Abstract
The aim of this review is to systematically describe and quantify the effects of PA interventions on alcohol and other drug use outcomes, and to identify any apparent effect of PA dose and type, possible mechanisms of effect, and any other aspect of intervention delivery (e.g. key behaviour change processes), within a framework to inform the design and evaluation of future interventions. Systematic searches were designed to identify published and grey literature on the role of PA for reducing the risk of progression to alcohol and other drug use (PREVENTION), supporting individuals to reduce alcohol and other drug use for harm reduction (REDUCTION), and promote abstinence and relapse prevention during and after treatment of alcohol and other drug use (TREATMENT). Searches identified 49,518 records, with 49,342 excluded on title and abstract. We screened 176 full text articles from which we included 32 studies in 32 papers with quantitative results of relevance to this review. Meta-analysis of two studies showed a significant effect of PA on prevention of alcohol initiation (risk ratio [RR]: 0.72, 95%CI: 0.61 to 0.85). Meta-analysis of four studies showed no clear evidence for an effect of PA on alcohol consumption (Standardised Mean Difference [SMD]: 0.19, 95%, Confidence Interval −0.57 to 0.18). We were unable to quantitatively examine the effects of PA interventions on other drug use alone, or in combination with alcohol use, for prevention, reduction or treatment. Among the 19 treatment studies with an alcohol and other drug use outcome, there was a trend for promising short-term effect but with limited information about intervention fidelity and exercise dose, there was a moderate to high risk of bias. We identified no studies reporting the cost-effectiveness of interventions. More rigorous and well-designed research is needed. Our novel approach to the review provides a clearer guide to achieve this in future research questions addressed to inform policy and practice for different populations and settings.
Keywords: Physical activity, Alcohol, Substance, Other drugs, Treatment, Prevention, Reduction
Highlights
-
•
A comprehensive systematic review of physical activity and alcohol and/or substance use.
-
•
Looks at the prevention, reduction, and treatment of alcohol and/or substance use.
-
•
Highlights what may be most effective and gaps in knowledge.
-
•
Considers different elements of physical activity interventions for best practice.
1. Introduction
1.1. Background
Globally, 5.9% and 1% of deaths are attributable to alcohol and other drug use, respectively (World Health Organisation, 2014). Worldwide, alcohol attributable deaths increased from 3.8% in 2004 (World Health Organisation, 2011) to 5.9% in 2012 (World Health Organisation, 2014), and alcohol use is the seventh leading risk factor for both death and disability adjusted life years (Griswold et al., 2018). Mental and addictive disorders affected more than one billion people worldwide in 2016 accounting for 7% of all global burden of disease (Rehm & Shield, 2019) with alcohol and other drug use accounting for 33.0 and 6.9 deaths per 100,000 people, respectively (Peacock et al., 2018). Globally, substance use has failed to decline between 2005 and 2010 (United Nations Office on Drugs and Crime, 2012), with a global lifetime substance use disorder (SUD) prevalence of 3.5% (Degenhardt et al., 2019).
In the UK, alcohol harms are associated with an economic annual cost of around £21 billion (£3.5bn in healthcare (Public Health England, 2013)). Other drug use in the UK has an economic cost of around £15 billion (The Centre for Social Justice, 2013) (£488 million through healthcare (The National Treatment Agency for Substance Misuse, 2012)). Alcohol and other drug use is the leading behavioural risk factor for death in the UK for those aged 15–49 (Public Health England, 2017) and there has been an increase in levels of substance use in the UK in recent years with nearly 1 in 10 adults aged 16–59 in England and Wales having used substances in the past year (Public Health England, 2014).
The global burden of alcohol and other drug use is well known but with relapse rates of up to 60% one year after treatment for clinically diagnosed substance use disorders (SUD) (McLellan, Lewis, O'Brien, & Kleber, 2000; Ramo & Brown, 2008), and specifically 60–90% for clinically diagnosed alcohol use disorders (AUD) (Miller, Walters, & Bennett, 2001; Xie, McHugo, Fox, & Drake, 2005) and pharmacological therapies associated with side effects (Fareed, Casarella, Amar, Vayalapalli, & Drexler, 2009; Maruyama, Macdonald, Borycki, & Zhao, 2013), there is a need for new treatments and preventive interventions.
Physical activity (PA, defined as any bodily movement produced by skeletal muscles that requires energy expenditure, inclusive of organised sport (World Health Organisation, 2017)) may affect alcohol and other drug use through various psychological mechanisms, including an acute reduction in cravings and urges, improved positive affect and mood, and sustained improvement in co-morbid depression and anxiety which are often linked to alcohol and drug use (Linke & Ussher, 2015). Involvement in exercise may help the avoidance of drug use cues, and provide exposure to new environments, which provide diversionary, safe, and immediately rewarding experiences (Linke & Ussher, 2015). Behaviourally, meaningful participation in structured and rewarding activities are a key part of overcoming SUDs, and some physical activities may offer the chance for identity transformation through exposure to such activities, informal social controls, and promoted personal agency (Landale, 2012). Physiologically, animal studies suggest neurobiological changes associated with exercise (Linke & Ussher, 2015; Lynch, Peterson, Sanchez, Abel, & Smith, 2013; Smith & Lynch, 2013), which may help to explain the consistent evidence that exercise acutely reduces consumption of cocaine, morphine, nicotine, and alcohol (Engelmann et al., 2014; Hashemi Nosrat Abadi, Vaghef, Babri, Mahmood-Alilo, & Beirami, 2013; Lynch et al., 2013; Sanchez, Moore, Brunzell, & Lynch, 2013; Thanos et al., 2013). The combination of cognitive, behavioural and physiological processes, while engaging in PA interventions, may provide a valuable approach to prevention, harm reduction and treatment for alcohol and drug use.
There is broad interest in the role of physical activity (PA) as a treatment and reduction strategy for alcohol and other drug use (Taylor, Oh, & Cullen, 2013; Volkow, 2011) and in how physical activity can be used to influence other health behaviours (Taylor, 2014; Thompson, Lambert, Greaves, & Taylor, 2018; Ussher, Faulkner, Angus, Hartmann-Boyce, & Taylor, 2019). Physical activity interventions could impact on the prevention, reduction, and treatment of alcohol and other drug use but previous reviews have been conceptually confusing and methodologically weak. For example, existing reviews have included studies with a focus on alcohol, substance use and smoking in a single meta-analysis, and have not discriminated between studies with a focus on efficacy (i.e., does a dose of exercise work?) versus effectiveness (conducted in different settings with different intervention engagement issues, and possible mechanisms by which exercise may influence outcomes) (Hallgren, Vancampfort, Giesen, Lundin, & Stubbs, 2017; Wang, Wang, Wang, Li, & Zhou, 2014; Zschucke, Heinz, & Strohle, 2012). The reviews have also not clearly differentiated between studies with a focus on prevention, harm reduction and treatment (Hallgren et al., 2017, Simonton, Young, & Johnson, 2018), included nicotine and cigarette smoking with alcohol and substances in the same analyses with studies reporting no outcome related directly to level of substance use (Simonton et al., 2018), used search strategies that were not comprehensive and only included randomised controlled trials (Zschucke et al., 2012).
Given the commonly different treatment approaches and prevalence levels for alcohol and other drug use this review will consider the influence of PA on each separately, even though there may be common potential processes involved. We include studies concerned with prevention, reduction and treatment of both alcohol and substance use in this one review because while the co-morbidity of the behaviours has long been recognised (Stinson et al., 2005), services and interventions for both have become aligned in the UK and globally. Physical activity and exercise as an intervention is rarely prioritised to be promoted within cognitive-behavioural therapies for alcohol and other drug use and a single review is more likely to provide a useful resource professionals and policy makers who are often working with clients with one or both conditions. Also, holistic approaches are routinely used and we are keen for the review to have as broad a reach as possible: For example, those working in the broader field of mental health treatment and prevention are likely to recognise the potential for physical activity to impact on common mechanisms such as depression and anxiety, which also co-exists with the uptake, use and recovery from alcohol and other drug use.
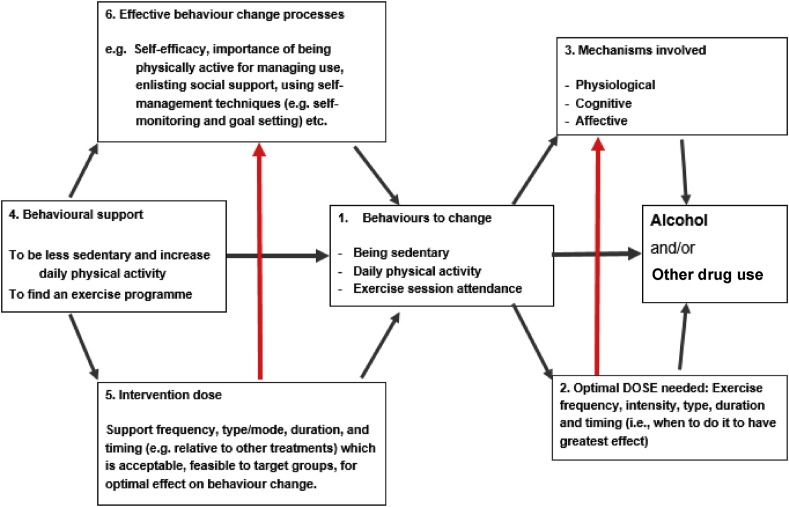
We used the framework shown in Fig. 1 (Taylor & Faulkner, 2014) to structure our review of quantitative literature to describe the complex interaction of the effects of PA on alcohol and drug use, and potential mechanisms of change.
Fig. 1.
Showing 6 topics of interest in our systematic review (red lines represent where dose can influence mechanism). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
This is to attempt to describe processes and outcomes which will be of direct relevance to those designing and implementing interventions with PA to address alcohol and other drug use. The framework highlights 6 important research questions: (1) Does PA and sedentary behaviour (SB) contribute to preventing alcohol and other drug use? (2) What do we know about how dose of behaviour influences these effects? (3) What do we know about the physiological, psychological and social processes/mechanisms that mediate any effects of PA on alcohol and other drug use? (4) What approaches are most effective in supporting changes in PA and SB in the context of influencing alcohol and other drug use? (5) How much support and in what form and duration is needed to optimise changes in PA and SB? (6) What processes of behaviour change and psychological mediators are most important to include in an intervention to change PA and SB in the context of influencing alcohol and other drug use? It also highlights how dose of intervention may affect behaviour change processes, and how dose of PA may affect psychological and physical mechanisms.
The present review is restricted to addressing these questions by considering studies in which quantitative data has been reported. A separate paper details our findings from the synthesis of qualitative studies (Horrell et al. under review).
2. Aims
Linked to Fig. 1, our aims were as follows:
Primary aim: to assess the effects of PA interventions, versus no PA control, on alcohol and other drug use outcomes.
Secondary aim: describe any apparent effect of PA dose, possible mechanisms of effect, impact of intervention type and dose, significant intervention components on alcohol and other drug use (including behaviour change processes), and report and analyse any cost-effectiveness or economic data.
3. Methods
Detailed methods for this review have been published elsewhere (Thompson, Taylor, et al., 2018), and is registered with PROSPERO (registration number CRD42017079322).
The scope of the review was to locate studies relating to PA and its potential to impact our three outcome domains:
-
1.
Reduce the risk of progression to alcohol and other drug use; by preventing the initiation of use among those who are abstinent and preventing the progression to a disorder (PREVENTION);
-
2.
Support individuals to reduce alcohol and other drug use for harm reduction; among the general population who do not have a diagnosed disorder or are not seeking structured treatment programmes (REDUCTION), and;
-
3.
Promote abstinence and relapse prevention during and after structured treatment programmes for SUD (including AUD) (TREATMENT).
To differentiate between reduction and treatment, studies involving participants who were diagnosed with SUD or who were actively seeking treatment were classified as ‘treatment’ studies. Studies involving participants who were neither seeking treatment nor diagnosed with SUD were classified as reduction studies. Prevention studies were those that involved an intervention that explicitly aimed to prevent participant initiation of use, or had outcomes reflecting progression from non-use to use in those who have previously not used alcohol and/or other drugs. The differentiation between these three categories was developed by an expert advisory group and consultation with practitioners and people with lived experience, based on differing population characteristics and different treatment pathways and options.
3.1. Eligibility criteria
Searches were not limited by country and 1978 was chosen as a cut-off point based on a frequency analysis on a subsample of relevant literature.
We included quantitative studies (RCTs, quasi-RCTs, non-randomised controlled trials, controlled before and after studies, prospective or retrospective cohort studies that include a control group, historically controlled trials, nested case-control studies, case-control studies, and before-and-after comparisons). No restriction was placed on the setting or country, who delivered an intervention or in what format, and the participant characteristics.
We included studies evaluating or comparing interventions that included the promotion of PA (either as a sole focus or a substantial part of a multi-component intervention) either explicitly or implicitly targeting alcohol and other drug use. The comparator could be no intervention, treatment as usual (e.g. pharmacotherapy and psychological therapies), or alternative PA interventions (e.g. running vs walking).
For prevention studies we looked at rates of progression from non-use to use (initiation) and prevalence rates of alcohol or other drugs. For reduction we included reductions in level of use measured and reported in various ways (e.g. drinks per day, percent days abstinent). For treatment outcomes we included reduction outcomes as well as abstinence and relapse rates.
Table 1 summarises population, intervention, comparator, and outcomes against our three domains of PA impact.
Table 1.
Population, Intervention, Control, and Outcomes (PICO) by review domain.
| (1) Prevention | (2) Reduction | (3) Treatment (and relapse prevention) | |
|---|---|---|---|
| Population | Adolescents, at risk groups | General population who use alcohol and other drugs but not receiving acute or long term care for a diagnosed SUD, at risk groups | Those receiving/have received acute or long term care for a diagnosed SUD |
| Intervention | Sport and PA based programmes (schools, community, public health interventions) | Public health level initiatives, targeted community and healthcare based interventions | Adjunct PA interventions, prescribed and supported PA interventions, motivational interventions |
| Control | Other non-PA control, usual care or no intervention | Other non-PA control, usual care or no intervention | Standalone usual care, non-PA control, |
| Outcomea | Levels of subsequent use of alcohol and other drugs, prevalence rates | % reduction in alcohol and other drug use, prevalence | Abstinence rates, % days abstinent, % reduction in alcohol and other drug use, relapse rates |
Outcomes listed are indicative and not exhaustive.
3.2. Information sources
A highly sensitive search strategy of published and grey literature was developed using background scoping searches, previously identified relevant research, and in consultation with subject experts and public and patient involvement. The strategy included searches of the following sources:
3.2.1. Database searching
-
•
MEDLINE (Ovid)
-
•
MEDLINE (PubMed)
-
•
Embase (Ovid)
-
•
PsycINFO (Ovid)
-
•
Cochrane Library (Wiley) (including Cochrane Database of Systematic Reviews; Cochrane Central Register of Controlled Trials; Database of Abstracts of Reviews of Effects; Health Technology Assessment Database; and, NHS Economic Evaluation Database)
-
•
International Bibliography of the Social Sciences (ProQuest)
-
•
Web of Science Core Collection
-
•
CINAHL (EBSCO)
-
•
AMED (EBSCO)
-
•
Social Policy and Practice (Ovid)
-
•
Applied Social Sciences Index and Abstracts (ProQuest)
-
•
SocINDEX (EBSCO)
-
•
Social Policy and Practice (EBSC)
3.2.2. Supplementary searching
-
•
Google Scholar
-
•
Google
-
•
Open Grey
-
•
ProQuest Dissertations & Theses
-
•
British Library EThOS
-
•
Scottish Addiction Studies online library
-
•
HRB National Drugs Library
-
•
NIDA International Drug Abuse Research Abstract Database
-
•
Tufts CEA Registry
-
•
Database of promoting health effectiveness reviews (DoPHER)
-
•
NHS Evidence (NICE)
-
•
Big Lottery Fund Database
3.3. Search
The search strategy was intentionally kept broad to encompass the three aims of the review (i.e. prevention, reduction, and treatment). The strategy included searches of the above databases from Jan 1, 1975 to June 2, 2017 and was peer reviewed using the PRESS checklist (McGowan et al., 2016) prior to execution. No additional search filters or limiters were used. The strategy was translated for use in each database. An updated search was conducted on March 1, 2018. The updated search was refined based on included studies from the original search in line with best practices (Garner et al., 2016). A supplementary search was completed immediately prior to publication to identify any significant subsequent studies published after the updated search.
See Appendix 1 for a sample search strategy.
3.3.1. Grey literature search
Extensive grey literature searching was conducted to ensure maximum coverage of the subject area. The grey literature strategy encompassed focused searches in Google, Google Scholar, and several specialized databases. We also conducted backwards and forwards citation chaining of all included studies, and directly contacted known experts in the field and the lead authors of key publications for knowledge of any other relevant work. Any paper which described a relevant intervention and reported outcome data was considered for inclusion, including white papers, conference proceedings, or PhD theses. Masters theses were excluded.
See Appendix 2 for sample grey literature search strategy.
3.4. Data management
Exported citations from traditional databases were imported and de-duplicated in EndNote X8 (Clarivate Analytics). Grey literature citations were manually imported into EndNote or, where available, captured through a browser-based citation management plug-in (such as Zotero [https://www.zotero.org/]) then imported into EndNote. Using a structured and piloted data extraction form, we extracted relevant outcome data, study characteristics, and participant characteristics from each included paper. Data were extracted by one reviewer and checked by another (JH and TT).
3.5. Selection process
Two phases of study selection took place. Titles and abstracts were screened by two reviewers (TT/JH) independently and disagreements resolved by discussion or, where necessary, a third reviewer (AT). Title and abstract screening was conducted using Rayyan software (QCRI; Doha, Qatar; https://rayyan.qcri.org/)). Two initial subsets of 500 results were screened by two reviewers and inclusion and exclusion discrepancies discussed following each in order to ensure good agreement between reviewers. Following this, a set of 1000 were completed and discussed before the remaining results screened independently by 2 reviewers. This helped ensure reliable and consistent screening. Full texts were obtained for studies appearing to meet the criteria above and screened by two reviewers (each paper reviewed by one member of the team and checked by another (JH/TT).
3.6. Appraisal of studies (quality and bias)
Studies were assessed for bias based on the primary outcome of interest within the aims of this review. Randomised controlled trials were assessed for quality and risk of bias using the Cochrane Risk of Bias Tool 2.0 (Higgins et al., 2016) which has been developed for assessing more appropriately behavioural interventions. Non-randomised studies assessed using the ROBINS-I (Sterne et al., 2016). The GRADE approach (Guyatt et al., 2008) was used to create indicate the overall quality of the evidence for each domain of prevention, reduction, and treatment.
3.7. Data synthesis
Where data allowed (e.g. data on the same outcome from at least two studies of similar design, intervention, and population), we conducted meta-analyses to estimate the overall effect and consistency of the intervention effect across studies. As the population and setting of studies were different, a random effects model was used to obtain the summary result as an estimate of the average intervention effect, rather than the common effect estimated from a fixed effects model (Borenstein, Hedges, Higgins, & Rothstein, 2010).
Data from non-randomised trials which used different study designs, or data from randomised trials and non-randomised trials, were not combined in meta-analyses (Higgins & Green, 2011). In these cases, where suitable numerical data were not available for pooling, or if pooling was considered inappropriate, we used other approaches to provide a systematic summary of the studies, including: tabulation, transformation of data into common rubric (e.g. days abstinent), groupings and clusters (e.g. different population to assess influence of country, age, socioeconomic status, type/intensity of intervention, setting), and textual descriptions including a detailed narrative synthesis (Popay et al., 2006).
We present dichotomous data as risk ratios with their associated 95% confidence intervals (CI).
For continuous data, we calculate the mean differences (MD) for outcomes measured by the same scale, or the standardised mean differences (SMD) for outcomes measured by different scales, and present both with a 95% CI.
If outcomes were collected at multiple time points, we attempt to present a summary effect over all time points.
Methods relating to issues of unit of analysis, dealing with missing data, assessing statistical heterogeneity, assessing reporting bias, sensitivity analysis, confidence in cumulative evidence, and external validity/generalisability are reported in the protocol (Thompson, Taylor, et al., 2018).
4. Results
4.1. Identification of studies (quantitative and qualitative)
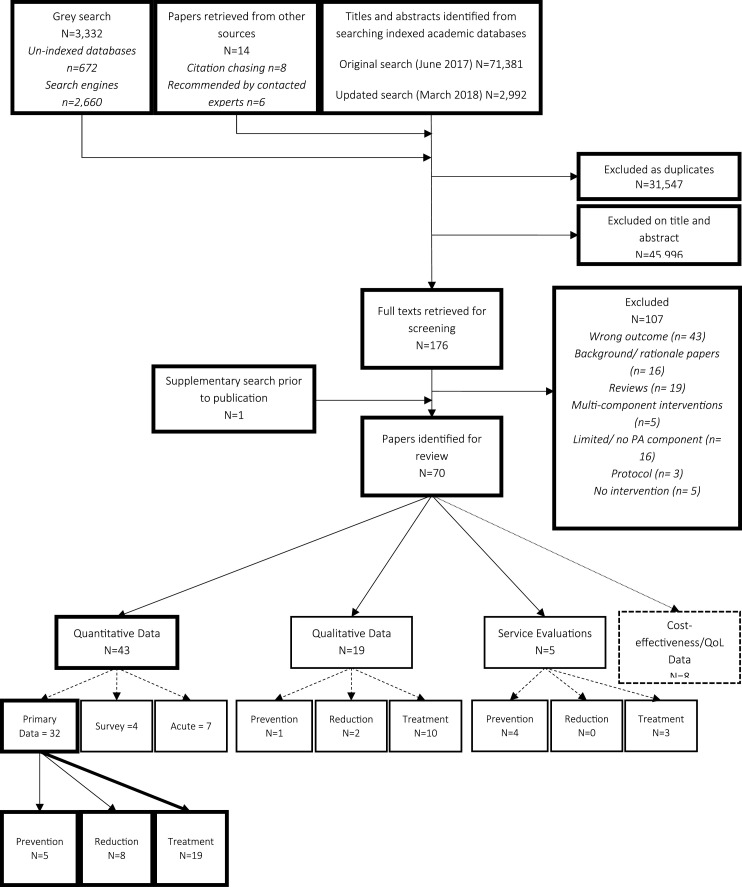
Database searches (June 2017 and March 2018) resulted in 42,826 results after de-duplication. Grey literatures searching returned 672 results from un-indexed databases and 2660 results were screened from search engines. Other sources (citation chasing and contacting experts) returned 14 results. Following title and abstract screening (and readings of grey literature without abstracts) by two reviewers (TT and JH) 45,996 results were excluded resulting in 176 full texts which were retrieved for further consideration. Following full text screening against the predefined inclusion criteria by two reviewers (TT and JH) with disputes resolved with the help of a third reviewer (AHT), 69 texts were included for review (See Fig. 1 for a flow diagram of identification of studies). One other paper was included following an additional search immediately prior to submission, bringing the total number of studies to 70.
4.2. Studies included in quantitative synthesis
Of the 70 identified texts, 32 are considered within this paper as containing quantitative data relating to the primary outcome of alcohol and other drug use in relation to the three domains of PA (see Fig. 2 ).
Fig. 2.
Identification of studies flow diagram.
Of the 32 studies considered within this paper, 11 studies present data on both alcohol and drug use (with the outcomes often being inseparable and measured via a single tool), 14 focus on just alcohol use, and seven focus on just other drug use. Table 2 presents a breakdown of the number of studies by domain and number of randomised controlled trials.
Table 2.
Included studies by domain and study design.
| Focus of studies |
Study designs |
|||||
|---|---|---|---|---|---|---|
| Domain | Total Studies (N) | Alcohol (n) | Other Drugs (n) | Both (n) | RCTs (n) | Other designs (n) |
| Prevention | 5 | 2 | 0 | 3 | 2 | 3 |
| Reduction | 8 | 5 | 0 | 3 | 3 | 5 |
| Treatment | 19 | 7 | 7 | 5 | 10 | 9 |
4.3. Prevention
Five studies were identified which were considered to meet the criteria for prevention (Butzer, LoRusso, Shin, & Khalsa, 2017; Collingwood, Reynolds, Kohl, Smith, & Sloan, 1991; Collingwood, Sunderlin, Reynolds, & Kohl 3rd, 2000; Velicer et al., 2013; Werch et al., 2003), three of which addressed both alcohol and other drug use (Butzer et al., 2017; Collingwood et al., 1991, 2000), and two focussed solely on alcohol (Velicer et al., 2013; Werch et al., 2003). The number of participants in each study ranged from 74 to 4158.
Characteristics of included studies are given in Table 3 .
Table 3.
Details of prevention studies.
| Study | Design | Focus | Population | Physical Activity Intervention | Comparison(s)/Control(s) | Outcomes and follow ups | Results | PA Data (including adherence) | Additional findings |
|---|---|---|---|---|---|---|---|---|---|
| Butzer et al. (2017) | RCT (preliminary) | Alcohol and other drugs | Seventh grade, middle school adolescents (N = 211). | Kripala Yoga (35 min, 1–2 sessions/week over 6 months); n = 117 | Physical Education (including group sports); n = 94 | (Youth Risk Behaviour Survey) | No differences | None | Yoga participants reported liking physical education significantly more than yoga. |
| USA | Age (years); mean (SD): 12.64 (0.33) Male (36.8%) | Have you ever had a drink of alcohol, other than a few sips? | |||||||
| Have you ever used [various substances]? | |||||||||
| Post intervention; 6 months; 1 year | |||||||||
| Collingwood et al. (1991) | Pre-Post | Alcohol and other drugs | Adolescents (N = 74) in either (1) a school based “at risk” prevention programme (n = 54), (2) a community counselling agency substance abuse programme (n = 11), or (3) a chemical dependency in-patient hospital-based programme (n = 9). | Physical fitness programme (1.5 h, 1–2/week over 9 weeks + assignment for two individual exercise sessions/week); 3 modules delivered to parent groups in one session (behaviour contracting, family fitness activities, and personal walking programme); a computerised fitness assessment system with built in reinforcement for participants. | N/A | Modified questions from the “Pride Questionnaire”. | Non-significant trend for decreases in alcohol and marijuana use. | Significant improvement in total sample in fitness tests (1 mile run, 1 min sit up, 1 min pushup, percent fat, and flexibility). | Fitness improvers demonstrated a trend for greater improvements in all areas, including self-reported substance use patterns. |
| USA | Age (years); mean: 16.8; (1) 17.5; (2) 15.1; (3) 15.1 | Post intervention | Significant decrease in % of multiple users. | ||||||
| Male (62.2%) | |||||||||
| Collingwood (2000) | Pre-Post | Alcohol and other drugs | Youth (N = 329 with complete data from a total of 3701) One senior high school (n = 34), two junior high schools (n = 77), three National Guard community sites (n = 218). | “First Choice” physical fitness programme based on the staff training and dissemination model. Consists of three components: (1) adolescent fitness skills and exercise training programme (3/week over 9–12 weeks); (2) parent training module; and (3) peer fitness leader's training programme. | N/A | Monthly usage questions from the American Drug and Alcohol Survey for 15 different substances. | No significant changes, other than a reduction in % reporting using alcohol at one community site | Consistent trend of increased physical activity levels and fitness. | |
| USA | (years); mean age range across sites: 10.9–15.5 | Post intervention | |||||||
| Male % range across sites: 47.5–60.8 | |||||||||
| Velicer et al. (2013) | Cluster Randomised Trial | Alcohol | Sixth grade students (N = 4158). | Energy Balance intervention: A fully tailored 30-min computerised PA intervention, plus moderately or minimally tailored intervention for television watching habits and fruit and vegetable consumption (once in sixth grade, three times in seventh grade, and once in eight grade). (Transtheoretical Model) | Substance use Prevention: A tailored 30-min computerised intervention aimed to reduce tobacco and alcohol use (once in sixth grade, three times in seventh grade, and once in eight grade). | Stage of change for alcohol and substance acquisition and cessation. | The energy balance arm had lower rates of alcohol acquisition at 12, 24, and 36 months compared to the substance use prevention arm. Too few reported using alcohol at baseline to measure cessation. | Energy balance group reported greater number of days doing at least 60 min of PA at 24 and 36 months than the substance use prevention group. | |
| USA | Age; mean (SD): 11.40 (0.69) | (Transtheoretical Model) | 12, 24, and 36 months | ||||||
| Male (52.2%) | |||||||||
| Werch et al. (2003) | Randomised Trial (3 arm) | Alcohol | Eighth grade school students (N = 454); attending an inner city middle school (n = 183), a suburban middle school (n = 110), or a rural junior high school (n = 161). | Sport Consultation: consisting of a health and fitness screen followed by a consultation protocol promoting an active lifestyle and emphasising the conflict of an active lifestyle and consuming alcohol. One off, mean length; minutes, mean (SD): 8.92 (2.53). | Sport Consultation plus Alcohol Preventive Consultation: Sport Consultation followed by an alcohol preventive consultation addressing risk/protective factors including influenceability, social norms; negative/positive outcome expectancies, and self-efficacy and behavioural capability. One off; mean length; minutes, mean (SD): 25.87 (5.59). | The Youth Alcohol and Health Survey (30-day frequency and quantity of alcohol, heavy alcohol use). | Decreases in alcohol consumption, alcohol initiation, and alcohol related problems regardless of group. | All groups increased self-reported moderate and vigorous PA. | |
| USA | Age; mean (SD) 13.2 (0.5) | Sport Consultation plus Alcohol Preventive Consultation plus Parent Print Materials: Sport Consultation plus Alcohol Preventive Consultation plus five parental mailed SPORT cards mailed once per week containing ‘check off’ health and fitness facts | 3 month post intervention | ||||||
| Male (37.9%) |
4.3.1. Populations
All included studies took place in the USA and were conducted among adolescents. All participants were of middle or high school age (average age range 10.9–17.5 years), and interventions were set within schools or in community settings such as community counselling agencies or National Guard community sites.
4.3.2. Interventions
Interventions varied greatly in terms of type, intensity, mode of delivery and duration. Some interventions contained no direct PA: One intervention (Werch et al., 2003) as part of a three arm experimental design consisted of a one of consultation promoting an active lifestyle emphasising the conflict between being active and consuming alcohol. This was added to by further consultation addressing risk/protective factors for alcohol use, and mailed cards sent once a week for five weeks to the parents of the adolescents as the comparator conditions. Another intervention (Velicer et al., 2013) was a 30-min tailored computer based intervention accessed 5 times over a three year period aimed at increasing PA levels (as well as a partially tailored element for increasing fruit and vegetable consumption and decreasing time spent watching television). Two studies focussed on more vigorous physical fitness (Collingwood et al., 1991, 2000) consisting of exercise training for one and a half hours three times a week for 9–12 weeks, and one study (Butzer et al., 2017) examined the impact of 35 min Kripala Yoga sessions delivered once or twice a week over six months.
4.3.3. Controls/comparators
Two studies were of pre-post within subjects design therefore had no control or comparison condition (Collingwood et al., 1991, 2000). The remaining three studies all utilised a randomised design: one comparing yoga to physical education as usual (Butzer et al., 2017), another a cluster (school) design comparing a computer based tailored substance use prevention (with no PA component) equal in contact time (Velicer et al., 2013), and the other a three arm individually randomised design comparing three versions of the same one off short counselling type intervention for increasing PA (Werch et al., 2003). None of the studies incorporated what could be considered a true control condition as they all either included experimental interventions as the comparator or an alternative PA intervention. It is not clear if one study actually decreased the level of PA completed by using yoga as an intervention in place of standard physical education (Butzer et al., 2017).
4.3.4. Outcomes
The main outcome of interest was subsequent levels of alcohol and other drug use representing a transition from not using to using (initiation). We also included studies which reported levels of use across time to show a reduction in use.
4.3.4.1. Initiation
The three studies of random design reported measures relating to alcohol use initiation (Butzer et al., 2017; Velicer et al., 2013; Werch et al., 2003). One study collected data at the end of the intervention period (Velicer et al., 2013), one at three months post intervention (Werch et al., 2003), and the other at one year post intervention (Butzer et al., 2017). All three used a different inventory for collecting the status of participants. One study reported significantly lower levels of alcohol use initiation at 12, 24 and 36 months in the “energy balance” intervention aimed at increasing PA compared to a comparison intervention aimed explicitly at reducing other drug use (Velicer et al., 2013), with 10.1% of the energy balance group having initiated alcohol use compared to 14.4% in the other drug use prevention intervention. A study with three experimental arms reported a reduction in 30-day heavy drinking (F(1,441) = 4.05, p = 0.04) and alcohol initiation (F(1,441) = 4.27, p = 0.03) at 3 months post intervention across all groups with no effect of group (Werch et al., 2003). One preliminary randomised study investigating the effects of a yoga intervention reported no difference in the proportion of participants who reported having ever tried a sip of alcohol in either arm at any time point (Butzer et al., 2017).
4.3.4.2. Reduction
One study reported a reduction in 30-day heavy drinking (F(1,441) = 4.05, p = 0.04) across all three experimental arms of the study with no difference between groups (Werch et al., 2003). Two non-randomised studies examining physical fitness interventions with pre-post measures showed non-significant trends for reduction in alcohol and other drug use levels (Collingwood et al., 1991, 2000).
4.3.4.3. Secondary outcomes
The reporting of data relating to PA levels and adherence was poor. Generally, all studies reported increases in reported levels of PA as a result of different modalities of intervention. Adherence is unknown due to lack of reporting. One study observed greater reductions in self-reported substance use patterns amongst those who demonstrated quantifiable improvements in physical fitness (Collingwood et al., 1991) compared to those who showed no improvement.
No serious adverse events related to PA were reported in any of the studies.
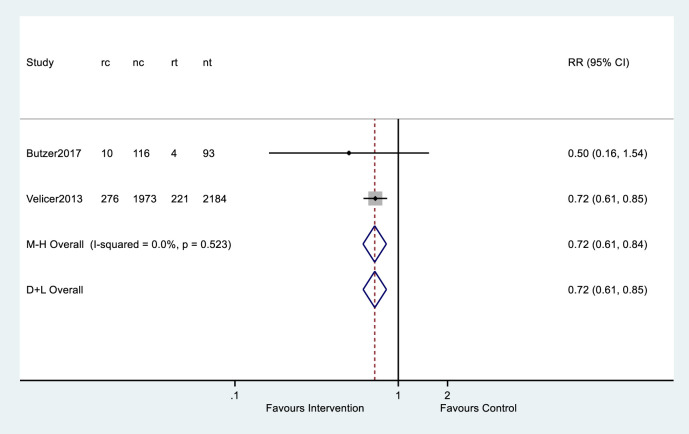
4.3.5. Meta-analyses
Of the five studies considered for prevention, only two studies had an outcome which could be combined for meta-analysis after conversion (Butzer et al., 2017; Velicer et al., 2013) and focussed on initiating alcohol use during or following intervention.
Of the two studies included, one (Butzer et al., 2017) reported the number of participants who had ever used alcohol at the end of the intervention, and the other (Velicer et al., 2013) reported percentage of people who had initiated alcohol use in each group at the end of intervention. Multiplying the percentage with the total number of participants, we obtain the number of participants who had initiated alcohol use at the end of intervention for each group.
The summary data from these two studies are combined in a meta-analysis. The overall risk ratio of alcohol use initiation is 0.72 (95% CI: 0.61 to 0.85), estimating from the random-effect meta-analysis, and 0.72 (95% CI: 0.61, 0.84), estimating from the fixed-effect meta-analysis (Fig. 3 ). There is evidence for the effect of the intervention on reducing the alcohol use initiation in middle school students. There is little between-study heterogeneity (I2 = 0.0%).
Fig. 3.
Alcohol Initiation at end of intervention.
4.3.6. Risk of bias and quality appraisal
Two studies of randomised design were judged at high risk of bias (Butzer et al., 2017; Velicer et al., 2013), with some concerns over the risk of bias for the other (Werch et al., 2003). Two studies of non-random design (Collingwood et al., 1991, 2000) were judged to have a severe risk of bias. (See Supplementary file 1).
4.3.7. Quality of the evidence
Using the GRADE approach for assessing the quality of evidence (Guyatt et al., 2008), the evidence for PA and the prevention of alcohol and other drug use was consistently downgraded due to study limitations, inconsistency of results, indirectness of evidence and imprecision. Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect (Table 4 ). Further research is likely to have an important impact and change our findings.
Table 4.
Summary of findings table -prevention.
| Physical activity and the prevention of alcohol and other drug use | ||||||
|---|---|---|---|---|---|---|
| Population: Adolescents | ||||||
| Settings: educational setting, community | ||||||
| Intervention: physical activity | ||||||
| Comparison: alternative non-physical activity intervention, usual care | ||||||
| Outcome | Illustrative comparative risk | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comment | |
| Assumed risk usual care | Corresponding risk physical activity intervention | |||||
| Alcohol use initiation | A 28% lower rate of alcohol use initiation compared to comparator | RR 0.72 (0.61, 0.85) | 5226 (5) | ⊕⊕◯◯ lowa | A reduction represents fewer participants reporting having initiated alcohol use at follow up | |
High and severe risk of bias found in most studies related to confounding, missing data, and outcome measurement.
4.4. Reduction
Eight studies were identified that were considered to meet the criteria for reduction where participants were not seeking treatment for, nor diagnosed with, a substance use disorder (including alcohol) (Correia, Benson, & Carey, 2005; Georgakouli et al., 2017; Murphy, Pagano, & Marlatt, 1986; Oaten & Cheng, 2006; Reddy, Dick, Gerber, & Mitchell, 2014; Scott & Myers, 1988; Weinstock, Capizzi, Weber, Pescatello, & Petry, 2014; Weinstock, Petry, Pescatello, & Henderson, 2016). Three focussed on both alcohol and other drug use (Correia et al., 2005; Reddy et al., 2014; Scott & Myers, 1988), and five focussed solely on alcohol use (Georgakouli et al., 2017; Murphy et al., 1986; Oaten & Cheng, 2006; Weinstock et al., 2014, 2016). No study focussed solely on PA for the reduction of other drug use. The number of participants in each study ranged from n = 11 to n = 133.
For details of included studies, see Table 5 .
Table 5.
Details of reduction studies.
| Study | Design | Focus | Population | Physical Activity Intervention | Comparison(s)/Control(s) | Outcomes and follow ups | Results | PA Data (including adherence) | Additional findings |
|---|---|---|---|---|---|---|---|---|---|
| Murphy et al. (1986) | RCT (3 arm) | Alcohol | Social drinkers recruited from undergraduate classes (N = 60). | Running group. Met as a group 3/week for 70 min and asked to run ‘some other time per week’ on their own for 8 weeks. | Meditation group. Instructed to meditate for 20 min twice a day. Met as a group 3/week for a group meditation session. | Daily journal recording alcohol intake. | Running condition reduced consumption by 60% at longest follow up from baseline, significantly lower than control, and a non-significant reduction compared to meditation. | Those in the running group showed significantly increased VO2 max levels post intervention compared to baseline. | 60 recruited, only 31 analysed |
| USA | Age range: 21–30 years | No treatment control. Asked to keep journals of their behaviour. | Weeks 1–2 (pre-intervention) mean, weeks 3–6 mean, and weeks 7–10 mean | ||||||
| Male (100%) | All subjects in the running group completed the 8 week intervention, running on average 3.4 times per week. | Those who ran less than 3.5 times per week reduced alcohol intake and increased VO2 max measure by the same amount as those who ran more than 3.5 times per week. | |||||||
| Correia et al. (2005) | RCT (3arm) | Alcohol and other drugs | Undergraduates at a large private university (N = 133, n = 105 randomised). | Activity Increase (AI): Oral and written instructions to increase days engaged in physical activity and creative/artistic activity by 50% in next 28 days, including signing a contract with behavioural targets and asked to self-monitor behaviour | Substance use Reduction (SR): Oral and written instructions to reduce frequency of consumption during next 28 days including signing a contract with behavioural targets and asked to self-monitor behaviour. | Daily Drinking Questionnaire indicating frequency and quantity of alcohol in previous 28 days. | Both SR and AI significantly reduced number of substance use days (includes alcohol); and number of total standard drinks from baseline to follow up. AI did not significantly differ from control. | AI group reported significantly more exercise days at follow up compared to SR and control group. SR reported significant decrease in PA days, AI reported significant increase in PA days | |
| USA | Age, mean (SD) 19.76 (3.76) | No change control. | 28 days | ||||||
| Male (31%) | |||||||||
| Georgakouli et al. (2017)) | Pre-Post | Alcohol | Heavy drinking male volunteers (N = 11). | 8-week supervised exercise intervention of moderate intensity (50–60% of Heart Rate Reserve). No more details. | Alcohol use questionnaire (not specified). How many alcohol units do you drink per day? How many AU did you drink last night? How many times did you consume alcohol over the last month? How many AU did you drink per occasion over the last month? How many days do you usually drink alcohol? How many AU do you usually drink per week? Time until first drink after an exercise session. | Significant decreases in alcohol use across all questions other than desire to stop or reduce drinking and amount drank last night. | Significant decreases found for weight and waist circumference and increases in flexibility and situps. Self-reported met minutes per week (IPAQ) significantly increased form baseline to follow up. | No change in desire to drink, but changes in amount drunk. | |
| Greece | Age, mean(SD): 30.3 (3.5) | Mid and post intervention | |||||||
| Male (100%) | |||||||||
| Oaten and Cheng (2006) | Pre-Post (within and between) | Alcohol | Sedentary undergraduates (N = 24); cohort 1 (n = 9), cohort 2 (n = 6), cohort 3 (n = 9). | Exercise programme: 3–4 times per week over 8 weeks of cardio vascular exercise, tailored to suit the individual by gym staff, including aerobic classes, free-weights, and resistance training. **All participants were subjected to a thought suppression task not reported as part of the intervention | Waiting list control phase (no exercise) | 7-day recall procedure with quantity the measure of interest (standard units of alcohol). | Average decrease of 5 drinks per week during exercise phase compared to waiting list control phase | No data in relation to adherence rates, other than 100% retention, and that participants attended the gymnasium, and attendance increased over time. | Improvements in a wide range of regulatory behaviours observed. |
| Australia | Age, mean (SD); 24 (6) | Baseline, 1 month, and 2 months | |||||||
| Male (25%) | |||||||||
| Reddy et al. (2014) | Pilot RCT | Alcohol and other drugs | Females aged 18–65 with at least sub-threshold PTSD (N = 38). | 12 Kripalu-based Hatha yoga session of 75 min incorporating trauma-sensitive yoga. The intervention also incorporated elements of “mindfulness ad dialectical behavioural therapy, a specialized form of cognitive behavioural therapy”. (n = 20) | An assessment control (n = 18). | AUDIT and DUDIT. | AUDIT and DUDIT scores improved in the yoga group and worsened in the control group over time. Changes were not significantly different between groups over time. | 69% of yoga group reported noticing PTSD symptoms less at follow up, compared to 80% of the control group reporting no difference or an increase in symptom perception. | |
| USA | Age, mean (SD); 44.4 (12.4) | Baseline, end of intervention, and 1 month after intervention | |||||||
| Female (100%) | |||||||||
| Scott and Myers (1988) | Non-RCT | Alcohol and other drugs | Native adolescents belonging to the River Desert Community of the Algonquin nation attending regular school gym classes (N = 74). | Treatment was administered during first 30 min of normally scheduled gym classes (every other day on a 4-day cycle for 70 min). Physical fitness training designed to enhance aerobic capacity, flexibility, and strength was delivered for 24 weeks, with students encouraged to set personal fitness goals. (n = 30) | Regular physical education classes emphasising sports-specific skills (n = 44). | The Native American Drug Use Survey. | Within and between subject tests showed no difference in experience with alcohol and drugs, recent (past 2 months) or long term (past 12 months) substance use. Alcohol and drug use in past 12 months showed greater increase in comparison group but was not significantly different. | Treatment groups showed significant greater improvement in cardiovascular fitness than the comparison group | Consistent pattern of increased use across grades, and from pre-test to post-test suggesting age and aging may influence use. |
| Canada | Age, mean (range); 14.6 (12–18) | Baseline, end of intervention | |||||||
| Male (47.2%) | |||||||||
| Weinstock et al. (2014)) | Pilot randomised trial | Alcohol | Sedentary hazardous drinking college students (N = 31). | MET: 50-min one off session framed as a “wellness intervention” for increasing exercise, providing personalised feedback on exercise habits in comparison to population norms and exercise guidelines. Along with developing a change plan to start exercising. Alcohol was not discussed. | MET + CM: MET intervention plus 8 weeks of contingency management. Weekly meeting with interventionist provided reinforcement for verified completion of activities in previous week and develop a new contract for the upcoming week. Verified completion of activities was rewarded with randomly drawn prizes averaging $230 if they completed all activities. Activities included walking with a pedometer, jogging on a treadmill for 15 min, or attending an exercise class at the gym; all activities were explicitly defined in terms of duration and length. | TLFB for previous 60 days to assess alcohol use. | No significant effects were found on alcohol outcomes relating to time or condition. | Both groups increased PA, MET + CM exercised significantly more often. | MET + CM drinking significantly more days than MET at baseline. |
| USA | Age, mean years (SD); MET: 20.1 (1.2); MET + CM: 21.0(2.3) Male; MET (26.7%); MET + CM (43.8%) | Baseline, end of intervention | MET + CM attended an average of 6.94 (SD = 2.24) sessions out of a possible 8, completing 17.9 (SD = 8.8) verified completed activities. | ||||||
| Both groups reported significant increases in exercise frequency, estimated weekly calorie expenditure, and VO2 max with no differences between groups. | |||||||||
| Weinstock et al. (2016) | Randomised trial | Alcohol | Sedentary heavy drinking college students (N = 70). | MI + EC (Motivational Interviewing + Exercise contracting): Two 50-min motivational interviewing sessions (one following baseline and 4 weeks later), plus eight weekly individually delivered exercise contracting sessions. Alcohol was not discussed unless raised by participant. Participants were reinforced ($5 gift certificate) for each EC session they attended. | MI + CM (Motivational Interviewing + Contingency management): Two 50-min motivational interviewing sessions (one following baseline and 4 weeks later), plus eight weekly individually delivered exercise contracting sessions. Alcohol was not discussed unless raised by participant. Participants were reinforced (draw from a prize bowl) for completing verified exercise activities as agreed in the EC sessions. | TLFB previous 60 days. | Significant reduction in total weekly standard drinks and weekly binge drinking episodes at 2 and 6 months compared to baseline with no differences between arms. | 89% of participants attended all eight exercise contracting sessions. An average of 30.4 activities were selected, of which 17.9 activities were verified completed. No change in cardiorespiratory fitness was observed. | Changes in exercise were not predictive of changes in drinking. |
| USA | Age, mean years (SD); MI + EC: 19.9 (1.3); MI + CM 20.1(1.6)Male; MI + EC (37.1); MI + CM (51.4%) | Baseline, 2 months (end of intervention), and 6 months post baseline | Both arms significantly increased exercise frequency during intervention period, which decreased at 6 months but still higher than baseline. MI + CM showed greater increases in exercise frequency than MI + EC. |
4.4.1. Populations
Five of the studies (four in the USA and one in Australia) recruited undergraduate university students (Correia et al., 2005; Murphy et al., 1986; Oaten & Cheng, 2006; Weinstock et al., 2014, 2016), one study conducted in Greece recruited heavy drinking male volunteers (Georgakouli et al., 2017), another study in the USA recruited females with at least sub-threshold post-traumatic stress disorder (Reddy et al., 2014), and another recruited “native” adolescents in Canada (Scott & Myers, 1988).
4.4.2. Interventions
Interventions varied in intensity and duration from a one off provision of oral and written instruction to increase and self-monitor PA in the next 28 days (Correia et al., 2005) to 8 weeks of three times weekly running session of 70 min with instructions to run “some other time of the week” on their own (Murphy et al., 1986). One study of within subject pre-post design reported no more information than an eight week supervised exercise intervention of moderate intensity at 50–60% of heart rate reserve (Georgakouli et al., 2017). Another intervention involving sedentary undergraduate students included three to four times per week over eight weeks of gym based exercise tailored to the individual (Oaten & Cheng, 2006) and also incorporated a “thought suppression” task. Two interventions recruiting alcohol drinking college students in the USA utilised a counselling-based intervention; one compared motivational enhancement therapy (MET) with MET plus contingency management (Weinstock et al., 2014); the other (Weinstock et al., 2016) consisted of an intervention including two motivational interviewing (MI) sessions with eight weekly exercise contracting sessions. The study compared the impact of contingency management, in one group reinforcing the completion of physical activities and in the other reinforcement was offered for attending the exercise contracting sessions. One study recruited women with at least sub-threshold PTSD and offered twelve 75-min sessions of trauma-sensitive hatha yoga incorporating elements of mindfulness and dialectical behavioural therapy.
4.4.3. Controls/comparators
Only three studies had what could be considered a true control condition. One three arm randomised trial (Murphy et al., 1986) compared running to either meditation or a no treatment control asked to keep journals of their behaviour. Another 3 arm randomised trial(Correia et al., 2005) compared oral and written advice to exercise with oral and written advice to reduce frequency of substance consumption and with a control group. Another two arm RCT compared hatha yoga with an assessment control group. One further study used a waiting list control phase (Oaten & Cheng, 2006).The remaining studies consisted of two experimental arms (Weinstock et al., 2014, 2016).
4.4.4. Outcomes
Two studies reported data collected using the timeline follow back method (Weinstock et al., 2014, 2016). Other studies report data collected using a variety of questionnaires designed to capture alcohol consumption on a daily or weekly basis, although one study collected data using the Alcohol Use Disorders Identification Test (AUDIT) and the Drug Use Disorder Identification Test (DUDIT) (Reddy et al., 2014). The majority of follow up data was collected at the end of the intervention period with the longest follow up at six months post baseline (Weinstock et al., 2016).
Of the randomised studies with a control group, one study of three times weekly running demonstrated a significant reduction in alcohol consumption of 60% at longest follow up compared to control, and a non-significant reduction compared to the meditation arm (Murphy et al., 1986). Providing written and oral information on increasing PA compared to information on other drug use reduction significantly reduced the number of drug use days (includes alcohol and other drugs) from baseline to follow up (Correia et al., 2005) by approximately 2 days in activity group for the previous 28 days. An intervention comparing yoga to a control group (Reddy et al., 2014) saw improvements in both AUDIT and DUDIT scores one month post intervention, and although the scores worsened for the control group, the differences were not statistically significant. One study using a wait list control design with 3 cohorts saw a reduction of 5 standard drinks per week during the intervention phase compared to the control phase. One small within subjects study (n = 11) reported a significant reduction in all variables at the end of the intervention relating to alcohol consumption, most notably a reduction of alcohol consumption from 19.00 (SD = 3.20) alcohol units at baseline to 11.64 (SD = 3.03) at follow up (Georgakouli et al., 2017). However, this study reported no change in variables related to desire to reduce or stop drinking. One study examining MET compared to MET plus contingency management found no differences on alcohol use for either time or condition (Weinstock et al., 2014) despite increases in self-reported levels of PA. However, this pilot study had a limited sample size (n = 31) and a baseline imbalance (the MET plus contingency management had significantly more drinking days at baseline than the MET alone group. The other study comparing two experimental conditions involving PA (Weinstock et al., 2016) showed that reinforcing either attendance at an exercise contracting session or for completing contracted exercise activities made no difference, as significant reductions in number of weekly drinks and weekly binge drinking episodes at all follow ups was seen in both arms, with no difference between groups. They also report that changes in PA levels were not predictive of the changes observed in alcohol drinking behaviour.
4.4.4.1. Secondary outcomes
Several studies (Georgakouli et al., 2017; Murphy et al., 1986; Scott & Myers, 1988; Weinstock et al., 2014) reported improvements in physical fitness measures as a result of intervention at follow up. Self-reported levels of PA were also shown to increase across a variety of interventions (Correia et al., 2005; Georgakouli et al., 2017; Weinstock et al., 2014). Adherence data relating to PA was sparse and rarely reported. One study reports 100% completion of the intervention, with participants averaging running 3.4 times per week (Murphy et al., 1986) over an eight week intervention, and another reports an average attendance of 6.94 sessions out of a possible eight exercise contracting sessions over eight weeks, where subsequently around 60% of planned activities were verified completed. No studies report mediating effects of PA on alcohol and substance use outcomes.
No serious adverse events related to PA were reported in any of the studies.
4.4.5. Meta-analyses
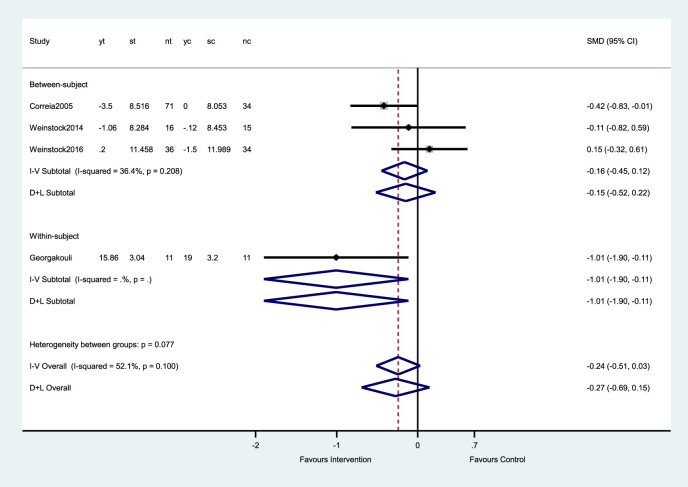
Only one analysis with four studies focussed on alcohol consumption was possible, presented as changes in total drinks per week at end of intervention.
Correia (2005) reported a three-arm randomised trial with two intervention groups and one control group. Both intervention groups involved PA, thus, we combined two intervention groups into one group using the methods described in the Cochrane handbook.
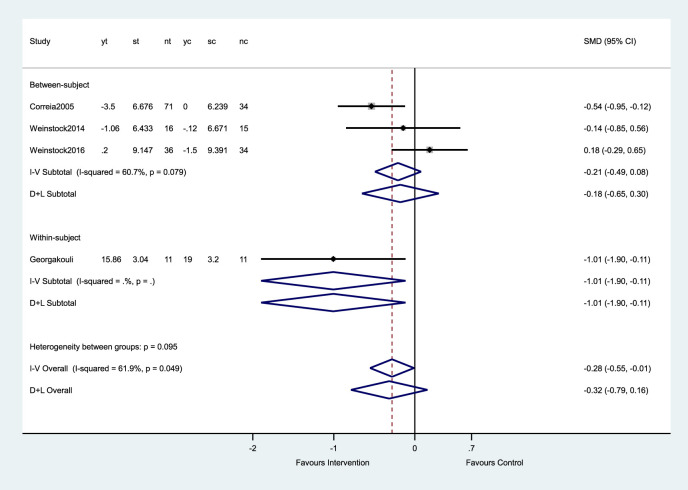
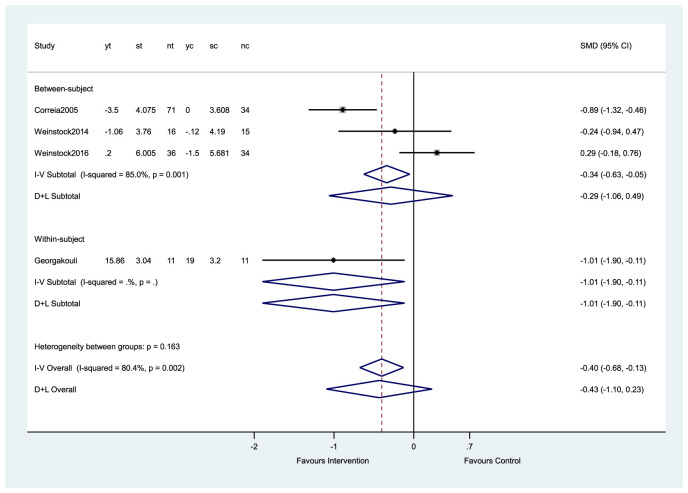
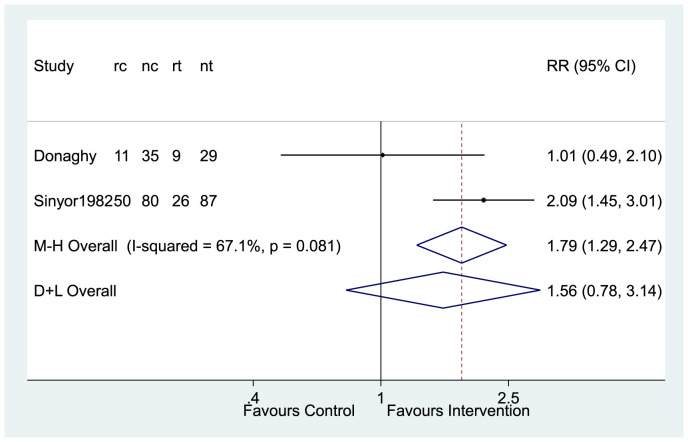
Three studies (Correia et al., 2005; Weinstock et al., 2014, 2016) reported mean units of drinks per week at baseline and the end of intervention. We calculated the change in mean units of drinks per week and its associated standard deviation for both intervention and control groups. The standard deviation was calculated by assuming 0.5 as the correlation coefficients between baseline measurements and final measurements (Fig. 4 ). We carried out a sensitivity analysis of assuming correlation coefficients to be 0.7 (Fig. 5 ) and 0.9 (Fig. 6 ).
Fig. 4.
Change in total drinks per week (assuming correlation coefficient of 0.5).
Fig. 5.
Sensitivity analysis. Change in total drinks per week (assuming correlation coefficient of 0.7).
Fig. 6.
Sensitivity analysis. Change in total drinks per week (assuming correlation coefficient of 0.9).
The overall standardised mean difference (SMD) in total drinks per week was −0.27 (95% CI: 0.69 to 0.15) from the random-effect meta-analysis and −0.24 (95%CI: 0.51 to 0.03) from the fixed-effect meta-analysis, suggesting insufficient evidence for the effect of exercise on reducing the total drinks per week.
A subgroup analysis of three randomised controlled trials (Correia et al., 2005; Weinstock et al., 2014, 2016) showed an overall SMD of −0.15 (95% CI: 0.52 to 0.22), indicating insufficient evidence for the effect of the intervention on reducing total drinks per week. There was one within-subject study (Georgakouli et al., 2017), where the SMD is −1.01 (95%CI: 1.90 to −0.11).
4.4.6. Risk of bias and quality appraisal
Of five randomised controlled trials, one study was judged at high risk of bias (Murphy et al., 1986) and four had some concerns over risk of bias (Correia et al., 2005; Reddy et al., 2014; Weinstock et al., 2014, 2016). Of three studies of non-randomised design, two were judged to be at severe risk of bias (Oaten & Cheng, 2006; Scott & Myers, 1988), and one at critical risk of bias (Georgakouli et al., 2017). (See supplementary file 1).
4.4.7. Quality of the evidence
Using the GRADE assessment of quality (Guyatt et al., 2008), the evidence for PA and reduction of alcohol and other drug use was consistently downgraded due to study limitations, inconsistency of results, indirectness of evidence and imprecision. We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. Further research is needed to draw any conclusions (Table 6 ).
Table 6.
Summary of findings table - reduction.
| Physical activity and the reduction of alcohol and other drug use | ||||||
|---|---|---|---|---|---|---|
| Population: Non-treatment seeking individuals using alcohol and/or other drugs, or individuals using alcohol and other drugs but not diagnosed with a use disorder | ||||||
| Settings: community | ||||||
| Intervention: physical activity | ||||||
| Comparison: alternative non-physical activity intervention, no intervention, usual care | ||||||
| Outcome | Illustrative comparative risk | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comment | |
| Assumed risk usual care | Corresponding risk physical activity intervention | |||||
| Reduction in alcohol and/or substance use levels | See comment | See comment | Standardised mean difference −0.27 (−0.69 to 0.15) | 413 (8) | ⊕◯◯◯ very lowa | Effect is uncertain |
High and severe risk of bias found in most studies related to confounding, classification of interventions, deviation form intended interventions, missing data, and outcome measurement.
4.5. Treatment
Nineteen studies identified were considered to meet the criteria for PA in the treatment of alcohol and other drug use (Abrantes et al., 2017; Brown et al., 2010, 2014; Buchowski et al., 2011; Burling, Seidner, Robbins-Sisco, Krinsky, & Hanser, 1992; Colledge et al., 2017; Cutter et al., 2014; De La Garza et al., 2016; Donaghy, 1997; Giesen, Zimmer, & Bloch, 2016; Hallgren, Romberg, Bakshi, & Andréasson, 2014; Linke et al., 2019; Mamen, Pallesen, & Martinsen, 2011; Rawson et al., 2015; Kirsten K; Roessler, Bilberg, et al., 2017; Shaffer, Lasalvia, & Stein, 1997; Sinyor, Brown, Rostant, & Seraganian, 1982; Weinstock, Barry, & Petry, 2008). Five report on both alcohol and other drug use (Burling et al., 1992; Colledge et al., 2017; Linke et al., 2019; Mamen et al., 2011; Weinstock et al., 2008), 7 on solely alcohol use (Abrantes et al., 2017; Brown et al., 2014; Donaghy, 1997; Giesen et al., 2016; Hallgren et al., 2014; Kirsten K; Roessler, Bilberg, et al., 2017; Sinyor et al., 1982), and 7 on solely other drug use (Brown et al., 2010; Buchowski et al., 2011; Cutter et al., 2014; De La Garza et al., 2016; Rawson et al., 2015; Shaffer et al., 1997; Trivedi et al., 2017). The number of participants in each study ranged from n = 12 (Buchowski et al., 2011) to n = 302 (Trivedi et al., 2017).
For details of included studies see Table 7 .
Table 7.
Details of treatment studies.
| Study | Focus | Design | Population | Physical Activity Intervention | Comparison(s)/Control(s) | Outcomes and follow up | Results | PA Data (including adherence) | Additional findings |
|---|---|---|---|---|---|---|---|---|---|
| Abrantes et al. (2017) USA | Alcohol | Pre-Post | Inactive women with depressive symptoms who were current patients in an alcohol and drug partial hospitalisation programme (N = 20). Age, mean (SD); 39.5 (10.6) | An hour-long consultation session with a PA counsellor who provided short and long-term benefits of increasing PA, utilising PA as a way to manage difficult emotions and alcohol cravings, discussed local opportunities for PA and ways to build it into daily life. They were then oriented with a Fitbit activity tracker, offered tips for monitoring step counts, duration and frequency of PA goals and an initial goal of 4500 steps per week (increasing 500 steps each week). Subsequent weekly/biweekly phone calls from PA counsellor to review progress, problem solve, encourage PA for managing cravings, and discuss maintaining increased PA. | N/A | TLFB (previous 90 days), alcohol use days, % days abstinent, drinks per drinking day | Significant reductions in alcohol use days, % days abstinent, but not for drinks per drinking day (changes remained significant under ITT to assumptions (baseline carried forward)). | Participants significantly increased self-reported minutes of all activity from baseline to follow up, but not MVPA. Average steps per day increased from 5290 at baseline to 9174 at follow up. | Measures of negative affect (PANAS) predicted session attendance. |
| Female (100%) | End of intervention (12 weeks) (n = 15) | No statistically significant differences were observed for cardiorespiratory or body composition measures from baseline to follow up. | |||||||
| Participants wore the FitBit for 73% of days and completed 4.7 of 6 scheduled phone PA counselling sessions | |||||||||
| Brown et al. (2014) USA | Alcohol | Preliminary RCT | Sedentary alcohol dependent adults (N = 49) | Group Aerobic Exercise (AE) (n = 26): Consisting of 1) moderate intensity aerobic exercise, 2) group behavioural treatment, and 3) an incentive system. Weekly exercise group sizes ranged from 2 to 5 and were led by an exercise physiologist who provide information on the benefits of PA. Sessions began at 20 min increasing to 40 min (treadmill, elliptical machine, or recumbent bicycle) by week 12, and were also “prescribed” to engage in moderate PA on 2–3 other occasions each week. Group behavioural treatment consisted of weekly (20 min) session based on cognitive and behavioural techniques for increasing motivation and maintaining PA. $5 was given for each session attended, and for returning a completed weekly PA monitoring form. | Brief advice to exercise (BA-E) (n = 23): 20-min discussion of the psychological and physical benefits of PA and provided a written summary of this information. Participants were reimbursed to monetary value similar to the AE group, but it was not contingent on attendance or completion of self-monitoring. | TLFB (previous 90 weeks) number of drinking days, and number of heavy drinking days. End of intervention (12 weeks), 24 weeks | AE reported significantly fewer drinking days and heavy drinking days relative to BA-E, but this difference was not sustained during the follow up period. | Participants attended an average of 8.44 (SD = 4.12) out of 12 sessions. 62% met criteria for adherence of attending 8 or more sessions. AE participants reported higher levels of PA during treatment and follow up compared to BA-E, but was not statistically significant. Adherent participants reported significantly greater levels of PA than BA-E during intervention, but not follow up. | Those who showed high adherence to PA in the AE group demonstrated significantly lower drinking days than those who had low adherence and those in the BA-E group but had significantly higher heavy drinking days than the BA-E group. |
| Age, mean (SD); 44.37 (10.75) | |||||||||
| Male (55%) | |||||||||
| Brown et al. (2010) USA | Other drugs | Pre-Post | Sedentary drug dependent adults engaged in outpatient substance abuse treatment (N = 16) | 3 components: 1) moderate intensity group exercise, 2) group behavioural treatment and 3) an incentive system. Weekly exercise sessions were led by an exercise physiologist. Sessions began at 20 min increasing to 40 min (treadmill, elliptical machine, or recumbent bicycle) by week 12, and were also “prescribed” to engage in moderate PA on 2–3 other occasions each week. Group behavioural treatment consisted of weekly (20 min) session based on cognitive and behavioural techniques for increasing motivation and maintaining PA. $5 was given for each session attended, and for returning a completed weekly PA monitoring form. | N/A | TLFB (previous 90 days) to collect alcohol and drug use outcomes (Percent days abstinent). End of intervention (12 weeks), 24 weeks | Two thirds of the sample remained abstinent throughout the intervention. Percent days abstinent significantly increased during the intervention period compared to the pre-treatment period and a trend for increased percent days abstinent at 3-month post intervention. | Participants attended an average of 8.6 (SD = 3.9) weekly exercise sessions out of 12; averaged 3.9 (SD = 1.1) days of exercise per week during the intervention; and engaged in 209 (SD = 180) minutes of PA and 147 (SD = 100) minutes of MVPA. | Low-attenders (less than 75% of session) were significantly more likely to relapse than high attenders (80% vs 20% respectively). |
| Age, mean (SD); 38.3 (10.1) | Cardiorespiratory measure significantly improved from baseline to 3 month follow up. | ||||||||
| Male (69%) | |||||||||
| Buchowski et al. (2011b) USA | Other drugs | Pre-Post | Sedentary non-treatment seeking cannabis dependent adults (N = 12). | 10 supervised 30-min treadmill exercise sessions (60–70% heart rate reserve) over 2 weeks | N/A | TLFB (previous 2 weeks) amount of cannabis used. End of intervention (2 weeks), 4 weeks | Daily cannabis use reduced significantly during the intervention and for follow up compared to the baseline. | The goal of 10 planned exercise sessions was met by all participants, with an average intensity of each exercise session in the moderate range (65–75% of age-predicted heart rate). | Significant pre-post exercise reductions in cannabis craving (averaged over 10 sessions, no cumulative effect) |
| Age, mean (SD); 25 (3) | |||||||||
| Female (66.7%) | |||||||||
| Burling et al. (1992) USA | Alcohol and other drugs | Non-RCT (3 arm) | Veterans of a residential program for homelessness and substance abuse (N = 34). | Voluntary participation (alongside the residential treatment program) in a softball team playing league games once a week over 6 months, with twice weekly practices, and a weekly team meeting to discuss individual and team issues such as attitudes and behaviours. | Comparison A: 102 veterans admitted to the same treatment program who chose not to participate in the softball team and remained in treatment for at least 30 days. | Length of stay, participation in outpatient treatment, dur/alcohol use. During residential treatment, and 3 months post-discharge | Softball team members (67.6% followed up) reported significantly higher abstinence rates at 3 months post discharge (91.3% compared to 55.74% in comparison B, not data for comparison group A). Even when assuming those lost to follow up as relapsed, softball team members still showed significantly higher abstinence rates at 3 months (61.76% vs 41.46%) | No data. | Softball team members stayed in treatment significantly longer than both comparison groups. They were also significantly more likely to complete a 13-week outpatient program after discharge. |
| Age, mean (SD); 38.85 (6.87) | Comparison B: 82 veterans admitted to the same treatment programme one year earlier and remained in treatment for at least 30 days | ||||||||
| Male (97.1%) | |||||||||
| Colledge et al. (2017) Switzerland | Alcohol and other drugs | Pilot RCT | People attending a heroin assisted treatment clinic (N = 24). | Exercise group (EX): 12 weeks offering two parallel exercise groups offered on two evenings a week following dispensing of diacetylmorphine. One group offered moderate to vigorous varied activities (including climbing, badminton, strength training and dance), the other group included walking with occasional coordination games for those less physically able for with a dislike of sports. Participation, not fitness, was the aim. (n = 13) | Comparison group: Scheduled at the same time as the EX group with the same frequency. Activities included board games, painting, cooking, museum visits, and billiard games. (n = 11) | TLFB (previous 30 days) total numbers of days consuming any alcohol or substances (including unprescribed medication). 6 weeks, 12 weeks | No differences were found for any substances between groups, across time, or group X time. | Number of vigorous PA minutes per day significantly increased in the EX condition compared to the comparison group. | Comparison group showed higher levels on ‘non-compliance’. |
| Age, mean (SD), EX: 42.7 (6.5); Comparison: 45.8 (4.2), | |||||||||
| Male, EX (69.2%), comparison (62.5%) | Neither group received advice to change their exercise or substance consumption habits. | 38.5% of participants attended at least 18 of 23 sessions, 53.8% attended between 5 and 17 sessions, 7.7% attended fewer than 5 sessions. | |||||||
| Cutter et al. (2014) USA | Other drugs | Pilot RCT | People attending a non-profit community-based organisation specializing in opioid dependence treatment receiving methadone maintenance therapy (N = 29). | Active video game play: Participants completed 5 active video games on the Wii Fit Plus (two aerobic, one strength, one balance, and one yoga) taking between 20 and 25 min 5 days per week for 8 weeks. (n = 15) | Sedentary game play: Participants played inactive video games for a atched amount of time and frequency to the active video game play group. (n = 14) | The Weekly Substance Use Inventory collected weekly detailed daily drug and alcohol use. Weekly urine toxicology screens tested for morphine, oxycodone, and cocaine. Baseline and weekly for 8 weeks | Significant reductions in self -reported levels of illicit opioid and cocaine use over time, but the reduction did not differ by group, nor was there a significant interaction with group by time. | Those in active video gameplay self-reported significantly higher levels overall of MVPA outside of the Wii Fit Plus sessions than those in the sedentary game play group. | There was no significant difference between groups for days retained in treatment. |
| Age, mean (SD) 43.4 (8.5) | |||||||||
| Female (59%) | Participants in both arms attended over 65% of scheduled sessions. | ||||||||
| De La Garza et al. (2016) USA | Other drugs | RCT (3 arm) | Treatment seeking people with concurrent cocaine and tobacco use disorder with no contraindications for vigorous PA. (N = 24). | Running: Three 30-min sessions per week for 4 weeks. Treadmill running at 75% of maximum heart rate. During each visit individuals also completed computerised CBT modules specifically designed for cocaine addiction. Contingency management: Up to $700 was reimbursed to participants if they attended all session. All participants were given a new pair of running shoes, socks, running shorts, and t-shirt at the beginning which they could keep upon completion of the study (n = 10) | Walking: Three 30-min sessions per week for 4 weeks. Treadmill walking at 25% of maximum heart rate. Plus other components of running group. (n = 7) | Daily measure of urine benzoylecgonine (to indicate cocaine use); once daily self-reported (yes/no) cocaine use in past 24 h. Three times weekly for 4 weeks | Non-significant increase in negative cocaine urines and self-report cocaine use in favour of exercising groups, with walking showing slightly larger improvements. When walking and running combined into one group, significant difference in number of self-reported abstinence in favour of exercise. No difference in pre-post craving. | All participants achieved their calculated target heart rate during sessions. | Non significant reductions in pre-post exercise self-reported cravings (VAS 0–100). |
| Age, mean (SD); Running 43.4 (7.4); walking 45.6 (1.6); sitting 45.7 (5.2); Male; Running (90%), walking (71.4%), sitting (71.4%) | Sitting/Control: Sitting passively for a matched duration and frequency without access to reading materials, mobile phone, or internet. Plus other components of running group. (n = 7) | ||||||||
| Over 90% retention in the exercise program. | |||||||||
| Donaghy (1997) Scotland | Alcohol | RCT | Problem drinkers attending an abstinence rehabilitation programme at 4 sites (2 inpatient and 2 outpatient) (N = 165). Original power analysis aimed for n = 120. | Trained physiotherapists led 30 min supervised group exercise sessions twice a week for three weeks. Participants maintained aerobic activity at 70–75% of maximum heart rate for at least 20 min at each session. Participants were encouraged to engage in walking, sports (such as badminton or football) and encouraged to use the gym facilities at the physiotherapy department. After 3 weeks, participants were given a 12 week home based exercise programme consisting of a booklet comprising illustrations of exercises, instructions, tables for setting goals and monitoring heart rate, designed to enable the problem drinker to continue to exercise independently at home following discharge from the rehabilitation programme. A 30-min tape with rhythmical music and voice over with the exercise instructions | Participants were instructed in a 30-min programme twice a week for 3 weeks that included some gentle stretching exercises of trunk and limbs, and breathing exercises. After 3 weeks, participants were given a tape with soft relaxation music and voice over with instructions for trunk and limb stretching and breathing exercises. | Blood samples to test for alcohol use, and self-reported alcohol use. Baseline, 1, 2, and 5 months | Blood samples and self-report showed no improvement in abstinence in the exercise group from 1 month to 2 months, and from 2 months to 5 months compared to control. Chi squared tests at each time point comparing the proportion of participants in each group reporting abstinence/controlled drinking vs uncontrolled drinking showed no differences at any time point. | The intervention group showed improved physiological fitness at 1,2 amd 5 months compared to control. The intervention group reported higher physical activity levels at 2 months than control, but not at 1 or 5 months. | |
| Age, mean (SD); females, 41 (7.77), males, 41 (8.67) | |||||||||
| Male (76.4 | |||||||||
| Giesen et al. (2016) Germany | Alcohol | Non-RCT (3 arm) | Currently abstinent patients with severe alcohol dependence in a long term residential facility (N = 44) | Usual care plus VIVA-Active Program: (1) aerobic exercise (indoor and aqua cycling) Participants were encouraged to exercise at moderate to vigorous intensity. Each session lasted 60 min; (2) functional training (strengthening, coordination, and flexibility exercises; (3) experience orientated group events (e.g. bicycle tours, canoeing, or other day trips). Participant were encouraged to attend twice a week, with two group events per year. 12 months intervention period. (n = 22) | Usual care control: (1) medical including basic care and specialist care; (2) resource-orientated social treatment = , including counselling and milieu therapy; and (3) occupational therapy, suburb or outside of the facility in sheltered workshops. (n = 22) | Relapse to drinking at least once during the 12 months. Collected via data from the residential facility. | During the 12 months among the active and adherent participants (n = 14) no one relapsed to drinking alcohol, whereas four patients in the control group (n = 18) and three of the dropout candidates (n = 8) had a relapse to drinking alcohol. | 14 out of 22 residents attended over the 12-month observation period. | Programme contributed to enhanced quality of life. |
| Age, mean (SD), EX: 52.14 (8.08); Comparison: 54.63 (9.41), | Healthy matched control group with no history of alcohol dependence (n = 24) | ||||||||
| Male, EX (78.6%), comparison (73.7%) | “The majority of participants attended twice a week”. | ||||||||
| Data collected objectively via a sensory armband showed a significant increase in PA levels (steps and kcal expenditure) per week from baseline to follow up for the intervention group, whereas both control remained the same. | |||||||||
| Hallgren et al. (2014) Sweden | Alcohol | Pilot RCT | Alcohol dependent adults attending an outpatient alcohol treatment clinic (N = 18). | Treatment as usual plus 10-week yoga intervention (1.5 h group sessions once per week led by an experienced yoga teacher). Participants were also given instructions on how to continue yoga practice at home and encouraged to complete it once per day. | Treatment as usual: individual counselling sessions with a CBT focus (1 h per week with a medical doctor or psychologist) and the prescription of medication for alcohol dependence as required. | TLFB (time period not reported): drinks per drinking day and weekly consumption (in number of standard drinks equivalent to 12 g of pure ethanol). Baseline and 6 months | Both groups decreased number of drinks per drinking day and drinks per week with greater reductions in the yoga group, but the differences were not statistically significant. | None reported. | |
| Linke et al. (2019) USA | Alcohol and other drugs | PrePost | Veterans seeking SUD treatment through an outpatient drug and alcohol programme at the VA San Diego Healthcare System (n = 15). | The ‘Go-Var!’ programme, grounded in the Socio-Ecological Model. A 12 week intervention consisting of (1) Weekly 90 min psychoeducation classes led by a licensed psychologist focussed on how exercise can aid recovery, motivation and goal setting for exercise, barriers to exercise, and exercise maintenance, (2) YMCA memberships and weekly group exercise sessions, and (3) provision of a FitBit Charge HR for self-monitoring. | N/A | TLFB (previous 30 days prior to most recent decision to stop using at baseline; and previous 90 days at 12 week follow up). Baseline and end of intervention (12 weeks). | Significant reductions from baseline to follow up for days of alcohol use per month, number of drinks per day, and days of drug use per month. | Significant increases in number of steps as measured by FitBit and in two measures of physical fitness (push ups and sit ups) at follow up compared to baseline. | |
| Age, mean (SD): 45 (9.67); Male (87%) | Of 15 participants, 11 completed follow up, attending an average of 6.8 of 12 weekly psychoeducation groups. No data on gym use. | ||||||||
| Mamen et al. (2011) Norway | Alcohol and other drugs | Pre-Post | Substance dependent individuals all polyusers (including alcohol) admitted to an outpatient unit of a hospital psychiatry department. (N = 33). Age, mean (SD): 31.2 (9.9) | An intervention (mean length of training 7.5 months, range 2–15 months) with training conducted on an almost daily basis. Each participant had a training partner assigned to them who had completed a course in applied physiology and psychiatry and helped with planning and monitoring. Training focussed on improving aerobic capacity/power and endurance strength and included jogging, cycling, cross-country skiing, and swimming; and group activities such as aerobics, mountain hiking, and ball games. | N/A | The Short Michigan Alcoholism Screening Test (SMAST): a 13 item “yes/no” response inventory where three or more “yes” responses indicate alcoholism. | No changes in mean scores for either measure from baseline to follow up. | Participants performed an average of 301 (±16) hours of physical training. 74% (±3%) was low intensity training below the lactate threshold. Participants showed improvements in VO2 max relative to body weight. No change in BMI was observed. | |
| Male (78.8%) | The Drug Abuse Screening Test-20 (DAST); a 20-item self-administered screening inventory with “yes/no” responses where 11 or more “yes responses indicate a substantial level of use. Collected at baseline, and upon discharge from treatment | ||||||||
| Rawson et al. (2015) USA | Other drugs | RCT | Methamphetamine dependent individuals newly entered into residential treatment (N = 135). | Exercise intervention: Structured exercise programme 3 time a week for 8 weeks. Sessions consisted of 5 min warm up, 30 min of treadmill exercise to maintain heart rate at 60–85% of maximum, followed by 15 min of incremental weight training, finished with a 5-min cool down. (n = 69) | Health education control: 55-min health education sessions 3 times a week for 8 weeks delivered by a trained health educator covering topics including stress reduction, health screening, healthy relationships, and sexually transmitted diseases. Consisted of facilitator discussion, handouts and media. (n = 66) | MA urine drug screen, self-reported MA use (substance use inventory). 1, 3, and 6 months post residential care | Exercise group showed moderately lower MA use rates at all follow ups reported by both urine drug screens and self-report, however these differences were not significantly different. | Participants attended an average of 17.4 (SD = 7.3 sessions. Participants who attended 16 or more sessions were significantly less likely to self-report MA use and 1, 3, and 6 months. Urine drug screens also showed high attenders more likely to be abstinent at all time points. There was no relationship between attendance at control sessions and MA use. | Lower severity MA use (<18 days in past 30 at baseline) group in exercise intervention showed significantly better outcomes in abstinence rates at all follow ups compared to lower use groups in health education control. |
| Age, mean (SD): 31.7 (6.9) | Those who were abstinent 1 month post discharge report significantly more PA than those who were not. Those with lower MA dependence more frequently engaged in PA. | ||||||||
| Male (80%) | |||||||||
| Roessler et al. (2017) Denmark | Alcohol | RCT (3 arm) | Individuals with harmful of dependent alcohol drinking levels attending outpatient treatment centres. (N = 175). Age, mean (SD): 45 (11.3) | Treatment as usual plus individual exercise: participants received a written training programme with running instructions encouraging twice weekly exercise during an individual session prior to start. This was followed up once or twice during the intervention period if requested. Participants requested to record exercise activity use wrist worn heart rate monitors. (n = 60) | Treatment as usual plus supervised group exercise: provided with running instruction depending on level of experience and 24 weeks of group exercise twice a week supervised by running instructors with backgrounds in sport science and psychology. Participants requested to record exercise activity use wrist worn heart rate monitors. (n = 62) | TLFB (previous 30 days), % alcohol free days, number of drinks per day, number of heavy drinking days. Baseline, 6 months, 12 months | At six months all groups showed marked reduction in excessive drinking with no differences between groups. The OR for reduced drinks per drinking day for individual exercise group (0.39 [0.15; 1.01] approached significance (p = 0.059) | No adherence data. A dose response effect was observed – alcohol consumption reduced by 4% for each increased exercising day in the intervention groups. | All participants (across groups) who reported completing moderate PA had significantly lower OR (0.12 [0.05; 0.31], p < 0.001) for excessive drinking than those reporting low levels of PA. Dose response: amount of alcohol consumption in the intervention groups decreased by 4% [95% CI: 0.03–6.8%], p < 0.0015, for each increased exercising day. |
| Male (68.6%) | Control group: participants were asked not to change their PA levels. (n = 53) | ||||||||
| Shaffer et al. (1997) USA | Other drugs | RCT | Individuals enrolled in an outpatient methadone maintenance programme (N = 59). | Usual care plus yoga intervention: 75-min instructor led hatha yoga sessions over 22 weeks. Frequency not reported. | Usual care: (1) methadone maintenance for 5 months; (2) Individual psychotherapy, and (3) Group Psychotherapy | Weekly report cards from the clinic detailing illicit drug use. Up to 5 months post baseline. | Remaining in treatment longer was positively correlated with reduced drug use (r = .12, p < 001) regardless of group. There were no differences on outcomes by group. | Participants attended an average of 8.18 intervention sessions compared to 10.42 usual care sessions. | |
| Age, years: 35.92; range 23–46. | |||||||||
| Male, n = 25, female n = 24 | |||||||||
| (Sinyor et al. (1982) Canada | Alcohol | Non-RCT (3 arm) | Individuals resident an inpatient rehabilitation centre for alcoholics (N = 58). | All participants took part in usual care consisting of several hours of daily intensive group therapy and counselling and urged to become members of alcoholics anonymous following release from the programme. Fitness classes took place early each weekday morning for 6 weeks, consisting of 20 min stretching and warm up, progressing to light calisthenics, followed by a 12-min walk/run (with residents encouraged to cover greater distances in shorter time spans) followed by 20 min of muscle strengthening exercises such as sit ups and push ups. | Cohort of patients who attended the same centre prior to the introduction of the fitness programme. (N = 19) | Participants were contacted by a researcher 3 months after discharge to confirm abstinence. Abstinence was corroborated by work colleagues or family members. 3 months. | 69.3% were still abstinent at 3 months who took part in the fitness programme, compared to 38% of those who were there before the fitness programme, and 36.9% of people who attended other treatment centres. | Intervention participants significantly reduced body fat %, increased VO2 max, and decreased basal heart rate. | |
| Age, mean: 42. | Cohort of patients attending other treatment centres without a fitness programme in Quebec at the same time as the intervention group (N = 80) | ||||||||
| Male (79.3%) | |||||||||
| Trivedi et al. (2017) USA | Other drugs | RCT | Adult stimulant users in residential stimulant abuse treatment (average stay just under 3 weeks) across 9 residential treatment addiction centres (N = 302). | Exercise intervention: Supervised treadmill exercise sessions 3 times a week for 12 weeks during the acute phase (at a dose of 12 kilocalories*kilogram of body weight*week). The maximum intensity for most participants was equivalent to walking at a moderate speed and incline for approximately 150 min per week. Extra sessions were scheduled for participants who needed extra sessions to achieve this dose. | Health education intervention: Matching the exercise intervention for contact time and frequency. One to one session in which informatin on health related topics (e.g. cancer, heart disease, mental health) was distributed via didactics, websites, audio, video, and written materials (exercise was not a topic). | TLFB for self reported drug use, and urine drug screens; % of stimulant abstinent days during weeks 4–12 (after leaving residential treatment). Collected 3 times a week at all study visits | No difference in any outcome between groups in any planned analysis, including with ITT (imputing missing data as positive for stimulant use) | Participants in the intervention group attended 64.0% (SD = 30.4%) of expected intervention sessions. Participants completed 69.2% of the prescribed exercise dose (i.e. approximately 79 min per week). | Post hoc analysis, adjusting for percent of sessions attended (exercise group attended 64.0% (SD 30.4%) and health education control attended 74.7% (SD28.7%), the adjusted proportion of abstinent days was 78.7% (SE = 0.02%) for the exercise group, and 73.9% (SE = 0.02%) for the health education group, a modest significant difference in favour of the exercise group (p = 0.03). Number needed to treat: 7.2. |
| Age, mean (SD): 39.0 (11) | |||||||||
| Male (60%) | |||||||||
| Weinstock et al. (2008) USA | Alcohol and other drugs | Retrospective controlled study | New admissions to intensive outpatient treatment for substance use disorders (including alcohol) (N = 187). Age, mean (SD): Exercisers, 36 (6.2); Non-exercisers, 35.4 (7.2). | Exercisers: identified retrospectively from a study involving contingency management for remaining abstinent and for completing 3 goal related activities a week over a 12-week intervention. Goals were coded as “exercise-related” or not, and those who completed at least one exercise related goal (objectively verified) were classed as exercisers. (n = 45) | Non-exercisers: sampled from the same study but were individuals who did not complete any exercise-related goals as part of the contingency management intervention. (n = 142) | Participants submitted breath and urine samples to confirm abstinence from alcohol, cocaine, and opioids to earn reinforcement for drug abstinence. Collected every 1–3 days during study period. | After controlling for all other variables, those who completed at least one exercise related activity achieved a longer duration of abstinence (6.04 (SD = 0.43) weeks) compared to those who did complete any exercise activity (4.75 (SD = 0.34) weeks) (p < 0.01) during the 12 week study period. | No data. | |
| Male: Exercisers (53.3%), non-exercisers (38.7) |
4.5.1. Populations
All studies included adults who were either diagnosed as alcohol or substance dependent (SUD) or were engaged in specialist treatment programmes across a variety of settings (e.g. inpatient, outpatient, community, or residential programmes), one focussed solely on currently abstinent patients with severe alcohol dependence (Giesen et al., 2016). Only one study included participants not receiving specialist alcohol or other drug treatment (non-treatment seeking cannabis dependent adults (Buchowski et al., 2011)). One study included people attending heroin assisted treatment (Colledge et al., 2017) and two studies those engaged in methadone maintenance therapy (Cutter et al., 2014; Shaffer et al., 1997). One study included inactive alcohol dependent women with depressive symptoms (Abrantes et al., 2017), one veterans of a residential programme for homelessness and other drug abuse (Burling et al., 1992), and one veterans attending an outpatient drug and alcohol programme (Linke et al., 2019). Along with alcohol, other drugs used included heroin, opioids, methamphetamine, cocaine, stimulants, and polysubstance use. The majority of the studies were conducted in the USA (n = 12), with one study conducted in each of Switzerland, Scotland, Germany, Sweden, Norway, Denmark, and Canada.
4.5.2. Interventions
Interventions varied greatly across studies: including: supervised treadmill exercise sessions three times a week aimed at achieving a predefined ‘dose’ of PA for 12 weeks (Trivedi et al., 2017); ten supervised treadmill sessions at 60–70% of heart rate reserve over two weeks (Buchowski et al., 2011); three 30-min treadmill session at 75% of maximum heart rate with concurrent computerised CBT modules and up to $700 and new running shoes, socks, shorts and a t-shirt for attending all sessions (De La Garza et al., 2016); one to one consultations with a PA counsellor weekly or biweekly for 12 weeks and provision of a FitBit activity tracker to guide progressive goal setting (Abrantes et al., 2017); a 12 week multicomponent intervention of group psychoeducation for exercise, gym membership and weekly group activity, and provision of FitBit activity tracker (Linke et al., 2019); community based participation in a soft ball team playing matches once a week with training sessions twice a week for six months (Burling et al., 1992); a 12 week multicomponent intervention consisting of moderate intensity aerobic exercise, group behavioural treatment, and an incentive system (Brown et al., 2014); 12 weeks of parallel groups chosen by the participant including either moderate to vigorous varied activities (e.g. climbing, badminton, strength training, or dance) or walking and coordination games for those less physically able or with a dislike of sports (Colledge et al., 2017); eight weeks of active video gameplay (Wii Fit Plus) for 20–25 min five times per week (Cutter et al., 2014); 10 weeks of weekly 90 min yoga sessions combined with instruction to complete yoga at home once per day (Hallgren et al., 2014); and twice weekly supervised running sessions for 24 weeks (Roessler, Bilberg, et al., 2017).
Adherence.
4.5.3. Controls/comparators
Of the 10 randomised controlled trials (three of which had three-arms), six employed controlled conditions matched to the PA intervention in terms of time, frequency, and duration without a PA element (Colledge et al., 2017; Cutter et al., 2014; De La Garza et al., 2016; Donaghy, 1997; Rawson et al., 2015; Trivedi et al., 2017), one compared brief advice to exercise (Brown et al., 2014), and three included control arms consisting of treatment as usual (Hallgren et al., 2014; Roessler, Bilberg, et al., 2017; Shaffer et al., 1997). Three prospective studies of non-randomised design compared PA with treatment as usual (Burling et al., 1992; Giesen et al., 2016; Sinyor et al., 1982); and one retrospective controlled study compared those who chose PA as a contingency management plan for preventing relapse with those who chose non-PA activities (Weinstock et al., 2008).
4.5.4. Outcomes
Of the 19 studies, seven included biochemical verification of abstinence (e.g. urine toxicology, blood samples, or breath tests) (Cutter et al., 2014; De La Garza et al., 2016; Donaghy, 1997; Hallgren et al., 2014; Rawson et al., 2015; Trivedi et al., 2017; Weinstock et al., 2008), nine studies relied on self-reported measures (Abrantes et al., 2017; Brown et al., 2010, 2014; Buchowski et al., 2011; Colledge et al., 2017; Linke et al., 2019; Mamen et al., 2011; Roessler, Bilberg, et al., 2017; Sinyor et al., 1982), and three studies included data obtained from secondary sources such as hospital or clinical records (Burling et al., 1992; Giesen et al., 2016; Shaffer et al., 1997). The most commonly used measure for obtaining alcohol and other drug use was the Timeline Follow Back (TLFB) method (Sobell & Sobell, 1992) used for the primary alcohol and other drug use outcome in nine studies (Abrantes et al., 2017; Brown et al., 2010, 2014; Buchowski et al., 2011; Colledge et al., 2017; Hallgren et al., 2014; Linke et al., 2019; Roessler, Bilberg, et al., 2017; Trivedi et al., 2017).
4.5.4.1. Alcohol
Of the studies with a control group, only one study (Brown et al., 2014) with 26 participants reported statistically significant beneficial effects of a multicomponent PA intervention on self-reported alcohol use (number of drinking and heavy drinking days) compared to usual care during the intervention period, but the difference was not sustained at 12 weeks follow up. Three other studies showed a non-significant trend in favour of a PA intervention compared to a control (Giesen et al., 2016; Hallgren et al., 2014; Sinyor et al., 1982), and two studies showed no differences between arms. One study of pre-post design showed a significant reduction in drinking days following a multicomponent PA intervention (12 weeks) with 44% remaining abstinent throughout (Abrantes et al., 2017).
4.5.4.2. Other drugs
All other drug use studies (n = 7) involved a control condition. Only one study reported significant reductions in levels of use of the targeted drug (cannabis) (Buchowski et al., 2011) at end of two weeks of ten treadmill running sessions among 12 participants compared to control. One three-arm study showed a non-significant trend for lower levels of cocaine use throughout the study in favour of walking and running conditions compared to a sitting condition (De La Garza et al., 2016), however when data from the walking and running groups were combined, it showed significant differences in favour of the active group compared to passive sitting. One other study showed a non-significant trend in favour of a PA intervention on abstinent rates up to 6 months post discharge from residential care for methamphetamine use (Rawson et al., 2015). Four other studies reported no significant differences between arms (Colledge et al., 2017; Cutter et al., 2014; Shaffer et al., 1997; Trivedi et al., 2017).
4.5.4.3. Comorbid alcohol and other drug use
Two studies with a control condition reported significant results. One of which demonstrated a higher rate of abstinence at three months post discharge from outpatient care following participation in a softball team (Burling et al., 1992). The other, a retrospective control comparison, showed those who chose to participate in a range physical activities achieved longer periods of abstinence than those who didn't (Weinstock et al., 2008).
Two studies of pre-post design reported significantly lower levels of use following a 12 week multicomponent PA intervention compared to baseline (Brown et al., 2010; Linke et al., 2019), but in one of these studies with a three month follow up the effect diminished (Brown et al., 2010). One other pre-post study reported no effect on screening scores for alcohol and other drug use of an adjuvant PA intervention during outpatient treatment (Mamen et al., 2011).
4.5.4.4. Secondary outcomes
PA levels were reported in a variety of ways, and in some cases not at all. Two studies using FitBit activity trackers reported significant increases in number of daily steps form baseline to follow up (Abrantes et al., 2017; Linke et al., 2019). Two studies reported higher self-reported levels of PA in the experimental arm compared to a comparison group (Cutter et al., 2014; Donaghy, 1997). Four studies reported measures of improved physical fitness associated with the intervention (Brown et al., 2010; Donaghy, 1997; Linke et al., 2019; Sinyor et al., 1982).
Adherence data was reported in the majority of studies, but in a wide variety of formats. Some were very detailed (e.g. Fitbit was worn for 73% of days and participants completed an average of 4.7 out of 6 scheduled telephone PA counselling sessions) (Abrantes et al., 2017), and some were particularly vague (e.g. “the majority of participants attended twice a week”) (Giesen et al., 2016). An adherence rate of around 60–70% of planned intervention sessions was the most commonly reported range (Abrantes et al., 2017; Brown et al., 2010, 2014; Cutter et al., 2014; Linke et al., 2019; Rawson et al., 2015; Trivedi et al., 2017). Some studies considered sensitivity analyses related to adherence to PA (regardless of allocation) or the intervention, and showed higher levels of adherence frequently associated with better outcomes related to alcohol or substance use (Brown et al., 2010, 2014; Rawson et al., 2015; Roessler, Bilberg, et al., 2017; Trivedi et al., 2017).
One study reported that better outcomes were reported for the PA intervention in patients with less severe methamphetamine use compared to those with higher levels (Rawson et al., 2015).
A dose-response relationship between PA and alcohol use was suggested by another study, reporting a 4% reduction in alcohol use for each extra exercising day (Roessler, Bilberg, et al., 2017).
No serious adverse events related to PA were reported in any of the studies.
4.5.5. Meta-analyses
Only two studies had outcome data on alcohol abstinence suitable for the meta-analysis. One other study (Giesen et al., 2016) reported relapse rates but the data were too small to incorporate.
One study (Donaghy, 1997) reported the number of people who relapsed back to alcohol use at the end of intervention. The other study (Sinyor et al., 1982) reported the abstinence rate from alcohol, based on which we calculated the number of people who relapsed. The results from these two studies were consistent, with overlapping confidence intervals.
The estimated overall risk ratio for alcohol abstinence was 1.56 (95%CI: 0.78 to 3.14) from fixed-effect meta-analysis and 1.79 (95%: 1.29 to 2.47) from random-effect meta-analyses. There was substantial between-study heterogeneity (I2 = 67.1%) (Fig. 7 ).
Fig. 7.
Abstinence from alcohol.
The results from random-effect meta-analysis accounted for the between-study heterogeneity, indicating insufficient evidence for the effect of PA interventions on alcohol abstinence.
4.5.6. Risk of bias and quality appraisal
Of the ten studies of randomised design, four were judged at high risk of bias (Donaghy, 1997; Hallgren et al., 2014; Roessler, Bilberg, et al., 2017; Shaffer et al., 1997) and six with some concerns over risk of bias (Brown et al., 2014; Colledge et al., 2017; Cutter et al., 2014; De La Garza et al., 2016; Rawson et al., 2015; Trivedi et al., 2017). Of the eight studies of non-random design, six were judged to be at severe risk of bias (Buchowski et al., 2011; Burling et al., 1992; Giesen et al., 2016; Mamen et al., 2011; Sinyor et al., 1982; Weinstock et al., 2008), and two at moderate risk of bias (Abrantes et al., 2017; Brown et al., 2010). (See supplementary file 1).
4.5.7. Quality of the evidence
Using the GRADE assessment of quality (Guyatt et al., 2008), the evidence for PA and the reduction of alcohol and other drug use was consistently downgraded due to study limitations, inconsistency of results, indirectness of evidence and imprecision, giving very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. Further research is needed to draw any conclusions (Table 8 ).
Table 8.
Summary of findings table - treatment.
| Physical activity and the treatment of alcohol and other drug use | ||||||
|---|---|---|---|---|---|---|
| Population: Individuals with a diagnosed substance use disorder, individuals seeking treatment for alcohol and other drug use | ||||||
| Settings: community | ||||||
| Intervention: physical activity | ||||||
| Comparison: alternative non-physical activity intervention, no intervention, usual care | ||||||
| Outcome | Illustrative comparative risk | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comment | |
| Assumed risk usual care | Corresponding risk physical activity intervention | |||||
| Abstinence from alcohol and/or substance use levels | See comment | See comment | RR 1.56 (0.78–3.14) | 1399 (19) | ⊕◯◯◯ very lowa | Effect is uncertain |
High and severe risk of bias found in most studies related to confounding, classification of interventions, deviation form intended interventions, reporting bias, and missing data.
4.6. Economic data
Whilst we had intended locating economic evaluations with a view to conduction an analysis of economic data, no useable data was found in any of the included studies.
5. Discussion
This is the most comprehensive review of evidence on the effects of PA interventions for the prevention, reduction, and treatment of alcohol and other drug use. The broad scope ensured maximum coverage of what is a relatively under researched field, while maintaining a clear framework to help the reader identify how research links to specific questions and phases in developing an evidence-base for efficacy, effectiveness, and mechanisms.
5.1. Prevention
The concept of using PA to prevent the initiation of alcohol and other drug use was the least well researched area with only five studies identified and all taking place in the USA. This is likely due to the challenges and cost of designing experimental studies requiring a long duration of follow up to evidence any effect. The multi-component nature of interventions which largely were targeted at younger people in education added to the complexity, as isolating the specific impact of PA was problematic. Whilst the meta-analysis completed within this review suggests a modest favourable effect of PA on subsequent initiation of alcohol and other drug use outcomes, this should be treated cautiously due to the heterogeneity of the interventions. One study focussed on “at risk” youth and showed favourable outcomes (Collingwood et al., 1991), particularly among those who increased their levels of physical fitness. It may be that interventions focussed on those who are at risk of initiating alcohol and other drug use are more beneficial than those that are broader in their aim. More robust larger studies accurately describing changes in PA levels (perhaps alongside structured exercise programmes) and subsequent outcomes are needed with appropriate statistical analysis to single out the effects of PA from other possible influences on outcomes.
The framework shown in Fig. 1, highlights the current limited research available on which PA related behaviours can influence uptake of alcohol and other drug use, while also laying out future research questions to be answered. For example, do structured exercise programmes and/or daily physical activity help to reduce the risk of initiating alcohol and other drug use and if so, is there a dose response and what are the cognitive, affective and physiological mechanisms? Related questions emerge in terms of what interventions can have sustainable effects on behaviour, and how much support and of what type is needed to influence behaviour change processes?
5.2. Reduction
Research relating to PA and the reduction of alcohol and other drug use among those not seeking treatment nor diagnosed with a use disorder was found to lack sufficient consistency to draw conclusions relating to its effect, highlighted by only four studies included in the meta-analysis for one common outcome. The studies identified were of different designs, and of low quality with all being considered at high risk of bias. The majority of studies included college students which limits generalisability, and the heterogeneity of interventions limits any inference about specific effective components and design.
With reference to Fig. 1, there remains uncertainty about which PA related behaviours can help reduce alcohol and other drug use. There is insufficient data to address our secondary aims in terms of PA dose, mechanisms of change, and detail related to effective intervention components. There are indications that alcohol consumption increased during COVID-19 lockdown in some cultures (Da, Im, & Schiano, 2020) and future research may help to understand if those who were less sedentary and did more daily physical activity or exercise were less likely to increase alcohol consumption to harmful levels and if so, was there a dose response relationship and what mechanisms were involved? We may also learn more about if and how individuals developed strategies to use PA to self-regulate alcohol and substance use during lockdown, though these processes may be best understood through mixed methods.
5.3. Treatment
The most well researched area was for PA in the treatment of alcohol and other drug use amongst those seeking treatment or diagnosed with a use disorder, yet conclusions are again difficult to make due to heterogeneity of study design, populations, interventions, and outcomes. Studies were a mix of efficacy and effectiveness studies and of generally poor quality (no studies rated at low risk of bias). In the absence of any adverse events being reported, not any of the studies reporting increases in levels of use, there is no indication that PA intervention pose any risk to people using alcohol and other drugs. With reference to our framework in Fig. 1, the intervention in only four studies included details of a tailored motivational element to the intervention (i.e. one to one or groups motivation sessions) (Abrantes et al., 2017; Brown et al., 2014; Brown, Prince, Minami, & Abrantes, 2016; Linke et al., 2019), rather than or in addition to a structured exercise programme. Such a tailored approach may offer those in the treatment setting greater scope to develop and use behaviour change skills to manage PA and an addiction when they are ready to make changes. In the studies that did report PA engagement during an intervention there appeared to be a dose response relationship, which implies interventions need a stronger focus on overcoming barriers to being physically active, especially for those with higher levels of drug use. From within subjects studies, only one did not report changes in levels of use at the end of intervention and was a yoga based intervention with no data on adherence to PA (Shaffer et al., 1997) suggesting the modality and dose of PA may be important in producing positive outcomes and the one study with longer term outcomes and reported a return to pre-intervention levels of use. More understanding of how to create changes in PA long term is needed, and consideration for this should be built into intervention design. Only one RCT included appropriate power calculations to detect changes in the primary outcome (Trivedi et al., 2017) but failed to detect significant changes in levels of drug (stimulant) use. The intervention was prescriptive in nature with no tailored motivational support where participants required to exercise regularly on a treadmill to complete a ‘dose’ of PA equivalent to the weekly guidelines of 150 min of MVPA per week, which suggests empowering individuals to complete PA through tailored approaches outlined above may have more success. There was also limited evidence to suggest PA may be more effective for people with lower levels of drug use, which may have implications for when PA interventions are introduced and may be best suited to when levels of use are stable or under control. Studies varied in terms of setting, whether as adjunct to an inpatient or outpatient programme, and no clear trend was evident to suggest how an intervention might be best placed.
Considerable heterogeneity in study design, populations, interventions, and outcomes limits any firm conclusions on the effects of PA on alcohol and other drug use. The majority were pilot studies or exploratory in nature with speculative interpretation and conclusions.
The treatment studies included in this review represent a wide variety of PA modalities and approaches, the majority of which have shown potentially promising effects on alcohol and other drug use outcomes. However, no studies included in the review included an objective measure of physical activity. Some studies did assess fitness change as an indicator of exercise adherence (and these studies had a tendency to report positive outcomes on alcohol and other drug use) but further research is needed that can quantify both sedentary behaviour and different intensities of PA.
6. Limitations
The range of literature we identified, in terms of study and intervention design, added to the challenge of conducting this review. We hope the way the manuscript is presented adds clarity but we accept that the framework used and focus on prevention, reduction and treatment may have involved over simplification in describing which populations were involved, what the intervention and control conditions involved and how the outcomes were defined. Despite the inclusion of numerous studies under each of the aims, meta analyses were limited by the lack of comparable data reported in the literature meaning any findings should be treated with caution. Because the review identified some studies which involved a multi-component intervention, we had to make some difficult decision about whether or not to include the study in a review of the effects of PA on our outcomes of interest. As a result, some multi-component interventions were excluded where PA was not deemed to be of sufficient focus or of sufficient intensity and participation was not evident.
7. Conclusions
This is the first rigorous systematic review of the effects of PA interventions for the prevention, reduction and treatment of alcohol and other drug use, and to determine if there is evidence for an optimal dose of PA, and any specific mechanisms involved in how PA influences alcohol and other drug use. Overall, the quality of evidence is limited, and only a few studies were adequately designed to provide any confidence in the findings. Firm conclusions are difficult to make due to the numerous limitations in the research identified. The review revealed that further research, with more rigorous approaches as outlined in this review, is need to understand how to make PA interventions acceptable and feasible (in terms of delivery mode and dose) in the context of prevention, reduction and treatment, and to test the effects of such interventions on alcohol and other drug use in well-designed studies.
Declaration of competing interest
JN has received, through her University, research funding from Mundipharma Research Ltd and Camurus AB to study novel opioid pharmacotherapy delivery systems and nasal naloxone.
Acknowledgements
This paper presents independent research funded by the NIHR under its Research for Patient Benefit (RfPB) Programme (Grant Reference Number PB-PG-0215-36117). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health & Social Care.
This report is independent research supported by the National Institute for Health Research Applied Research Collaboration South West Peninsula. The views expressed in this publication are those of the authors and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care.
References
- Abrantes A.M., Blevins C.E., Battle C.L., Read J.P., Gordon A.L., Stein M.D. Developing a Fitbit-supported lifestyle physical activity intervention for depressed alcohol dependent women. Journal of Substance Abuse Treatment. 2017;80:88–97. doi: 10.1016/j.jsat.2017.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M., Hedges L.V., Higgins J.P.T., Rothstein H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Research Synthesis Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- Brown R.A., Abrantes A.M., Minami H., Read J.P., Marcus B.H., Jakicic J.M. A preliminary, randomized trial of aerobic exercise for alcohol dependence. Journal of Substance Abuse Treatment. 2014;47(1):1–9. doi: 10.1016/j.jsat.2014.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown R.A., Abrantes A.M., Read J.P., Marcus B.H., Jakicic J., Strong D.R. A pilot study of aerobic exercise as an adjunctive treatment for drug dependence. Mental Health and Physical Activity. 2010;3(1):27–34. doi: 10.1016/j.mhpa.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown R.A., Prince M.A., Minami H., Abrantes A.M. An exploratory analysis of changes in mood, anxiety and craving from pre- to post-single sessions of exercise, over 12 weeks, among patients with alcohol dependence. Mental Health and Physical Activity. 2016;11:1–6. doi: 10.1016/j.mhpa.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchowski M.S., Meade N.N., Charboneau E., Park S., Dietrich M.S., Cowan R.L. Aerobic exercise training reduces cannabis craving and use in non-treatment seeking cannabis-dependent adults. PloS One. 2011;6(3) doi: 10.1371/journal.pone.0017465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burling T.A., Seidner A.L., Robbins-Sisco D., Krinsky A., Hanser S.B. Batter up! Relapse prevention for homeless veteran substance abusers via softball team participation. Journal of Substance Abuse. 1992;4(4):407–413. doi: 10.1016/0899-3289(92)90047-2. http://www.ncbi.nlm.nih.gov/pubmed/1338187 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Butzer B., LoRusso A., Shin S.H., Khalsa S.B. Evaluation of yoga for preventing adolescent substance use risk factors in a middle school setting: A preliminary group-randomized controlled trial. Journal of Youth and Adolescence. 2017;46(3):603–632. doi: 10.1007/s10964-016-0513-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colledge F., Vogel M., Dürsteler-Macfarland K., Strom J., Schoen S., Pühse U. A pilot randomized trial of exercise as adjunct therapy in a heroin-assisted treatment setting. Journal of Substance Abuse Treatment. 2017;76:49–57. doi: 10.1016/j.jsat.2017.01.012. [DOI] [PubMed] [Google Scholar]
- Collingwood T.R., Reynolds R., Kohl H.W., Smith W., Sloan S. Physical fitness effects on substance abuse risk factors and use patterns. Journal of Drug Education. 1991;21(1):73–84. doi: 10.2190/HV5J-4EYN-GPP7-Y3QG. http://www.ncbi.nlm.nih.gov/pubmed/2016666 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Collingwood T.R., Sunderlin J., Reynolds R., Kohl H.W., 3rd Physical training as a substance abuse prevention intervention for youth. Journal of Drug Education. 2000;30(4):435–451. doi: 10.2190/rvue-9xw7-tyrq-ejr8. [DOI] [PubMed] [Google Scholar]
- Correia C.J., Benson T.A., Carey K.B. Decreased substance use following increases in alternative behaviors: A preliminary investigation. Addictive Behaviors. 2005;30(1):19–27. doi: 10.1016/j.addbeh.2004.04.006. [DOI] [PubMed] [Google Scholar]
- Cutter C.J., Schottenfeld R.S., Moore B.A., Ball S.A., Beitel M., Savant J.D. A pilot trial of a videogame-based exercise program for methadone maintained patients. Journal of Substance Abuse Treatment. 2014;47(4):299–305. doi: 10.1016/j.jsat.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da B.L., Im G.Y., Schiano T.D. COVID-19 hangover: A rising tide of alcohol use disorder and alcohol-associated liver disease. Hepatology. 2020 doi: 10.1002/hep.31307. [DOI] [PubMed] [Google Scholar]
- De La Garza R., Yoon J.H., Thompson-Lake D.G.Y., Haile C.N., Eisenhofer J.D., Newton T.F. Treadmill exercise improves fitness and reduces craving and use of cocaine in individuals with concurrent cocaine and tobacco-use disorder. Psychiatry Research. 2016;245:133–140. doi: 10.1016/j.psychres.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L., Bharat C., Glantz M.D., Sampson N.A., Scott K., Lim C.C.W. The epidemiology of drug use disorders cross-nationally: Findings from the WHO's World Mental Health Surveys. International Journal of Drug Policy. 2019;71:103–112. doi: 10.1016/j.drugpo.2019.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaghy M.E. The investigation of exercise as an adjunct to the treatment and rehabilitation of the problem drinker. 1997. Retrieved from http://theses.gla.ac.uk/3250/1/1997donaghyphd.pdf.
- Engelmann A.J., Aparicio M.B., Kim A., Sobieraj J.C., Yuan C.J., Grant Y. Chronic wheel running reduces maladaptive patterns of methamphetamine intake: Regulation by attenuation of methamphetamine-induced neuronal nitric oxide synthase. Brain Structure and Function. 2014;219(2):657–672. doi: 10.1007/s00429-013-0525-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fareed A., Casarella J., Amar R., Vayalapalli S., Drexler K. Benefits of retention in methadone maintenance and chronic medical conditions as risk factors for premature death among older heroin addicts. Journal of Psychiatric Practice. 2009;15(3):227–234. doi: 10.1097/01.pra.0000351884.83377.e2. [DOI] [PubMed] [Google Scholar]
- Garner P., Hopewell S., Chandler J., MacLehose H., Schünemann H.J., Akl E.A. When and how to update systematic reviews: Consensus and checklist. BMJ (Online) 2016. [DOI] [PMC free article] [PubMed]
- Georgakouli K., Manthou E., Georgoulias P., Ziaka A., Fatouros I.G., Mastorakos G. Exercise training reduces alcohol consumption but does not affect HPA-axis activity in heavy drinkers. Physiology & Behavior. 2017;179:276–283. doi: 10.1016/j.physbeh.2017.07.003. [DOI] [PubMed] [Google Scholar]
- Giesen E.S., Zimmer P., Bloch W. Effects of an exercise program on physical activity level and quality of life in patients with severe alcohol dependence. Alcoholism Treatment Quarterly. 2016;34(1):63–78. doi: 10.1080/07347324.2016.1113109. [DOI] [Google Scholar]
- Griswold M.G., Fullman N., Hawley C., Arian N., Zimsen S.R.M., Tymeson H.D. Alcohol use and burden for 195 countries and territories, 1990-2016: A systematic analysis for the global burden of disease study 2016. The Lancet. 2018;392(10152):1015–1035. doi: 10.1016/S0140-6736(18)31310-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyatt G.H., Oxman A.D., Vist G.E., Kunz R., Falck-Ytter Y., Alonso-Coello P. Grade: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347. (.AD) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallgren M., Romberg K., Bakshi A.-S., Andréasson S. Yoga as an adjunct treatment for alcohol dependence: A pilot study. Complementary Therapies in Medicine. 2014;22(3):441–445. doi: 10.1016/j.ctim.2014.03.003. [DOI] [PubMed] [Google Scholar]
- Hallgren M., Vancampfort D., Giesen E.S., Lundin A., Stubbs B. Exercise as treatment for alcohol use disorders: Systematic review and meta-analysis. British Journal of Sports Medicine. 2017;51(14):1058. doi: 10.1136/bjsports-2016-096814. [DOI] [PubMed] [Google Scholar]
- Hashemi Nosrat Abadi T., Vaghef L., Babri S., Mahmood-Alilo M., Beirami M. Effects of different exercise protocols on ethanol-induced spatial memory impairment in adult male rats. Alcohol. 2013;47(4):309–316. doi: 10.1016/j.alcohol.2013.01.008. [DOI] [PubMed] [Google Scholar]
- Higgins J.P.T., Green S. The Cochrane collaboration. 2011. Cochrane handbook for systematic reviews of interventions. [updated March 2011] Table.7.7.a: Formulae for combining groups. [Google Scholar]
- Higgins J., Sterne J., Savovic J., Page M., Hrobjartsson A., Boutron I. A revised tool for assessing risk of bias in randomized trials. In: Chandler J., McKenzie J., Boutron I., Welch V., editors. Vol. 10. 2016. (Cochrane database of systematic reviews). Suppl 1. [Google Scholar]
- Landale S.A. Trajectories, transitions and turning points: Sports, substance misuse, and desistance. Durham university. 2012. Retrieved from http://www.opengrey.eu/item/display/10068/991480.
- Linke S.E., Hovsepians R., Schnebly B., Godfrey K., Noble M., Strong D.R. The Go-VAR (Veterans Active Recovery): An adjunctive, exercise-based intervention for veterans recovering from substance use disorders. Journal of Psychoactive Drugs. 2019;51(1):68–77. doi: 10.1080/02791072.2018.1560518. [DOI] [PubMed] [Google Scholar]
- Linke S.E., Ussher M. Exercise-based treatments for substance use disorders: Evidence, theory, and practicality. The American Journal of Drug and Alcohol Abuse. 2015;41(1):7–15. doi: 10.3109/00952990.2014.976708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch W.J., Peterson A.B., Sanchez V., Abel J., Smith M.A. Exercise as a novel treatment for drug addiction: A neurobiological and stage-dependent hypothesis. Neuroscience & Biobehavioral Reviews. 2013;37(8):1622–1644. doi: 10.1016/j.neubiorev.2013.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamen A., Pallesen S., Martinsen E. Changes in mental distress following individualized physical training in patients suffering from chemical dependence. European Journal of Sport Science. 2011;11(4):269–276. doi: 10.1080/17461391.2010.509889. [DOI] [Google Scholar]
- Maruyama A., Macdonald S., Borycki E., Zhao J. Hypertension, chronic obstructive pulmonary disease, diabetes and depression among older methadone maintenance patients in British Columbia. Drug and Alcohol Review. 2013;32(4):412–418. doi: 10.1111/dar.12031. [DOI] [PubMed] [Google Scholar]
- McGowan J., Sampson M., Salzwedel D.M., Cogo E., Foerster V., Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. Journal of Clinical Epidemiology. 2016 doi: 10.1016/j.jclinepi.2016.01.021. [DOI] [PubMed] [Google Scholar]
- McLellan A.T., Lewis D.C., O'Brien C.P., Kleber H.D. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. Journal of the American Medical Association. 2000;284(13):1689–1695. doi: 10.1001/jama.284.13.1689. http://www.ncbi.nlm.nih.gov/pubmed/11015800 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Miller W.R., Walters S.T., Bennett M.E. How effective is alcoholism treatment in the United States? Journal of Studies on Alcohol. 2001;62(2):211–220. doi: 10.15288/jsa.2001.62.211. http://www.ncbi.nlm.nih.gov/pubmed/11327187 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Murphy T.J., Pagano R.R., Marlatt G.A. Lifestyle modification with heavy alcohol drinkers: Effects of aerobic exercise and meditation. Addictive Behaviors. 1986;11(2):175–186. doi: 10.1016/0306-4603(86)90043-2. http://www.ncbi.nlm.nih.gov/pubmed/3526824 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Oaten M., Cheng K. Longitudinal gains in self-regulation from regular physical exercise. British Journal of Health Psychology. 2006;11(4):717–733. doi: 10.1348/135910706X96481. [DOI] [PubMed] [Google Scholar]
- Peacock A., Leung J., Larney S., Colledge S., Hickman M., Rehm J. Global statistics on alcohol, tobacco and illicit drug use: 2017 status report. Addiction. 2018. October 1. Blackwell Publishing Ltd. [DOI] [PubMed]
- Popay J., Roberts H., Sowden A., Petticrew M., Arai L., Rodgers M. Guidance on the conduct of narrative synthesis in systematic reviews: A product from the ESRC methods programme. Lancaster. 2006. http://www.lancs.ac.uk/shm/research/nssr/research/dissemination/publications/NS_Synthesis_Guidance_v1.pdf Retrieved from.
- Public Health England Alcohol treatment in England 2012-13. 2013. http://www.nta.nhs.uk/uploads/alcohol2012-13.pdf Retrieved from.
- Public Health England Drug treatment in England 2013-2014. 2014. http://www.nta.nhs.uk/uploads/drug-treatment-in-england-2013-14-commentary.pdf London. Retrieved from.
- Public Health England Health profile for England. 2017. https://www.gov.uk/government/publications/health-profile-for-england Retrieved from.
- Ramo D.E., Brown S.A. Classes of substance abuse relapse situations: A comparison of adolescents and adults. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors. 2008;22(3):372–379. doi: 10.1037/0893-164X.22.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawson R., Chudzynski J., Gonzales-Castaneda R., Ang A., Dickerson D., Mooney L. Impact of an exercise intervention on methamphetamine use outcomes post residential treatment care. Drug and Alcohol Dependence. 2015 doi: 10.1016/j.drugalcdep.2015.07.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy S., Dick A.M., Gerber M.R., Mitchell K. The effect of a yoga intervention on alcohol and drug abuse risk in veteran and civilian women with posttraumatic stress disorder. Journal of Alternative & Complementary Medicine. 2014;20(10):750. doi: 10.1089/acm.2014.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J., Shield K.D. January 1). Global burden of disease and the impact of mental and addictive disorders. Current Psychiatry Reports. Current Medicine Group LLC. 2019;1 doi: 10.1007/s11920-019-0997-0. [DOI] [PubMed] [Google Scholar]
- Roessler K.K., Bramsen R.H., Dervisevic A., Bilberg R. Exercise based interventions for alcohol use disorder: A comment on motivational aspects of participation. Scandinavian Journal of Psychology. 2017;58(1):23–28. doi: 10.1111/sjop.12334. [DOI] [PubMed] [Google Scholar]
- Roessler K.K., Bilberg R., Sogaard Nielsen A., Jensen K., Ekstrom C.T., Sari S. Exercise as adjunctive treatment for alcohol use disorder: A randomized controlled trial.(research article)(report) PloS One. 2017;12(10) doi: 10.1371/journal.pone.0186076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez V., Moore C.F., Brunzell D.H., Lynch W.J. Effect of wheel-running during abstinence on subsequent nicotine-seeking in rats. Psychopharmacology. 2013;227(3):403–411. doi: 10.1007/s00213-012-2964-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott K.A., Myers A.M. Impact of fitness training on native adolescents' self-evaluations and substance use. Canadian Journal of Public Health. 1988;79(6):424–429. [PubMed] [Google Scholar]
- Shaffer H.J., Lasalvia T.A., Stein J.P. Comparing hatha yoga with dynamic group psychotherapy for enhancing methadone maintenance treatment: A randomized clinical trial. Alternative Therapies in Health & Medicine. 1997;3(4):57. [PubMed] [Google Scholar]
- Simonton A.J., Young C.C., Johnson K.E. Physical activity interventions to decrease substance use in youth: a review of the literature. Substance Use & Misuse. 2018;53(12):2052–2068. doi: 10.1080/10826084.2018.1452338. [DOI] [PubMed] [Google Scholar]
- Sinyor D., Brown T., Rostant L., Seraganian P. The role of a physical fitness program in the treatment of alcoholism. Journal of Studies on Alcohol. 1982;43(3):380–386. doi: 10.15288/jsa.1982.43.380. http://www.ncbi.nlm.nih.gov/pubmed/7121004 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Smith M.A., Lynch W.J. The neurobiology of exercise and drug-seeking behaviour. In: Ekkekakis P., editor. Handbook on physical activity and mental health. Routledge; New York: 2013. [Google Scholar]
- Sobell L.C., Sobell M.B. Measuring alcohol consumption. Humana Press; Totowa, NJ: 1992. Timeline follow-back; pp. 41–72. [DOI] [Google Scholar]
- Sterne J.A., Hernán M.A., Reeves B.C., Savović J., Berkman N.D., Viswanathan M. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stinson F.S., Grant B.F., Dawson D.A., Ruan W.J., Huang B., Saha T. Comorbidity between DSM-IV alcohol and specific drug use disorders in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Drug and Alcohol Dependence. 2005;80(1):105–116. doi: 10.1016/j.drugalcdep.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Taylor A.H. Multiple behaviour change. In: Eklind R.C., Tenenbaum G., editors. Vol. 2. Sage; Thousand Oaks; CA: 2014. pp. 492–494. (Encyclopedia of sport and exercise psychology). [Google Scholar]
- Taylor A.H., Faulkner G. Evidence and theory into practice in different health care contexts: A call for more translational science. Mental Health and Physical Activity. 2014;7(1):1–5. doi: 10.1016/j.mhpa.2013.06.007. [DOI] [Google Scholar]
- Taylor A.H., Oh H., Cullen S. Acute effect of exercise on alcohol urges and attentional bias towards alcohol related images in high alcohol consumers. Mental Health and Physical Activity. 2013;6(3):220–226. doi: 10.1016/j.mhpa.2013.09.004. [DOI] [Google Scholar]
- Thanos P.K., Stamos J., Robison L.S., Heyman G., Tucci A., Wang G.-J. Daily treadmill exercise attenuates cocaine cue-induced reinstatement and cocaine induced locomotor response but increases cocaine-primed reinstatement. Behavioural Brain Research. 2013;239:8–14. doi: 10.1016/j.bbr.2012.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Centre for Social Justice . 2013. No Quick Fix: Exposing the depth of Britain's drugs and alcohol problem. (London) [Google Scholar]
- The National Treatment Agency for Substance Misuse Why invest? How drug treatment and recovery services work for individuals. Communities and Society. 2012 http://www.nta.nhs.uk/uploads/whyinvest2final.pdf London. Retrieved from. [Google Scholar]
- Thompson T.P., Lambert J.D., Greaves C.J., Taylor A.H. Intervention delivery fidelity assessment of a counseling-based intervention for promoting smoking reduction and increasing physical activity. Health Psychology. 2018;37(7):627–637. doi: 10.1037/hea0000613. [DOI] [PubMed] [Google Scholar]
- Thompson T.P., Taylor A.H., Wanner A., Husk K., Wei Y., Creanor S. Physical activity and the prevention, reduction, and treatment of alcohol and/or substance use across the lifespan (the PHASE review): Protocol for a systematic review. Systematic Reviews. 2018;7(1):9. doi: 10.1186/s13643-018-0674-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trivedi M.H., Greer T.L., Rethorst C.D., Carmody T., Grannemann B.D., Walker R. Randomized controlled trial comparing exercise to health education for stimulant use disorder: Results from the CTN-0037 STimulant Reduction Intervention Using Dosed Exercise (STRIDE) Study. Journal of Clinical Psychiatry. 2017;78(8):1075–1082. doi: 10.4088/JCP.15m10591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime World drug report 2012. 2012. http://www.unodc.org/documents/data-and-analysis/WDR2012/WDR_2012_web_small.pdf New York. Retrieved from.
- Ussher M.H., Faulkner G.E.J., Angus K., Hartmann-Boyce J., Taylor A.H. Cochrane database of systematic reviews. John Wiley and Sons Ltd; 2019. Exercise interventions for smoking cessation. October 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velicer W., Redding C., Paiva A., Mauriello L., Blissmer B., Oatley K. Multiple behavior interventions to prevent substance abuse and increase energy balance behaviors in middle school students. Practice, Policy, Research. 2013;3(1):82–93. doi: 10.1007/s13142-013-0197-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N.D. Physical activity may prevent substance abuse. 2011. http://www.drugabuse.gov/news-events/nida-notes/2011/03/physical-activity-may-prevent-substance-abuse from.
- Wang D., Wang Y., Wang Y., Li R., Zhou C. Impact of physical exercise on substance use disorders: A meta-analysis. PloS One. 2014;9(10) doi: 10.1371/journal.pone.0110728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstock J., Barry D., Petry N.M. Exercise-related activities are associated with positive outcome in contingency management treatment for substance use disorders. Addictive Behaviors. 2008;33(8):1072–1075. doi: 10.1016/j.addbeh.2008.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstock J., Capizzi J., Weber S.M., Pescatello L.S., Petry N.M. Exercise as an intervention for sedentary hazardous drinking college students: A pilot study. Mental Health and Physical Activity. 2014;7(1):55–62. doi: 10.1016/j.mhpa.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstock J., Petry N.M., Pescatello L.S., Henderson C.E. Sedentary college student drinkers can start exercising and reduce drinking after intervention. Psychology of Addictive Behaviors. 2016 doi: 10.1037/adb0000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werch C., Moore M., DiClemente C.C., Owen D.M., Jobli E., Bledsoe R. A sport-based intervention for preventing alcohol use and promoting physical activity among adolescents.(Research Papers) Journal of School Health. 2003;73(10):380. doi: 10.1111/j.1746-1561.2003.tb04181.x. [DOI] [PubMed] [Google Scholar]
- World Health Organisation Global status report on alcohol and health. 2011. http://www.who.int/substance_abuse/publications/global_alcohol_report/msbgsruprofiles.pdf Geneva. Retrieved from.
- World Health Organisation Global status report on alcohol and health 2014. 2014. http://www.who.int/substance_abuse/publications/global_alcohol_report/msb_gsr_2014_1.pdf?ua=1 Geneva. Retrieved from.
- World Health Organisation WHO | Physical activity. WHO. 2017. http://www.who.int/topics/physical_activity/en/ Retrieved from.
- Xie H., McHugo G.J., Fox M.B., Drake R.E. Substance abuse relapse in a ten-year prospective follow-up of clients with mental and substance use disorders. Psychiatric Services. 2005;56(10):1282–1287. doi: 10.1176/appi.ps.56.10.1282. [DOI] [PubMed] [Google Scholar]
- Zschucke E., Heinz A., Strohle A. Exercise and physical activity in the therapy of substance use disorders. Science World Journal. 2012 doi: 10.1100/2012/901741. [DOI] [PMC free article] [PubMed] [Google Scholar]