Abstract
Enzymatic inactivation of Rho-family GTPases by the glucosyltransferase domain of Clostridioides difficile Toxin B (TcdB) gives rise to various pathogenic effects in cells that are classically thought to be responsible for the disease symptoms associated with C. difficile infection (CDI). Recent in vitro studies have shown that TcdB can, under certain circumstances, induce cellular toxicities that are independent of glucosyltransferase (GT) activity, calling into question the precise role of GT activity. Here, to establish the importance of GT activity in CDI disease pathogenesis, we generated the first described mutant strain of C. difficile producing glucosyltransferase-defective (GT-defective) toxin. Using allelic exchange (AE) technology, we first deleted tcdA in C. difficile 630Δerm and subsequently introduced a deactivating D270N substitution in the GT domain of TcdB. To examine the role of GT activity in vivo, we tested each strain in two different animal models of CDI pathogenesis. In the non-lethal murine model of infection, the GT-defective mutant induced minimal pathology in host tissues as compared to the profound caecal inflammation seen in the wild-type and 630ΔermΔtcdA (ΔtcdA) strains. In the more sensitive hamster model of CDI, whereas hamsters in the wild-type or ΔtcdA groups succumbed to fulminant infection within 4 days, all hamsters infected with the GT-defective mutant survived the 10-day infection period without primary symptoms of CDI or evidence of caecal inflammation. These data demonstrate that GT activity is indispensable for disease pathogenesis and reaffirm its central role in disease and its importance as a therapeutic target for small-molecule inhibition.
Author summary
Novel non-antibiotic therapies are required for the treatment of Clostridioides difficile infection (CDI). An emerging class of promising therapeutics for CDI are antivirulence agents that block the actions of C. difficile Toxin B (TcdB), the primary determinant of virulence. In order to develop such treatments, molecular targets and mechanisms must be identified and validated. Historically the glucosyltransferase domain (GTD) represented an ideal target owing to its perceived importance for disease pathogenesis. However, studies capitalizing on recent advances in recombinant TcdB production have unveiled GTD-independent mechanisms of toxicity when applied at high concentrations in vitro, thus questioning the role of the GTD. Here we generate the first-reported mutant strain of C. difficile expressing glucosyltransferase-defective TcdB. Application thereof demonstrates that the GTD is essential for disease in mice and hamsters, thus reoffering the GTD as an ideal candidate for small-molecule inhibitor (SMI) development.
Introduction
Clostridioides difficile (previously known as Clostridium difficile [1]) is the leading cause of nosocomial diarrhea in the developed world [2]. The main virulence factors responsible for the onset of symptoms during C. difficile infection (CDI), including diarrhea and pseudomembranous colitis, are the monoglucosyltransferases Toxin A (TcdA; 308kDa) and Toxin B (TcdB; 270 kDa) [3]. The application of tcdA and tcdB-null mutant strains to in vivo models, coupled with the frequent isolation of clinical isolates producing only TcdB, has consolidated the notion that–though TcdA can contribute to disease severity–TcdB represents the primary virulence determinant for CDI [4–6]. TcdB is therefore the primary target for the development of novel toxin-targeted therapeutics, including monoclonal antibodies and small-molecule inhibitors (SMIs).
TcdB is a single polypeptide cytotoxin composed of four distinct domains: a receptor-binding domain (RBD), a translocation domain (TD), an autoprocessing domain (APD), and a glucosyltransferase domain (GTD). TcdB is endocytosed into endosomes following receptor binding to one of three defined receptors: chondroitin sulfate proteoglycan 4 (CSPG4), Nectin 3 and frizzled protein (FZD1, 2 and 7) at least in part due to interaction with the RBD [7–9]. Thereafter, vesicular acidification leads to a conformational change and protein unfurling, ascribed to the hydrophobic region of the TD, permitting membrane insertion and the formation of an endosomal pore, through which the GTD and APD translocate into the cytosol [10]. Cytosolic inositol hexakisphosphate (InsP6) acts as an allosteric activator to initiate the cysteine-protease activity of the APD, which cleaves the GTD, leading to its release into the cytosol [11]. The GTD then glucosylates Rho-family GTPases leading to the classical phenotype of rapid actin depolymerization, loss of structural integrity, cell rounding and apoptosis of the colonic epithelium [12].
Over the past decade, significant efforts have been made to characterize the contribution of the GTD to disease pathogenesis through the generation of recombinant TcdB defective in glucosyltransferase activity (GT-defective). These studies have unveiled novel GT-independent mechanisms of toxicity for TcdB. Rapid necrotic cell death was observed independent of the GTD when GT-defective TcdB was applied in vitro at ≥1nM [13]. In the same study, an active GTD domain was required to induce the classical cytopathic effect at concentrations of <10pM. The necrotic mechanism was later characterized to be dependent on the host NADPH oxidase complex [14]. Thereafter, a second GT-independent mechanism of cell death was discovered to occur through a pyknotic mechanism [15]. In a similar fashion to the aforementioned necrotic mechanism, the pyknotic pathway was restricted to high concentrations of TcdB. Finally, two studies investigating TcdB-induced inflammasome activation, using wild-type TcdB and GT-defective TcdB, yielded opposing conclusions on the dependence of GT activity on inflammasome activation [16, 17]. Such discoveries question the contribution of the GTD to the pathogenesis of CDI and divert focus for SMI development away from the GTD. Ultimately, in vivo substantiation of the in vitro discoveries is needed to clarify the importance of GT activity in a natural disease setting. Previous attempts have been made to correlate the relevance of the GT-independent mechanisms of TcdB to infection. Therein, GT-defective TcdB was injected into mice [18], and in parallel, mice were infected with a surrogate Bacillus megaterium host strain, engineered to secrete GT-defective TcdB [19]. In neither instance was a GT-independent effect of virulence observed. These experiments question the relevance of the GT-independent mechanisms of TcdB-induced toxicity to infection, but hitherto, no study has been conducted with a strain of C. difficile engineered to produce full-length GT-defective toxin.
This study sought to clarify the role of the GTD to disease pathogenesis in vivo through the generation of a mutant strain of C. difficile devoid of GT-activity and its application to murine and hamster models of infection.
Results and discussion
Mutant strain authentication and in vitro characterization
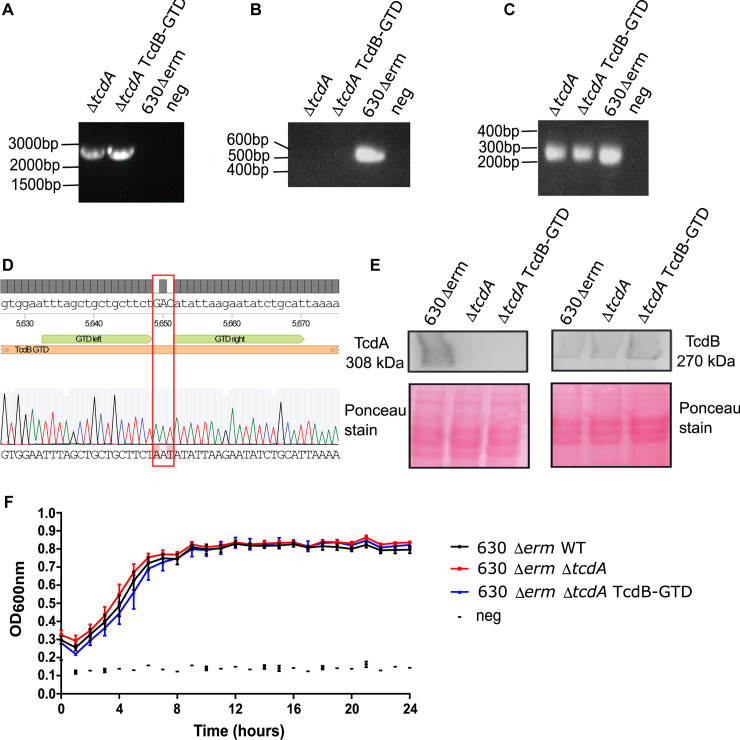
In an attempt to reconcile and clarify the role of the GTD to the pathogenesis of CDI, we applied allelic-exchange technology to delete the entire 8133bp tcdA gene from the chromosome of C. difficile 630Δerm [20], as described in materials and methods. Successful deletion was observed by the presence of a circa 2.7kb product following PCR with diagnostic primers flanking tcdA (Fig 1A). An additional PCR was conducted using internal primers annealing within tcdA to ensure the absence of contaminating wild-type sub-populations (Fig 1B). The selected mutant, designated 630ΔermΔpyrEΔtcdA possessed the 2.7Kb deletion fragment and lacked the circa 500bp internal fragment following both PCR reactions (Fig 1A and 1B). The deletion was confirmed to be as intended through Sanger sequencing of the resultant amplicon. Deletion of tcdA should permit the study of TcdB without the need to consider the contribution of TcdA-mediated virulence. Using the same technology, the trinucleotide gac encoding Asp 270 in tcdB was mutated to aat to encode Asn ensuing an Asp270Asn (D270N) substitution. TcdB D270N was previously shown to be the most defective variant for glucosyltransferase activity in vitro, and was fully capable of inducing the necrotic mechanism of cell death [13]. PCR with flanking primers (Fig 1C) followed by Sanger sequencing of the amplicon and sequence alignment using the Benchling bioinformatics platform, revealed that the gac-aat substitution had taken place as intended (Fig 1D). Finally, the pyrE allele was repaired in both strains exactly as described previously [21]. To probe for unintended polymorphisms arising as a consequence of the mutagenesis procedure, gDNA was extracted from each strain and analyzed by next generation sequencing (NGS). No unintended nucleotide variations were detected for the two mutant strains compared with the wild-type parental. Sequencing reads were deposited to the NCBI Sequencing Read Archive [22] under accession number PRJNA623295.
Fig 1. Development and authentication of a mutant strain producing GTD-defective TcdB.
a) Gel image following PCR of the tcdA gene using the flanking primers tcdA diag F/tcdA diag R. The presence of a circa 2.7kb band indicates successful gene deletion. b) Gel image following PCR of the tcdA gene using the internal primers tcdA int F/tcdA int R. The absence of a 500bp product indicates successful gene deletion. c) Gel image following PCR of the GTD of tcdB using GTD diag F/R primers. Strain labels: C. difficile 630Δerm (WT); C. difficile 630ΔermΔtcdA (tcdA); C. difficile 630ΔermΔtcdA GTD::D270N (GTD). d) Sequence alignment of the GTD region of tcdB for C. difficile 630ΔermΔtcdA GTD::D270N with the wild-type reference sequence of 630Δerm. The desired gac-aat substitution is highlighted in a red box. e) Western blot detection for TcdA and TcdB for the wild-type, ΔtcdA and GTD-D270N strains including Poncaeu stains to validate even protein loading. f) 24h automated growth curve of the wild-type, ΔtcdA and GTD-D270N strains.
Before proceeding with the animal experiments, it was first necessary to phenotype the mutants generated herein. The production of TcdA and TcdB was assessed by Western blot on 48h filter-sterilized supernatants of the wild-type and mutant strains. Neither the tcdA-deletion strain nor the GT-defective mutant were capable of producing TcdA, as intended (Fig 1E). In a similar fashion, neither strain was affected for the production of TcdB (Fig 1E). Ponceau staining demonstrated adequate and equal protein loading. The strains were then assessed for their growth capabilities through an automated 24h growth curve. No growth defects were observed for either mutant when compared with the wild-type parental (Fig 1F).
Glucosyltransferase activity is required for disease pathogenesis in a murine model
Having generated the requisite mutants, we next investigated their effects in a non-lethal mouse model of CDI. This model mimics human disease in that gastrointestinal (GI) dysbiosis is first induced with antibiotics, the inciting risk factor in a majority of human infections. Further, a majority of human infections do not result in death, but instead cause pathology in the distal GI tract, similar to the murine model of infection. Therefore, this model serves to help investigate whether GT activity was necessary for clinically relevant measures of TcdB-induced pathogenesis in vivo.
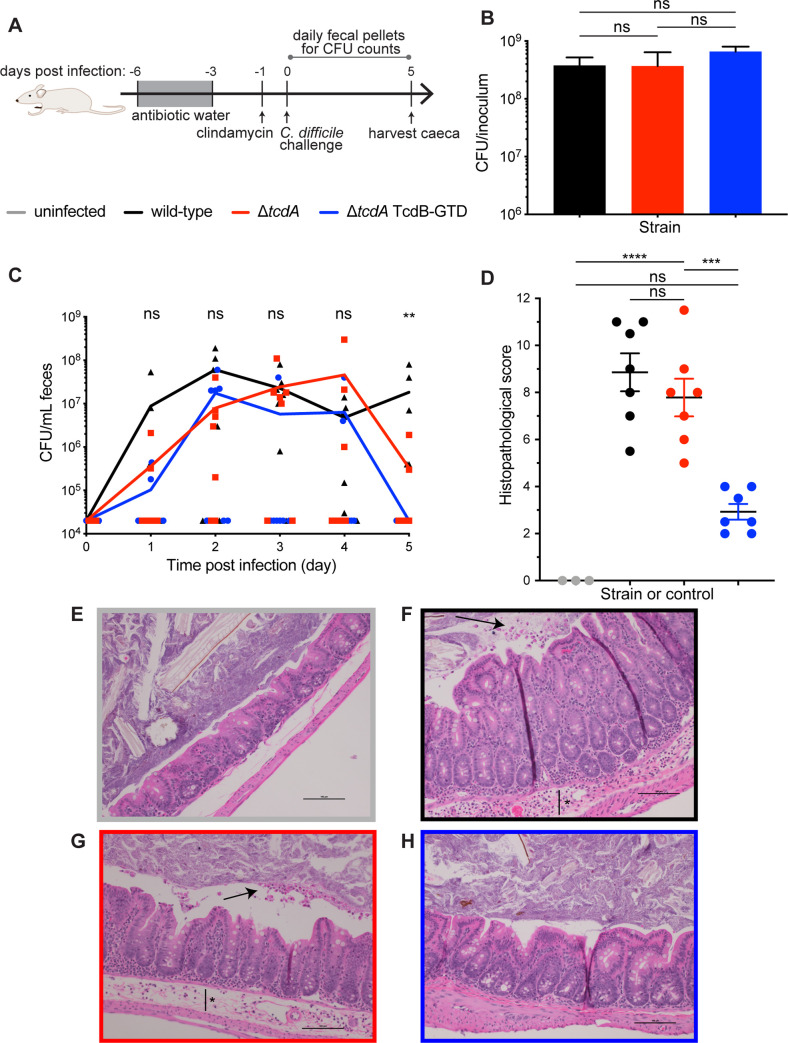
In this established model, pretreatment with an antibiotic cocktail followed by a single dose of clindamycin was used to disrupt the GI microbiome, creating a GI state permissive to C. difficile colonization (Fig 2A) [23]. Mice were then challenged with approximately 108 colony-forming units (CFUs) of either wild-type C. difficile 630Δerm (WT), the tcdA-deletion mutant C. difficile 630Δerm (ΔtcdA) or the GT-defective strain C. difficile 630Δerm GTD::D270N (TcdB-GTD). C. difficile burdens per inoculum, with mean averages of 3.8 × 108 for WT, 3.7 × 108 for ΔtcdA, and 6.6 × 108 TcdB-GTD, did not statistically significantly differ between the three strains (Fig 2B). To determine whether mutant strains were able to colonize in vivo, mice were monitored for 5 days post infection with daily CFU counts from fecal samples. Selective culturing confirmed that each mouse in all three groups shed detectable CFUs on at least one day. Genomic DNA isolated from one fecal sample per cage was amplified to identify the desired strain (S1A–S1C Fig). These data confirm that each group was colonized with the administered strain.
Fig 2. The GTD is required for typhlitis in murine infection.
a) Schematic of non-lethal mouse model of CDI. Swiss Webster mice, excluding those in the uninfected control group, were pretreated with an antibiotic cocktail in drinking water for three days (gray box, days -6 to -3), then orally dosed with 1 mg clindamycin on day -1 to induce dysbiosis. On day 0, mice were orally challenged with C. difficile 630Δerm (wild-type, n = 7), C. difficile 630ΔermΔtcdA (tcdA deletion mutant, n = 7), C. difficile 630ΔermΔtcdA GTD::D270N (GT-defective mutant, n = 7) or sterile PBS for the uninfected control group (n = 3). Fecal pellets were collected daily to analyze C. difficile burden and caeca were harvested on day 5 for histological analysis. b) C. difficile burden per 200 μL inoculum quantified for each bacterial strain. Statistical analysis between C. difficile strains was analyzed using one-way ANOVA with Tukey’s multiple comparison test (ns, non-significant). c) Daily C. difficile burden measured from selective culture of fecal samples. Graph displays each replicate with connecting line indicating the mean per group at each time point. Statistical analysis between groups was performed on each day for days 1–4 via Kruskal-Wallis test (ns, non-significant) and on day 5 via Kruskal-Wallis with multiple comparisons (**p<0.01 between wild-type and GT-defective mutant, all other comparisons non-significant). d) Histopathological score for combined inflammatory cell infiltrates (0–3), mucosal hypertrophy (0–3), epithelial disruption (0–3) and submucosal edema (0–3), with each pathological feature scored from normal (0) to severe (3) on H&E-stained caecal slides. Statistical analysis performed via one-way ANOVA with Tukey’s multiple comparison test (ns, non-significant; ***p<0.001, ****p<0.0001). Representative H&E image of caecal section from e) uninfected control group, f) wild-type group, g) tcdA deletion mutant group, and h) GT-defective mutant group. Images were taken with x20 magnification, and scale bar indicates 100 μM. Black arrows indicate apoptotic cell sloughage, black bar with asterisk indicates submucosal edema.
Aggregate daily CFUs within each group displayed a wide range, with multiple measurements falling below the limit of detection of 2 × 104 CFU/mL feces (Fig 2C). However, statistical analysis between shed CFUs of WT, ΔtcdA, and TcdB-GTD on days one to four were not significantly different (Fig 2C), indicating similar levels of colonization among the three groups over these days. We noted that on day five, C. difficile burdens were all below the limit of detection in the TcdB-GTD group, which was significantly less compared to WT (p = 0.0034) and narrowly missing significance as compared to the ΔtcdA group (p = 0.0538). While this could suggest that the TcdB-GTD mutant displays different colonization kinetics than the WT and ΔtcdA strains, we posit that the variance in these data are likely ascribed to a systematic technical error or the high limit of detection of the method (2 × 104 CFU/mL). Notwithstanding the potential differences in colonization kinetics, these data show that all strains colonized in vivo.
Having established that all groups were colonized, we asked whether GT activity was required for evidence of pathogenesis in the distal GI tract. Mice were sacrificed on day 5 post infection to harvest caecal tissue for histological analysis. H&E-stained slides of caecal samples were analysed for evidence of inflammatory cell infiltrates, mucosal hypertrophy, epithelial disruption and submucosal edema, with a maximal severity score of 12 (Fig 2D). WT and ΔtcdA groups displayed significant evidence of CDI. As compared to uninfected controls (Fig 2E), representative images of the WT and ΔtcdA groups display apoptotic cell sloughage (Fig 2F and 2G black arrows) and submucosal edema (Fig 2F and 2G black bar with asterisk). Histopathological scores were not significantly different between the WT and ΔtcdA groups (p = 0.6537). Thus, the absence of TcdA does not significantly alter disease severity, consistent with prior studies [4, 5]. In contrast, the TcdB-GTD group displayed significantly attenuated pathology, with scores significantly lower than WT (p<0.0001) and ΔtcdA (p = 0.0002), and lacking evidence of severe disease in representative images (Fig 2H). Further, pathology in the TcdB-GTD group was not significantly different than uninfected controls (p = 0.0957). Taken together, these data confirm that GT activity is required for pathogenesis in a clinically relevant model of CDI.
Glucosyltransferase activity is required for C. difficile pathogenesis in a hamster model
Having established that GT activity is required for pathogenesis in a non-lethal model of CDI, we next asked whether the TcdB-GTD mutant strain was capable of inducing virulence in a more sensitive animal model. To test this, we used the well-established hamster model of infection. Unlike the non-lethal mouse model of CDI, hamsters are exquisitely sensitive to C. difficile and uniformly succumb to fulminant infection when challenged with C. difficile expressing wild-type toxin, but survive when challenged with avirulent strains [4]. As a consequence, we reasoned that the hamster model could potentially reveal any symptoms of CDI which were not detected in the less sensitive murine model.
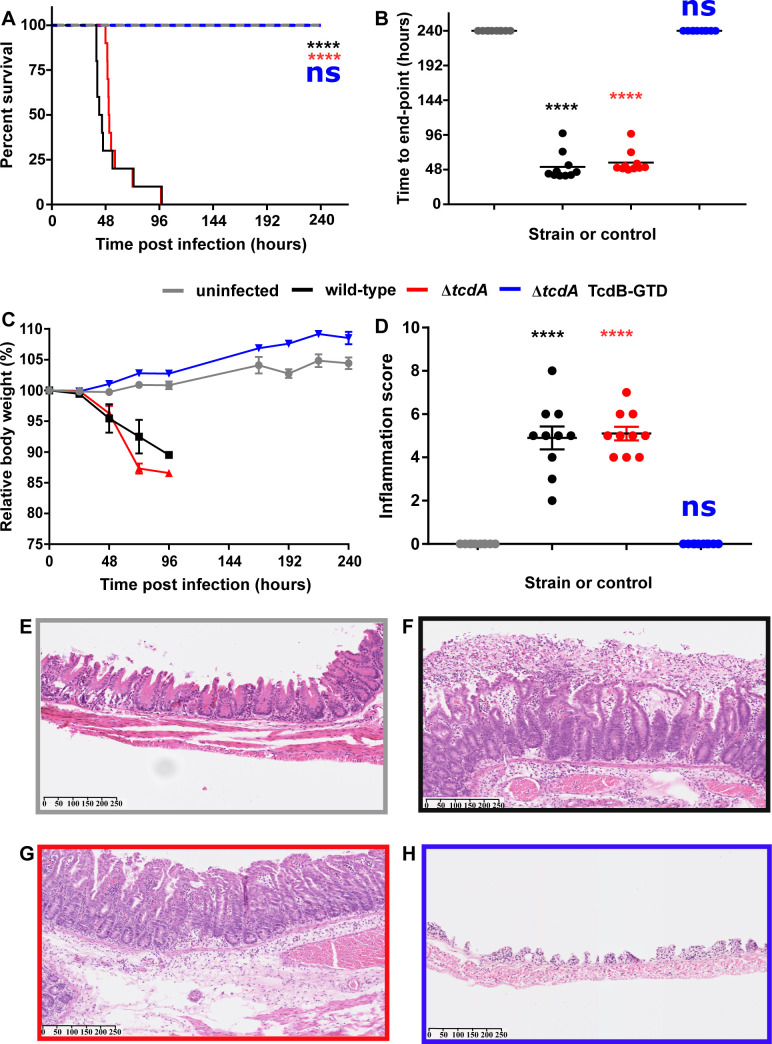
To this end, pre-conditioned Syrian Golden hamsters were infected with approximately 10,000 heat-resistant colony-forming units (HR-CFU) of either WT, ΔtcdA or TcdB-GTD. The uninfected control group was given sterile diluent at time-point 0. Ten animals were used per infection group or control. Hamsters were monitored at regular intervals for primary symptoms of CDI (severe wet tail, diarrhea, hypothermia, lying prone or unresponsive) and were euthanized at the onset of fulminant CDI or at the 240th hour post infection. Five animals infected with wild-type 630Δerm were symptomatic of fulminant CDI 36h following spore administration (Fig 3A). The remaining hamsters in this group reached this stage by the 96h time-point. The mean time to end-point following spore administration was 52h for the WT group (Fig 3B). Similarly, animals infected with the ΔtcdA strain reached fulminant CDI with an average time to end-point of 58h (Fig 3B). All animals in WT and ΔtcdA groups succumbed to fulminant infection by 96h (Fig 3A and 3B). Deletion of tcdA did not significantly reduce the time from spore administration to end point (P = 0.94), thus further supporting the centrality of TcdB to disease pathogenesis. Hamsters in both the WT and ΔtcdA groups lost significant weight, up to 12.5% relative to their starting weights (Fig 3C). Meanwhile, none of the subjects infected with the TcdB-GTD strain presented with any primary symptom of CDI during the 240h infection period. Consequently, all subjects in this group were euthanized at the 240h time-point (Fig 3A and 3B). Contrary to the results seen for the WT and ΔtcdA animals, subjects within this group gained up to 8% body weight relative to their starting weight (Fig 3C). Terminal colonization was assessed as described in Materials and Methods. Each infection group was colonized by C. difficile (S2 Fig). The approximately 2-log decrease observed between the 24-96h samples for the WT and ΔtcdA groups compared with the 240h GT-defective group, are in-line with previous 10-day colonization experiments [24]. Owing to the sampling procurement adopted, it is not possible for us to demonstrate that each mutant colonized the hamsters to the same extent. However, the NGS data assures us that the GT-defective mutant was devoid of unintended mutations which may have affected colonization. Taken together, these data indicate that the GTD is essential for the development of primary symptoms during CDI.
Fig 3. The GTD of TcdB is indispensable for in vivo pathogenesis in hamsters.
a) Survival plot of Syrian Golden hamsters infected with approximately 10,000 spores of C. difficile 630Δerm (wild-type, black lines), C. difficile 630ΔermΔtcdA (tcdA deletion mutant, red lines), C. difficile 630ΔermΔtcdA GTD::D270N (GT-defective mutant, blue lines) or sterile PBS for the uninfected control group (grey lines) (n = 10). Hamsters were monitored for a period of 240h for primary symptoms of CDI. Animals were euthanized at the onset of fulminant infection, or at the 240h time-point in the absence of considerable symptoms. Statistical significance between test groups and the uninfected control group was shown according to the Peto log-rank test (p = **** <0.0001) b) Time from inoculation to experimental endpoint. Statistical significance between test groups and the uninfected control group according to one-way ANOVA followed by Dunnet’s multiple comparison test (p = **** 0.001) c) Body weight of each animal subject, relative to starting weight. Data points represent the mean ±SEM of 10 animal subjects per infection or control group d) Terminal inflammation score for combined edema (0–3), tissue damage (0–3) and neutrophil infiltration (0–3) (maximum score of 9) as assessed by histopathological analysis of H&E stained caeca. Statistical significance between test group and the uninfected control group according to one-way ANOVA followed by Dunnet’s multiple comparison test (p = **** 0.0001). Representative transverse cross-section of H&E stained hamster caeca for e) Uninfected control group f) C. difficile 630Δerm (wild-type group) g) C. difficile 630ΔermΔtcdA (tcdA deletion group) h) C. difficile 630ΔermΔtcdA GTD::D270N (GT-defective group). Scale bars represent the μM range.
Having established that the GTD is required for the onset of primary symptoms for CDI, we next tested for any signs of inflammation induced by each respective mutant through histopathological analysis of hamster caeca. Both the WT and ΔtcdA groups showed significant signs of caecal inflammation yielding similar inflammation scores of approximately 5 based on the sum of edema, neutrophil infiltration and tissue damage, with a maximum score of 9 per animal subject (Fig 3D, 3F and 3G). On the contrary, the subjects in the uninfected control group and the TcdB-GTD groups showed no symptoms of inflammation yielding a score of zero for each individual subject (Fig 2D, 2E and 2H). The results from the histopathological analysis corroborate those of the primary infection study thus suggesting that the GTD is required for virulence in TcdB-induced CDI.
Concluding remarks
The data presented herein, in two well-established animal models of CDI, demonstrate that GT activity is essential for in vivo C. difficile disease pathogenesis. Although recombinant GT-defective TcdB is clearly capable of inducing cellular toxicity in vitro at higher nanomolar concentrations through both necrotic or pyknotic mechanisms [13, 15], the lack of any overt disease pathology for the GT-defective TcdB strain in either model tested here, suggests that the absolute amounts of toxin needed to induce these cellular phenotypes may not be reached during an infection in vivo. Future studies on the role of GT activity in other models and other aspects of disease such as recurrence and colonization kinetics are warranted to determine whether GT-independent effects play a role in other aspects of CDI.
Finally, the results presented here have important implications on our understanding of CDI disease pathogenesis and obvious consequences for the design of novel SMIs aiming to neutralize the toxic effects of TcdB as an alternative to antibiotic therapy. Before the discovery of the necrotic and pyknotic mechanisms of toxicity, the major focus for SMI development was focused on identification of GTD-targeted SMIs. Our demonstration that the GTD is essential for the development of symptoms during CDI, reoffers the GTD as a well-validated target for SMI development.
Materials & methods
Ethics statement
All murine experiments were carried out in accordance with APLAC protocols approved by the Stanford University Institutional Care and Use Committee (IACUC).
Bacterial growth conditions
For strain development and in vitro analyses, C. difficile was routinely maintained on Brain heart infusion medium (Oxoid) supplemented with 5μg/ml yeast extract, 0.1% w/v L-cysteine (BHIS), C. difficile selective supplement comprising 250μg/ml D-cycloserine, and 8 μg/ml cefoxitin (Oxoid) (BHIS CC), and where necessary, an additional supplementation of 15 μg/ml thiamphenicol (BHIS CCTM). C. difficile cultures were grown at 37°C in an anaerobic workstation (Don Whitley) with an anaerobic gas mixture comprising 80% N2, 10% H2 and 10% CO2.
For murine experiments, frozen stocks of wild-type and mutant strains were cultured on CDMN agar plates (C. difficile agar base (Oxoid) supplemented with 7% (v/v) defibrinated horse blood (Lampire Biological Laboratories), 32 mg/L moxalactam (Santa Cruz Biotechnology), 12 mg/L norfloxacin (Sigma-Aldrich) and 500 mg/L cysteine hydrochloride (Fischer) in an anaerobic chamber [27] at 37°C for 24 hours. Single colonies were picked and grown anaerobically for 16–18 hours at 37°C to saturation in 5 mL of pre-reduced reinforced Clostridial medium (RCM, Oxoid) for inoculation.
For hamster experiments, strains were cultured on blood agar for 5d in order to generate the spore stocks. Terminal colonization was assessed using C. difficile selective agar (Oxoid). In both instances, strains were maintained in an anaerobic workstation, as described above.
Mutant generation
Strains and primers used in this study are listed in Tables 1 and S1 respectively. An in-frame deletion mutant of tcdA in 630ΔermΔpyrE was generated using allelic-exchange technology [20]. Left and right homology arms annealing up and downstream of tcdA were amplified by PCR with primer sets tcdA LAF/LAR and RAF/RAR respectively. The fragments were spliced together by splicing by overlap extension (SOEing) PCR and were subsequently cloned into pMTL-YN3 [20], by means of their flanking SbfI and AscI restriction sites. The Knockout cassette [28] was conjugated into 630ΔermΔpyrE exactly as described previously [21]. Transconjugants were selected on the basis of thiamphenicol resistance on BHIS CCTM plates. Single cross-over integrants were identified following sub-culturing onto BHIS CCTM by PCR using two primer sets to screen for integration at the left or right homology arms: tcdA diag F/YN3 R and YN3 F/ tcdA diag R; each containing a primer annealing to the chromosome and a primer annealing to the KOC plasmid. Confirmed single cross-over clones were grown on non-selective BHIS medium and thereafter C. difficile minimal medium [29] containing 500μg/ml 5-fluoroorotic acid (FOA) and 1μg/ml uracil to force plasmid loss through the counter-selection marker pyrE, and to select for double cross-over mutants before confirming plasmid loss on the basis of thiamphenicol sensitivity. The desired deletion mutants were identified by PCR amplification of the tcdA locus using the diagnostic primers tcdA diag F and tcdA diag R. An additional PCR was conducted on putative mutants with internal primers annealing within tcdA to ensure the absence of contaminating wild-type sub-populations.
Table 1. Strains used in this study.
| Strain/Plasmid | Description | Origin |
|---|---|---|
| Strain | ||
| E. coli | ||
| Top 10 | Cloning host | Invitrogen |
| CA434 | Conjugation host | [25] |
| C. difficile | ||
| 630Δerm | Erythromycin sensitive clone of CD630 | [26] |
| 630ΔermΔpyrE | pyrE mutant to facilitate AE mutagenesis | [20] |
| 630ΔermΔpyrEΔtcdA | Initial tcdA-deletion mutant | This study |
| 630ΔermΔtcdA | pyrE-restored tcdA-deletion mutant | This study |
| 630ΔermΔpyrEΔtcdA.TcdB::GTD D270N | Initial GTD-defective mutant | This study |
| 630ΔermΔtcdA.TcdB::GTD D270N | pyrE-restored GTD-defective mutant | This study |
| Plasmid | ||
| pMTL-YN3 | Knockout vector for 630Δerm | [20] |
| pMTL-YN3-tcdA KOC | As above with knockout cassette for tcdA | This study |
| pMTL-YN3-TcdB::GTD D270N SC | As above with substitution cassette for TcdB::GTD D270N | This study |
| pMTL-YN1 | pyrE-restoration vector for 630Δerm | [20] |
For the generation of a GTD-defective mutant, two circa 1kb fragments were amplified by two PCR reactions for each target, comprising a forward and reverse primer containing SbfI and AscI restriction sites respectively, paired with internal mutagenic primers encompassing the desired nucleotide substitutions. The mutagenic forward primer GTD mut F, contained the exact reverse complemented sequence of the mutagenic reverse primer, GTD mut R to facilitate subsequent SOEing of the two fragments. Spliced products were then cloned into pMTL-YN3 as described above to generate a substitution cassette (SC) for GTD D270N. The procedure hereafter mimicked that described above for the chromosomal deletion, however, owing to the desired mutagenesis being a substitution rather than a deletion, putative mutants were assessed by PCR followed by Sanger sequencing of the amplicon. The read for each clone was aligned to the wild-type reference sequence and the desired substitution sequence to confirm the presence or absence of the desired codon substitution. The pyrE locus of each strain was then restored exactly as described previously [21].
Whole genome sequencing
Genomic DNA was extracted from both mutant strains and the wild-type parental and sent for next generation sequencing (NGS) using the Illumina MiSeq platform at MicrobesNG (University of Birmingham, UK). The paired reads were trimmed and mapped to the reference genome sequence for C. difficile 630 (Accession: AM180355. Thereafter, each strain was analyzed for any single nucleotide variations (SNVs), insertions or deletions of DNA compared with the reference genome sequence, using CLC Genomics Workbench software (Qiagen, Netherlands). Sequencing reads were deposited to the NCBI Sequencing Read Archive under accession number PRJNA623295.
Western blot detection of C. difficile toxins
Secreted TcdA and TcdB was detected by Western blot on 40x trichloracetic acid protein concentrates derived from 48h sterile-filtered supernatants exactly as described previously [21] using HRP-Chicken anti-Clostridium difficile Toxin A IgY and anti-Clostridium difficile Toxin B IgY antibodies (Gallus-Immunotech, USA) respectively.
Automated growth curve
Growth profiles of the wild-type parental and mutant strains were assessed by automated growth curve using a Promega Glomax plate reader (Promega, USA) exactly as described previously [30].
Murine model of infection
Age- and sex-matched male and female conventional Swiss Webster mice (SWEF, Taconic, bred in-house) ages 8–12 weeks were fed standard chow and had an average starting weight of 38 g. Mice were randomly divided into four groups: uninfected controls without antibiotic pre-treatment (n = 3), or infected with WT (n = 7), ΔtcdA (n = 7) or TcdB-GTD (n = 7). Mice, excluding those in the control group, were pre-treated with an antibiotic cocktail (kanamycin (0.4 mg/mL), gentamycin (0.035 mg/mL), colistin (850 U/mL), metronidazole (0.215 mg/mL) and vancomycin (0.045 mg/mL)) in drinking water for 3 days, starting 6 days before inoculation, as previously reported [23]. Mice were switched to regular water for 2 days, and then orally administered 1 mg of clindamycin on day -1 (excluding those in the uninfected control group). On day 0, experimental WT, ΔtcdA and TcdB-GTD were orally challenged with approximately 108 CFU (in 200 μL RCM) of the appropriate wild-type or mutant strain from overnight culture. Mice were monitored with daily weights, and fecal samples were collected for 5 days to measure daily C. difficile CFU burden. Mice were then sacrificed according to the guidelines on human termination on experimental day 5 after C. difficile challenge. Caecal tissues were collected for histological analysis. Genomic DNA from fecal samples from one mouse per cage was amplified to ensure colonization with the appropriate strain, using a protocol adapted from [31, 32]. Briefly, 10–30 mg fecal sample was resuspended in 500–700 μL TRIS-buffered saline (TBS, 50 mM TRIS, 150 mM NaCl, pH 7.4) and disrupted with 0.1 mm glass beads using Mini-BeadBeater-96 (Biospec Products) for 3 minutes. Genomic DNA was extracted from the supernatant with two rounds of phenol:chloroform:isoamyl alcohol (25:24:1) in a 1:1 ratio with supernatant, then ethanol precipitation was performed. The resulting DNA pellet was resuspended in 200 μL PBS and purified of PCR inhibitors using a QIAamp DNA blood Mini kit (Qiagen) before amplifying the regions of interest using tcdA int F and R primers (TcdA internal region) and GTD diag F and R primers (GTD-encoding region of TcdB).
Fecal and Inoculum and CFU quantification in the murine model
Fecal samples were collected from mice directly into Eppendorf tubes and placed on ice. To measure C. difficle CFU burdens, 1 μL feces was resuspended in 200 μL sterile PBS. Samples were then serially diluted 10-fold into PBS, with 10 μL struck onto CDMN plates in duplicate. Plates were incubated anaerobically at for 16–24 hours at 37°C before quantification. To enumerate inoculum CFUs, 200 μL of each strain was used as starting material, with serial dilution and plating as above.
Histopathological assessment of murine samples
Proximal colon and caecal sections were collected and fixed in 10% neutral buffered formalin, processed (Leica), paraffin embedded (Leica), sectioned at 5 μm, mounted on glass slides and H&E stained (HistoTec Laboratory). Sections were scored by a veterinary pathologist blinded to the identity of the samples (Dr. Donna M. Bouley, Stanford University Department of Comparative Medicine) using a scoring system adapted from Pawlowski et al [33]. Caecal sections were assessed for inflammatory cell infiltrates (0–3), mucosal hypertrophy (0–3), epithelial disruption (0–3) and submucosal edema (0–3) for a maximal score of 12, with each pathological feature scored from normal (0) to severe (3). Images representative of each treatment group are shown in Fig 2.
Hamster model of infection
Animal studies were planned and performed according to the ARRIVE guidelines [34] under license by Evotec Ltd, UK. Adult male Syrian Golden hamsters weighing between 82-111g were pre-conditioned with 30mg/kg clindamycin to disrupt their gut microbiota for a period of 5d. Hamsters were then randomly divided into four groups: uninfected controls (n = 10), or infected with WT (n = 10), ΔtcdA (n = 10) or TcdB-GTD (n = 10). Subjects in each experimental group were administered with approximately 10,000 spores (heat-resistant colony forming units, HR-CFU) of the appropriate wild-type or mutant strain or sterile PBS (uninfected control group). Animals were monitored daily for symptoms of CDI for a period of 240h. Animals were euthanized by pentobarbitone overdose, if they were deemed to be symptomatic of fulminant CDI. Criteria for fulminant CDI were: hypothermia <34°C, 20% weight loss, severe diarrhea, inability to reach food and water or severely hunched posture with piloerection. Euthanized subjects were dissected and terminal-colonization was determined in-house at the animal research facility using fecal samples plated on C. difficile selective medium (Oxoid, USA). The presence of C. difficile was confirmed using the C. difficile latex agglutination kit (Oxoid, USA). To confirm the identity of the isolates, HR-CFU were isolated from caecum, small intestine and colon samples in the research facility. Presumptive isolates were confirmed by colony PCR for tcdA flanking region, tcdA internal region and GTD-encoding region of tcdB. Hamster caeca were fixed in 10% buffered neutral formalin (BNF) and stored until histopathological assessment.
Histopathological assessment of hamster caeca
Fixed transverse cross-sections of hamster caeca were routinely processed for paraffin embedding, sectioned at 5 μm, mounted on glass slides, and H&E stained. Thereafter a trained pathologist individually scored each sample for edema (1–3), neutrophil infiltration (1–3) and tissue damage (1–3), with a maximum potential score of 9 per animal subject.
Statistical analysis
Statistical analyses (one-way ANOVA with Tukey’s or Dunnet’s multiple comparison test, Kruskall-Wallis test with multiple comparisons, as indicated in figure legends) were performed using the GraphPad Prism 7 and 8 software (GraphPad Software).
Supporting information
(PDF)
a) Gel image following genomic isolation of DNA from fecal samples and PCR of the tcdA gene using the internal primers tcdA int F/tcdA int R. The absence of a 500bp product indicates ΔtcdA isolate. b) Gel image following genomic isolation of DNA from fecal samples and PCR of the GTD of tcdB using GTD diag F/R primers. Strain labels: C. difficile 630Δerm (wild-type) cages 1 and 2; C. difficile 630ΔermΔtcdA (ΔtcdA) cages 1 and 2; C. difficile 630ΔermΔtcdA GTD::D270N (ΔtcdA TcdB-GTD) cages 1 and 2. c) Sequence alignment of the GTD region of tcdB for C. difficile 630ΔermΔtcdA GTD::D270N with the wild-type reference sequence of 630Δerm. The gac-aat substitution is highlighted in a red box.
(PDF)
Terminal burden (heat-resistant colony-forming units/g HR-CFU/g) of C. difficile for uninfected, WT, ΔtcdA and TcdB-GTD infection groups. Spores were isolated from fecal samples at the day of experimental end-point for each animal subject. Since the burden was determined at different time-points for each animal subject, it is not appropriate to perform statistical analyses for these data.
(PDF)
Acknowledgments
We thank A. Hryckowian (Department of Medicine, University of Wisconsin-Madison) and members of the Sonnenburg lab (Department of Microbiology and Immunology, Stanford University) for helpful discussions regarding the murine model of infection.
Data Availability
Sequencing reads were deposited to the NCBI Sequencing Read Archive under accession number PRJNA623295.
Funding Statement
This work was funded by the BBSRC Nottingham-Rothamsted Doctoral training partnership (grant no. BB/J014508.1), the Marie Skłodowska-Curie ITN, CLOSPORE (grant no. 642068), the NIHR Nottingham BRC (Reference no. BRC-1215-20003), the National Institutes of Health (grant R56 AI127455), the Stanford University Medical Scientist Training Program (to MG) and through an industry-partnered collaborative research operating grant between Canadian Institutes of Health Research and Merck & Company (RN171835 – 286650). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Lawson PA, Citron DM, Tyrrell KL, Finegold SM. Reclassification of Clostridium difficile as Clostridioides difficile (Hall and O'Toole 1935) Prevot 1938. Anaerobe. 2016;40:95–9. Epub 2016/07/03. 10.1016/j.anaerobe.2016.06.008 . [DOI] [PubMed] [Google Scholar]
- 2.Lessa FC, Mu Y, Bamberg WM, Beldavs ZG, Dumyati GK, Dunn JR, et al. Burden of Clostridium difficile infection in the United States. The New England journal of medicine. 2015;372 10.1056/NEJMoa1408913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kelly CP, LaMont JT. Clostridium difficile—more difficult than ever. The New England journal of medicine. 2008;359(18):1932–40. Epub 2008/10/31. 10.1056/NEJMra0707500 . [DOI] [PubMed] [Google Scholar]
- 4.Kuehne SA, Collery MM, Kelly ML, Cartman ST, Cockayne A, Minton NP. Importance of toxin A, toxin B, and CDT in virulence of an epidemic Clostridium difficile strain. The Journal of infectious diseases. 2014;209(1):83–6. 10.1093/infdis/jit426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuehne SA, Cartman ST, Heap JT, Kelly ML, Cockayne A, Minton NP. The role of toxin A and toxin B in Clostridium difficile infection. Nature. 2010;467(7316):711–3. 10.1038/nature09397 . [DOI] [PubMed] [Google Scholar]
- 6.Imwattana K, Knight DR, Kullin B, Collins DA, Putsathit P, Kiratisin P, et al. Clostridium difficile ribotype 017—characterization, evolution and epidemiology of the dominant strain in Asia. Emerg Microbes Infect. 2019;8(1):796–807. 10.1080/22221751.2019.1621670 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yuan P, Zhang H, Cai C, Zhu S, Zhou Y, Yang X, et al. Chondroitin sulfate proteoglycan 4 functions as the cellular receptor for Clostridium difficile toxin B. Cell research. 2015;25(2):157–68. 10.1038/cr.2014.169 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tao L, Zhang J, Meraner P, Tovaglieri A, Wu X, Gerhard R, et al. Frizzled proteins are colonic epithelial receptors for C. difficile toxin B. Nature. 2016;538(7625):350–5. 10.1038/nature19799 http://www.nature.com/nature/journal/v538/n7625/abs/nature19799.html#supplementary-information. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.LaFrance ME, Farrow MA, Chandrasekaran R, Sheng J, Rubin DH, Lacy DB. Identification of an epithelial cell receptor responsible for Clostridium difficile TcdB-induced cytotoxicity. Proc Natl Acad Sci U S A. 2015;112(22):7073–8. Epub 2015/06/04. 10.1073/pnas.1500791112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Orrell KE, Zhang Z, Sugiman-Marangos SN, Melnyk RA. Clostridium difficile toxins A and B: Receptors, pores, and translocation into cells. Critical reviews in biochemistry and molecular biology. 2017;52(4):461–73. Epub 2017/05/27. 10.1080/10409238.2017.1325831 . [DOI] [PubMed] [Google Scholar]
- 11.Reineke J, Tenzer S, Rupnik M, Koschinski A, Hasselmayer O, Schrattenholz A, et al. Autocatalytic cleavage of Clostridium difficile toxin B. Nature. 2007;446(7134):415–9. Epub 2007/03/06. 10.1038/nature05622 . [DOI] [PubMed] [Google Scholar]
- 12.Qa'Dan M, Ramsey M, Daniel J, Spyres LM, Safiejko-Mroczka B, Ortiz-Leduc W, et al. Clostridium difficile toxin B activates dual caspase-dependent and caspase-independent apoptosis in intoxicated cells. Cellular microbiology. 2002;4(7):425–34. Epub 2002/07/10. 10.1046/j.1462-5822.2002.00201.x . [DOI] [PubMed] [Google Scholar]
- 13.Chumbler NM, Farrow MA, Lapierre LA, Franklin JL, Haslam DB, Goldenring JR, et al. Clostridium difficile Toxin B causes epithelial cell necrosis through an autoprocessing-independent mechanism. PLoS pathogens. 2012;8(12):e1003072 Epub 2012/12/14. 10.1371/journal.ppat.1003072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Farrow MA, Chumbler NM, Lapierre LA, Franklin JL, Rutherford SA, Goldenring JR, et al. Clostridium difficile toxin B-induced necrosis is mediated by the host epithelial cell NADPH oxidase complex. Proc Natl Acad Sci U S A. 2013;110(46):18674–9. Epub 2013/10/30. 10.1073/pnas.1313658110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wohlan K, Goy S, Olling A, Srivaratharajan S, Tatge H, Genth H, et al. Pyknotic cell death induced by Clostridium difficile TcdB: chromatin condensation and nuclear blister are induced independently of the glucosyltransferase activity. Cellular microbiology. 2014;16(11):1678–92. 10.1111/cmi.12317 [DOI] [PubMed] [Google Scholar]
- 16.Ng J, Hirota SA, Gross O, Li Y, Ulke-Lemee A, Potentier MS, et al. Clostridium difficile toxin-induced inflammation and intestinal injury are mediated by the inflammasome. Gastroenterology. 2010;139(2):542–52, 52 e1-3. 10.1053/j.gastro.2010.04.005 . [DOI] [PubMed] [Google Scholar]
- 17.Xu H, Yang J, Gao W, Li L, Li P, Zhang L, et al. Innate immune sensing of bacterial modifications of Rho GTPases by the Pyrin inflammasome. Nature. 2014;513(7517):237–41. 10.1038/nature13449 . [DOI] [PubMed] [Google Scholar]
- 18.Li S, Shi L, Yang Z, Zhang Y, Perez-Cordon G, Huang T, et al. Critical roles of Clostridium difficile toxin B enzymatic activities in pathogenesis. Infection and immunity. 2015;83(2):502–13. Epub 11/17. 10.1128/IAI.02316-14 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang Z, Zhang Y, Huang T, Feng H. Glucosyltransferase activity of Clostridium difficile Toxin B is essential for disease pathogenesis. Gut microbes. 2015;6(4):221–4. Epub 2015/06/20. 10.1080/19490976.2015.1062965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ng YK, Ehsaan M, Philip S, Collery MM, Janoir C, Collignon A, et al. Expanding the Repertoire of Gene Tools for Precise Manipulation of the Clostridium difficile Genome: Allelic Exchange Using pyrE Alleles. PloS one. 2013;8(2):e56051 10.1371/journal.pone.0056051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bilverstone TW, Kinsmore NL, Minton NP, Kuehne SA. Development of Clostridium difficile R20291ΔPaLoc model strains and in vitro methodologies reveals CdtR is required for the production of CDT to cytotoxic levels. Anaerobe. 2017;44:51–4. 10.1016/j.anaerobe.2017.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pathak AK, Pathak V, Suling WJ, Riordan JR, Gurcha SS, Besra GS, et al. Synthesis of deoxygenated alpha(1—>5)-linked arabinofuranose disaccharides as substrates and inhibitors of arabinosyltransferases of Mycobacterium tuberculosis. Bioorg Med Chem. 2009;17(2):872–81. Epub 2008/12/06. 10.1016/j.bmc.2008.11.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen X, Katchar K, Goldsmith JD, Nanthakumar N, Cheknis A, Gerding DN, et al. A mouse model of Clostridium difficile-associated disease. Gastroenterology. 2008;135(6):1984–92. Epub 2008/10/14. 10.1053/j.gastro.2008.09.002 . [DOI] [PubMed] [Google Scholar]
- 24.Buckley AM, Spencer J, Maclellan LM, Candlish D, Irvine JJ, Douce GR. Susceptibility of hamsters to Clostridium difficile isolates of differing toxinotype. PloS one. 2013;8(5):e64121 Epub 2013/05/25. 10.1371/journal.pone.0064121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams DR, Young DI, Young M. Conjugative plasmid transfer from Escherichia coli to Clostridium acetobutylicum. Journal of general microbiology. 1990;136(5):819–26. Epub 1990/05/01. 10.1099/00221287-136-5-819 . [DOI] [PubMed] [Google Scholar]
- 26.Hussain HA, Roberts AP, Mullany P. Generation of an erythromycin-sensitive derivative of Clostridium difficile strain 630 (630Deltaerm) and demonstration that the conjugative transposon Tn916DeltaE enters the genome of this strain at multiple sites. Journal of medical microbiology. 2005;54(Pt 2):137–41. Epub 2005/01/28. 10.1099/jmm.0.45790-0 . [DOI] [PubMed] [Google Scholar]
- 27.Demian WL, Persaud A, Jiang C, Coyaud E, Liu S, Kapus A, et al. The Ion Transporter NKCC1 Links Cell Volume to Cell Mass Regulation by Suppressing mTORC1. Cell Rep. 2019;27(6):1886–96 e6. Epub 2019/05/09. 10.1016/j.celrep.2019.04.034 . [DOI] [PubMed] [Google Scholar]
- 28.Cowardin CA, Buonomo EL, Saleh MM, Wilson MG, Burgess SL, Kuehne SA, et al. The binary toxin CDT enhances Clostridium difficile virulence by suppressing protective colonic eosinophilia. Nature Microbiology. 2016;1:16108 10.1038/nmicrobiol.2016.108 http://www.nature.com/articles/nmicrobiol2016108#supplementary-information. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cartman ST, Minton NP. A mariner-Based Transposon System for In Vivo Random Mutagenesis of Clostridium difficile. Applied and environmental microbiology. 2010;76(4):1103–9. 10.1128/AEM.02525-09 PMC2820977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kuehne SA, Dempster AW, Collery MM, Joshi N, Jowett J, Kelly ML, et al. Characterization of the impact of rpoB mutations on the in vitro and in vivo competitive fitness of Clostridium difficile and susceptibility to fidaxomicin. The Journal of antimicrobial chemotherapy. 2018;73(4):973–80. Epub 2017/12/19. 10.1093/jac/dkx486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bouillaut L, McBride SM, Sorg JA. Genetic manipulation of Clostridium difficile. Curr Protoc Microbiol. 2011;Chapter 9:Unit-9A.2. 10.1002/9780471729259.mc09a02s20 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zoetendal EG, Akkermans AD, De Vos WM. Temperature gradient gel electrophoresis analysis of 16S rRNA from human fecal samples reveals stable and host-specific communities of active bacteria. Applied and environmental microbiology. 1998;64(10):3854–9. 10.1128/AEM.64.10.3854-3859.1998 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pawlowski SW, Calabrese G, Kolling GL, Platts-Mills J, Freire R, AlcantaraWarren C, et al. Murine model of Clostridium difficile infection with aged gnotobiotic C57BL/6 mice and a BI/NAP1 strain. The Journal of infectious diseases. 2010;202(11):1708–12. Epub 2010/10/26. 10.1086/657086 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG. Improving bioscience research reporting: The ARRIVE guidelines for reporting animal research. J Pharmacol Pharmacother. 2010;1(2):94–9. Epub 2011/02/26. 10.4103/0976-500X.72351 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
a) Gel image following genomic isolation of DNA from fecal samples and PCR of the tcdA gene using the internal primers tcdA int F/tcdA int R. The absence of a 500bp product indicates ΔtcdA isolate. b) Gel image following genomic isolation of DNA from fecal samples and PCR of the GTD of tcdB using GTD diag F/R primers. Strain labels: C. difficile 630Δerm (wild-type) cages 1 and 2; C. difficile 630ΔermΔtcdA (ΔtcdA) cages 1 and 2; C. difficile 630ΔermΔtcdA GTD::D270N (ΔtcdA TcdB-GTD) cages 1 and 2. c) Sequence alignment of the GTD region of tcdB for C. difficile 630ΔermΔtcdA GTD::D270N with the wild-type reference sequence of 630Δerm. The gac-aat substitution is highlighted in a red box.
(PDF)
Terminal burden (heat-resistant colony-forming units/g HR-CFU/g) of C. difficile for uninfected, WT, ΔtcdA and TcdB-GTD infection groups. Spores were isolated from fecal samples at the day of experimental end-point for each animal subject. Since the burden was determined at different time-points for each animal subject, it is not appropriate to perform statistical analyses for these data.
(PDF)
Data Availability Statement
Sequencing reads were deposited to the NCBI Sequencing Read Archive under accession number PRJNA623295.