Abstract
Disparities in sleep health are important but underrecognized contributors to health disparities. Understanding the factors contributing to sleep heath disparities and developing effective interventions are critical to improving all aspects of heath. Sleep heath disparities are impacted by socioeconomic status, racism, discrimination, neighborhood segregation, geography, social patterns, and access to health care as well as by cultural beliefs, necessitating a cultural appropriateness component in any intervention devised for reducing sleep health disparities. Pediatric sleep disparities require innovative and urgent intervention to establish a foundation of lifelong healthy sleep. Tapping the vast potential of technology in improving sleep health access may be an underutilized tool to reduce sleep heath disparities. Identifying, implementing, replicating, and disseminating successful interventions to address sleep disparities have the potential to reduce overall disparities in health and quality of life.
Key Words: bioinformatics, health disparities, sleep, vulnerable population
Abbreviations: AHI, apnea-hypopnea index; HSAT, home sleep apnea testing; PAP, positive airway pressure; PCP, primary care provider; SES, socioeconomic status
Sleep disparities have been recognized as an important contributor to disparities in overall health in socially disadvantaged groups.1 Not only understanding the causes of sleep health disparities and their impact on non-white and economically disadvantaged populations, but also identifying and testing potential solutions, and disseminating successful interventions that may improve sleep health and overall wellness, are critical.
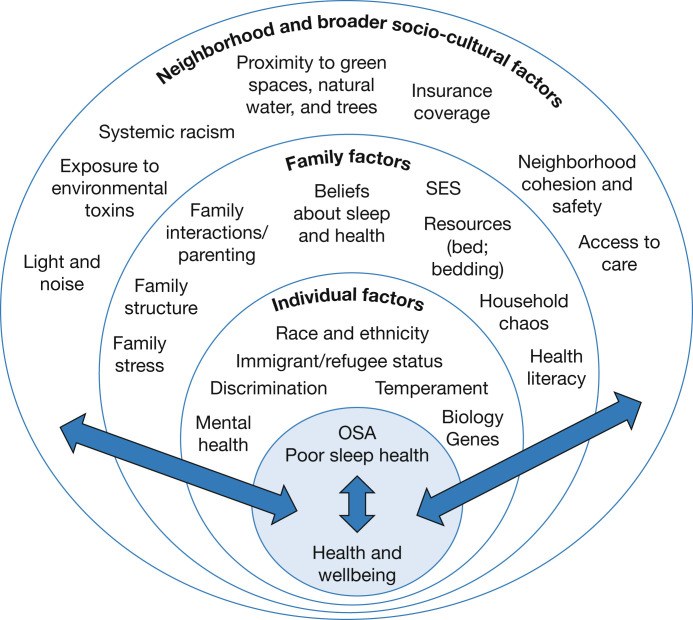
The sleep state is highly sensitive to external threats, because a sleeping individual is vulnerable. Thus, the environment surrounding the sleeping space affects sleep. In this review, we evaluate sleep heath disparities through a socio-ecological lens, which starts with the individual, to family and other direct interpersonal relationships, broadening to neighborhood and community influences, and public policy (Fig 1 ). The socio-ecological model incorporates these multiple levels, but it assumes that these levels interact with one another, and that together they exert a cumulative impact on health.2 Examining the multiple physical, social, cultural, and environment factors through the social-ecological lens allows us to understand sleep disparities within a broader context.
Figure 1.
Social-ecological factors contributing to sleep disparities at multiple levels: the individual level, the family level, and the broader neighborhood and socio-cultural context. As represented by the lateral blue arrows, factors at each level likely interact over time to contribute to sleep disparities.
We focus here on three main areas of sleep disparities: (1) disparities in insufficient sleep and sleep quality; (2) disparities in sleep apnea; and (3) disparities in pediatric sleep. Healthy sleep can be defined as of an optimal duration, high efficiency, fully restorative, well synchronized in timing with one’s biological rhythms, and highly regular in pattern over multiple days.3 In this review, we focus on two domains of sleep health that have been frequently examined in the extant literature: sleep duration (total 24-hour sleep) and sleep quality (subjective perception of sleep). We discuss potential approaches to address sleep disparities within each topic area, including gaps in knowledge/research potential (Table 1 ). Disparities in other areas of sleep may exist, including insomnia, restless leg syndrome, circadian rhythm, and shift work disorders; but these are beyond the scope of the current review.
Table 1.
Potential Solutions for Addressing Sleep Health Disparities
| Ecological Level | Factor Contributing to Sleep Disparities | Proposed Solutions |
|---|---|---|
| Individual and family levels | Language and cultural barriers | Language-based educational modules, culturally appropriate materials |
| Lack of sleep-specific resources | Provide beds and bedding, quiet, dark sleeping space for institutionalized and homeless individuals | |
| Beliefs about sleep and heath Health literacy |
Targeted sleep promotion education in clinics, daycares, schools, lay press, social media Mobile phone apps to promote healthy sleep |
|
| Perceived discrimination | Integrated cultural appropriateness and empowerment | |
| Racism and bias | Anti-racism education in medical training | |
| Neighborhood and broader sociocultural factors | Proximity to green spaces Light and noise Neighborhood cohesion and safety |
Improved urban planning
|
| Access to care: remote and rural locations, transportation barriers | Home sleep apnea testing (HSAT), Auto-PAP therapy, and remote PAP monitoring Electronic prescribing Telemedicine
Proactive screening of high-risk patients |
|
| Segregation and redlining | Revision of zoning laws and mortgage lending practices | |
| Access to care: insurance coverage for sleep-related services | Advocacy (position statements, policy work) |
Auto-PAP therapy = auto-adjusting positive airway pressure therapy.
Disparities in Sleep Duration and Sleep Quality
Epidemiological studies consistently document shorter sleep duration, poorer quality, delayed onset, and more fragmented sleep among those with low socioeconomic status (SES) and among Black, Latinx, Asian, and Indigenous nonwhite adults.4 Black adults in the United States report consistently shorter sleep durations across studies compared with white adults,5 and greater levels of daytime sleepiness.6 Hispanic and low-SES individuals additionally report shorter sleep durations.7 National Health and Nutrition Examination Survey data demonstrate higher likelhood of short sleep in nonwhite and low-SES participants.8 We attempt to understand the socio-ecological factors contributing to this observed difference in prevalence of sleep insuffiency, delayed sleep, and poorer quality sleep by race/ethnicity and SES.
Neighborhood and ecological features impact sleep, and thus residential segregation by race and ethnicity can contribute to sleep health disparities. Despite the Fair Housing Act of 1968, residential areas in the United States remain highly segregated. Nonwhite populations reside disproportionally in disadvantaged neighborhoods because of historical housing policies, so called “redlining.”9 These neighborhoods often have high rates of poverty, unemployment, and low rates of home ownership and college education. Living in disadvantaged neighborhoods (with composite low socioeconomic status measures) has been associated with insomnia symptoms (difficulties in initiating or maintaining sleep), and longer wake after sleep onset.10 Disparities in sleep may be even more severe in those lacking secure and stable places to sleep, such as refugees and homeless individuals, but few studies have examined sleep in these populations. In a convenience sample of homeless adults,11 sleep problems were highly prevalent and associated with high levels of self-reported distress related to living in urban areas.
Residential segregation also concentrates environmental features that are deleterious to sleep health (eg, inopportune light and noise, higher intra-urban heat, and poorer air quality) in disadvantaged communities. Neighborhood ambient features such as loud noises, bright lights, caustic air quality, and radiant heat may impair sleep. Bright street lights can contribute to circadian phase delay and inhibit melatonin secretion.12 Exposure to air pollution has been associated with sleep apnea; for example, in one study a 5-μg/m3 increase in annual particulate matter exposure was associated with 60% greater odds of sleep apnea.13 Urban areas, in historically “redlined” areas with dominant communities of color, have higher surface temperatures than those that are predominantly white with above-average incomes, in more “leafy” neighborhoods with greater tree canopy.14 Higher temperature and humidity negatively affect sleep, with more wakefulness and less rapid eye movement and slow wave sleep in those exposed to humid heat.15 The environmental and social features may modify sleep habits and contribute to poorer sleep quality, more sleep fragmentation, and less sleep opportunity. Those who reside in urban areas with dense intersections and populations are more likely to have shorter sleep duration.16 Historically disadvantaged groups, such as Blacks, immigrants, and those in poverty are more likely to live in neighborhoods with increased crowding, noise, light, and air pollution,17 which likely contributes to a greater burden of poor sleep health.1 , 10
Systemic racism has additional effects on sleep health through the consequences of psychosocial trauma, discrimination and micro-aggressions, and stereotype threats on sleep.18 These experiences can serve as external threats and impair the ability to be vulnerable in sleep. Active discrimination against Hispanics at both a structural level and at an individual, everyday level (so called micro-aggressions) increase stress, which adversely impacts sleep.19 Experiencing discrimination has been associated with shorter sleep duration, experienced much more often by Black women than White women in the Sister study.20 Those experiencing racism may have lower quality sleep because of greater “racism-related” vigilance—an inability to set aside worry and stress due to lifelong experiences with discrimination. A survey study of 3,000 Chicago residents found that racism-related vigilance mediated the association of difficulty falling asleep or maintaining sleep with Black race.21 Thus, these lived experiences of oppression and racism may contribute to poorer sleep.
Resident perception of neighborhood safety and social cohesion are also associated with sleep quality,22 possibly through similar effects on vigilance and external threats. Individuals living in socially adverse neighborhoods (eg, violent, low social cohesion) have shorter sleep and lower quality sleep compared with those living in cohesive, safe neighborhoods.22 , 23 Among 7,231 adults in the Health and Retirement study—a National Institute of Aging-sponsored longitudinal cohort study of adults older than age 50 intended to examine multiple aspects of aging in the United States—living in more disordered neighborhoods was associated with more difficulty falling asleep and more periods of being awake after going to sleep.24 Similarly, shorter sleep duration was associated with lower rated neighborhood trust and helping behavior among adults living in Philadelphia area communities.25 Incarcerated women reported poor sleep quality as measured by Pittsburgh Sleep Quality Index related to both perception of safety and the prison environment (noise, light, and uncomfortable bunks).26 These differential environments likely contribute to the reported lower sleep quality and opportunity and overall sleep disparities.
Beyond neighborhood factors, household and employment factors likely contribute to sleep health disparities. This may be related to shift work requirements more common in nonwhite and low SES employment.27 Both rotating and night shiftwork leads to reduced sleep duration, reduced sleep efficiency, mistimed rhythms, and irregular schedules.22 , 23 , 27 Greater acculturation has been associated with shorter sleep duration, sleep fragmentation, and worse self-reported sleep in the United States,28 although a recent study suggests a more complex relationship of acculturation to sleep parameters that varied by age, generation, and SES.29
Potential Intervention Models
A few small trials have explored targeted behavioral health interventions to improve sleep in individuals living in low-income communities. One pilot study examined implementing yoga and sleep hygiene interventions to subjects residing in an affordable housing community. The intervention group had improved sleep duration (6.9 hours per night vs 5.4 hours per night, P < .01) and improvements in patient-reported outcome measurement scores for sleep-related impairment, sleep disturbance, and sleep hygiene behaviors.30 Another explored qualitatively how to adapt sleep hygiene education to be contextually appropriate, factoring in chronic stress and trauma as well as adverse sleeping environments.31 Sleep interventions require attention to socio-contextual factors, perhaps more so for those experiencing discrimination, racism, and poverty. Innovative Spanish/English sleep education and promotion training modules have been developed and successfully pilot tested among health providers in the United States, Mexico, and the US-Mexico border32; these eliminate the contribution of language barriers to sleep health. . Taken together, these pilot studies demonstrate importance of linguistically, socially, and culturally responsive sleep health interventions, education, and promotion policies.
Implementing policies to eliminate segregation, diversify neighborhoods, and improve the geographic features may reduce sleep disparities. Urban design changes—such as creating parks, planting trees, and cultivating community gardens that improve neighborhood physical environment—may yield benefits for sleep through encouraging activity, enhancing neighborhood connections, and reducing adverse noise, heat, and light. Proximity to green space, natural water, and greater tree canopy has been associated with better sleep.33 More recreational areas and a better walking environment are also associated with weight loss and greater physical activity,34 which themselves are associated with improved sleep quality, latency, and duration.35 Community gardens may foster social cohesion and perceptions of safety while enhancing green space.36 These built and social environment neighborhood-level interventions may improve sleep health and overall health and wellness of their communities. Greater neighborhood safety and social cohesion are associated with longer sleep duration, decreased wake after sleep onset, and greater reported sleep quality.37 Through urban design, city planners may reduce sleep disparities by enhancing green space, reducing crime, improving air quality, building recreation facilities, and fostering community in disadvantaged neighborhoods. Efforts to reverse centuries of segregation and redlining may yield more integrated neighborhoods with fewer sleep and other health disparities.
Disparities in Sleep Apnea
OSA may be more prevalent in nonwhites but is also more severe at the time of diagnosis.38 , 39 OSA is more likely to be underdiagnosed in nonwhites. This is demonstrated in the Hispanic Community Health Study,40 in which 14% had apnea-hypopnea index (AHI) ≥15 but only 1% clinical diagnosis, and the Jackson Heart Study,41 in which 24% had AHI ≥15 but only 5% had a physician diagnosis of OSA.
Black adults have also been shown to have low rates of following through on referrals for sleep apnea consultation (in one study this included 160/421 [38%] patients), which may be explained in part by mistrust of the medical system as well as competing burdens and life stressors.42 Once initiated on therapy, African-Americans and low SES groups have lower adherence with treatment.43 The causes of this disparity are unclear, but potential reasons include poorer sleep health in general (shorter sleep duration,44 more irregular patterns) that makes adherence more difficult and reduced quality of interactions with the health system because of implicit biases and medical mistrust.45
The high-prevalence and yet underrecognized aspects of sleep apnea create a need for innovative models of care that embrace new technologies and leverage the realignment of traditional provider roles in an attempt to mitigate sleep health disparities in nonwhite and low SES populations.
Potential Interventions
Approaches aimed at improving access to sleep-related health-care services for underserved populations with geographic and functional barriers to care include empowering nonsleep specialists with sleep medicine knowledge, skill, and responsibility. Attention has been drawn to studies showing feasibility of primary care vs sleep specialist OSA management with comparable 6-month positive airway pressure (PAP) adherence and improvements in daytime sleepiness. In two randomized controlled trials, undiagnosed OSA patients were randomized to nurse or sleep specialist lead care, with comparable outcomes for daytime symptoms and PAP adherence.46 , 47 An underrecognized advantage of using primary care providers or nurses to deliver sleep health care is that there is a much higher proportion of nonwhite care providers in these groups as compared with sleep specialists. Concordant race provision of care has been demonstrated to be associated with improved communication.48 An alternative means to improve the quality of interactions is through the use of peer buddies. The use of peer buddies with OSA adherent on CPAP to provide support and counseling has been shown to increase CPAP adherence49; the recruitment of adherent minority patients to help support other minority patients may be a valuable tool. However, it is imperative that sleep medicine training programs invest in resources to attract a more diverse pool of sleep providers.
Screening in high-risk populations during hospitalization may enable recognition of sleep disorders that might otherwise not get referrals to a sleep center.39 This proactive screening in high-risk patients may mitigate implicit bias in the recognition of sleep disorders in nonwhites.
Accessibility to sleep apnea treatment has been improved by advances in remote diagnosis and treatment. By using home sleep apnea testing (HSAT), auto-titration devices, telemedicine, and web-based applications, OSA can be diagnosed without requiring a trip to the sleep laboratory. In one crossover study of 75 urban African American adults who had both HSAT and in-laboratory polysomnography, 82% preferred HSAT over polysomnography because of being able to “sleep in your own bed” and ease of use of the monitoring device.50
Telemedicine is a promising approach using heath informatics technology to address barriers to sleep specialty care for underserved populations in remote locations or with transportation challenges. Direct patient care through telemedicine has been found to be more cost effective than traditional consultation, which can offset some of the technology costs for patients with poor economic status or in rural locations.51 In addition to direct patient care, successful examples of telemedicine consultation between primary care providers (PCPs) and subspecialists include the Extension for Community Health Care Outcomes (Project ECHO) framework. A pilot “telementorship” Project ECHO-based program in sleep medicine was developed and trialed for Veterans Affairs PCPs; participants reported improved comfort in managing sleep complaints.52 Because of these potential benefits, the American Academy of Sleep Medicine has endorsed sleep telemedicine as a means to improve health-care access.53 The data collected by telemedicine can be accessed to provide insight into the program, quality assurance, and course correction to further optimize sleep heath delivery and monitor outcomes.
Despite the future potential of health informatics technology, pitfalls remain given the large “digital divide” in terms of disparities in access to technology. Poverty, language, health literacy barriers, time, and rurality limit access to internet connectivity and may reduce access to telehealth. However, because of the ongoing COVID 19 pandemic, telemedicine has been widely adopted and is likely to continue to receive broad support and funding.
Disparities in Pediatric Sleep
Insufficient and poor-quality sleep is prevalent throughout childhood and adolescence,54 with salient racial, ethnic, and socioeconomic sleep disparities.55 , 56 Over half of youth obtain insufficient sleep for their age.54 However, similar to studies of adult populations, those of African American or Latinx backgrounds are more likely than their non-Latinx White peers to exhibit sleep curtailment.57 Beyond these racial and ethnic sleep health disparities, children living in lower-SES homes and neighborhoods are also more likely to exhibit shortened and poorer quality (less efficient) sleep compared with children living in higher-SES settings.56 These disparities can emerge within the first year of life, with young children living in socioeconomically disadvantaged neighborhoods showing more fragmented sleep.58 Race, ethnicity, and SES are additionally associated with OSA. African American children are more likely to have OSA symptoms than non-Latinx White children and have increased OSA severity when diagnosed.59 Children living in lower-income neighborhoods are also more likely to experience OSA.60
Research simultaneously examining the independent associations of race, ethnicity, and SES to pediatric sleep yields mixed results across sleep outcomes. A recent review of 23 studies identifying racial and ethnic disparities in child sleep health demonstrated that most of these identified disparities persisted even after studies adjusted for different SES indicators.55 Socio-demographics associations are more mixed for pediatric OSA. For example, in the Childhood Adenotonsillectomy Trial trial, family income was linked to significantly increased OSA severity (apnea/hypopnea index [AHI]) in univariate analyses, but this association was no longer significant after adjusting for African American race and environmental tobacco smoke exposure.61 Childhood Adenotonsillectomy Trial data also demonstrate that including neighborhood-level SES indicators (percentage of single female-headed households and poverty rate) in analyses predicting AHI attenuates the link between race and AHI by up to 55%, whereas individual-level SES variables have no such effect.60 Differences across studies in SES variables (eg, individual vs neighborhood factors; subjective vs objective poverty,56 and sleep parameters (eg, subjective vs objective sleep quality or duration; AHI vs subjective daytime sleepiness for OSA) may contribute to inconsistent findings.
A number of socio-ecological factors at the child, family, neighborhood, and broader socio-cultural levels likely contribute to these observed sleep disparities and are putative mechanisms linking race, ethnicity, SES, and sleep outcomes (Fig 1). As previously discussed in relation to adult sleep health disparities, historical housing policies have resulted in a disproportionate number of racial/ethnic minority families living in poverty9 and, in turn, experiencing adverse neighborhood-level factors that contribute to poor sleep. For instance, increased exposure to allergens, air pollution, and environmental tobacco smoke in African American children living in poverty62 may contribute to OSA disparities through increased upper airway inflammation, higher rates of atopy, and asthma. Other factors including aspects of the neighborhood physical (green space; noise) and social (community violence exposure; perceptions of safety; social cohesion) environment have been linked to poor sleep quality and insufficient sleep in children.10 Regarding family factors, limited physical resources (ie, available sleep space, bed, and bedding) and household crowding56 , 63 could lead to poor sleep quality and shortened duration in lower-SES youth. At a family level, psychosocial factors including household chaos,64 parental health literacy,65 parenting practices,66 and parental mood,67 have also been associated with pediatric sleep health. In addition, there are salient factors at the child level that warrant further study in the context of pediatric sleep disparities, including child temperament and mental health comorbidities,67 immigrant/refugee status and detention history,68 and experiences of discrimination.69
Studies using qualitative methods have provided insights into the ways in which different socio-ecological factors may interact to create barriers to healthy sleep for youth and their families of primarily lower-SES and nonwhite backgrounds.70 , 71 Indeed, within a socio-ecological framework, these different sociocultural, neighborhood, family, and child factors likely interact over time to impact child sleep outcomes. Additional research designed to casually examine these putative social-ecological factors and child sleep over time is necessary. Socio-ecological factors beyond the neighborhood environment are particularly understudied in the context of racial, ethnic, and socioeconomic disparities in pediatric OSA. This future work is necessary, especially as research suggests that Black children are less likely to experience improvement after OSA treatment.72
Approaches to Addressing Pediatric Sleep Disparities
Exacerbating sleep health disparities, nonwhite children and those of lower SES may lack consistent access to health-care services.73 Although more research is needed, some studies have found differences by race in practice patterns related to both general pediatric sleep services74 and OSA diagnosis and treatment.75 Innovative methods to promote sleep health and increase sleep problem identification and treatment are necessary to help reduce these disparities. Sleep problems including insufficient sleep and OSA are under-identified in pediatric primary care, a point of access for sleep health promotion, screening, and treatment referral.76 Given the burden placed on primary care physicians to address many health domains in a short well child visit, addressing sleep via other methods and providers is warranted.77 Integrating behavioral health providers into primary care to address sleep is a feasible yet underresearched option.76 Given that implicit racial/ethnic bias in clinicians can impact patient care,78 research on methods to improve pediatric sleep disparities should also focus on clinician factors.
Some research suggests the value of addressing sleep in home visiting programs79 and early childcare settings.80 School programs also may benefit pediatric sleep health, although a recent school-based study showed no benefits for racial/ethnic minority youth.81 Preliminary research highlights the potential efficacy of targeting sleep in at-risk youth in supportive housing82 or through bed provision and sleep education programs for youth living in poverty.63 Drawing on pediatric asthma research,73 home health-care workers and care coordination should be investigated as a method to address sleep disparities among underserved youth and families. Leveraging mobile applications for sleep health and behavioral sleep treatment also may reduce disparities in access to care, but these applications may require additional tailoring to be responsive to youth of different racial, ethnic, and socioeconomic backgrounds.71 Overall, identifying youth, family, and other stakeholder perceptions about sleep health and treatments is critical for developing and implementing acceptable and efficacious methods to address pediatric sleep disparities.70 , 71
Conclusions
Sleep heath disparities disproportinately affect the same populations who suffer overall heath disparities. They are influenced by multiple factors, including neighborhoods, home environment, race/ethnicity, SES, immigration/refugee and incarceration status, geographical access, and cultural beliefs about sleep (Fig 1). Despite being highly prevalent, sleep disorders are disproportionatly underdiagnosed and undertreated in nonwhite and low SES groups. There is a dearth of education about sleep health, not only in the community but also among health-care providers. Despite these challenges, there are successful multidisciplinary models to address sleep heath disparities including sleep education, expanding access to sleep health services through a variety of modalities (providing PCPs with expertise in high-yield sleep medicine topics, training allied servies to deliver behavioral sleep care, and expanding telemedicine services), and improving neighborhood built features to foster community and healthy diet, and to encourage activity to improve sleep health. Utilization of technology and bioinformatics to increase the reach among rural/geographically remote/inner city populations with limited transportation offers particular promise to sustainably transform the sleep disparity landscape.
Acknowledgments
Financial/nonfinancial disclosures: The authors have reported to CHEST the following: D. A. J. is supported by the National Heart, Lung, and Blood Institute, (NHLBI) K01HL138211. S. R. P. has received grant funding through my institution from Bayer Pharmaceuticals, Philips Respironics, and Respicardia. A. A. W. is supported by career development awards from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K23HD094905) and the Sleep Research Society Foundation. S. S. has received an unrestricted research grant from ResMed Inc. None declared (M. E. B., R. T. C., C. M. B., B. N. P., S. P., M. R., I. E. T.).
Footnotes
Drs Billings and Cohen contributed equally to this manuscript.
References
- 1.Grandner M.A., Williams N.J., Knutson K.L., Roberts D., Jean-Louis G. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med. 2016;18:7–18. doi: 10.1016/j.sleep.2015.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Golden S.D., Earp J.A. Social ecological approaches to individuals and their contexts: twenty years of health education & behavior health promotion interventions. Health Educ Behav. 2012;39(3):364–372. doi: 10.1177/1090198111418634. [DOI] [PubMed] [Google Scholar]
- 3.Buysse D.J. Sleep health: Can we define it? Does it matter? Sleep. 2014;37(1):9–17. doi: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grandner M.A., Petrov M.E., Rattanaumpawan P., Jackson N., Platt A., Patel N.P. Sleep symptoms, race/ethnicity, and socioeconomic position. J Clin Sleep Med. 2013;9(9):897–905. doi: 10.5664/jcsm.2990. 905a-905d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruiter M.E., Decoster J., Jacobs L., Lichstein K.L. Normal sleep in African-Americans and Caucasian-Americans: a meta-analysis. Sleep Med. 2011;12(3):209–214. doi: 10.1016/j.sleep.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 6.Hayes A.L., Spilsbury J.C., Patel S.R. The Epworth score in African American populations. J Clin Sleep Med. 2009;5(4):344–348. [PMC free article] [PubMed] [Google Scholar]
- 7.Hale L., Do D.P. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30(9):1096–1103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whinnery J., Jackson N., Rattanaumpawan P., Grandner M.A. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37(3):601–611. doi: 10.5665/sleep.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams D.R., Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnson D.A., Billings M.E., Hale L. Environmental determinants of insufficient sleep and sleep disorders: implications for population health. Curr Epidemiol Rep. 2018;5(2):61–69. doi: 10.1007/s40471-018-0139-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reitzel L.R., Short N.A., Schmidt N.B., et al. Distress tolerance links sleep problems with stress and health in homeless. Am J Health Behav. 2017;41(6):760–774. doi: 10.5993/AJHB.41.6.10. [DOI] [PubMed] [Google Scholar]
- 12.Ohayon M.M., Milesi C. Artificial outdoor nighttime lights associate with altered sleep behavior in the American general population. Sleep. 2016;39(6):1311–1320. doi: 10.5665/sleep.5860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Billings M.E., Gold D., Szpiro A., et al. The association of ambient air pollution with sleep apnea: the multi-ethnic study of atherosclerosis. Ann Am Thorac Soc. 2019;16(3):363–370. doi: 10.1513/AnnalsATS.201804-248OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoffman J.S., Shandas V., Pendleton N. The effects of historical housing policies on resident exposure to intra-urban heat: a study of 108 US urban areas. Climate. 2020;8(1):12. [Google Scholar]
- 15.Okamoto-Mizuno K., Mizuno K. Effects of thermal environment on sleep and circadian rhythm. J Physiol Anthropol. 2012;31(1):14. doi: 10.1186/1880-6805-31-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson D.A., Hirsch J.A., Moore K.A., Redline S., Diez Roux A.V. Associations between the built environment and objective measures of sleep: the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2018;187(5):941–950. doi: 10.1093/aje/kwx302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Casey J.A., Morello-Frosch R., Mennitt D.J., Fristrup K., Ogburn E.L., James P. Race/ethnicity, socioeconomic status, residential segregation, and spatial variation in noise exposure in the contiguous United States. Environ Health Perspect. 2017;125(7) doi: 10.1289/EHP898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bailey Z.D., Krieger N., Agenor M., Graves J., Linos N., Bassett M.T. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- 19.Alcantara C., Patel S.R., Carnethon M., et al. Stress and sleep: results from the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. SSM Popul Health. 2017;3:713–721. doi: 10.1016/j.ssmph.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gaston S.A., Feinstein L., Slopen N., Sandler D.P., Williams D.R., Jackson C.L. Everyday and major experiences of racial/ethnic discrimination and sleep health in a multiethnic population of U.S. women: findings from the Sister Study. Sleep Med. 2020;71:97–105. doi: 10.1016/j.sleep.2020.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hicken M.T., Lee H., Ailshire J., Burgard S.A., Williams D.R. “Every shut eye, ain't sleep”: the role of racism-related vigilance in racial/ethnic disparities in sleep difficulty. Race Soc Probl. 2013;5(2):100–112. doi: 10.1007/s12552-013-9095-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson D.A., Simonelli G., Moore K., et al. The neighborhood social environment and objective measures of sleep in the multi-ethnic study of atherosclerosis. Sleep. 2017;40(1) doi: 10.1093/sleep/zsw016. zsw016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simonelli G., Dudley K.A., Weng J., et al. Neighborhood factors as predictors of poor sleep in the Sueno Ancillary Study of the Hispanic Community Health Study/Study of Latinos. Sleep. 2017;40(1) doi: 10.1093/sleep/zsw025. zsw025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen-Edinboro L.P., Kaufmann C.N., Augustinavicius J.L., et al. Neighborhood physical disorder, social cohesion, and insomnia: results from participants over age 50 in the Health and Retirement Study. Int Psychogeriatrics. 2014:1–8. doi: 10.1017/S1041610214001823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robbins R., Jean-Louis G., Gallagher R.A., et al. Examining social capital in relation to sleep duration, insomnia, and daytime sleepiness. Sleep Med. 2019;60:165–172. doi: 10.1016/j.sleep.2019.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harner H.M., Budescu M. Sleep quality and risk for sleep apnea in incarcerated women. Nurs Res. 2014;63(3):158–169. doi: 10.1097/NNR.0000000000000031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reid K.J., Weng J., Ramos A.R., et al. Impact of shift work schedules on actigraphy-based measures of sleep in Hispanic workers: results from the Hispanic Community Health Study/Study of Latinos ancillary Sueno study. Sleep. 2018;41(10) doi: 10.1093/sleep/zsy131. zsy131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dudley K.A., Johnson D.A., Weng J., et al. Acculturation and sleep patterns in US hispanic/latinos: the Hispanic Community Health Study/study of latinos (HCHS/SOL) Sueno anicllary study. Sleep. 2017;40:A310–A311. [Google Scholar]
- 29.Martinez-Miller E.E., Prather A.A., Robinson W.R., et al. US acculturation and poor sleep among an intergenerational cohort of adult Latinos in Sacramento, California. Sleep. 2019;42(3) doi: 10.1093/sleep/zsy246. zsy246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spadola C.E., Rottapel R.E., Zhou E.S., et al. A sleep hygiene and yoga intervention conducted in affordable housing communities: pilot study results and lessons for a future trial. Complement Ther Clin Pract. 2020;39:101121. doi: 10.1016/j.ctcp.2020.101121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rottapel R.E., Zhou E.S., Spadola C.E., et al. Adapting sleep hygiene for community interventions: a qualitative investigation of sleep hygiene behaviors among racially/ethnically diverse, low-income adults. Sleep Health. 2020;6(2):205–213. doi: 10.1016/j.sleh.2019.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baldwin C.M., Choi M., McClain D.B., Celaya A., Quan S.F. Spanish translation and cross-language validation of a sleep habits questionnaire for use in clinical and research settings. J Clin Sleep Med. 2012;8(2):137–146. doi: 10.5664/jcsm.1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson B.S., Malecki K.M., Peppard P.E., Beyer K.M.M. Exposure to neighborhood green space and sleep: evidence from the Survey of the Health of Wisconsin. Sleep Health. 2018;4(5):413–419. doi: 10.1016/j.sleh.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mayne S.L., Auchincloss A.H., Michael Y.L. Impact of policy and built environment changes on obesity-related outcomes: a systematic review of naturally occurring experiments. Obes Rev. 2015;16(5):362–375. doi: 10.1111/obr.12269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kredlow M.A., Capozzoli M.C., Hearon B.A., Calkins A.W., Otto M.W. The effects of physical activity on sleep: a meta-analytic review. J Behav Med. 2015;38(3):427–449. doi: 10.1007/s10865-015-9617-6. [DOI] [PubMed] [Google Scholar]
- 36.Teig E., Amulya J., Bardwell L., Buchenau M., Marshall J.A., Litt J.S. Collective efficacy in Denver, Colorado: strengthening neighborhoods and health through community gardens. Health Place. 2009;15(4):1115–1122. doi: 10.1016/j.healthplace.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 37.Troxel W.M., DeSantis A., Richardson A.S., et al. Neighborhood disadvantage is associated with actigraphy-assessed sleep continuity and short sleep duration. Sleep. 2019;41(10):zsy140. doi: 10.1093/sleep/zsy140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Williams N.J., Grandne M.A., Snipes A., et al. Racial/ethnic disparities in sleep health and health care: importance of the sociocultural context. Sleep Health. 2015;1(1):28–35. doi: 10.1016/j.sleh.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Quintos A., Naranjo M., Kelly C., Quan S.F., Sharma S. Recognition and treatment of sleep-disordered breathing in obese African American hospitalized patients may improve outcome. J Natl Med Assoc. 2019;111(2):176–184. doi: 10.1016/j.jnma.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 40.Redline S., Sotres-Alvarez D., Loredo J., et al. Sleep-disordered breathing in Hispanic/Latino individuals of diverse backgrounds: the Hispanic Community Health Study/Study of Latinos. Am J Respir Crit Care Med. 2014;189(3):335–344. doi: 10.1164/rccm.201309-1735OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Johnson D.A., Guo N., Rueschman M., Wang R., Wilson J.G., Redline S. Prevalence and correlates of obstructive sleep apnea among African Americans: the Jackson Heart Sleep Study. Sleep. 2018;41(10) doi: 10.1093/sleep/zsy154. zsy154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jean-Louis G., von Gizycki H., Zizi F., Dharawat A., Lazar J.M., Brown C.D. Evaluation of sleep apnea in a sample of black patients. J Clin Sleep Med. 2008;4(5):421–425. [PMC free article] [PubMed] [Google Scholar]
- 43.Pandey A., Mereddy S., Combs D., et al. Socioeconomic inequities in adherence to positive airway pressure therapy in population-level analysis. J Clin Med. 2020;9(2):442. doi: 10.3390/jcm9020442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Billings M.E., Rosen C.L., Wang R., et al. Is the relationship between race and continuous positive airway pressure adherence mediated by sleep duration? Sleep. 2013;36(2):221–227. doi: 10.5665/sleep.2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.FitzGerald C., Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19. doi: 10.1186/s12910-017-0179-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Andreu A.L., Chiner E., Sancho-Chust J.N., et al. Effect of an ambulatory diagnostic and treatment programme in patients with sleep apnoea. Eur Respir J. 2012;39(2):305–312. doi: 10.1183/09031936.00013311. [DOI] [PubMed] [Google Scholar]
- 47.Antic N.A., Buchan C., Esterman A., et al. A randomized controlled trial of nurse-led care for symptomatic moderate-severe obstructive sleep apnea. Am J Respir Crit Care Med. 2009;179(6):501–508. doi: 10.1164/rccm.200810-1558OC. [DOI] [PubMed] [Google Scholar]
- 48.Shen M.J., Peterson E.B., Costas-Muniz R., et al. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J Racial Ethn Health Disparities. 2018;5(1):117–140. doi: 10.1007/s40615-017-0350-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Parthasarathy S., Wendel C., Haynes P.L., Atwood C., Kuna S. A pilot study of CPAP adherence promotion by peer buddies with sleep apnea. J Clin Sleep Med. 2013;9(6):543–550. doi: 10.5664/jcsm.2744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Garg N., Rolle A.J., Lee T.A., Prasad B. Home-based diagnosis of obstructive sleep apnea in an urban population. J Clin Sleep Med. 2014;10(8):879–885. doi: 10.5664/jcsm.3960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wade V.A., Karnon J., Elshaug A.G., Hiller J.E. A systematic review of economic analyses of telehealth services using real time video communication. BMC Health Serv Res. 2010;10:233. doi: 10.1186/1472-6963-10-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Parsons E.C., Mattox E.A., Beste L.A., et al. Development of a sleep telementorship program for rural Department of Veterans Affairs primary care providers: sleep Veterans Affairs extension for community healthcare outcomes. Ann Am Thorac Soc. 2017;14(2):267–274. doi: 10.1513/AnnalsATS.201605-361BC. [DOI] [PubMed] [Google Scholar]
- 53.Singh J., Badr M.S., Diebert W., et al. American Academy of Sleep Medicine (AASM) position paper for the use of telemedicine for the diagnosis and treatment of sleep disorders. J Clin Sleep Med. 2015;11(10):1187–1198. doi: 10.5664/jcsm.5098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.National Sleep Foundation 2014 Sleep in America Poll: sleep in the modern family. 2014. https://www.sleepfoundation.org/professionals/sleep-americar-polls/2014-sleep-modern-family Accessed January 1, 2019.
- 55.Guglielmo D., Gazmararian J.A., Chung J., Rogers A.E., Hale L. Racial/ethnic sleep disparities in US school-aged children and adolescents: a review of the literature. Sleep Health. 2018;4(1):68–80. doi: 10.1016/j.sleh.2017.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.El-Sheikh M., Bagley E.J., Keiley M., Elmore-Staton L., Chen E., Buckhalt J.A. Economic adversity and children's sleep problems: multiple indicators and moderation of effects. Health Psychol. 2013;32(8):849–859. doi: 10.1037/a0030413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pena M.M., Rifas-Shiman S.L., Gillman M.W., Redline S., Taveras E.M. Racial/ethnic and socio-contextual correlates of chronic sleep curtailment in childhood. Sleep. 2016;39(9):1653–1661. doi: 10.5665/sleep.6086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Grimes M., Camerota M., Propper C.B. Neighborhood deprivation predicts infant sleep quality. Sleep Health. 2019;5(2):148–151. doi: 10.1016/j.sleh.2018.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rosen C.L., Larkin E.K., Kirchner H.L., et al. Prevalence and risk factors for sleep-disordered breathing in 8- to 11-year-old children: association with race and prematurity. J Pediatr. 2003;142(4):383–389. doi: 10.1067/mpd.2003.28. [DOI] [PubMed] [Google Scholar]
- 60.Wang R., Dong Y., Weng J., et al. Associations among neighborhood, race, and sleep apnea severity in children: a six-city analysis. Ann Am Thorac Soc. 2017;14(1):76–84. doi: 10.1513/AnnalsATS.201609-662OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Weinstock T.G., Rosen C.L., Marcus C.L., et al. Predictors of obstructive sleep apnea severity in adenotonsillectomy candidates. Sleep. 2014;37(2):261–269. doi: 10.5665/sleep.3394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Singh G.K., Siahpush M., Kogan M.D. Disparities in children's exposure to environmental tobacco smoke in the United States, 2007. Pediatrics. 2010;126(1):4–13. doi: 10.1542/peds.2009-2744. [DOI] [PubMed] [Google Scholar]
- 63.Mindell J.A., Sedmak R., Boyle J.T., Butler R., Williamson A.A. Sleep well!: a pilot study of an education campaign to improve sleep of socioeconomically disadvantaged children. J Clin Sleep Med. 2016;12(12):1593–1599. doi: 10.5664/jcsm.6338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Doane L.D., Breitenstein R.S., Beekman C., Clifford S., Smith T.J., Lemery-Chalfant K. Early life socioeconomic disparities in children's sleep: the mediating role of the current home environment. J Youth Adolesc. 2019;48(1):56–70. doi: 10.1007/s10964-018-0917-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bathory E., Tomopoulos S., Rothman R., et al. Infant sleep and parent health literacy. Acad Pediatr. 2016;16(6):550–557. doi: 10.1016/j.acap.2016.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mindell J.A., Sadeh A., Kohyama J., How T.H. Parental behaviors and sleep outcomes in infants and toddlers: a cross-cultural comparison. Sleep Med. 2010;11(4):393–399. doi: 10.1016/j.sleep.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 67.Newton A.T., Honaker S.M., Reid G.J. Risk and protective factors and processes for behavioral sleep problems among preschool and early school-aged children: a systematic review. Sleep Med Rev. 2020;52:101303. doi: 10.1016/j.smrv.2020.101303. [DOI] [PubMed] [Google Scholar]
- 68.Lorek A., Ehntholt K., Nesbitt A., et al. The mental and physical health difficulties of children held within a British immigration detention center: a pilot study. Child Abuse Negl. 2009;33(9):573–585. doi: 10.1016/j.chiabu.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 69.Slopen N., Lewis T.T., Williams D.R. Discrimination and sleep: a systematic review. Sleep Med. 2016;18:88–95. doi: 10.1016/j.sleep.2015.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Williamson A.A., Milaniak I., Watson B., et al. Early childhood sleep intervention in urban primary care: clinician and caregiver perspectives. J Pediatr Psychol. 2020;45(8):933–945. doi: 10.1093/jpepsy/jsaa024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Quante M., Khandpur N., Kontos E.Z., Bakker J.P., Owens J.A., Redline S. A qualitative assessment of the acceptability of smartphone applications for improving sleep behaviors in low-income and minority adolescents. Behav Sleep Med. 2018;17(5):1–13. doi: 10.1080/15402002.2018.1432483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Marcus C.L., Moore R.H., Rosen C.L., et al. A randomized trial of adenotonsillectomy for childhood sleep apnea. N Engl J Med. 2013;368(25):2366–2376. doi: 10.1056/NEJMoa1215881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Volerman A., Chin M.H., Press V.G. Solutions for asthma disparities. Pediatrics. 2017;139(3) doi: 10.1542/peds.2016-2546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Williamson A.A., Rubens S.L., Patrick K.E., Moore M., Mindell J.A. Differences in sleep patterns and problems by race in a clinical sample of black and white preschoolers. J Clin Sleep Med. 2017;13(11):1281–1288. doi: 10.5664/jcsm.6798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Boss E.F., Smith D.F., Ishman S.L. Racial/ethnic and socioeconomic disparities in the diagnosis and treatment of sleep-disordered breathing in children. Int J Pediatr Otorhinolaryngol. 2011;75(3):299–307. doi: 10.1016/j.ijporl.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 76.Honaker S.M., Saunders T. The sleep checkup: sleep screening, guidance, and management in pediatric primary care. Clin Pract Pediatr Psychol. 2018;6(3):201–210. [Google Scholar]
- 77.Sevecke J.R., Meadows T.J. It takes a village: multidisciplinary approach to screening and prevention of pediatric sleep issues. Med Sci (Basel) 2018;6(3):77. doi: 10.3390/medsci6030077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Maina I.W., Belton T.D., Ginzberg S., Singh A., Johnson T.J. A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Soc Sci Med. 2018;199:219–229. doi: 10.1016/j.socscimed.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 79.Paul I.M., Savage J.S., Anzman-Frasca S., Marini M.E., Mindell J.A., Birch L.L. INSIGHT responsive parenting intervention and infant sleep. Pediatrics. 2016;138(1) doi: 10.1542/peds.2016-0762. e20160762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wilson K.E., Miller A.L., Bonuck K., Lumeng J.C., Chervin R.D. Evaluation of a sleep education program for low-income preschool children and their families. Sleep. 2014;37(6):1117–1125. doi: 10.5665/sleep.3774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tavernier R., Kahn J., Kelter J., Sasson L., Adam E.K. Text message intervention improves objective sleep hours among adolescents: the moderating role of race-ethnicity. Sleep Health. 2017;3(1):62–67. doi: 10.1016/j.sleh.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 82.Labella M.H., Kalstabbakken A., Johnson J., et al. Promoting resilience by improving children's sleep: feasibility among families living in supportive housing. Prog Community Health partnersh. 2017;11(3):285–293. doi: 10.1353/cpr.2017.0033. [DOI] [PubMed] [Google Scholar]