Abstract
When SARS-CoV-2 emerged at the end of 2019, no approved therapeutics or vaccines were available. An urgent need for countermeasures during this crisis challenges the current paradigm of traditional drug discovery and development, which usually takes years from start to finish. Approaches that accelerate this process need to be considered. Here we propose the minimum data package required to move a compound into clinical development safely. We further define the additional data that should be collected in parallel without impacting the rapid path to clinical development. Accelerated paths for antivirals, immunomodulators, anticoagulants, and other agents have been developed and can serve as “roadmaps” to support prioritization of compounds for clinical testing. These accelerated paths are fueled by a skewed risk-benefit ratio and are necessary to advance therapeutic agents into human trials rapidly and safely for COVID-19. Such paths are adaptable to other potential future pandemics.
The global COVID19 pandemic underscores the urgent need for an accelerated path for drug discovery and development. In this Perspective, Grobler et al. outline roadmaps to support prioritization of the most promising therapeutic agents while ensuring clinical safety.
Introduction
In late 2019, a cluster of severe respiratory disease cases occurred in Wuhan, China (Hubei Daily, Reporter Yu Jinyi, 2019; World Health Organization, 2020c). By January 2020, a novel coronavirus was sequenced, human-to-human transmission was clearly documented (Centers for Disease Control and Prevention, 2020; Riou and Althaus, 2020), and additional cases caused by the same virus, now known as SARS-CoV-2, were identified in other countries, resulting in the identification of a new disease syndrome, COVID-19 (Arshad Ali et al., 2020; Munster et al., 2020; World Health Organization, 2020a, 2020b). As the virus continued to spread, resources were deployed rapidly to identify and develop prophylactic and therapeutic agents for patients. However, these initial activities were uncoordinated, leading to haphazard testing of non-optimal or potentially harmful interventions. One reason for the lack of coordination was the lack of an infrastructure and well-vetted guidelines to facilitate optimized drug testing during a global pandemic.
Without access to approved therapeutics, repurposing of agents by physicians for use in COVID-19 started soon after the initial virus outbreak. Drugs were chosen based on varying criteria, but use was empirical in nature and based on limited or no data on effectiveness against SARS-CoV-2 or COVID-19 disease sequelae. Agents such as hydroxychloroquine were tested based on evidence of a positive effect in a single non-human cell line assay (Liu et al., 2020). Additionally, antivirals used to treat other viral infections, such as HIV protease inhibitors (ritonavir and lopinavir), were tested without strong rationale or evidence to support their use against this new coronavirus (Musarrat et al., 2020; Wang, et al., 2020c; Yao et al., 2020). It is now clear, given results from randomized controlled clinical studies, that the vast majority of these approaches were not fruitful (Cao et al., 2020; Şimsek Yavuz and Ünal, 2020; Yao et al., 2020). This highlights the need for a coordinated, systematic approach to identify the most promising potential antiviral agents now and in the event of future pandemic threats.
After the early, hectic drug-testing period, well-controlled studies have focused on drugs with a stronger rationale to support their use. Among antiviral therapies that have been advanced for repurposing are the nucleos(t)ides remdesivir, favipiravir, galdesivir, AT-527, and EIDD-2801, which exhibit broad antiviral activity against multiple RNA viruses (Good et al., 2020; Jordan et al., 2018; Mulangu et al., 2019; Sheahan et al., 2017; Sheahan et al., 2020; Taylor et al., 2016; Toots et al., 2019). All have shown potent antiviral activity against SARS-CoV-2 in cell-based infection assays at drug levels either known or modeled to be achievable in humans. Of these, remdesivir has received an emergency use authorization (EUA) for COVID-19 treatment (Bose et al., 2020). Additionally, immunomodulatory agents such as IL-6 receptor antagonists (tocilizumab, sarilumab, olokizumab), IL-1 receptor antagonists (Anakinra [Kinaret]), Janus kinase inhibitors (baricitinib [Olumiant]; ruxolitinib), and Bruton tyrosine kinase (BTK) inhibitors (ibrutinib), all developed for other disease indications, are in clinical trials for COVID-19 (Maes et al., 2020; Picchianti Diamanti et al., 2020; Roschewski et al., 2020; Yeleswaram et al., 2020). Other immunomodulatory drugs such as dexamethasone, which has to date shown the best efficacy in severely/critically ill patients, have been advanced (Ledford, 2020; Horby et al., 2020), as have supportive therapies (e.g., complement-targeted therapeutics and anti-coagulants; Jodele and Köhl, 2020; Watson et al., 2020).
Following this initial wave of agents entering the clinic, there is a clear need to continue to accelerate identification of safe and more effective agents to expand the options for treatment of COVID-19 during the different stages of disease pathogenesis. Discovery and development of new drugs to treat or prevent infection typically takes many years. Timelines for traditional approaches, predicated on an understanding of the disease and the life cycle of the pathogen, exceed those required to address the urgency demanded by the current COVID-19 pandemic. The severity of this pandemic from both global health and economic perspectives has forced the field to re-imagine repurposing of approved or advanced agents for other indications and to accelerate discovery and development of novel agents. Rapid and effective repurposing of approved or advanced clinical agents is ideally coordinated across the healthcare industry to progress those with the greatest potential to treat the disease. A coordinated effort would provide a framework for prioritizing the most promising agents to advance into clinical studies, maximize collection of key safety and efficacy data, and conserve resources by focusing on agents with the greatest likelihood of clinical benefit. Since repurposed compounds were not optimized for treatment of COVID-19, a clearly defined and harmonized set of criteria for preclinical biological activity from standard preclinical assays and models is required to support prioritization for clinical studies.
It was against this backdrop that the Accelerating COVID-19 Therapeutics Interventions and Vaccines (ACTIV) public-private partnership was formed, focused on preclinical and clinical therapeutics, vaccines, and clinical trial capacity (Collins and Stoffels, 2020). The ACTIV preclinical working group has defined streamlined pathways and criteria for biological evaluation in standard preclinical assays and models of repurposed molecules in “pandemic response mode” to support their consideration for clinical development for COVID-19. Separate pathways for antiviral, immunomodulatory, anti-coagulative, and anti-complement approaches are presented here as a framework to help investigators seeking rapid solutions for COVID-19 treatment to prioritize compounds for limited preclinical and/or clinical resources.
Crisis Mode for Compound Identification and Development Versus Traditional Drug Discovery
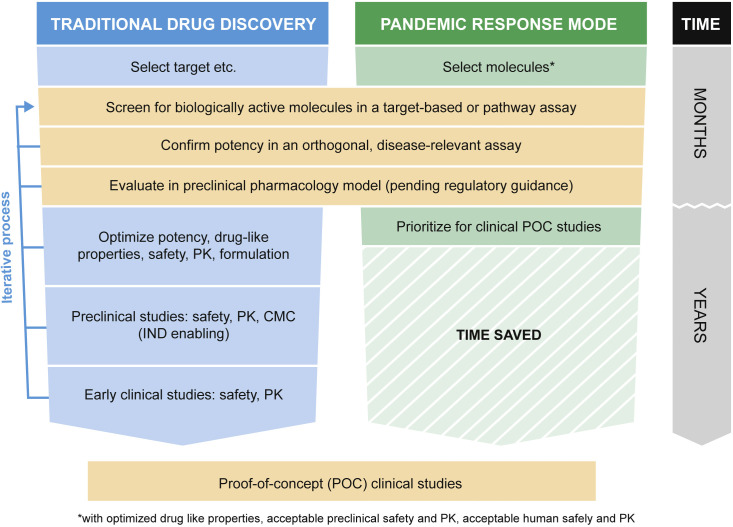
The urgency to make life-saving treatments for COVID-19 available precludes traditional drug discovery paths, given their typically protracted timelines. Traditional drug discovery is an iterative, multi-step process to identify compounds with properties that support their potential for clinical benefit (Figure 1 ). Target selection is based on an understanding of the underlying biology and usually requires validation as well as a tractable means to modify the activity of the target. In the case of drugs to treat viral infections including SARS-CoV-2, targets may include either virus or host targets with the potential to block virus infection or viral replication or to modulate the host response to infection. Demonstration of potent activity against the target is usually a starting point and is followed by lead compound optimization. This is an iterative process aimed at maximizing selectivity (no off-target activity), improving pharmacokinetic and pharmacodynamic (PK/PD) properties, minimizing potential safety and tolerability issues, and improving physical properties and stability that enable appropriate formulation. Evaluation of potency, PK, and safety are typically done sequentially—there is no reason to start resource-intensive PK studies on a compound until its potential to exert the desired biological effect is demonstrated. Demonstration of potency in a preclinical pharmacology model gives further confirmation of mechanism for antivirals and is critical to the demonstration of efficacy for systemic targets or pathways. A compound is advanced into early-stage human clinical studies only when it meets all the criteria for potency, PK/PD, safety, tolerability, and formulation. Compounds can and do fail at all stages of lead optimization; when they do, the process regresses back to the next most advanced compound in this screening funnel.
Figure 1.
Comparison of the Processes for Traditional Drug discovery and Pandemic Response Mode
A more rapid approach than traditional drug discovery and development, and one better suited for a pandemic response, is accelerated repurposing. For COVID-19 treatment, this repurposing involves identification and clinical evaluation of an approved or advanced clinical candidate that there is reason to believe has potential for use in treatment and for which there is experience demonstrating clinical PK/PD, safety, and tolerability to support testing. Such compounds include not only approved compounds but also those with completed phase 1 trials (post-multi-dose phase) for another indication, those in late stages of clinical development, and those that have not gained approval because of lack of efficacy in a previously tested indication but which nevertheless have preclinical and clinical data supportive of repurposing. The number of compounds that can effectively be repurposed is limited due to the typically high selectivity of drugs for their intended targets. The most likely candidates are those with activity against related targets and those that target a host response that impacts disease. While limited in number, they are worth pursuing given the potential to rapidly impact the course of the pandemic. Figure 1 outlines such an approach, whereby in rapid repurposing for pandemic response, compounds that require only a demonstration of disease-relevant activity are examined prior to nomination for clinical development, since PK and minimum safety have already been established in humans or at minimum in a preclinical species. Additionally, for those agents already in or beyond clinical development, the existence of an adequate clinical drug supply can again accelerate the timeline to testing in pandemic disease clinical trials and ensure subsequent access for patients. There is significant time saved from this rapid repurposing mode, which requires only months to generate the data necessary to support clinical trial nomination rather than years, as in the traditional drug discovery approach. Remdesivir is an example of an agent that was identified in such a manner. Clinical data for PK and safety already existed from clinical trials testing the compound against Ebola virus (Mulangu et al., 2019; Warren et al., 2016). In vitro assessment of anti-SARS-CoV-2 activity was generated rapidly and supported immediate clinical studies for COVID-19 treatment (Wang et al., 2020a; Wang et al., 2020b). The time to test remdesivir activity in vitro against SARS-CoV-2 to first emergency-use FDA approval for COVID-19 was only three months. However, it must be noted that remdesivir activity had already been demonstrated against other coronavirus family members prior to the emergence of SARS-CoV-2 (Sheahan et al., 2017), which likely accelerated its testing and EUA approval (Bose et al., 2020).
COVID-19 Disease and Opportunities for Intervention
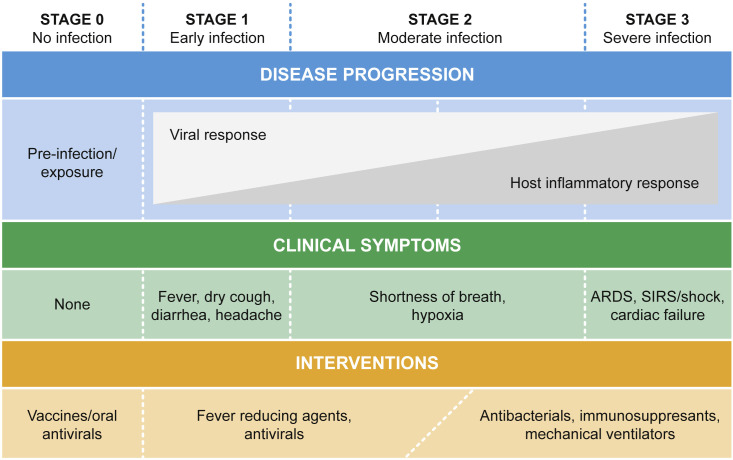
COVID-19 is characterized by four stages with distinct symptoms that increase in severity as the disease progresses (Alsuliman et al., 2020; Cascella et al., 2020; Jin et al., 2020; Wu and McGoogan, 2020; Figure 2 ). The spectrum of clinical signs and symptoms observed across the disease stages demonstrates the likely requirement for distinct interventions. The earlier the intervention, the greater the impact will be on disease severity and outcomes. In fact, stage 0, where there is no infection, is the ideal point of intervention with vaccines or antiviral agents (e.g., neutralizing antibodies) administered prophylactically.
Figure 2.
COVID-19: Stages, Symptoms, and Potential Treatments
Early infection (stage 1) is characterized by fever, dry cough, gastrointestinal symptoms, and headache that are similar to those manifested by many other viral infections (Alsuliman et al., 2020; Cascella et al., 2020; Jin et al., 2020; Wu and McGoogan, 2020). Orally or subcutaneously administered antiviral agents and symptomatic treatments likely will have the greatest impact in early infection. Drugs that are ideally suited for this stage are those that can be administered in an outpatient setting, as few patients in this group are hospitalized with severe symptoms.
Host inflammatory responses are a hallmark of severe infection that manifests in the later stages of COVID-19 disease and are characterized by a massive production of cytokines and damage to host tissues (Moore and June, 2020; Ye et al., 2020). Stage 2 is characterized by lung inflammation causing hypoxia and shortness of breath, which may or may not require oxygen supplementation (Alsuliman et al., 2020; Cascella et al., 2020; Jin et al., 2020; Wu and McGoogan, 2020). Stage 3, the most severe stage, is a hyperinflammatory state characterized by acute respiratory distress syndrome (ARDS), systemic inflammatory response syndrome (SIRS)/Shock, coagulation disorders, and cardiac failure (Alsuliman et al., 2020; Cascella et al., 2020; Jin et al., 2020; Wu and McGoogan, 2020). Once this hyperinflammatory state is triggered, it is unlikely that antiviral treatments alone will be sufficient to impact disease; thus, immunomodulatory agents that target these responses are necessary. Selection of agents to use in these later stages should be based on clear evidence implicating the target in one or more of the later stages of COVID-19 disease. Patients in stages 2 and 3 likely require treatment with agents that target the host inflammatory response and other disease processes, such as coagulation, in addition to antivirals.
Considerations around pharmacological profile, route and frequency of administration, and safety and tolerability of the interventions vary across disease stage and the nature of the intervention. Antivirals for use broadly in prophylaxis or treatment of early infection should ideally have a high barrier to the development of resistance, a simple regimen that maximizes patient adherence, and acceptable safety and tolerability for otherwise healthy individuals. For treatment of more severe infection in a hospital setting, there is considerably more flexibility with regards to route of administration and frequency, as parenteral administration is viable and reliance on the patient for adherence is less of an issue. For the sickest patients, compounds with less than ideal safety and tolerability profiles may have a place if their potential benefit outweighs possible liabilities.
Blueprints for Pandemic Response Agents
Antivirals
Antiviral agents that target either a viral protein or a host protein required for viral replication or pathology are effective against other viral pathogens (e.g., HIV, HCV, and Ebola). Therefore, this approach will also likely play an essential role in the COVID-19 treatment toolbox. Viral targets provide the advantage of specificity and being readily validated in vitro, and direct-acting antiviral agents typically exhibit good correlation between in vitro activity and clinical response if appropriate pharmacokinetic/safety levels are achieved, abrogating the need for preclinical pharmacology model data to support advancement to clinical studies. Selective drugs that target a viral protein also provide the potential to mitigate off-target activities that can lead to tolerability or safety issues, as they do not target a host function. One liability of direct-acting antivirals when used as monotherapies is the potential development of resistance that diminishes drug potency and that can emerge due to the inherent high viral mutation rate and viral genome plasticity. Certainly, some direct-acting antivirals have a high barrier to resistance, but the propensity to generate resistance should be determined in parallel with development activities during a pandemic response mode.
SARS-CoV-2 expresses several proteins that would be amenable to targeting by small-molecule antivirals. These include the RNA-dependent RNA polymerase, proteases, helicase, and membrane proteins such as the spike protein. Effective treatments that block viral replication of other viral pathogens that act by inhibiting similar targets are obvious candidates for evaluation as potential repurposed agents for use in COVID-19 treatment so long as there is a sufficient similarity to the target in SARS CoV-2. Host encoded proteins, such as proteases or kinases used by SARS-CoV-2, can also be attractive antiviral targets (Bouhaddou et al., 2020; Hoffmann et al., 2020a, 2020b).
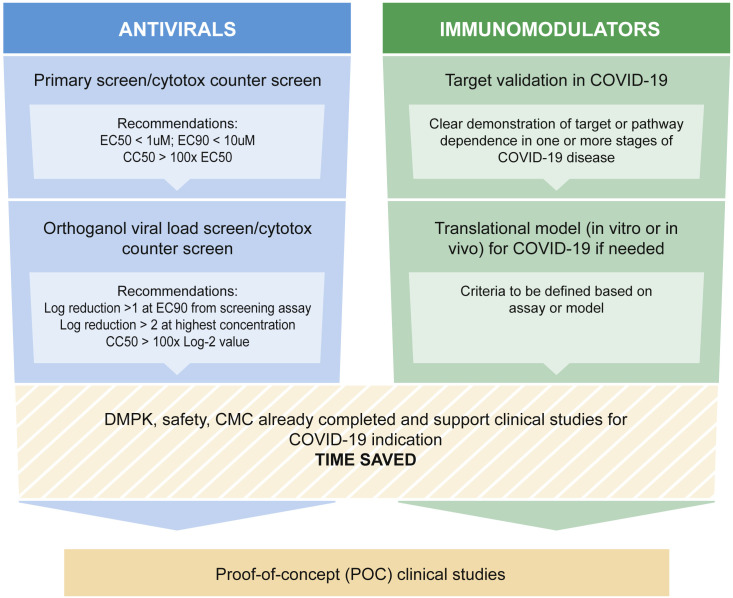
The accelerated preclinical development plan for clinical agents repurposed as SARS CoV-2 antivirals during the pandemic is shown in Figures 3 and S1. The premise of this streamlined plan is that only some preclinical activities are required during pandemic response mode; other activities that are also normally required at this stage of traditional drug development can be deferred and conducted in parallel with the clinical study. For COVID-19 repurposing of a clinical development stage or marketed compound, demonstration of its antiviral activity against SARS CoV-2 in cell-based assays in vitro is an essential step. There are multiple primary screening assays that differ in ways that may or may not impact the measurement of potency, including the form of the virus (e.g., full-length wild-type, reporter viruses, or sub-genomic replicons, etc.) and the cell line used (e.g., Vero cells). It is therefore essential that adequate control compounds with well-characterized antiviral activity be included as comparators to assess relative potency. Currently, the recommended reference compound is remdesivir, though the potency of this molecule depends on cellular enzymes to phosphorylate the prodrug and thus potency values vary from cell line to cell line (Eastman et al., 2020). Compounds that exhibit adequate potency in the primary assay—for example, EC90 < 10 μM—and an appropriate selectivity index—for example, CC50/EC50 > 100—should be tested in orthogonal assays to evaluate impact of virus production. When cytopathic effect is the basis for the primary screen, the orthogonal screen should demonstrate a direct activity on reducing viral load with a potency at least 100-fold higher than cytotoxicity. Additionally, for host-targeting antivirals, at least one of the two required assays should be performed with human cells, ideally primary human airway epithelial cells, stem-cell-derived organoids, or other translationally relevant human cell systems, to confirm that antiviral activity is maintained when targeting human proteins in a relevant cell type.
Figure 3.
Blueprints for Pandemic Response Mode for Antivirals and Immunomodulators for COVID-19
Critical to moving antivirals forward to the clinic is demonstration of adequate exposure of the compound in the target tissue (i.e., lungs) to achieve efficacy based on cell-based or animal model data. For antivirals in pandemic response mode, especially direct-acting antivirals, preclinical efficacy data may not be needed to enter the clinic. Such data should only be gating to human trials upon regulatory authority requirement or if there is a question of translatability of host-targeting antivirals from cellular to in vivo activity. In vivo efficacy data can also be useful for prioritizing agents for advanced clinical trials.
Immunomodulators
Stages 2 and 3 of COVID-19 are marked by increased host inflammatory response culminating in a hyperinflammation state in stage 3 that is life-threatening (Alsuliman et al., 2020; Jin et al., 2020). Indeed, hypercytokinemia is a hallmark of severe COVID-19 (Moore and June, 2020; Ye et al., 2020). Interestingly, delayed type I interferon responses also may contribute to disease progression, as they can delay optimal induction of the adaptive immune response (Hadjadj et al., 2020). The hypercytokinemia of stage 3 includes increased levels of proinflammatory cytokines IL-1β, IL1 Ra, IL-6, TNF-α and sIL2-Ra, and it often occurs despite diminishing viral load in patients (Moore and June, 2020; Ye et al., 2020). Thus, a number of potential targets for immunomodulation have the potential to impact COVID-19 disease progression.
The accelerated preclinical development plan for clinical agents repurposed as COVID-19 immunomodulators during the pandemic is shown in Figures 3 and S2. Unlike for antivirals, the target or pathway validation to confirm that a specific immunomodulatory intervention will have an impact on COVID-19 is much more challenging. Given the uncertain fidelity of translational preclinical pharmacology models for human disease, the validation likely will come from strong correlations in disease progression and outcome in humans. However, if such validation is not available, activity in a non-human primate model of COVID-19 is warranted prior to nomination for clinical development (Figure S2).
Following target validation, activity of an agent in a translational model, whether it be in vitro or in vivo, is critical to support nomination of clinical assessment in COVID-19. Most likely, any current clinical-stage or marketed compounds already will have such data, as it would have been a critical component of the original data package supporting clinical investigation in the originating disease indication. For this reason, some of the most advanced agents currently in clinical trials for COVID-19 are immunomodulatory agents whose targets have strong clinical association with COVID-19 disease progression—such as those targeting IL-6, including sarilumab, tocilizumab, siltuximab, clazakizumab, and sirukumab (Buonaguro et al., 2020; ClinicalTrials.gov, 2020; Fu et al., 2020; Guaraldi et al., 2020; Palanques-Pastor et al., 2020; Vaidya et al., 2020; Xu et al., 2020).
Additional Therapeutic Profiles
In addition to antivirals and immunomodulators, there are other therapeutic profiles that may be important to treat COVID-19. Notably, there is a marked increase in complement activation in severe disease. An increase in coagulopathy as indicated by elevated titers of D-dimers, thrombocytopenia, and blood clots in small vessels of all organs with disseminated intravascular coagulation has also been noted (Carvelli et al., 2020). As the understanding of the natural history of COVID-19 disease increases, additional findings will highlight the need for alternate types of therapeutic agents. The accelerated preclinical development plan for anti-complement and anti-coagulant therapies repurposed for COVID-19 during the pandemic is shown in Figure S3. Since many of these disease processes are associated with previously identified clinical conditions, therapeutics to address them are either already in clinical development or are marketed drugs. Thus, clinical trials to identify their efficacy for COVID-19 will be gated by the validation of the biological condition promoting poor outcomes for COVID-19 patients and thus supporting investigation of clinical intervention with these agents.
Conclusion
The emergence of the COVID-19 global pandemic caused by SARS-CoV-2 is a crisis in which response requires immediate action, including adaptation of the drug discovery and development process to speed quality agents into clinical trials. These new processes require gating criteria to include only those sets of data absolutely required to ensure translational activity with acceptable pharmacokinetics and safety via the intended route of administration. Additional, non-gating data such as target identification, mechanism of action, and combination evaluation for all agents, as well as resistance profiling and expanded antiviral profiling for antiviral agents, will also be important to obtain. These assays should be done in parallel to the gating criteria and in a less urgent manner. Assessment of resistance potential for antivirals, while not gating and variable in risk from agent to agent, should be determined rapidly as these agents move through clinical development. This will preclude prioritizing an agent with high resistance potential over others with less resistance potential. To provide the best therapeutic options, multiple validated mechanisms should be pursued. The blueprints for defined therapeutic agent assessment presented here outline the critical data needed to most rapidly and efficiently evaluate and prioritize agents for clinical development for COVID-19.
Hopefully, as therapeutic and prophylactic compounds and vaccines are approved for COVID-19, there will be a continuing effort for pandemic preparedness, which will discover and develop broadly active, potent therapeutics for many families of viruses with pandemic potential. Should such efforts not provide approved agents for a future pandemic, the principles described here could be adapted to generate blueprints for crisis mode drug discovery to address that pandemic.
To determine the best agents to prioritize for clinical trials, data must be of high quality and generated in standardized assays, or at minimum with robust and universally adopted controls that allow accurate comparison of potency. Dose-response assessment of all agents should be determined, and the datasets and analyses presented for prioritization rather than simply using a derived EC50 or EC90 number. The best practice is to include all known robust positive controls for the assay with each run such that relative potency can be compared from assay to assay to compensate for changes in protocol, cell adaptations, and other confounding variables from run to run and laboratory to laboratory. For antivirals against SARS-CoV-2, at a minimum, inclusion of remdesivir is recommended for in vitro assays. For best comparison, key assays should follow standardized protocols published and accepted by the global community. Additionally, for select profiles such as immunomodulators and in all cases requested by regulators, in vivo efficacy data in an appropriate model (see accompanying article by Hewitt et al., 2020) is essential. Indeed, though potentially unnecessary to start clinical assessment, such data is a selection criteria for consideration by networks such as the ACTIV clinical trials prioritization group. All data generated to support clinical development of agents should be made publicly available during pandemic crises to facilitate optimal learning and advancement in the shortest time frame.
Not addressed here, but critical to rapid response in a crisis mode, is availability of clinical drug supply. Most likely, the first agents to move to the clinical prioritization during a pandemic crisis will be molecules with sufficient potency, PK, and safety to provide therapeutic options until more potent compounds can be identified. There should also be sufficient amount of clinical drug supply on hand to support clinical trials. If not, accelerated paths to produce this clinical-grade material are mandatory. Additionally, commercial-scale manufacturing of any agent entering clinical trials must be established in parallel to the execution of the clinical trials to ensure adequate supplies are available to treat patients upon product approval, even though these efforts require a significant at-risk, front-loaded investment in material that may not be used for COVID-19 unless the product is approved.
The COVID-19 pandemic is a public health crisis due to the lack of vaccines and therapeutics developed ahead of time for preparedness. The problem has been compounded by the need to define, coordinate, and execute an accelerated response in the face of a rapidly spreading and deadly human pathogen. Use of the blueprints presented here can lead to optimal compound prioritization of potential therapeutics to address all known stages of COVID-19 as well as any other disease aspects that remain to be defined.
Acknowledgments
This work was done on behalf of the ACTIV Preclinical Working Group (https://www.nih.gov/research-training/medical-research-initiatives/activ/preclinical-working-group). We thank Nataliya Natasha Kushnir (Pfizer) for help with referencing and Katinka Vigh-Conrad for assistance with figures.
Declaration of interests
Authors of the manuscript are members of ACTIV Preclinical Working group. Jay A Grobler is a shareholder in Merck. Annaliesa S Anderson is an employee of Pfizer, receives a salary from Pfizer and may own Pfizer stock; she is also a non-salaried member of the Contrafect Scientific Advisory Board. Michael S. Diamond is a consultant for Inbios, Vir Biotechnology, and NGM Biopharmaceuticals and is on the Scientific Advisory Board of Moderna and Immunome. The Diamond laboratory has received unrelated funding support in sponsored research agreements from Moderna, Vir Biotechnology, and Emergent BioSolutions. John A.T. Young is an employee and shareholder of F.Hoffmann-La Roche, Ltd. Kara Carter is on the Scientific Advisory Board for the Alabama Drug Discovery and Development Consortium and owns stock in Evotec and Celldex Therapeutics.
Footnotes
Supplemental Information can be found online at https://doi.org/10.1016/j.chom.2020.09.017.
Supplemental Information
References
- Alsuliman T., Alasadi L., Alkharat B., Srour M., Alrstom A. A review of potential treatments to date in COVID-19 patients according to the stage of the disease. Curr. Res. Transl. Med. 2020;68:93–104. doi: 10.1016/j.retram.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arshad Ali S., Baloch M., Ahmed N., Arshad Ali A., Iqbal A. The outbreak of Coronavirus Disease 2019 (COVID-19)-An emerging global health threat. J. Infect. Public Health. 2020;13:644–646. doi: 10.1016/j.jiph.2020.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bose S., Adapa S., Aeddula N.R., Roy S., Nandikanti D., Vupadhyayula P.M., Naramala S., Gayam V., Muppidi V., Konala V.M. Medical Management of COVID-19: Evidence and Experience. J. Clin. Med. Res. 2020;12:329–343. doi: 10.14740/jocmr4201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouhaddou M., Memon D., Meyer B., White K.M., Rezelj V.V., Correa Marrero M., Polacco B.J., Melnyk J.E., Ulferts S., Kaake R.M. The Global Phosphorylation Landscape of SARS-CoV-2 Infection. Cell. 2020;182:685–712.e19. doi: 10.1016/j.cell.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buonaguro F.M., Puzanov I., Ascierto P.A. Anti-IL6R role in treatment of COVID-19-related ARDS. J. Transl. Med. 2020;18:165. doi: 10.1186/s12967-020-02333-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao B., Wang Y., Wen D., Liu W., Wang J., Fan G., Ruan L., Song B., Cai Y., Wei M. A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N. Engl. J. Med. 2020;382:1787–1799. doi: 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvelli J., Demaria O., Vely F., Batista L., Benmansour N.C., Fares J., Carpentier S., Thibult M.L., Morel A., Remark R. Association of COVID-19 inflammation with activation of the C5a-C5a1 axis. Nature. 2020 doi: 10.1038/s41586-020-2600-6. Published online July 29, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cascella M., Rajnik M., Cuomo A., Dulebohn S.C., Di Napoli R. StatPearls; 2020. Features, Evaluation and Treatment Coronavirus (COVID-19) [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention CDC Confirms Person-to-Person Spread of New Coronavirus in the United States. 2020. https://www.cdc.gov/media/releases/2020/p0130-coronavirus-spread.html Available from: Published: 30 Jan 2020. Accessed: 02 Jun 2020.
- ClinicalTrials.gov A Study to Evaluate the Efficacy and Safety of Sirukumab in Confirmed Severe or Critical Confirmed Coronavirus Disease (COVID)-19. 2020. https://clinicaltrials.gov/ct2/show/NCT04380961 Available from: Published: 11 Jun 2020. Accessed: 15 Jul 2020.
- Collins F.S., Stoffels P. Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV): An Unprecedented Partnership for Unprecedented Times. JAMA. 2020;323:2455–2457. doi: 10.1001/jama.2020.8920. [DOI] [PubMed] [Google Scholar]
- Eastman R.T., Roth J.S., Brimacombe K.R., Simeonov A., Shen M., Patnaik S., Hall M.D. Remdesivir: A Review of Its Discovery and Development Leading to Emergency Use Authorization for Treatment of COVID-19. ACS Cent. Sci. 2020;6:672–683. doi: 10.1021/acscentsci.0c00489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu B., Xu X., Wei H. Why tocilizumab could be an effective treatment for severe COVID-19? J. Transl. Med. 2020;18:164. doi: 10.1186/s12967-020-02339-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Good S.S., Moussa A., Zhou X.J., Pietropaolo K., Sommadossi J.P. Preclinical evaluation of AT-527, a novel guanosine nucleotide prodrug with potent, pan-genotypic activity against hepatitis C virus. PLoS ONE. 2020;15:e0227104. doi: 10.1371/journal.pone.0227104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guaraldi G., Meschiari M., Cozzi-Lepri A. Tocilizumab in patients with severe COVID-19: a retrospective cohort study. Lancet Rheumatol. 2020 doi: 10.1016/S2665-9913(20)30173-9. Published Online 24 Jun 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadjadj J., Yatim N., Barnabei L., Corneau A., Boussier J., Pere H., Charbit B., Bondet V., Chenevier-Gobeaux C., Breillat P. Impaired type I interferon activity and exacerbated inflammatory responses in severe Covid-19 patients. medRxiv. 2020 doi: 10.1101/2020.04.19.20068015. the preprint server for health sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hewitt J., Lutz C., Florence W.C., Pitt M.L.M., Rao S., Rappaport J., Haigwood N.L. ACTIVating Resources for the COVID-10 Pandemic: in vivo Models for Vaccines and Therapeutics. Cell Host Microbe. 2020;28:646–659. doi: 10.1016/j.chom.2020.09.016. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann M., Kleine-Weber H., Schroeder S., Kruger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.H., Nitsche A. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181:271–280.e278. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann M., Schroeder S., Kleine-Weber H., Müller M.A., Drosten C., Pöhlmann S. Nafamostat Mesylate Blocks Activation of SARS-CoV-2: New Treatment Option for COVID-19. Antimicrob. Agents Chemother. 2020;64 doi: 10.1128/AAC.00754-20. e00754-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horby P., Lim W.S., Emberson J.R., Mafham M., Bell J.L., Linsell L., Staplin N., Brightling C., Ustianowski A., Elmahi E., RECOVERY Collaborative Group Dexamethasone in Hospitalized Patients with Covid-19 - Preliminary Report. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubei Daily, Reporter Yu Jinyi Wuhan Municipal Health Commission announces pneumonia epidemic. 2019. https://crofsblogs.typepad.com/h5n1/2019/12/wuhan-municipal-health-commission-announces-pneumonia-epidemic.html Available from: Published: 31 Dec 2019. Accessed: 02 Jun 2020.
- Jin Y., Yang H., Ji W., Wu W., Chen S., Zhang W., Duan G. Virology, Epidemiology, Pathogenesis, and Control of COVID-19. Viruses. 2020;12:E372. doi: 10.3390/v12040372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jodele S., Köhl J. Tackling COVID-19 infection through complement-targeted immunotherapy. Br. J. Pharmacol. 2020 doi: 10.1111/bph.15187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan P.C., Stevens S.K., Deval J. Nucleosides for the treatment of respiratory RNA virus infections. Antivir. Chem. Chemother. 2018;26 doi: 10.1177/2040206618764483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ledford H. Coronavirus breakthrough: dexamethasone is first drug shown to save lives. Nature. 2020;582:469. doi: 10.1038/d41586-020-01824-5. [DOI] [PubMed] [Google Scholar]
- Liu J., Cao R., Xu M., Wang X., Zhang H., Hu H., Li Y., Hu Z., Zhong W., Wang M. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov. 2020;6:16. doi: 10.1038/s41421-020-0156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maes B., Bosteels C., De Leeuw E., Declercq J., Van Damme K., Delporte A., Demeyere B., Vermeersch S., Vuylsteke M., Willaert J. Treatment of severely ill COVID-19 patients with anti-interleukin drugs (COV-AID): A structured summary of a study protocol for a randomised controlled trial. Trials. 2020;21:468. doi: 10.1186/s13063-020-04453-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore J.B., June C.H. Cytokine release syndrome in severe COVID-19. Science. 2020;368:473–474. doi: 10.1126/science.abb8925. [DOI] [PubMed] [Google Scholar]
- Mulangu S., Dodd L.E., Davey R.T., Jr., Tshiani Mbaya O., Proschan M., Mukadi D., Lusakibanza Manzo M., Nzolo D., Tshomba Oloma A., Ibanda A., PALM Writing Group; PALM Consortium Study Team A Randomized, Controlled Trial of Ebola Virus Disease Therapeutics. N. Engl. J. Med. 2019;381:2293–2303. doi: 10.1056/NEJMoa1910993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munster V.J., Koopmans M., van Doremalen N., van Riel D., de Wit E. A Novel Coronavirus Emerging in China - Key Questions for Impact Assessment. N. Engl. J. Med. 2020;382:692–694. doi: 10.1056/NEJMp2000929. [DOI] [PubMed] [Google Scholar]
- Musarrat F., Chouljenko V., Dahal A., Nabi R., Chouljenko T., Jois S.D., Kousoulas K.G. The anti-HIV drug nelfinavir mesylate (Viracept) is a potent inhibitor of cell fusion caused by the SARSCoV-2 spike (S) glycoprotein warranting further evaluation as an antiviral against COVID-19 infections. J. Med. Virol. 2020 doi: 10.1002/jmv.25985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palanques-Pastor T., López-Briz E., Poveda Andrés J.L. Involvement of interleukin 6 in SARS-CoV-2 infection: siltuximab as a therapeutic option against COVID-19. Eur. J. Hosp. Pharm. Sci. Pract. 2020;27:297–298. doi: 10.1136/ejhpharm-2020-002322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Picchianti Diamanti A., Rosado M.M., Pioli C., Sesti G., Laganà B. Cytokine Release Syndrome in COVID-19 Patients, A New Scenario for an Old Concern: The Fragile Balance between Infections and Autoimmunity. Int. J. Mol. Sci. 2020;21:E3330. doi: 10.3390/ijms21093330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riou J., Althaus C.L. Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.4.2000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roschewski M., Lionakis M.S., Sharman J.P., Roswarski J., Goy A., Monticelli M.A., Roshon M., Wrzesinski S.H., Desai J.V., Zarakas M.A. Inhibition of Bruton tyrosine kinase in patients with severe COVID-19. Sci. Immunol. 2020;5:eabd0110. doi: 10.1126/sciimmunol.abd0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheahan T.P., Sims A.C., Graham R.L., Menachery V.D., Gralinski L.E., Case J.B., Leist S.R., Pyrc K., Feng J.Y., Trantcheva I. Broad-spectrum antiviral GS-5734 inhibits both epidemic and zoonotic coronaviruses. Sci. Transl. Med. 2017;9:eaal3653. doi: 10.1126/scitranslmed.aal3653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheahan T.P., Sims A.C., Zhou S., Graham R.L., Pruijssers A.J., Agostini M.L., Leist S.R., Schäfer A., Dinnon K.H., 3rd, Stevens L.J. An orally bioavailable broad-spectrum antiviral inhibits SARS-CoV-2 in human airway epithelial cell cultures and multiple coronaviruses in mice. Sci. Transl. Med. 2020;12:eabb5883. doi: 10.1126/scitranslmed.abb5883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Şimşek Yavuz S., Ünal S. Antiviral treatment of COVID-19. Turk. J. Med. Sci. 2020;50(SI-1):611–619. doi: 10.3906/sag-2004-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor R., Kotian P., Warren T., Panchal R., Bavari S., Julander J., Dobo S., Rose A., El-Kattan Y., Taubenheim B. BCX4430 - A broad-spectrum antiviral adenosine nucleoside analog under development for the treatment of Ebola virus disease. J. Infect. Public Health. 2016;9:220–226. doi: 10.1016/j.jiph.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toots M., Yoon J.J., Cox R.M., Hart M., Sticher Z.M., Makhsous N., Plesker R., Barrena A.H., Reddy P.G., Mitchell D.G. Characterization of orally efficacious influenza drug with high resistance barrier in ferrets and human airway epithelia. Sci. Transl. Med. 2019;11:eaax5866. doi: 10.1126/scitranslmed.aax5866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaidya G., Czer L.S.C., Kobashigawa J., Kittleson M., Patel J., Chang D., Kransdorf E., Shikhare A., Tran H., Vo A. Successful Treatment of Severe COVID-19 Pneumonia With Clazakizumab in a Heart Transplant Recipient: A Case Report. Transplant. Proc. 2020 doi: 10.1016/j.transproceed.2020.06.003. S0041-1345(20)32575-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M., Cao R., Zhang L., Yang X., Liu J., Xu M., Shi Z., Hu Z., Zhong W., Xiao G. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30:269–271. doi: 10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Zhang D., Du G., Du R., Zhao J., Jin Y., Fu S., Gao L., Cheng Z., Lu Q. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020;395:1569–1578. doi: 10.1016/S0140-6736(20)31022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Chen X., Lu Y., Chen F., Zhang W. Clinical characteristics and therapeutic procedure for four cases with 2019 novel coronavirus pneumonia receiving combined Chinese and Western medicine treatment. Biosci. Trends. 2020;14:64–68. doi: 10.5582/bst.2020.01030. [DOI] [PubMed] [Google Scholar]
- Warren T.K., Jordan R., Lo M.K., Ray A.S., Mackman R.L., Soloveva V., Siegel D., Perron M., Bannister R., Hui H.C. Therapeutic efficacy of the small molecule GS-5734 against Ebola virus in rhesus monkeys. Nature. 2016;531:381–385. doi: 10.1038/nature17180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson R.A., Johnson D.M., Dharia R.N., Merli G.J., Doherty J.U. Anti-coagulant and anti-platelet therapy in the COVID-19 patient: a best practices quality initiative across a large health system. (1995) Hosp Pract. 2020:1–11. doi: 10.1080/21548331.2020.1772639. Published online May 21 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Naming the coronavirus disease (COVID-19) and the virus that causes it. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it Available from: Published: 11 Feb 2020. Accessed: 02 Jul 2020.
- World Health Organization Novel Coronavirus (2019-nCoV). SITUATION REPORT - 1. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200622-covid-19-sitrep-154.pdf?sfvrsn=d0249d8d_2 Available from. Published: 20 Jan 2020. Accessed: 02 Jul 2020.
- World Health Organization Pneumonia of unknown cause – China. 2020. https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/ Available from: Published: 05 Jan 2020. Accessed: 02 Jul 2020.
- Wu Z., McGoogan J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- Xu X., Han M., Li T., Sun W., Wang D., Fu B., Zhou Y., Zheng X., Yang Y., Li X. Effective treatment of severe COVID-19 patients with tocilizumab. Proc. Natl. Acad. Sci. USA. 2020;117:10970–10975. doi: 10.1073/pnas.2005615117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao T.T., Qian J.D., Zhu W.Y., Wang Y., Wang G.Q. A systematic review of lopinavir therapy for SARS coronavirus and MERS coronavirus-A possible reference for coronavirus disease-19 treatment option. J. Med. Virol. 2020;92:556–563. doi: 10.1002/jmv.25729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye Q., Wang B., Mao J. The pathogenesis and treatment of the ‘Cytokine Storm’ in COVID-19. J. Infect. 2020;80:607–613. doi: 10.1016/j.jinf.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeleswaram S., Smith P., Burn T., Covington M., Juvekar A., Li Y., Squier P., Langmuir P. Inhibition of cytokine signaling by ruxolitinib and implications for COVID-19 treatment. Clin. Immunol. 2020;218:108517. doi: 10.1016/j.clim.2020.108517. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.