES was unable to be included as an analytic variable due to insufficient data reporting.6,9 Using parent-reported measures, a single recent cohort study of Latino childhood ALL survivors identified difficulties with attention, school-based learning, and peer relationships.20
To help address these knowledge gaps, we conducted a multidimensional study of cognitive outcomes using a combination of performance-based, parent report, and teacher report measures in a sample of Latino childhood ALL and LL survivors treated with contemporary regimens. The primary aim was to characterize their cognitive performance relative to published norms. Given the combined risk of treatment-related sequelae and lower SES within this cohort, we hypothesized that this sample would perform lower than normative populations.
2 |. METHODS
2.1 |. Participants
This was a cross-sectional cohort study nested in our Institutional Review Board approved childhood cancer survivorship research database that is registered on ClinicalTrials.gov (NCT01518400). As described in detail elsewhere,21 we developed a parent-directed clinical service as part of the standard of care that offers culturally and linguistically competent cognitive assessment and parental training in school advocacy and support for children and adolescents undergoing their initial survivorship evaluation following treatment for ALL and LL. At our institution, the standard for posttreatment care includes referral to our specialized cancer survivorship clinic, making eligible participants representative of our institution’s survivorship population as a whole. Survivors of both ALL and LL are provided this service and were included in this analysis because of their similarities in treatment exposures, cognitive risk, and long-term neurocognitive outcomes.4,5 Authorization for analysis and reporting of clinical data was obtained by written informed consent/assent.
Participants consisted of Latino survivors of pediatric ALL or LL aged 6–16 years, due to age specifications of the assessment measures. Having been born and educated in the United States, all participants spoke English as their primary language, whereas caregivers primarily spoke either Spanish or English. Nonparticipants were those who attended survivorship clinic and consented to the survivorship database research, but chose not to complete the assessments. Patients were excluded from the analysis if they had a preexisting neurodevelopmental or psychological disorder likely to impact their performance on the study measures, including established intellectual disability and/or developmental delay, autism, or severe mental health concerns. Additional criteria for exclusion from the analysis were history of relapse or cranial irradiation, or being non-Latino.
2.2 |. Measures
2.2.1 |. Medical and sociodemographic information
Through a combination of medical chart abstraction and caregiver history, information was collected on treatment variables (cumulative doses of intrathecal methotrexate and cytarabine, high-dose systemic methotrexate, receipt of cranial irradiation), language predominantly spoken in the home, insurance type (public or private), household size, and zip code to estimate income.22 Hollingshead SES classifications were scored based on parental marital status, education, and employment, with categories ranging from I (high SES) to V (low SES).23
2.3 |. Testing battery
The battery was based on recommendations from the Children’s Oncology Group (COG) Long-term Follow-up Guidelines for Survivors of Childhood, Adolescent and Young Adult Cancer,24 and the standardized testing battery specified in the COG study ALTE07C1 (NCT00772200),25 which evaluates critical functional domains empirically shown to be most affected by pediatric cancer and its treatment. Relative to ALTE07C1, our study battery was expanded to address the demographic profile of our patient population by adding more comprehensive evaluations across domains, standardized parental measures in Spanish, and a standardized measure of English language proficiency. Teacher measures were also included to provide a more complete understanding of functioning in school. Children in this sample were English dominant and tend to be categorized in school as English Language Learners.26 Therefore, all tests were administered using the English version following standardized procedures by a fully bilingual English/Spanish pediatric psychologist (native speaker Spanish). Published measures in Spanish (Behavior Assessment System for Children, Second Edition [BASC-2], Behavior Rating Inventory of Executive Function [BRIEF]) were utilized for parents when needed per their language preference. Table 1 summarizes a comparison of both batteries. Normative data for each measure were collected by the test developers, generally from large samples of typically developing and healthy children reflecting demographics of the United States census. Following are the measures included in our battery; reliability is expressed as Cronbach alpha values unless otherwise indicated.
TABLE 1.
Cognitive and behavioral battery (ages 6:0–16:11)
| Domain/test | ALTE07C1a | This study |
|---|---|---|
| Children | ||
| Intelligence | ||
| WISC-IV | Vocabulary, Block Design | Vocabulary, similarities, block design, matrix reasoning |
| English language proficiency | ||
| WMLS-R | Included | |
| Processing speed/attention | ||
| WISC-IV | Coding, Symbol Search | Coding, symbol search |
| CPT-3 | Included | |
| Memory | ||
| CMS | Story Memory, Faces, Dot Location | |
| NEPSY-II | Memory for designs, memory for design delayed | |
| CVLT-C | Included | Included |
| WISC-IV | Digit Span | Digit span, letter-number sequence |
| Executive functioning | ||
| D-KEFS | Trails, color-word interference | |
| Academic achievement | ||
| WIAT-III | Reading comprehension, numerical operations | |
| Parents | ||
| COG Language Preference Questionnaire | Sociodemographic survey | |
| Attention and behavioral/social/emotional function | ||
| BASC-2 | Included | Included |
| Executive function | ||
| BRIEF | Included | Included |
| Adaptive function | ||
| ABAS-II | Included | |
| Quality of life | ||
| PedsQL4.0 | Included | |
| Teachers | ||
| Attention and behavioral/social/emotional function | ||
| BASC-2 | Included | |
| Executive function | ||
| BRIEF | Included | |
ALTE07C1 test battery.24
2.3.1 |. Cognitive functioning
The WISC-IV is a test of intellectual function in individuals 6–16 years of age.27 The Verbal Comprehension, Perceptual Reasoning, Working Memory, and Processing Speed Indices were derived from prorated scores based on eight subtests. Reliability is 0.79–0.97; construct validity is well established.
2.3.2 |. Academic functioning
The Reading Comprehension and Numerical Operations subtests from the Wechsler Individual Achievement Test–Third Edition (WIAT-III) are used for children ages 4 and older.28 Reliability for these subtests is >0.80.
2.3.3 |. Language proficiency
The Woodcock-Muñoz Language Survey–Revised (WMLS-R) was administered to English language learners and provides norm-referenced measures of reading, writing, listening, comprehension, and cognitive-academic language proficiency (CALP) from Level 1 (negligible) to Level 6 (very advanced).29 Reliability is 0.76–0.91.
2.3.4 |. Attention
The Conner’s Continuous Performance Test (CPT-3) is a computerized test for individuals ages 8 and older and measures sustained visual attention, response inhibition, and task vigilance.30 Split-half and test–retest reliability are 0.92 and 0.67, respectively.
2.3.5 |. Executive functioning
The Delis–Kaplan Executive Function System (D-KEFS) assesses higher order cognitive problem solving and executive functioning in individuals ages 8–89 years.31 In our study, the two subtests of cognitive flexibility given were (1) Trail Making Test, which measures visuomotor attention, scanning, and sequencing, and (2) Color-Word Interference Test, which measures rapid naming and inhibition of overlearned responses. Internal consistency and test–retest reliability for these subtests are 0.70–0.79.32
2.3.6 |. Verbal learning and memory
The California Verbal Learning Test–Children’s Version (CVLT-C) is a verbal list learning task involving memorization of a list of words over multiple learning trials, delayed recall, and recognition recall for ages 5:0–16:11.33 Test–retest reliability of this measure is 0.80–0.84.
2.3.7 |. Nonverbal memory
The Memory for Designs and Memory for Designs Delayed from the NEPSY-II is normed for children ages 5–16 and is designed to assess spatial memory for novel and abstract visual information.34 Internal consistencies are 0.44–0.92 depending on the age.
2.3.8 |. Parent and teacher measures
The BRIEF is designed to assess executive functioning in school-aged children within the home and school environments.35 The BRIEF provides standardized observational reports of behavioral and emotional regulation, working memory, organization and planning, and attention in everyday life. Internal consistency is between 0.80–0.98; test–retest reliability is between 0.76 and 0.85. The BASC-2 provides a multidimensional measure of psychosocial and behavioral functioning.36 The Attention Problems scale measures problems a child or adolescent might have with different levels of attention. The scales and composites have high internal consistency of approximately 0.80–0.90, and test–retest reliability of approximately 0.70–0.80.
2.4 |. Statistical analysis
Comparability of study participants and nonparticipants was assessed using analysis of variance tests. To evaluate cognitive outcomes as compared to normative means, one-sample t-tests were used and score distributions were calculated. Survivors of ALL and LL were pooled for all analyses. Analyses were completed using SPSS Version 17.0 (Chicago, IL).
3 |. RESULTS
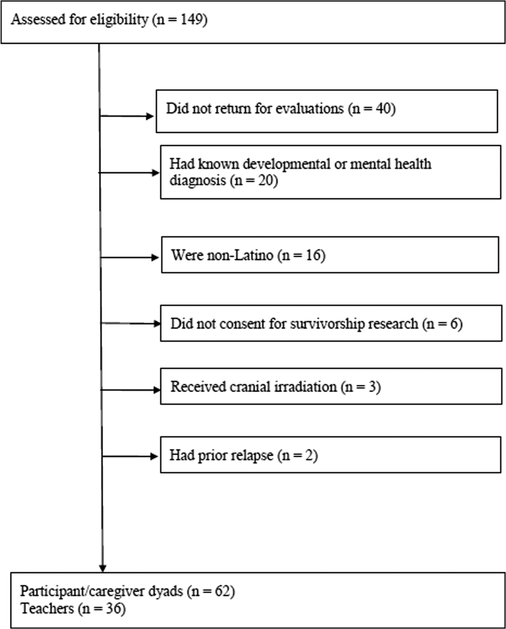
There were 149 patients screened for eligibility between January 2013 and December 2015. As shown in Figure 1, the analytical sample comprised 62 Latino children and their caregivers, as well as 36 teachers, after excluding from the analysis those who consented but did not schedule or otherwise return for assessments (n = 40), had one of several conditions known to increase cognitive risk above that of typical survivors in first remission (n = 20), were non-Latino (n = 16), did not provide consent (n = 6), had cranial irradiation (n = 3), or had relapsed (n = 2). See Table 2 for demographic and clinical characteristics. Participants had a mean age (±SD) of 10.8 ± 2.9 years at the time of assessment, 50.0% were male, and 56.5% of families identified that primarily Spanish was spoken in the home. Seventy-one percent of parents/caregivers reported Mexico as their specific Latino background, followed by Guatemala (11%), El Salvador (10%), and Colombia (3%), with 5% who did not specify country of origin. The majority of the sample (67.7%) were placed in the two lowest Hollingshead SES categories; 85.5% had public insurance. The mean posttreatment interval was 44.7 ± 30.4 months.
FIGURE 1.
Study profile
TABLE 2.
Participant characteristics (n = 62)
| N (%) | M± SD | |
|---|---|---|
| Demographic characteristics | ||
| Age at time of testing (years) | 10.8 ± 2.9 | |
| Sex | ||
| Male | 31 (50) | |
| Female | 31 (50) | |
| Race/ethnicity | ||
| Latino | 62 (100) | |
| Treatment characteristics | ||
| Acute lymphoblastic leukemia | 57(91.9) | |
| Lymphoblastic non-Hodgkin lymphoma | 5(8.1) | |
| Age at diagnosis (years) | 4.5 ± 2.7 | |
| Time posttreatment (months) | 44.7 ± 30.4 | |
| Cumulative dose of intrathecal methotrexate (mg) | 231.5 ± 48.2 | |
| Cumulative dose of intrathecal cytarabine (mg) | 65.0 ± 26.43 | |
| Received high-dose IV methotrexate (>1 g) | 9 (14.5) | |
| Social characteristics | ||
| Primary home language | ||
| English | 27 (43.5) | |
| Spanish | 35 (56.5) | |
| Hollingshead SES category | ||
| Category I | 1(1.6) | |
| Category II | 14 (22.6) | |
| Category III | 5(8.1) | |
| Category IV | 14 (22.6) | |
| Category V | 28 (45.2) | |
| Household size | 5.3 ± 1.5 | |
| Estimated household income (US dollars) | $46,519 ± $14,653 | |
| Insurance type | ||
| Public | 53 (85.5) | |
| Private | 9 (14.5) | |
The study sample did not differ significantly from all (n = 40) or the Latino subgroup (n = 20) of nonparticipants for clinical treatment or sociodemographic characteristics of interest. Potential differences in SES could not be assessed because only participants could provide data required for Hollingshead classification; however, there were no differences in estimated income or type of insurance. There were no demographic differences between those participants whose teachers did complete study measures (n = 36) and those that did not.
Test results for the cohort compared to normative data are shown in Table 3. Overall, participants performed similarly to published norms on most measures. However, the WISC-IV Working Memory Index (t=−9.58, P<0.001) was significantly lower in the below average range and was the only variable found to have a large effect size (Cohen’s d = 1.22). Significant differences were noted on additional measures, though remained within the average range and had small to moderate effect sizes. Specifically, participant mean scores were significantly lower on the WISC-IV Indices of Verbal Comprehension (t = −6.49, P < 0.001), Perceptual Reasoning (t = −2.19, P = 0.033), and Processing Speed (t = −3.34, P = 0.001). The WIAT-III Reading Comprehension (t = −3.49, P = 0.001) and immediate visual recall on the NEPSY-II Memory for Designs (t = −4.23, P < 0.001) were also lower than the mean group. Cohort means were similarly lower for visuomotor attention, scanning, and sequencing on the D-KEFS Trails Letter-Number Switching (t = −3.14, P = 0.003).
TABLE 3.
Participant outcomes in comparison to normative means
| Measure | Mean ± SD | Range | ≤16th percentile | 17–84th percentile | ≥85th percentile | tb | P | Effect sizeb |
|---|---|---|---|---|---|---|---|---|
| n (%) | ||||||||
| Wechsler Intelligence Scale for Children-Fourth Edition (WISC-IV)c n = 62 | ||||||||
| Verbal Comprehension Index | 90.60 ± 11.41 | 65–124 | 20 (32.3) | 40 (64.5) | 2 (3.2) | −6.49* | <0.001 | 0.82 |
| Perceptual Reasoning Index | 96.35 ± 13.12 | 69–123 | 13(21.0) | 44 (70.9) | 5 (8.1) | −2.19* | 0.033 | 0.28 |
| Working Memory Index | 87.53 ± 10.25 | 68–116 | 23(37.1) | 38 (61.3) | 1 (1.6) | −9.58* | <0.001 | 1.22 |
| Processing Speed Index | 94.55 ± 12.73 | 62–126 | 18 (29.0) | 41 (66.1) | 3 (4.8) | −3.34* | 0.001 | 0.43 |
| Wechsler Individual Achievement Test-Third Edition (WIAT-III)c n = 59 | ||||||||
| Reading Comprehension | 95.02 ± 10.78 | 69–118 | 10(17.5) | 45 (78.9) | 2 (3.5) | −3.49* | 0.001 | 0.46 |
| Numerical Operations | 98.54 ± 13.49 | 67–129 | 10(16.9) | 43 (72.9) | 6(10.2) | −0.08 | 0.410 | 0.11 |
| Woodcock-Munoz Language Survey-Revised (WMLS-R)d n = 57 | ||||||||
| Broad English CALP | 3.64 ± 0.65 | 2–5 | 3(5.2) | 47 (82.5) | 7 (12.3) | 1.61 | 0.113 | 0.21 |
| Conner's Continuous Performance Test (CPT-3)e n = 27 | ||||||||
| Omissions | 51.85 ± 9.58 | 42–79 | 0 | 21 (77.8) | 6(22.2) | 1.01 | 0.324 | 0.19 |
| Commissions | 46.78 ± 6.70 | 35–57 | 7(25.9) | 20 (74.1) | 0 | −2.50* | 0.019 | 0.48 |
| Hit Reaction Time | 51.89 ± 9.17 | 37–79 | 3 (11.1) | 19 (70.4) | 5 (18.5) | 1.07 | 0.294 | 0.21 |
| Variability | 50.85 ± 12.28 | 38–87 | 3(11.1) | 20 (74.1) | 4(14.8) | 0.36 | 0.722 | 0.07 |
| Preservations | 49.30 ± 6.50 | 44–70 | 0 | 25 (92.6) | 2 (7.4) | −0.56 | 0.578 | 0.11 |
| Hit Reaction Time Block Change | 54.63 ± 12.85 | 20–87 | 1 (3.7) | 18 (66.7) | 8 (29.6) | 1.87 | 0.072 | 0.36 |
| Delis-Kaplan Executive Function System (D-KEFS)f n = 50–52 | ||||||||
| Color Word Inhibition | 10.08 ± 2.20 | 5–15 | 6(11.5) | 40 (77.0) | 6(11.5) | 0.25 | 0.802 | 0.03 |
| Color Word Inhibition-Switching | 9.90 ± 2.63 | 1–13 | 8 (15.7) | 34 (66.7) | 9 (17.6) | −0.27 | 0.791 | 0.04 |
| Trails Letter-Number Switching | 8.54 ± 3.29 | 1–13 | 15 (30.0) | 31 (62.0) | 4 (8.0) | −3.14* | 0.003 | 0.44 |
| The California Verbal Learning Test-Children's Version (CVLT-C)g n = 58 | ||||||||
| Trial 1 | 0.04 ± 1.05 | −2.0 to 3.0 | 11 (19.0) | 32 (55.2) | 15 (25.8) | 0.31 | 0.755 | 0.04 |
| Trial 5 | −0.26 ± 1.09 | −3.5 to 2.0 | 20 (34.5) | 26 (44.8) | 12 (20.7) | −1.81 | 0.076 | 0.24 |
| Short Delay Free Recall | 0.02 ± 0.84 | −2.0 to 2.0 | 8(13.8) | 38 (65.5) | 12 (20.7) | 0.16 | 0.876 | 0.02 |
| Short Delay Cued Recall | 0 ± 0.82 | −2.0 to 1.5 | 9(15.5) | 35 (60.3) | 14(24.1) | 0 | 1.000 | 0 |
| Long Delay Free Recall | 0.21 ± 0.80 | −2.5 to 1.5 | 5 (8.6) | 38 (65.5) | 15 (25.8) | 1.97 | 0.054 | 0.26 |
| Long Delay Cued Recall | 0.09 ± 0.80 | −2.0 to 2.0 | 6(10.3) | 39 (67.2) | 13(22.4) | 0.90 | 0.372 | 0.12 |
| Discriminability | 0.03 ± 0.77 | −3.0 to 1.5 | 7(12.1) | 45 (77.6) | 6(10.3) | 0.26 | 0.799 | 0.03 |
| NEPSY-Second Edition (NEPSY-II)f n = 57–59 | ||||||||
| Memory for Designs | 8.44 ± 2.78 | 3–15 | 22 (38.6) | 31 (54.4) | 4(7.0) | −4.23* | 0.56 | |
| Memory for Designs Delayed | 9.44 ± 3.00 | 3–18 | 14 (24.6) | 34 (59.6) | 9 (15.8) | −1.42 | 0.162 | 0.19 |
| Behavior Rating Inventory of Executive Function (BRIEF) Parent Reporte n = 61–62 | ||||||||
| Behavioral Regulation Index | 48.81 ± 9.15 | 36–80 | 10(16.1) | 43 (69.4) | 9 (14.5) | −1.03 | 0.308 | 0.13 |
| Working Memory Scale | 56.55 ± 11.86 | 38–85 | 4(6.5) | 36(58.1) | 22 (35.5) | 4.35* | <0.001 | 0.55 |
| Metacognition Index | 53.51 ± 10.85 | 35–85 | 7 (11.5) | 38 (62.3) | 16(26.2) | 2.53* | 0.014 | 0.32 |
| Behavior Rating Inventory of Executive Function (BRIEF) Teacher Reporte n = 35 | ||||||||
| Behavioral Regulation Index | 47.74 ± 8.04 | 41–83 | 3 (8.6) | 21 (60.0) | 11 (31.4) | −1.66 | 0.106 | 0.28 |
| Working Memory Scale | 54.86 ± 14.22 | 38–96 | 2 (5.7) | 24 (68.6) | 9(25.7) | 2.02 | 0.051 | 0.34 |
| Metacognition Index | 53.26 ± 11.76 | 37–80 | 2 (5.7) | 24 (68.6) | 9 (25.7) | 1.64 | 0.110 | 0.28 |
| Behavior Assessment System for Children, Second Edition (BASC-2) Parent Reporte n = 61 | ||||||||
| Attention Problems | 51.08 ± 10.23 | 35–75 | 12 (19.7) | 33(54.1) | 16(26.2) | 0.83 | 0.412 | 0.11 |
| Behavior Assessment System for Children, Second Edition (BASC-2) Teacher Reporte n = 36 | ||||||||
| Attention Problems | 48.06 ± 9.46 | 37–69 | 11 (30.6) | 19(52.8) | 6 (16.7) | −1.23 | 0.226 | 0.21 |
One-sample t-test comparing survivors to normative means.
Cohen’s d.
Mean = 100, SD = 15.
Mean = 3.5, SD = 0.5.
Mean = 50, SD = 10.
Mean = 10, SD = 3.
Mean = 0, SD = 1.
P < 0.05.
Participants had more difficulties per parent report on the BRIEF Working Memory (t = 4.35, P < 0.001) and Metacognition Indices (t = 2.53, P = 0.014) when compared to normative data. Teacher report of more concerns on the BRIEF Working Memory approached significance (t=2.02, P=0.051). There were no differences in parental report on the BRIEF or BASC-2 for those children whose teachers did (n = 36) and did not complete a report.
Areas of relative strength in the average range were also identified, as participants had a relatively lower number of commission errors (impulsive responding to nontarget stimuli) while sustaining basic visual attention on the CPT-3 (t = −2.50, P = 0.019). They approached significance for a relatively higher free long delay recall (t = 1.97, P = 0.054) on the list learning tasks on the CVLT-C.
In addition to mean differences, Table 3 shows the distribution of the sample’s scores. As the measures’ normed scores are interpreted based on the normal curve, which places 68% of a distribution within one standard deviation above and below the mean, it is notable that a substantial proportion was in the below-average range of the 16th percentile on several measures. For example, while the WISC-IV Verbal Comprehension Index mean was in the average range, 32.3% of participants were below average, which is double the expected 16%. This pattern was seen in both those scores with significantly lower means in the average range and for several results that were not significantly lower, such as 34.5% below average for the CVLT-C Trial 5. The scores on the WMLS-R CALP29 in this sample of “very limited” (5.3%) and “limited” (19.3%) proficiency correspond with California schools’ general population, where a quarter of students are classified as English Language Learners.37
4 |. DISCUSSION
The aims of this study were to describe, using performance-based measures and parent/teacher reports, the cognitive profile of a Latino sample of childhood ALL and LL survivors and compare their outcomes to published norms. Our findings indicate that, although overall function was in the average range, multiple relative weaknesses in verbal comprehension, perceptual reasoning, working memory, processing speed, reading comprehension, nonverbal memory, and cognitive flexibility were present. While our results are broadly consistent with previously published studies of primarily on white/non-Hispanic subjects,5,10–12 our results represent an important contribution by including comprehensive evaluation of a Latino population, which has historically been underrepresented in this area of research.
Our study confirms research utilizing mostly white/European-American samples of ALL survivors exhibiting overall average cognitive functioning, with specific areas of mild deficits in the lower average range.5,10–12 These patterns were seen even though our sample at testing was relatively young (mean age 10.9 years) and early posttreatment (mean interval 43 months). Consistent with previous studies, our sample had significant differences in some measures of memory. The WISC-IV Working Memory Index, which has a strong component of auditory attention, was below average and parents reported clinical concerns in this area, as well. Visually based reasoning, executive functioning, and memory measures were also significantly lower, suggesting both auditory and visual abilities were impacted in this sample.
Although overall functioning was within the average range, a diverse group of cognitive functions were lower than norms, supporting the broad mild weaknesses of late effects for this group. Our results yield two practical implications for clinical practice and research. First, systematic cognitive evaluation of childhood ALL and LL survivors is indicated for detection of mild, but clinically important weaknesses that may not be readily apparent in the classroom and at home.38–40 This report adds important information about the growing population of Latino survivors of childhood ALL and LL, as, to our knowledge, only one other published study has focused on this group.20 Second, clinical care and research should routinely include race/ethnicity and sociodemographic variables, such as income, household size, parental education, and employment.20,38,41 It is important that SES not be conflated with ethnicity and race. As highlighted by Patel and colleagues, it is inappropriate to attribute poor outcomes due to ethnicity alone, as lower SES has a negative impact across ethnic groups.20 For example, a study of predominantly white survivors of childhood ALL found that household income below $80,000 per year was associated with poor physical, social, and emotional functioning.42 Additionally, English language development needs to be accounted for as language plays a central part in cognitive and academic evaluations.19,43,44 Studies able to adjust for these covariates may be able to delineate their effects from those of treatment but require larger samples to gain precision.
Our findings support providing expert, culturally competent cognitive evaluation for childhood ALL and LL survivors because cognitive deficits and academic difficulties may be subtle.38–40 As overall scores of our sample were within the average range, these weaknesses alone may not trigger intervention by conventional criteria. However, lower performance on a combination of functions likely negatively impacts academic achievement and may contribute to delayed identification and intervention. As many survivors do not have obvious behavioral and emotional difficulties, their struggles might be undetected or attributed to lack of effort. Parent and teacher reporting measures are frequently used to screen for cognitive and academic difficulties. Although there are concerns about the reliability and sensitivity of these reports, they are readily completed and inexpensive. The availability of teacher reports was modest (36/62, 58%) with common reasons for nonavailability being parent forgetting to ask, teachers not mailing it back, and children being tested during vacation. Nonetheless, we found that parent and teacher reports were mostly congruent with direct measurements of their children’s function. By parent report, small but statistically significant differences were identified in working memory and executive functioning. These suggest that subtle deficits can impact daily life for survivors, which may be particularly relevant in a population where higher stress levels,45 low education levels, and low English fluency hinder parents’ ability to assist with school work. Thus, a truly comprehensive approach for providing academic support to these survivors in the home, community, and school must take account of sociodemographic disparities.41
An important strength of this study was the use of detailed, direct cognitive performance measures in addition to parent and teacher reports, despite limitations of a low rate of teacher return. Utilizing multiple information sources provides a more complete perspective, but is seldom included in the literature concerning childhood ALL/LL survivors. Limitations of this study include the lack of matched controls to delineate more precisely the relative contributions of treatment and sociodemographic risk factors. On the other hand, our use of normative comparisons reflects common clinical and research practice. Another limitation is that while our participants are representative of the Latino population we serve, our sample was fairly homogeneous with respect to SES. Compounding this is the possibility of selection bias. As this study was nested within our clinical survivorship service, it was sometimes challenging to engage families where cognitive assessment was perceived as threatening, unnecessary, or addressable through existing academic supports. Given size and characteristics of our sample, we were not able to complete additional analyses to identify potential risk and protective factors in cognitive outcomes. Finally, another limitation is our cross-sectional study design, which cannot assess change over time.
Thus, opportunities for future research include the inclusion of comparison groups, larger samples, a wider representation of sociodemographic diversity, measures of acculturation for parents and survivors,46 and longitudinal designs that can evaluate long-term functioning and the impact of interventions. Although bilingualism is postulated to be a protective cognitive factor,47 underdeveloped English language skills as commonly found in many Latino children and households can have negative implications for academic achievement.48,49 Consequently, a better understanding of how language-related variables impact childhood ALL/LL survivors is also needed.
Acknowledgments
Funding information
Grant sponsor: The Larry & Helen Hoag Foundation.
Abbreviations
- ALL
acute lymphoblastic leukemia
- CALP
cognitive-academic language proficiency
- COG
Children’s Oncology Group
- LL
lymphoblastic lymphoma
- SES
socioeconomic status
Footnotes
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
REFERENCES
- 1.Howlader N, Noone AM, Krapcho M, et al. , eds, SEER Cancer Statistics Review, 1975–2013. Bethesda, MD: National Cancer Institute; 2016. http://seer.cancer.gov/crs/1975_2013/. [Google Scholar]
- 2.Schmidt E, Burkhardt B. Lymphoblastic lymphoma in childhood and adolescence, Pediatr Hematol Oncol. 2013;30(6):484–508. [DOI] [PubMed] [Google Scholar]
- 3.Cairo MS, Pinkerton R. Childhood. adolescent and young adult non-Hodgkin lymphoma: state of the science. Br J Haematol. 2016;173:507–530. [DOI] [PubMed] [Google Scholar]
- 4.Moleski M. Neuropsychological, neuroanatomical, and neurophysiological consequences of CNS chemotherapy for acute lymphoblastic leukemia. Arch Clin Neuropsychol. 2000;15(7):603–630. [PubMed] [Google Scholar]
- 5.Cheung YT, Krull KR. Neurocognitive outcomes in long-term survivors of childhood acute lymphoblastic leukemia treated on contemporary treatment protocols: a systematic review. Neurosci Biobehav Rev. 2015;53:108–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Campbell LK, Scaduto M, Sharp W, et al. A meta-analysis of the neurocognitive sequelae of treatment for childhood acute lymphocytic leukemia. Pediatr Blood Cancer. 2007;49(1):65–73. [DOI] [PubMed] [Google Scholar]
- 7.von der Weid NX. Adult life after surviving lymphoma in childhood. Support Care Cancer. 2008;16(4):339–345. [DOI] [PubMed] [Google Scholar]
- 8.Iyer NS, Balsamom LM, Bracken MB, Kadan-Lottick NS. Chemotherapy-only treatment effects on longt-term neurocognitive funcitoning in childhood ALL survivors: a review and meta-analysis. Blood. 2015;126(3):346–353. [DOI] [PubMed] [Google Scholar]
- 9.Pierson C, Waite E, Pykkonen B. A meta-analysis of the neuropsychological effects of chemotherapy in the treatment of childhood cancer. Pediatr Blood Cancer. 2016;63(11):1998–2003. [DOI] [PubMed] [Google Scholar]
- 10.Dodzik PA, Fulton R. Neuropsychological outcomes in children with acute lymphoblastic leukemia In: Mucci GA, Torno L, eds. Handbook of Long Term Care of Childhood Cancer Survivor New York: Springer Science + Business Media; 2015: 223–247. [Google Scholar]
- 11.Conklin HM, Krull KR, Reddick WE, Pei D, Cheng C, Pui CH. Cognitive outcomes following contemporary treatment without cranial irradiation for childhood acute lymphoblastic leukemia. J Natl Cancer Inst. 2012;104(18): 1386–1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacola LM, Krull KR, Pui CH, et al. Longitudinal assesment of neurocognitive outcomes in survivors of childhood acute lymphoblastic leukemia treated on a contemporary protocol. J Clin Oncol. 2016;34(11):1239–1247. 10.1200/JCO.2015.64.3205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kanellopoulos A, Andersson S, Zeller B, et al. Neurocognitive outcome in very long-term survivors of childood acute lymphoblastic leukemia after treatment with chemotherapy only. Pediatr Blood Cancer. 2016;63(1):133–138. [DOI] [PubMed] [Google Scholar]
- 14.Jacola LM, Edelstein K, Liu W, et al. Cognitive, behaviour, and academic functioning in adolescent and young adult survivors of childhood acute lymphoblastic leukaemia: a report from the Childhood Cancer Survivor Study. Lancet Psychiatr. 2016;3(10):965–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krull KR, Brinkman TM, Li C, et al. Neurocognitive outcomes decades after treatment for childhood acute lymphoblastic lekemia: a report from the St. Jude Lifetime Cohort Study. J Clin Oncol. 2013;31(35):4407–4415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hackman DA, Farah MJ. Socioeconomic status and the developing brain. Trends Cogn Sci. 2009;13(2):65–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hackman DA, Farah MJ, Meaney MJ. Socioeconomic status and the brain: mechanistic insights from human and animal research. Nature Rev Neurosci. 2010;11(9):651–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lawson GM, Farah MJ. Executive function as a mediator between SES and academic achievement throughout childhood. Int J Beha Dev. 2017;41(1):94–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.von Thomsen C, Gallupm L, Llorente AM. Intellectual abilities: theoretical and applied assessment considerations In: Llorente A, ed. Principlesof Neuropsychological Assessment with Hispanics. Verlag, NY: Springer; 2008:57–77. [Google Scholar]
- 20.Patel SK, Lo TT, Dennis JM, Bhatia S. Neurocognitive and behavioral outcomes in Latino childhood cancer survivors. Pediatr Blood Cancer. 2013;60(10):1696–1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bava L, Malvar J, Sposto R, et al. A parent-directed intervention for addressing academic risk in Latino survivors of childhood leukemia: results of a pilot study. Psychooncology. 2016;25:1246–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.United States Census Bureau. American FactFinder, Community Facts. 2017. http://factfinder.census.gov/faces/nav/jsf/pages/community_facts.xhtml.
- 23.Cirino PT, Chin CE, Sevcick RA, Wolf M, Morris RD. Measuring socioeconomic status: reliability and preliminary validity for different approaches. Assessment. 2002;9(2):145–155. [DOI] [PubMed] [Google Scholar]
- 24.Children’s Oncology Group. Long-term follow-up guidelines for survivors of childhood, adolescent, and young adult cancers. 2017. http://www.survivorshipguidelines.org/.
- 25.Children’s Oncology Group Study ALTE07C1: Neuropsychological and behavioral testing in younger patients with cancer. (Embry L, Principal Investigator). 2017. https://clinicaltrials.gov/ct2/show/NCT00772200?term=alte07c1&rank=1.
- 26.Bardack S American Institutes for Research. English Language Learner Center. Common ELL terms and definitions. 2010. http://www.air.org/sites/default/files/downloads/report/NEW_-_Common_ELL_TERMS_AND_DEFINITIONS_6_22_10_0.pdf.
- 27.Wechsler D, Kaplan E, Fein D, et al. The Wechsler Intelligence Scale for Children (WISC-IV). 4th ed. San Antonio, TX: Pearson; 2003. [Google Scholar]
- 28.Wechsler D Wechsler Individual Achievement Test (WIAT-III). San Antonio, TX: Pearson; 2009. [Google Scholar]
- 29.Woodcock RW, Munoz-Sandoval AF, Ruef ML, Alvarado CG. Woodcock-Munoz Language Survery—Revised (WMLS-R). St. Charles, IL: Houghton Miffin Harcourt; 2005. [Google Scholar]
- 30.Conners CK. Conners Continuous Performance Test 3rd Edition (Conners CPT3 ۛ). North Tonawanda, NY:Multi-Health Systems Inc.; 2014. [Google Scholar]
- 31.Delis DC, Kaplan E, Kramer JH. Delis-Kaplan Executive Functioning System (D-KEFS). San Antonio, TX: Pearson; 2001. [Google Scholar]
- 32.Strauss E, Sherman EMS, Spreen. A Compendium of Neuropsychological Tests: Administration, Norms, and Commentary. Oxford, UK: Oxford University Press; 2006. [Google Scholar]
- 33.Delis D, Kramer JH., Kaplan E, Ober BA. The California Verbal Learning Test–Child (CVLT-C). San Antonio, TX: Pearson; 1994. [Google Scholar]
- 34.Korkman M, Kirk U, Kemp S. NEPSY-II Second Edition San Antonio, TX: Pearson; 2007. [Google Scholar]
- 35.Gioia G, Isquith PK., Guy SC, Kenworthy L. Behavior Rating Inventory of Executive Function (BRIEF). Lutz, FL: PAR, Inc.; 2013. [Google Scholar]
- 36.Reynolds CR, Kamphaus RW. Behavior Assessment System for Children–Second Edition (BASC-2). San Antonio, TX: Pearson; 2004. [Google Scholar]
- 37.Hill LE. California’s English Learner Students. Public Policy Institute of California; 2012. http://www.ppic.org/publication/californiasenglish-learner-students/. Accessed September 26, 2017.
- 38.Nathan PC, Patel SK, Dilley K, et al. Guidelines for identification of, advocacy for, and intervention in neurocognitive problems in survivors of childhood cancer: a report from the Children’s Oncology Group. Arch Pediatr Adolesc Med. 2007;161(8):798–806. [DOI] [PubMed] [Google Scholar]
- 39.Walsh KS, Noll RB, Annett RD, et al. Standard of care for neuropsychological monitoring in pediatric neuro-oncology: lessons from the Children’s Oncology Group. Pediatr Blood Cancer. 2016;63(2):191–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Annett RD, Patel SK, Phipps S. Monitoring and assessment of neuropsychological outcomes as a standard of care in pediatric oncology. Pediatr Blood Cancer. 2015;62(Suppl 5):S460–S513. [DOI] [PubMed] [Google Scholar]
- 41.Bava L, Johns A, Freyer DR, Ruccione K. Development of a culturally competent service to improve academic functioning for Latino survivors of acute lymphoblastic leukemia: methodological considerations. J Pediatr Oncol Nurs. 2016;pii, 10.1177/1043454216676837 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kunin-Batson A, Kadan-Lottick N, Neglia JP. The contribution of neurocognitive functioning to quality of life after childhood acute lymphoblastic leukemia. Psychooncology. 2014;23(6):692–699. [DOI] [PubMed] [Google Scholar]
- 43.Rivera Mindt M, Arentoft A, Kubo Germano K, et al. Neuropsychological, cognitive, and theoretical considerations for evaluation of bilingual individuals. Neuropsychol Rev. 2008;18(3):255–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Manly JJ. Critical issues in cultural neuropsychology: Profit from diversity. Neuropsychol Rev 2008;18:179–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Patel SK, Wong AL, Cuevas M, Van Horn H. Parenting stress and neurocognitive late effects in childhood cancer survivors. Psychooncology. 2013;22(8):1774–1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lara M, Gamboa C, Kahramanian MI, et al. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bialystok E, Craik FIM, Luk G. Bilingualism consequences for mind and brain. Trends Cogni Sci. 2012;16(4):240–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Barac R, Bialystok E, Castro DC, Sanchez M. The cognitive development of young dual language learners: a critical review. Early Child Res Q. 2014;29(4):699–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Musu-Gillette L, Robinson J, McFarland J, KewalRamani A. Status and Trends in the Education of Racial and Ethnic Groups 2016. Washington, DC: U.S. Department of Education, National Center for Education Statistics (NCES 2016–007) http://nces.ed.gov/pubs2016/2016007.pdf [Google Scholar]