Nutritional content and timing are increasingly appreciated to constitute important human variables collectively impacting all aspects of human physiology and disease. However, person-specific mechanisms driving nutritional impacts on the human host remain incompletely understood, while current dietary recommendations remain empirical and nonpersonalized. Precision nutrition aims to harness individualized bodies of data, including the human gut microbiome, in predicting person-specific physiological responses (such as glycemic responses) to food.
KEYWORDS: machine learning, microbiome, personalized nutrition
ABSTRACT
Nutritional content and timing are increasingly appreciated to constitute important human variables collectively impacting all aspects of human physiology and disease. However, person-specific mechanisms driving nutritional impacts on the human host remain incompletely understood, while current dietary recommendations remain empirical and nonpersonalized. Precision nutrition aims to harness individualized bodies of data, including the human gut microbiome, in predicting person-specific physiological responses (such as glycemic responses) to food. With these advances notwithstanding, many unknowns remain, including the long-term efficacy of such interventions in delaying or reversing human metabolic disease, mechanisms driving these dietary effects, and the extent of the contribution of the gut microbiome to these processes. We summarize these conceptual advances, while highlighting challenges and means of addressing them in the next decade of study of precision medicine, toward generation of insights that may help to evolve precision nutrition as an effective future tool in a variety of “multifactorial” human disorders.
NUTRITION-MICROBIOME CROSS TALK
Food digestion and absorption.
Mammalian digestion is initiated by cognitive food perception, which stimulates the production of oral saliva and gastric secretions (1). Later on, the passage of a food bolus through the esophagus and stomach further stimulates the secretion of biliary and pancreatic secretions that play a fundamental role in food decomposition and digestion. Absorption of dietary nutrients takes place mainly in the small intestine, where structures called villi and microvilli greatly increase the mucosal surface area, thereby enhancing its absorptive capacity. Residues of food that was not absorbed in the small intestine reach the colon, in which absorption of water takes place, further solidifying stools. The proximal part of the gastrointestinal (GI) tract is loosely inhabited by microbes because of low pH, the presence of toxic bile acids, and high oxygen content (2). The GI tract gradually becomes more densely colonized by microbes distally. Depletion of dietary nutrients, such as fatty acids and carbohydrates in the intestinal lumen during the transit of food across the GI tract, renders the growth of many gut commensals dependent on nondietary host-derived energy sources by deconjugation of primary bile acids or degradation of mucin-derived glycans (3–7).
Dietary impacts on the microbiome.
The gut microbiome is strongly influenced by the composition (8–10), amount, and timing (11–18) of its host’s diet. Mounting evidence suggests that the timing of feeding has a predominant effect on downstream metabolic and immune functions in microbiome-dependent and -independent manners. In a given person, substantial variability was noticed when identical meals were consumed at different times of the day (19). The intestinal microbiome exhibits diurnal oscillations that are driven by feeding patterns (15, 17, 18). Circadian-clock perturbation (commonly termed “jet lag”) induces a dysbiosis that is associated with glucose intolerance and obesity that are transferable by fecal microbial transfer (FMT) (15, 18). The transcriptomic landscape of nonintestinal organs was shown to oscillate as a function of feeding timing, which is (at least partially) regulated by corresponding oscillations in gut-derived serum metabolites (14, 18). An irregular feeding pattern may result in impairments of fundamental physiological functions, such as hepatic detoxification. The peculiar propensity of the gut microbiome to adapt to dietary perturbation is mirrored by the speed at which this adaptation takes place (20–24). Dietary constituents may support or impede the growth of particular microbes and also contain foodborne microbes, directly contributing to the net composition of the microbial genetic pool in the gut (9). Other dietary elements act as “immunomodulators” and can indirectly affect the microbiome composition in an immune-dependent manner via regulation of cellular and secreted immune effectors (25–28).
Microbiome impacts on digestions and absorption.
Host-microbiome metabolic interactions are bidirectional. Intestinal motility is regulated by bacterial metabolism of bile acids and bacterially induced nitric oxide production in a diet-dependent manner (Fig. 1) (29–32). Food choices are hypothesized by some to be subjected to microbiome influences, although evidence supporting that notion remains scarce (33–35). Postdieting weight recidivism, a common complication in nutritional clinical practice, is modulated by a persistent diet-altered microbiome “memory” (36), at least in rodent models. Adiposity and weight gain in various mammals can be modified with microbiome manipulation and were hypothesized to be governed by the gut microbiomes’ capacity to extract energy from diet (37–40). Promotion of weight gain is commonly achieved in livestock by antibiotic treatment (41, 42), a practice that is futile in germfree (GF) poultry (43), suggesting that microbiome manipulation by antibiotics may enhance dietary energy extraction. In healthy individuals, a short course of oral vancomycin (an antibiotic agent that is not absorbed systemically and therefore affects only the gut) attenuated dietary energy harvest compared with that after administration of a placebo, as mirrored by stool calorie loss (44). Interestingly, GF mice were previously reported to be resilient to deleterious effects of high-fat diet (HFD) feeding, such as weight gain and glucose intolerance (45, 46); however, findings from recent studies using various types of HFDs suggest that vivarium-dependent factors may differentially induce this trait (47–52).
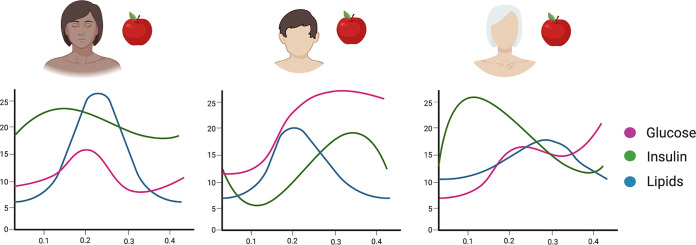
FIG 1.
Examples of dietary microbiome cross talk. During digestion, food is decomposed to fat, proteins, carbohydrates, minerals, and other substances. Interactions between dietary habits and the intestinal microbiome result in alterations of various aspects of mammalian physiology in intestinal and nonintestinal organs. The image was created at BioRender. LPS, lipopolysaccharides; TMAO, trimethylamine N-oxide.
Major macronutrients and the microbiome.
Dietary fibers, also termed “glycans” or “polysaccharides,” are mainly plant-derived complex polymers of covalently linked simple carbohydrates (5). Humans are virtually devoid of enzymes that can decompose fibers, whereas gut bacteria express thousands of genes that encode carbohydrate-degrading enzymes (53). The products of primary and secondary fiber degradation are utilized by other members of the gut microbiome and the host in a convoluted web of cross-feeding (5, 6, 54, 55). A combination of person-specific fiber degradation capacity and the given fiber most probably determines the effects of fiber on host metabolism and the microbiome; however, in general, an increased intake of dietary fibers is associated with a higher overall microbial diversity, dominated by enrichment of Bacteroidetes and Prevotella spp. (20, 21, 56–58), and coupled to favorable metabolic and immunologic effects, such as improved insulin resistance and lower susceptibility to infection and malignancy (59, 60). Inversely, fiber deprivation leads to decreased microbial diversity, lower colonic bacterial butyrate production, barrier dysfunction, and susceptibility to perturbation and infection (21, 61–67). There is a notable interpersonal variability in complex and simple-carbohydrate digestion that is believed to be microbiome mediated and has been the subject of extensive research (as described in the next section) (59, 68–70).
Carbohydrates, proteins, and fats have all been shown to interact with the gut microbiome. Western diets that are rich in fat induce weight gain and insulin resistance by impairing intestinal barrier function and propagating a Toll-like receptor 4-mediated inflammatory response that is termed “metabolic endotoxemia” (51, 71–81). The resulting deleterious effects can be diminished by treatment with antibiotics (82) or phenocopied to another host by fecal microbial transfer (37). Proteins are metabolized by gut microbes into small metabolites, such as short-chain fatty acids (SCFAs), neurotransmitters, and organic acids, that have physiological effects both locally and systemically (83–87). A plethora of widely consumed dietary and nondietary constituents, such as emulsifiers (88–90), nonnutritive sweeteners (91–96), trehalose (97), probiotics (98–101), omega-3 fatty acids (102), and medications (103–105), were shown to feature considerable microbiome-mediated health impacts and are a subject of intensive research that is beyond the scope of this review.
The microbiome as a “signaling hub.”
The intestinal microbiome generates downstream systemic signals, many of which are diet derived (106). One prominent example is the ketogenic diet, which aims at biochemically replacing carbohydrates with fat as a primary energy source through consumption of a low-carbohydrate, high-fat diet. This diet is commonly used in clinical practice to reduce seizure frequency in the treatment of drug-resistant epilepsy and is known to induce considerable microbiome and immune alterations; however, its mechanism of action remains unknown (107, 108). A recent study demonstrated that the ketogenic diet lacks an antiseizure effect in microbiome-depleted mice (either GF or antibiotic-treated mice) and that a fecal microbiome transfer from mice fed a ketogenic diet into mice fed a control diet induced a seizure-protective effect (109). A reduced amino acid gamma-glutamylation capacity of the ketogenic diet-associated microbiome was shown to elevate the seizure threshold in that mouse model of epilepsy. Collectively, evidence in support of an intensive cross talk between the gut microbiome and host nutrition, which may impact a variety of physiological and pathophysiological traits, is accumulating.
THE GUT MICROBIOME IN PRECISION NUTRITION
Dietary habits constitute a strong driver of interpersonal variance in the gut microbiome composition, and its influence prevails over that of genetics by most estimates (23, 110–112). One example of person-specific microbiome impact on dietary physiological responses to consumed food focused on artificial sweeteners, mainly saccharin, and demonstrated that glycemic responses to these seemingly inert food supplements were driven by variations in the human microbiome (95). Moreover, adverse glycemic responses to saccharin could be predicted using machine learning by utilizing microbiome data collected before sweetener exposure (95). Indeed, a longitudinal concurrent daily dietary log and stool metagenomic sequencing throughout 17 consecutive days for 34 healthy individuals recently revealed markedly person-specific diet-microbiome interactions (113). Whereas some aspects of optimal nutrition unanimously apply, most are person specific and may differ in a population based on genetic and environmental factors. Within the environmental component, the gut microbiome accounts for some variation in subject-specific responses to diets, as do the timing of meals, time between meals, level of physical activity, and multiple other individualized features.
Adherence to dietary recommendations in the long term is a salient obstacle to dietary interventions (114, 115). A tailored intervention can potentially increase compliance, improve patient selection, and prevent weight gain-weight loss cycles that may predispose to adverse cardiometabolic health outcomes (116). Microbiome-based predictions of person-specific responses to some foods were demonstrated to be accurate and clinically beneficial in several studies. The baseline microbiome predicted the response to caloric restriction in mice. Interestingly, cohousing mice before dietary intervention resulted in a convergence of their microbiome configuration and a subsequent similar response to the dietary intervention (117). Nonnutritive sweetener consumption induces glucose intolerance, which is transferable to germfree mice by fecal microbial transfer and can be abrogated by antibiotics, suggesting a microbiome-dependent effect (95). Intriguingly, a subject-specific response to nonnutritive sweeteners was exhibited in humans, with the microbiomes of responders and nonresponders clustering separately (95, 118). Similarly, the glycemic response to different types of bread could be reliably predicted based on microbiome features (119). In contrast, 16S rRNA sequencing of stool microbiomes before the commencement of low-carbohydrate/fat diets was not predictive of weight loss success (120). Several studies on dietary interventions to treat obesity and metabolic syndrome have reported various associations between microbiome parameters and treatment efficacy. However, their heterogeneous design, small sample sizes, and short-term intervention profoundly limit their translational potential (111, 121–124). The same applies to a few studies assessing the low FODMAP diet (a diet low in fermentable carbohydrates) in the treatment of irritable bowel syndrome (IBS) (125–129).
Trimethylamine N-oxide (TMAO) is produced by intestinal microbes from dietary choline, which originates mainly in red meat. High TMAO levels are associated with adverse cardiovascular outcomes due to atherosclerosis and thrombosis (130–135). TMAO production is largely microbiome dependent and can be suppressed by antibiotics (133) or inhibition of bacterial enzymes (136). Considerable interindividual variability in TMAO production capacity exists across populations, with carnivores and vegans/vegetarians having on average higher and lower TMAO production capacities, respectively (131). Identification of individuals with a nonfavorable TMAO production capacity can serve as a source of microbiome-based personal nutrition recommendation and can be achieved without expensive sequencing by an oral carnitine challenge test (137). Unfortunately, such personalized predictions are not provided by nutritionists at this time, and recommendations to avoid red meat are generally dispensed to patients with high cardiovascular risk.
Dietary fibers are nutritionally beneficial, and their metabolism is almost entirely dependent on the expression of specific bacterial genes, potentially making them a focus of precision nutrition (59, 69, 138). Dietary guidelines recommend consumption of ∼30 g fiber a day for adults (or 14 g for every 1,000 cal), but such general recommendations are suboptimal due to several considerations (139). The chemical structures of molecules jointly referred to as fibers vary, and so do the identities and functions of the bacterial strains that can degrade them. Therefore, the effect that fibers may have on host health and the host’s intestinal microbial community is highly individualized (5, 54, 140). Hence, high interpersonal variability in metabolic outcomes and microbiome readouts is exhibited in clinical trials testing fiber supplementation (141–143).
Although the gut microbiome is a key determinant of a person’s response to fiber consumption, no reliable means of predicting a person-specific response to fiber supplementation exist to date, although some associations between clinical outcomes and microbiome features (community diversity and certain abundances of taxa, mainly the Bacteroides, Prevotella, Bifidobacterium, and Ruminococcus genera) have been suggested by multiple studies (21, 58, 59, 123, 141, 144–152). Habitual dietary fiber consumption may best predict the response to fiber supplementation more than any other microbiome parameter, and long-term multigenerational fiber deprivation leads to the extinction of fiber-degrading taxa, resulting in a hampered recovery of those taxa upon reintroduction of fiber (10, 153, 154). Considering the benefits of fiber consumption and the fact that fiber degradation is exclusively bacterial and highly variable, microbiome-driven prediction of person-specific fiber degradation capacity constitutes an exciting future challenge in clinical nutrition.
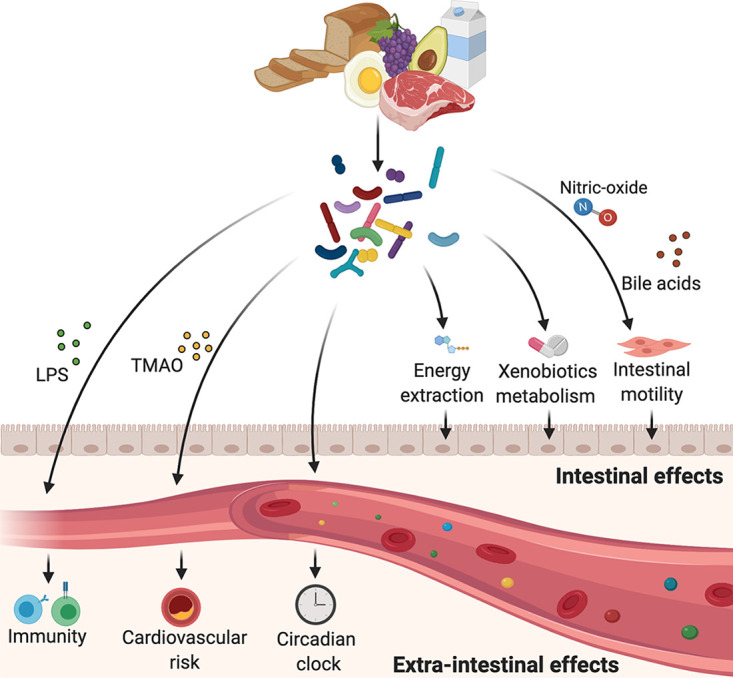
As previously discussed, gut microbes actively take part in carbohydrate metabolism and glucose homeostasis by degrading carbohydrates and by producing secondary bile acids and SCFAs that stimulate secretion of glucoregulatory hormones (e.g., glucagon-like peptide 1 [GLP-1], peptide YY [PYY]) (155–160). The postprandial surges in blood glucose levels (i.e., postprandial glycemic response, or PPGR) considerably vary between individuals, even following the ingestion of the same type and quantity of carbohydrates in identical meals or following exercise (Fig. 2) (119, 157, 161, 162). The Personalized Nutrition Project (PNP) demonstrated that a person-specific PPGR to real-life meals can be accurately predicted based on basic clinical parameters and microbiome data (163). The accuracy of the machine-learning pipeline that based its prediction on continuous glucose monitoring (CGM) data, stool microbiome sequencing, dietary logs, and other clinical variables from 800 individuals was validated in an additional validation cohort of 100 subjects. The algorithm predicted individual PPGRs better than models based on caloric/carbohydrate content only, and microbiome features accounted for the explained variability in PPGRs to various degrees. A personally tailored dietary intervention based on the algorithm’s predictions improved glycemic parameters in 26 prediabetic individuals. While some microbiome-based classifiers that were developed in a given geographical context exhibited poor accuracy when applied to subjects from different geographical origins (164, 165), the personalized nutrition concept was subsequently validated in another cohort of 327 subjects from a different geographical area (166). The clinical efficacy of a person-tailored dietary intervention based on the algorithm’s predictions in improving glycemic control in prediabetic individuals is currently being tested in a long-term randomized controlled trial (clinical trial NCT03222791).
FIG 2.
Person-specific postprandial responses. Genetic and nongenetic factors, such as age, the nature of a meal, habitual diet, level of physical activity, and the microbiome, account for considerable interindividual variability in energetic and endocrine postprandial responses, resulting in large differences in metabolic parameters following identical meals. The image was created at BioRender.
The recent PREDICT1 study assessed subject-specific postprandial metabolic responses (19). Unlike the PNP, PREDICT1 also predicted postprandial triglyceride (TG) levels and insulin responses in addition to glucose. Furthermore, it included 230 twin pairs with genomic data that allowed the investigator to estimate the contribution of inheritance to postprandial metabolic responses. As with the PNP, clinical and metabolic parameters as well as microbiome and CGM data were collected from 1,002 healthy individuals (and from an additional 100 individuals in the validation cohort). Genetics accounted for 48%, 9%, and 0% of the variability in postprandial glucose, insulin, and triglycerides, respectively, whereas the stool microbiome accounted for only 6.4%, 5.8%, and 7.5% of postprandial variability in blood glucose, insulin, and TG, respectively. A meal’s macronutrient composition and timing in relation to previous meal/sleep/exercise are well-established effectors of PPGR and were also shown in the PREDICT1 study to surpass the microbiome in their PPGR predictive power. Notably, the predictive algorithm developed in the PREDICT1 study reached an accuracy in PPGR prediction similar to that of the PNP (Pearson’s correlation coefficients [r] were 0.7 and 0.77 between predicted and measured PPGRs, respectively) despite the different inputs and machine-learning approaches used. Prediction of postprandial TG and insulin in the PREDICT1 study were less accurate. In summary, both the PNP and PREDICT1 studies provide good-quality evidence that dietary recommendations can be optimized to be patient tailored.
CURRENT CHALLENGES IN PRECISION DIETS AND FUTURE PROSPECTS
With these major advances in understanding the contribution of the microbiome to precision nutrition notwithstanding, many challenges need to be addressed in order to increase our mechanistic understanding of the forces shaping individualized human responses to food and the role that the microbiome plays in this complex and poorly understood process.
CGM systems are extremely pragmatic research tools, as they enable affordable real-life assessment of glucose levels in an outpatient setting without the inconvenience of a finger prick. However, the accuracy of CGM systems may pose a challenge in the nondiabetic setting. In a study funded by Abbott, a manufacturer of CGM systems, the concordance of CGM with direct capillary blood glucose measurement was <90% (167). Moreover, the within-individual variability in nondiabetics upon simultaneous PPGR measurement by two identical (19) or two different (168) sensor systems was not negligible. These differences may possibly stem from variations between sensors or from true differences in glucose kinetics in different anatomical locations.
While machine learning provides valuable insights into features possibly contributing to these physiological outcomes, their mechanistic elucidation merits further molecular-level research. Equally elusive are the potential roles of the viral, fungal, and parasitic microbiomes in contributing to personalized human responses to food, as well as roles played by niche-specific microbiomes along the oral and gastrointestinal regions. Additionally, better annotations of microbial reads currently constituting “dark matter” may enable us to refine and improve the utility of the microbiome, when coupled with other clinical features, in predicting food-induced human responses. Finally, as nutrition is estimated to impact a plethora of infectious, inflammatory, neoplastic, and even neurodegenerative processes, understanding of the causative food-induced and microbiome-modulated effects induced in the human host under these contexts may enable us to rationally harness precision nutrition as part of the therapeutic arsenal in these common and often devastating human diseases.
ACKNOWLEDGMENTS
We thank the members of the Elinav and Segal labs for discussions and apologize to authors whose work was not cited because of space constraints.
E.E. is the incumbent of the Sir Marc and Lady Tania Feldmann Professorial Chair, a senior fellow at the Canadian Institute of Advanced Research, and an international scholar at the Bill & Melinda Gates Foundation and the Howard Hughes Medical Institute (HHMI). E.S. and E.E. are salaried scientific consultants of DayTwo. E.E. is a salaried consultant of BiomX.
All authors performed extensive literature research, contributed substantially to discussion of the content, and wrote and edited the manuscript.
This minireview went through the journal's normal peer review process. DayTwo sponsored the minireview and its associated video but had no editorial input on the content.
REFERENCES
- 1.Livovsky DM, Pribic T, Azpiroz F. 2020. Food, eating, and the gastrointestinal tract. Nutrients 12:986. doi: 10.3390/nu12040986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Donaldson GP, Lee SM, Mazmanian SK. 2016. Gut biogeography of the bacterial microbiota. Nat Rev Microbiol 14:20–32. doi: 10.1038/nrmicro3552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim YS, Ho SB. 2010. Intestinal goblet cells and mucins in health and disease: recent insights and progress. Curr Gastroenterol Rep 12:319–330. doi: 10.1007/s11894-010-0131-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martens EC, Roth R, Heuser JE, Gordon JI. 2009. Coordinate regulation of glycan degradation and polysaccharide capsule biosynthesis by a prominent human gut symbiont. J Biol Chem 284:18445–18457. doi: 10.1074/jbc.M109.008094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koropatkin NM, Cameron EA, Martens EC. 2012. How glycan metabolism shapes the human gut microbiota. Nat Rev Microbiol 10:323–335. doi: 10.1038/nrmicro2746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sonnenburg JL, Xu J, Leip DD, Chen CH, Westover BP, Weatherford J, Buhler JD, Gordon JI. 2005. Glycan foraging in vivo by an intestine-adapted bacterial symbiont. Science 307:1955–1959. doi: 10.1126/science.1109051. [DOI] [PubMed] [Google Scholar]
- 7.Wahlström A, Sayin SI, Marschall HU, Bäckhed F. 2016. Intestinal crosstalk between bile acids and microbiota and its impact on host metabolism. Cell Metab 24:41–50. doi: 10.1016/j.cmet.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 8.Hall KD, Ayuketah A, Brychta R, Cai H, Cassimatis T, Chen KY, Chung ST, Costa E, Courville A, Darcey V, Fletcher LA, Forde CG, Gharib AM, Guo J, Howard R, Joseph PV, McGehee S, Ouwerkerk R, Raisinger K, Rozga I, Stagliano M, Walter M, Walter PJ, Yang S, Zhou M. 2019. Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake. Cell Metab 30:67–77.e3. doi: 10.1016/j.cmet.2019.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bisanz JE, Upadhyay V, Turnbaugh JA, Ly K, Turnbaugh PJ. 2019. Meta-analysis reveals reproducible gut microbiome alterations in response to a high-fat diet. Cell Host Microbe 26:1–8. doi: 10.1016/j.chom.2019.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Healey G, Murphy R, Butts C, Brough L, Whelan K, Coad J. 2018. Habitual dietary fibre intake influences gut microbiota response to an inulin-type fructan prebiotic: a randomised, double-blind, placebo-controlled, cross-over, human intervention study. Br J Nutr 119:176–189. doi: 10.1017/S0007114517003440. [DOI] [PubMed] [Google Scholar]
- 11.Smits SA, Leach J, Sonnenburg ED, Gonzalez CG, Lichtman JS, Reid G, Knight R, Manjurano A, Changalucha J, Elias JE, Dominguez-Bello MG, Sonnenburg JL. 2017. Seasonal cycling in the gut microbiome of the Hadza hunter-gatherers of Tanzania. Science 357:802–805. doi: 10.1126/science.aan4834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davenport ER, Mizrahi-Man O, Michelini K, Barreiro LB, Ober C, Gilad Y. 2014. Seasonal variation in human gut microbiome composition. PLoS One 9:e90731. doi: 10.1371/journal.pone.0090731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dubois G, Girard C, Lapointe FJ, Shapiro BJ. 2017. The Inuit gut microbiome is dynamic over time and shaped by traditional foods. Microbiome 5:151. doi: 10.1186/s40168-017-0370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thaiss CA, Levy M, Korem T, Dohnalová L, Shapiro H, Jaitin DA, David E, Winter DR, Gury-BenAri M, Tatirovsky E, Tuganbaev T, Federici S, Zmora N, Zeevi D, Dori-Bachash M, Pevsner-Fischer M, Kartvelishvily E, Brandis A, Harmelin A, Shibolet O, Halpern Z, Honda K, Amit I, Segal E, Elinav E. 2016. Microbiota diurnal rhythmicity programs host transcriptome oscillations. Cell 167:1495–1510.e12. doi: 10.1016/j.cell.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Leone V, Gibbons SM, Martinez K, Hutchison AL, Huang EY, Cham CM, Pierre JF, Heneghan AF, Nadimpalli A, Hubert N, Zale E, Wang Y, Huang Y, Theriault B, Dinner AR, Musch MW, Kudsk KA, Prendergast BJ, Gilbert JA, Chang EB. 2015. Effects of diurnal variation of gut microbes and high-fat feeding on host circadian clock function and metabolism. Cell Host Microbe 17:681–689. doi: 10.1016/j.chom.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mukherji A, Kobiita A, Ye T, Chambon P. 2013. Homeostasis in intestinal epithelium is orchestrated by the circadian clock and microbiota cues transduced by TLRs. Cell 153:812–827. doi: 10.1016/j.cell.2013.04.020. [DOI] [PubMed] [Google Scholar]
- 17.Zarrinpar A, Chaix A, Yooseph S, Panda S. 2014. Diet and feeding pattern affect the diurnal dynamics of the gut microbiome. Cell Metab 20:1006–1017. doi: 10.1016/j.cmet.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thaiss CA, Zeevi D, Levy M, Zilberman-Schapira G, Suez J, Tengeler AC, Abramson L, Katz MN, Korem T, Zmora N, Kuperman Y, Biton I, Gilad S, Harmelin A, Shapiro H, Halpern Z, Segal E, Elinav E. 2014. Transkingdom control of microbiota diurnal oscillations promotes metabolic homeostasis. Cell 159:514–529. doi: 10.1016/j.cell.2014.09.048. [DOI] [PubMed] [Google Scholar]
- 19.Berry SE, Valdes AM, Drew DA, Asnicar F, Mazidi M, Wolf J, Capdevila J, Hadjigeorgiou G, Davies R, Al Khatib H, Bonnett C, Ganesh S, Bakker E, Hart D, Mangino M, Merino J, Linenberg I, Wyatt P, Ordovas JM, Gardner CD, Delahanty LM, Chan AT, Segata N, Franks PW, Spector TD. 2020. Human postprandial responses to food and potential for precision nutrition. Nat Med 26:964–973. doi: 10.1038/s41591-020-0934-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu GD, Chen J, Hoffmann C, Bittinger K, Chen Y-Y, Keilbaugh SA, Bewtra M, Knights D, Walters WA, Knight R, Sinha R, Gilroy E, Gupta K, Baldassano R, Nessel L, Li H, Bushman FD, Lewis JD. 2011. Linking long-term dietary patterns with gut microbial enterotypes. Science 334:105–108. doi: 10.1126/science.1208344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walker AW, Ince J, Duncan SH, Webster LM, Holtrop G, Ze X, Brown D, Stares MD, Scott P, Bergerat A, Louis P, McIntosh F, Johnstone AM, Lobley GE, Parkhill J, Flint HJ. 2011. Dominant and diet-responsive groups of bacteria within the human colonic microbiota. ISME J 5:220–230. doi: 10.1038/ismej.2010.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Turnbaugh PJ, Ridaura VK, Faith JJ, Rey FE, Knight R, Gordon JI. 2009. The effect of diet on the human gut microbiome: a metagenomic analysis in humanized gnotobiotic mice. Sci Transl Med 1:1–12. doi: 10.1126/scitranslmed.3000322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, Ling AV, Devlin AS, Varma Y, Fischbach MA, Biddinger SB, Dutton RJ, Turnbaugh PJ. 2014. Diet rapidly and reproducibly alters the human gut microbiome. Nature 505:559–563. doi: 10.1038/nature12820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Henning SM, Yang J, Shao P, Lee RP, Huang J, Ly A, Hsu M, Lu QY, Thames G, Heber D, Li Z. 2017. Health benefit of vegetable/fruit juice-based diet: role of microbiome. Sci Rep 7:2167. doi: 10.1038/s41598-017-02200-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang C, Derrien M, Levenez F, Brazeilles R, Ballal SA, Kim J, Degivry MC, Quéré G, Garault P, Van Hylckama Vlieg JET, Garrett WS, Doré J, Veiga P. 2016. Ecological robustness of the gut microbiota in response to ingestion of transient food-borne microbes. ISME J 10:2235–2245. doi: 10.1038/ismej.2016.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang HH, Manuzon M, Lehman M, Wan K, Luo H, Wittum TE, Yousef A, Bakaletz LO. 2006. Food commensal microbes as a potentially important avenue in transmitting antibiotic resistance genes. FEMS Microbiol Lett 254:226–231. doi: 10.1111/j.1574-6968.2005.00030.x. [DOI] [PubMed] [Google Scholar]
- 27.Li Y, Innocentin S, Withers DR, Roberts NA, Gallagher AR, Grigorieva EF, Wilhelm C, Veldhoen M. 2011. Exogenous stimuli maintain intraepithelial lymphocytes via aryl hydrocarbon receptor activation. Cell 147:629–640. doi: 10.1016/j.cell.2011.09.025. [DOI] [PubMed] [Google Scholar]
- 28.Su D, Nie Y, Zhu A, Chen Z, Wu P, Zhang L, Luo M, Sun Q, Cai L, Lai Y, Xiao Z, Duan Z, Zheng S, Wu G, Hu R, Tsukamoto H, Lugea A, Liu Z, Pandol SJ, Han YP. 2016. Vitamin D signaling through induction of Paneth cell defensins maintains gut microbiota and improves metabolic disorders and hepatic steatosis in animal models. Front Physiol 7:498. doi: 10.3389/fphys.2016.00498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dey N, Wagner VE, Blanton LV, Cheng J, Fontana L, Haque R, Ahmed T, Gordon JI. 2015. Regulators of gut motility revealed by a gnotobiotic model of diet-microbiome interactions related to travel. Cell 163:95–107. doi: 10.1016/j.cell.2015.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pohl JM, Gutweiler S, Thiebes S, Volke JK, Klein-Hitpass L, Zwanziger D, Gunzer M, Jung S, Agace WW, Kurts C, Engel DR. 2017. Irf4-dependent CD103+ CD11b+ dendritic cells and the intestinal microbiome regulate monocyte and macrophage activation and intestinal peristalsis in postoperative ileus. Gut 66:2110–2120. doi: 10.1136/gutjnl-2017-313856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miller LE, Ouwehand AC. 2013. Probiotic supplementation decreases intestinal transit time: meta-analysis of randomized controlled trials. World J Gastroenterol 19:4718–4725. doi: 10.3748/wjg.v19.i29.4718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roland BC, Ciarleglio MM, Clarke JO, Semler JR, Tomakin E, Mullin GE, Pasricha PJ. 2015. Small intestinal transit time is delayed in small intestinal bacterial overgrowth. J Clin Gastroenterol 49:571–576. doi: 10.1097/MCG.0000000000000257. [DOI] [PubMed] [Google Scholar]
- 33.Alcock J, Maley CC, Aktipis CA. 2014. Is eating behavior manipulated by the gastrointestinal microbiota? Evolutionary pressures and potential mechanisms. Bioessays 36:940–949. doi: 10.1002/bies.201400071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Norris V, Molina F, Gewirtz AT. 2013. Hypothesis: bacteria control host appetites. J Bacteriol 195:411–416. doi: 10.1128/JB.01384-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Donnell MP, Fox BW, Chao P-H, Schroeder FC, Sengupta P. 2020. A neurotransmitter produced by gut bacteria modulates host sensory behaviour. Nature 583:415–416. doi: 10.1038/s41586-020-2395-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thaiss CA, Itav S, Rothschild D, Meijer MT, Levy M, Moresi C, Dohnalová L, Braverman S, Rozin S, Malitsky S, Dori-Bachash M, Kuperman Y, Biton I, Gertler A, Harmelin A, Shapiro H, Halpern Z, Aharoni A, Segal E, Elinav E. 2016. Persistent microbiome alterations modulate the rate of post-dieting weight regain. Nature 540:544–551. doi: 10.1038/nature20796. [DOI] [PubMed] [Google Scholar]
- 37.Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. 2006. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 444:1027–1031. doi: 10.1038/nature05414. [DOI] [PubMed] [Google Scholar]
- 38.Bäckhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A, Semenkovich CF, Gordon JI. 2004. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci U S A 101:15718–15723. doi: 10.1073/pnas.0407076101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cho I, Yamanishi S, Cox L, Methé BA, Zavadil J, Li K, Gao Z, Mahana D, Raju K, Teitler I, Li H, Alekseyenko AV, Blaser MJ. 2012. Antibiotics in early life alter the murine colonic microbiome and adiposity. Nature 488:621–626. doi: 10.1038/nature11400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cox LM, Blaser MJ. 2015. Antibiotics in early life and obesity. Nat Rev Endocrinol 11:182–190. doi: 10.1038/nrendo.2014.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gaskins HR, Collier CT, Anderson DB. 2002. Antibiotics as growth promotants: mode of action. Anim Biotechnol 13:29–42. doi: 10.1081/ABIO-120005768. [DOI] [PubMed] [Google Scholar]
- 42.Kruger Ben Shabat S, Sasson G, Doron-Faigenboim A, Durman T, Yaacoby S, Berg Miller ME, White BA, Shterzer N, Mizrahi I. 2016. Specific microbiome-dependent mechanisms underlie the energy harvest efficiency of ruminants. ISME J 10:2958–2972. doi: 10.1038/ismej.2016.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Forbes M, Park JT. 1959. Growth of germ-free and conventional chicks: effect of diet, dietary penicillin and bacterial environment. J Nutr 67:69–84. doi: 10.1093/jn/67.1.69. [DOI] [PubMed] [Google Scholar]
- 44.Basolo A, Hohenadel M, Ang QY, Piaggi P, Heinitz S, Walter M, Walter P, Parrington S, Trinidad DD, von Schwartzenberg RJ, Turnbaugh PJ, Krakoff J. 2020. Effects of underfeeding and oral vancomycin on gut microbiome and nutrient absorption in humans. Nat Med 26:589–598. doi: 10.1038/s41591-020-0801-z. [DOI] [PubMed] [Google Scholar]
- 45.Bäckhed F, Manchester JK, Semenkovich CF, Gordon JI. 2007. Mechanisms underlying the resistance to diet-induced obesity in germ-free mice. Proc Natl Acad Sci U S A 104:979–984. doi: 10.1073/pnas.0605374104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rabot S, Membrez M, Bruneau A, Gerard P, Harach T, Moser M, Raymond F, Mansourian R, Chou CJ. 2010. Germ-free C57BL/6J mice are resistant to high-fat-diet-induced insulin resistance and have altered cholesterol metabolism. FASEB J 24:4948–4959. doi: 10.1096/fj.10-164921. [DOI] [PubMed] [Google Scholar]
- 47.Fleissner CK, Huebel N, Abd El-Bary MM, Loh G, Klaus S, Blaut M. 2010. Absence of intestinal microbiota does not protect mice from diet-induced obesity. Br J Nutr 104:919–929. doi: 10.1017/S0007114510001303. [DOI] [PubMed] [Google Scholar]
- 48.Kübeck R, Bonet-Ripoll C, Hoffmann C, Walker A, Müller VM, Schüppel VL, Lagkouvardos I, Scholz B, Engel KH, Daniel H, Schmitt-Kopplin P, Haller D, Clavel T, Klingenspor M. 2016. Dietary fat and gut microbiota interactions determine diet-induced obesity in mice. Mol Metab 5:1162–1174. doi: 10.1016/j.molmet.2016.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Miyamoto J, Watanabe K, Taira S, Kasubuchi M, Li X, Irie J, Itoh H, Kimura I. 2018. Barley β-glucan improves metabolic condition via short-chain fatty acids produced by gut microbial fermentation in high fat diet fed mice. PLoS One 13:e0196579. doi: 10.1371/journal.pone.0196579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Just S, Mondot S, Ecker J, Wegner K, Rath E, Gau L, Streidl T, Hery-Arnaud G, Schmidt S, Lesker TR, Bieth V, Dunkel A, Strowig T, Hofmann T, Haller D, Liebisch G, Gérard P, Rohn S, Lepage P, Clavel T. 2018. The gut microbiota drives the impact of bile acids and fat source in diet on mouse metabolism. Microbiome 6:134. doi: 10.1186/s40168-018-0510-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Caesar R, Tremaroli V, Kovatcheva-Datchary P, Cani PD, Bäckhed F. 2015. Crosstalk between gut microbiota and dietary lipids aggravates WAT inflammation through TLR signaling. Cell Metab 22:658–668. doi: 10.1016/j.cmet.2015.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Watanabe K, Igarashi M, Li X, Nakatani A, Miyamoto J, Inaba Y, Sutou A, Saito T, Sato T, Tachibana N, Inoue H, Kimura I. 2018. Dietary soybean protein ameliorates high-fat diet-induced obesity by modifying the gut microbiota-dependent biotransformation of bile acids. PLoS One 13:e0202083. doi: 10.1371/journal.pone.0202083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cantarel BL, Lombard V, Henrissat B. 2012. Complex carbohydrate utilization by the healthy human microbiome. PLoS One 7:e28742. doi: 10.1371/journal.pone.0028742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Baxter NT, Schmidt AW, Venkataraman A, Kim KS, Waldron C, Schmidt TM. 2019. Dynamics of human gut microbiota and short-chain fatty acids in response to dietary interventions with three fermentable fibers. mBio 10:e02566-18. doi: 10.1128/mBio.02566-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Scott KP, Martin JC, Chassard C, Clerget M, Potrykus J, Campbell G, Mayer CD, Young P, Rucklidge G, Ramsay AG, Flint HJ. 2011. Substrate-driven gene expression in Roseburia inulinivorans: importance of inducible enzymes in the utilization of inulin and starch. Proc Natl Acad Sci U S A 108:4672–4679. doi: 10.1073/pnas.1000091107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schnorr SL, Candela M, Rampelli S, Centanni M, Consolandi C, Basaglia G, Turroni S, Biagi E, Peano C, Severgnini M, Fiori J, Gotti R, De Bellis G, Luiselli D, Brigidi P, Mabulla A, Marlowe F, Henry AG, Crittenden AN. 2014. Gut microbiome of the Hadza hunter-gatherers. Nat Commun 5:3654. doi: 10.1038/ncomms4654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.De Filippo C, Cavalieri D, Di Paola M, Ramazzotti M, Poullet JB, Massart S, Collini S, Pieraccini G, Lionetti P. 2010. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc Natl Acad Sci U S A 107:14691–14696. doi: 10.1073/pnas.1005963107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tap J, Furet JP, Bensaada M, Philippe C, Roth H, Rabot S, Lakhdari O, Lombard V, Henrissat B, Corthier G, Fontaine E, Doré J, Leclerc M. 2015. Gut microbiota richness promotes its stability upon increased dietary fibre intake in healthy adults. Environ Microbiol 17:4954–4964. doi: 10.1111/1462-2920.13006. [DOI] [PubMed] [Google Scholar]
- 59.Kovatcheva-Datchary P, Nilsson A, Akrami R, Lee YS, De Vadder F, Arora T, Hallen A, Martens E, Björck I, Bäckhed F. 2015. Dietary fiber-induced improvement in glucose metabolism is associated with increased abundance of Prevotella. Cell Metab 22:971–982. doi: 10.1016/j.cmet.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 60.Mehta RS, Nishihara R, Cao Y, Song M, Mima K, Qian ZR, Nowak JA, Kosumi K, Hamada T, Masugi Y, Bullman S, Drew DA, Kostic AD, Fung TT, Garrett WS, Huttenhower C, Wu K, Meyerhardt JA, Zhang X, Willett WC, Giovannucci EL, Fuchs CS, Chan AT, Ogino S. 2017. Association of dietary patterns with risk of colorectal cancer subtypes classified by Fusobacterium nucleatum in tumor tissue. JAMA Oncol 3:921–927. doi: 10.1001/jamaoncol.2016.6374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Desai MS, Seekatz AM, Koropatkin NM, Kamada N, Hickey CA, Wolter M, Pudlo NA, Kitamoto S, Terrapon N, Muller A, Young VB, Henrissat B, Wilmes P, Stappenbeck TS, Núñez G, Martens EC. 2016. A dietary fiber-deprived gut microbiota degrades the colonic mucus barrier and enhances pathogen susceptibility. Cell 167:1339–1353.e21. doi: 10.1016/j.cell.2016.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sonnenburg JL, Sonnenburg ED. 2019. Vulnerability of the industrialized microbiota. Science 366:eaaw9255. doi: 10.1126/science.aaw9255. [DOI] [PubMed] [Google Scholar]
- 63.McOrist AL, Miller RB, Bird AR, Keogh JB, Noakes M, Topping DL, Conlon MA. 2011. Fecal butyrate levels vary widely among individuals but are usually increased by a diet high in resistant starch. J Nutr 141:883–889. doi: 10.3945/jn.110.128504. [DOI] [PubMed] [Google Scholar]
- 64.Duncan SH, Belenguer A, Holtrop G, Johnstone AM, Flint HJ, Lobley GE. 2007. Reduced dietary intake of carbohydrates by obese subjects results in decreased concentrations of butyrate and butyrate-producing bacteria in feces. Appl Environ Microbiol 73:1073–1078. doi: 10.1128/AEM.02340-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Faith JJ, McNulty NP, Rey FE, Gordon JI. 2011. Predicting a human gut microbiota’s response to diet in gnotobiotic mice. Science 333:101–104. doi: 10.1126/science.1206025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kelly CJ, Zheng L, Campbell EL, Saeedi B, Scholz CC, Bayless AJ, Wilson KE, Glover LE, Kominsky DJ, Magnuson A, Weir TL, Ehrentraut SF, Pickel C, Kuhn KA, Lanis JM, Nguyen V, Taylor CT, Colgan SP. 2015. Crosstalk between microbiota-derived short-chain fatty acids and intestinal epithelial HIF augments tissue barrier function. Cell Host Microbe 17:662–671. doi: 10.1016/j.chom.2015.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ng KM, Aranda-Díaz A, Tropini C, Frankel MR, Van Treuren W, O'Laughlin CT, Merrill BD, Yu FB, Pruss KM, Oliveira RA, Higginbottom SK, Neff NF, Fischbach MA, Xavier KB, Sonnenburg JL, Huang KC. 2019. Recovery of the gut microbiota after antibiotics depends on host diet, community context, and environmental reservoirs. Cell Host Microbe 26:650–665.e4. doi: 10.1016/j.chom.2019.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jang C, Wada S, Yang S, Gosis B, Zeng X, Zhang Z, Shen Y, Lee G, Arany Z, Rabinowitz JD. 2020. The small intestine shields the liver from fructose-induced steatosis. Nat Metab 2:586–593. doi: 10.1038/s42255-020-0222-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhao L, Zhang F, Ding X, Wu G, Lam YY, Wang X, Fu H, Xue X, Lu C, Ma J, Yu L, Xu C, Ren Z, Xu Y, Xu S, Shen H, Zhu X, Shi Y, Shen Q, Dong W, Liu R, Ling Y, Zeng Y, Wang X, Zhang Q, Wang J, Wang L, Wu Y, Zeng B, Wei H, Zhang M, Peng Y, Zhang C. 2018. Gut bacteria selectively promoted by dietary fibers alleviate type 2 diabetes. Science 359:1151–1156. doi: 10.1126/science.aao5774. [DOI] [PubMed] [Google Scholar]
- 70.Park Y, Subar AF, Hollenbeck A, Schatzkin A. 2011. Dietary fiber intake and mortality in the NIH-AARP diet and health study. Arch Intern Med 171:1061–1068. doi: 10.1001/archinternmed.2011.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fava F, Gitau R, Griffin BA, Gibson GR, Tuohy KM, Lovegrove JA. 2013. The type and quantity of dietary fat and carbohydrate alter faecal microbiome and short-chain fatty acid excretion in a metabolic syndrome “at-risk” population. Int J Obes 37:216–223. doi: 10.1038/ijo.2012.33. [DOI] [PubMed] [Google Scholar]
- 72.Parks BW, Nam E, Org E, Kostem E, Norheim F, Hui ST, Pan C, Civelek M, Rau CD, Bennett BJ, Mehrabian M, Ursell LK, He A, Castellani LW, Zinker B, Kirby M, Drake TA, Drevon CA, Knight R, Gargalovic P, Kirchgessner T, Eskin E, Lusis AJ. 2013. Genetic control of obesity and gut microbiota composition in response to high-fat, high-sucrose diet in mice. Cell Metab 17:141–152. doi: 10.1016/j.cmet.2012.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Plovier H, Everard A, Druart C, Depommier C, Van Hul M, Geurts L, Chilloux J, Ottman N, Duparc T, Lichtenstein L, Myridakis A, Delzenne NM, Klievink J, Bhattacharjee A, Van Der Ark KCH, Aalvink S, Martinez LO, Dumas ME, Maiter D, Loumaye A, Hermans MP, Thissen JP, Belzer C, De Vos WM, Cani PD. 2017. A purified membrane protein from Akkermansia muciniphila or the pasteurized bacterium improves metabolism in obese and diabetic mice. Nat Med 23:107–113. doi: 10.1038/nm.4236. [DOI] [PubMed] [Google Scholar]
- 74.Turnbaugh PJ, Bäckhed F, Fulton L, Gordon JI. 2008. Diet-induced obesity is linked to marked but reversible alterations in the mouse distal gut microbiome. Cell Host Microbe 3:213–223. doi: 10.1016/j.chom.2008.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hildebrandt MA, Hoffmann C, Sherrill-Mix SA, Keilbaugh SA, Hamady M, Chen YY, Knight R, Ahima RS, Bushman F, Wu GD. 2009. High-fat diet determines the composition of the murine gut microbiome independently of obesity. Gastroenterology 137:1716–1724.e2. doi: 10.1053/j.gastro.2009.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhang C, Zhang M, Pang X, Zhao Y, Wang L, Zhao L. 2012. Structural resilience of the gut microbiota in adult mice under high-fat dietary perturbations. ISME J 6:1848–1857. doi: 10.1038/ismej.2012.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wan Y, Wang F, Yuan J, Li J, Jiang D, Zhang J, Li H, Wang R, Tang J, Huang T, Zheng J, Sinclair AJ, Mann J, Li D. 2019. Effects of dietary fat on gut microbiota and faecal metabolites, and their relationship with cardiometabolic risk factors: a 6-month randomised controlled-feeding trial. Gut 68:1417–1429. doi: 10.1136/gutjnl-2018-317609. [DOI] [PubMed] [Google Scholar]
- 78.Kim KA, Gu W, Lee IA, Joh EH, Kim DH. 2012. High fat diet-induced gut microbiota exacerbates inflammation and obesity in mice via the TLR4 signaling pathway. PLoS One 7:e47713. doi: 10.1371/journal.pone.0047713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D, Neyrinck AM, Fava F, Tuohy KM, Chabo C, Waget A, Delmée E, Cousin B, Sulpice T, Chamontin B, Ferrières J, Tanti J-F, Gibson GR, Casteilla L, Delzenne NM, Alessi MC, Burcelin R. 2007. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 56:1761–1772. doi: 10.2337/db06-1491. [DOI] [PubMed] [Google Scholar]
- 80.Saberi M, Woods NB, de Luca C, Schenk S, Lu JC, Bandyopadhyay G, Verma IM, Olefsky JM. 2009. Hematopoietic cell-specific deletion of Toll-like receptor 4 ameliorates hepatic and adipose tissue insulin resistance in high-fat-fed mice. Cell Metab 10:419–429. doi: 10.1016/j.cmet.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Amar J, Burcelin R, Ruidavets JB, Cani PD, Fauvel J, Alessi MC, Chamontin B, Ferriéres J. 2008. Energy intake is associated with endotoxemia in apparently healthy men. Am J Clin Nutr 87:1219–1223. doi: 10.1093/ajcn/87.5.1219. [DOI] [PubMed] [Google Scholar]
- 82.Cani PD, Bibiloni R, Knauf C, Waget A, Neyrinck AM, Delzenne NM, Burcelin R. 2008. Changes in gut microbiota control metabolic diet-induced obesity and diabetes in mice. Diabetes 57:1470–1481. doi: 10.2337/db07-1403. [DOI] [PubMed] [Google Scholar]
- 83.Świątecka D, Dominika Ś, Narbad A, Arjan N, Ridgway KP, Karyn RP, Kostyra H, Henryk K. 2011. The study on the impact of glycated pea proteins on human intestinal bacteria. Int J Food Microbiol 145:267–272. doi: 10.1016/j.ijfoodmicro.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 84.Zhu Y, Lin X, Zhao F, Shi X, Li H, Li Y, Zhu W, Xu X, Li C, Zhou G. 2015. Meat, dairy and plant proteins alter bacterial composition of rat gut bacteria. Sci Rep 5:16546–16514. doi: 10.1038/srep16546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Christensen L, Roager HM, Astrup A, Hjorth MF. 2018. Microbial enterotypes in personalized nutrition and obesity management. Am J Clin Nutr 108:645–651. doi: 10.1093/ajcn/nqy175. [DOI] [PubMed] [Google Scholar]
- 86.Sanz Y, Romaní-Perez M, Benítez-Páez A, Portune KJ, Brigidi P, Rampelli S, Dinan T, Stanton C, Delzenne N, Blachier F, Neyrinck AM, Beaumont M, Olivares M, Holzer P, Günther K, Wolters M, Ahrens W, Claus SP, Campoy C, Murphy R, Sadler C, Fernández L, van der Kamp JW. 2018. Towards microbiome-informed dietary recommendations for promoting metabolic and mental health: opinion papers of the MyNewGut project. Clin Nutr 37:2191–2197. doi: 10.1016/j.clnu.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 87.Portune KJ, Beaumont M, Davila AM, Tomé D, Blachier F, Sanz Y. 2016. Gut microbiota role in dietary protein metabolism and health-related outcomes: the two sides of the coin. Trends Food Sci Technol 57:213–232. doi: 10.1016/j.tifs.2016.08.011. [DOI] [Google Scholar]
- 88.Chassaing B, Van De Wiele T, De Bodt J, Marzorati M, Gewirtz AT. 2017. Dietary emulsifiers directly alter human microbiota composition and gene expression ex vivo potentiating intestinal inflammation. Gut 66:1414–1427. doi: 10.1136/gutjnl-2016-313099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Viennois E, Merlin D, Gewirtz AT, Chassaing B. 2017. Dietary emulsifier-induced low-grade inflammation promotes colon carcinogenesis. Cancer Res 77:27–40. doi: 10.1158/0008-5472.CAN-16-1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chassaing B, Koren O, Goodrich JK, Poole AC, Srinivasan S, Ley RE, Gewirtz AT. 2015. Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome. Nature 519:92–96. doi: 10.1038/nature14232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rodriguez-Palacios A, Harding A, Menghini P, Himmelman C, Retuerto M, Nickerson KP, Lam M, Croniger CM, McLean MH, Durum SK, Pizarro TT, Ghannoum MA, Ilic S, McDonald C, Cominelli F. 2018. The artificial sweetener Splenda promotes gut proteobacteria, dysbiosis, and myeloperoxidase reactivity in Crohn’s disease-like ileitis. Inflamm Bowel Dis 24:1005–1020. doi: 10.1093/ibd/izy060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Uebanso T, Ohnishi A, Kitayama R, Yoshimoto A, Nakahashi M, Shimohata T, Mawatari K, Takahashi A. 2017. Effects of low-dose non-caloric sweetener consumption on gut microbiota in mice. Nutrients 9:560. doi: 10.3390/nu9060560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bian X, Tu P, Chi L, Gao B, Ru H, Lu K. 2017. Saccharin induced liver inflammation in mice by altering the gut microbiota and its metabolic functions. Food Chem Toxicol 107:530–539. doi: 10.1016/j.fct.2017.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ruiz-Ojeda FJ, Plaza-Díaz J, Sáez-Lara MJ, Gil A. 2019. Effects of sweeteners on the gut microbiota: a review of experimental studies and clinical trials. Adv Nutr 10:S31–S48. doi: 10.1093/advances/nmy037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Suez J, Korem T, Zeevi D, Zilberman-Schapira G, Thaiss CA, Maza O, Israeli D, Zmora N, Gilad S, Weinberger A, Kuperman Y, Harmelin A, Kolodkin-Gal I, Shapiro H, Halpern Z, Segal E, Elinav E. 2014. Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature 514:181–186. doi: 10.1038/nature13793. [DOI] [PubMed] [Google Scholar]
- 96.Wang QP, Browman D, Herzog H, Gregory Neely G. 2018. Non-nutritive sweeteners possess a bacteriostatic effect and alter gut microbiota in mice. PLoS One 13:e0199080. doi: 10.1371/journal.pone.0199080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Collins J, Robinson C, Danhof H, Knetsch CW, van Leeuwen HC, Lawley TD, Auchtung JM, Britton RA. 2018. Dietary trehalose enhances virulence of epidemic Clostridium difficile. Nature 553:291–294. doi: 10.1038/nature25178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Goossens DAM, Jonkers DMAE, Russel MGVM, Stobberingh EE, Stockbrügger RW. 2006. The effect of a probiotic drink with Lactobacillus plantarum 299v on the bacterial composition in faeces and mucosal biopsies of rectum and ascending colon. Aliment Pharmacol Ther 23:255–263. doi: 10.1111/j.1365-2036.2006.02749.x. [DOI] [PubMed] [Google Scholar]
- 99.Laursen MF, Laursen RP, Larnkjær A, Michaelsen KF, Bahl MI, Licht TR. 2017. Administration of two probiotic strains during early childhood does not affect the endogenous gut microbiota composition despite probiotic proliferation. BMC Microbiol 17:175. doi: 10.1186/s12866-017-1090-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kristensen NB, Bryrup T, Allin KH, Nielsen T, Hansen TH, Pedersen O. 2016. Alterations in fecal microbiota composition by probiotic supplementation in healthy adults: a systematic review of randomized controlled trials. Genome Med 8:52. doi: 10.1186/s13073-016-0300-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zmora N, Zilberman-Schapira G, Suez J, Mor U, Dori-Bachash M, Bashiardes S, Kotler E, Zur M, Regev-Lehavi D, Brik RB-Z, Federici S, Cohen Y, Linevsky R, Rothschild D, Moor AE, Ben-Moshe S, Harmelin A, Itzkovitz S, Maharshak N, Shibolet O, Shapiro H, Pevsner-Fischer M, Sharon I, Halpern Z, Segal E, Elinav E. 2018. Personalized gut mucosal colonization resistance to empiric probiotics is associated with unique host and microbiome features. Cell 174:1388–1405.e21. doi: 10.1016/j.cell.2018.08.041. [DOI] [PubMed] [Google Scholar]
- 102.Watson H, Mitra S, Croden FC, Taylor M, Wood HM, Perry SL, Spencer JA, Quirke P, Toogood GJ, Lawton CL, Dye L, Loadman PM, Hull MA. 2018. A randomised trial of the effect of omega-3 polyunsaturated fatty acid supplements on the human intestinal microbiota. Gut 67:1974–1983. doi: 10.1136/gutjnl-2017-314968. [DOI] [PubMed] [Google Scholar]
- 103.Javdan B, Lopez JG, Chankhamjon P, Lee Y-CJ, Hull R, Wu Q, Wang X, Chatterjee S, Donia MS. 2020. Personalized mapping of drug metabolism by the human gut microbiome. Cell 181:1661–1679.e22. doi: 10.1016/j.cell.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Maier L, Pruteanu M, Kuhn M, Zeller G, Telzerow A, Anderson EE, Brochado AR, Fernandez KC, Dose H, Mori H, Patil KR, Bork P, Typas A. 2018. Extensive impact of non-antibiotic drugs on human gut commensals. Nature 555:623–628. doi: 10.1038/nature25979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Vieira-Silva S, Falony G, Belda E, Nielsen T, Aron-Wisnewsky J, Chakaroun R, Forslund SK, Assmann K, Valles-Colomer M, Nguyen TTD, Proost S, Prifti E, Tremaroli V, Pons N, Le Chatelier E, Andreelli F, Bastard J-P, Coelho LP, Galleron N, Hansen TH, Hulot JS, Lewinter C, Pedersen HK, Quinquis B, Rouault C, Roume H, Salem J-E, Søndertoft NB, Touch S, MetaCardis Consortium, et al. 2020. Statin therapy is associated with lower prevalence of gut microbiota dysbiosis. Nature 581:310–315. doi: 10.1038/s41586-020-2269-x. [DOI] [PubMed] [Google Scholar]
- 106.Schroeder BO, Bäckhed F. 2016. Signals from the gut microbiota to distant organs in physiology and disease. Nat Med 22:1079–1089. doi: 10.1038/nm.4185. [DOI] [PubMed] [Google Scholar]
- 107.Livingston S, Pauli LL. 1975. Ketogenic diet and epilepsy. Dev Med Child Neurol 17:818–819. doi: 10.1111/j.1469-8749.1975.tb04712.x. [DOI] [PubMed] [Google Scholar]
- 108.Ang QY, Alexander M, Newman JC, Tian Y, Cai J, Upadhyay V, Turnbaugh JA, Verdin E, Hall KD, Leibel RL, Ravussin E, Rosenbaum M, Patterson AD, Turnbaugh PJ. 2020. Ketogenic diets alter the gut microbiome resulting in decreased intestinal Th17 cells. Cell 181:1263–1275.e16. doi: 10.1016/j.cell.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Olson CA, Vuong HE, Yano JM, Liang QY, Nusbaum DJ, Hsiao EY. 2018. The gut microbiota mediates the anti-seizure effects of the ketogenic diet. Cell 173:1728–1741.e13. doi: 10.1016/j.cell.2018.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kurilshikov A, Wijmenga C, Fu J, Zhernakova A. 2017. Host genetics and gut microbiome: challenges and perspectives. Trends Immunol 38:633–647. doi: 10.1016/j.it.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 111.Cotillard A, Kennedy SP, Kong LC, Prifti E, Pons N, Le Chatelier E, Almeida M, Quinquis B, Levenez F, Galleron N, Gougis S, Rizkalla S, Batto J-M, Renault P, ANR MicroObes consortium, Doré J, Zucker J-D, Clément K, Ehrlich SD. 2013. Dietary intervention impact on gut microbial gene richness. Nature 500:585–588. doi: 10.1038/nature12480. [DOI] [PubMed] [Google Scholar]
- 112.Rothschild D, Weissbrod O, Barkan E, Kurilshikov A, Korem T, Zeevi D, Costea PI, Godneva A, Kalka IN, Bar N, Shilo S, Lador D, Vila AV, Zmora N, Pevsner-Fischer M, Israeli D, Kosower N, Malka G, Wolf BC, Avnit-Sagi T, Lotan-Pompan M, Weinberger A, Halpern Z, Carmi S, Fu J, Wijmenga C, Zhernakova A, Elinav E, Segal E. 2018. Environment dominates over host genetics in shaping human gut microbiota. Nature 555:210–215. doi: 10.1038/nature25973. [DOI] [PubMed] [Google Scholar]
- 113.Johnson AJ, Vangay P, Al-Ghalith GA, Hillmann BM, Ward TL, Shields-Cutler RR, Kim AD, Shmagel AK, Syed AN, Walter J, Menon R, Koecher K, Knights D, Personalized Microbiome Class Students. 2019. Daily sampling reveals personalized diet-microbiome associations in humans. Cell Host Microbe 25:789–802.e5. doi: 10.1016/j.chom.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 114.Wang T, Heianza Y, Sun D, Huang T, Ma W, Rimm EB, Manson JE, Hu FB, Willett WC, Qi L. 2018. Improving adherence to healthy dietary patterns, genetic risk, and long term weight gain: gene-diet interaction analysis in two prospective cohort studies. BMJ 360:j5644. doi: 10.1136/bmj.j5644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Stroebele-Benschop N, Dieze A, Hilzendegen C. 2018. Students’ adherence to dietary recommendations and their food consumption habits. Nutr Health 24:75–81. doi: 10.1177/0260106018772946. [DOI] [PubMed] [Google Scholar]
- 116.Mehta T, Smith DL, Muhammad J, Casazza K. 2014. Impact of weight cycling on risk of morbidity and mortality. Obes Rev 15:870–881. doi: 10.1111/obr.12222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Griffin NW, Ahern PP, Cheng J, Heath AC, Ilkayeva O, Newgard CB, Fontana L, Gordon JI. 2017. Prior dietary practices and connections to a human gut microbial metacommunity alter responses to diet interventions. Cell Host Microbe 21:84–96. doi: 10.1016/j.chom.2016.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Thomson P, Santibañez R, Aguirre C, Galgani JE, Garrido D. 2019. Short-term impact of sucralose consumption on the metabolic response and gut microbiome of healthy adults. Br J Nutr 122:856–862. doi: 10.1017/S0007114519001570. [DOI] [PubMed] [Google Scholar]
- 119.Korem T, Zeevi D, Zmora N, Weissbrod O, Bar N, Lotan-Pompan M, Avnit-Sagi T, Kosower N, Malka G, Rein M, Suez J, Goldberg BZ, Weinberger A, Levy AA, Elinav E, Segal E. 2017. Bread affects clinical parameters and induces gut microbiome-associated personal glycemic responses. Cell Metab 25:1243–1253.e5. doi: 10.1016/j.cmet.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 120.Fragiadakis GK, Wastyk HC, Robinson JL, Sonnenburg ED, Sonnenburg JL, Gardner CD. 2020. Long-term dietary intervention reveals resilience of the gut microbiota despite changes in diet and weight. Am J Clin Nutr 111:1127–1136. doi: 10.1093/ajcn/nqaa046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Dao MC, Everard A, Aron-Wisnewsky J, Sokolovska N, Prifti E, Verger EO, Kayser BD, Levenez F, Chilloux J, Hoyles L, MICRO-Obes Consortium, Dumas M-E, Rizkalla SW, Doré J, Cani PD, Clément K. 2016. Akkermansia muciniphila and improved metabolic health during a dietary intervention in obesity: relationship with gut microbiome richness and ecology. Gut 65:426–436. doi: 10.1136/gutjnl-2014-308778. [DOI] [PubMed] [Google Scholar]
- 122.Kong LC, Wuillemin P-H, Bastard J-P, Sokolovska N, Gougis S, Fellahi S, Darakhshan F, Bonnefont-Rousselot D, Bittar R, Doré J, Zucker J-D, Clément K, Rizkalla S. 2013. Insulin resistance and inflammation predict kinetic body weight changes in response to dietary weight loss and maintenance in overweight and obese subjects by using a Bayesian network approach. Am J Clin Nutr 98:1385–1394. doi: 10.3945/ajcn.113.058099. [DOI] [PubMed] [Google Scholar]
- 123.Korpela K, Flint HJ, Johnstone AM, Lappi J, Poutanen K, Dewulf E, Delzenne N, De Vos WM, Salonen A. 2014. Gut microbiota signatures predict host and microbiota responses to dietary interventions in obese individuals. PLoS One 9:e90702. doi: 10.1371/journal.pone.0090702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Clark RL, Famodu OA, Holásková I, Infante AM, Murray PJ, Olfert IM, McFadden JW, Downes MT, Chantler PD, Duespohl MW, Cuff CF, Olfert MD. 2019. Educational intervention improves fruit and vegetable intake in young adults with metabolic syndrome components. Nutr Res 62:89–100. doi: 10.1016/j.nutres.2018.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bennet SMP, Böhn L, Störsrud S, Liljebo T, Collin L, Lindfors P, Törnblom H, Öhman L, Simrén M. 2018. Multivariate modelling of faecal bacterial profiles of patients with IBS predicts responsiveness to a diet low in FODMAPs. Gut 67:872–881. doi: 10.1136/gutjnl-2016-313128. [DOI] [PubMed] [Google Scholar]
- 126.Chumpitazi BP, Hollister EB, Oezguen N, Tsai CM, McMeans AR, Luna RA, Savidge TC, Versalovic J, Shulman RJ. 2014. Gut microbiota influences low fermentable substrate diet efficacy in children with irritable bowel syndrome. Gut Microbes 5:165–175. doi: 10.4161/gmic.27923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Halmos EP, Christophersen CT, Bird AR, Shepherd SJ, Gibson PR, Muir JG. 2015. Diets that differ in their FODMAP content alter the colonic luminal microenvironment. Gut 64:93–100. doi: 10.1136/gutjnl-2014-307264. [DOI] [PubMed] [Google Scholar]
- 128.Valeur J, Småstuen MC, Knudsen T, Lied GA, Røseth AG. 2018. Exploring gut microbiota composition as an indicator of clinical response to dietary FODMAP restriction in patients with irritable bowel syndrome. Dig Dis Sci 63:429–436. doi: 10.1007/s10620-017-4893-3. [DOI] [PubMed] [Google Scholar]
- 129.Chumpitazi BP, Cope JL, Hollister EB, Tsai CM, McMeans AR, Luna RA, Versalovic J, Shulman RJ. 2015. Randomised clinical trial: gut microbiome biomarkers are associated with clinical response to a low FODMAP diet in children with the irritable bowel syndrome. Aliment Pharmacol Ther 42:418–427. doi: 10.1111/apt.13286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Koeth RA, Lam-Galvez BR, Kirsop J, Wang Z, Levison BS, Gu X, Copeland MF, Bartlett D, Cody DB, Dai HJ, Culley MK, Li XS, Fu X, Wu Y, Li L, DiDonato JA, Tang WHW, Garcia-Garcia JC, Hazen SL. 2019. l-Carnitine in omnivorous diets induces an atherogenic gut microbial pathway in humans. J Clin Invest 129:373–387. doi: 10.1172/JCI94601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Koeth RA, Wang Z, Levison BS, Buffa JA, Org E, Sheehy BT, Britt EB, Fu X, Wu Y, Li L, Smith JD, Didonato JA, Chen J, Li H, Wu GD, Lewis JD, Warrier M, Brown JM, Krauss RM, Tang WHW, Bushman FD, Lusis AJ, Hazen SL. 2013. Intestinal microbiota metabolism of l-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med 19:576–585. doi: 10.1038/nm.3145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Tang WHW, Wang Z, Levison BS, Koeth RA, Britt EB, Fu X, Wu Y, Hazen SL. 2013. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med 368:1575–1584. doi: 10.1056/NEJMoa1109400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Li Z, Wu Z, Yan J, Liu H, Liu Q, Deng Y, Ou C, Chen M. 2019. Gut microbe-derived metabolite trimethylamine N-oxide induces cardiac hypertrophy and fibrosis. Lab Invest 99:346–357. doi: 10.1038/s41374-018-0091-y. [DOI] [PubMed] [Google Scholar]
- 134.Cho CE, Taesuwan S, Malysheva OV, Bender E, Tulchinsky NF, Yan J, Sutter JL, Caudill MA. 2017. Trimethylamine-N-oxide (TMAO) response to animal source foods varies among healthy young men and is influenced by their gut microbiota composition: a randomized controlled trial. Mol Nutr Food Res 61:1–12. doi: 10.1002/mnfr.201600324. [DOI] [PubMed] [Google Scholar]
- 135.Zhu W, Gregory JC, Org E, Buffa JA, Gupta N, Wang Z, Li L, Fu X, Wu Y, Mehrabian M, Sartor RB, McIntyre TM, Silverstein RL, Tang WHW, Didonato JA, Brown JM, Lusis AJ, Hazen SL. 2016. Gut microbial metabolite TMAO enhances platelet hyperreactivity and thrombosis risk. Cell 165:111–124. doi: 10.1016/j.cell.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Wang Z, Roberts AB, Buffa JA, Levison BS, Zhu W, Org E, Gu X, Huang Y, Zamanian-Daryoush M, Culley MK, Didonato AJ, Fu X, Hazen JE, Krajcik D, Didonato JA, Lusis AJ, Hazen SL. 2015. Non-lethal inhibition of gut microbial trimethylamine production for the treatment of atherosclerosis. Cell 163:1585–1595. doi: 10.1016/j.cell.2015.11.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Wu WK, Chen CC, Liu PY, Panyod S, Liao BY, Chen PC, Kao HL, Kuo HC, Kuo CH, Chiu THT, Chen RA, Chuang HL, Te Huang Y, Zou HB, Hsu CC, Chang TY, Lin CL, Ho CT, Yu HT, Sheen LY, Wu MS. 2019. Identification of TMAO-producer phenotype and host-diet-gut dysbiosis by carnitine challenge test in human and germ-free mice. Gut 68:1439–1449. doi: 10.1136/gutjnl-2018-317155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Candela M, Biagi E, Soverini M, Consolandi C, Quercia S, Severgnini M, Peano C, Turroni S, Rampelli S, Pozzilli P, Pianesi M, Fallucca F, Brigidi P. 2016. Modulation of gut microbiota dysbioses in type 2 diabetic patients by macrobiotic Ma-Pi 2 diet. Br J Nutr 116:80–93. doi: 10.1017/S0007114516001045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Makki K, Deehan EC, Walter J, Bäckhed F. 2018. The impact of dietary fiber on gut microbiota in host health and disease. Cell Host Microbe 23:705–715. doi: 10.1016/j.chom.2018.05.012. [DOI] [PubMed] [Google Scholar]
- 140.Deehan EC, Yang C, Perez-Muñoz ME, Nguyen NK, Cheng CC, Triador L, Zhang Z, Bakal JA, Walter J. 2020. Precision microbiome modulation with discrete dietary fiber structures directs short-chain fatty acid production. Cell Host Microbe 27:389–404.e6. doi: 10.1016/j.chom.2020.01.006. [DOI] [PubMed] [Google Scholar]
- 141.Davis LMG, Martínez I, Walter J, Goin C, Hutkins RW. 2011. Barcoded pyrosequencing reveals that consumption of galactooligosaccharides results in a highly specific bifidogenic response in humans. PLoS One 6:e25200. doi: 10.1371/journal.pone.0025200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Roager HM, Vogt JK, Kristensen M, Hansen LBS, Ibrügger S, Mærkedahl RB, Bahl MI, Lind MV, Nielsen RL, Frøkiær H, Gøbel RJ, Landberg R, Ross AB, Brix S, Holck J, Meyer AS, Sparholt MH, Christensen AF, Carvalho V, Hartmann B, Holst JJ, Rumessen JJ, Linneberg A, Sicheritz-Pontén T, Dalgaard MD, Blennow A, Frandsen HL, Villas-Bôas S, Kristiansen K, Vestergaard H, Hansen T, Ekstrøm CT, Ritz C, Nielsen HB, Pedersen OB, Gupta R, Lauritzen L, Licht TR. 2019. Whole grain-rich diet reduces body weight and systemic low-grade inflammation without inducing major changes of the gut microbiome: a randomised cross-over trial. Gut 68:83–93. doi: 10.1136/gutjnl-2017-314786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Flint HJ, Duncan SH, Scott KP, Louis P. 2015. Links between diet, gut microbiota composition and gut metabolism. Proc Nutr Soc 74:13–22. doi: 10.1017/S0029665114001463. [DOI] [PubMed] [Google Scholar]
- 144.Benítez-Páez A, Kjølbæk L, Gómez del Pulgar EM, Brahe LK, Astrup A, Matysik S, Schött H-F, Krautbauer S, Liebisch G, Boberska J, Claus S, Rampelli S, Brigidi P, Larsen LH, Sanz Y. 2019. A multi-omics approach to unraveling the microbiome-mediated effects of arabinoxylan oligosaccharides in overweight humans. mSystems 4:e00209-19. doi: 10.1128/mSystems.00209-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Le Chatelier E, Nielsen T, Qin J, Prifti E, Hildebrand F, Falony G, Almeida M, Arumugam M, Batto J-M, Kennedy S, Leonard P, Li J, Burgdorf K, Grarup N, Jørgensen T, Brandslund I, Nielsen HB, Juncker AS, Bertalan M, Levenez F, Pons N, Rasmussen S, Sunagawa S, Tap J, Tims S, Zoetendal EG, Brunak S, Clément K, Doré J, Kleerebezem M, Kristiansen K, Renault P, Sicheritz-Ponten T, de Vos WM, Zucker J-D, Raes J, Hansen T, MetaHIT consortium, Bork P, Wang J, Ehrlich SD, Pedersen O. 2013. Richness of human gut microbiome correlates with metabolic markers. Nature 500:541–546. doi: 10.1038/nature12506. [DOI] [PubMed] [Google Scholar]
- 146.Martínez I, Lattimer JM, Hubach KL, Case JA, Yang J, Weber CG, Louk JA, Rose DJ, Kyureghian G, Peterson DA, Haub MD, Walter J. 2013. Gut microbiome composition is linked to whole grain-induced immunological improvements. ISME J 7:269–280. doi: 10.1038/ismej.2012.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.De Preter V, Vanhoutte T, Huys G, Swings J, Rutgeerts P, Verbeke K. 2007. Baseline microbiota activity and initial bifidobacteria counts influence responses to prebiotic dosing in healthy subjects. Aliment Pharmacol Ther 27:504–513. doi: 10.1111/j.1365-2036.2007.03588.x. [DOI] [PubMed] [Google Scholar]
- 148.Salonen A, Lahti L, Salojärvi J, Holtrop G, Korpela K, Duncan SH, Date P, Farquharson F, Johnstone AM, Lobley GE, Louis P, Flint HJ, De Vos WM. 2014. Impact of diet and individual variation on intestinal microbiota composition and fermentation products in obese men. ISME J 8:2218–2230. doi: 10.1038/ismej.2014.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Bouhnik Y, Raskine L, Simoneau G, Vicaut E, Neut C, Flourié B, Brouns F, Bornet FR. 2004. The capacity of nondigestible carbohydrates to stimulate fecal bifidobacteria in healthy humans: a double-blind, randomized, placebo-controlled, parallel-group, dose-response relation study. Am J Clin Nutr 80:1658–1664. doi: 10.1093/ajcn/80.6.1658. [DOI] [PubMed] [Google Scholar]
- 150.Christensen L, Vuholm S, Roager HM, Nielsen DS, Krych L, Kristensen M, Astrup A, Hjorth MF. 2019. Prevotella abundance predicts weight loss success in healthy, overweight adults consuming a whole-grain diet ad libitum: a post hoc analysis of a 6-wk randomized controlled trial. J Nutr 149:2174–2181. doi: 10.1093/jn/nxz198. [DOI] [PubMed] [Google Scholar]
- 151.Hjorth MF, Blædel T, Bendtsen LQ, Lorenzen JK, Holm JB, Kiilerich P, Roager HM, Kristiansen K, Larsen LH, Astrup A. 2019. Prevotella-to-Bacteroides ratio predicts body weight and fat loss success on 24-week diets varying in macronutrient composition and dietary fiber: results from a post-hoc analysis. Int J Obes 43:149–157. doi: 10.1038/s41366-018-0093-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Sandberg J, Kovatcheva-Datchary P, Björck I, Bäckhed F, Nilsson A. 2019. Abundance of gut Prevotella at baseline and metabolic response to barley prebiotics. Eur J Nutr 58:2365–2376. doi: 10.1007/s00394-018-1788-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Eilam O, Zarecki R, Oberhardt M, Ursell LK, Kupiec M, Knight R, Gophna U. 2014. Glycan degradation (GlyDeR) analysis predicts mammalian gut microbiota abundance and host diet-specific adaptions. mBio 5:e01526-14. doi: 10.1128/mBio.01526-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Sonnenburg ED, Smits SA, Tikhonov M, Higginbottom SK, Wingreen NS, Sonnenburg JL. 2016. Diet-induced extinctions in the gut microbiota compound over generations. Nature 529:212–215. doi: 10.1038/nature16504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Vrieze A, Van Nood E, Holleman F, Salojärvi J, Kootte RS, Bartelsman JFWM, Dallinga-Thie GM, Ackermans MT, Serlie MJ, Oozeer R, Derrien M, Druesne A, Van Hylckama Vlieg JET, Bloks VW, Groen AK, Heilig HGHJ, Zoetendal EG, Stroes ES, de Vos WM, Hoekstra JBL, Nieuwdorp M. 2012. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology 143:913–916.e7. doi: 10.1053/j.gastro.2012.06.031. [DOI] [PubMed] [Google Scholar]
- 156.Pedersen HK, Gudmundsdottir V, Nielsen HB, Hyotylainen T, Nielsen T, Jensen BAH, Forslund K, Hildebrand F, Prifti E, Falony G, Le Chatelier E, Levenez F, Doré J, Mattila I, Plichta DR, Pöhö P, Hellgren LI, Arumugam M, Sunagawa S, Vieira-Silva S, Jørgensen T, Holm JB, Trošt K, MetaHIT Consortium, Kristiansen K, Brix S, Raes J, Wang J, Hansen T, Bork P, Brunak S, Oresic M, Ehrlich SD, Pedersen O. 2016. Human gut microbes impact host serum metabolome and insulin sensitivity. Nature 535:376–381. doi: 10.1038/nature18646. [DOI] [PubMed] [Google Scholar]
- 157.Liu Y, Wang Y, Ni Y, Cheung CKY, Lam KSL, Wang Y, Xia Z, Ye D, Guo J, Tse MA, Panagiotou G, Xu A. 2020. Gut microbiome fermentation determines the efficacy of exercise for diabetes prevention. Cell Metab 31:77–91.e5. doi: 10.1016/j.cmet.2019.11.001. [DOI] [PubMed] [Google Scholar]
- 158.Kootte RS, Levin E, Salojärvi J, Smits LP, Hartstra AV, Udayappan SD, Hermes G, Bouter KE, Koopen AM, Holst JJ, Knop FK, Blaak EE, Zhao J, Smidt H, Harms AC, Hankemeijer T, Bergman J, Romijn HA, Schaap FG, Olde Damink SWM, Ackermans MT, Dallinga-Thie GM, Zoetendal E, de Vos WM, Serlie MJ, Stroes ESG, Groen AK, Nieuwdorp M. 2017. Improvement of insulin sensitivity after lean donor feces in metabolic syndrome is driven by baseline intestinal microbiota composition. Cell Metab 26:611–619.e6. doi: 10.1016/j.cmet.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 159.Udayappan SD, Hartstra AV, Dallinga-Thie GM, Nieuwdorp M. 2014. Intestinal microbiota and faecal transplantation as treatment modality for insulin resistance and type 2 diabetes mellitus. Clin Exp Immunol 177:24–29. doi: 10.1111/cei.12293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Psichas A, Sleeth ML, Murphy KG, Brooks L, Bewick GA, Hanyaloglu AC, Ghatei MA, Bloom SR, Frost G. 2015. 2. Int J Obes (Lond) 39:424–429. doi: 10.1038/ijo.2014.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Vrolix R, Mensink RP. 2010. Variability of the glycemic response to single food products in healthy subjects. Contemp Clin Trials 31:5–11. doi: 10.1016/j.cct.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 162.Vega-López S, Ausman LM, Griffith JL, Lichtenstein AH. 2007. Interindividual variability and intra-individual reproducibility of glycemic index values for commercial white bread. Diabetes Care 30:1412–1417. doi: 10.2337/dc06-1598. [DOI] [PubMed] [Google Scholar]
- 163.Zeevi D, Korem T, Zmora N, Israeli D, Rothschild D, Weinberger A, Ben-Yacov O, Lador D, Avnit-Sagi T, Lotan-Pompan M, Suez J, Mahdi JA, Matot E, Malka G, Kosower N, Rein M, Zilberman-Schapira G, Dohnalová L, Pevsner-Fischer M, Bikovsky R, Halpern Z, Elinav E, Segal E. 2015. Personalized nutrition by prediction of glycemic responses. Cell 163:1079–1095. doi: 10.1016/j.cell.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 164.Karlsson FH, Tremaroli V, Nookaew I, Bergström G, Behre CJ, Fagerberg B, Nielsen J, Bäckhed F. 2013. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature 498:99–103. doi: 10.1038/nature12198. [DOI] [PubMed] [Google Scholar]
- 165.He Y, Wu W, Zheng H-M, Li P, McDonald D, Sheng H-F, Chen M-X, Chen Z-H, Ji G-Y, Zheng Z-D-X, Mujagond P, Chen X-J, Rong Z-H, Chen P, Lyu L-Y, Wang X, Wu C-B, Yu N, Xu Y-J, Yin J, Raes J, Knight R, Ma W-J, Zhou H-W. 2018. Regional variation limits applications of healthy gut microbiome reference ranges and disease models. Nat Med 24:1532–1535. doi: 10.1038/s41591-018-0164-x. [DOI] [PubMed] [Google Scholar]
- 166.Mendes-Soares H, Raveh-Sadka T, Azulay S, Edens K, Ben-Shlomo Y, Cohen Y, Ofek T, Bachrach D, Stevens J, Colibaseanu D, Segal L, Kashyap P, Nelson H. 2019. Assessment of a personalized approach to predicting postprandial glycemic responses to food among individuals without diabetes. JAMA Netw Open 2:e188102. doi: 10.1001/jamanetworkopen.2018.8102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Bailey T, Bode BW, Christiansen MP, Klaff LJ, Alva S. 2015. The performance and usability of a factory-calibrated flash glucose monitoring system. Diabetes Technol Ther 17:787–794. doi: 10.1089/dia.2014.0378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Howard R, Guo J, Hall KD. 2020. Imprecision nutrition? Different simultaneous continuous glucose monitors provide discordant meal rankings for incremental postprandial glucose in subjects without diabetes. Am J Clin Nutr 2020:nqaa198. doi: 10.1093/ajcn/nqaa198. [DOI] [PMC free article] [PubMed] [Google Scholar]