Abstract
The objectives of our study were to (a) report how many children met an autism spectrum disorder (ASD) surveillance definition but had no clinical diagnosis of ASD in health or education records and (b) evaluate differences in demographic, individual, and service factors between children with and without a documented ASD diagnosis. ASD surveillance was conducted in selected areas of Arizona, Arkansas, Colorado, Georgia, Maryland, Minnesota, Missouri, New Jersey, North Carolina, Tennessee, and Wisconsin. Children were defined as having ASD if sufficient social and behavioral deficits and/or an ASD diagnosis were noted in health and/or education records. Among 4,498 children, 1,135 (25%) had ASD indicators without having an ASD diagnosis. Of those 1,135 children without a documented ASD diagnosis, 628 (55%) were not known to receive ASD services in public school. Factors associated with not having a clinical diagnosis of ASD were non-White race, no intellectual disability, older age at first developmental concern, older age at first developmental evaluation, special education eligibility other than ASD, and need for fewer supports. These results highlight the importance of reducing disparities in the diagnosis of children with ASD characteristics so that appropriate interventions can be promoted across communities.
Keywords: autism, diagnosis, disparities, surveillance
Lay Summary:
Children who did not have a clinical diagnosis of autism spectrum disorder (ASD) documented in health or education records were more likely to be non-White and have fewer developmental problems than children with a clinical diagnosis of ASD. They were brought to the attention of healthcare providers at older ages and needed fewer supports than children with a clinical diagnosis of ASD. All children with ASD symptoms who meet diagnostic criteria should be given a clinical diagnosis so they can receive treatment specific to their needs.
Introduction
One of the challenges of identifying children with autism spectrum disorder (ASD) stems from the complex nature of the diagnostic process. Typically, the diagnosis of ASD requires an observation of the child’s behavior and collection of developmental history to determine whether ASD diagnostic criteria are met [Lord, Elsabbagh, Baird, & Veenstra-Vanderweele, 2018]. The ability to access high-quality services and navigate complex health systems understandably influences the likelihood of ASD evaluation and diagnosis [Parish, Magaña, Rose, Timberlake, & Swaine, 2012; Zuckerman et al., 2014; Zuckerman et al., 2017]. Detection of ASD is also complicated by heterogeneity in symptom presentation [Lord et al., 2018], presence of co-occurring conditions [Close, Lee, Kaufmann, & Zimmerman, 2012; Levy et al., 2010], maturational changes [Fountain, Winter, & Bearman, 2012; Gotham, Pickles, & Lord, 2012; Lord, Luyster, Guthrie, & Pickles, 2012], and evolving diagnostic criteria [Matson, Kozlowski, Hattier, Horovitz, & Sipes, 2012; McPartland, Reichow, & Volkmar, 2012]. Consequently, some children with ASD characteristics do not receive a clinical diagnosis of ASD or may be diagnosed later than other children with a similar behavioral profile [Baio et al., 2018; Mandell, Ittenbauch, Levy, & Pinto-Martin, 2007; Magaña, et al., 2013].
There are numerous factors that influence the timing of ASD diagnosis, although birth cohort and socioeconomic variables such as race/ethnicity are most often reported in the literature [Daniels & Mandell, 2014]. Some studies found that children in older birth cohorts were diagnosed later than children in more recent cohorts, suggesting that the age of ASD diagnosis is decreasing with time [Daniels & Mandell, 2014]. Even still, white children are systematically diagnosed 1–2 years earlier than non-white children [Fountain et al., 2012; Mandell, Listerud, Levy, & Pinto-Martin, 2002; Valicenti-McDermott, Hottinger, Seijo, & Shulman, 2012]. One possible reason for continued racial/ethnic disparities in the timing of ASD diagnosis may be parent-doctor interactions. Non-white parents in one study more often reported that their doctor did not spend enough time with their child, did not listen to them carefully and did not make them feel like a partner than non-Latino white parents [Parish et al., 2012]. When their children were screened, non-white parents in another study reported fewer ASD concerns before ASD diagnosis than white parents, which could indicate different perceptions of similar behaviors based on cultural background [Donohue, Childs, Richards, & Robins, 2019]. Moreover, some evidence suggests healthcare providers are more likely to first diagnose developmental and behavioral disorders, such as conduct disorder, in non-white children when compared to white children who are eventually diagnosed with ASD [Mandell et al., 2007].
Other variables that contribute to delayed ASD diagnosis are co-occurring psychiatric and neurological disorders, fewer ASD symptoms, fewer functional limitations, and lack of intellectual disability [Durkin et al., 2017; Mandell et al., 2002; Ratto et al., 2017; Shatttuck et al., 2009; Maenner et al., 2013]. Parents who have children diagnosed with ASD later than others often attribute their first concerns to a behavioral or medical problem rather than a developmental problem [Daley, 2004]. Lastly, children with ASD who do not receive ASD services in public school are diagnosed later than other children [Daniels & Mandell, 2014; Keen & Ward, 2004].
Both presence and timing of an ASD diagnosis can lead to treatments associated with improved outcomes for some children, and less intensive intervention over time [Fernell, Eriksson, & Gillberg, 2013; Gourdine, Baffour, & Teasley, 2011; Howlin, Magiati, & Charman, 2009; Magiati, Tay, & Howlin, 2012]. Other possible benefits of confirming an ASD diagnosis are verifying that ASD best describes the overall pattern of symptoms according to the professional(s) who evaluated the child, providing parents with an explanation for their child’s behaviors, and easing communication between multiple providers. Additionally, confirming an ASD diagnosis can help inform policies to reduce disparities and plan for service needs [Heurta & Lord, 2012; Midence & O’Neil, 1999].
The Autism and Developmental Disabilities Monitoring (ADDM) Network is a surveillance program that tracks the prevalence and characteristics of 8-year-old children with ASD in multiple U.S. communities [Rice et al., 2007]. In the 2014 surveillance year, ADDM ASD ascertainment did not exclusively rely on a documented ASD diagnosis to establish prevalence. Rather, it conducted a record-review strategy that identified children with ASD from information contained in existing health and education records. Expert clinicians, using a standardized process, determined whether children satisfied ASD criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders—Fifth Edition (DSM-5). In addition, the expert clinicians coded multiple fields of information reflecting behavioral characteristics, intellectual functioning, co-occurring conditions, the presence of an existing ASD diagnosis documented in service records, and their degree of certainty the child had ASD. The objectives of this article are thus twofold: (a) report how many children who satisfied the ADDM DSM-5 ASD surveillance definition had no clinical diagnosis of ASD documented in health or education records and (b) evaluate differences in demographic, individual and service factors for children with and without a documented ASD diagnosis.
Methods
The DSM-5 surveillance population included 8-year-old children who had health and/or education records reviewed for ASD in 11 sites funded by the Centers for Disease Control and Prevention (CDC) as part of the 2014 ADDM Network (award cycle 2015–2018). Surveillance sites were in Arizona, Arkansas, Colorado, Georgia, Maryland, Minnesota, Missouri, New Jersey, North Carolina, Tennessee, and Wisconsin. The ADDM method is an active, multiple source, records-based system that monitors the prevalence of ASD among 8-year-old children across multiple US communities [Rice et al., 2007]. ADDM sites are chosen through a competitive review process. Each ADDM site functions as a public health authority, as specified under the Health Insurance Portability and Accountability Act of 1996 Privacy Rule and meets applicable local Institutional Review Board and privacy and confidentiality requirements.
ASD Case Ascertainment
A child was considered for ADDM ASD surveillance if he/she: (a) was born in 2006 (i.e., was 8 years old at any point during the 2014 surveillance year), (b) resided with a parent or legal guardian in a predefined surveillance area in 2014, and (c) received service for a behavioral, educational, developmental, or medical condition as evidenced by a discharge diagnosis, billing code, reason for referral, or education eligibility documented in health or education records. All ADDM sites except one (Missouri) had at least some access to education records. Six sites (Arizona, Georgia, Maryland, Minnesota, New Jersey, and North Carolina) reviewed education records for all school districts within their covered surveillance areas. Four ADDM sites (Arkansas, Colorado, Tennessee, and Wisconsin) reviewed education records in only some school districts within their covered surveillance areas (i.e., the proportion of the surveillance population residing in school districts accessed by these ADDM site ranged from 26% to 88%). In all, over 95% of the children in this sample were ascertained from sites that had at least partial access to education records.
Surveillance staff reviewed health and education records of children meeting eligibility criteria for social deficits that indicated symptoms of ASD (e.g., limited interest in other children or reduced eye contact). Information abstracted from records that contained a social deficit included developmental histories, verbatim descriptions of ASD symptoms, descriptions of co-occurring conditions, results of developmental tests, and documentation of a clinical ASD diagnosis referenced in the record or assigned by the community professional who evaluated the child (e.g., a statement that the child met criteria for an ASD diagnosis in the summary statement of a psychological report). All abstracted information was combined into one composite abstraction record if multiple health/education records were abstracted for the same child.
ASD Surveillance Case Status
Clinicians with advanced degrees and specialized training and experience in ASD applied a standardized coding scheme to each child’s composite abstraction record. ADDM record-review coding for ASD surveillance has been traditionally based on an algorithm created using DSM-IV-TR diagnoses of autistic disorder, Asperger disorder, or pervasive developmental disorder not otherwise specified (PDD-NOS). An algorithm based on the DSM-5 diagnosis of ASD, including the presence of a previous ASD diagnosis, was developed for the 2014 surveillance year. In order to meet the ADDM DSM-5 surveillance case status for ASD, the child had to have (a) the number and pattern of social and behavioral deficits defined by DSM-5 as meeting the criteria for ASD (i.e., three social deficits and two of four behavioral deficits) or (b) an existing clinical diagnosis of ASD documented in service records (i.e., DSM-IV-TR diagnoses of autistic disorder, Asperger disorder, or PDD-NOS or DSM-5 diagnosis of ASD). Figure 1 outlines the decision tree for ASD surveillance case status according to DSM-5 criteria. Inter-rater reliability for case status is monitored on an ongoing basis using a blinded, random 10% sample of abstracted records that are scored independently by two reviewers. For 2014, inter-rater agreement on DSM-5 case status (confirmed ASD vs. not ASD) was 92.3% when comparison samples from all sites were combined (k = 0.84).
Figure 1.
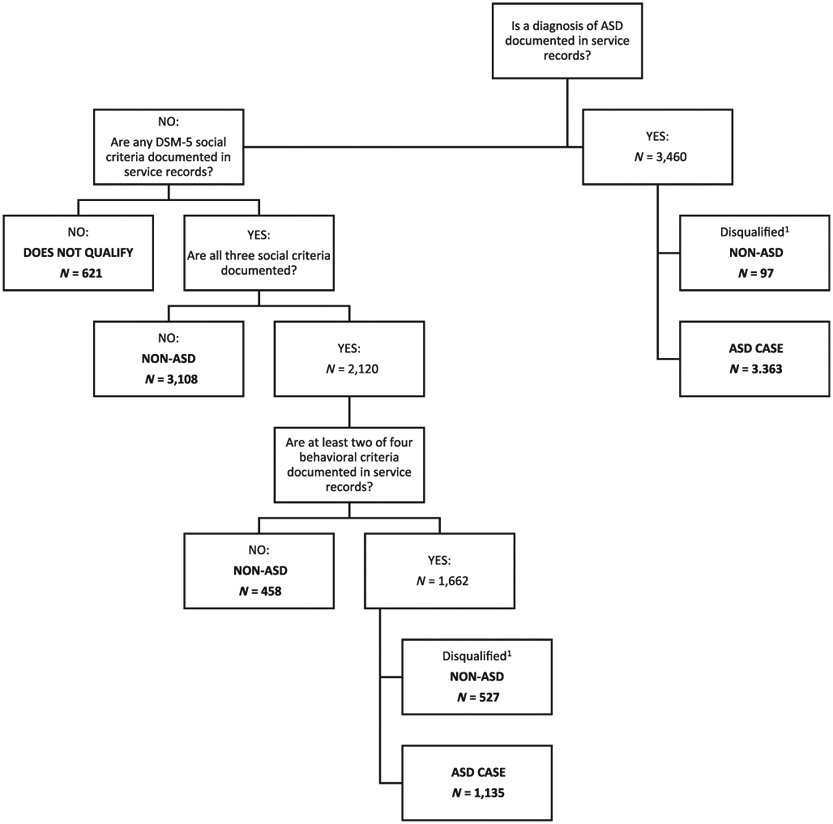
Decision tree to determine autism spectrum disorder (ASD) surveillance case status from the Autism and Developmental Disabilities Monitoring Network (2014) according to criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders—Fifth Edition. 1These cases were disqualified due to low clinician certainty the child had ASD.
The clinician who applied the surveillance-coding scheme rated the level of support needed by the child given all available information in abstracted records. The level of support needed was rated on a three-point scale with one representing the need of some support, two representing the need of substantial support, and three representing need of very substantial support (Table 1). Clinicians could overturn case status upon primary review, or call for a second review if their degree of certainty the child had ASD was low based on sufficient information to determine that symptoms were accounted for by another disorder, or any other reason (e.g., the person who evaluated the child for ASD clearly stated the child did not meet criteria for ASD but did meet criteria for attention deficit hyperactivity disorder [ADHD]).
Table 1.
Autism and Developmental Disabilities Monitoring Network (2014) Surveillance Ratings of Level of Support Needed by a Child with Autism Spectrum Disorder Given All Available Information in Service Records
| Level of support needed |
Description | Example |
|---|---|---|
| Some support needed | Without supports in place, deficits in social communication cause noticeable impairments. Difficulty initiating social interactions, and clear examples of atypical or unsuccessful response to social overtures of others. May appear to have decreased interest in social interactions. For example, a person who is able to speak in full sentences and engages in communication but whose to-and-fro conversation with others fails, and whose attempts to make friends are odd and typically unsuccessful | Inflexibility of behavior causes significant interference with functioning in one or more contexts. Difficulty switching between activities. Problems of organization and planning hamper independence |
| Substantial support needed | Marked deficits in verbal and nonverbal social communication skills; social impairments apparent even with supports in place;limited initiation of social interactions;and reduced or abnormal responses to social overtures from others. For example, a person who speaks simple sentences, whose interaction is limited to narrow special interests, and who has markedly odd nonverbal communication | Inflexibility of behavior, difficulty coping with change, or other restricted/repetitive behaviors appear frequently enough to be obvious to the casual observer and interfere with functioning in a variety of contexts. Distress and/or difficulty changing focus or action |
| Very substantial support needed | Severe deficits in verbal and nonverbal social communication skills cause severe impairments in functioning, very limited initiation of social interactions, and minimal response to social overtures from others. For example, a person with few words of intelligible speech who rarely initiates interaction and, when he or she does, makes unusual approaches to meet needs only and responds to only very direct social approaches | Inflexibility of behavior, extreme difficulty coping with change, or other restricted/ repetitive behaviors markedly interfere with functioning in all spheres. Great distress/difficulty changing focus or action action |
Note: These anchors/ratings are from the Diagnostic and Statistical Manual or Mental Disorders – Fifth Edition.
Data Analyses
Denominators for the total population within surveillance catchment areas (aggregate and by site) were determined from the National Center for Health Statistics Vintage 2016 Bridged-Race Estimates. Specifically, population denominators were derived by postcensal estimates of the number of children aged 8 years living in specified counties under DSM-5 surveillance (note that the DSM-5 catchments areas were smaller than the DSM-IV-TR catchment areas for the ADDM 2014 surveillance year due to resource constraints). Children living in school districts outside the surveillance area were subtracted from the county-level census denominators using school enrollment data from the U.S. Department of Education’s National Center for Education Statistics and adjusted for differences in race and sex within the applicable counties [CDC, 2016].
Frequencies of the number of children within the surveillance population(s) who met ADDM ASD case status are reported. Frequencies of those children, who met ADDM ASD case status who had an ASD diagnosis, and who had social and behavioral deficits exclusive of an ASD diagnosis, are also reported. Omnibus chi-square analyses compared the proportion of children who met ASD surveillance status and had a documented ASD diagnosis and those who did not have a documented ASD diagnosis on the following variables: age at first evaluation abstracted (3 years or older or younger than 3 years), autism educational exceptionality (no or yes), developmental concern noted by 3 years of age (no or yes), intellectual disability (no, yes, or unknown), level of support needed (some, substantial, or very substantial support), race/ethnicity (white non-Hispanic, black non-Hispanic, other race non-Hispanic, Hispanic, or unknown), child sex (male or female), and study site. Tennessee was chosen as the referent category for study site since the proportion of children with versus without an ASD diagnosis in Tennessee was closest to the average among all sites. All variables were then entered into an adjusted logistic regression model to identify odds ratios associated with not having a clinical diagnosis of ASD documented in health or education records controlling for all other variables considered. Post hoc analyses examined whether the same variables, excluding the receipt of ASD services in public school, were associated with neither having a clinical diagnosis of ASD nor receiving known services for ASD in school.
Results
There were 4,498 children who met ADDM ASD surveillance status based on DSM-5 social and behavioral deficits or a previous ASD diagnosis. Of those, 81.4% were male and 25.0% had known ID (23.8% had missing cognitive data). The racial and ethnic distribution of the sample was 51.0% white non-Hispanic, 23.9% black non-Hispanic, 16.1% Hispanic, 7.4% other race non-Hispanic, and 1.6% missing race and ethnicity data. A total of 3,363 (74.8%) had a documented clinical diagnosis of ASD and 1,135 (25.2%) had social and behavioral deficits exclusive of an ASD diagnosis documented in service records (Table 2). Of those 1,135 children without a documented ASD diagnosis, 55.3% (n = 628) were not known to receive ASD services in public school (Table 3).
Table 2.
The Number of Children Identified with Autism Spectrum Disorder (ASD) By the Autism and Developmental Disabilities Monitoring Network (2014) Who Did and Did Not Have an ASD Diagnosis Noted in Service Records
| Site | Total Population Number |
Number with ASD Number |
ASD diagnosis noted in service records Number (%) |
ASD social/behavioral criteria—but not diagnosis—documented in service records Number (%) |
ASD diagnosis-to-ASD criteria but no diagnosis prevalence ratio (PR) |
||
|---|---|---|---|---|---|---|---|
| PR | 95% CI | P | |||||
| Arizona | 9,478 | 162 | 99 (61.1) | 63 (38.9) | 1.6 | (1.1, 2.2) | <0.01 |
| Arkansas | 39,992 | 552 | 459 (83.2) | 93 (16.8) | 5.0 | (4.0, 6.2) | <0.01 |
| Colorado | 8,022 | 97 | 70 (72.2) | 27 (27.8) | 2.6 | (1.7, 4.1) | <0.01 |
| Georgia | 51,161 | 858 | 627 (73.1) | 231 (26.9) | 2.7 | (2.4, 3.2) | <0.01 |
| Maryland | 9,955 | 195 | 162 (83.1) | 33 (16.9) | 5.0 | (3.4, 7.2) | <0.01 |
| Minnesota | 9,767 | 220 | 111 (50.4) | 109 (49.6) | 1.0 | (0.8, 1.3) | 0.892 |
| Missouri | 12,205 | 197 | 174 (88.3) | 23 (11.7) | 7.7 | (5.0, 11.8) | <0.01 |
| New Jersey | 32,935 | 873 | 699 (80.1) | 174 (19.9) | 4.1 | (3.5, 4.8) | <0.01 |
| North Carolina | 30,283 | 498 | 314 (63.1) | 184 (36.9) | 1.7 | (1.4, 2.1) | <0.01 |
| Tennessee | 24,940 | 369 | 278 (75.3) | 91 (24.7) | 3.1 | (2.4, 3.9) | <0.01 |
| Wisconsin | 35,037 | 477 | 370 (77.6) | 107 (22.4) | 3.5 | (2.8, 4.3) | <0.01 |
| All sites combined | 263,775 | 4,498 | 3,363 (74.8) | 1,135 (25.2) | 3.0 | (2.8, 3.2) | <0.01 |
Table 3.
Characteristics of Children with ASD With and Without a Previous ASD Diagnosis, and Adjusted Odds Ratios (aOR) Associated with not Having a Documented Autism Spectrum Disorder (ASD) Diagnosis in Service Records Among Children Who Met ASD Surveillance Case Status According to Autism and Developmental Disabilities Monitoring Network (2014)
| ASD diagnosis documented in service records N = 3,363 % |
ASD criteria—but not ASD diagnosis—documented in service records N = 1,135 % |
aOR (95% CI) | P | |
|---|---|---|---|---|
| Age at first evaluation identified | ||||
| Younger than 3 years | 39.9 | 26.0 | 1.0 | REF |
| 3 years or older | 60.1 | 74.0 | 1.6 (1.4, 1.9) | <0.01 |
| Autism educational exceptionality | ||||
| Yes | 51.4 | 44.7 | 1.0 | REF |
| No | 48.6 | 55.3 | 1.5 (1.3, 1.8) | <0.01 |
| Developmental concern before 3 years of age | ||||
| Yes | 83.8 | 72.9 | 1.0 | REF |
| No | 16.2 | 27.1 | 1.5 (1.3, 1.8) | <0.01 |
| Intellectual disability (IQ ≤ 70) | ||||
| Yes | 27.3 | 18.1 | 1.0 | REF |
| No | 47.7 | 61.7 | 1.5 (1.2, 1.8) | <0.01 |
| Unknown | 25.0 | 20.3 | 1.0 (0.8, 1.3) | NS (0.7) |
| Level of support needed | ||||
| Very substantial support | 16.2 | 5.5 | 1.0 | REF |
| Substantial support | 53.2 | 47.6 | 2.2 (1.6, 3.0) | <0.01 |
| Some support | 30.6 | 47.0 | 3.3 (2.5, 4.6) | <0.01 |
| Race/ethnicity | ||||
| White non-Hispanic | 52.9 | 45.2 | 1.0 | REF |
| Black non-Hispanic | 22.7 | 27.5 | 1.7 (1.4, 2.0) | <0.01 |
| Other non-Hispanic | 7.0 | 8.3 | 1.6 (1.2, 2.1) | <0.01 |
| Hispanic | 15.5 | 18.1 | 1.6 (1.3, 2.0) | <0.01 |
| Unknown | 1.9 | 0.9 | 0.6 (0.3, 1.2) | NS (0.1) |
| Sex | ||||
| Male | 81.5 | 81.2 | 1.0 | REF |
| Female | 18.5 | 18.8 | 1.1 (0.9, 1.3) | NS (0.3) |
| Study site | ||||
| Arizona | 2.9 | 5.6 | 2.0 (1.3–3.1) | <0.01 |
| Arkansas | 13.6 | 8.2 | 0.6 (0.4–0.8) | <0.01 |
| Colorado | 2.1 | 2.4 | 0.9 (0.5–1.6) | NS (0.7) |
| Georgia | 18.6 | 20.4 | 1.0 (0.8–1.4) | NS (0.8) |
| Maryland | 4.8 | 2.9 | 0.7 (0.4–1.1) | NS (0.1) |
| Minnesota | 3.3 | 9.6 | 2.9 (2.0–4.3) | <0.01 |
| Missouri | 5.2 | 2.0 | 0.3 (0.2–0.6) | <0.01 |
| New Jersey | 20.8 | 15.3 | 0.7 (0.5–0.9) | <0.05 |
| North Carolina | 9.3 | 16.2 | 2.1 (1.5–2.9) | <0.01 |
| Tennessee | 8.3 | 8.0 | 1.0 | REF |
| Wisconsin | 11.0 | 9.4 | 0.9 (0.7–1.3) | NS (0.7) |
Table 3 shows differences between children who did and did not have a clinical ASD diagnosis documented in health or education records among predefined variables, and adjusted odds ratios associated with not having a documented ASD diagnosis for those same variables. In this analysis, the −2 log-likelihood value was smaller for the fitted model, indicating that the fitted model performed better than the intercept only model. Children who did not have a clinical diagnosis of ASD documented in health or education records were more likely than other children to have a developmental concern noted after 3 years of age, first evaluation after 3 years of age, receipt of special education services other than ASD, intellectual functioning outside of the disability range, need for fewer supports, and be from certain geographic areas (Table 3). They were also more likely to be black non-Hispanic, other non-Hispanic race, or Hispanic than white non-Hispanic. The absence of a documented ASD diagnosis was not influenced by child sex. Unadjusted analyses found very similar results with unchanged direction or significance of findings.
Additionally, we looked at children who did not have a clinical diagnosis nor were known to receive ASD services in public school (n = 628). These children were more likely than others to be evaluated after 3 years of age than at or before 3 years of age (OR = 1.3, 95% CI 1.1, 1.6), have average intellectual functioning versus intellectual disability (OR = 1.4, 95% CI 1.1, 1.9), need some support (OR = 4.5, 95% CI 2.6,8.0) or substantial support (OR = 11.3, 95% CI 6.4, 20.2) than very substantial support, and be non-Hispanic black (OR = 1.4, 95% CI 1.1, 1.7), other non-Hispanic race (OR = 1.7, 95% CI 1.2,2.4), or Hispanic (OR = 1.3, 95% CI 1.0, 1.7) than non-Hispanic white. They were less likely to be from Arkansas (OR = 0.49, 95% CI 0.32, 0.76), Georgia (OR = 0.63, 95% CI 0.43, 0.94), and Missouri (OR = 0.29, 95% CI 0.14, 0.57) than Tennessee. The absence of a clinical diagnosis or ASD educational services was not influenced by developmental concerns noted in the first 3 years or child sex (data not shown).
Discussion
Diagnosing children with ASD symptoms may facilitate delivery of services that maximize the developmental potential of the child and provide supports to their families, among other benefits (e.g., easing communication between multiple providers) [Heurta & Lord, 2012; Midence & O’Neil, 1999]. Our findings indicate that 25.2% of children with ASD identified by ADDM in surveillance year 2014 had enough symptoms in service records to satisfy ASD diagnostic criteria but did not have a clinical diagnosis of ASD documented in service records. Approximately 55.3% of these children were not known to receive ASD services in their school. Children identified by ADDM who did not have a clinical diagnosis of ASD differed from those who did have a clinical diagnosis in that they were more likely to be non-White, older than 3 years at first developmental concern, older than 3 years at first evaluation, have no intellectual disability, and need fewer supports. These findings complement those on timing of ASD diagnosis and highlight the need to address factors that facilitate disparities in both timing and documenting an ASD diagnosis in service records [Daniels & Mandell, 2014; Fountain et al., 2012; Mandell et al., 2002;Valicenti-McDermott et al., 2012].
Non-Hispanic black and Hispanic children were less likely than non-Hispanic white children to have a diagnosis of ASD noted in service records. Racial and ethnic disparities in ASD diagnosis are well-documented in a variety of clinical and surveillance reports [Bernier, Mao, & Yen, 2010; Durkin et al., 2017; Liptak et al., 2008; Mandell et al., 2002; Mandell et al., 2007; Mandell et al., 2009]. Some perceived barriers to ASD diagnosis reported by non-Hispanic black and Hispanic parents are confusion and frustration with the diagnostic process, high levels of stigma in some communities, lack of parental information about ASD, limited English proficiency, and provider dismissal of parental concerns [Parish et al., 2012; Zuckerman et al., 2014; Zuckerman et al., 2017]. Moreover, when seen in clinics, black parents eventually diagnosed with ASD report fewer ASD symptoms compared to white parents on written questionnaires [Donohue et al., 2019].
A few interventions have been shown to reduce disparities in ASD diagnosis. One such intervention is the use of patient navigators who explore parental understanding of and need for a diagnostic assessment, help complete documents required for the assessment, and ensure the family understands assessment results. Patient navigators can also help identify and develop a plan to address barriers to care. Previous research found that families that worked with a patient navigator were more likely than families who received routine clinical care to complete an ASD diagnostic assessment and receive timely ASD diagnosis [Feinberg et al., 2016]. Other effective or promising intervention strategies to reduce disparities in ASD dentification are using pictorial ASD screens to reduce linguistic and literacy demands [Janvier, Coffield, Harris, Mandell, & Cidav, 2019], asking healthcare providers to rate their likelihood of referral for certain disorders on a continuous rather than dichotomous scale [Begeer, Bouk, Boussaid, Terwogt, & Koot, 2009], and adopting a presumptive eligibility approach where early intervention services are based on an at-risk screen before diagnostic evaluation [Rotholz, Kinsman, Lacy, & Charles, 2017]. More research is needed on the utility of parent and provider education and stigma reduction in reducing disparities in ASD diagnosis.
As previously mentioned, one possible benefit of receiving a clinical diagnosis is to facilitate access to appropriate services. Over the past decade, many states have enacted laws that mandate insurance companies to reimburse evidence-based treatments for ASD; including but not limited to behavioral therapy (e.g., applied behavior analysis), occupational therapy, physical therapy, speech therapy, social skills training, and a combination of these [Barry et al., 2017; Dawson & Burner, 2011; Douglas, Benevides, & Carretta, 2017; Kasari, 2015; Zwaigenbaum et al., 2015]. However, justification for the medical necessity of therapies is most often needed before insurers will approve and reimburse service requests. Although comprehensive service use and insurance status are not surveyed in ADDM, a clinical diagnosis of ASD may support such justification and help reduce the financial burden of raising a child with special needs by decreasing out-of-pocket premiums. Recognizing and diagnosing children with ASD symptoms may, therefore, facilitate access to appropriate services and reduce financial strain.
Older children and those without ID were also less likely to have an ASD diagnosis documented in health or education records. These findings complement previous research that found earlier age of ASD diagnosis was associated with greater cognitive impairment [Shatttuck et al., 2009]. In our study, children with ASD symptoms without an ASD diagnosis still needed some support (47.0%), substantial support (47.6%) and very substantial support (5.5%) to function in daily life despite older age and cognitive abilities above the disability range. General developmental and ASD screening efforts may need to extend beyond the preschool years and among children from different backgrounds in order to identify those who could benefit from early interventions, including those specific to ASD.
The prevalence ratio for having a previous ASD diagnosis compared to having ASD symptoms without an ASD diagnosis varied substantially across sites (from 1.0 in Minnesota to 7.7 in Missouri), and the study site was a significant predictor of a clinical diagnosis documented in health or education records. These results highlight geographic differences in whether children with ASD symptoms receive a clinical diagnosis. Some communities (i.e., those with higher prevalence ratios) may diagnose more children included in ASD surveillance than other communities (i.e., those with lower prevalence ratios), even though children without a diagnosis could be receiving ASD services in a public school (as seen in 45.7% of our sample without a clinical diagnosis) or elsewhere. ADDM sites can use these results to inform policy efforts to strengthen screening and diagnostic frameworks within their communities and share effective practices with localities outside the ADDM Network.
It is important to reflect on the fact that one-fourth of children who met the ADDM ASD surveillance definition did not have a clinical diagnosis of ASD documented in health or education records and, of those, 55.3% were not known to receive ASD services in public school. We do not know whether children without a documented diagnosis would meet diagnostic criteria if evaluated specifically for ASD, or if they would present with subthreshold symptom presentation or have symptoms better accounted for by another disorder (e.g., ADHD). Based on information contained in health and/or education records, we do know that these children had the number and pattern of social and behavioral deficits to be confirmed as an ASD surveillance case, clinicians rated their degree of certainty the child had ASD as high versus low, and more than half of these children were rated to required substantial or very substantial support to function in daily life. In sum, these results indicate that some children with a significant number of ASD symptoms coupled with functional limitations may not have a clinical diagnosis of ASD and might remain unserved or underserved in education or healthcare settings.
There are some limitations associated with these analyses. ADDM record review surveillance is not nationally representative, thus results cannot be generalized to all U.S. communities. Moreover, ADDM 2014 data are subject to the following considerations: (a) some children with an ASD diagnosis given after records were abstracted may not have been considered for ASD surveillance (e.g., no social trigger documented in records), (b) it is possible that a child received an ASD diagnosis before records were abstracted that was not documented in the records we reviewed, (c) it is possible that children who did not have an ASD diagnosis nor receive ASD services in school received services elsewhere in the community, (d) children with social and behavioral deficits without an ASD diagnosis who were counted as surveillance cases may not be best described as having ASD, and (e) ASD case status was determined by a record-review method instead of through direct clinical evaluation of the child. Despite these limitations, ADDM record-review surveillance from 2014 provided in-depth information on the characteristics of children with and without ASD and counted children with an ASD phenotype irrespective of diagnostic confirmation. These strengths are unique to ADDM 2014 surveillance and allowed analyses on children who have ASD symptoms but no clinical diagnosis of ASD noted in health or education records.
In conclusion, we found that 25.2% of children identified by ADDM ASD surveillance had symptoms but no ASD diagnosis documented in health or education records and 55.3% of these children were not known to receive ASD services in school. Factors associated with not having a clinical ASD diagnosis were non-White race, no intellectual disability, older age at first concern, older age at first evaluation, special education eligibility other than ASD, and fewer supports needed. These results highlight the importance of reducing disparities in the diagnoses of children with ASD symptoms so that appropriate interventions can be promoted across communities.
Acknowledgments
We would like to thank ADDM principal investigators, project staff, and community partners. Funding was provided by the Centers for Disease Control and Prevention through cooperative agreements with each of the ADDM sites. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Footnotes
Conflict of Interest
The authors declare that they have no conflict of interest related to this work.
Contributor Information
Lisa D. Wiggins, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention, Atlanta, Georgia
Maureen Durkin, Department of Population Health Sciences, School of Medicine and Public Health, University of Wisconsin, Madison, Wisconsin.
Amy Esler, Department of Pediatrics, University of Minnesota, Minneapolis, Minnesota.
Li-Ching Lee, Department of Epidemiology, Bloomberg School of Public Health, John Hopkins University, Baltimore, Maryland.
Walter Zahorodny, Department of Pediatrics, Rutgers New Jersey Medical School, Newark, New Jersey.
Catherine Rice, Department of Psychiatry, Early Emory Center for Child Development and Enrichment, Emory University, Atlanta, Georgia.
Marshalyn Yeargin-Allsopp, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention, Atlanta, Georgia.
Nicole F. Dowling, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention, Atlanta, Georgia
Jennifer Hall-Lande, Institute on Community Integration, University of Minnesota, Minneapolis, Minnesota.
Michael J. Morrier, Department of Psychiatry, Early Emory Center for Child Development and Enrichment, Emory University, Atlanta, Georgia
Deborah Christensen, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention, Atlanta, Georgia.
Josephine Shenouda, Department of Pediatrics, Rutgers New Jersey Medical School, Newark, New Jersey.
Jon Baio, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention, Atlanta, Georgia.
References
- Baio J, Wiggins LD, Christensen DL, Daniels J, Warren Z, Kurzius-Spencer M, … Dowling NF (2018). Prevalence of autism spectrum disorder among children aged 8 years – Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2014. MMWR Surveillance Summaries, 67(6), 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry CL, Epstein AJ, Marcus SC, Kennedy-Hendrick A, Candon MK, Yei M, … Mandell D (2017). Effects of state insurance mandates on health care use and spending for autism spectrum disorder. Health Affairs, 36(10), 1754–1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begeer S, Bouk S, Boussaid W, Terwogt M, & Koot H (2009). Underdiagnosis and referral bias in autism in ethnic minorities. Journal of Autism and Developmental Disorders, 39, 142–148. [DOI] [PubMed] [Google Scholar]
- Bernier R, Mao A, & Yen J (2010). Psychopathology, families, and culture: Autism. Child and Adolescent Psychology Clinics of North America, 19(4), 855–867. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2016). Vintage 2016 Bridged-race postcensal population estimates for April 1, 2010, July 1, 2010–July 1, 2016, by year, county, singleyear of age (0 to 85+ years), bridged-race, Hispanic origin, and sex. https://www.cdc.gov/nchs/nvss/bridged_race.htm.
- Close HA, Lee LC, Kaufmann CN, & Zimmerman AW (2012). Co-occurring conditions and change in diagnosis in autism spectrum disorder. Pediatrics, 129, 305–316. [DOI] [PubMed] [Google Scholar]
- Daley TC (2004). From symptom recognition to diagnosis: children with autism in urban India. Social Science & Medicine, 58(7), 1323–1335. [DOI] [PubMed] [Google Scholar]
- Daniels A & Mandell D (2014). Explaining differences in age at autism spectrum disorder diagnosis: A critical review. Autism, 8(15), 583–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson G, & Burner K (2011). Behavioral interventions in children and adolescents with autism spectrum disorder: A review of recent findings. Current Opinions in Pediatrics, 23 (6), 616–620. [DOI] [PubMed] [Google Scholar]
- Donohue MR, Childs AW, Richards M, & Robins DL (2019). Race influences parent report of concerns about symptoms of autism spectrum disorder. Autism, 23(1), 100–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas MD, Benevides TW, & Carretta H (2017). Analyzing state autism private insurance mandates for allied health services: A pilot study. OTJR, 37(4), 218–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkin MS, Maenner MJ, Baio J, Christensen D, Daniels J, Fitzgerald R, … Yeargin-Allsopp M (2017). Autism spectrum disorder among U.S. children (2002–2010): Socioeconomic, racial, and ethnic disparities. American Journal of Public Health, 107(11), 181–1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg E, Abufhele M, Sandler J, Augustyn M, Cabral H, Chen N, … Silverstein M (2016). Reducing disparities in timely autism diagnosis through family navigation: Results from a randomized pilot trial. Psychiatric Services, 67, 912–915. [DOI] [PubMed] [Google Scholar]
- Fernell E, Eriksson MA, & Gillberg C (2013). Early identification of autism and impact on prognosis: A narrative review. Clinical Epidemiology, 5, 33–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fountain C, Winter AS, & Bearman PS (2012). Six developmental trajectories characterize children with autism. Pediatrics, 129(5), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotham K, Pickles A, & Lord C (2012). Trajectories of autism severity in children using standardized ADOS scores. Pediatrics, 130(5), 1278–1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gourdine R, Baffour T, & Teasley M (2011). Autism and the African-American community. Social Work in Public Health, 26, 454–470. [DOI] [PubMed] [Google Scholar]
- Heurta M, & Lord C (2012). Diagnostic evaluation of autism spectrum disorders. Pediatric Clinics of North America, 59, 103–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlin P, Magiati I, & Charman T (2009). Systematic review of early intensive behavioral interventions for children with autism. American Journal of Intellectual Disabilities, 114(1), 23–41. [DOI] [PubMed] [Google Scholar]
- Janvier YM, Coffield C, Harris JF, Mandell DS, & Cidav Z (2019). The developmental check-in: Development and initial testing of an autism screening tool targetin young children from underserved communities. Autism, 23(3), 689–698. [DOI] [PubMed] [Google Scholar]
- Kasari C (2015). Update on behavioral interventions for autism and developmental disabilities. Current Opinion in Neurology, 28(2), 124–129. [DOI] [PubMed] [Google Scholar]
- Keen D, & Ward S (2004). Autistic spectrum disorder: A child population profile. Autism, 8(1), 39–48. [DOI] [PubMed] [Google Scholar]
- Levy SE, Giarelli E, Lee LC, Schieve L, Kirby R, Cunniff C, … Rice C (2010). Autism spectrum disorder and co-occurring developmental, psychiatric, and medical conditions among children in multiple populations of the United States. Journal of Developmental and Behavioral Pediatrics, 31(4), 267–275. [DOI] [PubMed] [Google Scholar]
- Liptak GS, Benzoni LB, Mruzek DW, Nolan KW, Thingvoll MA, Wade CM, … Fryer G (2008). Disparities in diagnosis and access to health services for children with autism: Data from the National Survey of Children’s Health. Journal of Developmental and Behavioral Pediatrics, 29(3), 152–160. [DOI] [PubMed] [Google Scholar]
- Lord C, Elsabbagh M, Baird G, & Veenstra-Vanderweele J (2018). Autism spectrum disorder. Lancet, 392, 508–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Luyster R, Guthrie W, & Pickles A (2012). Patterns of developmental trajectories of toddlers with autism spectrum disorder. Journal of Consulting and Clinical Psychology, 80(3), 477–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maenner MJ, Schieve LA, Rice CE, Cunniff C, Giarelli E, Kirby RS, … Durkin MS (2013). Frequency and pattern of documented diagnostic features and the age of autism identification. Journal of the American Academy of Child and Adolescent Psychiatry, 52(4), 401–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magiati I, Tay X, & Howlin P (2012). Early comprehensive behaviorally based interventions for children with autism spectrum disorders: A summary of findings from recent reviews and meta-analyses. Neuropsychiatry, 2, 543–570. [Google Scholar]
- Mandell D, Ittenbauch RF, Levy SE, & Pinto-Martin J (2007). Disparities in diagnoses received prior to a diagnosis of autism spectrum disorder. Journal of Autism and Developmental Disorders, 37(9), 1795–1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandell D, Listerud J, Levy SE, & Pinto-Martin J (2002). Race differences in the age at diagnosis among Medicaid eligible children with autism. Journal of the American Academy of Child and Adolescent Psychiatry, 41(12), 1447–1453. [DOI] [PubMed] [Google Scholar]
- Mandell DS, Wiggins LD, Carpenter LA, Daniels J, DiGuiseppi C, Durkin MS, … Kirby RS (2009). Racial/ethnic disparities in the identification of children with autism spectrum disorders. American Journal of Public Health, 99(3), 493–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matson JL, Kozlowski AM, Hattier MA, Horovitz M, & Sipes M (2012). DSM-IV versus DSM-5 diagnostic criteria for toddlers with autism. Developmental Neurology, 15(3), 185–190. [DOI] [PubMed] [Google Scholar]
- McPartland JC, Reichow B, & Volkmar FR (2012). Sensitivity and specificity of proposed DSM-5 diagnostic criteria for autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 51(4), 368–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midence K, & O’Neil M (1999). The experience of parents in the diagnosis of autism: A pilot study. Autism, 3, 273–285. [Google Scholar]
- Parish S, Magaña S, Rose R, Timberlake M, & Swaine JG (2012). Health care of Latino children with autism and other developmental disabilities: Quality of provider interaction mediates utilization. American Journal of Intellectual and Developmental Disabilities, 117(4), 304–315. [DOI] [PubMed] [Google Scholar]
- Ratto AB, Kenworthy L, Yerys BE, Bascom J, Wieckowski AT, White SW, … Gutermuth-Anthony L (2017). What about girls? Sex-based differences in autistics traits and adaptive skills. Journal of Autism and Developmental Disorders, 48(5), 1698–1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice CE, Baio J, Van Naarden Braun K, Doernberg N, Meaney FJ, Kirby RS, & ADDM Network. (2007). A public health collaboration for the surveillance of autism spectrum disorders. Paediatric Perinatal Epidemiology, 21, 179–190. [DOI] [PubMed] [Google Scholar]
- Rotholz DA, Kinsman AM, Lacy KK, & Charles J (2017). Improving early identification and intervention for children at-risk for autism spectrum disorder. Pediatrics, 139(2), e20161061. [DOI] [PubMed] [Google Scholar]
- Shatttuck PT, Durkin M, Maenner M, Newshaffer C, Mandell D, Wiggins LD, … Cuniff C (2009). Timing of identification among children with an autism spectrum disorder: Findings from a population-based surveillance study. Journal of the American Academy of Child and Adolescent Psychiatry, 48(5), 474–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valicenti-McDermott M, Hottinger K, Seijo R, & Shulman L (2012). Age at diagnosis of autism spectrum disorder. Journal of Pediatrics, 161(3), 554–556. [DOI] [PubMed] [Google Scholar]
- Zuckerman KE, Lindly OJ, Reyes NM, Chavez AE, Macias K, Smith KN, & Reynolds A (2017). Dispariteis in diagnosis and treatment of autism in Latino and Non-Latino families. Pediatrics, 139(5), e20163010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman KE, Sinche B, Mejia A, Cobian BA, Becker T, & Nicolaidis C (2014). Latino parent’s perspectives of barriers to autism diagnosis. Academy of Pediatrics, 14(3), 301–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwaigenbaum L, Bauman ML, Choueiri R, Kasari C, Carter A, Granpeesheh D, … Natowicz M(2015). Early intervention for children with autism spectrum disorder under 3 years of age: Recommendations for practice and research. Pediatrics, 136(Supplement 1), S60. [DOI] [PMC free article] [PubMed] [Google Scholar]


