Abstract
In undergraduate and postgraduate medical education, mentoring offers personalized training and plays a key role in continuing medical education and the professional development of healthcare professionals. However, poor structuring of the mentoring process has been attributed to failings of the host organization and, as such, we have conducted a scoping review on the role of the host organization in mentoring programs. Guided by Levac et al’s methodological framework and a combination of thematic and content analysis, this scoping review identifies their “defining” and secondary roles. Whilst the “defining” role of the host is to set standards, nurture, and oversee the mentoring processes and relationships, the secondary roles comprise of supporting patient care and specific responsibilities toward the mentee, mentor, program, and organization itself. Critically, striking a balance between structure and flexibility within the program is important to ensure consistency in the mentoring approach whilst accounting for the changing needs and goals of the mentees and mentors.
Keywords: Host organization, mentoring, medical education, mentors, mentees, continuing medical education, continuing professional development
Introduction
Mentoring boasts many benefits. Through the provision of personalized training, learning and support, mentoring facilitates “the process by which health professionals keep updated to meet the needs of patients, the health service, and their own professional development.”1 Indeed, it not only enhances the academic, research, clinical, and personal development of both mentors and mentees, it also improves patient outcomes and boosts the reputation of the host organization managing the mentoring program (henceforth, the host).2-25 By providing opportunities for mentors and mentees to develop their social, personal, leadership, and managerial competencies,26 mentoring plays an integral part in the continuing medical education (CME) and continuing professional development (CPD) of physicians, nurses, and health professionals from the various allied health specialities.27-29
However, lapses in support and oversight of the mentor-mentee matching process, the nurturing of relationships between the mentee, mentor and the host organization, and the cultivation of a positive mentoring environment has hindered its full potential.28-36 With 2 recent reviews30,31 attributing ethical issues such as bullying and misappropriation of the mentee’s work to neglect on the part of the host, it is critical to scrutinize their role in mentoring programs.32-41
Studying mentoring
A dearth of data on the role of the host in mentoring has been attributed to a number of issues.1-20 Perhaps most significant has been the failure of many reviews in acknowledging and contending with the impact of mentoring’s evolving, entwined, context-specific, goal-sensitive, mentee-, mentor-, relationship-, and host-dependent nature.42-49 This suggests that peer, near-peer, group, mosaic, network, leadership, patient, youth, family, and e-mentoring should not be mistakenly conflated nor intermixed with preceptorship, supervision, role modeling, and networking which have their own specific approach and role in education and training.41 Acknowledging mentoring’s context specific nature, this review will focus on the role of the host in novice mentoring which is defined as the “dynamic, context-dependent, goal-sensitive, mutually beneficial relationship between an experienced clinician and junior clinicians and/or undergraduates focused upon advancing the development of the mentee.”50 Novice mentoring is the dominant form of mentoring in medical education.51-60
Methods
Design
A systematic scoping review was adopted to identify “the central sources and forms of evidence available” on host organzations.42 The flexible nature of a scoping review allows systematic extraction, synthesis,43 and summarizing44 of actionable and applicable information across a diverse range of study formats and settings. This circumnavigates the limitations posed by mentoring’s nature45-50 and a paucity of articles on host organizations.51-54
Levac et al’s55 adaptations of Arksey and O’Malley’s42 methodological framework for conducting scoping reviews was adopted to systematically study the potential size, gaps, and scope of available literature on host organizations in novice mentoring.56-60 The PRISMA-P 2015 checklist was used to develop the protocol for this study.61
Guided by local clinicians, educators, researchers, librarians (henceforth, the expert team), and prevailing reviews of CPD practices, the 8-member research team determined the primary research question to be “what is known about the role of the host organization in novice mentoring—particularly in Internal Medicine and its subspecialties as delineated by the American College of Physicians?”62 The secondary research question was then determined to be “what would make an effective host organization in these disciplines?” Narrowing this scoping review’s focus on novice mentoring in Internal Medicine was largely determined by the amount of prevailing data already present in the field of mentoring in undergraduate and postgraduate medical education. These questions were designed on the PCC (population, concept, and context) elements of the inclusion criteria63,64 and presented in a PICOS format (Table 1).
Table 1.
PICOs, inclusion criteria and exclusion criteria applied to database search.
| PICOS | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Population | Undergraduate and postgraduate medical students, residents, and/or postgraduate and clinical clerkship | General Surgery and Surgical Specialties |
| Tutors and learners in General Medicine, including Allergy and Immunology, Clinical Medicine, Community Medicine, Dermatology, General Practice, Geriatrics, Hospital Medicine, Neurology, Palliative Medicine, and Internal Medicine (Cardiology, Endocrinology, Gastroenterology, Hematology, Immunology, Infectious Disease, Nephrology, Respiratory Medicine, and Rheumatology) | Pathology, Radiology, Pediatrics, Psychiatry, Emergency Medicine, Obstetrics and Gynecology, Anesthesia, Allied Health (Dietetics, Occupational Therapy, Psychology, Chiropractic, Midwifery, Social Work), Nursing, and Clinical and Translational Science | |
| Tutors and learners in Clinical, Academia or Research setting. | Non-medical professions (e.g. Science, Veterinary, Dentistry) | |
| Peer, Near-peer, Mosaic, and E-mentoring | ||
| Tutoring, Preceptorship, Coaching, Role Modeling, Advising, and Sponsorship | ||
| Intervention | Interventions by HOs to create, modify, or evaluate novice mentoring processes or programs | |
| Comparison | Comparisons of the various characterizations, definitions, roles and descriptions of the HO and its impact upon the mentoring process, the mentoring relationship and oversight of the mentoring program | |
| Outcome | Concepts and constructs of HO | |
| Impact of HO and its impact upon the mentoring process, the mentoring relationship, and oversight of the mentoring program | ||
| Study design | Articles in English or translated to English | |
| All study designs including | ||
| Mixed methods research, meta-analyses, systematic reviews, randomized controlled trials, cohort studies, case-control studies, cross-sectional studies, and descriptive papers | ||
| Gray Literature/electronic and print information not controlled by commercial publishing | ||
| Case reports and series, ideas, editorials, and perspectives | ||
| Year of Publication: January 2000–December 2019 | ||
| Databases: PubMed, Embase, PsycINFO, ERIC, Cochrane Database of Systematic Reviews, Google Scholar and Scopus, GreyLit, OpenGrey, Web of Science databases |
Sampling
A search on 7 bibliographic databases (PubMed, Embase, PsycINFO, ERIC, Cochrane Database of Systematic Reviews, Google Scholar, and Scopus) was conducted between 24th April and 12th September 2018. A search of gray literature involving GreyLit, OpenGrey, and Web of Science databases was carried out between 18th October 2018 and 17th December 2018. In order to update the search so as to include articles published up to December 2019, a subsequent search of all 10 databases was conducted between 30th December 2019 and 4th January 2020. Accounts of novice mentoring prior to the year 2000 were omitted given the propensity of these articles to neglect clear descriptions of mentoring and conflate mentoring approaches.65,66 The PubMed Search Strategy may be found in Supplemental Appendix A.
Upon completion of the independent searches, each member of the research team compiled a list of titles and abstracts to be reviewed. They discussed their findings online and at weekly research team meetings, achieving consensus on the final list of titles and abstracts by using Sambunjak et al’s67 approach to “negotiated consensual validation.”
Analysis
Braun and Clarke’s68 approach to thematic analysis was adopted in the absence of an a priori framework and a clear definition of the host in novice mentoring.
Reiterative process
In keeping with the reiterative process outlined in Levac et al’s sixth stage, consultations with key stakeholders saw the expert team note that the themes identified were consistent with descriptions of medical education units which oversee and support multiple education programs.69,70 As such, drawing upon the roles of medical education units set out by the “AMEE Education Guide no. 28: The development and role of departments of medical education,”71 2 independent reviewers who were not involved in the thematic analysis adopted Hsieh and Shannon’s72 approach to directed content analysis. This process involves “identifying and operationalizing a priori coding categories”73 which aligns with the constructivist approach adopted in this scoping review. This approach circumnavigates the wide range of research methodologies employed in the articles and prevents statistical pooling and analysis.74-77 Quantifying the data and tabulating the frequency by which the themes and categories emerge also aids as a proxy indicator of their significance.78
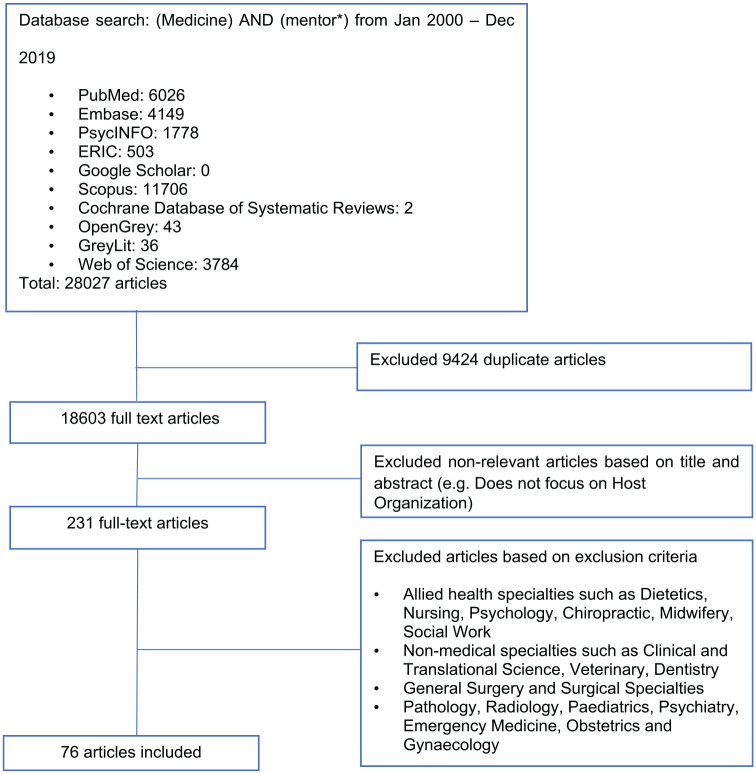
In total, 18 603 abstracts were identified from the 10 databases, 231 full-text articles were reviewed, and 76 full-text articles were analyzed79 (Figure 1: PRISMA flow chart).
Figure 1.
PRISMA flow chart.
Majority of the articles surveyed mentees and mentors instead of the host organization and the articles were predominantly qualitative or quantitative, retrospective or prospective in nature. The characteristics of the 76 included articles are featured in Supplemental Appendix B.
Quality assessment of studies
Whilst not commonly associated with systematic scoping reviews, quality assessments were deemed important to better influence and inform future practice. This sentiment was shared by the expert team. Two authors thus carried out individual appraisals using the Medical Education Research Study Quality Instrument (MERSQI)80 and the Consolidated Criteria for Reporting Qualitative Studies (COREQ)81 to evaluate the quality of the quantitative and qualitative studies included in this review.
The narrative produced was guided by the Best Evidence Medical Education (BEME) Collaboration guide82 and the STORIES (Structured approach to the Reporting In healthcare education of Evidence Synthesis) statement.83
Results
Comparisons between the themes and categories identified using thematic and directed content analysis revealed significant consistencies.
(1) “Defining” and secondary roles
An overwhelming majority of the included articles defined the host organization by the roles they play in their respective mentoring programs.67,83-141 These papers suggest that the “defining” roles47 of the host include:
establishing and/or complying with overarching goals, clinical standards, and curriculum requirements84,86-92,140
designing,83,88,92,95-102,132,135 influencing,47,90,92-94,122 and overseeing the mentoring program88,95,98,102-107
and nurturing the mentoring culture84,85,90-92,97,101,106,108-110 and mentoring relationships83,85,88,92,95-102
Characteristics of an effective host, in particular, were determined to be their ability to:
provide consistent leadership47,67,84,91,93,96,102,107,137,142-144
proactively support mentor and mentee participation47,67,83,85,93,96,101,103,107,111,118,120,129,134,142-145
cogently facilitate all mentoring processes47,67,87,91,92,99,101,106,107,111,118,127,138,143,144,146
proactively gather and revert feedback on the mentoring program and the mentoring relationships within47,89,101,116,126,134,142,146-148
and, finally, successfully initiate curricular reform to better meet the needs of their participants107,137,144,146
In addition, the secondary roles of the host comprise of supporting patient care and specific responsibilities toward the mentee, mentor, the overall program, and the organization itself. These are outlined in Table 2.
Table 2.
Secondary Roles of Host Organization.
| Roles in | Elaboration | References |
|---|---|---|
| Patient Care | Supports patient care delivery, safety, and health outcomes | 92,110,124,125 |
| Mentee and Mentors | Supports their personal | 47,85,88,92,108,113,120,142,144,149,150 |
| Professional and career development | 47,83,85,88,91,92,98,106,108,112,113,116-120,126,129,137,142-144,147,149-151 | |
| And addresses heavy workloads, stress, and anxiety amongst mentors and mentees | 88 | |
| Program | Reduces the proportion of ineffective matches and unnecessary evaluations of mentors, mentees, and the mentoring process to sustain the viability of the program | 47,88,126,129 |
| Organization | Maintains: | |
| Organizational practice and collaborations | 47,83,85,92,124,144 | |
| Research development | 47,92,108,111,128,133,142-144,147 | |
| Faculty development | 83,85,88,92,108,116,128,129,138,142,143,146 | |
| Satisfaction and retention | 83,88,92,96,108,110,116,126,129,138,144,146,152,153 | |
| Sustainability and productivity of the program | 47,85,96,118,124,142-144,153 |
(2) Balancing structure and flexibility
Although not a defining characteristic of the host organization, a key finding which emerged in numerous papers was the need for the host to balance structure and flexibility within the program.
Establishing a mentoring structure serves to ensure fairness and consistency in the mentoring approach and experience for all.67,83,85,88,90-93,95-101,104,107,111,118,121,123-125,129,133,134,136,138,142,144 Rigorous oversight and the just provision of support, in turn, influences the mentoring culture.47,92,104,106,107,142,151 It ensures transparent communication of the program’s mentoring philosophy, mentoring approach, as well as the goals and values of the program.47,88,95,98,101,103,104,124,149 It also facilitates recruitment and retention of mentors through the provision of financial remuneration,84,86,88,93,97,102,104,124,129,130,134,139,142,144,150 opportunities for academic promotion,83,86,93,106,138,139 formal recognition of their time and efforts,25,83,84,86,90,92,96,97,124,134,138,139,144,150 timely access to facilities, resources,47,105,144 research funding,84,136,154 and protected time.25,67,83,84,90,92,95-97,133,134,139,142,144,154
Yet, the host must also allow for flexibility47 within the mentoring program so as to adapt to the evolving mentee-, mentor-, host organization-, and relationship-dependent nature of each individual mentoring relationship.114 This is critical in enhancing the mentee’s sense of autonomy, connectivity, and advocacy.114,144 It is of note that flexibility is also encapsulated within the clinical standards and codes of conduct set out by prevailing host organizations.47,84,86-92 As outlined in Table 3, structure and flexibility within the mentoring program is evident in the various stages of the mentoring process.
Table 3.
Structure and Flexibility in Stages of Mentoring Processes.
| Stage | Elaboration | References |
|---|---|---|
| Structure | ||
| Matching Stage | The host establishes its selection, vetting, matching and training for mentees and mentors | 47,67,83,85,88,90-93,95-101,104,107,111,118,121,123-125,129,133,134,136,138,142 |
| And may use contractual agreements | 67,90,92-94,101,102,131 | |
| To align expectations | 47,84,85,88,90,92,97,101,108-110,131,139,142,144 | |
| And clarify goals, timelines, and roles | 53,106,112,115,118,119,138,156 | |
| And responsibilities | 53,54,106,112,115,118,119 | |
| Pre-mentoring Stage | Sets out its own objectives establishes and oversees the entry criteria, goals, selection, and matching processes | 84,92,97,99,101,103,105,124,142,144,147 |
| And the mentoring approach | 85,88,95,98,101,103,104,142 | |
| Within a formal curriculum | 47,87,88,94,95,98,104,111,116,117,119,126,130,134,136,139,148,150,155,156 | |
| Flexibility | ||
| Matching Stage | Accounts for the mentor’s and mentee’s goals and interests | 47,52,84,85,92,97,101,111,126,132,142,144 |
| Personalities | 101 | |
| Preferences on how they would like to initiate mentoring relationships | 67,101,110,111,129,132 | |
| Gender | 83,96,132 | |
| Background | 87,96 | |
| Ethnicity | 67,92 | |
| Pre-mentoring stage | Flexibility is apparent in the: | 47,67,90,92,97,101,106,108,109,117,129 |
| structure, form and frequency of meetings, codes of conduct, roles and responsibilities and standards of practice established | 47,87,90,92,96,97,101,141 | |
| consideration of individual mentee’s and mentor’s expectations | 47,108,111 | |
| goals | 47,85,105,106,147 | |
| Mentoring Process | Adaptable | 25,47,87,90,92,96,97,101,141 |
| And longitudinal evaluations are employed to account for changes in the mentoring relationships and shifts in individual academic, social, research, and personal situations of mentees and mentors | 84-87,89-93,96,97,102,115,142,144,149 | |
| Flexibility is also evident as hosts respond and adapt its approach and support in response to appraisals | 67,87,91,92,99,101,106,107,111,118,127,138,146 | |
Discussion
In addressing its primary and secondary questions, this SSR characterizes the host organization as a “team of educators and administrators83,102,104,112,116 with common values, goals and views on education and clearly delineated roles and responsibilities 86,87,90-92 who collaborate through coordinated lines of communication104, assessment, and reporting 88,95,98,103,104 in order to realize their “defining” and secondary roles. The “defining” roles of the host include establishing, nurturing, and overseeing mentoring relationships whilst ideally offering both structure and flexibility within the mentoring program.”83,84,86-110
To realize their “defining” roles, the host should design and incorporate the mentoring program as part of the formal curriculum.87,88,94,95,98,104,111,116,117,119,126,130,134,136,139,148,150,155 This will provide the program leaders with administrative, financial, and training support that will help streamline their response to the changing needs of the stakeholders and the mentoring process.67,87,91,92,99,101,106,107,111,118,127,138,146 Such resources will ensure that codes of conduct, standards of practice, timelines, roles, and responsibilities to be adhered to by mentees, mentors and the educationalists and administrators designing and spearheading the program are clearly overseen.84,86-92 A consistent framework is also critical in ensuring that mentoring takes place within reasonable boundaries.30,31 Establishing an implicit or contractual67,90,92-94,101,102,131 agreement between mentees and mentors on the expectations of the mentoring program would minimize the risk of misdemeanors and breaches in ethical conduct.
To ensure a flexible approach, the host must adopt adaptable, context sensitive, and stakeholder-specific assessment methods to provide mentees, mentors, and the mentoring relationship with personalized, appropriate, specific, timely, holistic, accessible, and longitudinal support.25,67,84,86,87,89-93,96,97,99,101,102,106,107,111,115,118,127,138,141,146,149 Adaptations should be guided by consistent evaluations of the mentee’s, mentor’s, and the host organization’s changing needs and goals. In the absence of a specific assessment tool, a combination of tools and assessors may be considered.83,88,91,92,96,98,106,108,110-113,116-120,124-126,128,129,133,137,138,146,147,149-153
The host should also work to establish an accessible and robust platform for mentors and mentees to communicate freely and confidentially. Such a platform would also encourage mentors and mentees to attune themselves and respond to any changes during the course of their mentoring relationship. To facilitate this, they should be provided with pre-mentoring workshops and longitudinal training programs to develop their communication and online literacy skills. Such skills will help them to circumnavigate obstacles such as conflicting schedules amidst urgent deadlines that may impede the progress of their mentoring projects.
Overall, these considerations will provide the host with the opportunity to deliver consistent, timely, appropriate, longitudinal leadership47,67,84,91,93,96,102,107,137,142-144, holistic support for the matching,47,67,83,85,93,96,101,103,107,111,118,120,129,134,142-145 and mentoring process47,67,87,91,92,99,101,106,107,111,118,127,138,143,144,146, personalized, specific and comprehensive feedback to all participants 47,89,101,116,126,134,142,146-148 and the successful development and execution of crucial curricular reform.107,137,144,146
Limitations
Too narrow a picture of the host organization may have been sketched in this scoping review given that it was explored in isolation from factors such as the dynamic nature of mentoring relationships, structures, environments, and even mentee-mentor matching processes. Concurrently, given the context-specific nature of the host and their roles in mentoring programs, conflation within the included articles of different healthcare, educational and CPD systems across different national and international contexts may prove to be problematic.
These limitations are compounded by the scoping review’s focus on articles published or translated into English. As a result, much of the data comes from North America and Europe, potentially skewing perspectives and raising questions as to the applicability of these findings in other healthcare settings. In addition, despite using the Endnote software to carry out independent searches and consolidation of the findings, relevant articles may have been unintentionally omitted.
However, despite these limitations, this scoping review was carried out with the required rigor and transparency advocated by Arksey and O’Malley,42 Levac et al,55 and Pham et al.157 As a result, we believe that the findings will help to inform the design and oversight of future mentoring programs. We also believe that this review may be of interest to educators and program designers in settings beyond the mentoring landscape due to the potential applicability of the findings to other aspects of medical education.
Directions for future research
This scoping review evidences the critical role of the host in mentoring programs and hints at their applicability to undergraduate and postgraduate medical education. Riding on ever improving communication technology and advances in the dissemination of information, the increasing use of technology-enhanced mentoring platforms will also see ever increasing demands for transparency and accountability. There is a need to conduct closer evaluations of all intra and interprofessional mentoring interactions to ensure that personal and professional boundaries are maintained with codes of conduct and standards of practice strictly adhered to.
Prospective studies should be conducted to better understand how balance between structure and flexibility can be better struck to ensure maximum efficacy. However, it is only with the curation and validation of effective assessment tools accounting for mentoring’s evolving nature that mentoring can realize its true potential in CPD programs.
Lessons for practice
(a) Mentoring’s role in CPD hinges on effective support and oversight by the host organization. This may be facilitated through the development of a formal mentoring program that is overseen by the wider education and administrative team.
(b) Collaborative efforts between educators and administrators are required to ensure that a clear organizational structure is established with the aim of meeting the critical “defining” roles of the host. These comprise of establishing, nurturing, and overseeing the mentoring relationships whilst balancing structure and flexibility within the program. This process must be guided by clear outcome measures, codes of conduct, standards of practice, and assessment points.
(c) Members of the host must be trained, briefed, supported, and appraised throughout the mentoring program. Their roles, responsibilities and lines of reporting should be clearly established.
(d) Mentoring in CPD should be run as a longitudinal program that is in turn supported by mentee and mentor training workshops.
(e) Mentoring’s role in CPD is to facilitate personalized social, academic, and leadership development opportunities especially when used in conjunction with e-mentoring. However, the effectiveness of such an approach pivots upon the host’s ability to assess and respond to the evolving needs of the mentee, mentor and the mentoring relationship.
Supplemental Material
Supplemental material, Supplementary_material for The Pivotal Role of Host Organizations in Enhancing Mentoring in Internal Medicine: A Scoping Review by Elisha Wan Ying Chia, Kuang Teck Tay, Shiwei Xiao, Yao Hao Teo, Yun Ting Ong, Min Chiam, Ying Pin Toh, Stephen Mason, Annelissa Mien Chew Chin and Lalit Kumar Radha Krishna in Journal of Medical Education and Curricular Development
Acknowledgments
The authors would like to dedicate this paper to the late Dr S Radha Krishna whose advice and ideas were integral to the success of this study. The authors would like to thank the anonymous reviewers whose advice and feedback greatly improved this manuscript.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: EWYC, KTT, SX, YHT, YTO, MC, YPT, SM, AMCC, LKRK were involved in data curation, formal analysis, investigation, preparing the original draft of the manuscript as well as reviewing and editing the manuscript. All authors have read and approved the manuscript.
ORCID iDs: Elisha Wan Ying Chia  https://orcid.org/0000-0002-7603-2688
https://orcid.org/0000-0002-7603-2688
Stephen Mason  https://orcid.org/0000-0002-4020-6869
https://orcid.org/0000-0002-4020-6869
Lalit Kumar Radha Krishna  https://orcid.org/0000-0002-7350-8644
https://orcid.org/0000-0002-7350-8644
Supplemental material: Supplemental material for this article is available online.
References
- 1. Peck C, McCall M, McLaren B, Rotem T. Continuing medical education and continuing professional development: international comparisons. BMJ. 2000;320:432-435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Alleyne SD, Horner MS, Walter G, Fleisher SH, Arzubi E, Martin A. Mentors’ perspectives on group mentorship: a descriptive study of two programs in child and adolescent psychiatry. Acad Psychiatry. 2009;33:377-382. [DOI] [PubMed] [Google Scholar]
- 3. Andre C, Deerin J, Leykum L. Students helping students: vertical peer mentoring to enhance the medical school experience. BMC Res Notes. 2017;10:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Buddeberg-Fischer B, Vetsch E, Mattanza G. Career support in medicine—experiences with a mentoring program for junior physicians at a university hospital. Psychosoc Med. 2004;1:Doc04. [PMC free article] [PubMed] [Google Scholar]
- 5. Bussey-Jones J, Bernstein L, Higgins S, et al. Repaving the road to academic success: the IMeRGE approach to peer mentoring. Acad Med. 2006;81:674-679. [DOI] [PubMed] [Google Scholar]
- 6. Chen MM, Sandborg CI, Hudgins L, Sanford R, Bachrach LK. A multifaceted mentoring program for junior faculty in academic pediatrics. Teach Learn Med. 2016;28:320-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Files JA, Blair JE, Mayer AP, Ko MG. Facilitated peer mentorship: a pilot program for academic advancement of female medical faculty. J Womens Health (Larchmt). 2008;17:1009-1015. [DOI] [PubMed] [Google Scholar]
- 8. Fleming GM, Simmons JH, Xu M, et al. A facilitated peer mentoring program for junior faculty to promote professional development and peer networking. Acad Med. 2015;90:819-826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kashiwagi DT, Varkey P, Cook DA. Mentoring programs for physicians in academic medicine: a systematic review. Acad Med. 2013;88:1029-1037. [DOI] [PubMed] [Google Scholar]
- 10. Lewellen-Williams C, Johnson VA, Deloney LA, Thomas BR, Goyol A, Henry-Tillman R. The POD: a new model for mentoring underrepresented minority faculty. Acad Med. 2006;81:275-279. [DOI] [PubMed] [Google Scholar]
- 11. Lord JA, Mourtzanos E, McLaren K, Murray SB, Kimmel RJ, Cowley DS. A peer mentoring group for junior clinician educators: four years’ experience. Acad Med. 2012;87:378-383. [DOI] [PubMed] [Google Scholar]
- 12. Pololi LH, Evans AT. Group peer mentoring: an answer to the faculty mentoring problem? A successful program at a large Academic Department of Medicine. J Contin Educ Health Prof. 2015;35:192-200. [DOI] [PubMed] [Google Scholar]
- 13. Pololi LH, Knight SM, Dennis K, Frankel RM. Helping medical school faculty realize their dreams: an innovative, collaborative mentoring program. Acad Med. 2002;77:377-384. [DOI] [PubMed] [Google Scholar]
- 14. Singh S, Singh N, Dhaliwal U. Near-peer mentoring to complement faculty mentoring of first-year medical students in India. J Educ Eval Health Prof. 2014;11:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Welch JL, Jimenez HL, Walthall J, Allen SE. The women in emergency medicine mentoring program: an innovative approach to mentoring. J Grad Med Educ. 2012;4:362-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Toh YP, Lam BL, Soo J, Chua KLL, Krishna L. Developing palliative care physicians through mentoring relationships. Palliat Med Care. 2017;4:1-6. [Google Scholar]
- 17. Yeam C, Loo WT, Ee MH, Kanesvaran R, Krishna L. An evidence-based evaluation of prevailing learning theories on mentoring in palliative medicine. Palliat Med Care. 2016;3:1-7. [Google Scholar]
- 18. Wu J, Wahab MT, Ikbal MFBM, Loo TWW, Kanesvaran R, Krishna LKR. Toward an interprofessional mentoring program in palliative care—a review of undergraduate and postgraduate mentoring in medicine, nursing, surgery and social work. J Palliat Med. 2016;6:1-11. [Google Scholar]
- 19. Wahab MT, Ikbal MFBM, Wu J, Loo WTW, Kanesvaran R, Krishna LKR. Creating effective interprofessional mentoring relationships in palliative care: lessons from medicine, nursing, surgery and social work. J Palliat Med. 2016;6: 1-10. [Google Scholar]
- 20. Loo WTW, Ikbal MFBM, Wu JT, et al. Towards a practice guided evidence based theory of mentoring in palliative care. J Palliat Care Med. 2017;7:296. [Google Scholar]
- 21. Tan B, Toh YL, Toh YP, Kanesvaran R, Krishna LKR. Extending mentoring in palliative medicine-systematic review on peer, near-peer and group mentoring in general medicine. J Palliat Med. 2017;7:323. [Google Scholar]
- 22. Kalen S, Ponzer S, Seeberger A, Kiessling A, Silen C. Longitudinal mentorship to support the development of medical students’ future professional role: a qualitative study. BMC Med Educ. 2015;15:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Balmer D, D’Alessandro D, Risko W, Gusic ME. How mentoring relationships evolve: a longitudinal study of academic pediatricians in a physician educator faculty development program. J Contin Educ Health Prof. 2011;31:81-86. [DOI] [PubMed] [Google Scholar]
- 24. Rashid P, Narra M, Woo H. Mentoring in surgical training. ANZ J Surg. 2015;85:225-229. [DOI] [PubMed] [Google Scholar]
- 25. Jackson VA, Palepu A, Szalacha L, Caswell C, Carr PL, Inui T. “Having the right chemistry”: a qualitative study of mentoring in academic medicine. Acad Med. 2003;78:328-334. [DOI] [PubMed] [Google Scholar]
- 26. Campbell C, Silver I, Sherbino J, Cate OT, Holmboe ES. Competency-based continuing professional development. Med Teach. 2010;32:657-662. [DOI] [PubMed] [Google Scholar]
- 27. Lin J, Chew YR, Toh YP, Krishna LKR. Mentoring in nursing: an integrative review of commentaries, editorials, and perspectives papers. Nurse Educ. 2018;43:E1-E5. [DOI] [PubMed] [Google Scholar]
- 28. Toh YP, Karthik R, Teo CC, Suppiah S, Cheung SL, Krishna L. Toward mentoring in palliative social work: a narrative review of mentoring programs in social work. Am J Hosp Palliat Care. 2017;35:523-531. [DOI] [PubMed] [Google Scholar]
- 29. Yap HW, Chua J, Toh YP, et al. Thematic review of mentoring in occupational therapy and physiotherapy between 2000 and 2015, sitting occupational therapy and physiotherapy in a holistic palliative medicine multidisciplinary mentoring program. J Palliat Med. 2017;2:46-55. [Google Scholar]
- 30. Lee FQH, Chua WJ, Cheong CWS, et al. A systematic scoping review of ethical issues in mentoring in surgery. J Med Educ Curric Dev. 2019;6:2382120519888915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cheong CWS, Chia EWY, Tay KT, et al. A systematic scoping review of ethical issues in mentoring in internal medicine, family medicine and academic medicine. Adv Health Sci Educ Theory Pract. 2020;25:195-226. [DOI] [PubMed] [Google Scholar]
- 32. Singh TSS, Singh A. Abusive culture in medical education: mentors must mend their ways. J Anaesth Clin Pharm. 2018;34:145-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Byerley JS. Mentoring in the era of# MeToo. JAMA. 2018;319:1199-1200. [DOI] [PubMed] [Google Scholar]
- 34. Walters KL, Simoni JM, Evans-Campbell TT, et al. Mentoring the mentors of underrepresented racial/ethnic minorities who are conducting HIV research: beyond cultural competency. AIDS Behav. 2016;20:288-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Soklaridis S, Zahn C, Kuper A, Gillis D, Taylor VH, Whitehead C. Men’s fear of mentoring in the# MeToo era—what’s at stake for academic medicine? N Engl J Med. 2018;379:2270-2274. [DOI] [PubMed] [Google Scholar]
- 36. Olasoji HO. Broadening conceptions of medical student mistreatment during clinical teaching: message from a study of “toxic” phenomenon during bedside teaching. Adv Med Educ Pract. 2018;9:483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Duck S. Stratagems, spoils, and a serpent’s tooth: on the delights and dilemmas of personal relationships. In: Cupach WR, Spitzberg BH, eds. The Dark Side of Interpersonal Communication. Hillsdale, NJ: Erlbaum, 1994:3-24. [Google Scholar]
- 38. Chopra V, Edelson DP, Saint S. Mentorship malpractice. JAMA. 2016;315:1453-1454. [DOI] [PubMed] [Google Scholar]
- 39. Long J. The dark side of mentoring. Aust Educ Res. 1997;24:115-133. [Google Scholar]
- 40. Walensky RP, Kim Y, Chang Y, et al. The impact of active mentorship: results from a survey of faculty in the Department of Medicine at Massachusetts General Hospital. BMC Med Educ. 2018;18:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Krishna LKR, Renganathan Y, Tay KT, et al. Educational roles as a continuum of mentoring’s role in medicine—a systematic review and thematic analysis of educational studies from 2000 to 2018. BMC Med Educ. 2019;19:439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19-32. [Google Scholar]
- 43. Du Mont J, Macdonald S, Kosa D, Elliot S, Spencer C, Yaffe M. Development of a comprehensive hospital-based elder abuse intervention: an initial systematic scoping review. PLoS One. 2015;10:e0125105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. O’Donovan J, O’Donovan C, Kuhn I, Sachs SE, Winters N. Ongoing training of community health workers in low-income andmiddle-income countries: a systematic scoping review of the literature. BMJ Open. 2018;8:e021467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lim SYS, Koh EYH, Tan BJX, Toh YP, Mason S, Krishna LKR. Enhancing geriatric oncology training through a combination of novice mentoring and peer and near-peer mentoring: a thematic analysis of mentoring in medicine between 2000 and 2017. J Geriatr Oncol. 2020;11:566-575. [DOI] [PubMed] [Google Scholar]
- 46. Chong JY, Ching AH, Renganathan Y, et al. Enhancing mentoring experiences through e-mentoring: a systematic scoping review of e-mentoring programs between 2000 and 2017. Adv Health Sci Educ Theory Pract. 2019;25:195-226. [DOI] [PubMed] [Google Scholar]
- 47. Tan YS, Teo SWA, Pei Y, et al. A framework for mentoring of medical students: thematic analysis of mentoring programmes between 2000 and 2015. Adv Health Sci Educ Theory Pract. 2018: 23:671-697. [DOI] [PubMed] [Google Scholar]
- 48. Low CQT, Toh YL, Teo SWA, Toh YP, Krishna L. A narrative review of mentoring programmes in general practice. Educ Prim Care. 2018;29:259-267. [DOI] [PubMed] [Google Scholar]
- 49. Hee JM, Yap HW, Ong ZX, et al. Understanding the mentoring environment through thematic analysis of the learning environment in medical education: a systematic review. J Gen Intern Med. 2019;34:2190-2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sheri K, Too JYJ, Chuah SEL, Toh YP, Mason S, Krishna LKR. A scoping review of mentor training programs in medicine between 1990 and 2017. Med Educ Online. 2019;24:1555435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Taufeeq Wahab M, Bin Mohamad Ikbal MF, Jingting W, Wesley LTW, Kanesvaran R, Radha Krishna LK. Creating effective interprofessional mentoring relationships in palliative care- lessons from medicine, nursing, surgery and social work. J Palliat Care Med. 2016;6:1-10. [Google Scholar]
- 52. Toh YP. Developing palliative care physicians through mentoring relationships. Palliat Med Care. 2017;4:1-6. [Google Scholar]
- 53. Jia Min Hee HWY, Zheng Xuan Ong, Simone Quek, Ying Pin Toh, Stephen Mason, lalit kumar radha krishna. Understanding the mentoring environment through thematic analysis of the learning environment in medical education: a systematic review. J Gen Intern Med. 2019;34:2190-2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Wahab M, Ikbal M, Wu J, Loo T, Kanesvaran R, Lalit K. Toward an interprofessional mentoring program in palliative care—a review of undergraduate and postgraduate mentoring in medicine, nursing, surgery and social work. J Palliat Care Med. 2016;6:1-14. [Google Scholar]
- 55. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Chambers D, Wilson P, Thompson C, Harden M. Social network analysis in healthcare settings: a systematic scoping review. PLoS One. 2012;7:e41911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Colquhoun HL, Levac D, O’Brien KK, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67:1291-1294. [DOI] [PubMed] [Google Scholar]
- 58. Thomas A, Menon A, Boruff J, Rodriguez AM, Ahmed S. Applications of social constructivist learning theories in knowledge translation for healthcare professionals: a scoping review. Implement Sci. 2014;9:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Mays N, Roberts E, Popay J. Synthesising research evidence. In: Allen P, Black N, Clarke A, Fulop N, Anderson S. (eds) Studying the organisation and delivery of health services: Research methods. London: Routledge; 2001:240. [Google Scholar]
- 60. Lorenzetti DL, Powelson SE. A scoping review of mentoring programs for academic librarians. J. Acad. Librariansh. 2015;41(2):186-196. [Google Scholar]
- 61. Osama T, Brindley D, Majeed A, et al. Teaching the relationship between health and climate change: a systematic scoping review protocol. BMJ Open. 2018;8(5):e020330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Physicians ACo. Subspecialties of internal medicine. Philadelphia, PA: American College of Physicians. Published 2018. Accessed May 20, 2018. [Google Scholar]
- 63. Peters M, Godfrey C, McInerney P, Soares C., Khalil H, Parker D. The Joanna Briggs Institute reviewers’ manual 2015: methodology for JBI scoping reviews. 2015. http://joannabriggs.org/assets/docs/sumari/Reviewers-Manual_Methodology-for-JBI-Scoping-Reviews_2015_v1.pdf. Accessed April 29, 2019.
- 64. Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141-146. [DOI] [PubMed] [Google Scholar]
- 65. Krishna L, Toh Y, Mason S, Kanesvaran R. Mentoring stages: a study of undergraduate mentoring in palliative medicine in Singapore. PLoS one. 2019;14(4):e0214643-e0214643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Ikbal MFBM, Wu JT, Wahab MT, Kanesvaran R, Krishna LKR. Mentoring in palliative medicine: guiding program design through thematic analysis of mentoring in internal medicine between 2000 and 2015. J Palliat Care Med. 2017;7:318. [Google Scholar]
- 67. Sambunjak D, Straus SE, Marusic A. A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine. J Gen Intern Med. 2010;25:72-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3:77-101. [Google Scholar]
- 69. Wen SH, Ren WM, Qu L, Wang Y, Carline JD, Fang GE. A survey on financial support and research achievement of medical education research units in China. Med Teach. 2011;33:e158-e162. [DOI] [PubMed] [Google Scholar]
- 70. Varpio L, Gruppen L, Hu W, et al. Working definitions of the roles and an organizational structure in health professions education scholarship: initiating an international conversation. Acad Med 2017;92:205-208. [DOI] [PubMed] [Google Scholar]
- 71. Davis MH, Karunathilake I, Harden RM. AMEE Education Guide no. 28: the development and role of departments of medical education. Med Teach. 2005;27:665-675. [DOI] [PubMed] [Google Scholar]
- 72. Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Quale Health Res. 2005;15:1277-1288. [DOI] [PubMed] [Google Scholar]
- 73. Neal JW, Neal ZP, Lawlor JA, Mills KJ, McAlindon K. What makes research useful for public school educators? Adm Policy Ment Health. 2018;45:432-446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Soemantri D, Herrera C, Riquelme A. Measuring the educational environment in health professions studies: a systematic review. Med Teach. 2010;32:947-952. [DOI] [PubMed] [Google Scholar]
- 75. Schönrock-Adema J, Heijne-Penninga M, van Hell EA, Cohen-Schotanus J. Necessary steps in factor analysis: enhancing validation studies of educational instruments. The PHEEM applied to clerks as an example. Med Teach. 2009;31:e226-e232. [DOI] [PubMed] [Google Scholar]
- 76. Riquelme A, Herrera C, Aranis C, Oporto J, Padilla O. Psychometric analyses and internal consistency of the PHEEM questionnaire to measure the clinical learning environment in the clerkship of a Medical School in Chile. Med Teach. 2009;31:e221-e225. [DOI] [PubMed] [Google Scholar]
- 77. Gordon M, Gibbs T. STORIES statement: publication standards for healthcare education evidence synthesis. BMC Med. 2014;12:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15:398-405. [DOI] [PubMed] [Google Scholar]
- 79. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264-269. [DOI] [PubMed] [Google Scholar]
- 80. Reed DA, Beckman TJ, Wright SM, Levine RB, Kern DE, Cook DA. Predictive validity evidence for medical education research study quality instrument scores: quality of submissions to JGIM’s Medical Education Special Issue. J Gen Intern Med. 2008;23:903-907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349-357. [DOI] [PubMed] [Google Scholar]
- 82. Haig A, Dozier M. BEME Guide no 3: systematic searching for evidence in medical education–Part 1: Sources of information. Med Teach. 2003;25:352-363. [DOI] [PubMed] [Google Scholar]
- 83. Frei E, Stamm M, Buddeberg-Fischer B. Mentoring programs for medical students-a review of the PubMed literature 2000-2008. BMC Med Educ. 2010;10:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. White HK, Buhr GT, Pinheiro SO. Mentoring: a key strategy to prepare the next generation of physicians to care for an aging America. J Am Geriatr Soc. 2009;57:1270-1277. [DOI] [PubMed] [Google Scholar]
- 85. Farkas AH, Allenbaugh J, Bonifacino E, Turner R, Corbelli JA. Mentorship of US medical students: a systematic review. J Gen Intern Med. 2019;34:2602-2609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Lin C-D, Lin BY-J, Lin C-C, Lee C-C. Redesigning a clinical mentoring program for improved outcomes in the clinical training of clerks. Med Educ Online. 2015;20:28327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Devi V, Abraham RR, Adiga A, Ramnarayan K, Kamath A. Fostering research skills in undergraduate medical students through Mentored Student Projects: example from an Indian medical school. Kathmandu University Med J. 2010;8:294-298. [DOI] [PubMed] [Google Scholar]
- 88. Dobie S, Smith S, Robins L. How assigned faculty mentors view their mentoring relationships: an interview study of mentors in medical education. Mentor Tutor. 2010;18:337-359. [Google Scholar]
- 89. Fleming M, House MS, Shewakramani MV, et al. The mentoring competency assessment: validation of a new instrument to evaluate skills of research mentors. Acad Med 2013;88:1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Straus SE, Johnson MO, Marquez C, Feldman MD. Characteristics of successful and failed mentoring relationships: a qualitative study across two academic health centers. Acad Med. 2013;88:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Fraser A. Mentoring resident doctors. N Zealand Med J. 2004;117:1-5. [PubMed] [Google Scholar]
- 92. Ikbal M, Wu J, Wahab M, Kanesvaran R, Krishna L. Mentoring in palliative medicine: Guiding program design through thematic analysis of mentoring in internal medicine between 2000 and 2015. J Palliat Care Med. 2017;7:318. [Google Scholar]
- 93. Mark S, Link H, Morahan PS, Pololi L, Reznik V, Tropez-Sims S. Innovative mentoring programs to promote gender equity in academic medicine. Acad Med. 2001;76:39-42. [DOI] [PubMed] [Google Scholar]
- 94. Gotterer GS, O’day D, Miller BM. The Emphasis program: a scholarly concentrations program at Vanderbilt University School of Medicine. Acad Med. 2010;85:1717-1724. [DOI] [PubMed] [Google Scholar]
- 95. Usmani A, Omaeer Q, Sultan ST. Mentoring undergraduate medical students: experience from Bahria University Karachi. J Pak Med Assoc. 2011;61:790. [PubMed] [Google Scholar]
- 96. Shamim MS. Mentoring programme for faculty in medical education: South-Asian perspective. J Pak Med Assoc. 2013;63:619-623. [PubMed] [Google Scholar]
- 97. Sheikh ASF, Sheikh SA, Huynh M-H, Mohamed MA. Mentoring among Pakistani postgraduate resident doctors. Postgraduate Med J. 2017;93:115-120. [DOI] [PubMed] [Google Scholar]
- 98. Kalén S, Ponzer S, Seeberger A, Kiessling A, Silén C. Longitudinal mentorship to support the development of medical students’ future professional role: a qualitative study. BMC Med Educ. 2015;15:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Dzau VJ, Soo KC. Mentorship in academic medicine: a catalyst of talents. Ann Acad Med Singapore. 2015;44:232-234. [PubMed] [Google Scholar]
- 100. Winston KA, Van Der Vleuten CP, Scherpbier AJ. The role of the teacher in remediating at-risk medical students. Med Teach. 2012;34:e732-e742. [DOI] [PubMed] [Google Scholar]
- 101. Sng JH, Pei Y, Toh YP, Peh TY, Neo SH, Krishna LKR. Mentoring relationships between senior physicians and junior doctors and/or medical students: a thematic review. Med Teach. 2017;39:866-875. [DOI] [PubMed] [Google Scholar]
- 102. Kashiwagi DT, Varkey P, Cook DA. Mentoring programs for physicians in academic medicine: a systematic review. Acad Med. 2013;88:1029-1037. [DOI] [PubMed] [Google Scholar]
- 103. Boninger M, Troen P, Green E, et al. Implementation of a longitudinal mentored scholarly project: an approach at two medical schools. Acad Med. 2010;85:429-437. [DOI] [PubMed] [Google Scholar]
- 104. Coates WC, Crooks K, Slavin SJ, Guiton G, Wilkerson L. Medical school curricular reform: fourth-year colleges improve access to career mentoring and overall satisfaction. Acad Med. 2008;83:754-760. [DOI] [PubMed] [Google Scholar]
- 105. Fornari A, Murray TS, Menzin AW, et al. Mentoring program design and implementation in new medical schools. Med Educ Online. 2014;19:24570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. von der Borch P, Dimitriadis K, Störmann S, et al. A novel large-scale mentoring program for medical students based on a quantitative and qualitative needs analysis. GMS Zeitschrift für medizinische Ausbildung. 2011;28:1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Davis OC, Nakamura J. A proposed model for an optimal mentoring environment for medical residents: a literature review. Acad Med. 2010;85:1060-1066. [DOI] [PubMed] [Google Scholar]
- 108. Toklu HZ, Fuller JC. Mentor-mentee relationship: a win-win contract in graduate medical education. Cureus. 2017;9:e1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Schäfer M, Pander T, Pinilla S, Fischer MR, von der Borch P, Dimitriadis K. The Munich-Evaluation-of-Mentoring-Questionnaire (MEMeQ)–a novel instrument for evaluating protégés’ satisfaction with mentoring relationships in medical education. BMC Med Educ. 2015;15:201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Harrison R, Anderson J, Laloë P-A, Santillo M, Lawton R, Wright J. Mentorship for newly appointed consultants: what makes it work? Postgrad Med J. 2014;90:439-445. [DOI] [PubMed] [Google Scholar]
- 111. Pinilla S, Pander T, von der Borch P, Fischer MR, Dimitriadis K. 5 years of experience with a large-scale mentoring program for medical students. GMS Zeitschrift für Medizinische Ausbildung. 2015;32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Buddeberg-Fischer B, Herta K-D. Formal mentoring programmes for medical students and doctors–a review of the Medline literature. Med Teach. 2006;28:248-257. [DOI] [PubMed] [Google Scholar]
- 113. DeFilippis E, Cowell E, Rufin M, Sansone S, Kang Y. Innovative mentoring for female medical students. Clin Teach. 2016;13:381-382. [DOI] [PubMed] [Google Scholar]
- 114. Hauer KE, Teherani A, Dechet A, Aagaard EM. Medical students’ perceptions of mentoring: a focus-group analysis. Med Teach. 2005;27:732-734. [DOI] [PubMed] [Google Scholar]
- 115. Beech BM, Calles-Escandon J, Hairston KG, Langdon MSE, Latham-Sadler BA, Bell RA. Mentoring programs for underrepresented minority faculty in academic medical centers: a systematic review of the literature. Acad Med 2013;88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Bhatia A, Singh N, Dhaliwal U. Mentoring for first year medical students: humanising medical education. Indian J Med Ethics. 2013;10:100-103. [DOI] [PubMed] [Google Scholar]
- 117. Han E-R, Chung E-K, Oh S-A, Woo Y-J, Hitchcock MA. Mentoring experience and its effects on medical interns. Singapore Med J. 2014;55:593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Iversen AC, Eady NA, Wessely SC. The role of mentoring in academic career progression: a cross-sectional survey of the Academy of Medical Sciences mentoring scheme. Journal of the Royal Society of Medicine. 2014;107(8):308-317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Kalén S, Ponzer S, Silén C. The core of mentorship: medical students’ experiences of one-to-one mentoring in a clinical environment. Adv Health Sci Educ. 2012;17:389-401. [DOI] [PubMed] [Google Scholar]
- 120. Arnold L, Cuddy PG, Hathaway SB, Quaintance JL, Kanter SL. Medical school factors that prepare students to become leaders in medicine. Acad Med. 2018;93:274-282. [DOI] [PubMed] [Google Scholar]
- 121. Ottenheijm RP, Zwietering PJ, Scherpbier AJ, Metsemakers JF. Early student-patient contacts in general practice: an approach based on educational principles. Med Teach. 2008;30:802-808. [DOI] [PubMed] [Google Scholar]
- 122. Thomas-Squance GR, Goldstone R, Martinez A, Flowers LK. Mentoring of students from under-represented groups using emotionally competent processes and content. Med Educ. 2011;45:1153-1154. [DOI] [PubMed] [Google Scholar]
- 123. Schmidt A, Schwedler A, Hahn EG. Does the training of mentors increase the contact frequency and the quality of support in a portfolio-based teaching module? GMS Z Med Ausbild. 2010;27:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Meinel FG, Dimitriadis K, von der Borch P, Störmann S, Niedermaier S, Fischer MR. More mentoring needed? A cross-sectional study of mentoring programs for medical students in Germany. BMC Med Educ. 2011;11:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Ludwig B, Turk B, Seitz T, Klaus I, Löffler-Stastka H. The search for attitude—a hidden curriculum assessment from a central European perspective. Wien Klin Wochenschr. 2018;130:134-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Thomas-MacLean R, Hamoline R, Quinlan E, Ramsden VR, Kuzmicz J. Discussing mentorship: an ongoing study for the development of a mentorship program in Saskatchewan. Can Fam Physician. 2010;56:e263-e272. [PMC free article] [PubMed] [Google Scholar]
- 127. Srinivasan M, Li S-TT, Meyers FJ, et al. “Teaching as a competency”: competencies for medical educators. Acad Med. 2011;86:1211-1220. [DOI] [PubMed] [Google Scholar]
- 128. Longo DR, Katerndahl DA, Turban DB, et al. The research mentoring relationship in family medicine: findings from the grant generating project. Fam Med-Kans City. 2011;43:240. [PubMed] [Google Scholar]
- 129. Straus SE, Chatur F, Taylor M. Issues in the mentor–mentee relationship in academic medicine: a qualitative study. Acad Med. 2009;84:135-139. [DOI] [PubMed] [Google Scholar]
- 130. Stenfors-Hayes T, Kalén S, Hult H, Dahlgren LO, Hindbeck H, Ponzer S. Being a mentor for undergraduate medical students enhances personal and professional development. Med Teach. 2010;32:148-153. [DOI] [PubMed] [Google Scholar]
- 131. Sozio SM, Chan KS, Beach MC. Development and validation of the Medical Student Scholar-Ideal Mentor Scale (MSS-IMS). BMC Med Educ. 2017;17:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Sanfey H, Hollands C, Gantt NL. Strategies for building an effective mentoring relationship. Am J Surg. 2013;206:714-718. [DOI] [PubMed] [Google Scholar]
- 133. Zier K, Coplit LD. Introducing INSPIRE, a scholarly component in undergraduate medical education. Mount Sinai J Med. 2009;76:387-391. [DOI] [PubMed] [Google Scholar]
- 134. Levy BD, Katz JT, Wolf MA, Sillman JS, Handin RI, Dzau VJ. An initiative in mentoring to promote residents’ and faculty members’ careers. Acad Med. 2004;79:845-850. [DOI] [PubMed] [Google Scholar]
- 135. Stamm M, Buddeberg-Fischer B. The impact of mentoring during postgraduate training on doctors’ career success. Med Educ. 2011;45:488-496. [DOI] [PubMed] [Google Scholar]
- 136. Miedzinski LJ, Wong WW, Morrison JC. Perceptions of a faculty mentorship programme. Med Educ. 2009;43:1084-1084. [DOI] [PubMed] [Google Scholar]
- 137. Guraya SY, Guraya SS, Almaramhy HH. The legacy of teaching medical professionalism for promoting professional practice: a systematic review. Biomed Pharmacol J. 2016;9:809-817. [Google Scholar]
- 138. Morrison LJ, Lorens E, Bandiera G, et al. Impact of a formal mentoring program on academic promotion of Department of Medicine faculty: a comparative study. Med Teach. 2014;36:608-614. [DOI] [PubMed] [Google Scholar]
- 139. Rothberg MB, Kleppel R, Friderici JL, Hinchey K. Implementing a resident research program to overcome barriers to resident research. Acad Med. 2014;89:1133-1139. [DOI] [PubMed] [Google Scholar]
- 140. Luckhaupt SE, Chin MH, Mangione CM, et al. Mentorship in academic general internal medicine. J Gen Intern Med. 2005;20:1014-1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Larkin GL. Mapping, modeling, and mentoring: charting a course for professionalism in graduate medical education. Camb Q Healthc Ethics. 2003;12:167-177. [DOI] [PubMed] [Google Scholar]
- 142. Elez E, Quintanar T, Bosch-Barrera J, et al. The medical oncology resident mentor: situation and workload. Clin Transl Oncol. 2019;21:304-313. [DOI] [PubMed] [Google Scholar]
- 143. Manabe YC, Nambooze H, Okello ES, et al. Group mentorship model to enhance the efficiency and productivity of PhD research training in Sub-Saharan Africa. Ann Glob Health. 2018;84:170-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Spence JP, Buddenbaum JL, Bice PJ, Welch JL, Carroll AE. Independent investigator incubator (I3): a comprehensive mentorship program to jumpstart productive research careers for junior faculty. BMC Med Educ. 2018;18:186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Sambunjak D, Straus SE, Marušić A. Mentoring in academic medicine: a systematic review. JAMA. 2006;296:1103-1115. [DOI] [PubMed] [Google Scholar]
- 146. Ramani S. Twelve tips to promote excellence in medical teaching. Med Teach. 2006;28:19-23. [DOI] [PubMed] [Google Scholar]
- 147. Dimitriadis K, von der Borch P, Störmann S, et al. Characteristics of mentoring relationships formed by medical students and faculty. Med Educ. 2012;17:17242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Kukreja S, Chhabra N, Kaur A, Arora R, Singh T. Introducing mentoring to 1st-year medical students of a private medical college in North India: A pilot study. Int J Appl Basic Med Res. 2017;7(Suppl 1):S67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Hawkins A, Jones K, Stanton A. A mentorship programme for final-year students. Clin Teach. 2014;11:345-349. [DOI] [PubMed] [Google Scholar]
- 150. Kalén S, Stenfors-Hayes T, Hylin U, Larm MF, Hindbeck H, Ponzer S. Mentoring medical students during clinical courses: a way to enhance professional development. Med Teach. 2010;32:e315-e321. [DOI] [PubMed] [Google Scholar]
- 151. Zuzuárregui JRP, Hohler AD. Comprehensive Opportunities for Research and Teaching Experience (CORTEX): a mentorship program. Neurology. 2015;84:2372-2376. [DOI] [PubMed] [Google Scholar]
- 152. Goldszmidt MA, Zibrowski EM, Watling CJ. Fostering education scholarship: the mentored research group. Med Educ. 2009;43:1084-1085. [DOI] [PubMed] [Google Scholar]
- 153. Kwan JY, Prokubovskaya A, Hopman WM, Carpenter J. Mentoring for female medical trainees in a dual-setting group. Med Educ. 2015;49:540-540. [DOI] [PubMed] [Google Scholar]
- 154. Sakushima K, Mishina H, Fukuhara S, et al. Mentoring the next generation of physician-scientists in Japan: a cross-sectional survey of mentees in six academic medical centers. BMC Med Educ. 2015;15:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Ho Y, Kwon OY, Park SY, Yoon TY. A study of satisfaction of medical students on their mentoring programs at one medical school in Korea. Korean J Med Educ. 2017;29:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Sayan M, Ohri N, Lee A, et al. The Impact of Formal Mentorship Programs on Mentorship Experience Among Radiation Oncology Residents From the Northeast. Front Oncol. 2019;9:1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5:371-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_material for The Pivotal Role of Host Organizations in Enhancing Mentoring in Internal Medicine: A Scoping Review by Elisha Wan Ying Chia, Kuang Teck Tay, Shiwei Xiao, Yao Hao Teo, Yun Ting Ong, Min Chiam, Ying Pin Toh, Stephen Mason, Annelissa Mien Chew Chin and Lalit Kumar Radha Krishna in Journal of Medical Education and Curricular Development