Abstract
Objective:
Patients with bipolar disorders have a high risk of suicidal behavior. Childhood maltreatment is a well-established risk factor for suicidal behavior. The objective of this study was to examine the association between childhood-maltreatment subtypes and vulnerability to suicide attempts in bipolar disorder using the Childhood Trauma Questionnaire (CTQ).
Methods:
A literature review was performed using the MEDLINE, Embase, and PsycINFO databases. Thirteen studies met the selection criteria. In the meta-analysis, the Childhood Trauma Questionnaire (CTQ) was used to assess a wide range of childhood maltreatment subtypes, which were analyzed by using a random-effects model to account for the likely variations of true effect sizes between the included studies.
Results:
In the systematic review, 13 studies met the selection criteria. The CTQ was selected for the meta-analysis to increase the homogeneity of assessment and to encompass a wide range of childhood-maltreatment subtypes. The data were analyzed using a random-effects model. Compared to bipolar non-attempters, bipolar suicide attempters had experienced childhood maltreatment with a significantly higher frequency and had higher total CTQ scores (Hedges’ g = -0.38, 95%CI -0.52 to -0.24, z = -5.27, p < 0.001) and CTQ sub-scores (sexual abuse: g = -0.39, 95%CI -0.52 to -0.26, z = -5.97; physical abuse: g = -0.26, 95%CI -0.39 to -0.13, z = -4.00; emotional abuse: g = -0.39, 95%CI -0.65 to -0.13, z = -2.97; physical neglect: g = -0.18, 95%CI -0.31 to -0.05, z = -2.79; emotional neglect: g = -0.27, 95%CI -0.43 to -0.11, z = -3.32).
Conclusions:
Childhood maltreatment, as assessed by the CTQ, may contribute to an increased risk of suicidal behavior among people with bipolar disorders. Recognizing maltreatment as an etiological risk factor is a crucial step toward furthering science-based preventive psychiatry.
Keywords: Suicidal behavior, vulnerability, childhood maltreatment, bipolar disorder
Introduction
Bipolar disorder (BD) is strongly associated with the risk of suicidal behavior (SB), and 10 to 15% of BD patients eventually die by suicide.1 SB is complex and multifactorial, resulting from the interaction of environmental and biological factors.2 Among short- and long-term environmental risk factors for SB, childhood-maltreatment (CM) plays an important role. World Health Organization data show that 25% of all adults report having been physically abused as children3 and this prevalence is as high as 57% among BD patients.4 In fact, CM has serious lifelong effects on neurobiology (e.g., neuroinflammation) and is strongly associated with unfavorable clinical course and disease progression in BD.5,6
CM is generally defined by sustained or repeated exposure to events that usually involve a betrayal of trust.7 Active examples of CM include childhood sexual and physical abuse, and various forms of emotional abuse. Passive examples include emotional and physical neglect.8 In this regard, strong evidence suggests that different types of adversity may contribute to SB in BD patients.5,6 The impact depends on timing, type, and severity of exposure,9 and has cumulative effects over time.10-12
Despite considerable interest in this subject, efforts to better understand the interactions between CM and SB have been hampered by a lack of consensus regarding the definition and measurement of CM. This heterogeneity decreases the internal and external validity of the available evidence, thereby limiting its generalizability and potential clinical applications. Indeed, prior research has highlighted the need to examine the specific impact of childhood trauma subtypes on severe BD outcomes.13
One potential solution to this problem is the systematic use of a validated and reliable questionnaire to obtain data that is replicable and generalizable across different contexts. Perhaps the most promising tool yet developed is the Childhood Trauma Questionnaire (CTQ),14 which is the most widely used quantitative measure of CM. The CTQ is available in multiple languages,15 has been validated in clinical and nonclinical settings,14 and possesses excellent test-retest stability.14 For these reasons, the CTQ is currently the front-runner for assessing CM – though each instrument has advantages and disadvantages, and newer instruments are being developed.16
Furthermore, several studies (including meta-analysis) have suggested a strong association between CM and SB in BD.5,6,12,13,17-20 However, evidence is lacking on the association between various subtypes of CM and SB, particularly when more homogeneous concepts of maltreatment are used (e.g., the CTQ). For instance, although a meta-analysis by Agnew-Blais et al. addressed subtypes of trauma and unfavorable clinical outcomes in BD, they employed a broad approach to collect data on childhood trauma, which was extracted from different questionnaires across studies.5 Therefore, deeper knowledge with a more narrow construct could guide future studies on this topic, such as explorations of the specific neurobiological consequences of childhood trauma on adult brains.21
In this context, we hypothesize that BD patients who attempted suicide have higher childhood trauma in differential subtypes measured by CTQ than BD patients without SB. We sought to conduct 1) a review of studies on CM (physical and emotional negligence and physical, emotional, and sexual abuse) using the CTQ and 2) a meta-analysis aimed at clarifying the relationship between the type of CM experienced based on a standardized and uniform method, the CTQ, and vulnerability to SB in BD.
Methods
Literature search
A systematic literature search of MEDLINE, Embase, and PsycINFO databases was performed for human studies published until February 2019 in English or French. The Medical Subject Heading (MeSH) term “suicide” was combined with the MeSH terms “bipolar disorder,” and “child abuse (adult survivors of child abuse),” and with the Title/Abstract (TIAB) terms “CTQ,” “child abuse,” “child neglect,” “child maltreatment,” “childhood abuse,” “childhood maltreatment,” “sexual abuse,” “physical abuse,” “emotional abuse,” and “family conflict.” An iterative process was used to ensure that all relevant articles were obtained. Bibliographical references of the selected papers and existing reviews were manually searched to identify additional potential studies. In cases of overlapping datasets, the most recently published studies were chosen.
Study selection
Abstract selection was based on the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) checklist,22 which describes items that should be included in reports of cohort studies. Abstracts identified through the literature search were independently evaluated by two reviewers (DD and SR-D) and were selected by consensus from all authors.
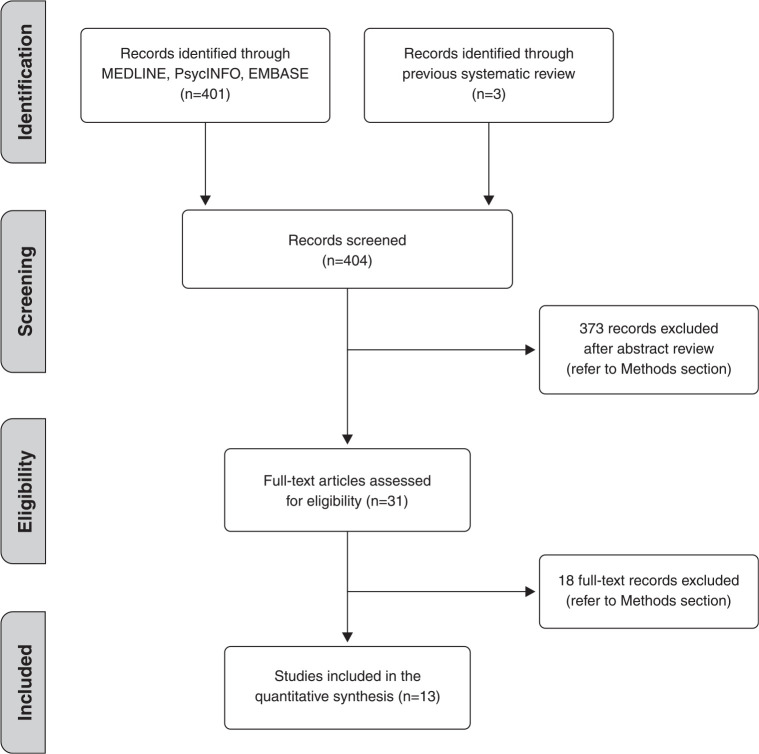
Studies that met the following inclusion criteria were included in this systematic review: 1) original articles published in an English or French language peer-reviewed journal; 2) that included CM assessment with the CTQ; 3) that included at least two groups of patients, of which at least one had a history of suicide attempt and who 4) have BD according to DSM criteria. A suicide attempt was defined as any act carried out with a certain intent to die, distinct from non-suicidal self-injury.23 As pointed out, since the study of CM is highly affected by subjectivity and heterogeneity across publications, a number of studies24-26 were excluded, despite their importance, due to not using the CTQ. After analysis of the titles and abstracts, the full articles were obtained for final review. The study selection process is shown in Figure 1.
Figure 1. Study selection process.
Of the 404 abstracts and records originally identified in previous systematic reviews, 13 met the inclusion criteria for this systematic review (Table 1). The quality of each study was assessed independently by two reviewers (DD and SRD) using the Crombie criteria adapted by Petticrew et al.27
Table 1. Review of studies exploring childhood abuse in BD patients with SB.
| Author (country) | Study type and population | Medication | Source of information on SB* | Instrument | Results |
|---|---|---|---|---|---|
| Janiri28 (Italy) | Cross-sectional study Outpatients diagnosed with BD-I (n=58) or II (n=46) (DSM-IV) (n=104) SA BD I (n= 49) >PC BD I (n=50) SA BD II (n=21) PC BD II (n=35) |
Stable drug treatment for at least of 6 months | Semi-structured questionnaire | CTQ | SA > PC: higher CTQ emotional abuse sub-scores were associated with lifetime suicide attempts. Only hyperthymic temperament differentiated patients with a history of suicidal ideation vs. those with a history of suicide attempt. The only statistically significant demographic difference between BD patients with and without SA was gender; there were more males in the non-suicidal group. |
| Pavlova29 (Canada) | Cross-sectional study Out- and inpatients diagnosed with BD-I (n=81) and BD-II (n=93) SA (n=69) PC (n=105) |
N/A | MINI-Plus | CTQ | None of the specific severity indicators for BD and childhood-maltreatment (total CTQ scores) were significantly associated with a history of suicide attempts. No CTQ sub-scores were evaluated. There was no statistically significant difference in age and gender between groups. |
| Duarte30 (Brazil) | Case-control study Outpatients diagnosed with BD-I (n=39) (DSM-IV) SA (n=20) PC (n=19) |
Yes† ‡ § || | MINI-Plus | CTQ | SA > PC: higher total CTQ scores and higher CTQ sub-scores (emotional, physical, and sexual abuse; emotional and physical neglect). No statistically significant difference in age, gender, education level, and parental education between groups. |
| Cakir31 (Turkey) | Cross-sectional study from an ongoing follow-up project Outpatients diagnosed with BD-I (n=135) (DSM-IV) SA (n=21) PC (n=114) |
Yes† ‡ § || | SCID-I | CTQ | SA > PC: higher total CTQ scores, higher CTQ emotional neglect sub-scores followed by emotional abuse subscale. No demographic comparison between BD with SA vs. BD without SA. |
| Bernegger32 (Austria) | Cross-sectional study Inpatients or outpatients with either major depressive (n=211) or BD (n=44) (DSM-IV-TR) SA BD (n=12, 17.1%) PC BD (n=32, 17.3%) |
N/A | VI-SURIAS SBQ-R | CTQ | SA > PC: higher total CTQ scores and higher CTQ sub-scores (emotional, physical, and sexual abuse; emotional and physical neglect) in females. No statistically significant difference in gender between groups. |
| Mert33 (Turkey) | Cross-sectional study Inpatients or outpatients diagnosed with BD-I (n=91) (DSM-IV) SA BD (n=61, 67%) PC BD (n=30, 33%) |
N/A | MINI-Plus | CTQ | SA BD-I: number of major depressive episodes and history of emotional neglect were predictors of suicide attempts in BD-I patients. No statistically significant difference in age, gender, education level, and marital and employment status between groups. |
| Janiri34 (Italy) | Cross-sectional study Outpatients diagnosed with BD-I (n=58) or II (n=46) (DSM-IV) (n=104) SA BD I (n=12) PC BD I (n=46) SA BD II (n=14) PC BD II (n=32) |
Stable medication for a minimum of 6 months | Semi-structured questionnaire | CTQ | SA BD-I > PC BDI: higher total CTQ scores and higher CTQ sub-scores for emotional and sexual abuse. SA BDII > PC BDII: higher total CTQ scores and higher CTQ sub-scores for emotional abuse. Emotional abuse: independent predictor of lifetime suicide attempts in BD patients. No statistically significant difference in age, gender, and education level between groups. |
| Li35 (China) | Cross-sectional study Outpatients diagnosed with diagnosis BD type I (DSM-IV) SA (n=31) PC (n=101) |
N/A | SCID-I | CTQ-SF | SA > PC: higher total CTQ scores and higher CTQ sub-scores (emotional, physical, and sexual abuse, as well as emotional and physical neglect), but not statistically significant. No demographic comparison between BD with SA vs. BD without SA. |
| Erten36 (Turkey) | Cross-sectional study Outpatients diagnosed BD (n=116) (DSM-IV) SA BD (n=36) PC BD (n=80)CHT history (at least one type: n=71, 61.2%) |
N/A | SI-HDRS-21 | CANQ | SA >PC: significant correlation between any type of CHT and suicide attempt. SA > PC: higher total CTQ scores and higher CTQ sub-scores for physical, sexual, and emotional abuse. No demographic comparison between BD with SA vs. BD without SA. Broad demographic description of the sample. |
| Watson37 (England) | Cross-sectional study Outpatients diagnosed with BD I (n=31), II (n=25), or NOS (n=4) (DSM-IV) SA (n=31) PC (n=24) |
Stable medication for a minimum of 4 weeks | SCID-IHDRS-17 | CTQ | SA > PC: higher total CTQ scores, higher CTQ emotional neglect sub-scale score followed by emotional abuse sub-scale. No demographic comparison between BD with SA vs. BD without SA. Broad demographic description of the sample. |
| Etain38 (France and Norway) | Cross-sectional study In and outpatients diagnosed BD (type I, type II, or NOS) (n=587) (DSM-IV) SA (n=211) PC (n=376) |
Yes† | SCID-I | CTQ | SA > PC: higher total CTQ scores and higher CTQ sub-score (emotional, physical and sexual abuse). Emotional and sexual abuse were independently associated with increased history of suicide attempt. No demographic comparison between BD with SA vs. BD without SA. Broad demographic description of the sample. |
| Pompili39 (Italy) | Cross-sectional study Inpatients with psychiatric disorder (DSM IV-TR) (n=62) (15% BD I, 26% BD II, 7% major depressive episode, 15% psychosis, or 8% other specified diagnosis) HSR (n=20) LSR (n=42) |
Yes | MMPI-2 | CTQ | HSR > LSR: higher risk of suicide with history of physical or sexual abuse. Patients who reported physical abuse by family members were more likely to be at higher risk for suicide. Being insulted - six times; bruises or marks - nine times; and punishment with a belt or hard object - 20 times more likely to be at higher risk for suicide. No demographic comparison between BD with SA vs. BD without SA. |
| Garno40 (USA) | Cross-sectional study Out and inpatients diagnosed with BD (n=100) (DSM-IV) |
Yes | SADS | CTQ | SA > PC: a near-significant relationship between lifetime suicide attempts and history of sexual abuse. Demographic comparison of BD with and without cluster B personality disorder. No demographic comparison between groups with and without SA. |
BD = bipolar disorder; CANQ = Childhood Abuse and Neglect Questionnaire; CHT = ; CTQ = Childhood Trauma Questionnaire; CTQ-SF = Childhood Trauma Questionnaire-Short Form; HDRS-17 = 17-item version of the Hamilton Depression Rating Scale41,42; HSR = higher suicidal risk; LSR = lower suicidal risk; MINI-Plus = Mini International Neuropsychiatric Interview-Plus; MMPI-2 = Minnesota Multiphasic Personality Inventory-2; N/A = not available; NOS = not otherwise specified; PC = patient controls (i.e., patients with no history of suicide attempt); SA = suicide attempters (i.e., patients with a history of suicide attempt); SADS = Schedule for Affective Disorders and Schizophrenia; SB = suicidal behavior; SBQ-R = Revised Suicidal Behaviors Questionnaire43; SCID = Structured Clinical Interview for DSM-IV Axis I disorders; SI-HDRS-21 = Structured Interview for Hamilton Depression Rating Scale-2144; VI-SURIAS = Viennese Suicide Risk Assessment Scale.
All studies included defined suicidal behavior as suicide attempt and focused on lifetime history of SA.
Antipsychotic medication.
Antidepressant medication.
Anxiolytic medication.
Mood stabilizers (lithium, valproic acid, or carbamazepine).
Although eligible and included in the systematic review (Table 1), five studies were not included in the meta-analysis because: 1) precise means and standard deviations (SD) were not available in the paper35; 2) they did not report CTQ scores for BD patients who attempted suicide vs. those who did not, and they did not report CTQ sub-scores29; 3) only the most recent study of Janiri et al.28 was selected to prevent sample overlapping.34 Of note, the second study performed a logistic regression to explore the association between childhood maltreatment and each BD severity indicator (i.e., unemployment, more than five lifetime depressive episodes, more than five lifetime manic episodes, history of psychotic symptoms, one or more hospitalizations for BD, and suicide attempts). Although requested, data could not be obtained directly from Janiri et al. about either study. Finally, two studies that used CTQ were excluded, one for not evaluating suicide behavior45 and the other for not addressing patients with major depressive disorder.46
Data extraction and analyses
To extract data from the studies, a standardized form was used that included the authors, date of publication, study design, settings, study population, CM scale, definition of SB, and CTQ scores (mean and SD). CTQ scores and CTQ sub-scores were explored in at least three different studies.
Analyses were performed using Comprehensive Meta-Analyses version 2.0 and SPSS version 20. Two groups were compared: suicide attempters (patients with a history of suicide attempt) and patient controls (i.e., patients with no personal history of SB, but with a history of bipolar disorders).
We used a random-effects model to account for likely variations in true effect size between the included studies47 and pooled Hedges’ g effect sizes for the subjects’ CTQ scores.48 The obtained effect sizes are usually considered small if < 0.3, moderate if between 0.4-0.8, and large if > 0.8.49
Heterogeneity was assessed using the Q statistic and the I2 index.50 Values of p < 0.10 for the former and > 35% for the latter were deemed as indicative of study heterogeneity. Finally, we used funnel plots, Rosenthal’s fail-safe N51 and Egger’s regression intercept52 to test for the presence of publication bias.50
Ethics statement
This study was conducted in accordance with the Declaration of Helsinki and according to local and international standards.
Results
Systematic review
Table 1 summarizes the 13 studies28,29,31-40 ,53 included in the systematic literature review. The design of all identified studies was cross-sectional. The percentage of males ranged from 31.3 to 39.8%.
Overall, the main findings in patients suffering from BD were:
A higher rate of suicide attempts in those who experienced childhood abuse;
Higher total CTQ scores and higher CTQ sub-scores in suicide attempters compared to non-attempters.
Meta-analysis
A total of six studies were included, comprising 1,033 participants, of whom 379 were suicide attempters and 654 were patient controls.
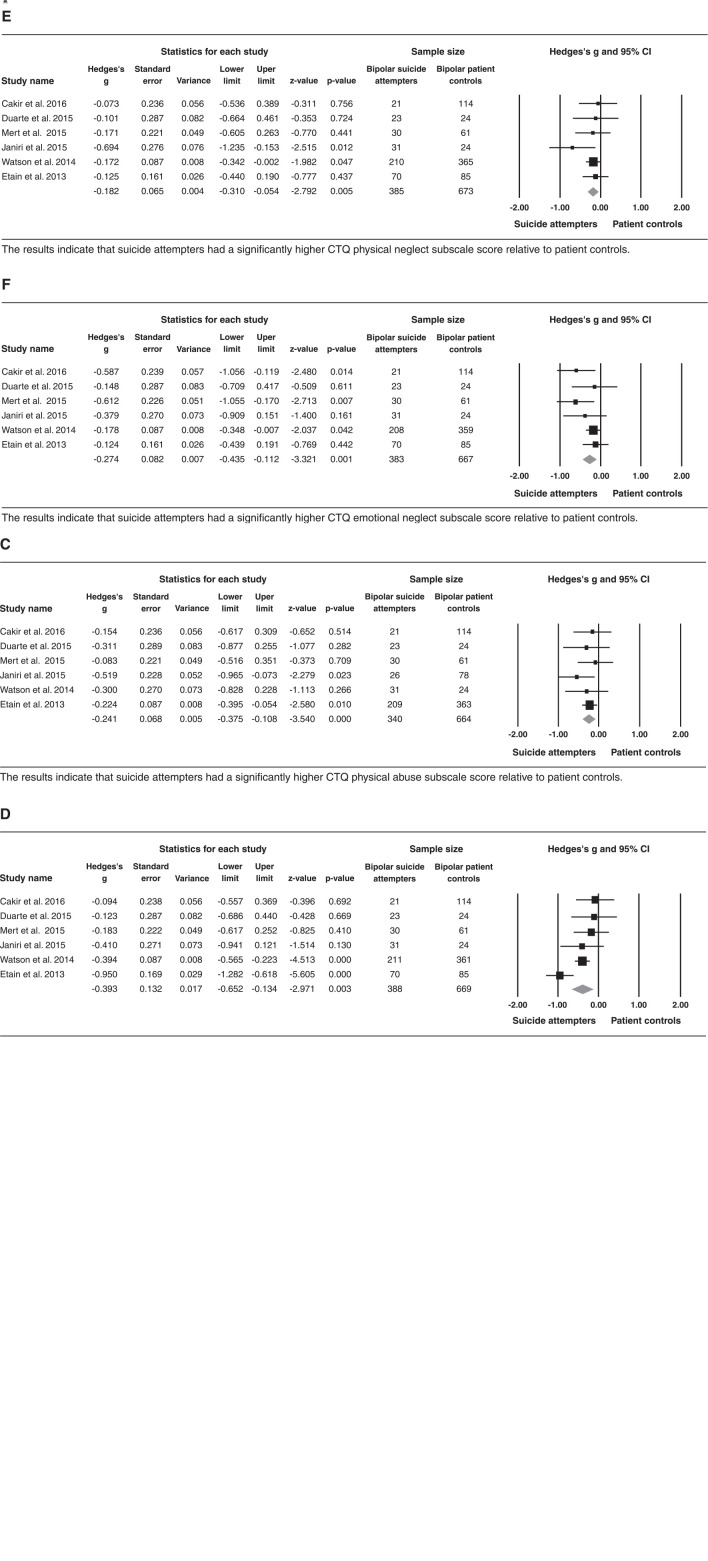
Suicide attempters had significantly higher CTQ total scores, sexual abuse CTQ sub-scores, physical abuse CTQ sub-scores, emotional abuse CTQ sub-scores, physical neglect CTQ sub-scores, and emotional neglect CTQ sub-scores than patient controls (Figure 2), all representing moderate to small effect sizes.
Figure 2. Comparison of the Childhood Trauma Questionnaire (CTQ) total score (A), CTQ sexual abuse sub-score (B), CTQ physical abuse sub-score (C), CTQ emotional abuse sub-score (D), CTQ physical neglect sub-score (E), and CTQ emotional neglect sub-score (F) between suicide attempters and patient controls in bipolar patients. 95%CI = 95% confidence interval.
Total CTQ between suicide attempters vs. patient controls
Suicide attempters had significantly higher CTQ total scores than patient controls, with a moderate effect size (Hedges’ g = -0.38, 95% confidence interval [95%CI] -0.52 to -0.24, z = -5.27, p < 0.001). The fail-safe N, i.e., the number of unpublished or missing null-findings that would be needed to render the results non-significant, was 35. Heterogeneity did not exceed that which was expected by chance (Q = 5.3; degrees of freedom [df] = 5; p = 0.37; I2 = 6.3), implying that the variance among the effect sizes was not greater than expected by sampling error. The funnel plots were reasonably symmetrical, suggesting a low risk of publication bias, and the more conservative Egger’s regression intercept suggested no publication bias (online-only supplementary Figure S1 (60.4KB, pdf) ). These results of funnel plots and Egger’s regression intercept were somewhat replicated in the CTQ subsets described below.
CTQ sexual abuse between suicide attempters vs. patient controls
Suicide attempters had significantly higher CTQ sexual abuse scores than patient controls, with a small effect size (Hedges’ g = -0.39, 95%CI -0.52 to -0.26, z = -5.9, p < 0.001). The fail-safe N was 45. Heterogeneity did not exceed that which was expected by chance (Q = 3.3; df = 5; p = 0.65; I2 = 0).
CTQ physical abuse between suicide attempters vs. patient controls
Suicide attempters had significantly higher CTQ physical abuse scores than patient controls, with a small effect size (Hedges’ g = -0.26, 95%CI -0.39 to -0.13, z = -4.0, p = 0.001). The fail-safe N was 15. Heterogeneity did not exceed that which was expected by chance (Q = 3.46; df = 5; p = 0.6; I2 = 0).
CTQ emotional abuse between suicide attempters vs. patient controls
Suicide attempters had significantly higher CTQ emotional abuse scores than patient controls, with a moderate effect size (Hedges’ g = -0.39, 95%CI -0.65 to -0.13, z = -2.88, p = 0.004). The fail-safe N was 11. Heterogeneity exceeded that which was expected by chance (Q = 14; df = 5; p = 0.016; I2 = 64.2) at p < 0.05, implying that the variance among the effect sizes was greater than that expected by sampling error. The study by Janiri et al.28 was likely responsible for the heterogeneity. After excluding this study, the heterogeneity disappeared and the main results remained significant.
CTQ physical neglect between suicide attempters vs. patient controls
Suicide attempters had significantly higher CTQ physical neglect scores than patient controls, with a small effect size (Hedges’ g = -0.18, 95%CI -0.31 to -0.05, z = -2.79, p = 0.005). The fail-safe N was 6. Heterogeneity did not exceed that which was expected by chance (Q = 3.87; df = 5; p = 0.56; I2 = 0).
CTQ emotional neglect between suicide attempters vs. patient controls
Suicide attempters had significantly higher CTQ emotional neglect scores than patient controls, with a small effect size (Hedges’ g = -0.27, 95%CI -0.43 to -0.11, z = -3.32, p = 0.001). The fail-safe N was 20. Heterogeneity did not exceed that which was expected by chance (Q = 2.23; df = 5; p = 0.28; I2 = 19.82).
Discussion
To the best of our knowledge, this is the first meta-analysis on the association between CTQ subscale scores and vulnerability to SB in BD (type 1, 2, and not otherwise specified). Overall, we found that, compared to patient controls, individuals with BD who attempted suicide had more severe CM with significantly higher CTQ total scores and significantly higher CTQ sub-scores. Our meta-analysis of six BD studies confirmed a significant but small to moderate effect size of higher CTQ total and subscale scores among suicide attempters than patient controls. Given the effect sizes, emotional abuse, sexual abuse and emotional neglect might contribute more to SB in BD in comparison to physical trauma (abuse or neglect).
These findings suggest that CM may be related to increased vulnerability to SB in bipolar patients, which is congruent with longitudinal studies that have highlighted the association between CM and SB in bipolar diagnosis.54-59 Furthermore, three recent reviews have addressed the impact of CM in clinical outcomes of BD patients5,13,60 and the neurobiological mechanisms of CM in mood disorders.12 Although the previously mentioned evidence, in conjunction with the results of the present review, point to an evident association between CM and SB in BD, we cannot affirm a causal mechanism or a cause-effect phenomenon.
The association between SB and CM is multifactorial and begins early in life. Parental figures, caregivers, and other close relatives provide social support during developmental stages, which is essential for healthy emotional regulation and stress resilience.61 The experience of repeated acts of maltreatment and negligence from such “protectors” signals an adverse environment that triggers epigenetic phenomena in key response systems, such as the serotonin transporter gene,12 the hypothalamic-pituitary-adrenal axis, and the serotonergic and sympathetic nervous systems,62,63 ultimately affecting the brain’s structure and function.64 For instance, the effect of childhood trauma on subcortical volumes in BD patients produces specific changes in grey matter volumes of the amygdala, hippocampus, and pre-frontal regions, which are key areas for emotional regulation and are involved in suicide attempts.12,30,65 In individuals who have experienced CM, BD emerges earlier,24 with greater severity,38 greater comorbidity,66 more suicidal behavior,40,53 and treatment resistance.5,40 Nevertheless, these negative outcomes are likely not unique to BD, since recent investigations have shown that CM is associated with an increased risk of SB in patients with schizophrenia,67 alcoholism,68 personality disorders,69 and substance abuse,70 as well in healthy volunteers.71-73
Among all subtypes of CM, we found that emotional abuse; sexual abuse and emotional neglect might have a greater contribution to SB in BD. These findings are in line with studies by Etain et al.,38,74 which show that emotional abuse is closely related to worse clinical outcomes in BD, including SB. In addition, sexual abuse seems to be a strong predictor for suicide.6,20 Although in this present study we found a lower magnitude of effect between physical trauma (abuse or neglect) and SB, this type of trauma does seem to have an important role in SB among individuals with BD.13 This could be mediated by drug abuse58,75 and gender effect, since physical abuse is more frequently reported in males and sexual abuse in females.76 Unfortunately, only a small number of studies have addressed emotional and physical neglect.38 Finally, the frequency and presence of more than one sub-type of trauma have a direct relationship with suicide attempts in BD.40
Regarding the impact of our findings on the severity of SB and, ultimately, on clinical practice, current evidence suggests that in BD patients, CM is associated with a higher number and earlier onset of suicide attempts, comorbid substance misuse, and overall worse bipolar outcomes, including more hospitalizations.5,6,12,13,17-20 Collectively, current evidence suggests that CM is a potential marker for identifying BD patients at high risk of unfavorable clinical outcomes and disease progression, and thereby vulnerable to SB.5 Thus, risk stratification in BD treatment could lead to the development of targeted treatment strategies.
The basis for valid stratification comes from the homogeneity of the collected data and the assessment of corresponding variables. Aside from the studies included in our systematic review, there is no uniformity for assessing CM and its potential association between BD and SB. Inherent challenges in assessing complex concepts like CM have resulted in a variety of heterogeneous definitions (i.e., childhood abuse, trauma, adversities, and early stress) and an even greater variety of instruments – over 40.77 Thus, to minimize discrepancies, the use of similar clinical interviews and validated questionnaires should be encouraged. Although the CTQ is not clearly superior to other available tools, its widespread use in research and its reliability (and validity) make it a promising instrument for professionals in research practice.70 However, as a drawback, the CTQ does not provide data on the timing of the trauma during neurodevelopment, which has been suggested to be of particular importance in first psychotic episode, for example.78
This systematic review and meta-analysis has some limitations that should be considered when interpreting the results. The most common limitation in meta-analyses is the combination of heterogeneous studies and the inclusion of poor-quality trials, consequently increasing the risk of publication bias. Nonetheless, these concerns were addressed in the present study by assessing both publication bias and heterogeneity, as well as by the use of a standard questionnaire (the CTQ), which increased internal validity, generalizability, and significantly reduced heterogeneity. The present meta-analysis included six studies, therefore potentially overcoming the drawback of the small number of studies used in some analyses, which inadequately increases the effect size.79 The studies did not differentiate CTQ scores across subsets of the population, such as those with low vs. high-lethality suicide attempts and/or those with violent vs. non-violent suicide attempts. Due to the lack of data, we could not explore the effect of CM on specific types of BD (e.g., BD type 1). Since CM was evaluated retrospectively among the studies included in this systematic review and meta-analysis, inferences on cause and effect cannot be made, and memory bias must be considered. Finally, we ruled out the effects of several variables (e.g., age and the severity of depressive and mania symptoms at the time of assessment), although the association between CM and SB in bipolar populations should be further investigated.
In conclusion, our findings suggest that CM severity and subtypes (especially emotional abuse, sexual abuse, and emotional neglect) could contribute to the development of SB in individuals with BD. These findings also highlight the importance of recognizing maltreatment as an etiological risk factor that must be evaluated in psychiatric consultations, particularly with BD patients. This is crucial to developing science-based preventive psychiatry and designing effective therapeutic regimens.
Disclosure
The authors report no conflicts of interest.
Footnotes
How to cite this article: Duarte D, Belzeaux R, Etain B, Greenway KT, Rancourt E, Correa H, et al. Childhood-maltreatment subtypes in bipolar patients with suicidal behavior: systematic review and meta-analysis. Braz J Psychiatry. 2020;42:558-567. http://dx.doi.org/10.1590/1516-4446-2019-0592
Corrigendum: http://dx.doi.org/10.1590/1516-4446-2020-0015
The authors of the article entitled “Childhood-maltreatment subtypes in bipolar patients with suicidal behavior: systematic review and meta-analysis” (http://dx.doi.org/10.1590/1516-4446-2019-0592), published in the Brazilian Journal of Psychiatry in ahead of print mode in early June 2020, identified some errors in the article.
First, one coauthor was inadvertently omitted from the author byline, namely, “Kyle T. Greenway”, which should be the fourth author. Below we reproduce the final, corrected, author byline, with the name of the new author underlined:
Dante Duarte,1,2 Raoul Belzeaux,3,4 Bruno Etain,5 Kyle T. Greenway,3 Emilie Rancourt,3 Humberto Correa,1 Gustavo Turecki,3 Stéphane Richard-Devantoy 3,6
As a result, the suggested citation should be as follows:
How to cite this article: Duarte D, Belzeaux R, Etain B, Greenway KT, Rancourt E, Correa H, et al. Childhood-maltreatment subtypes in bipolar patients with suicidal behavior: systematic review and meta-analysis. Braz J Psychiatry. 2020;42:558-567. http://dx.doi.org/10.1590/1516-4446-2019-0592.
Second, 2 errors in the abstract related to the number of articles included in the analysis. In the Methods section of the abstract, a total of “nine” abstracts is mentioned, and in the Results section of the abstract, “12.” These two numbers should read “13,” which was the final, correct number of studies analyzed. Also, in the Results section of the abstract, “In the literature review” was replaced with “In the systematic review.” Below we reproduce the complete corrected version of the abstract, with the corrections underlined:
Objective: Patients with bipolar disorders have a high risk of suicidal behavior. Childhood maltreatment is a well-established risk factor for suicidal behavior. The objective of this study was to examine the association between childhood-maltreatment subtypes and vulnerability to suicide attempts in bipolar disorder using the Childhood Trauma Questionnaire (CTQ).
Methods: A literature review was performed using the MEDLINE, Embase, and PsycINFO databases. Thirteen studies met the selection criteria. In the meta-analysis, the Childhood Trauma Questionnaire (CTQ) was used to assess a wide range of childhood maltreatment subtypes, which were analyzed by using a random-effects model to account for the likely variations of true effect sizes between the included studies.
Results: In the systematic review, 13 studies met the selection criteria. The CTQ was selected for the meta-analysis to increase the homogeneity of assessment and to encompass a wide range of childhood-maltreatment subtypes. The data were analyzed using a random-effects model. Compared to bipolar non-attempters, bipolar suicide attempters had experienced childhood maltreatment with a significantly higher frequency and had higher total CTQ scores (Hedges’ g = -0.38, 95%CI -0.52 to -0.24, z = -5.27, p < 0.001) and CTQ sub-scores (sexual abuse: g = -0.39, 95%CI -0.52 to -0.26, z = -5.97; physical abuse: g = -0.26, 95%CI -0.39 to -0.13, z = -4.00; emotional abuse: g = -0.39, 95%CI -0.65 to -0.13, z = -2.97; physical neglect: g = -0.18, 95%CI -0.31 to -0.05, z = -2.79; emotional neglect: g = -0.27, 95%CI -0.43 to -0.11, z = -3.32).
Conclusions: Childhood maltreatment, as assessed by the CTQ, may contribute to an increased risk of suicidal behavior among people with bipolar disorders. Recognizing maltreatment as an etiological risk factor is a crucial step toward furthering science-based preventive psychiatry.
Another error was identified in the fifth paragraph of the Methods section, relating to the total number of articles selected for inclusion in the meta-analysis. In this paragraph, it is mentioned that of the 13 studies identified in the systematic review, a total of three articles were not included in the meta-analysis; however, “three” should read “five,” reflecting the correct number of articles excluded from the meta-analysis. Below we reproduce the full corrected paragraph, with the correct number underlined:
Although eligible and included in the systematic review (Table 1), five studies were not included in the meta-analysis because: 1) precise means and standard deviations (SD) were not available in the paper35; 2) they did not report CTQ scores for BD patients who attempted suicide vs. those who did not, and they did not report CTQ sub-scores29; 3) only the most recent study of Janiri et al.28 was selected to prevent sample overlapping.34 Of note, the second study performed a logistic regression to explore the association between childhood maltreatment and each BD severity indicator (i.e., unemployment, more than five lifetime depressive episodes, more than five lifetime manic episodes, history of psychotic symptoms, one or more hospitalizations for BD, and suicide attempts). Although requested, data could not be obtained directly from Janiri et al. about either study. Finally, two studies that used CTQ were excluded, one for not evaluating suicide behavior45 and the other for not addressing patients with major depressive disorder.46
Finally, two adjustments were made in the Discussion section of the paper, as described below.
1) Towards the end of the first paragraph, the sentence “Given the effect sizes, emotional abuse, sexual abuse and emotional neglect might contribute more to SB in BD, whereas physical trauma (abuse or neglect) might contribute less” should read “Given the effect sizes, emotional abuse, sexual abuse and emotional neglect might contribute more to SB in BD in comparison to physical trauma (abuse or neglect).
2) In the sixth paragraph of the Discussion, the last word of the second sentence needs to be corrected from “CB” to “SB”: “Aside from the studies included in our systematic review, there is no uniformity for assessing CM and its potential association between BD and SB.”
References
- 1.Novick DM, Swartz HA, Frank E. Suicide attempts in bipolar I and bipolar II disorder: a review and meta-analysis of the evidence. Bipolar Disord. 2010;12:1–9. doi: 10.1111/j.1399-5618.2009.00786.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turecki G, Ernst C, Jollant F, Labonte B, Mechawar N. The neurodevelopmental origins of suicidal behavior. Trends Neurosci. 2012;35:14–23. doi: 10.1016/j.tins.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 3.Worl Health Organization (WHO) Global status report on violence prevention [Internet] 2014. [[cited 2020 Apr 20]]. www.who.int/violence_injury_prevention/violence/status_report/2014/report/report/en/
- 4.Post RM, Altshuler L, Leverich G, Nolen W, Kupka R, Grunze H, et al. More stressors prior to and during the course of bipolar illness in patients from the United States compared with the Netherlands and Germany. Psychiatry Res. 2013;210:880–6. doi: 10.1016/j.psychres.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 5.Agnew-Blais J, Danese A. Childhood maltreatment and unfavourable clinical outcomes in bipolar disorder: a systematic review and meta-analysis. Lancet Psychiatry. 2016;3:342–9. doi: 10.1016/S2215-0366(15)00544-1. [DOI] [PubMed] [Google Scholar]
- 6.Daruy-Filho L, Brietzke E, Lafer B, Grassi-Oliveira R. Childhood maltreatment and clinical outcomes of bipolar disorder. Acta Psychiatr Scand. 2011;124:427–34. doi: 10.1111/j.1600-0447.2011.01756.x. [DOI] [PubMed] [Google Scholar]
- 7.De Bellis MD. Developmental traumatology: the psychobiological development of maltreated children and its implications for research, treatment, and policy. Dev Psychopathol. 2001;13:539–64. doi: 10.1017/s0954579401003078. [DOI] [PubMed] [Google Scholar]
- 8.Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012;106:29–39. doi: 10.1016/j.physbeh.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 9.Teicher MH, Samson JA. Childhood maltreatment and psychopathology: a case for ecophenotypic variants as clinically and neurobiologically distinct subtypes. Am J Psychiatry. 2013;170:1114–33. doi: 10.1176/appi.ajp.2013.12070957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012;106:29–39. doi: 10.1016/j.physbeh.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 11.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–58. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 12.Jaworska-Andryszewska P, Rybakowski JK. Childhood trauma in mood disorders: neurobiological mechanisms and implications for treatment. Pharmacol Rep. 2018;71:112–20. doi: 10.1016/j.pharep.2018.10.004. [DOI] [PubMed] [Google Scholar]
- 13.Aas M, Henry C, Andreassen OA, Bellivier F, Melle I, Etain B. The role of childhood trauma in bipolar disorders. Int J Bipolar Disord. 2016;4:2. doi: 10.1186/s40345-015-0042-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151:1132–6. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- 15.Grassi-Oliveira R, Stein LM, Pezzi JC. Tradução e validação de conteúdo da versão em português do Childhood Trauma Questionnaire. Rev Saude Publica. 2006;40:249–55. doi: 10.1590/s0034-89102006000200010. [DOI] [PubMed] [Google Scholar]
- 16.MacDonald K, Thomas ML, Sciolla AF, Schneider B, Pappas K, Bleijenberg G, et al. Minimization of childhood maltreatment is common and consequential: results from a large, multinational sample using the childhood trauma questionnaire. PloS One. 2016;11:e0146058. doi: 10.1371/journal.pone.0146058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alloy LB, Abramson LY, Urosevic S, Walshaw PD, Nusslock R, Neeren AM. The psychosocial context of bipolar disorder: environmental, cognitive, and developmental risk factors. Clin Psychol Rev. 2005;25:1043–75. doi: 10.1016/j.cpr.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 18.Alloy LB, Abramson LY, Smith JM, Gibb BE, Neeren AM. Role of parenting and maltreatment histories in unipolar and bipolar mood disorders: mediation by cognitive vulnerability to depression. Clin Child Fam Psychol Rev. 2006;9:23–64. doi: 10.1007/s10567-006-0002-4. [DOI] [PubMed] [Google Scholar]
- 19.Etain B, Henry C, Bellivier F, Mathieu F, Leboyer M. Beyond genetics: childhood affective trauma in bipolar disorder. Bipolar Disord. 2008;10:867–76. doi: 10.1111/j.1399-5618.2008.00635.x. [DOI] [PubMed] [Google Scholar]
- 20.Fisher HL, Hosang GM. Childhood maltreatment and bipolar disorder: a critical review of the evidence. Mind Brain. 2010;1:75–85. [Google Scholar]
- 21.Heany SJ, Groenewold NA, Uhlmann A, Dalvie S, Stein DJ, Brooks SJ. The neural correlates of childhood trauma questionnaire scores in adults: a meta-analysis and review of functional magnetic resonance imaging studies. Dev Psychopathol. 2018;30:1475–85. doi: 10.1017/S0954579417001717. [DOI] [PubMed] [Google Scholar]
- 22.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–9. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 23.Mann JJ. Neurobiology of suicidal behaviour. Nat Rev Neurosci. 2003;4:819–28. doi: 10.1038/nrn1220. [DOI] [PubMed] [Google Scholar]
- 24.Leverich GS, McElroy SL, Suppes T, Keck PE, Jr, Denicoff KD, Nolen WA, et al. Early physical and sexual abuse associated with an adverse course of bipolar illness. Biol Psychiatry. 2002;51:288–97. doi: 10.1016/s0006-3223(01)01239-2. [DOI] [PubMed] [Google Scholar]
- 25.McIntyre RS, Soczynska JK, Mancini D, Lam C, Woldeyohannes HO, Moon S, et al. The relationship between childhood abuse and suicidality in adult bipolar disorder. Violence Vict. 2008;23:361–72. doi: 10.1891/0886-6708.23.3.361. [DOI] [PubMed] [Google Scholar]
- 26.Alvarez MJ, Roura P, Osés A, Foguet Q, Solà J, Arrufat FX. Prevalence and clinical impact of childhood trauma in patients with severe mental disorders. J Nerv Ment Dis. 2011;199:156–61. doi: 10.1097/NMD.0b013e31820c751c. [DOI] [PubMed] [Google Scholar]
- 27.Petticrew M, Roberts H. Systematic reviews in the social sciences: a practical guide. Oxford: Blackwell; 2006. [Google Scholar]
- 28.Janiri D, De Rossi P, Kotzalidis GD, Girardi P, Koukopoulos AE, Reginaldi D, et al. Psychopathological characteristics and adverse childhood events are differentially associated with suicidal ideation and suicidal acts in mood disorders. Eur Psychiatry. 2018;53:31–6. doi: 10.1016/j.eurpsy.2018.05.009. [DOI] [PubMed] [Google Scholar]
- 29.Pavlova B, Perroud N, Cordera P, Uher R, Alda M, Dayer A, et al. Anxiety disorders and childhood maltreatment as predictors of outcome in bipolar disorder. J Affect Disord. 2018;225:337–41. doi: 10.1016/j.jad.2017.08.048. [DOI] [PubMed] [Google Scholar]
- 30.Duarte DG, Neves Me C, Albuquerque MR, de Souza-Duran FL, Busatto G, Corrêa H. Gray matter brain volumes in childhood-maltreated patients with bipolar disorder type I: a voxel-based morphometric study. J Affect Disord. 2016;197:74–80. doi: 10.1016/j.jad.2016.02.068. [DOI] [PubMed] [Google Scholar]
- 31.Cakir S, Tasdelen Durak R, Ozyildirim I, Ince E, Sar V. Childhood trauma and treatment outcome in bipolar disorder. J Trauma Dissociation. 2016;17:397–409. doi: 10.1080/15299732.2015.1132489. [DOI] [PubMed] [Google Scholar]
- 32.Bernegger A, Kienesberger K, Carlberg L, Swoboda P, Ludwig B, Koller R, et al. Influence of sex on suicidal phenotypes in affective disorder patients with traumatic childhood experiences. PloS One. 2015;10:e0137763. doi: 10.1371/journal.pone.0137763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mert DG, Kelleci M, Mizrak A, Semiz M, Demir MO. Factors associated with suicide attempts in patients with bipolar disorder type I. Psychiatr Danub. 2015;27:236–41. [PubMed] [Google Scholar]
- 34.Janiri D, Sani G, Danese E, Simonetti A, Ambrosi E, Angeletti G, et al. Childhood traumatic experiences of patients with bipolar disorder type I and type II. J Affect Disord. 2015;175:92–7. doi: 10.1016/j.jad.2014.12.055. [DOI] [PubMed] [Google Scholar]
- 35.Li XB, Liu JT, Zhu XZ, Zhang L, Tang YL, Wang CY. Childhood trauma associates with clinical features of bipolar disorder in a sample of Chinese patients. J Affect Disord. 2014;168:58–63. doi: 10.1016/j.jad.2014.06.017. [DOI] [PubMed] [Google Scholar]
- 36.Erten E, Funda Uney A, Saatcioglu O, Ozdemir A, Fistikci N, Cakmak D. Effects of childhood trauma and clinical features on determining quality of life in patients with bipolar I disorder. J Affect Disord. 2014;162:107–13. doi: 10.1016/j.jad.2014.03.046. [DOI] [PubMed] [Google Scholar]
- 37.Watson S, Gallagher P, Dougall D, Porter R, Moncrieff J, Ferrier IN, et al. Childhood trauma in bipolar disorder. Aust N Z J Psychiatry. 2014;48:564–70. doi: 10.1177/0004867413516681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Etain B, Aas M, Andreassen OA, Lorentzen S, Dieset I, Gard S, et al. Childhood trauma is associated with severe clinical characteristics of bipolar disorders. J Clin Psychiatry. 2013;74:991–8. doi: 10.4088/JCP.13m08353. [DOI] [PubMed] [Google Scholar]
- 39.Pompili M, Iliceto P, Innamorati M, Rihmer Z, Lester D, Akiskal HS, et al. Suicide risk and personality traits in physically and/or sexually abused acute psychiatric inpatients: a preliminary study. Psychol Rep. 2009;105:554–68. doi: 10.2466/PR0.105.2.554-568. [DOI] [PubMed] [Google Scholar]
- 40.Garno JL, Goldberg JF, Ramirez PM, Ritzler BA. Impact of childhood abuse on the clinical course of bipolar disorder. Br J Psychiatry. 2005;186:121–5. doi: 10.1192/bjp.186.2.121. [DOI] [PubMed] [Google Scholar]
- 41.Hamilton M. Standardised assessment and recording of depressive symptoms. Psychiatr Neurol Neurochir. 1969;72:201–5. [PubMed] [Google Scholar]
- 42.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 43.Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment. 2001;8:443–54. doi: 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- 44.Williams JB. A structured interview guide for the Hamilton Depression Rating Scale. Arch Gen Psychiatry. 1988;45:742–7. doi: 10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]
- 45.Innamorati M, Erbuto D, Venturini P, Fagioli F, Ricci F, Lester D, et al. Factorial validity of the Childhood Trauma Questionnaire in Italian psychiatric patients. Psychiatry Res. 2016;245:297–302. doi: 10.1016/j.psychres.2016.08.044. [DOI] [PubMed] [Google Scholar]
- 46.Pompili M, Innamorati M, Lamis DA, Erbuto D, Venturini P, Ricci F, et al. The associations among childhood maltreatment, “male depression” and suicide risk in psychiatric patients. Psychiatry Res. 2014;220:571–8. doi: 10.1016/j.psychres.2014.07.056. [DOI] [PubMed] [Google Scholar]
- 47.Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342:d549. doi: 10.1136/bmj.d549. [DOI] [PubMed] [Google Scholar]
- 48.Hedges LV, Olkin I. Statistical methods for meta-analysis. London: Academic Press; 1985. [Google Scholar]
- 49.Egger M, Davey Smith G, Altman D. Systematic reviews in health care: meta-analysis in context. London: BMJ Publishing Group; 2001. [Google Scholar]
- 50.Cooper H, Hedges LV, Valentine JC. The handbook of research synthesis and meta-analysis. New York: Russell Sage Foundation Publications; 2009. [Google Scholar]
- 51.Rosenthal R. The file drawer problem and tolerance for null results. Psychol Bull. 1979;86:638–41. [Google Scholar]
- 52.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Duarte DG, Neves Mde C, Albuquerque MR, Neves FS, Correa H. Sexual abuse and suicide attempt in bipolar type I patients. Braz J Psychiatry. 2015;37:180–2. doi: 10.1590/1516-4446-2014-1624. [DOI] [PubMed] [Google Scholar]
- 54.Ernst C, Angst J, Foldenyi M. The Zurich Study. XVII. The Zurich Study. XVII. Sexual abuse in childhood. Frequency and relevance for adult morbidity data of a longitudinal epidemiological study. Eur Arch Psychiatry Clin Neurosci. 1993;242:293–300. doi: 10.1007/BF02190389. [DOI] [PubMed] [Google Scholar]
- 55.Leverich GS, Altshuler LL, Frye MA, Suppes T, Keck PE, Jr, McElroy SL, et al. Factors associated with suicide attempts in 648 patients with bipolar disorder in the Stanley Foundation Bipolar Network. J Clin Psychiatry. 2003;64:506–15. doi: 10.4088/jcp.v64n0503. [DOI] [PubMed] [Google Scholar]
- 56.Brezo J, Paris J, Vitaro F, Hebert M, Tremblay RE, Turecki G. Predicting suicide attempts in young adults with histories of childhood abuse. Br J Psychiatry. 2008;193:134–9. doi: 10.1192/bjp.bp.107.037994. [DOI] [PubMed] [Google Scholar]
- 57.Enns MW, Cox BJ, Afifi TO, De Graaf R, Ten Have M, Sareen J. Childhood adversities and risk for suicidal ideation and attempts: a longitudinal population-based study. Psychol Med. 2006;36:1769–78. doi: 10.1017/S0033291706008646. [DOI] [PubMed] [Google Scholar]
- 58.Fergusson DM, Boden JM, Horwood LJ. Exposure to childhood sexual and physical abuse and adjustment in early adulthood. Child Abuse Negl. 2008;32:607–19. doi: 10.1016/j.chiabu.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 59.Sugaya L, Hasin DS, Olfson M, Lin KH, Grant BF, Blanco C. Child physical abuse and adult mental health: a national study. J Trauma Stress. 2012;25:384–92. doi: 10.1002/jts.21719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Maniglio R. Prevalence of child sexual abuse among adults and youths with bipolar disorder: a systematic review. Clin Psychol Rev. 2013;33:561–73. doi: 10.1016/j.cpr.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 61.Labonte B, Turecki G. The epigenetics of suicide: explaining the biological effects of early life environmental adversity. Arch Suicide Res. 2010;14:291–310. doi: 10.1080/13811118.2010.524025. [DOI] [PubMed] [Google Scholar]
- 62.Bremner JD. Long-term effects of childhood abuse on brain and neurobiology. Child Adolesc Psychiatr Clin N Am. 2003;12:271–92. doi: 10.1016/s1056-4993(02)00098-6. [DOI] [PubMed] [Google Scholar]
- 63.Watts-English T, Fortson BL, Gibler N, Hooper SR, De Bellis MD. The psychobiology of maltreatment in childhood. J Soc Issues. 2006;62:717–36. [Google Scholar]
- 64.Pechtel P, Pizzagalli DA. Effects of early life stress on cognitive and affective function: an integrated review of human literature. Psychopharmacology (Berl) 2011;214:55–70. doi: 10.1007/s00213-010-2009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Janiri D, Sani G, Rossi P, Piras F, Iorio M, Banaj N, et al. Amygdala and hippocampus volumes are differently affected by childhood trauma in patients with bipolar disorders and healthy controls. Bipolar Disord. 2017;19:353–62. doi: 10.1111/bdi.12516. [DOI] [PubMed] [Google Scholar]
- 66.Leverich GS, Post RM. Course of bipolar illness after history of childhood trauma. Lancet. 2006;367:1040–2. doi: 10.1016/S0140-6736(06)68450-X. [DOI] [PubMed] [Google Scholar]
- 67.Roy A. Reported childhood trauma and suicide attempts in schizophrenic patients. Suicide Life Threat Behav. 2005;35:690–3. doi: 10.1521/suli.2005.35.6.690. [DOI] [PubMed] [Google Scholar]
- 68.Roy A. Distal risk factors for suicidal behavior in alcoholics: replications and new findings. J Affect Disord. 2003;77:267–71. doi: 10.1016/s0165-0327(02)00173-8. [DOI] [PubMed] [Google Scholar]
- 69.Bierer LM, Yehuda R, Schmeidler J, Mitropoulou V, New AS, Silverman JM, et al. Abuse and neglect in childhood: relationship to personality disorder diagnoses. CNS Spectr. 2003;8:737–54. doi: 10.1017/s1092852900019118. [DOI] [PubMed] [Google Scholar]
- 70.Roy A. Relationship of childhood trauma to age of first suicide attempt and number of attempts in substance dependent patients. Acta Psychiatr Scand. 2004;109:121–5. doi: 10.1046/j.0001-690x.2003.00234.x. [DOI] [PubMed] [Google Scholar]
- 71.Brown J, Cohen P, Johnson JG, Smailes EM. Childhood abuse and neglect: specificity of effects on adolescent and young adult depression and suicidality. J Am Acad Child Adolesc Psychiatry. 1999;38:1490–6. doi: 10.1097/00004583-199912000-00009. [DOI] [PubMed] [Google Scholar]
- 72.Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the adverse childhood experiences study. JAMA. 2001;286:3089–96. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- 73.Nelson EC, Heath AC, Madden PA, Cooper ML, Dinwiddie SH, Bucholz KK, et al. Association between self-reported childhood sexual abuse and adverse psychosocial outcomes: results from a twin study. Arch Gen Psychiatry. 2002;59:139–45. doi: 10.1001/archpsyc.59.2.139. [DOI] [PubMed] [Google Scholar]
- 74.Etain B, Lajnef M, Henry C, Aubin V, Azorin JM, Bellivier F, et al. Childhood trauma, dimensions of psychopathology and the clinical expression of bipolar disorders: a pathway analysis. J Psychiatr Res. 2017;95:37–45. doi: 10.1016/j.jpsychires.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 75.Aas M, Etain B, Bellivier F, Henry C, Lagerberg T, Ringen A, et al. Additive effects of childhood abuse and cannabis abuse on clinical expressions of bipolar disorders. Psychol Med. 2014;44:1653–62. doi: 10.1017/S0033291713002316. [DOI] [PubMed] [Google Scholar]
- 76.Fisher H, Morgan C, Dazzan P, Craig TK, Morgan K, Hutchinson G, et al. Gender differences in the association between childhood abuse and psychosis. Br J Psychiatry. 2009;194:319–25. doi: 10.1192/bjp.bp.107.047985. [DOI] [PubMed] [Google Scholar]
- 77.Roy CA, Perry JC. Instruments for the assessment of childhood trauma in adults. J Nerv Ment Dis. 2004;192:343–51. doi: 10.1097/01.nmd.0000126701.23121.fa. [DOI] [PubMed] [Google Scholar]
- 78.Alameda L, Ferrari C, Baumann PS, Gholam-Rezaee M, Do KQ, Conus P. Childhood sexual and physical abuse: age at exposure modulates impact on functional outcome in early psychosis patients. Psychol Med. 2015;45:2727–36. doi: 10.1017/S0033291715000690. [DOI] [PubMed] [Google Scholar]
- 79.Button KS, Ioannidis JP, Mokrysz C, Nosek BA, Flint J, Robinson ES, et al. Power failure: why small sample size undermines the reliability of neuroscience. Nat Rev Neurosci. 2013;14:365–76. doi: 10.1038/nrn3475. [DOI] [PubMed] [Google Scholar]