Abstract
BACKGROUND/OBJECTIVES
To determine racial/ethnic disparities in weekly counts of new COVID‐19 cases and deaths among nursing home residents or staff.
DESIGN
Cross‐sectional analysis of national nursing home COVID‐19 reports linked to other data. Multivariable two‐part models modeled disparities in count of cases or deaths, and logistic regressions modeled disparities in self‐reported shortages in staff and personal protective equipment (PPE), across nursing home groups with varying proportions of racial/ethnic minority residents, defined as low‐, medium‐, medium‐high–, and high‐proportion groups.
SETTING
A total of 12,576 nursing homes nationally.
PARTICIPANTS
None.
INTERVENTION
None.
MEASUREMENTS
Numbers of incident COVID‐19 confirmed cases among residents and staff, and incident COVID‐19 related deaths among residents (primary outcomes); and nursing home reported shortages in staff and PPE (secondary outcomes). All outcomes were reported for the week of May 25, 2020.
RESULTS
The number of weekly new COVID‐19 confirmed cases among residents ranged from an average of 0.4 cases per facility (standard deviation (SD) = 2.5) for the low‐proportion group (93.0% had zero new cases) to 1.5 cases per facility (SD = 6.3) for the high‐proportion group (78.9% had zero new cases). Multivariable regression estimated that compared with the low‐proportion group, the likelihood of having at least one new resident case was 76% higher (odds ratio = 1.76; 95% confidence interval = 1.38–2.25; P = .000) for the high‐proportion group. Similar across‐facility disparities were found for the weekly count of new COVID‐19 deaths among residents (ranging from 0.1 deaths per facility (SD = 1.1) for the low‐proportion group to 0.4 deaths (SD = 2.0) for the high‐proportion group) and in the weekly count of new COVID‐19 confirmed cases among staff (ranging from 0.3 cases (SD = 1.4] to 1.3 cases (SD = 4.4) per facility). No substantial disparities in self‐reported shortages of staff or PPE were found.
CONCLUSION
Nursing homes caring for disproportionately more racial/ethnic minority residents reported more weekly new COVID‐19 confirmed cases and/or deaths. Immediate actions are needed to address these system‐level disparities.
Keywords: COVID‐19, coronavirus, nursing home, race and ethnicity, disparity
INTRODUCTION
Since the first confirmed case of COVID‐19 among nursing home residents was identified in Seattle, WA, on February 28, 2020, 1 the novel coronavirus has spread rapidly in nursing homes and other long‐term care (LTC) facilities across almost all states in the United States. By July 9, 2020, 11,644 LTC facilities in 44 states (among 47 reporting states) reported a total of 283,973 cases and 56,143 COVID‐19 related deaths; nationally, 12% of all COVID‐19 cases, and 44% of all COVID‐19 deaths, occurred in LTC facilities. 2
In addition to disproportionately affecting older adults and persons with select underlying health conditions, COVID‐19 is found to have higher contraction rates and worse outcomes, including mortality, among racial/ethnic minorities. 3 , 4 , 5 , 6 , 7 For example, a recent study analyzed the electronic health records of 1,052 COVID‐19 confirmed cases in a large healthcare system in California and found that African Americans were 2.7 times as likely as non‐Hispanic Whites to be hospitalized, even after adjustment for age, sex, comorbidities, and income. 3
Racial/ethnic disparities in nursing home care, including outcomes for pneumonia and other infectious diseases, have been widely documented. 8 , 9 , 10 , 11 , 12 Convincing evidence also indicates that these widespread disparities largely exist across nursing homes, and racial/ethnic minority residents tend to be cared for in facilities with limited financial and clinical resources, inadequate nursing staff, and more care deficiencies. 11 , 12 , 13 These healthcare system–level disparities have persisted over time despite increasing state oversight of nursing homes and widely implemented quality improvement initiatives in recent decades. 11 , 12 , 13 , 14 , 15
Preliminary data from individual states suggest that similar to what was found in the general population, racial/ethnic minority nursing home residents bear a higher burden of COVID‐19 infections than non‐Hispanic White residents. 16 , 17 , 18 , 19 , 20 , 21 , 22 Our study of nursing homes in Connecticut reported more confirmed cases and deaths in facilities more predominated by racial/ethnic minority residents. 16 However, the findings were not definite due to lack of statistical significance. Moreover, none of previous nursing home studies was primarily designed to determine racial/ethnic disparities in COVID‐19 outcomes.
This study evaluated variations in the weekly numbers of new COVID‐19 cases and deaths in nursing homes, as reported by the Centers for Medicare & Medicaid Services (CMS) nationally, focusing on disparities between nursing homes with higher proportions of racial/ethnic minority residents and those with lower proportions. We further explored the potential disparities in self‐reported shortages of staff and personal protective equipment (PPE) across nursing homes.
METHODS
Data Sources
We analyzed CMSʼ Nursing Home COVID‐19 Public File for the data collection week of May 25 (through Sunday, May 31; available at https://data.cms.gov/stories/s/COVID-19-Nursing-Home-Data/bkwz-xpvg). Key data elements in the publicly available file include weekly counts of incident COVID‐19 cases and deaths among nursing home residents and staff separately, as well as facility capacity, staff, and supplies of PPE, as reported by individual nursing homes through the Center for Disease Control and Prevention's (CDCʼs) National Healthcare Safety Network system (COVID‐19 LTC Facility Module). This file is updated weekly, and the initial data reported are for the week ending on May 24. However, per CMSʼ instructions, numbers reported for that week may include both new cases (or deaths) in the week and cases (or deaths) identified before that week, which makes the data inappropriate for analyses due to unknown starting dates of reporting for individual nursing homes. For subsequent weeks, nursing homes reported only new cases and deaths identified in each reporting week. Thus, the data used in this study are the first available weekly incidence counts for all reporting nursing homes nationally. CMS and CDC performed data quality checks to ensure the accuracy of the reported numbers.
We linked the COVID‐19 incidence data to several other databases that included (1) the Nursing Home Compare (NHC) data files (updated on March 31, 2020) that CMS publishes and regularly updates to track nurse home organizational, staffing, and quality of care 23 ; (2) the LTCFocus file created by the Brown University for additional nursing home characteristics; (3) the Area Healthcare Resource File (https://data.hrsa.gov/topics/health-workforce/ahrf) for key county characteristics; and (4) the numbers of laboratory‐confirmed COVID‐19 cases and deaths in all counties in the United States, as published by the New York Times (https://github.com/nytimes/covid-19-data). These numbers have been compiled and updated in real time by the New York Times based on reports from state and local health agencies since the first reported coronavirus case in Snohomish County, Washington, on January 20, 2020. 24
Variables
Our primary outcomes of interest included numbers of COVID‐19 (1) laboratory‐confirmed new cases among residents; (2) new deaths among residents; and (3) confirmed new cases among staff for the reporting week (May 25–May 31). The secondary outcomes included a set of binary indicators that separately defined whether during the reporting week, the nursing home had a shortage of licensed nurses (registered nurses (RNs), licensed practical nurses (LPNs), or licensed vocational nurses (LVNs)); aides (nursing assistants, nurse aides, medication aides, or medication technicians); clinical staff (physicians or nurse practitioners/physician assistants); other staff; any of the above staff; N95 masks; surgical masks; face shields and goggles; gowns; gloves; any of the above PPE; and alcohol‐based hand sanitizer. The indicators defining shortages of individual PPE items and hand sanitizer were derived from the questions asking “if [the] facility has enough supply of [a PPE item] for one week” and were coded as 0 for an answer of “yes” and 1 for “no” (i.e., indicating a shortage).
The independent variable was percentage of racial/ethnic minority residents (African Americans, Hispanics, Asians or Pacific Islanders, and American Indians or Alaskan Natives) in the nursing home (obtained from the LTCFocus file), which was originally defined using the race and ethnicity information in the Minimum Data Set and Medicare enrollment databases. Our preliminary analyses suggested nonlinear associations of facility‐level racial/ethnic composition with focused outcomes. Thus, similar to previous studies, 14 , 15 , 16 we categorized nursing homes into quartiles to capture such nonlinear associations: nursing homes with low proportions of racial/ethnic minority residents (<2.92%, the 25th percentile), medium proportions (2.92%–11.11%, the median), medium‐high proportions (11.11%–30.18%), and high proportions (≥30.18%, the 75th percentile).
From the NHC files, we obtained a set of nursing home covariates that were found important to COVID‐19 infections or deaths, 16 , 17 , 18 , 19 including number of beds, average daily resident census, ownership status (for profit, nonprofit, or government owned), chain affiliation (yes/no), whether the nursing home is affiliated with a hospital, percentage of Medicare residents, percentage of Medicaid residents, average staffing levels (hours per resident day) for RN and for all nursing staff (including RNs, LPNs/LVNs, and certified nursing assistants) in 2019, and five‐star ratings for overall quality of care. RN and other nurse staffing levels were calculated based on daily resident census and CMS Payroll‐Based Journal system through which nursing homes electronically submit the number of hours that agency and contract staff are paid to work each day; the payroll‐based data are submitted quarterly and audited by CMS to ensure accuracy. 25 The five‐star ratings aggregate ratings of nursing home quality measures belonging to three domains—deficiency citations assigned during on‐site inspections, care processes and outcomes of residents, and nurse staffing to resident ratios—into a rating system of one to five stars, with more stars indicating better quality. 26 We further obtained a variable for facility‐level case mix from the LTCFocus file, which was calculated by averaging the acuity scores of all residents in the facility, with higher value indicating greater average acuity.
County‐level covariates included the total number of COVID‐19 confirmed cases as of May 31, 2020, less nursing home confirmed cases; the total number of COVID‐19 deaths as of May 31 in the county, less nursing home deaths; and several common county sociodemographic characteristics, including population size, percentage of older population (aged ≥65 years), median household income, percentage of population with high school education, and a measure of the degree to which each nursing home competes for patients with other nursing homes in the county. 27
Statistical Analyses
We compared differences in COVID‐19 confirmed cases and deaths, as well as other nursing home and county characteristics, by quartile groups based on proportions of racial/ethnic minority residents. Analyses of variance for continuous variables and chi‐square tests for categorical variables were used in statistical inference.
In multivariable analyses of the numbers of new COVID‐19 cases and deaths, we fit separate two‐part models at the nursing home level to account for the fact that a large number of nursing homes had a count of zero cases (or deaths). 28 The first part of the model was a generalized linear model with a logit link function and an assumed binomial distribution, which estimated the likelihood of a nursing home to have at least one new confirmed case (or death) identified in the week. The second part of the two‐part models is a count model that assumed a Poisson distribution and estimated the number of nursing home new cases (or deaths) conditional on at least one new case (or death) confirmed in the reporting week. Both parts of the models had three indicators for medium, medium‐high, and high concentrations of racial/ethnic minority residents as independent variables (each compared with the low concentration group), and controlled for the same nursing home and county covariates (Table 1), as well as indicators for states. After model estimation, we obtained the predicted counts of confirmed cases and deaths for all nursing homes and plotted each predicted count against the independent variables.
Table 1.
Nursing Home and County Characteristics by Nursing Home Quartile Groups of Proportion of Racial/Ethnic Minority Residents
| Nursing home characteristic | All nursing homes (n = 12,576) | Nursing homes by proportion of racial/ethnic minority residents a | |||
|---|---|---|---|---|---|
| Low (<2.92%) (n = 3,143) | Medium (2.92%–11.11%) (n = 3,149) | Medium‐high (11.11%–30.18%) (n = 3,140) | High (≥30.18%) (n = 3,144) | ||
| Racial/ethnic minority residents, % | 19.7 ± 21.7 | 0.8 ± 1.0 | 6.4 ± 2.4 | 19.4 ± 5.4 | 52.1 ± 16.2 |
| Total No. of beds | 108.2 ± 59.2 | 86.3 ± 44.8 | 102.9 ± 54.2 | 116.2 ± 58.8 | 127.3 ± 68.3 |
| No. of residents | 88.9 ± 52.8 | 70.3 ± 39.4 | 83.5 ± 47.7 | 94.4 ± 52.3 | 107.5 ± 61.9 |
| Ownership | |||||
| For profit | 8,861 (70.5) | 1,602 (51.0) | 2,147 (68.2) | 2,453 (78.1) | 2,659 (84.6) |
| Nonprofit | 2,938 (23.4) | 1,266 (40.3) | 799 (25.4) | 527 (16.8) | 346 (11.0) |
| Government owned | 777 (6.2) | 275 (8.8) | 203 (6.5) | 160 (5.1) | 139 (4.4) |
| Chain affiliated | 7,490 (59.6) | 1,659 (52.8) | 1,921 (61.0) | 1,980 (63.1) | 1,930 (61.4) |
| Hospital affiliated | 398 (3.2) | 164 (5.2) | 84 (2.7) | 70 (2.2) | 80 (2.5) |
| Medicaid residents, % | 60.1 ± 22.1 | 52.1 ± 22.4 | 56.9 ± 22.2 | 62.6 ± 20.3 | 69.0 ± 19.7 |
| Medicare residents, % | 13.4 ± 12.0 | 12.7 ± 12.2 | 14.7 ± 13.1 | 14.4 ± 12.3 | 11.9 ± 9.9 |
| Case mix index score | 1.3 ± 0.1 | 1.3 ± 0.1 | 1.3 ± 0.1 | 1.3 ± 0.1 | 1.3 ± 0.2 |
| RN hours per resident day | 0.7 ± 0.4 | 0.8 ± 0.4 | 0.7 ± 0.4 | 0.6 ± 0.4 | 0.5 ± 0.3 |
| Total nurse hours per resident day | 3.8 ± 0.8 | 4.0 ± 0.8 | 3.8 ± 0.8 | 3.7 ± 0.7 | 3.7 ± 0.8 |
| Overall five‐star rating | 3.1 ± 1.4 | 3.6 ± 1.3 | 3.2 ± 1.4 | 2.9 ± 1.4 | 2.7 ± 1.4 |
| County characteristic | |||||
| Total No. of COVID‐19 cases as of May 31, ×1,000 | 5.0 ± 14.3 | 1.7 ± 6.7 | 2.9 ± 8.1 | 4.7 ± 11.9 | 11.1 ± 22.8 |
| Total No. of COVID‐19 deaths as of May 31, ×1,000 | 0.3 ± 0.9 | 0.1 ± 0.4 | 0.2 ± 0.4 | 0.3 ± 0.7 | 0.6 ± 1.6 |
| Total population × 100,000 | 7.7 ± 16.8 | 2.4 ± 6.5 | 4.0 ± 8.0 | 7.2 ± 13.2 | 17.2 ± 26.7 |
| Population aged ≥65 y, % | 16.9 ± 4.0 | 18.6 ± 3.8 | 17.7 ± 4.1 | 16.4 ± 4.0 | 14.9 ± 3.1 |
| Medium household income ×$1,000 | 56.4 ± 15.0 | 54.3 ± 12.4 | 56.2 ± 14.4 | 57.7 ± 15.7 | 57.4 ± 16.7 |
| Population with high school graduation, % | 87.5 ± 5.3 | 89.3 ± 4.4 | 88.7 ± 4.6 | 87.4 ± 5.1 | 84.9 ± 5.7 |
| Market competition for nursing home care | 78.9 ± 24.8 | 71.0 ± 26.3 | 77.3 ± 24.3 | 82.2 ± 22.8 | 85.3 ± 23.0 |
Note: Data are given as mean ± standard deviation or number (percentage).
Abbreviation: RN, registered nurse.
All P values were <.001 for comparisons of group differences based on analyses of variance for continuous variables and chi‐square tests for categorical variables.
In multivariable analyses of shortages of staff, PPE, and alcohol‐based hand sanitizer, we fit separate logistic models at the nursing home level, in which the independent variables and covariates were specified in the same way. All two‐part and logistic regression models used robust variance‐covariance estimates to account for the clustering of nursing homes within counties. 29 Statistical analyses were performed with Stata®/MP, version 16.1. The research subjects review board at the University of Rochester Medical Center approved this study.
RESULTS
From a total of 15,857 nursing homes nationally, we identified 14,333 nursing homes that submitted the COVID‐19 data for the week ending May 31. Our study sample contained 12,576 nursing homes after excluding facilities that did not pass CMSʼ quality assurance check for submitted data (n = 432), or had missing data on the composition of racial/ethnic minority residents (n = 1,325). Supplementary Table S1 shows that compared with other nursing homes, nursing homes included in the sample were somewhat more likely to be nonprofit (n = 2,938 (23.4%] vs n = 657 (20.0%)), affiliated with a chain (n = 7,490 (59.6%) vs 1,221 (51.3%)), but not affiliated with a hospital (n = 12,178 (96.8%) vs 3,044 (91.5%)). They also tended to be larger facilities (mean bed size = 108 vs 92) with lower proportions of racial/ethnic minorities (19.7% vs 22.8%) and Medicare residents (13.4% vs 16.7%), and lower nurse staffing levels (3.8 vs 4.1 hours per resident day). They tended to be located in counties with fewer COVID‐19 cases (5,000 vs 7,800) and deaths (300 vs 400) as well.
Table 1 shows that among nursing homes in the study sample, those with higher proportions of racial/ethnic minority residents tended to be larger for‐profit facilities affiliated with a chain, and to have more Medicaid residents and lower RN and total nurse staffing hours. Nursing homes more predominated by racial/ethnic minority residents also tended to be located in counties with more COVID‐19 cases and deaths as of May 31, counties of lower socioeconomic status, and counties with higher competition for nursing home care.
The number of weekly new COVID‐19 confirmed cases among residents increased with higher nursing home proportion of racial/ethnic minorities (Table 2), from an average of 0.4 cases per facility (standard deviation (SD) = 2.5) for the low‐proportion group (93.0% of which had zero new cases) to 1.5 cases per facility (SD = 6.3) for the highest‐proportion group (78.9% had zero new cases). Multivariable two‐part model confirmed these bivariate trends. After controlling for nursing home, county, and state covariates, and compared with nursing homes in the low‐proportion group, the likelihoods of having at least one new resident case (the first part of the model) were 25% higher (odds ratio (OR) = 1.25; 95% confidence interval (CI) = 1.03–1.51; P = .025) for the medium‐proportion group, 44% higher (OR = 1.44; 95% CI = 1.14–1.82; P = .002) for the medium‐high–proportion group, and 76% higher (OR = 1.76; 95% CI = 1.38–2.25; P = .000) for the high‐proportion group. The second part of the two‐part model showed that conditional on having at least one new case, nursing home concentrations of racial/ethnic minority residents were not significantly associated with the count of new cases (Supplementary Table S2). Figure 1A presents the predicted number of new resident cases from the two‐part model, for all nursing homes (with zero or a positive count) and by quartile groups, which indicates a statistically significant trend in increased count as the proportion of racial/ethnic minority residents in nursing home increases.
Table 2.
Numbers of Incident Laboratory‐Confirmed COVID‐19 Cases and Deaths Reported in U.S. Nursing Homes During the Week of May 25, 2020 (May 25–May 31)
| Variable | All nursing homes (n = 12,576) | Nursing homes by proportion of racial/ethnic minority residents a | |||
|---|---|---|---|---|---|
| Low (<2.92%) (n = 3,143) | Medium (2.92%–11.11%) (n = 3,149) | Medium‐high (11.11%–30.18%) (n = 3,140) | High (≥30.18%) (n = 3,144) | ||
| No. of new COVID‐19 confirmed cases among residents | 0.9 ± 4.7 | 0.4 ± 2.5 | 0.7 ± 4.0 | 0.9 ± 5.2 | 1.5 ± 6.3 |
| 0 | 10,855 (86.3) | 2,922 (93.0) | 2,793 (88.7) | 2,659 (84.7) | 2,481 (78.9) |
| 1–10 | 1,453 (11.6) | 194 (6.2) | 303 (9.6) | 412 (13.1) | 544 (17.3) |
| 11–20 | 159 (1.3) | 14 (0.5) | 32 (1.0) | 47 (1.5) | 66 (2.1) |
| >20 | 109 (0.9) | 13 (0.4) | 21 (0.7) | 22 (0.7) | 53 (1.7) |
| No. of new COVID‐19 related deaths among residents | 0.3 ± 1.5 | 0.1 ± 1.1 | 0.3 ± 1.5 | 0.3 ± 1.2 | 0.4 ± 2.0 |
| 0 | 11,310 (89.9) | 2,975 (94.7) | 2,863 (90.9) | 2,778 (88.5) | 2,694 (85.7) |
| 1–5 | 1,145 (9.1) | 153 (4.9) | 248 (7.9) | 334 (10.6) | 410 (13.0) |
| >5 | 121 (1.0) | 15 (0.5) | 38 (1.2) | 28 (0.9) | 40 (1.3) |
| No. of new COVID‐19 confirmed cases among staff | 0.7 ± 3.0 | 0.3 ± 1.4 | 0.6 ± 2.4 | 0.8 ± 2.8 | 1.3 ± 4.4 |
| 0 | 10,375 (82.5) | 2,814 (89.5) | 2,676 (85.0) | 2,530 (80.6) | 2,355 (74.9) |
| 1–10 | 2,010 (16.0) | 318 (10.1) | 441 (14.0) | 557 (17.7) | 694 (22.1) |
| 11–20 | 123 (1.0) | 9 (0.3) | 22 (0.7) | 37 (1.2) | 55 (1.8) |
| >20 | 68 (0.5) | 2 (0.1) | 10 (0.3) | 16 (0.5) | 40 (1.3) |
Note: Data are given as mean ± standard deviation or number (percentage).
All P values were <.001 for comparisons of group differences based on analyses of variance for continuous variables and chi‐square tests for categorical variables.
Figure 1.
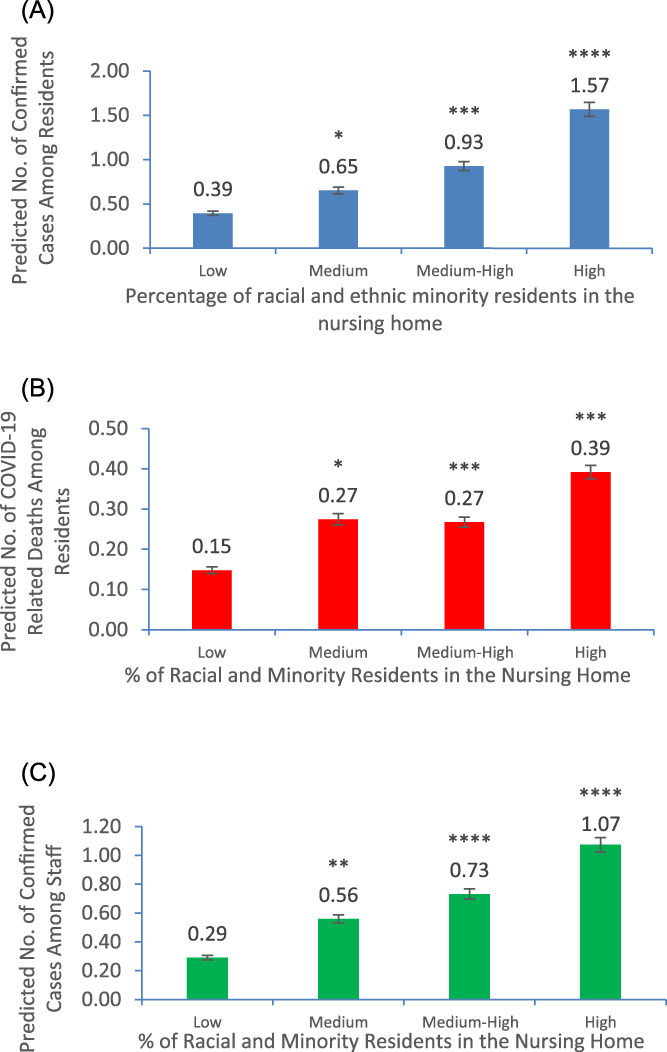
Predicted numbers of weekly new laboratory‐confirmed COVID‐19 cases among residents (A), new COVID‐19 related deaths among residents (B), and new laboratory‐confirmed COVID‐19 cases among staff (C), reported in U.S. nursing homes for the week of May 25, 2020 (Monday, May 25, to Sunday, May 31) and by nursing home groups with different percentages of racial and ethnic minority residents. Note: *P < .10, **P < .05, ***P < .01, ****P < .001. P values indicate the statistical significance of differences in predicted numbers between the “medium,” “medium‐high,” or “high” group and the “low” group, and were derived from the joint tests of the two‐part regression models. The two‐part models were used to derive the predicted numbers and 95% confidence intervals (error bars in each figure). All two‐part models adjusted for nursing home and county characteristics listed in Table 1, indicators for states, and the clustering of nursing homes within counties.
Table 2 further reveals increasing trends in weekly new COVID‐19 deaths among residents (e.g., from an average of 0.1 deaths per facility for the low‐proportion group to 0.4 deaths for the high‐proportion group), and in weekly new COVID‐19 confirmed cases among staff (e.g., from an average of 0.3 cases per facility for the low‐proportion group to 1.3 cases for the high‐proportion group) as nursing home proportion of racial/ethnic minority residents increases. These bivariate trends were similarly confirmed in multivariable analyses, as shown in Supplementary Tables S3 and S4, and as illustrated in Figure 1B,C.
In our study sample, 12,515 nursing homes (99.5%) had zero new COVID‐19 deaths among staff and the other 61 nursing homes had one to four staff deaths, resulting in an overall average count of 0.006. We did not run bivariate or multivariable analyses on staff new deaths given this extremely low count.
Table 3 shows results of the bivariate and multivariable (or adjusted) differences in self‐reported shortages of staff, PPE, and alcohol‐based hand sanitizer for the reporting week. Although it seems that nursing homes with higher proportions of racial/ethnic minorities were more likely to report shortage of aides (16.9% for the low‐proportion group, and 18.5% for the high‐proportion group with adjusted OR = 1.24; 95% CI = 1.02–1.50; P < .05), no clear patterns were found for shortages of other staff, PPE, or hand sanitizer, even though some of the adjusted analyses suggested statistically significant associations.
Table 3.
Rates of Nursing Home Self‐Reported Shortages of Staff, Personal Protective Equipment, and Hand Sanitizer During the Week of May 25, 2020 (May 25–May 31)
| Variable | All nursing homes (n = 12,576) | Nursing homes by concentration of racial/ethnic minority residents | |||
|---|---|---|---|---|---|
| Low (<2.92%) (n = 3,143) | Medium (2.92%–11.11%) (n = 3,149) | Medium‐high (11.11%–30.18%) (n = 3,140) | High (≥30.18%) (n = 3,144) | ||
| Shortage of any staff | |||||
| Unadjusted rate, % | 21.8 | 21.1 | 22.5 | 21.8 | 21.9 |
| Adjusted OR (95% CI) | Reference | 1.15 (1.01–1.31)** | 1.16 (0.99–1.35)* | 1.25 (1.04–1.49)** | |
| Shortage of licensed nurses (RNs, LPNs, or LVNs) | |||||
| Unadjusted rate, % | 15.6 | 15.1 | 15.7 | 15.8 | 15.7 |
| Adjusted OR (95% CI) | Reference | 1.09 (0.94–1.27) | 1.16 (0.98–1.39)* | 1.23 (1.02–1.49)** | |
| Shortage of aides (nursing assistants, nurse aides, medication aides, or medication technicians) | |||||
| Unadjusted rate, % | 18.0 | 16.9 | 18.2 | 18.3 | 18.5 |
| Adjusted OR (95% CI) | Reference | 1.11 (0.96–1.28) | 1.14 (0.96–1.36) | 1.24 (1.02–1.50)** | |
| Shortage of clinical staff (physicians or NPs/PAs) | |||||
| Unadjusted rate, % | 2.5 | 2.4 | 2.4 | 2.9 | 2.3 |
| Adjusted OR (95% CI) | Reference | 0.99 (0.68–1.44) | 1.18 (0.79–1.77) | 1.05 (0.67–1.63) | |
| Shortage of other staff | |||||
| Unadjusted rate, % | 9.4 | 9.4 | 10.1 | 9.3 | 8.6 |
| Adjusted OR (95% CI) | Reference | 1.19 (0.99–1.42)* | 1.18 (0.95–1.46) | 1.19 (0.93–1.53) | |
| Shortage of any PPE (defined below) | |||||
| Unadjusted rate, % | 25.2 | 24.8 | 24.6 | 25.1 | 26.4 |
| Adjusted OR (95% CI) | Reference | 0.95 (0.83–1.08) | 0.94 (0.81–1.09) | 0.93 (0.78–1.09) | |
| Shortage of PPE: N95 masks | |||||
| Unadjusted rate, % | 16.0 | 15.3 | 15.3 | 16.0 | 17.4 |
| Adjusted OR (95% CI) | Reference | 0.91 (0.78–1.06) | 0.88 (0.74–1.04) | 0.92 (0.75–1.13) | |
| Shortage of PPE: surgical masks | |||||
| Unadjusted rate, % | 8.5 | 8.6 | 7.9 | 8.3 | 9.3 |
| Adjusted OR (95% CI) | Reference | 0.84 (0.69–1.01)* | 0.85 (0.68–1.06) | 0.86 (0.68–1.11) | |
| Shortage of PPE: face shields and goggles | |||||
| Unadjusted rate, % | 8.5 | 7.8 | 7.9 | 8.6 | 9.8 |
| Adjusted OR (95% CI) | Reference | 0.89 (0.71–1.10) | 0.88 (0.70–1.09) | 0.85 (0.66–1.10) | |
| Shortage of PPE: gowns | |||||
| Unadjusted rate, % | 18.4 | 17.1 | 18.7 | 18.2 | 19.5 |
| Adjusted OR (95% CI) | Reference | 1.04 (0.90–1.21) | 0.96 (0.81–1.14) | 0.96 (0.80–1.16) | |
| Shortage of PPE: gloves | |||||
| Unadjusted rate, % | 5.4 | 4.0 | 4.3 | 5.4 | 7.7 |
| Adjusted OR (95% CI) | Reference | 0.82 (0.63–1.05) | 0.79 (0.60–1.03)* | 0.82 (0.61–1.10) | |
| Shortage of alcohol‐based hand sanitizer | |||||
| Unadjusted rate, % | 6.7 | 4.9 | 5.6 | 6.9 | 9.6 |
| Adjusted OR (95% CI) | Reference | 0.94 (0.74–1.21) | 0.97 (0.75–1.25) | 1.00 (0.75–1.33) | |
Note: Logistic regression models adjusted for nursing home and county characteristics listed in Table 1, indicators for states, and the clustering of nursing homes within counties.
Abbreviations: CI, confidence interval; LPN, licensed practical nurse; LVN, licensed vocational nurse; NP/PA, nurse practitioner/physician assistant; OR, odds ratio; PPE, personal protective equipment; RN, registered nurse.
*P < .10, ** P < .05, *** P < .01, and **** P < .01 when compared with the group of nursing homes with low concentrations of racial and ethnic minority residents.
DISCUSSION
This national study reveals that nursing homes caring for disproportionately more racial/ethnic minority residents tended to have more new COVID‐19 confirmed cases among their residents and staff, and more new COVID‐19 related deaths among residents (all reported for the week of May 25–May 31). These disparities across nursing homes persisted after adjustment for important nursing home, county, and state covariates, with predicted counts of cases and deaths per facility being two to four times as high in nursing homes with highest proportions of racial/ethnic minority residents as in nursing homes with low proportions. Meanwhile, although 22% of all nursing homes reported shortage of staff and 25% reported shortage of PPE for the reporting week, we did not find evidence of dramatic disparities in these self‐reported shortages across nursing homes.
The disparities in rates of COVID‐19 cases and deaths mirrored the system‐wide disparities reported before, in which nursing homes with lower resources and higher concentrations of racial/ethnic minorities have poorer outcomes. 11 , 12 , 13 Moreover, the nursing home literature in the past several decades indicates that nursing homes remain highly segregated, and racial/ethnic minority residents tend to be cared for in a small number of facilities located in communities of color with poorest quality of care and highly restricted resources. 13 , 30 , 31 , 32 Mor et al reported that nationally, 40% of Black residents, compared with 9% of White residents, resided in these “lower‐tier” nursing homes. 13 Thus, racial/ethnic disparities in nursing home outcomes are not due to race, but to fundamental inequalities inherent in the healthcare and nonhealthcare sectors that lead to worse health outcomes for racial/ethnic minority residents.
Our findings of disparities in COVID‐19 related outcomes bring to light this long‐standing issue of segregation in nursing home care. In addition, the magnitude of the estimated disparities—twofold to fourfold differences in infection and fatality counts across facilities—suggests that these institutional disparities are likely playing out in an exacerbated way under the coronavirus pandemic.
Although analyses in the study did not find substantial cross‐facility differences in self‐reported shortages of staff and PPE in the last week of May, it is likely that nursing homes predominated by racial/ethnic minority residents face more of other institution‐wide issues, such as poor testing capacity, and inadequate staff knowledge and training in infection control and prevention, that lead to worse COVID‐19 related outcomes for their residents and staff. In the future, the CMS COVID‐19 public reporting for nursing homes could be expanded to incorporate data collection for these more nuanced items, which would allow for a better understanding of, and potential solutions to, institutional disparities.
Our multivariable analyses and analyses in previous studies suggest that nursing home COVID‐19 transmission rates tend to be correlated with county prevalence rates. 16 , 22 However, our findings that disparities in nursing home COVID‐19 cases and deaths persisted after controlling for county‐level rates suggest that such disparities may be related to community‐level factors in a more profound way. For example, nursing homes predominated by racial/ethnic minority residents tend to be located in communities of color, where hospitals and other acute care sectors may be more overwhelmed by COVID‐19 outbreaks, which leads to delays in emergent and nonemergent medical care for symptomatic patients, and to heightened death tolls among nursing home residents. Moreover, nursing home staff from these communities, especially staff of color who make up over 50% of nursing home direct care workforce, 33 are more likely to live in crowded households and neighborhoods, travel to and from work by public transportation, and be low paid with few or no benefits, such as paid sick leave, all placing them at higher risks of COVID‐19 infection as well as inadvertent cross‐infection with residents. 34
The vulnerability of nursing home residents at large to previous respiratory disease outbreaks, 35 , 36 and to the current COVID‐19 pandemic, 1 , 2 is well documented thus far. However, the racial/ethnic disparities in COVID‐19 related morbidity and mortality found in this study, although perhaps not surprising, are rather disturbing given the fact that these disparities are largely traceable to systemic inequalities and discriminations prevailing in health care and society at large. Action is needed to ensure equal access to the prevention, testing, and treatment of COVID‐19 for all nursing home residents and staff, regardless of their race or ethnicity and where they reside. The recent Paycheck Protection Program and Health Care Enhancement Act, signed into law on April 24, 2020, requires the Department of Health and Human Services to report COVID‐19 data by race/ethnicity and to develop a strategic testing plan to address disparities in all communities. 37 The across‐facility disparities in COVID‐19 infection and death rates found in this study indicate that although all nursing homes may need help to mitigate the spread of the virus, immediate actions are needed to ensure that as the pandemic continues to evolve, 38 racial/ethnic minority nursing home residents, and the frontline workers caring for them, do not bear an additional layer of sufferings due to systemic inequalities. There is no doubt that addressing deep‐rooted health inequalities should comprise an essential part of efforts in this nationʼs current and future responses to the pandemic.
This study has several limitations. First, our study sample comprised 12,576 nursing homes with complete data. Although they constitute about 80% of all nursing homes nationally, their characteristics differ somewhat from those of excluded facilities, and results of this study should be interpreted with this caution in mind. Second, the cross‐sectional design of this study allows for estimation of associations only, which may be confounded by unmeasured nursing home or community covariates. Finally, this national study does not allow for a root‐cause analysis of the factors that may specifically underlie the across‐facility disparities we found. Future research in this line is needed to better inform efforts to rectify such disparities.
In conclusion, nursing homes caring for disproportionately more racial/ethnic minority residents tended to have more incident COVID‐19 confirmed cases among their residents and staff, and more incident COVID‐19 related deaths among residents. Immediate actions are needed to address these system‐level disparities.
Supporting information
Supplementary Table S1: Characteristics of Nursing Homes Included in Our Study Sample (n = 12,576) and Nursing Homes Excluded from the Study (n = 3,281)*.
Supplementary Table S2: Full Model Results: Two‐Part Model for Weekly Number of New COVID‐19 Confirmed Cases Among Nursing Home Residents.
Supplementary Table S3: Full Model Results: Two‐Part Model for Weekly Number of New COVID‐19 Related Deaths Among Nursing Home Residents.
Supplementary Table S4: Full Model Results: Two‐Part Model for Weekly Number of New COVID‐19 Confirmed Cases Among Nursing Home Staff.
ACKNOWLEDGMENTS
Financial Disclosure
The research of the authors was funded by National Institute of Health Grant R01MH117528 and Agency for Healthcare Research and Quality Grants R01HS026893 and R01HS024923.
Conflict of Interest
No conflict of interest for any author.
Author Contributions
Y.L., X.C., X.C., and H.T.‐G.: conception and design, acquisition of data, analysis and interpretation of data, critical revision for important intellectual content, and final approval of the version to be published. Y.L.: drafting of article.
Sponsorʼs Role
The views expressed in this article are those of the authors and do not necessarily represent the view of the National Institutes of Health (NIH) or the Agency for Healthcare Research and Quality (AHRQ). The NIH and the AHRQ have no role in study design, data collection, analyses, or interpretation of results.
REFERENCES
- 1. McMichael TM, Currie DW, Clark S, et al. Epidemiology of Covid‐19 in a long‐term care facility in King County, Washington. N Engl J Med. 2020;382:2005‐2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. KFF . State Data and Policy Actions to Address Coronavirus. Kaiser Family Foundation. https://www.kff.org/health-costs/issue-brief/state-data-and-policy-actions-to-address-coronavirus/. Accessed July 17, 2020.
- 3. Azar KMJ, Shen Z, Romanelli RJ, et al. Disparities in outcomes among COVID‐19 patients in a large health care system in California. Health Aff (Millwood). 2020;39(7):1253‐1262. [DOI] [PubMed] [Google Scholar]
- 4. Holtgrave DR, Barranco MA, Tesoriero JM, Blog DS, Rosenberg ES. Assessing racial and ethnic disparities using a COVID‐19 outcomes continuum for New York State. Ann Epidemiol. 2020;48:9‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hooper MW, Nápoles AM, Pérez‐Stable EJ. COVID‐19 and racial/ethnic disparities. JAMA. 2020;323(24):2466‐2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yan BW, Ng F, Chu J, Tsoh J, Nguyen T. Asian Americans facing high COVID‐19 case fatality, Health Affairs Blog, July 13, 2020.
- 7. Wadhera RK, Wadhera P, Gaba P, et al. Variation in COVID‐19 hospitalizations and deaths across New York City boroughs. JAMA. 2020;323:2192‐2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Li Y, Mukamel DB. Racial disparities in receipt of influenza and pneumococcus vaccinations among US nursing‐home residents. Am J Public Health. 2010;100((suppl 1)):S256‐S262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Li Y, Cai X, Glance LG. Disparities in 30‐day rehospitalization rates among Medicare skilled nursing facility residents by race and site of care. Med Care. 2015;53(12):1058‐1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zheng NT, Mukamel DB, Caprio T, Cai S, Temkin‐Greener H. Racial disparities in in‐hospital death and hospice use among nursing home residents at the end of life. Med Care. 2011;49(11):992‐998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Li Y, Yin J, Cai X, Temkin‐Greener J, Mukamel DB. Association of race and sites of care with pressure ulcers in high‐risk nursing home residents. JAMA. 2011;306(2):179‐186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rivera‐Hernandez M, Rahman M, Mor V, Trivedi AN. Racial disparities in readmission rates among patients discharged to skilled nursing facilities. J Am Geriatr Soc. 2019;67(8):1672‐1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82(2):227‐256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Li Y, Harrington C, Mukamel DB, Cen X, Cai X, Temkin‐Greener H. Nurse staffing hours at nursing homes with high concentrations of minority residents, 2001‐11. Health Aff (Millwood). 2015;34(12):2129‐2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Li Y, Harrington C, Temkin‐Greener H, et al. Deficiencies in care at nursing homes and racial/ethnic disparities across homes fell, 2006–11. Health Aff (Millwood). 2015;34(7):1139‐1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Li Y, Temkin‐Greener H, Gao S, Cai X. COVID‐19 infections and deaths among Connecticut nursing home residents: facility correlates. J Am Geriatr Soc. 2020;68(9):1899–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Harrington C, Ross L, Chapman S, Halifax E, Spurlock B, Bakerjian D. Nurse staffing and coronavirus infections in California nursing homes. Policy Polit Nurs Pract. 2020;21(3):174–186. [DOI] [PubMed] [Google Scholar]
- 18. McGregor MJ, Harrington C. COVID‐19 and long‐term care facilities: does ownership matter? CMAJ. 2020;192:E961‐E962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. He M, Li Y, Fang F. Is there a link between nursing home reported quality and COVID‐19 cases? evidence from California skilled nursing facilities. J Am Med Dir Assoc. 2020;21(7):905‐908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Abrams HR, Loomer L, Gandhi A, Grabowski DC. Characteristics of U.S. nursing homes with COVID‐19 cases. J Am Geriatr Soc. 2020;68:1653‐1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gebeloff R, Ivory D, Richtel M, et al. The striking racial divide in how Covid‐19 has hit nursing homes. The New York Times, May 21, 2020. https://www.nytimes.com/article/coronavirus-nursing-homes-racial-disparity.html?smid=em-share. Accessed September 8, 2020.
- 22. White EM, Kosar CM, Feifer RA, et al. Variation in SARS‐CoV‐2 prevalence in U.S. skilled nursing facilities. J Am Geriatr Soc. 2020;68(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Centers for Medicare and Medicaid Services . Nursing Home Compare. https://www.medicare.gov/nursinghomecompare/Data/About.html. Accessed August 18, 2020.
- 24. Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929‐936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Geng F, Stevenson DG, Grabowski DC. Daily nursing home staffing levels highly variable, often below CMS expectations. Health Aff (Millwood). 2019;38(7):1095‐1100. [DOI] [PubMed] [Google Scholar]
- 26. CMS . Design for Nursing Home Compare Five‐Star Quality Rating System, Technical Users' Guide. Centers for Medicare and Medicaid Services; 2018. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/downloads/usersguide.pdf. Accessed August 18, 2020.
- 27. Gruneir A, Lapane KL, Miller SC, Mor V. Long‐term care market competition and nursing home dementia special care units. Med Care. 2007;45(8):739‐745. [DOI] [PubMed] [Google Scholar]
- 28. Cameron AC, Trivedi PK. Regression Analysis of Count Data. 2nd ed. Cambridge, England: Cambridge University Press; 2013. [Google Scholar]
- 29. White H. A heteroskedasticity‐consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817‐830. [Google Scholar]
- 30. Smith DB, Feng Z, Fennell ML, Zinn J, Mor V. Racial disparities in access to long‐term care: the illusive pursuit of equity. J Health Polit Policy Law. 2008;33(5):861‐881. [DOI] [PubMed] [Google Scholar]
- 31. Smith DB, Feng Z, Fennell ML, Zinn JS, Mor V. Separate and unequal: racial segregation and disparities in quality across U.S. nursing homes. Health Aff (Millwood). 2007;26(5):1448‐1458. [DOI] [PubMed] [Google Scholar]
- 32. Fennell ML, Feng Z, Clark MA, Mor V. Elderly Hispanics more likely to reside in poor‐quality nursing homes. Health Aff (Millwood). 2010;29(1):65‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. PHI . Workforce Data Center. Direct care workers by race and ethnicity, 2017. https://phinational.org/policy-research/workforce-data-center/#tab=National+Data&natvar=Race+and+Ethnicity. Accessed August 18, 2020.
- 34. True S, Cubanski J, Garfield R, Rae M, Claxton G, Chidambaram P. COVID‐19 and workers at risk: examining the long‐term care workforce. https://www.kff.org/medicaid/issue‐brief/covid‐19‐and‐workers‐at‐risk‐examining‐the‐long‐term‐care‐workforce/?utm_campaign=KFF‐2020‐Medicaid%26utm_source=hs_email%26utm_medium=email%26utm_content=86855544%26_hsenc=p2ANqtz‐_lP7AwFxEYqlHmG5FM3pOFDsyr4pEhfDoldSbNFOF5tsTktGkIWQ2uExwLMu5pRSa12BxQyThwTWs5ieylTb7fYzFWnA%26_hsmi=86855544. Accessed August 20, 2020.
- 35. Lansbury LE, Brown CS, Nguyen‐Van‐Tam JS. Influenza in long‐term care facilities. Influenza Other Respi Viruses. 2017;11(5):356‐366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hand J, Rose EB, Salinas A, et al. Severe respiratory illness outbreak associated with human coronavirus NL63 in a long‐term care facility. Emerg Infect Dis. 2018;24(10):1964‐1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Congress . H.R.266 ‐ Paycheck Protection Program and Health Care Enhancement Act. 116th Congress (2019–2020). https://www.congress.gov/bill/116th-congress/house-bill/266. Accessed August 18, 2020.
- 38. Chidambaram P. Rising cases in long‐term care facilities are cause for concern. On‐line report of the Kaiser Family Foundation available at https://www.kff.org/coronavirus‐covid‐19/issue‐brief/rising‐cases‐in‐long‐term‐care‐facilities‐are‐cause‐for‐concern/?utm_campaign=KFF‐2020‐Coronavirus&utm_medium=email&_hsmi=91739953&_hsenc=p2ANqtz‐8FI‐8IHaLJ5zamdaofkbr‐UiNjfS13J0rkg6s0tPnfSbZtw8DntAF1LSOUUjrCGuigl8RYJK6NlkmtOcyLu0LFup5wai4PmlDrpbbyKKrAV3s_kpk&utm_content=91739953&utm_source=hs_email. Accessed July 21, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: Characteristics of Nursing Homes Included in Our Study Sample (n = 12,576) and Nursing Homes Excluded from the Study (n = 3,281)*.
Supplementary Table S2: Full Model Results: Two‐Part Model for Weekly Number of New COVID‐19 Confirmed Cases Among Nursing Home Residents.
Supplementary Table S3: Full Model Results: Two‐Part Model for Weekly Number of New COVID‐19 Related Deaths Among Nursing Home Residents.
Supplementary Table S4: Full Model Results: Two‐Part Model for Weekly Number of New COVID‐19 Confirmed Cases Among Nursing Home Staff.


