Abstract
Background
The public awareness toward the causes and consequences of antibiotic resistance (AR) is crucial to mitigate the inappropriate use of antibiotics (ABs), particularly in the low- and middle-income countries. There was no previous study that assessed the awareness, attitude, and knowledge about antibiotic use and AR among the Jordanian public in affluent and deprived areas.
Objective
This study aimed to assess the awareness, attitude, and knowledge about antibiotic use and AR in affluent and deprived areas in Jordan.
Setting
The survey was conducted in November 2019 in Amman, the capital of Jordan.
Method
A cross-sectional questionnaire was used to survey households in their areas in each of West Amman (affluent region) and East Amman (deprived region), Households were selected using proportionate random sampling method.
Results
A total of 620 householders (310 per area) completed the questionnaire. Pharmacists were perceived as strong influencers on householders’ decision, as 80.32% (n = 465/580) of those who used antibiotics in the last year follow pharmacists’ advice. Our results showed poor understanding of antibiotic usage among the Jordanian public, as only 14.2% (n = 44/310) of the sample in West Amman and 2.9% (n = 9/310) in East Amman disagreed with the statement “Antibiotics work on most coughs and colds.” Householders in West Amman showed much better understanding of AR compared to those in East Amman; 82.3% (n = 255/310) of West Amman respondents agreed with the statement “Antibiotic resistance occurs when bacteria change in some way that reduces or eliminates the effectiveness of the antibiotic.” compared to 31.9% (n = 99/310) of East Amman respondents on the same statement (P < .05).
Conclusion
The Jordanian community generally had poor knowledge and awareness toward antibiotics use and AR. Socio-economic factors could influence the public’s attitude toward antibiotics use and AR.
Keywords: antibiotic resistance, attitude, Jordan, self-medicating, public awareness
Introduction
Antibiotic resistance (AR) is a global healthcare concern1,2; it is attributed to multiple factors, such as rare discoveries of novel antibiotics3,4 and antibiotics misuse.5 Appropriate use of antibiotics is vital for management of AR,6 and patients’ demands and self-treatment of antibiotics are also key contributing factors to overusing and consequently developing resistance of antibiotics.5,7,8 Some developed countries, such as Australia, USA, Canada and most of the European countries have launched awareness-raising campaigns as a global cooperation against AR.9 Some studies have also focused on assessing the public knowledge and awareness toward AR.10-12
A study conducted in the UK showed that the public in poor areas had lack of knowledge on antibiotic usage compared to those in affluent areas.5 Another UK study showed that 38% of the public thought antibiotics are effective against most types of cough or colds and 43% did not know that antibiotics have an effect on normal flora.10 In Sweden, participants were confused about the difference between viruses and bacteria, and around 20% of them thought that antibiotics cure common colds.13 In Italy, only 9.8% of the public defined AR accurately and based on the study, predictors for taking antibiotics without a prescription were found to be age, and the belief that antibiotics are indicated for treating common cold.12 In Malaysia, the majority confused viral and bacterial infections and they did not know that antibiotics are not effective against common cold.14 In Hong Kong; however, results showed adequate knowledge and appropriate behaviour regarding antibiotics use. In the Arab world, around two thirds of the Jordanian community thought that antibiotics treat common cold and cough,8 and around half of participants in Kuwait had low knowledge on use of antibiotics and AR.15 In Jordan, community pharmacies are the most common pharmaceutical facilities in Jordan, and there are about 2500 pharmacies across the country. Community pharmacies provide a wide range of prescription and nonprescription medicines, as well as cosmetics, skincare products, and medical equipment. Pharmacies are highly accessible, and many patients, therefore, seek medical advice from pharmacists before visiting a physician.16 Therefore, ABs are easily accessible for the public since all pharmacies dispense ABs without prescription, and thus misuse of ABs among Jordanian public are expected to be high.17 Little is known about patient’s awareness and knowledge toward antibiotics use and resistance in different socio-economic areas in Jordan. This was the first study in the Middle East that investigated and compared the awareness, attitude and knowledge about antibiotics use and AR among the public residing in affluent and deprived areas.
Aim of the Study
This study aimed to assess the knowledge, attitude, and awareness about antibiotics use and AR in affluent and deprived areas in Jordan.
Method
Study Design and Population
This cross-sectional, researcher-administered survey was conducted in November 2019 in Amman, after receiving the institutional review board (IRB) approval from the University of Petra. Amman is the capital and most populous city of the Hashemite Kingdom of Jordan. The city can be divided based on socio-economic status of the population into: East Amman, the region of deprived people, where poverty and low health literacy are common, and West Amman where affluent people reside and householders have better healthcare services, education, and infrastructure, although the definitions of affluent and deprived neighborhoods are still arbitrary.18
The study population was the adult householders resided in either affluent (West Amman) or deprived region (East Amman) of the city. The household was defined as “one person or a group of people who have the accommodation as their only or main residence and for a group, either share at least one meal a day or share the living accommodation, that is, a living room or sitting room. People could be considered a household if they were related: full- or half-blood, foster, step-parent/child, in-laws, a married couple”.19
The study included those who were adults (18-70 years), mentally competent and able to listen and speak. An informed consent was obtained from each participant.
Sampling Scheme and Sample Size
Amman was generally categorized into 2 main regions (West and East), and each main region contained many areas. Firstly, 3 areas were selected from each region using random sampling. Secondly, the sample for each area was divided to districts depending on the number of households in each area. Finally, 1 household was selected randomly, and then every other 5th household was selected to be surveyed.
A proportion formula was adopted to calculate the sample size.20
Where, (Zα/2) is the critical value of the normal distribution at α/2 (eg, for a confidence level of 95%, α is 0.05, and the critical value is 1.96), MOE is the margin of error, (p) is the sample proportion, and (de) is the design effect for using multi-stage sampling taken as 1.5.
the sample size was 620 households distributed (Table 1) with 10% considered contingency.
Table 1.
Proportionate Random Sample of 620 Households From Regions in Amman.
| Region | Areas | Number of householders | Proportion | Sample size |
|---|---|---|---|---|
| West Amman | Abdoun | 141 | 22.74% | 310 |
| Khelda | 91 | 14.68% | ||
| TlaAlali | 78 | 12.58% | ||
| East Amman | Marka | 128 | 20.64% | 310 |
| Al Wehdat | 111 | 17.91% | ||
| Al Muqabalayn | 71 | 11.45% |
Questionnaire
The survey questionnaire was designed based on previously published and validated questionnaires about the knowledge and awareness of the general public about antibiotics use and AR with permission from the authors.5,8,14,15 New statements were also added in the questionnaire to enhance our understanding of the public attitude and knowledge about antibiotics use and AR.
The questionnaire included 4 parts with a total of 35 questions; 8 demographic and socio-economic questions, 4 statements about using antibiotics in the past, 15 questions assessed the participants’ knowledge on antibiotics use, action and resistance, and 8 questions measured respondents’ attitude toward antibiotics use and AR. The Arabic translated version of the questionnaire was used and validated to be suitable for researching the Jordanian population. The translation was validated by 2 bilingual linguistic experts from the University of Petra who applied cultural and linguistic validation. In order to ensure the practicality and comprehensibility of the questionnaire, a pilot study was performed using a group of 25 randomly chosen households; few modifications on the structure of the questionnaire were performed.
The survey was conducted by 3 trained researchers to collect the data from householders. The study was conducted in 2 regions; the first one involved the households of affluent areas of Amman (West Amman), where random areas of West Amman were chosen, and households of these areas interviewed face-to-face to complete the questionnaire by themselves. The second region involved the households of deprived areas of Amman (East Amman), where also random areas of East Amman were chosen, and households of these areas approached to answer the same questionnaire. For each house, only the householder was surveyed. Collected data were coded and entered into the electronic data sheet by the investigator (DAQ).
Data Analysis
Reliability test was conducted using Cronbach’s alpha test. The result of Cronbach’s alpha value was 0.71, indicated that the internal consistency between items of the questionnaire was considered acceptable according to Taber.21 Descriptive statistics were used to analyze the data and results were reported in frequency distribution tables and graphs. Inferential analysis, such as Pearson Chi-Square test (χ2) was used to compare the proportions between groups.
Multivariate logistic regression was used to identify predictors for good knowledge on antibiotics use. Choices of the dependent variables statement were “Yes” and “No” and people who answered (I do not know) were excluded. Independent variables were all statements in the demographic and personal information section. Predictors were tested against 2 knowledge statements; “Antibiotics work on most coughs and colds” to predict knowledge about antibiotic use and “An antibiotic will always be effective in the treatment of same infection in the future” to predict knowledge about antibiotic resistance. Both statements were chosen based on a committee decision, which included senior infectious disease consultant, senior otolaryngologist, and senior clinical pharmacist. The committee members chose 2 statements; the first one refers to the knowledge about antibiotic use, and the second refers to the knowledge about antibiotic resistance. The committee members rated all statements using rating scale (0-5), where 0 was considered completely irrelevant and 5 as completely relevant, then we calculated the mean for all statements; statements with the highest mean were chosen. To ensure reliability of our method, Kappa statistic was used to test interrater reliability. Value of kappa Below 0.5 was considered as bad reliability, above 0.5 and below 0.7 moderate reliability, Above 0.7 good, and above 0.8 great reliability.22 We found that raters’ judgments were close to each other by 91 % agreement (K = 0.91, P < .05). Therefore, the consistency between raters was excellent.
Results
A total of 711 householders were approached, 620 of them completed the questionnaire (87.2% response rate) in both West Amman (affluent area, n = 310) and East Amman (deprived area, n = 310). The majority of the 620 participants aged 18 to 30 years (47.9%, n = 297/620) and 31 to 40 years (26.61%, n = 165/620). More than half (58.71%, n = 364/620) of the included householders were males. Around one-third (32.74%, n = 203/620) of the participants had diploma degree or less and only 5.48%( n = 34/620) of them had MSc or PhD. Almost all included respondents (97.1%, n = 602/620) did not work or study in the medical field. The demographic and socio-economic features of the sample are summarized in Table 2.
Table 2.
Demographic Characteristics of Participants.
| Characteristic | Category | All participants | East Amman | West Amman |
|---|---|---|---|---|
| Age | 18-30 | 47.9% | 57.7% | 38.1% |
| 31-40 | 26.6% | 15.8% | 37.4% | |
| 41-50 | 20.6% | 22.3% | 19.0% | |
| >50 | 4.8% | 4.2% | 5.5% | |
| Gender | Male | 58.7% | 45.5% | 71.9% |
| Female | 41.3% | 54.5% | 28.1% | |
| Education level | Bachelor degree | 61.8% | 34.8% | 88.7% |
| MSc or PhD | 5.5% | 1.9% | 9% | |
| Diploma or less | 32.7% | 63.2% | 2.3% | |
| Monthly income | 1001-2000 JOD | 45.3% | 6.5% | 84.2% |
| More than 2000 JOD | 4.5% | 0.3% | 8.7% | |
| Less than 500 JOD | 50.2% | 93.2% | 7.1% | |
| Medical background | Yes | 2.9% | 1.3% | 4.5% |
| No | 97.1% | 98.7% | 95.5% | |
| Pharmacist or doctor in family | None | 89.5% | 96.1% | 82.9% |
| Pharmacist | 5.6% | 1.9% | 9.4% | |
| Doctor | 4.8% | 1.9% | 7.7% | |
| Medical insurance | Yes | 65.9% | 35.2% | (300, 96.8%) |
| No | 34.0% | 64.8% | (10, 3.2%) | |
| Chronic disease | Yes | 14.6% | 17.4% | 11.6% |
| No | 85.3% | 82.6% | 88.4% |
Prevalence of Using Antibiotics
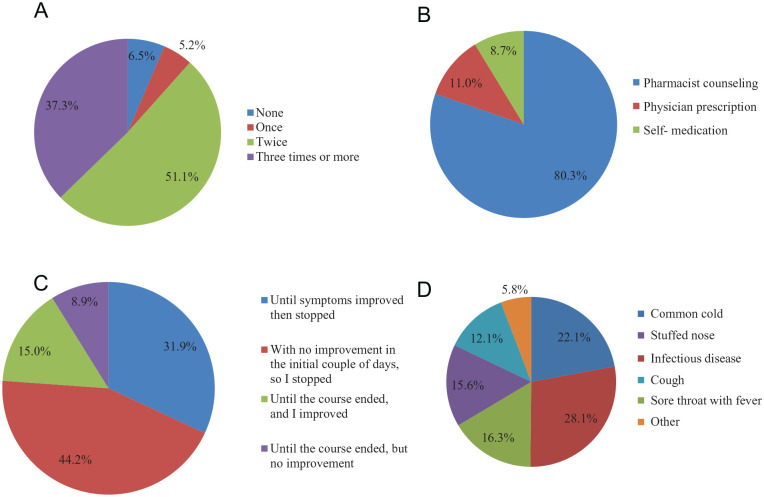
More than half (51.1%) of 620 householders used antibiotics at least twice in the last year and only 6.4% (n = 40/620) did not use antibiotics in the last year (Figure 1A); and most (80.2%, n = 465/580) of householders, who used antibiotics at least once in the last year, used antibiotic based on pharmacists’ counseling (Figure 1B). Around a quarter (22%, n = 128/580) of householders, who used antibiotics at least once in the last year, used antibiotic for common cold (Figure 1C). Around half (44.2%, n = 256/580) of householders, who used antibiotics at least once in the last year, stopped antibiotics courses after no improvement in the initial days of treatment (Figure 1D).
Figure 1.
Responses to the statements: (A) “During the last year, I used at least an antibiotic:”. (B) “During the last year, I used antibiotics based on:”. (C) “During the last year, I used antibiotics for:”. (D) “During the last year, I used antibiotics”.
Knowledge of Antibiotics Use and Resistance
As shown in Table 3, the majority (92.6%, n = 287/310) of the participants in West Amman displayed better understanding by disagreeing with the statement “Antibiotics are effective against viral infections” compared with 5.8% (n = 18/310) in East Amman (P < .05). Both groups of respondents possessed comparatively poor knowledge as only 6.5% (n = 20/310) in West Amman and 24.2% (n = 75/310) in East Amman knew about the negative effect of using antibiotics among animals.
Table 3.
Knowledge on Antibiotic Use and Resistance.
| Statements (correct response) | West Amman (n = 310) | East Amman (n = 310) | P value |
|---|---|---|---|
| Antibiotics are effective against viral infections (No) | 92.6 % | 5.8% | <.05 |
| Antibiotics are effective against bacterial infections (Yes) | 95.8% | 98.4% | >.05 |
| Antibiotics can kill the bacteria that normally live on the skin and in the gut (Yes) | 92.3% | 10.6% | <.05 |
| An antibiotic will always be effective in the treatment of same infection in the future (No) | 27.1% | 2.9% | >.05 |
| Antibiotics work on most coughs and colds (No) | 14.2% | 2.9% | >.05 |
| Antibiotics increase the speed of recovery from colds (No) | 8.7% | 2.6% | >.05 |
| Antibiotics are effective against fungal infections (No) | 68.1% | 3.2% | <.05 |
| Expensive antibiotics are more effective than cheaper ones (No) | 38.1% | 1.6% | <.05 |
| If you get side effects (nausea, diarrhea, etc) during a course of antibiotics treatment, you should stop taking them as soon as possible, without consulting your doctor or pharmacist (No) | 14.8% | 1.3% | >.05 |
| If you get allergy side effects (rash, shortness of breath, etc) during a course of antibiotics treatment, you should stop taking them as soon as possible, without consulting your doctor or pharmacist (Yes) | 100% | 100% | No difference |
| Antibiotics can cause imbalance in the body’s own bacterial flora (Yes) | 89.7% | 24.2% | <.05 |
| The overuse of antibiotics is the most important reason for increasing the resistance of bacteria to them (Yes) | 93.9% | 90.6% | >.05 |
| Patients, who do not continue their antibiotic course, are the prime reason for the resistance of bacteria (No) | 5.5% | 13.2% | >.05 |
| The use of antibiotics among animals can reduce the effect of antibiotics among humans (Yes) | 6.5% | 24.2% | >.05 |
| Antibiotic resistance occurs when bacteria change in some way that reduces or eliminates the effectiveness of the antibiotic (Yes) | 82.3% | 31.9% | <.05 |
Both groups showed poor knowledge as only 14.2% (n = 44/310) of the sample in West Amman and 2.9% (n = 9/310) in East Amman disagreed with the statement “Antibiotics work on most coughs and colds.” Respondents in West Amman showed a much better understanding on antibiotic usage and how the AR can occur compared to those in East Amman; 82.3% (n = 255/310) of the West Amman respondents agreed with the statement “Antibiotic resistance occurs when bacteria change in some way that reduces or eliminates the effectiveness of the antibiotic.” and 68.1% (n = 211/310) of them disagreed with the statement “Antibiotics are effective against fungal infections” compared to 31.9% (n = 99/310) and 3.2% (n = 10/310) of the East Amman respondents on the same statements, respectively (P < .05).
Attitude About Antibiotics Use and Resistance
There was a huge difference in attitude toward antibiotics use and AR between the participants in West Amman and East Amman (Table 4). Regarding sharing antibiotics with friends and relatives without medical consulting, there was a significantly higher proportion of participants strongly disagreeing and disagreeing with “It is good to be able to get antibiotics from relatives or friends without having to see a medical doctor” between West Amman and East Amman (98.7% vs 6.1%; P < .05).
Table 4.
Attitude Toward Antibiotic Use.
| Statements (correct response) | West Amman (n = 310) | East Amman (n = 310) | P value |
|---|---|---|---|
| I always complete the course of treatment with antibiotics even if I feel better (Strongly disagree/Disagree) | 2.9% | 79.4% | <.05 |
| It is good to be able to get antibiotics from relatives or friends without having to see a medical doctor (Strongly disagree/Disagree) | 98.7% | 6.1 % | <.05 |
| I prefer to be able to buy antibiotics from the pharmacy without a prescription (Strongly disagree/Disagree) | 91.3 % | 0.3 % | <.05 |
| The pharmacist is professionally capable of giving me the appropriate antibiotic for my case (Strongly agree/Agree) | 79.4% | 99.7% | >.05 |
| I prefer to keep antibiotics at home in case there may be a need for them later (Strongly disagree/Disagree) | 0.3 % | 0.3% | No Difference |
| When I have a sore throat, I prefer to use an antibiotic from day 1 (Strongly disagree/Disagree) | 95.8 % | 2.9% | <.05 |
| When I have fever, I prefer to use an antibiotic from day 1 (Strongly disagree/Disagree) | 95.8% | 9.7% | <.05 |
| If the prescribed antibiotic is costly, I will ask the pharmacist to change it to a cheaper one (Strongly disagree/Disagree) | 95.8% | 4.5% | <.05 |
Predictors of Good Knowledge About Antibiotics Use and AR
The odds of people agreement on the statement “Antibiotics work on most coughs and colds” were 4.65 times more likely in householders who lived in East Amman (OR 4.65; 95% CI: 3.12, 7.68; P = .001) compared with those who lived in the West. There were no significant predictors for this statement “An antibiotic will always be effective in the treatment of same infection in the future.” The results showed no chance for multicollinearity (all VIFs <3.00), our regression analysis process was accurate and specific.
Discussion
Even though public awareness and knowledge about antibiotics use and AR is a major healthcare issue, it has been rarely studied. In fact, this study was the first in the Middle East that aimed to investigate knowledge, attitude and awareness of Jordanian public toward antibiotics use and AR in affluent areas (West Amman) compared to deprived areas (East Amman).
Our sample was representative and provided us with comprehensive outcomes about householders in Amman. More than half 58.71% of our respondents were males and around half of them aged between 18 and 30 years. Around one-third 32.7% of the participants had diploma degree or less and only 5.48% of them had MSc or PhD. Also, the minority of our householders had medical education. Most of our results were consistent with the latest demographic data about Amman, which were released by Knoema Enterprise Data Solutions. According to these data, males accounted for 53.7% of the public, one third 30.0% of the population have low education level, and only 3.8% of students are in medical schools.23
Overall, the public residing in West Amman possessed better knowledge on and understanding of AR problems and antibiotics usage, compared to those in East Amman.
Our study adopted a reliable method for evaluating the public attitude and knowledge using a pre-validated questionnaire.5,8,14,15 Similar to our study, Mason et al5 targeted the public in both deprived and affluent areas of London. However, other studies conducted in Jordan, Kuwait, Sweden, Hong Kong and Malaysia targeted the public in general.8,11,14,15,24 Therefore, their findings did not focus on how much the socio-economic factors would influence the public’s awareness of using medications.
This was consistent with the results of a survey study conducted in Jordan around 10 years ago by Shehadeh et al.8 The public in Sweden and the UK showed better understanding than ours toward antibiotics usage, as around 20% and 38% of the Swedish and British communities, respectively, thought antibiotics work on cough.10,13 In Mongolia, most of respondents had lack of knowledge on antibiotic use.25 Lack of awareness campaigns towards the consequences of inappropriate use of antibiotics may well be the reason for our findings among the Jordanian public. Antibiotics were prescribed or dispensed for inappropriate reasons in Jordan.26-28
The vast majority of the Jordanian public and the British public thought that the overuse and underuse of antibiotics can contribute to the AR. Moreover, In Malaysia, more than half of participants were aware that overuse of antibiotics is the major causative factor for AR.24 Although debatable, to date there has been no robust scientific evidence supporting the current belief that stopping the antibiotic before the scheduled course end date would increase the chance of antibiotics resistance to bacteria.29 In Jordan, self-medication is common.30,31
In terms of practice, the role of pharmacists needs mentioning. They seem to have an important role to play in contributing to public knowledge about appropriate antibiotics treatment and AR, as the majority of the respondents stated that they used antibiotics based on reliable pharmacists counseling. The role of pharmacists’ independent prescribing of antibiotics should be regulated and monitored; in addition, pharmacists should receive continual professional development programmes to equip them with the proper clinical skills and knowledge on diagnosing and treating common upper respiratory tract infections in the community settings.
Our study had 2 major limitations. Firstly, our findings may not be representative of all Jordanian public. Also, the respondent’s opinion might not be closely related to the rest of the family members’ beliefs. However, Amman being the capital city has cultural diversity as it has residents from different areas of Jordan. Secondly, our study was a cross-sectional study, and therefore, it did not reflect any change in householders’ attitudes over time. Validated comparison of our findings with those in the literature is difficult. This is because the results may vary significantly among studies. This is due to the absence of a unified methodology approach, and the cultural and ethnical differences, and the diverse socio-demographics of study populations.
Conclusion
A lack of understanding about antibiotics effectiveness and AR existed in the Jordanian community particularly in deprived areas. Increased previous antibiotics use among those believing antibiotics to be effective for viral illnesses suggests that public awareness and professional practice monitoring are required about antibiotics usage.
Acknowledgments
We thank the University of Petra for facilitating our research.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: As the study involved confidential data, approval was obtained from the Institutional Review Board (IRB) at the University of Petra.
ORCID iDs: Derar H. Abdel-Qader  https://orcid.org/0000-0003-2576-4464
https://orcid.org/0000-0003-2576-4464
Najlaa Saadi Ismael  https://orcid.org/0000-0003-0858-6686
https://orcid.org/0000-0003-0858-6686
Osama Mohamed Ibrahim  https://orcid.org/0000-0002-2868-039X
https://orcid.org/0000-0002-2868-039X
References
- 1. Ventola CL. The antibiotic resistance crisis: causes and threats. P&T. 2015;40:277-283. [PMC free article] [PubMed] [Google Scholar]
- 2. Sengupta S, Chattopadhyay MK, Grossart HP. The multifaceted roles of antibiotics and antibiotic resistance in nature. Front Microbiol. 2013;4:1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Michael CA, Dominey-Howes D, Labbate M. The antimicrobial resistance crisis: causes, consequences, and management. Front Public Health. 2014;2:145 http://journal.frontiersin.org/article/10.3389/fpubh.2014.00145/abstract [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rather IA, Kim BC, Bajpai VK, Park YH. Self-medication and antibiotic resistance: crisis, current challenges, and prevention. Saudi J Biol Sci. 2017;24:808-812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mason T, Trochez C, Thomas R, Babar M, Hesso I, Kayyali R. Knowledge and awareness of the general public and perception of pharmacists about antibiotic resistance. BMC Public Health. 2018;18:711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Howard SJ, Catchpole M, Watson J, Davies SC. Global collaboration to encourage prudent antibiotic use. Lancet Infect Dis. 2013;13:1003-1004. [DOI] [PubMed] [Google Scholar]
- 7. Goossens H, Ferech M, Vanderstichele R, Elseviers M. Outpatient antibiotic use in Europe and association with resistance: a retrospective database study. Lancet. 2005;365:579-587. [DOI] [PubMed] [Google Scholar]
- 8. Shehadeh M, Suaifan G, Darwish RM, Wazaify M, Zaru L, Alja S. Knowledge, attitudes and behavior regarding antibiotics use and misuse among adults in the community of Jordan. A pilot study. Saudi Pharm J. 2012;20:125-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Earnshaw S, Mancarella G, Mendez A, Todorova B, Magiorakos AP, Possenti E. European Antibiotic Awareness Day: a five-year perspective of Europe-wide actions to promote prudent use of antibiotics. Euro Surveill. 2014;19:20928. [DOI] [PubMed] [Google Scholar]
- 10. Mcnulty CAM, Boyle P, Nichols T, Clappison P, Davey P. Don’t wear me out—the public’s knowledge of and attitudes to antibiotic use. J Antimicrob Chemother. 2007;59:727-738. [DOI] [PubMed] [Google Scholar]
- 11. You JHS, Yau B, Choi KC, Chau CTS, Huang QR, Lee SS. Public knowledge, attitudes and behavior on antibiotic use: a telephone survey in Hong Kong. Infection. 2008;36:153-157. [DOI] [PubMed] [Google Scholar]
- 12. Napolitano F, Izzo MT, Di Giuseppe G, Angelillo IF. Public knowledge, attitudes, and experience regarding the use of antibiotics in Italy. PLoS One. 2013;8:e84177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. André M, Vernby Å̊, Berg J, Lundborg CS. A survey of public knowledge and awareness related to antibiotic use and resistance in Sweden. J Antimicrob Chemother. 2010;65:1292-1296. [DOI] [PubMed] [Google Scholar]
- 14. Ka Keat L, Chew Charn T. A cross sectional study of public knowledge and attitude towards antibiotics in Putrajaya, Malaysia. South Med Rev. 2012;5:26-33. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3606936/ [PMC free article] [PubMed] [Google Scholar]
- 15. Awad AI, Aboud EA. Knowledge, attitude and practice towards antibiotic use among the public in Kuwait. PLoS One. 2015;10:e0117910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nazer LH, Tuffaha H. Health care and pharmacy practice in Jordan. Can J Hosp Pharm. 2017;70:150-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Albsoul-Younes A, Wazaify M, A-Myal T. Abuse and Misuse of Prescription and Nonprescription Drugs Sold in Community Pharmacies in Jordan. Subst Use Misuse. 2010;45(9):1319-29. [DOI] [PubMed] [Google Scholar]
- 18. Solari CD. Affluent neighborhood persistence and change in U.S. cities. City Community. 2014;11:370-388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pierson J, Thomas M. Collins Dictionary of Social Work. HarperCollins; 2006. 616 pp. [Google Scholar]
- 20. Daniel WW, Cross CL. Biostatistics: A Methodology for the Health Sciences. 2nd ed., Vol. 10 John Wiley & Sons; 2013. [Google Scholar]
- 21. Taber KS. The use of Cronbach’s alpha when developing and reporting research instruments in science education. Res Sci Educ. 2016;48:1273-1296. [Google Scholar]
- 22. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med. 2012;22:276-282. [PMC free article] [PubMed] [Google Scholar]
- 23. Knoema Enterprise Data Solutions. Amman demographics. https://ar.knoema.com/atlas/الأردن/Amman
- 24. Ka Keat L, Chew Charn T. A cross sectional study of public knowledge and attitude towards antibiotics in Putrajaya, Malaysia. South Med Rev. 2012;5:26-33. [PMC free article] [PubMed] [Google Scholar]
- 25. Togoobaatar G, Ikeda N, Ali M, Sonomjamts M, Dashdemberel S. Survey of non-prescribed use of antibiotics for children in an urban community in Mongolia. Bull World Health Organ. 2010;88:930-936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Abdel-Qader DH, Ismael NS, Al Meslamani AZ, et al. The role of clinical pharmacy in preventing prescribing errors in the emergency department of a governmental hospital in Jordan: a pre-post study [published online July 25, 2020]. Hosp Pharm. doi: 10.1177/0018578720942231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Abdel-Qader DH, Al Meslamani AZ, El-Shara’ AA, et al. Investigating prescribing errors in the emergency department of a large governmental hospital in Jordan [published online August 31, 2020]. J Pharm Health Serv Res. doi: 10.1111/jphs.12376 [DOI] [Google Scholar]
- 28. Abdel-Qader DH, Al Meslamani AZ, Lewis PJ, Hamadi S. Incidence, nature, severity, and causes of dispensing errors in community pharmacies in Jordan [published online August 17, 2020]. Int J Clin Pharmacol. doi: 10.1007/s11096-020-01126-w [DOI] [PubMed] [Google Scholar]
- 29. Darwin E, Gorton C. The antibiotic course has had its day. BMJ. 2017;2017:358. [DOI] [PubMed] [Google Scholar]
- 30. Abdel-Qader DH, Albassam A, Ismael NS, et al. Herbal medicine use in the Jordanian population: a nationally representative cross-sectional survey. J Pharm Pharmacogn Res. 2020;8:525-536. http://jppres.com/jppres/herbal-medicine-use-in-the-jordanian-population/ [Google Scholar]
- 31. Abdel-Qader DH, Al Meslamani AZ. Knowledge and beliefs of Jordanian community toward e-cigarettes: a national survey [published online August 9, 2020]. J Community Health. doi: 10.1007/s10900-020-00896-8 [DOI] [PubMed] [Google Scholar]