Abstract
Mutations in BRCA1 and BRCA2 cause deficiencies in homologous recombination repair (HR), resulting in repair of DNA double-strand breaks by the alternative non-homologous end-joining pathway, which is more error prone. HR deficiency of breast tumors is important because it is associated with better responses to platinum salt therapies and PARP inhibitors. Among other consequences of HR deficiency are characteristic somatic-mutation signatures and gene-expression patterns. The term “BRCA-like” (or “BRCAness”) describes tumors that harbor an HR defect but have no detectable germline mutation in BRCA1 or BRCA2. A better understanding of the genes and molecular events associated with tumors being BRCA-like could provide mechanistic insights and guide development of targeted treatments. Using data from The Cancer Genome Atlas (TCGA) for 1101 breast-cancer patients, we identified individuals with a germline mutation, somatic mutation, homozygous deletion, and/or hypermethylation event in BRCA1, BRCA2, and 59 other cancer-predisposition genes. Based on the assumption that BRCA-like events would have similar downstream effects on tumor biology as BRCA1/BRCA2 germline mutations, we quantified these effects based on somatic-mutation signatures and gene-expression profiles. We reduced the dimensionality of the somatic-mutation signatures and expression data and used a statistical resampling approach to quantify similarities among patients who had a BRCA1/BRCA2 germline mutation, another type of aberration in BRCA1 or BRCA2, or any type of aberration in one of the other genes. Somatic-mutation signatures of tumors having a non-germline aberration in BRCA1/BRCA2 (n = 80) were generally similar to each other and to tumors from BRCA1/BRCA2 germline carriers (n = 44). Additionally, somatic-mutation signatures of tumors with germline or somatic events in ATR (n = 16) and BARD1 (n = 8) showed high similarity to tumors from BRCA1/BRCA2 carriers. Other genes (CDKN2A, CTNNA1, PALB2, PALLD, PRSS1, SDHC) also showed high similarity but only for a small number of events or for a single event type. Tumors with germline mutations or hypermethylation of BRCA1 had relatively similar gene-expression profiles and overlapped considerably with the Basal-like subtype; but the transcriptional effects of the other events lacked consistency. Our findings confirm previously known relationships between molecular signatures and germline or somatic events in BRCA1/BRCA2. Our methodology represents an objective way to identify genes that have similar downstream effects on molecular signatures when mutated, deleted, or hypermethylated.
Introduction
Approximately 1–5% of breast-cancer patients carry a pathogenic germline variant in either BRCA1 or BRCA2 [1–5]. These genes play important roles in homologous recombination repair (HR) of double-stranded breaks and stalled or damaged replication forks [6, 7]. When the BRCA1 or BRCA2 gene products are unable to perform HR, cells may resort to non-homologous end-joining, a less effective means of repairing double-stranded breaks, potentially leading to an increased rate of DNA mutations [8–11]. Patients who carry biallelic loss of BRCA1 and BRCA2 due to germline variants and/or somatic events often respond well to poly ADP ribose polymerase (PARP) inhibitors and platinum-salt therapies, which increase the rate of DNA damage, typically causing the cells to enter programmed cell death [12–17].
The downstream effects of BRCA mutations are distinctive. For example, BRCA-mutant tumors exhibit an abundance of C-to-T transitions across the genome, potentially reflecting tumor cells’ impaired ability to repair specific types of DNA damage [18]. In large-scale sequencing projects, such mutational patterns (termed “somatic-mutation signatures”) have been observed in association with other types of molecular events, as well as environmental and endogenous exposures, across many cancer types [19, 20]. Among these signatures, the so-called “Signature 3” has been associated with BRCA mutations and HR [19, 21].
Other downstream effects of BRCA mutations include characteristic transcriptional responses. For example, it has been shown that the “Basal” gene-expression subtype is enriched for tumors with BRCA1 mutations [22–25], that BRCA1 mutations are commonly found in triple-negative breast tumors [26, 27], and that gene-expression profiles may predict PARP inhibitor responses [28, 29]. These patterns are consistently observable, even in the presence of hundreds of other mutations [25, 30].
In 2004, Turner, et al. coined the term “BRCAness” to describe patients who do not have a pathogenic germline variant in BRCA1 or BRCA2 but who have developed a tumor with an impaired ability to perform HR [31]. Here we use the alternative term “BRCA-like.” This category may be useful for clinical management of patients and especially for predicting treatment responses [31, 32]. Recent estimates suggest that the proportion of breast-cancer patients who fall into this category may be as high as 20% [33]. Davies, et al. demonstrated an ability to categorize patients into this category with high accuracy based on high-level mutational patterns [33]. Polak, et al. confirmed that somatic mutations, large deletions, and DNA hypermethylation of BRCA1 and BRCA2 are reliable indicators of being BRCA-like [21, 34–36]. They also showed a relationship between being BRCA-like and germline mutations in PALB2 and hypermethylation of RAD51C [21]. However, a considerable portion of breast tumors with HR deficiency lack a known driver. Furthermore, less is known about whether the downstream effects of germline variants, somatic variants, large deletions, and hypermethylation are similar to each other or whether these effects are similar for different genes.
An underlying assumption of the BRCA-like concept is that the effects of HR deficiency are similar across tumors, regardless of the genes that drive those deficiencies and despite considerable variation in genetic backgrounds, environmental factors, and the presence of other driver mutations. Based on this assumption—and in a quest to identify additional genes that contribute to being BRCA-like—we performed a systematic evaluation of multiomic and clinical data from 1101 patients in The Cancer Genome Atlas (TCGA) [25]. In performing these evaluations, we characterized each tumor using two types of molecular signature: 1) weights that represent the tumor’s somatic-mutation profile and 2) the tumor’s mRNA expression profile. To evaluate similarities among tumors based on these molecular profiles, we used a statistical-resampling approach designed to quantify similarities among patient subgroups, even when those subgroups are small, thus helping to account for rare events. We use “aberration” as a general term to describe germline mutations, somatic mutations, copy-number deletions, and hypermethylation events.
Methods
Data preparation and filtering
We obtained breast-cancer data from TCGA for 1101 patients in total. To determine germline-mutation status, we downloaded raw sequencing data from CGHub [37] for normal (blood) samples. We limited our analysis to whole-exome sequencing samples that had been sequenced using Illumina Genome Analyzer or HiSeq equipment. Because the sequencing data were stored in BAM format, we used Picard Tools (SamToFastq module, version 1.131, http://broadinstitute.github.io/picard) to convert the files to FASTQ format. We used the Burrows-Wheeler Alignment (BWA) tool (version 0.7.12) [38] to align the sequencing reads to version 19 of the GENCODE reference genome (hg19 compatible) [39]. We used sambamba (version 0.5.4) [40] to sort, index, mark duplicates, and flag statistics for the aligned BAM files. In cases where multiple BAM files were available for a single patient, we used bamUtil (version 1.0.13, https://github.com/statgen/bamUtil) to merge the BAM files.
When searching for relevant germline variants, we examined 61 genes from the BROCA Cancer Risk Panel (http://tests.labmed.washington.edu/BROCA) [41, 42]. We extracted genomic data for these genes using bedtools (intersectBed module, version 2) [43].
We used Picard Tools (CalculateHsMetrics module) to calculate alignment metrics. For exome-capture regions across all germline samples, the average sequencing coverage was 44.4. The average percentage of target bases that achieved at least 30X coverage was 33.7%. The average percentage of target bases that achieved at least 100X coverage was 12.3%.
To call DNA variants, we used freebayes (version v0.9.21-18-gc15a283) [44] and Pindel (https://github.com/genome/pindel). We used freebayes to identify single-nucleotide variants (SNVs) and small insertions or deletions (indels); we used Pindel to identify medium-sized insertions and deletions. Having called these variants, we used snpEff (version 4.1) [45] to annotate the variants and GEMINI (version 0.16.3) [46] to query the variant data.
To expedite execution of the above steps, we used the GNU Parallel software [47]. The scripts and code that we used to process the germline data can be found in an open-access repository: https://bitbucket.org/srp33/tcga_germline.
Geneticists experienced in variant interpretation (BHS, TW, SG, MCK) evaluated each of the germline variants for pathogenicity. Following accepted guidelines for variant classification [42], variants were reviewed individually, followed by a group discussion. In evaluating each variant, we first considered the likelihood of pathogenicity as reported in the University of Washington, Department of Laboratory Medicine clinical-variant database. In addition, we used functional annotations from SIFT [48], Polyphen2 [49], and GERP [50]. When evaluating splice-site variants, we assessed pathogenicity based on whether the variants had been shown experimentally to cause truncations. Additionally, we used NNsplice [51] and Rescue ESE [52] to evaluate splicing variants. We also used maximum entropy modeling [53] and Human Splicing Finder [54], which aggregate data from other splice prediction tools. We classified as benign any in-frame deletions that had been observed as naturally occurring transcripts. When evaluating potential effects of a variant on protein function, we evaluated the extent to which a given protein domain varies within the general population. This process for evaluating candidate cancer-predisposing variants is used in clinical practice and has been demonstrated to maximize actionable results and minimize the frequency of variants of unknown significance [42]. Personal and family histories were unavailable for TCGA patients, so this information could not be included in the evaluation process. The germline calls that we made for these patients were independent of variant-classification calls used in prior studies of TCGA data [25, 55].
To assess loss of heterozygosity (LOH), we used data from Riaz et al. [56]. They had made LOH calls for a large proportion of TCGA breast-cancer patients. Their process included an evaluation of data from Affymetrix SNP 6.0 arrays, genotyping via Affymetrix’s birdseed algorithm, and calculation of the log ratios and B-allele frequencies using PennCNV [57]. The ASCAT algorithm [58] was used to determine allele-specific copy number and loss of heterozygosity for each mutation.
We identified somatic SNVs and indels for each patient by examining variant calls that had been made using Mutect [59]; these variants had been made available via the Genomic Data Commons [60]. Somatic variants that 1) were synonymous 2) snpEff classified as having a “LOW” or “MODIFIER” effect on protein sequence, 3) SIFT [48] and Polyphen2 [49] both suggested to be benign [61], and 4) were observed at greater than 1% frequency across all populations in ExAC [62] were excluded. For BRCA1 and BRCA2, we examined candidate variants based on a priori observations of pathogenicity as reported in the University of Washington, Department of Laboratory Medicine clinical-variant database [63]. Based on these criteria, we categorized each variant as pathogenic, likely pathogenic, variant of uncertain significance (VUS), likely benign, or benign. Then we examined ClinVar [64] for evidence that VUS or likely benign variants had been classified by others as pathogenic; however, none met this criterion. To err on the side of sensitivity, we considered any BRCA1 and BRCA2 mutation to be “aberrant” if it fell into our pathogenic, likely pathogenic, or VUS categories. The final classifications are shown in S1 Table.
Using the somatic-mutation data for each patient, we derived mutation-signature profiles using the deconstructSigs (version 1.8.0) R package [65]. As input to this process, we used somatic-variant calls that had not been filtered for pathogenicity, as a way to ensure adequate representation of each signature. The output of this process was a vector for each tumor that indicated a weight for each signature [19]. S1 and S2 Figs illustrate these weights for two tumors that we analyzed.
We downloaded DNA methylation data via the Xena Functional Genomics Explorer [66]. These data were generated using the Illumina HumanMethylation27 and HumanMethylation450 BeadChip platforms. For the HumanMethylation27 arrays, we mapped probes to genes using a file provided by the manufacturer (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GPL8490). For the HumanMethylation450 arrays, we mapped probes to genes using an annotation file created by Price, et al. [67] (see http://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GPL16304). Typically, multiple probes mapped to a given gene. Using probe-level data from BRCA1, BRCA2, PTEN, and RAD51C, we performed a preliminary analysis to determine criteria for selecting and summarizing these probe-level values. We started with the assumption that in most cases, the genes would be methylated at low levels. We also assumed that probes nearest the transcription start site would be most informative. Upon plotting the data (S3 Fig), we decided to limit our analysis to probes that mapped to the genome within 300 nucleotides of each gene’s transcription start site. In some cases, probes appeared to be faulty because they showed considerably different methylation levels (“beta” values) than other probes in the region (S3 Fig). To mitigate the effects of these outliers, we calculated gene-level methylation values as the median beta value across any remaining probes for that gene.
To identify tumors that exhibited relatively high beta values—and thus could be considered to be hypermethylated—we used a univariate, outlier-detection algorithm, implemented in the extremevalues R packages (version 2.3.2) [68]. This enabled us to look for extreme values using one side of a specified distribution. This package supports five options for the distribution: normal (default), lognormal, exponential, pareto, and weibull. None of these distributions was a consistently good fit for the methylation (beta) values, in part because the shape of the data differed considerably across the genes (S4–S7 Figs). We used the exponential distribution because it identified hypermethylated genes at rates that were largely consistent with prior work [21]. We used the “getOutliersII” function with default parameter values.
We downloaded copy-number-variation data from the Xena Functional Genomics Explorer [66]. These data had been generated using Affymetrix SNP 6.0 arrays; CNV calls had been made using the GISTIC2 method [69]. The CNV calls had also been summarized to gene-level values using integer-based discretization. We focused on tumors with a gene count of “-2”, which indicates a homozygous deletion.
We used RNA-Sequencing data that had been aligned and summarized to gene-level values using the original TCGA pipeline [25]. To facilitate biological and clinical interpretation, we examined relationships between germline and somatic events and the Prosigna™ Breast Cancer Prognostic Gene Signature (PAM50) subtypes [70]. Netanely, et al. had previously published PAM50 subtypes for TCGA breast cancer samples; we reused this information in our study [71]. We also sought to identify tumors with unusually low expression levels. To do this, we used the getOutliersI function in the extremevalues package. We used the following non-default parameter values: alpha = c(0.000001, 0.000001), distribution = "lognormal", FLim = c(0.1, 0.9). RNA-Sequencing data have been shown to fit the log-normal distribution [72].
We parsed demographic, histopathological, and surgical variables for TCGA samples from the repository prepared by Rahman, et al. [73]. We obtained drug-response data from the TCGA legacy archive (https://portal.gdc.cancer.gov/legacy-archive) and standardized drug names using synonyms from the National Cancer Institute Thesaurus [74].
Quantitative analysis and visualization
To prepare, analyze, and visualize the data, we wrote computer scripts in the R programming language [75]. In writing these scripts, we used the following packages: readr [76], dplyr [77], ggplot2 [78], tidyr [79], reshape2 [80], ggrepel [81], cowplot [82], data.table [83], UpSetR [84], BSgenome.Hsapiens.UCSC.hg38 [85, 86], and Rtsne [87].
To reduce data dimensionality, we applied multidimensional scaling (MDS) [88] to the somatic-mutation signatures and gene-expression profiles. This reduced the data to two dimensions. To quantify homogeneity within a group of tumors that harbored a particular aberration, we calculated the pairwise Euclidean distance between each patient pair in the group and then calculated the median pairwise distance, based on the two-dimensional values [89]. As an additional measure of homogeneity, we used logistic regression to predict BRCA mutation status using the dimensionally reduced coordinates. In evaluating this approach, we used two-fold cross validation and configured the model to weight the minority class in inverse proportion to the frequency of the minority class.
When comparing two given groups, we used a similar resampling approach but instead calculated the median distance between each pair of individuals in either group. To determine whether the similarity within or between groups was statistically significant, we used a permutation approach. We randomized the patient identifiers, calculated the median pairwise distance within (or between) groups, and repeated those steps 100,000 times. This process resulted in an empirical null distribution against which we compared the actual median distance. We then derived empirical p-values by calculating the proportion of randomized median distances that were larger than the actual median distance. We adjusted the empirical p-values for multiple testing using Holm’s method [90]; we applied this correction to the p-values across all aberration types.
For visualization, we plotted the MDS values as Cartesian coordinates; we also used Barnes-Hut t-distributed Stochastic Neighbor Embedding (t-SNE) [91, 92] as an alternative method for visualizing the data.
We created a series of R scripts that execute all steps of our analysis and that generate the figures in this paper; these scripts are available at https://osf.io/9jhr2.
Ethics statement
Brigham Young University’s Institutional Review Board approved this study under exemption status. This study uses data collected from public repositories, other than the germline-variant data, which are restricted by TCGA data-access policies. We played no part in patient recruiting or in obtaining patient consent. We have adhered to guidelines from TCGA on handling data.
Results
We used clinical and molecular data from 1101 TCGA breast-cancer patients to evaluate the downstream effects of BRCA1 and BRCA2 germline mutations in tumors. We evaluated two types of downstream effects: 1) signatures that reflect a tumor’s overall somatic-mutation profile in a trinucleotide context and 2) tumor gene-expression levels. We used somatic-mutation signatures because they reflect the genomic effects of HR defects and have been associated with BRCA1/BRCA2 mutation status [18, 19]. We used gene-expression data because they are used to classify breast tumors into subtypes [93, 94] and often reflect genomic variation [61, 95, 96]. We assessed whether either of these types of profiles was more homogeneous in BRCA1/BRCA2 germline carriers than in randomly selected patients. In addition, we evaluated potential criteria for classifying tumors into the BRCA-like category. These criteria included somatic mutations, homozygous deletions, and DNA hypermethylation of BRCA1 and BRCA2. Similarly, we assessed whether these different types of aberrations have downstream effects similar to BRCA1/BRCA2 for 59 other cancer-predisposition genes.
Somatic-mutation signatures and gene-expression profiles across all breast-cancer patients
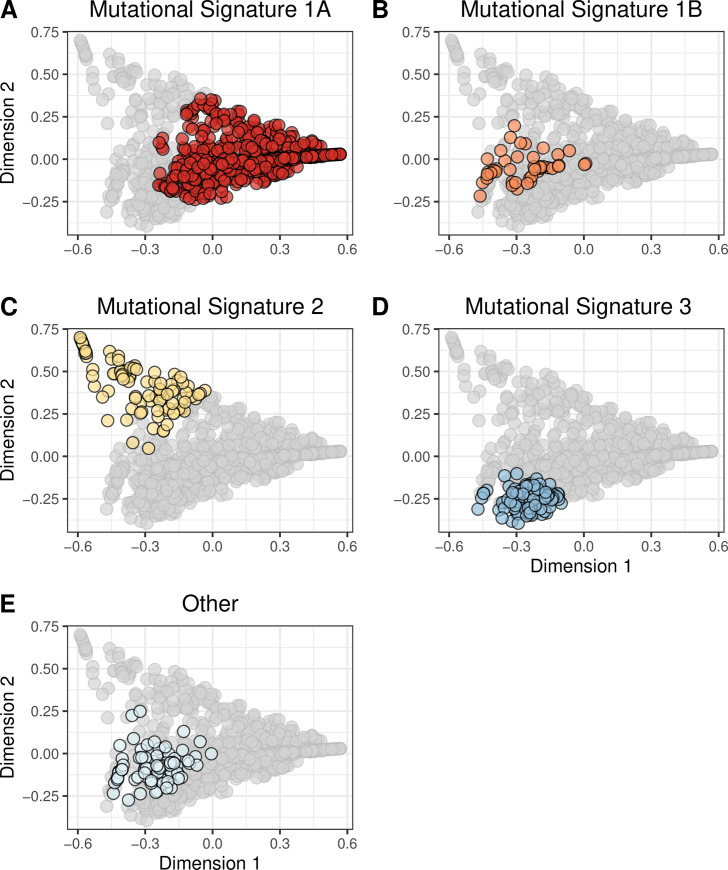
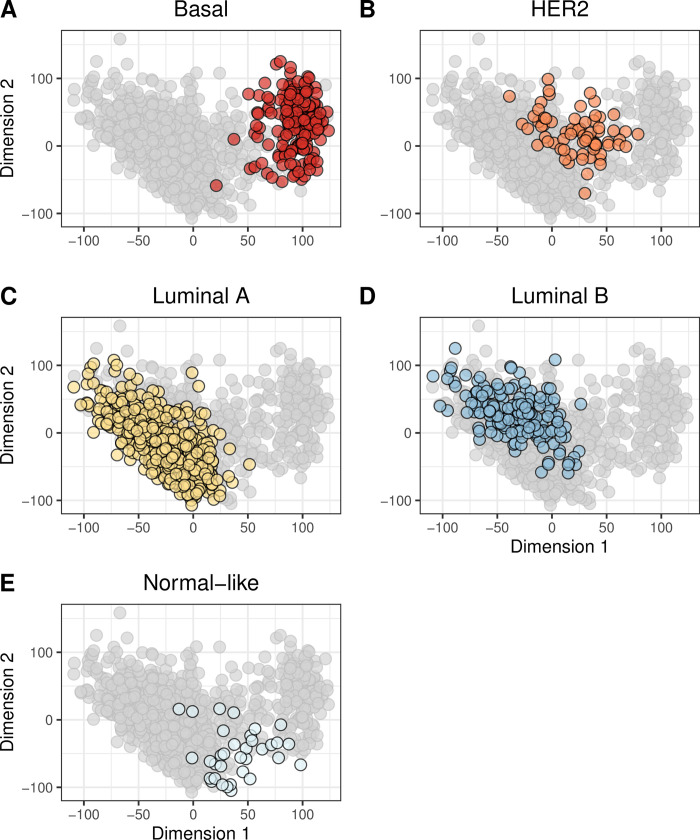
First, we identified the primary somatic-mutation signature associated with each TCGA breast-cancer patient. Approximately 91% of the patients were associated with somatic-mutation signature “1A” (n = 670), “1B” (n = 48), “2” (n = 98), or “3” (n = 130). The remaining patients were assigned to 12 other signatures (S8 Fig). Second, we identified the primary PAM50 gene-expression subtype associated with each patient. The Luminal A and Luminal B subtypes were most common, but each subtype was represented by at least 37 tumors (S9 Fig).
Although it is useful to evaluate the primary somatic-mutation signature or PAM50 subtype associated with each tumor, tumors are aggregates of multiple signatures and subtypes. To account for this diversity, we characterized the tumors based on 1) all 27 somatic-mutation signatures or 2) expression levels for all available genes. To enable easier interpretation of these profiles, we reduced dimensionality of the data using the MDS and t-SNE techniques (see Methods). Generally, tumors with the same primary somatic-mutation signature or PAM50 subtype clustered together in these visualizations (Figs 1 and 2; S10 and S11 Figs); however, in some cases, this did not happen. For example, the dimensionally reduced gene-expression profiles for Basal-like tumors formed a cluster that was mostly separate from the other tumors; but some Basal-like tumors were modestly distant from this cluster, and some Normal-like tumors clustered closely with the Basal-like tumors (Fig 2; S11 Fig). Tumors assigned to somatic-mutation “Signature 3” formed a cohesive cluster (Fig 1; S10 Fig), but some “Signature 3” tumors were modestly distant from this cluster. These observations highlight the importance of evaluating molecular profiles as a whole, not just using the primary category for each tumor.
Fig 1. Two-dimensional representation of somatic-mutation signatures using multidimensional scaling.
We summarized each tumor based on their somatic-mutation signatures, which represent overall mutational patterns in a trinucleotide context. We used multidimensional scaling (MDS) to reduce the data to two dimensions. Each point represents a single tumor, overlaid with colors that represent the tumor’s primary somatic-mutation signature. Mutational Signature 1A (A) was the most prevalent; these tumors were widely dispersed across the signature landscape. Signatures 1B (B), 2 (C), and 3 (D) were relatively small and formed cohesive clusters. The remaining 23 clusters were rare individually and were dispersed broadly.
Fig 2. Two-dimensional representation of gene-expression levels using multidimensional scaling.
We used multidimensional scaling (MDS) to reduce the gene-expression profiles to two dimensions. Each point represents a single tumor, overlaid with colors that represent the tumor’s primary PAM50 subtype. Generally, the PAM50 subtypes clustered cohesively, but there were exceptions. For example, some Basal-like tumors (A) exhbited expression patterns that differed considerably from the remaining Basal-like tumors. The normal-like tumors (E) showed the most variability in expression. This graph represents patients for whom we could identify a PAM50 subtype.
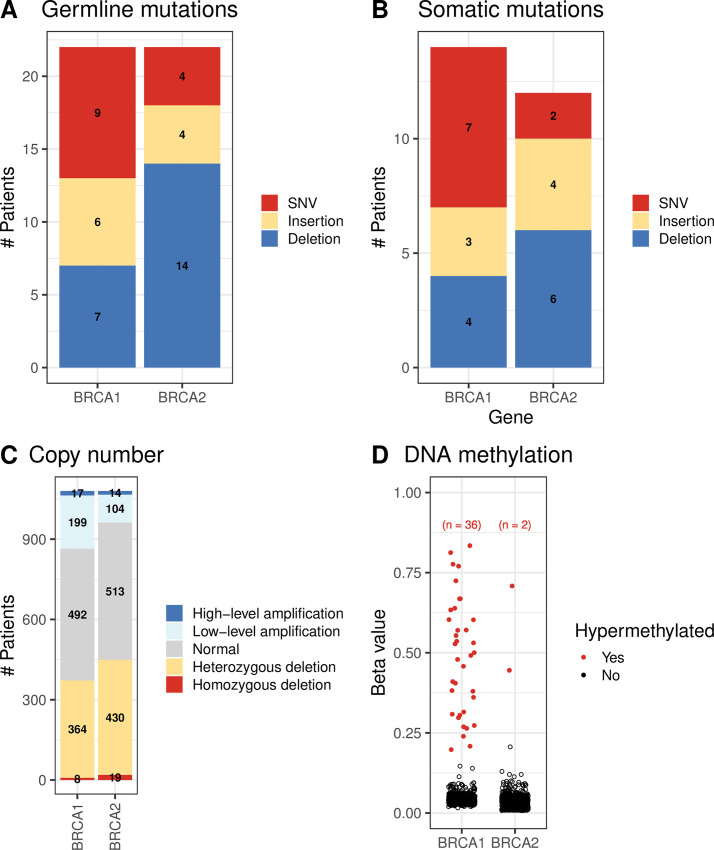
Aberrations in BRCA1 and BRCA2
Of 993 breast-cancer patients with available germline data, 22 harbored a pathogenic SNV or indel in BRCA1; 22 harbored a BRCA2 variant (Fig 3A). We were able to identify loss of heterozygosity (LOH) for all but 3 BRCA1 carriers and 7 BRCA2 carriers (S12 and S13 Figs). A somatic mutation, homozygous deletion, or hypermethylation event occurred in BRCA1 or BRCA2 for 80 patients (Fig 3B–3D). Most of these events were mutually exclusive with each other and with germline variants (S14 Fig).
Fig 3. Molecular aberrations in BRCA1 and BRCA2 across all breast-cancer patients.
A) Germline mutations, B) Somatic mutations, C) Copy-number variations, D) DNA methylation levels. SNV = single nucleotide variation.
BRCA1 carriers fell into the Basal (n = 17); Her2-enriched (n = 1), Luminal A (n = 2), and Luminal B (n = 1) gene-expression subtypes (S15 Fig) [22, 93, 94]. We were unable to assign a gene-expression subtype to one BRCA1 carrier due to missing data. Most BRCA2 carriers fell into the Luminal A subtype (n = 13); the remaining individuals were dispersed across the other subtypes. As demonstrated previously [19], the primary somatic-mutation signature for most BRCA1 and BRCA2 carriers was “Signature 3”; however, other signatures (especially “1A”) were also common (S16 Fig). S17 Fig shows the overlap between these two types of molecular profile.
Homogeneity of somatic mutation signature and expression profiles of germline BRCA1/2 carriers
The somatic-mutation signatures of BRCA1 germline carriers were more homogeneous than expected by chance (p = 0.00056; S18A, S19A and S20A Figs), as were those from BRCA2 carriers (p = 0.0003; S18B, S19B and S20B Figs). As an additional measure of homogeneity, we used logistic regression to predict BRCA aberration status based on the dimensionally reduced data. Using somatic-mutation signatures, we could predict the presence of BRCA1 germline mutations with a sensitivity of 0.72 and a specificity of 0.82. Additional classification results are shown in S2 Table.
None of the three BRCA1 carriers who lacked LOH events clustered closely with the remaining BRCA1 tumors (S18A and S19A Figs). Of the 7 BRCA2 tumors without detected LOH events, 3 clustered closely with the remaining BRCA2 tumors, while 4 did not (S18B and S19B Figs). It has been shown previously that germline BRCA1/BRCA2 mutations leave a recognizable imprint on a tumor’s mutational landscape [19]. This effect may be more consistent when a LOH event has occurred as a second “hit” within the same gene [97], but this was difficult to confirm with the available sample sizes.
Under the assumption that BRCA1/BRCA2 germline variants induce recognizable effects on tumor transcription, we assessed whether tumors from BRCA1/BRCA2 carriers have homogeneous gene-expression profiles. As expected based on the tumors’ primary PAM50 classification, 17 of 21 BRCA1 carriers (for whom we had gene-expression data) overlapped closely with the Basal-like subtype (S15 Fig). As a whole, the expression profiles for this group were more homogeneous than expected by chance (p = 0.0318; S21A, S22A and S23A Figs). However, expression values for BRCA2 carriers were not significantly homogeneous (p = 1.0; S23B Fig). Tumors from these individuals were dispersed across the gene-expression landscape (S21B and S22B Figs).
Similarities among individuals with BRCA1/BRCA2 aberrations
Next we evaluated similarities between BRCA1 and BRCA2 germline carriers. Somatic-mutation signatures for BRCA1 and BRCA2 carriers were highly similar to each other (p = 0.00014; S18A, S18B, S19A, S19B and S24A Figs). However, this pattern did not hold for gene-expression profiles. Although some BRCA2 carriers fell into the Basal-like gene-expression subtype, overall profiles for these patients were dissimilar to those from BRCA1 carriers (p = 1.0; S21A, S21B, S22A, S22B and S25A Figs).
Whether for somatic-mutation signatures or gene-expression profiles, tumors with BRCA1 hypermethylation were relatively homogeneous and highly similar to tumors from BRCA1 germline carriers (Table 1; S18G, S19G, S20G, S21G, S22G and S23G Figs). For gene-expression data, no other aberration type showed significant similarity to BRCA1 germline mutations. Somatic-mutation signatures from tumors with BRCA1 somatic mutations were significantly similar to those from BRCA1 germline mutations (Table 1). Only 2 tumors had BRCA2 hypermethylation, but the mutational signatures for these samples were significantly similar to tumors from BRCA2 germline carriers (p = 0.00054; S19H Fig). Likewise, tumors with a BRCA2 somatic mutation or homozygous deletion had mutational signatures that were similar to germline BRCA2 carriers (Table 1; S18D, S18F, S19D and S19F Figs). Aberrations in BRCA1 and BRCA2 appear to induce similar effects on somatic-mutation signatures—but not necessarily gene expression—whether those disruptions originate in the germline or via somatic events.
Table 1. Results of similarity comparisons among BRCA aberration groups.
We compared somatic-mutation signatures or gene-expression profiles between groups of patients who harbored aberrations in BRCA1 or BRCA2. We evaluated whether patients in one group (e.g., those who harbored a BRCA1 germline mutation) were more similar to patients in a second group (e.g., those with BRCA2 germline mutation) than random patient subsets of the same sizes. The numbers in this table represent empirical p-values from our resampling approach. In cases where an individual harbored an aberration in both comparison groups, we excluded that patient from the comparison. We used Holm’s method to correct for testing multiple hypotheses.
| Aberration Type 1 | Aberration Type 2 | Gene Expression | Mutational Signatures |
|---|---|---|---|
| BRCA1 germline mutation (n = 22) | BRCA2 germline mutation (n = 22) | 1.0 | 1.4e-04 |
| BRCA1 germline mutation (n = 22) | BRCA1 somatic mutation (n = 14) | 1.0 | 1.4e-04 |
| BRCA1 germline mutation (n = 22) | BRCA1 homozygous deletion (n = 8) | 1.0 | 0.30 |
| BRCA1 germline mutation (n = 22) | BRCA1 hypermethylation (n = 36) | 0.013 | 1.4e-04 |
| BRCA2 germline mutation (n = 22) | BRCA2 somatic mutation (n = 12) | 1.0 | 1.4e-04 |
| BRCA2 germline mutation (n = 22) | BRCA2 homozygous deletion (n = 19) | 1.0 | 1.4e-04 |
| BRCA2 germline mutation (n = 22) | BRCA2 hypermethylation (n = 2) | 1.0 | 5.4e-04 |
Evaluation of aberrations in other cancer-predisposing genes and clinical factors
Next we aggregated all patients who had any type of BRCA1 or BRCA2 aberration into a “BRCA-like reference group.” As a whole, mutational signatures for this group were more homogeneous than expected by chance (p = 0.00001; S26 Fig). We used this reference group to evaluate 59 other cancer-predisposition genes that might be associated with being BRCA-like. For the remaining evaluations, we used somatic-mutation signatures only.
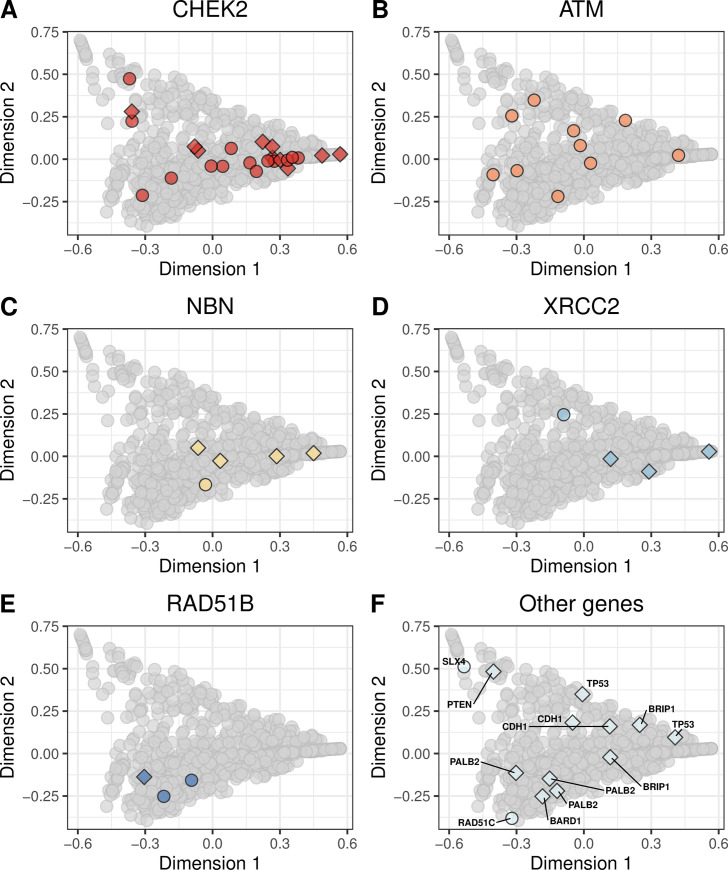
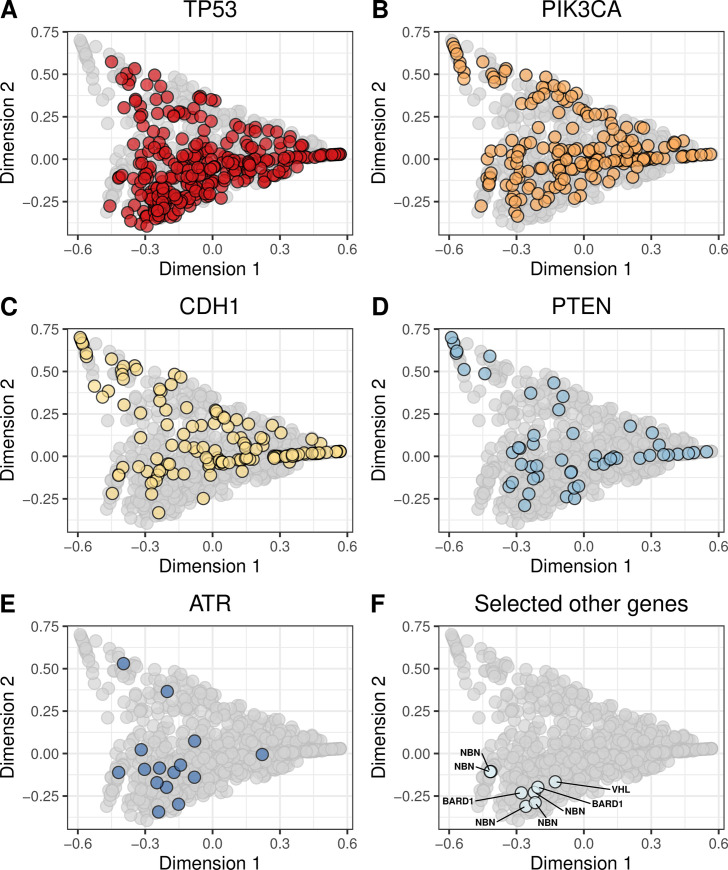
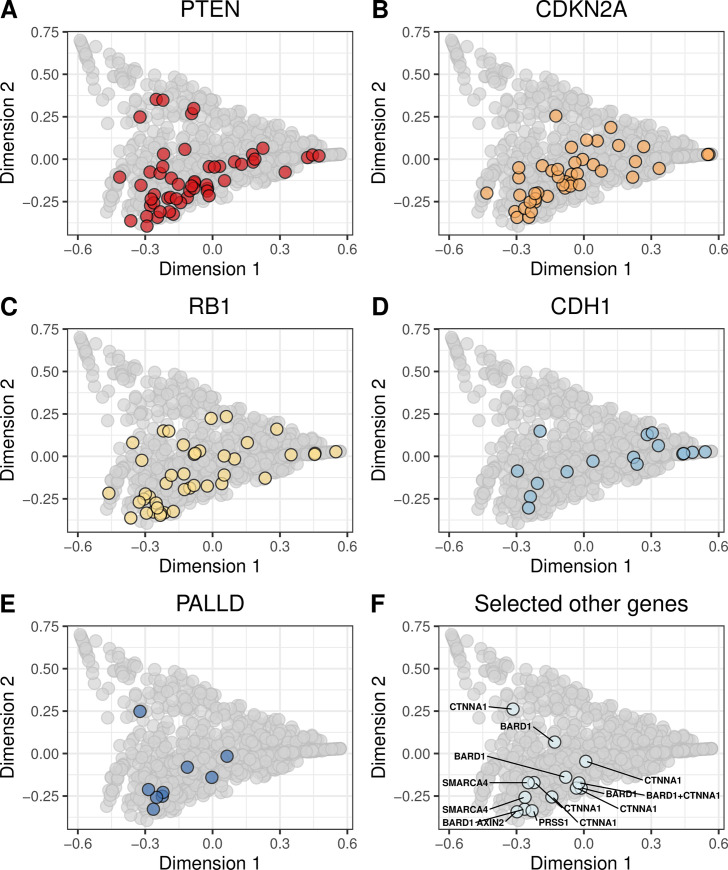
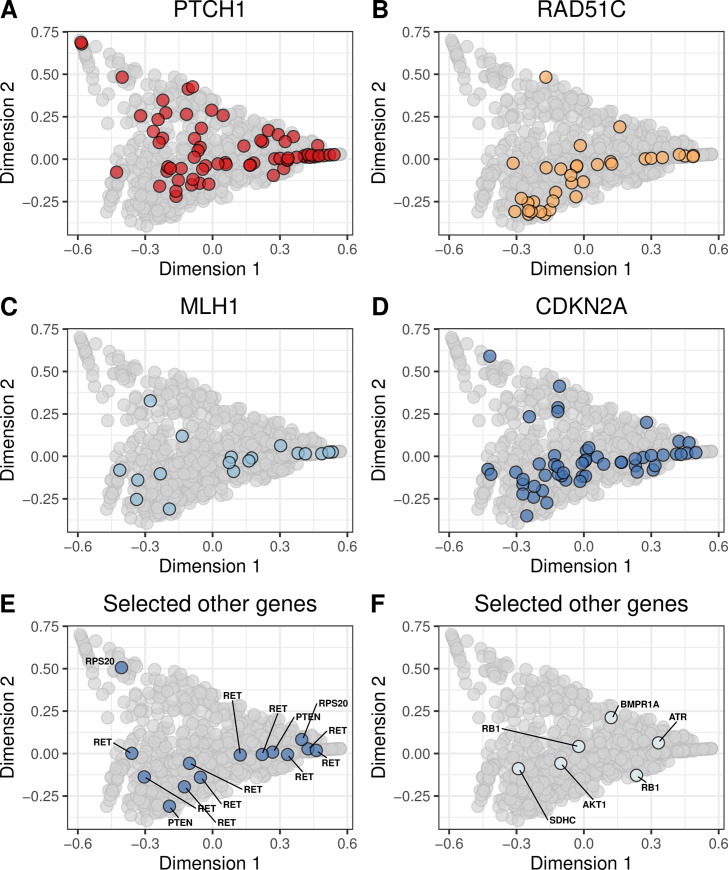
We evaluated whether molecular aberrations in the cancer-predisposition genes resulted in mutational signatures that were similar to our BRCA-like reference group. We found pathogenic and likely pathogenic germline mutations in 13 genes (ATM, BARD1, BRCA1, BRCA2, BRIP1, CDH1, CHEK2, NBN, PALB2, PTEN, RAD51B, RAD51C, SLX4, TP53, XRCC2). The most frequently mutated were CHEK2, ATM, and NBN (Fig 4; S27 and S28 Figs). We found potentially pathogenic somatic mutations in 55 genes, most frequently in TP53, PIK3CA, CDH1, and PTEN (Fig 5; S29 and S30 Figs). Homozygous deletions occurred most frequently in PTEN, CDKN2A, RB1, and CDH1 (Fig 6; S31 and S32 Figs). Hypermethylation occurred in 22 genes, most commonly GALNT12, PTCH1, CDKN2A, and RAD51C (Fig 7, S33 and S34 Figs). Using our resampling approach, we compared each aberration type in each gene against the BRCA-like reference group. In cases where an aberration overlapped between the reference and comparison groups, we excluded individuals who harbored both aberrations. For 11 genes (ATR, BARD1, CDKN2A, CTNNA1, PALB2, PALLD, PRSS1, RAD51B, SDHC, SMARCA4, VHL), at least one type of aberration attained statistical significance after multiple-testing correction (Table 2). A total of 8 aberrations occurred in BARD1: a germline mutation, 2 somatic mutations, and 5 homozygous deletions; as a group, these tumors were statistically similar to the BRCA-like reference group (p = 0.0018). ATR was mutated in 15 tumors and hypermethylated in 1 tumor; together, these tumors were statistically similar to the BRCA-like reference group (p = 0.0035). Tumors with an aberration in PRSS1 were also statistically similar to the BRCA-like reference group (p = 0.0069), but we only observed 2 aberrations in this gene. Other genes showed high similarity to the BRCA-like reference group for one type of aberration only; these included homozygous deletions in CDKN2A (n = 47; p = 0.00001), homozygous deletions in CTNNA1 (n = 6; p = 0.00004), germline mutations in PALB2 (n = 3; p = 0.00001), and homozygous deletions in PALLD (n = 9; p = 0.00001).
Fig 4. Non-BRCA germline mutations on the somatic-mutation signature landscape using multidimensional scaling.
Using the same two-dimensional representation of mutational signatures shown in Fig 1, this plot indicates which patients had germline mutations in non-BRCA cancer-predisposition genes. Diamond shapes indicate patients for whom no loss-of-heterozygosity was observed.
Fig 5. Non-BRCA somatic mutations on the somatic-mutation signature landscape using multidimensional scaling.
Using the same two-dimensional representation of mutational signatures shown in Fig 1, this plot indicates which patients had somatic mutations in non-BRCA cancer-predisposition genes. Diamond shapes indicate patients for whom no loss-of-heterozygosity was observed.
Fig 6. Non-BRCA homozygous deletions on the somatic-mutation signature landscape using multidimensional scaling.
Using the same two-dimensional representation of mutational signatures shown in Fig 1, this plot indicates which patients had homozygous deletions in non-BRCA cancer-predisposition genes. Diamond shapes indicate patients for whom no loss-of-heterozygosity was observed.
Fig 7. Non-BRCA hypermethylation events on the somatic-mutation signature landscape using multidimensional scaling.
Using the same two-dimensional representation of mutational signatures shown in Fig 1, this plot indicates which patients had hypermethylation events in non-BRCA cancer-predisposition genes. Diamond shapes indicate patients for whom no loss-of-heterozygosity was observed.
Table 2. Summary of comparisons between the BRCA-like reference group and groups of patients who harbored a specific type of aberration in a candidate BRCA-like gene.
We evaluated whether somatic-mutation signatures from patients who harbored a given type of aberration (e.g., BARD1 germline mutation) were more similar to the BRCA-like reference group than expected by random chance. The numbers in this table represent empirical p-values from our resampling approach. In cases where no patient had a given type of aberration in a given gene, we list “N/A”. The “Any” group represents individuals who harbored any type of aberration in a given gene. We used Holm’s method to correct for testing multiple hypotheses.
| Gene | Germline mutation | Somatic mutation | Homozygous deletion | Hypermethylation | Any |
|---|---|---|---|---|---|
| AKT1 | N/A | 1.0 (n = 21) | 1.0 (n = 3) | 0.13 (n = 1) | 1.0 (n = 25) |
| APC | N/A | 1.0 (n = 19) | 1.0 (n = 7) | N/A | 1.0 (n = 26) |
| ATM | 1.0 (n = 11) | 1.0 (n = 18) | 1.0 (n = 16) | N/A | 1.0 (n = 46) |
| ATR | N/A | 0.0018 (n = 15) | N/A | 1.0 (n = 1) | 0.0035 (n = 16) |
| AXIN2 | N/A | 1.0 (n = 6) | N/A | N/A | 1.0 (n = 7) |
| BAP1 | N/A | 1.0 (n = 6) | 1.0 (n = 7) | N/A | 1.0 (n = 13) |
| BARD1 | 0.0018 (n = 1) | 0.0018 (n = 2) | 0.054 (n = 5) | N/A | 0.0018 (n = 8) |
| BMPR1A | N/A | 1.0 (n = 2) | 1.0 (n = 8) | 1.0 (n = 1) | 1.0 (n = 11) |
| BRIP1 | 1.0 (n = 2) | 1.0 (n = 8) | N/A | N/A | 1.0 (n = 11) |
| CDH1 | 1.0 (n = 2) | 1.0 (n = 135) | 1.0 (n = 22) | N/A | 1.0 (n = 159) |
| CDK4 | N/A | 1.0 (n = 2) | N/A | N/A | 1.0 (n = 3) |
| CDKN2A | N/A | N/A | 0.0018 (n = 47) | 1.0 (n = 53) | 0.57 (n = 100) |
| CHEK1 | N/A | 1.0 (n = 4) | 1.0 (n = 16) | N/A | 1.0 (n = 20) |
| CHEK2 | 1.0 (n = 25) | 1.0 (n = 6) | 1.0 (n = 1) | N/A | 1.0 (n = 32) |
| CTNNA1 | N/A | 1.0 (n = 8) | 0.0069 (n = 6) | N/A | 1.0 (n = 14) |
| FAM175A | N/A | 0.085 (n = 2) | 1.0 (n = 3) | N/A | 0.055 (n = 5) |
| FH | N/A | 1.0 (n = 3) | 1.0 (n = 1) | N/A | 1.0 (n = 4) |
| FLCN | N/A | 1.0 (n = 2) | 1.0 (n = 8) | N/A | 1.0 (n = 10) |
| GALNT12 | N/A | 1.0 (n = 7) | 1.0 (n = 3) | 1.0 (n = 79) | 1.0 (n = 89) |
| GEN1 | N/A | 1.0 (n = 2) | 1.0 (n = 3) | N/A | 1.0 (n = 5) |
| GREM1 | N/A | 1.0 (n = 2) | 1.0 (n = 15) | N/A | 1.0 (n = 17) |
| HOXB13 | N/A | 1.0 (n = 3) | N/A | N/A | 1.0 (n = 4) |
| MEN1 | N/A | 1.0 (n = 9) | 1.0 (n = 3) | N/A | 1.0 (n = 13) |
| MLH1 | N/A | 1.0 (n = 13) | 1.0 (n = 4) | 1.0 (n = 19) | 1.0 (n = 36) |
| MRE11A | N/A | 1.0 (n = 2) | 1.0 (n = 8) | 1.0 (n = 2) | 1.0 (n = 12) |
| MSH2 | N/A | 1.0 (n = 4) | N/A | N/A | 1.0 (n = 5) |
| MSH6 | N/A | 1.0 (n = 7) | N/A | N/A | 1.0 (n = 8) |
| MUTYH | N/A | 1.0 (n = 3) | N/A | N/A | 1.0 (n = 3) |
| NBN | 1.0 (n = 5) | 1.0 (n = 5) | N/A | N/A | 1.0 (n = 10) |
| NF1 | N/A | 1.0 (n = 40) | 1.0 (n = 7) | N/A | 1.0 (n = 47) |
| NTHL1 | N/A | 1.0 (n = 1) | N/A | N/A | 1.0 (n = 1) |
| PALB2 | 0.0018 (n = 3) | 1.0 (n = 5) | N/A | N/A | 0.12 (n = 8) |
| PALLD | N/A | 1.0 (n = 6) | 0.0018 (n = 9) | 1.0 (n = 7) | 1.0 (n = 22) |
| PIK3CA | N/A | 1.0 (n = 190) | N/A | N/A | 1.0 (n = 191) |
| PMS2 | N/A | 1.0 (n = 5) | 0.49 (n = 1) | N/A | 1.0 (n = 6) |
| POLD1 | N/A | 1.0 (n = 3) | 1.0 (n = 2) | N/A | 1.0 (n = 6) |
| POLE | N/A | 0.091 (n = 16) | 1.0 (n = 4) | N/A | 0.33 (n = 20) |
| POT1 | N/A | 1.0 (n = 5) | 1.0 (n = 1) | N/A | 1.0 (n = 6) |
| PRKAR1A | N/A | 1.0 (n = 7) | N/A | N/A | 1.0 (n = 7) |
| PRSS1 | N/A | 1.0 (n = 1) | 0.0018 (n = 1) | N/A | 0.0069 (n = 2) |
| PTCH1 | N/A | 1.0 (n = 16) | 1.0 (n = 3) | 1.0 (n = 69) | 1.0 (n = 88) |
| PTEN | 1.0 (n = 1) | 1.0 (n = 51) | 0.30 (n = 56) | 1.0 (n = 2) | 1.0 (n = 110) |
| RAD51B | 0.0018 (n = 3) | 1.0 (n = 3) | 1.0 (n = 9) | N/A | 0.64 (n = 15) |
| RAD51C | 0.61 (n = 1) | 1.0 (n = 3) | 1.0 (n = 2) | 0.098 (n = 35) | 0.61 (n = 41) |
| RAD51D | N/A | 1.0 (n = 3) | 1.0 (n = 4) | N/A | 1.0 (n = 7) |
| RB1 | N/A | 1.0 (n = 19) | 1.0 (n = 45) | 1.0 (n = 2) | 1.0 (n = 66) |
| RET | N/A | 1.0 (n = 5) | 1.0 (n = 2) | 1.0 (n = 10) | 1.0 (n = 17) |
| RINT1 | N/A | 1.0 (n = 5) | N/A | N/A | 1.0 (n = 6) |
| RPS20 | N/A | N/A | N/A | 1.0 (n = 2) | 1.0 (n = 3) |
| SDHB | N/A | 1.0 (n = 1) | 1.0 (n = 7) | N/A | 1.0 (n = 9) |
| SDHC | N/A | N/A | N/A | 0.03 (n = 1) | 0.032 (n = 1) |
| SDHD | N/A | N/A | 1.0 (n = 16) | N/A | 1.0 (n = 16) |
| SLX4 | 1.0 (n = 1) | 1.0 (n = 10) | N/A | N/A | 1.0 (n = 12) |
| SMAD4 | N/A | 1.0 (n = 12) | 1.0 (n = 14) | N/A | 1.0 (n = 26) |
| SMARCA4 | N/A | 1.0 (n = 7) | 0.0018 (n = 2) | N/A | 1.0 (n = 9) |
| STK11 | N/A | 0.13 (n = 2) | 1.0 (n = 12) | N/A | 1.0 (n = 14) |
| TP53 | 1.0 (n = 2) | 1.0 (n = 302) | 1.0 (n = 15) | N/A | 1.0 (n = 319) |
| VHL | N/A | 0.0018 (n = 1) | 1.0 (n = 1) | N/A | 1.0 (n = 2) |
| XRCC2 | 1.0 (n = 4) | 1.0 (n = 3) | 1.0 (n = 4) | N/A | 1.0 (n = 11) |
Lastly, we evaluated whether the following data types were correlated with being BRCA-like: 1) unusually low mRNA expression in a given gene, 2) demographic, histopathological, and surgical observations, and 3) patient drug responses. First, we calculated the median Euclidean distance—based on somatic-mutation signatures—between each patient and the BRCA-like reference group. Then we used a two-sided Pearson correlation test to assess the relationship between these median distances and each candidate variable. In determining whether a tumor exhibited unusually low mRNA expression for a given gene, we used an outlier-detection technique (see Methods). Unusually low expression of BRCA1 (rho = 0.22, p = 0.0024) and RAD51C (rho = 0.20, p = 0.016) showed the strongest positive correlation with the reference group, whereas CDH1 (rho = -0.19, p = 0.023), PIK3CA (rho = -0.19, p = 0.025) and BARD1 (rho = -0.19, p = 0.028) showed the strongest negative correlation (S35 and S36 Figs). Triple-negative status and infiltrating ductal carcinoma histology were the most positively correlated clinical variables (S37 Fig). No chemotherapy treatment was significantly associated with being BRCA-like, though availability was limited for the drug data (n = 211; S38 Fig). Relationships among low mRNA expression and these factors are likely interwoven. For example, CDH1 expression has been associated with molecular subtypes such as triple-negative status [98]. Larger studies will be necessary to disentangle these effects.
Discussion
The concept of being BRCA-like has traditionally focused on tumors aberrations, under the hypothesis that their effects are similar to those of germline BRCA1 and BRCA2 mutations [31]. We evaluated this hypothesis for somatic mutations, homozygous deletions, and hypermethylation events in BRCA1 and BRCA2. Corroborating prior evidence [21, 33], we found that tumors with these aberration types had somatic-mutation signatures that were similar to those of germline carriers. Using this group as a reference, we evaluated each aberration type, as well as germline mutations, in 59 other cancer-predisposition genes in search of additional criteria that might be indicators of being BRCA-like. This search identified previously known associations with being BRCA-like, including germline mutations in PALB2 [21] and somatic mutations in ATR [32]. However, for a gene to be considered a strong candidate for inclusion in the BRCA-like definition, we required evidence of similarity across all available molecular data types. BARD1 and ATR met these criteria. Both genes interact directly with BRCA1 to help repair double-stranded breaks and control G1/S cell-cycle arrest [99]. Experimental evidence lends support to the hypothesis that inactivation of these genes has relevance to being BRCA-like. For example, in mice, inactivation of the Bard1 protein induces mammary tumors that are indistinguishable from tumors that result from Brca1 knock-out [100]. In triple-negative breast cancers, ATR inhibitors are highly efficient in patient-derived xenografts that have a BRCA1 mutation or that exhibit the BRCA-like phenocopy when combined with irinotecan, a clinically approved topoisomerase 1 inhibitor that causes double-stranded breaks [101].
Interestingly, other genes known to play a role in DNA damage repair [102]–including ATM, CHEK2, and RAD51C—did not attain statistical significance for any aberration type. The family-wise method we used to correct for multiple testing is generally conservative [90]. Accordingly, our results likely erred on the side of specificity rather than sensitivity for estimating whether a given gene should be considered a candidate for the BRCA-like category. This may explain why RAD51C hypermethylation, for example, did not reach statistical significance in our analysis, even though it has been highlighted in other studies [21, 33].
When using gene-expression profiles to characterize being BRCA-like, we observed a clear relationship between BRCA1 aberrations and the “Basal-like” gene-expression subtype, confirming prior findings [22–25]. Our findings extended to triple-negative tumors, again confirming prior evidence [26, 27]. Hedenfalk, et al. demonstrated that breast tumors from BRCA1 and BRCA2 carriers exhibit gene-expression patterns that are distinct from each other [103]; our analysis confirmed these findings. Rice, et al. identified correlations between transcriptional inactivation of BRCA1 and either germline mutations or hypermethylation of the same gene [104]. Considering potential effects across the transcriptome, our analysis provided additional evidence that gene-expression profiles from tumors of BRCA1 germline carriers are highly similar to tumors with BRCA1 hypermethylation. These findings did not extend to BRCA2. Moelans, et al. found that BRCA2 hypermethylation occurs frequently in ductal carcinoma in situ lesions and in adjacent invasive ductal cancer cells [105]; however, we identified only 2 samples that were hypermethylated for this gene.
Although gene-expression data may be less useful than somatic-mutation signatures for characterizing the effects of HR defects, they may hold promise as predictive biomarkers for specific patient subgroups. For example, Tutt, et al. observed that triple-negative hormone status was a reliable biomarker of objective treatment responses to carboplatin [106]. Severson, et al. treated HER2-negative patients with a combination of veliparib, a PARP inhibitor, and carboplatin, a platinum agent, in a neoadjuvant setting. In addition, they derived a gene-expression signature that characterized “BRCA1ness” and found that this signature was associated with response to this combination therapy [28]. In ovarian tumors, Konstantinopoulos, et al. derived a gene-expression signature that distinguished “BRCA-like” from “non–BRCA-like” samples and used this signature to accurately predict sensitivity or resistance to a platinum agent and a PARP inhibitor in patient-derived specimens [29]. Finally, Mulligan, et al. developed a 44-gene assay and showed that differences in expression of these genes between BRCA1/BRCA2 mutant and sporadic tumors were predictive of response to DNA-damaging agents [107]. We attempted to replicate these findings with TCGA data, but sample sizes were too small on a per-drug basis.
Davies, et al. aimed to develop a BRCA-like biomarker using somatic-mutation signatures [33]. Using a lasso logistic-regression model, they were able to identify aberrant BRCA1/BRCA2 tumors with near perfect accuracy and then extended their approach to identify tumors with an apparent functional HR deficiency that lacked known aberrations in these genes. In contrast, we focused on identifying candidate BRCA-like genes, rather than to develop a predictive biomarker for being BRCA-like itself (or for treatment responses). By identifying such genes, we aimed to provide insights into possible mechanisms of being BRCA-like. Such insights might indirectly be useful for predicting sensitivity to PARP inhibitors or platinum agents, although this connection is still tenuous [32, 108]. Polak, et al. used an alternative methodology to ours, associating somatic-mutation signatures with genomic aberrations in TCGA breast-cancer samples; they identified some of the same relationships that we identified [21]. However, our analysis extended to additional genes and factors, including extremely low-expressing genes and clinical variables. In addition, we explicitly compared the effects on somatic-mutation signatures of BRCA1 versus BRCA2 aberrations.
Different types of aberration may result in different downstream effects; however, these differences may result from technical challenges in identifying and filtering variants. Determining which genmic aberrations are pathogenic remains a challenging task [109], so it is likely that more- or less-stringent filtering of candidate aberrations would lead to more accurate results. In addition, we could not always determine whether mono- or bi-allelic inactivation of a given gene had occurred in a given tumor; mono-allelic inactivation may be insufficient to impair HR function [56].
Finally, we note methodological issues. To enable easier visualization, we reduced the molecular signatures to two dimensions. We also used the dimensionally reduced data as input to our statistical resampling approach. Accordingly, even though the number of original input variables was much larger for the gene-expression data, this approach enabled us to perform a more consistent comparison between the two data types. However, reducing the data to this extent likely failed to capture much of the biological signal in the data for either data type. Further refining this approach may help to strike a better balance between data interpretability and adequate data representation [110].
Supporting information
This tumor had a large proportion of C>T mutations, which are representative of Signature 3.
(PDF)
This tumor had a large proportion of C>T mutations, which are representative of Signature 3.
(PDF)
We extracted probe-level methylation (beta) values for all available breast-cancer samples in TCGA and plotted them relative to the transcription start site of each gene. These graphs illustrate beta values for four genes (BRCA1, BRCA2, PTEN, and RAD51C) and two microarray platforms (Illumina HumanMethylation 27K and 450K). Values in parenthesis indicate distance from the transcription start site (TSS). TSS distances marked as “NA” were unavailable. The 27K arrays have fewer probes per gene. In general, probes near the TSS exhibited relatively low methylation levels for these genes, whereas probes further from the TSS were more highly methylated. These observations are consistent with the assumption that most genes would be “on” by default. Some exceptions to this pattern are apparent (for example, cg13782816 on panel C); these exceptions may be caused by mismapped probes, cross hybridization, or misannotations. We calculated gene-level values as the median across all probes that were within 300 nucleotides of the TSS.
(PDF)
We used an outlier-detection methodology to estimate which tumors were hypermethylated for a given gene. This scatter plot illustrates the model fit for BRCA1. Asterisks represent tumors considered to be outliers.
(PDF)
We used an outlier-detection methodology to estimate which tumors were hypermethylated for a given gene. This scatter plot illustrates the model fit for BRCA2. Asterisks represent tumors considered to be outliers.
(PDF)
We used an outlier-detection methodology to estimate which tumors were hypermethylated for a given gene. This scatter plot illustrates the model fit for PTEN. Asterisks represent tumors considered to be outliers.
(PDF)
We used an outlier-detection methodology to estimate which tumors were hypermethylated for a given gene. This scatter plot illustrates the model fit for RAD51C. Asterisks represent tumors considered to be outliers.
(PDF)
Each TCGA breast-cancer patient was assigned to a primary somatic-mutation signature based on exome-wide mutational patterns. This plot illustrates the frequency of each somatic-mutation signature across all the patients.
(PDF)
Each TCGA breast-cancer patient was assigned to a primary PAM50 subtype based on tumor gene-expression levels. This plot illustrates the frequency of each PAM50 subtype across all the patients.
(PDF)
We summarized each tumor based on their somatic-mutation signatures, which represent overall mutational patterns in a trinucleotide context. We used the t-distributed Stochastic Neighbor Embedding (t-SNE) method to reduce the data to two dimensions. Each point represents a single tumor, overlaid with colors that represent the tumor’s primary somatic-mutation signature. Mutational Signature 1A (A) was the most prevalent; these tumors were widely dispersed across the signature landscape. Signatures 1B (B), 2 (C), and 3 (D) were relatively small and formed cohesive clusters. The remaining 23 clusters were rare individually and were dispersed broadly.
(PDF)
We used the t-distributed Stochastic Neighbor Embedding (t-SNE) method to reduce the gene-expression profiles to two dimensions. Each point represents a single tumor, overlaid with colors that represent the tumor’s primary PAM50 subtype. Generally, the PAM50 subtypes clustered cohesively, but there were exceptions. For example, some Basal-like tumors (A) exhbited expression patterns that differed considerably from the remaining Basal-like tumors. The normal-like tumors (E) showed the most variability in expression. This graph represents patients for whom we could identify a PAM50 subtype.
(PDF)
A total of 22 patients carried a germline mutation in BRCA1. We detected loss-of-heterozygosity events in tumors for all but 3 of these patients. Data are only shown for patients for whom we had both types of data.
(PDF)
A total of 22 patients carried a germline mutation in BRCA2. We detected loss-of-heterozygosity events in tumors from all but 7 of these patients. Data are only shown for patients for whom we had both types of data.
(PDF)
This graph indicates how many patients had each type of molecular aberration and the level of overlap among these aberrations within a given patient. In most cases, these aberrations were mutually exclusive from each other; however, some overlap did occur. For example, one patient had a somatic mutation in BRCA1 and hypermethylation of the same gene. This graph only depicts patients for whom all four types of molecular data were available.
(PDF)
Gene-expression subtypes were unavailable for some patients; One BRCA1 carrier is not represented in this figure; we could not assign a gene-expression subtype to this individual due to missing data.
(PDF)
This graph represents patients for whom we had both germline- and somatic-mutation data.
(PDF)
This graph represents patients for whom we could evaluate the status of both PAM50 subtype and somatic-mutation signatures.
(PDF)
Using the same two-dimensional representation of mutational signatures shown in Fig 1, this plot indicates which patients had germline mutations (A, B), somatic mutations (C, D), homozygous deletions (E, F), or hypermethylation events (G, H) in BRCA1 and BRCA2, respectively. Largely, these tumors had similar somatic-mutation signatures. Diamond shapes indicate patients for whom no loss-of-heterozygosity was observed. Data are shown for all patients, even those for whom we did not have all types of data.
(PDF)
Using the same two-dimensional representation of mutational signatures shown in S10 Fig, this plot indicates which patients had germline mutations (A, B), somatic mutations (C, D), homozygous deletions (E, F), or hypermethylation events (G, H) in BRCA1 and BRCA2, respectively. Largely, these tumors had similar somatic-mutation signatures. Diamond shapes indicate patients for whom no* loss-of-heterozygosity was observed. Data are shown for all patients, even those for whom we did not have all types of data.
(PDF)
We calculated the Euclidean distance between each pair of individuals who had germline mutations (A, B), somatic mutations (C, D), homozygous deletions (E, F), or hypermethylation events (G, H) in BRCA1 or BRCA2; the medians of these distances are illustrated using vertical, dashed lines. We then randomized the patient identifiers and calculated pairwise distances for the same number of randomly selected patients, which resulted in an empirical null distribution. We calculated p-values by comparing the actual distances against the randomized distances and then adjusted for multiple tests using Holm’s method.
(PDF)
Using the same two-dimensional representation of gene-expression profiles shown in Fig 2, this plot indicates which patients had germline mutations (A, B), somatic mutations (C, D), homozygous deletions (E, F), or hypermethylation events (G, H) in BRCA1 and BRCA2, respectively. Many of these tumors overlapped with the Basal-like subtype, but other tumors were dispersed broadly across the gene-expression landscape. Diamond shapes indicate patients for whom no loss-of-heterozygosity was observed. Data are shown for all patients, even those for whom we did not have all types of data.
(PDF)
Using the same two-dimensional representation of gene-expression profiles shown in S11 Fig, this plot indicates which patients had germline mutations (A, B), somatic mutations (C, D), homozygous deletions (E, F), or hypermethylation events (G, H) in BRCA1 and BRCA2, respectively. Many of these tumors overlapped with the Basal-like subtype, but other tumors were dispersed broadly across the gene-expression landscape. Diamond shapes indicate patients for whom no loss-of-heterozygosity was observed. Data are shown for all patients, even those for whom we did not have all types of data.
(PDF)
We calculated the Euclidean distance between each pair of individuals who had germline mutations (A, B), somatic mutations (C, D), homozygous deletions (E, F), or hypermethylation events (G, H) in BRCA1 or BRCA2; the medians of these distances are illustrated using vertical, dashed lines. We then randomized the patient identifiers and calculated pairwise distances for the same number of randomly selected patients, which resulted in an empirical null distribution. We calculated p-values by comparing the actual distances against the randomized distances and then adjusted for multiple tests using Holm’s method.
(PDF)
We identified patients who had a germline mutation in BRCA1 or BRCA2 and compared them against each other (A), those with a somatic mutation in the same gene (B-C), those with a homozygous deletion in the same gene (D-E) and those with DNA hypermethylation of the same gene (F-G). We calculated the Euclidean distance between each pair of individuals in these groups; these distances are illustrated using vertical, dashed lines. We then randomized the patient identifiers and calculated pairwise distances for groups of randomly selected patients, which resulted in an empirical null distribution. We calculated p-values by comparing the actual distances against the randomized distances.
(PDF)
We identified patients who had a germline mutation in BRCA1 or BRCA2 and compared them against each other (A), those with a somatic mutation in the same gene (B-C), those with a homozygous deletion in the same gene (D-E) and those with DNA hypermethylation of the same gene (F-G). We calculated the Euclidean distance between each pair of individuals in these groups; these distances are illustrated using vertical, dashed lines. We then randomized the patient identifiers and calculated pairwise distances for groups of randomly selected patients, which resulted in an empirical null distribution. We calculated p-values by comparing the actual distances against the randomized distances.
(PDF)
We calculated the Euclidean distance between each pair of individuals who had a germline mutation, somatic mutation, homozygous deletion, and/or hypermethylation event in BRCA1 and/or BRCA2; the median of these distances is illustrated using a vertical, dashed line. We then randomized the patient identifiers and calculated pairwise distances for the same number of randomly selected patients, which resulted in an empirical null distribution. We calculated a p-value by comparing the actual distance against the randomized distances.
(PDF)
This graph omits genes in which we observed no germline mutations. SNV = single-nucleotide variant.
(PDF)
Using the same two-dimensional representation of mutational signatures shown in S10 Fig, this plot indicates which patients had germline mutations in non-BRCA cancer-predisposition genes. Diamond shapes indicate patients for whom no loss-of-heterozygosity was observed.
(PDF)
This graph omits genes in which we observed no somatic mutations.
(PDF)
Using the same two-dimensional representation of mutational signatures shown in S10 Fig, this plot indicates which patients had somatic mutations in non-BRCA cancer-predisposition genes. Diamond shapes indicate patients for whom no loss-of-heterozygosity was observed.
(PDF)
This graph omits genes in which we observed no homozygous deletions.
(PDF)
Using the same two-dimensional representation of mutational signatures shown in S10 Fig, this plot indicates which patients had homozygous deletions in non-BRCA cancer-predisposition genes. Diamond shapes indicate patients for whom no loss-of-heterozygosity was observed.
(PDF)
Tumors that we classified as having hypermethylation events are highlighted as red points. This graph omits genes in which we observed no hypermethylation events.
(PDF)
Using the same two-dimensional representation of mutational signatures shown in S10 Fig, this plot indicates which patients had hypermethylation events in non-BRCA cancer-predisposition genes. Diamond shapes indicate patients for whom no loss-of-heterozygosity was observed.
(PDF)
For each gene, we identified tumors that expressed these genes at relatively low levels compared to other breast tumors; these low expressors are highlighted as red points.
(PDF)
We identified tumors with low expression for cancer-predisposition genes (see S35 Fig) and evaluated whether the somatic-mutation signatures of these tumors were relatively similar or dissimilar to the BRCA reference group. Each red rectangle represents a patient sample that expressed a given gene at low levels. Low expression of RAD51C and BRCA1 showed the strongest positive correlation between gene-expression status and the BRCAness reference group. Low expression of BARD1 and CDH1 showed the strongest negative correlation between gene-expression status and the BRCAness reference group. Genes for which no tumors exhibited low expression are omitted.
(PDF)
Red rectangles indicate patients that were positive for each respective clinical characteristic. Tumors with triple-negative hormone receptors, infiltrating ductal carcinoma histologies, or close surgical margins overlapped most with BRCA-aberrant tumors based on somatic-mutation signatures.
(PDF)
We evaluated clinical treatment responses for 211 TCGA patients for whom drug-response data were available. Responses for none of the drugs were significantly correlated with BRCA aberration status based on somatic-mutation signatures.
(PDF)
We evaluated somatic mutations in BRCA1 and BRCA2 based on variant type, predicted effects on protein sequence, evolutionary conservation, minor allele frequency, evidence in ClinVar, etc. This table provides information about each variant and specified criteria that we considered. A value of 1 in the Pathogenicity column indicates that we considered the variant to be pathogenic in our analyses.
(DOCX)
Via cross validation, we used gene-expression profiles and somatic-mutation signatures, respectively, to predict whether a given patient/tumor harbored particular types of aberrations. Sensitivity is equivalent to the true-positive rate. Specificity is equivalent to the true-negative rate. The area under the receiver operator characteristic curve (AUROC) quantifies the balance between sensitivity and specificity across a range of prediction thresholds.
(DOCX)
Acknowledgments
Results from this study are in part based upon data generated by TCGA and managed by the United States National Cancer Institute and National Human Genome Research Institute (see http://cancergenome.nih.gov). We thank the patients who participated in this study and shared their data publicly. We thank the Fulton Supercomputing Laboratory at Brigham Young University for providing computational facilities.
Data Availability
The datasets generated and analyzed during the current study are available in the Open Science Framework repository (https://osf.io/9jhr2). These data were generated by third parties; we did not play a role in generating the data but rather used it for secondary research. Furthermore, we did not have any special access privileges to the data; we obtained the data in the ways stated in this article. We are not permitted to share the germline-mutation data, but researchers can request access via the TCGA data access committee (https://www.cancer.gov/about-nci/organization/ccg/research/structural-genomics/tcga/contact).
Funding Statement
Funding for this study was provided through Brigham Young University Graduate Studies and the Simmons Center for Cancer Research. In addition, we acknowledge grant support from NIH 1R35CA197458, Komen Foundation SAC110020, and Breast Cancer Research Foundation BCRF18-088.
References
- 1.Hall JM, Lee MK, Newman B, Morrow JE, Anderson LA, Huey B, et al. Linkage of early-onset familial breast cancer to chromosome 17q21. Science. 1990. December;250(4988):1684–9. 10.1126/science.2270482 [DOI] [PubMed] [Google Scholar]
- 2.Moynahan ME, Chiu JW, Koller BH, Jasin M. Brca1 Controls Homology-Directed DNA Repair. Molecular Cell. 1999. October;4(4):511–8. 10.1016/s1097-2765(00)80202-6 [DOI] [PubMed] [Google Scholar]
- 3.Stratton MR, Rahman N. The emerging landscape of breast cancer susceptibility. Nat Genet. 2008. January;40(1):17–22. 10.1038/ng.2007.53 [DOI] [PubMed] [Google Scholar]
- 4.John EM, Miron A, Gong G, Phipps AI, Felberg A, Li FP, et al. Prevalence of pathogenic BRCA1 mutation carriers in 5 US racial/ethnic groups. JAMA. 2007. December;298(24):2869–76. 10.1001/jama.298.24.2869 [DOI] [PubMed] [Google Scholar]
- 5.Malone KE, Daling JR, Doody DR, Hsu L, Bernstein L, Coates RJ, et al. Prevalence and predictors of BRCA1 and BRCA2 mutations in a population-based study of breast cancer in white and black American women ages 35 to 64 years. Cancer Res. 2006. August;66(16):8297–308. 10.1158/0008-5472.CAN-06-0503 [DOI] [PubMed] [Google Scholar]
- 6.Li X, Heyer W-D. Homologous recombination in DNA repair and DNA damage tolerance. Cell Res. 2008. January;18(1):99–113. 10.1038/cr.2008.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Donovan PJ, Livingston DM. BRCA1 and BRCA2: Breast/ovarian cancer susceptibility gene products and participants in DNA double-strand break repair. Carcinogenesis. 2010. June;31(6):961–7. 10.1093/carcin/bgq069 [DOI] [PubMed] [Google Scholar]
- 8.Lord CJ, Ashworth A. The DNA damage response and cancer therapy. Nature. 2012. January;481(7381):287–94. 10.1038/nature10760 [DOI] [PubMed] [Google Scholar]
- 9.Tutt A, Bertwistle D, Valentine J, Gabriel A, Swift S, Ross G, et al. Mutation in Brca2 stimulates error-prone homology-directed repair of DNA double-strand breaks occurring between repeated sequences. EMBO J. 2001. September;20(17):4704–16. 10.1093/emboj/20.17.4704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xia F, Taghian DG, DeFrank JS, Zeng ZC, Willers H, Iliakis G, et al. Deficiency of human BRCA2 leads to impaired homologous recombination but maintains normal nonhomologous end joining. Proc Natl Acad Sci USA. 2001. July;98(15):8644–9. 10.1073/pnas.151253498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moynahan ME, Pierce AJ, Jasin M. BRCA2 is required for homology-directed repair of chromosomal breaks. Mol Cell. 2001. February;7(2):263–72. 10.1016/s1097-2765(01)00174-5 [DOI] [PubMed] [Google Scholar]
- 12.Moore K, Colombo N, Scambia G, Kim B-G, Oaknin A, Friedlander M, et al. Maintenance Olaparib in Patients with Newly Diagnosed Advanced Ovarian Cancer. N Engl J Med. 2018. December;379(26):2495–505. 10.1056/NEJMoa1810858 [DOI] [PubMed] [Google Scholar]
- 13.Robson M, Im S-A, Senkus E, Xu B, Domchek SM, Masuda N, et al. Olaparib for Metastatic Breast Cancer in Patients with a Germline BRCA Mutation. N Engl J Med. 2017. August;377(6):523–33. 10.1056/NEJMoa1706450 [DOI] [PubMed] [Google Scholar]
- 14.Litton JK, Rugo HS, Ettl J, Hurvitz SA, Gonçalves A, Lee K-H, et al. Talazoparib in Patients with Advanced Breast Cancer and a Germline BRCA Mutation. N Engl J Med. 2018. August;379(8):753–63. 10.1056/NEJMoa1802905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Commissioner O of the. Press Announcements—FDA approves first treatment for breast cancer with a certain inherited genetic mutation. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm592347.htm.
- 16.Tutt A, Robson M, Garber JE, Domchek SM, Audeh MW, Weitzel JN, et al. Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and advanced breast cancer: A proof-of-concept trial. Lancet. 2010. July;376(9737):235–44. 10.1016/S0140-6736(10)60892-6 [DOI] [PubMed] [Google Scholar]
- 17.Fong PC, Boss DS, Yap TA, Tutt A, Wu P, Mergui-Roelvink M, et al. Inhibition of poly(ADP-ribose) polymerase in tumors from BRCA mutation carriers. N Engl J Med. 2009. July;361(2):123–34. 10.1056/NEJMoa0900212 [DOI] [PubMed] [Google Scholar]
- 18.Nik-Zainal S, Alexandrov LB, Wedge DC, Van Loo P, Greenman CD, Raine K, et al. Mutational Processes Molding the Genomes of 21 Breast Cancers. Cell. 2012. May;979–93. 10.1016/j.cell.2012.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alexandrov LB, Nik-Zainal S, Wedge DC, Aparicio SAJR, Behjati S, Biankin AV, et al. Signatures of mutational processes in human cancer. Nature. 2013. August;500(7463):415–21. 10.1038/nature12477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zou X, Owusu M, Harris R, Jackson SP, Loizou JI, Nik-Zainal S. Validating the concept of mutational signatures with isogenic cell models. Nat Commun. 2018. May;9(1):1744 10.1038/s41467-018-04052-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Polak P, Kim J, Braunstein LZ, Karlic R, Haradhavala NJ, Tiao G, et al. A mutational signature reveals alterations underlying deficient homologous recombination repair in breast cancer. Nat Genet. 2017. October;49(10):1476–86. 10.1038/ng.3934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sorlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci U A. 2001;98(19):10869–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Foulkes WD, Stefansson IM, Chappuis PO, Bégin LR, Goffin JR, Wong N, et al. Germline BRCA1 mutations and a basal epithelial phenotype in breast cancer. J Natl Cancer Inst. 2003. October;95(19):1482–5. 10.1093/jnci/djg050 [DOI] [PubMed] [Google Scholar]
- 24.Lee E, McKean-Cowdin R, Ma H, Spicer DV, Van Den Berg D, Bernstein L, et al. Characteristics of triple-negative breast cancer in patients with a BRCA1 mutation: Results from a population-based study of young women. J Clin Oncol. 2011. November;29(33):4373–80. 10.1200/JCO.2010.33.6446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koboldt DC, Fulton RS, McLellan MD, Schmidt H, Kalicki-Veizer J, McMichael JF, et al. Comprehensive molecular portraits of human breast tumours. Nature. 2012. October;490(7418):61–70. 10.1038/nature11412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sørlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci U A. 2003. July;100(14):8418–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Foulkes WD, Brunet J-S, Stefansson IM, Straume O, Chappuis PO, Bégin LR, et al. The prognostic implication of the basal-like (cyclin E high/p27 low/p53+/glomeruloid-microvascular-proliferation+) phenotype of BRCA1-related breast cancer. Cancer Res. 2004. February;64(3):830–5. 10.1158/0008-5472.can-03-2970 [DOI] [PubMed] [Google Scholar]
- 28.Severson TM, Wolf DM, Yau C, Peeters J, Wehkam D, Schouten PC, et al. The BRCA1ness signature is associated significantly with response to PARP inhibitor treatment versus control in the I-SPY 2 randomized neoadjuvant setting. Breast Cancer Research. 2017. August;19(1):99 10.1186/s13058-017-0861-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Konstantinopoulos PA, Spentzos D, Karlan BY, Taniguchi T, Fountzilas E, Francoeur N, et al. Gene Expression Profile of BRCAness That Correlates With Responsiveness to Chemotherapy and With Outcome in Patients With Epithelial Ovarian Cancer. JCO. 2010. June;28(22):3555–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wood LD, Parsons DW, Jones S, Lin J, Sjöblom T, Leary RJ, et al. The genomic landscapes of human breast and colorectal cancers. Science. 2007. November;318(5853):1108–13. 10.1126/science.1145720 [DOI] [PubMed] [Google Scholar]
- 31.Turner N, Tutt A, Ashworth A. Hallmarks of ‘BRCAness’ in sporadic cancers. Nat Rev Cancer. 2004. October;4(10):814–9. 10.1038/nrc1457 [DOI] [PubMed] [Google Scholar]
- 32.Lord CJ, Ashworth A. BRCAness revisited. Nat Rev Cancer. 2016. February;16(2):110–20. 10.1038/nrc.2015.21 [DOI] [PubMed] [Google Scholar]
- 33.Davies H, Glodzik D, Morganella S, Yates LR, Staaf J, Zou X, et al. HRDetect is a predictor of BRCA1 and BRCA2 deficiency based on mutational signatures. Nat Med. 2017. April;23(4):517–25. 10.1038/nm.4292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Woodward AM, Davis TA, Silva AGS, Kirk JA, Leary JA. Large genomic rearrangements of both BRCA2 and BRCA1 are a feature of the inherited breast/ovarian cancer phenotype in selected families. J Med Genet. 2005. May;42(5):e31–1. 10.1136/jmg.2004.027961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hogervorst FBL, Nederlof PM, Gille JJP, McElgunn CJ, Grippeling M, Pruntel R, et al. Large Genomic Deletions and Duplications in the BRCA1 Gene Identified by a Novel Quantitative Method. Cancer Res. 2003. April;63(7):1449–53. [PubMed] [Google Scholar]
- 36.Esteller M, Silva JM, Dominguez G, Bonilla F, Matias-Guiu X, Lerma E, et al. Promoter hypermethylation and BRCA1 inactivation in sporadic breast and ovarian tumors. J Natl Cancer Inst. 2000. April;92(7):564–9. 10.1093/jnci/92.7.564 [DOI] [PubMed] [Google Scholar]
- 37.Wilks C, Cline MS, Weiler E, Diehkans M, Craft B, Martin C, et al. The Cancer Genomics Hub (CGHub): Overcoming cancer through the power of torrential data. Database (Oxford). 2014;2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li H, Durbin R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinforma Oxf Engl. 2009. July;25(14):1754–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harrow J, Frankish A, Gonzalez JM, Tapanari E, Diekhans M, Kokocinski F, et al. GENCODE: The reference human genome annotation for The ENCODE Project. Genome Res. 2012. September;22(9):1760–74. 10.1101/gr.135350.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tarasov A, Vilella AJ, Cuppen E, Nijman IJ, Prins P. Sambamba: Fast processing of NGS alignment formats. Bioinformatics. 2015. June;31(12):2032–4. 10.1093/bioinformatics/btv098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Walsh T, Lee MK, Casadei S, Thornton AM, Stray SM, Pennil C, et al. Detection of inherited mutations for breast and ovarian cancer using genomic capture and massively parallel sequencing. Proc Natl Acad Sci U S A. 2010. July;107(28):12629–33. 10.1073/pnas.1007983107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shirts BH, Casadei S, Jacobson AL, Lee MK, Gulsuner S, Bennett RL, et al. Improving performance of multigene panels for genomic analysis of cancer predisposition. Genet Med. 2016. October;18(10):974–81. 10.1038/gim.2015.212 [DOI] [PubMed] [Google Scholar]
- 43.Quinlan AR, Hall IM. BEDTools: A flexible suite of utilities for comparing genomic features. Bioinformatics. 2010. March;26(6):841–2. 10.1093/bioinformatics/btq033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Garrison E, Marth G. Haplotype-based variant detection from short-read sequencing. ArXiv12073907 Q-Bio [Internet]. 2012. July; Available from: http://arxiv.org/abs/1207.3907 [Google Scholar]
- 45.Cingolani P, Platts A, Wang LL, Coon M, Nguyen T, Wang L, et al. A program for annotating and predicting the effects of single nucleotide polymorphisms, SnpEff: SNPs in the genome of Drosophila melanogaster strain w1118; iso-2; iso-3. Fly (Austin). 2012;6(2):80–92. 10.4161/fly.19695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paila U, Chapman BA, Kirchner R, Quinlan AR. GEMINI: Integrative exploration of genetic variation and genome annotations. PLoS Comput Biol. 2013;9(7):e1003153 10.1371/journal.pcbi.1003153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tange O. GNU Parallel—The Command-Line Power Tool. Login USENIX Mag. 2011. February;36(1):42–7. [Google Scholar]
- 48.Kumar P, Henikoff S, Ng PC. Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc. 2009. January;4(7):1073–81. 10.1038/nprot.2009.86 [DOI] [PubMed] [Google Scholar]
- 49.Adzhubei I, Jordan DM, Sunyaev SR. Predicting functional effect of human missense mutations using PolyPhen-2. Curr Protoc Hum Genet Editor Board Jonathan Haines Al. 2013. January;Chapter 7:Unit7.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cooper GM, Stone EA, Asimenos G, NISC Comparative Sequencing Program, Green ED, Batzoglou S, et al. Distribution and intensity of constraint in mammalian genomic sequence. Genome Res. 2005. July;15(7):901–13. 10.1101/gr.3577405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Reese MG, Eeckman FH, Kulp D, Haussler D. Improved splice site detection in Genie. J Comput Biol. 1997;4(3):311–23. 10.1089/cmb.1997.4.311 [DOI] [PubMed] [Google Scholar]
- 52.Fairbrother WG, Yeo GW, Yeh R, Goldstein P, Mawson M, Sharp PA, et al. RESCUE-ESE identifies candidate exonic splicing enhancers in vertebrate exons. Nucleic Acids Res. 2004. July;32(suppl_2):W187–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yeo G, Burge CB. Maximum entropy modeling of short sequence motifs with applications to RNA splicing signals. J Comput Biol. 2004;11(2–3):377–94. 10.1089/1066527041410418 [DOI] [PubMed] [Google Scholar]
- 54.Desmet F-O, Hamroun D, Lalande M, Collod-Béroud G, Claustres M, Béroud C. Human Splicing Finder: An online bioinformatics tool to predict splicing signals. Nucleic Acids Res. 2009;37(9):e67–7. 10.1093/nar/gkp215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lu C, Xie M, Wendl MC, Wang J, McLellan MD, Leiserson MDM, et al. Patterns and functional implications of rare germline variants across 12 cancer types. Nat Commun. 2015. December;6:10086 10.1038/ncomms10086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Riaz N, Blecua P, Lim RS, Shen R, Higginson DS, Weinhold N, et al. Pan-cancer analysis of bi-allelic alterations in homologous recombination DNA repair genes. Nat Commun. 2017. October;8(1):857 10.1038/s41467-017-00921-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang K, Li M, Hadley D, Liu R, Glessner J, Grant SFA, et al. PennCNV: An integrated hidden Markov model designed for high-resolution copy number variation detection in whole-genome SNP genotyping data. Genome Res. 2007. November;17(11):1665–74. 10.1101/gr.6861907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Loo PV, Nordgard SH, Lingjærde OC, Russnes HG, Rye IH, Sun W, et al. Allele-specific copy number analysis of tumors. PNAS. 2010. September;107(39):16910–5. 10.1073/pnas.1009843107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cibulskis K, Lawrence MS, Carter SL, Sivachenko A, Jaffe D, Sougnez C, et al. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat Biotechnol. 2013;31(3):213–9. 10.1038/nbt.2514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jensen MA, Ferretti V, Grossman RL, Staudt LM. The NCI Genomic Data Commons as an engine for precision medicine. Blood. 2017. Jan;blood–2017–03–735654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dayton JB, Piccolo SR. Classifying cancer genome aberrations by their mutually exclusive effects on transcription. BMC Med Genomics. 2017. December;10(Suppl 4):66 10.1186/s12920-017-0303-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lek M, Karczewski KJ, Minikel EV, Samocha KE, Banks E, Fennell T, et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature. 2016. August;536(7616):285–91. 10.1038/nature19057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pritchard CC, Salipante SJ, Koehler K, Smith C, Scroggins S, Wood B, et al. Validation and implementation of targeted capture and sequencing for the detection of actionable mutation, copy number variation, and gene rearrangement in clinical cancer specimens. J Mol Diagn. 2014. January;16(1):56–67. 10.1016/j.jmoldx.2013.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Landrum MJ, Lee JM, Benson M, Brown G, Chao C, Chitipiralla S, et al. ClinVar: Public archive of interpretations of clinically relevant variants. Nucleic Acids Res. 2016. January;44(D1):D862–8. 10.1093/nar/gkv1222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rosenthal R, McGranahan N, Herrero J, Taylor BS, Swanton C. deconstructSigs: Delineating mutational processes in single tumors distinguishes DNA repair deficiencies and patterns of carcinoma evolution. Genome Biol. 2016. February;17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Goldman M, Craft B, Swatloski T, Cline M, Morozova O, Diekhans M, et al. The UCSC Cancer Genomics Browser: Update 2015. Nucleic Acids Res. 2015. January;43(D1):D812–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Price ME, Cotton AM, Lam LL, Farré P, Emberly E, Brown CJ, et al. Additional annotation enhances potential for biologically-relevant analysis of the Illumina Infinium HumanMethylation450 BeadChip array. Epigenetics Chromatin. 2013. March;6(1):4 10.1186/1756-8935-6-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Loo M van der. Extremevalues: An R-package for distribution-based outlier detection. 2017.
- 69.Mermel CH, Schumacher SE, Hill B, Meyerson ML, Beroukhim R, Getz G. GISTIC2.0 facilitates sensitive and confident localization of the targets of focal somatic copy-number alteration in human cancers. Genome Biol. 2011;12(4):R41 10.1186/gb-2011-12-4-r41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nielsen TO, Parker JS, Leung S, Voduc D, Ebbert M, Vickery T, et al. A comparison of PAM50 intrinsic subtyping with immunohistochemistry and clinical prognostic factors in tamoxifen-treated estrogen receptor-positive breast cancer. Clin Cancer Res. 2010. November;16(21):5222–32. 10.1158/1078-0432.CCR-10-1282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Netanely D, Avraham A, Ben-Baruch A, Evron E, Shamir R. Expression and methylation patterns partition luminal-A breast tumors into distinct prognostic subgroups. Breast Cancer Research. 2016. July;18(1):74 10.1186/s13058-016-0724-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Konishi T. Parametric analysis of RNA-seq expression data. Genes Cells. 2016;21(6):639–47. 10.1111/gtc.12372 [DOI] [PubMed] [Google Scholar]
- 73.Rahman M, Jackson LK, Johnson WE, Li DY, Bild AH, Piccolo SR. Alternative preprocessing of RNA-Sequencing data in The Cancer Genome Atlas leads to improved analysis results. Bioinformatics. 2015. November;31(22):3666–72. 10.1093/bioinformatics/btv377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sioutos N, Coronado S de, Haber MW, Hartel FW, Shaiu W-L, Wright LW. NCI Thesaurus: A semantic model integrating cancer-related clinical and molecular information. Journal of Biomedical Informatics. 2007. February;40(1):30–43. 10.1016/j.jbi.2006.02.013 [DOI] [PubMed] [Google Scholar]
- 75.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2016. [Google Scholar]
- 76.Wickham H, Hester J, Francois R. Readr: Read Tabular Data. 2016. [Google Scholar]
- 77.Wickham H, Francois R. Dplyr: A Grammar of Data Manipulation. 2016. [Google Scholar]
- 78.Wickham H. Ggplot2: Elegant Graphics for Data Analysis. Springer-Verlag; New York; 2009. [Google Scholar]
- 79.Wickham H, Henry L. Tidyr: Easily Tidy Data with ‘spread()’ and ‘gather()’ Functions. 2018. [Google Scholar]
- 80.Wickham H. Reshaping Data with the reshape Package. J Stat Softw. 2007;21(12):1–20. [Google Scholar]
- 81.Slowikowski K. Ggrepel: Automatically Position Non-Overlapping Text Labels with ‘ggplot2’. 2018. [Google Scholar]
- 82.Wilke CO. Cowplot: Streamlined Plot Theme and Plot Annotations for ‘ggplot2’. 2017. [Google Scholar]
- 83.Dowle M, Srinivasan A. Data. Table: Extension of ‘data.Frame‘. 2018. [Google Scholar]
- 84.Gehlenborg N. UpSetR: A More Scalable Alternative to Venn and Euler Diagrams for Visualizing Intersecting Sets. 2017. [Google Scholar]
- 85.Team TBD. BSgenome.Hsapiens.UCSC.Hg38: Full genome sequences for Homo sapiens (UCSC version hg38). 2015. [Google Scholar]
- 86.Huber W, Carey VJ, Gentleman R, Anders S, Carlson M, Carvalho BS, et al. Orchestrating high-throughput genomic analysis with Bioconductor. Nat Methods. 2015;12(2):115–21. 10.1038/nmeth.3252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Krijthe JH. Rtsne: T-Distributed Stochastic Neighbor Embedding using Barnes-Hut Implementation. 2015. [Google Scholar]
- 88.Torgerson WS. Multidimensional scaling: I. Theory and method. Psychometrika. 1952. Dec;17(4):401–19. [DOI] [PubMed] [Google Scholar]
- 89.Hayden D, Lazar P, Schoenfeld D, Inflammation and the Host Response to Injury Investigators. Assessing statistical significance in microarray experiments using the distance between microarrays. PLoS ONE. 2009. June;4(6):e5838 10.1371/journal.pone.0005838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Holm S. A Simple Sequentially Rejective Multiple Test Procedure. Scand J Stat. 1979;6(2):65–70. [Google Scholar]
- 91.van der Maaten LJP, Hinton GE. Visualizing High-Dimensional Data Using t-SNE. J Mach Learn Res. 2008;9:2579–605. [Google Scholar]
- 92.van der Maaten LJP. Accelerating t-SNE using Tree-Based Algorithms. J Mach Learn Res. 2014;15:3221–45. [Google Scholar]
- 93.Perou CM, Sørlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature. 2000. August;406(6797):747–52. 10.1038/35021093 [DOI] [PubMed] [Google Scholar]
- 94.Parker JS, Mullins M, Cheang MCU, Leung S, Voduc D, Vickery T, et al. Supervised risk predictor of breast cancer based on intrinsic subtypes. J Clin Oncol Off J Am Soc Clin Oncol. 2009. March;27(8):1160–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Miller LD, Smeds J, George J, Vega VB, Vergara L, Ploner A, et al. An expression signature for p53 status in human breast cancer predicts mutation status, transcriptional effects, and patient survival. Proc Natl Acad Sci U S A. 2005. September;102(38):13550–5. 10.1073/pnas.0506230102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Piccolo SR, Andrulis IL, Cohen AL, Conner T, Moos PJ, Spira AE, et al. Gene-expression patterns in peripheral blood classify familial breast cancer susceptibility. BMC Med Genomics. 2015. November;8:72 10.1186/s12920-015-0145-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Knudson AG. Mutation and Cancer: Statistical Study of Retinoblastoma. Proc Natl Acad Sci U S A. 1971. April;68(4):820–3. 10.1073/pnas.68.4.820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mahler-Araujo B, Savage K, Parry S, Reis-Filho JS. Reduction of E-cadherin expression is associated with non-lobular breast carcinomas of basal-like and triple negative phenotype. J Clin Pathol. 2008. May;61(5):615–20. 10.1136/jcp.2007.053991 [DOI] [PubMed] [Google Scholar]
- 99.Christou CM, Kyriacou K. BRCA1 and Its Network of Interacting Partners. Biology (Basel). 2012. December;2(1):40–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Cimmino F, Formicola D, Capasso M. Dualistic Role of BARD1 in Cancer. Genes (Basel). 2017. December;8(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Coussy F, El-Botty R, Château-Joubert S, Dahmani A, Montaudon E, Leboucher S, et al. BRCAness, SLFN11, and RB1 loss predict response to topoisomerase I inhibitors in triple-negative breast cancers. Sci Transl Med. 2020. February;12(531). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Deng C-X. BRCA1: Cell cycle checkpoint, genetic instability, DNA damage response and cancer evolution. Nucleic Acids Res. 2006;34(5):1416–26. 10.1093/nar/gkl010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hedenfalk I, Duggan D, Chen Y, Radmacher M, Bittner M, Simon R, et al. Gene-expression profiles in hereditary breast cancer. N Engl J Med. 2001. February;344(8):539–48. 10.1056/NEJM200102223440801 [DOI] [PubMed] [Google Scholar]
- 104.Rice JC, Ozcelik H, Maxeiner P, Andrulis I, Futscher BW. Methylation of the BRCA1 promoter is associated with decreased BRCA1 mRNA levels in clinical breast cancer specimens. Carcinogenesis. 2000. September;21(9):1761–5. 10.1093/carcin/21.9.1761 [DOI] [PubMed] [Google Scholar]
- 105.Moelans CB, Verschuur-Maes AH, Diest PJ van. Frequent promoter hypermethylation of BRCA2, CDH13, MSH6, PAX5, PAX6 and WT1 in ductal carcinoma in situ and invasive breast cancer. J Pathol. 2011;225(2):222–31. 10.1002/path.2930 [DOI] [PubMed] [Google Scholar]
- 106.Tutt A, Tovey H, Cheang MCU, Kernaghan S, Kilburn L, Gazinska P, et al. Carboplatin in BRCA1/2 -mutated and triple-negative breast cancer BRCAness subgroups: The TNT Trial. Nat Med. 2018. May;24(5):628–37. 10.1038/s41591-018-0009-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mulligan JM, Hill LA, Deharo S, Irwin G, Boyle D, Keating KE, et al. Identification and validation of an anthracycline/cyclophosphamide-based chemotherapy response assay in breast cancer. J Natl Cancer Inst. 2014. January;106(1):djt335 10.1093/jnci/djt335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Waddell N, Pajic M, Patch A-M, Chang DK, Kassahn KS, Bailey P, et al. Whole genomes redefine the mutational landscape of pancreatic cancer. Nature. 2015. February;518(7540):495–501. 10.1038/nature14169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Spurdle AB, Healey S, Devereau A, Hogervorst FBL, Monteiro ANA, Nathanson KL, et al. ENIGMAEvidence-based network for the interpretation of germline mutant alleles: An international initiative to evaluate risk and clinical significance associated with sequence variation in BRCA1 and BRCA2 genes. Hum Mutat. 2012;33(1):2–7. 10.1002/humu.21628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Vellido A, Martín-Guerrero JD, Lisboa PJG. Making machine learning models interpretable. In: In Proc European Symposium on Artificial Neural Networks, Computational InTELligence and Machine Learning. 2012. [Google Scholar]